Chinese medicine
It makes a nice change to be able to compliment an official government report.
|
Ever since the House of Lords report in 2000, the government has been vacillating about what should be done about herbalists. At the moment both western herbalists and traditional Chinese medicine (TCM) are essentially unregulated. Many (but not all) herbalists have been pushing for statutory regulation, which they see as government endorsement. It would give them a status like the General Medical Council. |
|
A new report has ruled out this possibility, for very good reasons [download local copy].
Back story (abridged!)
My involvement began with the publication in 2008 of a report on the Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine . That led to my post, A very bad report: gamma minus for the vice-chancellor. The report was chaired by the late Professor Michael Pittilo BSc PhD CBiol FIBiol FIBMS FRSH FLS FRSA, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The membership of the group consisted entirely of quacks and the vice -chancellor’s university ran a course in homeopathy (now closed).
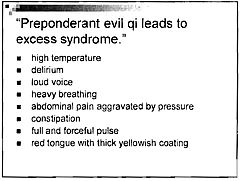
The Pittilo report recommended statutory regulation and "The threshold entry route to the register will normally be through a Bachelor degree with Honours". It ignored entirely the little problem that you can’t run a BSc degree in a subject that’s almost entirely devoid of evidence. It said, for example that acupuncturists must understand " yin/yang, 5 elements/phases, eight principles, cyclical rhythms, qi ,blood and body fluids". But of course there is nothing to "understand"! They are all pre-scientific myths. This “training dilemma” was pointed out in one of my earliest posts, You’d think it was obvious, but nonetheless the then Labour government seemed to take this absurd report seriously.
In 2009 a consultation was held on the Pittilo report. I and many of my friends spent a lot of time pointing out the obvious. Eventually the problem was again kicked into the long grass.
The THR scheme
Meanwhile European regulations caused the creation of the Traditional Herbal Registration (THR) scheme. It’s run by the Medicines and Healthcare products Regulatory Authority (MHRA). This makes it legal to put totally misleading claims on labels of herbal concoctions, as long as they are registered with THR, They also get an impressive-looking certification mark. All that’s needed to get THR registration is that the ‘medicines’ are not obviously toxic and they have been in use for 30 years. There is no need to supply any information whatsoever about whether they work or not. This appears to contradict directly the MHRA’s brief:
"”We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
After much effort, I elicited an admission from the MHRA that there was no reason to think that any herbal concoctions were effective, and that there was nothing to prevent them from adding a statement to say so on the label. They just chose not to do so. That’s totally irresponsible in my opinion. See Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. Over 300 herbal products have been registered under the THR scheme (a small percentage of the number of products being used). So far only one product of Tibetan medicine and one traditional Chinese medicine have been registered under THR. These are the only ones that can be sold legally now, because no herbs whatsoever have achieved full marketing authorisation -that requires good evidence of efficacy and that doesn’t exist for any herb.
The current report
Eventually, in early 2014, the Tory-led government set up yet another body, "Herbal Medicines and Practitioners Working Group " (HMPWG). My heart sank when I saw its membership (Annex A.2). The vice-chair was none other that the notorious David Tredinnick MP (Con, Bosworth). It was stuffed with people who had vested interests. I wrote to the chair and to the few members with scientific credentials to put my views to them.
But my fears were unfounded, because the report of the HMPWG was not written by the group, but by its chair only. David Walker is deputy chief medical officer and he had clearly listened. Here are some quotations.
The good thing about the European laws is that
"This legislation effectively banned the importation and sale of large-scale manufactured herbal medicine products. This step severely limited the scope of some herbal practitioners to continue practising, particularly those from the Traditional Chinese Medicine (TCM) and Ayurvedic traditions."
The biggest loophole is that
"At present under UK law it is permitted for a herbal practitioner to see individual patients, offer diagnoses and prepare herbal treatments on their own premises, as long as these preparations do not contain banned or restricted substances. This is unchanged by the Traditional Herbal Medicinal Products Directive. "
Walker recognised frankly that there is essentially no good evidence that any herb, western or Chinese, works well enough to make an acceptable treatment. And importantly he, unlike Pittilo, realised that this precludes statutory regulation.
"There are a small number of studies indicating benefit from herbal medicine in a limited range of conditions but the majority of herbal medicine practice is not supported by good quality evidence. A great deal of international, primary research is of poor quality. "
"ts. Herbal medicine practice is therefore currently based upon traditional practice rather than science. It is difficult to differentiate good practice from poor practice on the basis of this evidence in a way that could establish standards for statutory regulation"
The second problem was the harms done by herbs. Herbalists, western and Chinese, have no satisfactory way of reporting side effects
" . . . there is very limited understanding of the risks to patient safety from herbal medicines and herbal practice. A review of safety data was commissioned from HMAC as part of this review. This review identified many anecdotal reports and case studies but little systematically collected data. Most herbal medicine products have not been through the rigorous licensing process that is required of conventional pharmaceutical products to establish their safety and efficacy. Indeed, only a small proportion have even been subject to the less rigorous Traditional Herbal Registration (THR) process. "
"The anecdotal evidence of risk to patients from herbal products in the safety review highlighted the prominence of manufactured herbal medicines in the high profile serious incidents which have been reported in recent years. Many of these reports relate to harm thought to be caused by industrially manufactured herbal products which contained either dangerous herbs, the wrong constituents, toxic contaminants or adulterants. All such industrially manufactured products are now only available under European regulations if their safety is assured through MHRA licensing or THR
accreditation; and specific dangerous herbs have been banned under UK law. This has weakened the case for introduction of statutory regulation as a further safety measure. "
Then Walker identified correctly the training dilemma. Although it seems obvious, this is a big advance for a government document. Degrees that teach nonsense are not good training: they are miseducation.
"The third issue is the identification of educational standards for training practitioners and the benchmarking of standards for accrediting practitioners. With no good data on efficacy or safety, it is difficult for practitioners and patients to understand or quantify the potential benefits and risks of a proposed therapeutic intervention. Training programmes could accredit knowledge and skills in some areas including pharmacology and physiology, professional ethics and infection control but without a credible evidence base relating to the safety and effectiveness of herbal medicine it is hard to see how they could form the basis of accreditation in this field of practice.
There are a number of educational university programmes offering courses in herbal medicine although the number has declined in recent years. Some of these courses are accredited by practitioner organisations which is a potential governance risk as the accreditation may be based on benchmarks established by tradition and custom rather than science.
"
"The herbal medicine sector is in a dilemma" is Walker’s conclusion.
"Some practitioners would like to continue to practise as
they do now, with no further regulation, and accept that their practice is based on tradition and personal experience rather than empirical science. The logical consequence of adopting this form of practice is that we should take a precautionary approach in order to ensure public safety. The public should be protected through consumer legislation to prevent false claims, restricting the use of herbal products which are known to be hazardous to health"
The problem with this is, if course, is that although there is plenty of law, it’s rarely enforced : see Most alternative medicine is illegal Trading Standards very rarely enforce the Consumer Protection Regulations (2008) but Walker is too diplomatic to mention that fact.
"The herbals sector must recognise that its overall approach (including the rationale for use of products and methods of treatment, education and training, and interaction with the NHS) needs to be more science and evidence based if in order to be established as a profession on the same basis as other groups that are statutorily regulated."
So what happens next?
In the short term nothing will happen.
The main mistake has been avoided: there wil be no statutory regulation.
The other options are (a) do nothing, or (b) go for accreditation of a voluntary register (AR) by the Professional Standards Authority for Health and Social Care (PSA). Walker ends up recommending the latter, but only after a lot more work (see pages 28-29 of report). Of particular interest is recommendation 5.
"As a first step it would be helpful for the sector organisations to develop an umbrella voluntary register that could support the development of standards and begin to collaborate on the collection of safety data and the establishment of an academic infrastructure to develop training and research. This voluntary register could in due course seek accreditation from the Professional Standards Authority for Health and Social Care (PSA)."
So it looks as though nothing will happen for a long time, and herbalists and TCM may end up with the utterly ineffectual PSA. After all, the PSA have accredited voluntary registers of homeopaths, so clearly nothing is too delusional for them. It’s very obvious that, unlike Walker, the PSA are quite happy to ignore the training dilemma.
Omissions from the report
Good though this report is, by Department of Health standards, it omits some important points.
Endangered species and animal cruelty aren’t mentioned in the report. Traditional Chinese medicine, and its variants, are responsible for the near-extinction of rhinoceros, tiger and other species because of the superstitious belief that they have medicinal value. It’s not uncommon to find animal parts in Chinese medicines sold in the UK despite it being illegal
And the unspeakably cruel practice of farming bears to collect bile is a direct consequence of TCM.

A bile bear in a “crush cage” on Huizhou Farm, China (Wikipedia)
Statutory regulation of Chiropractors
The same arguments used in Walker’s report to deny statutory regulation of herbalism, would undoubtedly lead to denial of statutory regulation of chiropractors. The General Chiropractic Council was established in 1994, and has a status that’s the same as the General Medical Council. That was a bad mistake. The GCC has not protected the public, in fact it has acted as an advertising agency for chiropractic quackery.
Perhaps Prof. Walker should be asked to review the matter.
Follow-up
You can also read minutes of the HMPWG meetings (and here). But, as usual, all the interesting controversies have been sanitised.
Edzard Ernst has also commented on this topic: Once again: the regulation of nonsense will generate nonsense – the case of UK herbalists.
Since writing about anti-scientific degrees in Nature (March 2007), much has been revealed about the nonsense that is taught on these degrees. New Year’s day seems like a good time to assess how far we’ve got, five years on.
At the beginning of 2007 UCAS (the universities central admission service) offered 45 different BSc degrees in quackery, at 16 universities.
Now there are only 24 such degrees.
If you exclude chiropractic and osteopathy, which all run at private colleges, with some sort of "validation" from a university, there are now only 18 BSc/MSc courses being offered in eight universities.
Degrees in homeopathy, naturopathy and "nutritional therapy", reflexology and aromatherapy have vanished altogether from UCAS.
In the race to provide BScs in anti-science, Middlesex University has now overhauled the long-standing leader, Westminster, by a short head.
 Michael Driscoll, vice-chancellor of Middlesex |
|
Let’s see what’s gone.
The University of Central Lancashire (UCLAN) was the first to see sense. In August 2008 they announced closure of their “BSc” degree in homeopathy. On September 2008 they announced an internal review of their courses in homeopathy. herbalism and acupuncture. The report of this review closed down all of them in July 2009. I first asked for their teaching materials in July 2006. I finally got them in December 2010, after winning an appeal to the Information Commissioner, and then winning an appeal against that decision at an Information tribunal . By the time I got them, the course had been closed for over two years. That is just as well, because it turned out that UCLAN’s students were being taught dangerous nonsense. No wonder they tried so hard to conceal it.
Salford University was the next to go. They shut down their courses in complementary medicine, homeopathy and acupuncture. In January 2009 they announced " they are no longer considered “a sound academic fit” ". Shortly afterwards. a letter appeared in The Times from three heavyweights (plus me) congratulating the vice-chancellor on his decision.
University of Westminster
For many years, Westminster was the biggest supplier of BSc degrees in quackery. At the beginning of 2007 they offered 14 different BSc degrees in homeopathy, naturopathy, nutritional therapy, "complementary therapies", (western) herbal medicine and traditional Chinese medicine with acupuncture. Some of their courses were so bizarre that some of the students and even staff sent me slides which taught things like "amethysts emit high Yin energy". Like UCLAN, Westminster also held an internal review. Unlike UCLAN it came to the absurd conclusion that all would be well if they injected more science into the courses. The incompetence of the review meant that those who wrote it hadn’t noticed that if you try to put science into homeopathy or naturopathy, the whole subject vanishes in a puff of smoke. Nevertheless Westminster closed down entry to BSc homeopathy in March 2009 (though the subject remained as part of other courses).
Three years after the Nature article, all five BSc homeopathy degrees had shut their doors.
During 2011, Westminster shut down Naturopathy, Nutritional therapy, Therapeutic bodywork and Complementary Medicine. See, for example,
More dangerous nonsense from the University of Westminster: when will Professor Geoffrey Petts do something about it?
Now Westminster has only four courses in two subjects. They still teach some dangerous and untrue things, but I suspect the writing is on the wall for these too.
I have seen a document, dated 11 April 2011, which states
“The following courses have been identified as ‘at risk’ (School definition) and will be discussed at the APRG and University Review Group2, due to poor recruitment and high cost of delivery:
Integrated Health Scheme: BSc Complementary Medicine, Naturopathy; BSc Chinese Medicine; BSc Nutritional Therapy; BSc Herbal Medicine”
All but Chinese medicine and Herbal medicine have already gone. Almost there.
University of Wales
Since my first post in 2008 about the validation scam operated by the University of Wales, and some good investigations by BBC Wales TV, the outcome was the most spectacular so far. The entire institution collapsed. They no longer "validate" external degrees at dodgy business colleges, loony religious colleges or magic medicine colleges.
Another worthless validation: the University of Wales and nutritional therapy (October 2008) This is a ‘degree’ in nutrtional therapy. It is even more hilarious than usual, but it passed the validation anyway.
Scandal of the University of Wales and the Quality Assurance Agency (November 2010). This post followed the BBC Wales TV programme. At last the QAA began to notice, yet further confirmation of its utter ineptitude.
The University of Wales disgraced (but its vice chancellor is promoted) (October, 2011) The eventual collapse of the university was well-deserved. But it is very weird that the people who were responsible for it have still got their jobs. In fact the vice-chancellor, Marc Clement, was promoted despite his mendacious claim to be unaware of what was going on.
It remains to be seen how many of the many quack courses that were validated by the University of Wales will be taken on by other universities. The McTimoney College of Chiropractic is owned by BPP University (so much for their quality control, as explained in Private Eye). but still claims to be validated by Wales until 2017.
Some of the more minor players
Edinburgh Napier University. After an FOI request (rejected), Napier closed their herbal medicine degree in 2010.
Hot and cold herbal nonsense from Napier University Edinburgh: another course shuts. (June 2010)
As expected, the Scottish Information Commissioner agreed with that for England and Wales and ordered material to be sent. Edinburgh Napier University teaches reflexology, aromatherapy and therapeutic touch. Scottish Information Commissioner says you should know. Some of the horrors so discovered appeared in Yet more dangerous nonsense inflicted on students by Edinburgh Napier University. The embarrassment seems to have worked. Their remaining degrees in aromatherapy and reflexology have now vanished from UCAS too. All that remains is a couple of part time “Certificates of Credit” for aromatherapy and reflexology
Anglia Ruskin Univerity Not only have BSc degrees gone in aromatherapy and reflexology, but their midwifery degree now states "We are unable to accept qualifications in aromatherapy, massage and reflexology."
University of Derby Reflexology and aromatherapy have gone, though doubtless Spa management therapies have much nonsense left
University of Greenwich. BSc in Complementary Therapies (Nutritional Health) and BSc in Complementary Therapies (Nutritional Health) have been shut. The BSc Acupuncture is listed on their web site but it is under review, and is not listed in UCAS for 2012. (Acupuncture is run at International College of Oriental medicine, validated by Greenwich.). Only osteopathy (MOst) is still running, and that is a validation of an external course run at The European School of Osteopathy, in Maidstone
Thames Valley University was renamed the University of West London in 2010. The nonsense that was run there (e.g. Nutritional Fairy Tales from Thames Valley University) seems to have vanished. Their previous alt med guru, Nicola Robinson, appears now to be at London South Bank University (ranked 116 out of the 116 UK universities)
What’s left?
Chiropractic Surprisingly, given the total discreditation of chiropractic in the wake of the Simon Singh affair, and the internecine warfare that followed it, none of the chiropractic courses have shut yet. Some are clearly in trouble, so watch this space.
Osteopathy has also had no course closures since 2007. Like chiropractic it also suffers from internecine warfare. The General Osteopathic Council refuses to disown the utter nonsense of "craniosacral" osteopathy. But the more sensible practitioners do so and are roughly as effective as physiotherapists (though there are real doubts about how effective that is).
Excluding chiropractic and osteopathy, this is all that’s left. It now consists almost entirely of Chinese medicine and a bit of herbal.
