herbal medicine
|
The Science Museum is a wonderful place. As a child it seemed magical. So all the more disappointing to find that it houses an exhibition that promotes quackery. The exhibition is uncritical and sometimes downright dangerous. It does not teach you anything about science, it teaches anti-science and uncritical thinking. It was not originally like this. Most of the objects in the exhibition were originally part of Henry Wellcome’s Wellcome Museum of Medical History, based at 183 Euston Road. It was moved on permanent loan to the Science Museum in 1977 where it was known as The Wellcome Museum of the History of Medicine. |
|
Recently the Wellcome-Trust sponsored exhibition was the subject of a blog post at Purely a figment of your imagination, written by Alex Davenport. That reminded me that last June I was sent a lot of pictures of the exhibition but never got round to finishing writing them up. Here, somewhat tardily, is some of what I got.
It seems that the Wellcome Trust is not to blame, The free advertising for quacks was something added to the Wellcome collection by the Science Museum itself.
At the time, I wrote to the Science Museum to find out what was going on. The response was very disappointing, merely bland PR stuff. I was told that the person responsible for the display was Lisa O’Sullivan, Senior Curator of Medicine, but she was on sabbatical, so no response from her.
The clue to what went wrong came in a letter from Dr. Tim Boon, the Science Museum’s Chief Curator. The letter was relayed via the Museum’s Press Officer. A subsequent letter to Boon himself was not answered.
"Therefore, in addition to the overwhelming majority of the Upper Wellcome gallery that tells the story of the history of Western medicine since the rise of Civilisation up to the modern era, we devote a small section to these more anthropological concerns in our display called ‘Living Medical Traditions’.
Our message in this display is that these traditions are not ‘alternative’ systems in some parts of the world. Instead they are often the only choice of medical care to those communities. We do not make any claims for the validity of these traditions. For example, we include the use of acupuncture but do not say that acupuncture ‘works’. "
Unfortunately this is really not true: the tone is very much that it does work. The reason is clear in the next paragraph.
"As with all Science Museum galleries independent experts were consulted when developing this gallery. In this instance advice was sought from leading academics in the history of non-western medical traditions as well as practitioners and users of these traditions. We maintained editorial control throughout.”
Aha they asked "experts", but of course it is always possible to find some ‘expert’ to advocate any view, however barmy. The only experts that were consulted, we are told, is historians and practitioners of anti-scientific medicine. No scientists. Clearly the Museum allowed the quacks to write their own script, with no supervision from anyone who understands the science, It is meant to be a Science Museum, not a museum of anthropology.
The nonsense of quack medicine provides an excellent opportunity to explain simply how science tries to separate truth from falsehood. The Museum has not only missed that opportunity but it has actively promoted anti-science.
The Museum declined to name these mystery experts, but one of them is revealed in the 2006 newsletter of the British Medical Acupuncture Society [download the newsletter]. An article by Jonathan Freedman shows the delight of acupuncturists.
"The BMAS were approached by the Museum last Summer and asked if any members would be able to contribute a case study about acupuncture to feature in the ‘personal stories’ section of the exhibition."
"I think the final product has worked extremely well and shows Western Medical Acupuncture in a positive light. A selection of needles is displayed along with the BMAS leaflet and my own practice acupuncture leaflet."
In fact the Science Museum’s good name is used by Freedman to advertise his private practice.
Here is the free advertising in the Science Museum.
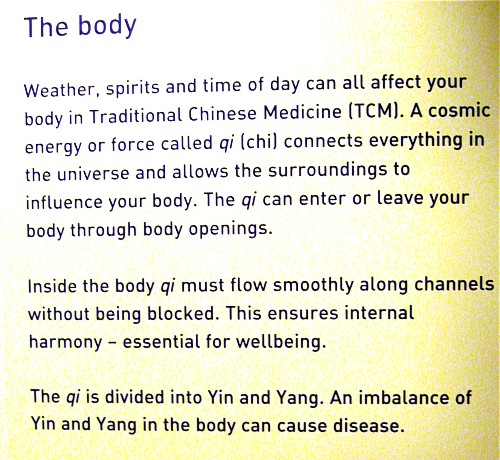
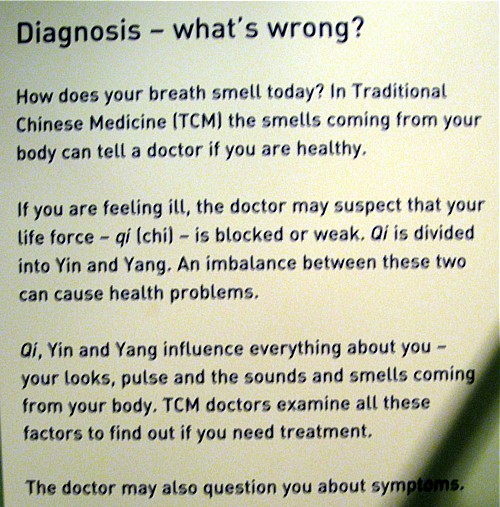
Traditional Chinese Medicine
There is plenty of this and it is totally uncritical. All it does is repeat the gobbledygook used by practitioners. In fact it was largely written by them.
There are recorded commercials too. Listen to this one.
Advertising for cupping at the Asanté Clinic.
In the recording, Dr Ke diagnoses an asthma patient as having mucus in the lungs -by looking at his tongue (no kidding) -and recommends cupping. He says
“We need to clear this mucus, or the phlegm, in the chest by using cupping, It’s improving, sort of, the flow of the water, and flow out, in other words, suck out the badness from the body”
This, needless to say, is total rubbish.
The recording took place at the Asanté Clinic, on the Archway campus of the University of Middlesex. Ah yes, Middlesex. Take a look at ‘More quackedemia. Dangerous Chinese medicine taught at Middlesex University‘.
Unani medicine, Another advertisement for a private clinic.
|
|
|
Listen to a diagnosis being made by looking at the iris.
Iridology is, of course, total bunk Just one of the many phoney methods of diagnosis used by alternative practitioners, as an aid to selling you an expensive treatment.
Ayervedic medicine
Listen to another advertisement, for private Ayurveda clinic
The display that accompanies the recording is totally uninformative. The practitioners have been allowed to advertise their wares with no trace of critical thought. No trace of science.
|
|
|
|
|
|
|
|
|
The power of blogs
I guess this incident is yet another example of the power of blogs. My own letters to the science museum produced precisely nothing, as is usually the case if you go through the “proper channels”. Alex Davenport’s blog,on the other hand, stung the Science Museum into a public response. It’s true that the response is much the same as the patronising PR junk that was sent to me last year, though it was labelled as being by Susannah Shute, Web Content Coordinator. The response even linked to a picture of the homeopathy exhibit.
It seems a bit more pressure is needed to persuade the museum to change this particular exhibition into science, rather than its present anti-science.
Follow-up
13 April 2011. Simon Singh arranged a meeting with the new director of the Science Museum, Ian Blatchford, and deputy director Heather Mayfield Our deputation consisted of Simon Singh, Alex Davenport, Marianne Baker and me. It was Alex’s blog on the science museum exhibit, and my post on the museum which followed it shortly, that caused the meeting. Alex had a follow-up blog too. I hadn’t realised that Simon had resigned as a trustee of the museum five years ago, in protest about the (dreadful) alternative medicine exhibit. I had various stonewalling responses to my attempts to pursue the matter out of the limelight, so eventually went public. After the blogs appeared, the Science Museum published a response which was, sadly, entirely vacuous. We had an excellent discussion, during which Ian Blatchford said he regretted the official response and changes to the exhibit are promised. there is an account of the meeting here.
We were sent a revised version, which was improved, but not, we said improved enough.
10 May 2011. Got an email from the person who originally brought the problem to my attention.
“Visited Science museum yesterday , wonderful news – all offensive material gone, and different ok stuff there”.
Well done, Science Museum.
The Prince of Wales’ Foundation for Integrated Health shut down amidst scandal in April 2010. In July, we heard that a new “College of Medicine” was to arise from its ashes. It seemed clear from the people involved that the name “College of Medicine” would be deceptive.
Now the College of Medicine has materialised, and it is clear that one’s worst fears were well justified.

At first sight, it looks entirely plausible and well-meaning. Below the logo one reads
“There is a new force in medicine. A force that brings patients, doctors, nurses and other health professionals together, instead of separating them into tribes.”
"That force is the new College of Medicine. Uniquely, it brings doctors and other health professionals together with patients and scientists.”
It is apparent from the outset that the well-meaning words fall into the trap described so clearly by James May (see What ‘holistic’ really means). It fails to distinguish between curing and caring.
As always, the clue lies not in the words, but in the people who are running it.
Who is involved?
After a bit of digging on the web site, you find the names of the people on the Science Council of the “College of Medicine”, The preamble says
“Good medicine must be grounded in good science as well as compassion. The College’s Science Council brings a depth of knowledge from many senior figures.”
But then come the names. With the odd exception the “science council” is like a roll-call of quacks, the dregs left over from the Prince’s Foundation. The link (attached to each name) gives the College’s bio, My links tell a rather different story.
-
Professor George Lewith You’ll find plenty about George Lewith on this blog.
-
Professor Mustafa Djamgoz Superficially respectable but seduced by ‘ancient wisdom’ He once wrote to me "There are many ‘eastern’ remedies (such as acupuncture that we witnessed dismissed 25 year ago) that work. ". Well it isn’t as simple as that.
-
Professor Simon Gibbons A phytochemist with exaggerated ideas of what you can get from plants.
-
Professor Jane Plant A respectable geochemist who became obsessed with alternative medicine, Read about her here,
-
Dr Peter Fisher The Queen’s Homeopathic Physician. Advocate of the most discreded of all forms of quackery. Lots about him here.
-
Dr Michael Loughlin A post-modernist-influenced theorist who hates Ben Goldacre. Read about him here.
-
Dr Hugh MacPherson An acupuncturist and fellow traveller of the Prince of Wales. Read here.
-
Professor Andrew Miles I’m sorry to see him in this company after the good job he did in ejecting quacks at the University of Buckingham.
-
Simon Mills A man who thinks herbs can be classified as "hot"and "cold", See here and here
-
Professor Nicola Robinson Head of the Centre for Complementary Healthcare & Integrated Medicine,Thames Valley University A well known advocate of unevidenced treatments. Try Googling her
-
Dr Catherine Zollman Another hangover from the Princes’ Foundation, and believer in magic medicine
It seems that the "Scientific Council" of the College of Medicine could more properly be called an "Antiscientific Council".
There are a few gaps in this table, to be filled in soon. One can guarantee that a great deal more will appear about the College on the web, very soon.
The Governing Council of the College is equally replete with quacks (plus a few surprising names). It has on it, for example, a spiritual healer (Angie-Buxton King), a homeopath (Christine Glover), a herbalist (Michael McIntyre). Westminster University’s king of woo (David Peters), not to mention the infamous Karol Sikora. Buxton-King offers a remarkable service to heal people or animals at a distance.
Meanwhile, it seemed worthwhile to provide a warning that the title of the College is very deceptive. It hides an agenda that could do much harm.
It is, quite simply, the Prince of Wales by stealth.
Follow-up
28 October 2010
Professor Sir Graeme Catto, who has, disgracefully, allowed his name to be used as president of this “College” has said to me “There are real problems in knowing how to care for folk with chronic conditions and the extent of the evidence base for medicine is pretty limited”.
Yes of course that is quite true. There are many conditions for which medicine can still do little. There is a fascinating discussion to be had about how best to care for them. The answer to that is NOT to bring in spiritual healers and peddlers of sugar pills to deceive patients with their fairy stories. The “College of Medicine” will delay and pervert the sort of discussion that Catto says, rightly, is needed.
29 October 2010
I need a press card. I see that the BMJ also had a piece about the “College of Medicine” yesterday: Prince’s foundation metamorphoses into new College of Medicine, by Nigel Hawkes. He got the main point right there in the title.
As was clear since July, the driving force was Michael Dixon, Devon GP and ex medical director of the Prince’s Foundation. Hawkes goes easy on the homeopaths and spiritual healers, but did spot something that I can’t find on their web site. The “Faculties” will include
“in 2011, neuromusculoskeletal care. Two of the six strong faculty members for this specialty are from the British Chiropractic Association, which sued the author Simon Singh for libel for his disobliging remarks about the evidence base for their interventions.”
The College certainly picks its moment to endorse chiropractic, a subject that is in chaos and disgrace after they lost the Singh affair.
One bit of good news emerges from Hawkes’ piece, There is at least one high profile doubter in the medical establishment, Lord (John) Walton (his 2000 report on CAM was less than blunt, and has been widely misquoted by quacks) is reported as saying, at the opening ceremony
“I’m here as a sceptic, and I’ve just told my former houseman that,” he said. The target of the remark was Donald Irvine, another former GMC president and a member of the new college’s advisory council.”
31 October 2010. I got an email that pointed out a remarkable service offered by a member of College’s Governing Council. Angie Buxton-King, a “spiritual healer” employed by UCLH seems to have another web site, The Beacon of Healing Light that is not mentioned in her biography on the College’s site. Perhaps it should have been because it makes some remarkable claims. The page about distant healing is the most bizarre.
Absent Healing/Distant Healing
"Absent healing is available when it is not possible to visit the patient or it is not possible for the patient to be brought to our healing room. This form of healing has proved to be very successful for humans and animals alike."
"We keep a healing book within our healing room and every night spend time sending healing to all those who have asked for it. We have found that if a picture of the patient is sent to us the healing is more beneficial, we also require a weekly update to monitor any progress or change in the patients situation. Donations are welcome for this service."
I wonder what the Advertising Standards people make of the claim that it is “very successful”? I wonder what the president of the College makes of it? I’ve asked him.
Other blogs about the “College of Medicine”
30 October 2010. Margaret McCartney is always worth reading. As a GP she is at the forefront of medicine. She’s written about the College in The Crisis in Caring and dangerous inference. She’s also provided some information about a "professional member" of the College of Medicine, in ..and on Dr Sam Everington, at the Bromley by Bow Centre….
It is one of the more insulting things about alternative medicine addicts that they claim to be the guardians of caring (as opposed to curing), They are not, and people like McCartney and Michael Baum are excellent examples.
Prince of Wales to become honorary president of the “College of Medicine?”
Last night I heard a rumour that the Prince of Wales is, despite all the earlier denials, to become Honorary President of the “College”. If this is true, it completes the wholesale transformation of the late, unlamented, Prince’s Foundation for Integrated Medicine into this new “College”. Can anybody take it seriously now?
Text messages to Graeme Catto and Michael Dixon, inviting them to deny the rumour, have met with silence.
Herbal nonsense at the College
29 July 2011. I got an email from the College if Medicine [download it]. It contains a lot of fantasy about herbal medicines, sponsered by a company that manufactures them. It is dangeroous and corrupt.
Western herbal medicine need not be mystical nonsense, but it usually it is,
Plants often contain chemicals that have pharmacological actions, with all the possibilities for good and for harm that implies (see Plants
as medicines). It would be quite possible to teach about the plant constituents and their actions in an entirely scientific way, but it seems that this is not what courses in herbal medicine choose to do. That is why they shouldn’t be called Bachelor of Science degrees.
We have recently revealed the ancient nonsense taught at Middlesex University in its "BSc (Hons)" degree in Traditional Chinese Medicine in Dangerous Chinese medicine taught at Middlesex University as well as similar dangerous gobbledygook from the University of Westminster: see Why degrees in Chinese medicine are a danger to patients.
Western Herbal medicine does not talk about "knotted spleen Qi", but has an equally barmy mystical vocabulary of its own. They have in common a tendency to divide herbs into hot and cold, a crude and baseless classification that dates from a time when nothing was known about physiology or the causes of disease.
