antiscience
Every single request for information about course materials in quack medicine that I have ever sent has been turned down by universities,
It is hardly as important as as refusal of FoI requests to see climate change documents, but it does indicate that some vice-chancellors are not very interested in openness. This secretiveness is exactly the sort of thing that leads to lack of trust in universities and in science as a whole.
The one case that I have won took over three years and an Information Tribunal decision against the University of Central Lancashire (UCLAN) before I got anything.
UCLAN spent £80,307.95.(inc VAT at 17.5%) in legal expenses alone (plus heaven knows how much in staff time) to prevent us from seeing what was taught on their now defunct “BSc (Hons) homeopathy”. This does not seem to me to be good use of taxpayers’ money. A small sample of what was taught has already been posted (more to come). It is very obvious why the university wanted to keep it secret, and equally obvious that it is in the public interest that it should be seen.
UCLAN had dropped not only its homeopathy "degree" before the information was revealed, They also set up an internal inquiry into all the rest of their courses in magic medicine which ended with the dumping of all of them.
Well, not quite all, There was one left. An “MSc” in homeopathy by e-learning. Why this was allowed to continue after the findings of UCLAN’s internal review, heaven only knows. It is run by the same Kate Chatfield who ran the now defunct BSc. Having started to defend the reputation against the harm done to it by offering this sort of rubbish, I thought I should finish. So I asked for the contents of this course too. It is, after all, much the same title as the course that UCLAN had just been ordered to release. But no, this request too was met with a refusal
Worse still, the refusal was claimed under section 43(2) if the Freedom of Information Act 2000. That is the public interest defence, The very defence that was dismissed in scathing terms by the Information Tribunal less than two months ago,
To add insult to injury, UCLAN said that it would make available the contents of the 86 modules in the course under its publication scheme, at a cost of £20 per module, That comes to £1,720 for the course, Some freedom of information.
Because this was a new request, it now has to go through the process of an internal reviw of the decision before it can ne referred to the Information Commissioner. That will be requested, and since internal reviews have, so far, never changed the initial judgment. the appeal to the Information Commissioner should be submitted within the month. I have been promised that the Information Commissioner will deal with it much faster this time than the two years it took last time.
And a bit more unfreedom
Middlesex University
I first asked Middlesex for materials from their homeopathy course on 1 Oct 2008. These courses are validated by Middlesex university (MU) but actually run by the Centre for Homeopathic Education. Thw MU site barely mentions homeopathy and all I got was the usual excuse that the uninsersity did not possess the teaching materials. As usual, the validation had been done without without looking at what was actually being taught. The did send me the validation document though [download it] As usual, the validation document shows no sign at all of the fact that the usbject of the "BSc" is utter nonsense. One wonderful passage says
“. . . the Panel were assured that the Team are clearly producing practitioners but wanted to explore what makes these students graduates? The Team stated that the training reflects the professional standards that govern the programme and the graduateness is achieved through developing knowledge by being able to access sources and critically analyse these sources . . . “
Given that the most prominent characteristic of homeopaths (and other advocates of magic medicine) is total lack of critical ability, this is hilarious. If they had critical ability they wouldn’t be homeopaths. Hilarious is not quite the right word, It is tragic that nonsense like this can be found in an official university document.
Middlesex, though it doesn’t advertise homeopathy, does advertise degrees in Traditional Chinese Medicine, Herbal Medicine and Ayurveda. On 2nd February 2010 I asked for teaching materials from these courses. Guess what? The request was refused. In this case the exemptions under FOIA were not even invoked but I was told that "All these materials are presently available only in one format at the University – via a student-only accessed virtual learning environment. ". Seems that they can’t print out the bits that I asked for, The internal review has been requested, then we shall see what the Information Commissioner has to say.
Two other cases are at present being considered by the Information Commissioner (Scotland), after requests under the Scottish FoIA were refused. They are interesting cases because they bear on the decision, currently being considered by the government, about whether they should implement the recommendations of the execrable Pittilo report.
Napier University Edinburgh. The first was for teaching material form the herbal medicine course at Napier University Edinburgh. I notice that this course no longer appears in UCAS or on Napier’s own web site, so maybe the idea that its contents might be disclosed has been sufficient to make the university do the sensible thing.
Robert Gordon University Aberdeen The second request was for teaching material from the “Introduction to Homeopathy” course at the Robert Gordon University Aberdeen. The particular interest that attaches to this is that the vice-chancellor of Robert Gordon university is Michael Pittilo. The fact that he is willing to tolerate such a course in his own university seems to me to disqualify him from expressing any view on medical subjects.
Michael Pittilo, Crohn’s disease and Andrew Wakefield
Michael Pittilo has not been active in science for some time now, but Medline does show scientiifc publications for Pittilo RM, between 1979 anf 1998. Between 1989 and 1995 there are five papers published jointly with one Andrew Wakefield. These papers alleged a relationship between measles virus and Crohn’s disease. The papers were published before tha infamous 1998 paper by Wakefield in the Lancet (now retracted) that brought disgrace on Wakefield and probably caused unnecessary deaths.. The link between measles and Crohn’s disease is now equally disproved.
The subject has been reviewed by Korzenik (2005) in Past and Current Theories of Etiology of IBD. Toothpaste, Worms, and Refrigerators
“Wakefield et al proposed that Crohn’s results from a chronic infection of submucosal endothelium of the intestines with the measles virus [Crohn’s disease: pathogenesis and persistent measles virus infection. Wakefield AJ, Ekbom A, Dhillon AP, Pittilo RM, Pounder RE., Gastroenterology, 1995, 108(3):911-6]”
"This led to considerable media interest and< public concern over use of live measles vaccine as well as other vaccines. A number of researchers countered these claims, with other studies finding that titers to measles were not increased in Crohn’s patients, granulomas were not associated with endothelium 49 , measles were not in granulomas50 and the measles vaccine is not associated with an increased risk of Crohn’s disease51–55 "
This bit of history is not strictly relevant to the Pittilo report, but I do find quite puzzling how the government chooses people from whom it wishes to get advice about medical problems.
Follow-up
I notice that the Robert Gordon university bulletin has announced that
“Professor Mike Pittilo, Principal of the University, has been made an MBE in the New Year Honours list for services to healthcare”.
That is a reward for writing a very bad report that has not yet been implemented, and one hopes, for the sake of patients, will never be implemented. I do sometimes wonder about the bizarre honours system in the UK.
Postcript.
On 16th February, the death of Michael Pittilo was announced. He had been suffeing from cancer and was only 55 years old. I wouldn’t wish that fate on my worst enemy.
The Yuletide edition of the BMJ carries a lovely article by Jeffrey Aronson, Patent medicines and secret remedies. (BMJ 2009;339:b5415).
I was delighted to be asked to write an editorial about it, In fact it proved quite hard work, because the BMJ thought it improper to be too rude about the royal family, or about the possibility of Knight Starvation among senior medics. The compromise version that appeared in the BMJ is on line (full text link).
The changes were sufficient that it seems worth posting the original version (with links embedded for convenience).
The cuts are a bit ironic, since the whole point of the article is to point out the stifling political correctness that has gripped the BMA, the royal colleges, and the Department of Health when it comes to dealing with evidence-free medicine. It has become commonplace for people to worry about the future of the print media, The fact of the matter is you can often find a quicker. smarter amd blunter response to the news on blogs than you can find in the dead tree media. I doubt that the BMJ is in any danger of course. It has a good reputation for its attitude to improper drug company influence (a perpetual problem for clinical journals) as well as for clinical and science articles. It’s great to see its editor, Fiona Godlee, supporting the national campaign for reform of the libel laws (please sign it yourself).
The fact remains that when it comes to the particular problem of magic medicine, the action has not come from the BMA, the royal colleges, and certainly not from the Department of Health, It has come from what Goldacre called the “intrepid, ragged band of bloggers”. They are the ones who’ve done the investigative journalism, sent complaints and called baloney wherever they saw it. This article was meant to celebrate their collective efforts and to celebrate the fact that those efforts are beginning to percolate upwards to influence the powers that be.
It seems invidious to pick on one example, but if you want an example of beautiful and trenchant writing on one of the topics dealt with here, you’d be better off reading Andrew Lewis’s piece "Meddling Princes, Medical Regulation and Licenses to Kill” than anything in a print journal.
I was a bit disappointed by removal of the comment about the Prince of Wales. In fact I’m not particularly republican compared with many of my friends. The royal family is clearly good for the tourist industry and that’s important. Since Mrs Thatcher (and her successors) destroyed large swathes of manufacturing and put trust in the vapourware produced by dishonest and/or incompetent bankers, it isn’t obvious how the UK can stay afloat. If tourists will pay to see people driving in golden coaches, that’s fine. We need the money. What is absolutely NOT acceptable is for royals to interfere in the democratic political process. That is what the Prince of Wales does incessantly. No doubt he is well-meaning, but that is not sufficient. If I wanted to know the winner of the 2.30 at Newmarket, it might make sense to ask a royal. In medicine it makes no sense at all. But the quality of the advice is irrelevant anyway. The royal web site itself says “As a constitutional monarch, the Sovereign must remain politically neutral.”. Why does she not apply that rule to her son? Time to put him over your knee Ma’am?
Two of the major bits that were cut out are shown in bold, The many other changes are small.
BMJ editorial December 2009
Secret remedies: 100 years onTime to look again at the efficacy of remedies Jeffrey Aronson in his article [1] gives a fascinating insight into how the BMA, BMJ and politicians tried, a century ago, to put an end to the marketing of secret remedies. They didn’t have much success. The problems had not improved 40 years later when A.J. Clark published his book on patent medicines [2]. It is astounding to see how little has changed since then. He wrote, for example, “On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”> Clark himself was sued for libel after he’d written in a pamphlet “ ‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”. Although he initially tried to fight the case, impending destitution eventually forced him to apologise [3]. If that happened today, the accusation would have been repeated on hundreds of web sites round the world within 24 hours, and the quack would, with luck, lose [4]. As early as 1927, Clark had written “Today some travesty of physical science appears to be the most popular form of incantation” [5]. That is even more true today. Homeopaths regularly talk utter nonsense about quantum theory [6] and ‘nutritional therapists’ claim to cure AIDS with vitamin pills or even with downloaded music files. Some of their writing is plain delusional, but much of it is a parody of scientific writing. The style, which Goldacre [7] calls ‘sciencey’, often looks quite plausible until you start to check the references. A 100 years on from the BMA’s efforts, we need once again to look at the efficacy of remedies. Indeed the effort is already well under way, but this time it takes a rather different form. The initiative has come largely from an “intrepid, ragged band of bloggers” and some good journalists, helped by many scientific societies, but substantially hindered by the BMA, the Royal Colleges, the Department of Health and a few vice-chancellors. Even NICE and the MHRA have not helped much. The response of the royal colleges to the resurgence in magic medicine that started in the 1970s seems to have been a sort of embarrassment. They pushed the questions under the carpet by setting up committees (often populated with known sympathizers) so as to avoid having to say ‘baloney’. The Department of Health, equally embarrassed, tends to refer the questions to that well-known medical authority, the Prince of Wales (it is his Foundation for Integrated Health that was charged with drafting National Occupational Standards in make-believe subjects like naturopathy [8]. Two recent examples suffice to illustrate the problems. The first example is the argument about the desirability of statutory regulation of acupuncture, herbal and traditional Chinese medicine (the Pittilo recommendations) [9]. Let’s start with a definition, taken from ‘A patients’ guide to magic medicine’ [10]. “Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety”. It seems to me to be self-evident that you cannot start to think about a sensible form of regulation unless you first decide whether what you are trying to regulate is nonsense, though this idea does not seem to have penetrated the thinking of the Department of Health or the authors of the Pittilo report. The consultation on statutory regulation has had many submissions [11] that point out the danger to patients of appearing to give official endorsement of treatments that don’t work. The good news is that there seems to have been a major change of heart at the Royal College of Physicians. Their submission points out with admirable clarity that the statutory regulation of things that don’t work is a danger to patients (though they still have a blank spot about the evidence for acupuncture, partly as a result of the recent uncharacteristically bad assessment of the evidence by NICE [12]). Things are looking up. Nevertheless, after the public consultation on the report ended on November 16th, the Prince of Wales abused his position to make a well-publicised intervention on behalf of herbalists [13]. Sometimes I think his mother should give him a firm lesson in the meaning of the term ‘constitutional monarchy’, before he destroys it. The other example concerns the recent ‘evidence check: homeopathy’ conducted by the House of Commons Science and Technology Select Committee (SCITECH). First the definition [10]: “Homeopathy: giving patients medicines that contain no medicine whatsoever”. When homeopathy was dreamt up, at the end of the 18th century, regular physicians were lethal blood-letters, and it’s quite likely that giving nothing saved people from them. By the mid-19th century, discoveries about the real causes of disease had started, but homeopaths remain to this day stuck in their 18th century time warp. In 1842 Oliver Wendell Holmes said all that needed to be said about medicine-free medicine [14]. It is nothing short of surreal that the UK parliament is still discussing it in 2009. Nevertheless it is worth watching the SCITECH proceedings [15]. The first two sessions are fun, if only for the statement by the Professional Standards Director of Boots that they sell homeopathic pills while being quite aware that they don’t work. I thought that was rather admirable honesty. Peter Fisher, clinical director of the Royal Homeopathic Hospital, went through his familiar cherry-picking of evidence, but at least repeated his condemnation of the sale of sugar pills for the prevention of malaria. But for pure comedy gold, there is nothing to beat the final session. The health minister, Michael O’Brien, was eventually cajoled into admitting that there was no good evidence that homeopathy worked but defended the idea that the taxpayer should pay for it anyway. It was much harder to understand the position of the chief scientific advisor in the Department of Health, David Harper. He was evasive and ill-informed. Eventually the chairman, Phil Willis, said “No, that is not what I am asking you. You are the Department’s Chief Scientist. Can you give me one specific reference which supports the use of homeopathy in terms of Government policy on health?”. But answer came there none (well, there were words, but they made no sense). Then at the end of the session Harper said “homeopathic practitioners would argue that the way randomised clinical trials are set up they do not lend themselves necessarily to the evaluation and demonstration of efficacy of homeopathic remedies, so to go down the track of having more randomised clinical trials, for the time being at least, does not seem to be a sensible way forward.” Earlier, Kent Woods (CEO of the MHRA) had said “the underlying theory does not really give rise to many testable hypotheses”. These two eminent people seemed to have been fooled by the limp excuses offered by homeopaths. The hypotheses are testable and homeopathy, because it involves pills, is particularly well suited to being tested by proper RCTs (they have been, and when done properly, they fail). If you want to know how to do it, all you have to do is read Goldacre in the Guardian [16]. It really isn’t vert complicated. “Imagine going to an NHS hospital for treatment and being sent away with nothing but a bottle of water and some vague promises.” “And no, it’s not a fruitcake fantasy. This is homeopathy and the NHS currently spends around £10million on it.” That was written by health journalist Jane Symons, in The Sun [17]. A Murdoch tabloid has produced a better account of homeopathy than anything that could be managed by the chief scientific advisor to the Department of Health. And it isn’t often that one can say that. These examples serve to show that the medical establishment is slowly being dragged, from the bottom up, into realising that matters of truth and falsehood are more important than their knighthoods. It is all very heartening, both for medicine and for democracy itself. David Colquhoun. Declaration of interests. I was A.J. Clark chair of pharmacology at UCL, 1985 – 2004. 1. Aronson, JK BMJ 2009;339:b5415 2. Clark, A,J, (1938) Patent Medicines FACT series 14, London. See also Patent medicines in 1938 and now https://www.dcscience.net/?p=257 3. David Clark “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3) 4. Lewis, A. (2007) The Gentle Art of Homeopathic Killing 5. A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927 6. Chrastina, D (2007) Quantum theory isn’t that weak, (response to Lionel Milgrom). 7 Goldacre, B. (2008) Bad Science. HarperCollins 8. Skills for Health web site 9. A very bad report: gamma minus for the vice-chancellor 10. A Patients’ Guide to Magic Medicine, and also in the Financial Times. 12. NICE fiasco, part 2. Rawlins should withdraw guidance and start again 13. BBC news 1 December 2009 Prince Charles: ‘Herbal medicine must be regulated’. 14. Oliver Wendell Holmes (1842) Homeopathy and Its Kindred Delusions. 15. House of Commons Science and technology committee. Evidence check: homeopathy. Videos and transcripts available at http://www.viewista.com/s/fywlp2/ez/1 16. Goldacre, B. A Kind of Magic Guardian 16 November 2007. 17. Homeopathy is resources drain says |
Follow-up
There is a good account of the third SCITECH session by clinical science consultant, Majikthyse, at The Three Amigos.
