badscience
As promised in my last post about Edinburgh Napier University, I wrote to the vice-chancellor of the university, Professor Dame Joan K. Stringer DBE, BA (Hons) CertEd PhD CCMI FRSA FRSE, to invite her to respond.
|
7 February, 2011 Dear Professor Stringer, I should be grateful if you could let me know about your opinion of the degrees that you offer in Aromatherapy and Reflexology I have posted on my blog a bit of the material that was sent to me as result of recent FoI requests. See https://www.dcscience.net/?p=4049 I submit that degrees like this detract from the intellectual respectability of what is, not doubt, in other respects a good university, but since you are mentioned in the post, it’s only fair to give you the chance to defend yourself. In fact you’d be very welcome to do so publicly by commenting on the post. Best regards David Colquhoun |
Over a month later, I have received no response at all. This seems to me to be a bit discourteous.
There is nothing new in failing to get any answer to letters to vice-chancellors. The only VC who has ever thanked me for opening his eyes is Terence Kealey, of the University of Buckingham. All the rest have stayed silent. I can interpret this silence only as guilt. They know it’s nonsense, but dare not say so. Of course it isn’t infrequent for the course to close down after public exposure of the nonsense they teach. So perhaps the letters get read, even if they don’t elicit a reply.
Meanwhile the university sent me more materials that are used to teach their students. So here is another sample, largely from what’s taught to the unfortunate “reflexology” students.
Remember, these pre-scientific myths are not being taught as history or anthropology. They are taught as though they were true, to students who are then let loose on patients, so they can make money from anyone who is gullible enough to believe what they say.
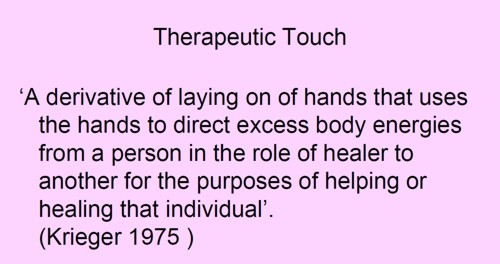
There are no "excess body energies". It’s made-up nonsense.
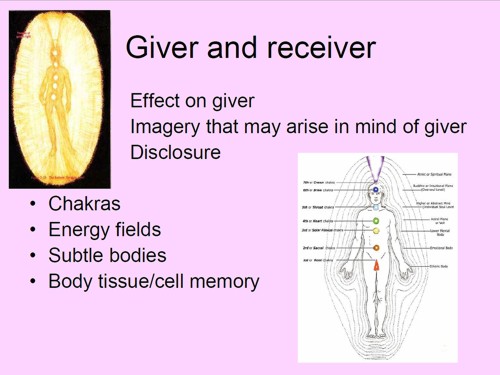
The diagram is pure imagination. It dates form a time before we knew anything about physiology, yet it is still being taught as though it meant something.
The admission that there is controversy is interesting. But it doesn’t seem to deter Napier’s teachers in the slightest.
How can anyone in the 21st century believe that the heart is "king of our emotional existence”?. That’s just preposterous pre-scientific myth,
You must be joking.
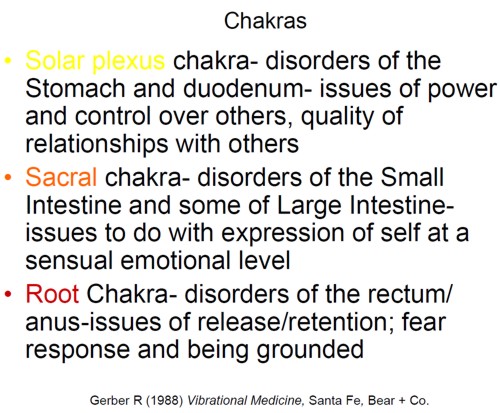
"Vibrational medicine" is a non-existent subject. Pure gobbledygook.
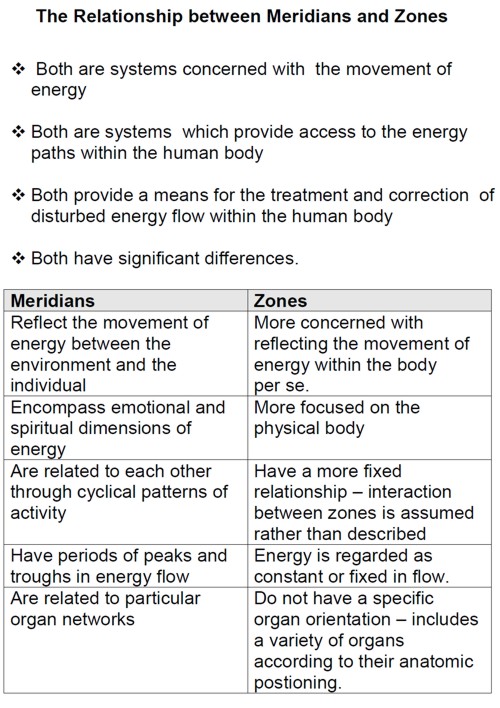
This is partly old, partly quite new. It is all preposterous made-up nonsense. There isn’t the slightest reason to think that "zones" or "meridians" exist. In fact there is good evidence from acupuncture studies to think that they don’t exist.
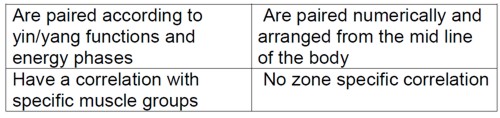
Now some slides from course CPT08102. The mention of the word ‘energy’ in the alternative world always rings alarm bells. Here’s why.
Well, it’s a good question. Pity about the answer.
Shouldn’t that read "as a practising reflexologist it is important than you have a MISunderstanding of the energy that surrounds us"?.
![]()
What logic? Have these people never heard of Hodgkin & Huxley (the answer, I imagine, is no)?
The mention of Kim Jobst immediately raises suspicions. He is a homeopath and endorser of the obviously fraudulent Q-link
pendant.
"when you as a reflexologist palpate the foot you not only produce the physical responses in the CNS but also enter the energetic body and move energy , , ". Well, no you don’t. This is purely made-up nonsense. The words sound "sciencey" but the meaning of the words is utterly obscure.
Yes we do live in an interconnected world. And sadly, that interconnectedness is used to spread myth and misinformation, usually with the aim of making money.
I guess Edinburgh Napier University makes money by teaching ancient myths as though they were true. In so doing they destroy their academic reputation.
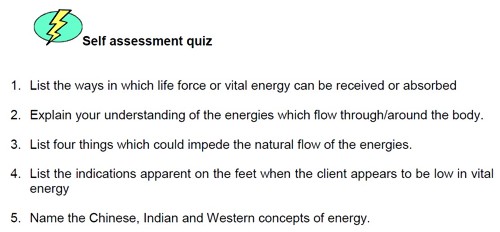
Here you are tested to see how much nonsense you have memorised successfully. If only they had sent ‘model answers’.
Remember, these pre-scientific myths are not being taught as history or anthropology. They are taught as though they were true, to students who are then let loose on patients, so they can make money from anyone who is gullible enough to believe what they say.
A 2009 systematic review of randomised controlled trials concludes that “The best evidence available to date does not demonstrate convincingly that reflexology is an effective treatment for any medical condition.”. So forget it.
How about it Professor Stringer? Isn’t it time to clean up your university?
Follow-up
I’m bored stiff with that barmiest of all the widespread forms of alternative medicine, homeopathy. It is clearly heading back to where it was in 1960, a small lunatic fringe of medicine. Nevertheless it’s worth looking at a recent development.
A paper has appeared by that arch defender of all things alternative, George Lewith.
The paper in question is “Homeopathy has clinical benefits in rheumatoid arthritis patients that are attributable to the
consultation process but not the homeopathic remedy: a randomized controlled clinical trial”, Sarah Brien, Laurie Lachance, Phil Prescott, Clare McDermott and George Lewith. [read it here]. It was published in Rheumatology.
Conclusion. Homeopathic consultations but not homeopathic remedies are associated with clinically relevant benefits for patients with active but relatively stable RA.
So yet another case where the homeopathic pills turn out the same as placebos, Hardly surprising since the pills are the same as the placebos, but it’s always good to hear it from someone whose private practice sells homeopathy for money.
The conclusion isn’t actually very novel, because Fisher & Scott (2001) had already found nine years ago that homeopathy was ineffective in reducing the symptoms if joint inflammation in RA. That is Peter Fisher, the Queens’ homeopathic physician, and Clinical Director of the Royal Hospital for Integrated Medicine (recently renamed to remove ‘homeopathy’ from its title). That paper ends with the remarkable statement [download the paper]
- "Over these years we have come to believe that conventional RCTs [randomised controlled trials] are unlikely to capture the possible benefits of homeopathy . . . . It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response."
That seemed to me at the time to amount to an admission that it was all ‘placebo effect’, though Fisher continues to deny that this is the case.
"Homeopathy has clinical benefits in rheumatoid arthritis patients" -the title says. But does it?
In fact this is mere spin. What the paper actually shows is that an empathetic consultation has some benefit (and even this is inconsistent). This is hardly surprising, but there is really not the slightest reason to suppose that the benefit, such as it is, has anything whatsoever to do with homeopathy.
Homeopathy, non-specific effects and good medicine is the title of an excellent editorial, in the same issue of Rheumatology, by Edzard Ernst. He points out that "The recognition of the therapeutic value of an empathetic consultation is by no means a new insight". Any therapy that provides only non-specific effects is unacceptable. Any good doctor provides that and, when it exists, real effective treatments too.
Lewith’s private clinic

The Centre for Complementary and Integrated Medicine is run by Drs Nick Avery and George Lewith. It is always a bit galling to real scientists, who often work 60 hours a week or more to get results, that people like Lewith get a professorial salary (in his case from the University of Southampton) but still have time to make more money by doing another job at the same time.
Avery is a homeopath. I wonder whether we can now look forward to the web site being changed in the near future so that there is a clear statement that the pills have no effect?
There is, at least, now no longer any mention of the Vega test on Lewith’s site. That is a test for food allergy that has been shown again and again to be fraudulent. The Environmental medicine page is brief, and avoids making any claims at all. It now contains the somewhat coy statement
“Specific food avoidance regimes are a controversial area and one in which there may be conflict between conventionally trained allergists and CAM practitioners.”
However the page about fibromyalgia still mentions homeopathy favourably. And it still fails to refer to my reanalysis of one of the positive trials which revealed a simple statistical mistake.
The front page of their web site boasts that "Dr George Lewith is now one of The Lifestyle 50!". " The Times, in an article on September 6th 2008, included George Lewith in The Lifestyle 50, this newspaper’s listing of the “top 50 people who influence the way we eat, exercise and think about ourselves”. Dr Lewith is included in the Alternatives category". It doesn’t mention that this is an honour he shares with such medical luminaries as Gillian ("I’m not a doctor") McKeith, Jennifer Ariston and the Pope,
But let’s end this on a happier note. There is one thing that I agree with wholeheartedly. Lewith says
"The use of bottled water seems to me to be a multi-billion pound industry, based on some of the cleverest marketing that I have ever encountered. There is absolutely no evidence that bottled water is any safer, better, or more “energising” than the water you get from the tap."
No connection of course with the multi-million pound industry of selling homeopathic water by clever marketing.
Some limitations of the paper by Brien et al.
Like any good trial, this one defined in advance a primary and secondary outcome.
The primary outcome was ACR20. which means the propertion of patients that showed an improvement of at least 20% of the number of tender and swollen joint counts and 20% improvement in 3 of the 5 remaining ACR core set measures (see Felsen 1995). Although it isn’t stressed in the paper, there was no detectable difference between consultation vs no consultation for this primary outcome.
The secondary outcome was 28-joint DAS (DAS-28), tender and swollen joint count, disease severity, pain, weekly patient
and physician GA and pain, and inflammatory markers (see, for example, Stucki. 1996). It was only on this outcome that an effect was seen between consultation and no consultation. The "effect size" (standardized mean score differences, adjusted for baseline differences) was an improvement of 0.7 in DAS-28 score, which runs on a scale from 0 – 10. Although this improvement is probably real (statistically significant), it is barely bigger than improvement of 0.6 which is said to be the smallest change that is clinically significant (Stucki. 1996).
Not only is the improvement by the consultation small in clinical terms. It is also rather inconsistent. for example Table 6 shows that the consultation seemded to result in a detectable effect on swollen joint count, but not on tender joint count. Neither was there any significant effect of the consultation on the response to “considering all the ways your arthritis affects you, please make a vertical line to show how well you are now”. There appeared to be an improvement on “negative mood score”, but not on “positive mood score”. Effects of the consultation on pain scores was marginal at best.
It seems to me that the conclusion that the consultation process helps patients, though not entirely implausible, gets marginal support from this study. It may be real, but if so it isn’t a large effect.
Like most alternative medicine advocates, the authors of this paper make the mistake of confusing caring and curing. Caring is good if there is nothing else that can be done (as is only too often the case). But what patients really want is cures and they’ll never get that from an empathetic consultation.
The problem of Human Resources
What does all this mean for alternative medicine on the NHS? Nobody denies the desirability of empathy. In fact it is now talked about so much that there is a danger that scientific medical education will be marginalised. My own experience of the NHS is that most doctors are quite good at empathy, without any need to resort to hocus pocus like homeopathy and all the myriad forms of mythical medicine.
It must be said that Drs Avery and Lewith have had proper medical training. Their views on alternative medicine seem bizarre to me, but at least they should do no great harm. Sadly, the same can’t be said for the majority of homeopaths who have no medical training and who continue to andanger the public by recommending sugar pills for anything from malaria to Dengue fever. People like that have no place in the NHS. Indeed some are in jail.
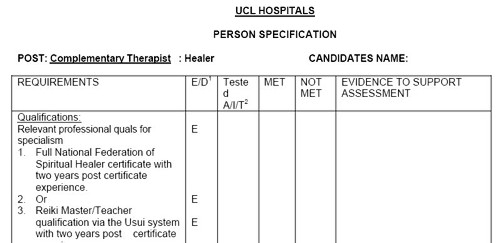
Not long ago, I was invited to tour the oncology wards at UCL hospital with their chief spiritual healer, Angie Buxton-King. Although in her private practice she offers some pretty bizarre services like healing humans and animals at a distance, I had the impression that on the wards she did a pretty good job holding hands with people who were nervous about injections and chatting to people in for their third lot of chemotherapy. I asked if she would object to being called a "supportive health care worker" rather than a spiritual healer. Somewhat reluctantly she said that she wouldn’t mind that. But it can’t be done because of the absurd box-ticking mentality of HR departments. There is no job-description for someone who holds hands with patients, and no formal qualifications. On the other hand, if you are sufficiently brainless, you can tick a box for a healer. Once again I wish that HR departments would not hinder academic integrity.
Follow-up
Steven Novella, at Science-Based medicine, has also written about this paper.
The mainstream media eventually catch up with bloggers. BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. It also exposed the uselessness of the Quality Assurance Agency (QAA). Both these things have been written about repeatedly here for some years. It was good to see them getting wider publicity.
Watch the video of the programme (Part 1, and Part 2) "Week In Week Out – University Challenged." “The programme examines how pop stars and evangelical Christians are running colleges offering courses validated by the University of Wales.” (I make a brief appearance, talking about validation of degrees in Chinese Medicine).

In October 2008 I posted Another worthless validation: the University of Wales and nutritional therapy. With the help of the Freedom of Information Act, it was possible to reveal the mind-boggling incompetence of the validation process used by the University of Wales.
McTimoney College of Chiropractic
The Chiropractic “degrees” from the McTimoney College of Chiropractic are also validated by the University of Wales by an equally incompetent, or perhaps I should say bogus, procedure. More details can be found at The McTimoney Chiropractic Association would seem to believe that chiropractic is “bogus”, and in a later post, Not much Freedom of Information at University of Wales, University of Kingston, Robert Gordon University or Napier University.
Andy Lewis has also written about chiropractic in The University of Wales is Responsible for Enabling Bogus* Chiropractic Claims to be Made.
Sadly the BBC programme did not have much to say about these domestic courses, but otherwise it was excoriating. In particular it had extensive interviews with Nigel Palastanga, whose astonishing admission that courses were validated withour seeing what was taught on them was revealed here two years ago. After that revelation, the vice-chancellor of UoW, Marc Clement BSc PhD CEng CPhys FIET FInstP, promoted Palastanga to be pro-vice-chancellor in charge of Learning, Teaching and Enhancement (I know, you couldn’t make it up).

In the documentary Palastanga said
"It’s a major business. We earn a considerable amount of money."
That was obvious two years ago, but it’s good to hear it from the horse’s mouth.
After a section that revealed a bit about what goes on at two very fundamentalist bible colleges which gave University of Wales degrees, A. C. Grayling commented thus.
"They are there to train advocates for the biblical message and that is absolutely not, by a very very long chalk, what a university should be doing.. . . A respectable British Higher education institution like the University of Wales shouldn’t be touching them with a bargepole."
Undaunted, Palastanga responded
“That’s his opinion. I would say they are validated to the highest standards. They match what are called QAA benchmark. We have serious academics looking at them, and their academic standards are established at the very highest level.”
And if you believe that, you will truly believe anything.
You can download here one of many moderator’s reports obtained under the Freedom of Information Act. This one is for the BSc (Hons) Chiropractic. It is entirely typical of theuncritical boxticking approach to validation, Nowhere does it say "subluxation is nonsense", though even the GCC now admit that.
Traditional Chinese Medicine
The University of Wales validates several courses in what almost everyone but them classifies as quackery. As well as chiropractic and “nutritional therapy”, there is herbalism. For example a course at a college in Barcelona issues University of Wales degrees in Traditional Chinese medicine, a subject that is a menace to public health.. I was asked to comment on the course, and on a bag of herbs that the presenter had been sold to treat depression.
|
Radix Bupleuri Chinensis
Radix Angelicae Sinensis Radix Paeoniae Lactiflorae Rhizoma Atractylodis Macrocephalae Sclerotium Poriae Cocos Radix Glycyrrhizae Uralensis Cortex Moutan Radicis (Paeonia Suffruticosa) Fructus Gardeniae Jasminoidis Herba Menthae Haplocalycis Zingiber officinale rhizome-fresh |
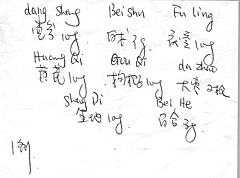 Ingredients of a custom mixture. |
There is no good evidence that any of the ingredients help depression, in fact next to nothing is known about most of them, apart from liquorice and ginger. Swallowing them would be rather reckless. They fall right into the description of any herbal medicine, in the Patients’ Guide, "Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety. "
Of the degrees, I said
"There’s no evidence that it [the herbs] does you any good. It may be dangerous because you have no idea of the dose. Degrees in Chinese Medicine consist of three years spent memorising myths and pre-scientific, er, untruths. That isn’t a degree, it’s a travesty."
Palastanga. responded
"We’ve had long debates in the Health Committee about where we would draw the line about what we validate. They have to demonstrate to us that there is some scientific basis for the practice, that there is an established curriculum, that there is an established safe practice."
The presenter asked him "So you are confident that Chinese medicine works? Palastanga replied
" I didn’t say that. I said that there is evidence that it does work . . We are trying to enforce these professions to undertake effective research."
That statement is simply not true, as shown by the response of the validation committee to the application for validation of the course in “Nutritional Therapy” at the Northern College of Acupuncture, documented previously. The fact of the matter is that the validation proceeded without looking at what was actually taught, and without even a detailed timetable of lectures. The committee looked only at the official documents presented to it and was totally negligent in failing to discover some of the bizarre beliefs of the people who were giving the course.