A recent post described the problems of finding out what exactly is taught on these courses: Not much Freedom of Information at University of Wales, University of Kingston, Robert Gordon University or Napier University
I lodged a Freedom of Information (Scotland) Act with Napier University Edinburgh on 10th August 2009. As almost always, it was refused, as was the internal review of my request. The response to the internal review came from Gerry Webber BA (Hons) 0 PHil MBA MCMI AUA (Fellow). Despite all those impressive sounding letters, he argued with a perfectly straight face that it was perfectly all right for the university to teach this sort of stuff. He ended
“On public interest grounds, I have therefore concluded that, in respect of the commercially sensitive information requested, the public interest is better served in withholding the information you have requested than in disclosing it.”
Despite all those impressive sounding letters after Dr Webber’s name, here was a solemn letter, on the university letterhead, defending the teaching of pseudoscientific nonsense The experience is surreal, but far from unique.
Although we won a judgement that compelled disclosure from the Information Commissioner for England and Wales, the Scottish law is slightly different so I had to appeal to the Scottish Information commissioner. [Download appeal]
A similar appeal was lodged for Robert Gordon’s University Aberdeen. They have already sent some homeopathy materials, and closed down the homeopathy course, as described at: Robert Gordon University stops its homeopathy course. Quackademia is crumbling. Napier University followed the same pattern, but a bit more slowly. They sent some of what I asked for without waiting for a formal judgement, after they had been contacted by the Scottish Information Commissioner.
Napier also shut down the degree from which the slides, below, were used. It is fascinating that so many places have done this shortly before what is taught is made public. Before that time the courses are defended and advertised. no doubt by people who have never given a moment’s thought to what is taught. In 2007, after my Nature article on the topic, the Glasgow Herald said
A spokeswoman for Napier University said it stood by the integrity of its BSc degrees.
“The BSc Herbal Medicine course uses an approach to teaching and training that we believe best prepares students for practice within a modern integrated healthcare system,” she said.
The university’s brochure for the course (still, carelessly, on the web at the time of writing), waxed lyrical about the herbal medicine course. Yet as soon as it becomes known what’s actually taught, the courses close.
What was taught on Napier’s Herbal Medicine “BSc”.
Materia medica starts with hot and cold herbs
Yes, but one of the problems is that very little is known about the therapeutic actions of herbs from "controlled enquiry". The material just isn’t there to fulfil this aim. To paraphrase their quotation,,you can call anything medicine, but plenty of people will argue with you if you can’t produce the evidence.
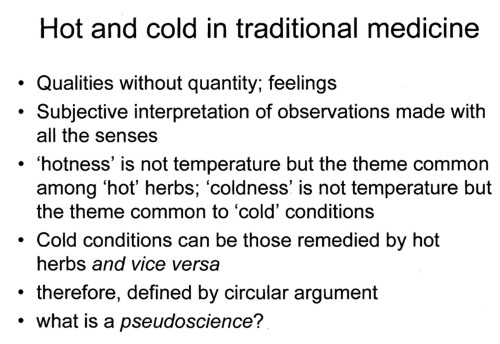
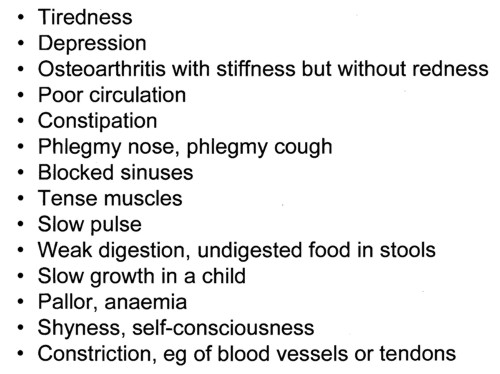
This slide strikes me as pure pre-scientific gobbledygook. All herbs and all diseases seem to fall into the ‘hot’ or ‘cold’ class. The ‘argument’ is entirely circular. Pure pseudoscience (is that what the lecturer told them in response to the last question?).
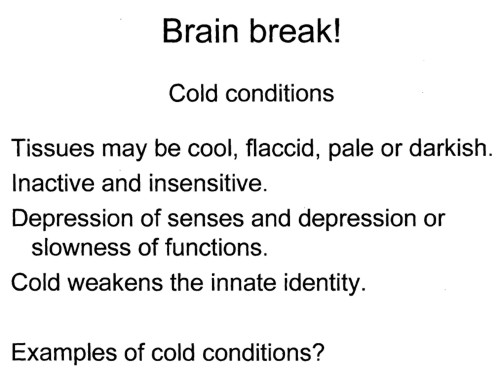
What do all these conditions have in common? They are all "cold". How can anyone take this sort of baloney seriously?
This quotation appears to have no comprehensible meaning at all. It carries overtones of the great "detox" fraud, and so perhaps is useful justification for slimming the wallets of the gullible.
Now we come to a real herb.
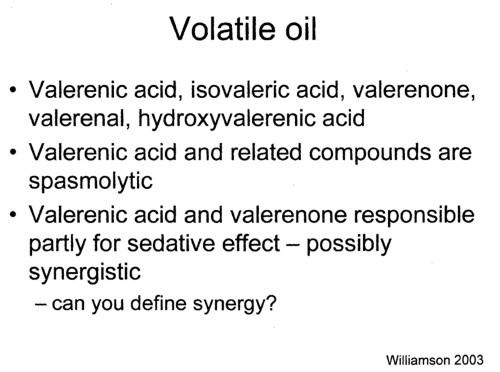
There is some real chenistry in this slide. Unfortunately it simply isn’t known whether these chemicals have any useful function. Usually it isn’t known either what dose of them you are giving in tincture of valerian. When I worked in a pharmacy in the 1950s, you could still find tincture of valerian on the shelves of a normal pharmacy, but iit soon vanished as paople realised it wasn’t much use. Disappeared from normal medicine, that is. it is still alive and well among herbalists.
Notice too, the mention of "synergy". The perpetual excuse of herbalists for giving impure mixtures of chemicals is that they might act synergistically. They are undeterred by the fact that no such synergy has ever been demonstrated properly. I asked that question ot Liz Williamson. editor of Potter’s herbal Cyclopedia, but answer came there none.
I’d be interested to know what answer was given to the last question, which isn’t as simple as it sounds. I wouldn’t mind betting it didn’t include a critical description of isobol analysis.
So what does Valerian do?
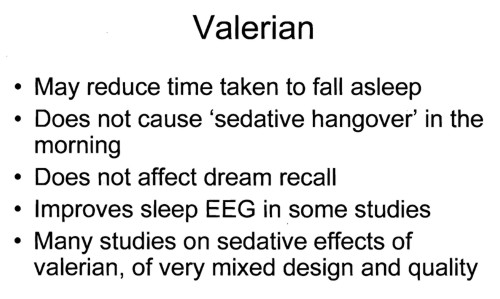
It seems, even from the lecture, that there is no unanimity that it does anything useful at all.
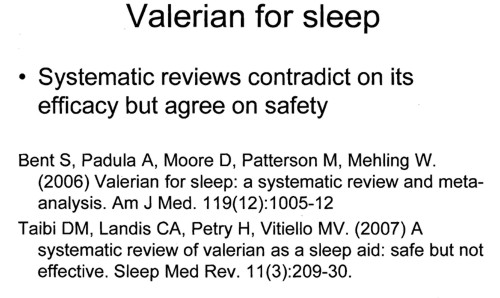
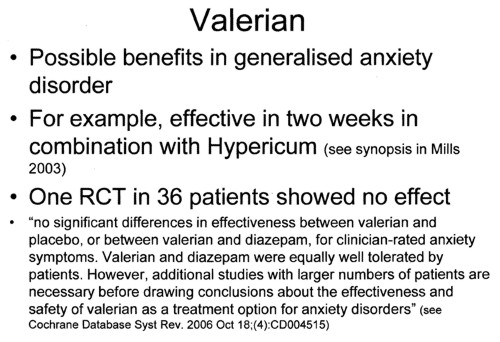
There is no worthwhile evidence to think it is useful for "generalises anxiety disorder" Let’s take another opinion.
The National Center for Complementary and Alternative Medicine (NCCAM) is the branch of the US National Institutes of Health which has spent around a billion dollars of US taxpayers’ money on research into alternative medicine, For all that effort they have failed to come up with a single useful treatment. Clearly they should be shut down. Nevertheless, as an organisation that is enthusiastic about alternative medicine, it’s interesting to see what they have to say about valerian.
What the Science Says
- Research suggests that valerian may be helpful for insomnia, but there is not enough evidence from well-designed studies to confirm this.
- There is not enough scientific evidence to determine whether valerian works for anxiety or for other conditions, such as depression and headaches.
Even NCCAM don’t pretend that there is any good reason to think it’s good for anything. So, you might ask, why are students being taught to treat people with it?
Simon Mills on "hot and cold herbs"
Many of the slides refer to a book by herbalist Simon Mills. You can see a video of a talk he gave in which he ‘explains’ "hot and cold herbs". It strikes me as pure gobbledygook. Make up your own mind.
Now take the test
This is a question from a Napier University exam paper
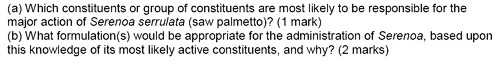
Which constituents are responsible for the actions of saw palmetto? Which actions would they be? This is what The National Center for Complementary and Alternative Medicine (NCCAM) says
about saw palmetto.
What the Science Says
- Several small studies suggest that saw palmetto may be effective for treating BPH symptoms.
- In 2006, a large study of 225 men with moderate-to-severe BPH found no improvement with 320 mg saw palmetto daily for 1 year versus placebo. NCCAM cofunded the study with the National Institute of Diabetes and Digestive and Kidney Diseases.
- There is not enough scientific evidence to support the use of saw palmetto for reducing the size of an enlarged prostate or for any other conditions.
- Saw palmetto does not appear to affect readings of prostate-specific antigen (PSA) levels. PSA is protein produced by cells in the prostate. The PSA test is used to screen for prostate cancer and to monitor patients who have had prostate cancer.
Magic Medicine
In the materials that I was sent, I see nothing to make me believe that herbalism is being taught as science. On the contrary, it all seems to confirm the definition given in the Patients’ Guide to Magic Medicine.
Herbal medicine BSc degrees still exist.
They are still running at the following universities.
The vice-chancellors are named because they are the people who must take responsibility for this sort of nonsense being taught in their universities.
University of East London (vice-chancellor from Feb 2010 is Patrick McGhee, who, in his previous job at University of Central Lancashire, did so much to prevent me from getting hold of their teaching materials, but then closed the courses anyway)
University of Lincoln (Vice chancellor, Professor Mary Stuart)
London Metropolitan University (vice-chancellor, (interim vice chancellor, Alfred Morris)
Middlesex University (vice-chancellor, Professor Michael Driscoll)
And, of course, the home of woo, the University of Westminster (vice-chancellor, Professor Geoffrey Petts). Their students are taught that Amethysts emit high Yin energy and that dowsing and pendulums can be used for diagnosis and treatment.
By the same token, we may congratulate Professor Dame Joan Stringer, vice-chancellor of Napier University Edinburgh for closing down the course from which these slides came. Perhaps now she should consider closing their ‘degrees’ in aromatherapy and ‘reflexology’
Follow-up
Yet another university has stopped its homeopathy course. The particular interest of this course was that it was being run at Robert Gordon University, Aberdeen, the vice-chancellor which was Michael Pittilo, until his recent premature death. Pittilo is the person who recommended to the government that herbalists and Chinese medicine practitioners should get honours degrees and be regulated like doctors. His report, was, in my opinions, disastrously bad.
It recently emerged that this, very bad, advice would not be accepted by the Department of Health (DH), so the campaign against the Pittilo proposals, on this blog and elsewhere was successful. The alternative DH proposals look pretty silly, but we won’t really know until after the election exactly what will happen.
Robert Gordon University (RGU): is the ‘post-1992’ university in Aberdeen, as opposed the the University of Aberdeen (where my son is at the moment). Much of RGU does an excellent job, but like so many post-1992 universities they harm themselves by running courses in barmy alternative medicine. RGU ran an Introduction To Homeopathy module (saved 9 April 2010).
In July 2009, I asked RGU to see some samples of the teaching materials on this module, partly as part of the campaign against Pittilo’s proposals. I asked to see the powerpoints and handouts for three lectures, (1) evidence for homeopathy, (2) first aid remedies, and (3) allergies.
In September 2009, this request, made under the Freedom of Information Act (Scotland), was, as always, rejected by RGU, though they did tell me that the evidence lecture had been produced by a lecturer from The Faculty of Homeopathy and the other two had been produced by a local GP.
So, as usual, I asked for the mandatory internal review of the decision. In October, the review upheld the original decision, as they almost always do. I referred the decision to the Scottish Information Commissioner (the law is slightly different in Scotland) and they have still not responded.
But on 8 April 2010 I got a letter from RGU.
|
“The above course requested is no longer part of the School of Nursing and Midwifery’s provision, and it was cessated [sic] in Semester One 2009/10. This followed a formal review of all Nursing and Midwifery modules and their viability. In the light of this the university has decided to release the information.” |
So yet another university has done the sensible thing. The course has been shut. Just for the record, I’ll reproduce a few of the slides from the lecture on “homeopathic remedies for allergies”.
Allergies can be dangerous, and occasionally lethal. To treat them with homeopathic pills, medicines that contain no medicine, is not just delusion, but a dangerous delusion which risks the lives of patients.
The "remedies" include nettles, sulphur, petroleum and arsenic. They’d be pretty scary but in fact the pills contain, in most cases, not a jot of nettle, sulphur, petroleum or arsenic. Homeopathic pharmacies stock thousands of bottles of identical sugar pills, each with a different label.


These dangerous delusions were being taught as fact in a UK university. The shame of it..
The Yuletide edition of the BMJ carries a lovely article by Jeffrey Aronson, Patent medicines and secret remedies. (BMJ 2009;339:b5415).
I was delighted to be asked to write an editorial about it, In fact it proved quite hard work, because the BMJ thought it improper to be too rude about the royal family, or about the possibility of Knight Starvation among senior medics. The compromise version that appeared in the BMJ is on line (full text link).
The changes were sufficient that it seems worth posting the original version (with links embedded for convenience).
The cuts are a bit ironic, since the whole point of the article is to point out the stifling political correctness that has gripped the BMA, the royal colleges, and the Department of Health when it comes to dealing with evidence-free medicine. It has become commonplace for people to worry about the future of the print media, The fact of the matter is you can often find a quicker. smarter amd blunter response to the news on blogs than you can find in the dead tree media. I doubt that the BMJ is in any danger of course. It has a good reputation for its attitude to improper drug company influence (a perpetual problem for clinical journals) as well as for clinical and science articles. It’s great to see its editor, Fiona Godlee, supporting the national campaign for reform of the libel laws (please sign it yourself).
The fact remains that when it comes to the particular problem of magic medicine, the action has not come from the BMA, the royal colleges, and certainly not from the Department of Health, It has come from what Goldacre called the “intrepid, ragged band of bloggers”. They are the ones who’ve done the investigative journalism, sent complaints and called baloney wherever they saw it. This article was meant to celebrate their collective efforts and to celebrate the fact that those efforts are beginning to percolate upwards to influence the powers that be.
It seems invidious to pick on one example, but if you want an example of beautiful and trenchant writing on one of the topics dealt with here, you’d be better off reading Andrew Lewis’s piece "Meddling Princes, Medical Regulation and Licenses to Kill” than anything in a print journal.
