Fair trading
The Scottish Universities Medical Journal asked me to write about the regulation of alternative medicine. It’s an interesting topic and not easy to follow because of the veritable maze of more than twenty overlapping regulators and quangos which fail utterly to protect the public against health fraud. In fact they mostly promote health fraud. The paper is now published, and here is a version with embedded links (and some small updates).
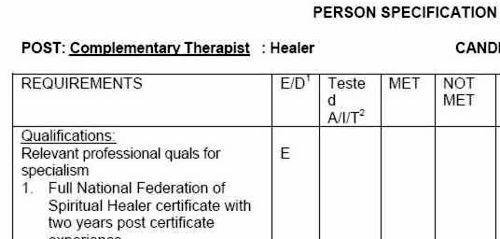
We are witnessing an increasing commercialisation of medicine. It’s really taken off since the passage of the Health and Social Security Bill into law. Not only does that mean having NHS hospitals run by private companies, but it means that “any qualified provider” can bid for just about any service. The problem lies, of course, in what you consider “qualified” to mean. Any qualified homeopath or herbalist will, no doubt, be eligible. University College London Hospital advertised for a spiritual healer. The "person specification" specified a "quallfication", but only HR people think that a paper qualification means that spiritual healing is anything but a delusion.
The vocabulary of bait and switch
First, a bit of vocabulary. Alternative medicine is a term that is used for medical treatments that don’t work (or at least haven’t been shown to work). If they worked, they’d be called “medicine”. The anti-malarial, artemesinin, came originally from a Chinese herb, but once it had been purified and properly tested, it was no longer alternative. But the word alternative is not favoured by quacks. They prefer their nostrums to be described as “complementary” –it sounds more respectable. So CAM (complementary and alternative medicine became the politically-correct euphemism. Now it has gone a stage further, and the euphemism in vogue with quacks at the moment is “integrated” or “integrative” medicine. That means, very often, integrating things that don’t work with things that do. But it sounds fashionable. In reality it is designed to confuse politicians who ask for, say, integrated services for old people.
Put another way, the salespeople of quackery have become rather good at bait and switch. The wikepedia definition is as good as any.
Bait-and-switch is a form of fraud, most commonly used in retail sales but also applicable to other contexts. First, customers are “baited” by advertising for a product or service at a low price; second, the customers discover that the advertised good is not available and are “switched” to a costlier product.
As applied to the alternative medicine industry, the bait is usually in the form of some nice touchy-feely stuff which barely mentions the mystical nonsense. But when you’ve bought into it you get the whole panoply of nonsense. Steven Novella has written eloquently about the use of bait and switch in the USA to sell chiropractic, acupuncture, homeopathy and herbal medicine: "The bait is that CAM offers legitimate alternatives, the switch is that it primarily promotes treatments that don’t work or are at best untested and highly implausible.".
The "College of Medicine" provides a near-perfect example of bait and switch. It is the direct successor of the Prince of Wales’ Foundation for Integrated Health. The Prince’s Foundation was a consistent purveyor of dangerous medical myths. When it collapsed in 2010 because of a financial scandal, a company was formed called "The College for Integrated Health". A slide show, not meant for public consumption, said "The College represents a new strategy to take forward the vision of HRH Prince Charles". But it seems that too many people have now tumbled to the idea that "integrated", in this context, means barmpottery. Within less than a month, the new institution was renamed "The College of Medicine". That might be a deceptive name, but it’s a much better bait. That’s why I described the College as a fraud and delusion.
Not only did the directors, all of them quacks, devise a respectable sounding name, but they also succeeded in recruiting some respectable-sounding people to act as figureheads for the new organisation. The president of the College is Professor Sir Graham Catto, emeritus professor of medicine at the University of Aberdeen. Names like his make the bait sound even more plausible. He claims not to believe that homeopathy works, but seems quite happy to have a homeopathic pharmacist, Christine Glover, on the governing council of his college. At least half of the governing Council can safely be classified as quacks.
So the bait is clear. What about the switch? The first thing to notice is that the whole outfit is skewed towards private medicine: see The College of Medicine is in the pocket of Crapita Capita. The founder, and presumably the main provider of funds (they won’t say how much) is the huge outsourcing company, Capita. This is company known in Private Eye as Crapita. Their inefficiency is legendary. They are the folks who messed up the NHS computer system and the courts computer system. After swallowing large amounts of taxpayers’ money, they failed to deliver anything that worked. Their latest failure is the court translation service.. The president (Catto), the vice president (Harry Brunjes) and the CEO (Mark Ratnarajah) are all employees of Capita.
The second thing to notice is that their conferences and courses are a bizarre mixture of real medicine and pure quackery. Their 2012 conference had some very good speakers, but then it had a "herbal workshop" with Simon Mills (see a video) and David Peters (the man who tolerates dowsing as a way to diagnose which herb to give you). The other speaker was Dick Middleton, who represents the huge herbal company, Schwabe (I debated with him on BBC Breakfast), In fact the College’s Faculty of Self-care appears to resemble a marketing device for Schwabe.
Why regulation isn’t working, and can’t work
There are various levels of regulation. The "highest" level is the statutory regulation of osteopathy and chiropractic. The General Chiropractic Council (GCC) has exactly the same legal status as the General Medical Council (GMC). This ludicrous state of affairs arose because nobody in John Major’s government had enough scientific knowledge to realise that chiropractic, and some parts of osteopathy, are pure quackery,
The problem is that organisations like the GCC function more to promote chiropractic than to regulate them. This became very obvious when the British Chiropractic Association (BCA) decided to sue Simon Singh for defamation, after he described some of their treatments as “bogus”, “without a jot of evidence”.
In order to support Singh, several bloggers assessed the "plethora of evidence" which the BCA said could be used to justify their claims. When, 15 months later, the BCA produced its "plethora" it was shown within 24 hours that the evidence was pathetic. The demolition was summarised by lawyer, David Allen Green, in The BCA’s Worst Day.
In the wake of this, over 600 complaints were made to the GCC about unjustified claims made by chiropractors, thanks in large part to heroic work by two people, Simon Perry and Allan Henness. Simon Perry’s Fishbarrel (browser plugin) allows complaints to be made quickly and easily -try it). The majority of these complaints were rejected by the GCC, apparently on the grounds that chiropractors could not be blamed because the false claims had been endorsed by the GCC itself.
My own complaint was based on phone calls to two chiropractors, I was told such nonsense as "colic is down to, er um, faulty movement patterns in the spine". But my complaint never reached the Conduct and Competence committee because it had been judged by a preliminary investigating committee that there was no case to answer. The impression one got from this (very costly) exercise was that the GCC was there to protect chiropractors, not to protect the public.
The outcome was a disaster for chiropractors, wno emerged totally discredited. It was also a disaster for the GCC which was forced to admit that it hadn’t properly advised chiropractors about what they could and couldn’t claim. The recantation culminated in the GCC declaring, in August 2010, that the mythical "subluxation" is a "historical concept " "It is not supported by any clinical research evidence that would allow claims to be made that it is the cause of disease.". Subluxation was a product of the fevered imagination of the founder of the chiropractic cult, D.D. Palmer. It referred to an imaginary spinal lesion that he claimed to be the cause of most diseases. .Since ‘subluxation’ is the only thing that’s distinguished chiropractic from any other sort of manipulation, the admission by the GCC that it does not exist, after a century of pretending that it does, is quite an admission.
The President of the BCA himself admitted in November 2011
“The BCA sued Simon Singh personally for libel. In doing so, the BCA began one of the darkest periods in its history; one that was ultimately to cost it financially,”
As a result of all this, the deficiencies of chiropractic, and the deficiencies of its regulator were revealed, and advertisements for chiropractic are somewhat less misleading. But this change for the better was brought about entirely by the unpaid efforts of bloggers and a few journalists, and not at all by the official regulator, the GCC. which was part of the problem. not the solution. And it was certainly not helped by the organisation that is meant to regulate the GCC, the Council for Health Regulatory Excellence (CHRE) which did nothing whatsoever to stop the farce.
At the other end of the regulatory spectrum, voluntary self-regulation, is an even worse farce than the GCC. They all have grand sounding "Codes of Practice" which, in practice, the ignore totally.
The Society of Homeopaths is just a joke. When homeopaths were caught out recommending sugar pills for prevention of malaria, they did nothing (arguably such homicidal advice deserves a jail sentence).
The Complementary and Natural Healthcare Council (CNHC) is widely know in the blogosphere as Ofquack. I know about them from the inside, having been a member of their Conduct and Competence Committee, It was set up with the help of a £900,000 grant from the Department of Health to the Prince of Wales, to oversee voluntary self-regulation. It fails utterly to do anything useful.. The CNHC code of practice, paragraph 15 , states
“Any advertising you undertake in relation to your professional activities must be accurate. Advertisements must not be misleading, false, unfair or exaggerated”.
When Simon Perry made a complaint to the CNHC about claims being made by a CNHC-registered reflexologist, the Investigating Committee upheld all 15 complaints. But it then went on to say that there was no case to answer because the unjustified claims were what the person had been taught, and were made in good faith.
This is precisely the ludicrous situation which will occur again and again if reflexologists (and many other alternative therapies) are “accredited”. The CNHC said, correctly, that the reflexologist had been taught things that were not true, but then did nothing whatsoever about it apart from toning down the advertisements a bit. They still register reflexologists who make outrageously false claims.
Once again we see that no sensible regulation is possible for subjects that are pure make-believe.
The first two examples deal (or rather, fail to deal) with regulation of outright quackery. But there are dozens of other quangos that sound a lot more respectable.
European Food Standards Agency (EFSA). One of the common scams is to have have your favourite quack treatment classified as a food not as a medicine. The laws about what you can claim have been a lot laxer for foods. But the EFSA has done a pretty good job in stopping unjustified claims for health benefits from foods. Dozens of claims made by makers of probiotics have been banned. The food industry, needless to say, objects very strongly to be being forced to tell the truth. In my view, the ESFA has not gone far enough. They recently issued a directive about claims that could legally be made. Some of these betray the previously high standards of the EFSA. For example you are allowed to say that "Vitamin C contributes to the reduction of tiredness and fatigue" (as long as the product contains above a specified amount of Vitamin C. I’m not aware of any trials that show vitamin C has the slightest effect on tiredness or fatigue, Although these laws do not come into effect until December 2012, they have already been invoked by the ASA has a reason not to uphold a complaint about a multivitamin pill which claimed that it “Includes 8 nutrients that can contribute to the reduction in tiredness and fatigue”
The Advertising Standards Authority (ASA). This is almost the only organisation that has done a good job on false health claims. Their Guidance on Health Therapies & Evidence says
"Whether you use the words ‘treatment’, ‘treat’ or ‘cure’, all are likely to be seen by members of the public as claims to alleviate effectively a condition or symptom. We would advise that they are not used"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
They are spot on.
