Michael Driscoll
It makes a nice change to be able to compliment an official government report.
|
Ever since the House of Lords report in 2000, the government has been vacillating about what should be done about herbalists. At the moment both western herbalists and traditional Chinese medicine (TCM) are essentially unregulated. Many (but not all) herbalists have been pushing for statutory regulation, which they see as government endorsement. It would give them a status like the General Medical Council. |
|
A new report has ruled out this possibility, for very good reasons [download local copy].
Back story (abridged!)
My involvement began with the publication in 2008 of a report on the Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine . That led to my post, A very bad report: gamma minus for the vice-chancellor. The report was chaired by the late Professor Michael Pittilo BSc PhD CBiol FIBiol FIBMS FRSH FLS FRSA, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The membership of the group consisted entirely of quacks and the vice -chancellor’s university ran a course in homeopathy (now closed).
The Pittilo report recommended statutory regulation and "The threshold entry route to the register will normally be through a Bachelor degree with Honours". It ignored entirely the little problem that you can’t run a BSc degree in a subject that’s almost entirely devoid of evidence. It said, for example that acupuncturists must understand " yin/yang, 5 elements/phases, eight principles, cyclical rhythms, qi ,blood and body fluids". But of course there is nothing to "understand"! They are all pre-scientific myths. This “training dilemma” was pointed out in one of my earliest posts, You’d think it was obvious, but nonetheless the then Labour government seemed to take this absurd report seriously.
In 2009 a consultation was held on the Pittilo report. I and many of my friends spent a lot of time pointing out the obvious. Eventually the problem was again kicked into the long grass.
The THR scheme
Meanwhile European regulations caused the creation of the Traditional Herbal Registration (THR) scheme. It’s run by the Medicines and Healthcare products Regulatory Authority (MHRA). This makes it legal to put totally misleading claims on labels of herbal concoctions, as long as they are registered with THR, They also get an impressive-looking certification mark. All that’s needed to get THR registration is that the ‘medicines’ are not obviously toxic and they have been in use for 30 years. There is no need to supply any information whatsoever about whether they work or not. This appears to contradict directly the MHRA’s brief:
"”We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
After much effort, I elicited an admission from the MHRA that there was no reason to think that any herbal concoctions were effective, and that there was nothing to prevent them from adding a statement to say so on the label. They just chose not to do so. That’s totally irresponsible in my opinion. See Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. Over 300 herbal products have been registered under the THR scheme (a small percentage of the number of products being used). So far only one product of Tibetan medicine and one traditional Chinese medicine have been registered under THR. These are the only ones that can be sold legally now, because no herbs whatsoever have achieved full marketing authorisation -that requires good evidence of efficacy and that doesn’t exist for any herb.
The current report
Eventually, in early 2014, the Tory-led government set up yet another body, "Herbal Medicines and Practitioners Working Group " (HMPWG). My heart sank when I saw its membership (Annex A.2). The vice-chair was none other that the notorious David Tredinnick MP (Con, Bosworth). It was stuffed with people who had vested interests. I wrote to the chair and to the few members with scientific credentials to put my views to them.
But my fears were unfounded, because the report of the HMPWG was not written by the group, but by its chair only. David Walker is deputy chief medical officer and he had clearly listened. Here are some quotations.
The good thing about the European laws is that
"This legislation effectively banned the importation and sale of large-scale manufactured herbal medicine products. This step severely limited the scope of some herbal practitioners to continue practising, particularly those from the Traditional Chinese Medicine (TCM) and Ayurvedic traditions."
The biggest loophole is that
"At present under UK law it is permitted for a herbal practitioner to see individual patients, offer diagnoses and prepare herbal treatments on their own premises, as long as these preparations do not contain banned or restricted substances. This is unchanged by the Traditional Herbal Medicinal Products Directive. "
Walker recognised frankly that there is essentially no good evidence that any herb, western or Chinese, works well enough to make an acceptable treatment. And importantly he, unlike Pittilo, realised that this precludes statutory regulation.
"There are a small number of studies indicating benefit from herbal medicine in a limited range of conditions but the majority of herbal medicine practice is not supported by good quality evidence. A great deal of international, primary research is of poor quality. "
"ts. Herbal medicine practice is therefore currently based upon traditional practice rather than science. It is difficult to differentiate good practice from poor practice on the basis of this evidence in a way that could establish standards for statutory regulation"
The second problem was the harms done by herbs. Herbalists, western and Chinese, have no satisfactory way of reporting side effects
" . . . there is very limited understanding of the risks to patient safety from herbal medicines and herbal practice. A review of safety data was commissioned from HMAC as part of this review. This review identified many anecdotal reports and case studies but little systematically collected data. Most herbal medicine products have not been through the rigorous licensing process that is required of conventional pharmaceutical products to establish their safety and efficacy. Indeed, only a small proportion have even been subject to the less rigorous Traditional Herbal Registration (THR) process. "
"The anecdotal evidence of risk to patients from herbal products in the safety review highlighted the prominence of manufactured herbal medicines in the high profile serious incidents which have been reported in recent years. Many of these reports relate to harm thought to be caused by industrially manufactured herbal products which contained either dangerous herbs, the wrong constituents, toxic contaminants or adulterants. All such industrially manufactured products are now only available under European regulations if their safety is assured through MHRA licensing or THR
accreditation; and specific dangerous herbs have been banned under UK law. This has weakened the case for introduction of statutory regulation as a further safety measure. "
Then Walker identified correctly the training dilemma. Although it seems obvious, this is a big advance for a government document. Degrees that teach nonsense are not good training: they are miseducation.
