acupuncture
Two days ago I wrote NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself
Now the official ‘guidance’ is out, and it is indeed quite as bad as the draft.
The relevant bits now read thus.
- Offer one of the following treatment options, taking into account patient preference: an exercise programme, a course of manual therapy or a course of acupuncture. Consider offering another of these options if the chosen treatment does not result in satisfactory improvement.
- Consider offering a structured exercise programme tailored to the person:
- This should comprise of up to a maximum of 8 sessions over a period of up to 12 weeks.
- Offer a group supervised exercise programme, in a group of up to 10 people.
- A one-to-one supervised exercise programme may be offered if a group programme is not suitable for a particular person.
- Consider offering a course of manual therapy, including spinal manipulation, comprising up to a maximum of nine sessions over a period of up to 12 weeks
- Consider offering a course of acupuncture needling comprising up to a maximum of 10 sessions over a period of up to 12 weeks.
The summary guidance still doesn’t mention chiropractic explicitly, just a coy reference to “spinal manipulation”. At a time when the British Chiropractic Association is busy trying to suppress free speech via the law courts, I guess it isn’t surprising that they don’t like to use the word.
The bias in the recommendations is perhaps not surprising because the guidance development group had a heavy representation from alternative medicine advocates, and of people with a record of what, is, in my view, excessive tolerance of mumbo-jumbo.
Royal College of General Practitioners (RCGP) played a large part in writing the guidance. That is an organisation thar has steadfastly refused to make any sort of sensible statement of policy about magic medicine. It isn’t long since I was told by a senior person at the RCGP that there was nothing odd about neuro-linguistic programming. That does not bode well.
Professor Martin Underwood, Professor of Primary Care Research Warwick Medical School, University of Warwick. Underwood chaired the guidance development group. Martin Underwood is also a GP in Coventry See also the British Osteopathic Association. Underwood was lead author of the BEAM trial (download reprint). It is well worth reading the comments on this trial too. It was a randomised trial (though not, of course, blind).
|
Our main aim was to estimate, for patients consulting their general practitioner with back pain, the effectiveness of adding the following to best care in general practice: a class based exercise programme (“back to fitness”), a package of treatment by a spinal manipulator (chiropractor, osteopath, or physiotherapist), or manipulation followed by exercise Conclusions |
In other words, none of them worked very well. The paper failed to distinguish between manipulation by physiotherapists, chiropractors and osteopaths and so missed a valuable chance to find out whether there is an advantage to employing people from alternative medicine (the very problem that this NICE guidance should have dealt with)
Steve Vogel, another member of the guidance development group, is an osteopath. Osteopathy has cast off its shady origins better than chiropractic, but it remains a largely evidence-free zone, and is still usually classified as alternative medicine.
Peter Dixon DC FCC FBCA is chairman of the General Chiropractic Council and founder of Peter Dixon Associates. They run six chiropractic clinics. The claims made by these clinics on their web site are mostly related to musculo-skeletal conditions (not, all spine-related however). But they also include
“Chiropractic is also suitable for relieving the symptoms of stress, and optimizing the way the body works is one of the best ways of enhancing health and wellbeing.”
I wonder how they could justify that claim? Then we get
A chiropractor is always willing to discuss individual conditions or answer questions in order to assess whether chiropractic may be of benefit.
Thanks for the invitation. I accepted it. After the first two phone calls, I had learned all I needed.
The first of Peter Dixon’s clinics that I called, was asked about my son who was suffeiing from perpetual colic. I asked for advice. I was put through to the chiropractor. Here are some extracts from the conversation.
“I think now it’s termed irritable baby syndrome. . . . . We’ve found chiropractic is very effective for colic . . . . £50 up to 3/4 hour which would involve taking a case history, examining the baby, with regard to seeing how the joints in the spine work because often colic is down to, er um, faulty movement patterns in the spine. We deal with an awful lot of things to do with the frame -how the spine moves -and it’s often problems with the way that the bones of the spine move in infants and babies that is the underlying cause in colicky symptoms. . . usually on the whole, I’ve shot myself in the foot by saying this in the past, if there are -um when I say back problems they’re usually temporary issues -when they are there the response for most babies is quite quick . . . it depends on how it’s related to what’s gone on in the birth process -there is usually some traumatic cause and it usually sets up a problem in the upper neck or the mid-back and that will drive those colic symptoms. . . . Yes it’s quite a straightforward thing we just check the baby’s spine and see if it’s problem we can deal with or not.”
Yes, I think you just shot yourself in the foot again. I have no idea in what fraction of cases a chiropractor would fail to claim that it was a case that they could deal with. At least that possibility was envisaged. But when I asked where he’d refer me to in such case I was told it might be a result of bottle feeding -“what they consume”. So I expect it would have been sent to some sort of “nutritional therapist” who would have used one of their usual battery of unreliable tests for food allergies.
I tried a second clinic in Peter Dixon’s empire and asked if chiropractic could help with asthma.”It can do, depending on what type of asthma you have". After some questions I was asked
“Do you have any general aches and pains otherwise, any tension .problems round the rib cage or thoracic spine . . . There are two things we’d look as chiropractors as to whether we could help or not and that would include the tension round the rib cage -in any type of asthma you’ll become tight round the rib cage and merely by keeping that area loose you’d help to stop the asthma from becoming quite as bad. And the second part is we’d look at the neck area with you to see if there is any restriction there -which houses the nerve supply to the lungs which can be indicated in some asthma cases also.”
I was invited to come for a free screen, so I asked if it usually worked quickly, “It depends what the problem is but you’d need a course I suspect”. £45 for the first appointment then £28 per session. “In most cases you’d need to look at a six to eight session course”.
Would anyone with experience of crying babies or of asthma like to comment on these proposed treatments? They are not my idea of evidence-based treatments and I find it quite surprising that someone who sponsors them is thought appropriate to write guidance for NICE.
This sort of ‘sting’ always makes me feel a bit uneasy, but it seems to be the only way to find out what actually goes on. And what goes on has all the appearance of classic bait and switch. You go in for your backache, and before you know where you are you are being sold a course of treatment to stop your baby crying.
Media follow-up after the NICE announcement
Sadly, I heard that the Today programme (my favourite news programme) was pretty wet. if only their science reporting was as good as their politics reporting.
The 27th May was certainly pretty busy for me, Apart from a couple of local paper interviews, this is what happened,
Sky News TV. Richard Suchet and two cameraman came to UCL and filmed a lot of stuff out of which a 20 second clip was used. And then they grumble that they don’t make money.
BBC TV 6 o’clock News. Similar, but at least only two people this time. Both TV stations spent ages showing pictures of people having needles pushed into them and very little time discussing the problems. A pathetically bad attempt at science reporting. Radio, on the whole, did much better
BBC Three Counties Radio (09.20) Host Ronnie Barbour, The daytime talk shows may be appalling to some of us, but the hosts did a far better job of airing the problems than TV [download the mp3].
Radio 5 Live Victoria Derbyshire [download the mp3]
BBC Radio Sheffield (12.05) was the best talk show by far. First speaker was Steve Vogel, the osteopath from the guidance development group. Although invited by the rather sensible host, Rony, to respond to the idea that a secondary consequence of the guidance would be to introduce hocus-pocus, he steadfastly refused to answer the question. At the end a rather sensible GP summed up the view from the coalface. [play the mp3]
Radio 4 PM programme This excellent early evening news programme is run by Eddie Mair. It was the best interview yet. The other side was put by Martin Underwood, chair of the guidance development group [play the mp3]
Underwood said “the evidence shows that it [acupuncture] works”. I disagree. The evidence shows that acupuncture, in a non-blind comparison with no acupuncture shows a small, variable additional effect that doesn’t last and is of marginal clinical significance, That is not what I call “works”. Underwood then indulges in the subgroup analysis fallacy by asserting that a few people get a large benefit from acupuncture. Or perhaps a few people just happen to get better that day. I was not convinced.
More 4 News TV 20.20 was an interview, with the other side being put by my old friend, George Lewith.
During the introduction, an acupuncturist. Lisa Sherman, ‘explained’ acupuncture in the usual sort of utterly meaningless words that illustrate perfectly the problem.
George Lewith said that “we don’t have a good pretend form of acupuncture”. “We don’t have a good placebo and we can demonstrate that acupuncture is literally twice as effective as conventional care”. The first is simply nonsense: huge efforts have gone into developing good controls in acupuncture studies (see, for example, Barker Bausell’s book, Snake Oil Science). And I hope that George will send the references for his “twice as effective” claim. It seems to me to be nothing short of preposterous.
My conclusions
So what went wrong?
One problem could be regarded as medical arrogance. The fact is that the problem of low back pain has not been solved, either by drugs or anything else. It is a failure of medicine (and of pharmacology). That should be the premise of all discussions, and it smacks of arrogance not to tell people straight out. Of course there are some cases when causes can be identified, and perhaps remedied, usually by surgery, but these are the exceptions not the rule.
One consequence of the inability of medicine to help much is that patients get desperate, and willing to try anything. And of course if they happen to have a remission, that is attributed to the treatment, however preposterous that treatment may have been. Conditions like back pain that come and go unpredictable are a gift for quacks.
Another consequence, for researchers rather than patients, is to clutch at straws. Even small and inconsistent effects are seized on as ‘successes’. This phenomenon seems to be part of the reason for the NICE guidance. Another reason is, almost certainly, the grinding of axes by some of the people who wrote it.
What should be done now?
Professor Sir Michael Rawlins is a sensible chap. He cares about evidence, But it does seem that in this case, he might have taken his eye off the ball, for once. In my opinion, he should restore the reputation of NICE by withdrawing this guidance and starting again.
Follow-up
An interesting document has come my way. It shows the responses of the guidance group to the consultation on the draft guidance. Many people made comments not unlike mone, but they were all brushed aside in a way that looks to me rather partisan. The document appears to have vanished from NICE’s web site, but you can download it here.
Friday 29th May. The Times prints a letter from two consultants in pain medicine, Joan Hestor and Stephen Ward. It says, inter alia
“As experienced pain specialists we feel that NICE has lost its way in publishing these guidelines.”
“We are saddened that NICE has chosen to ignore our important role and promote seemingly unworkable and for the most part clinically ineffective treatments”
Friday 29th May. NICE has had a good reputation in the USA for its important, and usually high-quality, attempts to assess what works and what doesn’t. That makes it all the sadder to see it condemned already from the USA for its latest effort. The excellent Yale neurologist, Steven Novella, has written about it on his Neurologica blog.
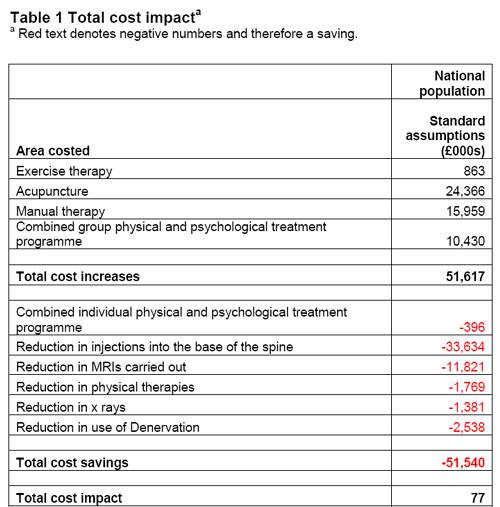
Friday 29th May. A correspondent points out that the costings of the guidance can be found on the NICE web site. Table 1 has a strong air of make-believe.
The Daily Mail (29 May 2009). Their article quotes serious criticisms of NICE.
Dr Ron Cooper, past chairman of the group and a consultant pain specialist in Northern Ireland, said: ‘I have never known so many pain medicine specialists to be so furious. More patients will end up having more expensive surgery, which is unnecessary, risky and has worse results.
‘NICE made it difficult for us to submit evidence to a committee on which there was not one experienced pain physician.
‘The guidelines will make us the laughing stock of Europe, Australia and the U.S. where pain specialists will continue to have full access to a wide range of treatments.’
Chirowatch suspended. 30 May 2009. The invaluable chiro-watch site, http://www.chirowatch.com, run by Dr Canadian physician, Dr Tom Polevoy, has been “suspended”. In fact the whole of his domain, healthwatcher.net, has been disabled. It seems that this was the result of a legal threat to his ISP, not by chiropractors this time, but by William O’Neill of the Canadian Cancer Research Group, which is far from being what the respectable-sounding title suggests, according to Dr Stephen Barrett. The site will be back soon, I’m told. Meanwhile you can read the suspended page here, and the only result of their hamfisted bullying will be to vastly increase the number of people who read it. You can read lots more at Quackwatch’s chirobase and at ebm-first.
A new blog, Not as NICE as you think appeared on May 30th. It is written by a pain physician, Stephen Ward. and is devoted to pointing out the serious problems raised by NICE’s guidance. It starts with the (very critical) World Institute of Pain Press Release.
British Medical Journal has more flak for the NICE guidelines
And the BMJ has published a letter signed by 50 consultants in pain medicine, NICE guidelines on low back pain are flawed.(this will probably appear as a letter in the print edition of the BMJ).
First the MHRA lets down the public by allowing deceptive labelling of sugar pills (see here, and this this blog). Now it is the turn of NICE to betray its own principles.
The National Institute for Health and Clinical Excellence (NICE) describes its job thus
“NICE is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health.”
Its Guidance document on Low Back Pain will be published on Wednesday 27 May 2009, but the newspapers have already started to comment, presumably on the assumption that it will have changed little from the Draft Guidance of September 2008. These comments may have to be changed as soon as the final version becomes available.
The draft guidance, though mostly sensible, has two recommendations that I believe to be wrong and dangerous. The recommendations include (page 7) these three.
- Consider offering a course of manual therapy including spinal manipulation of up to 9 sessions over up to 12 weeks.
- Consider offering a course of acupuncture needling comprising up to 10 sessions over a period of up to 12 weeks.
- Consider offering a structured exercise programme tailored to the individual.
All three of this options are accompanied by a footnote that reads thus.
“A choice of any of these therapies may be offered, taking into account patient preference.”
On the face if it, this might seem quite reasonable. All three choices seem to be about as effective (or ineffective) as each other, so why not let patients choose between them?
Actually there are very good reasons, but NICE does not seem to have thought about them. In the past I have had a high opinion of NICE but it seems that even they are now getting bogged down in the morass of political correctness and officialdom that is the curse of the Department of Health. It is yet another example of DC’s rule number one.
Never trust anyone who uses the word ‘stakeholder’.
They do use it, often.
So what is so wrong?
For a start, I take it that the reference to “spinal manipulation” in the first recommendation is a rather cowardly allusion to chiropractic. Why not say so, if that’s whar you mean? Chiropractic is mentioned in the rest of the report but the word doesn’t seem to occur in the recommendations. Is NICE perhaps nervous that it would reduce the credibility of the report if the word chiropractic were said out loud?
Well, they have a point, I suppose. It would.
That aside, here’s what’s wrong.
The Evidence
I take as my premise that the evidence says that no manipulative therapy has any great advantage over the others. They are all more or less equally effective. Perhaps I should say, more or less equally ineffective, because anyone who claims to have the answer to low back pain is clearly deluded (and I should know: nobody has fixed mine yet). So for effectiveness there are no good grounds to choose between exercise, physiotherapy, acupuncture or chiropractic. There is, though, an enormous cultural difference. Acupuncture and chiropractic are firmly in the realm of alternative medicine. They both invoke all sorts of new-age nonsense for which there isn’t the slightest good evidence. That may not poison your body, but it certainly poisons your mind.
Acupuncturists talk about about “Qi”, “meridians”, “energy flows”. The fact that “sham” and “real” acupuncture consistently come out indistinguishable is surely all the evidence one needs to dismiss such nonsense. Indeed there is a small group of medical acupuncturists who do dismiss it. Most don’t. As always in irrational subjects, acupuncture is riven by internecine strife between groups who differ in the extent of their mystical tendencies,
Chiropractors talk of “subluxations”, an entirely imaginary phenomenon (but a cause of much unnecessary exposure to X-rays). Many talk of quasi-religious things like “innate energy”. And Chiropractic is even more riven by competing factions than acupuncture. See, for example, Chiropractic wars Part 3: internecine conflict.
The bait and switch trick
This is the basic trick used by ‘alternative therapists’ to gain respectability.
There is a superb essay on it by the excellent Yale neurologist Steven Novella: The Bait and Switch of Unscientific Medicine. The trick is to offer some limited and reasonable treatment (like back manipulation for low back pain). This, it seems, is sufficient to satisfy NICE. But then, once you are in the showroom, you can be exposed to all sorts of other nonsense about “subluxations” or “Qi”. Still worse, you will also be exposed to the claims of many chiropractors and acupuncturists to be able to cure all manner of conditions other than back pain. But don’t even dare to suggest that manipulation of the spine is not a cure for colic or asthma or you may find yourself sued for defamation. The shameful legal action of the British Chiropractic Association against Simon Singh (follow it here) led to an addition to DC’s Patients’ Guide to Magic Medicine.
(In the face of such tragic behaviour, one has to be able to laugh).
Libel: A very expensive remedy, to be used only when you have no evidence. Appeals to alternative practitioners because truth is irrelevant.
NICE seems to have fallen for the bait and switch trick, hook line and sinker.
The neglected consequences
Once again, we see the consequences of paying insufficient attention to the Dilemmas of Alternative Medicine.
The lying dilemma
If acupuncture is recommended we will have acupuncturists telling patients about utterly imaginary things like “Qi” and “meridians”. And we will have chiropractors telling them about subluxations and innate energy. It is my opinion that these things are simply make-believe (and that is also the view of a minority of acupuncturist and chiropractors). That means that you have to decide whether the supposed benefits of the manipulation are sufficient to counterbalance the deception of patients.
Some people might think that it was worth it (though not me). What is unforgivable is not to consider even the question. The NICE guidance says not a word about this dilemma. Why not?
The training dilemma
The training dilemma is even more serious. Once some form of alternative medicine has successfully worked the Bait and Switch trick and gained a toehold in the NHS, there will be an army of box-ticking HR zombies employed to ensure that they have been properly trained in “subluxations” or “Qi”. There will be quangos set up to issue National Occupational Standards in “subluxations” or “Qi”. Skills for Health will issue “competences” in “subluxations” or “Qi” (actually they already do). There will be courses set up to teach about “subluxations” or “Qi”, some even in ‘universities’ (there already are).
The respectability problem
But worst of all, it will become possible for aupuncturists and chiropractors to claim that they now have official government endorsement from a prestigious evidence-based organisation like NICE for “subluxations” or “Qi”. Of course this isn’t true. In fact the words “subluxations” or “Qi” are not even mentioned in the draft report. That is the root of the problem. They should have been. But omitting stuff like that is how the Bait and Switch trick works.
