causality
‘We know little about the effect of diet on health. That’s why so much is written about it’. That is the title of a post in which I advocate the view put by John Ioannidis that remarkably little is known about the health effects if individual nutrients. That ignorance has given rise to a vast industry selling advice that has little evidence to support it.
The 2016 Conference of the so-called "College of Medicine" had the title "Food, the Forgotten Medicine". This post gives some background information about some of the speakers at this event. I’m sorry it appears to be too ad hominem, but the only way to judge the meeting is via the track record of the speakers.

Quite a lot has been written here about the "College of Medicine". It is the direct successor of the Prince of Wales’ late, unlamented, Foundation for Integrated Health. But unlike the latter, its name is disguises its promotion of quackery. Originally it was going to be called the “College of Integrated Health”, but that wasn’t sufficently deceptive so the name was dropped.
For the history of the organisation, see
Don’t be deceived. The new “College of Medicine” is a fraud and delusion
The College of Medicine is in the pocket of Crapita Capita. Is Graeme Catto selling out?
The conference programme (download pdf) is a masterpiece of bait and switch. It is a mixture of very respectable people, and outright quacks. The former are invited to give legitimacy to the latter. The names may not be familiar to those who don’t follow the antics of the magic medicine community, so here is a bit of information about some of them.
The introduction to the meeting was by Michael Dixon and Catherine Zollman, both veterans of the Prince of Wales Foundation, and both devoted enthusiasts for magic medicne. Zollman even believes in the battiest of all forms of magic medicine, homeopathy (download pdf), for which she totally misrepresents the evidence. Zollman works now at the Penny Brohn centre in Bristol. She’s also linked to the "Portland Centre for integrative medicine" which is run by Elizabeth Thompson, another advocate of homeopathy. It came into being after NHS Bristol shut down the Bristol Homeopathic Hospital, on the very good grounds that it doesn’t work.
Now, like most magic medicine it is privatised. The Penny Brohn shop will sell you a wide range of expensive and useless "supplements". For example, Biocare Antioxidant capsules at £37 for 90. Biocare make several unjustified claims for their benefits. Among other unnecessary ingredients, they contain a very small amount of green tea. That’s a favourite of "health food addicts", and it was the subject of a recent paper that contains one of the daftest statistical solecisms I’ve ever encountered
"To protect against type II errors, no corrections were applied for multiple comparisons".
If you don’t understand that, try this paper.
The results are almost certainly false positives, despite the fact that it appeared in Lancet Neurology. It’s yet another example of broken peer review.
It’s been know for decades now that “antioxidant” is no more than a marketing term, There is no evidence of benefit and large doses can be harmful. This obviously doesn’t worry the College of Medicine.
Margaret Rayman was the next speaker. She’s a real nutritionist. Mixing the real with the crackpots is a standard bait and switch tactic.
Eleni Tsiompanou, came next. She runs yet another private "wellness" clinic, which makes all the usual exaggerated claims. She seems to have an obsession with Hippocrates (hint: medicine has moved on since then). Dr Eleni’s Joy Biscuits may or may not taste good, but their health-giving properties are make-believe.
Andrew Weil, from the University of Arizona
gave the keynote address. He’s described as "one of the world’s leading authorities on Nutrition and Health". That description alone is sufficient to show the fantasy land in which the College of Medicine exists. He’s a typical supplement salesman, presumably very rich. There is no excuse for not knowing about him. It was 1988 when Arnold Relman (who was editor of the New England Journal of Medicine) wrote A Trip to Stonesville: Some Notes on Andrew Weil, M.D..
“Like so many of the other gurus of alternative medicine, Weil is not bothered by logical contradictions in his argument, or encumbered by a need to search for objective evidence.”
This blog has mentioned his more recent activities, many times.
Alex Richardson, of Oxford Food and Behaviour Research (a charity, not part of the university) is an enthusiast for omega-3, a favourite of the supplement industry, She has published several papers that show little evidence of effectiveness. That looks entirely honest. On the other hand, their News section contains many links to the notorious supplement industry lobby site, Nutraingredients, one of the least reliable sources of information on the web (I get their newsletter, a constant source of hilarity and raised eyebrows). I find this worrying for someone who claims to be evidence-based. I’m told that her charity is funded largely by the supplement industry (though I can’t find any mention of that on the web site).
Stephen Devries was a new name to me. You can infer what he’s like from the fact that he has been endorsed byt Andrew Weil, and that his address is "Institute for Integrative Cardiology" ("Integrative" is the latest euphemism for quackery). Never trust any talk with a title that contains "The truth about". His was called "The scientific truth about fats and sugars," In a video, he claims that diet has been shown to reduce heart disease by 70%. which gives you a good idea of his ability to assess evidence. But the claim doubtless helps to sell his books.
Prof Tim Spector, of Kings College London, was next. As far as I know he’s a perfectly respectable scientist, albeit one with books to sell, But his talk is now online, and it was a bit like a born-again microbiome enthusiast. He seemed to be too impressed by the PREDIMED study, despite it’s statistical unsoundness, which was pointed out by Ioannidis. Little evidence was presented, though at least he was more sensible than the audience about the uselessness of multivitamin tablets.
Simon Mills talked on “Herbs and spices. Using Mother Nature’s pharmacy to maintain health and cure illness”. He’s a herbalist who has featured here many times. I can recommend especially his video about Hot and Cold herbs as a superb example of fantasy science.
Annie Anderson, is Professor of Public Health Nutrition and
Founder of the Scottish Cancer Prevention Network. She’s a respectable nutritionist and public health person, albeit with their customary disregard of problems of causality.
Patrick Holden is chair of the Sustainable Food Trust. He promotes "organic farming". Much though I dislike the cruelty of factory farms, the "organic" industry is largely a way of making food more expensive with no health benefits.
The Michael Pittilo 2016 Student Essay Prize was awarded after lunch. Pittilo has featured frequently on this blog as a result of his execrable promotion of quackery -see, in particular, A very bad report: gamma minus for the vice-chancellor.
Nutritional advice for patients with cancer. This discussion involved three people.
Professor Robert Thomas, Consultant Oncologist, Addenbrookes and Bedford Hospitals, Dr Clare Shaw, Consultant Dietitian, Royal Marsden Hospital and Dr Catherine Zollman, GP and Clinical Lead, Penny Brohn UK.
Robert Thomas came to my attention when I noticed that he, as a regular cancer consultant had spoken at a meeting of the quack charity, “YestoLife”. When I saw he was scheduled tp speak at another quack conference. After I’d written to him to point out the track records of some of the people at the meeting, he withdrew from one of them. See The exploitation of cancer patients is wicked. Carrot juice for lunch, then die destitute. The influence seems to have been temporary though. He continues to lend respectability to many dodgy meetings. He edits the Cancernet web site. This site lends credence to bizarre treatments like homeopathy and crystal healing. It used to sell hair mineral analysis, a well-known phony diagnostic method the main purpose of which is to sell you expensive “supplements”. They still sell the “Cancer Risk Nutritional Profile”. for £295.00, despite the fact that it provides no proven benefits.
Robert Thomas designed a food "supplement", Pomi-T: capsules that contain Pomegranate, Green tea, Broccoli and Curcumin. Oddly, he seems still to subscribe to the antioxidant myth. Even the supplement industry admits that that’s a lost cause, but that doesn’t stop its use in marketing. The one randomised trial of these pills for prostate cancer was inconclusive. Prostate Cancer UK says "We would not encourage any man with prostate cancer to start taking Pomi-T food supplements on the basis of this research". Nevertheless it’s promoted on Cancernet.co.uk and widely sold. The Pomi-T site boasts about the (inconclusive) trial, but says "Pomi-T® is not a medicinal product".
There was a cookery demonstration by Dale Pinnock "The medicinal chef" The programme does not tell us whether he made is signature dish "the Famous Flu Fighting Soup". Needless to say, there isn’t the slightest reason to believe that his soup has the slightest effect on flu.
In summary, the whole meeting was devoted to exaggerating vastly the effect of particular foods. It also acted as advertising for people with something to sell. Much of it was outright quackery, with a leavening of more respectable people, a standard part of the bait-and-switch methods used by all quacks in their attempts to make themselves sound respectable. I find it impossible to tell how much the participants actually believe what they say, and how much it’s a simple commercial drive.
The thing that really worries me is why someone like Phil Hammond supports this sort of thing by chairing their meetings (as he did for the "College of Medicine’s" direct predecessor, the Prince’s Foundation for Integrated Health. His defence of the NHS has made him something of a hero to me. He assured me that he’d asked people to stick to evidence. In that he clearly failed. I guess they must pay well.
Follow-up
This article has been re-posted on The Winnower, so it now has a digital object identifier: DOI: 10.15200/winn.142935.50603
The latest news: eating red meat doesn’t do any harm. But why isn’t that said clearly? Alarmism makes better news, not only for journalists but for authors and university PR people too.
I’ve already written twice about red meat.
In May 2009 Diet and health. What can you believe: or does bacon kill you? based on the WCRF report (2007).
In March 2012 How big is the risk from eating red meat now? An update.
In the first of these I argued that the evidence produced by the World Cancer Research Fund (WCRF) for a causal relationship was very thin indeed. An update by WCRF in 2010 showed a slightly smaller risk, and weakened yet further the evidence for causality, though that wasn’t reflected in their press announcement.
The 2012 update added observations from two very large cohort studies. The result was that the estimates of risk were less than half as big as in 2009. The relative risk of dying from colorectal cancer was 1.21 (95% Confidence interval 1.04–1.42) with 50 g of red or processed meat per day, whereas in the new study the relative risk for cancer was only 1.10 (1.06-1.14) for a larger ‘dose’, 85 g of red meat. Again this good news was ignored and dire warnings were issued.
This reduction in size of the effect as samples get bigger is exactly what’s expected for spurious correlations, as described by Ioannidis and others. And it seems to have come true. The estimate of the harm done by red meat has vanished entirely in the latest study.
The EPIC study
This is the European Prospective Investigation into Cancer and Nutrition, another prospective cohort study, so it isn’t randomised [read the original paper]. And it was big, 448,568 people from ten different European countries. These people were followed for a median time of 12.7 years, and during follow-up 26,344 of them died.
The thing that was different about this paper was that red meat was found to pose no detectable risk, as judged by all-cause mortality. But this wasn’t even mentioned in the headline conclusions.
Conclusions: The results of our analysis support a moderate positive association between processed meat consumption and mortality, in particular due to cardiovascular diseases, but also to cancer.
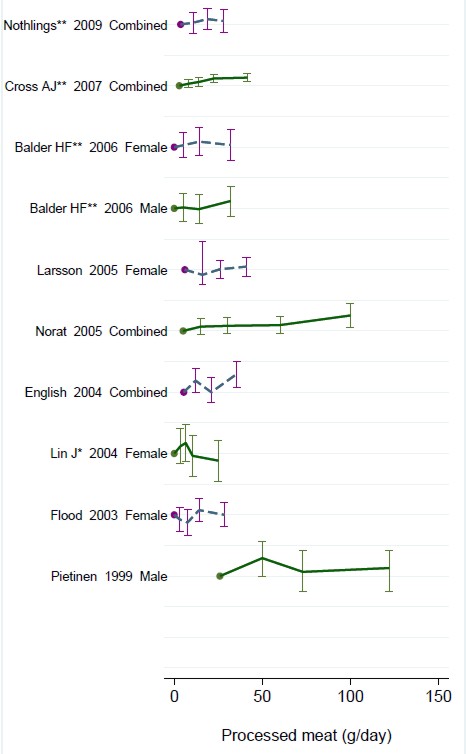
To find the result you have to dig into Table 3.