"The third issue is the identification of educational standards for training practitioners and the benchmarking of standards for accrediting practitioners. With no good data on efficacy or safety, it is difficult for practitioners and patients to understand or quantify the potential benefits and risks of a proposed therapeutic intervention. Training programmes could accredit knowledge and skills in some areas including pharmacology and physiology, professional ethics and infection control but without a credible evidence base relating to the safety and effectiveness of herbal medicine it is hard to see how they could form the basis of accreditation in this field of practice.
There are a number of educational university programmes offering courses in herbal medicine although the number has declined in recent years. Some of these courses are accredited by practitioner organisations which is a potential governance risk as the accreditation may be based on benchmarks established by tradition and custom rather than science.
"
"The herbal medicine sector is in a dilemma" is Walker’s conclusion.
"Some practitioners would like to continue to practise as
they do now, with no further regulation, and accept that their practice is based on tradition and personal experience rather than empirical science. The logical consequence of adopting this form of practice is that we should take a precautionary approach in order to ensure public safety. The public should be protected through consumer legislation to prevent false claims, restricting the use of herbal products which are known to be hazardous to health"
The problem with this is, if course, is that although there is plenty of law, it’s rarely enforced : see Most alternative medicine is illegal Trading Standards very rarely enforce the Consumer Protection Regulations (2008) but Walker is too diplomatic to mention that fact.
"The herbals sector must recognise that its overall approach (including the rationale for use of products and methods of treatment, education and training, and interaction with the NHS) needs to be more science and evidence based if in order to be established as a profession on the same basis as other groups that are statutorily regulated."
So what happens next?
In the short term nothing will happen.
The main mistake has been avoided: there wil be no statutory regulation.
The other options are (a) do nothing, or (b) go for accreditation of a voluntary register (AR) by the Professional Standards Authority for Health and Social Care (PSA). Walker ends up recommending the latter, but only after a lot more work (see pages 28-29 of report). Of particular interest is recommendation 5.
"As a first step it would be helpful for the sector organisations to develop an umbrella voluntary register that could support the development of standards and begin to collaborate on the collection of safety data and the establishment of an academic infrastructure to develop training and research. This voluntary register could in due course seek accreditation from the Professional Standards Authority for Health and Social Care (PSA)."
So it looks as though nothing will happen for a long time, and herbalists and TCM may end up with the utterly ineffectual PSA. After all, the PSA have accredited voluntary registers of homeopaths, so clearly nothing is too delusional for them. It’s very obvious that, unlike Walker, the PSA are quite happy to ignore the training dilemma.
Omissions from the report
Good though this report is, by Department of Health standards, it omits some important points.
Endangered species and animal cruelty aren’t mentioned in the report. Traditional Chinese medicine, and its variants, are responsible for the near-extinction of rhinoceros, tiger and other species because of the superstitious belief that they have medicinal value. It’s not uncommon to find animal parts in Chinese medicines sold in the UK despite it being illegal
And the unspeakably cruel practice of farming bears to collect bile is a direct consequence of TCM.

A bile bear in a “crush cage” on Huizhou Farm, China (Wikipedia)
Statutory regulation of Chiropractors
The same arguments used in Walker’s report to deny statutory regulation of herbalism, would undoubtedly lead to denial of statutory regulation of chiropractors. The General Chiropractic Council was established in 1994, and has a status that’s the same as the General Medical Council. That was a bad mistake. The GCC has not protected the public, in fact it has acted as an advertising agency for chiropractic quackery.
Perhaps Prof. Walker should be asked to review the matter.
Follow-up
You can also read minutes of the HMPWG meetings (and here). But, as usual, all the interesting controversies have been sanitised.
Edzard Ernst has also commented on this topic: Once again: the regulation of nonsense will generate nonsense – the case of UK herbalists.
Since writing about anti-scientific degrees in Nature (March 2007), much has been revealed about the nonsense that is taught on these degrees. New Year’s day seems like a good time to assess how far we’ve got, five years on.
At the beginning of 2007 UCAS (the universities central admission service) offered 45 different BSc degrees in quackery, at 16 universities.
Now there are only 24 such degrees.
If you exclude chiropractic and osteopathy, which all run at private colleges, with some sort of "validation" from a university, there are now only 18 BSc/MSc courses being offered in eight universities.
Degrees in homeopathy, naturopathy and "nutritional therapy", reflexology and aromatherapy have vanished altogether from UCAS.