Alternative medicine advocates crave, above all, respectability and acceptance. It is sad that NICE seems to have given them more credibility and acceptance without having considered properly the secondary consequences of doing so,
How did this failure of NICE happen?
It seems to have been a combination of political correctness, failure to consider secondary consequences, and excessive influence of the people who stand to make money from the acceptance of alternative medicine.
Take, for example, the opinion of the British Pain Society. This organisation encompasses not just doctors. It
includes “doctors, nurses, physiotherapists, scientists, psychologists, occupational therapists and other healthcare professionals actively engaged in the diagnosis and treatment of pain and in pain research for the benefit of patients”. Nevertheless, their response to the draft guidelines pointed out that the manipulative therapies as a whole were over-represented.
|
Manipulation The guidelines assess 9 large groups of interventions of which manual therapies are only one part. The full GDG members panel of 13 individuals included two proponents of spinal manipulation/mobilisation (P Dixon and S Vogel). In addition, the chair of the panel (M Underwood) is the lead author of the UKBEAM trial on which the positive recommendation for |
It seems that the Pain Society were quite right.
LBC 97.3 Breakfast Show (25 May 2009) had a quick discussion on acupuncture (play mp3 file). After I had my say, the other side was put by Rosey Grandage. She has (among other jobs) a private acupuncture practice so she is not quite as unbiassed as me). As usual, she misrepresents the evidence by failing to distinguish between blind and non-blind studies. She also misrepresented what I said by implying that I was advocating drugs. That was not my point and I did not mention drugs (they, like all treatments, have pretty limited effectiveness, and they have side effects too). She said “there is very good evidence to show they (‘Qi’ and ‘meridians’] exist”. That is simply untrue.
There can’t be a better demonstration of the consequences of falling for bait and switch than the defence mounted by Rosey Grandage. NICE may not mention “Qi” and “meridians”; but the people they want to allow into the NHS have no such compunctions.
I first came across Rosey Grandage when I discovered her contribution to the Open University/BBC course K221. That has been dealt with elsewhere. A lot more information about acupuncture has appeared since then. She doesn’t seem to have noticed it. Has she not seen the Nordic Cochrane Centre report? Nor read Barker Bausell, or Singh & Ernst? Has she any interest in evidence that might reduce her income? Probably not.
Where to find out more
An excellent review of chiropractic can be found at the Layscience site. It was written by the indefatigable ‘Blue Wode’ who has provided enormous amounts of information at the admirable ebm-first site (I am authorised to reveal that ‘Blue Wode’ is the author of that site). There you will also find much fascinating information about both acupuncture and about chiropractic.
I’m grateful to ‘Blue Wode’ for some of the references used here.
Follow-up
| The Prince of Wales’ Foundation for Integrated Health (FiH) is a propaganda organisation that aims to persuade people, and politicians, that the Prince’s somewhat bizarre views about alternative medicine should form the basis of government health policy.
His attempts are often successful, but they are regarded by many people as being clearly unconstitutional. |
 |
The FiH’s 2009 AnnualConferen ce conference was held at The King’s Fund, London 13 – 14 May 2009. It was, as always, an almost totally one-sided affair devoted to misrepresentation of evidence and the promotion of magic medicine. But according to the FiH, at least, it was a great success. The opening speech by the Quacktitioner Royal can be read here. It has already been analysed by somebody who knows rather more about medicine than HRH. He concludes
“It is a shocking perversion of the real issues driven by one man; unelected, unqualified and utterly misguided”.
We are promised some movie clips of the meeting. They might even make a nice UK equivalent of “Integrative baloney @ Yale“.
This post is intended to provide some background information about the speakers at the symposium. But let’s start with what seems to me to be the real problem. The duplicitous use of the word “integrated” to mean two quite different things.
The problem of euphemisms: spin and obfuscation
One of the problems of meetings like this is the harm done by use of euphemisms. After looking at the programme, it becomes obvious that there is a rather ingenious bit of PR trickery going on. It confuses (purposely?) the many different definitions of the word “integrative” . One definition of “Integrative medicine” is this (my emphasis).
” . . . orienting the health care process to engage patients and caregivers in the full range of physical, psychological, social, preventive, and therapeutic factors known to be effective and necessary for the achievement of optimal health.”
That is a thoroughly admirable aim. And that, I imagine, is the sense in which several of the speakers (Marmot, Chantler etc) used the term. Of course the definition is rather too vague to be very helpful in practice, but nobody would dream of objecting to it.
But another definition of the same term ‘integrative medicine’ is as a PR-friendly synonym for ‘alternative medicine’, and that is clearly the sense in which it is used by the Prince of Wales’ Foundation for Integrated Health (FIH), as is immediately obvious from their web site.
The guide to the main therapies supports everything from homeopathy to chiropractic to naturopathy, in a totally uncritical way. Integrated service refers explicitly to integration of ‘complementary’ medicine, and that itself is largely a euphemism for alternative medicine. For example, the FIH’s guide to homeopathy says
“What is homeopathy commonly used for?
Homeopathy is most often used to treat chronic conditions such as asthma; eczema; arthritis; fatigue disorders like ME; headache and migraine; menstrual and menopausal problems; irritable bowel syndrome; Crohn’s disease; allergies; repeated ear, nose, throat and chest infections or urine infections; depression and anxiety.”
But there is not a word about the evidence, and perhaps that isn’t surprising because the evidence that it works in any of these conditions is essentially zero.
The FIH document Complementary Health Care: A Guide for Patients appears to have vanished from the web after its inaccuracy received a very bad press, e.g. in the Times, and also here. It is also interesting that the equally widely criticised Smallwood report (also sponsored by the Prince of Wales) seems to have vanished too).
The programme for the meeting can be seen here, for Day 1, and Day 2
Conference chair Dr Phil Hammond, GP, comedian and health service writer. Hammond asked the FIH if I could speak at the meeting to provide a bit of balance. Guess what? They didn’t want balance.
09:30 Opening session
Dr Michael Dixon OBE
09:30 Introduction: a new direction for The Prince’s Foundation for Integrated Health and new opportunities in integrated health and care. Dr Michael Dixon, Medical Director, FIH
Michael Dixon is devoted to just about every form of alternative medicine. As well as being medical director of the Prince’s Foundation he also runs the NHS Alliance. Despite its name, the NHS Alliance is nothing to do with the NHS and acts, among other things, as an advocate of alternative medicine on the NHS, about which it has published a lot.
Dr Dixon is also a GP at College Surgery, Cullompton, Devon, where his “integrated practice” includes dozens of alternative practitioners. They include not only disproven things like homeopathy and acupuncture, but also even more bizarre practitioners in ‘Thought Field Therapy‘ and ‘Frequencies of Brilliance‘.
To take only one of these, ‘Frequencies of Brilliance’ is bizarre beyond belief. One need only quote its founder and chief salesperson.
“Frequencies of Brilliance is a unique energy healing technique that involves the activation of energetic doorways on both the front and back of the body.”
“These doorways are opened through a series of light touches. This activation introduces high-level Frequencies into the emotional and physical bodies. It works within all the cells and with the entire nervous system which activates new areas of the brain.”
“Frequencies of Brilliance is a 4th /5th dimensional work. The process is that of activating doorways by lightly touching the body or working just above the body.”
“Each doorway holds the highest aspect of the human being and is complete in itself. This means that there is a perfect potential to be accessed and activated throughout the doorways in the body.”
Best of all, it can all be done at a distance (that must help sales a lot). One is reminded of the Skills for Health “competence” in distant healing (inserted on a government web site at the behest (you guessed it) of the Prince’s Foundation, as related here)
“The intent of a long distance Frequencies of Brilliance (FOB) session is to enable a practitioner to facilitate a session in one geographical location while the client is in another.
A practitioner of FOB that has successfully completed a Stage 5 Frequency workshop has the ability to create and hold a stable energetic space in order to work with a person that is not physically present in the same room.
The space that is consciously created in the Frequencies of Brilliance work is known as the “Gap”. It is a space of nonlinear time. It contains ”no time and no space” or respectively “all time and all space”. Within this “Gap” a clear transfer of the energies takes place and is transmitted to an individual at a time and location consciously intended. Since this dimensional space is in non-linear time the work can be performed and sent backward or forward in time as well as to any location.
The Frequencies of Brilliance work cuts through the limitations of our physical existence and allows us to experience ourselves in other dimensional spaces. Therefore people living in other geographic locations than a practitioner have an opportunity to receive and experience the work.
The awareness of this dimensional space is spoken about in many indigenous traditions, meditation practices, and in the world of quantum physics. It is referred to by other names such as the void, or vacuum space, etc.”
This is, of course, preposterous gobbledygook. It, and other things in Dr Dixon’s treatment guide, seem to be very curious things to impose on patients in the 21st century.
Latest news. The Mid-Devon Star announces yet more homeopathy in Dr Dixon’s Cullompton practice. This time it comes in the form of a clinic run from the Bristol Homeopathic Hospital. I guess they must be suffering from reduced commissioning like all the other homeopathic hospitals, but Dr Dixon seems to have come to their rescue. The connection seems to be with Bristol’s homeopathic consultant, Dr Elizabeth A Thompson. On 11 December 2007 I wrote to Dr Thompson, thus
|
In March 2006, a press release http://www.ubht.nhs.uk/press/view.asp?257 announced a randomised trial for homeopathic treatment of asthma in children. This was reported also on the BBC http://news.bbc.co.uk/1/hi/england/bristol/4971050.stm . I’d be very grateful if you could let me know when results from this trial will become available. Yours sincerely David Colquhoun |
The reply, dated 11 December 2007, was unsympathetic
|
I have just submitted the funders report today and we have set ourselves the deadline to publish two inter-related papers by March 1st 2007. Can I ask why you are asking and what authority you have to gain this information. I shall expect a reply to my questions, |
I answered this question politely on the same day but nevertheless my innocent enquiry drew forth a rather vitriolic complaint from Dr Thompson to the Provost of UCL (dated 14 December 2007). In this case, the Provost came up trumps. On 14 January 2008 he replied to Thompson: “I have looked at the email that you copied to me, and I must say that it seems an entirely proper and reasonable request. It is not clear to me why Professor Colquhoun should require some special authority to make such direct enquiries”. Dr Thompson seems to be very sensitive. We have yet to see the results of her trial in which I’m still interested.
Not surprisingly, Dr Dixon has had some severe criticism for his views, not least from the UK’s foremost expert on the evidence for efficacy, Prof Edzard Ernst. Accounts of this can be found in Pulse,
and on Andrew Lewis’s blog.
Dixon is now (in)famous in the USA too. The excellent Yale neurologist, Steven Novella, has written an analysis of his views on Science Based Medicine. He describes Dr. Michael Dixon as “A Pyromaniac In a Field of (Integrative) Straw Men”
Peter Hain
09:40 Politics and people: can integrated health and care take centre stage in 2009/2010? Rt Hon Peter Hain MP
It seems that Peter Hain was converted to alternative medicine when his first baby, Sam, was born with eczema. After (though possibly not because of) homeopathic treatment and a change in diet, the eczema got better. This caused Hain, while Northern Ireland Secretary to spend £200,000 of taxpayers’ money to set up a totally uninformative customer satisfaction survey, which is being touted elsewhere in this meeting as though it were evidence (see below). I have written about this episode before: see Peter Hain and Get Well UK: pseudoscience and privatisation in Northern Ireland.
I find it very sad that a hero of my youth (for his work in the anti-apartheid movement) should have sunk to promoting junk science, and even sadder that he does so at my expense.
There has been a report on Hain’s contribution in Wales Online.
09:55 Why does the Health Service need a new perspective on health and healing? Sir Cyril Chantler, Chair, King’s Fund, previous Dean, Guy’s Hospital and Great Ormond Street
Cyril Chantler is a distinguished medical administrator. He also likes to talk and we have discussed the quackery problem several times. He kindly sent me the slides that he used. Slide 18 says that in order to do some good we “need to demonstrate that the treatment is clinically effective and cost effective for NHS use”. That’s impeccable, but throughout the rest of the slides he talks of integrating with complementary” therapies, the effectiveness of which is either already disproved or simply not known.
I remain utterly baffled by the reluctance of some quite sensible people to grasp the nettle of deciding what works. Chantler fails to grasp the nettle, as does the Department of Health. Until they do so, I don’t see how they can be taken seriously.
10.05 Panel discussion
The Awards
10:20 Integrated Health Awards 2009 Introduction: a review of the short-listed applications
10:45 Presentations to the Award winners by the special guest speaker
11:00 Keynote address by special guest speaker
Getting integrated
Dr David Peters
12:00 Integration, long term disease and creating a sustainable NHS. Professor David Peters, Clinical Director and Professor of Integrated Healthcare, University of Westminster
I first met David Peters after Nature ran my article, Science Degrees without the Science. .One of the many media follow-ups of that article was on Material World (BBC Radio 4). This excellent science programme, presented by Quentin Cooper, had a discussion between me and David Peters ( listen to the mp3 file).
There was helpful intervention from Michael Marmot who had talked, in the first half of the programme, about his longitudinal population studies.
Marmot stressed the need for proper testing. In the case of
homeopathy and acupuncture, that proper testing has largely been done. The tests were failed.
The University of Westminster has, of course, gained considerable notoriety as the university that runs more degree programmes in anti-scientific forms of medicine than any other. Their lecture on vibrational medicine teaches students that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbances at all levels of being”. So far their vice-chancellor, Professor Geoffrey Petts, has declined to answer enquiries about whether he thinks such gobbledygook is appropriate for a BSc degree.
But he did set up an internal enquiry into the future of their alternative activities. Sadly that enquiry seems to have come to the nonsensical conclusion that the problem can be solved by injection of good science into the courses, as reported here and in the Guardian.
It seems obvious that if you inject good science into their BSc in homeopathy the subject will simply vanish in a puff of smoke.
In 2007, the University of Westminster did respond to earlier criticism in Times Higher Education, but their response seemed to me to serve only to dig themselves deeper into a hole.
Nevertheless, Westminster has now closed down its homeopathy degree (the last in the country to go) and there is intense internal discussion going on there. I have the impression that Dr Peters’ job is in danger. The revelation of more slides from their courses on homeopathy, naturopathy and Chinese herbal medicine shows that these courses are not only barmy, but also sometimes dangerous.
Professor Chris Fowler
12:10 Educating tomorrow’s integrated doctors. Professor Chris Fowler, Dean for Education, Barts and The London School of Medicine and Dentistry
I first came across Dr Fowler when I noticed him being praised for his teaching of alternative medicine to students at Barts and the London Medical School on the web site of the Prince’s Foundation. I wrote him a polite letter to ask if he really thought that the Prince of Wales was the right person to consult about the education of medical students. The response I got was, ahem, unsympathetic. But a little while later I noticed that two different Barts students had set up public blogs that criticised strongly the nonsense that was being inflicted on them.
At that point, I felt it was necessary to support the students who, it seemed to me, knew more about medical education than Professor Fowler. It didn’t take long to uncover the nonsense that was being inflicted on the students: read about it here.
There is a follow-up to this story here. Fortunately, Barts’ Director of Research, and, I’m told, the Warden of Barts, appear to agree with my view of the harm that this sort of thing can do to the reputation of Barts, so things may change soon,
Dame Donna Kinnair
12:30 Educating tomorrow’s integrated nurses.
Dame Donna Kinnair, Director of Nursing, Southwark PCT
As far as I can see, Donna Kinnair has no interest in alternative medicine. She is director of nursing at Southwark primary care trust and was an adviser to Lord Laming throughout his inquiry into the death of Victoria Climbié. I suspect that her interest is in integrating child care services (they need it, judging by the recent death of ‘Baby P’). Perhaps her presence shows the danger of using euphemisms like ‘integrated medicine’ when what you really mean is the introduction of unproven or disproved forms of medicine.
Michael Dooley
12:40 Integrating the care of women: an example of the new paradigm. Michael Dooley, Consultant Obstetrician and Gynecologist
DC’s rule 2. Never trust anyone who uses the word ‘paradigm’. It is a sure-fire sign of pseudoscience. In this case, the ‘new paradigm’ seems to be the introduction of disproven treatment. Dooley is a gynaecologist and Medical Director of the Poundbury Clinic. His clinic offers a whole range of unproven and disproved treatments. These include acupuncture as an aid to conception in IVF. This is not recommended by the Cochrane review, and one report suggests that it hinders conception rather than helps.
12.40 Discussion
13.00 – 14.00 Lunch and Exhibition
15.30 Tea
Boo Armstrong and Get Well UK
16.00 Integrated services in action: The Northern
Ireland experience: what has it shown us and what are its implications?
Boo Armstrong of Get Well UK with a team from the NI study
I expect that much will be made of this “study”, which, of course, tells you absolutely nothing whatsoever about the effectiveness of the alternative treatments that were used in it. This does not appear to be the view of Boo Armstrong, On the basis of the “study”, her company’s web site proclaims boldly
“Complementary Medicine Works
Get Well UK ran the first government-backed complementary therapy project in the UK, from February 2007 to February 2008″
This claim appears, prima facie, to breach the Unfair Trading Regulations of May 2008. The legality of the claim is, at the moment, being judged by a Trading Standards Officer. In any case, the “study” was not backed by the government as a whole, but just by Peter Hain’s office. It is not even clear that it had ethical approval.
The study consisted merely of asking people who had seen an alternative medicine practitioner whether they felt better or worse. There was no control group; no sort of comparison was made. It is surely obvious to the most naive person that a study like this cannot even tell you if the treatment has a placebo effect, never mind that it has any genuine effects of its own. To claim that it does so seems to be simply dishonest. There is no reason at all to think that the patients would not have got better anyway.
It is not only Get Well UK who misrepresent the evidence. The Prince’s
Foundation itself says
“Now a new, year long trial supported by the Northern Ireland health service has . . . demonstrated that integrating complementary and conventional medicine brings measurable benefits to patients’ health.”
That is simply not true. It is either dishonest or stupid. Don’t ask me which, I have no idea.
This study is no more informative than the infamous Spence (2005) ‘study’ of the same type, which seems to be the only thing that homeopaths can produce to support their case.
There is an excellent analysis of the Northern Ireland ‘study’ by Andy Lewis, The Northern Ireland NHS Alternative Medicine ‘Trial’. He explains patiently, yet again, what constitutes evidence and why studies like this are useless.