I was a bit disappointed by removal of the comment about the Prince of Wales. In fact I’m not particularly republican compared with many of my friends. The royal family is clearly good for the tourist industry and that’s important. Since Mrs Thatcher (and her successors) destroyed large swathes of manufacturing and put trust in the vapourware produced by dishonest and/or incompetent bankers, it isn’t obvious how the UK can stay afloat. If tourists will pay to see people driving in golden coaches, that’s fine. We need the money. What is absolutely NOT acceptable is for royals to interfere in the democratic political process. That is what the Prince of Wales does incessantly. No doubt he is well-meaning, but that is not sufficient. If I wanted to know the winner of the 2.30 at Newmarket, it might make sense to ask a royal. In medicine it makes no sense at all. But the quality of the advice is irrelevant anyway. The royal web site itself says “As a constitutional monarch, the Sovereign must remain politically neutral.”. Why does she not apply that rule to her son? Time to put him over your knee Ma’am?
Two of the major bits that were cut out are shown in bold, The many other changes are small.
BMJ editorial December 2009
Secret remedies: 100 years onTime to look again at the efficacy of remedies Jeffrey Aronson in his article [1] gives a fascinating insight into how the BMA, BMJ and politicians tried, a century ago, to put an end to the marketing of secret remedies. They didn’t have much success. The problems had not improved 40 years later when A.J. Clark published his book on patent medicines [2]. It is astounding to see how little has changed since then. He wrote, for example, “On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”> Clark himself was sued for libel after he’d written in a pamphlet “ ‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”. Although he initially tried to fight the case, impending destitution eventually forced him to apologise [3]. If that happened today, the accusation would have been repeated on hundreds of web sites round the world within 24 hours, and the quack would, with luck, lose [4]. As early as 1927, Clark had written “Today some travesty of physical science appears to be the most popular form of incantation” [5]. That is even more true today. Homeopaths regularly talk utter nonsense about quantum theory [6] and ‘nutritional therapists’ claim to cure AIDS with vitamin pills or even with downloaded music files. Some of their writing is plain delusional, but much of it is a parody of scientific writing. The style, which Goldacre [7] calls ‘sciencey’, often looks quite plausible until you start to check the references. A 100 years on from the BMA’s efforts, we need once again to look at the efficacy of remedies. Indeed the effort is already well under way, but this time it takes a rather different form. The initiative has come largely from an “intrepid, ragged band of bloggers” and some good journalists, helped by many scientific societies, but substantially hindered by the BMA, the Royal Colleges, the Department of Health and a few vice-chancellors. Even NICE and the MHRA have not helped much. The response of the royal colleges to the resurgence in magic medicine that started in the 1970s seems to have been a sort of embarrassment. They pushed the questions under the carpet by setting up committees (often populated with known sympathizers) so as to avoid having to say ‘baloney’. The Department of Health, equally embarrassed, tends to refer the questions to that well-known medical authority, the Prince of Wales (it is his Foundation for Integrated Health that was charged with drafting National Occupational Standards in make-believe subjects like naturopathy [8]. Two recent examples suffice to illustrate the problems. The first example is the argument about the desirability of statutory regulation of acupuncture, herbal and traditional Chinese medicine (the Pittilo recommendations) [9]. Let’s start with a definition, taken from ‘A patients’ guide to magic medicine’ [10]. “Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety”. It seems to me to be self-evident that you cannot start to think about a sensible form of regulation unless you first decide whether what you are trying to regulate is nonsense, though this idea does not seem to have penetrated the thinking of the Department of Health or the authors of the Pittilo report. The consultation on statutory regulation has had many submissions [11] that point out the danger to patients of appearing to give official endorsement of treatments that don’t work. The good news is that there seems to have been a major change of heart at the Royal College of Physicians. Their submission points out with admirable clarity that the statutory regulation of things that don’t work is a danger to patients (though they still have a blank spot about the evidence for acupuncture, partly as a result of the recent uncharacteristically bad assessment of the evidence by NICE [12]). Things are looking up. Nevertheless, after the public consultation on the report ended on November 16th, the Prince of Wales abused his position to make a well-publicised intervention on behalf of herbalists [13]. Sometimes I think his mother should give him a firm lesson in the meaning of the term ‘constitutional monarchy’, before he destroys it. The other example concerns the recent ‘evidence check: homeopathy’ conducted by the House of Commons Science and Technology Select Committee (SCITECH). First the definition [10]: “Homeopathy: giving patients medicines that contain no medicine whatsoever”. When homeopathy was dreamt up, at the end of the 18th century, regular physicians were lethal blood-letters, and it’s quite likely that giving nothing saved people from them. By the mid-19th century, discoveries about the real causes of disease had started, but homeopaths remain to this day stuck in their 18th century time warp. In 1842 Oliver Wendell Holmes said all that needed to be said about medicine-free medicine [14]. It is nothing short of surreal that the UK parliament is still discussing it in 2009. Nevertheless it is worth watching the SCITECH proceedings [15]. The first two sessions are fun, if only for the statement by the Professional Standards Director of Boots that they sell homeopathic pills while being quite aware that they don’t work. I thought that was rather admirable honesty. Peter Fisher, clinical director of the Royal Homeopathic Hospital, went through his familiar cherry-picking of evidence, but at least repeated his condemnation of the sale of sugar pills for the prevention of malaria. But for pure comedy gold, there is nothing to beat the final session. The health minister, Michael O’Brien, was eventually cajoled into admitting that there was no good evidence that homeopathy worked but defended the idea that the taxpayer should pay for it anyway. It was much harder to understand the position of the chief scientific advisor in the Department of Health, David Harper. He was evasive and ill-informed. Eventually the chairman, Phil Willis, said “No, that is not what I am asking you. You are the Department’s Chief Scientist. Can you give me one specific reference which supports the use of homeopathy in terms of Government policy on health?”. But answer came there none (well, there were words, but they made no sense). Then at the end of the session Harper said “homeopathic practitioners would argue that the way randomised clinical trials are set up they do not lend themselves necessarily to the evaluation and demonstration of efficacy of homeopathic remedies, so to go down the track of having more randomised clinical trials, for the time being at least, does not seem to be a sensible way forward.” Earlier, Kent Woods (CEO of the MHRA) had said “the underlying theory does not really give rise to many testable hypotheses”. These two eminent people seemed to have been fooled by the limp excuses offered by homeopaths. The hypotheses are testable and homeopathy, because it involves pills, is particularly well suited to being tested by proper RCTs (they have been, and when done properly, they fail). If you want to know how to do it, all you have to do is read Goldacre in the Guardian [16]. It really isn’t vert complicated. “Imagine going to an NHS hospital for treatment and being sent away with nothing but a bottle of water and some vague promises.” “And no, it’s not a fruitcake fantasy. This is homeopathy and the NHS currently spends around £10million on it.” That was written by health journalist Jane Symons, in The Sun [17]. A Murdoch tabloid has produced a better account of homeopathy than anything that could be managed by the chief scientific advisor to the Department of Health. And it isn’t often that one can say that. These examples serve to show that the medical establishment is slowly being dragged, from the bottom up, into realising that matters of truth and falsehood are more important than their knighthoods. It is all very heartening, both for medicine and for democracy itself. David Colquhoun. Declaration of interests. I was A.J. Clark chair of pharmacology at UCL, 1985 – 2004. 1. Aronson, JK BMJ 2009;339:b5415 2. Clark, A,J, (1938) Patent Medicines FACT series 14, London. See also Patent medicines in 1938 and now https://www.dcscience.net/?p=257 3. David Clark “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3) 4. Lewis, A. (2007) The Gentle Art of Homeopathic Killing 5. A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927 6. Chrastina, D (2007) Quantum theory isn’t that weak, (response to Lionel Milgrom). 7 Goldacre, B. (2008) Bad Science. HarperCollins 8. Skills for Health web site 9. A very bad report: gamma minus for the vice-chancellor 10. A Patients’ Guide to Magic Medicine, and also in the Financial Times. 12. NICE fiasco, part 2. Rawlins should withdraw guidance and start again 13. BBC news 1 December 2009 Prince Charles: ‘Herbal medicine must be regulated’. 14. Oliver Wendell Holmes (1842) Homeopathy and Its Kindred Delusions. 15. House of Commons Science and technology committee. Evidence check: homeopathy. Videos and transcripts available at http://www.viewista.com/s/fywlp2/ez/1 16. Goldacre, B. A Kind of Magic Guardian 16 November 2007. 17. Homeopathy is resources drain says |
Follow-up
There is a good account of the third SCITECH session by clinical science consultant, Majikthyse, at The Three Amigos.
16 December 2009.. Recorded an interview for BBC Radio 5 Live. It was supposed to go out early on 17th.
17 December 2009. The editorial is mentioned in Editor’s Choice, by deputy editor Tony Delamothe. I love his way of putting the problem "too many at the top of British medicine seem frozen in the headlights of the complementary medicine bandwagon". He sounds remarkably kind given that I was awarded (by the editor, Fiona Godlee, no less) a sort of booby prize at the BMJ party for having generated a record number of emails during the editing of a single editorial (was it really 24?). Hey ho.
17 December 2009. More information on very direct political meddling by the Prince of Wales in today’s Guardian, and in Press Association report.
17 December 2009. Daily Telegraph reports on the editorial, under the heading “ ‘Nonsense’ alternative medicines should not be regulated“. Not a bad account for a non-health journalist.
17 December 2009. Good coverage in the excellent US blog, Neurologica, by the superb Steven Novella.’ “Intrepid, Ragged Band of Bloggers” take on CAM‘ provides a chance to compare and contrast the problems in the UK and the USA.’
18 December 2009. Article in The Times by former special advisor, Paul Richards. “The influence of Prince Charles the lobbyist is out of hand. Our deference stops us asking questions.”
“A good starting point might be publication of all correspondence over the past 30 years. Then we will know the extent, and influence, of Prince Charles the lobbyist.”
Comments in the BMJ Quite a lot of comments had appeared by January 8th, though sadly they were mostly from the usual suspects who appear every time one suggests evidence matters. A reply was called for, so I sent this (the version below has links).
After a long delay, this response eventually appeared in the BMJ on January 15 2010.
It’s good to see so many responses, though somewhat alarming to see that several of them seem to expect an editorial to provide a complete review of the literature. I ‘ll be happy to provide references for any assertion that I made.
I also find it a bit odd that some people think that an editorial is not the place to express an opinion robustly. That view seems to me to be a manifestation of the very sort of political correctness that I was deploring. It’s a bit like the case when the then health minister, Lord Hunt, referred to psychic surgery as a “profession” when he should have called it a fraudulent conjuring trick. Anything I write is very mild compared with what Thomas Wakley wrote in the Lancet, a journal which he founded around the time UCL came into existence. For example (I quote)
“[We deplore the] “state of society which allows various sets of mercenary, goose-brained monopolists and charlatans to usurp the highest privileges…. This is the canker-worm which eats into the heart of the medical body.” Wakley, T. The Lancet 1838-9, 1
I don’t think it is worth replying to people who cite Jacques Benveniste or Andrew Wakefield as authorities. Neither is it worth replying to people who raise the straw man argument about wicked pharmaceutical companies (about which I am on record as being as angry as anyone). But I would like to reply directly to some of the more coherent comments.
Sam Lewis and Robert Watson. [comment] Thank you for putting so succinctly what I was trying to say.
Peter Fisher [comment]. I have a lot of sympathy for Peter Fisher. He has attempted to do some good trials of homeopathy (they mostly had negative outcomes). He said he was "very angry" when the non-medical homeopaths were caught out recommending their sugar pills for malaria prevention (not that this as stopped such dangerous claims which are still commonplace). He agreed with me that there was not sufficient scientific basis for BSc degrees in homeopathy. I suppose that it isn’t really surprising that he continues to cherry pick the evidence. As clinical director of the Royal London Homeopathic Hospital and Homeopathic physician to the Queen, just imagine the cognitive dissonance that would result if he were to admit publicly that is all placebo after all. He has come close though. His (negative) trial for homeopathic treatment of rheumatoid arthritis included the words "It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response” [2]. [download
the paper]. When it comes to malaria, it matters a lot.
Adrian White [comment] seems to be cross because I cited my own blog. I did that simply because if he follows the links there he will find the evidence. In the case of acupuncture it has been shown time after time that "real" acupuncture does not differ perceptibly from sham. That is true whether the sham consists of retractable needles or real needles in the "wrong" places. A non-blind comparison between acupuncture and no acupuncture usually shows some advantage for the former but it is, on average, too small to be of much clinical significance [3]. I agree that there is no way to be sure that this advantage is purely placebo effect but since it is small and transient it really doesn’t matter much. Nobody has put it more clearly than Barker Bausell in his book, Snake Oil Science [4]
White also seems to have great faith in peer review. I agree that in real science it is probably the best system we have. But in alternative medicine journals the "peers" are usually other true believers in whatever hocus pocus is being promoted and peer reveiw breaks down altogether.
R. M. Pittilo [comment] I’m glad that Professor Pittilo has replied in person because I did single out his report for particular criticism. I agree that his report said that NHS funding should be available to CAM only where there is evidence of efficacy. That was not my criticism. My point was that in his report, the evidence for efficacy was assessed by representatives of Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Every one of them would have been out of work if they had found their subjects were nonsense and that, no doubt, explains why the assessment was so bad. To be fair, they did admit that the evidence was not all that it might be and recommended (as always) more research I’d like to ask Professor Pittilo how much money should be spent on more research in the light of the fact that over a billion dollars has been spent in the USA on CAM research without producing a single useful treatment. Pittilo says "My own view is that both statutory regulation and the quest for evidence should proceed together" but he seems to neglect the possibility that the quest for evidence might fail. Experience in the USA suggests that is exactly what has, to a large extent, already happened.
I also find it quite absurd that the Pittilo report should recommend, despite a half-hearted admission that the evidence is poor, that entry to these subjects should be via BSc Honours degrees. In any case he is already thwarted in that ambition because universities are closing down degrees in these subjects having realised that the time to run a degree is after, not before, you have some evidence that the subject is not nonsense. I hope that in due course Professor Pittilo may take the same action about the courses in things like homeopathy that are run by the university of which he is vice-chancellor. That could only enhance the academic reputation of Robert Gordon’s University.
George Lewith [comment] You must be aware that the proposed regulatory body, the Health Professions Council, has already broken its own rules about "evidence-based practice" by agreeing to take on, if asked, practitioners of Herbal Medicine, Chinese Medicine and Acupuncture. They have (shamefully) excluded the idea that claims of efficacy would be regulated. In other word they propose to provide exactly the sort of pseudo-regulation which would endanger patients They are accustomed to the idea that regulation is to do only with censoring practitioners who are caught in bed with patients. However meritorious that may be, it is not the main problem with pseudo-medicine, an area in which they have no experience. I’m equally surprised that Lewith should recommend that Chinese evaluation of Traditional Chinese medicine should be included in meta-analyses, in view of the well-known fact that 99% of evaluations from China are positive: “No trial published in China or Russia/USSR found a test treatment to be ineffective” [5]. He must surely realise that medicine in China is a branch of politics. In fact the whole resurgence in Chinese medicine and acupuncture in post-war times has less to do with ancient traditions than with Chinese nationalism, in particular the wish of Mao Tse-Tung to provide the appearance of health care for the masses (though it is reported that he himself preferred Western Medicine).
1. Lord Hunt thinks “psychic surgery” is a “profession”. https://www.dcscience.net/?p=258
2. Fisher, P. Scott, DL. 2001 Rheumatology 40, 1052 – 1055. [pdf file]
3. Madsen et al, BMJ 2009;338:a3115 [pdf file]
4. R, Barker Bausell, Snake Oil Science, Oxford University Press, 2007
5. Vickers, Niraj, Goyal, Harland and Rees (1998, Controlled Clinical Trials, 19, 159-166) “Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials”. [pdf file]
15 January 2010. During the SciTech hearings, Kent Woods (CEO of the MHRA) made a very feeble attempt to defend the MHRA’s decision to allow misleading labelling of homeopathic products. Now they have published their justification for this claim. It is truly pathetic, as explained by Martin at LayScience: New Evidence Reveals the MHRA’s Farcical Approach to Homeopathy. This mis-labelling cause a great outcry in 2006, as documented in The MHRA breaks its founding principle: it is an intellectual disgrace, and Learned Societies speak out against CAM, and the MHRA.