In the race to provide BScs in anti-science, Middlesex University has now overhauled the long-standing leader, Westminster, by a short head.
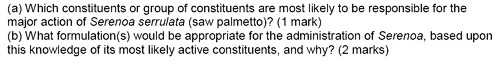
 Michael Driscoll, vice-chancellor of Middlesex |
|
Let’s see what’s gone.
The University of Central Lancashire (UCLAN) was the first to see sense. In August 2008 they announced closure of their “BSc” degree in homeopathy. On September 2008 they announced an internal review of their courses in homeopathy. herbalism and acupuncture. The report of this review closed down all of them in July 2009. I first asked for their teaching materials in July 2006. I finally got them in December 2010, after winning an appeal to the Information Commissioner, and then winning an appeal against that decision at an Information tribunal . By the time I got them, the course had been closed for over two years. That is just as well, because it turned out that UCLAN’s students were being taught dangerous nonsense. No wonder they tried so hard to conceal it.
Salford University was the next to go. They shut down their courses in complementary medicine, homeopathy and acupuncture. In January 2009 they announced " they are no longer considered “a sound academic fit” ". Shortly afterwards. a letter appeared in The Times from three heavyweights (plus me) congratulating the vice-chancellor on his decision.
University of Westminster
For many years, Westminster was the biggest supplier of BSc degrees in quackery. At the beginning of 2007 they offered 14 different BSc degrees in homeopathy, naturopathy, nutritional therapy, "complementary therapies", (western) herbal medicine and traditional Chinese medicine with acupuncture. Some of their courses were so bizarre that some of the students and even staff sent me slides which taught things like "amethysts emit high Yin energy". Like UCLAN, Westminster also held an internal review. Unlike UCLAN it came to the absurd conclusion that all would be well if they injected more science into the courses. The incompetence of the review meant that those who wrote it hadn’t noticed that if you try to put science into homeopathy or naturopathy, the whole subject vanishes in a puff of smoke. Nevertheless Westminster closed down entry to BSc homeopathy in March 2009 (though the subject remained as part of other courses).
Three years after the Nature article, all five BSc homeopathy degrees had shut their doors.
During 2011, Westminster shut down Naturopathy, Nutritional therapy, Therapeutic bodywork and Complementary Medicine. See, for example,
More dangerous nonsense from the University of Westminster: when will Professor Geoffrey Petts do something about it?
Now Westminster has only four courses in two subjects. They still teach some dangerous and untrue things, but I suspect the writing is on the wall for these too.
I have seen a document, dated 11 April 2011, which states
“The following courses have been identified as ‘at risk’ (School definition) and will be discussed at the APRG and University Review Group2, due to poor recruitment and high cost of delivery:
Integrated Health Scheme: BSc Complementary Medicine, Naturopathy; BSc Chinese Medicine; BSc Nutritional Therapy; BSc Herbal Medicine”
All but Chinese medicine and Herbal medicine have already gone. Almost there.
University of Wales
Since my first post in 2008 about the validation scam operated by the University of Wales, and some good investigations by BBC Wales TV, the outcome was the most spectacular so far. The entire institution collapsed. They no longer "validate" external degrees at dodgy business colleges, loony religious colleges or magic medicine colleges.
Another worthless validation: the University of Wales and nutritional therapy (October 2008) This is a ‘degree’ in nutrtional therapy. It is even more hilarious than usual, but it passed the validation anyway.
Scandal of the University of Wales and the Quality Assurance Agency (November 2010). This post followed the BBC Wales TV programme. At last the QAA began to notice, yet further confirmation of its utter ineptitude.
The University of Wales disgraced (but its vice chancellor is promoted) (October, 2011) The eventual collapse of the university was well-deserved. But it is very weird that the people who were responsible for it have still got their jobs. In fact the vice-chancellor, Marc Clement, was promoted despite his mendacious claim to be unaware of what was going on.
It remains to be seen how many of the many quack courses that were validated by the University of Wales will be taken on by other universities. The McTimoney College of Chiropractic is owned by BPP University (so much for their quality control, as explained in Private Eye). but still claims to be validated by Wales until 2017.
Some of the more minor players
Edinburgh Napier University. After an FOI request (rejected), Napier closed their herbal medicine degree in 2010.
Hot and cold herbal nonsense from Napier University Edinburgh: another course shuts. (June 2010)
As expected, the Scottish Information Commissioner agreed with that for England and Wales and ordered material to be sent. Edinburgh Napier University teaches reflexology, aromatherapy and therapeutic touch. Scottish Information Commissioner says you should know. Some of the horrors so discovered appeared in Yet more dangerous nonsense inflicted on students by Edinburgh Napier University. The embarrassment seems to have worked. Their remaining degrees in aromatherapy and reflexology have now vanished from UCAS too. All that remains is a couple of part time “Certificates of Credit” for aromatherapy and reflexology
Anglia Ruskin Univerity Not only have BSc degrees gone in aromatherapy and reflexology, but their midwifery degree now states "We are unable to accept qualifications in aromatherapy, massage and reflexology."