16 December 2009.. Recorded an interview for BBC Radio 5 Live. It was supposed to go out early on 17th.
17 December 2009. The editorial is mentioned in Editor’s Choice, by deputy editor Tony Delamothe. I love his way of putting the problem "too many at the top of British medicine seem frozen in the headlights of the complementary medicine bandwagon". He sounds remarkably kind given that I was awarded (by the editor, Fiona Godlee, no less) a sort of booby prize at the BMJ party for having generated a record number of emails during the editing of a single editorial (was it really 24?). Hey ho.
17 December 2009. More information on very direct political meddling by the Prince of Wales in today’s Guardian, and in Press Association report.
17 December 2009. Daily Telegraph reports on the editorial, under the heading “ ‘Nonsense’ alternative medicines should not be regulated“. Not a bad account for a non-health journalist.
17 December 2009. Good coverage in the excellent US blog, Neurologica, by the superb Steven Novella.’ “Intrepid, Ragged Band of Bloggers” take on CAM‘ provides a chance to compare and contrast the problems in the UK and the USA.’
18 December 2009. Article in The Times by former special advisor, Paul Richards. “The influence of Prince Charles the lobbyist is out of hand. Our deference stops us asking questions.”
“A good starting point might be publication of all correspondence over the past 30 years. Then we will know the extent, and influence, of Prince Charles the lobbyist.”
Comments in the BMJ Quite a lot of comments had appeared by January 8th, though sadly they were mostly from the usual suspects who appear every time one suggests evidence matters. A reply was called for, so I sent this (the version below has links).
After a long delay, this response eventually appeared in the BMJ on January 15 2010.
It’s good to see so many responses, though somewhat alarming to see that several of them seem to expect an editorial to provide a complete review of the literature. I ‘ll be happy to provide references for any assertion that I made.
I also find it a bit odd that some people think that an editorial is not the place to express an opinion robustly. That view seems to me to be a manifestation of the very sort of political correctness that I was deploring. It’s a bit like the case when the then health minister, Lord Hunt, referred to psychic surgery as a “profession” when he should have called it a fraudulent conjuring trick. Anything I write is very mild compared with what Thomas Wakley wrote in the Lancet, a journal which he founded around the time UCL came into existence. For example (I quote)
“[We deplore the] “state of society which allows various sets of mercenary, goose-brained monopolists and charlatans to usurp the highest privileges…. This is the canker-worm which eats into the heart of the medical body.” Wakley, T. The Lancet 1838-9, 1
I don’t think it is worth replying to people who cite Jacques Benveniste or Andrew Wakefield as authorities. Neither is it worth replying to people who raise the straw man argument about wicked pharmaceutical companies (about which I am on record as being as angry as anyone). But I would like to reply directly to some of the more coherent comments.
Sam Lewis and Robert Watson. [comment] Thank you for putting so succinctly what I was trying to say.
Peter Fisher [comment]. I have a lot of sympathy for Peter Fisher. He has attempted to do some good trials of homeopathy (they mostly had negative outcomes). He said he was "very angry" when the non-medical homeopaths were caught out recommending their sugar pills for malaria prevention (not that this as stopped such dangerous claims which are still commonplace). He agreed with me that there was not sufficient scientific basis for BSc degrees in homeopathy. I suppose that it isn’t really surprising that he continues to cherry pick the evidence. As clinical director of the Royal London Homeopathic Hospital and Homeopathic physician to the Queen, just imagine the cognitive dissonance that would result if he were to admit publicly that is all placebo after all. He has come close though. His (negative) trial for homeopathic treatment of rheumatoid arthritis included the words "It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response” [2]. [download
the paper]. When it comes to malaria, it matters a lot.
Adrian White [comment] seems to be cross because I cited my own blog. I did that simply because if he follows the links there he will find the evidence. In the case of acupuncture it has been shown time after time that "real" acupuncture does not differ perceptibly from sham. That is true whether the sham consists of retractable needles or real needles in the "wrong" places. A non-blind comparison between acupuncture and no acupuncture usually shows some advantage for the former but it is, on average, too small to be of much clinical significance [3]. I agree that there is no way to be sure that this advantage is purely placebo effect but since it is small and transient it really doesn’t matter much. Nobody has put it more clearly than Barker Bausell in his book, Snake Oil Science [4]
White also seems to have great faith in peer review. I agree that in real science it is probably the best system we have. But in alternative medicine journals the "peers" are usually other true believers in whatever hocus pocus is being promoted and peer reveiw breaks down altogether.
R. M. Pittilo [comment] I’m glad that Professor Pittilo has replied in person because I did single out his report for particular criticism. I agree that his report said that NHS funding should be available to CAM only where there is evidence of efficacy. That was not my criticism. My point was that in his report, the evidence for efficacy was assessed by representatives of Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Every one of them would have been out of work if they had found their subjects were nonsense and that, no doubt, explains why the assessment was so bad. To be fair, they did admit that the evidence was not all that it might be and recommended (as always) more research I’d like to ask Professor Pittilo how much money should be spent on more research in the light of the fact that over a billion dollars has been spent in the USA on CAM research without producing a single useful treatment. Pittilo says "My own view is that both statutory regulation and the quest for evidence should proceed together" but he seems to neglect the possibility that the quest for evidence might fail. Experience in the USA suggests that is exactly what has, to a large extent, already happened.
I also find it quite absurd that the Pittilo report should recommend, despite a half-hearted admission that the evidence is poor, that entry to these subjects should be via BSc Honours degrees. In any case he is already thwarted in that ambition because universities are closing down degrees in these subjects having realised that the time to run a degree is after, not before, you have some evidence that the subject is not nonsense. I hope that in due course Professor Pittilo may take the same action about the courses in things like homeopathy that are run by the university of which he is vice-chancellor. That could only enhance the academic reputation of Robert Gordon’s University.
George Lewith [comment] You must be aware that the proposed regulatory body, the Health Professions Council, has already broken its own rules about "evidence-based practice" by agreeing to take on, if asked, practitioners of Herbal Medicine, Chinese Medicine and Acupuncture. They have (shamefully) excluded the idea that claims of efficacy would be regulated. In other word they propose to provide exactly the sort of pseudo-regulation which would endanger patients They are accustomed to the idea that regulation is to do only with censoring practitioners who are caught in bed with patients. However meritorious that may be, it is not the main problem with pseudo-medicine, an area in which they have no experience. I’m equally surprised that Lewith should recommend that Chinese evaluation of Traditional Chinese medicine should be included in meta-analyses, in view of the well-known fact that 99% of evaluations from China are positive: “No trial published in China or Russia/USSR found a test treatment to be ineffective” [5]. He must surely realise that medicine in China is a branch of politics. In fact the whole resurgence in Chinese medicine and acupuncture in post-war times has less to do with ancient traditions than with Chinese nationalism, in particular the wish of Mao Tse-Tung to provide the appearance of health care for the masses (though it is reported that he himself preferred Western Medicine).
1. Lord Hunt thinks “psychic surgery” is a “profession”. https://www.dcscience.net/?p=258
2. Fisher, P. Scott, DL. 2001 Rheumatology 40, 1052 – 1055. [pdf file]
3. Madsen et al, BMJ 2009;338:a3115 [pdf file]
4. R, Barker Bausell, Snake Oil Science, Oxford University Press, 2007
5. Vickers, Niraj, Goyal, Harland and Rees (1998, Controlled Clinical Trials, 19, 159-166) “Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials”. [pdf file]
15 January 2010. During the SciTech hearings, Kent Woods (CEO of the MHRA) made a very feeble attempt to defend the MHRA’s decision to allow misleading labelling of homeopathic products. Now they have published their justification for this claim. It is truly pathetic, as explained by Martin at LayScience: New Evidence Reveals the MHRA’s Farcical Approach to Homeopathy. This mis-labelling cause a great outcry in 2006, as documented in The MHRA breaks its founding principle: it is an intellectual disgrace, and Learned Societies speak out against CAM, and the MHRA.
22 January 2010 Very glad to see that the minister himself has chosen to respond in the BMJ to the editorial
|
Rt Hon. Mike O’Brien QC MP, Minister of State for Health Services I am glad that David Colquhoun was entertained by my appearance before the Health Select Committee on Homeopathy. But he is mistaken when he says, “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense.” Regulation is about patient safety. Acupuncture, herbal and traditional Chinese medicine involve piercing the skin and/or the ingestion of potentially harmful substances and present a possible risk to patients. The Pittilo Report recommends statutory regulation and we have recently held a public consultation on whether this is a sensible way forward. Further research into the efficacy of therapies such as Homeopathy is unlikely to settle the debate, such is the controversy surrounding the subject. That is why the Department of Health’s policy towards complementary and alternative medicines is neutral. Whether I personally think Homeopathy is nonsense or not is besides the point. As a Minister, I do not decide the correct treatment for patients. Doctors do that. I do not propose on this occasion to interfere in the doctor-patient relationship. |
Here is my response to the minister
|
I am very glad that the minister himself has replied. I think he is wrong in two ways, one relatively trivial but one very important. First, he is wrong to refer to homeopathy as controversial. It is not. It is quite the daftest for the common forms of magic medicine and essentially no informed person believes a word of it. Of course, as minister, he is free to ignore scientific advice, just as the Home Secretary did recently. But he should admit that that is what he is doing, and not hide behind the (imagined) controversy. Second, and far more importantly, he is wrong, dangerously wrong, to say it I was mistaken to claim that “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense". According to that view it would make sense to grant statutory regulation to voodoo and astrology. The Pittilo proposals would involve giving honours degrees in nonsense if one took the minister’s view that it doesn’t matter whether the subjects are nonsense or not. Surely he isn’t advocating that? The minister is also wrong to suppose that regulation, in the form proposed by Pittilo, would do anything to help patient safety. Indeed there is a good case to be made that it would endanger patients (not to mention endangering tigers and bears). The reason for that is that the main danger to patients arises from patients being given “remedies” that don’t work. The proposed regulatory body, the Health Professions Council, has already declared that it is not interested in whether the treatments work or not. That in itself endangers patients. In the case of Traditional Chinese Medicine, there is also a danger to patients from contaminated medicines. The HPC is not competent to deal with that either. It is the job of the MHRA and/or Trading Standards. There are much better methods of ensuring patient safety that those proposed by Pittilo. In order to see the harm that can result from statutory regulation, it is necessary only to look at the General Chiropractic Council. Attention was focussed on chiropractic when the British Chiropractic Association decided, foolishly, to sue Simon Singh for defamation. That led to close inspection of the strength of the evidence for their claims to benefit conditions like infant colic and asthma. The evidence turned out to be pathetic, and the result was that something like 600 complaints were made to the GCC about the making of false health claims (including two against practices run by the chair of the GCC himself). The processing of these complaints is still in progress, but what is absolutely clear is that the statutory regulatory body, the GCC, had done nothing to discourage these false claims. On the contrary it had perpetrated them itself. No doubt the HPC would be similarly engulfed in complaints if the Pittilo proposals went ahead. It is one thing to say that the government chooses to pay for things like homeopathy, despite it being known that they are only placebos, because some patients like them. It is quite another thing to endanger patient safety by advocating government endorsement in the form of statutory regulation, of treatments that don’t work. I would be very happy to meet the minister to discuss the problems involved in ensuring patient safety. He has seen herbalists and other with vested interests. He has been lobbied by the Prince of Wales. Perhaps it is time he listened to the views of scientists too. |
Both the minister’s response, and my reply, were reformatted to appear as letters in the print edition of the BMJ, as well as comments on the web..