22 January 2010 Very glad to see that the minister himself has chosen to respond in the BMJ to the editorial
|
Rt Hon. Mike O’Brien QC MP, Minister of State for Health Services I am glad that David Colquhoun was entertained by my appearance before the Health Select Committee on Homeopathy. But he is mistaken when he says, “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense.” Regulation is about patient safety. Acupuncture, herbal and traditional Chinese medicine involve piercing the skin and/or the ingestion of potentially harmful substances and present a possible risk to patients. The Pittilo Report recommends statutory regulation and we have recently held a public consultation on whether this is a sensible way forward. Further research into the efficacy of therapies such as Homeopathy is unlikely to settle the debate, such is the controversy surrounding the subject. That is why the Department of Health’s policy towards complementary and alternative medicines is neutral. Whether I personally think Homeopathy is nonsense or not is besides the point. As a Minister, I do not decide the correct treatment for patients. Doctors do that. I do not propose on this occasion to interfere in the doctor-patient relationship. |
Here is my response to the minister
|
I am very glad that the minister himself has replied. I think he is wrong in two ways, one relatively trivial but one very important. First, he is wrong to refer to homeopathy as controversial. It is not. It is quite the daftest for the common forms of magic medicine and essentially no informed person believes a word of it. Of course, as minister, he is free to ignore scientific advice, just as the Home Secretary did recently. But he should admit that that is what he is doing, and not hide behind the (imagined) controversy. Second, and far more importantly, he is wrong, dangerously wrong, to say it I was mistaken to claim that “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense". According to that view it would make sense to grant statutory regulation to voodoo and astrology. The Pittilo proposals would involve giving honours degrees in nonsense if one took the minister’s view that it doesn’t matter whether the subjects are nonsense or not. Surely he isn’t advocating that? The minister is also wrong to suppose that regulation, in the form proposed by Pittilo, would do anything to help patient safety. Indeed there is a good case to be made that it would endanger patients (not to mention endangering tigers and bears). The reason for that is that the main danger to patients arises from patients being given “remedies” that don’t work. The proposed regulatory body, the Health Professions Council, has already declared that it is not interested in whether the treatments work or not. That in itself endangers patients. In the case of Traditional Chinese Medicine, there is also a danger to patients from contaminated medicines. The HPC is not competent to deal with that either. It is the job of the MHRA and/or Trading Standards. There are much better methods of ensuring patient safety that those proposed by Pittilo. In order to see the harm that can result from statutory regulation, it is necessary only to look at the General Chiropractic Council. Attention was focussed on chiropractic when the British Chiropractic Association decided, foolishly, to sue Simon Singh for defamation. That led to close inspection of the strength of the evidence for their claims to benefit conditions like infant colic and asthma. The evidence turned out to be pathetic, and the result was that something like 600 complaints were made to the GCC about the making of false health claims (including two against practices run by the chair of the GCC himself). The processing of these complaints is still in progress, but what is absolutely clear is that the statutory regulatory body, the GCC, had done nothing to discourage these false claims. On the contrary it had perpetrated them itself. No doubt the HPC would be similarly engulfed in complaints if the Pittilo proposals went ahead. It is one thing to say that the government chooses to pay for things like homeopathy, despite it being known that they are only placebos, because some patients like them. It is quite another thing to endanger patient safety by advocating government endorsement in the form of statutory regulation, of treatments that don’t work. I would be very happy to meet the minister to discuss the problems involved in ensuring patient safety. He has seen herbalists and other with vested interests. He has been lobbied by the Prince of Wales. Perhaps it is time he listened to the views of scientists too. |
Both the minister’s response, and my reply, were reformatted to appear as letters in the print edition of the BMJ, as well as comments on the web..
It seems very reasonable to suggest that taxpayers have an interest in knowing what is taught in universities. The recent Pittilo report suggested that degrees should be mandatory in Acupuncture, Herbal Medicine and Traditional Chinese Medicine. So it seems natural to ask to see what is actually taught in these degrees, so one can judge whether it protects the public or endangers them.
Since universities in the UK receive a great deal of public money, it’s easy. Just request the material under the Freedom of Information Act.
Well, uh, it isn’t as simple as that.
Every single application that I have made has been refused. After three years of trying, the Information Commissioner eventually supported my appeal to see teaching materials from the Homeopathy "BSc" at the University of Central Lancashire. He ruled that every single objection (apart from one trivial one) offered by the universities was invalid. In particular, it was ruled that univerities were not "commercial" organisations for the purposes of the Act.
So problem solved? Not a bit of it. I still haven’t seen any of the materials from the original request because the University of Central Lancashire appealed against the decision and the case of University of Central Lancashire v Information Commissioner is due to be heard on November 3rd, 4th and 5th in Manchester. I’m joined (as lawyers say) as a witness. Watch this space.
UCLan is not the exception. It is the rule. I have sought under the Freedom of Information Act, teaching materials from UClan (homeopathy), University of Salford (homeopathy, reflexology and nutritional therapy), University of Westminster (homeopathy, reflexology and nutritional therapy), University of West of England, University of Plymouth and University of East London, University of Wales (chiropractic and nutritional therapy), Robert Gordon University Aberdeen (homeopathy), Napier University Edinburgh (herbalism).
In every single case, the request for teaching materials has been refused. And that includes the last three, which were submitted after the decision of the Information Commissioner. They will send things like course validation documents, but these are utterly uninformative box-ticking documents. They say nothing whatsoever about what is actually taught.
The fact that I have been able to discover quite a lot about what’s being taught owes nothing whatsoever to the Freedom of Information Act. It is due entirely to the many honest individuals who have sent me teaching materials, often anonymously. We should be grateful to them. Their principles are rather more impressive than those of their principals.
Since this started about three years ago, two of the universities, UCLan and Salford, have shut down entry to all of their CAM courses. And Westminster has shut two of them, with more rumoured to be closing soon. They are to be congratulated for that, but is far from being the end of the matter. The Department of Health, and some of the Royal Colleges, have yet to catch up with the universities, The Pittolo report, which recommends making degrees compulsory, is being considered by the Department of Health. The consultation ends on November 2nd: if you haven’t yet responded, please do so now (see how here, and here).
A common excuse: the university does not possess teaching materials (yes, really)
Several of the universities claim that they cannot send teaching materials, because they have no access to them. This happens when the university has accredited a course that is run by another, privately run, institution. The place that does the actual teaching, being private, is exempt from the Freedom of Information Act.
The ludicrous corollary of this excuse is that the university has accredited the course without checking on what is taught, and in some cases without even having seen a timetable.
The University of Wales
In fact the University of Wales doesn’t run courses at all. Like the (near moribund) University of London, it acts as a degree-awarding authority for a lot of Welsh Universities. It also validates a lot of courses in non-university institutions, 34 or so of them in the UK, and others scattered round the world.
Many of them are theological colleges. It does seem a bit odd that St Petersburg Christian University, Russia, and International Baptist Theological Seminary, Prague, should be accredited by the University of Wales.
They also validate the International Academy of Osteopathy, Ghent (Belgium), Osteopathie Schule Deutschland, the Istituto Superiore Di Osteopatia, Milan, the Instituto Superior De Medicinas Tradicionales, Barcelona, the Skandinaviska Osteopathögskolan (SKOS) Gothenburg, Sweden and the College D’Etudes Osteopathiques, Canada.
The 34 UK institutions include the Scottish School of Herbal Medicine, the Northern College of Acupuncture and the Mctimoney College of Chiropractic.
The case of the Nutritional Therapy course has been described already in Another worthless validation: the University of Wales and nutritional therapy. It emerged that the course was run by a grade 1 new-age fantasist. It is worth recapitulating the follow up.
What does the University of Wales say? So far, nothing. Last week I sent brief and polite emails to Professor Palastanga and to
Professor Clement to try to discover whether it is true that the validation process had indeed missed the fact that the course organiser’s writings had been described as “preposterous, made-up, pseudoscientific nonsense” in the Guardian.
So far I have had no reply from the vice-chancellor, but on 26 October I did get an answer from Prof Palastanga.
As regards the two people you asked questions about – J.Young – I personally am not familiar with her book and nobody on the validation panel raised any concerns about it. As for P.Holford similarly there were no concerns expressed about him or his work. In both cases we would have considered their CV’s as presented in the documentation as part of the teaching team. In my experience of conducting degree validations at over 16 UK Universities this is the normal practice of a validation panel.
I have to say this reply confirms my worst fears. Validation committees such as this one simply don’t do their duty. They don’t show the curiosity that is needed to discover the facts about the things that they are meant to be judging. How could they not have looked at the book by the very person that they are validating? After all that has been written about Patrick Holford, it is simply mind-boggling that the committee seems to have been quite unaware of any of it.It is yet another example of the harm done to science by an unthinking, box-ticking approach.
Incidentally, Professor Nigel Palastanga has now been made Pro Vice-Chancellor (Quality) at the University of Wales and publishes bulletins on quality control. Well well.
The McTimoney College of Chiropractic was the subject of my next Freedom of Information request to the University of Wales. The reasons for that are, I guess, obvious. They sent me hundreds of pages of validation documents, Student Handbooks (approx 50 pages), BSc (Hons) Chiropractic Course Document. And so on. Reams of it. The documents mostly are in the range of 40 to 100 pages. Tons of paper, but none of it tells you anyhing whatsover of interest about what’s being taught. They are a testament to the ability of universities to produce endless vacuous prose with
very litlle content.
They did give me enough information to ask for a sample of the teaching materials on particular topics. But I gor blank refusal, on the grounds that they didn’t possess them. Only McTimoney had them. Their (unusually helpful) Freedom of Information officer replied thus.
“The University is entirely clear about the content of the course but the day to day timetabling of teaching sessions is a matter for the institution rather than the University and we do not require or possess timetable information. The Act does not oblige us to request the information but there is no reason you should not approach McTimoney directly on this.”
So the university doesn’t know the timetable. It doesn’t know what is taught in lectures, but it is " entirely clear about the content of the course".
This response can be described only as truly pathetic.
Either this is a laughably crude form of obstruction of my request, or perhaps, even more frighteningly, the university really believes that its endless box-ticking documents actually provide some useful control of quality. Perhaps the latter interpretation is more charitable. After all, the QAA, CHRE, UUK and every HR department share similar delusions about what constitutes quality.
Perhaps it is just yet another consequence of having science run largely by people who have never done it and don’t understand it.
Validation is a business. The University of Wales validates no fewer than 11,675 courses altogether. Many of these are perfectly ordinary courses in universities in Wales, but they validate 594 courses at non-Welsh accredited institutions, an activity that earned them £5,440,765 in the financial year 2007/8. There’s nothing wrong with that if they did the job properly. In the two cases I’ve looked at, they haven’t done the job properly. They have ticked boxes but they have not looked at what’s being taught or who is teaching it.
The University of Kingston
The University of Kingston offers a “BSc (Hons)” in acupuncture. In view of the fact that the Pittilo group has recommended degrees in acupuncture, there is enormous public interest in what is taught in such degrees, so I asked.
They sent the usual boring validation documents and a couple of sample exam papers . The questions were very clinical, and quite beyond the training of acupuncturists. The validation was done by a panel of three, Dr Larry Roberts (Chair, Director of Academic Development, Kingston University), Mr Roger Hill (Accreditation Officer, British Acupuncture Accreditation Board) and Ms Celia Tudor-Evans (Acupuncturist, College of Traditional Acupuncture, Leamington Spa). So nobody with any scientific expertise, and not a word of criticism.
|
Further to your recent request for information I am writing to advise that the University does not hold the following requested information: (1) Lecture handouts/notes and powerpoint presentations for the following sessions, mentioned in Template 3rd year weekend and weekday course v26Aug2009_LRE1.pdf (a) Skills 17: Representational systems + Colour & Sound ex. Tongue feedback 11 (b) Mental Disease + Epilepsy Pulse feedback 21 (c) 18 Auricular Acupuncture (d) Intro. to Guasha + practice Cupping, moxa practice Tongue feedback 14 (2) I cannot see where the students are taught about research methods and statistics. I would like to see Lecture handouts/notes and PowerPoint presentations for teaching in this area, but the ‘timetables’ that you sent don’t make clear when or if it is taught. The BSc Acupuncture is delivered by a partner college, the College of Integrated Chinese Medicine (CICM), with Kingston University providing validation only. As such, the University does not hold copies of the teaching materials used on this course. In order to obtain copies of the teaching materials required you may wish to contact the College of Integrated Chinese Medicine directly. This completes the University’s response to your information request. |
So again we see that Kingston has validated the course but has not seen a timetable, far less what is taught. My reply was thus
|
Yes I am exceedingly unhappy about it. The university attaches its name to the course so it must obviously be able to get the material simply by asking for it (I’m surprised that the university should endorse a course without knowing what is taught on it, but that’s another matter). I request formally that you obtain this material. If necessary please read this as a formal appeal. |
I await with interest. In every single case so far, the internal review has merely confirmed the initial refusal. It means a bit of a delay before the case goes to the Information Commisssioner’s Office.
Napier University Edinburgh
Napier University runs a "BSc (Hons) Herbal medicine". (brochure here). Since herbal medicine is a subject of the Pittilo recommendations, there is enormous public interest in what they teach. So I asked, under the Freedom of Information (Scotland) Act (2002). They sent quite quickly validation and accreditation documents, some examination papers, timetables and lecture lists.
The validation was the usual vacuous box-ticking stuff though it did reveal that the course “made extensive use of techniques such as tongue and pulse diagnosis”, which are well known phoney diagnosis methods, about as much use as a pendulum (as used at Westminster University).
As at Kingston University, the exam papers they chose to send were mostly "pretend doctor" stuff. One of them was
Discuss the herbal practitioner’s role in the management of IHD [ischaemic heart disease)
How one would like to see what the students said, and, even more one would like to see the model answer. Amateurs who try to treat potentially serious conditions are a danger to the public.
So then we got to the interesting bit, the request for actual teaching materials.
|
I have looked at the material that you sent and I’d now like to make the following supplementary request (A) Lecture notes/handouts and powerpoint slides for the following small smaple of lectures HRB09102 Materia Medica 4 Materia Medica 3 HRB08103 Clinical Medicine and Diagnosis 4 (HRB09104) HRB09100 Materia Medica & Herbal Practice BSc Herbal Medicine : Materia Medica HRB07102 Lastly, I can see nowhere in the timetable, lectures that deal with Research methods, clinical trial design and statistics. |
No prizes for guessing the result Total refusal to send any of them. To make matters worse, the main grounds for refusal were the very "commercial interests" which, after careful legal examination, the Information Commissioner (for England and Wales) had decided were invalid. They say too that "The public interest in withholding the information is greater than the public interest in its release".. It is hard to see how the public interest is served by concealing from the people who pay for the degrees what is taught on degrees that Pittilo wants to make compulsory. [Download the whole response]
The matter is now under internal appeal (read the appeal) and eventually we shall find out whether the Scottish Information Commissioner backs the judgement.
Robert Gordon University Aberdeen
This case has particular interest because the Vice-Chancellor of Robert Gordon University is Professor Michael Pittilo, chair of the highly contentious steering group that recommended degress in CAM. Robert Gordon University (RGU) does not teach herbal medicine or acupuncture. But they do run An Introduction to Homeopathy. All the degrees in homeopathy have closed. It is perhaps the daftest and most discredited of all the popular forms of Magic Medicine. But Professor Pittilo thinks it is an appropriate subject to teach in his university.
So again I asked for information under the Freedom of Information (Scotland) Act 2002. They sent me quite quckly a list of the powerpoint presentations used on the courses [download it]. I asked for a small sample of the powerpoints. And again the university did not possess them!
|
I should like to see only the following three powerpoint presentations in the first instance, please.