The ASA’s Guidance for Advertisers of Homeopathic Services is wonderful.
"In the simplest terms, you should avoid using efficacy claims, whether implied or direct,"
"To date, the ASA has have not seen persuasive evidence to support claims that homeopathy can treat, cure or relieve specific conditions or symptoms."
That seems to condemn the (mis)labelling allowed by the MHRA as breaking the rules.. Sadly, though, the ASA has no powers to enforce its decisions and only too often they are ignored. The Nightingale collaboration has produced an excellent letter that you can hand to any pharmacist who breaks the rules
The ASA has also judged against claims made by "Craniosacral therapists" (that’s the lunatic fringe of osteopathy). They will presumably uphold complaints about similar claims made (I’m ashamed to say) by UCLH Hospitals.
The private examination company Edexcel sets exams in antiscientific subjects, so miseducating children. The teaching of quackery to 16 year-olds has been approved by a maze of quangos, none of which will take responsibility, or justify their actions. So far I’ve located no fewer than eight of them. The Office of the Qualifications and Examinations Regulator (OfQual), Edexcel, the Qualifications and Curriculum Authority (QCA), Skills for Health, Skills for Care, National Occupational Standards (NOS), private exam company VTCT and the schools inspectorate, Ofsted.. Asking any of these people why they approve of examinations in imaginary subjects meets with blank incomprehension. They fail totally to protect tha public from utter nonsense.
The Department of Education has failed to do anything about the miseducation of children in quackery. In fact it has encouraged it by, for the first time, giving taxpayers’ money to a Steiner (Waldorf) school (at Frome, in Somerset). Steiner schools are run by a secretive and cult-like body of people (read about it). They teach about reincarnation, karma, gnomes, and all manner of nonsense, sometimes with unpleasant racial overtones. The teachers are trained in Steiner’s Anthroposophy, so if your child gets ill at school they’ll probably get homeopathic sugar pills. They might well get measles or mumps too, since Steiner people don’t believe in vaccination.
Incredibly, the University of Aberdeen came perilously close to appointing a chair in anthroposophical medicine. This disaster was aborted by bloggers, and a last minute intervention from journalists. Neither the university’s regulatory mechanisms. nor any others, seemed to realise that a chair in mystical barmpottery was a bad idea.
Trading Standards offices and the Office of Fair Trading.
It is the statutory duty of Trading Standards to enforce the Consumer Protection Regulations (2008) This European legislation is pretty good. it caused a lawyer to write " Has The UK Quietly Outlawed “Alternative” Medicine?". Unfortunately Trading Standards people have consistently refused to enforce these laws. The whole organisation is a mess. Its local office arrangement fails totally to deal with the age of the internet. The situation is so bad that a group of us decided to put them to the test. The results were published in the Medico-Legal Journal, Rose et al., 2012. "Spurious Claims for Health-care Products: An Experimental Approach to Evaluating Current UK Legislation and its Implementation". They concluded "EU directive 2005/29/EC is
largely ineffective in preventing misleading health claims for consumer products in
the UK"
Skills for Health is an enormous quango which produces HR style "competences" for everything under the son. They are mostly quite useless. But those concerned with alternative medicine are not just useless. They are positively harmful. Totally barmy. There are competences and National Occupational Standards for every lunatic made-up therapy under the sun. When I phoned them to discover who’d written them, I learned that the had been drafted by the Prince of Wales’ Foundation for Magic Medicine. And when I joked by asking if they had a competence for talking to trees, I was told, perfectly seriously, “You’d have to talk to LANTRA, the land-based organisation for that.”
That was in January 2008. A lot of correspondence with the head of Skills for Health got nowhere at all. She understood nothing and it hasn’t improved a jot.
This organisation costs a lot of taxpayers’ money and it should have been consigned to the "bonfire of the quangos" (but of course there was no such bonfire in reality). It is a disgrace.
The Quality Assurance Agency (QAA) is supposed to ensure the quality of university courses. In fact it endorses courses in nonsense alternative medicine and so does more harm than good. The worst recent failure of the QAA was in the case of the University of Wales: see Scandal of the University of Wales and the Quality Assurance Agency. The university was making money by validating thousands of external degrees in everything from fundamentalist theology to Chinese Medicine. These validations were revealed as utterly incompetent by bloggers, and later by BBC Wales journalist Ciaran Jenkins (now working for Channel 4).
The mainstream media eventually caught up with bloggers. In 2010, BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. The programme can be seen on YouTube (Part 1, and Part 2). The programme also exposed, incidentally, the uselessness of the Quality Assurance Agency (QAA) which did nothing until the scam was exposed by TV and blogs. Eventually the QAA sent nine people to Malaysia to investigate a dodgy college that had been revealed by the BBC. The trip cost £91,000. It could have been done for nothing if anyone at the QAA knew how to use Google.
The outcome was that the University of Wales stopped endorsing external courses, and it was soon shut down altogether (though bafflingly, its vice-chancellor, Marc Clement was promoted). The credit for this lies entirely with bloggers and the BBC. The QAA did nothing to help until the very last moment.
Throughout this saga Universities UK (UUK), has maintained its usual total passivity. They have done nothing whatsoever about their members who give BSc degrees in anti-scientific subjects. (UUK used to known as the Committee of Vice-Chancellors and Principals).
Council for Health Regulatory Excellence (CHRE), soon to become the PSAHSC,
Back now to the CHRE, the people who failed so signally to sort out the GCC. They are being reorganised. Their consultation document says
"The Health and Social Care Act 20122 confers a new function on the Professional Standards Authority for Health and Social Care (the renamed Council for Healthcare Regulatory Excellence). From November 2012 we will set standards for organisations that hold voluntary registers for people working in health and social care occupations and we will accredit the register if they meet those standards. It will then be known as an ‘Accredited Register’. "
They are trying to decide what the criteria should be for "accreditation" of a regulatory body. The list of those interested has some perfectly respectable organisations, like the British Psychological Society. It also contains a large number of crackpot organisations, like Crystal and Healing International, as well as joke regulators like the CNHC.
They already oversee the Health Professions Council (HPC) which is due to take over Herbal medicine and Traditional Chinese Medicine, with predictably disastrous consequences.
Two of the proposed criteria for "accreditation" appear to be directly contradictory.
Para 2.5 makes the whole accreditation pointless from the point of view of patients
2.5 It will not be an endorsement of the therapeutic validity or effectiveness of any particular discipline or treatment.
Since the only thing that matters to the patient is whether the therapy works (and is safe), accrediting of organisations that ignore this will merely give the appearance of official approval of crystal healing etc etc. This appears to contradict directly
A.7 The organisation can demonstrate that there either is a sound knowledge base underpinning the profession or it is developing one and makes that explicit to the public.
A "sound knowledge base", if it is to mean anything useful at all, means knowledge that the treatment is effective. If it doesn’t mean that, what does it mean?
It seems that the official mind has still not grasped the obvious fact that there can be no sensible regulation of subjects that are untrue nonsense. If it is nonsense, the only form of regulation that makes any sense is the law.
Please fill in the consultation. My completed return can be downloaded as an example, if you wish.
Medicines and Healthcare products Regulatory Agency (MHRA) should be a top level defender of truth. Its strapline is
"We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
The MHRA did something (they won’t tell me exactly what) about one of the most cruel scams that I’ve ever encountered, Esperanza Homeopathic Neuropeptide, peddled for multiple sclerosis, at an outrageous price ( £6,759 for 12 month’s supply). Needless to say there was not a jot of evidence that it worked (and it wasn’t actually homeopathic).
Astoundingly, Trading Standards officers refused to do anything about it.
The MHRA admit (when pushed really hard) that there is precious little evidence that any of the herbs work, and that homeopathy is nothing more than sugar pills. Their answer to that is to forget that bit about "ensuring that medicines … work"
Here’s the MHRA’s Traditional Herbal Registration Certificate for devils claw tablets.

The wording "based on traditional use only" has to be included because of European legislation. Shockingly, the MHRA have allowed them to relegate that to small print, with all the emphasis on the alleged indications. The pro-CAM agency NCCAM rates devil’s claw as "possibly effective" or "insufficient evidence" for all these indications, but that doesn’t matter because the MHRA requires no evidence whatsoever that the tablets do anything. They should, of course, added a statement to this effect to the label. They have failed in their duty to protect and inform the public by allowing this labelling.
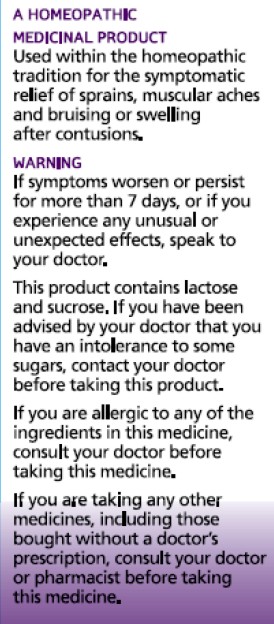
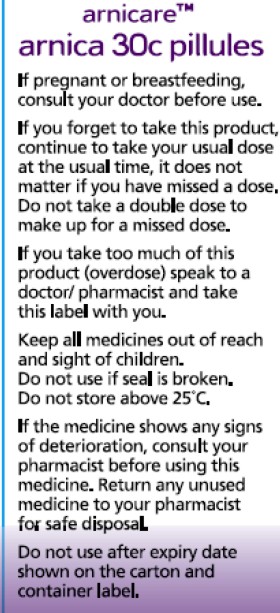
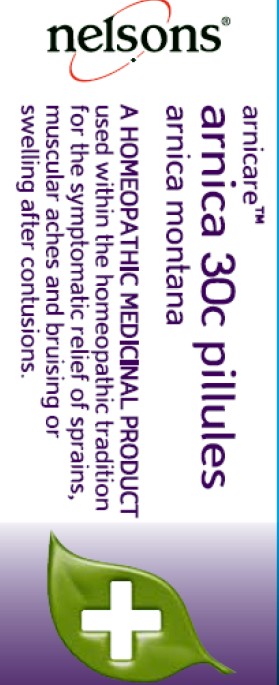
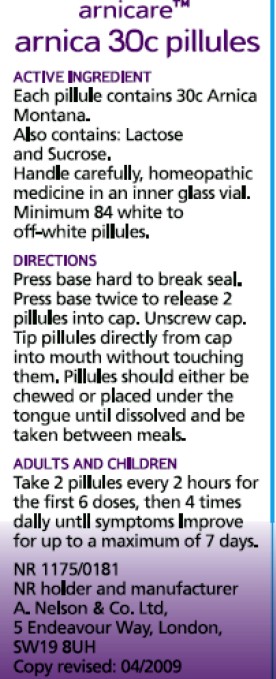
But it gets worse. Here is the MHRA’s homeopathic marketing authorisation for the homeopathic medicinal product Arnicare Arnica 30c pillules
It is nothing short of surreal.
|
|
Since the pills contain nothing at all, they don’t have the slightest effect on sprains, muscular aches or bruising. The wording on the label is exceedingly misleading.