Palastanga went on to raise the usual straw man argument, about how little regular medicine is based on good evidence (though admittedly that is certainly true in his own field -he is a physiotherapist).
Fazley International College Kuala Lumpur

This business college in Kuala Lumpur offered University of Wales degrees. Its 32-year old president is a part time pop star with impressive looking qualifications
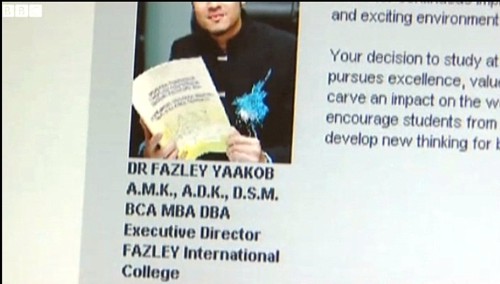
The presenter pointed out that
" His doctorate and his MBA were awarded in that citadel of education, Cambridge. Here he is, pictured at the city’s prestigious business school. He was there for all of four days and walked away with a doctorate. But the degree was not from the University of Cambridge, but from the now defunct "European Business School Cambridge". It never had the right to award degrees."
Neither the University of Wales nor the QAA had noticed this unfortunate fact. Once the TV team had done their job for them, the UoW withdrew support. though, as of 15 November 2010, that is not obvious from Fazley’s web site.
Mr (not Dr) Fazley seemed rather pleased about how students were attracted by the connection with the Prince of Wales. The fact that he is Chancellor of the University of Wales seems not inappropriate, given the amount of quackery they promote.
Quality Assurance Agency (QAA)
In 2007, I wrote, in Nature (see also here),
“Why don’t regulators prevent BSc degrees in anti-science? The Quality Assurance Agency for Higher Education (QAA) claims that “We safeguard and help to improve the academic standards and quality of higher education in the UK.” It costs taxpayers £11.5 million (US$22 million) annually. It is, of course, not unreasonable that governments should ask whether universities are doing a good job. But why has the QAA not noticed that some universities are awarding BSc degrees in subjects that are not, actually, science? The QAA report on the University of Westminster courses awards a perfect score for ‘curriculum design, content and organization,’ despite this content consisting largely of what I consider to be early-nineteenth-century myths, not science. It happens because the QAA judges courses only against the aims set by those who run the QAA, and if their aims are to propagate magic as science, that’s fine.”
That was illustrated perfectly in the documentary when Dr Stephen Jackson of the QAA appeared to try to justify the fact that the QAA had, like the University of Wales, failed entirely to spot any of the obvious problems. He had a nice dark suit, tie and poppy, but couldn’t disguise the fact that the QAA had given high ratings to some very dubious courses.
The QAA sent nine people to the other side of the globe, at a cost of £91,000. They could have done a lot better if they’d spent 10 minutes with Google at home.
Universities UK (UUK)
Needless to say, the Committee of Vice-Chancellors and Principals has said nothing at all. As usual, Laurie Taylor had it all worked out in Times Higher Education (4th November).
Speaking to our reporter Keith Ponting (30), he commended UUK’s decision to say absolutely nothing whatsoever about the abolition of all public funding for the arts and humanities.
He also praised UUK’s total silence on Lord Browne’s view that student courses should primarily be evaluated by their employment returns.
When pressed by Ponting for his overall view of UUK’s failure to respond in any way at all to any aspect of the Browne Review, he described it as “welcome evidence, in a world of change, of UUK’s consistent commitment over the years to ineffectual passivity”.
Meanwhile, a University of Wales video on YouTube
Caveat emptor
Follow-up
A couple of days later, a search of Google news for the “University of Wales” shows plenty of fallout. The vice-chancellor claims that ““The Minister’s attack came as a complete and total surprise to me”. That can’t be true. It is over two years since I told him what was going on, and if he was unaware of it, that is dereliction of duty. It is not the TV programme that brought the University into disrepute, it was the vice-chancellor.
|
Steve Jones, UCL’s star geneticist, has been commissioned by the BBC Trust to write a report on the impartiality of science journalism on the BBC. It covers both TV and radio, and all channels. Current programmes can be found by the BBC Science home page. |
|
It is not uncommon for bloggers to be critical of science reporting in the mainstream media. Now is our chance to do something constructive about it. If you have opinions about this, please leave them in the comments here, and/or email them to
Here are some of my own opinions, to get things going. Many programmes I haven’t seen/heard, so my selection may not be representative, but it is wide enough to include examples that are superb and examples of some that I think are not good enough.
Problem areas
There are two particular topics that are real problems for broadcasters. One is the whole area of alternative medicine and the ‘supplement’ industry. The other is anything to do with climate change. Both have formidable lobby groups which, to the inexperienced journalist, may sound like quite plausible scientists (some even have academic titles). Creationists can also be a problem. though not many programmes take them very seriously. Both quacks and climate deniers rarely have anything to say that is real science. They have different motivations. Examples are given below.
Many programmes are superb
David Attenbrough is an obvious example. His programmes can’t be bettered. The photography is breathtakingly beautiful and the science is always accurate. For me, they alone are worth the licence fee, and I don’t want the licence fee to be reduced. It helps that Attenborough knows the science so well. It also helps that most of the time the science isn’t very difficult and isn’t very controversial either.
There have been many other superb programmes. Steve Jones own 6-part TV series "In the blood" was a beautiful example. The fact that his comments are sought frequently by the BBC is greatly to their credit. Much depends on producers being sufficiently well-informed to know whom to ask.
More recently Brian Cox’s "Wonders" series has provided an excellent example of how science programmes can be made popular without being inaccurate,
Also excellent were Jim Al-Khalili’s Chemistry: A Volatile History and Michael Moseley’s Medical Mavericks.
Simon Singh has made consistently good programmes. His wonderful documentary on Fermat’s Last Theorem was a masterpiece.. He is a master at making programmes that make really difficult subjects accessible to the public, without making them misleading.
Tim Harford’s programm, More or Less has made a great contribution to public understanding of statistics.
Ben Goldacre‘s two part Radio 4 Programme, The Rise of the Lifestyle Nutritionists was a superb explanation of a contentious area.
It would be useful if all presenters of programmes with any scientific content had to listen to Harford or Goldacre. It might make them a bit more critical about the problem of causality that beset the observational epidemiology items that predominate among the items picked out from press releases by so many news programmes.
These programmes were so successful because they were made by people who know what they are talking about. They confirm the view that the best science programmes are made by scientists, not by journalists. There are exceptions of course. It could be argued that some of Robert Winston’s programmes have strayed too far from his area of expertise to reach the same high standards. And some journalists have produced excellent programmes. Two examples follow.
Geoff Watts has kept up a consistently high standard on Radio 4. from Science Now, through Medicine Now to Leading Edge, the standard has always been high. It is good straight science in its social context. He avoids controversies, for example his excellent programme about Charles Darwin does not include a creationist to provide (phony) ‘balance’.
After the demise of Medicine Now in 1998, Watts wrote in the BMJ thus.
In the early days of the programme you could have listened for several weeks in a row without hearing from patients. I used to defend this on the grounds that Medicine Now was there to talk about disease and its treatment, not the experience of disease and its treatment. I was wrong. To make that distinction is simply to parallel the fault for which doctors themselves take a deal of stick—being interested in the illness to the exclusion of the person who’s suffering from it. I was persuaded, reluctantly, to accept more lay voices, and I am now embarrassed that I didn’t sooner see the need for them.
The swing of the pendulum may push the whole patient experience thing too far: to a point at which it’s professional knowledge and objective analysis that is elbowed into the wings. One of the vogue concepts among BBC managers in recent years has been “accessibility”. But this is a weasel word, too easily used as justification for editing out anything that might require the audience to concentrate and think. If a patient has a rash, it’s a lot simpler for the reporter to inquire about the urge to scratch than to explore the events in the immune system that caused the skin to redden, swell, and itch in the first place. How sad if people lose an opportunity to hear from the researchers, speaking their own words, who are actually trying to find out.
This summarises a lot of the problems of science programmes. They too easily become trivial vox pops, and Watts resisted this tendency very successfully.
A great problem for programmes about medicine arises from the pressure exerted by the alternative medicine industry (ot which more later). Watts would not tolerate nonsense. He says
Medicine Now was stabled in the BBC’s Science Unit, and it was the broad acceptance of science and its methodology which shaped editorial choices. When complementary medicine was on the agenda, we expected evidence from our contributors not testaments of faith.
Material World is another good Radio 4 programme. Quentin Cooper does, on the whole, a good job. But sometimes even he falls foul of the phony balance argument After my piece in Nature on the shameful degrees in pseudo-scientific medicine got discussed on Material World, (audio here) but my opponent was not a scientist at all, but the head of “Complementary Therapies” at the University of Westminster, a man who presides over courses that teach “amethysts emit high Yin energy“. It is simply impossible to have a proper scientific discussion with people who believe nonsense like that. They don’t accept the ground rules at all. It is a good example of phony balance (see below).
Some programmes are quite bad
Alternative Medicine: the evidence. This series if three TV programmes was shown in February 2006 on BBC 2, in conjunction with the Open University. It illustrates well three problems with science programming. (1) Despite the title, tt was surprisingly weak at showing evidence, (2) It showed the defensive and unhelpful response that, only too often, the BBC shows when complaints are made. And (3) it showed that association with a university is not, per se, enough to guarantee quality.
Because of the title, I’d looked forward to this programme, and made minute by minute notes, which are recounted in BBC2 and the Open University on Alternative Medicine. It turned out that the evidence was thin on the ground, and what there was was not always accurate I complained to the BBC, but got nowhere [download my complaint and some subsequent correspondence]. I was fobbed off with defensive PR. (Much the same happened when I complained to the Open University.)
Worse still, a letter in defence of the programme that appeared in the Guardian, turned out to have been written by the BBC and was not even seen by some of its "signatories" -see .Alternative Medicine series: dirty tricks at the BBC? All this took a lot of work and got nowhere.
Simon Singh, the eminent science author, wrote two articles that exposed the very misleading portrayal of anaesthesia with acupuncture In the Guardian he wrote A groundbreaking experiment … or a sensationalised TV stunt?, and in the Daily Telegraph he wrote Did we really witness the ‘amazing power’ of acupuncture?. Singh also sent complaints to the BBC, but he persisted after the complaints were fobbed off and eventually his complaints reached the BBC Trustees. Two of his three serious complaints were upheld.
Phone-in programmes are notoriously bad for both balance and phony balance. In the alternative medicine field, equal time is always given to scientists, astrologers and crystal healers. The presenters are usually ill-informed and the callers are usually even less well informed. A particularly bad example follows.
Call You and Yours. The Radio 4 programme, You and Yours, at its best, can be quite good. It did a good job on a "snoring remedy" that I’d investigated, though it omitted some things that should, in my view, have been included. But they also have phone in versions of the programme. On 29th February 2010, they ran a phone-in programme about herbal medicine, hosted by Julian Worricker, someone who clearly was totally unaware of the controversies that surrounded this subject and, particularly, its regulation. The worst thing about this programme was that it featured a resident ‘expert’ That was Michael McIntyre who is chair of the European Herbal & Traditional Medicine Practitioners Association. McIntyre is a well known advocate of alternative medicine, who constantly fudges the need for proper evidence.
I went through the programme carefully, making detailed notes, which appear at Some truly appalling reporting of science by the BBC. It was one of the most biassed programmes on the topic I have ever heard. i sent a complaint to the BBC, referring to the detailed analysis which had already appeared here. To my dismay, they wouldn’t accept a complaint in the form. They wanted me to type the whole thing in a little box on the complaint site. where there is no formatting and no live links. I protested in vain that if they wanted a printed version, all the had to do was print the web page. At this point I decided that there was no point in spending yet more time to cope with the inflexibility of the complaints procedure.
Today programme. I’m an avid listener toToday, the best news programme on radio John Humphrys has no greater fan than I. For politics it is superb. But for science it is, sad to say, not always so good. One reason is that the presenters don’t know enough about the topics to ask the same sort of tough questions that they fire at politicians. Another reason is that they suffer badly from the phony balance problem (see below). A third reason is that they tend to pick up on silly survey press releases (the sort of ‘men with long big toes are better in bed’ pseudo-science); They may quite rightly laugh at them but this sort of thing doesn’t count as science reporting.. The Today programme is admirably serious about politics, but the science is often dumbed down and uncritical.
What needs to be done to improve BBC science
Link to the sources. Despite pressure from bloggers, the BBC web site still does not usually link to original sources, the paper on which claims are based. The whole virtue of the web is that it makes this very easy to do.
Anonymity of reporters. Too often reports of science on the BBC web site are anonymous. There is no excuse for that. Every report should carry the name and email address of the person who wrote it, Most newspapers do this, but the BBC is lagging behind.
Reaction to criticism. In most cases that I’ve tried, the reaction to constructive criticism has been obstructive and defensive. Producers seem very reluctant to admit that any mistakes were made. That needs to be changed.
Science correspondents are too often uncritical. A few more with the approach of investigative journalists would improve standards. An example is provided by a recent report “It’s good to think – but not too much, scientists say“. This is typical of the sort of work that many people find a bit hard to take seriously, but the report reads a bit like a regurgitation of press releases. There is no link to original sources and no attempt at evaluation.
Press releases. One reason for misleading reports stems from misleading press releases. Press releases often come from media departments who regard their job as getting their university into the headlinse, rather than explaining science. Worse still, sometimes the misleading hyps stems from the authors themselves (one example here, but there are hundreds to choose from). This makes it very important that science reporters should read the paper and have good enough critical faculties to read through the hype.
Complaints procedure needs to be improved. Complaints should be accepted in any form, The present web form is suitable only for short and simple criticicisms. An email address should be provided and it should accept attached documents. Certainly complaints in the form of web pages should be welcomed, because the live links provide the simplest way to refer to source documents.
The problem of phony balance. This is biggest problem of the lot.
In the wake of the report by the Science and Technology Committee (STC) on the lack of evidence for homeopathy, and the Chinese medicine poisoning, the BBC carried at least three very bad reports. Being a strong supporter of the BBC that saddens me. These cases are summarised at Some truly appalling reporting of science by the BBC. The worst was the case of Call You and Yours. There was also a totally imbalanced and ill-informed report on statutory regulation, and a very irresponsible video of a woman who claimed homeopathy cured her cancer. .
The question of balance is important. Ofcom imposes an obligation that reporting should reflect the balance of viewpoints. Section 5 of Ofcom’s broadcasting code says (emphasis is mine).
“Section 5: Due Impartiality and Due Accuracy and Undue Prominence of Views and Opinions”
“To ensure that news, in whatever form, is reported with due accuracy and presented with due impartiality.”
“Meaning of “due impartiality”: “Due” is an important qualification to the concept of impartiality. Impartiality itself means not favouring one side over another. “Due” means adequate or appropriate to the subject and nature of the programme. So “due impartiality” does not mean an equal division of time has to be given to every view, or that every argument and every facet of every argument has to be represented.”
The BBC Trust has a very similar definition of “due impartiality”.
Thus the rules stare quite explicitly that "impartial" does not mean giving equal time to any view, however batty,
In practice, though, producers often seem to play it too safe, and choose to give the same time time to the view that the earth is flat as is does to the view that the earth is spherical (OK, an oblate ellipsoid). This often gives a quite misleading impression of the state of play of informed opinion. Inappropriate use of “equal time” is the most common cause for misleading reports
on science.
Minority views should be heard of course, but they should not be given equal prominence to views that are held by the vast majority of informed people. Inevitably the worst cases arise in the areas of quack medicine, climate change and evolution.
Somebody said recently, it is as though after an air crash one gave equal time to the air accident investigator and a representative gravity-deniers association. That is scarcely an exaggeration of what happens on the BBC too often.
Worse still, far more time was given (especially on ‘Call You and Yours’) to the viewpoint that any scientist, indeed any informed person, would regard as quackery.
One thing that could be done about this false balance is to have better informed producers, or, more likely, to have better informed science reporters who can give advice on the state of opinion (and to make sure that their advice is sought).
Unless the BBC starts to be more critical in some of its reports, it could lose its preeminence. In the last few years it has become increasingly the case that the best critical evaluations of science are to be found not in the BBC or other mainstream media, but on blogs written by working scientists. Perhaps the BBC should ask them more often than it does at present.
Now give your opinions, below or email them to trust.science@bbc.co.uk
Follow-up
The Open University is a wonderful institution
I should have made it clear the Open University has played a big role in producing some of the best programmes. I was, quite rightly, corrected by a letter from an OU scientist. I’ll quote from it.
David Attenborough’s series on Life In Cold Blood, Charles Darwin and the Tree Of Life, Life – these are all Open University commissions. Life In Cold Blood also won a BAFTA and we have a string of other awards. I believe this is some of the very best science broadcasting the Open University puts out and I’m not surprised to see it at the top of your list.
More Or Less is an Open University commission – see e.g. http://www.open2.net/moreorless/
Material World is another one of our occasional commissions -see e.g. http://www.open2.net/materialworld/index.html
Geoff Watts contributed to the BBC Darwin season last year, which was heavily supported by Open University programmes.
See for example http://www.bbc.co.uk/darwin/We support the series with a considerable amount of on-line material both for credit and not for credit. This material is accessible to the public at these open2.net sites, and at http://www.open.ac.uk/openlearn/.
It is clear that the criticisms levelled at the Alternative Medicine series are very much the exception to the usual excellent work of the OU. I’m told that that programme had nothing to do with the science faculty. Clearly it was an unusual aberation. I presume it was connected with the OU’s course K221, which I wrote about in 2006, under the title Open University Quacks. That sort of thing is quite atypical of the Open University, and something of an embarrassment to the many top rate people who work there. As usual, the blame lies not with scientists but with senior managers. After hearing about course K221, I had a long correspondence with Professor David Vincent, a pro-vice chancellor. He made sympathetic noises, but did absolutely nothing. That’s par for the course with senior administrators.
The Open University has been a magnificent success from the outset. Its first vice-chancellor was Walter Laing Macdonald Perry . Before he took that job, he was professor of Pharmacology in Edinburgh (and one of my Ph.D. supervisors). He did a great job.
Failure to report negative results
A classic example of a sin of omission by the BBC (and the rest of the mainstream media too) occurred recently in the reporting of the alleged effect of B vitamins on the development of Alzheimer’s disease. A positive trial was widely reported, but two weeks later a trial appeared that measured the eight thing -cognitive deficiency – and that showed no effect at all. As far as I can tell it was barely reported at all, The details are at https://www.dcscience.net/?p=3516
There is something very offensive about the idea that a ‘bachelor of science’ degree can be awarded by a university, as a prize for memorising gobbledygook.
Once the contents of the ‘degrees’ has been exposed to public ridicule, many universities have stopped doing it. All (or nearly all) of these pseudo-degrees have closed at the University of Salford, the University of Central Lancashire, Robert Gordon University, the University of Buckingham, and even at the University of Westminster (the worst offender), one course has closed (with rumours of more to follow).
|
I’ve already written about the course in Traditional Chinese Medicine at the University of Salford (Chinese medicine -acupuncture gobbledygook revealed) and at the University of Westminster: see Why degrees in Chinese medicine are a danger to patients. The former has closed, but not the latter. Here is another one. One place that has yet to come under close scrutiny is Middlesex University. |

Michael Driscoll, VC of Middlesex University. The buck stops with him. |
Their “Complementary Health” courses are as follows (April 2010).