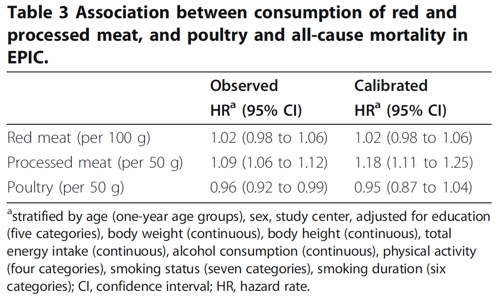
So, by both methods of calculation, the relative risk from eating red meat is negligible (except possibly in the top group, eating more than 160 g (7 oz) per day).
There is still an association between intake of processed meat and all-cause mortality, as in previous studies, though the association of processed meat with all-cause mortality, 1.09, or 1.18 depending on assumptions, is, if anything, smaller than was observed in the 2012 study, in which the relative risk was 1.20 (Table 2).
Assumptions, confounders and corrections.
The lowest meat eaters had only 13% of current smokers, but for the biggest red meat eaters it was 40%, for males. The alcohol consumption was 8.2 g/day for the lowest meat eaters but 23.4 g/day for the highest-meat group (the correlations were a bit smaller for women and also for processed meat eaters).
These two observations necessitate huge corrections to remove the (much bigger) effects of smoking and drinking if we want find the association for meat-eating alone. The main method for doing the correction is to fit the Cox proportional hazards model. This model assumes that there are straight-line relationships between the logarithm of the risk and the amount of each of the risk factors, e.g smoking, drinking, meat-eating and other risk factors. It may also include interactions that are designed to detect whether, for example, the effect of smoking on risk is or isn’t the same for people who drink different amounts.
Usually the straight-line assumption isn’t tested, and the results will depend on which risk factors (and which interactions between them) are included in the calculations. Different assumptions will give different answers. It simply isn’t known how accurate the corrections are when trying to eliminate the big effect of smoking in order to isolate the small effect of meat-eating. And that is before we get to other sorts of correction. For example, the relative risk from processed meat in Table 3, above, was 9% or 18% (1.09, or 1.18) depending on the outcome of a calculation that was intended to increase the accuracy of food intake records ("calibration").
The Conclusions of the new study don’t even mention the new result with red meat. All they mention is the risk from processed meat.
In this population, reduction of processed meat consumption to less than 20 g/day would prevent more than 3% of all deaths. As processed meat consumption is a modifiable risk factor, health promotion activities should include specific advice on lowering processed meat consumption.
Well, you would save that number of lives if, and only if, the processed meat was the cause of death. Too many epidemiologists, the authors pay lip service to the problem of causality in the introduction, but then go on to assume it in the conclusions. In fact the problem of causality isn’t even metnioned anywhere in either the 2012 study, or the new 2013 EPIC trial.
So is the risk of processed meat still real? Of course I can’t answer that. All that can be said is that it’s quite small, and as sample sizes get bigger, estimates of the risk are getting smaller. It wouldn’t be surprising if the risk from processed meat were eventually found not to exist, just as has happened for red (unprocessed) meat
The Japanese study
Last year there was another cohort study, with 51,683 Japanese. The results were even more (non-) dramatic [Nagao et al, 2012] than in the EPIC trial. This is how they summarise the results for the relative risks (with 95% confidence intervals).
"…for the highest versus lowest quintiles of meat consumption (77.6 versus 10.4 g/day) among men were 0.66 (0.45 — 0.97) for ischemic heart disease, 1.10 (0.84 — 1.43) for stroke and 1.00 (0.84 — 1.20) for total cardiovascular disease. The corresponding HRs (59.9 versus 7.5 g/day) among women were 1.22 (0.81 — 1.83), 0.91 (0.70 — 1.19) and 1.07 (0.90 — 1.28). The associations were similar when the consumptions of red meat, poultry, processed meat and liver were examined separately.
CONCLUSION: Moderate meat consumption, up to about 100 g/day, was not associated with increased mortality from ischemic heart disease, stroke or total cardiovascular disease among either gender."
In this study, the more meat (red or processed) you eat, the lower your risk of ischaemic heart disease (with the possible exception of overweight women). The risk of dying from any cardiovascular disease was unrelated to the amount of meat eaten (relative risk 1.0) whether processed meat or not.
Of course it’s possible that things which risky for Japanese people differ from those that are risky for Europeans. It’s also possible that even processed meat isn’t bad for you.
The carnitine study
The latest meat study to hit the headlines didn’t actually look at the effects of meat at all, though you wouldn’t guess that from the pictures of sausages in the headlines (not just in newspapers, but also in NHS Choices). The paper [reprint] was about carnitine, a substance that occurs particularly in beef, with lower amounts in pork and bacon, and in many other foods. The paper showed that bacteria in the gut can convert carnitine to a potentially toxic substance, trimethylamine oxide (TMAO). That harms blood vessels (at least in mice). But to show an effect in human subjects they were given an amount of carnitine equivalent to over 1 lb of steak, hardly normal, even in the USA.
The summary of the paper says it is an attempt to explain "the well-established link between high levels of red meat consumption and CVD [cardiovascular disease] risk". As we have just seen, it seems likely that this risk is far from being “well-established”. There is little or no such risk to explain.
It would be useful to have a diagnostic marker for heart disease, but this paper doesn’t show that carnitine or TMAO) is useful for that. It might also be noted that the authors have a maze of financial interests.
Competing financial interests Z.W. and B.S.L. are named as co-inventors on pending patents held by the Cleveland Clinic relating to cardiovascular diagnostics and have the right to receive royalty payments for inventions or discoveries related to cardiovascular diagnostics from Liposciences. W.H.W.T. received research grant support from Abbott Laboratories and served as a consultant for Medtronic and St. Jude Medical. S.L.H. and J.D.S. are named as co-inventors on pending and issued patents held by the Cleveland Clinic relating to cardiovascular diagnostics and therapeutics patents. S.L.H. has been paid as a consultant or speaker by the following companies: Cleveland Heart Lab., Esperion, Liposciences, Merck & Co. and Pfizer. He has received research funds from Abbott, Cleveland Heart Lab., Esperion and Liposciences and has the right to receive royalty payments for inventions or discoveries related to cardiovascular diagnostics from Abbott Laboratories, Cleveland Heart Lab., Frantz Biomarkers, Liposciences and Siemens.
The practical significance of this work was summed up the dietitian par excellence, Catherine Collins, on the BBC’s Inside Health programme.
Listen to Catherine Collins on carnitine.
She points out that the paper didn’t mean that we should change what we already think is a sensible diet.
At most, it suggests that it’s not a good idea to eat 1 lb steaks very day.
And the paper does suggest that it’s not sensible to take the carnitine supplements that are pushed by every gym. According to NIH
"twenty years of research finds no consistent evidence that carnitine supplements can improve exercise or physical performance in healthy subjects".
Carnitine supplements are a scam. And they could be dangerous.
Follow-up
Another blog on this topic, one from Cancer Research UK also fails to discuss the problem of causality. Neither does it go into the nature (and fallibility) of the corrections for counfounders like smoking and alcohol,. Nevertheless that, and an earlier post on Food and cancer: why media reports are often misleading, are a good deal more realistic than most newspaper reports.
This is a slightly-modified version of the article that appeared in BMJ blogs yesterday, but with more links to original sources, and a picture. There are already some comments in the BMJ.
The original article, diplomatically, did not link directly to UCL’s Grand Challenge of Human Wellbeing, a well-meaning initiative which, I suspect, will not prove to be value for money when it comes to practical action.
Neither, when referring to the bad effects of disempowerment on human wellbeing (as elucidated by, among others, UCL’s Michael Marmot), did I mention the several ways in which staff have been disempowered and rendered voiceless at UCL during the last five years. Although these actions have undoubtedly had a bad effect on the wellbeing of UCL’s staff, it seemed a litlle unfair to single out UCL since similar things are happening in most universities. Indeed the fact that it has been far worse at Imperial College (at least in medicine) has probably saved UCL from being denuded. One must be thankful for small mercies.
There is, i think, a lesson to be learned from the fact that formal initiatives in wellbeing are springing up at a time when university managers are set on taking actions that have exactly the opposite effect. A ‘change manager’ is not an adequate substitute for a vote. Who do they imagine is being fooled?
The A to Z of the wellbeing industry
From angelic reiki to patient-centred care
Nobody could possibly be against wellbeing. It would be like opposing motherhood and apple pie. There is a whole spectrum of activities under the wellbeing banner, from the undoubtedly well-meaning patient-centred care at one end, to downright barmy new-age claptrap at the other end. The only question that really matters is, how much of it works?
Let’s start at the fruitcake end of the spectrum.
One thing is obvious. Wellbeing is big business. And if it is no more than a branch of the multi-billion-dollar positive-thinking industry, save your money and get on with your life.
In June 2010, Northamptonshire NHS Foundation Trust sponsored a “Festival of Wellbeing” that included a complementary therapy taster day. In a BBC interview one practitioner used the advertising opportunity, paid for by the NHS, to say “I’m an angelic reiki master teacher and also an angel therapist.” “Angels are just flying spirits, 100 percent just pure light from heaven. They are all around us. Everybody has a guardian angel.” Another said “I am a member of the British Society of Dowsers and use a crystal pendulum to dowse in treatment sessions. Sessions may include a combination of meditation, colour breathing, crystals, colour scarves, and use of a light box.” You couldn’t make it up.
The enormous positive-thinking industry is no better. Barbara Ehrenreich’s book, Smile Or Die: How Positive Thinking Fooled America and the World, explains how dangerous the industry is, because, as much as guardian angels, it is based on myth and delusion. It simply doesn’t work (except for those who make fortunes by promoting it). She argues that it fosters the sort of delusion that gave us the financial crisis (and pessimistic bankers were fired for being right). Her interest in the industry started when she was diagnosed with cancer. She says
”When I was diagnosed, what I found was constant exhortations to be positive, to be cheerful, to even embrace the disease as if it were a gift. If that’s a gift, take me off your Christmas list,”
It is quite clear that positive thinking does nothing whatsoever to prolong your life (Schofield et al 2004; Coyne et al 2007; 2,3), any more than it will cure tuberculosis or cholera. “Encouraging patients to “be positive” only may add to the burden of having cancer while providing little benefit” (Schofield et al 2004). Far from being helpful, it can be rather cruel.
Just about every government department, the NHS, BIS, HEFCE, and NICE, has produced long reports on wellbeing and stress at work. It’s well known that income is correlated strongly with health (Marmot, M., 2004). For every tube stop you go east of Westminster you lose a year of life expectancy (London Health Observatory). It’s been proposed that what matters is inequality of income (Wilkinson & Pickett, 2009). The nature of the evidence doesn’t allow such a firm conclusion (Lynch et al. 2004), but that isn’t really the point. The real problem is that nobody has come up with good solutions. Sadly the recommendations at the ends of all these reports don’t amount to a hill of beans. Nobody knows what to do, partly because pilot studies are rarely randomised so causality is always dubious, and partly because the obvious steps are either managerially inconvenient, ideologically unacceptable, or too expensive.
Take two examples:
Sir Michael Marmot’s famous Whitehall study (Marmot, M., 2004) has shown that a major correlate of illness is lack of control over one’s own fate: disempowerment. What has been done about it?
In universities it has proved useful to managers to increase centralisation and to disempower academics, precisely the opposite of what Marmot recommends.
|
As long as it’s convenient to managers they are not going to change policy. Rather, they hand the job to the HR department which appoints highly paid “change managers,” who add to the stress by sending you stupid graphs that show you emerging from the slough of despond into eternal light once you realise that you really wanted to be disempowered after all. Or they send you on some silly “resilience” course. |
|
A second example comes from debt. According to a BIS report (Mental Capital and Wellbeing), debt is an even stronger risk factor for mental disorder than low income. So what is the government’s response to that? To treble tuition fees to ensure that almost all graduates will stay in debt for most of their lifetime. And this was done despite the fact that the £9k fees will save nothing for the taxpayer: in fact they’ll cost more than the £3k fees. The rise has happened, presumably, because the ideological reasons overrode the government’s own ideas on how to make people happy.