University of Derby Reflexology and aromatherapy have gone, though doubtless Spa management therapies have much nonsense left
University of Greenwich. BSc in Complementary Therapies (Nutritional Health) and BSc in Complementary Therapies (Nutritional Health) have been shut. The BSc Acupuncture is listed on their web site but it is under review, and is not listed in UCAS for 2012. (Acupuncture is run at International College of Oriental medicine, validated by Greenwich.). Only osteopathy (MOst) is still running, and that is a validation of an external course run at The European School of Osteopathy, in Maidstone
Thames Valley University was renamed the University of West London in 2010. The nonsense that was run there (e.g. Nutritional Fairy Tales from Thames Valley University) seems to have vanished. Their previous alt med guru, Nicola Robinson, appears now to be at London South Bank University (ranked 116 out of the 116 UK universities)
What’s left?
Chiropractic Surprisingly, given the total discreditation of chiropractic in the wake of the Simon Singh affair, and the internecine warfare that followed it, none of the chiropractic courses have shut yet. Some are clearly in trouble, so watch this space.
Osteopathy has also had no course closures since 2007. Like chiropractic it also suffers from internecine warfare. The General Osteopathic Council refuses to disown the utter nonsense of "craniosacral" osteopathy. But the more sensible practitioners do so and are roughly as effective as physiotherapists (though there are real doubts about how effective that is).
Excluding chiropractic and osteopathy, this is all that’s left. It now consists almost entirely of Chinese medicine and a bit of herbal.
Glyndwr university (Known as North East Wales Institute until 2008) Ranked 104 out of 116 UK universities
BSc Acupuncture (B341) BSc
BSc Complementary Therapies for Healthcare (B343)
Cardiff Metropolitan University (UWIC) (Known as University of Wales Institute Cardiff (UWIC) until Nov 2011.) The vice-chancellor of Cardiff Metropolitan, Antony Chapman, is in the QAA’s board of directors, so perhaps it isn’t surprising that the QAA has done nothing.
BSc Complementary Therapies (3 years) (B390)
BSc Complementary Therapies (4 yrs inc Foundation) (B300)
University of Lincoln
Acupuncture (B343) 3FT Hon BSc
Herbal Medicine (B342) 3FT Hon BSc
University of East London Ranked 113 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
London South Bank University Ranked 116 out of 116 UK universities
Acupuncture (B343) 4FT Deg MCM
The Manchester Metropolitan University Ranked 93 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
Middlesex University
Acupuncture (B348) 3FT Hon BSc
Ayurvedic Medicine (A900) 4FT Oth MCM
Herbal Medicine (B347) 3FT Hon BSc
Traditional Chinese Medicine (BT31) 4FT Hon BSc
University of Westminster
Chinese Medicine: Acupuncture (B343) 3FT Hon BSc
Chinese Medicine: Acupuncture with Foundation (B341) 4FT/5FT Hon BSc/MSci
Herbal Medicine (B342) 3FT Hon BSc
Herbal Medicine with Foundation Year (B340) 4FT/5FT Hon BSc/MSci
It seems that acupuncture hangs on in universities that are right at the bottom of the rankings.
Manchester Metropolitan gets the booby prize for actually starting a new course, just as all around are closing theirs. Dr Peter Banister, who was on the committee that approved the course (but now retired), has told me ” I am sceptical in the current economic climate whether it will prove to be successful”. Let’s hope he’s right.
But well done Westminster. Your position as the leader in antiscientific degrees has now been claimed by Middlesex University. Their "degrees" in Ayurveda mark out Middlesex University as the new King of Woo.
Over to you, Professor Driscoll. As vice-chancellor of Middlesex University, the buck stops with you.
Both still teach Chinese and herbal medicine, which are potentially dangerous. There is not a single product from either that has marketing authorisation from the MHRA, though the MHRA has betrayed its trust by allowing misleading labelling of herbal medicines without requiring any evidence whatsoever that they work, see, for example
Why degrees in Chinese medicine are a danger to patients
More quackedemia. Dangerous Chinese medicine taught at Middlesex University
Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me
Sub-degree courses
In contrast to the large reduction in the number of BSc and MSc degrees, there has actually been an increase in two year foundation degrees and HND courses in complementary medicine, at places right near the bottom of the academic heap. The subject is sinking to the bottom. With luck it will vanish entirely from universities before too long.
Research-intensive Universities
Although all of the degrees in magic medicine are from post-1992 universities, the subject has crept into more prestigious universities. Of these, the University of Southampton is perhaps the worst, because of the presence of George Lewith, and his defender, Stephen Holgate. Others have staunch defenders of quackery, including the University of Warwick, University of Edinburgh and St Batholomew’s.
Why have all these courses closed?
One reason is certainly the embarrassment caused by exposure of what’s taught on the courses. Professors Petts (Westminster) and Driscoll (Middlesex) must be aware that googling their names produces references to this and other skeptical blogs on the front page. Thanks to some plain brown emails, and, after a three year battle, the Freedom of Information Act, it has been possible to show here the nonsense that has been foisted on students by some universities. Not only is this a burden on the taxpayer, but, more importantly, some of it is a danger to patients.