- Complementary Health Sciences (Ayurveda) Degree, BSc Honours
- Herbal Medicine Degree, BSc Honours
- Traditional Chinese Acupuncture Degree, BSc Honours
- Traditional Chinese Medicine Degree, BSc Honours
and also two postgraduate courses
I asked Middlesex University for samples of their teaching materials under the Freedom of Information Act, and, as usual, the request was refused. As usual, I then asked for the mandatory internal review of the decision, and this time, most unusually, the internal review did not confirm the initial refusal and I was sent a bundle of teaching materials about Chinese Herbal Medicine, It was not all I asked for, but it is quite enough to show the absurd ideas that are still being taught as part of bachelor of Science degree in a UK University.
Not only are the ideas absurd, pre-scientific, indeed antiscientific. They are also dangerous. People who have been taught this nonsense are going out and being let loose on sick people.
The vice-chancellor of Middlesex University, Professor Michael Driscoll, is an economist, not a biologist. Surely you don’t need to be a scientist to feel a bit suspicious when you read on the Middlesex web site about
Traditional Chinese Acupuncture and Moxibustion including distribution of meridians-collaterals and location of acupoints; needling and moxibustion techniques;
Have any of the members of the Executive ever thought to ask about what goes on in these courses? Even if it is beyond an economist to see through the nonsense, surely it should be possible for Professor Margaret House, Deputy Vice-Chancellor Academic, whose interests lie in water quality, should be able to, though as Dean of the School of Health and Social Sciences she appears to sponsor the nonsense. And Professor Waqar Ahmad, Deputy Vice-Chancellor Research and Enterprise, who has written a s book on Ethnicity, Health and Health Care, should surely be able to distinguish sense from nonsense in health care? In that respect, I’d have less confidence in Katie Bell, Chief Marketing Officer, who joined Middlesex University in 2009 following a career in brand marketing for Nestlé UK and GlaxoSmithKline Consumer Healthcare. Marketing people seldom have much regard for truth.
Have any of the University’s Governors ever asked what is going on in their name? It’s true that none of the long list of distinguished-sounding governors is a scientist. Surely you don’t need to be to question whether or not what follows can be described as ‘science’.
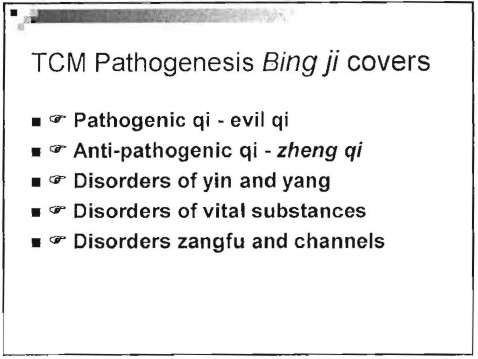
My guess is that none of these distinguished people has ever bothered to look at the dangerous nonsense that is being taught in their University. It is not in the nature of ‘managers’ to look far beyond ticked-boxes and profit, They should have done of course, but to make it easier for them, here is a small selection of the slides that I was sent (the copyright for them lies with the university: these few slides come under the heading ‘ ‘fair quotation’ and it is undoubtedly in the public interest to show them).
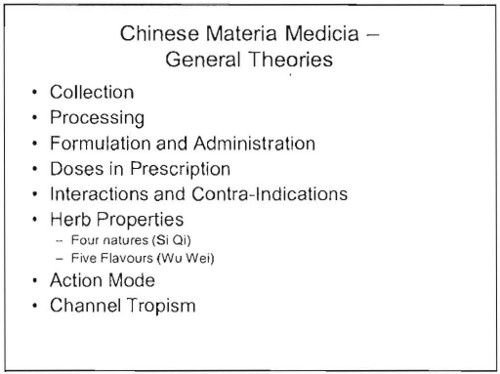
Course CMH 1211
e 
Uhuh, my spleen qi is well and truly knotted already though when I learned physiology it was not thought that the spleen had much to do with emotions.
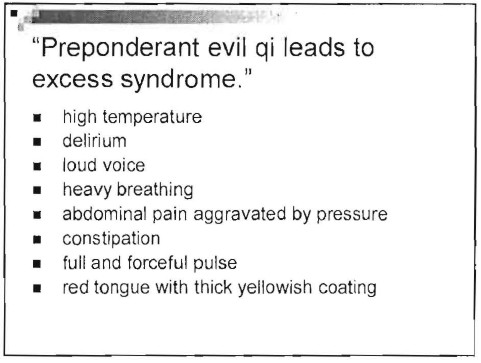
Ah so at least the problem of heavy breathers is solved. But high temperature, abdominal pain and abnormal pulse can be signs of serious illness. If your only explanation for them is “preponderant evil Qi”, you are a menace to public health.
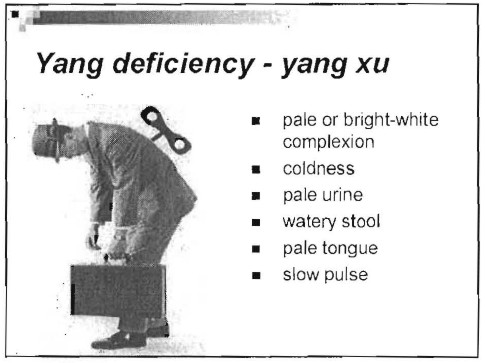
All these symptoms could be the result of a serious disease. It is not only antiquated nonsense to talk about them in terms of Yin, Yang and Qi. It endangers people,
Course CMH 2212
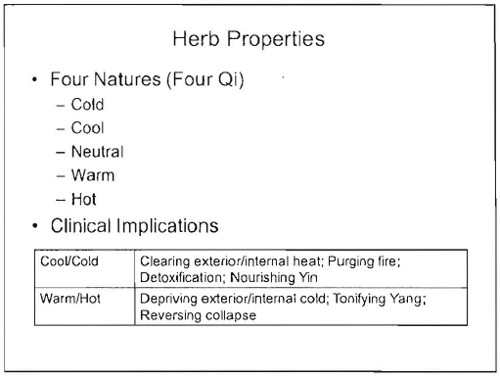
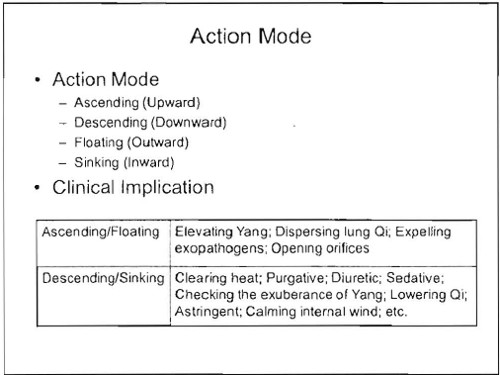
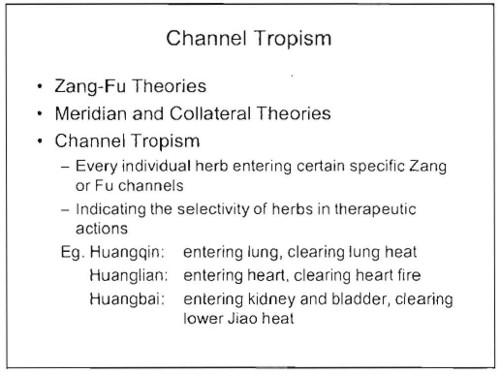
Chinese materia medica. Some of the herbs are likely to contain active ingredients (indeed some are very dangerous). It would be quite possible to study the ingredients of these herbs and to investigate how they work in the light of what has been learned about physiology and pharmacology in the last 200 years. Pharmacology has a long history of doing that, But is seems to play no part in this course. Herbs are “cold” or “hot” and may “check the exuberance of yang”.
and so on, just preposterous, made-up nonsense from another era.
If it were taught as cultural history, it might be interesting. But it is being taught as though it were true, and an appropriate way to treat sick people.
Course CMH 3214
Would you trust your child to someone who’d been taught that “causes of paediatric diseases are relatively simple”, and “children are pure yang”?
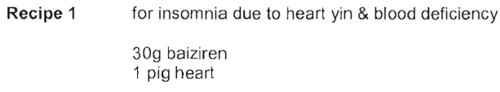
Now some Chinese recipes
Course CMH 3100
![]()
This may or may not taste good, but to recommend it for diabetes is seriously irresponsible.
The programme specification for the “BSc (Hons) Traditonal Chinese medicine” can be found here. [local copy download]
It is written with all the official trappings, just as though the degree was about science. It isn’t. It is a danger to public health.
I have asked the vice-chancellor, Michael Driscoll, to express his view of these comments
Follow-up
A rather unexpected comment from a London acupuncturist.
“At least,I knew that Professor David Colquhoun is very skeptical about Chinese medicine. he comment Chinese medicine study”not only are the ideas absurd, pre-scientific, indeed antiscientific. They are also dangerous. People who have been taught this nonsense are going out and being let loose on sick people.” “
“But,I still like to read his blog as His article very is respectable. I think. Look this…”
The skeptic blog featured this post in its weekly roundup.
27 May 2010. Times Higher Education reported the decision of Middlesex University to close its philosophy department. This department seems to have a remarkable reputation, not least for a post-1992 university. Three academics and four students have been suspended and gagged in classical bullying style.
This has happened while they continue to teach dangerous rubbish like that described above.
I left a comment at Times Higher, as follows.
It is a reflection on the quality of university management that Middlesex has chosen to shut its philosophy department while continuing to run degrees in quackery. These courses not only offer an Hons BSc for memorising chunks of anti-scientific nonsense. They also pose a real danger to patients. See https://www.dcscience.net/?p=2923
I can think of no better illustration than this of the crass nature of the judgements made by Middlesex’s management. They are either ignorant of what constitutes science, or they are corrupt. I see no other possibilities. In either case they should not be running a university.
I think Prof Michael Driscoll owes the world an explanation.
This post recounts a complicated story that started in January 2009, but has recently come to what looks like a happy ending. The story involves over a year’s writing of letters and meetings, but for those not interested in the details, I’ll start with a synopsis.
Synopsis of the synopsis
In January 2009, a course in "integrated medicine" was announced that, it was said, would be accredited by the University of Buckingham. The course was to be led by Drs Rosy Daniel and Mark Atkinson. So I sent an assessment of Rosy Daniel’s claims to "heal" cancer to Buckingham’s VC (president), Terence Kealey, After meeting Karol Sikora and Rosy Daniel, I sent an analysis of the course tutors to Kealey who promptly demoted Daniel, and put Prof Andrew Miles in charge of the course. The course went ahead in September 2009. Despite Miles’ efforts, the content was found to be altogether too alternative. The University of Buckingham has now terminated its contract with the "Faculty of Integrated Medicine", and the course will close. Well done.Buckingham.
Synopsis
- January 2009. I saw an announcement of a Diploma in Integrated Medicine, to be accredited by the University of Buckingham (UB). The course was to be run by Drs Rosy Daniel and Mark Atkinson of the College of Integrated Medicine, under the nominal directorship of Karol Sikora (UB’s Dean of Medicine). I wrote to Buckingham’s vice-chancellor (president), Terence Kealey, and attached a reprint of Ernst’s paper on carctol, a herbal cancer ‘remedy’ favoured by Daniiel.
- Unlike most vice-chancellors, Kealey replied at once and asked me to meet Sikora and Daniel. I met first Sikora alone, and then, on March 19 2009, both together. Rosy Daniel gave me a complete list of the speakers she’d chosen. Most were well-known alternative people, some, in my view, the worst sort of quack. After discovering who was to teach on the proposed course, I wrote a long document about the proposed speakers and sent it to the vice-chancellor of the University of Buckingham, Terence Kealey on March 23rd 2009.. Unlike most VCs, he took it seriously. At the end of this meeting I asked Sikora, who was in nominal charge of the course, how many of the proposed tutors he’d heard of. The answer was "none of them"
- Shortly before this meeting, I submitted a complaint to Trading Standards about Rosy Daniel’s commercial site, HealthCreation, for what seemed to me to be breaches of the Cancer Act 1939, by claims made for Carctol. Read the complaint.
- On 27th April 2009, I heard from Kealey that he’d demoted Rosy Daniel from being in charge of the Diploma and appointed Andrew Miles, who had recently been appointed as Buckingham’s Professor of Public Health Education and Policy &Associate Dean of Medicine (Public Health). Terence Kealey said "You’ve done us a good turn, and I’m grateful". Much appreciated. Miles said the course “needs in my view a fundamental reform of content. . . “
- Although Rosy Daniel had been demoted, she was still in charge of delivering the course at what had, by this time, changed its name to the Faculty of Integrated Medicine which, despite its name, is not part of the university.
- Throughout the summer I met Miles (of whom more below) several times and exchanged countless emails, but still didn’t get the revised list of speakers. The course went ahead on 30 September 2009. He also talked with Michael Baum and Edzard Ernst.
- By January 2010, Miles came to accept that the course was too high on quackery to be a credit to the university, and simply fired The Faculty of Integrated Medicine. Their contract was not renewed. Inspection of the speakers, even after revision of the course, shows why.
- As a consequence, it is rumoured that Daniel is trying to sell the course to someone else. The University of Middlesex, and unbelievably, the University of Bristol, have been mentioned, as well as Thames Valley University, the University of Westminster, the University of Southampton and the University of East London. Will the VCs of these institutions not learn something from Buckingham’s experience? It is to be hoped that they would at the very least approach Buckingham to ask pertinent questions? But perhaps a more likely contender for an organisation with sufficient gullibility is the Prince of Wales newly announced College of Integrated Medicine. [but see stop press]
The details of the story
The University of Buckingham (UB) is the only private university in the UK. Recently it announced its intention to start a school of medicine (the undergraduate component is due to start in September 2011). The dean of the new school is Karol Sikora.
Karol Sikora shot to fame after he appeared in a commercial in the USA. The TV commercial was sponsored by a far-right Republican campaign group, “Conservatives for Patients’ Rights” It designed to prevent the election of Barack Obama, by pouring scorn on the National Health Serrvice. A very curious performance. Very curious indeed. And then there was a bit of disagreement about the titles that he claimed to have.
As well as being dean of medicine at UB. Karol Sikora is also medical research director of CancerPartnersUK. a private cancer treatment company. He must be a very busy man.
Karol Sikora’s attitude to quackery is a mystery wrapped in an enigma. As well as being a regular oncologist, he is also a Foundation Fellow of that well known source of unreliable information, The Prince of Wales Foundation for Integrated Health. He spoke at their 2009 conference.
In the light of that, perhaps it is not, after all, so surprising thet the first action of UB’s medical school was to accredit a course a Diploma in Integrated Medicine. This course has been through two incarnations. The first prospectus (created 21 January 2009) advertised the course as being run by the British College of Integrated Medicine.But by the time that UB issued a press release in July 2009, the accredited outfit had changed its name to the Faculty of Integrated Medicine That grand title makes it sound like part of a university. It isn’t.

Rosy Daniel runs a company, Health Creation which, among other things, recommended a herbal concoction. Carctol. to "heal" cancer, . I wrote to Buckingham’s vice-chancellor (president), Terence Kealey, and attached a reprint of Ernst’s paper on Carctol. . Unlike most university vice-chancellors, he took it seriously. He asked me to meet Karol Sikora and Rosy Daniel to discuss it. After discovering who was teaching on this course, I wrote a document about their backgrounds and sent it to Terence Kealey. The outcome was that he removed Rosy Daniel as course director and appointed in her place Andrew Miles, with a brief to reorganise the course. A new prospectus, dated 4 September 2009, appeared. The course is not changed as much as I’d have hoped, although Miles assures me that while the lecture titles themselves may not have changed, he had ordered fundamental revisions to the teaching content and the teaching emphases.
In the new prospectus the British College of Integrated Medicine has been renamed as the Faculty of Integrated Medicine, but it appears to be otherwise unchanged. That’s a smart bit of PR. The word : “Faculty” makes it sound as though the college is part of a university. It isn’t. The "Faculty" occupies some space in the Apthorp Centre in Bath, which houses, among other things, Chiropract, Craniopathy (!) and a holistic vet,
The prospectus now starts thus.

The Advisory Board consists largely of well-know advocates of alternative medicine (more information about them below).

Most of these advisory board members are the usual promoters of magic medicine. But three of them seem quite surprising,Stafford Lightman, Nigel Sparrow and Nigel Mathers.
Stafford Lightman? Well actually I mentioned to him in April that his name was there and he asked for it to be removed, on the grounds that he’d had nothing to do with the course. It wasn’t removed for quite a while, but the current advisory board has none of these people. Nigel Sparrow and Nigel Mathers, as well as Lightman, sent letters of formal complaint to Miles and Terence Kealey, the VC of Buckingham, to complain that their involvement in Rosy Daniel’s set-up had been fundamentally misrepresented by Daniel. With these good scientists having extricated themselves from Daniel’s organisation, the FIM has only people who are firmly in the alternative camp (or quackery, as i’d prefer to call it). For example, people like Andrew Weil and George Lewith.
Andrew Weil, for example, while giving his address as the University of Arizona, is primarily a supplement salesman. He was recently reprimanded by the US Food and Drugs Administration
“Advertising on the site, the agencies said in the Oct. 15 letter, says “Dr. Weil’s Immune Support Formula can help maintain a strong defense against the flu” and claims it has “demonstrated both antiviral and immune-boosting effects in scientific investigation.”
The claims are not true, the letter said, noting the “product has not been approved, cleared, or otherwise authorized by FDA for use in the diagnosis, mitigation, prevention, treatment, or cure of the H1N1 flu virus.”
This isn’t the first time I’ve come across people’s names being used to support alternative medicine without the consent of the alleged supporter. There was, for example, the strange case of Dr John Marks and Patrick Holford.
Misrepresentation of this nature seems to be the order of the day. Could it be that people like Rosy Daniel are so insecure or, indeed, so unimportant within the Academy in real terms (where is there evidence of her objective scholarly or clinical stature?), that they seek to attach themselves, rather like limpets to fishing boats, to people of real stature and reputation, in order to boost their own or others’ view of themselves by a manner of proxy?
The background
When the course was originally proposed, a brochure appeared. It said accreditation by the University of Buckingham was expected soon.
Not much detail appeared in the brochure, Fine words are easy to write but what matters is who is doing th teaching. So I wrote to the vice-chancellor of Buckingham, Terence Kealey. I attached a reprint of Ernst’s paper on carctol, a herbal cancer ‘remedy’ favoured by Daniel (download the cached version of her claims, now deleted).
Terence Kealey
Kealey is regarded in much of academia as a far-right maverick, because he advocates ideas such as science research should get no public funding,and that universities should charge full whack for student fees. He has, in fact, publicly welcomed the horrific cuts being imposed on the Academy by Lord Mandelson. His piece in The Times started
“Wonderful news. The Government yesterday cut half a billion pounds from the money it gives to universities”
though the first comment on it starts
"Considerable accomplishment: to pack all these logical fallacies and bad metaphors in only 400 words"
He and I are probably at opposite ends of the political spectrum. Yet he is the only VC who has been willing to talk about questions like this. Normally letters to vice-chancellors about junk degrees go unanswered. Not so with Kealey. I may disagree with a lot of his ideas, but he is certainly someone you can do business with.
Kealey responded quickly to my letter, sent in January 2009, pointing out that Rosy Daniel’s claims about Carctol could not be supported and were possibly illegal. He asked me to meet Sikora and Daniel. I met first Sikora alone, and then, on March 19 2009, both together. Rosy Daniel gave me a complete list of the speakers she’d chosen to teach on this new Diploma on IM.
After discovering who was to teach on the proposed course, I wrote a long document about the proposed speakers and sent it to Terence Kealey on March 23rd 2009. It contained many names that will be familiar to anyone who has taken an interest in crackpot medicine, combined with a surprisingly large element of vested financial interests. Unlike most VCs, Kealey took it seriously.
The remarkable thing about this meeting was that I asked Sikora how many names where familiar to him on the list of people who had been chosen by Rosy Daniel to teach on the course. His answer was "none of them". Since his name and picture feature in all the course descriptions, this seemed like dereliction of duty to me.