If you "pregnant or breastfeeding" there is no need to waste you doctor’s time before swallowing a few sugar pills.
"Do not take a double dose to make up for a missed one". Since the pills contain nothing, it doesn’t matter a damn.
"If you overdose . . " it won’t have the slightest effect because there is nothing in them
And it gets worse. The MHRA-approved label specifies ACTIVE INGREDIENT. Each pillule contains 30c Arnica Montana
No, they contain no arnica whatsoever.
|
|
It truly boggles the mind that men with dark suits and lots of letters after their names have sat for hours only to produce dishonest and misleading labels like these.
When this mislabeling was first allowed, it was condemned by just about every scientific society, but the MHRA did nothing.
The Nightingale Collaboration.
This is an excellent organisation, set up by two very smart skeptics, Alan Henness and Maria MacLachlan. Visit their site regularly, sign up for their newsletter Help with their campaigns. Make a difference.
Conclusions
The regulation of alternative medicine in the UK is a farce. It is utterly ineffective in preventing deception of patients.
Such improvements as have occurred have resulted from the activity of bloggers, and sometime the mainstream media. All the official regulators have, to varying extents, made things worse.
The CHRE proposals promise to make matters still worse by offering "accreditation" to organisations that promote nonsensical quackery. None of the official regulators seem to be able to grasp the obvious fact that is impossible to have any sensible regulation of people who promote nonsensical untruths. One gets the impression that politicians are more concerned to protect the homeopathic (etc, etc) industry than they are to protect patients.
Deception by advocates of alternative medicine harms patients. There are adequate laws that make such deception illegal, but they are not being enforced. The CHRE and its successor should restrict themselves to real medicine. The money that they spend on pseudo-regulation of quacks should be transferred to the MHRA or a reformed Trading Standards organisation so they can afford to investigate and prosecute breaches of the law. That is the only form of regulation that makes sense.
Follow-up
The shocking case of the continuing sale of “homeopathic vaccines” for meningitis, rubella, pertussis etc was highlighted in an excellent TV programme by BBC South West. The failure of the MHRA and the GPC do take any effective action is a yet another illustration of the failure of regulators to do their job. I have to agree with Andy Lewis when he concludes
“Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator.”
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
This is another short interruption in the epic self-destruction of chiropractors. In a sense it is more serious. One expects quacks to advocate quackery. What you don’t expect is that the National Institute of Clinical Excellence (NICE) will endorse it. Neither do you expect the Medicines and Healthcare products Regulatory Agency (MHRA) to betray its mandate to make sure that medicines work.
The saga of the NICE low back pain guidance has been the subject of a deluge of criticism, It seems doubtful that the guidance can survive, not least because of its absurd endorsement of chiropractic, at a time when chiropractic is undergoing self-immolation as a consequence of the persecution of Simon Singh by the British Chiropractic Association (see here, and here, and here, and here and thousands of other sites).
The other betrayal has come to the for after the MHRA approved highly misleading labelling of a homeopathic preparation. At the time,
in 2006, when the principle was approved by the MHRA, just about every scientific organisation, even the Royal Society, condemned the action. What was discouraging that the clinical organisations all stayed silent. It is still a mystery why the MHRA made this enormous mistake, Some said that European regulations required it, but that is quite untrue, as Les Rose has shown. It appears to have been the result of a pusillanimous MHRA bowing to pressure from a deeply unscientific Department of Health (a letter from Caroline Flint at the time borders on the surreal).
On 20 May 2009, the British Medical Journal printed an article Drugs agency grants its first licence to homoeopathic product by Deborah Cohen (available free). The comments were mostly highly critical of the MHRA. The BMJ asked, as it does from time to time, for my comment to be converted to a letter
for the print edition. That isn’t freely available, so here it is.
|
Published 9 June 2009, doi:10.1136/bmj.b2333 LettersHomoeopathic product licenceMHRA label seems to be illegalThe strap line for the Medicines and Healthcare products Regulatory Agency (MHRA) is “We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe.” Yet the MHRA has made mockery of its own aims by ignoring the bit about “ensuring that medicines work” and allowing Arnica 30C pills to be labelled: “a homoeopathic medicinal product used within the homoeopathic tradition for the symptomatic relief of sprains, muscular aches, and bruising or swelling after contusions.”1 This label should be illegal anyway because the pills contain no trace of the ingredient on the label, but this deceit has been allowed through a legal loophole for a long time now. If you sold strawberry jam that contained not a trace of strawberry you’d be in trouble. But I can see no legal loophole that allows the manufacturers of Arnica 30C to evade the provisions of the Consumer Protection from Unfair Trading Regulations 2008. One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction, or malformations.” The consumer protection laws apply to the way that “the average consumer” will interpret the label. The average consumer is unlikely to know that “used within the homoeopathic tradition” is a form of weasel words that actually means “there isn’t a jot of evidence that the medicine works.” Since there is not the slightest evidence that Arnica 30C pills provide symptomatic relief of sprains, etc, the labelling that the MHRA has approved seems to be illegal. The MHRA is not selling anything itself, so I presume that it won’t find itself in court, but anyone who follows its advice could well do so. Cite this as: BMJ 2009;338:b2333 David Colquhoun, research professor1 University College London, London WC1E 6BT Competing interests: None declared. References |
It is, I suppose, just a sign of the chaos that reigns in the multiple agencies and quangos responsible for ‘regulation’ that one arm of government proposes action that a different branch would consider illegal. That is an inevitable consequence of trying to regulate something without first deciding whether it is nonsense or not. The Department of Health appears to be quite incapable of grasping this simple and obvious fact.
Follow-up
Health: best treatments. The Guardian seems to the be picking up BMJ stories and ran this one.
| The Prince of Wales’ Foundation for Integrated Health (FiH) is a propaganda organisation that aims to persuade people, and politicians, that the Prince’s somewhat bizarre views about alternative medicine should form the basis of government health policy.
His attempts are often successful, but they are regarded by many people as being clearly unconstitutional. |
 |
The FiH’s 2009 AnnualConferen ce conference was held at The King’s Fund, London 13 – 14 May 2009. It was, as always, an almost totally one-sided affair devoted to misrepresentation of evidence and the promotion of magic medicine. But according to the FiH, at least, it was a great success. The opening speech by the Quacktitioner Royal can be read here. It has already been analysed by somebody who knows rather more about medicine than HRH. He concludes
“It is a shocking perversion of the real issues driven by one man; unelected, unqualified and utterly misguided”.
We are promised some movie clips of the meeting. They might even make a nice UK equivalent of “Integrative baloney @ Yale“.
This post is intended to provide some background information about the speakers at the symposium. But let’s start with what seems to me to be the real problem. The duplicitous use of the word “integrated” to mean two quite different things.
The problem of euphemisms: spin and obfuscation
One of the problems of meetings like this is the harm done by use of euphemisms. After looking at the programme, it becomes obvious that there is a rather ingenious bit of PR trickery going on. It confuses (purposely?) the many different definitions of the word “integrative” . One definition of “Integrative medicine” is this (my emphasis).
” . . . orienting the health care process to engage patients and caregivers in the full range of physical, psychological, social, preventive, and therapeutic factors known to be effective and necessary for the achievement of optimal health.”
That is a thoroughly admirable aim. And that, I imagine, is the sense in which several of the speakers (Marmot, Chantler etc) used the term. Of course the definition is rather too vague to be very helpful in practice, but nobody would dream of objecting to it.
But another definition of the same term ‘integrative medicine’ is as a PR-friendly synonym for ‘alternative medicine’, and that is clearly the sense in which it is used by the Prince of Wales’ Foundation for Integrated Health (FIH), as is immediately obvious from their web site.
The guide to the main therapies supports everything from homeopathy to chiropractic to naturopathy, in a totally uncritical way. Integrated service refers explicitly to integration of ‘complementary’ medicine, and that itself is largely a euphemism for alternative medicine. For example, the FIH’s guide to homeopathy says
“What is homeopathy commonly used for?
Homeopathy is most often used to treat chronic conditions such as asthma; eczema; arthritis; fatigue disorders like ME; headache and migraine; menstrual and menopausal problems; irritable bowel syndrome; Crohn’s disease; allergies; repeated ear, nose, throat and chest infections or urine infections; depression and anxiety.”
But there is not a word about the evidence, and perhaps that isn’t surprising because the evidence that it works in any of these conditions is essentially zero.
The FIH document Complementary Health Care: A Guide for Patients appears to have vanished from the web after its inaccuracy received a very bad press, e.g. in the Times, and also here. It is also interesting that the equally widely criticised Smallwood report (also sponsored by the Prince of Wales) seems to have vanished too).
The programme for the meeting can be seen here, for Day 1, and Day 2
Conference chair Dr Phil Hammond, GP, comedian and health service writer. Hammond asked the FIH if I could speak at the meeting to provide a bit of balance. Guess what? They didn’t want balance.
09:30 Opening session
Dr Michael Dixon OBE
09:30 Introduction: a new direction for The Prince’s Foundation for Integrated Health and new opportunities in integrated health and care. Dr Michael Dixon, Medical Director, FIH
Michael Dixon is devoted to just about every form of alternative medicine. As well as being medical director of the Prince’s Foundation he also runs the NHS Alliance. Despite its name, the NHS Alliance is nothing to do with the NHS and acts, among other things, as an advocate of alternative medicine on the NHS, about which it has published a lot.
Dr Dixon is also a GP at College Surgery, Cullompton, Devon, where his “integrated practice” includes dozens of alternative practitioners. They include not only disproven things like homeopathy and acupuncture, but also even more bizarre practitioners in ‘Thought Field Therapy‘ and ‘Frequencies of Brilliance‘.
To take only one of these, ‘Frequencies of Brilliance’ is bizarre beyond belief. One need only quote its founder and chief salesperson.
“Frequencies of Brilliance is a unique energy healing technique that involves the activation of energetic doorways on both the front and back of the body.”
“These doorways are opened through a series of light touches. This activation introduces high-level Frequencies into the emotional and physical bodies. It works within all the cells and with the entire nervous system which activates new areas of the brain.”