Glyndwr university (Known as North East Wales Institute until 2008) Ranked 104 out of 116 UK universities
BSc Acupuncture (B341) BSc
BSc Complementary Therapies for Healthcare (B343)
Cardiff Metropolitan University (UWIC) (Known as University of Wales Institute Cardiff (UWIC) until Nov 2011.) The vice-chancellor of Cardiff Metropolitan, Antony Chapman, is in the QAA’s board of directors, so perhaps it isn’t surprising that the QAA has done nothing.
BSc Complementary Therapies (3 years) (B390)
BSc Complementary Therapies (4 yrs inc Foundation) (B300)
University of Lincoln
Acupuncture (B343) 3FT Hon BSc
Herbal Medicine (B342) 3FT Hon BSc
University of East London Ranked 113 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
London South Bank University Ranked 116 out of 116 UK universities
Acupuncture (B343) 4FT Deg MCM
The Manchester Metropolitan University Ranked 93 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
Middlesex University
Acupuncture (B348) 3FT Hon BSc
Ayurvedic Medicine (A900) 4FT Oth MCM
Herbal Medicine (B347) 3FT Hon BSc
Traditional Chinese Medicine (BT31) 4FT Hon BSc
University of Westminster
Chinese Medicine: Acupuncture (B343) 3FT Hon BSc
Chinese Medicine: Acupuncture with Foundation (B341) 4FT/5FT Hon BSc/MSci
Herbal Medicine (B342) 3FT Hon BSc
Herbal Medicine with Foundation Year (B340) 4FT/5FT Hon BSc/MSci
It seems that acupuncture hangs on in universities that are right at the bottom of the rankings.
Manchester Metropolitan gets the booby prize for actually starting a new course, just as all around are closing theirs. Dr Peter Banister, who was on the committee that approved the course (but now retired), has told me ” I am sceptical in the current economic climate whether it will prove to be successful”. Let’s hope he’s right.
But well done Westminster. Your position as the leader in antiscientific degrees has now been claimed by Middlesex University. Their "degrees" in Ayurveda mark out Middlesex University as the new King of Woo.
Over to you, Professor Driscoll. As vice-chancellor of Middlesex University, the buck stops with you.
Both still teach Chinese and herbal medicine, which are potentially dangerous. There is not a single product from either that has marketing authorisation from the MHRA, though the MHRA has betrayed its trust by allowing misleading labelling of herbal medicines without requiring any evidence whatsoever that they work, see, for example
Why degrees in Chinese medicine are a danger to patients
More quackedemia. Dangerous Chinese medicine taught at Middlesex University
Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me
Sub-degree courses
In contrast to the large reduction in the number of BSc and MSc degrees, there has actually been an increase in two year foundation degrees and HND courses in complementary medicine, at places right near the bottom of the academic heap. The subject is sinking to the bottom. With luck it will vanish entirely from universities before too long.
Research-intensive Universities
Although all of the degrees in magic medicine are from post-1992 universities, the subject has crept into more prestigious universities. Of these, the University of Southampton is perhaps the worst, because of the presence of George Lewith, and his defender, Stephen Holgate. Others have staunch defenders of quackery, including the University of Warwick, University of Edinburgh and St Batholomew’s.
Why have all these courses closed?
One reason is certainly the embarrassment caused by exposure of what’s taught on the courses. Professors Petts (Westminster) and Driscoll (Middlesex) must be aware that googling their names produces references to this and other skeptical blogs on the front page. Thanks to some plain brown emails, and, after a three year battle, the Freedom of Information Act, it has been possible to show here the nonsense that has been foisted on students by some universities. Not only is this a burden on the taxpayer, but, more importantly, some of it is a danger to patients.
When a course closes, it is often said that it is because of falling student numbers (though UCLAN and Salford did not use that excuse). Insofar as that is true, the credit must go to the whole of the skeptical movement that has grown so remarkably in the last few years. Ben Goldacre’s "ragged band of bloggers" have produced a real change in universities and in society as a whole.
The people who should have done the job have either been passive or an active hindrance. The list is long. Vice-chancellors and Universities UK (UUK), the Quality Assurance Agency (QAA), the Hiigher Education Funding Council England (HEFCE), Skills for Health, the Medicines and Health Regulatory Authority ( MHRA) , the Health Professions Council (HPC), the Department of Health, the Prince of Wales and his reincarnated propaganda organisation, the "College of Medicine", the King’s Fund, the Universities and Colleges Union (UCU), OfQual, Edexcel, National Occupational Standards and Qualifications and the Curriculum Authority (QCA).
Whatever happened to that "bonfire of the quangos"?
Follow-up
2 January 2012 The McTimoney College of Chiropractic (owned by BPP University) claims that its “validation” by the University of Wales will continue until 2017. This contradicts the statement from UoW. Watch this space.
3 January 2012. Thanks to Neil O’Connell for drawing my attention to a paper in Pain. The paper is particularly interesting because it comes from the Southampton group which has previously been sympathetic to acupuncture. Its authors include George Lewith. It shows, yet again that there is no detectable difference between real and sham acupuncture treatment. It also shows that the empathy of the practitioner has little effect: in fact the stern authoritarian practitioner may have been more effective.
Patients receiving acupuncture demonstrated clinically important improvements from baseline (i.e., a 29.5% reduction in pain), but despite this, acupuncture has no specific efficacy over placebo for this group of patients. The clinical effect of acupuncture treatment and associated controls is not related to the use of an acupuncture needle, nor mediated by empathy, but is practitioner related and may be linked to the perceived authority of the practitioner.”
Sadly. the trial didn’t include a no-treatment group, so it is impossible to say how much of the improvement is regression to the mean and how much is a placebo effect. The authors admit that it could be mostly the former.
Surely now the misplaced confidence in acupuncture shown by some medical and university people must be in tatters.
In yet another sign that even acupuncture advovates are beginning to notice that it doesn’t work, a recent article Paradoxes in Acupuncture Research: Strategies for Moving Forward, shows some fascinating squirming.
3 January 2012. The Daily Telegraph has carried a piece about closure of university courses, written by Michael Hanlon. On 31 January they carried a much longer piece.
3 January 2012. It is a great pity that some physiotherapists seem to have fallen hook, line and sinker for the myths of acupuncture. Physiotherapists are, by and large, the respectable face of manipulative therapy. Their evidence base is certainly not all one would wish, but at least they are free of the outrageous mumbo humbo of chiropractors. Well, most of them are, but not the Acupuncture Association of Chartered Physiotherapists (AACP), or, still worse, The Association of Chartered Physiotherapists in Energy Medicine, a group that is truly away with the fairies. These organisations are bringing a very respectable job into disrepute. And the Health Professions Council, which is meant to be their regulator, has, like most regulators, done nothing whatsoever to stop it.
5 January 2012. Times Higher Education gives a history of the demise of the University of Wales, Boom or Bust. It’s a useful timeline, but like so many journalists, it’s unwilling to admit that bloggers were on to the problem long before the BBC, never mind the QAA.
There was also a leader on the same topic, Perils of the export business. It again fails to take the QAA to task for its failures.
Interviews for Deutsche Welle and Middle East Broadcasting Center TV.
17 January 2012 Another question answered. I just learned that the ludicrous course in Nutritional Therapy, previously validated by the University of Wales (and a contributor to its downfall), is now being validated by, yes, you guessed, Middlesex University. Professor Driscoll seems determined to lead his univerity to the bottom of the academic heap. His new partnership with the Northern college of Acupuncture is just one of a long list of validations that almost rivals that of the late University of Wales. The course has, of course, an enthusiastic testimonial, from a student. It starts
I work full time as a team leader for a pension company but I am also a kinesiologist and work in my spare time doing kinesiology, reiki and Indian head massage.
Evidently she’s a believer in the barmiest and totally disproved forms of magic medicine. And Middlesex University will give her a Master of Science degree. I have to say I find it worrying that she’s a team leader for a pension company. Does she also believe in the value of worthless derivatives. I wonder?
18 January 2012. the story has gone international, with an interview that I did for Deutsche Welle, UK universities drop alternative medicine degree programs. I’m quoted as saying “They’re dishonest, they teach things that aren’t true, and things that are dangerous to patients in some cases”. That seems fair enough.
There is also an interesting item from July 2010 about pressure to drop payment for homeopathy by German health insurance
31 January 2012
The Daily Telegraph carried a prominent 1200 word account (the title wasn’t mine). The published version was edited slightly.
There’s been no official announcement, but four more of Westminster’s courses in junk medicine have quietly closed.
For entry in 2011 they offer
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Complementary Medicine (B255) | 3FT Hon BSc |
| Complementary Medicine (B301) | 4FT Hon MHSci |
| Complementary Medicine: Naturopathy (B391) | 3FT Hon BSc |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSci |
| Nutritional Therapy (B400) | 3FT Hon BSc |
But for entry in 2012
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSc |
At the end of 2006, Westminster was offering 14 different BSc degrees in seven flavours of junk medicine. In October 2008, it was eleven. This year it’s eight, and next year only four degrees in two subjects. Since "Integrated Health" was ‘merged’ with Biological Sciences in May 2010, two of the original courses have been dropped each year. This September there will be a final intake for Nutrition Therapy and Naturopathy. That leaves only two, Chinese Medicine (acupuncture and (Western) Herbal Medicine.
The official reason given for the closures is always that the number of applications has fallen. I’m told that the number of applications has halved over the last five or six years. If that’s right, it counts as a big success for the attempts of skeptics to show the public the nonsense that’s taught on these degrees. Perhaps it is a sign that we are emerging from the endarkenment.
Rumour has it that the remaining degrees will eventually close too. Let’s hope so. Meanwhile, here is another helping hand.
There is already quite a bit here about the dangers of Chinese medicine, e.g. here and, especially, here. A submission to the Department of Health gives more detail. There has been a lot on acupuncture here too. There is now little doubt that it’s no more than a theatrical, and not very effective, placebo. So this time I’ll concentrate on Western herbal medicine.
Western Herbal Medicine
Herbal medicine is just a branch of pharmacology and it could be taught as such. But it isn’t. It comes overlaid with much superstitious nonsense. Some of it can be seen in slides from Edinburgh Napier University (the difference being that Napier closed that course, and Westminster hasn’t)
Even if it were taught properly, it wouldn’t be appropriate for a BSc for several reasons.
First, there isn’t a single herbal that has full marketing authorisation from the MHRA. In other words, there isn’t a single herb for which there is good evidence that it works to a useful extent.
Second, the fact that the active principals in plants are virtually always given in an unknown dose makes them potentially dangerous. This isn’t 1950s pharmacology. It’s 1920s pharmacology, dating from a time before methods were worked out for standardising the potency of natural products (see Plants as Medicines).
Third, if you are going to treat illness with chemicals, why restrict yourself to chemicals that occur in plants?
It was the herbal medicine course that gave rise to the most virulent internal complaints at the University of Westminster. These complaints revealed the use of pendulum dowsing by some teachers on the course and the near-illegal, and certainly dangerous, teaching about herbs in cancer.
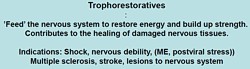
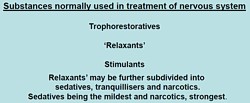
Here are a few slides from Principles of Herbal Medicine(3CT0 502). The vocabulary seems to be stuck in a time warp. When I first started in the late 1950s, words like tonic, carminative, demulcent and expectorant were common Over the last 40 years all these words have died out in pharmacology, for the simple reason that it became apparent that there were no such actions. But these imaginary categories are still alive and well in the herbal world.
There was a lecture on a categories of drugs so old-fashioned that I’ve never even heard the words: "nervines". and "adaptogens".
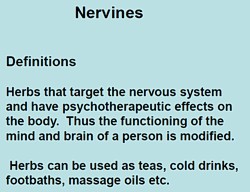 |
  |
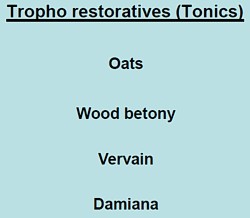 |
The "tonics" listed here seem quite bizarre. In the 1950s, “tonics” containing nux vomica (a small dose of strychnine) and gentian (tastes nasty) were common, but they vanished years ago, because they don’t work. None of those named here even get a mention in NCCAM’s Herbs-at-a-glance. Oats? Come on! |
|
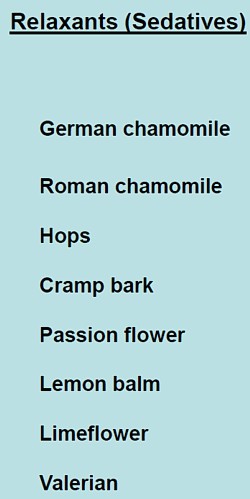
The only ‘relaxant’ here for which there is the slightest evidence is Valerian. I recall tincture of Valerian in a late 1950s pharmacy. It smells terrible, According to NCCAM
Not much, for something that’s been around for centuries. And for chamomile
None of this near-total lack of evidence is mentioned on the slides. |
 |
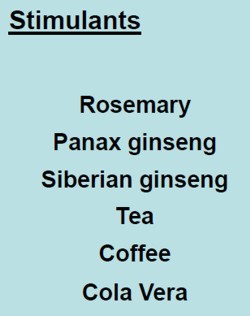
What about the ‘stimulants‘? Rosemary? No evidence at all. Tea and coffee aren’t medicine (and not very good stimulants for me either).
|
Ginseng, on the other hand, is big business. That doesn’t mean it works of course. NCCAM says of Asian ginseng (Panax Ginseng).
|
 |
Thymoleptics – antidepressants are defined as "herbs that engender a feeling of wellbeing. They uplift the spirit, improve the mood and counteract depression".
Oats, Lemon balm, Damiana, Vervain. Lavender and Rosemary are just old bits of folklore
|
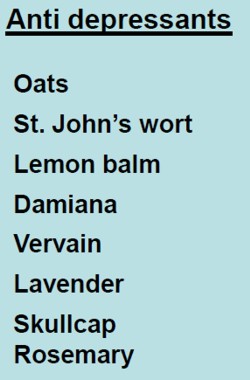 |
The only serious contender here is St John’s Wort. At one time this was the prize exhibit for herbalists. It has been shown to be as good as the conventional SSRIs for treatment of mild to moderate depression. Sadly it has turned out that the SSRIs are themselves barely better than placebos. NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
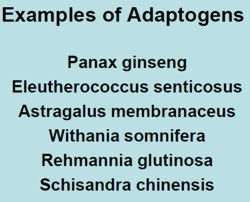
"Adaptogens" are another figment of the herbalists’ imaginations. They are defined in the lecture thus.
|
|
Well, it would be quite nice if such drugs existed. Sadly they don’t.
- The evidence for using astragalus for any health condition is limited. High-quality clinical trials (studies in people) are generally lacking.
Another lecture dealt with "stimulating herbs". No shortage of them, it seems.
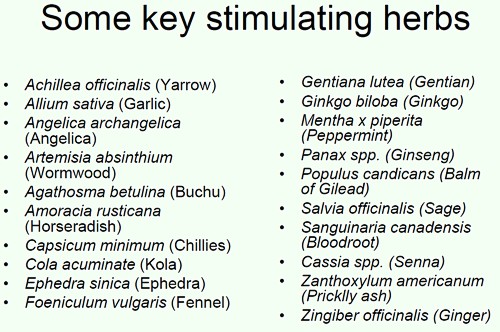
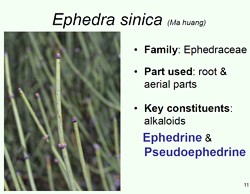
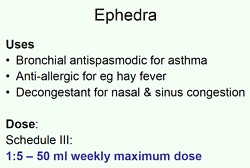
Well at least one of these has quite well-understood effects in pharmacology, ephedrine, a sympathomimetic amine. It isn’t used much because it can be quite dangerous, even with the controlled dose that’s used in real medicine. In the uncontrolled dose in herbal medicines it is downright dangerous.
|
|
|
|
This is what NCCAM says about Ephedra
- An NCCAM-funded study that analyzed phone calls to poison control centers found a higher rate of side effects from ephedra, compared with other herbal products.