When a course closes, it is often said that it is because of falling student numbers (though UCLAN and Salford did not use that excuse). Insofar as that is true, the credit must go to the whole of the skeptical movement that has grown so remarkably in the last few years. Ben Goldacre’s "ragged band of bloggers" have produced a real change in universities and in society as a whole.
The people who should have done the job have either been passive or an active hindrance. The list is long. Vice-chancellors and Universities UK (UUK), the Quality Assurance Agency (QAA), the Hiigher Education Funding Council England (HEFCE), Skills for Health, the Medicines and Health Regulatory Authority ( MHRA) , the Health Professions Council (HPC), the Department of Health, the Prince of Wales and his reincarnated propaganda organisation, the "College of Medicine", the King’s Fund, the Universities and Colleges Union (UCU), OfQual, Edexcel, National Occupational Standards and Qualifications and the Curriculum Authority (QCA).
Whatever happened to that "bonfire of the quangos"?
Follow-up
2 January 2012 The McTimoney College of Chiropractic (owned by BPP University) claims that its “validation” by the University of Wales will continue until 2017. This contradicts the statement from UoW. Watch this space.
3 January 2012. Thanks to Neil O’Connell for drawing my attention to a paper in Pain. The paper is particularly interesting because it comes from the Southampton group which has previously been sympathetic to acupuncture. Its authors include George Lewith. It shows, yet again that there is no detectable difference between real and sham acupuncture treatment. It also shows that the empathy of the practitioner has little effect: in fact the stern authoritarian practitioner may have been more effective.
Patients receiving acupuncture demonstrated clinically important improvements from baseline (i.e., a 29.5% reduction in pain), but despite this, acupuncture has no specific efficacy over placebo for this group of patients. The clinical effect of acupuncture treatment and associated controls is not related to the use of an acupuncture needle, nor mediated by empathy, but is practitioner related and may be linked to the perceived authority of the practitioner.”
Sadly. the trial didn’t include a no-treatment group, so it is impossible to say how much of the improvement is regression to the mean and how much is a placebo effect. The authors admit that it could be mostly the former.
Surely now the misplaced confidence in acupuncture shown by some medical and university people must be in tatters.
In yet another sign that even acupuncture advovates are beginning to notice that it doesn’t work, a recent article Paradoxes in Acupuncture Research: Strategies for Moving Forward, shows some fascinating squirming.
3 January 2012. The Daily Telegraph has carried a piece about closure of university courses, written by Michael Hanlon. On 31 January they carried a much longer piece.
3 January 2012. It is a great pity that some physiotherapists seem to have fallen hook, line and sinker for the myths of acupuncture. Physiotherapists are, by and large, the respectable face of manipulative therapy. Their evidence base is certainly not all one would wish, but at least they are free of the outrageous mumbo humbo of chiropractors. Well, most of them are, but not the Acupuncture Association of Chartered Physiotherapists (AACP), or, still worse, The Association of Chartered Physiotherapists in Energy Medicine, a group that is truly away with the fairies. These organisations are bringing a very respectable job into disrepute. And the Health Professions Council, which is meant to be their regulator, has, like most regulators, done nothing whatsoever to stop it.
5 January 2012. Times Higher Education gives a history of the demise of the University of Wales, Boom or Bust. It’s a useful timeline, but like so many journalists, it’s unwilling to admit that bloggers were on to the problem long before the BBC, never mind the QAA.
There was also a leader on the same topic, Perils of the export business. It again fails to take the QAA to task for its failures.
Interviews for Deutsche Welle and Middle East Broadcasting Center TV.
17 January 2012 Another question answered. I just learned that the ludicrous course in Nutritional Therapy, previously validated by the University of Wales (and a contributor to its downfall), is now being validated by, yes, you guessed, Middlesex University. Professor Driscoll seems determined to lead his univerity to the bottom of the academic heap. His new partnership with the Northern college of Acupuncture is just one of a long list of validations that almost rivals that of the late University of Wales. The course has, of course, an enthusiastic testimonial, from a student. It starts
I work full time as a team leader for a pension company but I am also a kinesiologist and work in my spare time doing kinesiology, reiki and Indian head massage.
Evidently she’s a believer in the barmiest and totally disproved forms of magic medicine. And Middlesex University will give her a Master of Science degree. I have to say I find it worrying that she’s a team leader for a pension company. Does she also believe in the value of worthless derivatives. I wonder?
18 January 2012. the story has gone international, with an interview that I did for Deutsche Welle, UK universities drop alternative medicine degree programs. I’m quoted as saying “They’re dishonest, they teach things that aren’t true, and things that are dangerous to patients in some cases”. That seems fair enough.
There is also an interesting item from July 2010 about pressure to drop payment for homeopathy by German health insurance
31 January 2012
The Daily Telegraph carried a prominent 1200 word account (the title wasn’t mine). The published version was edited slightly.
