Back pain
Of all types of alternative medicine, acupuncture is the one that has received the most approval from regular medicine. The benefit of that is that it’s been tested more thoroughly than most others. The result is now clear. It doesn’t work. See the evidence in Acupuncture is a theatrical placebo.
This blog has documented many cases of misreported tests of acupuncture, often from people have a financial interests in selling it. Perhaps the most egregious spin came from the University of Exeter. It was published in a normal journal, and endorsed by the journal’s editor, despite showing clearly that acupuncture didn’t even have much placebo effect.
Acupuncture got a boost in 2009 from, of all unlikely sources, the National Institute for Health and Care Excellence (NICE). The judgements of NICE and the benefit / cost ratio of treatments are usually very good. But the guidance group that they assembled to judge treatments for low back pain was atypically incompetent when it came to assessment of evidence. They recommended acupuncture as one option. At the time I posted “NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself“. That was soon followed by two more posts:
NICE fiasco, part 2. Rawlins should withdraw guidance and start again“,
and
“The NICE fiasco, Part 3. Too many vested interests, not enough honesty“.
At the time, NICE was being run by Michael Rawlins, an old friend. No doubt he was unaware of the bad guidance until it was too late and he felt obliged to defend it.
Although the 2008 guidance referred only to low back pain, it gave an opening for acupuncturists to penetrate the NHS. Like all quacks, they are experts at bait and switch. The penetration of quackery was exacerbated by the privatisation of physiotherapy services to organisations like Connect Physical Health which have little regard for evidence, but a good eye for sales. If you think that’s an exaggeration, read "Connect Physical Health sells quackery to NHS".
When David Haslam took over the reins at NICE, I was optimistic that the question would be revisited (it turned out that he was aware of this blog). I was not disappointed. This time the guidance group had much more critical members.
The new draft guidance on low back pain was released on 24 March 2016. The final guidance will not appear until September 2016, but last time the final version didn’t differ much from the draft.
Despite modern imaging methods, it still isn’t possible to pinpoint the precise cause of low back pain (LBP) so diagnoses are lumped together as non-specific low back pain (NSLBP).
The summary guidance is explicit.
“1.2.8 Do not offer acupuncture for managing non-specific low back 7 pain with or without sciatica.”
The evidence is summarised section 13.6 of the main report (page 493).There is a long list of other proposed treatments that are not recommended.
Because low back pain is so common, and so difficult to treat, many treatments have been proposed. Many of them, including acupuncture, have proved to be clutching at straws. It’s to the great credit of the new guidance group that they have resisted that temptation.
Among the other "do not offer" treatments are
- imaging (except in specialist setting)
- belts or corsets
- foot orthotics
- acupuncture
- ultrasound
- TENS or PENS
- opioids (for acute or chronic LBP)
- antidepressants (SSRI and others)
- anticonvulsants
- spinal injections
- spinal fusion for NSLBP (except as part of a randomised controlled trial)
- disc replacement
At first sight, the new guidance looks like an excellent clear-out of the myths that surround the treatment of low back pain.
The positive recommendations that are made are all for things that have modest effects (at best). For example “Consider a group exercise programme”, and “Consider manipulation, mobilisation”. The use of there word “consider”, rather than “offer” seems to be NICE-speak -an implicit suggestion that it doesn’t work very well. My only criticism of the report is that it doesn’t say sufficiently bluntly that non-specific low back pain is largely an unsolved problem. Most of what’s seen is probably a result of that most deceptive phenomenon, regression to the mean.
One pain specialist put it to me thus. “Think of the billions spent on back pain research over the years in order to reach the conclusion that nothing much works – shameful really.” Well perhaps not shameful: it isn’t for want of trying. It’s just a very difficult problem. But pretending that there are solutions doesn’t help anyone.
Follow-up
Almost all the revelations about what’s taught on university courses in alternative medicine have come from post-1992 universities. (For readers not in the UK, post-1992 universities are the many new univerities created in 1992, from former polytechnics etc, and Russell group universities are the "top 20" research-intensive universities)
It is true that all the undergraduate courses are in post-1992 universities, but the advance of quackademia is by no means limited to them. The teaching at St Bartholomew’s Hospital Medical School, one of the oldest, was pretty disgraceful for example, though after protests from their own students, and from me, it is now better, I believe.

Quackery creeps into all universities to varying extents. The good ones (like Southampton) don’t run "BSc" degrees, but it still infiltrates through two main sources,
The first is via their HR departments, which are run by people who tend to be (I quote) "credulous and moronic" when it comes to science.
The other main source is in teaching to medical students. The General Medical Council says that medical students must know something about alterantive medicine and that’s quite right, A lot of their patients will use it. The problem is that the guidance is shockingly vague .
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
In many medical schools, the information that medical students get is quite accurate. At UCL and at King’s (London) I have done some of the familiarisation myself. In other good medical schools, the students get some shocking stuff. St Bartholomew’s Hospital medical School was one example. Edinburgh University was another.
But there is one Russell group university where alternative myths are propagated more than any other that I know about. That is the University of Southampton.
In general, Southampton is a good place, I worked there for three years myself (1972 – 1975). The very first noise spectra I measured were calculated on a PDP computer in their excellent Institute of Sound and Vibration Research, before I wrote my own programs to do it.
But Southanpton also has a The Complementary and Integrated Medicine Research Unit . Oddly the unit’s web site, http://www.cam-research-group.co.uk, is not a university address, and a search of the university’s web site for “Complementary and Integrated Medicine Research Unit” produces no result. Nevertheless the unit is “within the School of Medicine at the University of Southampton”
Notice the usual euphemisms ‘complementary’ and ‘integrated’ in the title: the word ‘alternative’ is never used. This sort of word play is part of the bait and switch approach of alternative medicine.
The unit is quite big: ten research staff, four PhD students and two support staff It is headed by George Lewith.
Teaching about alternative medicine to Southampton medical students.
The whole medical class seems to get quite a lot compared with other places I know about. That’s 250 students (210 on the 5-year course plus another 40 from the 4-year graduate-entry route).
Year 1: Lecture by David Owen on ‘holism’ within the Foundation Course given to all 210 medical students doing the standard (5-year) course.
Year 2: Lecture by Lewith (on complementary medicine, focusing on acupuncture for pain) given within the nervous systems course to the whole medical student year-group (210 students).
Year 3 SBOM (scientific basis of medicine) symposium: The 3-hour session (“Complementary or Alternative Medicine: You Decide”). I’m told that attendance at this symposium is often pretty low, but many do turn up and all of them are officially ‘expected’ to attend.
There is also an optional CAM special study module chosen by 20 students in year 3, but also a small number of medical students (perhaps 2 – 3 each year?) choose to do a BMedSci research project supervised by the CAM research group and involving 16-18 weeks of study from October to May in Year 4. The CAM research group also supervise postgraduate students doing PhD research.
As always, a list of lectures doesn’t tell you much. What we need to know is what’s taught to the students and something about the people who teach it. The other interesting question is how it comes about that alternative medicine has been allowed to become so prominent in a Russell group university. It must have support from on high. In this case it isn’t hard to find out where it comes from. Here are some details.
Year 1 Dr David Owen
David Owen is not part of Lewith’s group, but a member of the Division of Medical Education headed by Dr Faith Hill (of whom, more below). He’s one of the many part-time academics in this area, being also a founder of The Natural Practice .
Owen is an advocate of homeopathy (a past president of the Faculty of Homeopathy). Homeopathy is, of course, the most barmy and discredited of all the popular sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes it).
And he’s also a member of the British Society of Environmental Medicine (BSEM). That sounds like a very respectable title, but don’t be deceived. It is an organisation that promotes all sorts of seriously fringe ideas. All you have to do is notice that the star speaker at their 2011 conference was none other than used-to-be a doctor, Andrew Wakefield, a man who has been responsible for the death of children from measles by causing an unfounded scare about vaccination on the basis of data that turned out to have been falsified. There is still a letter of support for Wakefield on the BSEM web site.
The BSEM specialises in exaggerated claims about ‘environmental toxins’ and uses phony allergy tests like kinesiology and the Vega test that misdiagnose allergies, but provide en excuse to prescribe expensive but unproven nutritional supplements, or expensive psychobabble like "neuro-linguistic programming".
Other registered "ecological physicians" include the infamous Dr Sarah Myhill, who, in 2010, was the subject of a damning verdict by the GMC, and Southampton’s George Lewith.
If it is wrong to expose medical students to someone who believes that dose-response curves have a negative slope (the smaller the dose the bigger the effect -I know, it’s crazy), then it is downright wicked to expose students to a supporter of Andrew Wakefield.
David Owen’s appearance on Radio Oxford, with the indomitable Andy Lewis appears on his Quackometer blog.
Year 2 Dr George Lewith
Lewith is a mystery wrapped in an enigma. He’s participated in some research that is quite good by the (generally pathetic) standards of the world of alternative medicine.
In 2001 he showed that the Vega test did not work as a method of allergy diagnosis. "Conclusion Electrodermal testing cannot be used to diagnose environmental allergies", published in the BMJ .[download reprint].
In 2003 he published "A randomized, double-blind, placebo-controlled proving trial of Belladonna 30C” [download reprint] that showed homeopathic pills with no active ingredients had no effects: The conclusion was "”Ultramolecular homeopathy has no observable clinical effects" (the word ultramolecular, in this context, means that the belladonna pills contained no belladonna).
In 2010 he again concluded that homeopathic pills were no more than placebos, as described in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). [download reprint]
What i cannot understand is that, despite his own findings, his private practice continues to prescribe the Vega machine and continues to prescribe homeopathic pills. And he continues to preach this subject to unfortunate medical students.