A momentous decision was promulgated (as lawyers say) by the Information Tribunal on December 8th 2009. It marks a step forward in Freedom of Information about how universities spend your money. It has taken 3.5 years to get to this point. Perhaps now there will be an end to the attempts of every single university that I’ve
approached to conceal what they teach.
Decision
"The Tribunal upholds the decision notice dated 30th. March, 2009, dismisses the appeal and directs that all the steps required by the Decision Notice be taken within 28 days of the date of this Decision"
Back story for this case
24th July 2006. I asked the University of Central Lancashire (UCLAN) for copies of teaching materials and validation documents for their "BSc" degree in homeopathy (this degree no longer exists: it was abolished in 2008). A year later, UCLAN shut the rest of its courses in alternative medicine, after an internal review.
21 August 2006. I was sent the validation documents but refused the teaching materials as UCLAN claimed they were exempt under section 43(2) of the Freedom of Information Act (FOIA)(commercial interests). Two days later I sent a request for the mandatory internal review of the refusal.
4th October 2006. The internal review confirmed the original decision (it always does), and cited, as well as section .43(2) of FOIA, section 21.
21 October 2006. I appealed to the Information Commissioner. The basis of the appeal was that the university might have financial interests in the outcome, but not commercial interests, because universities are not commercial organisations as defined in section 43(2) of the FOIA. In addition, even if the commercial argument was not allowed, the public interest in knowing what was taught was sufficient to justify release of the requested materials.
21 January 2008. The Information Commissioner finally got round to starting on the case.
29 September 2008 The vice-chancellor, Malcolm McVicar, raised an objection to complying with my request under s.36(2)(c) of FOIA. This states that “In the reasonable opinion of a qualified person, disclosure of the information under this Act” “(c) would otherwise prejudice, or would be likely otherwise to prejudice, the effective conduct of public affairs..”
30 March 2009. The decision of the Information Commissioner was published. It has already been described here. Apart from one trivial matter, my appeal was upheld, and UCLAN was ordered to release the requested material within 35 days. However UCLAN did not release the material, but rather launched an appeal against the Information Commissioner. The appeal was heard by an Information Tribunal.
The full text of the Freedom of Information Act is here.
The Information Tribunal
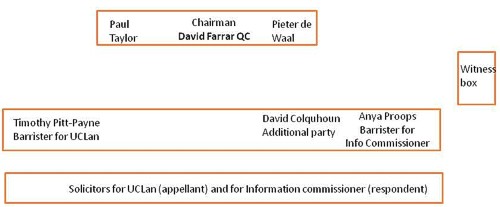
The Tribunal heard the case of University of Central Lancashire v Information Commissioner in Manchester on November 3, 4 and 5. I was an ‘additional party’ to the proceedings and attended in person for the first two days, with the aim of helping the Information Commissioner’s case. This is what the tribunal looked like.
I was amazed to find myself sitting next to the barrister for the Information Commisioner, and still more amazed to be invited to cross-question the witnesses, after she had questioned them.
The witnesses were Malcom McVicar (vice-chancellor of UCLAN), Peter Hyett, (executive director of finance at UCLAN) and David Phoenix (Deputy vice-chancellor, UCLAN).
The outcome
The decision in full can be read here.
|
Decision The Tribunal upholds the decision notice dated 30th. March, 2009, dismisses the appeal and directs that all the steps required by the Decision Notice be taken within 28 days of the date of this Decision. |
So we won.
The details of the decision contain some matters of great interest for universities, in particular the dismissal of the idea that the public can be reassured by either internal or external (e.g. QAA) validation procedures. I’ll try to summarise them (paragraph numbering as in the decision
notice).
Commercial interests
The one disappointing thing about the Tribunal’s decision was that it contradicted the Information Commissioner’s decision on the meaning of commercial interests.
31 "Therefore, whether on a broad or narrow construction of the statutory words, we are satisfied that UCLAN `s interests in teaching material produced for its degree courses are properly described as “commercial”.
However, that does not affect the outcome because the Tribunal decided that there was no reason to think that the course materials actually had the commercial value that UCLAN said they did. For
example:
36 We were not impressed by the claim that third parties with copyright in the disclosed materials would be alienated by UCLAN `s compliance with a decision that this information must be provided. None gave evidence to that effect.
37 It was not clear to us how a competitor could significantly exploit access to this material, without infringing UCLAN `s copyright or brazenly aping the content of a course, which would surely attract the scorn of the wider academic community. Moreover, it seemed to us likely that most potential students would be attracted to a particular course by the reputation of the teaching staff and a range of extra – curricular factors at least as much as by a comparative study of the powerpoint presentations and notes provided to current students.
and
39 Finally, in this particular case, we doubt whether this course had a significant commercial value, given the limited enrolment and the virtual absence of overseas interest.
At this point, the appeal is essentially dismissed. Nevetheless, the Tribunal went on to discuss the other defences offered by UCLAN, and some of their conclusions are more interesting than the subtle distinction between ‘financial interests’ and ‘commercial interests’.
40 In the light of this finding, it is not strictly necessary to decide the balance of public interest as to disclosure. Nevertheless, since the issue has been carefully and very fully argued, we shall shortly indicate our view, had the likelihood of prejudice been established.
Public Interest
The commercial interest defence is subject to the public interest argument in s.1(2((b) of the FOIA’
(b) in all the circumstances of the case, the public interest in maintaining the exclusion of the duty to confirm or deny outweighs the public interest in disclosing whether the public authority
holds the information.
Hence, the decision notice says
41 As ever, the question is whether the public interest in maintaining the exemption outweighs the interest in disclosure.
On the question of public interest, the Tribunal comes down strongly on the side of the Commissioner and me.
46 The public interest in disclosure seems to us appreciably stronger. Apart from the universal arguments about transparency and the improvement of public awareness, we find that there are particular interests here, arising from the nature of a university and the way it is funded.
It is particularly interesting that the Tribunal dismissed the role of internal and external validation as a substitute for transparency. As part of their case (para 18) UCLAN had argued
"Moreover, standards were ensured by the validation procedures which were required before a course was launched and which involved independent expert external monitors and by quality assurance (Q.A.A.) which demands a continuing compliance with national standards."
This cut no ice with the Tribunal. In one of his few direct interjections the Tribunal Chairman, David Farrar Q.C., questioned a witness directly about the internal validation processes, Evidently he was not impressed by the answers. During my own cross questioning of the deputy vice-chancellor, I put to him the view that since the QAA [Quality Assurance Agency] was not allowed to take any notice of the content of courses, that getting a high mark from the QAA was not a substitute for seeing what was actually taught. The deputy vice-chancellor did not seem to disagree strongly with that view.
47 First, the public has a legitimate interest in monitoring the content and the academic quality of a course, particularly a relatively new course in a new area of study, funded, to a very significant extent, by the taxpayer. It is no answer, we consider, to say that this function is performed by the process of validation or the continuing monitoring of standards with external input. Whether or not these processes are conducted with critical rigour, it must be open to those outside the academic community to question what is being taught and to what level in our universities. The apparent perception in some quarters that the intellectual demands of some or many degree courses have been relaxed, that higher classes of degree are too lightly earned, may be largely or entirely unfounded. But it is highly important that the material necessary to a fair judgement be available. That material will often, if not always, include the basic content of the course, such as is requested here.
48 Secondly, this is especially the case where, as with the BSc. (Homeopathy), there is significant public controversy as to the value of such study within a university. In this case, that factor standing alone would have persuaded us that the balance of public interest favoured disclosure.
49 We are not attracted by the somewhat patrician argument that the general public, uninstructed in the specialist subject under scrutiny, would be incapable of forming a proper judgement. That might be so, were it impossible to seek independent expertise to assist in making an assessment. Happily, it is not.
50 Finally, there is a public interest in opening up new methods of teaching and new insights as to the content of courses, so as to stimulate the spread of good practice.
So, a hands down win on the public interest argument.
Prejudice to effective conduct of public affairs
I found incomprehensible the argument that disclosure would ‘prejudice the effective conduct of public affairs’. But it was raised (at the last minute) by UCLAN, and it was considered by the Tribunal. This defence refers to s.36(2)(c) of FOIA. It states that “In the reasonable opinion of a qualified person, disclosure of the information under this Act” “(c) would otherwise prejudice, or would be likely otherwise to prejudice, the effective conduct of public affairs..”
As noted at paragraph 17, it is common ground, established as to (iii), by the jurisprudence of the Tribunal, that this exemption is engaged if three requirements are met. They can be shortly labelled
(i) qualified person
(ii) reasonable opinion
(iii) reasonably arrived at.
The Tribunal seemed to be distinctly unimpressed by the arguments presented by UCLAN.
56 A reasonable opinion may be one with which the Tribunal emphatically disagrees, provided it is based on sound argument and evidence. With great respect to Professor McVicar, whose sincerity is not in question, we can find no adequate evidential basis for this opinion and consider that it rests on two misconceptions as to the application of FOIA. We do not find that it passes the required test of objective reasonableness.
57 We considered separately whether the opinion was reasonably arrived at. Again, our answer is no.
58 Section 36 provides for an exceptional exemption which the public authority creates by its own action, albeit subject to scrutiny of its reasonableness, the likelihood of prejudice and the question of the public interest. That factor of itself justifies a requirement that the authority provide substantial evidence as to the advice (other than legal advice) and the arguments presented to the qualified person upon which his opinion was founded. We emphasise that no set formula is required, just a simple clear record of the process.
59 The need for such evidence is all the greater where, as here, the authority invokes s.36 for the first time after the complaint to the IC [Information Commissioner].
60 The evidence consists of a briefly argued email from Dr. Bostock suggesting that s.36(2)(c) be invoked on the very broadly argued grounds already reviewed. The tone implicitly acknowledges that the claim is rather speculative. We are not concerned with the slightly uncertain use of possibility and likely but the impression left is of a last minute idea, not really thought through or investigated
but merely discussed with solicitors to tie it in to the FOIA. It was sent to the Vice Chancellor at 3.20pm. on a Friday afternoon, 26th. September, 2008, asking for the Vice Chancellor’s agreement. That agreement was forthcoming in a single sentence without further comment in an email reply timed at 12.05pm.on the following Monday.61 We find that the process of forming the necessary opinion was, to say the least, perfunctory, indeed far short of the careful assessment and investigation that normally supports a qualified opinion for the purposes of s.36.
62 Accordingly, we do not find that it was reasonably arrived at.
Conclusion
62 It is for these reasons that we uphold the Decision Notice. We record our gratitude for the helpful and succinct submissions of counsel on both sides and the incisive contribution of Professor Colquhoun. We wish to add that, whilst we have not accepted the great majority of the arguments advanced by UCLAN, we do not in any way seek to cast doubt on the veracity of the evidence of its witnesses, nor the honesty and loyalty with which they have sought to serve its interests.
63 Our decision is unanimous.
Signed David Farrar Q.C.
Watch this space to see what can now be revealed.
Follow-up
It seems very reasonable to suggest that taxpayers have an interest in knowing what is taught in universities. The recent Pittilo report suggested that degrees should be mandatory in Acupuncture, Herbal Medicine and Traditional Chinese Medicine. So it seems natural to ask to see what is actually taught in these degrees, so one can judge whether it protects the public or endangers them.
Since universities in the UK receive a great deal of public money, it’s easy. Just request the material under the Freedom of Information Act.
Well, uh, it isn’t as simple as that.
Every single application that I have made has been refused. After three years of trying, the Information Commissioner eventually supported my appeal to see teaching materials from the Homeopathy "BSc" at the University of Central Lancashire. He ruled that every single objection (apart from one trivial one) offered by the universities was invalid. In particular, it was ruled that univerities were not "commercial" organisations for the purposes of the Act.
So problem solved? Not a bit of it. I still haven’t seen any of the materials from the original request because the University of Central Lancashire appealed against the decision and the case of University of Central Lancashire v Information Commissioner is due to be heard on November 3rd, 4th and 5th in Manchester. I’m joined (as lawyers say) as a witness. Watch this space.
UCLan is not the exception. It is the rule. I have sought under the Freedom of Information Act, teaching materials from UClan (homeopathy), University of Salford (homeopathy, reflexology and nutritional therapy), University of Westminster (homeopathy, reflexology and nutritional therapy), University of West of England, University of Plymouth and University of East London, University of Wales (chiropractic and nutritional therapy), Robert Gordon University Aberdeen (homeopathy), Napier University Edinburgh (herbalism).
In every single case, the request for teaching materials has been refused. And that includes the last three, which were submitted after the decision of the Information Commissioner. They will send things like course validation documents, but these are utterly uninformative box-ticking documents. They say nothing whatsoever about what is actually taught.
The fact that I have been able to discover quite a lot about what’s being taught owes nothing whatsoever to the Freedom of Information Act. It is due entirely to the many honest individuals who have sent me teaching materials, often anonymously. We should be grateful to them. Their principles are rather more impressive than those of their principals.
Since this started about three years ago, two of the universities, UCLan and Salford, have shut down entry to all of their CAM courses. And Westminster has shut two of them, with more rumoured to be closing soon. They are to be congratulated for that, but is far from being the end of the matter. The Department of Health, and some of the Royal Colleges, have yet to catch up with the universities, The Pittolo report, which recommends making degrees compulsory, is being considered by the Department of Health. The consultation ends on November 2nd: if you haven’t yet responded, please do so now (see how here, and here).