“Frequencies of Brilliance is a 4th /5th dimensional work. The process is that of activating doorways by lightly touching the body or working just above the body.”
“Each doorway holds the highest aspect of the human being and is complete in itself. This means that there is a perfect potential to be accessed and activated throughout the doorways in the body.”
Best of all, it can all be done at a distance (that must help sales a lot). One is reminded of the Skills for Health “competence” in distant healing (inserted on a government web site at the behest (you guessed it) of the Prince’s Foundation, as related here)
“The intent of a long distance Frequencies of Brilliance (FOB) session is to enable a practitioner to facilitate a session in one geographical location while the client is in another.
A practitioner of FOB that has successfully completed a Stage 5 Frequency workshop has the ability to create and hold a stable energetic space in order to work with a person that is not physically present in the same room.
The space that is consciously created in the Frequencies of Brilliance work is known as the “Gap”. It is a space of nonlinear time. It contains ”no time and no space” or respectively “all time and all space”. Within this “Gap” a clear transfer of the energies takes place and is transmitted to an individual at a time and location consciously intended. Since this dimensional space is in non-linear time the work can be performed and sent backward or forward in time as well as to any location.
The Frequencies of Brilliance work cuts through the limitations of our physical existence and allows us to experience ourselves in other dimensional spaces. Therefore people living in other geographic locations than a practitioner have an opportunity to receive and experience the work.
The awareness of this dimensional space is spoken about in many indigenous traditions, meditation practices, and in the world of quantum physics. It is referred to by other names such as the void, or vacuum space, etc.”
This is, of course, preposterous gobbledygook. It, and other things in Dr Dixon’s treatment guide, seem to be very curious things to impose on patients in the 21st century.
Latest news. The Mid-Devon Star announces yet more homeopathy in Dr Dixon’s Cullompton practice. This time it comes in the form of a clinic run from the Bristol Homeopathic Hospital. I guess they must be suffering from reduced commissioning like all the other homeopathic hospitals, but Dr Dixon seems to have come to their rescue. The connection seems to be with Bristol’s homeopathic consultant, Dr Elizabeth A Thompson. On 11 December 2007 I wrote to Dr Thompson, thus
|
In March 2006, a press release http://www.ubht.nhs.uk/press/view.asp?257 announced a randomised trial for homeopathic treatment of asthma in children. This was reported also on the BBC http://news.bbc.co.uk/1/hi/england/bristol/4971050.stm . I’d be very grateful if you could let me know when results from this trial will become available. Yours sincerely David Colquhoun |
The reply, dated 11 December 2007, was unsympathetic
|
I have just submitted the funders report today and we have set ourselves the deadline to publish two inter-related papers by March 1st 2007. Can I ask why you are asking and what authority you have to gain this information. I shall expect a reply to my questions, |
I answered this question politely on the same day but nevertheless my innocent enquiry drew forth a rather vitriolic complaint from Dr Thompson to the Provost of UCL (dated 14 December 2007). In this case, the Provost came up trumps. On 14 January 2008 he replied to Thompson: “I have looked at the email that you copied to me, and I must say that it seems an entirely proper and reasonable request. It is not clear to me why Professor Colquhoun should require some special authority to make such direct enquiries”. Dr Thompson seems to be very sensitive. We have yet to see the results of her trial in which I’m still interested.
Not surprisingly, Dr Dixon has had some severe criticism for his views, not least from the UK’s foremost expert on the evidence for efficacy, Prof Edzard Ernst. Accounts of this can be found in Pulse,
and on Andrew Lewis’s blog.
Dixon is now (in)famous in the USA too. The excellent Yale neurologist, Steven Novella, has written an analysis of his views on Science Based Medicine. He describes Dr. Michael Dixon as “A Pyromaniac In a Field of (Integrative) Straw Men”
Peter Hain
09:40 Politics and people: can integrated health and care take centre stage in 2009/2010? Rt Hon Peter Hain MP
It seems that Peter Hain was converted to alternative medicine when his first baby, Sam, was born with eczema. After (though possibly not because of) homeopathic treatment and a change in diet, the eczema got better. This caused Hain, while Northern Ireland Secretary to spend £200,000 of taxpayers’ money to set up a totally uninformative customer satisfaction survey, which is being touted elsewhere in this meeting as though it were evidence (see below). I have written about this episode before: see Peter Hain and Get Well UK: pseudoscience and privatisation in Northern Ireland.
I find it very sad that a hero of my youth (for his work in the anti-apartheid movement) should have sunk to promoting junk science, and even sadder that he does so at my expense.
There has been a report on Hain’s contribution in Wales Online.
09:55 Why does the Health Service need a new perspective on health and healing? Sir Cyril Chantler, Chair, King’s Fund, previous Dean, Guy’s Hospital and Great Ormond Street
Cyril Chantler is a distinguished medical administrator. He also likes to talk and we have discussed the quackery problem several times. He kindly sent me the slides that he used. Slide 18 says that in order to do some good we “need to demonstrate that the treatment is clinically effective and cost effective for NHS use”. That’s impeccable, but throughout the rest of the slides he talks of integrating with complementary” therapies, the effectiveness of which is either already disproved or simply not known.
I remain utterly baffled by the reluctance of some quite sensible people to grasp the nettle of deciding what works. Chantler fails to grasp the nettle, as does the Department of Health. Until they do so, I don’t see how they can be taken seriously.
10.05 Panel discussion
The Awards
10:20 Integrated Health Awards 2009 Introduction: a review of the short-listed applications
10:45 Presentations to the Award winners by the special guest speaker
11:00 Keynote address by special guest speaker
Getting integrated
Dr David Peters
12:00 Integration, long term disease and creating a sustainable NHS. Professor David Peters, Clinical Director and Professor of Integrated Healthcare, University of Westminster
I first met David Peters after Nature ran my article, Science Degrees without the Science. .One of the many media follow-ups of that article was on Material World (BBC Radio 4). This excellent science programme, presented by Quentin Cooper, had a discussion between me and David Peters ( listen to the mp3 file).
There was helpful intervention from Michael Marmot who had talked, in the first half of the programme, about his longitudinal population studies.
Marmot stressed the need for proper testing. In the case of
homeopathy and acupuncture, that proper testing has largely been done. The tests were failed.
The University of Westminster has, of course, gained considerable notoriety as the university that runs more degree programmes in anti-scientific forms of medicine than any other. Their lecture on vibrational medicine teaches students that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbances at all levels of being”. So far their vice-chancellor, Professor Geoffrey Petts, has declined to answer enquiries about whether he thinks such gobbledygook is appropriate for a BSc degree.
But he did set up an internal enquiry into the future of their alternative activities. Sadly that enquiry seems to have come to the nonsensical conclusion that the problem can be solved by injection of good science into the courses, as reported here and in the Guardian.
It seems obvious that if you inject good science into their BSc in homeopathy the subject will simply vanish in a puff of smoke.
In 2007, the University of Westminster did respond to earlier criticism in Times Higher Education, but their response seemed to me to serve only to dig themselves deeper into a hole.
Nevertheless, Westminster has now closed down its homeopathy degree (the last in the country to go) and there is intense internal discussion going on there. I have the impression that Dr Peters’ job is in danger. The revelation of more slides from their courses on homeopathy, naturopathy and Chinese herbal medicine shows that these courses are not only barmy, but also sometimes dangerous.
Professor Chris Fowler
12:10 Educating tomorrow’s integrated doctors. Professor Chris Fowler, Dean for Education, Barts and The London School of Medicine and Dentistry
I first came across Dr Fowler when I noticed him being praised for his teaching of alternative medicine to students at Barts and the London Medical School on the web site of the Prince’s Foundation. I wrote him a polite letter to ask if he really thought that the Prince of Wales was the right person to consult about the education of medical students. The response I got was, ahem, unsympathetic. But a little while later I noticed that two different Barts students had set up public blogs that criticised strongly the nonsense that was being inflicted on them.
At that point, I felt it was necessary to support the students who, it seemed to me, knew more about medical education than Professor Fowler. It didn’t take long to uncover the nonsense that was being inflicted on the students: read about it here.
There is a follow-up to this story here. Fortunately, Barts’ Director of Research, and, I’m told, the Warden of Barts, appear to agree with my view of the harm that this sort of thing can do to the reputation of Barts, so things may change soon,
Dame Donna Kinnair
12:30 Educating tomorrow’s integrated nurses.
Dame Donna Kinnair, Director of Nursing, Southwark PCT
As far as I can see, Donna Kinnair has no interest in alternative medicine. She is director of nursing at Southwark primary care trust and was an adviser to Lord Laming throughout his inquiry into the death of Victoria Climbié. I suspect that her interest is in integrating child care services (they need it, judging by the recent death of ‘Baby P’). Perhaps her presence shows the danger of using euphemisms like ‘integrated medicine’ when what you really mean is the introduction of unproven or disproved forms of medicine.
Michael Dooley
12:40 Integrating the care of women: an example of the new paradigm. Michael Dooley, Consultant Obstetrician and Gynecologist
DC’s rule 2. Never trust anyone who uses the word ‘paradigm’. It is a sure-fire sign of pseudoscience. In this case, the ‘new paradigm’ seems to be the introduction of disproven treatment. Dooley is a gynaecologist and Medical Director of the Poundbury Clinic. His clinic offers a whole range of unproven and disproved treatments. These include acupuncture as an aid to conception in IVF. This is not recommended by the Cochrane review, and one report suggests that it hinders conception rather than helps.
12.40 Discussion
13.00 – 14.00 Lunch and Exhibition
15.30 Tea
Boo Armstrong and Get Well UK
16.00 Integrated services in action: The Northern
Ireland experience: what has it shown us and what are its implications?
Boo Armstrong of Get Well UK with a team from the NI study
I expect that much will be made of this “study”, which, of course, tells you absolutely nothing whatsoever about the effectiveness of the alternative treatments that were used in it. This does not appear to be the view of Boo Armstrong, On the basis of the “study”, her company’s web site proclaims boldly
“Complementary Medicine Works
Get Well UK ran the first government-backed complementary therapy project in the UK, from February 2007 to February 2008″
This claim appears, prima facie, to breach the Unfair Trading Regulations of May 2008. The legality of the claim is, at the moment, being judged by a Trading Standards Officer. In any case, the “study” was not backed by the government as a whole, but just by Peter Hain’s office. It is not even clear that it had ethical approval.
The study consisted merely of asking people who had seen an alternative medicine practitioner whether they felt better or worse. There was no control group; no sort of comparison was made. It is surely obvious to the most naive person that a study like this cannot even tell you if the treatment has a placebo effect, never mind that it has any genuine effects of its own. To claim that it does so seems to be simply dishonest. There is no reason at all to think that the patients would not have got better anyway.