Western herbal medicine need not be mystical nonsense, but it usually it is,
Plants often contain chemicals that have pharmacological actions, with all the possibilities for good and for harm that implies (see Plants
as medicines). It would be quite possible to teach about the plant constituents and their actions in an entirely scientific way, but it seems that this is not what courses in herbal medicine choose to do. That is why they shouldn’t be called Bachelor of Science degrees.
We have recently revealed the ancient nonsense taught at Middlesex University in its "BSc (Hons)" degree in Traditional Chinese Medicine in Dangerous Chinese medicine taught at Middlesex University as well as similar dangerous gobbledygook from the University of Westminster: see Why degrees in Chinese medicine are a danger to patients.
Western Herbal medicine does not talk about "knotted spleen Qi", but has an equally barmy mystical vocabulary of its own. They have in common a tendency to divide herbs into hot and cold, a crude and baseless classification that dates from a time when nothing was known about physiology or the causes of disease.
A recent post described the problems of finding out what exactly is taught on these courses: Not much Freedom of Information at University of Wales, University of Kingston, Robert Gordon University or Napier University
I lodged a Freedom of Information (Scotland) Act with Napier University Edinburgh on 10th August 2009. As almost always, it was refused, as was the internal review of my request. The response to the internal review came from Gerry Webber BA (Hons) 0 PHil MBA MCMI AUA (Fellow). Despite all those impressive sounding letters, he argued with a perfectly straight face that it was perfectly all right for the university to teach this sort of stuff. He ended
“On public interest grounds, I have therefore concluded that, in respect of the commercially sensitive information requested, the public interest is better served in withholding the information you have requested than in disclosing it.”
Despite all those impressive sounding letters after Dr Webber’s name, here was a solemn letter, on the university letterhead, defending the teaching of pseudoscientific nonsense The experience is surreal, but far from unique.
Although we won a judgement that compelled disclosure from the Information Commissioner for England and Wales, the Scottish law is slightly different so I had to appeal to the Scottish Information commissioner. [Download appeal]
A similar appeal was lodged for Robert Gordon’s University Aberdeen. They have already sent some homeopathy materials, and closed down the homeopathy course, as described at: Robert Gordon University stops its homeopathy course. Quackademia is crumbling. Napier University followed the same pattern, but a bit more slowly. They sent some of what I asked for without waiting for a formal judgement, after they had been contacted by the Scottish Information Commissioner.
Napier also shut down the degree from which the slides, below, were used. It is fascinating that so many places have done this shortly before what is taught is made public. Before that time the courses are defended and advertised. no doubt by people who have never given a moment’s thought to what is taught. In 2007, after my Nature article on the topic, the Glasgow Herald said
A spokeswoman for Napier University said it stood by the integrity of its BSc degrees.
“The BSc Herbal Medicine course uses an approach to teaching and training that we believe best prepares students for practice within a modern integrated healthcare system,” she said.
The university’s brochure for the course (still, carelessly, on the web at the time of writing), waxed lyrical about the herbal medicine course. Yet as soon as it becomes known what’s actually taught, the courses close.
What was taught on Napier’s Herbal Medicine “BSc”.
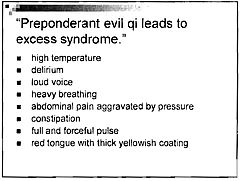
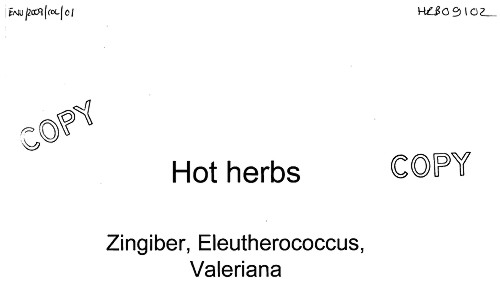
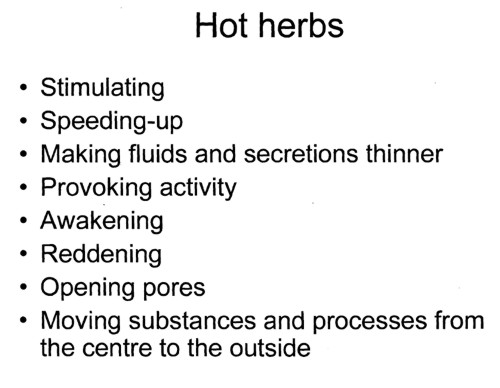
Materia medica starts with hot and cold herbs
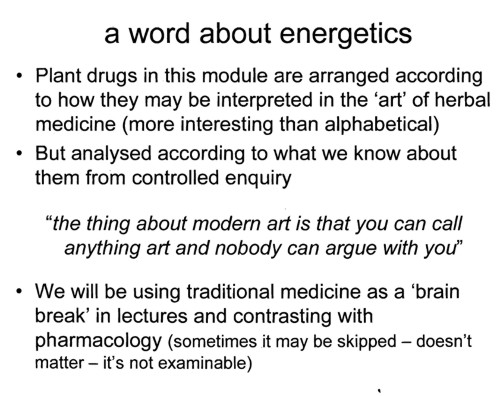
Yes, but one of the problems is that very little is known about the therapeutic actions of herbs from "controlled enquiry". The material just isn’t there to fulfil this aim. To paraphrase their quotation,,you can call anything medicine, but plenty of people will argue with you if you can’t produce the evidence.