After seeing my analysis of the speakers, Terence Kealey reacted with admirable speed. He withdrew the original brochure, demoted Rosy Daniel (in principle anyway) and brought in Prof Andrew Miles to take responsibility for the course. This meant that he had to investigate the multiple conflicts of interests of the various speakers and to establish some sort of way forward in the ‘mess’ of what had been agreed before Miles’ appointment to Buckingham
Andrew Miles.
Miles is an interesting character, a postdoctoral neuroendocrinologist, turned public health scientist. I’d come across him before as editor-in-chief of the Journal of Evaluation in Clinical Practice This is a curious journal that is devoted mainly to condemning Evidence Based Medicine. Much of its content seems to be in a style that I can only describe as post-modernist-influenced libertarian.
The argument turns on what you mean by ‘evidence’ and, in my opinion, Miles underestimates greatly the crucial problem of causality, a problem that can be solved only by randomisation, His recent views on the topic can be read here.
An article in Miles’ journal gives its flavour: "Andrew Miles, Michael Loughlin and Andreas Polychronis, Medicine and evidence: knowledge and action in clinical practice". Journal of Evaluation in Clinical Practice 2007, 13, 481–503 [download pdf]. This paper launches an attack on Ben Goldacre, in the following passage.
“Loughlin identifies Goldacre [36] as a particularly luminous example of a commentator who is able not only to combine audacity with outrage, but who in a very real way succeeds in manufacturing a sense of having been personally offended by the article in question. Such moralistic posturing acts as a defence mechanism to protect cherished assumptions from rational scrutiny and indeed to enable adherents to appropriate the ‘moral high ground’, as well as the language of ‘reason’ and ‘science’ as the exclusive property of their own favoured approaches. Loughlin brings out the Orwellian nature of this manoeuvre and identifies a significant implication.”
"If Goldacre and others really are engaged in posturing then their primary offence, at least according to the Sartrean perspective adopted by Murray et al. is not primarily intellectual, but rather it is moral. Far from there being a moral requirement to ‘bend a knee’ at the EBM altar, to do so is to violate one’s primary duty as an autonomous being.”
This attack on one of my heroes was occasioned because he featured one of the most absurd pieces of post-modernist bollocks ever, in his Guardian column in 2006. I had a go at the same paper on this blog, as well as an earlier one by Christine Barry, along the same lines. There was some hilarious follow-up on badscience.net. After this, it is understandable that I had not conceived a high opinion of Andrew Miles. I feared that Kealey might have been jumping out of the frying pan into the fire.
After closer acquaintance I have changed my mind, In the present saga Andrew Miles has done an excellent job. He started of sending me links to heaven knows how many papers on medical epistemology, to Papal Encyclicals on the proposed relationship between Faith and Reason and on more than one occasion articles from the Catholic Herald (yes, I did read it). This is not entirely surprising, as Miles is a Catholic priest as well as a public health academic, so has two axes to grind. But after six months of talking, he now sends me links to junk science sites of the sort that I might get from, ahem, Ben Goldacre.
Teachers on the course
Despite Andrew Miles best efforts, he came in too late to prevent much of the teaching being done in the parallel universe of alternative medicine, The University of Buckingham had a pre-Miles, legally-binding contract (now terminated) with the Faculty of Integrated Medicine, and the latter is run by Dr Rosy Daniel and Dr Mark Atkinson. Let’s take a look at their record.
Rosy Daniel BSc, MBBCh
Dr Rosy Daniel first came to my attention through her commercial web site, Health Creation. This site, among other things, promoted an untested herbal concoction, Carctol, for "healing" cancer.
Carctol: Profit before Patients? is a review by Edzard Ernst of the literature, such as it is, and concludes
Carctol and the media hype surrounding it must have given many cancer patients hope. The question is whether this is a good or a bad thing. On the one hand, all good clinicians should inspire their patients with hope [6]. On the other hand, giving hope on false pretences is cruel and unethical. Rosy Daniel rightly points out that all science begins with observations [5]. But all science then swiftly moves on and tests hypotheses. In the case of Carctol, over 20 years of experience in India and almost one decade of experience in the UK should be ample time to do this. Yet, we still have no data. Even the small number of apparently spectacular cases observed by Dr. Daniel have not been published in the medical literature.
On this basis I referred Health Creation to Trading Standards officer for a prima facie breach of the Cancer Act 1939. ]Download the complaint document]. Although no prosecution was brought by Trading Standards, they did request changes in the claims that were being made. Here is an example.
A Google search of the Health Creation site for “Carctol” gives a link
Dr Daniel has prescribed Carctol for years and now feels she is seeing a breakthrough. Dr Daniel now wants scientists to research the new herbal medicine
But going to the link produces
Access denied.
You are not authorized to access this page.
You can download the cached version of this page, which shows the sort of claims that were being made before Trading Standards Officers stepped in. There are now only a few oblique references to Carctol on the Health Creation site, e.g. here..
Both Rosy Daniel and Karol Sikora were speakers at the 2009 Princes’s Foundation Conference, in some odd company.
Mark Atkinson MBBS BSc (Hons) FRIPH
Dr Mark Atkinson is co-leader of the FiM course. He is also a supplement salesman, and he has promoted the Q-link pendant. The Q-link pendant is a simple and obvious fraud designed to exploit paranoia about WiFi killing you. When Ben Goldacre bought one and opened it. He found
“No microchip. A coil connected to nothing. And a zero-ohm resistor, which costs half a penny, and is connected to nothing.”
Nevertheless, Mark Atkinson has waxed lyrical about this component-free device.
“As someone who used to get tired sitting in front of computers and used to worry about the detrimental effects of external EMF’s, particularly as an avid user of mobile phones, I decided to research the various devices and technologies on the market that claim to strengthen the body’s subtle energy fields. It was Q Link that came out top. As a Q link wearer, I no longer get tired whilst at my computer, plus I’m enjoying noticeably higher energy levels and improved mental performance as a result of wearing my Q Link. I highly recommend it.” Dr Mark Atkinson, Holistic Medical Physician
Mark Atkinson is also a fan of Emo-trance. He wrote, In Now Magazine,
"I wanted you to know that of all the therapies I’ve trained in and approaches that I have used (and there’s been a lot) none have excited me and touched me so deeply than Emotrance."
"Silvia Hartmann’s technique is based on focusing your thoughts on parts of your body and guiding energy. It can be used for everything from insomnia to stress. The good news is that EmoTrance shows you how to free yourself from these stuck emotions and release the considerable amounts of energy that are lost to them."
Aha so this particular form of psychobabble is the invention of Silvia Hartmann. Silvia Hartmann came to my attention because her works feature heavily in on of the University of Westminster’s barmier “BSc” degrees, in ‘naturopaths’, described here. She is fanous, apart from Emo-trance, for her book Magic, Spells and Potions
“Dr Hartmann has created techniques that will finally make magic work for you in ways you never believed to be possible.”
Times Higher Education printed a piece with the title ‘Energy therapy’ project in school denounced as ‘psychobabble’. They’d phoned me a couple of days earlier to see whether I had an opinion about “Emotrance”. As it happens, I knew a bit about it because it had cropped up in a course given at, guess where, the University of Westminster . It seems that a secondary school had bought this extreme form of psychobabble. The comments on the Times Higher piece were unusually long and interesting.
It turned out that the inventor of “Emotrance”, Dr Silvia Hartmann PhD., not only wrote books about magic spells and potions, but also that her much vaunted doctorate had been bought from the Universal Life Church, current cost $29.99.
The rest of the teachers
The rest of the teachers on the course, despite valiant attempts at vetting by Andrew Miles, includes many names only too well-known to anybody who has taken and interest in pseudo-scientific medicine. Here are some of them.
Damien Downing:, even the Daily Mail sees through him. Enough said.
Kim Jobst, homoepath and endorser of the obviously fraudulent Q-link
pendant. His Plaxo profile says
About Kim A. Jobst
Consultant, Wholystic Care Physician [sic!] , Medical Homoeopath, Specialist in Neurodegeneration and Dementia, using food state nutrition, diet and lifestyle to facilitate Healing and Growth;
Catherine Zollman, Well known ally of HRH and purveyer of woo.
Harald Walach, another homeopath, fond of talking nonsense about "quantum effects".
Nicola Hembry, a make-believe nutritionist and advocate of vitamin C and laetrile for cancer
Simon Mills, a herbalist who is inclined to diagnoses like “hot damp”, ro be treated with herbs that tend to “cool and dry.”
David Peters, of the University of Westminster. Enough said.
Nicola Robinson of Thames Valley University. Advocate of unevidenced treatmsnts.
Michael Dixon, of whom more here.
And last but not least,
Karol Sikora.
The University of Buckingham removes accreditation of the Faculty of Integrated Medicine
The correspondence has been long and, at times, quite blunt. Here are a few quotations from it, The University of Buckingham, being private, is exempt from the Freedom of Information Act (2000) but nevertheless they have allowed me to reproduce the whole of the correspondence. The University, through its VC, Terence Keeley, has been far more open than places that are in principle subject to FOIA, but which, in practice, always try to conceal material. I may post the lot, as time permits, but meanwhile here are some extracts. They make uncomfortable reading for advocates of magic medicine.
Miles to Daniel, 8 Dec 2009
” . . . now that the University has taken his [Sikora’s] initial advice in trialing the DipSIM and has found it cost-ineffective, the way forward is therefore to alter that equation through more realistic financial contribution from IHT/FIM at Bath or to view the DipSIM as an experiment that has failed and which must give way to other more viable initiatives."
"The University is also able to confirm that we hold no interest in jointly developing any higher degrees on the study of IM with IHT/FIM at Bath. This is primarily because we are developing our own Master’s degree in Medicine of the Person in collaboration with various leading international societies and scholars including the WHO and which is based on a different school of thought. "
Miles to Daniel 15 Dec 2009
"Dear Rosy
It appears that you have not fully assimilated the content of my earlier e-mails and so I will reiterate the points I have already made to you and add to them.
The DipSIM is an external activity – in fact, it is an external collaboration and nothing more. It is not an internal activity and neither is it in any way part of the medical school and neither will it become so and so the ‘normal rules’ of academic engagement and scholarly interchange do not apply. Your status is one of external collaborator and not one of internal or even visiting academic colleague. There is no “joint pursuit” of an academically rigorous study of IM by UB and IHT/FIM beyond the DipSIM and there are no plans, and never have been, for the “joint definition of research priorities” in IM. The DipSIM has been instituted on a trial basis and this has so far shown the DipSIM to be profoundly cost-ineffective for the University. You appear to misunderstand this – deliberately or otherwise."
Daniel to Miles 13 Jan 2010
"However, I am aware that weather permitting you and Karol will be off to the Fellows meeting for the newly forming National College (for which role I nominated you to Dr Michael Dixon and Prof David Peters.)
I have been in dialogue with Michael and Boo Armstrong from FIH and they are strongly in favour of forming a partnership with FIM so that we effectively become one of many new faculties within the College (which is why we change our name to FIM some months ago).
I have told Michael about the difficulties we are having and he sincerely hopes that we can resolve them so that we can all move forward as one. "
Miles to Daniel 20 Jan 2010
"Congratulations on the likely integration of your organisation into the new College of Integrative Health which will develop out of the Prince’s Foundation for Integrated Health. This
will make an entirely appropriate home for you for the longer term.Your image of David Colquhoun "alive and kicking" as the Inquisitor General, radiating old persecutory energy and believing "priestess healers" (such as you describe youself) to be best "tortured, drowned and even burnt alive", will remain with me, I suspect, for many years to come (!). But then, as the Inquisitor General did say, ‘better to burn in this life than in the next’ (!). Overall, then, I reject your conclusion on the nature of the basis of my decision making and playfully suggest that it might form part of the next edition of Frankfurt’s recent volume ["On Bullshit] http://press.princeton.edu/titles/7929.html I hope you will forgive my injection of a little academic humour in an otherwise formal and entirely serious communication.
The nature of IM, with its foundational philosophy so vigorously opposed by mainstream medicine and the conitnuing national and international controversies which engulf homeopaths, acupuncturists, herbalists, naturopaths, transcendental meditators, therapeutic touchers, massagers, reflexologists, chiropractors, hypnotists, crystal users, yoga practitioners, aromatherapists, energy channelers, chinese medicine practitioners et al, can only bring the University difficulties as we seek to establish a formal and internationally recognised School of Medicine and School of Nursing.
I do not believe my comments in relation to governance at Bath are "offensive". They are, on the contrary, entirely accurate and of concern to the University. There have been resignations at senior level from your Board due to misrepresentation of your position and there has been a Trading Standards Authority investigation into further instances of misrepresentation. I am advised that an audit is underway of your compliance with the Authority’s instructions. You have therefore not dealt with my concerns, you have merely described them as "offensive".
I note from your e-mail that you are now in discussions with other universities and given the specific concerns of the University of Buckingham which I have dealt with exhaustively in this and other correspondences and the incompatibility of the developments at UB with the DipSIM and your own personal ambitions, etc., I believe you to have taken a very wise course and I wish you well in your negotiations. In these circumstances I feel it appropriate to enhance those negotiations by confirming that the University of Buckingham will not authorise the intake of a second cohort of students and that the relationship between IHT and the University will cease following the graduation of those members of the current course that are successful in their studies – the end of February 2011."
From Miles 2 Feb 2010
"Here is the list of teachers – you can subtract me (I withdrew from teaching when the antics ay Bath started) and also Professor John Cox (Former President of The Royal College of Psychiatrists and Former Secretary General of the World Psychiatric Association) who withdrew when he learned of some of the stuff going on…. Karol Sikora continues to teach. Michael Loughlin and Carmel Martin are both good colleagues of mine and, I can assure you – taught the students solid stuff! Michael taught medical epistemology and Carmel the emerging field of systems complexity in health services (Both of them have now withdrawn from teaching commitments).
The tutors shown are described by Rosy as the finest minds in IM teaching in the country. I interviewed tham all personally on (a) the basis of an updated CV & (b) via a 30 min telephone interview with me personally. Some were excluded from teaching because they were not qualified to do so academically (e.g. Boo Armstrong, Richard Falmer, not even a first degree, etc, etc., but gave a short presentation in a session presided over by an approved teacher) and others were approved because of their academic qualifications, PhD, MD, FRCP etc etc etc) and activity within the IM field. Each approved teacher was issued with highly specific teaching guidance form me (no bias, reference to opposing schools of thought, etc etc) and each teacher was required to complete and sign a Conflicts of Interest form. All of these documentations are with me here. Short of all this governance it’s impossible to bar them from teaching because who else would then do it?! Anyway, the end is in sight – Hallelujah! "
From Miles 19 Feb 2010
"Dear David
Just got back to the office after an excellent planning meeting for the new Master’s Degree in Person-centred Medicine and a hearty (+ alcoholic) lunch at the Ath! Since I shall never be a FRS, the Ath seems to me the next best ‘club’ (!). Michael Baum is part of the steering committee and you might like to take his thoughts on the direction of the programme. Our plans may even find their way into your Blog as an example of how to do things (vs how not to do things, i.e. CAM, IM, etc!). This new degree will sit well alongside the new degrees in Public Health – i.e. the population/utilitarian outlook of PH versus the individual person-centred approach., etc. "
And an email from a senior UB spokesperson
"Rumour has it that now that Buckingham has dismissed the ‘priestess healer of Bath’, RD [Rosy Daniel] , explorations are taking place with other universities, most of which are subject to FoI request from DC at the time of writing. Will these institutions have to make the same mistakes Buckingham did before taking the same action? Rumour also has it that RD changed the name of her institution to FIM in order to fit neatly into the Prince’s FIH, a way, no doubt, of achieving ‘protection’ and ‘accreditation’ in parallel with particularly lucrative IM ‘education’ (At £9,000 a student and with RD’s initial course attracting 20 mainly GPs, that’s £180,00 – not bad business…. And Buckingham’s ‘share of this? £12,000!”
The final bombshell; even the Prince of Wales’ FIH rejects Daniel and Atkinson?
Only today (31 March) I was sent, from a source that I can’t reveal, an email which comes from someone who "represent the College and FIH . . . ".. This makes it clear that the letter comes from the Prince of Wales’ Foundation for Integrated Health
|
Dr Rosy Daniel BSc MBBCh Director of the Faculty of Integrated Medicine Medical Director Health Creation 30th March 2010 RE: Your discussion paper and recent correspondence Thank you for meeting with [XXXXXX] and myself this evening to discuss your proposals concerning a future relationship between your Faculty of Integrated Medicine and the new College. As you know, he and I have been asked to represent the College and FIH in this matter. We are aware of difficulties facing your organisations and the FIM DipSIM course. As a consequence of these, it is not possible for the College to enter into an association with you, any of your organisations nor the DipSIM course at the present time. It would, therefore, be wrong to represent to others that any such association has been agreed. You will appreciate that, in these circumstances, you will not receive an invitation to the meeting of 15th April 2010 nor to other planned events. I am sorry to disappoint you in this matter. Yours sincerely |
Conclusions
I’ll confess to feeling almost a little guilty for having appeared to persecute the particular individuals involved in thie episode. But patients are involved and so is the law, and both of these are more important than individuals, The only unfair aspect is that, while it seems that even the Prince of Wales’ Foundation for Integrated Health has rejected Daniel and Atkinson, that Foundation embraces plenty of people who are just as deluded, and potentially dangerous, as those two. The answer to that problem is for the Prince to stop endorsing treatments that don’t work.
As for the University of Buckingham. Well, despite the ‘right wing maverick’ Kealey and the ‘anti-evidence’ Miles, I really think they’ve done the right thing. They’ve listened, they’ve maintained academic rigour and they’ve released all information for which I asked and a lot more. Good for them, I say.
Follow-up
15 April 2010. This story was reported by Times Higher Education, under the title “It’s terminal for integrated medicine diploma“. That report didn’t attract comments. But on 25th April Dr Rosy Daniel replied with “‘Terminal’? We’ve only just begun“. This time there were some feisty responses. Dr Daniel really should check her facts before getting into print.
3 March 2011. Unsurprisingly, Dr Daniel is up and running again, under the name of the British College of Integrated Medicine. The only change seems to be that Mark Atkinson has jumped ship altogether, and, of course, she is now unable to claim endorsement by Buckingham, or any other university. Sadly, though, Karol Sikora seems to have learned nothing from the saga related above. He is still there as chair of the Medical Advisory Board, along with the usual suspects mentioned above.
Every single request for information about course materials in quack medicine that I have ever sent has been turned down by universities,
It is hardly as important as as refusal of FoI requests to see climate change documents, but it does indicate that some vice-chancellors are not very interested in openness. This secretiveness is exactly the sort of thing that leads to lack of trust in universities and in science as a whole.
The one case that I have won took over three years and an Information Tribunal decision against the University of Central Lancashire (UCLAN) before I got anything.
UCLAN spent £80,307.95.(inc VAT at 17.5%) in legal expenses alone (plus heaven knows how much in staff time) to prevent us from seeing what was taught on their now defunct “BSc (Hons) homeopathy”. This does not seem to me to be good use of taxpayers’ money. A small sample of what was taught has already been posted (more to come). It is very obvious why the university wanted to keep it secret, and equally obvious that it is in the public interest that it should be seen.
UCLAN had dropped not only its homeopathy "degree" before the information was revealed, They also set up an internal inquiry into all the rest of their courses in magic medicine which ended with the dumping of all of them.