His analogy starts
” . . . the Apple Marketing Board approach the NHS and ask for £200,000 to do a study to show the truth behind the statement ‘An apple a day keeps the doctor away’. The Minister, being particularly fond of apples, agrees and the study begins.”
16.30 Social enterprise and whole systems integrated care. Dee Kyne, Sandwell PCT and a GP. Developing an integrated service in secondary care
Dee Kyne appears to be CEO of KeepmWell Ltd (a financial interest that is not mentioned).
Peter Mackereth, Clinical Lead, Supportive Services, Christie Hospital NHS Foundation Trust
I had some correspondence with Mackereth when the Times (7 Feb 2007) published a picture of the Prince of Wales inspecting an “anti-MRSA aromatherapy inhaler” in his department at the Christie. It turned out that the trial they were doing was not blind No result has been announced anyway, and on enquiry, I find that the trial has not even started yet. Surprising, then to find that the FIH is running the First Clinical Aromatherapy Conference at the Christie Hospital, What will there be to talk about?
Much of what they do at the Christie is straightforward massage, but they also promote the nonsensical principles of “reflexology” and acupuncture.
The former is untested. The latter is disproven.
Parallel Sessions
Developing a PCT funded musculoskeletal service Dr Roy Welford, Glastonbury Health Centre
Roy Welford is a Fellow of the Faculty of Homeopathy, and so promotes disproven therapies. The Glastonbury practice also advertises acupuncture (disproven), osteopathy and herbal medicine (largely untested so most of it consists of giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety).
Making the best of herbal self-prescription in integrated practice: key remedies and principles. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon
Simon Mills is a herbalist who now describes himself as a “phytotherapist” (it sounds posher, but the evidence, or lack of it, is not changed by the fancy name). Mills likes to say things like “there are herbs for heating and drying”, “hot and cold” remedies, and to use meaningless terms like “blood cleanser”, but he appears to be immune to the need for good evidence that herbs work before you give them to sick people. He says, at the end of a talk, “The hot and the cold remain the trade secret of traditional medicine”. And this is the 21st Century.
Practical ways in which complementary approaches can improve the treatment of cancer. Professor Jane Plant, Author of “Your life in your hands” and Chief Scientist, British Geological Society and Professor Karol Sikora, Medical Director, Cancer Partners UK
Jane Plant is a geologist who, through her own unfortunate encounter with breast cancer, became obsessed with the idea that a dairy-free diet cured her. Sadly there is no good evidence for that idea, according to the World Cancer Research Fund Report, led by Professor Sir Michael Marmot. No doubt her book on the subject sells well, but it could be held that it is irresponsible to hold out false hopes to desperate people. She is a supporter of the very dubious CancerActive organisation (also supported by Michael Dixon OBE –see above) as well as the notorious pill salesman, Patrick Holford (see also here).
Karol Sikora, formerly an oncologist at the Hammersmith Hospital, is now Dean of Medicine at the University of Buckingham (the UK’s only private university). He is also medical director at CancerPartners UK, a private cancer company.
He recently shot to fame when he appeared in a commercial in the USA sponsored by “Conservatives for Patients’ Rights”, to pour scorn on the NHS, and to act as an advocate for the USA’s present health system. A very curious performance. Very curious indeed.
His attitude to quackery is a mystery wrapped in an enigma. One was somewhat alarmed to see him sponsoring a course at what was, at first, called the British College of Integrated Medicine, and has now been renamed the Faculty of Integrated Medicine That grand title makes it sound like part of a university. It isn’t.

The alarm was as result of the alliance with Dr Rosy Daniel (who promotes an untested herbal conconction, Carctol, for ‘healing’ cancer) and Dr Mark Atkinson (a supplement salesman who has also promoted the Qlink pendant. The Qlink pendant is a simple and obvious fraud designed to exploit paranoia about WiFi killing you.
The first list of speakers on the proposed diploma in Integrated Medicine was an unholy alliance of outright quacks and commercial interests. It turned out that, although Karol Sikora is sponsoring the course, he knew nothing about the speakers. I did and when I pointed this out to Terence Kealey, vice-chancellor of Buckingham, he immediately removed Rosy Daniel from directing the Diploma. At the moment the course is being revamped entirely by Andrew Miles. There is hope that he’ll do a better job. It has not yet been validated by the University of Buckingham. Watch this space for developments.
Stop press It is reported in the Guardian that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear. More developments in the follow-up.
The role of happy chickens in healing: farms as producers of health as well as food – the Care Farm Initiative Jonathan Dover, Project Manager, Care Farming, West Midlands.
“Care farming is a partnership between farmers, participants and health & social care providers. It combines the care of the land with the care of people, reconnecting people with nature and their communities.”
Sounds lovely, I wonder how well it works?
What can the Brits learn from the Yanks when it comes to integrated health? Jack Lord, Chief Executive Humana Europe
It is worth noticing that the advisory board of Humana Europe includes Micheal Dixon OBE, a well known advocate of alternative medicine (see
above). Humana Europe is a private company, a wholly owned subsidiary of Humana Inc., a health benefits company with 11 million members and 22,000 employees and headquarters in Louisville, Kentucky. In 2005 it entered into a business partnership with Virgin Group. Humana was mentioned in the BBC Panorama programme “NHS for Sale”. The company later asked that it be pointed out that they provide commissioning services, not clinical services [Ed. well not yet anyway].
Humana’s document “Humana uses computer games to help people lead healthier lives” is decidedly bizarre. Hang on, it was only a moment ago that we were being told that computer games rewired your brain.
Day 2 Integrated health in action
09.00 Health, epidemics and the search for new solutions. Sir Michael Marmot, Professor of Epidemiology and Public Health, Royal Free and University College Medical School
It is a mystery to me that a distinguished epidemiologist should be willing to keep such dubious company. Sadly I don’t know what he said, but judging my his publications and his appearence on Natural World, I can’t imagine he’d have much time for homeopaths.
9.25 Improving health in the workplace. Dame Carol Black, National Director, Health and Work, Department of Health
This is not the first time that Dame Carol has been comtroversial.
9.45 Integrated health in focus: defeating obesity. Professor Chris Drinkwater, President, NHS Alliance.
The NHS Alliance was mentioned above. Enough said.
10.00 Integrated healthcare in focus: new approaches to managing asthma, eczema and allergy. Professor Stephen Holgate, Professor of Immunopharmacology, University of Southampton
10.15 Using the natural environment to increase activity. The Natural England Project: the results from year one. Dr William Bird and Ruth Tucker, Natural England.
10.30 Panel discussion
10.45 Coffee
Self help in action
11.10 Your health, your way: supporting self care through care planning and the use of personal budgets. Angela Hawley, Self Care Lead, Department of Health
11.25 NHS Life Check: providing the signposts to
integrated health. Roy Lambley, Project Director, NHS LifeCheck Programme
This programme was developed with the University of Westminster’s “Health and Well-being Network”. This group, with one exception, is separate from Westminster’s extensive alternative medicine branch (it’s mostly psychologists).
11.45 The agony and the ecstasy of helping patients to help themselves: tips for clinicians, practices and PCTs. Professor
Ruth Chambers, FIH Foundation Fellow.
11.55 Providing self help in practice: Department of Health Integrated Self Help Information Project. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon and Dr Sam Everington, GP, Bromley by Bow.
The Culm Valley Integrated Centre for health is part of the College Surgery Partnership, associated with Michael Dixon OBE (yes, again!).
Simon Mills is the herbalist who says “The hot and the cold remain the trade secret of traditional medicine” .
Sam Everington, in contrast, seems to be interested in ‘integration’ in the real sense of the word, rather than quackery.
Integrated health in action
How to make sense of the evidence on complementary approaches: what works? What might work? What doesn’t work?
Dr Hugh MacPherson, Senior Research Fellow in Health Sciences, York University and Dr Catherine Zollman, Bravewell Fellow
Hugh MacPherson‘s main interest is in acupuncture and he publishes in alternative medicine journals. Since the recent analysis in the BMJ from the Nordic Cochrane Centre (Madsen et al., 2009) it seems that acupuncture is finally dead. Even its placebo effect is too small to be useful. Catherine Zollman is a Bristol GP who is into homeopathy as well as acupuncture. She is closely connected with the Prince’s Foundation via the Bravewell Fellowship. That fellowship is funded by the Bravewell Collaboration, which is run by Christie Mack, wife of John Mack (‘Mack the Knife’), head of Morgan Stanley (amazingly, they still seem to have money). This is the group which, by sheer wealth, has persuaded so many otherwise respectable US universities to embrace every sort of quackery (see, for example, Integrative baloney @ Yale)
The funding of integrated services
14.15 How to get a PCT or practice- based commissioner to fund your integrated service. A PCT Chief Executive and a Practice-Based Commissioning lead.
14.30 How I succeeded: funding an integrated service. Dr John Ribchester, Whitstable
14.45 How we created an acupuncture service in St Albans and Harpenden PBC group. Mo Girach, Chief Executive, STAHCOM
Uhuh Acupunture again. Have these people never read Bausell’s
book? Have they not read the BMJ? Acupuncture is now ell-established to be based on fraudulent principles, and not even to have a worthwhile placeobo effect. STAHCOM seem to be more interested in money than in what works.
Dragon’s Den. Four pitchers lay out their stall for the commissioning dragons
And at this stage there is no prize for guessing that all four are devoted to trying to get funds for discredited treatments
- An acupuncture service for long-term pain. Mike Cummings Chair, Medical Acupuncture Association
- Manipulation for the treatment of back pain Simon Fielding, Founder Chairman of the General Osteopathic Council
- Nigel Clarke, Senior Partner, Learned Lion Partners Homeopathy for long term conditions
- Peter Fisher, Director, Royal Homeopathic Hospital
Sadly it is not stated who the dragons are. One hopes they will be more interested in evidence than the supplicants.
Mike Cummings at least doesn’t believe the nonsense about meridians and Qi. It’s a pity he doesn’t look at the real evidence though.
You can read something about him and his journal at BMJ Group promotes acupuncture: pure greed.
Osteopathy sounds a bit more respectable than the others, but in fact it has never shaken off its cult-like origins. Still many osteopaths make absurd claims to cure all sorts of diseases. Offshoots of osteopathy like ‘cranial osteopathy’ are obvious nonsense. There is no reason to think that osteopathy is any better than any other manipulative therapy and it is clear that all manipulative therapies should be grouped into one.
Osteopathy and chiropractic provide the best ever examples of the folly of giving official government recognition to a branch of alternative medicine before the evidence is in.
Learned Lion Partners is a new one on me. It seems it is
part of Madsen Gornall Ashe Chambers (‘MGA Chambers’) “a grouping of top level, independent specialists who provide a broad range of management consultancy advice to the marketing community”. It’s a management consultant and marketing outfit. So don’t expect too much when it comes to truth and evidence. The company web site says nothing about alternative medicine, but only that Nigel Clarke
“. . . has very wide experience of public affairs issues and campaigns, having worked with clients in many sectors in Europe, North America and the Far East. He has particular expertise in financial, competition and healthcare issues. “
However, all is revealed when we see that he is a Trustee of the Prince’s Foundation where his entry says
“Nigel Clarke is senior partner of Learned Lion Partners. He is a director of Vidapulse Ltd, Really Easy Ltd, Newscounter Ltd and Advanced Transport Systems Ltd. He has worked on the interfaces of public policy for 25 years. He has been chair of the General Osteopathic Council since May 2001, having been a lay member since it was formed. He is now a member of the Council for Healthcare Regulatory Excellence”
The Council for Healthcare Regulatory Excellence is yet another quango that ticks boxes and fails absolutely to grasp the one important point, does it work?. I came across them at the Westminster Forum, and they seemed a pretty pathetic way to spend £2m per year.
Peter Fisher is the last supplicant to the Dragons. He is clinical director of the Royal London Homeopathic Hospital (RLHH), and Queen’s homeopathic physician, It was through him that I got an active interest in quackery. The TV programme QED asked me to check the statistics in a paper of his that claimed that homeopathy was good for fibrositis (there was an elementary mistake and no evidence for an effect). Peter Fisher is also remarkable because he agreed with me that BSc degrees in homeopathy were not justified (on TV –see the movie). And he condemned homeopaths who were caught out recommending their sugar pills for malaria. To that extent Fisher represents the saner end of the homeopathic spectrum. Nevertheless he still maintains that sugar pills work and have effects of their own, and tries to justify the ‘memory of water’ by making analogies with a memory stick or CD. This is so obviously silly that no more comment is needed.
Given Fisher’s sensible condemnation of the malaria fiasco, I was rather surprised to see that he appeared on the programme of a conference at the University of Middlesex, talking about “A Strategy To Research The Potential Of Homeopathy In Pandemic Flu”. The title of the conference was Developing Research Strategies in CAM. A colleague, after seeing the programme, thought it was more like “a right tossers’ ball”.
Much of the homeopathy has now vanished from the RLHH as a result of greatly reduced commissioning by PCTs (read about it in Fisher’s own words). And the last homeopathy degree in the UK has closed down. It seems an odd moment for the FIH to be pushing it so hard.
Follow-up
Stop press It is reported in the Guardian (22 May 2009) that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear, oh dear.
This fascinating fact seems to have been unearthed first by the admirable NHS Blog Doctor, in his post ‘Imperial College confirm that Karol Sikora does not work for them and does not speak on their behalf‘.
|
It seems that bits of good news don’t come singly. First honours degrees in acupuncture vanish, Now a big chain of shops selling Chinese herbs and acupuncture has gone into administration. It seems that, at last, people are getting fed up with being conned out of their hard-earned money |
 Herbmedic Barking |
A local newspaper, The North Herts Comet reported thus.
Customers of Herbmedic, which trades under the name Herbs and Acupuncture, on Queensway in Stevenage have been left counting the cost after shelling out hundreds of pounds for treatment they never received.
The company, which has practices across the country, is now in the hands of receivers, Macintyre Hudson.
Sandra Emery, of The Paddocks in Stevenage, paid £350 for 10 treatment sessions, but only received one before the practice closed.
She said: “A standard course of treatment is 10 sessions, so most customers will have bought this package.
Claudia Gois, of Walden End in Stevenage, paid £240 for 12 treatment sessions but only received four before the practice closed.
She said: “I went there on Friday and it was closed. There was no warning or anything.
“I got in touch with head office and they said it’s very unlikely I will get money back.
This report was on 1st April, The company’s web site shows no sign of any problems, In fact they are still advertising jobs. So was this an April Fool joke?
No it wasn’t. A visit to Companies House soon settled the matter. The whole company is insolvent, as of 27 March 2009..
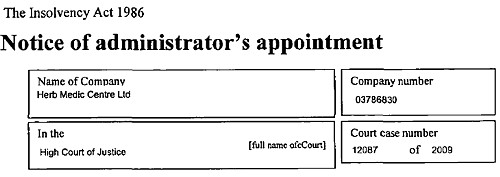
Download the whole administration notice and the company report.
Criticisms of Herbmedic
This chain of shops was investigated by the BBC’s
Inside Out programme. (September 25th 2006).
“We sent an undercover reporter to branches of the Herbmedic chain in southern England.
On each occasion, the reporter claimed to be suffering from tiredness and was prescribed herbal remedies after a consultation lasting less than five minutes.
The herbalists, who describe themselves as “doctors”, didn’t ask any questions about the patient’s medical history or take any notes.”
This is so bad that even Andrew Fowler, a past President of the Register of Chinese Herbal Medicine, described it as “malpractice”.
“Herbmedic has been investigated by the authorities in the past.
In 2002, trading standards officers prosecuted the branch in Southampton for selling herbal remedies with 26 times the permitted legal limit of lead.
And in October 2003, the Advertising Standards Authority banned Herbmedic from describing its practitioners as “doctors”.
Despite the ban, all three of the stores visited by Inside Out referred to the herbalist as the doctor.”
See also the BBC report Herbalists’ customers ‘at risk’, and a report in the Sunday Times, Herbmedic accused of high-pressure selling.
Read the Advertising Standards report. Seven different complaints against Herbmedic were upheld.
This is entirely consistent with my own experience. I went into one of their shops and asked about a cure for diabetes (hoping the be able to refer them to Trading Standards, but the young lady behind the counter had such a poor grasp of English that her reply was incomprehensible. She just kept trying to push me into having a consultation with “the doctor” who appeared to speak no English at all. I left.
The chequered history of Herbmedic
The company that his just gone into administration is Herbmedic Centre Ltd. It has been in existence for only two years. Its predecessor, known simply as Herbmedic, was dissolved on 13 March 2007, Companies House said
Company Filing History Type Date Description Order GAZ2(A) 13/03/2007 FINAL GAZETTE: DISSOLVED VIA VOLUNTARY STRIKE-OFF GAZ1(A) 28/11/2006 FIRST GAZETTE NOTICE FOR VOLUNTARY STRIKE-OFF 652a 16/10/2006 APPLICATION FOR STRIKING-OFF
Another Chinese medicine chain seems to be having a few problems too
Harmony Medical Distribution Ltd (“specialists in acupuncture and holistic medicine”) seems to be still in business(web site here), but several very similar companies have been dissolved, Harmomy Medics Ltd (dissolved 19 Sep 2006) ,, Harmony Medical Services (UK ) Ltd. (dissolved 6 May 2008) and Harmony Medical Services Ltd (dissolved 17 Oct 2008)
Given this history of companies that dissolve every couple of years and then mysteriously reincarnate with a slightly different name, one wonders if this really is the end of herbmedic, or it is just a device for shedding bad debts. Is this just another “pre-pack administration“?
Watch this space for more.
What’s the latest evidence on acupuncture anyway?
A correspondent drew my attention to the 2009 Annual Evidence Update on acupuncture complied by the NHS Complementary and Alternative Medicine Specialist Library. This includes no fewer than 56 systematic reviews and meta-analyses. Although the reviews are complied by alternative medicine sympathisers, they seem mostly to be pretty fair. Well apart form one thing.
Almost all of the reviews fail to come up with any positive evidence that acupuncture works well enough to be clinically useful. Only two come close, and they are the two singled out as “editor’s picks”. Perhaps that’s not entirely surprising given that the editor is Dr Mike Cummings.
Again and again, the results are inconclusive: #8 is pretty typical
Acupuncture for tension-type headache: a meta-analysis of randomized, controlled trials.
This meta-analysis suggests that acupuncture compared with sham for tension-type headache has limited efficacy for the reduction of headache frequency. There exists a lack of standardization of acupuncture point selection and treatment course among randomized, controlled trials. More research is needed to investigate the treatment of specific tension-type headache subtypes.
Vast effort and a lot of money is being put into trials, yet there are very few (if any) positive results. Very often there are no results at whatsoever. All we hear, again and again, is “more research is needed”.