Please can you let me know also who produced the powerpoints. (1) Evidence for homeopathy I note that you will have to request them but since they are being offered as part of a course offered by RGU, so RGU is responsible for their quality, I presume that this should cause no problem. |
The request was refused on much the same grounds as used by Napier University. As usual, the internal review just confirmed the initial proposal (but dropped the obviously ludicrous public interest defence). The internal review said
“it is mainly the quality of our courses (including course material) and teaching which has given us the position of "the best modern university in Scotland"
I am bound to ask, if the university is so proud of its course material, why is it expending so much time and money to prevent anyone from seeing a small sample of it?
My appeal has been sent to the Scottish Information Commissioner [download the appeal].
What are vice-chancellors thinking about?
I find it very difficult to imagine what is going through the heads of vice-chancellors who run courses in mumbo-jumbo. Most of them don’t believe a word of it (though Michael Pittilo might be an exception) yet they foist it on their students. How do they sleep at night?
Recently the excellent Joe Collier wrote a nice BMJ blog which applauded the lack of respect for authority in today’s students, Joe Collier says good riddance to old-fashioned respect. I couldn’t resist leaving a comment.
|
I couldn’t agree more. There is nothing quite so unnerving as being addressed as “Sir”. It is an advantage of age that you realise what second-rate people come to occupy very grand positions. Still odder since, if occasionally they are removed for incompetence, they usually move to an even grander position. I guess that when I was an undergraduate, I found vice-chancellors somewhat imposing. That is, by and large, not a view that survives closer acquaintance. |
Should teaching materials be open to the public?
There is only one university in the world that has, as a matter of policy, made all of its teaching material open to the public, that is the Massachusetts Institute of Technology (MIT). I can recommend strongly course 18.06, a wonderful set of lectures on Linear Algebra by Gilbert Strang. (It is also a wonderful demonstration of why blackboards may be better than Powerpoint for subjects like this). Now they are on YouTube too.
A lot of other places have made small moves in the same direction, as discussed recently in Times Higher Education, Get it Out in the Open.
Now the OU is working with other British universities to help them develop and share open course materials. In June, at the celebrations for the 40th anniversary of the OU, Gordon Brown announced funding to establish the Support Centre for Open Resources in Education at the OU, as part of a £7.8 million grant designed to enhance the university’s national role.
The funding follows a separate grant of £5.7 million from the Higher Education Funding Council for England for universities across the sector to make thousands of hours of free learning materials available.
Much material is available on the web, when individual teachers choose to place it there, but at the same time there is a move in the other direction. In particular, the widespread adoption of Moodle has resulted in a big decrease in openness. Usually you have to be registered on a course to see the material. Even other people in the university can’t see it. I think that is a deplorable development (so, presumably, does HEFCE).
Conclusion
I was told by the Univerity of Kingston that
“The course is one which the University has validated and continues to be subject to the University’s quality assurance procedures, such as internal subject reviews, annual monitoring and external examining”
The only conclusion to be drawn from this is that “quality arrurance procedures” work about as well in universities as they did in the case of baby Peter. No doubt they were introduced with worthy aims. But in practice they occupy vast amounts of time for armies of bureaucrats, and because the brain does not need to be engaged they end up endorsing utter nonsenes. The system is broken.
Resistance is futile. You can see a lot of the stuff here
It is hard to keep secrets in the internet age. Thanks to many wonderful people who have sent me material. you can see plenty of what is taught, despite the desperate attempts of vice-chancellors to conceal it. Try these links.
What is actually taught
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself
https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients
https://www.dcscience.net/?p=2043
More make-believe from the University of Westminster. This time its Naturopathy
https://www.dcscience.net/?p=1812
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
https://www.dcscience.net/?p=1329
The opposite of science
https://www.dcscience.net/?p=1191
Bad medicine. Barts sinks further into the endarkenment.
https://www.dcscience.net/?p=1143
A letter to the Times, and progress at Westminster
https://www.dcscience.net/?p=984
Nutritional Fairy Tales from Thames Valley University
https://www.dcscience.net/?p=260
Westminster University BSc: amethysts emit high yin energy
https://www.dcscience.net/?p=227
References for Pittilo report consultation
A very bad report: gamma minus for the vice-chancellor
https://www.dcscience.net/?p=235
The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on the Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire,
https://www.dcscience.net/?p=2310
An excellent submission to the consultation on statutory regulation of alternative medicine (Pittilo report)
https://www.dcscience.net/?p=2329
Follow-up
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
More boring politics, but it matters. The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register should normally be through a Bachelor degree with Honours
For the background on this appalling report, see earlier posts.
A very bad report: gamma minus for the vice-chancellor
The Times (blame subeditor for the horrid title), and some follow up on the Times piece
The Health Professions Council breaks its own rules: the result is nonsense
Chinese medicine -acupuncture gobbledygook revealed
Consultation opens on the Pittilo report: help stop the Department of Health making a fool of itself
Why degrees in Chinese medicine are a danger to patients
The Department of Health consultation shuts on November 2nd. If you haven’t responded yet, please do. It would be an enormous setback for reason and common sense if the government were to give a stamp of official approval to people who are often no more than snake-oil salesman.
Today I emailed my submission to the Pittilo consultation to the Department of Health, at HRDListening@dh.gsi.gov.uk
The submission
I sent the following documents, updated versions of those already posted earlier.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
- An example of dangerous (and probably illegal) claims that are routinely made by TCM practitioners [download pdf]f
I also completed their questionnaire, despite its deficiencies. In case it is any help to anyone, this is what I said:
The questionnaire
Q1: What evidence is there of harm to the public currently as a result of the activities of acupuncturists, herbalists and traditional Chinese medicine practitioners? What is its likelihood and severity?
Harm
No Harm
Unsure
Comment
The major source of harm is the cruel deception involved in making false claims of benefit to desperate patients. This applies to all three.
In the case of herbal and TCM there is danger from toxicity because herbal preparations are unstandardised so those that do contain an active ingredient are given in an unknown dose. This is irresponsible and dangerous (but would not be changed by the proposals for regulation).
In addition TCM suffers from recurrent problems of contamination with heavy metals, prescription drugs and so on. Again this would not be the business of the proposed form of regulation.
Q2: Would this harm be lessened by statutory regulation? If so, how?
Yes
No
Unsure
The proposed form of regulation would be no help at all. The HPC has already said that it is not concerned with whether or not the drug works, and, by implication, does not see itself as preventing false health claims (just as the GCC doesn’t do this). False claims are the responsibility of Trading Standards who are meant to enforce the Consumer Protection Unfair Trading Regulations (May 2008), though they do not at present enforce them very effectively. Also Advertisng Standards. The proposed regulation would not help, and could easily hinder public safety as shown by the fact that the GCC has itself been referred to the Advertisng Standards Authority.
The questions of toxicity and contamination are already the responsibility of Trading Standards and the MHRA. Regulation by the HPC would not help at all. The HPC is not competent to deal with such questions.
Q3: What do you envisage would be the benefit to the public, to practitioners and to businesses, associated with introducing statutory regulation?
Significant benefit
Some benefit
No benefit
Unsure
This question is badly formulated because the answer is different according to whether you are referring to the public, to practitioners or to businesses.
The public would be endangered by the form of regulation that is proposed, as is shown very clearly by the documents that I have submitted separately.
In the case of practitioners and businesses, there might be a small benefit, if the statutory regulation gave the impression that HM and TCM had government endorsement and must therefore be safe and effective.
There is also one way that the regulation could harm practitioners and businesses. If the HPC received a very large number of complaints about false health claims, just as the GCC has done recently, not only would it cost a large amount of money to process the claims, but the attendant bad publicity could harm practitioners. It is quite likely that this would occur since false claims to benefit sick people are rife in the areas of acupuncture, HM and TCM.
Q4: What do you envisage would be the regulatory burden and financial costs to the public, to practitioners, and to businesses, associated with introducing statutory regulation? Are these costs justified by the benefits and are they proportionate to the risks? If so, in what way?
Justified
Not Justified
Unsure
Certainly not justified. Given that I believe that the proposed form of regulation would endanger patients, no cost at all would be justified. But even if there were a marginal benefit, the cost would be quite unjustified. The number of practitioners involved is very large. It would involve a huge expansion of an existing quango, at a time when the government is trying to reduce the number of quangos. Furthermore, if the HPC were flooded with complaints about false health claims, as the GCC has been, the costs in legal fees could be enormous.
Q5: If herbal and TCM practitioners are subject to statutory regulation, should the right to prepare and commission unlicensed herbal medicines be restricted to statutorily regulated practitioners?
Yes
No
Unsure
I don’t think it would make much difference. The same (often false) ideas are shared by all HM people and that would continue to be the same with or without SR.
Q6: If herbal and TCM practitioners are not statutorily regulated, how (if at all) should unlicensed herbal medicines prepared or commissioned by these practitioners be regulated?
They could carry on as now, but the money that would have been spent on SR should instead be used to give the Office of Trading Standards and the MHRA the ability to exert closer scrutiny and to enforce more effectively laws that already exist. Present laws, if enforced, are quite enough to protect the public.
Q7: What would be the effect on public, practitioners and businesses if, in order to comply with the requirements of European medicines legislation, practitioners were unable to supply manufactured unlicensed herbal medicines commissioned from a third party?
Significant effect
Some effect
No effect
Unsure
European laws,especialliy in food area, are getting quite strict about the matters of efficacy. The proposed regulation, which ignores efficacy, could well be incompatible with European law, if not now, then soon. This would do no harm to legitimate business though it might affect adversely businesses which make false claims (and there are rather a lot of the latter).
Q8: How might the risk of harm to the public be reduced other than by orthodox statutory regulation? For example by voluntary self-regulation underpinned by consumer protection legislation and by greater public awareness, by accreditation of voluntary registration bodies, or by a statutory or voluntary licensing regime?
Voluntary self-regulation
Accreditation of voluntary bodies
Statutory or voluntary licensing
Unsure
I disagree with the premise, for reasons given in detail in separate documents. I believe that ‘orthodox statutory regulation’, if that means the Pittilo proposals, would increase, not decrease, the risk to the public. Strengthening the powers of Trading Standards, the MHRA and such consumer protection legislation would be far more effective in reducing risk to the public than the HPC could ever be. Greater public awareness of the weakness of the evidence for the efficacy of these treatments would obviously help too, but can’t do the job on its own.
Q10: What would you envisage would be the benefits to the public, to practitioners, and to businesses, for the alternatives to statutory regulation outlined at Question 8?
It depends on which alternative you are referring to. The major benefit of enforcement of existing laws by Trading Standards and/or the MHRA would be (a) to protect the public from risk, (b) to protect the public from health fraud and (c) almost certainly lower cost to the tax payer.
Q11: If you feel that not all three practitioner groups justify statutory regulation, which group(s) does/do not and please give your reasons why/why not?
Acupuncture
Herbal Medicine
TCM
Unsure
None of them. The differences are marginal. In the case of acupuncture there has been far more good research than for HM or TCM. But the result of that research is to show that in most cases the effects are likely to be no more than those expected of a rather theatrical placebo. Furthermore the extent to which acupuncture has a bigger effect than no-acupuncture in a NON-BLIND comparison, is usually too small and transient to offer any clinical advantage (so it doesn’t really matter whether the effect is placebo or not, it is too small to be useful).
In the case of HM, and even more of TCM, there is simply not enough research to give much idea of their usefulness, with a small handful of exceptions.
This leads to a conclusion that DH seems to have ignored in the past. It makes absolutely no sense to talk about “properly trained practitioners” without first deciding whether the treatments work or not. There can be no such thing as “proper training” in a discipline that offers no benefit over placebo. It is a major fault of the Pittilo recommendations that they (a) ignore this basic principle and (b) are very over-optimistic about the state of the evidence.
Q12: Would it be helpful to the public for these practitioners to be regulated in a way which differentiates them from the regulatory regime for mainstream professions publicly perceived as having an evidence base of clinical effectiveness? If so, why? If not, why not?
Yes
No
Unsure
It might indeed be useful if regulation pointed out the very thin evidence base for HM and TCM but it would look rather silly. The public would say how can it be that the DH is granting statutory regulation to things that don’t work?
Q13: Given the Government’s commitment to reducing the overall burden of unnecessary statutory regulation, can you suggest which areas of healthcare practice present sufficiently low risk so that they could be regulated in a different, less burdensome way or de-regulated, if a decision is made to statutorily regulate acupuncturists, herbalists and traditional Chinese medicine practitioners?
Yes
No
Unsure
As stated above, the.only form of regulation that is needed, and the only form that would protect the public, is through consumer protection regulations, most of which already exist (though they are enforced in a very inconsistent way). Most statutory regulation is objectionable, not on libertarian grounds, but because it doesn’t achieve the desired ends (and is expensive). In this case of folk medicine, like HM and TCM, the effect would be exactly the opposite of that desired as shown in separate documents that I have submitted to the consultation.
Q14: If there were to be statutory regulation, should the Health Professions Council (HPC) regulate all three professions? If not, which one(s) should the HPC not regulate?
Yes
No
Unsure
The HPC should regulate none of them. It has never before regulated any form of alternative medicine and it is ill-equipped to do so. Its statement that it doesn’t matter that there is very little evidence that the treatments work poses a danger to patients (as well as being contrary to its own rules).
Q15: If there were to be statutory regulation, should the Health Professions Council or the General Pharmaceutical Council/Pharmaceutical Society of Northern Ireland regulate herbal medicine and traditional Chinese medicine practitioners?
HPC
GPC/PSNI
Unsure
Neither. The GPC is unlikely to care about whether the treatments work any more than the RPSGB did, or the GCC does now. The problems would be exactly the same whichever body did it.
Q16: If neither, who should and why?
As I have said repeatedly, it should be left to Trading Standards, the MHRA and other consumer protection regulation.
Q17:
a) Should acupuncture be subject to a different form of regulation from that for herbalism and traditional Chinese medicine? If so, what?
Yes
No
Unsure
b) Can acupuncture be adequately regulated through local means, for example through Health and Safety legislation, Trading Standards legislation and Local Authority licensing?
Yes
No
Unsure
(a) No -all should be treated the same. Acupuncture is part of TCM
(b) Yes
Q18.
a) Should the titles acupuncturist, herbalist and [traditional] Chinese medicine practitioner be protected?
b) If your answer is no which ones do you consider should not be legally protected?
Yes
No
Unsure
No. It makes no sense to protect titles until such time as it has been shown that the practitioners can make a useful contribution to medicine (above placebo effect). That does not deny that placebos may be useful at times. but if that is all they are doing, the title should be ‘placebo practitioners’.
Q19: Should a new model of regulation be tested where it is the functions of acupuncture, herbal medicine and TCM that are protected, rather than the titles of acupuncturist, herbalist or Chinese medicine practitioner?
Yes
No
Unsure
No. This makes absolutely no sense when there is so little knowledge about what is meant by the ” functions of acupuncture, herbal medicine and TCM”.Insofar as they don’t work (better than placebo), there IS no function. Any attempt to define function when there is so little solid evidence (at least for HM and TCM) is doomed to failure.
Q20: If statutory professional self-regulation is progressed, with a model of protection of title, do you agree with the proposals for “grandparenting” set out in the Pittilo report?
Yes
No
Unsure
No. I believe the Pittilo report should be ignored entirely. The whole process needs to be thought out again in a more rational way.
Q22: Could practitioners demonstrate compliance with regulatory requirements and communicate effectively with regulators, the public and other healthcare professionals if they do not achieve the standard of English language competence normally required for UK registration? What additional costs would occur for both practitioners and regulatory authorities in this case?