It is not only Get Well UK who misrepresent the evidence. The Prince’s
Foundation itself says
“Now a new, year long trial supported by the Northern Ireland health service has . . . demonstrated that integrating complementary and conventional medicine brings measurable benefits to patients’ health.”
That is simply not true. It is either dishonest or stupid. Don’t ask me which, I have no idea.
This study is no more informative than the infamous Spence (2005) ‘study’ of the same type, which seems to be the only thing that homeopaths can produce to support their case.
There is an excellent analysis of the Northern Ireland ‘study’ by Andy Lewis, The Northern Ireland NHS Alternative Medicine ‘Trial’. He explains patiently, yet again, what constitutes evidence and why studies like this are useless.
His analogy starts
” . . . the Apple Marketing Board approach the NHS and ask for £200,000 to do a study to show the truth behind the statement ‘An apple a day keeps the doctor away’. The Minister, being particularly fond of apples, agrees and the study begins.”
16.30 Social enterprise and whole systems integrated care. Dee Kyne, Sandwell PCT and a GP. Developing an integrated service in secondary care
Dee Kyne appears to be CEO of KeepmWell Ltd (a financial interest that is not mentioned).
Peter Mackereth, Clinical Lead, Supportive Services, Christie Hospital NHS Foundation Trust
I had some correspondence with Mackereth when the Times (7 Feb 2007) published a picture of the Prince of Wales inspecting an “anti-MRSA aromatherapy inhaler” in his department at the Christie. It turned out that the trial they were doing was not blind No result has been announced anyway, and on enquiry, I find that the trial has not even started yet. Surprising, then to find that the FIH is running the First Clinical Aromatherapy Conference at the Christie Hospital, What will there be to talk about?
Much of what they do at the Christie is straightforward massage, but they also promote the nonsensical principles of “reflexology” and acupuncture.
The former is untested. The latter is disproven.
Parallel Sessions
Developing a PCT funded musculoskeletal service Dr Roy Welford, Glastonbury Health Centre
Roy Welford is a Fellow of the Faculty of Homeopathy, and so promotes disproven therapies. The Glastonbury practice also advertises acupuncture (disproven), osteopathy and herbal medicine (largely untested so most of it consists of giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety).
Making the best of herbal self-prescription in integrated practice: key remedies and principles. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon
Simon Mills is a herbalist who now describes himself as a “phytotherapist” (it sounds posher, but the evidence, or lack of it, is not changed by the fancy name). Mills likes to say things like “there are herbs for heating and drying”, “hot and cold” remedies, and to use meaningless terms like “blood cleanser”, but he appears to be immune to the need for good evidence that herbs work before you give them to sick people. He says, at the end of a talk, “The hot and the cold remain the trade secret of traditional medicine”. And this is the 21st Century.
Practical ways in which complementary approaches can improve the treatment of cancer. Professor Jane Plant, Author of “Your life in your hands” and Chief Scientist, British Geological Society and Professor Karol Sikora, Medical Director, Cancer Partners UK
Jane Plant is a geologist who, through her own unfortunate encounter with breast cancer, became obsessed with the idea that a dairy-free diet cured her. Sadly there is no good evidence for that idea, according to the World Cancer Research Fund Report, led by Professor Sir Michael Marmot. No doubt her book on the subject sells well, but it could be held that it is irresponsible to hold out false hopes to desperate people. She is a supporter of the very dubious CancerActive organisation (also supported by Michael Dixon OBE –see above) as well as the notorious pill salesman, Patrick Holford (see also here).
Karol Sikora, formerly an oncologist at the Hammersmith Hospital, is now Dean of Medicine at the University of Buckingham (the UK’s only private university). He is also medical director at CancerPartners UK, a private cancer company.
He recently shot to fame when he appeared in a commercial in the USA sponsored by “Conservatives for Patients’ Rights”, to pour scorn on the NHS, and to act as an advocate for the USA’s present health system. A very curious performance. Very curious indeed.
His attitude to quackery is a mystery wrapped in an enigma. One was somewhat alarmed to see him sponsoring a course at what was, at first, called the British College of Integrated Medicine, and has now been renamed the Faculty of Integrated Medicine That grand title makes it sound like part of a university. It isn’t.

The alarm was as result of the alliance with Dr Rosy Daniel (who promotes an untested herbal conconction, Carctol, for ‘healing’ cancer) and Dr Mark Atkinson (a supplement salesman who has also promoted the Qlink pendant. The Qlink pendant is a simple and obvious fraud designed to exploit paranoia about WiFi killing you.
The first list of speakers on the proposed diploma in Integrated Medicine was an unholy alliance of outright quacks and commercial interests. It turned out that, although Karol Sikora is sponsoring the course, he knew nothing about the speakers. I did and when I pointed this out to Terence Kealey, vice-chancellor of Buckingham, he immediately removed Rosy Daniel from directing the Diploma. At the moment the course is being revamped entirely by Andrew Miles. There is hope that he’ll do a better job. It has not yet been validated by the University of Buckingham. Watch this space for developments.
Stop press It is reported in the Guardian that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear. More developments in the follow-up.
The role of happy chickens in healing: farms as producers of health as well as food – the Care Farm Initiative Jonathan Dover, Project Manager, Care Farming, West Midlands.
“Care farming is a partnership between farmers, participants and health & social care providers. It combines the care of the land with the care of people, reconnecting people with nature and their communities.”
Sounds lovely, I wonder how well it works?
What can the Brits learn from the Yanks when it comes to integrated health? Jack Lord, Chief Executive Humana Europe
It is worth noticing that the advisory board of Humana Europe includes Micheal Dixon OBE, a well known advocate of alternative medicine (see
above). Humana Europe is a private company, a wholly owned subsidiary of Humana Inc., a health benefits company with 11 million members and 22,000 employees and headquarters in Louisville, Kentucky. In 2005 it entered into a business partnership with Virgin Group. Humana was mentioned in the BBC Panorama programme “NHS for Sale”. The company later asked that it be pointed out that they provide commissioning services, not clinical services [Ed. well not yet anyway].
Humana’s document “Humana uses computer games to help people lead healthier lives” is decidedly bizarre. Hang on, it was only a moment ago that we were being told that computer games rewired your brain.
Day 2 Integrated health in action
09.00 Health, epidemics and the search for new solutions. Sir Michael Marmot, Professor of Epidemiology and Public Health, Royal Free and University College Medical School
It is a mystery to me that a distinguished epidemiologist should be willing to keep such dubious company. Sadly I don’t know what he said, but judging my his publications and his appearence on Natural World, I can’t imagine he’d have much time for homeopaths.
9.25 Improving health in the workplace. Dame Carol Black, National Director, Health and Work, Department of Health
This is not the first time that Dame Carol has been comtroversial.
9.45 Integrated health in focus: defeating obesity. Professor Chris Drinkwater, President, NHS Alliance.
The NHS Alliance was mentioned above. Enough said.
10.00 Integrated healthcare in focus: new approaches to managing asthma, eczema and allergy. Professor Stephen Holgate, Professor of Immunopharmacology, University of Southampton
10.15 Using the natural environment to increase activity. The Natural England Project: the results from year one. Dr William Bird and Ruth Tucker, Natural England.
10.30 Panel discussion
10.45 Coffee
Self help in action
11.10 Your health, your way: supporting self care through care planning and the use of personal budgets. Angela Hawley, Self Care Lead, Department of Health
11.25 NHS Life Check: providing the signposts to
integrated health. Roy Lambley, Project Director, NHS LifeCheck Programme
This programme was developed with the University of Westminster’s “Health and Well-being Network”. This group, with one exception, is separate from Westminster’s extensive alternative medicine branch (it’s mostly psychologists).
11.45 The agony and the ecstasy of helping patients to help themselves: tips for clinicians, practices and PCTs. Professor
Ruth Chambers, FIH Foundation Fellow.
11.55 Providing self help in practice: Department of Health Integrated Self Help Information Project. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon and Dr Sam Everington, GP, Bromley by Bow.
The Culm Valley Integrated Centre for health is part of the College Surgery Partnership, associated with Michael Dixon OBE (yes, again!).
Simon Mills is the herbalist who says “The hot and the cold remain the trade secret of traditional medicine” .
Sam Everington, in contrast, seems to be interested in ‘integration’ in the real sense of the word, rather than quackery.
Integrated health in action
How to make sense of the evidence on complementary approaches: what works? What might work? What doesn’t work?
Dr Hugh MacPherson, Senior Research Fellow in Health Sciences, York University and Dr Catherine Zollman, Bravewell Fellow
Hugh MacPherson‘s main interest is in acupuncture and he publishes in alternative medicine journals. Since the recent analysis in the BMJ from the Nordic Cochrane Centre (Madsen et al., 2009) it seems that acupuncture is finally dead. Even its placebo effect is too small to be useful. Catherine Zollman is a Bristol GP who is into homeopathy as well as acupuncture. She is closely connected with the Prince’s Foundation via the Bravewell Fellowship. That fellowship is funded by the Bravewell Collaboration, which is run by Christie Mack, wife of John Mack (‘Mack the Knife’), head of Morgan Stanley (amazingly, they still seem to have money). This is the group which, by sheer wealth, has persuaded so many otherwise respectable US universities to embrace every sort of quackery (see, for example, Integrative baloney @ Yale)
The funding of integrated services
14.15 How to get a PCT or practice- based commissioner to fund your integrated service. A PCT Chief Executive and a Practice-Based Commissioning lead.
14.30 How I succeeded: funding an integrated service. Dr John Ribchester, Whitstable
14.45 How we created an acupuncture service in St Albans and Harpenden PBC group. Mo Girach, Chief Executive, STAHCOM
Uhuh Acupunture again. Have these people never read Bausell’s
book? Have they not read the BMJ? Acupuncture is now ell-established to be based on fraudulent principles, and not even to have a worthwhile placeobo effect. STAHCOM seem to be more interested in money than in what works.
Dragon’s Den. Four pitchers lay out their stall for the commissioning dragons
And at this stage there is no prize for guessing that all four are devoted to trying to get funds for discredited treatments
- An acupuncture service for long-term pain. Mike Cummings Chair, Medical Acupuncture Association
- Manipulation for the treatment of back pain Simon Fielding, Founder Chairman of the General Osteopathic Council
- Nigel Clarke, Senior Partner, Learned Lion Partners Homeopathy for long term conditions
- Peter Fisher, Director, Royal Homeopathic Hospital
Sadly it is not stated who the dragons are. One hopes they will be more interested in evidence than the supplicants.
Mike Cummings at least doesn’t believe the nonsense about meridians and Qi. It’s a pity he doesn’t look at the real evidence though.