A common excuse: the university does not possess teaching materials (yes, really)
Several of the universities claim that they cannot send teaching materials, because they have no access to them. This happens when the university has accredited a course that is run by another, privately run, institution. The place that does the actual teaching, being private, is exempt from the Freedom of Information Act.
The ludicrous corollary of this excuse is that the university has accredited the course without checking on what is taught, and in some cases without even having seen a timetable.
The University of Wales
In fact the University of Wales doesn’t run courses at all. Like the (near moribund) University of London, it acts as a degree-awarding authority for a lot of Welsh Universities. It also validates a lot of courses in non-university institutions, 34 or so of them in the UK, and others scattered round the world.
Many of them are theological colleges. It does seem a bit odd that St Petersburg Christian University, Russia, and International Baptist Theological Seminary, Prague, should be accredited by the University of Wales.
They also validate the International Academy of Osteopathy, Ghent (Belgium), Osteopathie Schule Deutschland, the Istituto Superiore Di Osteopatia, Milan, the Instituto Superior De Medicinas Tradicionales, Barcelona, the Skandinaviska Osteopathögskolan (SKOS) Gothenburg, Sweden and the College D’Etudes Osteopathiques, Canada.
The 34 UK institutions include the Scottish School of Herbal Medicine, the Northern College of Acupuncture and the Mctimoney College of Chiropractic.
The case of the Nutritional Therapy course has been described already in Another worthless validation: the University of Wales and nutritional therapy. It emerged that the course was run by a grade 1 new-age fantasist. It is worth recapitulating the follow up.
What does the University of Wales say? So far, nothing. Last week I sent brief and polite emails to Professor Palastanga and to
Professor Clement to try to discover whether it is true that the validation process had indeed missed the fact that the course organiser’s writings had been described as “preposterous, made-up, pseudoscientific nonsense” in the Guardian.
So far I have had no reply from the vice-chancellor, but on 26 October I did get an answer from Prof Palastanga.
As regards the two people you asked questions about – J.Young – I personally am not familiar with her book and nobody on the validation panel raised any concerns about it. As for P.Holford similarly there were no concerns expressed about him or his work. In both cases we would have considered their CV’s as presented in the documentation as part of the teaching team. In my experience of conducting degree validations at over 16 UK Universities this is the normal practice of a validation panel.
I have to say this reply confirms my worst fears. Validation committees such as this one simply don’t do their duty. They don’t show the curiosity that is needed to discover the facts about the things that they are meant to be judging. How could they not have looked at the book by the very person that they are validating? After all that has been written about Patrick Holford, it is simply mind-boggling that the committee seems to have been quite unaware of any of it.It is yet another example of the harm done to science by an unthinking, box-ticking approach.
Incidentally, Professor Nigel Palastanga has now been made Pro Vice-Chancellor (Quality) at the University of Wales and publishes bulletins on quality control. Well well.
The McTimoney College of Chiropractic was the subject of my next Freedom of Information request to the University of Wales. The reasons for that are, I guess, obvious. They sent me hundreds of pages of validation documents, Student Handbooks (approx 50 pages), BSc (Hons) Chiropractic Course Document. And so on. Reams of it. The documents mostly are in the range of 40 to 100 pages. Tons of paper, but none of it tells you anyhing whatsover of interest about what’s being taught. They are a testament to the ability of universities to produce endless vacuous prose with
very litlle content.
They did give me enough information to ask for a sample of the teaching materials on particular topics. But I gor blank refusal, on the grounds that they didn’t possess them. Only McTimoney had them. Their (unusually helpful) Freedom of Information officer replied thus.
“The University is entirely clear about the content of the course but the day to day timetabling of teaching sessions is a matter for the institution rather than the University and we do not require or possess timetable information. The Act does not oblige us to request the information but there is no reason you should not approach McTimoney directly on this.”
So the university doesn’t know the timetable. It doesn’t know what is taught in lectures, but it is " entirely clear about the content of the course".
This response can be described only as truly pathetic.
Either this is a laughably crude form of obstruction of my request, or perhaps, even more frighteningly, the university really believes that its endless box-ticking documents actually provide some useful control of quality. Perhaps the latter interpretation is more charitable. After all, the QAA, CHRE, UUK and every HR department share similar delusions about what constitutes quality.
Perhaps it is just yet another consequence of having science run largely by people who have never done it and don’t understand it.
Validation is a business. The University of Wales validates no fewer than 11,675 courses altogether. Many of these are perfectly ordinary courses in universities in Wales, but they validate 594 courses at non-Welsh accredited institutions, an activity that earned them £5,440,765 in the financial year 2007/8. There’s nothing wrong with that if they did the job properly. In the two cases I’ve looked at, they haven’t done the job properly. They have ticked boxes but they have not looked at what’s being taught or who is teaching it.
The University of Kingston
The University of Kingston offers a “BSc (Hons)” in acupuncture. In view of the fact that the Pittilo group has recommended degrees in acupuncture, there is enormous public interest in what is taught in such degrees, so I asked.
They sent the usual boring validation documents and a couple of sample exam papers . The questions were very clinical, and quite beyond the training of acupuncturists. The validation was done by a panel of three, Dr Larry Roberts (Chair, Director of Academic Development, Kingston University), Mr Roger Hill (Accreditation Officer, British Acupuncture Accreditation Board) and Ms Celia Tudor-Evans (Acupuncturist, College of Traditional Acupuncture, Leamington Spa). So nobody with any scientific expertise, and not a word of criticism.
|
Further to your recent request for information I am writing to advise that the University does not hold the following requested information: (1) Lecture handouts/notes and powerpoint presentations for the following sessions, mentioned in Template 3rd year weekend and weekday course v26Aug2009_LRE1.pdf (a) Skills 17: Representational systems + Colour & Sound ex. Tongue feedback 11 (b) Mental Disease + Epilepsy Pulse feedback 21 (c) 18 Auricular Acupuncture (d) Intro. to Guasha + practice Cupping, moxa practice Tongue feedback 14 (2) I cannot see where the students are taught about research methods and statistics. I would like to see Lecture handouts/notes and PowerPoint presentations for teaching in this area, but the ‘timetables’ that you sent don’t make clear when or if it is taught. The BSc Acupuncture is delivered by a partner college, the College of Integrated Chinese Medicine (CICM), with Kingston University providing validation only. As such, the University does not hold copies of the teaching materials used on this course. In order to obtain copies of the teaching materials required you may wish to contact the College of Integrated Chinese Medicine directly. This completes the University’s response to your information request. |
So again we see that Kingston has validated the course but has not seen a timetable, far less what is taught. My reply was thus
|
Yes I am exceedingly unhappy about it. The university attaches its name to the course so it must obviously be able to get the material simply by asking for it (I’m surprised that the university should endorse a course without knowing what is taught on it, but that’s another matter). I request formally that you obtain this material. If necessary please read this as a formal appeal. |
I await with interest. In every single case so far, the internal review has merely confirmed the initial refusal. It means a bit of a delay before the case goes to the Information Commisssioner’s Office.
Napier University Edinburgh
Napier University runs a "BSc (Hons) Herbal medicine". (brochure here). Since herbal medicine is a subject of the Pittilo recommendations, there is enormous public interest in what they teach. So I asked, under the Freedom of Information (Scotland) Act (2002). They sent quite quickly validation and accreditation documents, some examination papers, timetables and lecture lists.
The validation was the usual vacuous box-ticking stuff though it did reveal that the course “made extensive use of techniques such as tongue and pulse diagnosis”, which are well known phoney diagnosis methods, about as much use as a pendulum (as used at Westminster University).
As at Kingston University, the exam papers they chose to send were mostly "pretend doctor" stuff. One of them was
Discuss the herbal practitioner’s role in the management of IHD [ischaemic heart disease)
How one would like to see what the students said, and, even more one would like to see the model answer. Amateurs who try to treat potentially serious conditions are a danger to the public.
So then we got to the interesting bit, the request for actual teaching materials.
|
I have looked at the material that you sent and I’d now like to make the following supplementary request (A) Lecture notes/handouts and powerpoint slides for the following small smaple of lectures HRB09102 Materia Medica 4 Materia Medica 3 HRB08103 Clinical Medicine and Diagnosis 4 (HRB09104) HRB09100 Materia Medica & Herbal Practice BSc Herbal Medicine : Materia Medica HRB07102 Lastly, I can see nowhere in the timetable, lectures that deal with Research methods, clinical trial design and statistics. |
No prizes for guessing the result Total refusal to send any of them. To make matters worse, the main grounds for refusal were the very "commercial interests" which, after careful legal examination, the Information Commissioner (for England and Wales) had decided were invalid. They say too that "The public interest in withholding the information is greater than the public interest in its release".. It is hard to see how the public interest is served by concealing from the people who pay for the degrees what is taught on degrees that Pittilo wants to make compulsory. [Download the whole response]
The matter is now under internal appeal (read the appeal) and eventually we shall find out whether the Scottish Information Commissioner backs the judgement.
Robert Gordon University Aberdeen
This case has particular interest because the Vice-Chancellor of Robert Gordon University is Professor Michael Pittilo, chair of the highly contentious steering group that recommended degress in CAM. Robert Gordon University (RGU) does not teach herbal medicine or acupuncture. But they do run An Introduction to Homeopathy. All the degrees in homeopathy have closed. It is perhaps the daftest and most discredited of all the popular forms of Magic Medicine. But Professor Pittilo thinks it is an appropriate subject to teach in his university.
So again I asked for information under the Freedom of Information (Scotland) Act 2002. They sent me quite quckly a list of the powerpoint presentations used on the courses [download it]. I asked for a small sample of the powerpoints. And again the university did not possess them!
|
I should like to see only the following three powerpoint presentations in the first instance, please.
Please can you let me know also who produced the powerpoints. (1) Evidence for homeopathy I note that you will have to request them but since they are being offered as part of a course offered by RGU, so RGU is responsible for their quality, I presume that this should cause no problem. |
The request was refused on much the same grounds as used by Napier University. As usual, the internal review just confirmed the initial proposal (but dropped the obviously ludicrous public interest defence). The internal review said
“it is mainly the quality of our courses (including course material) and teaching which has given us the position of "the best modern university in Scotland"
I am bound to ask, if the university is so proud of its course material, why is it expending so much time and money to prevent anyone from seeing a small sample of it?
My appeal has been sent to the Scottish Information Commissioner [download the appeal].
What are vice-chancellors thinking about?
I find it very difficult to imagine what is going through the heads of vice-chancellors who run courses in mumbo-jumbo. Most of them don’t believe a word of it (though Michael Pittilo might be an exception) yet they foist it on their students. How do they sleep at night?
Recently the excellent Joe Collier wrote a nice BMJ blog which applauded the lack of respect for authority in today’s students, Joe Collier says good riddance to old-fashioned respect. I couldn’t resist leaving a comment.
|
I couldn’t agree more. There is nothing quite so unnerving as being addressed as “Sir”. It is an advantage of age that you realise what second-rate people come to occupy very grand positions. Still odder since, if occasionally they are removed for incompetence, they usually move to an even grander position. I guess that when I was an undergraduate, I found vice-chancellors somewhat imposing. That is, by and large, not a view that survives closer acquaintance. |
Should teaching materials be open to the public?
There is only one university in the world that has, as a matter of policy, made all of its teaching material open to the public, that is the Massachusetts Institute of Technology (MIT). I can recommend strongly course 18.06, a wonderful set of lectures on Linear Algebra by Gilbert Strang. (It is also a wonderful demonstration of why blackboards may be better than Powerpoint for subjects like this). Now they are on YouTube too.
A lot of other places have made small moves in the same direction, as discussed recently in Times Higher Education, Get it Out in the Open.
Now the OU is working with other British universities to help them develop and share open course materials. In June, at the celebrations for the 40th anniversary of the OU, Gordon Brown announced funding to establish the Support Centre for Open Resources in Education at the OU, as part of a £7.8 million grant designed to enhance the university’s national role.
The funding follows a separate grant of £5.7 million from the Higher Education Funding Council for England for universities across the sector to make thousands of hours of free learning materials available.
Much material is available on the web, when individual teachers choose to place it there, but at the same time there is a move in the other direction. In particular, the widespread adoption of Moodle has resulted in a big decrease in openness. Usually you have to be registered on a course to see the material. Even other people in the university can’t see it. I think that is a deplorable development (so, presumably, does HEFCE).
Conclusion
I was told by the Univerity of Kingston that
“The course is one which the University has validated and continues to be subject to the University’s quality assurance procedures, such as internal subject reviews, annual monitoring and external examining”
The only conclusion to be drawn from this is that “quality arrurance procedures” work about as well in universities as they did in the case of baby Peter. No doubt they were introduced with worthy aims. But in practice they occupy vast amounts of time for armies of bureaucrats, and because the brain does not need to be engaged they end up endorsing utter nonsenes. The system is broken.
Resistance is futile. You can see a lot of the stuff here
It is hard to keep secrets in the internet age. Thanks to many wonderful people who have sent me material. you can see plenty of what is taught, despite the desperate attempts of vice-chancellors to conceal it. Try these links.