Yes
No
Unsure
No. It is a serious problem, in TCM especially, that many High Street practitioners speak hardly any English at all. That adds severely to the already considerable risks. There would be no reliable way to convey what was expected of them. it would be absurd for the taxpayer to pay for them to learn English for the purposes of practising TCM (of course there might be the same case as for any other immigrant for teaching English on social grounds).
Q23: What would the impact be on the public, practitioners and businesses (financial and regulatory burden) if practitioners unable to achieve an English language IELTS score of 6.5 or above are unable to register in the UK?
Significant impact
Some impact
No impact
Unsure
The question is not relevant. The aim of regulation is to protect the public from risk (and it should be, but isn’t, an aim to protect them from health fraud). It is not the job of regulation to promote businesses
Q24: Are there any other matters you wish to draw to our attention?
I have submitted three documents via HRDListening@dh.gsi.gov.uk. The first of these puts the case against the form of regulation proposed by Pittilo, far more fluently than is possible in a questionnaire.
Another shows examples of what is actually taught in degrees in acupuncture, HM and TCM. They show very graphically the extent to which the Pittilo proposals would endanger the public, if they were to be implemented..
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
This post has been translated into Belorussian..
Chinese medicine and herbal medicine are in the news at the moment. There is a real risk that the government could endorse them by accepting the Pittilo report.
In my view traditional Chinese medicine endangers people. The proposed ‘regulation’ would do nothing to protect the public. Quite on the contrary, it would add to the dangers, by giving an official stamp of approval while doing nothing for safety.
The government’s idea of improving safety is to make sure that practitioners are ‘properly trained’. But it is the qualifications that cause the danger in the first place. The courses teach ideas that are plain wrong and often really dangerous.
Why have government (and some universities) not noticed this? That’s easy to see. Governments, quangos and university validation committees simply don’t look. They tick boxes but never ask what actually goes on. Here’s some examples of what goes on for them to think about. They show clearly the sort of dangerous rubbish that is taught on some of these ‘degrees’.
These particular slides are from the University of Westminster, but similar courses exist in only too many other places. Watch this space for more details on courses at Edinburgh Napier University, Middlesex University and the University of East London
Just a lot of old myths. Sheer gobbledygook,
SO much for a couple of centuries of physiology,
It gets worse.
Plain wrong.
Curious indeed. The fantasy gobbledygook gets worse.
Now it is getting utterly silly. Teaching students that the brain is made of marrow is not just absurd, but desperately dangerous for anyone unlucky (or stupid) enough to go to such a person when they are ill.
Here’s another herbal lecture., and this time the topic is serious. Cancer.
Herbal approaches for patients with cancer.
I’ve removed the name of the teacher to spare her the acute embarrassment of having these dangerous fantasies revealed. The fact that she probably believes them is not a sufficient excuse for endangering the public. There is certainly no excuse for the university allowing this stuff to be taught as part of a BSc (Hons).
First get them scared with some bad statistics.
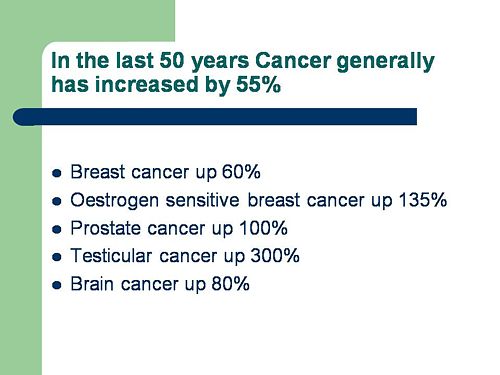
No fuss there about distinguishing incidence, age-standardisation and death rates. And no reference. Perhaps a reference to the simple explanation of statistics at Cancer Research UK might help? Perhaps this slide would have been better (from CDC). Seems there is some mistake in slide 2.
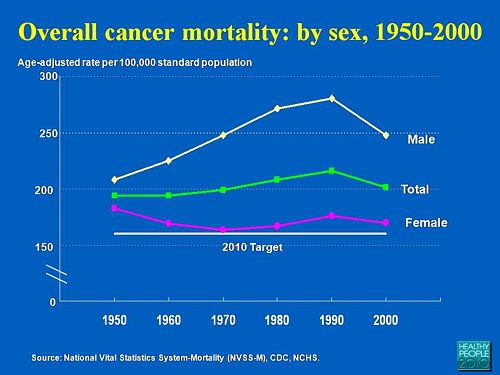
Straight on to a truly disgraceful statement in slide 3
The is outrageous and very possibly illegal under the Cancer Act (1939). It certainly poses a huge danger to patients. It is a direct incentive to make illegal, and untrue claims by using weasel words in an attempt to stay just on the right side of the law. But that, of course, is standard practice in alternative medicine,
Slide 11 is mostly meaningless. “Strengthen vitality” sounds good but means nothing. And “enhancing the immune system” is what alternative medicine folks always say when they can think of nothing else. Its meaning is ill-defined and there is no reason to think that any herbs do it.
The idea of a ‘tonic’ was actually quite common in real medicine in the 1950s. The term slowly vanished as it was realised that it was a figment of the imagination. In the fantasy world of alternative medicine, it lives on.
Detoxification, a marketing term not a medical one, has been extensively debunked quite recently. The use of the word by The Prince of Wales’ company, Duchy Originals recently fell foul of the Advertising Standards Authority, and his herbal ‘remedies’ were zapped by the MHRA (Medicines and Health Regulatory Authority).
And of course the antioxidant myth is a long-disproved hypothesis that has become a mere marketing term.
“Inhibits the recurrence of cancer”! That sounds terrific. But if it is so good why is it not even mentioned in the two main resources for information about herbs?
In the UK we have the National Library for Health Complementary and Alternative Medicine Specialist Library (NeLCAM), now a part of NHS Evidence. It was launched in 2006. The clinical lead was none other than Peter Fisher, clinical director of the Royal London Homeopathic Hospital, and the Queen’s homeopathic physician. The library was developed with the School of Integrated Health at the University of Westminster (where this particular slide was shown to undergraduates). Nobody could accuse these people of being hostile to magic medicine,
It seems odd, then, that NeLCAM does not seem to thnk to think that Centella asiatica, is even worth mentioning.
In the USA we have the National Center for Alternative and Complementary Medicine (NCCAM), an organisation that is so friendly to alternative medicine that it has spent a billion dollars on research in the area, though it has produced not a single good treatment for that vast expenditure. But NCCAM too does not even mention Centella asiatica in its herb list. It does get a mention in Cochrane reviews but only as a cosmetic cream and as an unproven treatment for poor venous circulation in the legs.
What on earth is a “lymph remedy”. Just another marketing term?
“especially valuable in the treatment of breast, throat and uterus cancer.“
That is a very dramatic claim. It as as though the hapless students were being tutored in doublespeak. What is meant by “especially valuable in the treatment of”? Clearly a desperate patient would interpret those words as meaning that there was at least a chance of a cure. That would be a wicked deception because there isn’t the slightest reason to think it works. Once again there this wondrous cure is not even mentioned in either NELCAM or NCCAM. Phytolacca is mentioned, as Pokeweed, in Wikipedia but no claims are mentioned even there. And it isn’t mentioned in Cochrane reviews either. The dramatic claims are utterly unfounded.
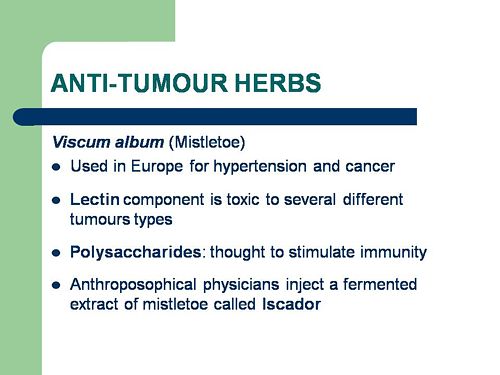
Ah the mistletoe story, again.
NHS Evidence (NeLCAM) lists three completed assessments. One concludes that more research is needed. Another concludes that “Rigorous trials of mistletoe extracts fail to demonstrate efficacy of this therapy”, and the third says “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
NCCAM says of mistletoe
- More than 30 human studies using mistletoe to treat cancer have been done since the early 1960s, but major weaknesses in many of these have raised doubts about their findings (see Question 6).
- Very few bad side effects have been reported from the use of mistletoe extract, though mistletoe plants and berries are poisonous to humans (see Question 7).
- The U.S. Food and Drug Administration (FDA) has not approved mistletoe as a treatment for cancer or any other medical condition (see Question 8).
- The FDA does not allow injectable mistletoe to be imported, sold, or used except for clinical research (see Question 8).
Cochrane reviews lists several reviews of mistletoe with similar conclusions. For example “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
Anthroposophy is one of the highest grades of fantasy you can find. A post on that topic is in the works.
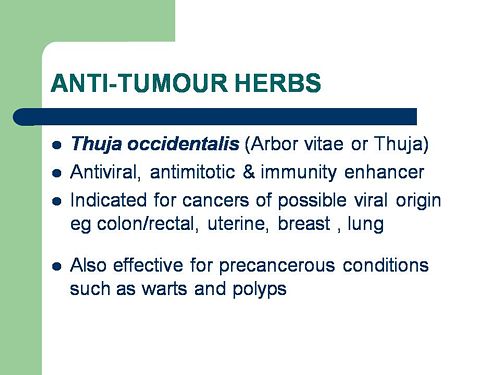
“Indicated for cancers . . . colon/rectal, uterine, breast, lung“. A cure for lung cancer? That, of course, depends on how you interpret the weasel words “indicated for”. Even Wikipedia makes no mention of any claims that Thuja benefits cancer. NHS Evidence (NeLCAM) doesn’t mention Thuja for any indication. Neither does NCCAM. Nor Cochrane reviews. That is not the impression the hapless students of this BSc lecture were given. In my view suggestions that you can cure lung cancer with this tree are just plain wicked.
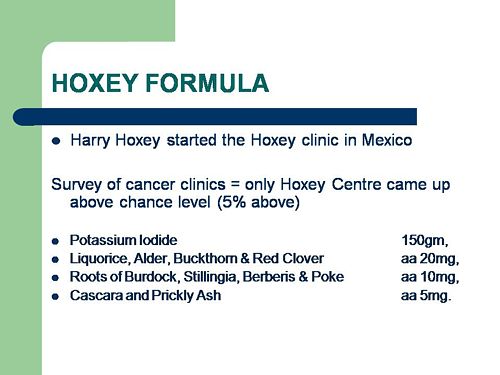
Pure snake oil, and not even spelled correctly, Harry Hoxsey’s treatment centres in the USA were closed by court order in the 1950s.
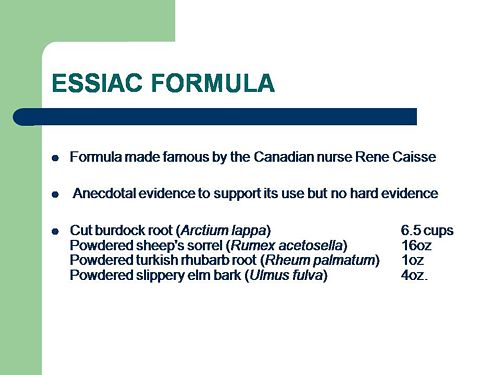
At least this time it is stated that there is no hard evidence to support this brand of snake oil.
More unfounded claims when it says “treated successfully many cancer patients”. No references and no data to support the claim. It is utterly unfounded and claims to the contrary endanger the public.
Gerson therapy is one of the most notorious and unpleasant of the quack cancer treatments. The Gerson Institute is on San Diego, but their clinics are in Mexico and Hungary. It is illegal in the USA. According to the American Cancer Society you get “a strict low-salt, low-fat, vegetarian diet and drinking juice from about twenty pounds of fresh fruits and vegetables each day. One glass of juice is consumed each hour, thirteen times a day. In addition, patients are given several coffee enemas each day. Various supplements, such as potassium, vitamin B12, pancreatic enzymes, thyroid hormone, and liver extracts, are used to stimulate organ function, particularly of the liver and thyroid.”. At one time you also got several glasses of raw calf liver every day but after infections killed several people] carrot juice was given instead.
Cancer Research UK says “there is no evidence to show that Gerson therapy works as a cure for cancer”, and “The Gerson diet can cause some very serious side effects.” Nobody (except perhaps the Price of Wales) has any belief in this unpleasant, toxic and expensive folk-lore.
Again patients are endangered by teaching this sort of stuff.
And finally, the usual swipe at vaccines. It’s nothing to do with herbalism. but just about every alternative medicine advocate seems to subscribe to the anti-vaccination lobby.. It is almost as though they have an active preference for things that are known to be wrong. They seem to believe that medicine and science are part of an enormous conspiracy to kill everyone.
Perhaps this dangerous propaganda might have been ameliorated if the students had been shown this slide (from a talk by Melinda Wharton).
Left to people like this, we would still have smallpox, diphtheria. tetanus and rabies, Take a look at Vaccine-preventable diseases.
This is the sort of ‘education’ which the Pittilo report wants to make compulsory.
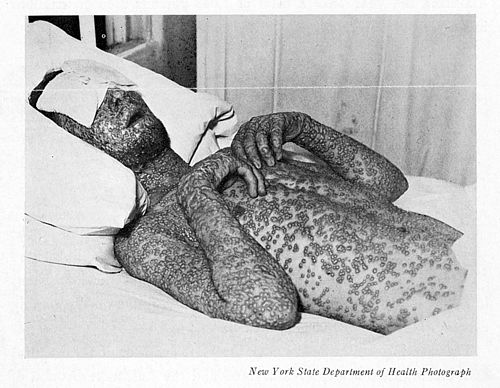
Smallpox in Baltimore, USA, 1939. This man was not vaccinated.
Conclusion
This selection of slides shows that much of the stuff taught in degrees in herbal medicine poses a real danger to public safety and to public health.
Pittilo’s idea that imposing this sort of miseducation will help safety is obviously and dangerously wrong. The Department of Health must reject the Pittilo recommendations on those grounds.
Follow-up
The much-delayed public consultation on the Pittilo report has just opened.
It is very important that as many people as possible respond to it. It’s easy to say that the consultation is sham. It will be if it is left only to acupuncturists and Chinese medicine people to respond to it. Please write to them before the closing date, November 2nd 2009. The way to send your evidence is here.
There is a questionnaire that you can complete, with the usual leading questions. Best do it anyway, but I’d suggest also sending written evidence as attachment too. I just got from DoH the email address where you can send it. They said
| if you have material you wish to send which you can’t easily “shoehorn” into the questionnaire, please send it to the following mailbox:
HRDListening@dh.gsi.gov.uk |
Here are three documents that I propose to submit in response to the consultation.I ‘d welcome criticisms that might make it more convincing. Use any parts of them you want in your own response.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
|
I’ve written quite a lot about the Pittilo report already, in particular A very bad report: gamma minus for the vice-chancellor, and in The Times (see also the blog version).
Intriguingly, these posts are at number 2 in a Google search for “Michael Pittilo”. |
 |
Briefly, the back story is this.
It is now over a year since the Report to Ministers from “The Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK” [download the report].
The chair of the steering group was Professor R. Michael Pittilo, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The reason thet the report is so disastrously bad in its assessment of evidence is that it was written entirely by people with vested interests.
The committee consisted of five acupuncturists, five herbalists and five representatives of traditional Chinese medicine (plus eleven observers). There was not a single scientist or statistician to help in the assessment of evidence. And it shows: The assessment of the evidence in the report was execrable. Every one of the committee members would have found themselves out of work if they had come to any conclusion other than that their treatment works, Disgracefully, these interests were not declared in the report, though they are not hard to find. The university of which the chair is vice-chancellor runs a course in homeopathy, the most discredited of the popular forms of alternative medicine. That tells you all you need to know about the critical faculties of Michael Pittilo.