At some point someone will have to decide it is all a charade and start to spend time and money on investigating things that are more promising.
Follow-up
A correspondent checked with Companies House to discover more about two of the directors of Herbmedic, Mr. Li Mao and Mr Xiao Xuan Chen. They have a chequered history indeed. [download the complete list]
Mr. Li Mao is, or has been, on the board of 31 different companies. Of these 6 are active, 5 are in administration, 14 were dissolved, 4 were liquidated and 2 are active with proposal to strike off. Not only is Her Medic centre Ltd in administration, but so is Dr China (UK) Ltd, and Great Chinese Herbal Medicine Ltd
With record like that, my correspondent wonders whether they should be disqualified.
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
It is almost six months now since I posted Quackery creeps into good universities too -but through Human Resources. One example given there was the University of Leicester. This is an excellent university. It does first class research and it was the alma mater of the incomparable David Attenborough who has done more than anyone to show us the true beauty and wonder of the natural world.
Nevertheless, their well-meaning occupational health department had a section about “complementary therapies” that contained a lot of statements that were demonstrably untrue. They even recommended the utterly outrageous SCENAR device. So I pointed this out to them, and I had a quick and sympathetic response from their HR director.
But three months later, nothing had changed. Every now and then, I’d send a polite reminder, but it seemed the occupational health staff were very wedded to their quackery. The last reminder went on 6th February, but this time I copied it to Leicester’s vice-chancellor. This time it worked. There is still a link to Complementary Therapies on the Wellbeing site, but if you click on it, this is what you see.
Complementary therapiesSome employees may have an interest in complementary therapies such as acupuncture, yoga, Indian head massage, Reiki, sports & remedial massage, reflexology and hypnotherapy. If you have an interest in any of these, Staff Counselling can happily provide details of practitioners in the local area. Some of these practitioners offer discounts from their normal rates for University of Leicester staff. However, the University of Leicester cannot vouch for, or recommend any of these therapies to staff as being effective. We would urge members of staff who believe that such therapies might be effective to contact their GP prior to undertaking any of them. Further, the University of Leicester shall not be liable for any damage of any kind arising out of or related to the services of any complementary therapists or treatments listed here. If you would like further information, please contact Chris Wilson at: staffcounsel&welfare@le.ac.uk or telephone 1702. |
That’s not bad. Pity it doesn’t say alternative, rather than complementary though. Euphemisms aren’t really helpful.
In fact I have a bit of a problem with “wellbeing” too. It is a harmless word that has been highjacked so that its use now makes one think of mud baths provided by expensive hotels for their rich and gullible customers.
Leicester’s HR director wrote
“Unfortunately an instruction I had given previously had not been fully complied with. I spoke to the manager of the Staff Counselling team on Friday and gave clear instructions as to the content of this site. I had been assured that the offending information had been removed, but found that it had not.
I have now checked the site for myself and can say, with confidence, that all claims for the efficacy of complimentary [sic] therapies have been removed including SCENAR.”
The similarity between quack treatments and religion is intriguing. It seems that the devotion of the occupational health people to their baloney was so great that they wouldn’t take it down even when told to do so. The more irrational the belief, the greater the fervour with which it is defended,
What’s the lesson from this minor saga? It seems that most VCs and many HR people are too sensible to believe in alternative baloney, but that they are a bit too ready to tolerate it, perhaps on grounds of political correctness. Tolerance is a virtue, but lies about health are not in the least virtuous. If you point out that people are saying things for which there isn’t the slightest evidence, they will often respond. Just be prepared to send a few reminders.
It may also be useful to point out that some of the claims made are almost certainly illegal. Even people who care little about evidence of efficacy are impressed by the idea that they might be prosecuted by Trading Standards officers.
Who needs mystical medicine when you have real wonders like these.
(Click the google video logo for a bigger version)
Or try the pitcher plant video, or the Bird of paradise, or the Bower Bird, or the giant Amazon lilies.
Follow-up
This letter appeared in the Times on Friday 30 January, 2009. It was prompted by the news from the University of Salford, but its main purpose was to try to point out to the Department of Health that you can’t hope to regulate alternative treatments in any sensible way while continuing to push under the carpet the crucial question of which ones work and which don’t.
| Sir
We would like to congratulate the vice-chancellor of the University of Salford, Professor Michael Harloe for his principled decision to drop “all the University’s programmes associated with complementary medicine within the School of Community, Health Sciences & Social Care”. This includes their “Homeopathy in Practice” degree. It is also encouraging that the University of Central Lancashire recently closed its BSc in Homeopathy to new students, and announced a review of all its activities in alternative medicine. Although universities are now taking sensible actions, government policy in the area of regulation of alternative medicine is in urgent need of revision. In May 2008 the Steering Group chaired by Professor Pittilo recommended to the Department of Health that entry into acupuncture, herbal medicine and traditional Chinese medicine should “normally be through a bachelor degree with honours”. But, in the same month, new regulations on Unfair Trading came into effect. One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. One part of government seeks to endorse unproven and disproved treatments, at the same time as another part makes them illegal. The reason for this chaotic situation is simple. The Department of Health, and the Medicines and Healthcare products Regulatory Agency (MHRA), have consistently failed to grasp the nettle of deciding which treatments work and which don’t. That is the first thing you want to know about any treatment. Vice-chancellors seem now to be asking the question, and the government should do so too. The ideal mechanism already exists. The question should be referred to the National Institute for Health and Clinical Excellence (NICE). That was recommended by a House of Lords report in 2000, and it was recommended again by the Smallwood report (commissioned by the Prince of Wales) in 2005. Now it should be done. Sir Walter Bodmer FRCPath, FRS, FMedSci, FRCP (hon) FRCS(hon) Professor David Colquhoun, FRS Dame Bridget Ogilvie , AC, DBE, FRS, FAA, Professor Dame Nancy Rothwell, FRS, FMedSci, FRCP (hon) |
(Actually, the Times removed the qualifications of the signatories, but left the titles!)
An earlier, longer, version of the letter tried to preempt the obvious criticism by including, as the second paragraph, this passage.
“It makes no sense to offer Bachelor of Science degrees in subjects that have no scientific basis. Not only is homeopathy scientifically absurd, but also the best quality clinical trials show that it is not distinguishable from placebo. From the point of view of the patient, there is nothing wrong with placebo effects. Conventional drugs benefit from them too. There is everything wrong with surrounding the placebo effect with mystical mumbo-jumbo and awarding degrees in it.”
Universities drop degree courses in alternative medicine
In the same issue, there was a related article by the Times’ education editor, Alexandra Frean: Universities drop degree courses in alternative medicine..
“Universities are increasingly turning their backs on homoeopathy and complementary medicine amid opposition from the scientific community to “pseudo-science” degrees.
The University of Salford has stopped offering undergraduate degrees in the subjects, and the University of Westminster announced yesterday that it plans to strengthen the “science base” content of its courses after an internal review which examined their scientific credibility.
Both universities are following the lead of the University of Central Lancashire, which last year stopped recruiting new students to its undergraduate degree in homoeopathic medicine.
The decisions by Salford and Westminster open a new chapter in the fierce debate about the place of awarding of Bachelor of Science degrees in subjects that are not science.”
The article ends thus.
“Other universities are more robust in their defence of their courses
Ian Appleyard, principal lecturer in acupuncture at London South Bank University, said that acupuncture should be studied for the very reason that it was not well understood from the standpoint of Western scientific medicine. Acupuncture had been used by a significant proportion of the world’s population for thousands of years.
“Recent large-scale clinical trials such Haake and meta-analysis from reputable institutions such as The Cochrane Collaboration, have shown that there is evidence to support the therapeutic benefits of acupuncture treatment for back pain and migraine,” he said.”
Uhuh, it seems that Ian Appleyard has been reading the misleading BBC report on the recent trials. In fact they show precisely the opposite of what he claims. The fact that advocates of alternative medicine can misinterpret the evidence so badly is, I guess, at the heart of the problem.
What’s happening at the University of Westminster?
Westminster has regularly been labelled as the University that has more quackery courses than any other.
It is also the only university for which we have much idea about what is taught. The university, like all others, has tried to keep secret what they teach. That itself shows that they aren’t very proud of it. But a surprising amount has leaked out from Westminster, nonetheless. The set of “vibrational medicine” slides, including “Amethysts emit high Yin energy”, have caused much hilarity. The Westminster “miasmatic” examination question gets some laughs too, after it was published in Nature. The set of homeopathic materia medica notes that have come into my possession are pretty good too (coming on line soon).
Recently it emerged that the University of Westminster had followed the example of the University of Central Lancashire (UCLAN), and set up a review of its activities in alternative medicine. But unlike UCLAN it was kept secret, and as far as one can tell, it asked for no input from critics.
Well the outcome of this review turned up in my mail recently. Click the picture to read the whole letter from the Vice-Chancellor.
There is no doubt that the outcome, so far, is rather disappointing. Here are some quotations from this letter, with my comments interleaved.
“The Audit was Chaired by Professor Alan Jago and carried out its review using a comprehensive evidence base”
Alan Jago is a pro- vice chancellor, and formerly from Westminster’s School of Architecture and the Built Environment, so no specialist knowledge there.
“The panel made a number of recommendations to me as a result of their Audit. Many of these recommendations concern the University’s processes for review and validation of courses and these will be passed to the Pro Vice Chancellor responsible for Quality to consider.”
Uhuh, sounds like box-ticking again When will universities learn that validation procedures are, on the whole, not worth the paper they are written on.
“The overarching aim of these actions then is to strengthen and make more explicit the ‘scientific’ nature of the Integrated Health undergraduate degrees.
In order to do this we will:
Strengthen learning outcomes particularly in discipline and clinical modules to reflect the science outcomes embedded in the courses.
Revise course specific regulations to explicitly identify that the core health sciences modules have to be passed to complete a degree of the BSc Scheme.
Strengthen the final year project offer to provide more scientific projects through working with Biosciences staff.
Strengthen the scientific/academic qualifications of staff through development
of existing staff and appointments where they become available.”
This seems to me to be whistling in the wind. Remember, we are talking about “bachelor of science” degrees in things like homeopathy and naturotherapy. These are things that are not science at all. In fact they are antiscience to their core.
If you were successful in raising the increasing the scientific level of the staff, many of the subjects they are meant to be teaching would vanish in a puff of smoke.
Certainly the responses of the Westminster staff to earlier enquiries (here, and here) showed little sign of scientific thinking.
And I wonder what Westminster’s admirable biomedical scientists think about taking on homeopathy students for projects?
“I am certain that this work will place Complementary therapies courses in an extremely strong position to meet the external challenges of the future.
I’m sorry to say, Professor Petts, that the scientific community is not likely to share your certainty.
Remember, Peter Fisher is on record as saying that there is not enough science in homeopathy to justifiy offering a BSc degree in it (watch the movie). He is the Queen’s Homeopathic Physician, and Clinical Director of the Royal London Homeopathic Hospital But Westminster still seems to know better.
It seems, so far, that Westminster has missed a chance to change for the better.
Follow-up
Times Higher Education published a pretty pathetic report on the Westminster audit. They did ask me for comments but then failed to publish most of them. I suppose a magazine like that is so dependent on advertising that they can’t afford to upset the authorities. Nevertheless, do they really have to be quite so bland?
I hear that the internal audit has made everyone at the University of Woominster Westminster more nervous and that staff and students have been advised not to share teaching material with people outside the university. Having seen some of them, I’m not surprised they are ashamed of them.
Acupuncture in the BMJ
A new review appeared in the BMJ today. It is by Madsen et al., from the Nordic Cochrane Centre, Copenhagen. Here are the conclusions.
- The analgesic effect of acupuncture is small and cannot be distinguished from bias resulting from incomplete blinding.
- The analgesic effect of placebo acupuncture is moderate but very variable as some large trials report substantial effects.
- The effect of acupuncture seems to be unrelated to the type of placebo acupuncture used as control.
The results confirm, yet again, that there is essentially no difference between “real” acupuncture and sham acupuncture. All that talk about meridians and Qi really is so much mumbo jumbo.
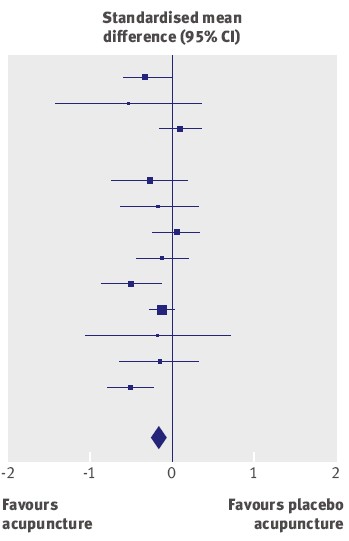
The average effect (the diamond at the bottom) is essentially zero.
It has often been supposed that acupuncture is a theatrical placebo, but because of the placebo effect it produces more pain relief than (non-blind) controls. This study confirms that there is likely to be such an effect, but it also finds that the size of the placebo effect is too small to be useful to patients. Here is the comparison between sham acupuncture and no acupuncture at all.
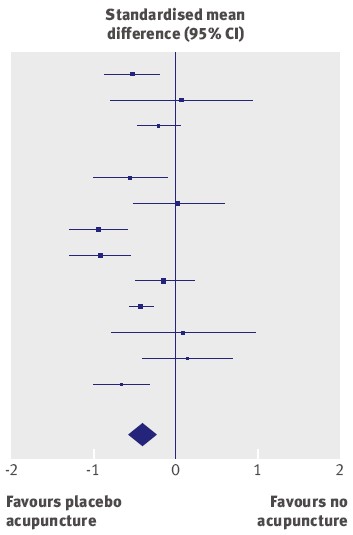
The results of different trials are very variable, but the average effect (diamond at the bottom) favours sham acupuncture over no acupuncture at all.
But how big is the effect? The numbers along the bottom of the graph are ‘standardised mean differences’. The average value of -0.42 (95% confidence limits -0.6 to -0.23) between ‘no acupuncture’ and ‘sham acupuncture’ corresponds to a difference of about 10 points on a 100 point scale. This difference is big enough to be real, in the sense that it isn’t just chance. But is it big enough to be useful to the patient? Probably not. Madsen et al conclude
“a consensus report characterised a 10mm reduction on a 100 mm visual analogue scale as representing a “minimal” change or “little change”. Thus, the apparent analgesic effect of acupuncture seems to be below a clinically relevant pain improvement.”
This makes nonsense of the Pittilo report. Notice that these results, yet again, make nonsense of the proposals in the gamma-minus Pittilo report, to pseudo-regulate acupuncture, and to have degrees in the subject.
Cochrane reviews of Acupuncture : and a bad report from BBC
Two new Cochrane reviews appeared last week, Acupuncture for tension-type headache, and Acupuncture for migraine prophylaxis.
You can’t blame subeditors for the appalling title of the BBC’s report on Acupuncture ‘works for headaches’. The content is pretty misleading too. (The link is to a version saved at 19.35 on 21 January 2009.). Furthermore, like far too many of the BBC reports, it is anonymous. One has no idea to blame This is important, if only because the BBC news site is so influential. Twelve hours after posting the misleading title has been copied all round the world.
In the Guardian, Ian Sample had a much better report, Even’fake’ acupuncture reduces the severity of headaches and migraines. Sadly the print edition had the title “Acupuncture aids migraines, researchers
find”, but that can be blamed on subeditors who have a problem with reading (in fact Sample had seen neither title).
The BBC report seemed to call for a complaint. This is what I sent.
| I wish to complain about the report on acupuncture at http://news.bbc.co.uk/1/hi/health/7838231.stm
The title itself was highly misleading “Acupuncture works for headaches” is precisely the opposite of what was shown, namely that it is no better than sham acupuncture controls. The article goes on to say
It is not said that there isn’t the slightest reason to think this is true (or even means anything) , and that the work which is being reported is strong evidence that it’s not true
That is wrong. University of Salford , for example has just closed its acupuncture course after a number of us have pointed out that it is teaching things that aren’t true
It is exactly the opposite of an endorsement. It is one more nail in the coffin of acupuncture as generally understood. This article, I contend, is partial and misleading. Unfortunately it is anonymous. |
Follow-up
Today’s BBC report on the BMJ paper is almost as partisan as the one that I just complained about. “Confusion on acupuncture benefit ” exaggerates greatly the amount of confusion. Worse still, it quotes only two well-known advocates of acupuncture, people who make their living from it. No independent scientific voice is to be heard.
One of those cited is Adrian White. He is described as “a researcher into acupuncture at the Peninsula Medical School”. There is no mention of the fact that he is also Editor in Chief of the journal Acupuncture in Medicine. The other person who is quoted is Mike O’Farrell, the chief executive of the British Acupuncture Council. What do you expect him to say?
I’ve just sent another complaint, about today’s BBC report. The more the merrier.
The BMJ itself published an editorial on the Madsen paper. It seems very odd that they should have chosen the editors of the BMJ-group journal, Acupuncture in Medicine, to comment on a paper that sounds the death knell for the subject from which they make their living. Needless to say, the editorial attempted to wriggle out of the obvious conclusions. Worse still, the Health editor of the BBC web site referred to the editorial in his defence, in response to my complaint.
Channel 4 News does a lot better than the BBC, or the BMJ editorial, with its report Acupuncture ‘fails to relieve pain’
“Claims that acupuncture can relieve pain have been undermined by the results of a new study.”
“senior researcher Asbjorn Hrobjartsson said: “Our findings question both the traditional foundation of acupuncture…and the prevailing theory that acupuncture has an important effect on pain in general”. “
The Daily Telegraph also, like almost everyone else, did better than the BBC, with “Acupuncture ‘has almost no effect in relieving pain’”
“The pain relieving effects of acupuncture are so small that they may be clinically irrelevant, according to a review of research into the treatment.”
Even Metro, the free London Newspaper, is more accurate then the BBC. They carry a short report “Acupuncture ‘has no medical point’.”
“The pain-relieving effects of acupuncture compared with a placebo are so small they may be clinically irrelevant.”
New review puts in doubt traditional foundation of acupuncture. Believe it or not, that is the title of the report on Madsen et al from the Prince’s Foundation for Integretad Health! Don’t get too excited though. They haven’t even bothered to look at the original paper, but merely cite the dreadful BBC report. Much prominence is given to the acupuncturists, White and O’Farrell, and the important finding isn’t mentioned at all. Another gamma minus.
Congratulations to the vice-chancellor of the University of Salford, Michael Harloe.
Times Higher Education announced on 15th January 2009 Salford to shut complementary medicine BSc.