You can read something about him and his journal at BMJ Group promotes acupuncture: pure greed.
Osteopathy sounds a bit more respectable than the others, but in fact it has never shaken off its cult-like origins. Still many osteopaths make absurd claims to cure all sorts of diseases. Offshoots of osteopathy like ‘cranial osteopathy’ are obvious nonsense. There is no reason to think that osteopathy is any better than any other manipulative therapy and it is clear that all manipulative therapies should be grouped into one.
Osteopathy and chiropractic provide the best ever examples of the folly of giving official government recognition to a branch of alternative medicine before the evidence is in.
Learned Lion Partners is a new one on me. It seems it is
part of Madsen Gornall Ashe Chambers (‘MGA Chambers’) “a grouping of top level, independent specialists who provide a broad range of management consultancy advice to the marketing community”. It’s a management consultant and marketing outfit. So don’t expect too much when it comes to truth and evidence. The company web site says nothing about alternative medicine, but only that Nigel Clarke
“. . . has very wide experience of public affairs issues and campaigns, having worked with clients in many sectors in Europe, North America and the Far East. He has particular expertise in financial, competition and healthcare issues. “
However, all is revealed when we see that he is a Trustee of the Prince’s Foundation where his entry says
“Nigel Clarke is senior partner of Learned Lion Partners. He is a director of Vidapulse Ltd, Really Easy Ltd, Newscounter Ltd and Advanced Transport Systems Ltd. He has worked on the interfaces of public policy for 25 years. He has been chair of the General Osteopathic Council since May 2001, having been a lay member since it was formed. He is now a member of the Council for Healthcare Regulatory Excellence”
The Council for Healthcare Regulatory Excellence is yet another quango that ticks boxes and fails absolutely to grasp the one important point, does it work?. I came across them at the Westminster Forum, and they seemed a pretty pathetic way to spend £2m per year.
Peter Fisher is the last supplicant to the Dragons. He is clinical director of the Royal London Homeopathic Hospital (RLHH), and Queen’s homeopathic physician, It was through him that I got an active interest in quackery. The TV programme QED asked me to check the statistics in a paper of his that claimed that homeopathy was good for fibrositis (there was an elementary mistake and no evidence for an effect). Peter Fisher is also remarkable because he agreed with me that BSc degrees in homeopathy were not justified (on TV –see the movie). And he condemned homeopaths who were caught out recommending their sugar pills for malaria. To that extent Fisher represents the saner end of the homeopathic spectrum. Nevertheless he still maintains that sugar pills work and have effects of their own, and tries to justify the ‘memory of water’ by making analogies with a memory stick or CD. This is so obviously silly that no more comment is needed.
Given Fisher’s sensible condemnation of the malaria fiasco, I was rather surprised to see that he appeared on the programme of a conference at the University of Middlesex, talking about “A Strategy To Research The Potential Of Homeopathy In Pandemic Flu”. The title of the conference was Developing Research Strategies in CAM. A colleague, after seeing the programme, thought it was more like “a right tossers’ ball”.
Much of the homeopathy has now vanished from the RLHH as a result of greatly reduced commissioning by PCTs (read about it in Fisher’s own words). And the last homeopathy degree in the UK has closed down. It seems an odd moment for the FIH to be pushing it so hard.
Follow-up
Stop press It is reported in the Guardian (22 May 2009) that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear, oh dear.
This fascinating fact seems to have been unearthed first by the admirable NHS Blog Doctor, in his post ‘Imperial College confirm that Karol Sikora does not work for them and does not speak on their behalf‘.
|
It seems that bits of good news don’t come singly. First honours degrees in acupuncture vanish, Now a big chain of shops selling Chinese herbs and acupuncture has gone into administration. It seems that, at last, people are getting fed up with being conned out of their hard-earned money |
 Herbmedic Barking |
A local newspaper, The North Herts Comet reported thus.
Customers of Herbmedic, which trades under the name Herbs and Acupuncture, on Queensway in Stevenage have been left counting the cost after shelling out hundreds of pounds for treatment they never received.
The company, which has practices across the country, is now in the hands of receivers, Macintyre Hudson.
Sandra Emery, of The Paddocks in Stevenage, paid £350 for 10 treatment sessions, but only received one before the practice closed.
She said: “A standard course of treatment is 10 sessions, so most customers will have bought this package.
Claudia Gois, of Walden End in Stevenage, paid £240 for 12 treatment sessions but only received four before the practice closed.
She said: “I went there on Friday and it was closed. There was no warning or anything.
“I got in touch with head office and they said it’s very unlikely I will get money back.
This report was on 1st April, The company’s web site shows no sign of any problems, In fact they are still advertising jobs. So was this an April Fool joke?
No it wasn’t. A visit to Companies House soon settled the matter. The whole company is insolvent, as of 27 March 2009..
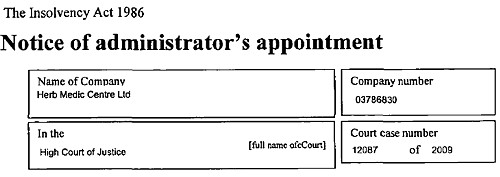
Download the whole administration notice and the company report.
Criticisms of Herbmedic
This chain of shops was investigated by the BBC’s
Inside Out programme. (September 25th 2006).
“We sent an undercover reporter to branches of the Herbmedic chain in southern England.
On each occasion, the reporter claimed to be suffering from tiredness and was prescribed herbal remedies after a consultation lasting less than five minutes.
The herbalists, who describe themselves as “doctors”, didn’t ask any questions about the patient’s medical history or take any notes.”
This is so bad that even Andrew Fowler, a past President of the Register of Chinese Herbal Medicine, described it as “malpractice”.
“Herbmedic has been investigated by the authorities in the past.
In 2002, trading standards officers prosecuted the branch in Southampton for selling herbal remedies with 26 times the permitted legal limit of lead.
And in October 2003, the Advertising Standards Authority banned Herbmedic from describing its practitioners as “doctors”.
Despite the ban, all three of the stores visited by Inside Out referred to the herbalist as the doctor.”
See also the BBC report Herbalists’ customers ‘at risk’, and a report in the Sunday Times, Herbmedic accused of high-pressure selling.
Read the Advertising Standards report. Seven different complaints against Herbmedic were upheld.
This is entirely consistent with my own experience. I went into one of their shops and asked about a cure for diabetes (hoping the be able to refer them to Trading Standards, but the young lady behind the counter had such a poor grasp of English that her reply was incomprehensible. She just kept trying to push me into having a consultation with “the doctor” who appeared to speak no English at all. I left.
The chequered history of Herbmedic
The company that his just gone into administration is Herbmedic Centre Ltd. It has been in existence for only two years. Its predecessor, known simply as Herbmedic, was dissolved on 13 March 2007, Companies House said
Company Filing History Type Date Description Order GAZ2(A) 13/03/2007 FINAL GAZETTE: DISSOLVED VIA VOLUNTARY STRIKE-OFF GAZ1(A) 28/11/2006 FIRST GAZETTE NOTICE FOR VOLUNTARY STRIKE-OFF 652a 16/10/2006 APPLICATION FOR STRIKING-OFF
Another Chinese medicine chain seems to be having a few problems too
Harmony Medical Distribution Ltd (“specialists in acupuncture and holistic medicine”) seems to be still in business(web site here), but several very similar companies have been dissolved, Harmomy Medics Ltd (dissolved 19 Sep 2006) ,, Harmony Medical Services (UK ) Ltd. (dissolved 6 May 2008) and Harmony Medical Services Ltd (dissolved 17 Oct 2008)
Given this history of companies that dissolve every couple of years and then mysteriously reincarnate with a slightly different name, one wonders if this really is the end of herbmedic, or it is just a device for shedding bad debts. Is this just another “pre-pack administration“?
Watch this space for more.
What’s the latest evidence on acupuncture anyway?
A correspondent drew my attention to the 2009 Annual Evidence Update on acupuncture complied by the NHS Complementary and Alternative Medicine Specialist Library. This includes no fewer than 56 systematic reviews and meta-analyses. Although the reviews are complied by alternative medicine sympathisers, they seem mostly to be pretty fair. Well apart form one thing.
Almost all of the reviews fail to come up with any positive evidence that acupuncture works well enough to be clinically useful. Only two come close, and they are the two singled out as “editor’s picks”. Perhaps that’s not entirely surprising given that the editor is Dr Mike Cummings.
Again and again, the results are inconclusive: #8 is pretty typical
Acupuncture for tension-type headache: a meta-analysis of randomized, controlled trials.
This meta-analysis suggests that acupuncture compared with sham for tension-type headache has limited efficacy for the reduction of headache frequency. There exists a lack of standardization of acupuncture point selection and treatment course among randomized, controlled trials. More research is needed to investigate the treatment of specific tension-type headache subtypes.
Vast effort and a lot of money is being put into trials, yet there are very few (if any) positive results. Very often there are no results at whatsoever. All we hear, again and again, is “more research is needed”.
At some point someone will have to decide it is all a charade and start to spend time and money on investigating things that are more promising.
Follow-up
A correspondent checked with Companies House to discover more about two of the directors of Herbmedic, Mr. Li Mao and Mr Xiao Xuan Chen. They have a chequered history indeed. [download the complete list]
Mr. Li Mao is, or has been, on the board of 31 different companies. Of these 6 are active, 5 are in administration, 14 were dissolved, 4 were liquidated and 2 are active with proposal to strike off. Not only is Her Medic centre Ltd in administration, but so is Dr China (UK) Ltd, and Great Chinese Herbal Medicine Ltd
With record like that, my correspondent wonders whether they should be disqualified.
Recently I wrote a piece for the National Health Executive (“the Independent Journal for Senior Health Service Managers”), with the title Medicines that contain no medicine and other follies
In the interests of what journalists call balance (but might better be called equal time for the Flat Earth Society), an article appeared straight after mine, Integrating Homeopathy into Primary Care. It was by Rachel Roberts “Research consultant for the Society of Homeopaths”.
This defence was so appalling that I sent them a response (after first doing a bit of checking on its author). To my surprise, they published the response in full [download pdf of printed version]. Their title was

As always, the first step is to Google the author, to find out a bit more. It seems that Rachel Roberts runs a business Integrated Homeopathic Training. (a financial interest that was not mentioned in her article). She will sell you flash cards (‘Matmedcards’) for £70 (+£9 p&p) for 120 cards (yes, seriously). The card for Conium maculatum is remarkable. It says on the reverse side
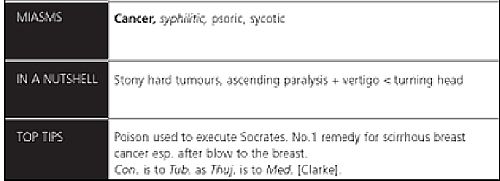
Yes, it says (my emphasis)
“The poison used to execute Socrates. No 1 remedy for scirrhous breast cancer. Esp after blow to the breast”
No doubt she would claim that the word “remedy” was a special weasel word of homeopaths that did not imply any therapeutic efficacy. But its use in this context seems to me to be cruel deception, even murderous. It also appears to breach the Cancer Act 1939, as well as the Unfair Trading laws.