Lewith is also one of the practitioners recommended by BSEM. He’s a director of the "College of Medicine". And he’s also an advisor to a charity called Yes To Life. (see A thoroughly dangerous charity: YesToLife promotes nonsense cancer treatments).
3rd year Student Selected Unit
The teaching team includes:
- David Owen – Principal Clinical Teaching Fellow SoM, Holistic Physician
- George Lewith – Professor of Health Research and Consultant Physician
- Caroline Eyles – Homeopathic Physician
- Susan Woodhead – Acupuncturist
- Elaine Cooke – Chiropractic Practitioner
- Phine Dahle – Psychotherapist
- Keith Carr – Reiki Master
- Christine Rose – Homeopath and GP
- David Nicolson – Nutritionalist
- Shelley Baker – Aromatherapist
- Cheryl Dunford – Hypnotherapist
- Dedj Leibbrandt – Herbalist
More details of the teaching team here. There is not a single sceptic among them, so the students don’t get a debate, just propaganda.
In this case. there’s no need for the Freedom of Information Act. The handouts. and the powerpoints are on their web site. They seem to be proud of them
Let’s look at some examples
Chiropractic makes an interesting case, because, in the wake of the Singh-BCA libel case, the claims of chiropractors have been scrutinised as never before and most of their claims have turned out to be bogus. There is a close relationship between Lewith’s unit and the Anglo-European Chiropractic College (the 3rd year module includes a visit there). In fact the handout provided for students, Evidence for Chiropractic Care , was written by the College. It’s interesting because it provides no real evidence whatsoever for the effectiveness of chiropractic care. It’s fairly honest in stating that the view at present is that, for low back pain, it isn’t possible to detect any difference between the usefulness of manipulation by a physiotherapist, by an osteopath or by a chiropractor. Of course it does not draw the obvious conclusion that this makes chiropractic and osteopathy entirely redundant -you can get the same result without all the absurd mumbo jumbo that chiropractors and osteopaths love, or their high-pressure salesmanship and superfluous X-rays. Neither does it mention the sad, but entirely possible, outcome that none of the manipulations are effective for low back pain. There is, for example, no mention of the fascinating paper by Artus et al [download reprint]. This paper concludes
"symptoms seem to improve in a similar pattern in clinical trials following a wide
variety of active as well as inactive treatments."
This paper was brought to my attention through the blog run by the exellent physiotherapist, Neil O’Connell. He comments
“If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery.”
This sort of critical thinking is conspicuously absent from this (and all the other) Southampton handouts. The handout is a superb example of bait and switch: No nonsense about infant colic, innate energy or imaginary subluxations appears in it.
Acupuncture is another interesting case because there is quite a lot of research evidence, in stark contrast to the rest of traditional Chinese medicine, for which there is very little research.
|
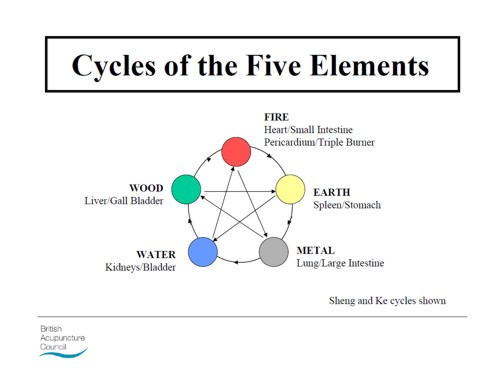
There is a powerpoint show by Susan Woodhead (though it is labelled British Acupuncture Council). The message is simple and totally uncritical. It works. |

|
In fact there is now a broad consensus about acupuncture.
(1) Real acupuncture and sham acupuncture have been found to be indistinguishable in many trials. This is the case regardless of whether the sham is a retractable needle (or even a toothpick) in the "right" places, or whether it is real needles inserted in the "wrong" places. The latter finding shows clearly that all that stuff about meridians and flow of Qi is sheer hocus pocus. It dates from a pre-scientific age and it was wrong.
(2) A non-blind comparison of acupuncture versus no acupuncture shows an advantage for acupuncture. But the advantage is usually too small to be of any clinical significance. In all probability it is a placebo effect -it’s hard to imagine a more theatrical event than having someone in a white coat stick long needles into you, like a voodoo doll. Sadly, the placebo effect isn’t big enough to be of much use.
Needless to say, none of this is conveyed to the medical students of Southampton. Instead they are shown crude ancient ideas that date from long before anything was known about physiology as though they were actually true. These folks truly live in some alternative universe. Here are some samples from the acupuncture powerpoint show by Susan Woodhead.
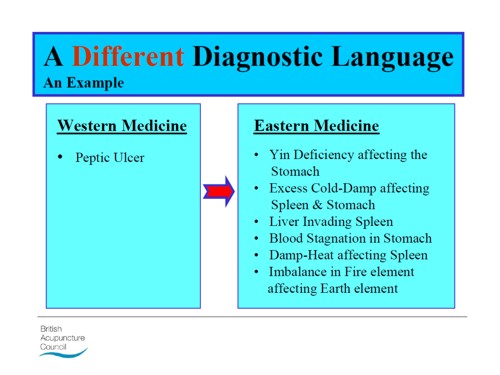
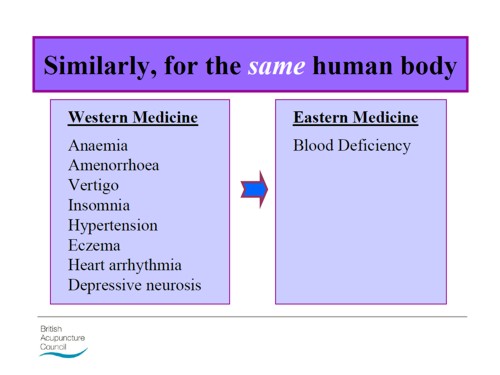
Well this is certainly a "different diagnostic language", but no attempt is made to say which one is right. In the mind of the acupuncurist it seems both are true. It is a characteristic of alternative medicine advocates that they have no difficulty in believing simultaneously several mutually contradictory propositions.
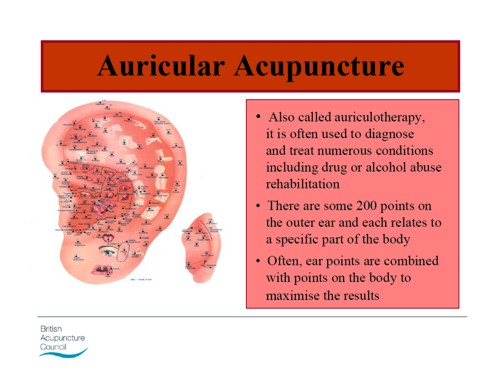
As a final exmple of barminess, just look at the acupuncture points (allegedly) on the ear The fact that it is a favoured by some people in the Pentagon as battlefield acupuncture, is more reminiscent of the mad general, Jack D. Ripper, in Dr Strangelove than it is of science.
There is an equally uncritical handout on acupuncture by Val Hopwood. It’s dated March 2003, a time before some of the most valuable experiments were done.
The handout says "sham acupuncture
is generally less effective than true acupuncture", precisely the opposite of what’s known now. And there are some bits that give you a good laugh, always helpful in teaching. I like
“There is little doubt that an intact functioning nervous system is required for acupuncture to produce
analgesia or, for that matter, any physiological changes”
and
Modern techniques: These include hybrid techniques such as electro-acupuncture . . . and Ryadoraku [sic] therapy and Vega testing.
Vega testing!! That’s been disproved dozens of times (not least by George Lewith). And actually the other made-up nonsense is spelled Ryodoraku.
It’s true that there is a short paragraph at the end of the handout headed "Scientific evaluation of acupuncture" but it doesn’t cite a single reference and reads more like excuses for why acupuncture so often fails when it’s tested properly.
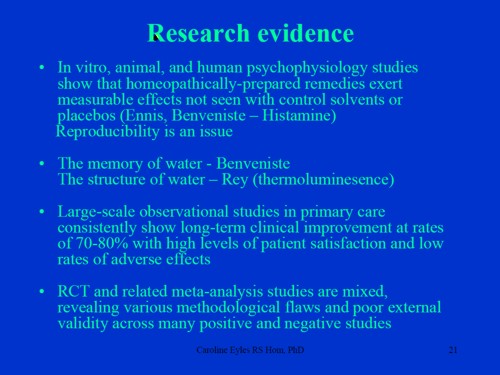
Homeopathy. Finally a bit about that most boring of topics, the laughable medicine that contains no medicine, homeopathy. Caroline Eyles is a member for the Society of Homeopaths, the organisation that did nothing when its members were caught out in the murderous practice of recommending homeopathy for prevention of malaria. The Society of Homeopaths also endorses Jeremy Sherr, a man so crazy that he believes he can cure AIDS and malaria with sugar pills.
The homeopathy handout given to the students has 367 references, but somehow manages to omit the references to their own boss’s work showing that the pills are placebos. The handout has all the sciencey-sounding words, abused by people who don’t understand them.
"The remedy will be particularly effective if matched to the specific/particular characteristics of the individual (the ‘totality’ of the patient) on all levels, including the emotional and mental levels, as well as just the physical symptoms. ‘Resonance’ with the remedy’s curative power will then be at it’s [sic] best."
The handout is totally misleading about the current state of research. It says
"increasing clinical research confirms it’s [sic] clinical effectiveness in treating patients, including babies and animals (where a placebo effect would be hard to justify)."
|
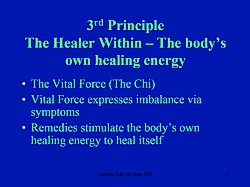
The powerpont show by Caroline Eyles shows all the insight of a mediaeval vitalist |
|
Anyone who has to rely on the utterly discredited Jacques Benveniste as evidence is clearly clutching at straws. What’s more interesting about this slide the admission that "reproducibility is a problem -oops, an issue" and that RCTs (done largely by homeopaths of course) have "various methodological flaws and poor external validity". You’d think that if that was the best that could be produced after 200 yours, they’d shut up shop and get another job. But, like aging vicars who long since stopped believing in god, but are damned if they’ll give up the nice country rectory, they struggle on, sounding increasingly desperate.