Well, not quite all, There was one left. An “MSc” in homeopathy by e-learning. Why this was allowed to continue after the findings of UCLAN’s internal review, heaven only knows. It is run by the same Kate Chatfield who ran the now defunct BSc. Having started to defend the reputation against the harm done to it by offering this sort of rubbish, I thought I should finish. So I asked for the contents of this course too. It is, after all, much the same title as the course that UCLAN had just been ordered to release. But no, this request too was met with a refusal
Worse still, the refusal was claimed under section 43(2) if the Freedom of Information Act 2000. That is the public interest defence, The very defence that was dismissed in scathing terms by the Information Tribunal less than two months ago,
To add insult to injury, UCLAN said that it would make available the contents of the 86 modules in the course under its publication scheme, at a cost of £20 per module, That comes to £1,720 for the course, Some freedom of information.
Because this was a new request, it now has to go through the process of an internal reviw of the decision before it can ne referred to the Information Commissioner. That will be requested, and since internal reviews have, so far, never changed the initial judgment. the appeal to the Information Commissioner should be submitted within the month. I have been promised that the Information Commissioner will deal with it much faster this time than the two years it took last time.
And a bit more unfreedom
Middlesex University
I first asked Middlesex for materials from their homeopathy course on 1 Oct 2008. These courses are validated by Middlesex university (MU) but actually run by the Centre for Homeopathic Education. Thw MU site barely mentions homeopathy and all I got was the usual excuse that the uninsersity did not possess the teaching materials. As usual, the validation had been done without without looking at what was actually being taught. The did send me the validation document though [download it] As usual, the validation document shows no sign at all of the fact that the usbject of the "BSc" is utter nonsense. One wonderful passage says
“. . . the Panel were assured that the Team are clearly producing practitioners but wanted to explore what makes these students graduates? The Team stated that the training reflects the professional standards that govern the programme and the graduateness is achieved through developing knowledge by being able to access sources and critically analyse these sources . . . “
Given that the most prominent characteristic of homeopaths (and other advocates of magic medicine) is total lack of critical ability, this is hilarious. If they had critical ability they wouldn’t be homeopaths. Hilarious is not quite the right word, It is tragic that nonsense like this can be found in an official university document.
Middlesex, though it doesn’t advertise homeopathy, does advertise degrees in Traditional Chinese Medicine, Herbal Medicine and Ayurveda. On 2nd February 2010 I asked for teaching materials from these courses. Guess what? The request was refused. In this case the exemptions under FOIA were not even invoked but I was told that "All these materials are presently available only in one format at the University – via a student-only accessed virtual learning environment. ". Seems that they can’t print out the bits that I asked for, The internal review has been requested, then we shall see what the Information Commissioner has to say.
Two other cases are at present being considered by the Information Commissioner (Scotland), after requests under the Scottish FoIA were refused. They are interesting cases because they bear on the decision, currently being considered by the government, about whether they should implement the recommendations of the execrable Pittilo report.
Napier University Edinburgh. The first was for teaching material form the herbal medicine course at Napier University Edinburgh. I notice that this course no longer appears in UCAS or on Napier’s own web site, so maybe the idea that its contents might be disclosed has been sufficient to make the university do the sensible thing.
Robert Gordon University Aberdeen The second request was for teaching material from the “Introduction to Homeopathy” course at the Robert Gordon University Aberdeen. The particular interest that attaches to this is that the vice-chancellor of Robert Gordon university is Michael Pittilo. The fact that he is willing to tolerate such a course in his own university seems to me to disqualify him from expressing any view on medical subjects.
Michael Pittilo, Crohn’s disease and Andrew Wakefield
Michael Pittilo has not been active in science for some time now, but Medline does show scientiifc publications for Pittilo RM, between 1979 anf 1998. Between 1989 and 1995 there are five papers published jointly with one Andrew Wakefield. These papers alleged a relationship between measles virus and Crohn’s disease. The papers were published before tha infamous 1998 paper by Wakefield in the Lancet (now retracted) that brought disgrace on Wakefield and probably caused unnecessary deaths.. The link between measles and Crohn’s disease is now equally disproved.
The subject has been reviewed by Korzenik (2005) in Past and Current Theories of Etiology of IBD. Toothpaste, Worms, and Refrigerators
“Wakefield et al proposed that Crohn’s results from a chronic infection of submucosal endothelium of the intestines with the measles virus [Crohn’s disease: pathogenesis and persistent measles virus infection. Wakefield AJ, Ekbom A, Dhillon AP, Pittilo RM, Pounder RE., Gastroenterology, 1995, 108(3):911-6]”
"This led to considerable media interest and< public concern over use of live measles vaccine as well as other vaccines. A number of researchers countered these claims, with other studies finding that titers to measles were not increased in Crohn’s patients, granulomas were not associated with endothelium 49 , measles were not in granulomas50 and the measles vaccine is not associated with an increased risk of Crohn’s disease51–55 "
This bit of history is not strictly relevant to the Pittilo report, but I do find quite puzzling how the government chooses people from whom it wishes to get advice about medical problems.
Follow-up
I notice that the Robert Gordon university bulletin has announced that
“Professor Mike Pittilo, Principal of the University, has been made an MBE in the New Year Honours list for services to healthcare”.
That is a reward for writing a very bad report that has not yet been implemented, and one hopes, for the sake of patients, will never be implemented. I do sometimes wonder about the bizarre honours system in the UK.
Postcript.
On 16th February, the death of Michael Pittilo was announced. He had been suffeing from cancer and was only 55 years old. I wouldn’t wish that fate on my worst enemy.
I don’t know about you, but I’m bored stiff with homeopathy. There are a lot more important things. Nevertheless, it remains a gross insult to reason, and there has been such enormous success in combating it over the last five years so, this is not the moment to stop.
|
Hats off to the Merseyside Skeptics Society. I admit that when I first heard about the 10:23 campaign, it seemed to be a bit of a gimmick, but in fact it turned out to be an enormous success., not just in the UK but also in Canada, Australia and New Zealand |

|
The campaign was focussed on Boots, the UK’s biggest pharmacy chain, In particular the fact that Boots sell homeopathic pills. and regularly gives appallingly bad advice about all forms of quackery that they stock.
I’ve been criticising Boots for years now, starting with Mis-education at Boots the Chemist in May 2006. was largely about homeopathy, but Boots’ quackery is not restricted to homeopathy, In November 2007, Don’t Trust Boots described Boots’ promotion of vitamin pills that were
advertised by Boots to increase your energy, and also the appallingly bad advice given by shop staff on this product.
In March 2008, Boots did it again, with a big promotion written up as Boots reaches new level of dishonesty with CoQ10 promotion. The strategy seems clear by now. Launch an enormous publicity effort, and rely on journalists to parrot the press release. Put mendacious advertisements in every newspaper. Eventually the advertisements are found to be inaccurate by the Advertising Standards Authority. Boots are told to stop using the advertisement, but suffer no penalty at all. By that time the advertising campaign is over anyway, and they can rely now on inaccurate advice from "Boots expert team"; face to face in the store, to continue the promotion in a way that evades all regulation.
Boots is deeply involved too in the great ‘detox’ scam, as recounted, for example, in “Detox”: nonsense for the gullible, along with the Prince of Wales. And, most recently, Lactium: more rubbish from Boots the Chemists. And a more serious problem.
The nauseating hypocrisy of Boots’ Corporate Social Responsibility statement beggars belief. The same stuff is repeated on the current Alliance Boots site.
“Trust – The essence of the way we do business. We are trusted because we deliver on our promises.”
You must be joking.
Who owns Boots?
Boots started in 1849 as a single shop in Nottingham. Within my lifetime, they were rather ethical pharmacies (my recollection is that they didn’t sell homeopathic pills). They were also an ethical pharmaceutical company. They developed ibuprofen, which was launched in 1969. But since then the company was involved in a complicated series of acquisitions. Now it is a supranational conglomerate with presence in 20 countries, and almost beyond the reach of the law. Boots’ executive chairman is Stefano Pessina, who, with private equity firm Kohlberg Kravis Roberts in a £11.1 billion deal last year, took the firm private in 2007. In 2008 they announced a 20% increase in profits, to £771 million In 2008 they moved their headquarters out of the UK, to Geneva, partly, it seems, so they can be closer to other giants of Big Pharma, and partly, no doubt, to put pressure on the UK government not to tax them too much, On the other hand, tax may not be a big consideration because, according to The Times, the ultimate owners of Boots are based in Gibralter
The disgraced head of HBOS, Andy Hornby, was appointed as chief executive of Alliance Boots in June 2009. Before playing his part in ruining the UK economy he used to work for grocery chain, Asda. I’d guess that he has limited interest in pharmacology.
The economics of such organisations are beyond most people. a bit like the two cow economics joke perhaps.
"VENTURE CAPITALISM – AN ICELANDIC CORPORATION
You have two cows.You sell three of them to your publicly listed company, using letters of credit opened by your brother-in-law at the bank, then execute a debt/equity swap with an associated general offer so that you get all four cows back, with a tax exemption for five cows. The milk rights of the six cows are transferred via an intermediary to a Cayman Island Company secretly owned by the majority shareholder who sells the rights to all seven cows back to your listed company. The annual report says the company owns eight cows, with an option on one more. You sell one cow to buy a new president of the United States, leaving you with nine cows. No balance sheet provided with the release. The public then buys your bull."
Clearly there is not the slightest chance of an organisation like this will have any sort of conscience about selling useless pills, The only way that they can be influenced is by public mockery of their outrageous behaviour. If the publicity harms their image enough they may decide to cut their losses, because it pays, not because it is right.
10:23 a great success
The campaign was a success because it got good coverage in the newspapers, radio and TV. Boots, rather like vice-chancellors, seems to be uninterested in reason or morals, but will certainly be sensitive about its public image, There is a partial list of coverage at the 10.23 site.
Laura Donnelly had a good account in the Telegraph, "Homeopathy: medicine that’s hard to swallow?". And Hadley Freeman in the Guardian showed that fashion journalists can spot nonsense too, in "Me and my homeopathic overdose. How I knocked back a bottle of homeopathic ‘medicine’ and lived to tell the tale"
The spoof published on the NewsArse site (despite the name, it is excellent) hit the nail on the head, because it uses exactly the naive sort of post ho ergo propter hoc argument that homoeopaths love.,
Homeopathy proven to work after overdosing protesters eventually fall asleep
Homeopathic practitioners are today claiming victory for the efficacy of their remedies, after a protest by the 10:23 group who overdosed on homeopathic sleeping pills, left each participant asleep within just 36 hours of taking the remedy.
Funniest of all though, was the bleating by homeopaths themselves. Try, for example, Homeopathy Heals. Like all the others it alleges a conspiracy by big Pharma: “it seems to be driven by those working for Pharma behind the scenes”. It seems to have escaped the attention of these conspiritorialists that the demonstration was aimed at Boots and Boots IS Big Pharma. The two are inextricably linked and both use the same tactics to increase sales.
My small contribution
Apart form contributing to Laura Donnelly’s piece in the Telegraph, "Homeopathy: medicine that’s hard to swallow?"., I had a few more calls.
Mary English, homeopath and astrologer
The most interesting was a talk show on Radio 5 live, where I was was pitted against a homeopath, Mary English [play the mp3 file, 4.4
Mb]. Having come across Mary English before, I was well-prepared to talk about her record not only in homeopathy, but also in astrology. The presenter didn’t give me time to raise these points but he did a pretty good job himself in asking her the relevant questions.
Mary English’s website is a delight. "Homeopathy and Astrology can heal you".
" If you eat a whole bottle of them it wouldn’t make any difference because it’s the dose that you have, not the quantity of the tablets"
"It’s the frequency of dose . . .because it’s vibrational medicine"
The host asked "what’s vibrational medicine?"
"it works with your bodies systems as opposed to against it"
No doubt Mary English is quite sincere, She just, like so many homeopaths, seems to be quite unaware that these words don’t mean anything at all. Just pure gobbeldygook.
Some of her claims are bizarre, even by the standards of homeopaths. She has researched the birth charts of Indigo Children, and written a book, "How to survive a Pisces" Her claim to homeopathic fame is that she has done "provings" of "remedies" including thunderstorm, and shipwreck and Stanton Drew Stone Circle, and Old Wardour Castle. Ahem, suddenly Arnica 30C sounds quite sane.
Less excusably, Mary English went on to claim that there is good evidence that homeopathy works. She just hasn’t read, or hasn’t understood the evidence. But since she earns her living as a homeopath
and astrologer, she hasn’t got much incentive to read the evidence. if she did, her income would dry up.
The presenter put directly to Mary English the recommendation of homeopathy for malaria prevention. "You wouldn’t condone that would you?". Quite disgracefully that question was avoided. She
changed the subject without answering the question. The quackometer’s classic post on The Gentle Art of Homeopathic Killing came to mind (see also here for links to full text)
Some herbal stuff
Herbal medicine rather than homeopathy was the topic of the other two weekend gigs. That arose from the Pittilo proposals for statutory regulation of herbalists and Chinese medicine.
The BBC TV interview, together with a herbalist, Rhona Edmonds, is now in YouTube. A Welsh member of the European parliament, Jill Evans (Plaid Cymru) , has been backing herbalists on the grounds that they are a “well-respected profession”. Oh yes? The Prince of Wales has also had support from another MEP. Mike Nattrass (UKIP). It seems that our fringe parties have even more trouble with science than the Labour and Conservative parties (and, tragically, that includes the Green party too).
There was also an early morning talk show interview on Sunday 31 January, against the same herbalist [play mp3 file] She claims "we treat all sorts of conditions",. Yes indeed, that’s the problem. "If we were recognised it would give the public even more confidence". And that is the problem too. They don’t deserve that confidence.
The analogy between alternative medicine and religion is often striking. Both involve blind faith, and both are characterised by tendency to split into sects that war with each other even more viciously than they war with unbelievers. All the discussions of herbalism ignore the fact that an enormous number of herbalists (2536 as of 4th February) have signed a petition opposing the idea of statutory regulation, even in the ineffective form that is being proposed.
The Prince of Wales declares war on . . . the Enlightenment
That was the headline of an article in The Times (February 4th, 2010). There can be no more high profile propagandist for every form of magic medicine than the Prince of Wales. Nothing seems to stretch his credulity. But even I was taken aback by his latest pronouncement. It seems he’s been called an enemy of the enlightenment (yes, by me among many others).
“I was accused once of being the enemy of the Enlightenment,” “I felt proud of that.”
“We cannot go on like this, just imagining that the principles of the Enlightenment still apply now. I don’t believe they do. But if you challenge people who hold the Enlightenment as the ultimate answer to everything, you do really upset them.”
So it seems he wants to return medicine not just to 1800, but to 1500, the dark ages. Can he really think that life in 1500 was some sort of utopia? Of course one suspects that his disapproval of the enlightenment is restricted to medical matters. He hasn’t been seen to reject other products of the enlightenment, like cars, aircraft, telephones, radio, TV and the internet.
I suspect that the Prince of Wales needs a history lesson.
Follow-up
Thanks to a colleague for pointing out an excellent sketch from the Newsjack show on BBC Radio 7, broadcast on 4th February 2009. [play mp3 file, 2.4 Mb]. I quote.
“Last weekend, people up and down rhe country engaged in a mass anti-homeopathy protest, swallowing whole bottles of remedies outside Boots.”
“It’s very easy to sneer at homeopathy but we at Newsjack believe it’s important to listen to both sides of the debate. So to put the case for homeopathy we have invited on a ridiculous charlatan who extorts money from innocent people while providing no services of any actual value.”
“Will you please welcome His Royal Highness, the Prince of Wales”
The Yuletide edition of the BMJ carries a lovely article by Jeffrey Aronson, Patent medicines and secret remedies. (BMJ 2009;339:b5415).
I was delighted to be asked to write an editorial about it, In fact it proved quite hard work, because the BMJ thought it improper to be too rude about the royal family, or about the possibility of Knight Starvation among senior medics. The compromise version that appeared in the BMJ is on line (full text link).
The changes were sufficient that it seems worth posting the original version (with links embedded for convenience).
The cuts are a bit ironic, since the whole point of the article is to point out the stifling political correctness that has gripped the BMA, the royal colleges, and the Department of Health when it comes to dealing with evidence-free medicine. It has become commonplace for people to worry about the future of the print media, The fact of the matter is you can often find a quicker. smarter amd blunter response to the news on blogs than you can find in the dead tree media. I doubt that the BMJ is in any danger of course. It has a good reputation for its attitude to improper drug company influence (a perpetual problem for clinical journals) as well as for clinical and science articles. It’s great to see its editor, Fiona Godlee, supporting the national campaign for reform of the libel laws (please sign it yourself).
The fact remains that when it comes to the particular problem of magic medicine, the action has not come from the BMA, the royal colleges, and certainly not from the Department of Health, It has come from what Goldacre called the “intrepid, ragged band of bloggers”. They are the ones who’ve done the investigative journalism, sent complaints and called baloney wherever they saw it. This article was meant to celebrate their collective efforts and to celebrate the fact that those efforts are beginning to percolate upwards to influence the powers that be.
It seems invidious to pick on one example, but if you want an example of beautiful and trenchant writing on one of the topics dealt with here, you’d be better off reading Andrew Lewis’s piece "Meddling Princes, Medical Regulation and Licenses to Kill” than anything in a print journal.
I was a bit disappointed by removal of the comment about the Prince of Wales. In fact I’m not particularly republican compared with many of my friends. The royal family is clearly good for the tourist industry and that’s important. Since Mrs Thatcher (and her successors) destroyed large swathes of manufacturing and put trust in the vapourware produced by dishonest and/or incompetent bankers, it isn’t obvious how the UK can stay afloat. If tourists will pay to see people driving in golden coaches, that’s fine. We need the money. What is absolutely NOT acceptable is for royals to interfere in the democratic political process. That is what the Prince of Wales does incessantly. No doubt he is well-meaning, but that is not sufficient. If I wanted to know the winner of the 2.30 at Newmarket, it might make sense to ask a royal. In medicine it makes no sense at all. But the quality of the advice is irrelevant anyway. The royal web site itself says “As a constitutional monarch, the Sovereign must remain politically neutral.”. Why does she not apply that rule to her son? Time to put him over your knee Ma’am?
Two of the major bits that were cut out are shown in bold, The many other changes are small.