“The University of Salford is to stop offering undergraduate degrees in acupuncture and complementary medicine because they are no longer considered “a sound academic fit”.”
This is the first time that a University has decided to stop teaching quackery altogether. The university’s press officer told me (22 January 2009)
| “all the University’s programmes associated with complementary medicine within the School of Community, Health Sciences & Social Care will be run out. This includes the Homeopathy in Practice programme. “ |
| Salford, before it became a university, was home to the great L.S. Lowry |

Salford’s Peel building, where L.S.Lowry worked |
“Managers concluded last year that the BSc traditional Chinese medicine and other degrees with a complementary medicine element “cannot really be held to be a good fit with the strategic direction of the school, and resource and energy would be better directed elsewhere”.
There are more than 70 students registered on the Chinese medicine degree course.
The university will continue to offer these subjects at postgraduate level, as short courses and as part of continuing professional development programmes. Traditional Chinese medicine work will also be linked to the university’s allied
health professions courses.”
Another report appeared in the Manchester Evening News: “Needle over acupuncture course”. “A UNIVERSITY has scrapped a course in acupuncture and aromatherapy branded `anti-science’ by critics.
Salford University said the three-year degree in traditional Chinese medicine didn’t fit with the `strategic direction’ bosses want to adopt.
The move is part of wider cuts which will see 150 teaching and support staff jobs axed.”
One of their students raised the question that the university must dread.
“First-year student Gary Leese, who is organising a petition, said: “Why did the university launch the course if they didn’t think it was good enough?”
The comments left by the readers of the Manchester Evening News were mostly very sensible. The first to come in, from someone with the beautifully Lancastrian name, Gladys Rowbotham, said “Some common sense at last!”.
A brief report appeared also in the Manchester Confidential
Why now?
This is rather an interesting development. On 19th April 2007, I sent a Freedom of Information request to Salford to ask for course validation documents for their courses in Homeopathy and in Traditional Chinese Medicine. I also asked for course materials for specified courses. This request was even less successful than usual. Not only were the course materials refused (as they always are), but, unusually, the validation documents were refused too. The excuse for this was more pathetic than usual too. They claimed it would cost more than £450 to email a few documents and powerpoints, and claimed exemption under Section 21 of the Freedom of Information Act, “Information Reasonably Accessible to the Applicant by Other Means”, rather than the more usual excuse (Section 43, “Commercial interests”).
It was never explained what “other means” were meant to be available. Perhaps they thought I should pay £3000 in fees and enrol for the course?
On 6th April 2007, Times Higher Education (THE) ran an opinion piece “Credible endeavour or pseudoscience?“. In this, I wrote, as follows.
“Clearly the buck stops with university vice-chancellors who award the degrees. Two weeks ago, after the publication of my opinion article and a special report on university homoeopathy courses in the journal Nature , the BBC tried to get one of the vice-chancellors to defend themselves. They did not succeed. Letters to vice-chancellors on this go unanswered. Requests to see course materials have repeatedly been refused. The QAA is exempt from the Freedom of Information Act. Teaching materials and the names of examiners are kept secret. This I find incomprehensible and indefensible.”
After this appeared, I was sent by the University of Salford a copy of Michael Harloe’s defence of their position at that time, as sent to THE. It relied heavily on validation by the Quality Assurance Agency. But the QAA is merely a box-ticking organisation that would give top marks to a course in astrology, given a sufficient mound of paperwork, as I pointed out in Nature, “Their own rules prevent them from doing anything useful”.
The statement also said that the courses teach critical thinking about alternative medicine. But it has been pointed out over and over again that what alternative medicine advocates lack, above anything else, is any faculty of critical self-appraisal.
One has to have some sympathy with a vice chancellor who is put on the spot and forced to defend courses in which he probably does not really believe himself. Perhaps it is not surprising that letters so often go unanswered. What can they say? There really is no answer that doesn’t leave the hapless VC with egg on his face.
If there is one lesson from this, it is not to be discouraged if you get no answer from a vice-chancellor. It has probably been read and may well get acted on eventually. Shutting down a course is no easy matter. It takes time.
I said the buck stops with the vice chancellor. Professor Harloe has grasped the nettle and done the right thing. Let’s hope a few more now follow his excellent lead..
What does this mean for the Pittilo report?
The gamma-minus Pittilo report (see also. The Times) recommended more degrees in alternative medicine, but there seems to be something of a trend developing in exactly the opposite direction.
The University of Central Lancashire has closed the first year entry to its “BSc” in Homeopathy, and announced a review of all its activities in the area of alternative medicine. Now we have Salford. There are stirrings among the good scientists even at the University of Westminster which has a new Dean and VC.
This rather absurd situation has arisen because of the adamant refusal of the government, and of a dozen or more quangos, to grasp the nettle of whether or not the alternative treatments work. Time and time again, the one important question that you want to know about any sort of treatment, namely, is it effective, has been pushed under the carpet.
The sort of absurd political correctness that leads to the fraudulent conjurers known as ‘psychic surgeons’ being referred to as a “profession” by the Department of Health has obscured reality. Even the MHRA was persuaded to allow misleading labelling of homeopathic and herbal “remedies”. thus betraying its job. In its own words “The MHRA is the government agency that is responsible for ensuring that medicines and medical devices work, . . .”.
There is a lesson here. You can’t go on avoiding reality for ever. One consolation is that, in the end, it is the universities who are leading the way, albeit slowly.
All we need now is for the Department of Health, the MHRA and the endless box-ticking quangos to wake up too.
I’m perfectly happy to think of alternative medicine as being a voluntary, self-imposed tax on the gullible (to paraphrase Goldacre again). But only as long as its practitioners do no harm and only as long as they obey the law of the land. Only too often, though, they do neither.
When I talk about law, I don’t mean lawsuits for defamation. Defamation suits are what homeopaths and chiropractors like to use to silence critics. heaven knows, I’ve becomes accustomed to being defamed by people who are, in my view. fraudsters, but lawsuits are not the way to deal with it.
I’m talking about the Trading Standards laws Everyone has to obey them, and in May 2008 the law changed in a way that puts the whole health fraud industry in jeopardy.
The gist of the matter is that it is now illegal to claim that a product will benefit your health if you can’t produce evidence to justify the claim.
I’m not a lawyer, but with the help of two lawyers and a trading standards officer I’ve attempted a summary. The machinery for enforcing the law does not yet work well, but when it does, there should be some very interesting cases.
The obvious targets are homeopaths who claim to cure malaria and AIDS, and traditional Chinese Medicine people who claim to cure cancer.
But there are some less obvious targets for prosecution too. Here is a selection of possibilities to savour..
- Universities such as Westminster, Central Lancashire and the rest, which promote the spreading of false health claims
- Hospitals, like the Royal London Homeopathic Hospital, that treat patients with mistletoe and marigold paste. Can they produce any real evidence that they work?
- Edexcel, which sets examinations in alternative medicine (and charges for them)
- Ofsted and the QCA which validate these exams
- Skills for Health and a whole maze of other unelected and unaccountable quangos which offer “national occupational standards” in everything from distant healing to hot stone therapy, thereby giving official sanction to all manner of treatments for which no plausible evidence can be offered.
- The Prince of Wales Foundation for Integrated Health, which notoriously offers health advice for which it cannot produce good evidence
- Perhaps even the Department of Health itself, which notoriously referred to “psychic surgery” as a profession, and which has consistently refused to refer dubious therapies to NICE for assessment.
The law, insofar as I’ve understood it, is probably such that only the first three or four of these have sufficient commercial elements for there to be any chance of a successful prosecution. That is something that will eventually have to be argued in court.
But lecanardnoir points out in his comment below that The Prince of Wales is intending to sell herbal concoctions, so perhaps he could end up in court too.
The laws
We are talking about The Consumer Protection from Unfair Trading Regulations 2008. The regulations came into force on 26 May 2008. The full regulations can be seen here, or download pdf file. They can be seen also on the UK Statute Law Database.
The Office of Fair Trading, and Department for Business, Enterprise & Regulatory Reform (BERR) published Guidance on the Consumer Protection from Unfair Trading Regulations 2008 (pdf file),
Statement of consumer protection enforcement principles (pdf file), and
The Consumer Protection from Unfair Trading Regulations: a basic guide for business (pdf file).
Has The UK Quietly Outlawed “Alternative” Medicine?
On 26 September 2008, Mondaq Business Briefing published this article by a Glasgow lawyer, Douglas McLachlan. (Oddly enough, this article was reproduced on the National Center for Homeopathy web site.)
“Proponents of the myriad of forms of alternative medicine argue that it is in some way “outside science” or that “science doesn’t understand why it works”. Critical thinking scientists disagree. The best available scientific data shows that alternative medicine simply doesn’t work, they say: studies repeatedly show that the effect of some of these alternative medical therapies is indistinguishable from the well documented, but very strange “placebo effect” ”
“Enter The Consumer Protection from Unfair Trading Regulations 2008(the “Regulations”). The Regulations came into force on 26 May 2008 to surprisingly little fanfare, despite the fact they represent the most extensive modernisation and simplification of the consumer protection framework for 20 years.”
The Regulations prohibit unfair commercial practices between traders and consumers through five prohibitions:-
- General Prohibition on Unfair Commercial
Practices (Regulation 3)- Prohibition on Misleading Actions (Regulations 5)
- Prohibition on Misleading Omissions (Regulation 6)
- Prohibition on Aggressive Commercial Practices (Regulation 7)
- Prohibition on 31 Specific Commercial Practices that are in all Circumstances Unfair (Schedule 1). One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. The definition of “product” in the Regulations includes services, so it does appear that all forms medical products and treatments will be covered.
Just look at that!
| One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations” |
Section 5 is equally powerful, and also does not contain the contentious word “cure” (see note below)
Misleading actions
5.—(1) A commercial practice is a misleading action if it satisfies the conditions in either paragraph (2) or paragraph (3).
(2) A commercial practice satisfies the conditions of this paragraph—
(a) if it contains false information and is therefore untruthful in relation to any of the matters in paragraph (4) or if it or its overall presentation in any way deceives or is likely to deceive the average consumer in relation to any of the matters in that paragraph, even if the information is factually correct; and
(b) it causes or is likely to cause the average consumer to take a transactional decision he would not have taken otherwise.
These laws are very powerful in principle, But there are two complications in practice.
One complication concerns the extent to which the onus has been moved on to the seller to prove the claims are true, rather than the accuser having to prove they are false. That is a lot more favourable to the accuser than before, but it’s complicated.
The other complication concerns enforcement of the new laws, and at the moment that is bad.
Who has to prove what?
That is still not entirely clear. McLachlan says
“If we accept that mainstream evidence based medicine is in some way accepted by mainstream science, and alternative medicine bears the “alternative” qualifier simply because it is not supported by mainstream science, then where does that leave a trader who seeks to refute any allegation that his claim is false?
Of course it is always open to the trader to show that his the alternative therapy actually works, but the weight of scientific evidence is likely to be against him.”
On the other hand, I’m advised by a Trading Standards Officer that “He doesn’t have to refute anything! The prosecution have to prove the claims are false”. This has been confirmed by another Trading Standards Officer who said
“It is not clear (though it seems to be) what difference is implied between “cure” and “treat”, or what evidence is required to demonstrate that such a cure is false “beyond reasonable doubt” in court. The regulations do not provide that the maker of claims must show that the claims are true, or set a standard indicating how such a proof may be shown.”
The main defence against prosecution seems to be the “Due diligence defence”, in paragraph 17.
Due diligence defence
17. —(1) In any proceedings against a person for an offence under regulation 9, 10, 11 or 12 it is a defence for that person to prove—
(a) that the commission of the offence was due to—
(i) a mistake;
(ii) reliance on information supplied to him by another person;
(iii) the act or default of another person;
(iv) an accident; or
(v) another cause beyond his control; and
(b) that he took all reasonable precautions and exercised all due diligence to avoid the commission of such an offence by himself or any person under his control.
If “taking all reasonable precautions” includes being aware of the lack of any good evidence that what you are selling is effective, then this defence should not be much use for most quacks.
Douglas McLachlan has clarified, below, this difficult question
False claims for health benefits of foods
A separate bit of legislation, European regulation on nutrition and health claims made on food, ref 1924/2006, in Article 6, seems clearer in specifying that the seller has to prove any claims they make.
Article 6
Scientific substantiation for claims
1. Nutrition and health claims shall be based on and substantiated by generally accepted scientific evidence.
2. A food business operator making a nutrition or health claim shall justify the use of the claim.
3. The competent authorities of the Member States may request a food business operator or a person placing a product on the market to produce all relevant elements and data establishing compliance with this Regulation.
That clearly places the onus on the seller to provide evidence for claims that are made, rather than the complainant having to ‘prove’ that the claims are false.
On the problem of “health foods” the two bits of legislation seem to overlap. Both have been discussed in “Trading regulations and health foods“, an editorial in the BMJ by M. E. J. Lean (Professor of Human Nutrition in Glasgow).
“It is already illegal under food labelling regulations (1996) to claim that food products can treat or prevent disease. However, huge numbers of such claims are still made, particularly for obesity ”
“The new regulations provide good legislation to protect vulnerable consumers from misleading “health food” claims. They now need to be enforced proactively to help direct doctors and consumers towards safe, cost effective, and evidence based management of diseases.”
In fact the European Food Standards Agency (EFSA) seems to be doing a rather good job at imposing the rules. This, predictably, provoked howls of anguish from the food industry There is a synopsis here.
“Of eight assessed claims, EFSA’s Panel on Dietetic Products, Nutrition and Allergies (NDA) rejected seven for failing to demonstrate causality between consumption of specific nutrients or foods and intended health benefits. EFSA has subsequently issued opinions on about 30 claims with seven drawing positive opinions.”
“. . . EFSA in disgust threw out 120 dossiers supposedly in support of nutrients seeking addition to the FSD’s positive list.
If EFSA was bewildered by the lack of data in the dossiers, it needn’t hav been as industry freely admitted it had in many cases submitted such hollow documents to temporarily keep nutrients on-market.”
Or, on another industry site, “EFSA’s harsh health claim regime”
“By setting an unworkably high standard for claims substantiation, EFSA is threatening R&D not to mention health claims that have long been officially approved in many jurisdictions.”
Here, of course,”unworkably high standard” just means real genuine evidence. How dare they ask for that!
Enforcement of the law
Article 19 of the Unfair Trading regulations says
19. —(1) It shall be the duty of every enforcement authority to enforce these Regulations.
(2) Where the enforcement authority is a local weights and measures authority the duty referred to in paragraph (1) shall apply to the enforcement of these Regulations within the authority’s area.
Nevertheless, enforcement is undoubtedly a weak point at the moment. The UK is obliged to enforce these laws, but at the moment it is not doing so effectively.
A letter in the BMJ from Rose & Garrow describes two complaints under the legislation in which it appears that a Trading Standards office failed to enforce the law. They comment
” . . . member states are obliged not only to enact it as national legislation but to enforce it. The evidence that the government has provided adequate resources for enforcement, in the form of staff and their proper training, is not convincing. The media, and especially the internet, are replete with false claims about health care, and sick people need protection. All EU citizens have the right to complain to the EU Commission if their government fails to provide that protection.”
This is not a good start. A lawyer has pointed out to me
“that it can sometimes be very difficult to get Trading Standards or the OFT to take an interest in something that they don’t fully understand. I think that if it doesn’t immediately leap out at them as being false (e.g “these pills cure all forms of cancer”) then it’s going to be extremely difficult. To be fair, neither Trading Standards nor the OFT were ever intended to be medical regulators and they have limited resources available to them. The new Regulations are a useful new weapon in the fight against quackery, but they are no substitute for proper regulation.”
Trading Standards originated in Weights and Measures. It was their job to check that your pint of beer was really a pint. Now they are being expected to judge medical controversies. Either they will need more people and more training, or responsibility for enforcement of the law should be transferred to some more appropriate agency (though one hesitates to suggest the MHRA after their recent pathetic performance in this area).
Who can be prosecuted?
Any “trader”, a person or a company. There is no need to have actually bought anything, and no need to have suffered actual harm. In fact there is no need for there to be a complainant at all. Trading standards officers can act on their own. But there must be a commercial element. It’s unlikely that simply preaching nonsense would be sufficient to get you prosecuted, so the Prince of Wales is, sadly, probably safe.
Universities who teach that “Amethysts emit high Yin energy” make an interesting case. They charge fees and in return they are “falsely claiming that a product is able to cure illnesses”.
In my view they are behaving illegally, but we shan’t know until a university is taken to court. Watch this space.
The fact remains that the UK is obliged to enforce the law and presumably it will do so eventually. When it does, alternative medicine will have to change very radically. If it were prevented from making false claims, there would be very little of it left apart from tea and sympathy
Follow-up
New Zealand must have similar laws.
Just as I was about to post this I found that in New Zealand a
“couple who sold homeopathic remedies claiming to cure bird flu, herpes and Sars (severe acute respiratory syndrome) have been convicted of breaching the Fair Trading Act.”
They were ordered to pay fines and court costs totalling $23,400.
A clarification form Douglas McLachlan
On the difficult question of who must prove what, Douglas McLachlan, who wrote Has The UK Quietly Outlawed “Alternative” Medicine?, has kindly sent the following clarification.
“I would agree that it is still for the prosecution to prove that the trader committed the offence beyond a reasonable doubt, and that burden of proof is always on the prosecution at the outset, but I think if a trader makes a claim regarding his product and best scientific evidence available indicates that that claim is false, then it will be on the trader to substantiate the claim in order to defend himself. How will the trader do so? Perhaps the trader might call witness after witness in court to provide anecdotal evidence of their experiences, or “experts” that support their claim – in which case it will be for the prosecution to explain the scientific method to the Judge and to convince the Judge that its Study evidence is to be preferred.
Unfortunately, once human personalities get involved things could get clouded – I could imagine a small time seller of snake oil having serious difficulty, but a well funded homeopathy company engaging smart lawyers to quote flawed studies and lead anecdotal evidence to muddy the waters just enough for a Judge to give the trader the benefit of the doubt. That seems to be what happens in the wider public debate, so it’s easy to envisage it happening a courtroom.”
The “average consumer”.
(3) A commercial practice is unfair if—
(a) it contravenes the requirements of professional diligence; and
(b) it materially distorts or is likely to materially distort the economic behaviour of the average consumer with regard to the product.
It seems,therefore, that what matters is whether the “average consumer” would infer from what is said that a claim was being made to cure a disease. The legal view cited by Mojo (comment #2, below) is that expressions such as “can be used to treat” or “can help with” would be considered by the average consumer as implying successful treatment or cure.