Nothing illustrates better the futility of the wellbeing industry than the response that is reported to have been given to a reporter who posed as an applicant for a “health, safety, and wellbeing adviser” with a local council. When he asked what “wellbeing” advice would involve, a member of the council’s human resources team said: “We are not really sure yet as we have only just added that to the role. We’ll want someone to make sure that staff take breaks, go for walks — that kind of stuff.”
The latest wellbeing notion to re-emerge is the happiness survey. Jeremy Bentham advocated “the greatest happiness for the greatest number,” but neglected to say how you measure it. A YouGov poll asks, “what about your general well-being right now, on a scale from 1 to 10.” I have not the slightest idea about how to answer such a question. As always some things are good, some are bad, and anyway wellbeing relative to whom? Writing this is fun. Trying to solve an algebraic problem is fun. Constant battling with university management in order to be able to do these things is not fun. The whole exercise smacks of the sort of intellectual arrogance that led psychologists in the 1930s to claim that they could sum up a person’s intelligence in a single number. That claim was wrong and it did great social harm.
HEFCE has spent a large amount of money setting up “pilot studies” of wellbeing in nine universities. Only one is randomised, so there will be no evidence for causality. The design of the pilots is contracted to a private company, Robertson Cooper, which declines to give full details but it seems likely that the results will be about as useless as the notorious Durham fish oil “trials”(Goldacre, 2008).
Lastly we get to the sensible end of the spectrum: patient-centred care. Again this has turned into an industry with endless meetings and reports and very few conclusions. Epstein & Street (2011) say
“Helping patients to be more active in consultations changes centuries of physician-dominated dialogues to those that engage patients as active participants. Training physicians to be more mindful, informative, and empathic transforms their role from one characterized by authority to one that has the goals of partnership, solidarity, empathy, and collaboration.”
That’s fine, but the question that is constantly avoided is what happens when a patient with metastatic breast cancer expresses a strong preference for Vitamin C or Gerson therapy, as advocated by the YesToLife charity. The fact of the matter is that the relationship can’t be equal when one party, usually (but not invariably) the doctor, knows a lot more about the problem than the other.
What really matters above all to patients is getting better. Anyone in their right mind would prefer a grumpy condescending doctor who correctly diagnoses their tumour, to an empathetic doctor who misses it. It’s fine for medical students to learn social skills but there is a real danger of so much time being spent on it that they can no longer make a correct diagnosis. Put another way, there is confusion between caring and curing. It is curing that matters most to patients. It is this confusion that forms the basis of the bait and switch tactics (see also here) used by magic medicine advocates to gain the respectability that they crave but rarely deserve.
If, as is only too often the case, the patient can’t be cured, then certainly they should be cared for. That’s a moral obligation when medicine fails in its primary aim. There is a lot of talk about individualised care. It is a buzzword of quacks and also of the libertarian wing which says NICE is too prescriptive. It sounds great, but it helps only if the individualised treatment actually works.
Nobody knows how often medicine fails to be “patient-centred.”. Even less does anyone know whether patient-centred care can improve the actual health of patients. There is a strong tendency to do small pilot trials that are as likely to mislead as inform. One properly randomised trial (Kinmonth et al., 1998) concluded
“those committed to achieving the benefits of patient centred consulting should not lose the focus on disease management.”
Non-randomised studies may produce more optimistic conclusions (e.g. Hojat et al, 2011), but there is no way to tell if this is simply because doctors find it easy to be empathetic with patients who have better outcomes.
Obviously I’m in favour of doctors being nice to patients and to listening to their wishes. But there is a real danger that it will be seen as more important than curing. There is also a real danger that it will open the doors to all sorts of quacks who claim to provide individualised empathic treatment, but end up recommending Gerson therapy for metastatic breast cancer. The new College of Medicine, which in reality is simply a reincarnation of the late unlamented Prince’s Foundation for Integrated Health, lists as its founder Capita, the private healthcare provider that will, no doubt, be happy to back the herbalists and homeopaths in the College of Medicine, and, no doubt, to make a profit from selling their wares to the NHS.
In my own experience as a patient, there is not nearly as much of a problem with patient centred care as the industry makes out. Others have been less lucky, as shown by the mid-Staffordshire disaster (Delamothe, 2010), That seems to have resulted from PR being given priority over patients. Perhaps all that’s needed is to save money on all the endless reports and meetings (“the best substitute for work”), ban use of PR agencies (paid lying) and to spend the money on more doctors and nurses so they can give time to people who need it. This is a job that will be hindered considerably by the government’s proposals to sell off NHS work to private providers who will be happy to make money from junk medicine.
Reference
Wilkinson. R & Pickett, K. 2009 , The Spirit Level, ISBN 978 1 84614 039 6
A footnote on Robertson Cooper and "resilience"
I took up the offer of Robertson Cooper to do their free "resilience" assessment, the company to which HEFCE has paid an undisclosed amount of money.
The first problem arose when it asked about your job. There was no option for scientist, mathematician, university or research, so I was forced to choose "education and training". (a funny juxtaposition since training is arguably the antithesis of education). It had 195 questions. mostly as unanswerable as in the YouGov happiness survey. I particularly liked question 124 "I see little point in many of the theoretical models I come across". The theoretical models that I come across most are Markov models for the intramolecular changes in a receptor molecule when it binds a ligand (try, for example, Joint distributions of apparent open and shut times of single-ion channels and maximum likelihood fitting of mechanisms). I doubt the person who wrote the question has ever heard of a model of that sort. The answer to that question (and most of the others) would not be worth the paper they are written on.
The whole exercise struck me as the worst sort of vacuous HR psychobabble. It is worrying that HEFCE thinks it is worth spending money on it.
Follow-up
This post recounts a complicated story that started in January 2009, but has recently come to what looks like a happy ending. The story involves over a year’s writing of letters and meetings, but for those not interested in the details, I’ll start with a synopsis.
Synopsis of the synopsis
In January 2009, a course in "integrated medicine" was announced that, it was said, would be accredited by the University of Buckingham. The course was to be led by Drs Rosy Daniel and Mark Atkinson. So I sent an assessment of Rosy Daniel’s claims to "heal" cancer to Buckingham’s VC (president), Terence Kealey, After meeting Karol Sikora and Rosy Daniel, I sent an analysis of the course tutors to Kealey who promptly demoted Daniel, and put Prof Andrew Miles in charge of the course. The course went ahead in September 2009. Despite Miles’ efforts, the content was found to be altogether too alternative. The University of Buckingham has now terminated its contract with the "Faculty of Integrated Medicine", and the course will close. Well done.Buckingham.
Synopsis
- January 2009. I saw an announcement of a Diploma in Integrated Medicine, to be accredited by the University of Buckingham (UB). The course was to be run by Drs Rosy Daniel and Mark Atkinson of the College of Integrated Medicine, under the nominal directorship of Karol Sikora (UB’s Dean of Medicine). I wrote to Buckingham’s vice-chancellor (president), Terence Kealey, and attached a reprint of Ernst’s paper on carctol, a herbal cancer ‘remedy’ favoured by Daniiel.
- Unlike most vice-chancellors, Kealey replied at once and asked me to meet Sikora and Daniel. I met first Sikora alone, and then, on March 19 2009, both together. Rosy Daniel gave me a complete list of the speakers she’d chosen. Most were well-known alternative people, some, in my view, the worst sort of quack. After discovering who was to teach on the proposed course, I wrote a long document about the proposed speakers and sent it to the vice-chancellor of the University of Buckingham, Terence Kealey on March 23rd 2009.. Unlike most VCs, he took it seriously. At the end of this meeting I asked Sikora, who was in nominal charge of the course, how many of the proposed tutors he’d heard of. The answer was "none of them"
- Shortly before this meeting, I submitted a complaint to Trading Standards about Rosy Daniel’s commercial site, HealthCreation, for what seemed to me to be breaches of the Cancer Act 1939, by claims made for Carctol. Read the complaint.
- On 27th April 2009, I heard from Kealey that he’d demoted Rosy Daniel from being in charge of the Diploma and appointed Andrew Miles, who had recently been appointed as Buckingham’s Professor of Public Health Education and Policy &Associate Dean of Medicine (Public Health). Terence Kealey said "You’ve done us a good turn, and I’m grateful". Much appreciated. Miles said the course “needs in my view a fundamental reform of content. . . “
- Although Rosy Daniel had been demoted, she was still in charge of delivering the course at what had, by this time, changed its name to the Faculty of Integrated Medicine which, despite its name, is not part of the university.
- Throughout the summer I met Miles (of whom more below) several times and exchanged countless emails, but still didn’t get the revised list of speakers. The course went ahead on 30 September 2009. He also talked with Michael Baum and Edzard Ernst.
- By January 2010, Miles came to accept that the course was too high on quackery to be a credit to the university, and simply fired The Faculty of Integrated Medicine. Their contract was not renewed. Inspection of the speakers, even after revision of the course, shows why.
- As a consequence, it is rumoured that Daniel is trying to sell the course to someone else. The University of Middlesex, and unbelievably, the University of Bristol, have been mentioned, as well as Thames Valley University, the University of Westminster, the University of Southampton and the University of East London. Will the VCs of these institutions not learn something from Buckingham’s experience? It is to be hoped that they would at the very least approach Buckingham to ask pertinent questions? But perhaps a more likely contender for an organisation with sufficient gullibility is the Prince of Wales newly announced College of Integrated Medicine. [but see stop press]
The details of the story
The University of Buckingham (UB) is the only private university in the UK. Recently it announced its intention to start a school of medicine (the undergraduate component is due to start in September 2011). The dean of the new school is Karol Sikora.
Karol Sikora shot to fame after he appeared in a commercial in the USA. The TV commercial was sponsored by a far-right Republican campaign group, “Conservatives for Patients’ Rights” It designed to prevent the election of Barack Obama, by pouring scorn on the National Health Serrvice. A very curious performance. Very curious indeed. And then there was a bit of disagreement about the titles that he claimed to have.
As well as being dean of medicine at UB. Karol Sikora is also medical research director of CancerPartnersUK. a private cancer treatment company. He must be a very busy man.
Karol Sikora’s attitude to quackery is a mystery wrapped in an enigma. As well as being a regular oncologist, he is also a Foundation Fellow of that well known source of unreliable information, The Prince of Wales Foundation for Integrated Health. He spoke at their 2009 conference.
In the light of that, perhaps it is not, after all, so surprising thet the first action of UB’s medical school was to accredit a course a Diploma in Integrated Medicine. This course has been through two incarnations. The first prospectus (created 21 January 2009) advertised the course as being run by the British College of Integrated Medicine.But by the time that UB issued a press release in July 2009, the accredited outfit had changed its name to the Faculty of Integrated Medicine That grand title makes it sound like part of a university. It isn’t.

Rosy Daniel runs a company, Health Creation which, among other things, recommended a herbal concoction. Carctol. to "heal" cancer, . I wrote to Buckingham’s vice-chancellor (president), Terence Kealey, and attached a reprint of Ernst’s paper on Carctol. . Unlike most university vice-chancellors, he took it seriously. He asked me to meet Karol Sikora and Rosy Daniel to discuss it. After discovering who was teaching on this course, I wrote a document about their backgrounds and sent it to Terence Kealey. The outcome was that he removed Rosy Daniel as course director and appointed in her place Andrew Miles, with a brief to reorganise the course. A new prospectus, dated 4 September 2009, appeared. The course is not changed as much as I’d have hoped, although Miles assures me that while the lecture titles themselves may not have changed, he had ordered fundamental revisions to the teaching content and the teaching emphases.