How have topics like this become so embedded in a medical course at a Russell group university?
The details above are a bit tedious and repetitive. It’s already established that hardly any alternative medicine works. Don’t take my word for it. Check the web site of the US National Center for Complementary and Alternative Medicine (NCCAM) who, at a cost of over $2 billion have produced nothing useful.
A rather more interesting question is how a good university like Southampton comes to be exposing its medical students to teaching like this. There must be some powerful allies higher up in the university. In this case it’s pretty obvious who thay are.
Professor Stephen Holgate MD DSc CSc FRCP FRCPath FIBiol FBMS FMed Sci CBE has to be the primary suspect, He’s listed as one of Southampton’s Outstanding Academics. His work is nothing to do with alternative medicine but he’s been a long term supporter of the late unlamented Prince of Wales’ Foundation, and he’s now on the advisory board of it’s successor, the so called "College of Medicine" (for more information about that place see the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health, and also Don’t be deceived. The new “College of Medicine” is a fraud and delusion ). His description on that site reads thus.
"Stephen Holgate is MRC Clinical Professor of Immunopharmacology at the University of Southampton School of Medicine and Honorary Consultant Physician at Southampton University Hospital Trust. He is also chair of the MRC’s Populations and Systems Medicine Board. Specialising in respiratory medicine, he is the author of over 800 peer-reviewed papers and contributions to scientific journals and editor of major textbooks on asthma and rhinitis. He is Co-Editor of Clinical and Experimental Allergy, Associate Editor of Clinical Science and on the editorial board of 25 other scientific journals."
Clearly a busy man. Personally I’m deeply suspicious of anyone who claims to be the author of over 800 papers. He graduated in medicine in 1971, so that is an average of over 20 papers a year since then, one every two or three weeks. I’d have trouble reading that many, never mind writing them.
Holgate’s long-standing interest in alternative medicine is baffling. He’s published on the topic with George Lewith, who, incidentally, is one of the directors of the "College of Medicine"..
It may be unkind to mention that, for many years now, I’ve been hearing rumours that Holgate is suffering from an unusually bad case of Knight starvation.
The Division of Medical Education appears to be the other big source of support for. anti-scientific medicine. That is very odd, I know, but it was also the medical education people who were responsible for mis-educating medical students at. St. Bartholomew’s and at Edinburgh university. Southampton’s Division of Medical Education has a mind-boggling 60 academic and support staff. Two of them are of particular interest here.
Faith Hill is director of the division. Her profile doesn’t say anything about alternative medicine, but her interest is clear from a 2003 paper, Complementary and alternative medicine: the next generation of health promotion?. The research consisted of reporting anecdotes from interviews of 52 unnamed people (this sort of thing seems to pass for research in the social sciences). It starts badly by misrepresenting the conclusions of the House of Lords report (2000) on CAM. Although it comes to no useful conclusions, it certainly shows a high tolerance of nonsensical treatments.
Chris Stephens is Associate Dean of Medical Education & Student Experience. His sympathy is shown by a paper he wrote In 2001, with David Owen (the homeopath, above) and George Lewith: Can doctors respond to patients’ increasing interest in complementary and alternative medicine?. Two of the conclusions of this paper were as follows.
"Doctors are training in complementary and alternative medicine and report benefits both for their patients and themselves"
Well, no actually. It wasn’t true then, and it’s probably even less true now. There’s now a lot more evidence and most of it shows alternative medicine doesn’t work.
"Doctors need to address training in and practice of complementary and alternative medicine within their own organisations"
Yes they certainly need to do that.
And the first thing that Drs Hill and Stephens should do is look a bit more closely about what’s taught in their own university, I hope that this post helps them,
Follow-up
4 July 2011. A correspondent has just pointed out that Chris Stephens is a member of the General Chiropractic Council. The GCC is a truly pathetic pseudo-regulator. In the wake of the Simon Singh affair it has been kept busy fending off well-justified complaints against untrue claims made by chiropractors. The GCC is a sad joke, but it’s even sadder to see a Dean of Medical Education at the University of Southampton being involved with an organisation that has treated little matters of truth with such disdain.
A rather unkind tweet from (ex)-chiropractor @RichardLanigan.
“Chris is just another light weight academic who likes being on committees. Regulatory bodies are full of them”
Chiropractors are getting very touchy indeed, all over the world. And no wonder, because their claims are being exposed as baseless as never before, in the wake of their attempts to stifle criticism by legal action..
In March, Shaun Holt appeared on Breakfast TV in New Zealand. Holt has done a lot of good work on TV in debunking some of the preposterous claims made by quacks. See him on YouTube.
This time he talked about chiropractic. Here is the video.
One could argue that he was over generous to chiropractic, especially when talking about their effectiveness in treating low back pain. He said, quite rightly, that chiropractors are no better than physiotherapists at treating low back pain.
But a recent trial suggests that neither are much good. “A randomised controlled trial of spinal manipulative therapy in acute low back pain” (Juni et al., 2009 in the BMJ; see also coverage in Pulse). This trial compared standard care with standard care plus spinal manipulative therapy (SMT). The results were negative, despite the fact that this sort of A + B vs B design is inherently biassed in favour of the treatment (see A trial design that generates only ”positive” results, Ernst & Lee 2008, Postgrad Med J.).
"SMT was performed by a specialist in manual medicine, chiropractice and rheumatology (GH), a specialist in physical medicine (DV) or an osteopath (RvB), all proficient in SMT."
"Conclusions: SMT is unlikely to result in relevant early pain reduction in patients with acute low back pain."
Admittedly, the trial was quite small (104 patients, 52 in each group) so it will need to be confirmed. but the result is entirely in line with what we knew already.
It also adds to the evidence that the recommendation by NICE of SMT by chiropractors constitutes their biggest failure ever to assess evidence properly. If NICE don’t amend this advice soon, they are in danger of damaging their hitherto excellent record.
Despite the moderate tone and accuracy of what Holt said on TV, the New Zealand Chiropractors’ Association made a formal complaint. That is what they like to do, as I learned recently, to my cost. It is so much easier than producing evidence.
Quite absurdly the New Zealand Broadcasting Standards Authority (BSA) has upheld some of the complaints. Their judgement can be read here.
The BSA consists of four people, two lawyers and two journalists. So not a trace of scientific expertise among them. Having people like that judging the claims of chiropractors makes as much sense as having them judged by Mr Justice Eady. They seem to be the sort of people who think that if there is a disagreement, the truth must lie half-way between the opposing views.
One of the BSA members, Tapu Misa, has used her newspaper column to quote approvingly the views of the notorious Dr Mercola web site on flu prevention “Your best defence, it says, is to eat right, get lots of sleep, avoid sugar and stress, load up on garlic, Vitamin D and krill oil”. (Snake oil is said to be good too.) There are some odd attitudes to science in some of her other columns too (e.g. here and here). Not quite the person to be judging the evidence for and against chiropractic, I think.
In fact the TV show in question was more than fair to chiropractors. It adopted the media’s usual interpretation of fair and balanced: equal time for the flat earthers. A Chiropractor was invited to reply to Holt’s piece. Here he is.
The chiropractor, Doug Blackbourn, started very plausibly, though a tendency to omit every third syllable made transcription hard work. He established that if you cut yourself you get better (without any help). He established that nerves run down the spinal cord. So far, so good. But then he quickly moved on to the usual flights of fancy.
"We have two premises. The body heals itself and the nervous system runs the body. Now the nervous system runs the body, travels down through the spinal cord so chiropractic is not based on the belief that, you know, energy flows, it’s based on the fact that your nervous system runs the body and [inaudible] affects the overall health of the body"
This statement is totally vague. It has nothing whatsoever to do with the main question, can chiropractors do anything useful. It is sheer flannel.
We’re seeing people, heck, diabetes. I had a quadriplegic come in one time for adjustment, we’ve got stroke people, we’ve got all sorts of conditions. We’re not treating the condition, We’re allowing, checking the spine to see if there’s any interference there that will slow the body down"
“Interference”? “slowing the body down”? These are utterly meaningless phrases that simply serve to distract from the only question that matters.
"Chiropractice is the most safest [sic] profession to go to to get your spine adjusted"
Hmm I thought it was the only job that uses the word ‘adjustment’.
Worst of all was his response to a question about asthma.
Presenter: "So chiropractors are not out there claiming they will cure asthma for example?". Chiropractor: "No"
This is simply untrue, both in New Zealand and in the UK. For a start, just look at what Blackbourn’s own web site says about asthma.
"The challenge, of course, with allergy and asthma medication is there is no end-point. There is no cure. Asthma and allergies, for the most part, are lifelong conditions requiring lifelong medication. Might there be a better way, an alternative solution?
“Alternative” is the key word. Medical treatment is designed to combat symptoms, and is successful to a certain extent with allergies and asthma. Underlying causes are not addressed, however, and symptoms continue year after year. What else might be done?
Enter chiropractic care. Chiropractic health care, with its unique comprehensive approach, is able to offer positive benefit to a variety of conditions and ailments. In the case of allergies and asthma, these “hypersensitivity conditions” may respond well to therapy designed to normalize the body’s flow of nerve signals. To use a metaphor, chiropractic treatment removes roadblocks to the body’s natural healing abilities. Restoring these imbalances may help reduce such hypersensitivity reactions."