I asked the Bristol Trading Standards Office, and got a reply remarkably quickly. It ended thus.
“. . . . the use of the card for “hemlock” as an example amounts to advice in connection with the treatment (of cancer)”. I will initially write to IHT and require that they remove this, and any other, reference to cancer treatment from their website.
When I checked again a couple of weeks later, the hemlock sample card had been been replaced by one about chamomile (it is described as the opium of homeopathy. Luckily the pills contain no opium (and no chamomile either) or that would be breaking another law. Bafflingly, it is not (yet) against the law to sell pills that contain no trace of the ingredient on the label, if they are labelled ‘homeopathic’.
Presumably the packs still contain a claim to cure cancer. And what is said in the privacy of the consulting room will never be known.
Political correctness is a curious thing. I felt slightly guilty when I reported this breach of the Cancer Act. It felt almost sneaky. The feeling didn’t last long though. We are talking about sick people here.
It isn’t hard to imagine a desperate woman suffering from cancer reading that Ms Roberts knows the “No 1 remedy for scirrhous breast cancer”. She might actually believe it. She might buy some hemlock pills that contain no hemlock (or anything else). She might die as a result. It is not a joke. It is, literally, deadly serious.
It is also deadly serious that the Department of Health and some NHS managers are so stifled by political correctness that they refer to homeopaths as “professionals” and pay them money.
Ms Roberts, in her article, is at pains to point out that
|
 |
Well it is already well known that the the Code of Ethics of the Society of Homeopaths is something of a joke. This is just one more example.
The Code of Ethics, para 72 says homeopaths have a legal obligation
“To avoid making claims (whether explicit or implied; orally or in writing) implying cure of any named disease.”
Like, perhaps, claiming to have the “No 1 remedy for scirrhous breast cancer”?
Obviously voluntary self-regulation isn’t worth the paper it’s written on.
You don’t need to go to her web site to find “claims . . . implying cure of any named disease”. In her article she says
“Conditions which responded well to homeopathy included childhood eczema and asthma, migraine, menopausal problems, inflammatory bowel disease, irritable bowel syndrome, arthritis, depression and chronic fatigue syndrome.”
No doubt they will say that the claim that asthma and migraine “responded well” to their sugar pills carries no suggestion that they can cure a named disease. And if you believe that, you’ll believe anything.
I have to say that I find Ms Robert’s article exceedingly puzzling. It comes with 29 references, so it looks, to use Goldacre’s word, ‘sciencey’. If you read the references, and more importantly, know about all the work that isn’t referred to, you see it is the very opposite of science. I see only two options.
Either it is deliberate deception designed to make money, or it shows, to a mind-boggling extent, an inability to understand what constitutes evidence.
The latter, more charitable, view is supported by the fact that Ms Roberts trots out, yet again, the infamous 2005 Spence paper, as though it constituted evidence for anything at all. In this paper 6544 patients at the Bristol Homeopathic Hospital were asked if the felt better after attending the out-patient department. Half of them reported that the felt ‘better’ or ‘much better’. Another 20% said they were ‘slightly better’ (but that is what you say to be nice to the doctor). The patients were not compared with any other group at all. What could be less surprising than that half of the relatively minor complaints that get referred for homeopathy get ‘better or much better’ on their own?
This sort of study can’t even tell you if homeopathic treatment has a placebo effect, never mind that it has a real effect of its own. It is a sign of the desperation of homeopaths that they keep citing this work.
Whatever the reason, the conclusion is clear. Never seek advice from someone who has a financial interest in the outcome. Ms Roberts makes her living from homeopathy. If she were to come to the same conclusion as the rest of the world, that it is a placebo and a fraud, her income would vanish. It is asking too much of anyone to do that.
| This is the mistake made time and time again by the Department of Health and by the NHS. The Pittilo report does the same thing The execrably bad assessment of evidence in that report is, one suspects, not unrelated to the fact that it was done entirely by people who would lose their jobs if they were to come to any conclusion other than their treatments work. |  |
At present , the regulation of alternative medicine is chaotic because the government and the dozen or so different quangos involved are trying to regulate while avoiding the single most important question – do the treatments work?
They should now grasp that nettle and refer the question to NICE.
Follow-up
It is almost six months now since I posted Quackery creeps into good universities too -but through Human Resources. One example given there was the University of Leicester. This is an excellent university. It does first class research and it was the alma mater of the incomparable David Attenborough who has done more than anyone to show us the true beauty and wonder of the natural world.
Nevertheless, their well-meaning occupational health department had a section about “complementary therapies” that contained a lot of statements that were demonstrably untrue. They even recommended the utterly outrageous SCENAR device. So I pointed this out to them, and I had a quick and sympathetic response from their HR director.
But three months later, nothing had changed. Every now and then, I’d send a polite reminder, but it seemed the occupational health staff were very wedded to their quackery. The last reminder went on 6th February, but this time I copied it to Leicester’s vice-chancellor. This time it worked. There is still a link to Complementary Therapies on the Wellbeing site, but if you click on it, this is what you see.
Complementary therapiesSome employees may have an interest in complementary therapies such as acupuncture, yoga, Indian head massage, Reiki, sports & remedial massage, reflexology and hypnotherapy. If you have an interest in any of these, Staff Counselling can happily provide details of practitioners in the local area. Some of these practitioners offer discounts from their normal rates for University of Leicester staff. However, the University of Leicester cannot vouch for, or recommend any of these therapies to staff as being effective. We would urge members of staff who believe that such therapies might be effective to contact their GP prior to undertaking any of them. Further, the University of Leicester shall not be liable for any damage of any kind arising out of or related to the services of any complementary therapists or treatments listed here. If you would like further information, please contact Chris Wilson at: staffcounsel&welfare@le.ac.uk or telephone 1702. |
That’s not bad. Pity it doesn’t say alternative, rather than complementary though. Euphemisms aren’t really helpful.
In fact I have a bit of a problem with “wellbeing” too. It is a harmless word that has been highjacked so that its use now makes one think of mud baths provided by expensive hotels for their rich and gullible customers.
Leicester’s HR director wrote
“Unfortunately an instruction I had given previously had not been fully complied with. I spoke to the manager of the Staff Counselling team on Friday and gave clear instructions as to the content of this site. I had been assured that the offending information had been removed, but found that it had not.
I have now checked the site for myself and can say, with confidence, that all claims for the efficacy of complimentary [sic] therapies have been removed including SCENAR.”
The similarity between quack treatments and religion is intriguing. It seems that the devotion of the occupational health people to their baloney was so great that they wouldn’t take it down even when told to do so. The more irrational the belief, the greater the fervour with which it is defended,
What’s the lesson from this minor saga? It seems that most VCs and many HR people are too sensible to believe in alternative baloney, but that they are a bit too ready to tolerate it, perhaps on grounds of political correctness. Tolerance is a virtue, but lies about health are not in the least virtuous. If you point out that people are saying things for which there isn’t the slightest evidence, they will often respond. Just be prepared to send a few reminders.
It may also be useful to point out that some of the claims made are almost certainly illegal. Even people who care little about evidence of efficacy are impressed by the idea that they might be prosecuted by Trading Standards officers.
Who needs mystical medicine when you have real wonders like these.
(Click the google video logo for a bigger version)
Or try the pitcher plant video, or the Bird of paradise, or the Bower Bird, or the giant Amazon lilies.
Follow-up
I’m perfectly happy to think of alternative medicine as being a voluntary, self-imposed tax on the gullible (to paraphrase Goldacre again). But only as long as its practitioners do no harm and only as long as they obey the law of the land. Only too often, though, they do neither.
When I talk about law, I don’t mean lawsuits for defamation. Defamation suits are what homeopaths and chiropractors like to use to silence critics. heaven knows, I’ve becomes accustomed to being defamed by people who are, in my view. fraudsters, but lawsuits are not the way to deal with it.
I’m talking about the Trading Standards laws Everyone has to obey them, and in May 2008 the law changed in a way that puts the whole health fraud industry in jeopardy.
The gist of the matter is that it is now illegal to claim that a product will benefit your health if you can’t produce evidence to justify the claim.
I’m not a lawyer, but with the help of two lawyers and a trading standards officer I’ve attempted a summary. The machinery for enforcing the law does not yet work well, but when it does, there should be some very interesting cases.
The obvious targets are homeopaths who claim to cure malaria and AIDS, and traditional Chinese Medicine people who claim to cure cancer.
But there are some less obvious targets for prosecution too. Here is a selection of possibilities to savour..
- Universities such as Westminster, Central Lancashire and the rest, which promote the spreading of false health claims
- Hospitals, like the Royal London Homeopathic Hospital, that treat patients with mistletoe and marigold paste. Can they produce any real evidence that they work?
- Edexcel, which sets examinations in alternative medicine (and charges for them)
- Ofsted and the QCA which validate these exams
- Skills for Health and a whole maze of other unelected and unaccountable quangos which offer “national occupational standards” in everything from distant healing to hot stone therapy, thereby giving official sanction to all manner of treatments for which no plausible evidence can be offered.
- The Prince of Wales Foundation for Integrated Health, which notoriously offers health advice for which it cannot produce good evidence
- Perhaps even the Department of Health itself, which notoriously referred to “psychic surgery” as a profession, and which has consistently refused to refer dubious therapies to NICE for assessment.
The law, insofar as I’ve understood it, is probably such that only the first three or four of these have sufficient commercial elements for there to be any chance of a successful prosecution. That is something that will eventually have to be argued in court.
But lecanardnoir points out in his comment below that The Prince of Wales is intending to sell herbal concoctions, so perhaps he could end up in court too.
The laws
We are talking about The Consumer Protection from Unfair Trading Regulations 2008. The regulations came into force on 26 May 2008. The full regulations can be seen here, or download pdf file. They can be seen also on the UK Statute Law Database.
The Office of Fair Trading, and Department for Business, Enterprise & Regulatory Reform (BERR) published Guidance on the Consumer Protection from Unfair Trading Regulations 2008 (pdf file),
Statement of consumer protection enforcement principles (pdf file), and
The Consumer Protection from Unfair Trading Regulations: a basic guide for business (pdf file).