In the new prospectus the British College of Integrated Medicine has been renamed as the Faculty of Integrated Medicine, but it appears to be otherwise unchanged. That’s a smart bit of PR. The word : “Faculty” makes it sound as though the college is part of a university. It isn’t. The "Faculty" occupies some space in the Apthorp Centre in Bath, which houses, among other things, Chiropract, Craniopathy (!) and a holistic vet,
The prospectus now starts thus.

The Advisory Board consists largely of well-know advocates of alternative medicine (more information about them below).

Most of these advisory board members are the usual promoters of magic medicine. But three of them seem quite surprising,Stafford Lightman, Nigel Sparrow and Nigel Mathers.
Stafford Lightman? Well actually I mentioned to him in April that his name was there and he asked for it to be removed, on the grounds that he’d had nothing to do with the course. It wasn’t removed for quite a while, but the current advisory board has none of these people. Nigel Sparrow and Nigel Mathers, as well as Lightman, sent letters of formal complaint to Miles and Terence Kealey, the VC of Buckingham, to complain that their involvement in Rosy Daniel’s set-up had been fundamentally misrepresented by Daniel. With these good scientists having extricated themselves from Daniel’s organisation, the FIM has only people who are firmly in the alternative camp (or quackery, as i’d prefer to call it). For example, people like Andrew Weil and George Lewith.
Andrew Weil, for example, while giving his address as the University of Arizona, is primarily a supplement salesman. He was recently reprimanded by the US Food and Drugs Administration
“Advertising on the site, the agencies said in the Oct. 15 letter, says “Dr. Weil’s Immune Support Formula can help maintain a strong defense against the flu” and claims it has “demonstrated both antiviral and immune-boosting effects in scientific investigation.”
The claims are not true, the letter said, noting the “product has not been approved, cleared, or otherwise authorized by FDA for use in the diagnosis, mitigation, prevention, treatment, or cure of the H1N1 flu virus.”
This isn’t the first time I’ve come across people’s names being used to support alternative medicine without the consent of the alleged supporter. There was, for example, the strange case of Dr John Marks and Patrick Holford.
Misrepresentation of this nature seems to be the order of the day. Could it be that people like Rosy Daniel are so insecure or, indeed, so unimportant within the Academy in real terms (where is there evidence of her objective scholarly or clinical stature?), that they seek to attach themselves, rather like limpets to fishing boats, to people of real stature and reputation, in order to boost their own or others’ view of themselves by a manner of proxy?
The background
When the course was originally proposed, a brochure appeared. It said accreditation by the University of Buckingham was expected soon.
Not much detail appeared in the brochure, Fine words are easy to write but what matters is who is doing th teaching. So I wrote to the vice-chancellor of Buckingham, Terence Kealey. I attached a reprint of Ernst’s paper on carctol, a herbal cancer ‘remedy’ favoured by Daniel (download the cached version of her claims, now deleted).
Terence Kealey
Kealey is regarded in much of academia as a far-right maverick, because he advocates ideas such as science research should get no public funding,and that universities should charge full whack for student fees. He has, in fact, publicly welcomed the horrific cuts being imposed on the Academy by Lord Mandelson. His piece in The Times started
“Wonderful news. The Government yesterday cut half a billion pounds from the money it gives to universities”
though the first comment on it starts
"Considerable accomplishment: to pack all these logical fallacies and bad metaphors in only 400 words"
He and I are probably at opposite ends of the political spectrum. Yet he is the only VC who has been willing to talk about questions like this. Normally letters to vice-chancellors about junk degrees go unanswered. Not so with Kealey. I may disagree with a lot of his ideas, but he is certainly someone you can do business with.
Kealey responded quickly to my letter, sent in January 2009, pointing out that Rosy Daniel’s claims about Carctol could not be supported and were possibly illegal. He asked me to meet Sikora and Daniel. I met first Sikora alone, and then, on March 19 2009, both together. Rosy Daniel gave me a complete list of the speakers she’d chosen to teach on this new Diploma on IM.
After discovering who was to teach on the proposed course, I wrote a long document about the proposed speakers and sent it to Terence Kealey on March 23rd 2009. It contained many names that will be familiar to anyone who has taken an interest in crackpot medicine, combined with a surprisingly large element of vested financial interests. Unlike most VCs, Kealey took it seriously.
The remarkable thing about this meeting was that I asked Sikora how many names where familiar to him on the list of people who had been chosen by Rosy Daniel to teach on the course. His answer was "none of them". Since his name and picture feature in all the course descriptions, this seemed like dereliction of duty to me.
After seeing my analysis of the speakers, Terence Kealey reacted with admirable speed. He withdrew the original brochure, demoted Rosy Daniel (in principle anyway) and brought in Prof Andrew Miles to take responsibility for the course. This meant that he had to investigate the multiple conflicts of interests of the various speakers and to establish some sort of way forward in the ‘mess’ of what had been agreed before Miles’ appointment to Buckingham
Andrew Miles.
Miles is an interesting character, a postdoctoral neuroendocrinologist, turned public health scientist. I’d come across him before as editor-in-chief of the Journal of Evaluation in Clinical Practice This is a curious journal that is devoted mainly to condemning Evidence Based Medicine. Much of its content seems to be in a style that I can only describe as post-modernist-influenced libertarian.
The argument turns on what you mean by ‘evidence’ and, in my opinion, Miles underestimates greatly the crucial problem of causality, a problem that can be solved only by randomisation, His recent views on the topic can be read here.
An article in Miles’ journal gives its flavour: "Andrew Miles, Michael Loughlin and Andreas Polychronis, Medicine and evidence: knowledge and action in clinical practice". Journal of Evaluation in Clinical Practice 2007, 13, 481–503 [download pdf]. This paper launches an attack on Ben Goldacre, in the following passage.
“Loughlin identifies Goldacre [36] as a particularly luminous example of a commentator who is able not only to combine audacity with outrage, but who in a very real way succeeds in manufacturing a sense of having been personally offended by the article in question. Such moralistic posturing acts as a defence mechanism to protect cherished assumptions from rational scrutiny and indeed to enable adherents to appropriate the ‘moral high ground’, as well as the language of ‘reason’ and ‘science’ as the exclusive property of their own favoured approaches. Loughlin brings out the Orwellian nature of this manoeuvre and identifies a significant implication.”
"If Goldacre and others really are engaged in posturing then their primary offence, at least according to the Sartrean perspective adopted by Murray et al. is not primarily intellectual, but rather it is moral. Far from there being a moral requirement to ‘bend a knee’ at the EBM altar, to do so is to violate one’s primary duty as an autonomous being.”
This attack on one of my heroes was occasioned because he featured one of the most absurd pieces of post-modernist bollocks ever, in his Guardian column in 2006. I had a go at the same paper on this blog, as well as an earlier one by Christine Barry, along the same lines. There was some hilarious follow-up on badscience.net. After this, it is understandable that I had not conceived a high opinion of Andrew Miles. I feared that Kealey might have been jumping out of the frying pan into the fire.
After closer acquaintance I have changed my mind, In the present saga Andrew Miles has done an excellent job. He started of sending me links to heaven knows how many papers on medical epistemology, to Papal Encyclicals on the proposed relationship between Faith and Reason and on more than one occasion articles from the Catholic Herald (yes, I did read it). This is not entirely surprising, as Miles is a Catholic priest as well as a public health academic, so has two axes to grind. But after six months of talking, he now sends me links to junk science sites of the sort that I might get from, ahem, Ben Goldacre.
Teachers on the course
Despite Andrew Miles best efforts, he came in too late to prevent much of the teaching being done in the parallel universe of alternative medicine, The University of Buckingham had a pre-Miles, legally-binding contract (now terminated) with the Faculty of Integrated Medicine, and the latter is run by Dr Rosy Daniel and Dr Mark Atkinson. Let’s take a look at their record.
Rosy Daniel BSc, MBBCh
Dr Rosy Daniel first came to my attention through her commercial web site, Health Creation. This site, among other things, promoted an untested herbal concoction, Carctol, for "healing" cancer.
Carctol: Profit before Patients? is a review by Edzard Ernst of the literature, such as it is, and concludes
Carctol and the media hype surrounding it must have given many cancer patients hope. The question is whether this is a good or a bad thing. On the one hand, all good clinicians should inspire their patients with hope [6]. On the other hand, giving hope on false pretences is cruel and unethical. Rosy Daniel rightly points out that all science begins with observations [5]. But all science then swiftly moves on and tests hypotheses. In the case of Carctol, over 20 years of experience in India and almost one decade of experience in the UK should be ample time to do this. Yet, we still have no data. Even the small number of apparently spectacular cases observed by Dr. Daniel have not been published in the medical literature.
On this basis I referred Health Creation to Trading Standards officer for a prima facie breach of the Cancer Act 1939. ]Download the complaint document]. Although no prosecution was brought by Trading Standards, they did request changes in the claims that were being made. Here is an example.
A Google search of the Health Creation site for “Carctol” gives a link
Dr Daniel has prescribed Carctol for years and now feels she is seeing a breakthrough. Dr Daniel now wants scientists to research the new herbal medicine
But going to the link produces
Access denied.
You are not authorized to access this page.
You can download the cached version of this page, which shows the sort of claims that were being made before Trading Standards Officers stepped in. There are now only a few oblique references to Carctol on the Health Creation site, e.g. here..
Both Rosy Daniel and Karol Sikora were speakers at the 2009 Princes’s Foundation Conference, in some odd company.
Mark Atkinson MBBS BSc (Hons) FRIPH
Dr Mark Atkinson is co-leader of the FiM course. He is also a supplement salesman, and he has promoted the Q-link pendant. The Q-link pendant is a simple and obvious fraud designed to exploit paranoia about WiFi killing you. When Ben Goldacre bought one and opened it. He found
“No microchip. A coil connected to nothing. And a zero-ohm resistor, which costs half a penny, and is connected to nothing.”
Nevertheless, Mark Atkinson has waxed lyrical about this component-free device.
“As someone who used to get tired sitting in front of computers and used to worry about the detrimental effects of external EMF’s, particularly as an avid user of mobile phones, I decided to research the various devices and technologies on the market that claim to strengthen the body’s subtle energy fields. It was Q Link that came out top. As a Q link wearer, I no longer get tired whilst at my computer, plus I’m enjoying noticeably higher energy levels and improved mental performance as a result of wearing my Q Link. I highly recommend it.” Dr Mark Atkinson, Holistic Medical Physician
Mark Atkinson is also a fan of Emo-trance. He wrote, In Now Magazine,
"I wanted you to know that of all the therapies I’ve trained in and approaches that I have used (and there’s been a lot) none have excited me and touched me so deeply than Emotrance."
"Silvia Hartmann’s technique is based on focusing your thoughts on parts of your body and guiding energy. It can be used for everything from insomnia to stress. The good news is that EmoTrance shows you how to free yourself from these stuck emotions and release the considerable amounts of energy that are lost to them."
Aha so this particular form of psychobabble is the invention of Silvia Hartmann. Silvia Hartmann came to my attention because her works feature heavily in on of the University of Westminster’s barmier “BSc” degrees, in ‘naturopaths’, described here. She is fanous, apart from Emo-trance, for her book Magic, Spells and Potions
“Dr Hartmann has created techniques that will finally make magic work for you in ways you never believed to be possible.”
Times Higher Education printed a piece with the title ‘Energy therapy’ project in school denounced as ‘psychobabble’. They’d phoned me a couple of days earlier to see whether I had an opinion about “Emotrance”. As it happens, I knew a bit about it because it had cropped up in a course given at, guess where, the University of Westminster . It seems that a secondary school had bought this extreme form of psychobabble. The comments on the Times Higher piece were unusually long and interesting.