Blackbourn’s web site describes him thus
"As a Doctor of Chiropractic, Dr. Doug Blackbourn . . ."
But the qualifications of “Dr” Blackbourn are B.App.Sc (Chiro) M.N.Z.C.A , the same as those of “Dr” Brian Kelly.
After a performance like this, perhaps someone should submit a complaint to the New Zealand Broadcasting Standards Authority.
After all, I notice that they have dismissed complaints from one chiropractor, Sean Parker, after a TV programme looked at the business practices of his private chiropractic practice, The Spinal Health Foundation. Perhaps the BSA understands business better than it understands science.
Follow-up
Is chiropractic crumbling in New Zealand? The New Zealand College of Chiropractic featured in my editorial in the New Zealand Medical Journal, and in the fallout from that article, It’s principle, “Dr” Brian Kelly (B App Sci (Chiro)) seems to be getting desperate. His college is now canvassing for recruits in Canada. They are promised all the woo.
- Subluxation centered techniques – Gonstead, Toggle Recoil, Thompson, Diversified
- Traditional philosophy featuring vitalism and innate healing – congruent curriculum
Perhaps Canada is a good place to recruit, gven the $500 million class action being brought against chiropractors in Canada, after Sandra Nette became tetraplegic immediately after a chiropractor manipulated her neck, Canadian chiropractors must be looking for somewhere to hide.
Stuff and Nonsense. jdc described this story at the time the complaint was lodged.
Shaun Holt’s own blog follows the action.
New Zealand Doctor covers the story.
Bay of Plenty Times “Bay researcher slams television complaint ruling“
In July 2008 I wrote an editorial in the New Zealand Medical Journal (NZMJ), at the request of its editor.
The title was Dr Who? deception by chiropractors. It was not very flattering and it resulted in a letter from lawyers representing the New Zealand Chiropractic Association. Luckily the editor of the NZMJ, Frank Frizelle, is a man of principle, and the legal action was averted. It also resulted in some interesting discussions with disillusioned chiropractors that confirmed one’s worst fears. Not to mention revealing the internecine warfare between one chiropractor and another.
This all occurred before the British Chiropractic Association sued Simon Singh for defamation. The strength of the reaction to that foolhardy action now has chiropractors wondering if they can survive at all. The baselessness of most of their claims has been exposed as never before. No wonder they are running scared. The whole basis of their business is imploding.
Needless to say chiropractors were very cross indeed. Then in February 2009 I had a polite email from a New Zealand chiropractor, David Owen, asking for help to find one of the references in the editorial. I’d quoted Preston Long as saying
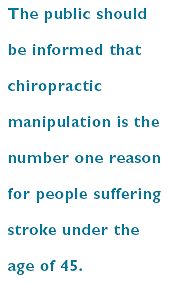
"Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
And I’d given the reference as
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10
I’d found the quotation, and the reference, in Ernst’s 2005 article, The value of Chiropractic, but at the time I couldn’t find the Journal of Quality Healthcare. I did find the same article on the web. At least the article had the same title, the same author and the same quotation. But after finding, and reading, the article, I neglected to change the reference from J Quality Health Care to http://skepticreport.com/sr/?p=88. I should have done so and for that I apologise.
When I asked Ernst about the Journal of Quality Healthcare, he couldn’t find his copy of the Journal either, but he and his secretary embarked on a hunt for it, and eventually it was found.

![]()
|
It turns out that Journal of Quality Healthcare shut down in 2004, without leaving a trace on the web, or even in the British Library. It was replaced by a different journal, Patient Safety and Quality Healthcare (PSQH) A reprint was obtained from them. It is indeed the same as the web version that I’d read, and it highlighted the quotation in question. The reprint of the original article, which proved so hard to find, can be downloaded here. |
|
The full quotation is this
"Sixty-two clinical neurologists from across Canada, all certified members of the Royal College of Physicians and Surgeons, issued a warning to the Canadian public, which was reported by Brad Stewart, MD. The warning was entitled Canadian Neurologists Warn Against Neck Manipulation. The final conclusion was that endless non-scientific claims are being made as to the uses of neck manipulation(Stewart, 2003). They need to be stopped. The public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45."
I have often condemned the practice of citing papers without reading them (it is, of course, distressingly common), so I feel bad about this, though I had in fact read the paper in question in its web version. I’m writing about it because I feel one should be open about mistakes, even small ones.
I’m also writing about it because one small section of the magic medicine community seems to think they have nailed me because of it. David Owen, the New Zealand chiropractor, wrote to the editor of the NZMJ, thus.
|
The quote [in question] is the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45. Long PH. Stroke and Manipulation. J Quality Health Care. 2004:3:8-10 This quote actually comes from the following blog article http://www.skepticreport.com/medicalquackery/strokespinal.htm [DC the URL is now http://skepticreport.com/sr/?p=88] I have attached all my personal communications with Colquhoun. They demonstrate this is not a citation error. Prof Colquhoun believes the origin of the quote doesn’t matter because Long was quoting from a Canadian Neurologists’ report (this is also incorrect). As you can see he fails to provide any evidence at all to support the existance [sic] of the “J Quality Health Care.” Colquhoun ‘s belief that my forwarding this complaint is me “resorting to threats” is the final nail in the coffin. If he had any leg to stand on where is the threat? This may seem pedantic but it surely reflects a serious ethical breach. Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility? Incidentally, at the end of the article, conflicts of interest are listed as none. As Colquhoun is a Professor of Pharmacology and much of his research funding no doubt comes from the pharmaceutical industry how can he have no conflict of interest with therapies that do not advocate the use of drugs and compete directly against the billions spent on pain medications each year? If I may quote Colquhoun himself in his defence of his article (Journal of the New Zealand Medical Association, 05-September-2008, Vol 121 No 1281) I’ll admit, though, that perhaps ‘intellect’ is not what’s deficient in this case, but rather honesty. David Owen |
Financial interests
Well, here is a threat: I’m exposed as a shill of Big Pharma. ". . . much of his funding no doubt comes from the pharmaceutical industry". I can’t count how many times this accusation has been thrown at me by advocates of magic medicine. Oddly enough none of them has actually taken the trouble to find out where my research funding has come from. None of them even knows enough about the business to realise the extreme improbability that the Pharmaceutical Industry would be interested in funding basic work on the stochastic properties of single molecules. They fund only clinicians who can help to improve their profits,
The matter of funding is already on record, but I’ll repeat it now. The media ‘nutritional therapist’, Patrick Holford, said, in the British Medical Journal
“I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry “
To which my reply was
” Oh dear, Patrick Holford really should check before saying things like “I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry”. Unlike Holford, when I said “no competing interests”, I meant it. My research has never been funded by the drug industry, but always by the Medical Research Council or by the Wellcome Trust. Neither have I accepted hospitality or travel to conferences from them. That is because I would never want to run the risk of judgements being clouded by money. The only time I have ever taken money from industry is in the form of modest fees that I got for giving a series of lectures on the basic mathematical principles of drug-receptor interaction, a few years ago.”
I spend a lot of my spare time, and a bit of my own money, in an attempt to bring some sense into the arguments. The alternative medicine gurus make their livings (in some cases large fortunes) out of their wares.
So who has the vested interest?
Does chiropractic actually cause stroke?
As in the case of drugs and diet, it is remarkably difficult to be sure about causality. A patient suffers a vertebral artery dissection shortly after visiting a chiropractor, but did the neck manipulation cause the stroke? Or did it precipitate the stroke in somebody predisposed to one? Or is the timing just coincidence and the stroke would have happened anyway? There has been a lot of discussion about this and a forthcoming analysis will tackle the problem of causality head-on,
My assessment at the moment, for what it’s worth, is that there are some pretty good reasons to suspect that neck manipulation can be dangerous, but it seems that serious damage is rare.
In a sense, it really doesn’t matter much anyway, because it is now apparent that chiropractic is pretty well discredited without having to resort to arguments about rare (though serious) effects. There is real doubt about whether it is even any good for back pain (see Cochrane review), and good reason to think that the very common claims of chiropractors to be able to cure infant colic, asthma and so on are entirely, ahem, bogus. (See also Steven Novella, ebm-first, and innumerable other recent analyses.)
Chiropractic is entirely discredited, whether or not it may occasionally kill people.
Complaint sent to UCL
I had an enquiry about this problem also from my old friend George Lewith. I told him what had happened. Soon after this, a complaint was sent to Tim Perry and Jason Clarke, UCL’s Director and Deputy Director of Academic Services. The letter came not from Lewith or Owen, but from Lionel Milgom. Milgrom is well known in the magic medicine community for writing papers about how homeopathy can be “explained” by quantum entanglement. Unfortunately for him, his papers have been read by some real physicists and they are no more than rather pretentious metaphors. See, for example, Danny Chrastina’s analysis, and shpalman, here. Not to mention Lewis, AP Gaylard and Orac.
|
Dear Mr Perry and Mr Clark, I would like to bring to your attention an editorial (below) that appeared in the most recent issue of the New Zealand Medical Journal. In it, one of your Emeritus Professors, David Colquhoun, is accused of a serious ethical breach, and I quote – “Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility?” Professor Colquhoun is well-known for writing extensively and publicly excoriating many forms of complementary and alternative medicine, particularly with regard to the alleged unscientific nature and unethical behaviour of its practitioners. Professor Colquhoun is also a voluble champion for keeping the libel laws out of science. While such activities are doubtlessly in accord with the venerable Benthamite liberal traditions of UCL, I am quite certain hypocrisy is not. And though Professor Colquhoun has owned up to his error, as the NZMJ’s editor implies, it leaves a question mark over his credibility. As custodians of the college’s academic quality therefore, you might care to consider the possible damage to UCL’s reputation of perceived professorial cant; emeritus or otherwise. Yours Sincerely Dr Lionel R Milgrom |
So, as we have seen, the quotation was correct, the reference was correct, and I’d read the article from which it came I made a mistake in citing the original paper rather than the web version of the same paper..