- Other studies and systematic reviews have found an increased risk of heart, psychiatric, and gastrointestinal problems, as well as high blood pressure and stroke, with ephedra use.
- According to the U.S. Food and Drug Administration (FDA), there is little evidence of ephedra’s effectiveness, except for short-term weight loss. However, the increased risk of heart problems and stroke outweighs any benefits.
It seems that what is taught in the BSc Herbal Medicine degree consists largely of folk-lore and old wives’ tales. Some of it could be quite dangerous for patients.
A problem for pharmacognosists
While talking about herbal medicine, it’s appropriate to mention a related problem, though it has nothing to do with the University of Westminster.
My guess is that not many people have even heard of pharmacognosy. If it were not for my humble origins as an apprentice pharmacist in Grange Road, Birkenhead (you can’t get much more humble than that) I might not know either.
Pharmacognosy is a branch of botany, the study of plant drugs. I recall inspecting powered digitalis leaves under a microscope. In Edinburgh, in the time of the great pharmacologist John Henry Gaddum, medical students might be presented in the oral exam with a jar of calabar beans and required to talk about their anticholinesterase effects of the physostigmine that they contain.
The need for pharmacognosy has now all but vanished, but it hangs on in the curriculum for pharmacy students. This has engendered a certain unease about the role of pharmacognists. They often try to justify their existence by rebranding themselves as "phytotherapists". There are even journals of phytotherapy. It sounds a lot more respectable that herbalism. At its best, it is more respectable, but the fact remains that there no herbs whatsoever that have well-documented medical uses.
The London School of Pharmacy is a case in point. Simon Gibbons (Professor of Phytochemistry, Department of Pharmaceutical and Biological Chemistry). The School of Pharmacy) has chosen, for reasons that baffle me, to throw in his lot with the reincarnated Prince of Wales Foundation known as the “College of Medicine“. That organisation exists largely (not entirely) to promote various forms of quackery under the euphemism “integrated medicine”. On their web site he says "Western science is now recognising the extremely high value of herbal medicinal products . . .", despite the fact that there isn’t a single herbal preparation with efficacy sufficient for it to get marketing authorisation in the UK. This is grasping at straws, not science.
The true nature of the "College of Medicine" is illustrated, yet again, by their "innovations network". Their idea of "innovation" includes the Bristol Homeopathic Hospital and the Royal London Hospital for Integrated medicine, both devoted to promoting the utterly discredited late-18th century practice of giving people pills that contain no medicine. Some "innovation".
It baffles me that Simon Gibbons is willing to appear on the same programme as Simon Mills and David Peters, and George Lewith. Mills’ ideas can be judged by watching a video of a talk he gave in which he ‘explains’ “hot and cold herbs”. It strikes me as pure gobbledygook. Make up your own mind. He too has rebranded himself as "phytotherapist" though in fact he’s an old-fashioned herbalist with no concern for good evidence. David Peters is the chap who, as Clinical Director of the University of Westminster’s ever-shrinking School of Quackery, tolerates dowsing as a way to select ‘remedies’.
The present chair of Pharmacognosy at the School of Pharmacy is Michael Heinrich. He, with Simon Gibbons, has written a book Fundamentals of pharmacognosy and phytotherapy. As well as much good chemistry, it contains this extraordinary statement
“TCM [traditional Chinese medicine] still contains very many remedies which were selected by their symbolic significance rather than their proven effects; however this does not mean that they are all ‘quack’remedies! There may even be some value in medicines such as tiger bone, bear gall, turtle shell, dried centipedes, bat dung and so on. The herbs, however, are well researched and are becoming increasingly popular as people become disillusioned with Western Medicine.”
It is irresponsible to give any solace at all to the wicked industries that kill tigers and torture bears to extract their bile. And it is simple untrue that “herbs are well-researched”. Try the test,
A simple test for herbalists. Next time you encounter a herbalist, ask them to name the herb for which there is the best evidence of benefit when given for any condition. Mostly they refuse to answer, as was the case with Michael McIntyre (but he is really an industry spokesman with few scientific pretensions). I asked Michael Heinrich, Professor of Pharmacognosy at the School of Pharmacy. Again I couldn’t get a straight answer. Usually, when pressed, the two things that come up are St John’s Wort and Echinacea. Let’s see what The National Center for Complementary and Alternative Medicine (NCCAM) has to say about them. NCCAM is the branch of the US National Institutes of Health which has spent around a billion dollars of US taxpayers’ money on research into alternative medicine, For all that effort they have failed to come up with a single useful treatment. Clearly they should be shut down. Nevertheless, as an organisation that is enthusiastic about alternative medicine, their view can only be overoptimistic.
For St John’s Wort . NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
For Echinacea NCCAM says
- Study results are mixed on whether echinacea can prevent or effectively treat upper respiratory tract infections such as the common cold. For example, two NCCAM-funded studies did not find a benefit from echinacea, either as Echinacea purpurea fresh-pressed juice for treating colds in children, or as an unrefined mixture of Echinacea angustifolia root and Echinacea purpurea root and herb in adults. However, other studies have shown that echinacea may be beneficial in treating upper respiratory infections.
If these are the best ones, heaven help the rest.
Follow-up
The mainstream media eventually catch up with bloggers. BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. It also exposed the uselessness of the Quality Assurance Agency (QAA). Both these things have been written about repeatedly here for some years. It was good to see them getting wider publicity.
Watch the video of the programme (Part 1, and Part 2) "Week In Week Out – University Challenged." “The programme examines how pop stars and evangelical Christians are running colleges offering courses validated by the University of Wales.” (I make a brief appearance, talking about validation of degrees in Chinese Medicine).

In October 2008 I posted Another worthless validation: the University of Wales and nutritional therapy. With the help of the Freedom of Information Act, it was possible to reveal the mind-boggling incompetence of the validation process used by the University of Wales.
McTimoney College of Chiropractic
The Chiropractic “degrees” from the McTimoney College of Chiropractic are also validated by the University of Wales by an equally incompetent, or perhaps I should say bogus, procedure. More details can be found at The McTimoney Chiropractic Association would seem to believe that chiropractic is “bogus”, and in a later post, Not much Freedom of Information at University of Wales, University of Kingston, Robert Gordon University or Napier University.
Andy Lewis has also written about chiropractic in The University of Wales is Responsible for Enabling Bogus* Chiropractic Claims to be Made.
Sadly the BBC programme did not have much to say about these domestic courses, but otherwise it was excoriating. In particular it had extensive interviews with Nigel Palastanga, whose astonishing admission that courses were validated withour seeing what was taught on them was revealed here two years ago. After that revelation, the vice-chancellor of UoW, Marc Clement BSc PhD CEng CPhys FIET FInstP, promoted Palastanga to be pro-vice-chancellor in charge of Learning, Teaching and Enhancement (I know, you couldn’t make it up).

In the documentary Palastanga said
"It’s a major business. We earn a considerable amount of money."
That was obvious two years ago, but it’s good to hear it from the horse’s mouth.
After a section that revealed a bit about what goes on at two very fundamentalist bible colleges which gave University of Wales degrees, A. C. Grayling commented thus.
"They are there to train advocates for the biblical message and that is absolutely not, by a very very long chalk, what a university should be doing.. . . A respectable British Higher education institution like the University of Wales shouldn’t be touching them with a bargepole."
Undaunted, Palastanga responded
“That’s his opinion. I would say they are validated to the highest standards. They match what are called QAA benchmark. We have serious academics looking at them, and their academic standards are established at the very highest level.”
And if you believe that, you will truly believe anything.
You can download here one of many moderator’s reports obtained under the Freedom of Information Act. This one is for the BSc (Hons) Chiropractic. It is entirely typical of theuncritical boxticking approach to validation, Nowhere does it say "subluxation is nonsense", though even the GCC now admit that.
Traditional Chinese Medicine
The University of Wales validates several courses in what almost everyone but them classifies as quackery. As well as chiropractic and “nutritional therapy”, there is herbalism. For example a course at a college in Barcelona issues University of Wales degrees in Traditional Chinese medicine, a subject that is a menace to public health.. I was asked to comment on the course, and on a bag of herbs that the presenter had been sold to treat depression.
|
Radix Bupleuri Chinensis
Radix Angelicae Sinensis Radix Paeoniae Lactiflorae Rhizoma Atractylodis Macrocephalae Sclerotium Poriae Cocos Radix Glycyrrhizae Uralensis Cortex Moutan Radicis (Paeonia Suffruticosa) Fructus Gardeniae Jasminoidis Herba Menthae Haplocalycis Zingiber officinale rhizome-fresh |
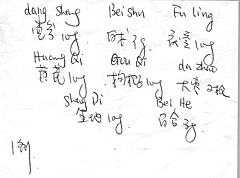 Ingredients of a custom mixture. |
There is no good evidence that any of the ingredients help depression, in fact next to nothing is known about most of them, apart from liquorice and ginger. Swallowing them would be rather reckless. They fall right into the description of any herbal medicine, in the Patients’ Guide, "Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety. "
Of the degrees, I said
"There’s no evidence that it [the herbs] does you any good. It may be dangerous because you have no idea of the dose. Degrees in Chinese Medicine consist of three years spent memorising myths and pre-scientific, er, untruths. That isn’t a degree, it’s a travesty."
Palastanga. responded
"We’ve had long debates in the Health Committee about where we would draw the line about what we validate. They have to demonstrate to us that there is some scientific basis for the practice, that there is an established curriculum, that there is an established safe practice."
The presenter asked him "So you are confident that Chinese medicine works? Palastanga replied
" I didn’t say that. I said that there is evidence that it does work . . We are trying to enforce these professions to undertake effective research."
That statement is simply not true, as shown by the response of the validation committee to the application for validation of the course in “Nutritional Therapy” at the Northern College of Acupuncture, documented previously. The fact of the matter is that the validation proceeded without looking at what was actually taught, and without even a detailed timetable of lectures. The committee looked only at the official documents presented to it and was totally negligent in failing to discover some of the bizarre beliefs of the people who were giving the course.
Palastanga went on to raise the usual straw man argument, about how little regular medicine is based on good evidence (though admittedly that is certainly true in his own field -he is a physiotherapist).
Fazley International College Kuala Lumpur

This business college in Kuala Lumpur offered University of Wales degrees. Its 32-year old president is a part time pop star with impressive looking qualifications
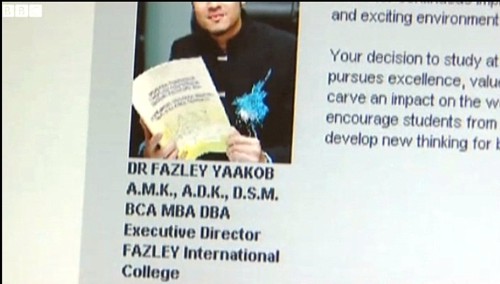
The presenter pointed out that
" His doctorate and his MBA were awarded in that citadel of education, Cambridge. Here he is, pictured at the city’s prestigious business school. He was there for all of four days and walked away with a doctorate. But the degree was not from the University of Cambridge, but from the now defunct "European Business School Cambridge". It never had the right to award degrees."
Neither the University of Wales nor the QAA had noticed this unfortunate fact. Once the TV team had done their job for them, the UoW withdrew support. though, as of 15 November 2010, that is not obvious from Fazley’s web site.
Mr (not Dr) Fazley seemed rather pleased about how students were attracted by the connection with the Prince of Wales. The fact that he is Chancellor of the University of Wales seems not inappropriate, given the amount of quackery they promote.
Quality Assurance Agency (QAA)
In 2007, I wrote, in Nature (see also here),
“Why don’t regulators prevent BSc degrees in anti-science? The Quality Assurance Agency for Higher Education (QAA) claims that “We safeguard and help to improve the academic standards and quality of higher education in the UK.” It costs taxpayers £11.5 million (US$22 million) annually. It is, of course, not unreasonable that governments should ask whether universities are doing a good job. But why has the QAA not noticed that some universities are awarding BSc degrees in subjects that are not, actually, science? The QAA report on the University of Westminster courses awards a perfect score for ‘curriculum design, content and organization,’ despite this content consisting largely of what I consider to be early-nineteenth-century myths, not science. It happens because the QAA judges courses only against the aims set by those who run the QAA, and if their aims are to propagate magic as science, that’s fine.”
That was illustrated perfectly in the documentary when Dr Stephen Jackson of the QAA appeared to try to justify the fact that the QAA had, like the University of Wales, failed entirely to spot any of the obvious problems. He had a nice dark suit, tie and poppy, but couldn’t disguise the fact that the QAA had given high ratings to some very dubious courses.
The QAA sent nine people to the other side of the globe, at a cost of £91,000. They could have done a lot better if they’d spent 10 minutes with Google at home.
Universities UK (UUK)
Needless to say, the Committee of Vice-Chancellors and Principals has said nothing at all. As usual, Laurie Taylor had it all worked out in Times Higher Education (4th November).
Speaking to our reporter Keith Ponting (30), he commended UUK’s decision to say absolutely nothing whatsoever about the abolition of all public funding for the arts and humanities.
He also praised UUK’s total silence on Lord Browne’s view that student courses should primarily be evaluated by their employment returns.
When pressed by Ponting for his overall view of UUK’s failure to respond in any way at all to any aspect of the Browne Review, he described it as “welcome evidence, in a world of change, of UUK’s consistent commitment over the years to ineffectual passivity”.
Meanwhile, a University of Wales video on YouTube
Caveat emptor
Follow-up
A couple of days later, a search of Google news for the “University of Wales” shows plenty of fallout. The vice-chancellor claims that ““The Minister’s attack came as a complete and total surprise to me”. That can’t be true. It is over two years since I told him what was going on, and if he was unaware of it, that is dereliction of duty. It is not the TV programme that brought the University into disrepute, it was the vice-chancellor.
Systems biology is all the rage, No surprise then, to see the University of Westminster advertising a job for a systems biologist in the The Department of Molecular and Applied Biosciences. Well, no surprise there -until you read the small print.
Much has been wriiten here about the University of Westminster, which remains the biggest provider of junk sciencne degrees in the UK, despite having closed two of them.
Senior Lecturer in Systems BiologyUniversity of Westminster – Department of Molecular and Applied Biosciences, School of Life SciencesCavendish Site Salary £37,886 – £50,751 (Inc. LWA) The Department of Molecular and Applied Biosciences wishes to appoint a Senior Lecturer in Systems Biology. The post-holder will teach on the undergraduate and postgraduate degree programmes within the School of Life Sciences, particularly in the areas of Molecular Biology, Bioinformatics and/or statistics, establish their own and participate in ongoing research programmes and undertake external income generation activities. The candidate should have an active interest in bridging the gap between western life sciences and Chinese medicine using emerging systems biology approaches, specifically in metabolomics and proteomics with a goal of developing novel diagnostic technologies facilitating the creation of a personalised approach to medical care. They should therefore be willing to work closely with colleagues in the life sciences as well as with clinicians and clinical researchers from within the East Asian medical tradition. The post is available from 1st October 2010 or as soon as possible thereafter. The closing date for applications, together with a short statement on why you believe you are suitable for the position and a description of your research plans, is Monday 6th September 2010. Interviews are expected to be held later in September. Administrative contact (for queries only): Tayjal Tailor (t.tailor1@wmin.ac.uk) Reference Number: 50000360 Closing Date: Friday 3 September 2010 |
A note about systems biology
Systems biology is about about how whole organs behave, as opposed to single cells or single molecules, It has to be the ultimate aim of biology. There is one case in which this has been done with some success, That is the modelling of the behaviour of the whole heart by Denis Noble and his colleagues in the Phyiology department (now gone) in Oxford. They adopted a bottom up approach. They measured the currents that flow though many sorts of ion channels in single cells from various parts of the heart, and how individual cells communicate with each other. Starting from this solid basis, together with a lot of computer power, they were able to model successfully a lot of phenomena that occur in the whole heart, but can’t be investigated in single cells. For example their work cast light on abnormal heart rhythms like ventricular fibrillation, and on the effect of drugs on heart rhythm.