What is actually taught
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself
https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients
https://www.dcscience.net/?p=2043
More make-believe from the University of Westminster. This time its Naturopathy
https://www.dcscience.net/?p=1812
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
https://www.dcscience.net/?p=1329
The opposite of science
https://www.dcscience.net/?p=1191
Bad medicine. Barts sinks further into the endarkenment.
https://www.dcscience.net/?p=1143
A letter to the Times, and progress at Westminster
https://www.dcscience.net/?p=984
Nutritional Fairy Tales from Thames Valley University
https://www.dcscience.net/?p=260
Westminster University BSc: amethysts emit high yin energy
https://www.dcscience.net/?p=227
References for Pittilo report consultation
A very bad report: gamma minus for the vice-chancellor
https://www.dcscience.net/?p=235
The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on the Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire,
https://www.dcscience.net/?p=2310
An excellent submission to the consultation on statutory regulation of alternative medicine (Pittilo report)
https://www.dcscience.net/?p=2329
Follow-up
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
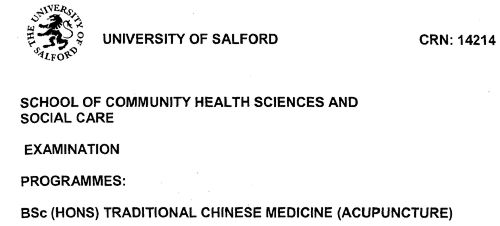
Acupuncture has been in the news since, in a moment of madness, NICE gave it some credence,
Some people still seem to think that acupuncture is somehow more respectable than, say, homeopathy and crystal healing. If you think that, read Barker Bausell’s book ot Trick or Treatment. It is now absolutely clear that ‘real’ acupuncture is indistinguishable from sham, whether the sham control uses retractable needles, or real needles in the ‘wrong’ places. There has been no clear demonstration of long-lived benefits in any condition, and it is likely that it is no more than a theatrical placebo.
In particular, the indistinguishability of ‘real’ and sham acupuncture shows, beyond reasonable doubt that all the stuff about “energy flow in meridians” is so much hokum.
There is a small group of ‘medical acupuncturists‘ that believes that it is hokum. but who nonetheless maintain that acupuncture works, despite the evidence to the contrary. But most acupuncturists go for the wholesale gobbledygook.
If you don’t believe that, take a look at the exam paper that has come into my possession. It is this year’s exam from the University of Salford. Salford has, very sensibly, now decided to stop all its degrees in alternative medicine, so don’t hold this against the university too much.
You can download the entire exam paper. Here are a few highlights.
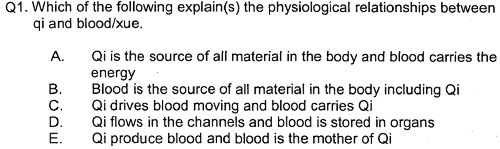
So students, in 2009, are being taught the crudest form of vitalism.
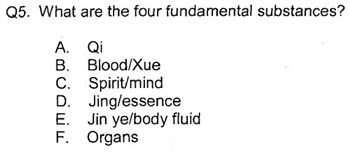
Oh really. Perhaps protons neutrons and electrons?
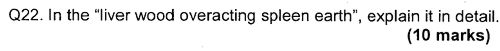
OK I’d fail that one because the words have no obvious meaning at all.
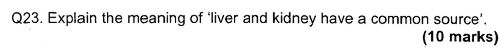
Perhaps an elementary textbook of embryology would help?
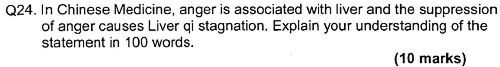
How one would love to see a set of model answers for these questions.
All this is ancient hokum being taugh to hapless students in the 21st century as though it were fact. The University of Salford has understood that and closed the course. All we need now is for NICE and the Department of Health to understand what it is that they are promoting.
NICE neglected the cultural cost of their guidance
When National Institute for Health and Clinical Excellence (NICE) included an acupuncture option on their low back pain guidance, they quite forget that one effect of their decision would be to ensure that new generations of students would have their minds poisoned with intellectual junk like this. That is why NICE really must think again. . See also
NICE falls for bait and switch by acupuncturists and chiropractors
NICE fiasco part 2 Rawlins should withdraw guidance and start again
NICE fiasco Part 3. Too many vested interests, not enough honesty
Pittilo and statutory regulation
Public consultation is due to open shortly on the appalling report of the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK (see also, The Times)
One of the recommendations is that acupuncture and Chinese herbal medicine should have statutory regulation by the Health Professions Council (HPC), despite the fact that that would involve the HPC breaking its own rules. Another recommendation of Pittilo is that entry to the “profession” (his word, not mine) should be by means of honours degree only. So he wants to impose on students exams like this one in order to “protect the public”? The absurdity of that proposal should be obvious now. This exam paper will form part of my evidence to the consultation.
And there is one other small problem. Universities are busy shutting down their degrees in alternative medicine, now that the ridiculousness of what is taught has been exposed. They have shut down entirely at the University of Salford and at the University of Central Lancashire, And even the University of Westminster is working on closing them.
All we need now is for the common sense and integrity that has been shown by these universities to spread to the Department of Health (and NICE).
Follow-up
Here is a short break from the astonishing festival of chiropractic that has followed the British Chiropractic Association (BCA) v Simon Singh defamation case, and the absurd NICE guidance on low back pain.
|
Singh’s statement already has over 10000 signatories, many very distinguished, Sign it now if you haven’t already. And getting on for 600 separate complaints about exaggerated and false claims by chiropractors have been lodged with the General Chiropractic Council and with Trading Standards offices. |
The BCA has exposed the baselessness of most of chiropractic’s claims more effectively than any sceptic could have done.
The University of Westminster is seeing the light?
It is only recently that the University of Westminster suspended entry to degrees in homeopathy and remedial massage and neuromuscular therapy. Luckily for science, they have a new Dean who knows bullshit when she sees it. I suspect than she has been instrumental in starting to restore Westminster’s reputation. The job isn’t finished yet though. According to the UCAS site Westminster still offers
- Chinese Medicine: Acupuncture with Foundation (B341) 4FT Hon BSc
- Health Sciences: Complementary Ther with Foundn (B300) 4FT Hon BSc
- Health Sciences: Complementary Therapies (B255) 3FT Hon BSc
- Health Sciences: Herbal Medicine (B342) 3FT Hon BSc
- Health Sciences: Herbal Medicine with Foundation (B340) 4FT Hon BSc
- Health Sciences: Naturopathy (B391) 3FT Hon BSc
- Health Sciences: Naturopathy with Foundation (B392) 4FT Hon BSc
- Health Sciences: Nutritional Therapy (B400) 3FT Hon BSc
- Health Sciences: Nutritional Therapy with Foundn (B402) 4FT Hon BSc
With the possible exception of herbal medicine, which could be taught scientifically. all the rest is as delusional as homeopathy.
Rumour has it that Naturopathy may be next for the chop, so it seems appropriate to help the dean by showing a bit more of what the hapless students get taught. Remember that, according to Westminster, this is a bachelor of science degree!
Psychotherapeutic Approaches in Naturopathy 3CMW606
“This module is a core subject for BSc (Hons) Health Sciences: Naturopathy and option for BSc (Hons) Health Sciences: Complementary Therapies; BSc (Hons) Health Sciences: Therapeutic Bodywork; Graduate Diploma in Therapeutic Bodywork.”
Lectures 3 – 5 of this course are about the Theory and Application of EmoTrance.
EMOTRANCE? No I had never heard of it either. But it takes only two minutes with Google to discover that it yet another product of the enormous navel-gazing self-help industry. A new variant is born almost every day, and no doubt they make buckets of money for their inventors. You can download a primer from http://emotrance.com/. The web site announces.
“EmoTrance REAL energy healing for the 21st Century”
Here are three quotations from the primer.
|
And then I thought of the lady in the supermarket whose husband had died, and I spend the following time sending her my best wishes, and my best space time quantum healing efforts for her void. It doesn’t matter how “bad”; something is or how old, it is ONLY AN ENERGY and energy can be moved with consciousness in quantum time, easily, and just for the asking. Is EmoTrance a Science? |
Now back to Westminster
Here are a few slides about EmoTrance
|
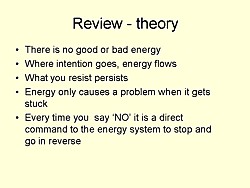
|
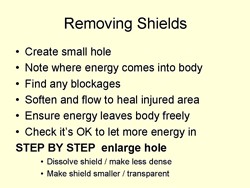
|
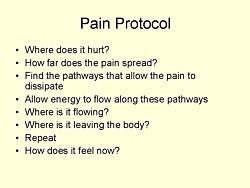
|
So it is pure vitalistic psycho-babble. The usual undefined use of impressive sounding words like “energy” and “quantum” with no defined meaning. Just preposterous made-up gobbledygook.
Before getting to EmoTrance, the course Psychotherapeutic Approaches in Naturopathy (3CMW606) had a lecture on Flower Essences. The evidence says, not surprisingly, that the effects of flower essences is not distinguishable from placebo “The hypothesis that flower remedies are associated with effects beyond a placebo response is not supported by data from rigorous clinical trials.” (See Ernst Wien. Klin. Wochenschr. 2002 114(23-24):963-6). Here are two of the slides.
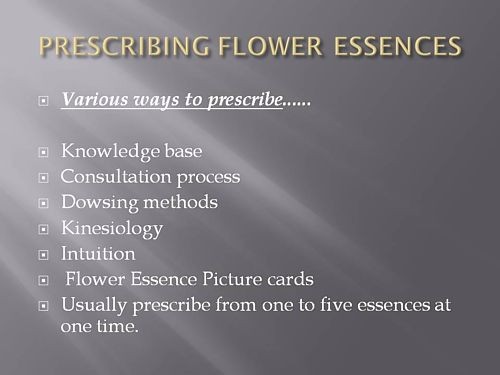
This last slide departs from the simply silly to the totally mad. Dowsing? Kinesiology?
Pendulums I’m told from more than one source that the use of pendulums is not uncommon. both in teaching and by students in the Westminster University polyclinic Apparently they provide an excellent way to choose a ‘remedy’ or make a diagnosis (well, I expect they are as good as the alternatives). If in doubt, guess.
Of course pendulums were popular with Cherie Blair who is reported to have taken her son Leo to a pendulum waver, Jack Temple, rather than have him vaccinated with MMR. At least her delusions affected fewer people than those of her husband (the latest Iraq body count is about 100,000).
Kinesiology was originally a word that applied to the perfectly sensible science of human movement. But Applied Kinesiology more often refers now to a fraudulent and totally ineffective diagnostic method invented by (you guessed) a chiropractor. It has been widely used by alternative medicine to misdiagnose food allergies. It does not work (Garrow, 1988: download reprint).
General Chiropractic Council It is a mind-boggling sign of the incompetence of the General Chiropractic Council that they manage to include kinesiology within their definition of “evidence based care”. Their definition is clearly sufficiently flexible to include anything whatsoever. The incompetence of the GCC is documented in superb detail on jdc325’s blog (James Cole).
Council for Healthcare Regulatory Excellence (CHRE) is yet another example of the network of ineffective and incompetent quangos that plague us.. It is meant to ensure that regulation is effective but utterly fails to do so. The CHRE is quoted as saying “[The GCC] takes its role seriously and aspires to, and often maintains, excellence.”. Like endorsing kinesiology and ‘craniosacral therapy’ perhaps? Quangos like the CHRE not only fail to ensure regulatory excellence, they actually endorse rubbish. They do more harm than good.
The reading list for the course includes the following books. I guess the vibrational medicine (whatever that means) was covered already in the now infamous ‘amethysts emit high yin energy‘ lectures.
Reading List
Essential:
Hartman S (2003) Oceans of Energy: The Patterns and Techniques of EmoTrance: Vol 1.DragonRising. ISBN: 1873483732.
Lynch V and Lynch P (2001) Emotional Healing in Minutes. Thorsons: London. ISBN: 0007112580Recommended:
Gerber R (2001) Vibrational Medicine for the 21st Century. Piatkus Publishers: London.
Gurudas (1989) Flower Essences and Vibrational Medicine. Cassandra Press: California, USA
Hartman S (2000) Adventures in EFT: The Essential Field Guide to Emotional Freedom Techniques. DragonRising. ISBN: 1873483635.
Hartman S (2004) Living Energy: The Patterns and Techniques of EmoTrance: Vol 2. DragonRising.ISBN: 1873483740.
Hartman S (2006) Energy Magic: The Patterns and Techniques of EmoTrance: Vol 3. Dragon Rising.ISBN: 1873483767.
Real magic.
Sylvia Hartman’s books seem to feature heavily in the reading list. I just got news of her latest effort
Welcome to a special update to the June 2009 newsletter to announce Silvia Hartmann’s latest book “Magic, Spells & Potions” is now available to pre-order from our site. The eBook edition will be released this Sunday, the most magical day of the year.
http://DragonRising.com/store/magic_spells_and_potions/?r=DR0609MSAP
If you do pre-order this exciting new book, not only will you be amongst the first to receive your copy, but you will also be entered into an exciting competition for Silvia Hartmann’s handmade copal amber magic pendant. Each paperback book pre-ordered will also be signed by the author and contain a unique blessing for the reader.
Because this is a serious book on real magic, potions and fortune telling if you are a beginner Silvia has provided ample sample spells and potions for you to practice working with before you start covering the advanced material.
What? No honestly, I didn’t invent that.
The idea that stuff of this sort is appropriate for a bachelor of science degree is simply ludicrous. I have no doubt that Westminster’s new dean can see that as well as anyone else. She has the delicate diplomatic job of extirpating the nonsense, I wish her well.
Follow-up
Two days ago I wrote NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself
Now the official ‘guidance’ is out, and it is indeed quite as bad as the draft.
The relevant bits now read thus.
- Offer one of the following treatment options, taking into account patient preference: an exercise programme, a course of manual therapy or a course of acupuncture. Consider offering another of these options if the chosen treatment does not result in satisfactory improvement.
- Consider offering a structured exercise programme tailored to the person:
- This should comprise of up to a maximum of 8 sessions over a period of up to 12 weeks.
- Offer a group supervised exercise programme, in a group of up to 10 people.
- A one-to-one supervised exercise programme may be offered if a group programme is not suitable for a particular person.
- Consider offering a course of manual therapy, including spinal manipulation, comprising up to a maximum of nine sessions over a period of up to 12 weeks
- Consider offering a course of acupuncture needling comprising up to a maximum of 10 sessions over a period of up to 12 weeks.