I leave it to the reader to judge whether this constitutes a "serious ethical breach", whether I’d slipped in an "unsupported statement", and whether it constitutes "hypocrisy"
Follow-up
It so happens that no sooner was this posted than there appeared Part 2 of the devastating refutation of Lionel Milgrom’s attempt to defend homeopathy, written by AP Gaylard. Thanks to Mojo (comment #2) for pointing this out.
Peter Dixon is a chiropractor. He is chair of the General Chiropractic Council (GCC). He was also a member of the hotly-disputed NICE low back pain guidance group that endorsed (you guessed it) the use of chiropractic, a decision that has led to enormous criticism of the standards of the National Institute of health and Clinical Excellence (NICE).
As a consequence largely of the decision of the British Chiropractic Association (BCA) to sue Simon Singh for defamation, there has been an unprecedented interest taken in the claims made by chiropractors in general.
Peter Dixon has a problem because something like 600 individual complaints about unjustified health claims have been sent to the GCC. Even when a web site does not claim to be able to benefit things like asthma and colic, a phone call may reveal that claims are made in private (one of the many complaints to the GCC concerns such behaviour by two practices belonging to, ahem, Peter Dixon Associates).
The crucial question is, as always, one of evidence. The BCA claim to have a plethora of evidence for their claims, but they have been strangely reluctant to produce it. In fact evidence is cited on the “Your first visit” page on Dixon’s site.
At the bottom we see “How effective is Chiropractic?”.
That sounds very impressive indeed: . ” . . . patients who received chiropractic treatment improved by 70% more than those given hospital out-patient.”
But hang on. If we look at the paper, Meade et al., 1990 [download reprint], we see that Figure 2 looks like this.
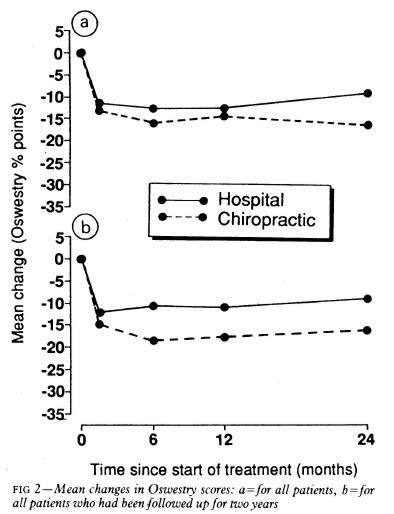
Several things jump out. First, the Oswestry disability index scale runs for 0 to 100, but scores are plotted only from 0 to 35, so the size of the effects are exaggerated. Second, there are no error bars on the points. Third there is essentially no advantage for chiropractic at all when all patients are taken together (top graph). Fourth, and most important, the patients who were followed up for two years (bottom graph) seem to show a slight advantage for chiropractic but on average, the effect is 7 percent (on the 100 point scale, NOT 70 percent as claimed on the web site of Peter Dixon Associates.
What sort of mistake was made?
The abstract of the paper itself says “A benefit of about 7% points on the Oswestry scale was seen at two years.” How did this become “improved by 70% more”?
It could have been simple a typographical error, but that seems unlikely, Who’d boast about a 7% improvement?
Perhaps it is a question of relative versus absolute change. The Figure does not show the actual scores on the 100 point scale, but rather the change in score, relative to a questionnaire given just before starting treatment. If we look at the lower part of the Figure, restricted to those patients who stayed with the trail for 2 years (by this time 28% of the patients had dropped out), we see that there is a reduction in score (improvement) of about 10 points on the 100 point scale with hospital treatment (not a very impressive response). The improvement with those sent to private chiropractic clinics was about seven points bigger. So a change from 10 to 17 is a 70 percent change. What’s wrong with that?
What’s wrong is that it is highly misleading, as relative changes often are. Imagine that the hospital number had been 7 points and the chiropractic number had been 14 (both out of 100). That would mean that both treatments had provided very modest benefits to the patients. Would it then be fair to describe the chiropractic patients as have improved by 100 percent more than the hospital patients, when in fact neither got much benefit? Of course it would not. To present the results in this way would be highly deceptive.
Put another way, a 70% increase in a trivial effect is still pretty trivial.
That isn’t all either. The paper has been analysed in some detail on the ebm-first site. The seven point difference on a 100 point scale, though it may be real, is too small to be ‘clinically significant’ In other words the patient would scarcely notice such a small change. Another problem lies in the nature of the comparison. Patients were, quite properly, allocated at random to chiropractic or to to hospital treatment. BUT the comparion was very from blind. one group was treated in hospital. The other group was sent to private chiropractic clinics. The trivial 7 point difference could easily be as much to do with the thickness of the carpets rather than any effect of spinal manipulation.
What this paper really tells you is that neither treatment is very effective and that there is little to choose between them.
It is really most unfortunate that the chairman of the GCC should show himself to be so careless about evidence at a time when the evidence for the claims of chiropractors is under inspection as never before. It does not add to their case for criticising Simon Singh and it does not add to one’s confidence in the judgement of the NICE guidance group.
Follow-up
The Pain Society revolt. A letter has been sent from several distinguished members of the British Pain Society to its President and Council.
“We, the undersigned, call upon the President of the British Pain Society to issue a statement to NICE and to the press condemning outright the conclusions of the recent UK National Institute for Health and Clinical Excellence (NICE) guidelines . . .”
The sigificance of this letter is that the present president of the British Pain Society is Professor Paul Watson who was a member of the NICE guidance group that produced the recommendations which have engendered such criticism. He was clinical advisor to the guidance group. There is a video of Paul Watson talking about back pain, that seems to me to illustrate very well the problem with the guidance. He says it is a huge problem (everyone knows that) and that something must be done, but he doesn’t say what. There is no admission that, in very many cases, nobody knows what to do. It is exactly this sort of hubris that that makes the NICE report so bad,
One caustic comment on the letter says
“We are led by a physiotherapist! A Professor who cannot even interpret straight forward evidence when it is presented to him on a plate.
Who’s going to be the next BPS President? A Hospital Porter?”
The first post was NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself.
That was followed by NICE fiasco, part 2. Rawlins should withdraw guidance and start again.
Since then, something of a maelstrom has engulfed NICE, so it’s time for an update.
It isn’t only those who are appalled that NHS should endorse voodoo medicine on the basis of very slim evidence who are asking NICE to rethink their guidance on low back pain. Pain specialists are up in arms too, and have even started a blog, ‘Not Nearly as NICE as you think …‘, to express their views. Equally adverse opinions are being expressed in the Britsh Medical Journal. A letter there is signed by over 50 specialists in pain medicine. It ends thus
“Because of these new guidelines patients will continue to experience unnecessary pain and suffering and their rights to appropriately individually tailored treatment have been removed on the basis of a flawed analysis of available evidence. We believe the guidelines do not reflect best practice, remove patient choice and are not in our patients’ best interests.”
In a contribution headed “NICE misguidance”. Dr Michel Vagg ends
It seems to me that this guideline has been used as a propaganda vehicle to allow cherry-picked evidence to be enshrined as doctrine. This is an abuse of the guideline development process . . . ”
I have to say, though, that it seems to me that some of these people are promoting their own interests as much as chiropractors and acupuncturists. The evidence that spinal injections produce worthwhile benefits seems to be as thin as the evidence that chiropractic and acupuncture produce worthwhile benefits. But no doubt the injections are good for the budgets of PCTs or private practice doctors.. Could it perhaps be the case that some of the clinicians’ anger is being generated by doctors who are rushing to defend their own favourite ineffective treatment?
Why, oh why, can’t either NICE or the pain consultants bring themselves to state the obvious, that nothing works very well. The only thing that can be said for most of the regular treatments is that although they may not be much more effective than acupuncture or chiropractic, at least they don’t come with the intellectually-offensive hokum that accompanies the latter. Very sensible attempts have been made to identify the cause of low back pain [reviewed here], Occasionally they succeed. Mostly they don’t.
One clinician’s letter deserves special attention because it goes into the evidence, and the costs, in some detail. Its conclusions are very different from those in the NICE guidance.
The letter, a Review of NICE guidance, is from Dr C.J.D. Wells [download the whole letter]. He is a pain relief consultant from Liverpool.
Let’s look at some highlights.
Wells points out the absurdity of the cost estimates
“In the pricing section, they estimate that this will require an increase of facilities so that 3,500 patients can be treated instead of 1,000 at present (again see comments on pricing). This is not many treatments for the 20 million sufferers, of whom we can estimate that at least 2 million will have significant long-term disability and psychological distress”
And that is without even costing all the secondary costs of miseducating a new generation of students in fables about “Qi”, meridians, energy flow, subluxations and innate intelligence.
“The abysmal ignorance of the committee is reflected in the poor overall advice. So if you have a committee with special interests in Exercise, Manipulation, PMP’s, and Surgery, and you call an expert on Acupuncture, you get advice to use Exercise, Manipulation, Acupuncture, PMP’s and Surgery. Amazing.”
Another pain consutant, Charles Guaci, says in a comment in the Daily Mail.
I am a Pain Consultant of 30 years experience, have published two books (one translated into different languages).
NICE never asked me for my opinion.
This is the most ridicuculous pseudo-scientific document I have ever seen.
The panel consisted of a surgeon, psychologist, osteopath, acupuncturist a physiotherapist and an academic; not one pain consultant! The conclusions are simply a means of increasing the employment of their friends!