This work was mostly done before the term ‘systems biology" thought of. It was called physiology. It is impressive work, and systems biology became a fashionable buzzword among research administrators and funding agencies. Despite the amount of money thrown at the problem, I’m not aware of any success that remotely approaches Noble’s.. One reason for that is that people have not been willing to put in the groundwork. In the case of the heart, the models were built on -many years of basic research on the electrophysiology of single heart cells. People have tried to model from the top down, without doing the spade work first. There has developed a perception that computing power can compensate for lack of basic knowledge about things work. It can’t. The usual aphorism applies: garbage in, garbage out.
Here’s an example, which eas noted in the diary pages for 29 June, 2008. While in Edinbuurgh, to give a talk to the European Conference on Mathematical and Theoretical Biology, I noticed a poster. It described an attempt to model on a computer the entire metabolic network of yeast.
“81 of the 662 intracellular concentrations were defined . . . The remainder were set to the median concentration of c. 0.2 mM.”
Ahem. We didn’t know the concentrations so we just made them up so we could run the program.
It’s interesting that even people in the business seem to realise that even that it isn’t living up to the hype. The Fixing proteomics web site shows why.
Put another way, if you try to run before you can walk, you risk falling falling on your face.
For these reasons, it seems to me that that most attempts at system biology have been disappointing (please correct me if I’m wrong)
Systems biology for Chinese medicine
If systems biology suffers from trying to run before it can walk in regular biology, where at least something is known about the functions of cells, how much more true that must be of Chinese medicine. In Chinese medicine almost all the treatments have never been tested properly in man. The odds are that most don’t work at all, and some are very poisonous (not to mention the cruelty and destruction of endangered species that is involved in making some of their more bizarre medicines). The idea that you can explain it with systems biology, is ludicrous in the extreme.
One can’t imagine any vaguely competent biologist who’d want to touch a project as bizarre as this with a bargepole.
Eastmedicine
This advertisement stems presumably from EASTmedicine is the University of Westminster’s research centre for East Asian Sciences and Traditions in Medicine. The proclaimed aims are to focus on “understanding, development and evaluation of East Asian medicines as living traditions”. The director of EASTmedicine, Volker Scheid, is a herbalist and acupuncturist and, as such, a firm believer in alternative medicine. When he isn’t at the University he has a private practice, the Traditional Acupuncture Centre, in London.
The website of his private practice makes some astonishing claims
"Acupuncture is effective in the treatment of numerous conditions including headache, migraine, digestive problems, menstrual disorders, indeterminate aches and pains, asthma, hayfever, stress, tiredness, depression and anxiety. Also commonly treated are chronic conditions such as arthritis, back pain, ulcerative colitis, irritable bowel syndrome, eczema, sinusitis, high blood pressure and repetitive strain injuries."
These claims simply cannot be justified by any worthwhile evidence. It will be interesting to see what Trading Standards make of them.
Dr Scheid describes himself as a "scholar physician". Physician seems a rather pretentious description for someone whose qualifications are stated to be PhD, MBAcC, FRCHM. But in similar vein he describes himself thus "I am one of the West’s leading experts on Chinese medical formulas and treatment strategies".
Although Scheid sells acupuncture treatments to patients, he seems ro be more anthropologist than medical. In a discussion of two acupuncture papers
"From the Perspective of the Anthropologist –
Volker Scheid, London, UK
From a perspective anchored in the cultural studies of science, technology and medicine my main interest in these papers is their status as cultural artifacts that provide access to the lifeworlds of a particular research community. If any, life-world debate and argument marks sites of contestation." Forsch Komplementärmed 2007;14:371–375
Scheid shows not the slightest interest in whether acupuncture works other than as a placebo. Since he is selling acupuncture, he presumably starts from the premise that it works.
Volker Scheid has had a £205,000 Wellcome Trust for the History of Medicine Project Grant: 2009 2012; Treating the Liver: Towards a Transnational History of East Asian Medicine; There’s nothing wrong with writing the history of long-outdated systems of medicine, though one could hardly imagine that the history would be very impartial, when it is written by a true believer. Another taste of his style can be found in his paper on Globalising Chinese Medical Understandings of Menopause. There is lots of rather pretentious stuff about culture, but very little about what actually works, Towards the end of the paper we come to the usual feeble excuse.
" . . once traditional medicines allow themselves to be evaluated by biomedical research methods, the odds against receiving fair treatment are heavily stacked against them."
The translation of that into plain English is something like ‘when we test our treatments properly we find they don’t work, so we blame the methods and carry on with selling them anyway’.
Judging from its web site, EASTmedicine does not to do any serious clinical trials to test whether the treaments work in man, They just know that they do. But they are hoping to add some spurious scientific background to their dubious claims by hiring someone to do compuations that will cast no light whatsoever on the question that really matters, Do they work or not?
The agenda is made clear by the statement
EASTmedicine seeks to describe and analyse the dynamics of these transformations with a specific view of managing their integration into contemporary health care.
So it is just yet another group of people pushing to have unproven and disproved treatments accepted by real medicine.
The University of Westminster appears to be determined to make itself the laughing stock by persisting in promoting junk science at a time when most other universities have realise that the harm done to their reputations is not worth the income it generates, Plenty of it has been revealed here.
The vice-chancellor of Westminster, Prof Geoffrey Petts, made into the pages of Private Eye (see Crystal balls. Professor Petts in Private Eye when he announced that he wouldn’t get rid of the junk, but would make it more ‘scientific’. Well, credit where it’s due, They have dropped homeopathy. see The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University For 2010 they still off ten different “BSc (Hons)” degrees in pre-scientific forms of medicine. It will take more than a bit od talk about systems biology to make anyone believe that these courses have anything to do with science.
For example, look at some slides from their lectures on “energy medicine”, Westminster University BSc: “amethysts emit high yin energy”
More make-believe from the University of Westminster. This time it’s Naturopathy , or
Why degrees in Chinese medicine are a danger to patients
The Dean of the School of the Life Sciences, Jane Lewis, is an entirely respectable marine biologist. She has had the thankless task of merging the real science with the alternative medicine in a single school. I phoned her to get a reaction
" outcome of merger of the school and trying to bring various parts of the school together" " "things are much more rigorous than they were".
DC: "Why don’t you just phase it out?"
"I’m not in a poition to do that. i move things forward as seems best -for the whole school I have to say". We’re retaining those bits thatI think have some good standing -I see NICE has approved the use of acupuncture for lower back pain and some other bits and pieces so I see acupuncture as something that does have some standing, andwe make sure it rigorously taught"
"DCHave you looked at the stuff on naturopathy?" "Are amethysts emit high Yin energy still taught?" " i don’t think so".
It seems, as so often in this case, that the senior people don’t really know what’s being taught under their noses. Prof
Lewis says she has not read about the background
to the (unusually) daft advice from NICE. Neither has she read Barker Bausell’s book on acupuncture research. If she had done any of these things,I suspect she would not have such a high opinion of it as appears to be the case.
Bait and switch. Astonishingly there is a now a whole organisation devoted to the respectabalisation of Traditional Chinese Medicine Good Practice in Traditional Chinese Medicine Research in the Post-genomic Era It sounds nice and sciencey but, as usual, they are trying to run before they can walk. The first thing has to be to do good clinical trials to find out if there is anything there to be investigated. If, and only if, this is the case, would there be any case for fancy talk about "proteomics"
and "the post-genomic era".
I do hope that no funding agency would be fooled into parting with money on the basis of the present vacuous rhetoric.
Professor Lewis said that I have I have quoted things like "amethysts emit high Yin energy" out of context. There is a simple solution to that. I have asked Westminster to make available the entire contents of the courses. Then we shall all be able to see the context of what their sudents are being taught.
Follow up
A brief report of this matter has appeared in Times Higher Education. In a statement, the University of Westminster says “its research into Chinese medicine is following the lead of “top research institutions”. I’m not aware of anyhting quite like this from anywhere else. In any case, Westminster should be able to think for themselves.
It seems very reasonable to suggest that taxpayers have an interest in knowing what is taught in universities. The recent Pittilo report suggested that degrees should be mandatory in Acupuncture, Herbal Medicine and Traditional Chinese Medicine. So it seems natural to ask to see what is actually taught in these degrees, so one can judge whether it protects the public or endangers them.
Since universities in the UK receive a great deal of public money, it’s easy. Just request the material under the Freedom of Information Act.
Well, uh, it isn’t as simple as that.
Every single application that I have made has been refused. After three years of trying, the Information Commissioner eventually supported my appeal to see teaching materials from the Homeopathy "BSc" at the University of Central Lancashire. He ruled that every single objection (apart from one trivial one) offered by the universities was invalid. In particular, it was ruled that univerities were not "commercial" organisations for the purposes of the Act.
So problem solved? Not a bit of it. I still haven’t seen any of the materials from the original request because the University of Central Lancashire appealed against the decision and the case of University of Central Lancashire v Information Commissioner is due to be heard on November 3rd, 4th and 5th in Manchester. I’m joined (as lawyers say) as a witness. Watch this space.
UCLan is not the exception. It is the rule. I have sought under the Freedom of Information Act, teaching materials from UClan (homeopathy), University of Salford (homeopathy, reflexology and nutritional therapy), University of Westminster (homeopathy, reflexology and nutritional therapy), University of West of England, University of Plymouth and University of East London, University of Wales (chiropractic and nutritional therapy), Robert Gordon University Aberdeen (homeopathy), Napier University Edinburgh (herbalism).
In every single case, the request for teaching materials has been refused. And that includes the last three, which were submitted after the decision of the Information Commissioner. They will send things like course validation documents, but these are utterly uninformative box-ticking documents. They say nothing whatsoever about what is actually taught.
The fact that I have been able to discover quite a lot about what’s being taught owes nothing whatsoever to the Freedom of Information Act. It is due entirely to the many honest individuals who have sent me teaching materials, often anonymously. We should be grateful to them. Their principles are rather more impressive than those of their principals.
Since this started about three years ago, two of the universities, UCLan and Salford, have shut down entry to all of their CAM courses. And Westminster has shut two of them, with more rumoured to be closing soon. They are to be congratulated for that, but is far from being the end of the matter. The Department of Health, and some of the Royal Colleges, have yet to catch up with the universities, The Pittolo report, which recommends making degrees compulsory, is being considered by the Department of Health. The consultation ends on November 2nd: if you haven’t yet responded, please do so now (see how here, and here).
A common excuse: the university does not possess teaching materials (yes, really)
Several of the universities claim that they cannot send teaching materials, because they have no access to them. This happens when the university has accredited a course that is run by another, privately run, institution. The place that does the actual teaching, being private, is exempt from the Freedom of Information Act.
The ludicrous corollary of this excuse is that the university has accredited the course without checking on what is taught, and in some cases without even having seen a timetable.
The University of Wales
In fact the University of Wales doesn’t run courses at all. Like the (near moribund) University of London, it acts as a degree-awarding authority for a lot of Welsh Universities. It also validates a lot of courses in non-university institutions, 34 or so of them in the UK, and others scattered round the world.
Many of them are theological colleges. It does seem a bit odd that St Petersburg Christian University, Russia, and International Baptist Theological Seminary, Prague, should be accredited by the University of Wales.
They also validate the International Academy of Osteopathy, Ghent (Belgium), Osteopathie Schule Deutschland, the Istituto Superiore Di Osteopatia, Milan, the Instituto Superior De Medicinas Tradicionales, Barcelona, the Skandinaviska Osteopathögskolan (SKOS) Gothenburg, Sweden and the College D’Etudes Osteopathiques, Canada.
The 34 UK institutions include the Scottish School of Herbal Medicine, the Northern College of Acupuncture and the Mctimoney College of Chiropractic.
The case of the Nutritional Therapy course has been described already in Another worthless validation: the University of Wales and nutritional therapy. It emerged that the course was run by a grade 1 new-age fantasist. It is worth recapitulating the follow up.
What does the University of Wales say? So far, nothing. Last week I sent brief and polite emails to Professor Palastanga and to
Professor Clement to try to discover whether it is true that the validation process had indeed missed the fact that the course organiser’s writings had been described as “preposterous, made-up, pseudoscientific nonsense” in the Guardian.
So far I have had no reply from the vice-chancellor, but on 26 October I did get an answer from Prof Palastanga.
As regards the two people you asked questions about – J.Young – I personally am not familiar with her book and nobody on the validation panel raised any concerns about it. As for P.Holford similarly there were no concerns expressed about him or his work. In both cases we would have considered their CV’s as presented in the documentation as part of the teaching team. In my experience of conducting degree validations at over 16 UK Universities this is the normal practice of a validation panel.
I have to say this reply confirms my worst fears. Validation committees such as this one simply don’t do their duty. They don’t show the curiosity that is needed to discover the facts about the things that they are meant to be judging. How could they not have looked at the book by the very person that they are validating? After all that has been written about Patrick Holford, it is simply mind-boggling that the committee seems to have been quite unaware of any of it.It is yet another example of the harm done to science by an unthinking, box-ticking approach.
Incidentally, Professor Nigel Palastanga has now been made Pro Vice-Chancellor (Quality) at the University of Wales and publishes bulletins on quality control. Well well.
The McTimoney College of Chiropractic was the subject of my next Freedom of Information request to the University of Wales. The reasons for that are, I guess, obvious. They sent me hundreds of pages of validation documents, Student Handbooks (approx 50 pages), BSc (Hons) Chiropractic Course Document. And so on. Reams of it. The documents mostly are in the range of 40 to 100 pages. Tons of paper, but none of it tells you anyhing whatsover of interest about what’s being taught. They are a testament to the ability of universities to produce endless vacuous prose with
very litlle content.
They did give me enough information to ask for a sample of the teaching materials on particular topics. But I gor blank refusal, on the grounds that they didn’t possess them. Only McTimoney had them. Their (unusually helpful) Freedom of Information officer replied thus.
“The University is entirely clear about the content of the course but the day to day timetabling of teaching sessions is a matter for the institution rather than the University and we do not require or possess timetable information. The Act does not oblige us to request the information but there is no reason you should not approach McTimoney directly on this.”
So the university doesn’t know the timetable. It doesn’t know what is taught in lectures, but it is " entirely clear about the content of the course".
This response can be described only as truly pathetic.
Either this is a laughably crude form of obstruction of my request, or perhaps, even more frighteningly, the university really believes that its endless box-ticking documents actually provide some useful control of quality. Perhaps the latter interpretation is more charitable. After all, the QAA, CHRE, UUK and every HR department share similar delusions about what constitutes quality.
Perhaps it is just yet another consequence of having science run largely by people who have never done it and don’t understand it.
Validation is a business. The University of Wales validates no fewer than 11,675 courses altogether. Many of these are perfectly ordinary courses in universities in Wales, but they validate 594 courses at non-Welsh accredited institutions, an activity that earned them £5,440,765 in the financial year 2007/8. There’s nothing wrong with that if they did the job properly. In the two cases I’ve looked at, they haven’t done the job properly. They have ticked boxes but they have not looked at what’s being taught or who is teaching it.
The University of Kingston
The University of Kingston offers a “BSc (Hons)” in acupuncture. In view of the fact that the Pittilo group has recommended degrees in acupuncture, there is enormous public interest in what is taught in such degrees, so I asked.
They sent the usual boring validation documents and a couple of sample exam papers . The questions were very clinical, and quite beyond the training of acupuncturists. The validation was done by a panel of three, Dr Larry Roberts (Chair, Director of Academic Development, Kingston University), Mr Roger Hill (Accreditation Officer, British Acupuncture Accreditation Board) and Ms Celia Tudor-Evans (Acupuncturist, College of Traditional Acupuncture, Leamington Spa). So nobody with any scientific expertise, and not a word of criticism.
|
Further to your recent request for information I am writing to advise that the University does not hold the following requested information: (1) Lecture handouts/notes and powerpoint presentations for the following sessions, mentioned in Template 3rd year weekend and weekday course v26Aug2009_LRE1.pdf (a) Skills 17: Representational systems + Colour & Sound ex. Tongue feedback 11 (b) Mental Disease + Epilepsy Pulse feedback 21 (c) 18 Auricular Acupuncture (d) Intro. to Guasha + practice Cupping, moxa practice Tongue feedback 14 (2) I cannot see where the students are taught about research methods and statistics. I would like to see Lecture handouts/notes and PowerPoint presentations for teaching in this area, but the ‘timetables’ that you sent don’t make clear when or if it is taught. The BSc Acupuncture is delivered by a partner college, the College of Integrated Chinese Medicine (CICM), with Kingston University providing validation only. As such, the University does not hold copies of the teaching materials used on this course. In order to obtain copies of the teaching materials required you may wish to contact the College of Integrated Chinese Medicine directly. This completes the University’s response to your information request. |
So again we see that Kingston has validated the course but has not seen a timetable, far less what is taught. My reply was thus
|
Yes I am exceedingly unhappy about it. The university attaches its name to the course so it must obviously be able to get the material simply by asking for it (I’m surprised that the university should endorse a course without knowing what is taught on it, but that’s another matter). I request formally that you obtain this material. If necessary please read this as a formal appeal. |
I await with interest. In every single case so far, the internal review has merely confirmed the initial refusal. It means a bit of a delay before the case goes to the Information Commisssioner’s Office.