It turned out that the inventor of “Emotrance”, Dr Silvia Hartmann PhD., not only wrote books about magic spells and potions, but also that her much vaunted doctorate had been bought from the Universal Life Church, current cost $29.99.
The rest of the teachers
The rest of the teachers on the course, despite valiant attempts at vetting by Andrew Miles, includes many names only too well-known to anybody who has taken and interest in pseudo-scientific medicine. Here are some of them.
Damien Downing:, even the Daily Mail sees through him. Enough said.
Kim Jobst, homoepath and endorser of the obviously fraudulent Q-link
pendant. His Plaxo profile says
About Kim A. Jobst
Consultant, Wholystic Care Physician [sic!] , Medical Homoeopath, Specialist in Neurodegeneration and Dementia, using food state nutrition, diet and lifestyle to facilitate Healing and Growth;
Catherine Zollman, Well known ally of HRH and purveyer of woo.
Harald Walach, another homeopath, fond of talking nonsense about "quantum effects".
Nicola Hembry, a make-believe nutritionist and advocate of vitamin C and laetrile for cancer
Simon Mills, a herbalist who is inclined to diagnoses like “hot damp”, ro be treated with herbs that tend to “cool and dry.”
David Peters, of the University of Westminster. Enough said.
Nicola Robinson of Thames Valley University. Advocate of unevidenced treatmsnts.
Michael Dixon, of whom more here.
And last but not least,
Karol Sikora.
The University of Buckingham removes accreditation of the Faculty of Integrated Medicine
The correspondence has been long and, at times, quite blunt. Here are a few quotations from it, The University of Buckingham, being private, is exempt from the Freedom of Information Act (2000) but nevertheless they have allowed me to reproduce the whole of the correspondence. The University, through its VC, Terence Keeley, has been far more open than places that are in principle subject to FOIA, but which, in practice, always try to conceal material. I may post the lot, as time permits, but meanwhile here are some extracts. They make uncomfortable reading for advocates of magic medicine.
Miles to Daniel, 8 Dec 2009
” . . . now that the University has taken his [Sikora’s] initial advice in trialing the DipSIM and has found it cost-ineffective, the way forward is therefore to alter that equation through more realistic financial contribution from IHT/FIM at Bath or to view the DipSIM as an experiment that has failed and which must give way to other more viable initiatives."
"The University is also able to confirm that we hold no interest in jointly developing any higher degrees on the study of IM with IHT/FIM at Bath. This is primarily because we are developing our own Master’s degree in Medicine of the Person in collaboration with various leading international societies and scholars including the WHO and which is based on a different school of thought. "
Miles to Daniel 15 Dec 2009
"Dear Rosy
It appears that you have not fully assimilated the content of my earlier e-mails and so I will reiterate the points I have already made to you and add to them.
The DipSIM is an external activity – in fact, it is an external collaboration and nothing more. It is not an internal activity and neither is it in any way part of the medical school and neither will it become so and so the ‘normal rules’ of academic engagement and scholarly interchange do not apply. Your status is one of external collaborator and not one of internal or even visiting academic colleague. There is no “joint pursuit” of an academically rigorous study of IM by UB and IHT/FIM beyond the DipSIM and there are no plans, and never have been, for the “joint definition of research priorities” in IM. The DipSIM has been instituted on a trial basis and this has so far shown the DipSIM to be profoundly cost-ineffective for the University. You appear to misunderstand this – deliberately or otherwise."
Daniel to Miles 13 Jan 2010
"However, I am aware that weather permitting you and Karol will be off to the Fellows meeting for the newly forming National College (for which role I nominated you to Dr Michael Dixon and Prof David Peters.)
I have been in dialogue with Michael and Boo Armstrong from FIH and they are strongly in favour of forming a partnership with FIM so that we effectively become one of many new faculties within the College (which is why we change our name to FIM some months ago).
I have told Michael about the difficulties we are having and he sincerely hopes that we can resolve them so that we can all move forward as one. "
Miles to Daniel 20 Jan 2010
"Congratulations on the likely integration of your organisation into the new College of Integrative Health which will develop out of the Prince’s Foundation for Integrated Health. This
will make an entirely appropriate home for you for the longer term.Your image of David Colquhoun "alive and kicking" as the Inquisitor General, radiating old persecutory energy and believing "priestess healers" (such as you describe youself) to be best "tortured, drowned and even burnt alive", will remain with me, I suspect, for many years to come (!). But then, as the Inquisitor General did say, ‘better to burn in this life than in the next’ (!). Overall, then, I reject your conclusion on the nature of the basis of my decision making and playfully suggest that it might form part of the next edition of Frankfurt’s recent volume ["On Bullshit] http://press.princeton.edu/titles/7929.html I hope you will forgive my injection of a little academic humour in an otherwise formal and entirely serious communication.
The nature of IM, with its foundational philosophy so vigorously opposed by mainstream medicine and the conitnuing national and international controversies which engulf homeopaths, acupuncturists, herbalists, naturopaths, transcendental meditators, therapeutic touchers, massagers, reflexologists, chiropractors, hypnotists, crystal users, yoga practitioners, aromatherapists, energy channelers, chinese medicine practitioners et al, can only bring the University difficulties as we seek to establish a formal and internationally recognised School of Medicine and School of Nursing.
I do not believe my comments in relation to governance at Bath are "offensive". They are, on the contrary, entirely accurate and of concern to the University. There have been resignations at senior level from your Board due to misrepresentation of your position and there has been a Trading Standards Authority investigation into further instances of misrepresentation. I am advised that an audit is underway of your compliance with the Authority’s instructions. You have therefore not dealt with my concerns, you have merely described them as "offensive".
I note from your e-mail that you are now in discussions with other universities and given the specific concerns of the University of Buckingham which I have dealt with exhaustively in this and other correspondences and the incompatibility of the developments at UB with the DipSIM and your own personal ambitions, etc., I believe you to have taken a very wise course and I wish you well in your negotiations. In these circumstances I feel it appropriate to enhance those negotiations by confirming that the University of Buckingham will not authorise the intake of a second cohort of students and that the relationship between IHT and the University will cease following the graduation of those members of the current course that are successful in their studies – the end of February 2011."
From Miles 2 Feb 2010
"Here is the list of teachers – you can subtract me (I withdrew from teaching when the antics ay Bath started) and also Professor John Cox (Former President of The Royal College of Psychiatrists and Former Secretary General of the World Psychiatric Association) who withdrew when he learned of some of the stuff going on…. Karol Sikora continues to teach. Michael Loughlin and Carmel Martin are both good colleagues of mine and, I can assure you – taught the students solid stuff! Michael taught medical epistemology and Carmel the emerging field of systems complexity in health services (Both of them have now withdrawn from teaching commitments).
The tutors shown are described by Rosy as the finest minds in IM teaching in the country. I interviewed tham all personally on (a) the basis of an updated CV & (b) via a 30 min telephone interview with me personally. Some were excluded from teaching because they were not qualified to do so academically (e.g. Boo Armstrong, Richard Falmer, not even a first degree, etc, etc., but gave a short presentation in a session presided over by an approved teacher) and others were approved because of their academic qualifications, PhD, MD, FRCP etc etc etc) and activity within the IM field. Each approved teacher was issued with highly specific teaching guidance form me (no bias, reference to opposing schools of thought, etc etc) and each teacher was required to complete and sign a Conflicts of Interest form. All of these documentations are with me here. Short of all this governance it’s impossible to bar them from teaching because who else would then do it?! Anyway, the end is in sight – Hallelujah! "
From Miles 19 Feb 2010
"Dear David
Just got back to the office after an excellent planning meeting for the new Master’s Degree in Person-centred Medicine and a hearty (+ alcoholic) lunch at the Ath! Since I shall never be a FRS, the Ath seems to me the next best ‘club’ (!). Michael Baum is part of the steering committee and you might like to take his thoughts on the direction of the programme. Our plans may even find their way into your Blog as an example of how to do things (vs how not to do things, i.e. CAM, IM, etc!). This new degree will sit well alongside the new degrees in Public Health – i.e. the population/utilitarian outlook of PH versus the individual person-centred approach., etc. "
And an email from a senior UB spokesperson
"Rumour has it that now that Buckingham has dismissed the ‘priestess healer of Bath’, RD [Rosy Daniel] , explorations are taking place with other universities, most of which are subject to FoI request from DC at the time of writing. Will these institutions have to make the same mistakes Buckingham did before taking the same action? Rumour also has it that RD changed the name of her institution to FIM in order to fit neatly into the Prince’s FIH, a way, no doubt, of achieving ‘protection’ and ‘accreditation’ in parallel with particularly lucrative IM ‘education’ (At £9,000 a student and with RD’s initial course attracting 20 mainly GPs, that’s £180,00 – not bad business…. And Buckingham’s ‘share of this? £12,000!”
The final bombshell; even the Prince of Wales’ FIH rejects Daniel and Atkinson?
Only today (31 March) I was sent, from a source that I can’t reveal, an email which comes from someone who "represent the College and FIH . . . ".. This makes it clear that the letter comes from the Prince of Wales’ Foundation for Integrated Health
|
Dr Rosy Daniel BSc MBBCh Director of the Faculty of Integrated Medicine Medical Director Health Creation 30th March 2010 RE: Your discussion paper and recent correspondence Thank you for meeting with [XXXXXX] and myself this evening to discuss your proposals concerning a future relationship between your Faculty of Integrated Medicine and the new College. As you know, he and I have been asked to represent the College and FIH in this matter. We are aware of difficulties facing your organisations and the FIM DipSIM course. As a consequence of these, it is not possible for the College to enter into an association with you, any of your organisations nor the DipSIM course at the present time. It would, therefore, be wrong to represent to others that any such association has been agreed. You will appreciate that, in these circumstances, you will not receive an invitation to the meeting of 15th April 2010 nor to other planned events. I am sorry to disappoint you in this matter. Yours sincerely |
Conclusions
I’ll confess to feeling almost a little guilty for having appeared to persecute the particular individuals involved in thie episode. But patients are involved and so is the law, and both of these are more important than individuals, The only unfair aspect is that, while it seems that even the Prince of Wales’ Foundation for Integrated Health has rejected Daniel and Atkinson, that Foundation embraces plenty of people who are just as deluded, and potentially dangerous, as those two. The answer to that problem is for the Prince to stop endorsing treatments that don’t work.
As for the University of Buckingham. Well, despite the ‘right wing maverick’ Kealey and the ‘anti-evidence’ Miles, I really think they’ve done the right thing. They’ve listened, they’ve maintained academic rigour and they’ve released all information for which I asked and a lot more. Good for them, I say.
Follow-up
15 April 2010. This story was reported by Times Higher Education, under the title “It’s terminal for integrated medicine diploma“. That report didn’t attract comments. But on 25th April Dr Rosy Daniel replied with “‘Terminal’? We’ve only just begun“. This time there were some feisty responses. Dr Daniel really should check her facts before getting into print.
3 March 2011. Unsurprisingly, Dr Daniel is up and running again, under the name of the British College of Integrated Medicine. The only change seems to be that Mark Atkinson has jumped ship altogether, and, of course, she is now unable to claim endorsement by Buckingham, or any other university. Sadly, though, Karol Sikora seems to have learned nothing from the saga related above. He is still there as chair of the Medical Advisory Board, along with the usual suspects mentioned above.
There is no topic more widely discussed than what one should eat in order to stay healthy. And there are few topics where there evidence is so lacking in quality. This post isn’t about quackery, but about something much more important. it is about the real science (if it merits that description) behind dietary advice. I’m not an expert in nutrition, but I do know a bit about the nature of evidence. I’m continually astonished by the weakness of the evidence for some things that have become received truths, and nowhere is that more true than in nutrition.
|
The BMJ used my review of Gary Taube’s book, The Diet Delusion, to start off their new Round Table feature [full text link to BMJ]. The published version had some big cuts so I publish the original version here. Taubes was kind enough to send me a copy of the book after I’d mentioned his wonderful New York Times piece in my previous excursion into the murky world of diet and health, Diet and health. What can you believe: or does bacon kill you? |
|
The biggest omission in the BMJ version was Taubes’ own ten point summary of his conclusions (on page 454).