All evidence submitted to NICE was ignored.
It is almost certain than unless NICE rethink their ideas that Pain Consultants will be seeking a judicial review as well as full disclosure of how the panel arrived at their bizarre findings under the Freedom of information act.
Patients should realise that they are being taken for a ride.
Despite the outcry from opponents of magic medicine and from pain specialists, the assessment by the normally excellent NHS Choices site was disappointing. It made no mention at all of the secondary consequences of recommending CAM and described the assertions of the guidance group quite uncritically.
The reputation of NICE
NICE has been criticised before, though usually unjustly. In the past I have often supported them. For example. when NICE said that treatment of dementia with anticholinesterase drugs like galantamine was ineffective, there was a great outcry, but NICE were quite right. There is little or no rationale for such treatments, and more importantly, very little evidence that they work. But patients, especially when they are desperate, have greater faith in drug treatments than most pharmacologists, They want to clutch at straws. A bit like the NICE guidance committee, faced with a bunch of treatments most of which are almost ineffective, clutched at the straws of acupuncture and chiropractic. But this time it isn’t only the patients who are cross. It is most of the medical and scientific world too.
One interpretation of these bizarre events is that they represent a case of medical/scientific arrogance. Ben Goldacre wrote of another aspect of the same problem thus week, in Dodgy academic PR [download the paper on which this is based].
The first job of a scientist is to say openly when the answer to a question is not known. But scientists are under constant pressure to exaggerate the importance of their results. Last year we published an article which I feel may, if verified, turn out to be the second most important that I have ever been an author on. Because it happened to be published in Nature (not because of its quality), a press release was written (by an arts graduate!). It took some argument to prevent the distorted and exaggerated account being imposed on the public. This is typical of the sort of thing reported in Goldacre’s column. I reported a similar case a while ago, Why honey isn’t a wonder cough cure: more academic spin.
If NICE does not reconsider this guidance, it is hard to see how it can be taken seriously in the future. I hope that when NICE’s director, Professor Sir Michael Rawlins, returns from his trips abroad, he will find time to look at the case himself.
Indirectly, then, it can be argued that NICE’s bizarre guidance is just another manifestation of the management of science being passed from the hands of scientists into the hands of administrators and spin experts. It is yet another example of DC’s rule
Never trust anyone who uses the word ‘stakeholder’
Some bone-headed bureaucrat decides that any charlatan or quack is a ‘stakeholder’ in the provision of NHS care and gives them a quite disproportionate say in how taxpayers’ money is spent. The bureaucrats are so busy following processes and procedures, ticking boxes, and so deficient in scientific education, that they failed to notice that they’ve been caught out by the old trick of used car salesmen, bait and switch.
The consequences
The expected consequences have already started to materialise. The Prince of Wales’ Foundation for Magic Medicine is jubilant about having been endorsed by NICE. And I’m told that “The chiropractors have now just written letters to all health boards in Scotland asking for contracts for their services to deal with back pain”.
There could hardly have been a worse time for NICE to endorse chiropractic. We are in the middle of a storm about free speech because of the disgraceful action of the British Chiropractic Associaton in suing one of our best science writers, Simon Singh, for defamation because he had the temerity to express an opinion, Of course, even if the BCA wins in court, it will be the overall loser, because chiropractic claims are now being scrutinised as never before (just look at what they told me).
Follow-up
A much-cited paper. The paper that is most often cited by chiropractors who claim to be able to cure colic by spinal manipulation is Klougart N, Nilsson N and Jacobsen J (1989) Infantile Colic Treated by Chiropractors: A Prospective Study of 316 Cases, J Manip Physiol Ther,12:281-288. This is not easy to get hold of but Steve Vogel has sent me s scanned copy which you can download here. As evidence it is about as useless as the infamous Spence study so beloved of homeopaths. There was no control group at all. It simply follows 316 babies and found that most of them eventually got better. Well, they do, don’t they? It is a sign of the pathetic standard of reaearch in chiropractic that anyone should think this paper worth mentioning at all.
June 6 2009. More flak for NICE from the Royal College of Anaesthetists, and more adverse comment in the BMJ. And of course the blogs. for example, “If this is “evidence based medicine” I want my old job back“.
“Acupuncture on the NHS: a dangerous precedent”: a good analysis at counterknowledge.com.
June 6 2009, Comment sent to the BMJ. The comment was submitted, as below, early on Friday 5th June. The BMJ said it was a “sensitive issue” and for the next five days lawyers pondered over it.
Underwood and Littlejohns describe their guidance as being a “landmark”. I can only agree with that description. It is the first time that NICE has ever endorsed alternative medicine in the face of all the evidence. The guidance group could hardly have picked a worse moment to endorse chiropractic. Chiropractors find it so hard to find evidence for their practices that, when one of our finest science writers, Simon Singh, asked to see the evidence they sued him for defamation. I suggest that the guidance group should look at the formidable list of people who are supporting Singh, after his brave decision to appeal against this iniquitous persecution.
Of course I’m sure this bizarre decision has nothing to do with the presence on the guidance group of Peter Dixon, chair of the General Chiropractic Council. Nevertheless, I am curious to know why it is that when I telephoned two of the practices belonging to Peter Dixon Associates, I was told that they could probably treat infantile colic and asthma. Such claims have just been condemned by the Advertising Standards Authority.
The low back pain guidance stands a good chance of destroying NICE’s previously excellent reputation for dispassionate assessment of benefits and costs. Yes, that is indeed a landmark of sorts.
If NICE is ever to recover its reputation, I think that it will have to start again. Next time it will have to admit openly that none of the treatments work very well in most cases. And it will have to recognise properly the disastrous cultural consequences of giving endorsement to people who, when asked to produce evidence, resort to legal intimidation.
Eventually, on Wednesday 10 June the comment appeared in the BMJ, and it wasn’t greatly changed. Nevertheless if is yet another example of legal chill. This is the final version.
Underwood and Littlejohns describe their guidance as being a “landmark”. I can only agree with that description. It is the first time that NICE has ever endorsed alternative medicine in the face of all the evidence. The guidance group could hardly have picked a worse moment to endorse chiropractic. Chiropractors are so sensitive about criticisms of their practices that, when one of our finest science writers, Simon Singh, queried the evidence-base for their therapeutic claims they sued him for defamation. I suggest that the guidance group should look at the formidable list of people who are supporting Singh, after his brave decision to appeal against an illiberal court ruling in this iniquitous persecution.
One wonders whether this bizarre decision by NICE has anything to do with the presence on the guidance group of Peter Dixon, chair of the General Chiropractic Council. I am also curious to know why it is that when I telephoned two of the practices belonging to Peter Dixon Associates, I was told that chiropractic could be effective in the treatment of infantile colic and asthma. Similar claims about treating colic have just been condemned by the Advertising Standards Authority.
The low back pain guidance stands a good chance of destroying NICE’s previously excellent reputation for dispassionate assessment of benefits and costs. Yes, that is indeed a landmark of sorts.
If NICE is ever to recover its reputation, I think that it will have to start again. Next time it will have to admit openly that none of the treatments works very well in most cases. And it will have to recognise properly the disastrous cultural consequences of giving endorsement to people who, instead of engaging in scientific debate, resort to legal intimidation.
Bait and switch. Oh dear, oh dear. Just look at this. British Chiropractic Association tell their members to hide their sins from prying eyes.
Excellent round-up of the recent outburst of writing about “chiroquacktic” (Tut, tut, is there no respect?).
Dr Crippen writes “NICE recommends a cure for all known disease” [Ed some exaggeration, surely]
Two days ago I wrote NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself
Now the official ‘guidance’ is out, and it is indeed quite as bad as the draft.
The relevant bits now read thus.
- Offer one of the following treatment options, taking into account patient preference: an exercise programme, a course of manual therapy or a course of acupuncture. Consider offering another of these options if the chosen treatment does not result in satisfactory improvement.
- Consider offering a structured exercise programme tailored to the person:
- This should comprise of up to a maximum of 8 sessions over a period of up to 12 weeks.
- Offer a group supervised exercise programme, in a group of up to 10 people.
- A one-to-one supervised exercise programme may be offered if a group programme is not suitable for a particular person.
- Consider offering a course of manual therapy, including spinal manipulation, comprising up to a maximum of nine sessions over a period of up to 12 weeks
- Consider offering a course of acupuncture needling comprising up to a maximum of 10 sessions over a period of up to 12 weeks.
The summary guidance still doesn’t mention chiropractic explicitly, just a coy reference to “spinal manipulation”. At a time when the British Chiropractic Association is busy trying to suppress free speech via the law courts, I guess it isn’t surprising that they don’t like to use the word.
The bias in the recommendations is perhaps not surprising because the guidance development group had a heavy representation from alternative medicine advocates, and of people with a record of what, is, in my view, excessive tolerance of mumbo-jumbo.
Royal College of General Practitioners (RCGP) played a large part in writing the guidance. That is an organisation thar has steadfastly refused to make any sort of sensible statement of policy about magic medicine. It isn’t long since I was told by a senior person at the RCGP that there was nothing odd about neuro-linguistic programming. That does not bode well.
Professor Martin Underwood, Professor of Primary Care Research Warwick Medical School, University of Warwick. Underwood chaired the guidance development group. Martin Underwood is also a GP in Coventry See also the British Osteopathic Association. Underwood was lead author of the BEAM trial (download reprint). It is well worth reading the comments on this trial too. It was a randomised trial (though not, of course, blind).
|
Our main aim was to estimate, for patients consulting their general practitioner with back pain, the effectiveness of adding the following to best care in general practice: a class based exercise programme (“back to fitness”), a package of treatment by a spinal manipulator (chiropractor, osteopath, or physiotherapist), or manipulation followed by exercise Conclusions |
In other words, none of them worked very well. The paper failed to distinguish between manipulation by physiotherapists, chiropractors and osteopaths and so missed a valuable chance to find out whether there is an advantage to employing people from alternative medicine (the very problem that this NICE guidance should have dealt with)
Steve Vogel, another member of the guidance development group, is an osteopath. Osteopathy has cast off its shady origins better than chiropractic, but it remains a largely evidence-free zone, and is still usually classified as alternative medicine.