Napier University Edinburgh
Napier University runs a "BSc (Hons) Herbal medicine". (brochure here). Since herbal medicine is a subject of the Pittilo recommendations, there is enormous public interest in what they teach. So I asked, under the Freedom of Information (Scotland) Act (2002). They sent quite quickly validation and accreditation documents, some examination papers, timetables and lecture lists.
The validation was the usual vacuous box-ticking stuff though it did reveal that the course “made extensive use of techniques such as tongue and pulse diagnosis”, which are well known phoney diagnosis methods, about as much use as a pendulum (as used at Westminster University).
As at Kingston University, the exam papers they chose to send were mostly "pretend doctor" stuff. One of them was
Discuss the herbal practitioner’s role in the management of IHD [ischaemic heart disease)
How one would like to see what the students said, and, even more one would like to see the model answer. Amateurs who try to treat potentially serious conditions are a danger to the public.
So then we got to the interesting bit, the request for actual teaching materials.
|
I have looked at the material that you sent and I’d now like to make the following supplementary request (A) Lecture notes/handouts and powerpoint slides for the following small smaple of lectures HRB09102 Materia Medica 4 Materia Medica 3 HRB08103 Clinical Medicine and Diagnosis 4 (HRB09104) HRB09100 Materia Medica & Herbal Practice BSc Herbal Medicine : Materia Medica HRB07102 Lastly, I can see nowhere in the timetable, lectures that deal with Research methods, clinical trial design and statistics. |
No prizes for guessing the result Total refusal to send any of them. To make matters worse, the main grounds for refusal were the very "commercial interests" which, after careful legal examination, the Information Commissioner (for England and Wales) had decided were invalid. They say too that "The public interest in withholding the information is greater than the public interest in its release".. It is hard to see how the public interest is served by concealing from the people who pay for the degrees what is taught on degrees that Pittilo wants to make compulsory. [Download the whole response]
The matter is now under internal appeal (read the appeal) and eventually we shall find out whether the Scottish Information Commissioner backs the judgement.
Robert Gordon University Aberdeen
This case has particular interest because the Vice-Chancellor of Robert Gordon University is Professor Michael Pittilo, chair of the highly contentious steering group that recommended degress in CAM. Robert Gordon University (RGU) does not teach herbal medicine or acupuncture. But they do run An Introduction to Homeopathy. All the degrees in homeopathy have closed. It is perhaps the daftest and most discredited of all the popular forms of Magic Medicine. But Professor Pittilo thinks it is an appropriate subject to teach in his university.
So again I asked for information under the Freedom of Information (Scotland) Act 2002. They sent me quite quckly a list of the powerpoint presentations used on the courses [download it]. I asked for a small sample of the powerpoints. And again the university did not possess them!
|
I should like to see only the following three powerpoint presentations in the first instance, please.
Please can you let me know also who produced the powerpoints. (1) Evidence for homeopathy I note that you will have to request them but since they are being offered as part of a course offered by RGU, so RGU is responsible for their quality, I presume that this should cause no problem. |
The request was refused on much the same grounds as used by Napier University. As usual, the internal review just confirmed the initial proposal (but dropped the obviously ludicrous public interest defence). The internal review said
“it is mainly the quality of our courses (including course material) and teaching which has given us the position of "the best modern university in Scotland"
I am bound to ask, if the university is so proud of its course material, why is it expending so much time and money to prevent anyone from seeing a small sample of it?
My appeal has been sent to the Scottish Information Commissioner [download the appeal].
What are vice-chancellors thinking about?
I find it very difficult to imagine what is going through the heads of vice-chancellors who run courses in mumbo-jumbo. Most of them don’t believe a word of it (though Michael Pittilo might be an exception) yet they foist it on their students. How do they sleep at night?
Recently the excellent Joe Collier wrote a nice BMJ blog which applauded the lack of respect for authority in today’s students, Joe Collier says good riddance to old-fashioned respect. I couldn’t resist leaving a comment.
|
I couldn’t agree more. There is nothing quite so unnerving as being addressed as “Sir”. It is an advantage of age that you realise what second-rate people come to occupy very grand positions. Still odder since, if occasionally they are removed for incompetence, they usually move to an even grander position. I guess that when I was an undergraduate, I found vice-chancellors somewhat imposing. That is, by and large, not a view that survives closer acquaintance. |
Should teaching materials be open to the public?
There is only one university in the world that has, as a matter of policy, made all of its teaching material open to the public, that is the Massachusetts Institute of Technology (MIT). I can recommend strongly course 18.06, a wonderful set of lectures on Linear Algebra by Gilbert Strang. (It is also a wonderful demonstration of why blackboards may be better than Powerpoint for subjects like this). Now they are on YouTube too.
A lot of other places have made small moves in the same direction, as discussed recently in Times Higher Education, Get it Out in the Open.
Now the OU is working with other British universities to help them develop and share open course materials. In June, at the celebrations for the 40th anniversary of the OU, Gordon Brown announced funding to establish the Support Centre for Open Resources in Education at the OU, as part of a £7.8 million grant designed to enhance the university’s national role.
The funding follows a separate grant of £5.7 million from the Higher Education Funding Council for England for universities across the sector to make thousands of hours of free learning materials available.
Much material is available on the web, when individual teachers choose to place it there, but at the same time there is a move in the other direction. In particular, the widespread adoption of Moodle has resulted in a big decrease in openness. Usually you have to be registered on a course to see the material. Even other people in the university can’t see it. I think that is a deplorable development (so, presumably, does HEFCE).
Conclusion
I was told by the Univerity of Kingston that
“The course is one which the University has validated and continues to be subject to the University’s quality assurance procedures, such as internal subject reviews, annual monitoring and external examining”
The only conclusion to be drawn from this is that “quality arrurance procedures” work about as well in universities as they did in the case of baby Peter. No doubt they were introduced with worthy aims. But in practice they occupy vast amounts of time for armies of bureaucrats, and because the brain does not need to be engaged they end up endorsing utter nonsenes. The system is broken.
Resistance is futile. You can see a lot of the stuff here
It is hard to keep secrets in the internet age. Thanks to many wonderful people who have sent me material. you can see plenty of what is taught, despite the desperate attempts of vice-chancellors to conceal it. Try these links.
What is actually taught
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself
https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients
https://www.dcscience.net/?p=2043
More make-believe from the University of Westminster. This time its Naturopathy
https://www.dcscience.net/?p=1812
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
https://www.dcscience.net/?p=1329
The opposite of science
https://www.dcscience.net/?p=1191
Bad medicine. Barts sinks further into the endarkenment.
https://www.dcscience.net/?p=1143
A letter to the Times, and progress at Westminster
https://www.dcscience.net/?p=984
Nutritional Fairy Tales from Thames Valley University
https://www.dcscience.net/?p=260
Westminster University BSc: amethysts emit high yin energy
https://www.dcscience.net/?p=227
References for Pittilo report consultation
A very bad report: gamma minus for the vice-chancellor
https://www.dcscience.net/?p=235
The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on the Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire,
https://www.dcscience.net/?p=2310
An excellent submission to the consultation on statutory regulation of alternative medicine (Pittilo report)
https://www.dcscience.net/?p=2329
Follow-up
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
More boring politics, but it matters. The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register should normally be through a Bachelor degree with Honours
For the background on this appalling report, see earlier posts.
A very bad report: gamma minus for the vice-chancellor
The Times (blame subeditor for the horrid title), and some follow up on the Times piece
The Health Professions Council breaks its own rules: the result is nonsense
Chinese medicine -acupuncture gobbledygook revealed
Consultation opens on the Pittilo report: help stop the Department of Health making a fool of itself
Why degrees in Chinese medicine are a danger to patients
The Department of Health consultation shuts on November 2nd. If you haven’t responded yet, please do. It would be an enormous setback for reason and common sense if the government were to give a stamp of official approval to people who are often no more than snake-oil salesman.
Today I emailed my submission to the Pittilo consultation to the Department of Health, at HRDListening@dh.gsi.gov.uk
The submission
I sent the following documents, updated versions of those already posted earlier.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
- An example of dangerous (and probably illegal) claims that are routinely made by TCM practitioners [download pdf]f
I also completed their questionnaire, despite its deficiencies. In case it is any help to anyone, this is what I said:
The questionnaire
Q1: What evidence is there of harm to the public currently as a result of the activities of acupuncturists, herbalists and traditional Chinese medicine practitioners? What is its likelihood and severity?
Harm
No Harm
Unsure
Comment
The major source of harm is the cruel deception involved in making false claims of benefit to desperate patients. This applies to all three.
In the case of herbal and TCM there is danger from toxicity because herbal preparations are unstandardised so those that do contain an active ingredient are given in an unknown dose. This is irresponsible and dangerous (but would not be changed by the proposals for regulation).
In addition TCM suffers from recurrent problems of contamination with heavy metals, prescription drugs and so on. Again this would not be the business of the proposed form of regulation.
Q2: Would this harm be lessened by statutory regulation? If so, how?
Yes
No
Unsure
The proposed form of regulation would be no help at all. The HPC has already said that it is not concerned with whether or not the drug works, and, by implication, does not see itself as preventing false health claims (just as the GCC doesn’t do this). False claims are the responsibility of Trading Standards who are meant to enforce the Consumer Protection Unfair Trading Regulations (May 2008), though they do not at present enforce them very effectively. Also Advertisng Standards. The proposed regulation would not help, and could easily hinder public safety as shown by the fact that the GCC has itself been referred to the Advertisng Standards Authority.
The questions of toxicity and contamination are already the responsibility of Trading Standards and the MHRA. Regulation by the HPC would not help at all. The HPC is not competent to deal with such questions.
Q3: What do you envisage would be the benefit to the public, to practitioners and to businesses, associated with introducing statutory regulation?
Significant benefit
Some benefit
No benefit
Unsure
This question is badly formulated because the answer is different according to whether you are referring to the public, to practitioners or to businesses.
The public would be endangered by the form of regulation that is proposed, as is shown very clearly by the documents that I have submitted separately.
In the case of practitioners and businesses, there might be a small benefit, if the statutory regulation gave the impression that HM and TCM had government endorsement and must therefore be safe and effective.
There is also one way that the regulation could harm practitioners and businesses. If the HPC received a very large number of complaints about false health claims, just as the GCC has done recently, not only would it cost a large amount of money to process the claims, but the attendant bad publicity could harm practitioners. It is quite likely that this would occur since false claims to benefit sick people are rife in the areas of acupuncture, HM and TCM.
Q4: What do you envisage would be the regulatory burden and financial costs to the public, to practitioners, and to businesses, associated with introducing statutory regulation? Are these costs justified by the benefits and are they proportionate to the risks? If so, in what way?
Justified
Not Justified
Unsure
Certainly not justified. Given that I believe that the proposed form of regulation would endanger patients, no cost at all would be justified. But even if there were a marginal benefit, the cost would be quite unjustified. The number of practitioners involved is very large. It would involve a huge expansion of an existing quango, at a time when the government is trying to reduce the number of quangos. Furthermore, if the HPC were flooded with complaints about false health claims, as the GCC has been, the costs in legal fees could be enormous.
Q5: If herbal and TCM practitioners are subject to statutory regulation, should the right to prepare and commission unlicensed herbal medicines be restricted to statutorily regulated practitioners?
Yes
No
Unsure
I don’t think it would make much difference. The same (often false) ideas are shared by all HM people and that would continue to be the same with or without SR.
Q6: If herbal and TCM practitioners are not statutorily regulated, how (if at all) should unlicensed herbal medicines prepared or commissioned by these practitioners be regulated?
They could carry on as now, but the money that would have been spent on SR should instead be used to give the Office of Trading Standards and the MHRA the ability to exert closer scrutiny and to enforce more effectively laws that already exist. Present laws, if enforced, are quite enough to protect the public.
Q7: What would be the effect on public, practitioners and businesses if, in order to comply with the requirements of European medicines legislation, practitioners were unable to supply manufactured unlicensed herbal medicines commissioned from a third party?
Significant effect
Some effect
No effect
Unsure
European laws,especialliy in food area, are getting quite strict about the matters of efficacy. The proposed regulation, which ignores efficacy, could well be incompatible with European law, if not now, then soon. This would do no harm to legitimate business though it might affect adversely businesses which make false claims (and there are rather a lot of the latter).
Q8: How might the risk of harm to the public be reduced other than by orthodox statutory regulation? For example by voluntary self-regulation underpinned by consumer protection legislation and by greater public awareness, by accreditation of voluntary registration bodies, or by a statutory or voluntary licensing regime?
Voluntary self-regulation
Accreditation of voluntary bodies
Statutory or voluntary licensing
Unsure
I disagree with the premise, for reasons given in detail in separate documents. I believe that ‘orthodox statutory regulation’, if that means the Pittilo proposals, would increase, not decrease, the risk to the public. Strengthening the powers of Trading Standards, the MHRA and such consumer protection legislation would be far more effective in reducing risk to the public than the HPC could ever be. Greater public awareness of the weakness of the evidence for the efficacy of these treatments would obviously help too, but can’t do the job on its own.
Q10: What would you envisage would be the benefits to the public, to practitioners, and to businesses, for the alternatives to statutory regulation outlined at Question 8?
It depends on which alternative you are referring to. The major benefit of enforcement of existing laws by Trading Standards and/or the MHRA would be (a) to protect the public from risk, (b) to protect the public from health fraud and (c) almost certainly lower cost to the tax payer.
Q11: If you feel that not all three practitioner groups justify statutory regulation, which group(s) does/do not and please give your reasons why/why not?
Acupuncture
Herbal Medicine
TCM
Unsure
None of them. The differences are marginal. In the case of acupuncture there has been far more good research than for HM or TCM. But the result of that research is to show that in most cases the effects are likely to be no more than those expected of a rather theatrical placebo. Furthermore the extent to which acupuncture has a bigger effect than no-acupuncture in a NON-BLIND comparison, is usually too small and transient to offer any clinical advantage (so it doesn’t really matter whether the effect is placebo or not, it is too small to be useful).
In the case of HM, and even more of TCM, there is simply not enough research to give much idea of their usefulness, with a small handful of exceptions.
This leads to a conclusion that DH seems to have ignored in the past. It makes absolutely no sense to talk about “properly trained practitioners” without first deciding whether the treatments work or not. There can be no such thing as “proper training” in a discipline that offers no benefit over placebo. It is a major fault of the Pittilo recommendations that they (a) ignore this basic principle and (b) are very over-optimistic about the state of the evidence.
Q12: Would it be helpful to the public for these practitioners to be regulated in a way which differentiates them from the regulatory regime for mainstream professions publicly perceived as having an evidence base of clinical effectiveness? If so, why? If not, why not?
Yes
No
Unsure
It might indeed be useful if regulation pointed out the very thin evidence base for HM and TCM but it would look rather silly. The public would say how can it be that the DH is granting statutory regulation to things that don’t work?
Q13: Given the Government’s commitment to reducing the overall burden of unnecessary statutory regulation, can you suggest which areas of healthcare practice present sufficiently low risk so that they could be regulated in a different, less burdensome way or de-regulated, if a decision is made to statutorily regulate acupuncturists, herbalists and traditional Chinese medicine practitioners?