The drugstore detox delusion. A nice analysis “detox” at .Science-based Pharmacy
The National Health Executive (“the Independent Journal for Senior Health Service Managers) asked for an article about quackery. This is a version of that article with live links.
Download the pdf version.
There is a Russian translation here (obviously I can’t vouch for its accuracy).
On May 23 th 2006 a letter was sent to the chief executives of 467 NHS Trusts. It was reported as a front page story in the Times, and it was the lead item on the Today programme. The letter urged the government not to spend NHS funds on “unproven and disproved treatments”. Who can imagine anything more simple and self-evident than that? But in politics nothing is simple.
It turns out that quite a lot of patients are deeply attached to unproven and disproved treatments. They clamour for them and, since “patient choice” is high on the agenda at the moment, they quite often get them. Unproven and disproved treatments cost quite a lot of money that the NHS should be spending on things that work.
In January 2007, the Association of Directors of Public Health issued its own list of unproven and disproved treatments. It included, among others, tonsillectomy and adenoidectomy, carpal tunnel surgery and homeopathy. They all matter, but here I’ll concentrate on alternative treatments, of which homeopathy is one of the most widespread.
It should be simple. We have a good mechanism for deciding which treatments are cost-effective, in the form of the National Institute for Clinical Excellence (NICE). If homeopathy and herbalism are not good ways to spend NHS money, why has NICE not said so? The answer to that is simple. NICE has not been asked. It can consider only those questions that are referred to it by the Department of Health (DoH).
The government often says that it takes the best scientific advice, but the DoH seems to have something of a blank spot when it comes to alternative medicine. Nobody knows why. Perhaps it is the dire lack of anyone with a scientific education in government. Or could there be something in the rumour that the DoH lives in terror of being at the receiving end of a rant from the general direction of Clarence House if it doesn’t behave? Whatever the reason, the matter has still not been referred to NICE, despite many requests to do so.
A judgement from NICE would be useful, but it is hardly essential. It isn’t hard to understand. At its simplest the whole problem can be summed up very briefly.
- Homeopathy: giving patients medicines that contain no medicine whatsoever.
- Herbal medicine: giving patients an unknown dose of a medicine, of unknown effectiveness and unknown safety.
- Acupuncture: a rather theatrical placebo, with no real therapeutic benefit in most if not all cases.
- Chiropractic: an invention of a 19 th century salesmen, based on nonsensical principles, and shown to be no more effective than other manipulative therapies, but less safe.
- Reflexology: plain old foot massage, overlaid with utter nonsense about non-existent connections between your feet and your thyroid gland.
- Nutritional therapy: self-styled ‘nutritionists’ making unjustified claims about diet to sell unnecessary supplements.
Of these, ‘nutritional therapy’, or ‘nutritional medicine’, is a relative newcomer. At their worst, they claim that Vitamin C can cure AIDS, and have been responsible for many deaths in Africa. There isn’t the slightest need for them since the nutrition area is already covered by registered dietitians who have far better training.
There have been several good honest summaries of the evidence that underlies these interpretations, written in a style quite understandable by humanities graduates. Try, for example, Trick or Treatment (Singh & Ernst, Bantam Press 2008): a copy should be presented to every person in the DoH and every NHS manager. In some areas the evidence is now quite good. Homeopathy, when tested properly, comes out no different from placebo. That is hardly surprising because the ‘treatment’ pill contains no medicine so it is the same as the placebo pill.
Acupuncture has also been tested well in the last 10 years. A lot of ingenuity has been put into designing sham acupuncture to use as a control. There is still a bit of doubt in a few areas, but overwhelmingly the results show that real acupuncture is not distinguishable from sham. Acupuncture, it seems, is nothing more than a particularly theatrical placebo. All the stuff about meridians and “Qi” is so much mumbo-jumbo. In contrast, herbal medicines have hardly been tested at all.
It is quite easy to get an impression that some of these fringe forms of medicine work better than they do. They form efficient lobby groups and they have friends in high places. They long for respectability and they’ve had a surprising amount of success in getting recognised by the NHS. Some (like chiropractic) have even got official government recognition.
One can argue about whether it was money well-spent, but in the USA almost a billion dollars has been spent on research on alternative medicine by their National Center for Complementary and Alternative Medicine (NCCAM), which was set up as a result of political pressure from the (huge) alternative medicine industry. That has produced not a single effective alternative treatment, but at least it has shown clearly that most don’t work.
The letter of 23 May 2006 proved to be remarkably effective. Tunbridge Wells Homeopathic Hospital has closed and commissioning of homeopathic services has fallen drastically. That has released money for treatments that work, and providing treatments that work is the job of the NHS.
It is sometimes asked, what is wrong with placebo effects as long as the patient feels better? First it must be said that much of the apparent benefit of placebos like homeopathy isn’t a placebo effect, but merely spontaneous recovery. Echinacea cures your cold in only seven days when otherwise it would have taken a week. But when there is a genuine psychosomatic placebo effect, it can be a real benefit. As always, though, one must consider the cost as well as the benefit.
And there are a lot of hidden costs in this approach. One cost is the need to lie to patients to achieve a good placebo effect. That contradicts the trend towards more openness in medicine. And there is a major cost to the taxpayer in the training of people. If the NHS employs homeopaths or spiritual healers because they are nice people who can elicit a good placebo effect, the Human Resources department will insist that they are fully-qualified in myths. ““Full National Federation of Spiritual Healer certificate. or a full Reiki Master qualification, and two years post certificate experience” (I quote). That is one reason why you can find in UK universities, undergraduates being taught at taxpayers’ expense, that “amethysts emit high Yin energy”.
There is a solution to all of this. There is room in the NHS for nice, caring people, to hold the hands of sick patients. They might be called ‘healthcare workers in supportive and palliative care’. They could do a good job, without any of the nonsense of homeopathy or spiritualism. Likewise, manipulative therapists could get together to dispense with the nonsense elements in chiropractic, and to make a real attempt to find out what works best.
All that stands in the way of this common sense approach is the rigidity of Human Resources departments which demand formal qualifications in black magic before you can cheer up sick patients. The over-formalisation of nonsense has done great harm. You have only to note that Skills for Health has listed ‘competences’ in Distant Healing (in the presence of the client or in the absence of the client).
When I asked Skills for Health if they would be defining a ‘competence’ in talking to trees, I was told, in all seriousness, ““You’d have to talk to LANTRA, the land-based organisation for that”.
I’m not joking. I wish I were.
Follow-up
Herbal medicine is, unlike homeopathy, not ridiculous, It is merely Pharmacology, as practised up to circa 1900. Whereas good trials have now shown acupuncture to be sham and homeopathy to be a placebo, there has been very little good research on herbs.
Most herbalism could fairly be described giving to sick patients an unknown dose of a substance with unknown efficacy and unknown safety.
How odd, then, to visit the Royal Society of Medicine to be greeted thus.
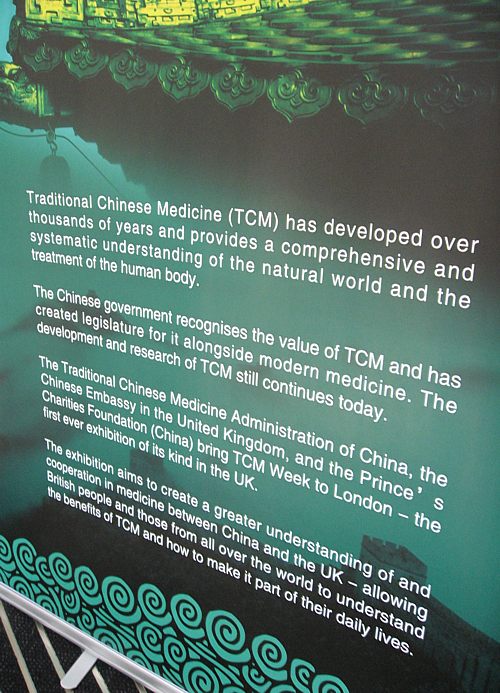
Just look at the words!
“Traditional Chinese Medicine (TCM) has developed over thousands of years”
That’s partly true
“and provides a comprehensive and systematic understanding of the natural world and the treatment of the human body.”
and that is total nonsense. TCM provides no understanding and virtually none of it is known to be useful for treating anything.
| Another poster at the RSM exhibition provides some of the explanation. What on earth, one wonders, do they mean by “making efforts to modernise TCM “? So far, the idea of modernising TCM doesn’t seem to include any great effort to find out if it works. Much of the promotion of TCM seems to be not so much ‘ancient wisdom’, but modern nationalist propaganda by the Chinese government. |
 |
The history is fascinating, but you won’t learn it from the posters on display at the exhibition.
“The Daoguang emperor though it [acupuncture] was a barrier to medical progress and removed it from the curriculum of the Imperial Medical Institute,”
“By the start of the twentieth century, acupuncture was extinct in the West and dormant in the East. It might have fallen out of favour permanently, but it suddenly experienced a revival in 1949 as a direct result of the communist revolution and the establishment of the People’s Republic of China. Chairman Mao Tse-tung engineered a resurgence in traditional Chinese medicine, which included not just acupuncture but also Chinese herbal medicine and other therapies ”
“His motivation was partly ideological, inasmuch as he wanted to reinforce a sense of national pride in Chinese medicine. However he was also driven by necessity. He had promised to deliver affordable healthcare .. . . ”
“Mao did not care whether traditional Chinese medicine worked, as long as he could keep the masses contented. In fact, his personal physician, Zhisui Li, wrote a memoir entitled ‘The Private Life of Chairman Mao’, in which he quoted Mao as saying”
“Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine.” “
Singh & Ernst Trick or Treatmant, page 46.
Or, as put more succinctly by Shapiro
“You would never know that TCM was fashioned in the twentieth century, as we shall see, from a ragbag of therapies in post-revolutionary China.”
Rose Shapiro, Suckers, how alternative medicine makes fools of us all.
Why is the Royal Society of Medicine allowing such mendacious posters? As it happens, I and a friend were visiting the RSM to see their Academic Dean, with a view to finding out why the RSM had failed to take any public position on alternative medicine. The answer appeared to be money, and that was the answer to why the TCM exhibition was being held on their premises too. The Dean no more believed in TCM than we did, but, well, they need the income. He pointed out (looking suitably sheepish) that the address given for the exhibition was not the RSM, but Number 1 Wimpole Street (that, of course, is also the address of the RSM).
Ah, so that’s OK then.
It has to be said that the RSM isn’t alone in its spineless attitude. Both the British Medical Association (BMA) and the Royal College of General Practitioners (RCGP) have failed to make any clear condemnation of mystical medicine. This is in stark contrast to just about every relevant scientific society (here is a summary).
It is a mystery to me why much of medicine should still be dominated by a mindset that seems to have lagged 200 years behind every other science. Perhaps medicine is just too complicated.
UCL Hospitals’ skeleton in the cupboard
Make no mistake, University College London Hospital is top class. The UCLH Trust. runs seven hospitals All but one of them are excellent. But in 2002 the Royal London Homeopathic Hospital was acquired as part of the UCLH group, to the intense embarrassment of UCL scientists.
Let’s start with the good bit. Usually I don’t like anecdotes, so just think of this as a vote of thanks, not evidence.
A personal history of UCH
I owe UCLH a lot personally. On December 13th 1984, my wife had
a subarachnoid haemorrhage when she was seven months pregnant. After misdiagnosis at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millilmetre from the pituitary on the other. It was a bit tricky but I think we got it”.
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds).. Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. | 
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album.. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. Heaven knows what it would have cost in the USA.
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew playing cricket in Bangladesh, Feb 2005. |
But now the the less desirable side of UCLH
Herbs and homeopaths at UCLH
| Recently I was sent the UCLH Annual Review 2007 – 2008. There was a lot of good stuff in it and worth a read despite there being too much hyperbole and too many pictures of men in dark suits. But buried among all the high tech stuff, what do we find but an advertisement for 1900-style pharmacology in the form of the herbal clinic at the Royal London Homeopathic Hospital, accompanied by a load of utterly inaccurate information from the TV botanist, David Bellamy. Take, for example, the claim about Devil’s Claw for osteoarthritis. Even alternative medicine advocates said “The authors concluded that there are insufficient high-quality trials to determine the safety and efficacy of Devil’s Claw (Harpagophytum procumbens) in the treatment of osteoarthritis, and that definitive trials are needed.”
Reading between the lines, I’d guess that the opening of this clinic has a subtext. It is well known that funding for homeopathy has dried up (partly as a result of our letter to NHS Trusts that appeared in the There have been problems before with the herbal activities at the RLHH before (see Conflicts of Interest at the Homeopathic Hospital). It appeared that the Khans, who run the Marigold homeopathic podiatry clinic (no, seriously, it is real) were largely prescribing a herbal product that was made by their own company. without even the hospital trust, never mind the patients, being made aware of it. In normal medicine this would be regarded as a rather serious offence, but as far as I know, nothing was ever done about it. |
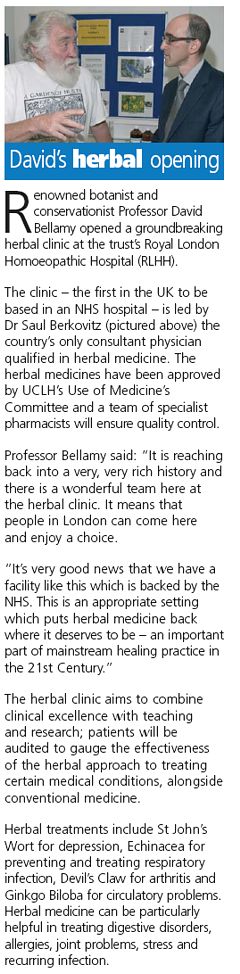 |
The ethics of alternative medicine are truly one of life’s great mysteries.
Reading further in the annual review, we come to the page about the RLHH. The homeopathy side must really have run down because it seems to have diversified into selling cosmetics and groceries. That sounds like desperation.

Good heavens, they sell “chemical-free sun cream”. One wonders what it can be made of, if not chemicals. This is the language of low-grade advertising agencies, not what one expects from an NHS hospital trust.
But next to this there is a much more interesting item. Just look at the last sentence.
I wonder if this could possibly have anything to do with the fact that Michael Baum and I visited the Trust headquarters in August 2006 to propose that the RLHH might be turned into a centre of supportive and palliative care? It would be nice to think so. But it seems they haven’t gone nearly far enough yet. If all they do is replace the waning homeopathy We know they are under pressure from their royal patrons, but that, in a constitutional monarchy, is simply not acceptable. |
 |
Michael Baum is a cancer surgeon who has taken a particular interest in palliative and supportive care. He is someone whose views should be taken seriously. He is also the author of the magnificent “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong” Here is a quotation from that letter. The UCLH Trust should bear it in mind.
| The power of my authority comes with a knowledge built on 40 years of study and 25 years of active involvement in cancer research. I’m sensitive to the danger of abusing this power and, as a last resort, I know that the General Medical Council (GMC) is watching over my shoulder to ensure I respect a code of conduct with a duty of care that respects patients’ dignity and privacy and reminds me that my personal beliefs should not prejudice my advice. Your power and authority rest on an accident of birth. Furthermore, your public utterances are worthy of four pages, whereas, if lucky, I might warrant one. I don’t begrudge you that authority and we probably share many opinions about art and architecture, but I do beg you to exercise your power with extreme caution when advising patients with life threatening diseases to embrace unproven therapies. There is no equivalent of the GMC for the monarchy, so it is left either to sensational journalism or, more rarely, to the quiet voice of loyal subjects such as myself to warn you that you may have overstepped the mark. It is in the nature of your world to be surrounded by sycophants (including members of the medical establishment hungry for their mention in the Queen’s birthday honours list) who constantly reinforce what they assume are your prejudices. Sir, they patronise you! Allow me this chastisement. |
Follow-up
The photo album chronicling the birth of my son, is really just for family and friends, but at least one blog picked up on the wider significance.

It may be only post-1992 universities that run degrees in nonsense, but you can find plenty even in the highest places. Like St Bartholomew’s (founded in 1123). That well known source of misleading medical advice, The Prince’s Foundation for Integrated Health (FiH), published last March, “Teaching integrated health at Barts and the London“. This consists of an interview with two members of staff from what is now known as the Barts and The London School of Medicine and Dentistry (SMD)..
| Dr Mark Carroll BSc (Hons), PhD, FHEA is Associate Dean (Education Quality) in the Centre for Medical Education (SMD), specialising in all aspects of quality assurance in the SMD |  |
| Prof Chris Fowler BSc MA MS FRCP FRCS(Urol) FEBU is Dean of Education |  |
They say they are dubious about alternative medicine, but rather keen on integrated medicine. Seems odd, since the latter is really just a euphemism for the former.
After seeing the FiH posting, I wrote to Carroll and Fowler to get more information.
From Carroll 20 March
We are at an early stage in the planning process for the “Integrated Health & Wellbeing” strand in our new MBBS curriculum. I can send you our ideas (attached). Much will depend on whether we can make a new appointment of someone who can lead on the planning
From Fowler 25 March 2008
Our discussions with the PFIH [Prince’s Foundation for Integrated Health] have only progressed to the stage of indicating an indicative curriculum for integrated health. We don’t have the sort of detail that you are asking for at present. We are hoping that they will work with us to get someone to champion the development.
. . .
Your views would be welcome
So I sent them some views on 26 March (read them here). I also said “I find it quite astonishing that a respectable medical school should feel it appropriate to have parts of its curriculum in the hands of the Prince of Wales.”. It seems, though, that only one sort of view was wanted. On 27 March. Fowler wrote
“I find your insinuation unnecessary and insulting. We have been working on a serious response to the GMC’s requirement that we teach medical students about the range of options available to patients. It is fatuous to suggest that the Prince of Wales is personally involved in any practical sense. The Prince’s Foundation for Integrated Health is an important stakeholder and I think that it entirely reasonable both to talk to them and to seek funding to help us to develop an area that is deficient in our current provision.”
Uhuh, not a very nice response to a rather moderate letter. Lesson 1: never trust anyone who uses the word “stakeholder”.
It does seem very odd that a medical school like Barts should turn to the Prince of Wales’ Foundation for advice on medicine. After all, the bad advice given by the “Patients Guide” is rather well documented (see also here). If messrs Fowler and Carroll were really unaware of that, I’d argue that they aren’t doing their job properly.
It seems that Barts, like Edinburgh, has over-reacted to pressure from the General Medical Council (GMC). Actually all that the GMC require is that
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
There is nothing there about saying that they work. Certainly medical students need to be familiar with alternative medicine, given the number of theit patients that use it. That is a job I have done myself, both at UCL and at Kings College London. I’d argue that I am marginally better qualified to assess the evidence than the Prince of Wales.