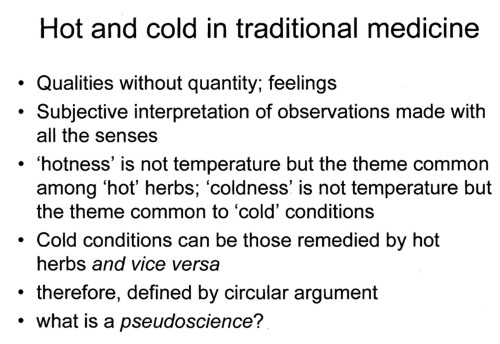
This slide strikes me as pure pre-scientific gobbledygook. All herbs and all diseases seem to fall into the ‘hot’ or ‘cold’ class. The ‘argument’ is entirely circular. Pure pseudoscience (is that what the lecturer told them in response to the last question?).
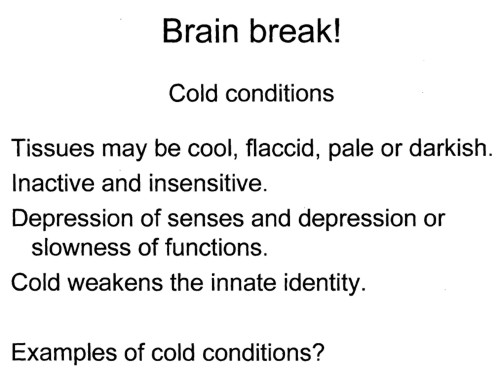
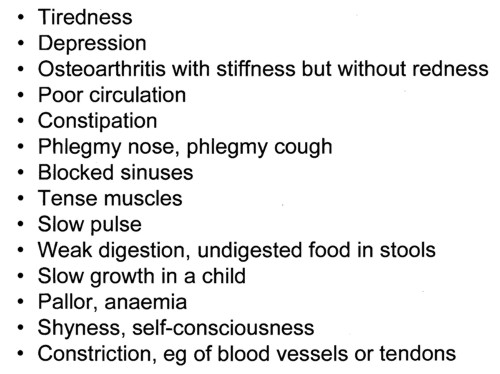
What do all these conditions have in common? They are all "cold". How can anyone take this sort of baloney seriously?
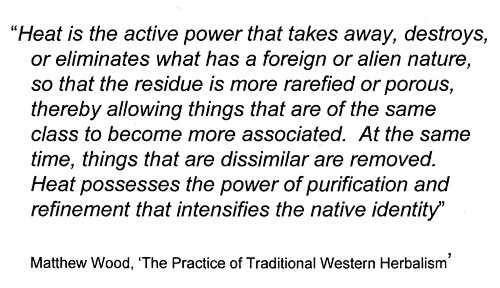
This quotation appears to have no comprehensible meaning at all. It carries overtones of the great "detox" fraud, and so perhaps is useful justification for slimming the wallets of the gullible.
Now we come to a real herb.
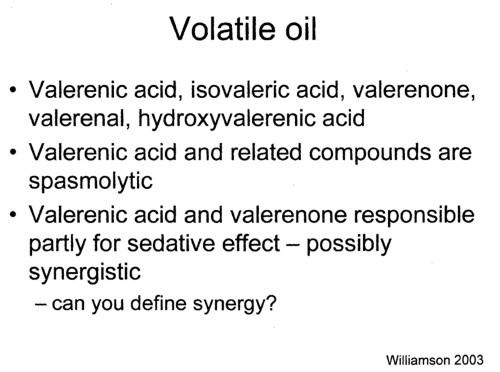
There is some real chenistry in this slide. Unfortunately it simply isn’t known whether these chemicals have any useful function. Usually it isn’t known either what dose of them you are giving in tincture of valerian. When I worked in a pharmacy in the 1950s, you could still find tincture of valerian on the shelves of a normal pharmacy, but iit soon vanished as paople realised it wasn’t much use. Disappeared from normal medicine, that is. it is still alive and well among herbalists.
Notice too, the mention of "synergy". The perpetual excuse of herbalists for giving impure mixtures of chemicals is that they might act synergistically. They are undeterred by the fact that no such synergy has ever been demonstrated properly. I asked that question ot Liz Williamson. editor of Potter’s herbal Cyclopedia, but answer came there none.
I’d be interested to know what answer was given to the last question, which isn’t as simple as it sounds. I wouldn’t mind betting it didn’t include a critical description of isobol analysis.
So what does Valerian do?