Peter Dixon DC FCC FBCA is chairman of the General Chiropractic Council and founder of Peter Dixon Associates. They run six chiropractic clinics. The claims made by these clinics on their web site are mostly related to musculo-skeletal conditions (not, all spine-related however). But they also include
“Chiropractic is also suitable for relieving the symptoms of stress, and optimizing the way the body works is one of the best ways of enhancing health and wellbeing.”
I wonder how they could justify that claim? Then we get
A chiropractor is always willing to discuss individual conditions or answer questions in order to assess whether chiropractic may be of benefit.
Thanks for the invitation. I accepted it. After the first two phone calls, I had learned all I needed.
The first of Peter Dixon’s clinics that I called, was asked about my son who was suffeiing from perpetual colic. I asked for advice. I was put through to the chiropractor. Here are some extracts from the conversation.
“I think now it’s termed irritable baby syndrome. . . . . We’ve found chiropractic is very effective for colic . . . . £50 up to 3/4 hour which would involve taking a case history, examining the baby, with regard to seeing how the joints in the spine work because often colic is down to, er um, faulty movement patterns in the spine. We deal with an awful lot of things to do with the frame -how the spine moves -and it’s often problems with the way that the bones of the spine move in infants and babies that is the underlying cause in colicky symptoms. . . usually on the whole, I’ve shot myself in the foot by saying this in the past, if there are -um when I say back problems they’re usually temporary issues -when they are there the response for most babies is quite quick . . . it depends on how it’s related to what’s gone on in the birth process -there is usually some traumatic cause and it usually sets up a problem in the upper neck or the mid-back and that will drive those colic symptoms. . . . Yes it’s quite a straightforward thing we just check the baby’s spine and see if it’s problem we can deal with or not.”
Yes, I think you just shot yourself in the foot again. I have no idea in what fraction of cases a chiropractor would fail to claim that it was a case that they could deal with. At least that possibility was envisaged. But when I asked where he’d refer me to in such case I was told it might be a result of bottle feeding -“what they consume”. So I expect it would have been sent to some sort of “nutritional therapist” who would have used one of their usual battery of unreliable tests for food allergies.
I tried a second clinic in Peter Dixon’s empire and asked if chiropractic could help with asthma.”It can do, depending on what type of asthma you have". After some questions I was asked
“Do you have any general aches and pains otherwise, any tension .problems round the rib cage or thoracic spine . . . There are two things we’d look as chiropractors as to whether we could help or not and that would include the tension round the rib cage -in any type of asthma you’ll become tight round the rib cage and merely by keeping that area loose you’d help to stop the asthma from becoming quite as bad. And the second part is we’d look at the neck area with you to see if there is any restriction there -which houses the nerve supply to the lungs which can be indicated in some asthma cases also.”
I was invited to come for a free screen, so I asked if it usually worked quickly, “It depends what the problem is but you’d need a course I suspect”. £45 for the first appointment then £28 per session. “In most cases you’d need to look at a six to eight session course”.
Would anyone with experience of crying babies or of asthma like to comment on these proposed treatments? They are not my idea of evidence-based treatments and I find it quite surprising that someone who sponsors them is thought appropriate to write guidance for NICE.
This sort of ‘sting’ always makes me feel a bit uneasy, but it seems to be the only way to find out what actually goes on. And what goes on has all the appearance of classic bait and switch. You go in for your backache, and before you know where you are you are being sold a course of treatment to stop your baby crying.
Media follow-up after the NICE announcement
Sadly, I heard that the Today programme (my favourite news programme) was pretty wet. if only their science reporting was as good as their politics reporting.
The 27th May was certainly pretty busy for me, Apart from a couple of local paper interviews, this is what happened,
Sky News TV. Richard Suchet and two cameraman came to UCL and filmed a lot of stuff out of which a 20 second clip was used. And then they grumble that they don’t make money.
BBC TV 6 o’clock News. Similar, but at least only two people this time. Both TV stations spent ages showing pictures of people having needles pushed into them and very little time discussing the problems. A pathetically bad attempt at science reporting. Radio, on the whole, did much better
BBC Three Counties Radio (09.20) Host Ronnie Barbour, The daytime talk shows may be appalling to some of us, but the hosts did a far better job of airing the problems than TV [download the mp3].
Radio 5 Live Victoria Derbyshire [download the mp3]
BBC Radio Sheffield (12.05) was the best talk show by far. First speaker was Steve Vogel, the osteopath from the guidance development group. Although invited by the rather sensible host, Rony, to respond to the idea that a secondary consequence of the guidance would be to introduce hocus-pocus, he steadfastly refused to answer the question. At the end a rather sensible GP summed up the view from the coalface. [play the mp3]
Radio 4 PM programme This excellent early evening news programme is run by Eddie Mair. It was the best interview yet. The other side was put by Martin Underwood, chair of the guidance development group [play the mp3]
Underwood said “the evidence shows that it [acupuncture] works”. I disagree. The evidence shows that acupuncture, in a non-blind comparison with no acupuncture shows a small, variable additional effect that doesn’t last and is of marginal clinical significance, That is not what I call “works”. Underwood then indulges in the subgroup analysis fallacy by asserting that a few people get a large benefit from acupuncture. Or perhaps a few people just happen to get better that day. I was not convinced.
More 4 News TV 20.20 was an interview, with the other side being put by my old friend, George Lewith.
During the introduction, an acupuncturist. Lisa Sherman, ‘explained’ acupuncture in the usual sort of utterly meaningless words that illustrate perfectly the problem.
George Lewith said that “we don’t have a good pretend form of acupuncture”. “We don’t have a good placebo and we can demonstrate that acupuncture is literally twice as effective as conventional care”. The first is simply nonsense: huge efforts have gone into developing good controls in acupuncture studies (see, for example, Barker Bausell’s book, Snake Oil Science). And I hope that George will send the references for his “twice as effective” claim. It seems to me to be nothing short of preposterous.
My conclusions
So what went wrong?
One problem could be regarded as medical arrogance. The fact is that the problem of low back pain has not been solved, either by drugs or anything else. It is a failure of medicine (and of pharmacology). That should be the premise of all discussions, and it smacks of arrogance not to tell people straight out. Of course there are some cases when causes can be identified, and perhaps remedied, usually by surgery, but these are the exceptions not the rule.
One consequence of the inability of medicine to help much is that patients get desperate, and willing to try anything. And of course if they happen to have a remission, that is attributed to the treatment, however preposterous that treatment may have been. Conditions like back pain that come and go unpredictable are a gift for quacks.
Another consequence, for researchers rather than patients, is to clutch at straws. Even small and inconsistent effects are seized on as ‘successes’. This phenomenon seems to be part of the reason for the NICE guidance. Another reason is, almost certainly, the grinding of axes by some of the people who wrote it.
What should be done now?
Professor Sir Michael Rawlins is a sensible chap. He cares about evidence, But it does seem that in this case, he might have taken his eye off the ball, for once. In my opinion, he should restore the reputation of NICE by withdrawing this guidance and starting again.
Follow-up
An interesting document has come my way. It shows the responses of the guidance group to the consultation on the draft guidance. Many people made comments not unlike mone, but they were all brushed aside in a way that looks to me rather partisan. The document appears to have vanished from NICE’s web site, but you can download it here.
Friday 29th May. The Times prints a letter from two consultants in pain medicine, Joan Hestor and Stephen Ward. It says, inter alia
“As experienced pain specialists we feel that NICE has lost its way in publishing these guidelines.”
“We are saddened that NICE has chosen to ignore our important role and promote seemingly unworkable and for the most part clinically ineffective treatments”
Friday 29th May. NICE has had a good reputation in the USA for its important, and usually high-quality, attempts to assess what works and what doesn’t. That makes it all the sadder to see it condemned already from the USA for its latest effort. The excellent Yale neurologist, Steven Novella, has written about it on his Neurologica blog.
Friday 29th May. A correspondent points out that the costings of the guidance can be found on the NICE web site. Table 1 has a strong air of make-believe.
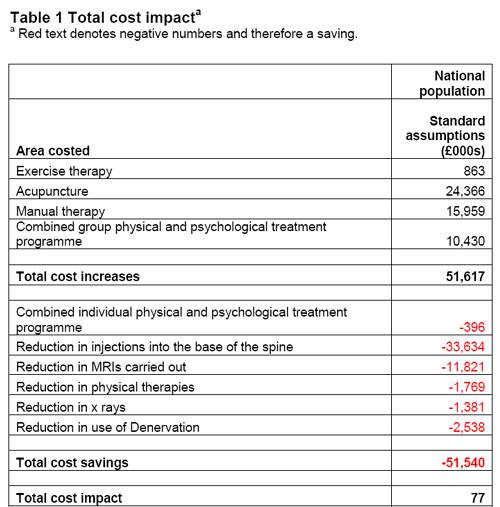
The Daily Mail (29 May 2009). Their article quotes serious criticisms of NICE.
Dr Ron Cooper, past chairman of the group and a consultant pain specialist in Northern Ireland, said: ‘I have never known so many pain medicine specialists to be so furious. More patients will end up having more expensive surgery, which is unnecessary, risky and has worse results.
‘NICE made it difficult for us to submit evidence to a committee on which there was not one experienced pain physician.