BMJ editorial December 2009
Secret remedies: 100 years onTime to look again at the efficacy of remedies Jeffrey Aronson in his article [1] gives a fascinating insight into how the BMA, BMJ and politicians tried, a century ago, to put an end to the marketing of secret remedies. They didn’t have much success. The problems had not improved 40 years later when A.J. Clark published his book on patent medicines [2]. It is astounding to see how little has changed since then. He wrote, for example, “On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”> Clark himself was sued for libel after he’d written in a pamphlet “ ‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”. Although he initially tried to fight the case, impending destitution eventually forced him to apologise [3]. If that happened today, the accusation would have been repeated on hundreds of web sites round the world within 24 hours, and the quack would, with luck, lose [4]. As early as 1927, Clark had written “Today some travesty of physical science appears to be the most popular form of incantation” [5]. That is even more true today. Homeopaths regularly talk utter nonsense about quantum theory [6] and ‘nutritional therapists’ claim to cure AIDS with vitamin pills or even with downloaded music files. Some of their writing is plain delusional, but much of it is a parody of scientific writing. The style, which Goldacre [7] calls ‘sciencey’, often looks quite plausible until you start to check the references. A 100 years on from the BMA’s efforts, we need once again to look at the efficacy of remedies. Indeed the effort is already well under way, but this time it takes a rather different form. The initiative has come largely from an “intrepid, ragged band of bloggers” and some good journalists, helped by many scientific societies, but substantially hindered by the BMA, the Royal Colleges, the Department of Health and a few vice-chancellors. Even NICE and the MHRA have not helped much. The response of the royal colleges to the resurgence in magic medicine that started in the 1970s seems to have been a sort of embarrassment. They pushed the questions under the carpet by setting up committees (often populated with known sympathizers) so as to avoid having to say ‘baloney’. The Department of Health, equally embarrassed, tends to refer the questions to that well-known medical authority, the Prince of Wales (it is his Foundation for Integrated Health that was charged with drafting National Occupational Standards in make-believe subjects like naturopathy [8]. Two recent examples suffice to illustrate the problems. The first example is the argument about the desirability of statutory regulation of acupuncture, herbal and traditional Chinese medicine (the Pittilo recommendations) [9]. Let’s start with a definition, taken from ‘A patients’ guide to magic medicine’ [10]. “Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety”. It seems to me to be self-evident that you cannot start to think about a sensible form of regulation unless you first decide whether what you are trying to regulate is nonsense, though this idea does not seem to have penetrated the thinking of the Department of Health or the authors of the Pittilo report. The consultation on statutory regulation has had many submissions [11] that point out the danger to patients of appearing to give official endorsement of treatments that don’t work. The good news is that there seems to have been a major change of heart at the Royal College of Physicians. Their submission points out with admirable clarity that the statutory regulation of things that don’t work is a danger to patients (though they still have a blank spot about the evidence for acupuncture, partly as a result of the recent uncharacteristically bad assessment of the evidence by NICE [12]). Things are looking up. Nevertheless, after the public consultation on the report ended on November 16th, the Prince of Wales abused his position to make a well-publicised intervention on behalf of herbalists [13]. Sometimes I think his mother should give him a firm lesson in the meaning of the term ‘constitutional monarchy’, before he destroys it. The other example concerns the recent ‘evidence check: homeopathy’ conducted by the House of Commons Science and Technology Select Committee (SCITECH). First the definition [10]: “Homeopathy: giving patients medicines that contain no medicine whatsoever”. When homeopathy was dreamt up, at the end of the 18th century, regular physicians were lethal blood-letters, and it’s quite likely that giving nothing saved people from them. By the mid-19th century, discoveries about the real causes of disease had started, but homeopaths remain to this day stuck in their 18th century time warp. In 1842 Oliver Wendell Holmes said all that needed to be said about medicine-free medicine [14]. It is nothing short of surreal that the UK parliament is still discussing it in 2009. Nevertheless it is worth watching the SCITECH proceedings [15]. The first two sessions are fun, if only for the statement by the Professional Standards Director of Boots that they sell homeopathic pills while being quite aware that they don’t work. I thought that was rather admirable honesty. Peter Fisher, clinical director of the Royal Homeopathic Hospital, went through his familiar cherry-picking of evidence, but at least repeated his condemnation of the sale of sugar pills for the prevention of malaria. But for pure comedy gold, there is nothing to beat the final session. The health minister, Michael O’Brien, was eventually cajoled into admitting that there was no good evidence that homeopathy worked but defended the idea that the taxpayer should pay for it anyway. It was much harder to understand the position of the chief scientific advisor in the Department of Health, David Harper. He was evasive and ill-informed. Eventually the chairman, Phil Willis, said “No, that is not what I am asking you. You are the Department’s Chief Scientist. Can you give me one specific reference which supports the use of homeopathy in terms of Government policy on health?”. But answer came there none (well, there were words, but they made no sense). Then at the end of the session Harper said “homeopathic practitioners would argue that the way randomised clinical trials are set up they do not lend themselves necessarily to the evaluation and demonstration of efficacy of homeopathic remedies, so to go down the track of having more randomised clinical trials, for the time being at least, does not seem to be a sensible way forward.” Earlier, Kent Woods (CEO of the MHRA) had said “the underlying theory does not really give rise to many testable hypotheses”. These two eminent people seemed to have been fooled by the limp excuses offered by homeopaths. The hypotheses are testable and homeopathy, because it involves pills, is particularly well suited to being tested by proper RCTs (they have been, and when done properly, they fail). If you want to know how to do it, all you have to do is read Goldacre in the Guardian [16]. It really isn’t vert complicated. “Imagine going to an NHS hospital for treatment and being sent away with nothing but a bottle of water and some vague promises.” “And no, it’s not a fruitcake fantasy. This is homeopathy and the NHS currently spends around £10million on it.” That was written by health journalist Jane Symons, in The Sun [17]. A Murdoch tabloid has produced a better account of homeopathy than anything that could be managed by the chief scientific advisor to the Department of Health. And it isn’t often that one can say that. These examples serve to show that the medical establishment is slowly being dragged, from the bottom up, into realising that matters of truth and falsehood are more important than their knighthoods. It is all very heartening, both for medicine and for democracy itself. David Colquhoun. Declaration of interests. I was A.J. Clark chair of pharmacology at UCL, 1985 – 2004. 1. Aronson, JK BMJ 2009;339:b5415 2. Clark, A,J, (1938) Patent Medicines FACT series 14, London. See also Patent medicines in 1938 and now https://www.dcscience.net/?p=257 3. David Clark “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3) 4. Lewis, A. (2007) The Gentle Art of Homeopathic Killing 5. A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927 6. Chrastina, D (2007) Quantum theory isn’t that weak, (response to Lionel Milgrom). 7 Goldacre, B. (2008) Bad Science. HarperCollins 8. Skills for Health web site 9. A very bad report: gamma minus for the vice-chancellor 10. A Patients’ Guide to Magic Medicine, and also in the Financial Times. 12. NICE fiasco, part 2. Rawlins should withdraw guidance and start again 13. BBC news 1 December 2009 Prince Charles: ‘Herbal medicine must be regulated’. 14. Oliver Wendell Holmes (1842) Homeopathy and Its Kindred Delusions. 15. House of Commons Science and technology committee. Evidence check: homeopathy. Videos and transcripts available at http://www.viewista.com/s/fywlp2/ez/1 16. Goldacre, B. A Kind of Magic Guardian 16 November 2007. 17. Homeopathy is resources drain says |
Follow-up
There is a good account of the third SCITECH session by clinical science consultant, Majikthyse, at The Three Amigos.
16 December 2009.. Recorded an interview for BBC Radio 5 Live. It was supposed to go out early on 17th.
17 December 2009. The editorial is mentioned in Editor’s Choice, by deputy editor Tony Delamothe. I love his way of putting the problem "too many at the top of British medicine seem frozen in the headlights of the complementary medicine bandwagon". He sounds remarkably kind given that I was awarded (by the editor, Fiona Godlee, no less) a sort of booby prize at the BMJ party for having generated a record number of emails during the editing of a single editorial (was it really 24?). Hey ho.
17 December 2009. More information on very direct political meddling by the Prince of Wales in today’s Guardian, and in Press Association report.
17 December 2009. Daily Telegraph reports on the editorial, under the heading “ ‘Nonsense’ alternative medicines should not be regulated“. Not a bad account for a non-health journalist.
17 December 2009. Good coverage in the excellent US blog, Neurologica, by the superb Steven Novella.’ “Intrepid, Ragged Band of Bloggers” take on CAM‘ provides a chance to compare and contrast the problems in the UK and the USA.’
18 December 2009. Article in The Times by former special advisor, Paul Richards. “The influence of Prince Charles the lobbyist is out of hand. Our deference stops us asking questions.”
“A good starting point might be publication of all correspondence over the past 30 years. Then we will know the extent, and influence, of Prince Charles the lobbyist.”
Comments in the BMJ Quite a lot of comments had appeared by January 8th, though sadly they were mostly from the usual suspects who appear every time one suggests evidence matters. A reply was called for, so I sent this (the version below has links).
After a long delay, this response eventually appeared in the BMJ on January 15 2010.
It’s good to see so many responses, though somewhat alarming to see that several of them seem to expect an editorial to provide a complete review of the literature. I ‘ll be happy to provide references for any assertion that I made.
I also find it a bit odd that some people think that an editorial is not the place to express an opinion robustly. That view seems to me to be a manifestation of the very sort of political correctness that I was deploring. It’s a bit like the case when the then health minister, Lord Hunt, referred to psychic surgery as a “profession” when he should have called it a fraudulent conjuring trick. Anything I write is very mild compared with what Thomas Wakley wrote in the Lancet, a journal which he founded around the time UCL came into existence. For example (I quote)
“[We deplore the] “state of society which allows various sets of mercenary, goose-brained monopolists and charlatans to usurp the highest privileges…. This is the canker-worm which eats into the heart of the medical body.” Wakley, T. The Lancet 1838-9, 1
I don’t think it is worth replying to people who cite Jacques Benveniste or Andrew Wakefield as authorities. Neither is it worth replying to people who raise the straw man argument about wicked pharmaceutical companies (about which I am on record as being as angry as anyone). But I would like to reply directly to some of the more coherent comments.
Sam Lewis and Robert Watson. [comment] Thank you for putting so succinctly what I was trying to say.
Peter Fisher [comment]. I have a lot of sympathy for Peter Fisher. He has attempted to do some good trials of homeopathy (they mostly had negative outcomes). He said he was "very angry" when the non-medical homeopaths were caught out recommending their sugar pills for malaria prevention (not that this as stopped such dangerous claims which are still commonplace). He agreed with me that there was not sufficient scientific basis for BSc degrees in homeopathy. I suppose that it isn’t really surprising that he continues to cherry pick the evidence. As clinical director of the Royal London Homeopathic Hospital and Homeopathic physician to the Queen, just imagine the cognitive dissonance that would result if he were to admit publicly that is all placebo after all. He has come close though. His (negative) trial for homeopathic treatment of rheumatoid arthritis included the words "It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response” [2]. [download
the paper]. When it comes to malaria, it matters a lot.
Adrian White [comment] seems to be cross because I cited my own blog. I did that simply because if he follows the links there he will find the evidence. In the case of acupuncture it has been shown time after time that "real" acupuncture does not differ perceptibly from sham. That is true whether the sham consists of retractable needles or real needles in the "wrong" places. A non-blind comparison between acupuncture and no acupuncture usually shows some advantage for the former but it is, on average, too small to be of much clinical significance [3]. I agree that there is no way to be sure that this advantage is purely placebo effect but since it is small and transient it really doesn’t matter much. Nobody has put it more clearly than Barker Bausell in his book, Snake Oil Science [4]
White also seems to have great faith in peer review. I agree that in real science it is probably the best system we have. But in alternative medicine journals the "peers" are usually other true believers in whatever hocus pocus is being promoted and peer reveiw breaks down altogether.
R. M. Pittilo [comment] I’m glad that Professor Pittilo has replied in person because I did single out his report for particular criticism. I agree that his report said that NHS funding should be available to CAM only where there is evidence of efficacy. That was not my criticism. My point was that in his report, the evidence for efficacy was assessed by representatives of Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Every one of them would have been out of work if they had found their subjects were nonsense and that, no doubt, explains why the assessment was so bad. To be fair, they did admit that the evidence was not all that it might be and recommended (as always) more research I’d like to ask Professor Pittilo how much money should be spent on more research in the light of the fact that over a billion dollars has been spent in the USA on CAM research without producing a single useful treatment. Pittilo says "My own view is that both statutory regulation and the quest for evidence should proceed together" but he seems to neglect the possibility that the quest for evidence might fail. Experience in the USA suggests that is exactly what has, to a large extent, already happened.
I also find it quite absurd that the Pittilo report should recommend, despite a half-hearted admission that the evidence is poor, that entry to these subjects should be via BSc Honours degrees. In any case he is already thwarted in that ambition because universities are closing down degrees in these subjects having realised that the time to run a degree is after, not before, you have some evidence that the subject is not nonsense. I hope that in due course Professor Pittilo may take the same action about the courses in things like homeopathy that are run by the university of which he is vice-chancellor. That could only enhance the academic reputation of Robert Gordon’s University.
George Lewith [comment] You must be aware that the proposed regulatory body, the Health Professions Council, has already broken its own rules about "evidence-based practice" by agreeing to take on, if asked, practitioners of Herbal Medicine, Chinese Medicine and Acupuncture. They have (shamefully) excluded the idea that claims of efficacy would be regulated. In other word they propose to provide exactly the sort of pseudo-regulation which would endanger patients They are accustomed to the idea that regulation is to do only with censoring practitioners who are caught in bed with patients. However meritorious that may be, it is not the main problem with pseudo-medicine, an area in which they have no experience. I’m equally surprised that Lewith should recommend that Chinese evaluation of Traditional Chinese medicine should be included in meta-analyses, in view of the well-known fact that 99% of evaluations from China are positive: “No trial published in China or Russia/USSR found a test treatment to be ineffective” [5]. He must surely realise that medicine in China is a branch of politics. In fact the whole resurgence in Chinese medicine and acupuncture in post-war times has less to do with ancient traditions than with Chinese nationalism, in particular the wish of Mao Tse-Tung to provide the appearance of health care for the masses (though it is reported that he himself preferred Western Medicine).
1. Lord Hunt thinks “psychic surgery” is a “profession”. https://www.dcscience.net/?p=258
2. Fisher, P. Scott, DL. 2001 Rheumatology 40, 1052 – 1055. [pdf file]
3. Madsen et al, BMJ 2009;338:a3115 [pdf file]
4. R, Barker Bausell, Snake Oil Science, Oxford University Press, 2007
5. Vickers, Niraj, Goyal, Harland and Rees (1998, Controlled Clinical Trials, 19, 159-166) “Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials”. [pdf file]
15 January 2010. During the SciTech hearings, Kent Woods (CEO of the MHRA) made a very feeble attempt to defend the MHRA’s decision to allow misleading labelling of homeopathic products. Now they have published their justification for this claim. It is truly pathetic, as explained by Martin at LayScience: New Evidence Reveals the MHRA’s Farcical Approach to Homeopathy. This mis-labelling cause a great outcry in 2006, as documented in The MHRA breaks its founding principle: it is an intellectual disgrace, and Learned Societies speak out against CAM, and the MHRA.
22 January 2010 Very glad to see that the minister himself has chosen to respond in the BMJ to the editorial
|
Rt Hon. Mike O’Brien QC MP, Minister of State for Health Services I am glad that David Colquhoun was entertained by my appearance before the Health Select Committee on Homeopathy. But he is mistaken when he says, “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense.” Regulation is about patient safety. Acupuncture, herbal and traditional Chinese medicine involve piercing the skin and/or the ingestion of potentially harmful substances and present a possible risk to patients. The Pittilo Report recommends statutory regulation and we have recently held a public consultation on whether this is a sensible way forward. Further research into the efficacy of therapies such as Homeopathy is unlikely to settle the debate, such is the controversy surrounding the subject. That is why the Department of Health’s policy towards complementary and alternative medicines is neutral. Whether I personally think Homeopathy is nonsense or not is besides the point. As a Minister, I do not decide the correct treatment for patients. Doctors do that. I do not propose on this occasion to interfere in the doctor-patient relationship. |
Here is my response to the minister
|
I am very glad that the minister himself has replied. I think he is wrong in two ways, one relatively trivial but one very important. First, he is wrong to refer to homeopathy as controversial. It is not. It is quite the daftest for the common forms of magic medicine and essentially no informed person believes a word of it. Of course, as minister, he is free to ignore scientific advice, just as the Home Secretary did recently. But he should admit that that is what he is doing, and not hide behind the (imagined) controversy. Second, and far more importantly, he is wrong, dangerously wrong, to say it I was mistaken to claim that “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense". According to that view it would make sense to grant statutory regulation to voodoo and astrology. The Pittilo proposals would involve giving honours degrees in nonsense if one took the minister’s view that it doesn’t matter whether the subjects are nonsense or not. Surely he isn’t advocating that? The minister is also wrong to suppose that regulation, in the form proposed by Pittilo, would do anything to help patient safety. Indeed there is a good case to be made that it would endanger patients (not to mention endangering tigers and bears). The reason for that is that the main danger to patients arises from patients being given “remedies” that don’t work. The proposed regulatory body, the Health Professions Council, has already declared that it is not interested in whether the treatments work or not. That in itself endangers patients. In the case of Traditional Chinese Medicine, there is also a danger to patients from contaminated medicines. The HPC is not competent to deal with that either. It is the job of the MHRA and/or Trading Standards. There are much better methods of ensuring patient safety that those proposed by Pittilo. In order to see the harm that can result from statutory regulation, it is necessary only to look at the General Chiropractic Council. Attention was focussed on chiropractic when the British Chiropractic Association decided, foolishly, to sue Simon Singh for defamation. That led to close inspection of the strength of the evidence for their claims to benefit conditions like infant colic and asthma. The evidence turned out to be pathetic, and the result was that something like 600 complaints were made to the GCC about the making of false health claims (including two against practices run by the chair of the GCC himself). The processing of these complaints is still in progress, but what is absolutely clear is that the statutory regulatory body, the GCC, had done nothing to discourage these false claims. On the contrary it had perpetrated them itself. No doubt the HPC would be similarly engulfed in complaints if the Pittilo proposals went ahead. It is one thing to say that the government chooses to pay for things like homeopathy, despite it being known that they are only placebos, because some patients like them. It is quite another thing to endanger patient safety by advocating government endorsement in the form of statutory regulation, of treatments that don’t work. I would be very happy to meet the minister to discuss the problems involved in ensuring patient safety. He has seen herbalists and other with vested interests. He has been lobbied by the Prince of Wales. Perhaps it is time he listened to the views of scientists too. |
Both the minister’s response, and my reply, were reformatted to appear as letters in the print edition of the BMJ, as well as comments on the web..
A momentous decision was promulgated (as lawyers say) by the Information Tribunal on December 8th 2009. It marks a step forward in Freedom of Information about how universities spend your money. It has taken 3.5 years to get to this point. Perhaps now there will be an end to the attempts of every single university that I’ve
approached to conceal what they teach.
Decision
"The Tribunal upholds the decision notice dated 30th. March, 2009, dismisses the appeal and directs that all the steps required by the Decision Notice be taken within 28 days of the date of this Decision"
Back story for this case
24th July 2006. I asked the University of Central Lancashire (UCLAN) for copies of teaching materials and validation documents for their "BSc" degree in homeopathy (this degree no longer exists: it was abolished in 2008). A year later, UCLAN shut the rest of its courses in alternative medicine, after an internal review.
21 August 2006. I was sent the validation documents but refused the teaching materials as UCLAN claimed they were exempt under section 43(2) of the Freedom of Information Act (FOIA)(commercial interests). Two days later I sent a request for the mandatory internal review of the refusal.
4th October 2006. The internal review confirmed the original decision (it always does), and cited, as well as section .43(2) of FOIA, section 21.
21 October 2006. I appealed to the Information Commissioner. The basis of the appeal was that the university might have financial interests in the outcome, but not commercial interests, because universities are not commercial organisations as defined in section 43(2) of the FOIA. In addition, even if the commercial argument was not allowed, the public interest in knowing what was taught was sufficient to justify release of the requested materials.
21 January 2008. The Information Commissioner finally got round to starting on the case.
29 September 2008 The vice-chancellor, Malcolm McVicar, raised an objection to complying with my request under s.36(2)(c) of FOIA. This states that “In the reasonable opinion of a qualified person, disclosure of the information under this Act” “(c) would otherwise prejudice, or would be likely otherwise to prejudice, the effective conduct of public affairs..”
30 March 2009. The decision of the Information Commissioner was published. It has already been described here. Apart from one trivial matter, my appeal was upheld, and UCLAN was ordered to release the requested material within 35 days. However UCLAN did not release the material, but rather launched an appeal against the Information Commissioner. The appeal was heard by an Information Tribunal.
The full text of the Freedom of Information Act is here.
The Information Tribunal
The Tribunal heard the case of University of Central Lancashire v Information Commissioner in Manchester on November 3, 4 and 5. I was an ‘additional party’ to the proceedings and attended in person for the first two days, with the aim of helping the Information Commissioner’s case. This is what the tribunal looked like.