Yes
No
Unsure
As stated above, the.only form of regulation that is needed, and the only form that would protect the public, is through consumer protection regulations, most of which already exist (though they are enforced in a very inconsistent way). Most statutory regulation is objectionable, not on libertarian grounds, but because it doesn’t achieve the desired ends (and is expensive). In this case of folk medicine, like HM and TCM, the effect would be exactly the opposite of that desired as shown in separate documents that I have submitted to the consultation.
Q14: If there were to be statutory regulation, should the Health Professions Council (HPC) regulate all three professions? If not, which one(s) should the HPC not regulate?
Yes
No
Unsure
The HPC should regulate none of them. It has never before regulated any form of alternative medicine and it is ill-equipped to do so. Its statement that it doesn’t matter that there is very little evidence that the treatments work poses a danger to patients (as well as being contrary to its own rules).
Q15: If there were to be statutory regulation, should the Health Professions Council or the General Pharmaceutical Council/Pharmaceutical Society of Northern Ireland regulate herbal medicine and traditional Chinese medicine practitioners?
HPC
GPC/PSNI
Unsure
Neither. The GPC is unlikely to care about whether the treatments work any more than the RPSGB did, or the GCC does now. The problems would be exactly the same whichever body did it.
Q16: If neither, who should and why?
As I have said repeatedly, it should be left to Trading Standards, the MHRA and other consumer protection regulation.
Q17:
a) Should acupuncture be subject to a different form of regulation from that for herbalism and traditional Chinese medicine? If so, what?
Yes
No
Unsure
b) Can acupuncture be adequately regulated through local means, for example through Health and Safety legislation, Trading Standards legislation and Local Authority licensing?
Yes
No
Unsure
(a) No -all should be treated the same. Acupuncture is part of TCM
(b) Yes
Q18.
a) Should the titles acupuncturist, herbalist and [traditional] Chinese medicine practitioner be protected?
b) If your answer is no which ones do you consider should not be legally protected?
Yes
No
Unsure
No. It makes no sense to protect titles until such time as it has been shown that the practitioners can make a useful contribution to medicine (above placebo effect). That does not deny that placebos may be useful at times. but if that is all they are doing, the title should be ‘placebo practitioners’.
Q19: Should a new model of regulation be tested where it is the functions of acupuncture, herbal medicine and TCM that are protected, rather than the titles of acupuncturist, herbalist or Chinese medicine practitioner?
Yes
No
Unsure
No. This makes absolutely no sense when there is so little knowledge about what is meant by the ” functions of acupuncture, herbal medicine and TCM”.Insofar as they don’t work (better than placebo), there IS no function. Any attempt to define function when there is so little solid evidence (at least for HM and TCM) is doomed to failure.
Q20: If statutory professional self-regulation is progressed, with a model of protection of title, do you agree with the proposals for “grandparenting” set out in the Pittilo report?
Yes
No
Unsure
No. I believe the Pittilo report should be ignored entirely. The whole process needs to be thought out again in a more rational way.
Q22: Could practitioners demonstrate compliance with regulatory requirements and communicate effectively with regulators, the public and other healthcare professionals if they do not achieve the standard of English language competence normally required for UK registration? What additional costs would occur for both practitioners and regulatory authorities in this case?
Yes
No
Unsure
No. It is a serious problem, in TCM especially, that many High Street practitioners speak hardly any English at all. That adds severely to the already considerable risks. There would be no reliable way to convey what was expected of them. it would be absurd for the taxpayer to pay for them to learn English for the purposes of practising TCM (of course there might be the same case as for any other immigrant for teaching English on social grounds).
Q23: What would the impact be on the public, practitioners and businesses (financial and regulatory burden) if practitioners unable to achieve an English language IELTS score of 6.5 or above are unable to register in the UK?
Significant impact
Some impact
No impact
Unsure
The question is not relevant. The aim of regulation is to protect the public from risk (and it should be, but isn’t, an aim to protect them from health fraud). It is not the job of regulation to promote businesses
Q24: Are there any other matters you wish to draw to our attention?
I have submitted three documents via HRDListening@dh.gsi.gov.uk. The first of these puts the case against the form of regulation proposed by Pittilo, far more fluently than is possible in a questionnaire.
Another shows examples of what is actually taught in degrees in acupuncture, HM and TCM. They show very graphically the extent to which the Pittilo proposals would endanger the public, if they were to be implemented..
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
This post has been translated into Belorussian..
Chinese medicine and herbal medicine are in the news at the moment. There is a real risk that the government could endorse them by accepting the Pittilo report.
In my view traditional Chinese medicine endangers people. The proposed ‘regulation’ would do nothing to protect the public. Quite on the contrary, it would add to the dangers, by giving an official stamp of approval while doing nothing for safety.
The government’s idea of improving safety is to make sure that practitioners are ‘properly trained’. But it is the qualifications that cause the danger in the first place. The courses teach ideas that are plain wrong and often really dangerous.
Why have government (and some universities) not noticed this? That’s easy to see. Governments, quangos and university validation committees simply don’t look. They tick boxes but never ask what actually goes on. Here’s some examples of what goes on for them to think about. They show clearly the sort of dangerous rubbish that is taught on some of these ‘degrees’.
These particular slides are from the University of Westminster, but similar courses exist in only too many other places. Watch this space for more details on courses at Edinburgh Napier University, Middlesex University and the University of East London
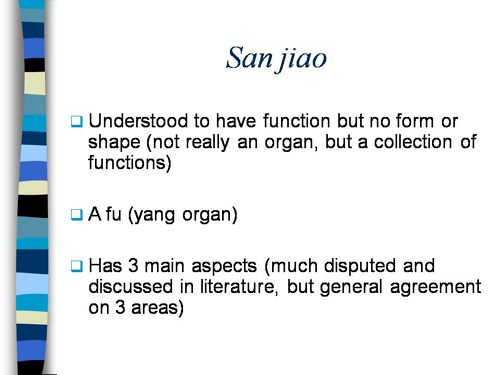
Just a lot of old myths. Sheer gobbledygook,
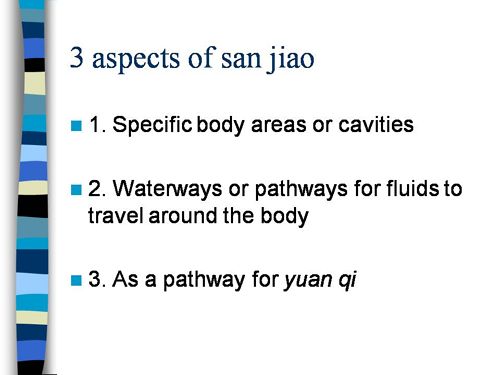
SO much for a couple of centuries of physiology,
It gets worse.
Plain wrong.
Curious indeed. The fantasy gobbledygook gets worse.
Now it is getting utterly silly. Teaching students that the brain is made of marrow is not just absurd, but desperately dangerous for anyone unlucky (or stupid) enough to go to such a person when they are ill.
Here’s another herbal lecture., and this time the topic is serious. Cancer.
Herbal approaches for patients with cancer.
I’ve removed the name of the teacher to spare her the acute embarrassment of having these dangerous fantasies revealed. The fact that she probably believes them is not a sufficient excuse for endangering the public. There is certainly no excuse for the university allowing this stuff to be taught as part of a BSc (Hons).
First get them scared with some bad statistics.
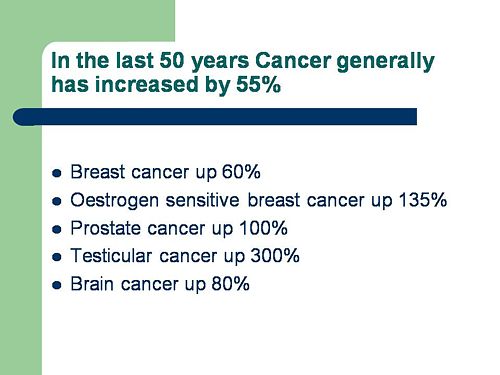
No fuss there about distinguishing incidence, age-standardisation and death rates. And no reference. Perhaps a reference to the simple explanation of statistics at Cancer Research UK might help? Perhaps this slide would have been better (from CDC). Seems there is some mistake in slide 2.
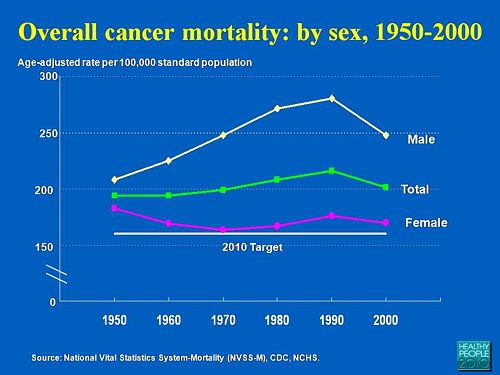
Straight on to a truly disgraceful statement in slide 3
The is outrageous and very possibly illegal under the Cancer Act (1939). It certainly poses a huge danger to patients. It is a direct incentive to make illegal, and untrue claims by using weasel words in an attempt to stay just on the right side of the law. But that, of course, is standard practice in alternative medicine,
Slide 11 is mostly meaningless. “Strengthen vitality” sounds good but means nothing. And “enhancing the immune system” is what alternative medicine folks always say when they can think of nothing else. Its meaning is ill-defined and there is no reason to think that any herbs do it.
The idea of a ‘tonic’ was actually quite common in real medicine in the 1950s. The term slowly vanished as it was realised that it was a figment of the imagination. In the fantasy world of alternative medicine, it lives on.
Detoxification, a marketing term not a medical one, has been extensively debunked quite recently. The use of the word by The Prince of Wales’ company, Duchy Originals recently fell foul of the Advertising Standards Authority, and his herbal ‘remedies’ were zapped by the MHRA (Medicines and Health Regulatory Authority).
And of course the antioxidant myth is a long-disproved hypothesis that has become a mere marketing term.
“Inhibits the recurrence of cancer”! That sounds terrific. But if it is so good why is it not even mentioned in the two main resources for information about herbs?
In the UK we have the National Library for Health Complementary and Alternative Medicine Specialist Library (NeLCAM), now a part of NHS Evidence. It was launched in 2006. The clinical lead was none other than Peter Fisher, clinical director of the Royal London Homeopathic Hospital, and the Queen’s homeopathic physician. The library was developed with the School of Integrated Health at the University of Westminster (where this particular slide was shown to undergraduates). Nobody could accuse these people of being hostile to magic medicine,
It seems odd, then, that NeLCAM does not seem to thnk to think that Centella asiatica, is even worth mentioning.
In the USA we have the National Center for Alternative and Complementary Medicine (NCCAM), an organisation that is so friendly to alternative medicine that it has spent a billion dollars on research in the area, though it has produced not a single good treatment for that vast expenditure. But NCCAM too does not even mention Centella asiatica in its herb list. It does get a mention in Cochrane reviews but only as a cosmetic cream and as an unproven treatment for poor venous circulation in the legs.
What on earth is a “lymph remedy”. Just another marketing term?
“especially valuable in the treatment of breast, throat and uterus cancer.“
That is a very dramatic claim. It as as though the hapless students were being tutored in doublespeak. What is meant by “especially valuable in the treatment of”? Clearly a desperate patient would interpret those words as meaning that there was at least a chance of a cure. That would be a wicked deception because there isn’t the slightest reason to think it works. Once again there this wondrous cure is not even mentioned in either NELCAM or NCCAM. Phytolacca is mentioned, as Pokeweed, in Wikipedia but no claims are mentioned even there. And it isn’t mentioned in Cochrane reviews either. The dramatic claims are utterly unfounded.
Ah the mistletoe story, again.
NHS Evidence (NeLCAM) lists three completed assessments. One concludes that more research is needed. Another concludes that “Rigorous trials of mistletoe extracts fail to demonstrate efficacy of this therapy”, and the third says “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
NCCAM says of mistletoe
- More than 30 human studies using mistletoe to treat cancer have been done since the early 1960s, but major weaknesses in many of these have raised doubts about their findings (see Question 6).
- Very few bad side effects have been reported from the use of mistletoe extract, though mistletoe plants and berries are poisonous to humans (see Question 7).
- The U.S. Food and Drug Administration (FDA) has not approved mistletoe as a treatment for cancer or any other medical condition (see Question 8).
- The FDA does not allow injectable mistletoe to be imported, sold, or used except for clinical research (see Question 8).
Cochrane reviews lists several reviews of mistletoe with similar conclusions. For example “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
Anthroposophy is one of the highest grades of fantasy you can find. A post on that topic is in the works.
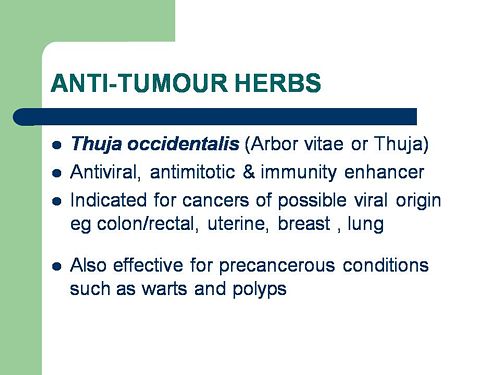
“Indicated for cancers . . . colon/rectal, uterine, breast, lung“. A cure for lung cancer? That, of course, depends on how you interpret the weasel words “indicated for”. Even Wikipedia makes no mention of any claims that Thuja benefits cancer. NHS Evidence (NeLCAM) doesn’t mention Thuja for any indication. Neither does NCCAM. Nor Cochrane reviews. That is not the impression the hapless students of this BSc lecture were given. In my view suggestions that you can cure lung cancer with this tree are just plain wicked.
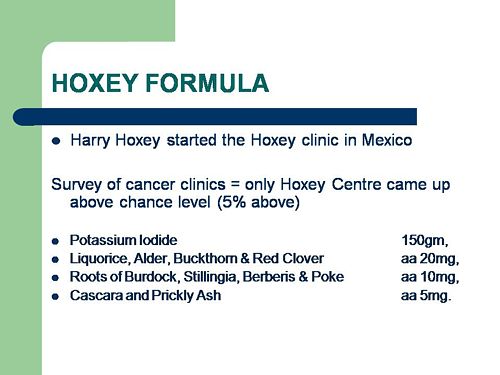
Pure snake oil, and not even spelled correctly, Harry Hoxsey’s treatment centres in the USA were closed by court order in the 1950s.
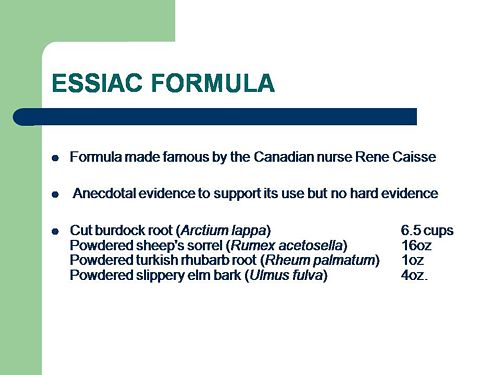
At least this time it is stated that there is no hard evidence to support this brand of snake oil.
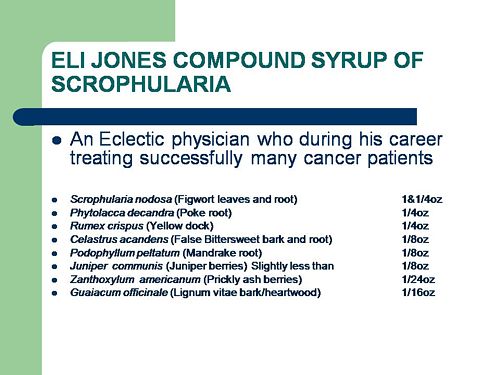
More unfounded claims when it says “treated successfully many cancer patients”. No references and no data to support the claim. It is utterly unfounded and claims to the contrary endanger the public.