The summary guidance still doesn’t mention chiropractic explicitly, just a coy reference to “spinal manipulation”. At a time when the British Chiropractic Association is busy trying to suppress free speech via the law courts, I guess it isn’t surprising that they don’t like to use the word.
The bias in the recommendations is perhaps not surprising because the guidance development group had a heavy representation from alternative medicine advocates, and of people with a record of what, is, in my view, excessive tolerance of mumbo-jumbo.
Royal College of General Practitioners (RCGP) played a large part in writing the guidance. That is an organisation thar has steadfastly refused to make any sort of sensible statement of policy about magic medicine. It isn’t long since I was told by a senior person at the RCGP that there was nothing odd about neuro-linguistic programming. That does not bode well.
Professor Martin Underwood, Professor of Primary Care Research Warwick Medical School, University of Warwick. Underwood chaired the guidance development group. Martin Underwood is also a GP in Coventry See also the British Osteopathic Association. Underwood was lead author of the BEAM trial (download reprint). It is well worth reading the comments on this trial too. It was a randomised trial (though not, of course, blind).
|
Our main aim was to estimate, for patients consulting their general practitioner with back pain, the effectiveness of adding the following to best care in general practice: a class based exercise programme (“back to fitness”), a package of treatment by a spinal manipulator (chiropractor, osteopath, or physiotherapist), or manipulation followed by exercise Conclusions |
In other words, none of them worked very well. The paper failed to distinguish between manipulation by physiotherapists, chiropractors and osteopaths and so missed a valuable chance to find out whether there is an advantage to employing people from alternative medicine (the very problem that this NICE guidance should have dealt with)
Steve Vogel, another member of the guidance development group, is an osteopath. Osteopathy has cast off its shady origins better than chiropractic, but it remains a largely evidence-free zone, and is still usually classified as alternative medicine.
Peter Dixon DC FCC FBCA is chairman of the General Chiropractic Council and founder of Peter Dixon Associates. They run six chiropractic clinics. The claims made by these clinics on their web site are mostly related to musculo-skeletal conditions (not, all spine-related however). But they also include
“Chiropractic is also suitable for relieving the symptoms of stress, and optimizing the way the body works is one of the best ways of enhancing health and wellbeing.”
I wonder how they could justify that claim? Then we get
A chiropractor is always willing to discuss individual conditions or answer questions in order to assess whether chiropractic may be of benefit.
Thanks for the invitation. I accepted it. After the first two phone calls, I had learned all I needed.
The first of Peter Dixon’s clinics that I called, was asked about my son who was suffeiing from perpetual colic. I asked for advice. I was put through to the chiropractor. Here are some extracts from the conversation.
“I think now it’s termed irritable baby syndrome. . . . . We’ve found chiropractic is very effective for colic . . . . £50 up to 3/4 hour which would involve taking a case history, examining the baby, with regard to seeing how the joints in the spine work because often colic is down to, er um, faulty movement patterns in the spine. We deal with an awful lot of things to do with the frame -how the spine moves -and it’s often problems with the way that the bones of the spine move in infants and babies that is the underlying cause in colicky symptoms. . . usually on the whole, I’ve shot myself in the foot by saying this in the past, if there are -um when I say back problems they’re usually temporary issues -when they are there the response for most babies is quite quick . . . it depends on how it’s related to what’s gone on in the birth process -there is usually some traumatic cause and it usually sets up a problem in the upper neck or the mid-back and that will drive those colic symptoms. . . . Yes it’s quite a straightforward thing we just check the baby’s spine and see if it’s problem we can deal with or not.”
Yes, I think you just shot yourself in the foot again. I have no idea in what fraction of cases a chiropractor would fail to claim that it was a case that they could deal with. At least that possibility was envisaged. But when I asked where he’d refer me to in such case I was told it might be a result of bottle feeding -“what they consume”. So I expect it would have been sent to some sort of “nutritional therapist” who would have used one of their usual battery of unreliable tests for food allergies.
I tried a second clinic in Peter Dixon’s empire and asked if chiropractic could help with asthma.”It can do, depending on what type of asthma you have". After some questions I was asked
“Do you have any general aches and pains otherwise, any tension .problems round the rib cage or thoracic spine . . . There are two things we’d look as chiropractors as to whether we could help or not and that would include the tension round the rib cage -in any type of asthma you’ll become tight round the rib cage and merely by keeping that area loose you’d help to stop the asthma from becoming quite as bad. And the second part is we’d look at the neck area with you to see if there is any restriction there -which houses the nerve supply to the lungs which can be indicated in some asthma cases also.”
I was invited to come for a free screen, so I asked if it usually worked quickly, “It depends what the problem is but you’d need a course I suspect”. £45 for the first appointment then £28 per session. “In most cases you’d need to look at a six to eight session course”.
Would anyone with experience of crying babies or of asthma like to comment on these proposed treatments? They are not my idea of evidence-based treatments and I find it quite surprising that someone who sponsors them is thought appropriate to write guidance for NICE.
This sort of ‘sting’ always makes me feel a bit uneasy, but it seems to be the only way to find out what actually goes on. And what goes on has all the appearance of classic bait and switch. You go in for your backache, and before you know where you are you are being sold a course of treatment to stop your baby crying.
Media follow-up after the NICE announcement
Sadly, I heard that the Today programme (my favourite news programme) was pretty wet. if only their science reporting was as good as their politics reporting.
The 27th May was certainly pretty busy for me, Apart from a couple of local paper interviews, this is what happened,
Sky News TV. Richard Suchet and two cameraman came to UCL and filmed a lot of stuff out of which a 20 second clip was used. And then they grumble that they don’t make money.
BBC TV 6 o’clock News. Similar, but at least only two people this time. Both TV stations spent ages showing pictures of people having needles pushed into them and very little time discussing the problems. A pathetically bad attempt at science reporting. Radio, on the whole, did much better
BBC Three Counties Radio (09.20) Host Ronnie Barbour, The daytime talk shows may be appalling to some of us, but the hosts did a far better job of airing the problems than TV [download the mp3].
Radio 5 Live Victoria Derbyshire [download the mp3]
BBC Radio Sheffield (12.05) was the best talk show by far. First speaker was Steve Vogel, the osteopath from the guidance development group. Although invited by the rather sensible host, Rony, to respond to the idea that a secondary consequence of the guidance would be to introduce hocus-pocus, he steadfastly refused to answer the question. At the end a rather sensible GP summed up the view from the coalface. [play the mp3]
Radio 4 PM programme This excellent early evening news programme is run by Eddie Mair. It was the best interview yet. The other side was put by Martin Underwood, chair of the guidance development group [play the mp3]
Underwood said “the evidence shows that it [acupuncture] works”. I disagree. The evidence shows that acupuncture, in a non-blind comparison with no acupuncture shows a small, variable additional effect that doesn’t last and is of marginal clinical significance, That is not what I call “works”. Underwood then indulges in the subgroup analysis fallacy by asserting that a few people get a large benefit from acupuncture. Or perhaps a few people just happen to get better that day. I was not convinced.
More 4 News TV 20.20 was an interview, with the other side being put by my old friend, George Lewith.
During the introduction, an acupuncturist. Lisa Sherman, ‘explained’ acupuncture in the usual sort of utterly meaningless words that illustrate perfectly the problem.
George Lewith said that “we don’t have a good pretend form of acupuncture”. “We don’t have a good placebo and we can demonstrate that acupuncture is literally twice as effective as conventional care”. The first is simply nonsense: huge efforts have gone into developing good controls in acupuncture studies (see, for example, Barker Bausell’s book, Snake Oil Science). And I hope that George will send the references for his “twice as effective” claim. It seems to me to be nothing short of preposterous.
My conclusions
So what went wrong?
One problem could be regarded as medical arrogance. The fact is that the problem of low back pain has not been solved, either by drugs or anything else. It is a failure of medicine (and of pharmacology). That should be the premise of all discussions, and it smacks of arrogance not to tell people straight out. Of course there are some cases when causes can be identified, and perhaps remedied, usually by surgery, but these are the exceptions not the rule.
One consequence of the inability of medicine to help much is that patients get desperate, and willing to try anything. And of course if they happen to have a remission, that is attributed to the treatment, however preposterous that treatment may have been. Conditions like back pain that come and go unpredictable are a gift for quacks.
Another consequence, for researchers rather than patients, is to clutch at straws. Even small and inconsistent effects are seized on as ‘successes’. This phenomenon seems to be part of the reason for the NICE guidance. Another reason is, almost certainly, the grinding of axes by some of the people who wrote it.
What should be done now?
Professor Sir Michael Rawlins is a sensible chap. He cares about evidence, But it does seem that in this case, he might have taken his eye off the ball, for once. In my opinion, he should restore the reputation of NICE by withdrawing this guidance and starting again.
Follow-up
An interesting document has come my way. It shows the responses of the guidance group to the consultation on the draft guidance. Many people made comments not unlike mone, but they were all brushed aside in a way that looks to me rather partisan. The document appears to have vanished from NICE’s web site, but you can download it here.
Friday 29th May. The Times prints a letter from two consultants in pain medicine, Joan Hestor and Stephen Ward. It says, inter alia
“As experienced pain specialists we feel that NICE has lost its way in publishing these guidelines.”
“We are saddened that NICE has chosen to ignore our important role and promote seemingly unworkable and for the most part clinically ineffective treatments”
Friday 29th May. NICE has had a good reputation in the USA for its important, and usually high-quality, attempts to assess what works and what doesn’t. That makes it all the sadder to see it condemned already from the USA for its latest effort. The excellent Yale neurologist, Steven Novella, has written about it on his Neurologica blog.
Friday 29th May. A correspondent points out that the costings of the guidance can be found on the NICE web site. Table 1 has a strong air of make-believe.
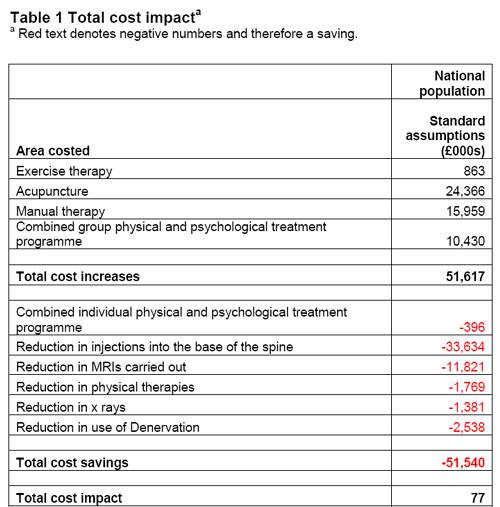
The Daily Mail (29 May 2009). Their article quotes serious criticisms of NICE.
Dr Ron Cooper, past chairman of the group and a consultant pain specialist in Northern Ireland, said: ‘I have never known so many pain medicine specialists to be so furious. More patients will end up having more expensive surgery, which is unnecessary, risky and has worse results.
‘NICE made it difficult for us to submit evidence to a committee on which there was not one experienced pain physician.
‘The guidelines will make us the laughing stock of Europe, Australia and the U.S. where pain specialists will continue to have full access to a wide range of treatments.’
Chirowatch suspended. 30 May 2009. The invaluable chiro-watch site, http://www.chirowatch.com, run by Dr Canadian physician, Dr Tom Polevoy, has been “suspended”. In fact the whole of his domain, healthwatcher.net, has been disabled. It seems that this was the result of a legal threat to his ISP, not by chiropractors this time, but by William O’Neill of the Canadian Cancer Research Group, which is far from being what the respectable-sounding title suggests, according to Dr Stephen Barrett. The site will be back soon, I’m told. Meanwhile you can read the suspended page here, and the only result of their hamfisted bullying will be to vastly increase the number of people who read it. You can read lots more at Quackwatch’s chirobase and at ebm-first.
A new blog, Not as NICE as you think appeared on May 30th. It is written by a pain physician, Stephen Ward. and is devoted to pointing out the serious problems raised by NICE’s guidance. It starts with the (very critical) World Institute of Pain Press Release.
British Medical Journal has more flak for the NICE guidelines
And the BMJ has published a letter signed by 50 consultants in pain medicine, NICE guidelines on low back pain are flawed.(this will probably appear as a letter in the print edition of the BMJ).
First the MHRA lets down the public by allowing deceptive labelling of sugar pills (see here, and this this blog). Now it is the turn of NICE to betray its own principles.
The National Institute for Health and Clinical Excellence (NICE) describes its job thus
“NICE is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health.”
Its Guidance document on Low Back Pain will be published on Wednesday 27 May 2009, but the newspapers have already started to comment, presumably on the assumption that it will have changed little from the Draft Guidance of September 2008. These comments may have to be changed as soon as the final version becomes available.
The draft guidance, though mostly sensible, has two recommendations that I believe to be wrong and dangerous. The recommendations include (page 7) these three.
- Consider offering a course of manual therapy including spinal manipulation of up to 9 sessions over up to 12 weeks.
- Consider offering a course of acupuncture needling comprising up to 10 sessions over a period of up to 12 weeks.
- Consider offering a structured exercise programme tailored to the individual.
All three of this options are accompanied by a footnote that reads thus.
“A choice of any of these therapies may be offered, taking into account patient preference.”
On the face if it, this might seem quite reasonable. All three choices seem to be about as effective (or ineffective) as each other, so why not let patients choose between them?
Actually there are very good reasons, but NICE does not seem to have thought about them. In the past I have had a high opinion of NICE but it seems that even they are now getting bogged down in the morass of political correctness and officialdom that is the curse of the Department of Health. It is yet another example of DC’s rule number one.
Never trust anyone who uses the word ‘stakeholder’.
They do use it, often.
So what is so wrong?
For a start, I take it that the reference to “spinal manipulation” in the first recommendation is a rather cowardly allusion to chiropractic. Why not say so, if that’s whar you mean? Chiropractic is mentioned in the rest of the report but the word doesn’t seem to occur in the recommendations. Is NICE perhaps nervous that it would reduce the credibility of the report if the word chiropractic were said out loud?