Has The UK Quietly Outlawed “Alternative” Medicine?
On 26 September 2008, Mondaq Business Briefing published this article by a Glasgow lawyer, Douglas McLachlan. (Oddly enough, this article was reproduced on the National Center for Homeopathy web site.)
“Proponents of the myriad of forms of alternative medicine argue that it is in some way “outside science” or that “science doesn’t understand why it works”. Critical thinking scientists disagree. The best available scientific data shows that alternative medicine simply doesn’t work, they say: studies repeatedly show that the effect of some of these alternative medical therapies is indistinguishable from the well documented, but very strange “placebo effect” ”
“Enter The Consumer Protection from Unfair Trading Regulations 2008(the “Regulations”). The Regulations came into force on 26 May 2008 to surprisingly little fanfare, despite the fact they represent the most extensive modernisation and simplification of the consumer protection framework for 20 years.”
The Regulations prohibit unfair commercial practices between traders and consumers through five prohibitions:-
- General Prohibition on Unfair Commercial
Practices (Regulation 3)- Prohibition on Misleading Actions (Regulations 5)
- Prohibition on Misleading Omissions (Regulation 6)
- Prohibition on Aggressive Commercial Practices (Regulation 7)
- Prohibition on 31 Specific Commercial Practices that are in all Circumstances Unfair (Schedule 1). One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. The definition of “product” in the Regulations includes services, so it does appear that all forms medical products and treatments will be covered.
Just look at that!
| One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations” |
Section 5 is equally powerful, and also does not contain the contentious word “cure” (see note below)
Misleading actions
5.—(1) A commercial practice is a misleading action if it satisfies the conditions in either paragraph (2) or paragraph (3).
(2) A commercial practice satisfies the conditions of this paragraph—
(a) if it contains false information and is therefore untruthful in relation to any of the matters in paragraph (4) or if it or its overall presentation in any way deceives or is likely to deceive the average consumer in relation to any of the matters in that paragraph, even if the information is factually correct; and
(b) it causes or is likely to cause the average consumer to take a transactional decision he would not have taken otherwise.
These laws are very powerful in principle, But there are two complications in practice.
One complication concerns the extent to which the onus has been moved on to the seller to prove the claims are true, rather than the accuser having to prove they are false. That is a lot more favourable to the accuser than before, but it’s complicated.
The other complication concerns enforcement of the new laws, and at the moment that is bad.
Who has to prove what?
That is still not entirely clear. McLachlan says
“If we accept that mainstream evidence based medicine is in some way accepted by mainstream science, and alternative medicine bears the “alternative” qualifier simply because it is not supported by mainstream science, then where does that leave a trader who seeks to refute any allegation that his claim is false?
Of course it is always open to the trader to show that his the alternative therapy actually works, but the weight of scientific evidence is likely to be against him.”
On the other hand, I’m advised by a Trading Standards Officer that “He doesn’t have to refute anything! The prosecution have to prove the claims are false”. This has been confirmed by another Trading Standards Officer who said
“It is not clear (though it seems to be) what difference is implied between “cure” and “treat”, or what evidence is required to demonstrate that such a cure is false “beyond reasonable doubt” in court. The regulations do not provide that the maker of claims must show that the claims are true, or set a standard indicating how such a proof may be shown.”
The main defence against prosecution seems to be the “Due diligence defence”, in paragraph 17.
Due diligence defence
17. —(1) In any proceedings against a person for an offence under regulation 9, 10, 11 or 12 it is a defence for that person to prove—
(a) that the commission of the offence was due to—
(i) a mistake;
(ii) reliance on information supplied to him by another person;
(iii) the act or default of another person;
(iv) an accident; or
(v) another cause beyond his control; and
(b) that he took all reasonable precautions and exercised all due diligence to avoid the commission of such an offence by himself or any person under his control.
If “taking all reasonable precautions” includes being aware of the lack of any good evidence that what you are selling is effective, then this defence should not be much use for most quacks.
Douglas McLachlan has clarified, below, this difficult question
False claims for health benefits of foods
A separate bit of legislation, European regulation on nutrition and health claims made on food, ref 1924/2006, in Article 6, seems clearer in specifying that the seller has to prove any claims they make.
Article 6
Scientific substantiation for claims
1. Nutrition and health claims shall be based on and substantiated by generally accepted scientific evidence.
2. A food business operator making a nutrition or health claim shall justify the use of the claim.
3. The competent authorities of the Member States may request a food business operator or a person placing a product on the market to produce all relevant elements and data establishing compliance with this Regulation.
That clearly places the onus on the seller to provide evidence for claims that are made, rather than the complainant having to ‘prove’ that the claims are false.
On the problem of “health foods” the two bits of legislation seem to overlap. Both have been discussed in “Trading regulations and health foods“, an editorial in the BMJ by M. E. J. Lean (Professor of Human Nutrition in Glasgow).
“It is already illegal under food labelling regulations (1996) to claim that food products can treat or prevent disease. However, huge numbers of such claims are still made, particularly for obesity ”
“The new regulations provide good legislation to protect vulnerable consumers from misleading “health food” claims. They now need to be enforced proactively to help direct doctors and consumers towards safe, cost effective, and evidence based management of diseases.”
In fact the European Food Standards Agency (EFSA) seems to be doing a rather good job at imposing the rules. This, predictably, provoked howls of anguish from the food industry There is a synopsis here.
“Of eight assessed claims, EFSA’s Panel on Dietetic Products, Nutrition and Allergies (NDA) rejected seven for failing to demonstrate causality between consumption of specific nutrients or foods and intended health benefits. EFSA has subsequently issued opinions on about 30 claims with seven drawing positive opinions.”
“. . . EFSA in disgust threw out 120 dossiers supposedly in support of nutrients seeking addition to the FSD’s positive list.
If EFSA was bewildered by the lack of data in the dossiers, it needn’t hav been as industry freely admitted it had in many cases submitted such hollow documents to temporarily keep nutrients on-market.”
Or, on another industry site, “EFSA’s harsh health claim regime”
“By setting an unworkably high standard for claims substantiation, EFSA is threatening R&D not to mention health claims that have long been officially approved in many jurisdictions.”
Here, of course,”unworkably high standard” just means real genuine evidence. How dare they ask for that!
Enforcement of the law
Article 19 of the Unfair Trading regulations says
19. —(1) It shall be the duty of every enforcement authority to enforce these Regulations.
(2) Where the enforcement authority is a local weights and measures authority the duty referred to in paragraph (1) shall apply to the enforcement of these Regulations within the authority’s area.
Nevertheless, enforcement is undoubtedly a weak point at the moment. The UK is obliged to enforce these laws, but at the moment it is not doing so effectively.
A letter in the BMJ from Rose & Garrow describes two complaints under the legislation in which it appears that a Trading Standards office failed to enforce the law. They comment
” . . . member states are obliged not only to enact it as national legislation but to enforce it. The evidence that the government has provided adequate resources for enforcement, in the form of staff and their proper training, is not convincing. The media, and especially the internet, are replete with false claims about health care, and sick people need protection. All EU citizens have the right to complain to the EU Commission if their government fails to provide that protection.”
This is not a good start. A lawyer has pointed out to me
“that it can sometimes be very difficult to get Trading Standards or the OFT to take an interest in something that they don’t fully understand. I think that if it doesn’t immediately leap out at them as being false (e.g “these pills cure all forms of cancer”) then it’s going to be extremely difficult. To be fair, neither Trading Standards nor the OFT were ever intended to be medical regulators and they have limited resources available to them. The new Regulations are a useful new weapon in the fight against quackery, but they are no substitute for proper regulation.”
Trading Standards originated in Weights and Measures. It was their job to check that your pint of beer was really a pint. Now they are being expected to judge medical controversies. Either they will need more people and more training, or responsibility for enforcement of the law should be transferred to some more appropriate agency (though one hesitates to suggest the MHRA after their recent pathetic performance in this area).
Who can be prosecuted?
Any “trader”, a person or a company. There is no need to have actually bought anything, and no need to have suffered actual harm. In fact there is no need for there to be a complainant at all. Trading standards officers can act on their own. But there must be a commercial element. It’s unlikely that simply preaching nonsense would be sufficient to get you prosecuted, so the Prince of Wales is, sadly, probably safe.
Universities who teach that “Amethysts emit high Yin energy” make an interesting case. They charge fees and in return they are “falsely claiming that a product is able to cure illnesses”.
In my view they are behaving illegally, but we shan’t know until a university is taken to court. Watch this space.
The fact remains that the UK is obliged to enforce the law and presumably it will do so eventually. When it does, alternative medicine will have to change very radically. If it were prevented from making false claims, there would be very little of it left apart from tea and sympathy
Follow-up
New Zealand must have similar laws.
Just as I was about to post this I found that in New Zealand a
“couple who sold homeopathic remedies claiming to cure bird flu, herpes and Sars (severe acute respiratory syndrome) have been convicted of breaching the Fair Trading Act.”
They were ordered to pay fines and court costs totalling $23,400.
A clarification form Douglas McLachlan
On the difficult question of who must prove what, Douglas McLachlan, who wrote Has The UK Quietly Outlawed “Alternative” Medicine?, has kindly sent the following clarification.
“I would agree that it is still for the prosecution to prove that the trader committed the offence beyond a reasonable doubt, and that burden of proof is always on the prosecution at the outset, but I think if a trader makes a claim regarding his product and best scientific evidence available indicates that that claim is false, then it will be on the trader to substantiate the claim in order to defend himself. How will the trader do so? Perhaps the trader might call witness after witness in court to provide anecdotal evidence of their experiences, or “experts” that support their claim – in which case it will be for the prosecution to explain the scientific method to the Judge and to convince the Judge that its Study evidence is to be preferred.
Unfortunately, once human personalities get involved things could get clouded – I could imagine a small time seller of snake oil having serious difficulty, but a well funded homeopathy company engaging smart lawyers to quote flawed studies and lead anecdotal evidence to muddy the waters just enough for a Judge to give the trader the benefit of the doubt. That seems to be what happens in the wider public debate, so it’s easy to envisage it happening a courtroom.”
The “average consumer”.
(3) A commercial practice is unfair if—
(a) it contravenes the requirements of professional diligence; and
(b) it materially distorts or is likely to materially distort the economic behaviour of the average consumer with regard to the product.
It seems,therefore, that what matters is whether the “average consumer” would infer from what is said that a claim was being made to cure a disease. The legal view cited by Mojo (comment #2, below) is that expressions such as “can be used to treat” or “can help with” would be considered by the average consumer as implying successful treatment or cure.
The drugstore detox delusion. A nice analysis “detox” at .Science-based Pharmacy