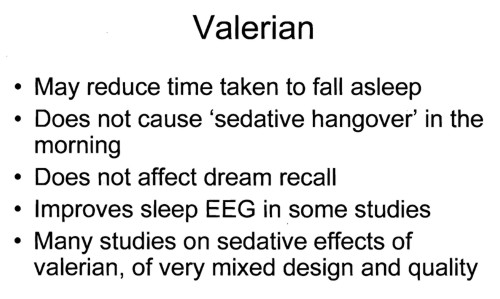
It seems, even from the lecture, that there is no unanimity that it does anything useful at all.
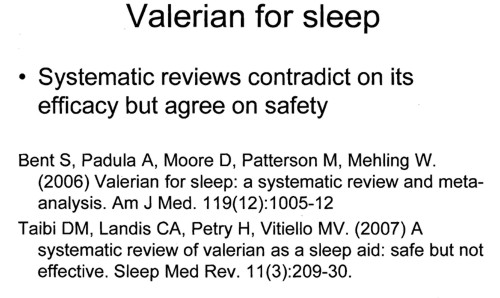
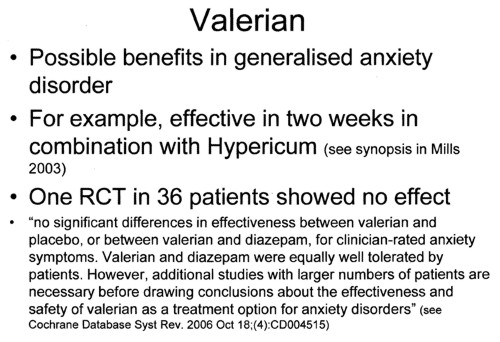
There is no worthwhile evidence to think it is useful for "generalises anxiety disorder" Let’s take another opinion.
The National Center for Complementary and Alternative Medicine (NCCAM) is the branch of the US National Institutes of Health which has spent around a billion dollars of US taxpayers’ money on research into alternative medicine, For all that effort they have failed to come up with a single useful treatment. Clearly they should be shut down. Nevertheless, as an organisation that is enthusiastic about alternative medicine, it’s interesting to see what they have to say about valerian.
What the Science Says
- Research suggests that valerian may be helpful for insomnia, but there is not enough evidence from well-designed studies to confirm this.
- There is not enough scientific evidence to determine whether valerian works for anxiety or for other conditions, such as depression and headaches.
Even NCCAM don’t pretend that there is any good reason to think it’s good for anything. So, you might ask, why are students being taught to treat people with it?
Simon Mills on "hot and cold herbs"
Many of the slides refer to a book by herbalist Simon Mills. You can see a video of a talk he gave in which he ‘explains’ "hot and cold herbs". It strikes me as pure gobbledygook. Make up your own mind.
Now take the test
This is a question from a Napier University exam paper
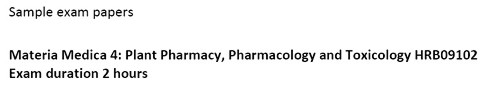
Which constituents are responsible for the actions of saw palmetto? Which actions would they be? This is what The National Center for Complementary and Alternative Medicine (NCCAM) says
about saw palmetto.
What the Science Says
- Several small studies suggest that saw palmetto may be effective for treating BPH symptoms.
- In 2006, a large study of 225 men with moderate-to-severe BPH found no improvement with 320 mg saw palmetto daily for 1 year versus placebo. NCCAM cofunded the study with the National Institute of Diabetes and Digestive and Kidney Diseases.
- There is not enough scientific evidence to support the use of saw palmetto for reducing the size of an enlarged prostate or for any other conditions.
- Saw palmetto does not appear to affect readings of prostate-specific antigen (PSA) levels. PSA is protein produced by cells in the prostate. The PSA test is used to screen for prostate cancer and to monitor patients who have had prostate cancer.
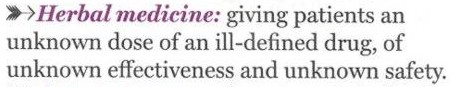
Magic Medicine
In the materials that I was sent, I see nothing to make me believe that herbalism is being taught as science. On the contrary, it all seems to confirm the definition given in the Patients’ Guide to Magic Medicine.
Herbal medicine BSc degrees still exist.
They are still running at the following universities.
The vice-chancellors are named because they are the people who must take responsibility for this sort of nonsense being taught in their universities.
University of East London (vice-chancellor from Feb 2010 is Patrick McGhee, who, in his previous job at University of Central Lancashire, did so much to prevent me from getting hold of their teaching materials, but then closed the courses anyway)
University of Lincoln (Vice chancellor, Professor Mary Stuart)
London Metropolitan University (vice-chancellor, (interim vice chancellor, Alfred Morris)
Middlesex University (vice-chancellor, Professor Michael Driscoll)
And, of course, the home of woo, the University of Westminster (vice-chancellor, Professor Geoffrey Petts). Their students are taught that Amethysts emit high Yin energy and that dowsing and pendulums can be used for diagnosis and treatment.
By the same token, we may congratulate Professor Dame Joan Stringer, vice-chancellor of Napier University Edinburgh for closing down the course from which these slides came. Perhaps now she should consider closing their ‘degrees’ in aromatherapy and ‘reflexology’