‘The guidelines will make us the laughing stock of Europe, Australia and the U.S. where pain specialists will continue to have full access to a wide range of treatments.’
Chirowatch suspended. 30 May 2009. The invaluable chiro-watch site, http://www.chirowatch.com, run by Dr Canadian physician, Dr Tom Polevoy, has been “suspended”. In fact the whole of his domain, healthwatcher.net, has been disabled. It seems that this was the result of a legal threat to his ISP, not by chiropractors this time, but by William O’Neill of the Canadian Cancer Research Group, which is far from being what the respectable-sounding title suggests, according to Dr Stephen Barrett. The site will be back soon, I’m told. Meanwhile you can read the suspended page here, and the only result of their hamfisted bullying will be to vastly increase the number of people who read it. You can read lots more at Quackwatch’s chirobase and at ebm-first.
A new blog, Not as NICE as you think appeared on May 30th. It is written by a pain physician, Stephen Ward. and is devoted to pointing out the serious problems raised by NICE’s guidance. It starts with the (very critical) World Institute of Pain Press Release.
British Medical Journal has more flak for the NICE guidelines
And the BMJ has published a letter signed by 50 consultants in pain medicine, NICE guidelines on low back pain are flawed.(this will probably appear as a letter in the print edition of the BMJ).
First the MHRA lets down the public by allowing deceptive labelling of sugar pills (see here, and this this blog). Now it is the turn of NICE to betray its own principles.
The National Institute for Health and Clinical Excellence (NICE) describes its job thus
“NICE is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health.”
Its Guidance document on Low Back Pain will be published on Wednesday 27 May 2009, but the newspapers have already started to comment, presumably on the assumption that it will have changed little from the Draft Guidance of September 2008. These comments may have to be changed as soon as the final version becomes available.
The draft guidance, though mostly sensible, has two recommendations that I believe to be wrong and dangerous. The recommendations include (page 7) these three.
- Consider offering a course of manual therapy including spinal manipulation of up to 9 sessions over up to 12 weeks.
- Consider offering a course of acupuncture needling comprising up to 10 sessions over a period of up to 12 weeks.
- Consider offering a structured exercise programme tailored to the individual.
All three of this options are accompanied by a footnote that reads thus.
“A choice of any of these therapies may be offered, taking into account patient preference.”
On the face if it, this might seem quite reasonable. All three choices seem to be about as effective (or ineffective) as each other, so why not let patients choose between them?
Actually there are very good reasons, but NICE does not seem to have thought about them. In the past I have had a high opinion of NICE but it seems that even they are now getting bogged down in the morass of political correctness and officialdom that is the curse of the Department of Health. It is yet another example of DC’s rule number one.
Never trust anyone who uses the word ‘stakeholder’.
They do use it, often.
So what is so wrong?
For a start, I take it that the reference to “spinal manipulation” in the first recommendation is a rather cowardly allusion to chiropractic. Why not say so, if that’s whar you mean? Chiropractic is mentioned in the rest of the report but the word doesn’t seem to occur in the recommendations. Is NICE perhaps nervous that it would reduce the credibility of the report if the word chiropractic were said out loud?
Well, they have a point, I suppose. It would.
That aside, here’s what’s wrong.
The Evidence
I take as my premise that the evidence says that no manipulative therapy has any great advantage over the others. They are all more or less equally effective. Perhaps I should say, more or less equally ineffective, because anyone who claims to have the answer to low back pain is clearly deluded (and I should know: nobody has fixed mine yet). So for effectiveness there are no good grounds to choose between exercise, physiotherapy, acupuncture or chiropractic. There is, though, an enormous cultural difference. Acupuncture and chiropractic are firmly in the realm of alternative medicine. They both invoke all sorts of new-age nonsense for which there isn’t the slightest good evidence. That may not poison your body, but it certainly poisons your mind.
Acupuncturists talk about about “Qi”, “meridians”, “energy flows”. The fact that “sham” and “real” acupuncture consistently come out indistinguishable is surely all the evidence one needs to dismiss such nonsense. Indeed there is a small group of medical acupuncturists who do dismiss it. Most don’t. As always in irrational subjects, acupuncture is riven by internecine strife between groups who differ in the extent of their mystical tendencies,
Chiropractors talk of “subluxations”, an entirely imaginary phenomenon (but a cause of much unnecessary exposure to X-rays). Many talk of quasi-religious things like “innate energy”. And Chiropractic is even more riven by competing factions than acupuncture. See, for example, Chiropractic wars Part 3: internecine conflict.
The bait and switch trick
This is the basic trick used by ‘alternative therapists’ to gain respectability.
There is a superb essay on it by the excellent Yale neurologist Steven Novella: The Bait and Switch of Unscientific Medicine. The trick is to offer some limited and reasonable treatment (like back manipulation for low back pain). This, it seems, is sufficient to satisfy NICE. But then, once you are in the showroom, you can be exposed to all sorts of other nonsense about “subluxations” or “Qi”. Still worse, you will also be exposed to the claims of many chiropractors and acupuncturists to be able to cure all manner of conditions other than back pain. But don’t even dare to suggest that manipulation of the spine is not a cure for colic or asthma or you may find yourself sued for defamation. The shameful legal action of the British Chiropractic Association against Simon Singh (follow it here) led to an addition to DC’s Patients’ Guide to Magic Medicine.
(In the face of such tragic behaviour, one has to be able to laugh).
Libel: A very expensive remedy, to be used only when you have no evidence. Appeals to alternative practitioners because truth is irrelevant.
NICE seems to have fallen for the bait and switch trick, hook line and sinker.
The neglected consequences
Once again, we see the consequences of paying insufficient attention to the Dilemmas of Alternative Medicine.
The lying dilemma
If acupuncture is recommended we will have acupuncturists telling patients about utterly imaginary things like “Qi” and “meridians”. And we will have chiropractors telling them about subluxations and innate energy. It is my opinion that these things are simply make-believe (and that is also the view of a minority of acupuncturist and chiropractors). That means that you have to decide whether the supposed benefits of the manipulation are sufficient to counterbalance the deception of patients.
Some people might think that it was worth it (though not me). What is unforgivable is not to consider even the question. The NICE guidance says not a word about this dilemma. Why not?
The training dilemma
The training dilemma is even more serious. Once some form of alternative medicine has successfully worked the Bait and Switch trick and gained a toehold in the NHS, there will be an army of box-ticking HR zombies employed to ensure that they have been properly trained in “subluxations” or “Qi”. There will be quangos set up to issue National Occupational Standards in “subluxations” or “Qi”. Skills for Health will issue “competences” in “subluxations” or “Qi” (actually they already do). There will be courses set up to teach about “subluxations” or “Qi”, some even in ‘universities’ (there already are).
The respectability problem
But worst of all, it will become possible for aupuncturists and chiropractors to claim that they now have official government endorsement from a prestigious evidence-based organisation like NICE for “subluxations” or “Qi”. Of course this isn’t true. In fact the words “subluxations” or “Qi” are not even mentioned in the draft report. That is the root of the problem. They should have been. But omitting stuff like that is how the Bait and Switch trick works.
Alternative medicine advocates crave, above all, respectability and acceptance. It is sad that NICE seems to have given them more credibility and acceptance without having considered properly the secondary consequences of doing so,
How did this failure of NICE happen?
It seems to have been a combination of political correctness, failure to consider secondary consequences, and excessive influence of the people who stand to make money from the acceptance of alternative medicine.
Take, for example, the opinion of the British Pain Society. This organisation encompasses not just doctors. It
includes “doctors, nurses, physiotherapists, scientists, psychologists, occupational therapists and other healthcare professionals actively engaged in the diagnosis and treatment of pain and in pain research for the benefit of patients”. Nevertheless, their response to the draft guidelines pointed out that the manipulative therapies as a whole were over-represented.
|
Manipulation The guidelines assess 9 large groups of interventions of which manual therapies are only one part. The full GDG members panel of 13 individuals included two proponents of spinal manipulation/mobilisation (P Dixon and S Vogel). In addition, the chair of the panel (M Underwood) is the lead author of the UKBEAM trial on which the positive recommendation for |
It seems that the Pain Society were quite right.
LBC 97.3 Breakfast Show (25 May 2009) had a quick discussion on acupuncture (play mp3 file). After I had my say, the other side was put by Rosey Grandage. She has (among other jobs) a private acupuncture practice so she is not quite as unbiassed as me). As usual, she misrepresents the evidence by failing to distinguish between blind and non-blind studies. She also misrepresented what I said by implying that I was advocating drugs. That was not my point and I did not mention drugs (they, like all treatments, have pretty limited effectiveness, and they have side effects too). She said “there is very good evidence to show they (‘Qi’ and ‘meridians’] exist”. That is simply untrue.
There can’t be a better demonstration of the consequences of falling for bait and switch than the defence mounted by Rosey Grandage. NICE may not mention “Qi” and “meridians”; but the people they want to allow into the NHS have no such compunctions.
I first came across Rosey Grandage when I discovered her contribution to the Open University/BBC course K221. That has been dealt with elsewhere. A lot more information about acupuncture has appeared since then. She doesn’t seem to have noticed it. Has she not seen the Nordic Cochrane Centre report? Nor read Barker Bausell, or Singh & Ernst? Has she any interest in evidence that might reduce her income? Probably not.
Where to find out more
An excellent review of chiropractic can be found at the Layscience site. It was written by the indefatigable ‘Blue Wode’ who has provided enormous amounts of information at the admirable ebm-first site (I am authorised to reveal that ‘Blue Wode’ is the author of that site). There you will also find much fascinating information about both acupuncture and about chiropractic.
I’m grateful to ‘Blue Wode’ for some of the references used here.