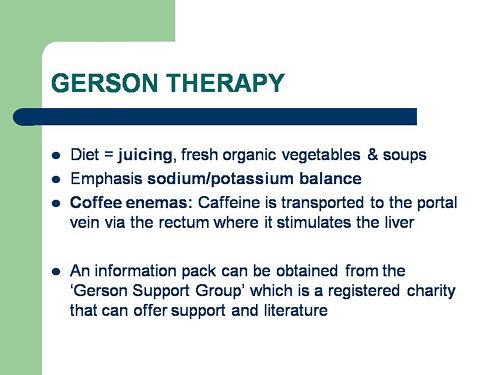
Gerson therapy is one of the most notorious and unpleasant of the quack cancer treatments. The Gerson Institute is on San Diego, but their clinics are in Mexico and Hungary. It is illegal in the USA. According to the American Cancer Society you get “a strict low-salt, low-fat, vegetarian diet and drinking juice from about twenty pounds of fresh fruits and vegetables each day. One glass of juice is consumed each hour, thirteen times a day. In addition, patients are given several coffee enemas each day. Various supplements, such as potassium, vitamin B12, pancreatic enzymes, thyroid hormone, and liver extracts, are used to stimulate organ function, particularly of the liver and thyroid.”. At one time you also got several glasses of raw calf liver every day but after infections killed several people] carrot juice was given instead.
Cancer Research UK says “there is no evidence to show that Gerson therapy works as a cure for cancer”, and “The Gerson diet can cause some very serious side effects.” Nobody (except perhaps the Price of Wales) has any belief in this unpleasant, toxic and expensive folk-lore.
Again patients are endangered by teaching this sort of stuff.
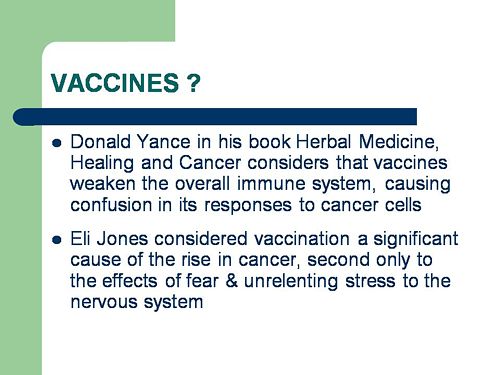
And finally, the usual swipe at vaccines. It’s nothing to do with herbalism. but just about every alternative medicine advocate seems to subscribe to the anti-vaccination lobby.. It is almost as though they have an active preference for things that are known to be wrong. They seem to believe that medicine and science are part of an enormous conspiracy to kill everyone.
Perhaps this dangerous propaganda might have been ameliorated if the students had been shown this slide (from a talk by Melinda Wharton).
Left to people like this, we would still have smallpox, diphtheria. tetanus and rabies, Take a look at Vaccine-preventable diseases.
This is the sort of ‘education’ which the Pittilo report wants to make compulsory.
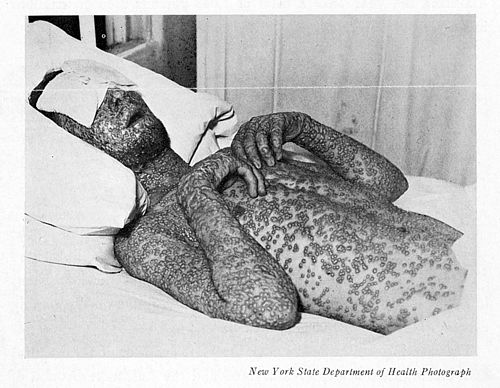
Smallpox in Baltimore, USA, 1939. This man was not vaccinated.
Conclusion
This selection of slides shows that much of the stuff taught in degrees in herbal medicine poses a real danger to public safety and to public health.
Pittilo’s idea that imposing this sort of miseducation will help safety is obviously and dangerously wrong. The Department of Health must reject the Pittilo recommendations on those grounds.
Follow-up
The much-delayed public consultation on the Pittilo report has just opened.
It is very important that as many people as possible respond to it. It’s easy to say that the consultation is sham. It will be if it is left only to acupuncturists and Chinese medicine people to respond to it. Please write to them before the closing date, November 2nd 2009. The way to send your evidence is here.
There is a questionnaire that you can complete, with the usual leading questions. Best do it anyway, but I’d suggest also sending written evidence as attachment too. I just got from DoH the email address where you can send it. They said
| if you have material you wish to send which you can’t easily “shoehorn” into the questionnaire, please send it to the following mailbox:
HRDListening@dh.gsi.gov.uk |
Here are three documents that I propose to submit in response to the consultation.I ‘d welcome criticisms that might make it more convincing. Use any parts of them you want in your own response.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
|
I’ve written quite a lot about the Pittilo report already, in particular A very bad report: gamma minus for the vice-chancellor, and in The Times (see also the blog version).
Intriguingly, these posts are at number 2 in a Google search for “Michael Pittilo”. |
 |
Briefly, the back story is this.
It is now over a year since the Report to Ministers from “The Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK” [download the report].
The chair of the steering group was Professor R. Michael Pittilo, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The reason thet the report is so disastrously bad in its assessment of evidence is that it was written entirely by people with vested interests.
The committee consisted of five acupuncturists, five herbalists and five representatives of traditional Chinese medicine (plus eleven observers). There was not a single scientist or statistician to help in the assessment of evidence. And it shows: The assessment of the evidence in the report was execrable. Every one of the committee members would have found themselves out of work if they had come to any conclusion other than that their treatment works, Disgracefully, these interests were not declared in the report, though they are not hard to find. The university of which the chair is vice-chancellor runs a course in homeopathy, the most discredited of the popular forms of alternative medicine. That tells you all you need to know about the critical faculties of Michael Pittilo.
The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register normally be through a Bachelor degree with Honours
Let’s consider the virtue of these two recommendations.
Regulation by the Health Professions Council (HPC) breaks their own rules
For a start, this should be ruled out by the HPC’s own rules, which require “Practise based on evidence of efficacy” as a condition for registration. Since there is practically no “evidence of efficacy”, it follows that the HPC can’t regulate acupuncture, herbal and Chinese medicine as Pittilo recommends. Or so you’d think. But the official mind seems to have an infinite capacity for doublespeak. The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
In other words, the HPC simply decided to ignore its own rules, Its excuse for doing so is that regulation would protect “public safety” . But it simply would not do that. It is ell known that some Chinese herbs are adulterated with dangerous substances, but laws against that already exist. Trading Standards are much more likely to take appropriate action than the HPC. The Medicines and Health Regulatory Authority (MHRA) already deals with the licensing of herbal medicines. and, despite the fact that it recently betrayed its trust by allowing them to be labelled in a misleading way, they are the people to do it, not the HPC.
The Pittilo report (page 11) says
In future, it is hoped that more Government funding can be allocated to research into traditional/herbal medicines and acupuncture and that grants will become available to encourage practitioners to undertake postgraduate research work.
So they are asking for more government money.
In March 2007, the Chinese Government pledged to spend over $130 million over the next five years on research into the effectiveness of traditional Chinese medicine. It is to be hoped that this money will be targeted effectively to evaluate TCM.
It seems to have escaped the notice of Pittilo that roughly 100 percent of trials of Chinese medicine done in China come out positive. Elsewhere, very few come out positive,(see Vickers et al., 1998, Controlled Clinical Trials, 19, 159-166: download reprint) The Department of Health would be unwise to rely on Chinese research. Remember that modern acupuncture was not so much a product of ancient wisdom, but rather it stems from nationalist propaganda by Mao Tse-Tung, who needed a cheap way to keep the peasants quiet, though he was too sensible to use it himself.
The HPC report (page 5) cites these with the words
” . . . a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base.”
This sentence seems to assume that the outcomes of research will be to strengthen the evidence base. Thus far, precisely the opposite has been the case. The Pittilo group has apparently not noticed that the US National Institutes of Health has already spent a billion dollars on research in alternative medicine and failed to come up with a single effective treatment. There are better ways to spend money on health. See, for example $2.5B Spent, No Alternative Med Cures found. .An enornous amount of research has already been done and the outcomes have produced no good treatments,
The proposed regulation would endanger the public, not protect it.
The excuse given by the HPC for breaking its own rules is that it should do so to protect the public.
Likewise Ann Keen, Health Minister, said:
“Patient safety is paramount, whether people are accessing orthodox health service treatments or using alternative treatments”
So first we need to identify what dangers are posed by acupuncture, herbal medicine and traditional Chinese medicine.
- Acupuncture is fairly safe. Its biggest danger lies in the unjustified claims that are routinely made for what can be achieved by being impaled by needles. This poses a danger that people may use acupuncture in place of treatments that work
- Herbal medicines are unstandardised, so even the very few that may work are dangerous to patients because the dose of active principle is unknown and varies from one batch to another. Taking a herbal medicine is a bit like swallowing a random number of tablets, False health claims pose a danger to patients too, when they cause patients to avoid treatments that work.
- Traditional Chinese Medicine is probably the most dangerous. Like the other two, the medicines are unstandardised so the dose is never known. False health claims abound. And in addition to these dangers, many cases have been found of Chinese medicines being adulterated with poisonous substances or with conventional drugs.
The form of regulation proposed by Pittilo would do little or nothing to protect the public from any of these dangers.
The proposals accept the herbal and Chinese medicine as traditionally practised. Nothing would be done about one of the major dangers, the lack of standardisation. That is a problem that was solved by pharmacologists in the 1930s, when international standards were set for the biological activity of things like tincture of digitalis, and assays were devised so that different batches could be adjusted to the same potency. Now, 80 years later, it is being proposed by Pittilo that we should return to the standards of safety that existed at the beginning of the last century. That is a threat to public safety., but the proposed regulation would do nothing whatsoever to protect the public from this dangerous practice. On the contrary, it would give official government sanction to it.
The other major danger is that patients are deceived by false health claims. This is dangerous (as well as dishonest) because it can cause patients to avoid treatments that work better, The internet abounds with claims that herbs can cure anything from diabetes to cancer. Many are doubtless illegal, but regulators like the HPC have traditionally ignored such claims: they are left to Trading Standards, Advertising Standards and the Medicines and Health Regulatory Authority (MHRA) to deal with. The MHRA already also has responsibility for monitoring side effects. The HPC would not do this.
The analogy with chiropractic and the GCC
The foolishness of allowing statutory regulation for unproven treatments has recently been illustrated quite dramatically by the case of chiropractic. Chiropractors have had statutory regulation by the General Chiropractic Council, which was established by the Chiropractors Act of 1994. The British Chiropractic Association (BCA) recently decided to sue the science writer, Simon Singh, for defamation when he cast doubt on some of the claims made by chiropractors, in particular their claims to be able to cure colic and asthma in children. That led to close examination of the claims. In fact there is no reason to think that spinal manipulation works for asthma, or that it works for colic. In fact there is quite good evidence that the claims are false. The result was that about 600 well-justified complaints have been lodged with the GCC (enough to bankrupt the GCC if the complaints are dealt with properly).
The point of this story is that the statutory regulator had nothing whatsoever to prevent these false health claims being made. Two of the complaints concern practices run by the chair of the GCC. Worse, the GCC actually endorsed such claims. The statutory regulator saw its duty to defend chiropractic (apart from a handful of cases of sexual misdemeanours), not to protect the patient from false health claims. The respectability conferred by statutory regulation made false health claims easier and endangered the public. It would be a disaster if the same mistake were made again.
On 11th December 2008 I got a letter form the HPC which said
in our opinion a lack of evidence of efficacy would not impede our ability to set standards or deal with complaints we receive. The vast majority of cases we consider are related to conduct.
But perhaps that is because they haven’t tried “regulating” quacks before. Now that the public is far more conscious about health fraud than it used to be, one can predict confidently that the HPC would be similarly overwhelmed by a deluge of complaints about the unjustified health claims made by acupuncturists, herbal medicine and traditional Chinese medicine practitioners. There is no shortage of them to complain about.
The education problem
The Pittilo report recommends that the entry level for registration should be a bachelors degree with honours. At first sight it seems reasonable to ask that practitioners should be ‘properly qualified’, but when one looks at what is actually taught on these degrees it becomes clear that they endanger, rather than protect, the public,
There are two very big problems with this recommendation.
Firstly, you can’t have a bachelors degree with honours until after you have decided whether or not there is anything useful to teach. If and when any of the subjects under consideration and shown to work to a useful extent, then it would be quite reasonable to establish degrees in them. Even the report does not pretend seriously that that stage has been reached. The proposal to set up degrees in subjects, at least some of which are quite likely to have no more than placebo value, is self-evidently nonsense,
The time for degrees, and the time for government endorsement by statutory regulation, is after the therapies have been shown to work, not before.
The absurdity of thinking that the public will be protected because a practitioner has a degree in, say, acupuncture, is shown with startling clarity by a recently revealed examination paper in acupuncture’
You can download the entire exam paper. Here are a few highlights from it.
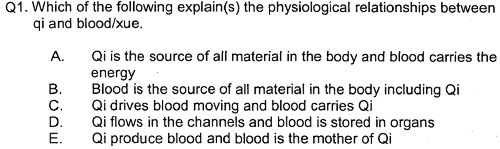
So students, in 2009, are being taught the crudest form of vitalism.
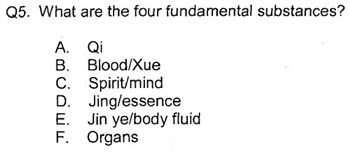
Teaching of traditional Chinese medicine is just as bad. Here are two slides from a course run by the University of Westminster.
The first ‘explains’ the mysterious and entirly mythical “Qi”.
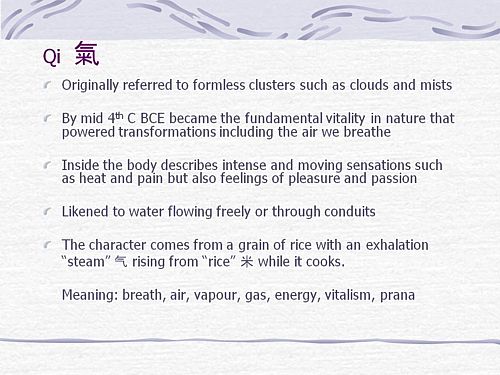
So “Qi” means breath, air, vapour, gas, energy, vitalism. This is meaningless nonsense.
The second slide shows the real dangers posed by the way Chinese medicine is taught, The symptoms listed at the top could easily be a clue to serious illness, yat students are taught to treat them with ginger. Degrees like this endanger the public.
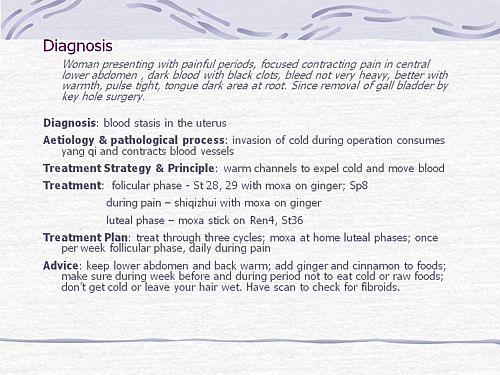
There are more mind-boggling slides from lectures on Chinese medicine and cancer: they show that what students are being taught is terrifyingly dangerous to patients.
It is entirely unacceptable that students are being taught these ancient myths as though they were true, and being encouraged to treat sick people on their basis. The effect of the Pittilo recommendations would be to force new generations of students to have this sort of thing forced on them. In fact the course for which this exam was set has already closed its doors. That is the right thing to do.
Here’s another example. The course leader for “BSc (Hons) Herbal Medicine” at the Univsrsity of Central Lancashire is Graeme Tobyn BA. But Tobyn is not only a herbalist but also an astrologer. In an interview he said
“At the end I asked her if I could cast her horoscope. She threw up her hands and said, ‘I knew this would happen if I came to an alternative practitioner.”
“I think the ruler of the ascendant was applying to Uranus in the ninth house, which was very pertinent.”
This would be preposterous even in the life style section of a downmarket women’s magazine, The Pittilo report wants to make degrees run my people like this compulsory. Luckily the Univerity of Central Lancashire is much more sensible and the course is being closed.
The matter is, in any case, being taken out of the hands of the government by the fact that universities are closing degrees in complementary medicine, including courses in some of those under discussion here, The University of Salford and the University of Central Lancashire have recently announced the closure of all the degree programmes in complementary and alternative medicine. The largest provider of such degrees, the University of Westminster has already shut down two of them, and the rest are being assessed at the moment. It is likely that the rest will be closed in the future.