Well, they have a point, I suppose. It would.
That aside, here’s what’s wrong.
The Evidence
I take as my premise that the evidence says that no manipulative therapy has any great advantage over the others. They are all more or less equally effective. Perhaps I should say, more or less equally ineffective, because anyone who claims to have the answer to low back pain is clearly deluded (and I should know: nobody has fixed mine yet). So for effectiveness there are no good grounds to choose between exercise, physiotherapy, acupuncture or chiropractic. There is, though, an enormous cultural difference. Acupuncture and chiropractic are firmly in the realm of alternative medicine. They both invoke all sorts of new-age nonsense for which there isn’t the slightest good evidence. That may not poison your body, but it certainly poisons your mind.
Acupuncturists talk about about “Qi”, “meridians”, “energy flows”. The fact that “sham” and “real” acupuncture consistently come out indistinguishable is surely all the evidence one needs to dismiss such nonsense. Indeed there is a small group of medical acupuncturists who do dismiss it. Most don’t. As always in irrational subjects, acupuncture is riven by internecine strife between groups who differ in the extent of their mystical tendencies,
Chiropractors talk of “subluxations”, an entirely imaginary phenomenon (but a cause of much unnecessary exposure to X-rays). Many talk of quasi-religious things like “innate energy”. And Chiropractic is even more riven by competing factions than acupuncture. See, for example, Chiropractic wars Part 3: internecine conflict.
The bait and switch trick
This is the basic trick used by ‘alternative therapists’ to gain respectability.
There is a superb essay on it by the excellent Yale neurologist Steven Novella: The Bait and Switch of Unscientific Medicine. The trick is to offer some limited and reasonable treatment (like back manipulation for low back pain). This, it seems, is sufficient to satisfy NICE. But then, once you are in the showroom, you can be exposed to all sorts of other nonsense about “subluxations” or “Qi”. Still worse, you will also be exposed to the claims of many chiropractors and acupuncturists to be able to cure all manner of conditions other than back pain. But don’t even dare to suggest that manipulation of the spine is not a cure for colic or asthma or you may find yourself sued for defamation. The shameful legal action of the British Chiropractic Association against Simon Singh (follow it here) led to an addition to DC’s Patients’ Guide to Magic Medicine.
(In the face of such tragic behaviour, one has to be able to laugh).
Libel: A very expensive remedy, to be used only when you have no evidence. Appeals to alternative practitioners because truth is irrelevant.
NICE seems to have fallen for the bait and switch trick, hook line and sinker.
The neglected consequences
Once again, we see the consequences of paying insufficient attention to the Dilemmas of Alternative Medicine.
The lying dilemma
If acupuncture is recommended we will have acupuncturists telling patients about utterly imaginary things like “Qi” and “meridians”. And we will have chiropractors telling them about subluxations and innate energy. It is my opinion that these things are simply make-believe (and that is also the view of a minority of acupuncturist and chiropractors). That means that you have to decide whether the supposed benefits of the manipulation are sufficient to counterbalance the deception of patients.
Some people might think that it was worth it (though not me). What is unforgivable is not to consider even the question. The NICE guidance says not a word about this dilemma. Why not?
The training dilemma
The training dilemma is even more serious. Once some form of alternative medicine has successfully worked the Bait and Switch trick and gained a toehold in the NHS, there will be an army of box-ticking HR zombies employed to ensure that they have been properly trained in “subluxations” or “Qi”. There will be quangos set up to issue National Occupational Standards in “subluxations” or “Qi”. Skills for Health will issue “competences” in “subluxations” or “Qi” (actually they already do). There will be courses set up to teach about “subluxations” or “Qi”, some even in ‘universities’ (there already are).
The respectability problem
But worst of all, it will become possible for aupuncturists and chiropractors to claim that they now have official government endorsement from a prestigious evidence-based organisation like NICE for “subluxations” or “Qi”. Of course this isn’t true. In fact the words “subluxations” or “Qi” are not even mentioned in the draft report. That is the root of the problem. They should have been. But omitting stuff like that is how the Bait and Switch trick works.
Alternative medicine advocates crave, above all, respectability and acceptance. It is sad that NICE seems to have given them more credibility and acceptance without having considered properly the secondary consequences of doing so,
How did this failure of NICE happen?
It seems to have been a combination of political correctness, failure to consider secondary consequences, and excessive influence of the people who stand to make money from the acceptance of alternative medicine.
Take, for example, the opinion of the British Pain Society. This organisation encompasses not just doctors. It
includes “doctors, nurses, physiotherapists, scientists, psychologists, occupational therapists and other healthcare professionals actively engaged in the diagnosis and treatment of pain and in pain research for the benefit of patients”. Nevertheless, their response to the draft guidelines pointed out that the manipulative therapies as a whole were over-represented.
|
Manipulation The guidelines assess 9 large groups of interventions of which manual therapies are only one part. The full GDG members panel of 13 individuals included two proponents of spinal manipulation/mobilisation (P Dixon and S Vogel). In addition, the chair of the panel (M Underwood) is the lead author of the UKBEAM trial on which the positive recommendation for |
It seems that the Pain Society were quite right.
LBC 97.3 Breakfast Show (25 May 2009) had a quick discussion on acupuncture (play mp3 file). After I had my say, the other side was put by Rosey Grandage. She has (among other jobs) a private acupuncture practice so she is not quite as unbiassed as me). As usual, she misrepresents the evidence by failing to distinguish between blind and non-blind studies. She also misrepresented what I said by implying that I was advocating drugs. That was not my point and I did not mention drugs (they, like all treatments, have pretty limited effectiveness, and they have side effects too). She said “there is very good evidence to show they (‘Qi’ and ‘meridians’] exist”. That is simply untrue.
There can’t be a better demonstration of the consequences of falling for bait and switch than the defence mounted by Rosey Grandage. NICE may not mention “Qi” and “meridians”; but the people they want to allow into the NHS have no such compunctions.
I first came across Rosey Grandage when I discovered her contribution to the Open University/BBC course K221. That has been dealt with elsewhere. A lot more information about acupuncture has appeared since then. She doesn’t seem to have noticed it. Has she not seen the Nordic Cochrane Centre report? Nor read Barker Bausell, or Singh & Ernst? Has she any interest in evidence that might reduce her income? Probably not.
Where to find out more
An excellent review of chiropractic can be found at the Layscience site. It was written by the indefatigable ‘Blue Wode’ who has provided enormous amounts of information at the admirable ebm-first site (I am authorised to reveal that ‘Blue Wode’ is the author of that site). There you will also find much fascinating information about both acupuncture and about chiropractic.
I’m grateful to ‘Blue Wode’ for some of the references used here.
Follow-up
In March 2007 I wrote a piece in Nature on Science degrees without the science. At that time there were five “BSc” degrees in homeopathy. A couple of weeks ago I checked the UCAS site for start in 2009, and found there was only one full “BSc (hons)” left and that was at Westminster University.
Today I checked again and NOW THERE ARE NONE.
A phone call to the University of Westminster tonight confirmed that they have suspended entry to their BSc (Hons) homeopathy degree.
They say that they have done so because of “poor recruitment”. It was a purely financial decision. Nothing to do with embarrasment. Gratifying though it is that recruits for the course are vanishing, that statement is actually pretty appalling It says that the University of Westminster doesn’t care whether it’s nonsense, but only about whether it makes money.
Nevertheless the first part of this post is not entirely outdated before it even appeared, because homeopathy will still be taught as part of Complementary Therapies. And Naturopathy and “Nutritional Therapy” are still there..
According to their ‘School of Integrated Health‘, “The University of Westminster has a vision of health care for the 21st Century”. Yes, but it is what most people would call a vision of health care in the 18th century.
The revelation that the University of Westminster teaches that Amethysts emit high Yin energy caused something of a scandal.
Since then I have acquired from several sources quite a lot more of their teaching material, despite the fact that the university has refused to comply with the Freedom of Information Act.
In view of the rather silly internal review conducted by Westminster’s Vice-Chancellor, Professor Geoffrey Petts, this seems like a good moment to make a bit more of it public,
I think that revelation of the material is justified because it is in the
public interest to know how the University if Westminster is spending taxpayers’ money. Another motive is to defend the reputation of the post-1992 universities. I have every sympathy with the ex-polytechnics in their efforts to convert themselves into universities. In many ways they have succeeded. That effort
is impeded by teaching mystical versions of medicine.
If the University of Westminster is being brought into disrepute, blame its vice-chancellor, not me.
Homeopathic spiders
Here are a few slides from a lecture on how good spider venom is for you. It is from Course 3CTH502 Homeopathic Materia Medica II. No need to worry though, because they are talking about homeopathic spider venom, so there is nothing but sugar in the pills. The involvement of spiders is pure imagination. No more than mystical gobbledygook.
You are in hurry, or play with your fingers? You need spider venom pills (that contain no spider venom).
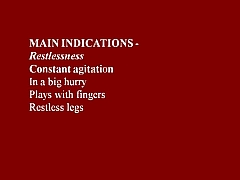

You break furniture? Time goes too fast for you? Try the tarantula-free tarantula pills.
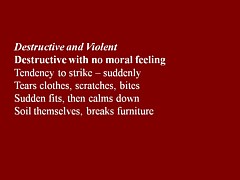
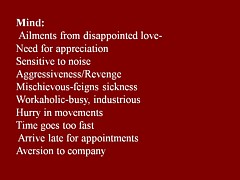
You are preoccupied with sex? You play with ropes? What you need is Mygale (which contains no Mygale)

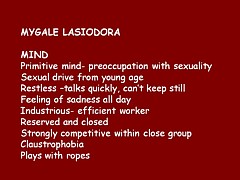
Much more seriously, the same sugar pills are recommended for serious conditions, chorea, ‘dim sight’, gonorrhoea, syphilis and burning hot urine.
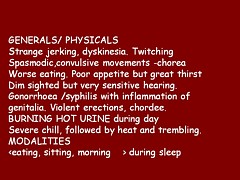
This isn’t just preposterous made-up stuff. It is dangerous.
There is a whole lot more fantasy stuff in the handouts for Homeopathy Materia Medica II (3CTH502). Here are a couple of examples.
Aurum metallicum (metallic gold) [Download the whole handout]
Affinities MIND, VASCULAR SYSTEM, Nerves, Heart, Bones, Glands, Liver, Kidneys, RIGHT SIDE, Left side.
Causations Emotions. Ailments from disappointed love and grief, offence or unusual responsibility, abuse of mercury or allopathic drugs.
Aurum belongs to the syphilitic miasm but has elements of sycosis (Aur-Mur).
Potassium salts are the subject of some fine fantasy, in “The Kali’s” [sic]. (there is much more serious stuff to worry about here than a few misplaced apostrophes.). [Download the whole handout]
“The radioactive element of potassium emits negative electrons from the atom nucleus and is thought to be significant in the sphere of cell processes especially in relation to functions relating to automatism and rhythmicity.”
“Kali people are very conscientious with strong principles. They have their rules and they stick to them, ‘a man of his word’.”
“Potassium acts in a parasympathetic way, tending towards depression”
“They [“Kali people=] are not melancholic like the Natrum’s but rather optimistic.”
Radioactive potassium is involved in automaticity? Total nonsense.
Where is the science?
Yes, it is true that the students get a bit of real science. There isn’t the slightest trace that I can find of any attempt to resolve the obvious fact that what they are taught in the science bits contradict directly what they are told in the other bits. Sounds like a recipe for stress to me.
They even get a bit of incredibly elementary statistics. But they can’t even get that right. This slide is from PPP – Res Quant data analysis.
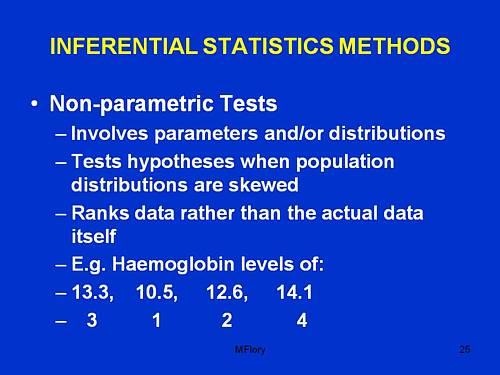
“Involves parameters and/or distributions”. This has no useful meaning whatsoever, that I can detect.
“Tests hypotheses when population distributions are skewed”. Well yes, though nothing there about forms of non-Gaussian properties other than skew, nothing about normalising transformations, and nothing about the Central Limit theorem.
“Ranks data rather than the actual data itself”. This is plain wrong. Randomisation tests on the original data are generally the best (uniformly most powerful) sort of non-parametric test. It seems to have escaped the attention of the tutor that ranking is a short-cut approximation that allowed tables to be constructed, before we had computers.
The students are told about randomised controlled trials. But amazingly in the lecture PPP-RCTs, the little matter of blinding is barely mantioned. And the teacher’s ideas about randomisation are a bit odd too.
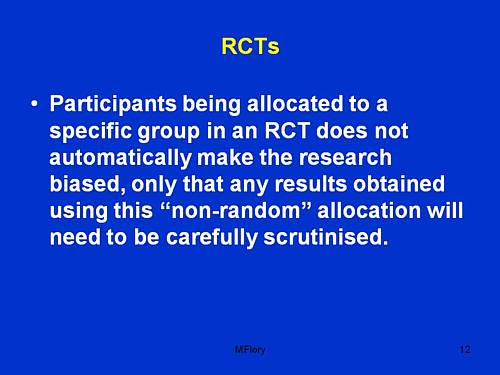
Sorry, but if you fiddle the randomisation, no amount of “careful scrutiny” will rescue you from bias.
An Introduction to Naturopathic Philosophy
Naturopathy is just about as barmy as homeopathy. You can see something about it at the University of Wales. How about this slide from Westminster’s An Introduction to Naturopathic Philosophy.