Oddly enough, the bad education in Edinburgh came also from a Professor of Medical Education and Director of Undergraduate Learning and Teaching,
The result is manifested in two ways. Barts has a “Science in Medicine” course that has resulted in medical students being placed with homeopaths. And it has a Special Studies Module in Ayurvedic Medicine. Let’s take a look at them.
An Introduction to Ayurvedic Medicine
| The aims of this Special Study Module are “To introduce the concepts and principles which underpin Ayurvedic medicine. To introduce Year 1 and 2 medical students to the Ayurvedic approach to patient assessment, diagnosis and treatment”, and to “Critically evaluate the evidence base for Ayurvedic treatments and yoga therapy”. Just one small snag there. There is next to no evidence base to be assessed. | Click to enlarge |
The module is given by Professor Shrikala Warrier, who is Dean of MAYUR: The Ayurvedic University of Europe. That sounds quite grand. But the web site of The Ayurvedic University of Europe is rather unusual for a university. It lists two courses but has no list of staff. Could it be that Professor Shrikala Warrier is the staff? Neither is it clear where Professor Warrier’s professorial title comes from. Her own private university perhaps?
The two courses it offers are B.Sc.(Hons) Ayurveda and B.Sc.(Hons) Yoga. It says that the course the “BA(Hons)Ayurvedic Studies is a three year programme of study developed in collaboration with Thames Valley University in London”. That’s odd too, because there is no mention of it on the Thames Valley University web site (and TVU is not in London, it’s in Slough). Elsewhere it is stated that the “programme has been validated by MAHE, which is also the degree awarding body”. MAHE is not explained but it appears to refer to the Manipal Academy of Higher Education, in Goa, India. That looks like a pretty good place. It does not offer degrees in Ayurveda, though there is a small Department of Ayurvedic medicine within the otherwise entirely conventional Kasturba Medical College-Manipal. Their first year physiology exam would tax our students.
Elsewhere we see the same address, 81 Wimpole Street, listed as The Manipal Ayurvedic University of Europe (a joint venture between The Manipal University and the Ayurvedic Company of Great Britain) Prof. S. Warrier, B.A.(Hons), M.A., Ph.D., MILT, Dean of Academic Planning.
If one checks Mayur Ltd at Companies House, one finds that it has two directors, Lady Sarah Morritt and Professor Shrikala Warrier. The company report shows that no accounts have been filed up to now and their 2008 accounts are overdue.
The business history of ayurveda is nothing if not tortuous. The London Gazette (May 2008) notifies us that
AYURVEDA HOLDINGS LIMITED (chairman Lady Sarah Morritt) was passed a Special Resolution: “That the company be wound up voluntarily.”
If you email the Ayurvedic University of Europe, the reply comes not from a University address but from unififiedherbal.com. That seems to be some sort of marketing company, at the same address, 81 Wimpole Street. But efforts to find out more about it from Companies House show that UnifiedHerbal.com was dissolved on 3 October 2006.
Several of the links are broken on the web site of Ayurvedic University of Europe, but one that does work is ‘products’. That takes you to the sales pages of http://www.drwarrier.co.uk/. That doesn’t look much like a university, but no prizes for guessing the address. Yes, it’s 81 Wimpole Street again. They will sell you all sorts of cosmetics, though Companies House lists Dr Warrier Limited, and tells us
Last Accounts Made Up To : 31/08/2007 (DORMANT) and
Next Return Due : 26/09/2008 OVERDUE. Their registered office is
at Harold House, Waltham Cross EN8 7AF.
From drwarrier.co.uk you can buy, for example,
The most commonly prescribed Ayurvedic formula. Triphala is an effective blood purifier that detoxifies the liver, helps digestion and assimilation, and reduces serum cholesterol and lipid levels.
Blood purifier? Detox? Where have we seen this sort of utter gobbledygook before? Or perhaps she can sell you some
Traditionally used for obesity and overweight, and reducing and preventing accumulation of cholesterol (LDL). Its anti-inflammatory and detoxifying actions help reduce arthritic pain and swelling.
There isn’t the slightest evidence for these effects in man. Hence, no doubt, the usual weasel words. “traditionally used for . . . ”
The sales department alone casts rather a large doubt on Prof Warrier’s ability to teach medical students how to “critically evaluate the evidence base for Ayurvedic treatments”.
It does seem a bit surprising that a top flight medical school should think that this is an appropriate place to educate its students.
Medicine in Society
The syllabus at Barts includes something called Medicine and Society. Page 5 of the second year Tutor Guide mentions “complementary therapies” as part of the course. There is little hint about what that means in practice.
It turns out that the alt med placements are at the Greenwich Natural Health Centre. Nothing is too barmy for them Acupuncture. Cranial Osteopathy, Craniosacral Therapy, Herbal Therapy, Homeopathy, Hot Stone Therapy and Nutritional therapy to name but a few of the preposterous make-believe stuff that is on offer.
Medical students are having to spend their time listing to stuff like this, on ‘hot stone therapy’.
“Hot stone therapy / massage is a kind of massage that uses treated volcanic rocks such as basalt and basinite that are believed to promote relaxation as well as eliminating negative energy within the client’s body, mind and soul.”
“These stones are carefully gathered and handcrafted for various sizes, shapes and weights according to what part of the body it will be use on.”
Or this, on ‘nutritional therapy’.
“Many of us lack the basic raw materials (from food and drink) to function at our best. Intensive farming, pollution, stress, stimulants and an over-reliance on processed foods are just some of the reasons for us being deficient in vital nutrients. As a result, we may develop serious degenerative diseases like cancer or arthritis.”
“Some clients may experience reactions like headaches, skin eruptions or bad breath during the first stage of treatment. These are quite normal and are due to detoxification, which is usually followed by a sense of well-being and increased energy.”
That must be about as close as you can get to claiming you can prevent cancer by taking vitamin pills. It is wrong and it is dangerous,
Sigh. What century are we living in?
According to Barts’ second year Tutor Guide, “Placement tutors are responsible for student assessment”.
What sort of grade will the student get if they tell their tutor in homeopathy or ‘Nutritional therapy’ that they are talking nonsense?
What do the students think?
Could the Ayurvedic course be the very same course that is referred to by a second year medical student on the Unprotected Text blog?
“When I found out my friend had been attached to a “doctor” in Ayurvedic “medicine” for the year I was horrified, as was she, and the school would not allow her to change claiming that the point is not to learn the medicine but its role in the multidisciplinary healthcare team.
I don’t believe that there is such a role.
The very fact that a student is forced to put up with this as a part of their education is appalling.”
A comment left on Unprotected Text by someone writing as ‘Barts Medic’ said
“I was HORRIFIED to hear that some of my friends have their medsoc placements
at such RUBBISH places too!last week, they were forced into a room one by room to be touched up (‘massaged’)
by the ‘doctor-person’ to HEAL them. she rubbed them all over, and CHANTED! WTF.if i was given a CRAPPY placement like that, i wouldnt turn up either”.
And there is an excellent statement about “holistic medicine” on Unprotected Text. Better, perhaps, than you’d get from the GMC.
“Holistic medicine is in fact a world away from homeopathy, although the two are often confused predominantly by homeopaths trying to validate their branch of “medicine”. Much of what is taught in medical school is in fact, holistic, and so it should be. The importance of mentality, or spirituality in medicine should not be used to excuse homeopathy.”
“That doesn’t seem to add up” is another blog that relates the experiences of another student who has been exposed to “Enforced quackery Day 1, “, “Enforced quackery Day 2“, “Enforced quackery Days 3 and 4“. He says
“. . .by the end of day 3 the students *still* hadn’t seen any patients and that, when confronted with this fact the person in charge is reported to have said that this was because she was scared of what the students might say to the patients… Apart from this being a massive insult to the professionalism of the students, it is at least an encouraging sign that they have not been very effectively indoctrinated.”
It seems that we shall soon have some more documentary evidence. It is truly impressive to find that Barts’ medical students are so bright and that they have the courage to speak up about it.
So there is one good thing. We have some very perspicacious medical students in London.
Pity that one can’t say the same thing of their teachers.
Follow-up
I have it on good authority that the unhappy students who were placed at the Greenwich Natural Health Centre were presented with one of the more absurd documents ever to be produced by homeopaths, “An Overview of positive homeopathy research and surveys“.
There is no need to argue about whether homeopaths cherry-pick the evidence. The selective use of evidence is announced proudly, right there in the title.
What excuse can Bart’s have for exposing medical students to such profoundly anti-educational stuff as this?
Later there appeared on the That doesn’t seem to add up blog, Enforced
Quackery – the literature. The unfortunate students who were pushed into a homeopathic placement were give a print out of a page from Sue Young’s homeopathic web site. It is merely a bit of phony history that attempts to link Pasteur with homeopathy.
Sue Young, incidentally, is a homeopath who has consistently breached the Code of Ethicsof the Society of Homeopaths by claiming to treat serious diseases, though needless to say the Society did nothing about it. She is also the person who wrote a wholly inaccurate account of the reasons why my blog left the UCL server (see alse here and here). She didn’t, needless to say, ask me, but luckily she was soon corrected on quackometer and in the Guardian.
Incidentally, the Unprotected Text blog continues to provide a fascinating student view on medical education. Students show more sense than their teachers not only about alternative nonsense but also about other gimmicks like ‘problem based learning’.
It’s hard enough to communicate basic ideas about how to assess evidence to adults without having the effort hindered by schools.
The teaching of quackery to 16 year-olds has been approved by a maze of quangos, none of which will take responsibility, or justify their actions. So far I’ve located no fewer than eight of them.
[For non-UK readers, quango = Quasi-Autonomous Non-Governmental Organisation].





![]()


A lot of odd qualifications are accredited by OfQual (see here). Consider, for example, Edexcel Level 3 BTEC Nationals in Health and Social Care (these exams are described here), Download the specifications here and check page 309.
Unit 23: Complementary Therapies for Health and Social Care
NQF Level 3: BTEC National
Guided learning hours: 60Unit abstract
“In order to be able to take a holistic view towards medicine and health care, health and social care professionals need to understand the potential range of complementary therapies available and how they may be used in the support of conventional medicine.”
Well, Goldacre has always said that homeopathy makes the perfect vehicle for teaching how easy it is to be deceived by bad science, so what’s wrong? But wait
“Learners will consider the benefits of complementary therapies to health and wellbeing, as well as identifying any contraindications and health and safety issues in relation to their use.”
Then later
“The holistic approach to illnesses such as cancer could be used as a focus here. For example, there could be some tutor input to introduce ideas about the role of complementary therapies in the treatment and management of cancer, this being followed up by individual or small group research by learners using both the internet and the services available locally/regionally. If available, a local homeopathic hospital, for example, would be an interesting place to visit.”
It’s true that to get a distinction, you have to “evaluate the evidence relating to the use of complementary therapies in contemporary society”, but it isn’t at all clear that this refers to evidence about whether the treatment works.
The really revealing bit comes when you get to the
“Indicative reading for learners
There are many resources available to support this unit.Websites
www.acupuncture.org.uk British Acupuncture Council
www.bant.org.uk British Association for Nutritional Therapy
www.exeter.ac.uk/sshs/compmed Exeter University’s academic department of Complementary medicine
www.gcc-uk.org General Chiropractic Council
www.nimh.org.uk National Institute of Medical Herbalists
www.nursingtimes.net The Nursing Times
www.osteopathy.org.uk General Osteopathic Council
www.the-cma.org.uk The Complementary Medical Association”
This list is truly astonishing. Almost every one of them can be relied on to produce self-serving inaccurate information about the form of “therapy” it exists to promote. The one obvious exception is the reference to Exeter University’s academic department of complementary medicine (and the link to that one is wrong). The Nursing Times should be an exception too, but their articles about CAM are just about always written by people who are committed to it.
It is no consolation that the 2005 version was even worse. In its classification of ‘therapies’ it said “Pharmaceutically mediated: eg herbalism, homeopathy “. Grotesque! And this is the examinng body!
The Teacher
This particular educational disaster came to my attention when I had a letter from a teacher. She had been asked to teach this unit, and wanted to know if I could provide any resources for it. She said that Edexcel hadn’t done so. She asked ” Do you know of any universities that teach CT’s [sic] so I could contact them about useful teaching resources?.” She seemed to think that reliable information about homeopathy could be found from a ‘university’ homeopathy teacher. Not a good sign. It soon emerged why.
She said.
“My students are studying BTEC National Health Studies and the link is Edexcel BTEC National Complimentary [sic] studies.”
“I am a psychotherapist with an MA in Education and Psychology. I am also trained in massage and shiatsu and have plenty of personal experience of alternative therapy”
Shiatsu uh? It seems the teacher is already committed to placebo medicine. Nevertheless I spent some time looking for some better teaching material for 16 year-old children. There is good stuff at Planet
Science, and in some of the pamphlets from Sense about Science, not least their latest, I’ve got nothing to lose by trying it – A guide to weighing up claims about cures and treatments. I sent all this stuff to her, and prefaced the material by saying
“First of all, I should put my cards on the table and say that I am quite appalled by the specification of Unit 23. In particular, it has almost no emphasis at all on the one thing that you want to know about any therapy, namely does it work? The reference list for reading consists almost entirely of organisations that are trying to sell you various sorts of quackery, There is no hint of balance; furthermore it is all quite incompatible with unit 22, which IS concerned with evidence.”
At this point the teacher the teacher came clean too, As always, anyone who disagrees with the assessment (if any) of the evidence by a true believer is unmeasured and inflammatory.
“I have found your responses very unmeasured and inflammatory and I am sorry to say that this prejudicial attitude has meant that I have not found your comments useful.”
shortly followed by
“I am not coming from a scientific background, neither is the course claiming to be scientific.”
That will teach me to spend a couple of hours trying to help a teacher.
What does Edexcel say?
I wrote to Edexcel’s science subject advisors with some questions about what was being taught. The response that I got was not from the science subject advisors but from the Head of Customer support, presumably a PR person.
| From: (Bola Arabome) 12/11/2008 04.31 PM
Dear Professor Colquhoun Thank you for email communication concerning the complementary therapies unit which is available in our BTEC National in Health and BTEC National in Health and Social Care qualifications. I have replied on behalf of Stephen Nugus, our science subject advisor, because your questions do not refer to a science qualification. I would like to answer your questions as directly as possible and then provide some background information relating to the qualifications. The units and whole qualifications for all awarding bodies are accredited by the regulator, the Qualifications and Curriculum Authority. The resource reading list is also produced by us to help teachers and learners. The qualification as a whole is related to the National Occupational Standards for the vocational sectors of Health and Health and social care with consultation taken from the relevant sector skills councils . As you will be aware many of these complementary therapies are available in care centres and health centres under the NHS and in the private sector. The aim of BTEC qualifications is to prepare people for work in these particular sectors. Clearly a critical awareness is encouraged with reference to health and safety and regulation. There are other units, in some cases compulsory, within the qualification with a scientific approach. ‘ ‘ ‘ ‘ ‘ Stephen Harris Head of Customer Support |
Aha, so it seems that teaching people to treat sick patients is “not a science qualification”. Just a business qualification perhaps?. I haven’t yet managed to reach the people who make these decisions, so I persisted with the PR man. Here is part of the next letter (Edexcel’s reply in italic).
| 19 November
I find it quite fascinating that Edexcel regards the treatment of sick patients as not being part of science (“do not refer to a science qualification”). Does that mean Edexcel regard the “Health” part of “Health and Social Care” as being nothing to do with science, and that it therefore doesn’t matter if Health Care is unscientific, or even actively anti-scientific? I am sorry if my answer lacked clarity. My comment, that I had taken your enquiry on behalf of our Science Advisor because this was not a science qualification, was intended to explain why I was replying. It was not intended as a comment on the relationship between Health and Social Care and science. At Edexcel we use bureaucratic categories where we align our management of qualifications with officially recognised occupational sectors. Often we rely on sector bodies such as Sector Skills Councils to endorse or even approve the qualifications we offer. Those involved in production of our Science qualifications and our (4) You say “The qualification as a whole is related to the National Occupational Standards for the vocational sectors of Health and Health and social care with consultation taken from the relevant sector skills councils”. Are you aware that the Skills for Health specifications for Alternative medicine were written essentially by the Prince of Wales Foundation? The qualification was approved by both ‘Skills for Health’ and ‘Skills for Care and Development’ prior to being accredited by QCA. It uses the NOS in Health and Social Care as the basis for many of the mandatory units. The ‘Complementary Therapies’ NOS were not used. This was not a requirement of a ‘Health and Social Care’ qualification. “Are the NOS in Health and Social Care that you mention the ones listed here? http://www.ukstandards.org/Find_Occupational_Standards.aspx?NosFindID=1&ClassificationItemId=174 If so, I can see nothing there about ‘complementary therapies’. if I have missed it, I’d be very grateful if you could let me know where it is. If it is not there, I remain very puzzled about the provenance of Unit 23, since you say it is not based on Skills for Health.” |
Now we are immediately at sea, struggling under a tidal wave of acronyms for endless overlapping quangos. In this one short paragraph we have no fewer than four of them. ‘Skills for Health’, ‘Skills for Care and Development’ , ‘Quality and Curriculum Authority (QCA) and NOS.
It seems that the specification of unit 23 was written by Edexcel, but Harris (25 Nov) declines to name those responsible
“When I refer to our “Health and Social care team” I mean the mix of Edexcel Staff and the associates we employ on a contract basis as writers, examiners and external verifiers. The writers are generally recruited from those who are involved in teaching and assessment the subjects in schools and colleges. The editorial responsibility lies with the Edexcel Staff. I do not have access to the names of the writers and in any case would not be able to pass on this information. Specifications indicate the managers responsible for authorising publication”
“Edexcel takes full responsibility for its ethical position on this and other issues. However we can not accept responsibility for the opinions expressed in third party materials. There is a disclaimer to this effect at the beginning of the specification. ”
” You have the correct link to the Health NOS . These are the standards, which where appropriate, influence our qualifications. However in the case of Unit 23 I understand that there is no link with the Health NOS. I don’t know if the NOS cover the unit 23 content.”
So, contrary to what I was told at first, neither Skills for Health, nor NOS were involved Or were they (see below)?
So who does take responsibility? Aha that is secret. And the approval by the QCA is also secret.
“I cannot provide you with copies of any correspondence between Skills for Health and Edexcel. We regard this as confidential. “
What does the QCA say?