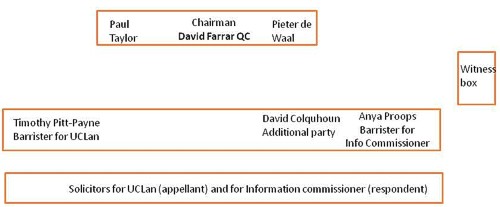
I was amazed to find myself sitting next to the barrister for the Information Commisioner, and still more amazed to be invited to cross-question the witnesses, after she had questioned them.
The witnesses were Malcom McVicar (vice-chancellor of UCLAN), Peter Hyett, (executive director of finance at UCLAN) and David Phoenix (Deputy vice-chancellor, UCLAN).
The outcome
The decision in full can be read here.
|
Decision The Tribunal upholds the decision notice dated 30th. March, 2009, dismisses the appeal and directs that all the steps required by the Decision Notice be taken within 28 days of the date of this Decision. |
So we won.
The details of the decision contain some matters of great interest for universities, in particular the dismissal of the idea that the public can be reassured by either internal or external (e.g. QAA) validation procedures. I’ll try to summarise them (paragraph numbering as in the decision
notice).
Commercial interests
The one disappointing thing about the Tribunal’s decision was that it contradicted the Information Commissioner’s decision on the meaning of commercial interests.
31 "Therefore, whether on a broad or narrow construction of the statutory words, we are satisfied that UCLAN `s interests in teaching material produced for its degree courses are properly described as “commercial”.
However, that does not affect the outcome because the Tribunal decided that there was no reason to think that the course materials actually had the commercial value that UCLAN said they did. For
example:
36 We were not impressed by the claim that third parties with copyright in the disclosed materials would be alienated by UCLAN `s compliance with a decision that this information must be provided. None gave evidence to that effect.
37 It was not clear to us how a competitor could significantly exploit access to this material, without infringing UCLAN `s copyright or brazenly aping the content of a course, which would surely attract the scorn of the wider academic community. Moreover, it seemed to us likely that most potential students would be attracted to a particular course by the reputation of the teaching staff and a range of extra – curricular factors at least as much as by a comparative study of the powerpoint presentations and notes provided to current students.
and
39 Finally, in this particular case, we doubt whether this course had a significant commercial value, given the limited enrolment and the virtual absence of overseas interest.
At this point, the appeal is essentially dismissed. Nevetheless, the Tribunal went on to discuss the other defences offered by UCLAN, and some of their conclusions are more interesting than the subtle distinction between ‘financial interests’ and ‘commercial interests’.
40 In the light of this finding, it is not strictly necessary to decide the balance of public interest as to disclosure. Nevertheless, since the issue has been carefully and very fully argued, we shall shortly indicate our view, had the likelihood of prejudice been established.
Public Interest
The commercial interest defence is subject to the public interest argument in s.1(2((b) of the FOIA’
(b) in all the circumstances of the case, the public interest in maintaining the exclusion of the duty to confirm or deny outweighs the public interest in disclosing whether the public authority
holds the information.
Hence, the decision notice says
41 As ever, the question is whether the public interest in maintaining the exemption outweighs the interest in disclosure.
On the question of public interest, the Tribunal comes down strongly on the side of the Commissioner and me.
46 The public interest in disclosure seems to us appreciably stronger. Apart from the universal arguments about transparency and the improvement of public awareness, we find that there are particular interests here, arising from the nature of a university and the way it is funded.
It is particularly interesting that the Tribunal dismissed the role of internal and external validation as a substitute for transparency. As part of their case (para 18) UCLAN had argued
"Moreover, standards were ensured by the validation procedures which were required before a course was launched and which involved independent expert external monitors and by quality assurance (Q.A.A.) which demands a continuing compliance with national standards."
This cut no ice with the Tribunal. In one of his few direct interjections the Tribunal Chairman, David Farrar Q.C., questioned a witness directly about the internal validation processes, Evidently he was not impressed by the answers. During my own cross questioning of the deputy vice-chancellor, I put to him the view that since the QAA [Quality Assurance Agency] was not allowed to take any notice of the content of courses, that getting a high mark from the QAA was not a substitute for seeing what was actually taught. The deputy vice-chancellor did not seem to disagree strongly with that view.
47 First, the public has a legitimate interest in monitoring the content and the academic quality of a course, particularly a relatively new course in a new area of study, funded, to a very significant extent, by the taxpayer. It is no answer, we consider, to say that this function is performed by the process of validation or the continuing monitoring of standards with external input. Whether or not these processes are conducted with critical rigour, it must be open to those outside the academic community to question what is being taught and to what level in our universities. The apparent perception in some quarters that the intellectual demands of some or many degree courses have been relaxed, that higher classes of degree are too lightly earned, may be largely or entirely unfounded. But it is highly important that the material necessary to a fair judgement be available. That material will often, if not always, include the basic content of the course, such as is requested here.
48 Secondly, this is especially the case where, as with the BSc. (Homeopathy), there is significant public controversy as to the value of such study within a university. In this case, that factor standing alone would have persuaded us that the balance of public interest favoured disclosure.
49 We are not attracted by the somewhat patrician argument that the general public, uninstructed in the specialist subject under scrutiny, would be incapable of forming a proper judgement. That might be so, were it impossible to seek independent expertise to assist in making an assessment. Happily, it is not.
50 Finally, there is a public interest in opening up new methods of teaching and new insights as to the content of courses, so as to stimulate the spread of good practice.
So, a hands down win on the public interest argument.
Prejudice to effective conduct of public affairs
I found incomprehensible the argument that disclosure would ‘prejudice the effective conduct of public affairs’. But it was raised (at the last minute) by UCLAN, and it was considered by the Tribunal. This defence refers to s.36(2)(c) of FOIA. It states that “In the reasonable opinion of a qualified person, disclosure of the information under this Act” “(c) would otherwise prejudice, or would be likely otherwise to prejudice, the effective conduct of public affairs..”
As noted at paragraph 17, it is common ground, established as to (iii), by the jurisprudence of the Tribunal, that this exemption is engaged if three requirements are met. They can be shortly labelled
(i) qualified person
(ii) reasonable opinion
(iii) reasonably arrived at.
The Tribunal seemed to be distinctly unimpressed by the arguments presented by UCLAN.
56 A reasonable opinion may be one with which the Tribunal emphatically disagrees, provided it is based on sound argument and evidence. With great respect to Professor McVicar, whose sincerity is not in question, we can find no adequate evidential basis for this opinion and consider that it rests on two misconceptions as to the application of FOIA. We do not find that it passes the required test of objective reasonableness.
57 We considered separately whether the opinion was reasonably arrived at. Again, our answer is no.
58 Section 36 provides for an exceptional exemption which the public authority creates by its own action, albeit subject to scrutiny of its reasonableness, the likelihood of prejudice and the question of the public interest. That factor of itself justifies a requirement that the authority provide substantial evidence as to the advice (other than legal advice) and the arguments presented to the qualified person upon which his opinion was founded. We emphasise that no set formula is required, just a simple clear record of the process.
59 The need for such evidence is all the greater where, as here, the authority invokes s.36 for the first time after the complaint to the IC [Information Commissioner].
60 The evidence consists of a briefly argued email from Dr. Bostock suggesting that s.36(2)(c) be invoked on the very broadly argued grounds already reviewed. The tone implicitly acknowledges that the claim is rather speculative. We are not concerned with the slightly uncertain use of possibility and likely but the impression left is of a last minute idea, not really thought through or investigated
but merely discussed with solicitors to tie it in to the FOIA. It was sent to the Vice Chancellor at 3.20pm. on a Friday afternoon, 26th. September, 2008, asking for the Vice Chancellor’s agreement. That agreement was forthcoming in a single sentence without further comment in an email reply timed at 12.05pm.on the following Monday.61 We find that the process of forming the necessary opinion was, to say the least, perfunctory, indeed far short of the careful assessment and investigation that normally supports a qualified opinion for the purposes of s.36.
62 Accordingly, we do not find that it was reasonably arrived at.
Conclusion
62 It is for these reasons that we uphold the Decision Notice. We record our gratitude for the helpful and succinct submissions of counsel on both sides and the incisive contribution of Professor Colquhoun. We wish to add that, whilst we have not accepted the great majority of the arguments advanced by UCLAN, we do not in any way seek to cast doubt on the veracity of the evidence of its witnesses, nor the honesty and loyalty with which they have sought to serve its interests.
63 Our decision is unanimous.
Signed David Farrar Q.C.
Watch this space to see what can now be revealed.
Follow-up
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
Chiropractors are getting very touchy indeed, all over the world. And no wonder, because their claims are being exposed as baseless as never before, in the wake of their attempts to stifle criticism by legal action..
In March, Shaun Holt appeared on Breakfast TV in New Zealand. Holt has done a lot of good work on TV in debunking some of the preposterous claims made by quacks. See him on YouTube.
This time he talked about chiropractic. Here is the video.
One could argue that he was over generous to chiropractic, especially when talking about their effectiveness in treating low back pain. He said, quite rightly, that chiropractors are no better than physiotherapists at treating low back pain.
But a recent trial suggests that neither are much good. “A randomised controlled trial of spinal manipulative therapy in acute low back pain” (Juni et al., 2009 in the BMJ; see also coverage in Pulse). This trial compared standard care with standard care plus spinal manipulative therapy (SMT). The results were negative, despite the fact that this sort of A + B vs B design is inherently biassed in favour of the treatment (see A trial design that generates only ”positive” results, Ernst & Lee 2008, Postgrad Med J.).
"SMT was performed by a specialist in manual medicine, chiropractice and rheumatology (GH), a specialist in physical medicine (DV) or an osteopath (RvB), all proficient in SMT."
"Conclusions: SMT is unlikely to result in relevant early pain reduction in patients with acute low back pain."
Admittedly, the trial was quite small (104 patients, 52 in each group) so it will need to be confirmed. but the result is entirely in line with what we knew already.
It also adds to the evidence that the recommendation by NICE of SMT by chiropractors constitutes their biggest failure ever to assess evidence properly. If NICE don’t amend this advice soon, they are in danger of damaging their hitherto excellent record.
Despite the moderate tone and accuracy of what Holt said on TV, the New Zealand Chiropractors’ Association made a formal complaint. That is what they like to do, as I learned recently, to my cost. It is so much easier than producing evidence.
Quite absurdly the New Zealand Broadcasting Standards Authority (BSA) has upheld some of the complaints. Their judgement can be read here.
The BSA consists of four people, two lawyers and two journalists. So not a trace of scientific expertise among them. Having people like that judging the claims of chiropractors makes as much sense as having them judged by Mr Justice Eady. They seem to be the sort of people who think that if there is a disagreement, the truth must lie half-way between the opposing views.
One of the BSA members, Tapu Misa, has used her newspaper column to quote approvingly the views of the notorious Dr Mercola web site on flu prevention “Your best defence, it says, is to eat right, get lots of sleep, avoid sugar and stress, load up on garlic, Vitamin D and krill oil”. (Snake oil is said to be good too.) There are some odd attitudes to science in some of her other columns too (e.g. here and here). Not quite the person to be judging the evidence for and against chiropractic, I think.
In fact the TV show in question was more than fair to chiropractors. It adopted the media’s usual interpretation of fair and balanced: equal time for the flat earthers. A Chiropractor was invited to reply to Holt’s piece. Here he is.
The chiropractor, Doug Blackbourn, started very plausibly, though a tendency to omit every third syllable made transcription hard work. He established that if you cut yourself you get better (without any help). He established that nerves run down the spinal cord. So far, so good. But then he quickly moved on to the usual flights of fancy.
"We have two premises. The body heals itself and the nervous system runs the body. Now the nervous system runs the body, travels down through the spinal cord so chiropractic is not based on the belief that, you know, energy flows, it’s based on the fact that your nervous system runs the body and [inaudible] affects the overall health of the body"
This statement is totally vague. It has nothing whatsoever to do with the main question, can chiropractors do anything useful. It is sheer flannel.
We’re seeing people, heck, diabetes. I had a quadriplegic come in one time for adjustment, we’ve got stroke people, we’ve got all sorts of conditions. We’re not treating the condition, We’re allowing, checking the spine to see if there’s any interference there that will slow the body down"
“Interference”? “slowing the body down”? These are utterly meaningless phrases that simply serve to distract from the only question that matters.
"Chiropractice is the most safest [sic] profession to go to to get your spine adjusted"
Hmm I thought it was the only job that uses the word ‘adjustment’.
Worst of all was his response to a question about asthma.
Presenter: "So chiropractors are not out there claiming they will cure asthma for example?". Chiropractor: "No"
This is simply untrue, both in New Zealand and in the UK. For a start, just look at what Blackbourn’s own web site says about asthma.
"The challenge, of course, with allergy and asthma medication is there is no end-point. There is no cure. Asthma and allergies, for the most part, are lifelong conditions requiring lifelong medication. Might there be a better way, an alternative solution?
“Alternative” is the key word. Medical treatment is designed to combat symptoms, and is successful to a certain extent with allergies and asthma. Underlying causes are not addressed, however, and symptoms continue year after year. What else might be done?
Enter chiropractic care. Chiropractic health care, with its unique comprehensive approach, is able to offer positive benefit to a variety of conditions and ailments. In the case of allergies and asthma, these “hypersensitivity conditions” may respond well to therapy designed to normalize the body’s flow of nerve signals. To use a metaphor, chiropractic treatment removes roadblocks to the body’s natural healing abilities. Restoring these imbalances may help reduce such hypersensitivity reactions."
Blackbourn’s web site describes him thus
"As a Doctor of Chiropractic, Dr. Doug Blackbourn . . ."
But the qualifications of “Dr” Blackbourn are B.App.Sc (Chiro) M.N.Z.C.A , the same as those of “Dr” Brian Kelly.
After a performance like this, perhaps someone should submit a complaint to the New Zealand Broadcasting Standards Authority.
After all, I notice that they have dismissed complaints from one chiropractor, Sean Parker, after a TV programme looked at the business practices of his private chiropractic practice, The Spinal Health Foundation. Perhaps the BSA understands business better than it understands science.
Follow-up
Is chiropractic crumbling in New Zealand? The New Zealand College of Chiropractic featured in my editorial in the New Zealand Medical Journal, and in the fallout from that article, It’s principle, “Dr” Brian Kelly (B App Sci (Chiro)) seems to be getting desperate. His college is now canvassing for recruits in Canada. They are promised all the woo.
- Subluxation centered techniques – Gonstead, Toggle Recoil, Thompson, Diversified
- Traditional philosophy featuring vitalism and innate healing – congruent curriculum
Perhaps Canada is a good place to recruit, gven the $500 million class action being brought against chiropractors in Canada, after Sandra Nette became tetraplegic immediately after a chiropractor manipulated her neck, Canadian chiropractors must be looking for somewhere to hide.
Stuff and Nonsense. jdc described this story at the time the complaint was lodged.
Shaun Holt’s own blog follows the action.
New Zealand Doctor covers the story.
Bay of Plenty Times “Bay researcher slams television complaint ruling“
In July 2008 I wrote an editorial in the New Zealand Medical Journal (NZMJ), at the request of its editor.
The title was Dr Who? deception by chiropractors. It was not very flattering and it resulted in a letter from lawyers representing the New Zealand Chiropractic Association. Luckily the editor of the NZMJ, Frank Frizelle, is a man of principle, and the legal action was averted. It also resulted in some interesting discussions with disillusioned chiropractors that confirmed one’s worst fears. Not to mention revealing the internecine warfare between one chiropractor and another.
This all occurred before the British Chiropractic Association sued Simon Singh for defamation. The strength of the reaction to that foolhardy action now has chiropractors wondering if they can survive at all. The baselessness of most of their claims has been exposed as never before. No wonder they are running scared. The whole basis of their business is imploding.
Needless to say chiropractors were very cross indeed. Then in February 2009 I had a polite email from a New Zealand chiropractor, David Owen, asking for help to find one of the references in the editorial. I’d quoted Preston Long as saying
"Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
And I’d given the reference as
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10
I’d found the quotation, and the reference, in Ernst’s 2005 article, The value of Chiropractic, but at the time I couldn’t find the Journal of Quality Healthcare. I did find the same article on the web. At least the article had the same title, the same author and the same quotation. But after finding, and reading, the article, I neglected to change the reference from J Quality Health Care to http://skepticreport.com/sr/?p=88. I should have done so and for that I apologise.
When I asked Ernst about the Journal of Quality Healthcare, he couldn’t find his copy of the Journal either, but he and his secretary embarked on a hunt for it, and eventually it was found.

![]()
|
It turns out that Journal of Quality Healthcare shut down in 2004, without leaving a trace on the web, or even in the British Library. It was replaced by a different journal, Patient Safety and Quality Healthcare (PSQH) A reprint was obtained from them. It is indeed the same as the web version that I’d read, and it highlighted the quotation in question. The reprint of the original article, which proved so hard to find, can be downloaded here. |
|
The full quotation is this
"Sixty-two clinical neurologists from across Canada, all certified members of the Royal College of Physicians and Surgeons, issued a warning to the Canadian public, which was reported by Brad Stewart, MD. The warning was entitled Canadian Neurologists Warn Against Neck Manipulation. The final conclusion was that endless non-scientific claims are being made as to the uses of neck manipulation(Stewart, 2003). They need to be stopped. The public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45."
I have often condemned the practice of citing papers without reading them (it is, of course, distressingly common), so I feel bad about this, though I had in fact read the paper in question in its web version. I’m writing about it because I feel one should be open about mistakes, even small ones.
I’m also writing about it because one small section of the magic medicine community seems to think they have nailed me because of it. David Owen, the New Zealand chiropractor, wrote to the editor of the NZMJ, thus.
|
The quote [in question] is the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45. Long PH. Stroke and Manipulation. J Quality Health Care. 2004:3:8-10 This quote actually comes from the following blog article http://www.skepticreport.com/medicalquackery/strokespinal.htm [DC the URL is now http://skepticreport.com/sr/?p=88] I have attached all my personal communications with Colquhoun. They demonstrate this is not a citation error. Prof Colquhoun believes the origin of the quote doesn’t matter because Long was quoting from a Canadian Neurologists’ report (this is also incorrect). As you can see he fails to provide any evidence at all to support the existance [sic] of the “J Quality Health Care.” Colquhoun ‘s belief that my forwarding this complaint is me “resorting to threats” is the final nail in the coffin. If he had any leg to stand on where is the threat? This may seem pedantic but it surely reflects a serious ethical breach. Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility? Incidentally, at the end of the article, conflicts of interest are listed as none. As Colquhoun is a Professor of Pharmacology and much of his research funding no doubt comes from the pharmaceutical industry how can he have no conflict of interest with therapies that do not advocate the use of drugs and compete directly against the billions spent on pain medications each year? If I may quote Colquhoun himself in his defence of his article (Journal of the New Zealand Medical Association, 05-September-2008, Vol 121 No 1281) I’ll admit, though, that perhaps ‘intellect’ is not what’s deficient in this case, but rather honesty. David Owen |
Financial interests
Well, here is a threat: I’m exposed as a shill of Big Pharma. ". . . much of his funding no doubt comes from the pharmaceutical industry". I can’t count how many times this accusation has been thrown at me by advocates of magic medicine. Oddly enough none of them has actually taken the trouble to find out where my research funding has come from. None of them even knows enough about the business to realise the extreme improbability that the Pharmaceutical Industry would be interested in funding basic work on the stochastic properties of single molecules. They fund only clinicians who can help to improve their profits,
The matter of funding is already on record, but I’ll repeat it now. The media ‘nutritional therapist’, Patrick Holford, said, in the British Medical Journal
“I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry “
To which my reply was
” Oh dear, Patrick Holford really should check before saying things like “I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry”. Unlike Holford, when I said “no competing interests”, I meant it. My research has never been funded by the drug industry, but always by the Medical Research Council or by the Wellcome Trust. Neither have I accepted hospitality or travel to conferences from them. That is because I would never want to run the risk of judgements being clouded by money. The only time I have ever taken money from industry is in the form of modest fees that I got for giving a series of lectures on the basic mathematical principles of drug-receptor interaction, a few years ago.”