"“As I emerge from this research, though, certain conclusions seem inescapable to me, based on existing knowledge
- Dietary fat, whether saturated or not, is not a cause of obesity, heart disease, or any other chronic disease of civilization
- The problem is the carbohydrates in the diet, their effect on insulin secretion, and thus the hormonal regulation of homeostasis – the entire harmonic ensemble of the human body. The more easily digestible and refined the carbohydrates, the greater the effect on our health, weight, and well-being.
- Sugars – sucrose and high-fructose corn syrup specifically – are particularly harmful, probably because the combination of fructose and glucose simultaneously elevates insulin levels while overloading the liver with carbohydrates.
- Through their direct effect on insulin and blood sugar, refined carbohydrates, starches, and sugars are the dietary cause of coronary heart disease and diabetes. They are the most likely dietary causes of cancer, Alzheimer’s disease, and the other chronic diseases of civilization.
- Obesity is a disorder of excess fat accumulation, not overeating, and not sedentary behaviour.
- Consuming excess calories does not cause us to grow fatter, any more than it causes a child to grow taller. Expending more energy than we consume does not lead to long-term weight loss; it leads to hunger.
- Fattening and obesity are caused by an imbalance – a disequilibrium – in the hormonal regulation of adipose tissue and fat metabolism. Fat synthesis and storage exceed the mobilization of fat from the adipose tissue and its subsequent oxidation. We become leaner when the hormonal regulation of the fat tissue reverses this balance.
- Insulin is the primary regulator of fat storage. When insulin levels are elevated – either chronically or after a meal – we accumulate fat in our fat tissue. When insulin levels fall, we release fat from our fat tissue and use it for fuel.
- By stimulating insulin secretion, carbohydrates make us fat and ultimately cause obesity. The fewer carbohydrates we consume, the leaner we will be.
- By driving fat accumulation, carbohydrates also increase hunger and decrease the amount of energy we expend in metabolism and physical activity.”
It is on these bases that Taubes suggests that the increase in obesity is, in part, a consequence of the recommendation of a low fat, and hence high sugar diet.
|
The Diet Delusion [ pp 601] (published in the USA as Good Calories, Bad Calories) Gary Taubes 2008 There is no topic more widely discussed than what one should eat in order to stay healthy. And there are few topics where the evidence is so lacking in quality. It is also a topic that is besieged by gurus, cranks and supplement hucksters. You need to beware of misleading titles. Dietitians are good. Nutritionists are sometimes good. But titles like ‘nutritional therapist’ and ‘nutritional medicine’ are usually warning signs of alternative therapists and/or pill salespeople. Gary Taubes is a journalist, but he is quite an exceptional journalist. His account of the importance of randomisation for the establishment of causality is one of the best ever and it was published not in an academic journal, but in the New York Times [1]. His book, The Diet Delusion, is in the same mould. It is more complete and more scholarly than most professional scientists could manage. Not only does it cover the literature right back to Samuel Johnson, but it is also particularly good at unravelling what one might call the politics of science. And by politics I don’t mean the vast lobbying industry that has built up with the aim of selling you unnecessary supplements, but the politics of academia. Obesity sounds simple. If you are fat it is because you eat too much or exercise too little, right? Well no, it’s not as simple as that. For a start, it has been shown time and time again that low fat diets, and exercise, have small and temporary effects on weight. The problem with diet and health revolves round causality. The law of conservation of energy is an inevitable truth, but says nothing about causality. It could imply that you get fat because you eat too much, or equally the causal arrow could point the other way and “we eat more, move less and have less energy to expend because we are metabolically or hormonally driven to get fat”. The assumption that positive caloric balance is the cause of weight gain has predominated since the 1970s and “this simple misconception has led to a century of misguided obesity research”. At the heart of the problem is the paucity of randomised trials, which are the only way to establish causality. Those that there are have usually shown that diet does not matter as much as we are told. Taubes concludes
I think it can certainly be argued that the problem of causality has been greatly underestimated. We are warned constantly of the dangers of processed meat, on the basis of very unconvincing evidence [2]. This is one reason why we still know so little about the causes of obesity, diabetes and heart disease. For Taubes, a major villain was the US nutritionist Ancel Keys (1904 – 2004). His It is quite possible that there was rather more to be said for the Atkins diet than was apparent at the time. The fact that Atkins was not a university scientist, that his views were extreme and that he was so obviously out to make a lot of money from it, gave him all the appearance of being yet another profiteering diet guru. He was dismissed by the medical establishment as a quack. Taubes points out that conflict of interest cuts both ways. Atkins’ sternest critics at Harvard were funded by General Foods, Coca-Cola and the sugar industry. It adds up to a sorry story of a conflict of vested interests and scientific vanity. Taubes’ final judgement is harsh. He quotes Robert Merton’s description [4] of what science is, or should be.
He then comments
It took Taubes five years to write this book, and he has nothing to sell apart from his ideas. No wonder it is so much better than a scientist can produce. Such is the corruption of science by the cult of managerialism that no university would allow you to spend five years on a book [5]. I find all ten points in his summary convincing. But his most important conclusion is that you cannot have any certainty without randomised trials. The business of nutrition is greatly at fault for not having put more effort into organising randomised trials. Until they are done, we’ll never really know, and we shouldn’t pretend that we do. 1. Taubes G. Do we really know what makes us healthy? New York Times 2007 Sep 16.[full text link] [pdf file] 2. Colquhoun, D. (3 May 2009) Diet and health. What can you believe: or does bacon kill you?. 3. Greenberg, S.A.. 2009 How citation distortions create unfounded authority: analysis of a citation network. BMJ ;339:b2680 [pdf file]. 4. Merton, R. K. Behavior Patterns of Scientists . Leonardo, Vol.3 1970; 3(2):213-220. From Jstor [or pdf file] 5. Lawrence PA. The mismeasurement of science. Curr Biol 2007; 17(15):R583-R585.PM:17686424 [pdf file] [commentary] |
If length had allowed, there should certainly have been a reference here to Robert Lustig of UCSF. He is an academic nutritionist who supports the main thesis of Taubes’ book. See, for example, his 2005 review, Childhood obesity: behavioral aberration or biochemical drive? Reinterpreting the First Law of Thermodynamics [full
text link]. Lustig’s slide show, The Trouble with Fructose is available in the NIH web site.
There are a couple of other articles by Taubes that are well worth reading. The Scientist and the Stairmaster Why most of us believe that exercise makes us thinner—and why we’re wrong. Gary Taubes, in New York Magazine, and We can’t work it out, in the Guardian.
You can see Taubes in action on YouTube, for example in “on Cholesterol and Science Practices“, and “on Carbohydrates and Degenerative Diseases“. There is also a video of Taubes on medical grand rounds at Dartmouth-Hitchcock Medical Center in June 2009. You can see Robert Lustig on YouTube too: “Sugar: The Bitter Truth“.
Follow-up
22 December.2009, Unlike the serious questions dealt with in the Diet Delusion, this concerns merely another bit of the ubiquitous nutribollocks that crops up in the media, While writing this I was listening to the excellent early evening news programme, PM, run by Eddie Mair, when a diet-related topic came up, it was nonsense about how a cocktail made with vodka, cointreau, acai juice and pomegranate juice would not give you a hangover. I suppose it was meant as christmas fun but whenever I hear the words ‘antioxidant‘ or ‘superfood; I feel an email coming on. It seems that Eddie Mair liked the fact that the email contained the words ‘quack’ and ‘codswallop’ because the next thing I knew I was asked to give an interview on next day’s programme. The mp3 is here.
This article has been reposted on The Winnower, and now has a digital object identifier DOI: 10.15200/winn.142934.47856
This post is not about quackery, nor university politics. It is about inference, How do we know what we should eat? The question interests everyone, but what do we actually know? Not as much as you might think from the number of column-inches devoted to the topic. The discussion below is a synopsis of parts of an article called “In praise of randomisation”, written as a contribution to a forthcoming book, Evidence, Inference and Enquiry.
About a year ago just about every newspaper carried a story much like this one in the Daily Telegraph,
|
Sausage a day can increase bowel cancer risk By Rebecca Smith, Medical Editor Last Updated: 1:55AM BST 31/03/2008
|
||||
What, I wondered, was the evidence behind these dire warnings. They did not come from a lifestyle guru, a diet faddist or a supplement salesman. This is nothing to do with quackery. The numbers come from the 2007 report of the World Cancer Research Fund and American Institute for Cancer Research, with the title ‘Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective‘. This is a 537 page report with over 4,400 references. Its panel was chaired by Professor Sir Michael Marmot, UCL’s professor of Epidemiology and Public Health. He is a distinguished epidemiologist, renowned for his work on the relation between poverty and health.
Nevertheless there has never been a randomised trial to test the carcinogenicity of bacon, so it seems reasonable to ask how strong is the evidence that you shouldn’t eat it? It turns out to be surprisingly flimsy.
In praise of randomisation
Everyone knows about the problem of causality in principle. Post hoc ergo propter hoc; confusion of sequence and consequence; confusion of correlation and cause. This is not a trivial problem. It is probably the main reason why ineffective treatments often appear to work. It is traded on by the vast and unscrupulous alternative medicine industry. It is, very probably, the reason why we are bombarded every day with conflicting advice on what to eat. This is a bad thing, for two reasons. First, we end up confused about what we should eat. But worse still, the conflicting nature of the advice gives science as a whole a bad reputation. Every time a white-coated scientist appears in the media to tell us that a glass of wine per day is good/bad for us (delete according to the phase of the moon) the general public just laugh.
In the case of sausages and bacon, suppose that there is a correlation between eating them and developing colorectal cancer. How do we know that it was eating the bacon that caused the cancer – that the relationship is causal? The answer is that there is no way to be sure if we have simply observed the association. It could always be that the sort of people who eat bacon are also the sort of people who get colorectal cancer. But the question of causality is absolutely crucial, because if it is not causal, then stopping eating bacon won’t reduce your risk of cancer. The recommendation to avoid all processed meat in the WCRF report (2007) is sensible only if the relationship is causal. Barker Bausell said:
[Page39] “But why should nonscientists care one iota about something as esoteric as causal inference? I believe that the answer to this question is because the making of causal inferences is part of our job description as Homo Sapiens.”
That should be the mantra of every health journalist, and every newspaper reader.
|
The essential basis for causal inference was established over 70 years ago by that giant of statistics Ronald Fisher, and that basis is randomisation. Its first popular exposition was in Fisher’s famous book, The Design of Experiments (1935). The Lady Tasting Tea has become the classical example of how to design an experiment. . |
|
Briefly, a lady claims to be able to tell whether the milk was put in the cup before or after the tea was poured. Fisher points out that to test this you need to present the lady with an equal number of cups that are ‘milk first’ or ‘tea first’ (but otherwise indistinguishable) in random order, and count how many she gets right. There is a beautiful analysis of it in Stephen Senn’s book, Dicing with Death: Chance, Risk and Health. As it happens, Google books has the whole of the relevant section Fisher’s tea test (geddit?), but buy the book anyway. Such is the fame of this example that it was used as the title of a book, The Lady Tasting Tea was published by David Salsburg (my review of it is here)
Most studies of diet and health fall into one of three types, case-control studies, cohort (or prospective) studies, or randomised controlled trials (RCTs). Case-control studies are the least satisfactory: they look at people who already have the disease and look back to see how they differ from similar people who don’t have the disease. They are retrospective. Cohort studies are better because they are prospective: a large group of people is followed for a long period and their health and diet is recorded and later their disease and death is recorded. But in both sorts of studies,each person decides for him/herself what to eat or what drugs to take. Such studies can never demonstrate causality, though if the effect is really big (like cigarette-smoking and lung cancer) they can give a very good indication. The difference in an RCT is that each person does not choose what to eat, but their diet is allocated randomly to them by someone else. This means that, on average, all other factors that might influence the response are balanced equally between the two groups. Only RCTs can demonstrate causality.