The strapline of the QCA is
“We are committed to building a world-class education and training framework. We develop and modernise the curriculum, assessments, examinations and qualifications.”
Referring school children to the Society of Homeopaths for advice seems to be world-class bollocks rather than world-class education.
When this matter was brought to light by Graeme Paton in the Daily Telegraph, he quoted Kathleen Tattersall, CEO of the QCA. She said
“The design of these diplomas has met Ofqual’s high standards. We will monitor them closely as they are delivered to make sure that learners get a fair deal and that standards are set appropriately.”
Just the usual vacuous bureaucratic defensive sound-bite there. So I wrote to Kathleen Tattersall myself with some specific questions. The letter went on 2nd September 2008. Up to today, 26 November, I had only letters saying
“Thank you for your email of 12 November addressed to Kathleen Tattersall, a response is being prepared which will be forwarded to you shortly.”
“Thank you for your email of 25th November addressed to Kathleen Tattersall. A more detailed response is being prepared which will be sent to you shortly.”
Here are some of the questions that I asked.
| I wrote to Edexcel’s subject advisors about unit 23 and I was told “your questions do not refer to a science qualification”. This seems to mean that if it comes under the name “Health Care” then the care of sick patients is treated as though it were nothing to do with science, That seems to me to be both wrong and dangerous, and I should like to hear your view about that question.
Clearly the fundamental problem here is that the BTEC is intended as a vocational training for careers in alternative medicine, As a body concerned with education, surely you cannot ignore the view of 99% of scientists and doctors that almost all alternative medicine is fraud. That doesn’t mean that you can’t make a living from it, but it surely does create a dilemma for an educational organisation. What is your view of that dilemma? |
Eventually, on 27th November, I get a reply (of sorts) It came not from the Kathleen Tattersall of the QCA but from yet another regulatory body, OfQual, the office of the Qualifications and Examinations Regulator. You’d think that they’d know the answers, but if they do they aren’t telling, [download whole letter. It is very short. The “more detailed response” says nothing.

Ofqual does not take a view on the detailed content of vocational qualifications as that responsibility sits with the relevant Sector Skills Council which represents employers and others involved in the sector. Ofqual accredits the specifications, submitted by sector-skilled professionals, after ensuring they meet National Occupational Standards. Ofqual relies on the professional judgement of these sector-skilled professionals to include relevant subjects and develop and enhance the occupational standards in their profession. The accreditation of this BTEC qualification was supported by both Skills for Health, and Skills for Care and Development, organisations which represent the emerging Sector Qualifications Strategies and comply with the relevant National Occupational Standards Isabel Nisbet Acting Chief Executive |
So no further forward. Every time I ask a question, the buck gets passed to another quango (or two, or three). This letter, in any case, seems to contradict what Edexcel said about the involvement of Skills for Health (that’s the talking to trees outfit),
A nightmare maze of quangos
You may well be wondering what the relationship is between Ofqual and the QCA. There is an ‘explanation’ here.
Ofqual will take over the regulatory responsibilities of the Qualifications and Curriculum Authority (QCA), with stronger powers in relation to safeguarding the standards of qualifications and assessment and an explicit remit as a market regulator. The QCA will evolve into the Qualifications and Curriculum Development Agency (QCDA): supporting Ministers with advice and undertaking certain design and delivery support functions in relation to the curriculum, qualifications, learning and development in the Early Years Foundation Stage, and National Curriculum and Early Years Foundation Stage assessments.
Notice tha QCA won’t be abolished. There will be yet another quango.
The result of all this regulatory bureaucracy seems to be worse regulation, Exactly the same thing happens with accreditiation of dodgy degrees in universities.
At one time, a proposal for something like Unit 23 would have been shown to any competent science teacher, who would have said”you must be joking” and binned it. Now a few hundred bureaucrats tick their boxes and rubbish gets approved.
There seems to be nobody in any of these quangos with the education to realise that if you want to know the truth about homeopathy, the last person you ask is the Society of Homeopaths or the Prince of Wales.
What next?
So the mystery remains. I can’t find out who is responsible for the provenance of the appallingly anti-science Unit 23, and I can’t find out how it got approved. Neither can I get a straight answer to the obvious question about whether it is OK to encourage vocational qualifications for jobs that are bordering on being fraudulent.
.All I can get is platitudes and bland assurances. Everything that might be informative is clouded in secrecy.
The Freedom of Information requests are in. Watch this space. But don’t hold your breath.
Follow-up
Here are some attempts to break through the wall of silence.
Edexcel. I sent them this request.
Freedom of Information Act
Hello
I should like to see please all documents from Edexcel and OfQual or QCA (and communications between then) that concern the formulation and approval of Unit 23 (Complementary Therapies) in the level3 BTEC (page 309 in attached document). In vew of the contentious nature of the subject matter, I believe that is is in the public interest that this information be provided
David Colquhoun
The answer was quite fast, and quite unequivocal, Buzz off.
| Dear Mr Colquhoun,
Thank you of your e-mail of today’s date. I note your request for information pursuant to The Freedom of Information Act. As you may know this Act only applies to public bodies and not to the private sector. Edexcel Limited is privately owned and therefore not subject to this Act. Edexcel is therefore not obliged to provide information to you and is not prepared to give you the information you seek. Please do not hesitate to contact me again if you have any further queries. Kate Gregory |
This lack of public accountability just compounds their appalling inability to distinguish education from miseducation.
International Therapy Examination Council (ITEC)
Mojo’s comment, below, draws attention to the Foundation degree in Complementary Therapies offered by Cornwall College, Camborne, Cornwall (as well as to the fact that the Royal National Lifeboat Institution has been wasting money on ‘research’ on homeopathy –write to them).
At least the courses are held on the Camborne campus of Cornwall College, not on the Duchy campus (do we detect the hand of the Quacktitioner Royal in all this nonsense?).
Cornwall College descends to a new level of barminess in its course Crystal Healing VTCT Level 3
“Who is this course for?
This course is designed to enhance the skills of the Holistic Therapist. Crystals may be used on their own in conjunction with other therapies such as Indian Head Massage, Aromatherapy and Reflexology. Due to the nature of the demands of the holistic programme this course is only suitable for students over the age of 18.”
“What will I be doing on the course?
Students will study the art of Crystal healing which is an energy based treatment where crystals and gemstones are used to channel and focus various energy frequencies.”
| .VTCT stands for the Vocational Training Charitable Trust.
It is yet another organisation that runs vocational exams, and it is responsible for this particular horror |
 |
The crystals are here. I quote.
Objectives
- the use of interpersonal skills with client
- how to complement other therapies with crystals
- the types and effects of different crystals
- uses of crystals including cleansing, energising, configurations
- concepts of auras and chakras
This is, of course, pure meaningless nonsense. Utter bollocks being offered as further education
Cornwall College has many courses run by ITEC.
The College says
“You will become a professional practitioner with the International Therapy Examination Council (ITEC), study a number of essential modules to give a vocational direction to your study that include: Homeopathy and its application,”
| Who on earth, I hear you cry, are ITEC? That brings us to the seventh organisation in the maze of quangos and private companies involved in the miseducation of young people about science and medicine. It appears, like Edexcel, to be a private company though its web site is very coy about that. |  |
After the foundation degree you can go on to “a brand new innovative BSc in Complementary Health Studies (from Sept 2009)”
The ITEC web site says
- ITEC qualifications are accredited by the Office of the Qualifications and Examination Regulator (OFQUAL)
- ITEC qualifications are funded in the uk by the on behalf of Department for Innovation, Universities and Skills (DIUS)
- ITEC qualifications have been mapped to the National Occupational Standards, where they exist
Oddly enough, there is no mention of accreditation by a University (not that that is worth much). So a few more Freedom of Information requests are going off, in an attempt to find out why are kids are being miseducated about science and medicine.
Meanwhile you can judge the effect of all that education in physiology by one of the sample questions for ITEC Unit 4, reflexology.
The pancreas reflex:
A Extends across both feet
B Is on the right foot only
C Is on the left foot only
D Is between the toes on both feet
Uhuh, they seem to have forgotten the option ‘none of the above’.
Or how about a sample question from ITEC Unit 47 – Stone Therapy Massage
Which organ of the body is associated with the element fire?
A Heart
B Liver
C Spleen
D Pancreas
Or perhaps this?
Which incantation makes hot stones work best?
A Incarcerous
B Avada Kedavra,
C Dissendium
D Expelliarmus.
(OK I made the last one up, with help from Harry Potter, but it makes just about as much sense as the real ones).
And guess what? You can’t use the Freedom of Information Act to find out how this preposterous rubbish got into the educational system because ” ITEC is a private organisation therefore does not come under this legislation”. The ability to conduct business in secret is a side effect of the privatisation of public education is another reason why it’s a bad idea.
Ofsted
|
Ofsted has inspected Cornwall College. They say “We inspect and regulate to achieve excellence in the care of children and young people, and in education and skills for learners of all ages.”. I can find no mention of this nonsense in their report, so I’ve asked them. |

|
Ofsted has admitted a spectacular failure in its inspection of child care in the London Borough of Haringey. Polly Curtis wrote in the Guardian (6 Dec 2008) “We failed over Haringey – Ofsted head”. It was the front page story. But of course Ofsted don’t take the blame, they say they were supplied with false information,
That is precisely what happens whenever a committee or quango endorses rubbish. They look only at the documents sent to them and they don’t investigate, don’t engage their brains.
In the case of these courses in utter preposterous rubbish, it seems rather likely that the ultimate source of the misinformation is the Princes’ Foundation for Integrated Health. Tha views of the Prince of Wales get passed on to the ludicrous Skills for Health and used as a criterion by all the other organisations, without a moment of critical appraisal intervening at any point.
2 December 2008 A link from James Randi has sent the hit rate for this post soaring. Someone there left are rather nice comment.
“A quango seems to be a kind of job creation for the otherwise unemployable ‘educated ‘( degree in alternative navel contemplation) middle classes who can’t be expected to do anything useful like cleaning latines ( the only other thing they seem qualified for ). I really hate to think of my taxes paying for this codswollop.”
Today brings a small setback for those of us interested in spreading sensible ideas about science. According to a press release
“The BMJ Group is to begin publishing a medical journal on acupuncture from next year, it was announced today (Tuesday 11 November 2008).
This will be the first complementary medicine title that the BMJ Group has published.”
And they are proud of that? What one earth is going on? The BMJ group is a publishing company which says, of itself,
“Our brand stands for medical credibility. We are one of the world’s best known and most respected medical publishers.”
Well perhaps it used to be.
They have certainly picked a very bad moment for this venture. In the last year there have been at least five good books that assess the evidence carefully and honestly. Of these, the ones that are perhaps the best on the subject of acupuncture are Singh & Ernst’s Trick or Treatment and Barker Bausell’s Snake Oil Science. Both Ernst and Bausell have first hand experience of acupuncture research. And crucially, none of these authors has any financial interest in whether the judgement goes for acupuncture or against it.
Here are quotations from Singh & Ernst’s conclusions
“Reliable conclusions from systematic reviews make it clear that acupuncture does not work for a whole range of conditions, except as a placebo.”
“There are some high quality trials that support the use of acupuncture for some types of pain and nausea, but there are also high quality trials that contradict this conclusion. In short, the evidence is neither consistent nor convincing – it is borderline.”
The House of Lords’ report in 2000 tended to give acupuncture the benefit of the (very considerable) doubt that existed at the time the report was written. Since that time there have been a lot of very well-designed trials of acupuncture.
Now it is quite clear that, for most (and quite possibly all) conditions, acupuncture is no more than a particularly theatrical placebo. Perhaps that is not surprising insofar as the modern western practice of acupuncture owes more to Chinese nationalistic propaganda that started in the time of Mao-Tse Tung than it owes to ancient wisdom (which often turns out to be bunk anyway).
The BMJ Group has decided to endorse acupuncture at a time when it is emerging that the evidence for any specific effect is very thin indeed. Well done.
The journal in question is this.
Acupuncture in Medicine is a quarterly title, which aims to build the evidence base for acupuncture. It is currently self-published by the British Medical Acupuncture Society (BMAS).
One good thing can be said about the Society and the Journal. That is that they don’t espouse all the mumbo-jumbo about ‘meridians’ and ‘Qi’. This, of course, puts them at odds with the vast majority of acupuncture teaching. This sort of internecine warfare between competing sects is characteristic of all sorts of alternative medicine. But that is just ideology. What matters is whether or not sticking needles in you is actually anything more than a placebo.
British Medical Acupuncture Society (BMAS)
The British Medical Acupuncture Society (BMAS). is “a registered charity established to encourage the use and scientific understanding of acupuncture within medicine for the public benefit.”. The phrase “encourage the use” suggests that they do not even envisage the possibility that it might not work. Their web site includes these claims.
Acupuncture can help in a variety of conditions:
- Pain relief for a wide range of painful conditions
- Nausea, especially postoperative nausea and vomiting
- Overactive bladder, also known as bladder detrusor instability
- Menstrual and menopausal problems, eg period pains and hot flushes
- Allergies such as hay fever and some types of allergic rashes
- Some other skin problems such as ulcers, itching and localised rashes
- Sinus problems and more
Presumably the word “help” is chosen carefully to fall just short of “cure”. The claims are vaguely worded, but let’s see what we can find about them from systematic reviews. It appears that the BMAS is being rather optimistic about the evidence.
BMJ Clinical Evidence is considered reliable and is particular interesting because it is owned by the BMJ Publishing Group.
Low Back Pain (chronic) Acupuncture is listed as being of “unknown effectiveness”.
Dysmenorrhoea Acupuncture is listed as being of “unknown effectiveness”.
Osteoarthritis of the knee. Acupuncture is listed as being of “unknown effectiveness”.
Psoriasis (chronic plaque) Acupuncture is listed as being of “unknown effectiveness”.
Neck pain “Acupuncture may be more effective than some types of sham treatment (not further defined) or inactive treatment (not further defined) at improving pain relief at the end of treatment or in the short term (less than 3 months), but not in the intermediate term (not defined) or in the long term (not defined)”
Headache (chronic tension-type) Acupuncture is listed as being of “unknown effectiveness”.
What about the greatest authority, the Cochrane Reviews?
Cochrane Reviews
Low back pain The data do not allow firm conclusions about the effectiveness of acupuncture for acute low-back pain. For chronic low-back pain, acupuncture is more effective for pain relief and functional improvement than no treatment or sham treatment immediately after treatment and in the short-term only. Acupuncture is not more effective than other conventional and “alternative” treatments. The data suggest that acupuncture and dry-needling may be useful adjuncts to other therapies for chronic low-back pain. Because most of the studies were of lower methodological quality, there certainly is a further need for higher quality trials in this area.
Chronic asthma. There is not enough evidence to make recommendations about the value of acupuncture in asthma treatment. Further research needs to consider the complexities and different types of acupuncture.
But most of the vaguely-worded claims made by BMAS have not been the subject of Cochrane reviews. The obvious interpretation of that is that there is not enough evidence to make it worth writing a review. In which case, why does BMAS claim that acupuncture can “help”?
Bandolier is another excellent source of high quality information, This was their view in September 2006
“Large, high-quality randomised trials of acupuncture have been published since the reviews. In fibromyalgia, chemotherapy-induced nausea and vomiting, breech presentation, tension headache, and migraine, all were negative compared with sham acupuncture. One in osteoarthritis of the knee, had statistical improvement over sham acupuncture at three months, but not later. Both large trials and this review of reviews come to the same general conclusion; that over a whole range of conditions and outcomes acupuncture cannot yet be shown to be effective.”
After thousands of years of acupuncture (or at least almost 40 years in the West) there seems to be very little to show for it.
The journal: Acupuncture in Medicine
What about the journal in question? Like all journals devoted to alternative medicine, it claims to be evidence-based. And like all journals devoted to alternative medicine it suffers from a fatal conflict of interest. If this journal were ever to conclude that acupuncture is a placebo, it would destroy the journal and the livelihoods of many of the people who write for it.
Scanning the first three issues of 2008 shows that it is very much like other alternative medicine journals. Most of the papers don’t address the critical question, is it a placebo. And most papers end up rather limply, with a statement along the lines “acupuncture may be useful for ***. More research is needed.”
The editor in chief of the journal is Dr Adrian White, and its editor is Michael Cummings. White is quoted by Ernst in the Guardian in 2004.
“We need to provide hard evidence to support what we all see in our clinics every day: that the modern approach to acupuncture works, and is highly relevant to the new, patient-centred NHS.” .
That means the answer is assumed in advance. That just isn’t science.. ‘We know the answer, all we have to do now is get some evidence’.
Why should the BMJ Group want to do a thing like this?
The press release says
Commenting on the move, BMJ and BMJ Journals Publishing Director, Peter Ashman, said “The journal is a good complement for our existing portfolio of journals and we’re certain that the Society’s members and other subscribers will appreciate the benefits of the decision the BMAS has made on their behalf.”
He continued: “The BMAS is ambitious for its journal to grow and flourish and we’re looking forward to working with the Society to develop an editorial and commercial strategy which will achieve the aims of BMAS and those of its members, while reaching out to the wider global community interested in this fascinating area of medicine.”
Yes, you got it. Money. The same motive that causes some vice-chancellors to bring their university into disrepute by awarding BSc degrees in subjects that are not only not science, but which are oftenly openly anti-science.
Conscience doesn’t seem to bother these people, so let’s put the problem in purely cash terms.
Both the BMJ Group and the vice-chancellors will have to decide whether the cash they gain is sufficient to counterbalance the corrosive effects of their actions on their own reputations.
Follow-up
Only a couple of days later, two new trials show acupuncture is no different from sham controls for helping IVF pregnancy rates. James Randerson in the Guardian writes thus.
“Acupuncture aimed at improving IVF success rates is widely offered by fertility clinics in the UK. In the first of the studies, researchers in Hong Kong split 370 women receiving IVF into two groups. One group received real acupuncture before and after having an IVF embryo implanted into their uterus. The other had the same procedure, except the treatment used retractable needles that did not penetrate the skin.”
“Of the 185 who received the sham treatment, 91 achieved a clinical pregnancy (foetal heartbeat identified using ultrasound) and 71 had a successful delivery. This compared with 72 clinical pregnancies in the true acupuncture group and 55 live births. The differences between the groups were not statistically significant.”
“In a second study, researchers in Chicago used a similar design in which 124 women received true or sham acupuncture. The control group had their skin punctured by real acupuncture needles, but not at genuine “Qi-lines” on the body. In the true acupuncture group, 43.9% achieved a clinical pregnancy, compared with 55.2% of the women given the sham treatment. “
The original paper for the first study can be seen here.