The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register normally be through a Bachelor degree with Honours
Let’s consider the virtue of these two recommendations.
Regulation by the Health Professions Council (HPC) breaks their own rules
For a start, this should be ruled out by the HPC’s own rules, which require “Practise based on evidence of efficacy” as a condition for registration. Since there is practically no “evidence of efficacy”, it follows that the HPC can’t regulate acupuncture, herbal and Chinese medicine as Pittilo recommends. Or so you’d think. But the official mind seems to have an infinite capacity for doublespeak. The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
In other words, the HPC simply decided to ignore its own rules, Its excuse for doing so is that regulation would protect “public safety” . But it simply would not do that. It is ell known that some Chinese herbs are adulterated with dangerous substances, but laws against that already exist. Trading Standards are much more likely to take appropriate action than the HPC. The Medicines and Health Regulatory Authority (MHRA) already deals with the licensing of herbal medicines. and, despite the fact that it recently betrayed its trust by allowing them to be labelled in a misleading way, they are the people to do it, not the HPC.
The Pittilo report (page 11) says
In future, it is hoped that more Government funding can be allocated to research into traditional/herbal medicines and acupuncture and that grants will become available to encourage practitioners to undertake postgraduate research work.
So they are asking for more government money.
In March 2007, the Chinese Government pledged to spend over $130 million over the next five years on research into the effectiveness of traditional Chinese medicine. It is to be hoped that this money will be targeted effectively to evaluate TCM.
It seems to have escaped the notice of Pittilo that roughly 100 percent of trials of Chinese medicine done in China come out positive. Elsewhere, very few come out positive,(see Vickers et al., 1998, Controlled Clinical Trials, 19, 159-166: download reprint) The Department of Health would be unwise to rely on Chinese research. Remember that modern acupuncture was not so much a product of ancient wisdom, but rather it stems from nationalist propaganda by Mao Tse-Tung, who needed a cheap way to keep the peasants quiet, though he was too sensible to use it himself.
The HPC report (page 5) cites these with the words
” . . . a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base.”
This sentence seems to assume that the outcomes of research will be to strengthen the evidence base. Thus far, precisely the opposite has been the case. The Pittilo group has apparently not noticed that the US National Institutes of Health has already spent a billion dollars on research in alternative medicine and failed to come up with a single effective treatment. There are better ways to spend money on health. See, for example $2.5B Spent, No Alternative Med Cures found. .An enornous amount of research has already been done and the outcomes have produced no good treatments,
The proposed regulation would endanger the public, not protect it.
The excuse given by the HPC for breaking its own rules is that it should do so to protect the public.
Likewise Ann Keen, Health Minister, said:
“Patient safety is paramount, whether people are accessing orthodox health service treatments or using alternative treatments”
So first we need to identify what dangers are posed by acupuncture, herbal medicine and traditional Chinese medicine.
- Acupuncture is fairly safe. Its biggest danger lies in the unjustified claims that are routinely made for what can be achieved by being impaled by needles. This poses a danger that people may use acupuncture in place of treatments that work
- Herbal medicines are unstandardised, so even the very few that may work are dangerous to patients because the dose of active principle is unknown and varies from one batch to another. Taking a herbal medicine is a bit like swallowing a random number of tablets, False health claims pose a danger to patients too, when they cause patients to avoid treatments that work.
- Traditional Chinese Medicine is probably the most dangerous. Like the other two, the medicines are unstandardised so the dose is never known. False health claims abound. And in addition to these dangers, many cases have been found of Chinese medicines being adulterated with poisonous substances or with conventional drugs.
The form of regulation proposed by Pittilo would do little or nothing to protect the public from any of these dangers.
The proposals accept the herbal and Chinese medicine as traditionally practised. Nothing would be done about one of the major dangers, the lack of standardisation. That is a problem that was solved by pharmacologists in the 1930s, when international standards were set for the biological activity of things like tincture of digitalis, and assays were devised so that different batches could be adjusted to the same potency. Now, 80 years later, it is being proposed by Pittilo that we should return to the standards of safety that existed at the beginning of the last century. That is a threat to public safety., but the proposed regulation would do nothing whatsoever to protect the public from this dangerous practice. On the contrary, it would give official government sanction to it.
The other major danger is that patients are deceived by false health claims. This is dangerous (as well as dishonest) because it can cause patients to avoid treatments that work better, The internet abounds with claims that herbs can cure anything from diabetes to cancer. Many are doubtless illegal, but regulators like the HPC have traditionally ignored such claims: they are left to Trading Standards, Advertising Standards and the Medicines and Health Regulatory Authority (MHRA) to deal with. The MHRA already also has responsibility for monitoring side effects. The HPC would not do this.
The analogy with chiropractic and the GCC
The foolishness of allowing statutory regulation for unproven treatments has recently been illustrated quite dramatically by the case of chiropractic. Chiropractors have had statutory regulation by the General Chiropractic Council, which was established by the Chiropractors Act of 1994. The British Chiropractic Association (BCA) recently decided to sue the science writer, Simon Singh, for defamation when he cast doubt on some of the claims made by chiropractors, in particular their claims to be able to cure colic and asthma in children. That led to close examination of the claims. In fact there is no reason to think that spinal manipulation works for asthma, or that it works for colic. In fact there is quite good evidence that the claims are false. The result was that about 600 well-justified complaints have been lodged with the GCC (enough to bankrupt the GCC if the complaints are dealt with properly).
The point of this story is that the statutory regulator had nothing whatsoever to prevent these false health claims being made. Two of the complaints concern practices run by the chair of the GCC. Worse, the GCC actually endorsed such claims. The statutory regulator saw its duty to defend chiropractic (apart from a handful of cases of sexual misdemeanours), not to protect the patient from false health claims. The respectability conferred by statutory regulation made false health claims easier and endangered the public. It would be a disaster if the same mistake were made again.
On 11th December 2008 I got a letter form the HPC which said
in our opinion a lack of evidence of efficacy would not impede our ability to set standards or deal with complaints we receive. The vast majority of cases we consider are related to conduct.
But perhaps that is because they haven’t tried “regulating” quacks before. Now that the public is far more conscious about health fraud than it used to be, one can predict confidently that the HPC would be similarly overwhelmed by a deluge of complaints about the unjustified health claims made by acupuncturists, herbal medicine and traditional Chinese medicine practitioners. There is no shortage of them to complain about.
The education problem
The Pittilo report recommends that the entry level for registration should be a bachelors degree with honours. At first sight it seems reasonable to ask that practitioners should be ‘properly qualified’, but when one looks at what is actually taught on these degrees it becomes clear that they endanger, rather than protect, the public,
There are two very big problems with this recommendation.
Firstly, you can’t have a bachelors degree with honours until after you have decided whether or not there is anything useful to teach. If and when any of the subjects under consideration and shown to work to a useful extent, then it would be quite reasonable to establish degrees in them. Even the report does not pretend seriously that that stage has been reached. The proposal to set up degrees in subjects, at least some of which are quite likely to have no more than placebo value, is self-evidently nonsense,
The time for degrees, and the time for government endorsement by statutory regulation, is after the therapies have been shown to work, not before.
The absurdity of thinking that the public will be protected because a practitioner has a degree in, say, acupuncture, is shown with startling clarity by a recently revealed examination paper in acupuncture’
You can download the entire exam paper. Here are a few highlights from it.
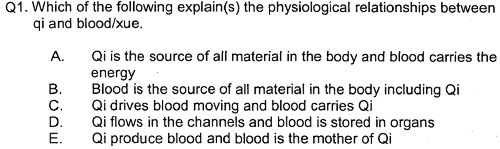
So students, in 2009, are being taught the crudest form of vitalism.
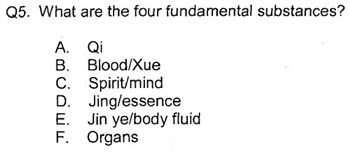
Teaching of traditional Chinese medicine is just as bad. Here are two slides from a course run by the University of Westminster.
The first ‘explains’ the mysterious and entirly mythical “Qi”.
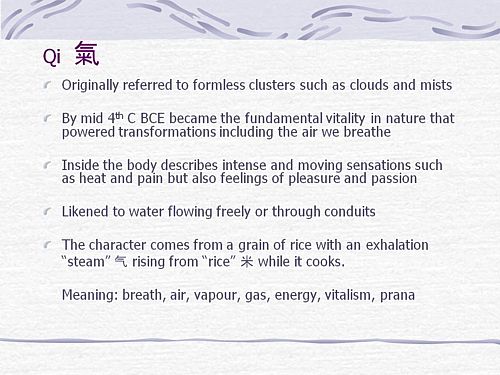
So “Qi” means breath, air, vapour, gas, energy, vitalism. This is meaningless nonsense.
The second slide shows the real dangers posed by the way Chinese medicine is taught, The symptoms listed at the top could easily be a clue to serious illness, yat students are taught to treat them with ginger. Degrees like this endanger the public.
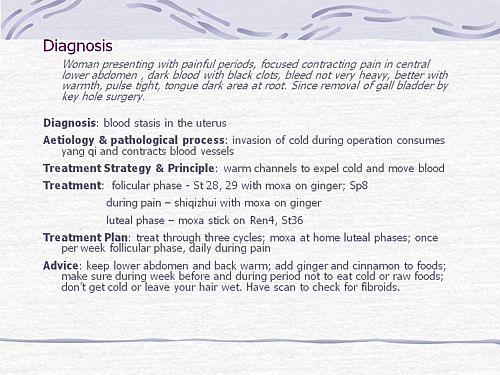
There are more mind-boggling slides from lectures on Chinese medicine and cancer: they show that what students are being taught is terrifyingly dangerous to patients.
It is entirely unacceptable that students are being taught these ancient myths as though they were true, and being encouraged to treat sick people on their basis. The effect of the Pittilo recommendations would be to force new generations of students to have this sort of thing forced on them. In fact the course for which this exam was set has already closed its doors. That is the right thing to do.
Here’s another example. The course leader for “BSc (Hons) Herbal Medicine” at the Univsrsity of Central Lancashire is Graeme Tobyn BA. But Tobyn is not only a herbalist but also an astrologer. In an interview he said
“At the end I asked her if I could cast her horoscope. She threw up her hands and said, ‘I knew this would happen if I came to an alternative practitioner.”
“I think the ruler of the ascendant was applying to Uranus in the ninth house, which was very pertinent.”
This would be preposterous even in the life style section of a downmarket women’s magazine, The Pittilo report wants to make degrees run my people like this compulsory. Luckily the Univerity of Central Lancashire is much more sensible and the course is being closed.
The matter is, in any case, being taken out of the hands of the government by the fact that universities are closing degrees in complementary medicine, including courses in some of those under discussion here, The University of Salford and the University of Central Lancashire have recently announced the closure of all the degree programmes in complementary and alternative medicine. The largest provider of such degrees, the University of Westminster has already shut down two of them, and the rest are being assessed at the moment. It is likely that the rest will be closed in the future.
The revelation that Westminster had been teaching its first year students that “amethysts emit high yin energy” and that students had been taught to diagnose disease and choose treatments by means of a dowsing pendulum, showed very clearly the sort of utter nonsense that undergraduates were being forced to learn to get a ‘bachelors degree with honours’. It stretches credulity to its limits to imagine that the public is protected by degrees like this. Precisely the opposite is true. The universities have recognised this, and shut the degrees. One exception is Professor Pittilo’s own university which continues to run a course in homeopathy, the most discredited of all the popular types alternative medicine.
A simpler, more effective and cheaper way to protect the public
I must certainly agree with the minister that protection of the public is an important matter. Having established that the Pittllo recommendations are more likely to endanger the public than protect them, it is essential to suggest alternative proposals that would work better.
Luckily, that is easy, because mechanisms already exist for dealing with the dangers that were listed above. The matter of adulteration, which is serious in traditional Chinese medicine, is a matter that is already the responsibility of the Office of Trading Standards. The major problem of false claims being made for treatment is also the responsibility of the Office of Trading Standards, which has a statutory duty to enforce the Unfair Trading Consumer Protection Regulations of May 2008. These laws state, for example, that
“One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”
The monitoring of false claims, and of side effects of treatments, is also the responsibility of the Medicines and Health Regulatory Authority (MHRA).
Rather than setting up complicated, expensive and ineffective ‘regulation’ by the HPC, all that need to be done is to ensure that the MHRA and/or Trading Standards have the funds to enforce existing laws. At the moment, they are not being implemented effectively, so I’d recommend that responsibility for enforcing the law against false health claims be transferred entirely to the MHRA, which has much more expertise in such matters than Trading Standards This would be both cheaper and more effective than the present system in which the responsibility is divided between the two organisations in an unclear way.
This proposal would protect the public against unsafe and adulterated treatments, and it would protect the public against false and fraudulent claims. That is what matters. It would do so more effectively,
more cheaply and more honestly than the Pittilo recommendations. There would be no reduction in patient choice either, There is no proposal to ban acupuncture, herbal medicine or traditional Chinese medicine. All that is necessary is to ensure that they don’t endanger the public.
Since the root of the problem lies in the fact that the evidence for the effectiveness is very weak. the question of efficacy, and cost-benefit ratio, should be referred to NICE. This was recommended by the House of Lords Report (2000). It is recommended again by the Smallwood report (sponsored by the Prince of Wales Foundation). It is baffling that this has not been done already. It does not seem wise to spend large amounts of money on new research at the moment, in the light of the fact that the US National Institutes of Health has already spent over $1 billion on such research without finding a single useful treatment.
The results of all this research has been to show that hardly any alternative treatment are effective. That cannot be ignored.
Conclusion
Recent events show that the halcyon days for alternative medicine are over. When the Pittilo report first appeared, it was greeted with derision in the media. For example, in The Times Alice Miles wrote
“This week came the publication of the Report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK. Otherwise known as twaddle.”
In the Independent, Dominic Lawson wrote
So now we will have degrees in quackery.
What, really, is the difference between acupuncture and psychic surgery?
People will no doubt continue to use it and that is their right and their responsibility. But if the government were to accept the recommendations of the Pittilo report it would be seen, quite rightly, as being anti-scientific and of posing a danger to the public.
Fortunately there is a better, and cheaper, way to protect the public.
Follow-up
Margaret McCartney’s blog in the Financial Times puts rhw view of a GP with her usual sense, humour and incisiveness.
“This report would, if implemented, create lots more nonsense exam papers funded by a lot more public money – and would produce practitioners without the absolutely crucial skill of how to assess evidence and reject or use it appropriately”
The Times has covered the story (with some interesting comments) Consultation on how to regulate complementary and alternative therapies
Times Higher Education UK-wide consultation on CAM regulation is launched Excellent response from Andy Lewis.
The Sun has by far the best coverage up to now, Jane Symons writes “Regulating quacks helps them prey on gullible patients“
Acupuncture has been in the news since, in a moment of madness, NICE gave it some credence,
Some people still seem to think that acupuncture is somehow more respectable than, say, homeopathy and crystal healing. If you think that, read Barker Bausell’s book ot Trick or Treatment. It is now absolutely clear that ‘real’ acupuncture is indistinguishable from sham, whether the sham control uses retractable needles, or real needles in the ‘wrong’ places. There has been no clear demonstration of long-lived benefits in any condition, and it is likely that it is no more than a theatrical placebo.
In particular, the indistinguishability of ‘real’ and sham acupuncture shows, beyond reasonable doubt that all the stuff about “energy flow in meridians” is so much hokum.
There is a small group of ‘medical acupuncturists‘ that believes that it is hokum. but who nonetheless maintain that acupuncture works, despite the evidence to the contrary. But most acupuncturists go for the wholesale gobbledygook.
If you don’t believe that, take a look at the exam paper that has come into my possession. It is this year’s exam from the University of Salford. Salford has, very sensibly, now decided to stop all its degrees in alternative medicine, so don’t hold this against the university too much.