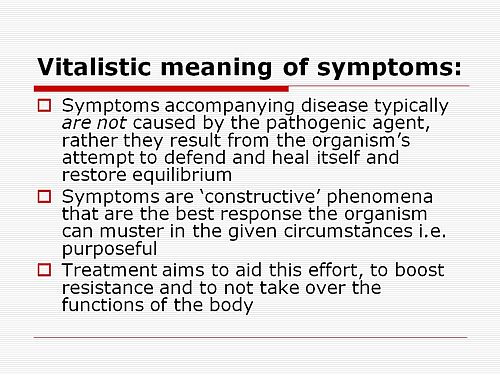
So if you get tuberculosis, it isn’t caused by Mycobacterium tuberculosis? And the symptoms are “constructive”? So you don;t need to do anything. It’s all for the best really.
This isn’t just nonsense. It’s dangerous nonsense.
Traditional Chinese Medicine
Ever wondered what the mysterious “Qi” is? Worry no more. All is explained on this slide.
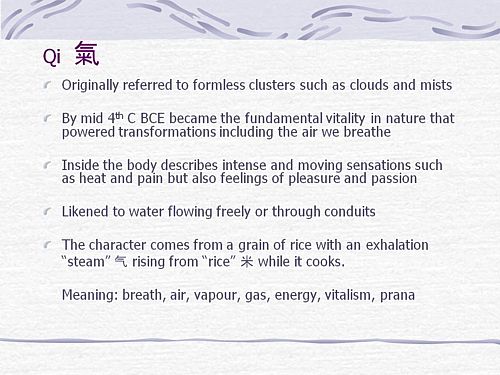
It means breath, air, vapour, gas, energy, vitalism. Or perhaps prana? Is that quite clear now?
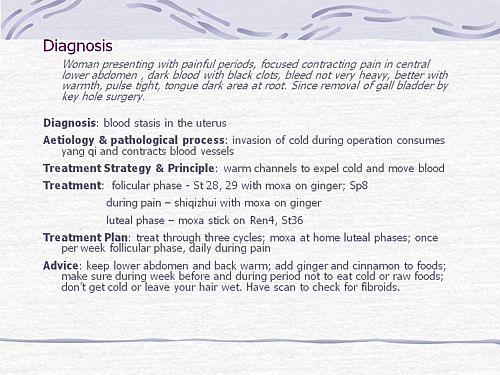
What can we make of this one? Anyone can see that the description is barely written in English and that vital information is missing (such as the age of the woman). And it’s nonsense to suggest that “invasion of cold” (during keyhole surgery!) would cause prolonged constriction of blood vessels (never mind that it would “consume yang qi”). Not being a clinician, I showed it to an oncologist friend. He said that it was impossible to tell from the description whether the problem was serious or not, but that any abdominal pain should be investigated properly. There isn’t anything here about referral for proper investigation. Just a lot of stuff about ginger and cinnamon. Anyone who was taught in this way could be a real danger to the public. It isn’t harmless nonsense It’s potentially harmful nonsense.
And finally, it’s DETOX
Surely everyone knows by now that ‘detox’ is no more than a marketing word? Well not at the University of Westminster. They have a long handout that tells you all the usual myths and a few new ones.
It is written by Jennifer Harper-Deacon, who describes herself modestly, thus.
Jennifer Harper-Deacon is a qualified and registered Naturopath and acupuncturist who holds a PhD in Natural Health and MSc in Complementary Therapies. She is a gifted healer and Reiki Master who runs her own clinic in Surrey where she believes in treating the ‘whole’ person by using a combination of Chinese medicine and naturopathic techniques that she has qualified in, including nutritional medicine, Chinese and Western herbalism, homoeopathy, applied kinesiology, reflexology, therapeutic massage, aromatherapy and flower remedies.
It seems that there is no limit on the number of (mutually incompatible) forms of nuttiness that she believes. Here are a few quotations from her handout for Westminster students.
“Detoxification is the single most powerful tool used by natural health professionals to prevent and reverse disease”
What? To “prevent and reverse” malaria? tuberculosis? Parkinson’s disease? AIDS? cancer?
“When you go on to a raw food only diet, especially fruit, the stored toxins are brought up from the deep organs such as the liver and kidneys, to the superficial systems of elimination.”;
Very odd. I always though that kidneys were a system of elimination.
“The over-use and mis-use of antibiotics has weakened the body’s ability to attack and destroy new strains of resistant bacteria, virulent viruses, which have led to our immune system becoming compromised.”
Certainly over-use and mis-use are problems. But I always thought it was the bacteria that became resistant.
“The beauty about detoxification therapy is that it addresses the very causative issues of health problems”
That is another dangerous and silly myth. Tuberculosis is not caused by mythical and un-named “toxins”. It is caused by Mycobacterium tuberculosis.
“Naturopathy follows the logic of cause and effect therefore believes that we simply need pure food and water, sunshine, air, adequate rest and sleep coupled with the right amount of exercise for health.”
Try telling that to someone with AIDS.
“Colon cleansing is one of the most important parts of any detoxification programme.”
The strange obsession with enemas in the alternative world is always baffling.
“Frankincense: holds the capacity to physically strengthen our defence system and can rebuild energy levels when our immune system is weak. Revered as a herb of protection, frankincense can also strengthen our spiritual defences when our Wei qi is low, making us more susceptible to negative energies. This calming oil has the ability to deepen the breath, helping us to let go of stale air and emotions, making it ideal oil to use inhale prior to meditating.”
This is so much hot air. There is a bit of evidence that frankincense might have some anti-inflammatory action and that’s it.
But this has to be my favourite.
“Remember when shopping to favour fruits and vegetables which are in season and locally grown (and ideally organic) as they are more vibrationally compatible with the body.”
Locally grown vegetables are “more vibrationally compatible with the body”? Pure mystical gobbledygook. Words fail me.
OK there’s a whole lot more, but that will do for now.
It’s good that Westminster is shutting down its Homeopathy BSc, but it seems they have a bit further to go.
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
BSc courses in homeopathy are closing. Is it a victory for campaigners, or just the end of the Blair/Bush era?
The Guardian carries a nice article by Anthea Lipsett, The Opposite of Science (or download pdf of print version).
Dr Peter Davies, dean of Westminster’s school of integrated health, says
“he welcomes the debate but it isn’t as open as he would like.”
Well you can say that again. The University of Westminster has refused to send me anything much, and has used flimsy excuses to avoid complying with the Freedom of Information Act. Nevertheless a great deal has leaked out. Not just amethysts emit hig Yin energy, but a whole lot more (watch this space). Given what is already in the public, arena, how can they possibly say things like this?
“Those teaching the courses insist they are academically rigorous and scientific.”
There’s another remark from an unlikely source that I can agree with too. George Lewith, of Southampton University and Upper Harley Street, is quoted as saying
“The quality of degrees is an open joke . . . ”
Whatever next? [Note: Lewith told me later that he was quoted out of context by the Guardian, so it seems that after all he is happy with the courses. So sadly I have to withdraw the credit that I was giving him].
The article emphasises nicely the view that universities that run BSc degrees in things that are fundamentally the opposite of science are deceiving young people and corrupting science itself.
Professor Petts of Westminster seems to think that the problem can be solved by putting more science into the courses The rest of the world realises that as soon as you apply science to homeopathy or naturopathy, the whole subject vanishes in a puff of smoke, I fear that Professor Petts will have to do better,
“He [DC] believes the climate is starting to change after the Bush/Blair era where people believed in things because they wished they were true. “This has been going on for a generation and it’s about time for a swing in the other direction,” he suggests.”
Well, one can always hope.
Follow-up
It is almost six months now since I posted Quackery creeps into good universities too -but through Human Resources. One example given there was the University of Leicester. This is an excellent university. It does first class research and it was the alma mater of the incomparable David Attenborough who has done more than anyone to show us the true beauty and wonder of the natural world.
Nevertheless, their well-meaning occupational health department had a section about “complementary therapies” that contained a lot of statements that were demonstrably untrue. They even recommended the utterly outrageous SCENAR device. So I pointed this out to them, and I had a quick and sympathetic response from their HR director.
But three months later, nothing had changed. Every now and then, I’d send a polite reminder, but it seemed the occupational health staff were very wedded to their quackery. The last reminder went on 6th February, but this time I copied it to Leicester’s vice-chancellor. This time it worked. There is still a link to Complementary Therapies on the Wellbeing site, but if you click on it, this is what you see.
Complementary therapiesSome employees may have an interest in complementary therapies such as acupuncture, yoga, Indian head massage, Reiki, sports & remedial massage, reflexology and hypnotherapy. If you have an interest in any of these, Staff Counselling can happily provide details of practitioners in the local area. Some of these practitioners offer discounts from their normal rates for University of Leicester staff. However, the University of Leicester cannot vouch for, or recommend any of these therapies to staff as being effective. We would urge members of staff who believe that such therapies might be effective to contact their GP prior to undertaking any of them. Further, the University of Leicester shall not be liable for any damage of any kind arising out of or related to the services of any complementary therapists or treatments listed here. If you would like further information, please contact Chris Wilson at: staffcounsel&welfare@le.ac.uk or telephone 1702. |
That’s not bad. Pity it doesn’t say alternative, rather than complementary though. Euphemisms aren’t really helpful.
In fact I have a bit of a problem with “wellbeing” too. It is a harmless word that has been highjacked so that its use now makes one think of mud baths provided by expensive hotels for their rich and gullible customers.
Leicester’s HR director wrote
“Unfortunately an instruction I had given previously had not been fully complied with. I spoke to the manager of the Staff Counselling team on Friday and gave clear instructions as to the content of this site. I had been assured that the offending information had been removed, but found that it had not.
I have now checked the site for myself and can say, with confidence, that all claims for the efficacy of complimentary [sic] therapies have been removed including SCENAR.”
The similarity between quack treatments and religion is intriguing. It seems that the devotion of the occupational health people to their baloney was so great that they wouldn’t take it down even when told to do so. The more irrational the belief, the greater the fervour with which it is defended,
What’s the lesson from this minor saga? It seems that most VCs and many HR people are too sensible to believe in alternative baloney, but that they are a bit too ready to tolerate it, perhaps on grounds of political correctness. Tolerance is a virtue, but lies about health are not in the least virtuous. If you point out that people are saying things for which there isn’t the slightest evidence, they will often respond. Just be prepared to send a few reminders.
It may also be useful to point out that some of the claims made are almost certainly illegal. Even people who care little about evidence of efficacy are impressed by the idea that they might be prosecuted by Trading Standards officers.
Who needs mystical medicine when you have real wonders like these.
(Click the google video logo for a bigger version)
Or try the pitcher plant video, or the Bird of paradise, or the Bower Bird, or the giant Amazon lilies.
Follow-up
Notice
I heard, in January 2011, that Barts has a new Dean of Education, and no longer teaches about alternative medicine in the way that has caused so much criticism in the last two years. That’s good news.
What on earth has gone wrong at the Barts and The London School of Medicine and Dentistry (SMD)?

It is not so long ago that I discovered that the very sensible medical students at Barts were protesting vigourously about being forced to mix with various quacks. A bit of investigation soon showed that the students were dead right: see St Bartholomew’s teaches antiscience, but students revolt.
Now it seems that these excellent students have not yet succeeded in educating their own Dr Mark Carroll who, ironically, has the title Associate Dean (Education Quality) in the Centre for Medical Education (SMD), specialising in all aspects of quality assurance in the SMD,
Recently this letter was sent to all medical students. They are so indignant at the way they are being treated, it didn’t take long for a copy of the letter to reach me via a plain brown email.
| Does any medical student have a particular interest in Complementary Medicine? If so, a group at Westminster University would like to contact you (see email message below) with a view to some collaborative work. Further details from Dr Mark Carroll ( m.carroll@qmul.ac.uk ).
|
A student of naturopathy? Does Mark Carroll have the slightest idea what naturopathy is (or pretends to be)? If so, why is he promoting it? If not, he clearly hasn’t done his homework.
You can get a taste of naturopathy in Another worthless validation: the University of Wales and nutritional therapy, or in Nutritional Fairy Tales from Thames Valley University.
It is a branch of quackery that is so barmy that it’s actually banned in some US states. A pharmacist was fined $1 miilion for practising it. But Barts encourages it.
Or read here about the College of Natural Nutrition: bizarre teaching revealed. They claim to cure thyroid cancer with castor oil compresses, and a holder of their diploma was fined £800 000 for causing brain damage to a patient.
I removed the name of the hapless naturopathy student, I have no wish for her to get abusive mail. It isn’t her fault that she has been misled by people who should know better. If you feel angry about this sort of thing then that should be directed to the people who mislead them. The poor student has been misled in to taking courses that teach amethysts emit high yin energy by the University of Westminster’s Vice-chancellor, Professor Geoffrey Petts, But note that Professor Petts has recently set up a review of the teaching of what he must know to be nonsense (though it hasn’t got far yet). In contrast, Dr Carroll appears to be quite unrepentant. He is the person you to whom you should write if you feel indignant.
He claims Barts is "ahead of the game". Which game? Apparently the game of leading medicine back to the dark ages and the High Street quack shop. But, Dr Carroll, it isn’t a game. Sick people are involved.
Dr Carroll is the Associate Dean (Education Quality) in the Centre for Medical Education (SMD), specialising in all aspects of quality assurance in the SMD. This has to be the ultimate irony. It’s true that the Prince of Wales approach to medicine has penetrated slightly into other, otherwise good, medical schools (for example, Edinburgh) but I’m not aware of any other that has gone so far down the road of irrationality as at Barts.
Dr Carroll, I suggest you listen to your students a bit more closely.
You might also listen to President Obama. He has just allocated $1.1 billion “to compare drugs, medical devices, surgery and other ways of treating specific conditions“. This has infuriated the drug industry and far-right talk show host Rush Limbaugh. Doubtless it will infuriate quacks too, if any of it is spent on testing their treatments properly.