Randomisation is a rather beautiful idea. It allows one to remove, in a statistical sense, bias that might result from all the sources that you hadn’t realised were there. If you are aware of a source of bias, then measure it. The danger arises from the things you don’t know about, or can’t measure (Senn, 2004; Senn, 2003). Although it guarantees freedom from bias only in a long run statistical sense, that is the best that can be done. Everything else is worse.
Ben Goldacre has referred memorably to the newspapers’ ongoing “Sisyphean task of dividing all the inanimate objects in the world into the ones that either cause or cure cancer” (Goldacre, 2008). This has even given rise to a blog. “The Daily Mail Oncological Ontology Project“. The problem arises in assessing causality.
It wouldn’t be so bad if the problem were restricted to the media. It is much more worrying that the problem of establishing causality often seems to be underestimated by the authors of papers themselves. It is a matter of speculation why this happens. Part of the reason is, no doubt, a genuine wish to discover something that will benefit mankind. But it is hard not to think that hubris and self-promotion may also play a role. Anything whatsoever that purports to relate diet to health is guaranteed to get uncritical newspaper headlines.
At the heart of the problem lies the great difficulty in doing randomised studies of the effect of diet and health. There can be no better illustration of the vital importance of randomisation than in this field. And, notwithstanding the generally uncritical reporting of stories about diet and health, one of the best accounts of the need for randomisation was written by a journalist, Gary Taubes, and it appeared in the New York Times (Taubes, 2007).
The case of hormone replacement therapy
In the 1990s hormone replacement therapy (HRT) was recommended not only to relieve the unpleasant symptoms of the menopause, but also because cohort studies suggested that HRT would reduce heart disease and osteoporosis in older women. For these reasons, by 2001, 15 million US women (perhaps 5 million older women) were taking HRT (Taubes, 2007). These recommendations were based largely on the Harvard Nurses’ Study. This was a prospective cohort study in which 122,000 nurses were followed over time, starting in 1976 (these are the ones who responded out of the 170,000 requests sent out). In 1994, it was said (Manson, 1994) that nearly all of the more than 30 observational studies suggested a reduced risk of coronary heart disease (CHD) among women receiving oestrogen therapy. A meta-analysis gave an estimated 44% reduction of CHD. Although warnings were given about the lack of randomised studies, the results were nevertheless acted upon as though they were true. But they were wrong. When proper randomised studies were done, not only did it turn out that CHD was not reduced: it was actually increased.
The Women’s Health Initiative Study (Rossouw et al., 2002) was a randomized double blind trial on 16,608 postmenopausal women aged 50-79 years and its results contradicted the conclusions from all the earlier cohort studies. HRT increased risks of heart disease, stroke, blood clots, breast cancer (though possibly helped with osteoporosis and perhaps colorectal cancer). After an average 5.2 years of follow-up, the trial was stopped because of the apparent increase in breast cancer in the HRT group. The relative risk (HRT relative to placebo) of CHD was 1.29 (95% confidence interval 1.02 to 1.63) (286 cases altogether) and for breast cancer 1.26 (1.00 -1.59) (290 cases). Rather than there being a 44% reduction of risk, it seems that there was actually a 30% increase in risk. Notice that these are actually quite small risks, and on the margin of statistical significance. For the purposes of communicating the nature of the risk to an individual person it is usually better to specify the absolute risk rather than relative risk. The absolute number of CHD cases per 10,000 person-years is about 29 on placebo and 36 on HRT, so the increased risk of any individual is quite small. Multiplied over the whole population though, the number is no longer small.
Several plausible reasons for these contradictory results are discussed by Taubes,(2007): it seems that women who choose to take HRT are healthier than those who don’t. In fact the story has become a bit more complicated since then: the effect of HRT depends on when it is started and on how long it is taken (Vandenbroucke, 2009).
This is perhaps one of the most dramatic illustrations of the value of randomised controlled trials (RCTs). Reliance on observations of correlations suggested a 44% reduction in CHD, the randomised trial gave a 30% increase in CHD. Insistence on randomisation is not just pedantry. It is essential if you want to get the right answer.
Having dealt with the cautionary tale of HRT, we can now get back to the ‘Sisyphean task of dividing all the inanimate objects in the world into the ones that either cause or cure cancer’.
The case of processed meat
The WCRF report (2007) makes some pretty firm recommendations.
- Don’t get overweight
- Be moderately physically active, equivalent to brisk walking for at least 30 minutes every day
- Consume energy-dense foods sparingly. Avoid sugary drinks. Consume ‘fast foods’ sparingly, if at all
- Eat at least five portions/servings (at least 400 g or 14 oz) of a variety of non-starchy vegetables and of fruits every day. Eat relatively unprocessed cereals (grains) and/or pulses (legumes) with every meal. Limit refined starchy foods
- People who eat red meat to consume less than 500 g (18 oz) a week, very little if any to be processed.
- If alcoholic drinks are consumed, limit consumption to no more than two drinks a day for men and one drink a day for women.
- Avoid salt-preserved, salted, or salty foods; preserve foods without using salt. Limit consumption of processed foods with added salt to ensure an intake of less than 6 g (2.4 g sodium) a day.
- Dietary supplements are not recommended for cancer prevention.
These all sound pretty sensible but they are very prescriptive. And of course the recommendations make sense only insofar as the various dietary factors cause cancer. If the association is not causal, changing your diet won’t help. Note that dietary supplements are NOT recommended. I’ll concentrate on the evidence that lies behind “People who . . . very little if any to be processed.”
The problem of establishing causality is dicussed in the report in detail. In section 3.4 the report says
” . . . causal relationships between food and nutrition, and physical activity can be confidently inferred when epidemiological evidence, and experimental and other biological findings, are consistent, unbiased, strong, graded, coherent, repeated, and plausible.”
The case of processed meat is dealt with in chapter 4.3 (p. 148) of the report.
“Processed meats” include sausages and frankfurters, and ‘hot dogs’, to which nitrates/nitrites or other preservatives are added, are also processed meats. Minced meats sometimes, but not always, fall inside this definition if they are preserved chemically. The same point applies to ‘hamburgers’.
The evidence for harmfulness of processed meat was described as “convincing”, and this is the highest level of confidence in the report, though this conclusion has been challenged (Truswell, 2009) .
How well does the evidence obey the criteria for the relationship being causal?
Twelve prospective cohort studies showed increased risk for the highest intake group when compared to the lowest, though this was statistically significant in only three of them. One study reported non-significant decreased risk and one study reported that there was no effect on risk. These results are summarised in this forest plot (see also Lewis & Clark, 2001)
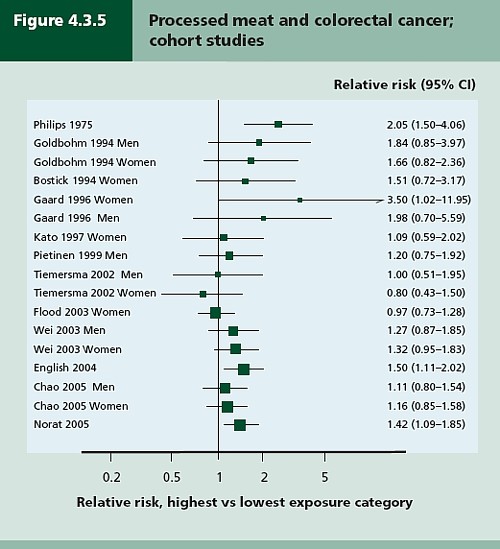
Each line represents a separate study. The size of the square represents the precision (weight) for each. The horizontal bars show the 95% confidence intervals. If it were possible to repeat the observations many times on the same population, the 95% CL would be different on each repeat experiment, but 19 out of 20 (95%) of the intervals would contain the true value (and 1 in 20 would not contain the true value). If the bar does not overlap the vertical line at relative risk = 1 (i.e. no effect) this is equivalent to saying that there is a statistically significant difference from 1 with P < 0.05. That means, very roughly, that there is a 1 in 20 chance of making a fool of yourself if you claim that the association is real, rather than being a result of chance (more detail here),
There is certainly a tendency for the relative risks to be above one, though not by much, Pooling the results sounds like a good idea. The method for doing this is called meta-analysis .
Meta-analysis was possible on five studies, shown below. The outcome is shown by the red diamond at the bottom, labelled “summary effect”, and the width of the diamond indicates the 95% confidence interval. In this case the final result for association between processed meat intake and colorectal cancer was a relative risk of 1.21 (95% CI 1.04–1.42) per 50 g/day. This is presumably where the headline value of a 20% increase in risk came from.
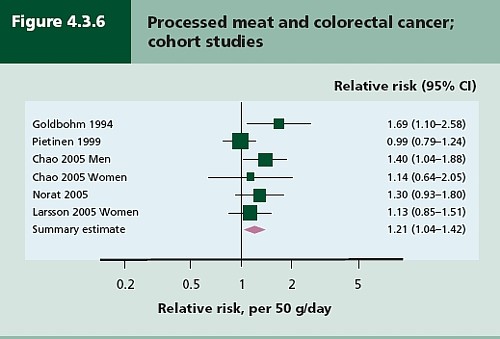
Support came from a meta-analysis of 14 cohort studies, which reported a relative risk for processed meat of 1.09 (95% CI 1.05 – 1.13) per 30 g/day (Larsson & Wolk, 2006). Since then another study has come up with similar numbers (Sinha etal. , 2009). This consistency suggests a real association, but it cannot be taken as evidence for causality. Observational studies on HRT were just as consistent, but they were wrong.
The accompanying editorial (Popkin, 2009) points out that there are rather more important reasons to limit meat consumption, like the environmental footprint of most meat production, water supply, deforestation and so on.
So the outcome from vast numbers of observations is an association that only just reaches the P = 0.05 level of statistical significance. But even if the association is real, not a result of chance sampling error, that doesn’t help in the least in establishing causality.
There are two more criteria that might help, a good relationship between dose and response, and a plausible mechanism.
Dose – response relationship
|
It is quite possible to observe a very convincing relationship between dose and response in epidemiological studies, The relationship between number of cigarettes smoked per day and the incidence of lung cancer is one example. Indeed it is almost the only example. |
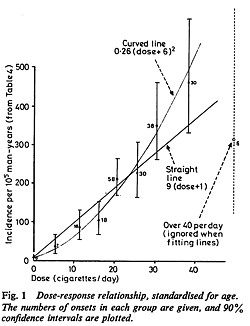 Doll & Peto, 1978 |
There have been six studies that relate consumption of processed meat to incidence of colorectal cancer. All six dose-response relationships are shown in the WCRG report. Here they are.