You can download the entire exam paper. Here are a few highlights.
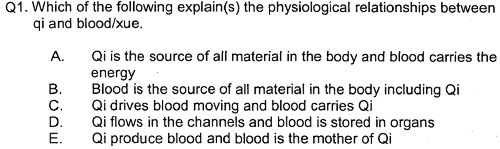
So students, in 2009, are being taught the crudest form of vitalism.
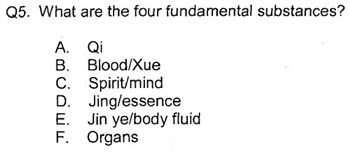
Oh really. Perhaps protons neutrons and electrons?
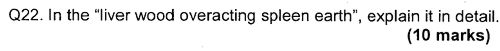
OK I’d fail that one because the words have no obvious meaning at all.
Perhaps an elementary textbook of embryology would help?
How one would love to see a set of model answers for these questions.
All this is ancient hokum being taugh to hapless students in the 21st century as though it were fact. The University of Salford has understood that and closed the course. All we need now is for NICE and the Department of Health to understand what it is that they are promoting.
NICE neglected the cultural cost of their guidance
When National Institute for Health and Clinical Excellence (NICE) included an acupuncture option on their low back pain guidance, they quite forget that one effect of their decision would be to ensure that new generations of students would have their minds poisoned with intellectual junk like this. That is why NICE really must think again. . See also
NICE falls for bait and switch by acupuncturists and chiropractors
NICE fiasco part 2 Rawlins should withdraw guidance and start again
NICE fiasco Part 3. Too many vested interests, not enough honesty
Pittilo and statutory regulation
Public consultation is due to open shortly on the appalling report of the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK (see also, The Times)
One of the recommendations is that acupuncture and Chinese herbal medicine should have statutory regulation by the Health Professions Council (HPC), despite the fact that that would involve the HPC breaking its own rules. Another recommendation of Pittilo is that entry to the “profession” (his word, not mine) should be by means of honours degree only. So he wants to impose on students exams like this one in order to “protect the public”? The absurdity of that proposal should be obvious now. This exam paper will form part of my evidence to the consultation.
And there is one other small problem. Universities are busy shutting down their degrees in alternative medicine, now that the ridiculousness of what is taught has been exposed. They have shut down entirely at the University of Salford and at the University of Central Lancashire, And even the University of Westminster is working on closing them.
All we need now is for the common sense and integrity that has been shown by these universities to spread to the Department of Health (and NICE).
Follow-up
|
.The University of Central Lancashire (UCLAN) is the first place I asked to see teaching materials that were used on its homeopathy “BSc” course. The request was refused, and subsequent internal appeals were refused too, Clearly UCLAN had something to hide. |

|
An appeal to the information commissioner took almost two years to be judged, but the case was won. The eventual decision by the Information
Commissioner rejected all the grounds that UClan had used to evade the Freedom of Information Act.
UClan appealed against the judgement and I still haven’t got the stuff but that hardly matters now, because the course in question shut its doors. In any case, plenty of stuff from similar courses has leaked out already.
Meanwhile, in September 2008, UCLAN announced an internal review of all its courses in magic medicine, The review seemed to be genuine. For a start they asked me to give evidence to the review (something that no other university has done). They also asked Michael Eslea to give evidence. He is the UCLAN psychologist, whose magnificent open letter probably tipped the authorities into holding the review.
Just in case it is useful to anyone, here is a copy of the written evidence that I sent [download pdf],
|
Report of the Working Party on the Review of issues associated with Homeopathy, Acupuncture and Chinese Herbal Medicine
1. Introduction As a consequence of concerns expressed by some colleagues within the University of Central Lancashire (UCLan) Dr Malcolm McVicar, Vice Chancellor appointed a working party to review the issues associated with the University offering courses in Homeopathy, Acupuncture and Chinese Herbal Medicine. MEMBERSHIP: Eileen Martin (Chair) Pro-Vice Chancellor and Dean of Faculty of Health and Social Care |
The report was the subject of a special meeting of UCLAN’s Academic Board on 9th July 2009. The following resolutions were passed.
|
Resolutions R1 That further minor revisions be made to the report prior to publication on the University’s website; R2 That the University refrain from offering any practitioner-qualifying courses in Homeopathy, Acupuncture and Chinese Herbal Medicine until such disciplines have achieved statutory regulation status; R3 That the University consider offering a limited number of postgraduate research studentships (leading to Masters by Research of PhD) to suitably qualified UCLan students and staff in these disciplines. They should have interdisciplinary supervisory teams to facilitate development of a broad range of research skills and to contribute to the generation of knowledge in CAM; R4 That the University consider how more interdisciplinary teaching can be achieved, where appropriate, within both undergraduate and postgraduate teaching to facilitate greater exposure to subject expertise and different paradigms. |
Resolutions 1, 3 and 4 say very little. Resolution 4 sounds thoroughly relativist. We are talking about medicine, about treating sick patients. There is only one “paradigm”. That is to find treatments that are as effective and safe as possible. There aren’t two sorts of medicine, regular and alternative. There is just medicine that works and medicine that doesn’t work. It’s a good illustration of DC’s rule number 2, “never trust anyone who uses the word paradigm”.
Resolution 2 is the really interesting one, because none if the topics, Homeopathy, Acupuncture and Chinese Herbal Medicine, is subject to statutory regulation.
If taken literally, resolution 2 means that all the UCLan courses in alternative medicine will close their doors. Bafflingly, this inevitable conclusion is not stated explicitly.
At least resolution 2 means that homeopathy, already closed, will stay closed. It is never likely to get statutory regulation.
For practical purposes, we can ignore for the moment the obvious fact that statutory regulation of nonsense subjects results only in nonsense. The only forms of alternative medicine that have got “statutory regulation” at the moment are chiropractic and osteopathy. The public has not been safeguarded by the General Chiropractic Council (GCC). The GCC, on the contrary, has endangered the public by allowing false health claims to be made with impunity. Perhaps the members of the review committee had not noticed that the Simon SIngh affair has resulted in almost 600 complaints being made to the GCC? The faith of the review in statutory regulation is clearly misplaced.
The Pittilo report is critical for what happens next
Acupuncture and Chinese Herbal Medicine are not subject to statutory regulation at present, so one would suppose that these degrees will close their doors too. However the infamous Pittilo report has proposed that they should become regulated by the Health Professions Council (HPC). The many problems of the Pittilo report have been documented here, in “A very bad report: gamma minus for the vice-chancellor“. There was also a high-profile critique of the report in The Times (and on this blog).
The HPC has, as one of its criteria for regulation, “evidence-based practice”. Disgracefully, the HPC has already shown its willingness to ignore its own rules and to act as statutory regulator for Acupuncture and Chinese Herbal medicine. This rather disgraceful behaviour is documented in “Health Professions Council ignores its own rules: the result is nonsense“.
The UCLAN report seems to assume that the recommendations of the Pittilo report will be accepted. But the long-awaited consultation has still not opened. We can be sure that when it does, the opposition to it will be very strong indeed.
The report in full
Here are a few comments on the report itself. Download the full report (as of July 15th).
i have to say that when I visited Preston to give evidence, my views seem to be treated seriously, even sympathetically, so it was a great disappointment to see the outcome. So what’s wrong? The major disaster is declared early in the report.
Section 2, Context
The debate is centred on a number of key themes which relate to:-
1. The quality of and/or absence of an evidence base to support claims of the efficacy and benefits of such treatments, linked to issues of public safety/protection and professional regulation.
Sounds good. What matters about any sort of medicine is whether or not it works and whether it is safe. It therefore verges on the incredible that we read in section 4.1
“conclusions from research into the efficacy of the various CAM’s are outside the remit of this report.”
The whole point about CAM is that there is very little evidence that any of it works. So the review committee decided to ignore the most important problem of the lot. I can’t see how any rational decision can be made without first deciding whether the treatment is better than placebo. That, surely, is the main question, and it was dodged.
UCLAN has failed to grasp the nettle, just as the Department of Health has also consistently failed to do so.
Section 4,1 Efficacy This section repeats the assertion, absurd to my mind, that it is possible to judge CAM courses while declining to assess whether they work or not.
Section 4.2 Role of Universities in Society.
There is universal agreement that critical thinking is crucial to the idea of a university, but the judgement of whether CAM teaches critical thinking is simply fudged. Again the report fails to grasp the nettle.
“Disagreements about critical thinking within CAMs arises because some will argue that such substantiation and assessment can occur within the discipline, whilst others will argue that the methodology for substantiation, that is evidence provision, is universal. As a result, the latter will demand that evidence is provided using methods from one field (e.g. randomised controlled trials) for use in another.”
Sadly, the report dodged the crucial judgement once again. The most obvious characteristic of every form of alternative medicine is their total lack of critical self-appraisal. It is very sad that the review committee could not bring itself to say so.
Section 4.4 Nomenclature of degrees
Recommendation
The nomenclature of courses, leading to a professional as well as an academic award, should reflect the professional route; for example Bachelor with Honours in Complementary Medicine, B Comp. Med.(Hons) or B Acupuncture (Hons).
This sounds to me like another truly pathetic fudge. What on earth is solved by changing the name of the degree? You’d still be teaching students the same load of gobbledygook and then letting them loose on sick people, whether you call it a Bachelor of Science, a Bachelor of Arts, or, as is recommended here, a Bachelor of nothing whatsoever.
Well, I suppose there is a (doubtless unintended) irony in calling CAM degrees “Bachelor of nothing whatsoever”.
Section 4.4 Ethical, non-harm and economic considerations
This section list a lot of reasons why teaching alternative medicine should be unethical. but nevertheless manages to conclude that
” . . . it is not unethical to offer courses in Homeopathy, Acupuncture and Chinese Herbal Medicine at a university.”
I find the logic by which this bizarre conclusion was reached quite impossible to follow. Like much of the rest of the report this conclusion seems to stem from a reluctance to grapple with the really important questions, like ‘does it work or not?’.
Despite this the recommendation is perhaps the most interesting of all.
“Recommendation
• The University refrains from offering any CAM courses until such disciplines have achieved statutory regulation status.”
This recommendation was accepted, and passed as a resolution at Academic Board. If it is implemented now, than there will be no more alternative medicine degrees next year at the University of Central Lancashire. If and when this happens, the University must be congratulated on its return to rational medicine.
Follow-up
Michael Eslea, UCLAN’s hero in resisting nonsense from the inside, has posted on this topic.
17 July 2009. It seemed odd that that no announcement was made about the future if the remaining CAM courses at UCLAN. So I asked deputy Vice-Chancellor Patrick McGhee for clarification. After a couple of days, I got this response.
|
From: CTheobald@uclan.ac.uk To: d.colquhoun@ucl.ac.uk Hi David, I have been asked to respond to your question below on the running of acupuncture and Chinese herbal medicine at UCLan. It is correct to assume that UCLan will not be taking any new entrants onto these programmes until further notice. Best Wishes Chris Chris Theobald |
So the report may have been disappointing, but it has done the job. As several people have pointed out in comments, it would be asking too much to expect a university to say “sorry we just noticed that we have been running junk-science courses for years”. But they have done the right thing anyway.
This is a follow-up of the poat on BBC2 and the Open University on Alternative Medicine.
Following the article by Simon Singh in the Guardian (25 March 2006), two letters appeared on April 1, 2006. The first, from Prof. Edzard Ernst, confirmed that he felt the BBC had ignored and misrepresented his advice.
|
In its response to our criticism of the Alternative Medicine series, the BBC says “it is extremely unusual that Professor Ernst should make these comments so long after the series was aired” (Report, March 25). I made my criticism in writing two months before the programme was broadcast. The reason why I reiterated them when I did was simply because Simon Singh interviewed me in my capacity as adviser to the BBC. Extremely unusual? Long after? I don’t think so.
Prof Edzard Ernst Peninsula Medical School, Exeter |
The second letter defended the BBC. It was unequivocal in its support of the entire series of programmes, and its appearence surprised me. In the light of all that has been written, one might have hoped that the BBC would listen and learn from its mistakes. The letter has ten signatories.
|
We are all scientists involved as consultants or contributors to the BBC2 series, Alternative Medicine. We do not in any way recognise the experience of working on the series as described in your article (Was this proof of acupuncture’s power … or a sensationalised TV stunt?, Science, March 25), nor do we share the views of those scientists you have quoted in it. In all its dealings with us, the BBC asked for advice and input where needed, took on board our feedback and incorporated our comments into the final edit of the programme as transmitted, where appropriate. Far from feeling dissatisfied with the final outcome, we feel the series seemed well balanced and informative, doing full justice to the subject matter it addressed. Dr Jack Tinker Prof Brian Berman Prof Liz Williamson Dr Andrew Vickers Dr James Warner Dr Mike Cummings Prof Gary Green Dr Carl Albrecht Dr Jen Cleland Professor Irving Kirsch |
But all is not what it seems. Contrary to appearances, this letter was actually written by the BBC who also compiled the signatories (it seems to have been the responsibility of Kim Creed, of BBC Factual Publicity).
- One of the signatories. Dr James Warner, had never seen the letter until after it was published, and tells me that “[I] substantially do not agree with the sentiments expressed therein. Indeed, we had to resist attempts by the programme makers to sensationalise our work”.
The Guardian has published a correction. - Six other signatories tell me that their approval was limited to the way their own contribution was treated, and was not intended as approval of the whole series. One commented ” I’ve obviously been naïve, and I am very fed up with this whole thing”. Another says ” I suppose I (foolishly by the sounds of things) extrapolated from my own programme and experience, without considering the wider implications of the concluding sentence”.
- Only one of the eight signatories whom I’ve asked has actually seen all three programmes, as they were transmitted. This makes it rather odd that they should appear to endorse so unequivocally the whole series.
- One of the signatories, Carl Albrecht, gives his address as “University of Johannesburg”, but oddly the BBC forgot to mention that Dr Albrecht is co-owner (at least until very recently) of the South African Company, Phyto Nova, that makes, promotes and sells the untested herb, Sutherlandia, for treatment of AIDS (see, for example, here).
He is, therefore, highly biassed. He is also exceedingly controversial. One of his strongest critics has been Stuart Thomson, Director of the Gaia Research Institute,
hardly an organisation that is biassed against “natural medicines”. Albrecht is indeed a very curious choice of advisor for a programme about science. - Three of the signatories (Berman, Cummings and Albrecht) are heavily committed to CAM, and so unlikely to be critical of anything that favours it, even apart from financial interests in the outcome. Brian Berman even has is own an entry in Quackwatch. So several of the signatories are pretty much committed in advance. Asking them if they endorse the programmes is about as informative as asking a group of priests if the endorse god.
- It gets worse. This morning, 6th April, I heard from Andrew Vickers, of the Memorial Sloan-Kettering Cancer Center, New York. This is what he says.
“I didn’t sign this letter ”
“I was shown the text of the letter but didn’t fully agree with it and told them so. I said something along the lines that the series didn’t do ‘full justice to the subject matter’ (how could it possibly?) but that what they did was fair and reasonable within the constraints set by the medium. You are also right to point out that my comments only go so far as the acupuncture episodes (which I saw) rather than the other two shows (which I did not). No doubt had I been shown a final version for signature I would have also pointed this out.”
The BBC brought us superb programmes like Life on Earth and Planet Earth. They bring us superb news (I’m listening to the incomparable John Humphrys on the Today Programme right now). They have suffered unjustly at the hands of spin-meisters like Alastair Campbell and the execrable Hutton Report (If the Hutton Report had been an undergraduate essay, it would have scored alpha-plus for collection of evidence and gamma-minus for ability to connect evidence to conclusions).
How ironic it is, then, to see the BBC behaving in this case like spin artists. Deny everything, and, if necessary, falsify the evidence.

 >
>