The revelation that Westminster had been teaching its first year students that “amethysts emit high yin energy” and that students had been taught to diagnose disease and choose treatments by means of a dowsing pendulum, showed very clearly the sort of utter nonsense that undergraduates were being forced to learn to get a ‘bachelors degree with honours’. It stretches credulity to its limits to imagine that the public is protected by degrees like this. Precisely the opposite is true. The universities have recognised this, and shut the degrees. One exception is Professor Pittilo’s own university which continues to run a course in homeopathy, the most discredited of all the popular types alternative medicine.
A simpler, more effective and cheaper way to protect the public
I must certainly agree with the minister that protection of the public is an important matter. Having established that the Pittllo recommendations are more likely to endanger the public than protect them, it is essential to suggest alternative proposals that would work better.
Luckily, that is easy, because mechanisms already exist for dealing with the dangers that were listed above. The matter of adulteration, which is serious in traditional Chinese medicine, is a matter that is already the responsibility of the Office of Trading Standards. The major problem of false claims being made for treatment is also the responsibility of the Office of Trading Standards, which has a statutory duty to enforce the Unfair Trading Consumer Protection Regulations of May 2008. These laws state, for example, that
“One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”
The monitoring of false claims, and of side effects of treatments, is also the responsibility of the Medicines and Health Regulatory Authority (MHRA).
Rather than setting up complicated, expensive and ineffective ‘regulation’ by the HPC, all that need to be done is to ensure that the MHRA and/or Trading Standards have the funds to enforce existing laws. At the moment, they are not being implemented effectively, so I’d recommend that responsibility for enforcing the law against false health claims be transferred entirely to the MHRA, which has much more expertise in such matters than Trading Standards This would be both cheaper and more effective than the present system in which the responsibility is divided between the two organisations in an unclear way.
This proposal would protect the public against unsafe and adulterated treatments, and it would protect the public against false and fraudulent claims. That is what matters. It would do so more effectively,
more cheaply and more honestly than the Pittilo recommendations. There would be no reduction in patient choice either, There is no proposal to ban acupuncture, herbal medicine or traditional Chinese medicine. All that is necessary is to ensure that they don’t endanger the public.
Since the root of the problem lies in the fact that the evidence for the effectiveness is very weak. the question of efficacy, and cost-benefit ratio, should be referred to NICE. This was recommended by the House of Lords Report (2000). It is recommended again by the Smallwood report (sponsored by the Prince of Wales Foundation). It is baffling that this has not been done already. It does not seem wise to spend large amounts of money on new research at the moment, in the light of the fact that the US National Institutes of Health has already spent over $1 billion on such research without finding a single useful treatment.
The results of all this research has been to show that hardly any alternative treatment are effective. That cannot be ignored.
Conclusion
Recent events show that the halcyon days for alternative medicine are over. When the Pittilo report first appeared, it was greeted with derision in the media. For example, in The Times Alice Miles wrote
“This week came the publication of the Report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK. Otherwise known as twaddle.”
In the Independent, Dominic Lawson wrote
So now we will have degrees in quackery.
What, really, is the difference between acupuncture and psychic surgery?
People will no doubt continue to use it and that is their right and their responsibility. But if the government were to accept the recommendations of the Pittilo report it would be seen, quite rightly, as being anti-scientific and of posing a danger to the public.
Fortunately there is a better, and cheaper, way to protect the public.
Follow-up
Margaret McCartney’s blog in the Financial Times puts rhw view of a GP with her usual sense, humour and incisiveness.
“This report would, if implemented, create lots more nonsense exam papers funded by a lot more public money – and would produce practitioners without the absolutely crucial skill of how to assess evidence and reject or use it appropriately”
The Times has covered the story (with some interesting comments) Consultation on how to regulate complementary and alternative therapies
Times Higher Education UK-wide consultation on CAM regulation is launched Excellent response from Andy Lewis.
The Sun has by far the best coverage up to now, Jane Symons writes “Regulating quacks helps them prey on gullible patients“
Acupuncture has been in the news since, in a moment of madness, NICE gave it some credence,
Some people still seem to think that acupuncture is somehow more respectable than, say, homeopathy and crystal healing. If you think that, read Barker Bausell’s book ot Trick or Treatment. It is now absolutely clear that ‘real’ acupuncture is indistinguishable from sham, whether the sham control uses retractable needles, or real needles in the ‘wrong’ places. There has been no clear demonstration of long-lived benefits in any condition, and it is likely that it is no more than a theatrical placebo.
In particular, the indistinguishability of ‘real’ and sham acupuncture shows, beyond reasonable doubt that all the stuff about “energy flow in meridians” is so much hokum.
There is a small group of ‘medical acupuncturists‘ that believes that it is hokum. but who nonetheless maintain that acupuncture works, despite the evidence to the contrary. But most acupuncturists go for the wholesale gobbledygook.
If you don’t believe that, take a look at the exam paper that has come into my possession. It is this year’s exam from the University of Salford. Salford has, very sensibly, now decided to stop all its degrees in alternative medicine, so don’t hold this against the university too much.
You can download the entire exam paper. Here are a few highlights.
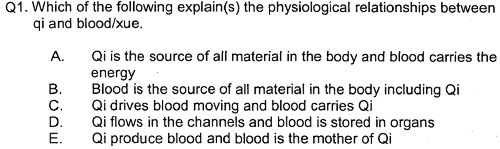
So students, in 2009, are being taught the crudest form of vitalism.
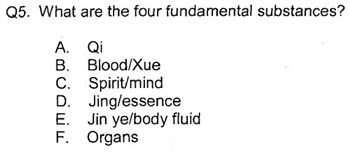
Oh really. Perhaps protons neutrons and electrons?
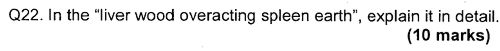
OK I’d fail that one because the words have no obvious meaning at all.
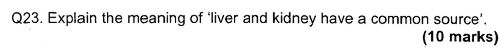
Perhaps an elementary textbook of embryology would help?
How one would love to see a set of model answers for these questions.
All this is ancient hokum being taugh to hapless students in the 21st century as though it were fact. The University of Salford has understood that and closed the course. All we need now is for NICE and the Department of Health to understand what it is that they are promoting.
NICE neglected the cultural cost of their guidance
When National Institute for Health and Clinical Excellence (NICE) included an acupuncture option on their low back pain guidance, they quite forget that one effect of their decision would be to ensure that new generations of students would have their minds poisoned with intellectual junk like this. That is why NICE really must think again. . See also
NICE falls for bait and switch by acupuncturists and chiropractors
NICE fiasco part 2 Rawlins should withdraw guidance and start again
NICE fiasco Part 3. Too many vested interests, not enough honesty
Pittilo and statutory regulation
Public consultation is due to open shortly on the appalling report of the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK (see also, The Times)
One of the recommendations is that acupuncture and Chinese herbal medicine should have statutory regulation by the Health Professions Council (HPC), despite the fact that that would involve the HPC breaking its own rules. Another recommendation of Pittilo is that entry to the “profession” (his word, not mine) should be by means of honours degree only. So he wants to impose on students exams like this one in order to “protect the public”? The absurdity of that proposal should be obvious now. This exam paper will form part of my evidence to the consultation.
And there is one other small problem. Universities are busy shutting down their degrees in alternative medicine, now that the ridiculousness of what is taught has been exposed. They have shut down entirely at the University of Salford and at the University of Central Lancashire, And even the University of Westminster is working on closing them.
All we need now is for the common sense and integrity that has been shown by these universities to spread to the Department of Health (and NICE).
Follow-up
|
.The University of Central Lancashire (UCLAN) is the first place I asked to see teaching materials that were used on its homeopathy “BSc” course. The request was refused, and subsequent internal appeals were refused too, Clearly UCLAN had something to hide. |

|
An appeal to the information commissioner took almost two years to be judged, but the case was won. The eventual decision by the Information
Commissioner rejected all the grounds that UClan had used to evade the Freedom of Information Act.
UClan appealed against the judgement and I still haven’t got the stuff but that hardly matters now, because the course in question shut its doors. In any case, plenty of stuff from similar courses has leaked out already.
Meanwhile, in September 2008, UCLAN announced an internal review of all its courses in magic medicine, The review seemed to be genuine. For a start they asked me to give evidence to the review (something that no other university has done). They also asked Michael Eslea to give evidence. He is the UCLAN psychologist, whose magnificent open letter probably tipped the authorities into holding the review.
Just in case it is useful to anyone, here is a copy of the written evidence that I sent [download pdf],
|
Report of the Working Party on the Review of issues associated with Homeopathy, Acupuncture and Chinese Herbal Medicine
1. Introduction As a consequence of concerns expressed by some colleagues within the University of Central Lancashire (UCLan) Dr Malcolm McVicar, Vice Chancellor appointed a working party to review the issues associated with the University offering courses in Homeopathy, Acupuncture and Chinese Herbal Medicine. MEMBERSHIP: Eileen Martin (Chair) Pro-Vice Chancellor and Dean of Faculty of Health and Social Care |
The report was the subject of a special meeting of UCLAN’s Academic Board on 9th July 2009. The following resolutions were passed.
|
Resolutions R1 That further minor revisions be made to the report prior to publication on the University’s website; R2 That the University refrain from offering any practitioner-qualifying courses in Homeopathy, Acupuncture and Chinese Herbal Medicine until such disciplines have achieved statutory regulation status; R3 That the University consider offering a limited number of postgraduate research studentships (leading to Masters by Research of PhD) to suitably qualified UCLan students and staff in these disciplines. They should have interdisciplinary supervisory teams to facilitate development of a broad range of research skills and to contribute to the generation of knowledge in CAM; R4 That the University consider how more interdisciplinary teaching can be achieved, where appropriate, within both undergraduate and postgraduate teaching to facilitate greater exposure to subject expertise and different paradigms. |
Resolutions 1, 3 and 4 say very little. Resolution 4 sounds thoroughly relativist. We are talking about medicine, about treating sick patients. There is only one “paradigm”. That is to find treatments that are as effective and safe as possible. There aren’t two sorts of medicine, regular and alternative. There is just medicine that works and medicine that doesn’t work. It’s a good illustration of DC’s rule number 2, “never trust anyone who uses the word paradigm”.
Resolution 2 is the really interesting one, because none if the topics, Homeopathy, Acupuncture and Chinese Herbal Medicine, is subject to statutory regulation.
If taken literally, resolution 2 means that all the UCLan courses in alternative medicine will close their doors. Bafflingly, this inevitable conclusion is not stated explicitly.
At least resolution 2 means that homeopathy, already closed, will stay closed. It is never likely to get statutory regulation.
For practical purposes, we can ignore for the moment the obvious fact that statutory regulation of nonsense subjects results only in nonsense. The only forms of alternative medicine that have got “statutory regulation” at the moment are chiropractic and osteopathy. The public has not been safeguarded by the General Chiropractic Council (GCC). The GCC, on the contrary, has endangered the public by allowing false health claims to be made with impunity. Perhaps the members of the review committee had not noticed that the Simon SIngh affair has resulted in almost 600 complaints being made to the GCC? The faith of the review in statutory regulation is clearly misplaced.
The Pittilo report is critical for what happens next
Acupuncture and Chinese Herbal Medicine are not subject to statutory regulation at present, so one would suppose that these degrees will close their doors too. However the infamous Pittilo report has proposed that they should become regulated by the Health Professions Council (HPC). The many problems of the Pittilo report have been documented here, in “A very bad report: gamma minus for the vice-chancellor“. There was also a high-profile critique of the report in The Times (and on this blog).
The HPC has, as one of its criteria for regulation, “evidence-based practice”. Disgracefully, the HPC has already shown its willingness to ignore its own rules and to act as statutory regulator for Acupuncture and Chinese Herbal medicine. This rather disgraceful behaviour is documented in “Health Professions Council ignores its own rules: the result is nonsense“.
The UCLAN report seems to assume that the recommendations of the Pittilo report will be accepted. But the long-awaited consultation has still not opened. We can be sure that when it does, the opposition to it will be very strong indeed.
The report in full
Here are a few comments on the report itself. Download the full report (as of July 15th).
i have to say that when I visited Preston to give evidence, my views seem to be treated seriously, even sympathetically, so it was a great disappointment to see the outcome. So what’s wrong? The major disaster is declared early in the report.
Section 2, Context
The debate is centred on a number of key themes which relate to:-
1. The quality of and/or absence of an evidence base to support claims of the efficacy and benefits of such treatments, linked to issues of public safety/protection and professional regulation.
Sounds good. What matters about any sort of medicine is whether or not it works and whether it is safe. It therefore verges on the incredible that we read in section 4.1
“conclusions from research into the efficacy of the various CAM’s are outside the remit of this report.”
The whole point about CAM is that there is very little evidence that any of it works. So the review committee decided to ignore the most important problem of the lot. I can’t see how any rational decision can be made without first deciding whether the treatment is better than placebo. That, surely, is the main question, and it was dodged.
UCLAN has failed to grasp the nettle, just as the Department of Health has also consistently failed to do so.
Section 4,1 Efficacy This section repeats the assertion, absurd to my mind, that it is possible to judge CAM courses while declining to assess whether they work or not.
Section 4.2 Role of Universities in Society.
There is universal agreement that critical thinking is crucial to the idea of a university, but the judgement of whether CAM teaches critical thinking is simply fudged. Again the report fails to grasp the nettle.
“Disagreements about critical thinking within CAMs arises because some will argue that such substantiation and assessment can occur within the discipline, whilst others will argue that the methodology for substantiation, that is evidence provision, is universal. As a result, the latter will demand that evidence is provided using methods from one field (e.g. randomised controlled trials) for use in another.”
Sadly, the report dodged the crucial judgement once again. The most obvious characteristic of every form of alternative medicine is their total lack of critical self-appraisal. It is very sad that the review committee could not bring itself to say so.
Section 4.4 Nomenclature of degrees
Recommendation
The nomenclature of courses, leading to a professional as well as an academic award, should reflect the professional route; for example Bachelor with Honours in Complementary Medicine, B Comp. Med.(Hons) or B Acupuncture (Hons).
This sounds to me like another truly pathetic fudge. What on earth is solved by changing the name of the degree? You’d still be teaching students the same load of gobbledygook and then letting them loose on sick people, whether you call it a Bachelor of Science, a Bachelor of Arts, or, as is recommended here, a Bachelor of nothing whatsoever.
Well, I suppose there is a (doubtless unintended) irony in calling CAM degrees “Bachelor of nothing whatsoever”.
Section 4.4 Ethical, non-harm and economic considerations
This section list a lot of reasons why teaching alternative medicine should be unethical. but nevertheless manages to conclude that
” . . . it is not unethical to offer courses in Homeopathy, Acupuncture and Chinese Herbal Medicine at a university.”
I find the logic by which this bizarre conclusion was reached quite impossible to follow. Like much of the rest of the report this conclusion seems to stem from a reluctance to grapple with the really important questions, like ‘does it work or not?’.
Despite this the recommendation is perhaps the most interesting of all.
“Recommendation
• The University refrains from offering any CAM courses until such disciplines have achieved statutory regulation status.”
This recommendation was accepted, and passed as a resolution at Academic Board. If it is implemented now, than there will be no more alternative medicine degrees next year at the University of Central Lancashire. If and when this happens, the University must be congratulated on its return to rational medicine.
Follow-up
Michael Eslea, UCLAN’s hero in resisting nonsense from the inside, has posted on this topic.
17 July 2009. It seemed odd that that no announcement was made about the future if the remaining CAM courses at UCLAN. So I asked deputy Vice-Chancellor Patrick McGhee for clarification. After a couple of days, I got this response.
|
From: CTheobald@uclan.ac.uk To: d.colquhoun@ucl.ac.uk Hi David, I have been asked to respond to your question below on the running of acupuncture and Chinese herbal medicine at UCLan. It is correct to assume that UCLan will not be taking any new entrants onto these programmes until further notice. Best Wishes Chris Chris Theobald |
So the report may have been disappointing, but it has done the job. As several people have pointed out in comments, it would be asking too much to expect a university to say “sorry we just noticed that we have been running junk-science courses for years”. But they have done the right thing anyway.