I spend a lot of my spare time, and a bit of my own money, in an attempt to bring some sense into the arguments. The alternative medicine gurus make their livings (in some cases large fortunes) out of their wares.
So who has the vested interest?
Does chiropractic actually cause stroke?
As in the case of drugs and diet, it is remarkably difficult to be sure about causality. A patient suffers a vertebral artery dissection shortly after visiting a chiropractor, but did the neck manipulation cause the stroke? Or did it precipitate the stroke in somebody predisposed to one? Or is the timing just coincidence and the stroke would have happened anyway? There has been a lot of discussion about this and a forthcoming analysis will tackle the problem of causality head-on,
My assessment at the moment, for what it’s worth, is that there are some pretty good reasons to suspect that neck manipulation can be dangerous, but it seems that serious damage is rare.
In a sense, it really doesn’t matter much anyway, because it is now apparent that chiropractic is pretty well discredited without having to resort to arguments about rare (though serious) effects. There is real doubt about whether it is even any good for back pain (see Cochrane review), and good reason to think that the very common claims of chiropractors to be able to cure infant colic, asthma and so on are entirely, ahem, bogus. (See also Steven Novella, ebm-first, and innumerable other recent analyses.)
Chiropractic is entirely discredited, whether or not it may occasionally kill people.
Complaint sent to UCL
I had an enquiry about this problem also from my old friend George Lewith. I told him what had happened. Soon after this, a complaint was sent to Tim Perry and Jason Clarke, UCL’s Director and Deputy Director of Academic Services. The letter came not from Lewith or Owen, but from Lionel Milgom. Milgrom is well known in the magic medicine community for writing papers about how homeopathy can be “explained” by quantum entanglement. Unfortunately for him, his papers have been read by some real physicists and they are no more than rather pretentious metaphors. See, for example, Danny Chrastina’s analysis, and shpalman, here. Not to mention Lewis, AP Gaylard and Orac.
|
Dear Mr Perry and Mr Clark, I would like to bring to your attention an editorial (below) that appeared in the most recent issue of the New Zealand Medical Journal. In it, one of your Emeritus Professors, David Colquhoun, is accused of a serious ethical breach, and I quote – “Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility?” Professor Colquhoun is well-known for writing extensively and publicly excoriating many forms of complementary and alternative medicine, particularly with regard to the alleged unscientific nature and unethical behaviour of its practitioners. Professor Colquhoun is also a voluble champion for keeping the libel laws out of science. While such activities are doubtlessly in accord with the venerable Benthamite liberal traditions of UCL, I am quite certain hypocrisy is not. And though Professor Colquhoun has owned up to his error, as the NZMJ’s editor implies, it leaves a question mark over his credibility. As custodians of the college’s academic quality therefore, you might care to consider the possible damage to UCL’s reputation of perceived professorial cant; emeritus or otherwise. Yours Sincerely Dr Lionel R Milgrom |
So, as we have seen, the quotation was correct, the reference was correct, and I’d read the article from which it came I made a mistake in citing the original paper rather than the web version of the same paper..
I leave it to the reader to judge whether this constitutes a "serious ethical breach", whether I’d slipped in an "unsupported statement", and whether it constitutes "hypocrisy"
Follow-up
It so happens that no sooner was this posted than there appeared Part 2 of the devastating refutation of Lionel Milgrom’s attempt to defend homeopathy, written by AP Gaylard. Thanks to Mojo (comment #2) for pointing this out.
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
This post has been translated into Belorussian..
Chinese medicine and herbal medicine are in the news at the moment. There is a real risk that the government could endorse them by accepting the Pittilo report.
In my view traditional Chinese medicine endangers people. The proposed ‘regulation’ would do nothing to protect the public. Quite on the contrary, it would add to the dangers, by giving an official stamp of approval while doing nothing for safety.
The government’s idea of improving safety is to make sure that practitioners are ‘properly trained’. But it is the qualifications that cause the danger in the first place. The courses teach ideas that are plain wrong and often really dangerous.
Why have government (and some universities) not noticed this? That’s easy to see. Governments, quangos and university validation committees simply don’t look. They tick boxes but never ask what actually goes on. Here’s some examples of what goes on for them to think about. They show clearly the sort of dangerous rubbish that is taught on some of these ‘degrees’.
These particular slides are from the University of Westminster, but similar courses exist in only too many other places. Watch this space for more details on courses at Edinburgh Napier University, Middlesex University and the University of East London
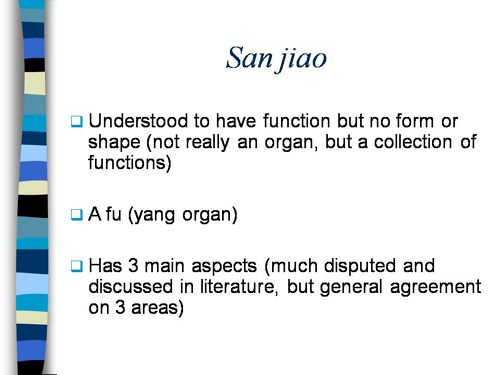
Just a lot of old myths. Sheer gobbledygook,
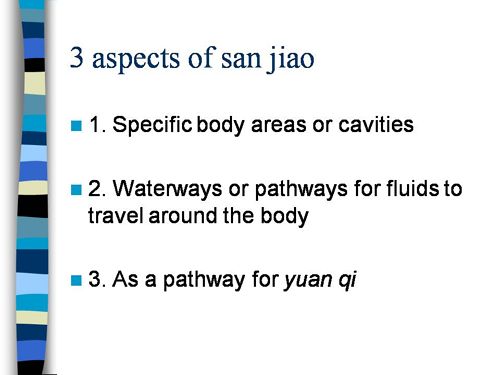
SO much for a couple of centuries of physiology,
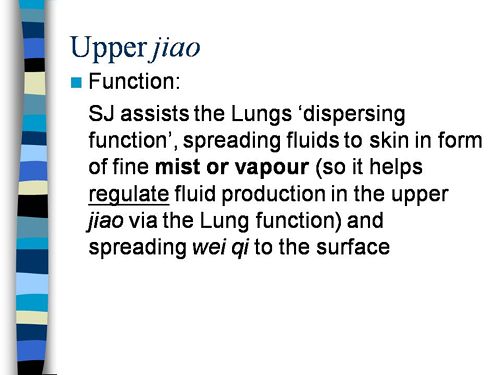
It gets worse.
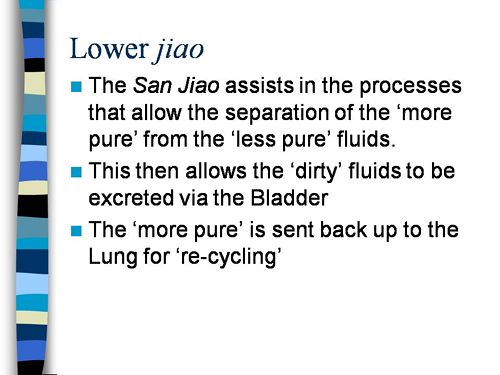
Plain wrong.
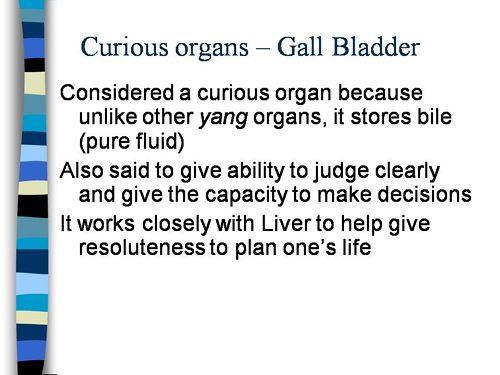
Curious indeed. The fantasy gobbledygook gets worse.
Now it is getting utterly silly. Teaching students that the brain is made of marrow is not just absurd, but desperately dangerous for anyone unlucky (or stupid) enough to go to such a person when they are ill.
Here’s another herbal lecture., and this time the topic is serious. Cancer.
Herbal approaches for patients with cancer.
I’ve removed the name of the teacher to spare her the acute embarrassment of having these dangerous fantasies revealed. The fact that she probably believes them is not a sufficient excuse for endangering the public. There is certainly no excuse for the university allowing this stuff to be taught as part of a BSc (Hons).
First get them scared with some bad statistics.
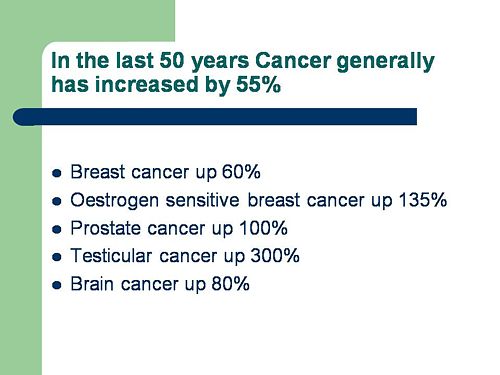
No fuss there about distinguishing incidence, age-standardisation and death rates. And no reference. Perhaps a reference to the simple explanation of statistics at Cancer Research UK might help? Perhaps this slide would have been better (from CDC). Seems there is some mistake in slide 2.
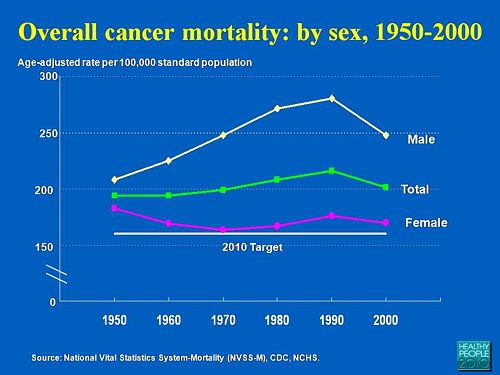
Straight on to a truly disgraceful statement in slide 3
The is outrageous and very possibly illegal under the Cancer Act (1939). It certainly poses a huge danger to patients. It is a direct incentive to make illegal, and untrue claims by using weasel words in an attempt to stay just on the right side of the law. But that, of course, is standard practice in alternative medicine,
Slide 11 is mostly meaningless. “Strengthen vitality” sounds good but means nothing. And “enhancing the immune system” is what alternative medicine folks always say when they can think of nothing else. Its meaning is ill-defined and there is no reason to think that any herbs do it.
The idea of a ‘tonic’ was actually quite common in real medicine in the 1950s. The term slowly vanished as it was realised that it was a figment of the imagination. In the fantasy world of alternative medicine, it lives on.
Detoxification, a marketing term not a medical one, has been extensively debunked quite recently. The use of the word by The Prince of Wales’ company, Duchy Originals recently fell foul of the Advertising Standards Authority, and his herbal ‘remedies’ were zapped by the MHRA (Medicines and Health Regulatory Authority).
And of course the antioxidant myth is a long-disproved hypothesis that has become a mere marketing term.
“Inhibits the recurrence of cancer”! That sounds terrific. But if it is so good why is it not even mentioned in the two main resources for information about herbs?
In the UK we have the National Library for Health Complementary and Alternative Medicine Specialist Library (NeLCAM), now a part of NHS Evidence. It was launched in 2006. The clinical lead was none other than Peter Fisher, clinical director of the Royal London Homeopathic Hospital, and the Queen’s homeopathic physician. The library was developed with the School of Integrated Health at the University of Westminster (where this particular slide was shown to undergraduates). Nobody could accuse these people of being hostile to magic medicine,
It seems odd, then, that NeLCAM does not seem to thnk to think that Centella asiatica, is even worth mentioning.
In the USA we have the National Center for Alternative and Complementary Medicine (NCCAM), an organisation that is so friendly to alternative medicine that it has spent a billion dollars on research in the area, though it has produced not a single good treatment for that vast expenditure. But NCCAM too does not even mention Centella asiatica in its herb list. It does get a mention in Cochrane reviews but only as a cosmetic cream and as an unproven treatment for poor venous circulation in the legs.
What on earth is a “lymph remedy”. Just another marketing term?
“especially valuable in the treatment of breast, throat and uterus cancer.“
That is a very dramatic claim. It as as though the hapless students were being tutored in doublespeak. What is meant by “especially valuable in the treatment of”? Clearly a desperate patient would interpret those words as meaning that there was at least a chance of a cure. That would be a wicked deception because there isn’t the slightest reason to think it works. Once again there this wondrous cure is not even mentioned in either NELCAM or NCCAM. Phytolacca is mentioned, as Pokeweed, in Wikipedia but no claims are mentioned even there. And it isn’t mentioned in Cochrane reviews either. The dramatic claims are utterly unfounded.
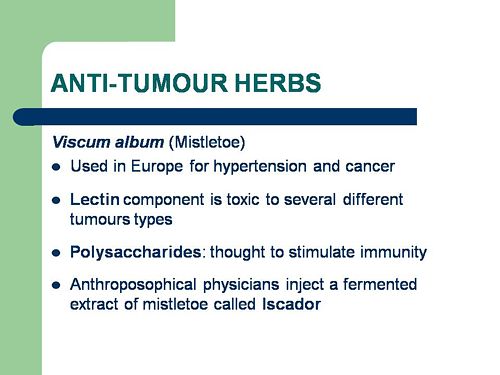
Ah the mistletoe story, again.
NHS Evidence (NeLCAM) lists three completed assessments. One concludes that more research is needed. Another concludes that “Rigorous trials of mistletoe extracts fail to demonstrate efficacy of this therapy”, and the third says “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
NCCAM says of mistletoe
- More than 30 human studies using mistletoe to treat cancer have been done since the early 1960s, but major weaknesses in many of these have raised doubts about their findings (see Question 6).
- Very few bad side effects have been reported from the use of mistletoe extract, though mistletoe plants and berries are poisonous to humans (see Question 7).
- The U.S. Food and Drug Administration (FDA) has not approved mistletoe as a treatment for cancer or any other medical condition (see Question 8).
- The FDA does not allow injectable mistletoe to be imported, sold, or used except for clinical research (see Question 8).
Cochrane reviews lists several reviews of mistletoe with similar conclusions. For example “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
Anthroposophy is one of the highest grades of fantasy you can find. A post on that topic is in the works.
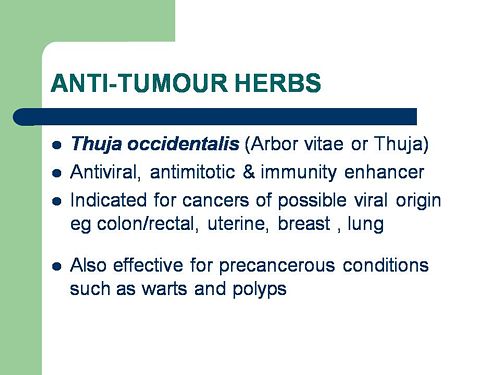
“Indicated for cancers . . . colon/rectal, uterine, breast, lung“. A cure for lung cancer? That, of course, depends on how you interpret the weasel words “indicated for”. Even Wikipedia makes no mention of any claims that Thuja benefits cancer. NHS Evidence (NeLCAM) doesn’t mention Thuja for any indication. Neither does NCCAM. Nor Cochrane reviews. That is not the impression the hapless students of this BSc lecture were given. In my view suggestions that you can cure lung cancer with this tree are just plain wicked.
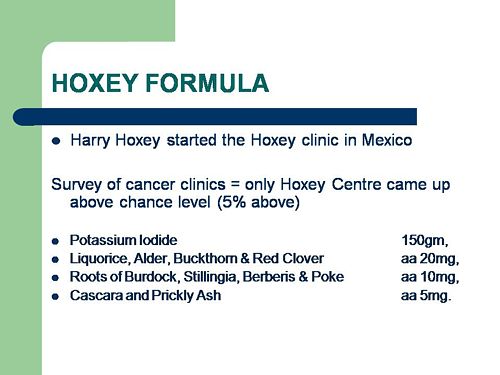
Pure snake oil, and not even spelled correctly, Harry Hoxsey’s treatment centres in the USA were closed by court order in the 1950s.
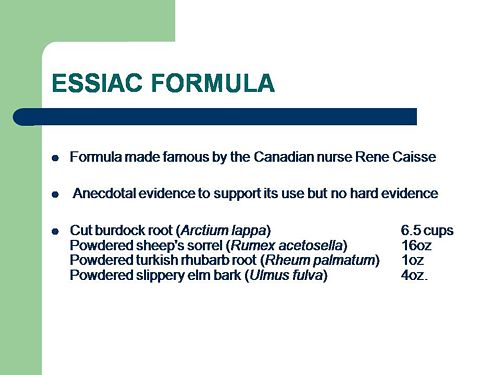
At least this time it is stated that there is no hard evidence to support this brand of snake oil.
More unfounded claims when it says “treated successfully many cancer patients”. No references and no data to support the claim. It is utterly unfounded and claims to the contrary endanger the public.
Gerson therapy is one of the most notorious and unpleasant of the quack cancer treatments. The Gerson Institute is on San Diego, but their clinics are in Mexico and Hungary. It is illegal in the USA. According to the American Cancer Society you get “a strict low-salt, low-fat, vegetarian diet and drinking juice from about twenty pounds of fresh fruits and vegetables each day. One glass of juice is consumed each hour, thirteen times a day. In addition, patients are given several coffee enemas each day. Various supplements, such as potassium, vitamin B12, pancreatic enzymes, thyroid hormone, and liver extracts, are used to stimulate organ function, particularly of the liver and thyroid.”. At one time you also got several glasses of raw calf liver every day but after infections killed several people] carrot juice was given instead.
Cancer Research UK says “there is no evidence to show that Gerson therapy works as a cure for cancer”, and “The Gerson diet can cause some very serious side effects.” Nobody (except perhaps the Price of Wales) has any belief in this unpleasant, toxic and expensive folk-lore.
Again patients are endangered by teaching this sort of stuff.
And finally, the usual swipe at vaccines. It’s nothing to do with herbalism. but just about every alternative medicine advocate seems to subscribe to the anti-vaccination lobby.. It is almost as though they have an active preference for things that are known to be wrong. They seem to believe that medicine and science are part of an enormous conspiracy to kill everyone.
Perhaps this dangerous propaganda might have been ameliorated if the students had been shown this slide (from a talk by Melinda Wharton).
Left to people like this, we would still have smallpox, diphtheria. tetanus and rabies, Take a look at Vaccine-preventable diseases.
This is the sort of ‘education’ which the Pittilo report wants to make compulsory.
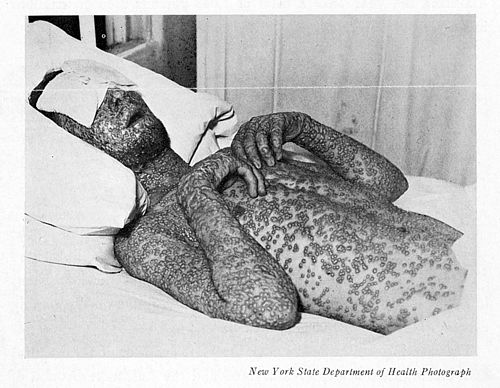
Smallpox in Baltimore, USA, 1939. This man was not vaccinated.
Conclusion
This selection of slides shows that much of the stuff taught in degrees in herbal medicine poses a real danger to public safety and to public health.
Pittilo’s idea that imposing this sort of miseducation will help safety is obviously and dangerously wrong. The Department of Health must reject the Pittilo recommendations on those grounds.