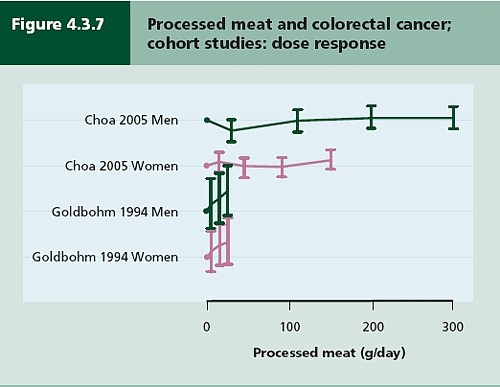
This Figure was later revised to
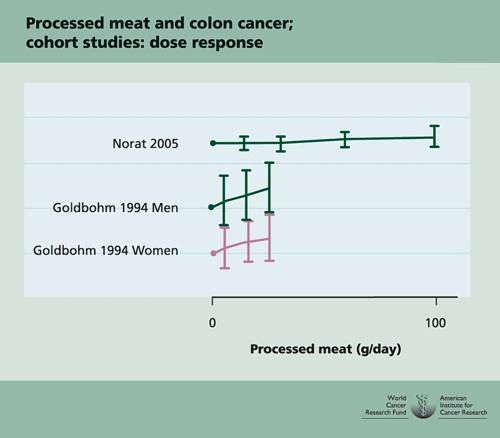
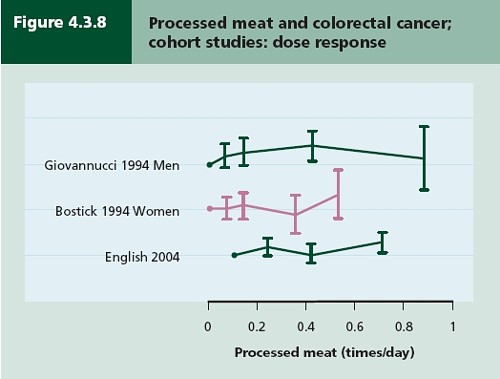
This is the point where my credulity begins to get strained. Dose – response curves are part of the stock in trade of pharmacologists. The technical description of these six curves is, roughly, ‘bloody horizontal’. The report says “A dose-response relationship was also apparent from cohort studies that measured consumption in times/day”. I simply cannot agree that any relationship whatsoever is “apparent”.
They are certainly the least convincing dose-response relationships I have ever seen. Nevertheless a meta-analysis came up with a slope for response curve that just reached the 5% level of statistical significance.
The conclusion of the report for processed meat and colorectal cancer was as follows.
“There is a substantial amount of evidence, with a dose-response relationship apparent from cohort studies. There is strong evidence for plausible mechanisms operating in humans. Processed meat is a convincing cause of colorectal cancer.”
But the dose-response curves look appalling, and it is reasonable to ask whether public policy should be based on a 1 in 20 chance of being quite wrong (1 in 20 at best –see Senn, 2008). I certainly wouldn’t want to risk my reputation on odds like that, never mind use it as a basis for public policy.
So we are left with plausibility as the remaining bit of evidence for causality. Anyone who has done much experimental work knows that it is possible to dream up a plausible explanation of any result whatsoever. Most are wrong and so plausibility is a pretty weak argument. Much play is made of the fact that cured meats contain nitrates and nitrites, but there is no real evidence that the amount they contain is harmful.
The main source of nitrates in the diet is not from meat but from vegetables (especially green leafy vegetables like lettuce and spinach) which contribute 70 – 90% of total intake. The maximum legal content in processed meat is 10 – 25 mg/100g, but lettuce contains around 100 – 400 mg/100g with a legal limit of 200 – 400 mg/100g. Dietary nitrate intake was not associated with risk for colorectal cancer in two cohort studies.(Food Standards Agency, 2004; International Agency for Research on Cancer, 2006).
To add further to the confusion, another cohort study on over 60,000 people compared vegetarians and meat-eaters. Mortality from circulatory diseases and mortality from all causes were not detectably different between vegetarians and meat eaters (Key et al., 2009a). Still more confusingly, although the incidence of all cancers combined was lower among vegetarians than among meat eaters, the exception was colorectal cancer which had a higher incidence in vegetarians than in meat eaters (Key et al., 2009b).
Mente et al. (2009) compared cohort studies and RCTs for effects of diet on risk of coronary heart disease. “Strong evidence” for protective effects was found for intake of vegetables, nuts, and “Mediterranean diet”, and harmful effects of intake of trans–fatty acids and foods with a high glycaemic index. There was also a bit less strong evidence for effects of mono-unsaturated fatty acids and for intake of fish, marine ω-3 fatty acids, folate, whole grains, dietary vitamins E and C, beta carotene, alcohol, fruit, and fibre. But RCTs showed evidence only for “Mediterranean diet”, and for none of the others.
As a final nail in the coffin of case control studies, consider pizza. According to La Vecchia & Bosetti (2006), data from a series of case control studies in northern Italy lead to: “An inverse association was found between regular pizza consumption (at least one portion of pizza per week) and the risk of cancers of the digestive tract, with relative risks of 0.66 for oral and pharyngeal cancers, 0.41 for oesophageal, 0.82 for laryngeal, 0.74 for colon and 0.93 for rectal cancers.”
What on earth is one meant to make of this? Pizza should be prescribable on the National Health Service to produce a 60% reduction in oesophageal cancer? As the authors say “pizza may simply represent a general and aspecific indicator of a favourable Mediterranean diet.” It is observations like this that seem to make a mockery of making causal inferences from non-randomised studies. They are simply uninterpretable.
Is the observed association even real?
The most noticeable thing about the effects of red meat and processed meat is not only that they are small but also that they only just reach the 5 percent level of statistical significance. It has been explained clearly why, in these circumstances, real associations are likely to be exaggerated in size (Ioannidis, 2008a; Ioannidis, 2008b; Senn, 2008). Worse still, there as some good reasons to think that many (perhaps even most) of the effects that are claimed in this sort of study are not real anyway (Ioannidis, 2005). The inflation of the strength of associations is expected to be bigger in small studies, so it is noteworthy that the large meta-analysis by Larsson & Wolk, 2006 comments “In the present meta-analysis, the magnitude of the relationship of processed meat consumption with colorectal cancer risk was weaker than in the earlier meta-analyses”.
This is all consistent with the well known tendency of randomized clinical trials to show initially a good effect of treatment but subsequent trials tend to show smaller effects. The reasons, and the cures, for this worrying problem are discussed by Chalmers (Chalmers, 2006; Chalmers & Matthews, 2006; Garattini & Chalmers, 2009)
What do randomized studies tell us?
The only form of reliable evidence for causality comes from randomised controlled trials. The difficulties in allocating people to diets over long periods of time are obvious and that is no doubt one reason why there are far fewer RCTs than there are observational studies. But when they have been done the results often contradict those from cohort studies. The RCTs of hormone replacement therapy mentioned above contradicted the cohort studies and reversed the advice given to women about HRT.
Three more illustrations of how plausible suggestions about diet can be refuted by RCTs concern nutritional supplements and weight-loss diets
Many RCTs have shown that various forms of nutritional supplement do no good and may even do harm (see Cochrane reviews). At least we now know that anti-oxidants per se do you no good. The idea that anti-oxidants might be good for you was never more than a plausible hypothesis, and like so many plausible hypotheses it has turned out to be a myth. The word anti-oxidant is now no more than a marketing term, though it remains very profitable for unscrupulous salesmen.
The randomised Women’s Health Initiative Dietary Modification Trial (Prentice et al., 2007; Prentice, 2007) showed minimal effects of dietary fat on cancer, though the conclusion has been challenged on the basis of the possible inaccuracy of reported diet (Yngve et al., 2006).
Contrary to much dogma about weight loss (Sacks et al., 2009) found no differences in weight loss over two years between four very different diets. They assigned randomly 811 overweight adults to one of four diets. The percentages of energy derived from fat, protein, and carbohydrates in the four diets were 20, 15, and 65%; 20, 25, and 55%; 40, 15, and 45%; and 40, 25, and 35%. No difference could be detected between the different diets: all that mattered for weight loss was the total number of calories. It should be added, though, that there were some reasons to think that the participants may not have stuck to their diets very well (Katan, 2009).
The impression one gets from RCTs is that the details of diet are not anything like as important as has been inferred from non-randomised observational studies.
So does processed meat give you cancer?
After all this, we can return to the original question. Do sausages or bacon give you colorectal cancer? The answer, sadly, is that nobody really knows. I do know that, on the basis of the evidence, it seems to me to be an exaggeration to assert that “The evidence is convincing that processed meat is a cause of bowel cancer”.
In the UK there were around 5 cases of colorectal cancer per 10,000 population in 2005, so a 20% increase, even if it were real, and genuinely causative. would result in 6 rather than 5 cases per 10,000 people, annually. That makes the risk sound trivial for any individual. On the other hand there were 36,766 cases of colorectal cancer in the UK in 2005. A 20% increase would mean, if the association were causal, about 7000 extra cases as a result of eating processed meat, but no extra cases if the association were not causal.
For the purposes of public health policy about diet, the question of causality is crucial. One has sympathy for the difficult decisions that they have to make, because they are forced to decide on the basis of inadequate evidence.
If it were not already obvious, the examples discussed above make it very clear that the only sound guide to causality is a properly randomised trial. The only exceptions to that are when effects are really big. The relative risk of lung cancer for a heavy cigarette smoker is 20 times that of a non-smoker and there is a very clear relationship between dose (cigarettes per day) and response (lung cancer incidence), as shown above. That is a 2000% increase in risk, very different from the 20% found for processed meat (and many other dietary effects). Nobody could doubt seriously the causality in that case.
The decision about whether to eat bacon and sausages has to be a personal one. It depends on your attitude to the precautionary principle. The observations do not, in my view, constitute strong evidence for causality, but they are certainly compatible with causality. It could be true so if you want to be on the safe side then avoid bacon. Of course life would not be much fun if your actions were based on things that just could be true.
My own inclination would be to ignore any relative risk based on observational data if it was less than about 2. The National Cancer Institute (Nelson, 2002) advises that relative risks less than 2 should be “viewed with caution”, but fails to explain what “viewing with caution” means in practice, so the advice isn’t very useful.
In fact hardly any of the relative risks reported in the WCRF report (2007) reach this level. Almost all relative risks are less than 1.3 (or greater than 0.7 for alleged protective effects). Perhaps it is best to stop worrying and get on with your life. At some point it becomes counterproductive to try to micromanage `people’s diet on the basis of dubious data. There is a price to pay for being too precautionary. It runs the risk of making people ignore information that has got a sound basis. It runs the risk of excessive medicalisation of everyday life. And it brings science itself into disrepute when people laugh at the contradictory findings of observational epidemiology.
The question of how diet and other ‘lifestyle interventions’ affect health is fascinating to everyone. There is compelling reason to think that it matters. For example one study demonstrated that breast cancer incidence increased almost threefold in first-generation Japanese women who migrated to Hawaii, and up to fivefold in the second generation (Kolonel, 1980). Since then enormous effort has been put into finding out why. The first great success was cigarette smoking but that is almost the only major success. Very few similar magic bullets have come to light after decades of searching (asbestos and mesothelioma, or UV radiation and skin cancer count as successes).
The WCRF report (2007) has 537 pages and over 4400 references and we still don’t know.
Sometimes I think we should say “I don’t know” rather more often.
More material
-
Listen to Ben Goldacre’s Radio 4 programmes. The Rise of the Lifetsyle Nutritionists. Part 1 and Part 2 (mp3 files), and at badscience.net.
-
Risk The Science and Politics of Fear, Dan Gardner. Virgin
Books, 2008 -
Some bookmarks about diet and supplements
Follow up
Dan Gardner, the author of Risk, seems to like the last line at least, according to his blog.
Report of the update, 2010
The 2010 report has been updated in WCRF/AICR Systematic Literature Review Continuous Update Project Report [big pdf file]. This includes studies up to May/June 2010.
The result of addition of the new data was to reduce slightly the apparent risk from eating processed meat from 1.21 (95% CI = 1.04-1.42) in the original study to 1.18 (95% CI = 1.10-1.28) in the update. The change is too small to mean much, though it is in direction expected for false correlations. More importantly, the new data confirm that the dose-response curves are pathetic. The evidence for causality is weakened somewhat by addition of the new data.
Dose-response graph of processed meat and colorectal cancer