National Health Service
A constant theme of this blog is that the NHS should not pay for useless treatments. By and large, NICE does a good job of preventing that. But NICE has not been allowed by the Department of Health to look at quackery.
I have the impression that privatisation of many NHS services will lead to an increase in the provision of myth-based therapies. That is part of the "bait and switch" tactic that quacks use in the hope of gaining respectability. A prime example is the "College of Medicine", financed by Capita and replete with quacks, as one would expect since it is the reincarnation of the Prince’s Foundation for Integrated Health.
One such treatment is acupuncture. Having very recently reviewed the evidence, we concluded that "Acupuncture is a theatrical placebo: the end of a myth". Any effects it may have are too small to be useful to patients. That’s the background for an interesting case study.
A colleague got a very painful frozen shoulder. His GP referred him to the Camden & Islington NHS Trust physiotherapy service. That service is now provided by a private company, Connect Physical Health.
That proved to be a big mistake. The first two appointments were not too bad, though they resulted in little improvement. But at the third appointment he was offered acupuncture. He hesitated, but agreed, in desperation to try it. It did no good. At the next appointment the condition was worse. After some very painful manipulation, the physiotherapist offered acupuncture again. This time he refused on the grounds that "I hadn’t noticed any effect the first time, because there is no evidence that it works and that I was concerned by her standards of hygiene". The physiotherapist then became "quite rude" and said that she would put down that the patient had refused treatment.
The lack of response was hardly surprising. NHS Evidence says
"There is no clinical evidence to show that other treatments, such as transcutaneous electrical nerve stimulation (TENS), Shiatsu massage or acupuncture are effective in treating frozen shoulder."
In fact it now seems beyond reasonable doubt that acupuncture is no more than a theatrical placebo.
According to Connect’s own web site “Our services are evidence-based”. That is evidently untrue in this case, so I asked them for the evidence that acupuncture was effective.
I’d noticed that in other places, Connect Physical Health also offers the obviously fraudulent craniosacral therapy (for example, here) and discredited chiropractic quackery. So I asked them about the evidence for their effectiveness too.
This is what they said.
|
Many thanks for your comments via our web site. In response, we thought you might like to access the sources for some of the evidence which underpins our MSK services: Integrating Evidence-Based Acupuncture into Physiotherapy for the Benefit of the Patient – you can obtain the information you require from www.aacp.org.uk The General Chiropractic Council www.gcc-uk.org/page.cfm We have also attached a copy of the NICE Guidelines. |
So, no Cochrane reviews, no NHS Evidence. Instead I was referred to the very quack organisations that promote the treatments in question, the Acupuncture Association of Chartered Physiotherapists, and the totally discredited General Chiropractic Council.
The NICE guidelines that they sent were nothing to do with frozen shoulder. They were the guidelines for low back pain which caused such a furore when they were first issued (and which, in any case, don’t recommend chiropractic explicitly).
When I pointed out these deficiencies I got this.
|
Your email below has been forwarded to me. I am sorry if you feel that that that information we pointed you towards to enable you to make your own investigations into the evidence base for the services provided by Connect Physical Health and your hospital did not meet with your expectations. ‘ ‘ ‘ Please understand that our NHS services in Camden were commissioned by the Primary Care Trust. The fully integrated MSK service model included provision for acupuncture and other manual therapy provided by our experienced Chartered Physiotherapists. If you have any problems with the evidence base for the use of acupuncture or manual therapy within the service, which has been commissioned on behalf of the GPs in Camden Borough, then I would politely recommend that you direct your observations to the clinical commissioning authorities and other professional bodies who do spend time evidencing best practice and representing the academic arguments. I am sure they will be pleased to pick up discussions with you about the relative merits of the interventions being procured by the NHS. Yours sincerely, Mark Mark Philpott BSc BSc MSc MMACP MCSP
Head of Operations, Community MSK Services Connect Physical Health 35 Apex Business Village Cramlington Northumberland NE23 7BF |
So, "don’t blame us, blame the PCT". A second letter asked why they were shirking the little matter of evidence.
|
In response to your last email, I would like to say that Connect does not wish to be drawn into a debate over two therapeutic options (acupuncture and craniosacral therapy) that are widely practiced [sic] within and outside the NHS by very respectable practitioners. You will be as aware, as Connect is, that there are lots of treatments that don’t have a huge evidence base that are practiced in mainstream medicine. Connect has seen many carefully selected patients helped by acupuncture and manual therapy (craniosacral therapy / chiropractic) over many years. Lack of evidence doesn’t mean they don’t work, just that benefit is not proven. Furthermore, nowhere on our website do we state that ALL treatments / services / modalities that Connect offer are ‘Evidence Based’. We do however offer many services that are evidence based, where the evidence exists. We aim to offer ‘choice’ to patients, from a range of services that are safe and delivered by suitably trained professionals and practitioners in line with Codes of Practice and Guidelines from the relevant governing bodies. Connect’s service provision in Camden is meticulously assessed and of a high standard and we are proud of the services provided. |
This response is so wrong, on so many levels, that I gave up on Mr Philpott at this point. At least he admitted implicitly that all of their treatments are not evidence-based. In that case their web site needs to change that claim.
If, by "governing bodies" he means jokes like the GCC or the CNHC then I suppose the behaviour of their employees is not surprising. Mr Philpott is evidently not aware that "craniosacral therapy" has been censured by the Advertising Standards Authority. Well he is now, but evidently doesn’t seem to give a damn.
Next I wrote to the PCT and it took several mails to find out who was responsible for the service. Three mails produced no response so I sent a Freedom of Information Act request. In the end I got some
"Connect PHC provide the Community musculoskeletal service for Camden. The specification for the service specifically asks for the provision of evidence based management and treatments see paragraph on Governance page 14 of attached.. Patients are treated with acupuncture as per the NICE Guidelines (May 2009) for the management of low back pain … . .. Chiropractors are not employed in the service and craniosacral therapy is not provided as part of the service either."
Another letter, pointing out that they were using acupuncture for things other than low back pain got no more information. They did send a copy of the contract with Connect. It makes no mention whatsoever of alternative treatments. It should have done, so part of the responsibility for the failure must lie with the PCT.
The contract does, however, say (page 18)
The service to be led by a lead clinician/manager who can effectively demonstrate ongoing and evidence-based development of clinical guidelines, policies and protocols for effective working practices within the service
In my opinion, Connect Physical Health are in breach of contract
Another example of Connect ignoring evidence
The Connect Physical Health web site has an article about osteoarthritis of the knee
Physiotherapy can be extremely beneficial to help to reduce the symptoms of OA. Treatments such as mobilizations, rehab exercises, acupuncture and taping can help to reduce pain, increase range of movement, increase muscle strength and aid return to functional activities and sports.
There is little enough evidence that physiotherapy does any of these things, but at least it is free of mystical mumbo-jumbo. Although at one time the claim for acupuncture was thought to have some truth, the 2010 Cochrane review concludes otherwise
Sham-controlled trials show statistically significant benefits; however, these benefits are small, do not meet our pre-defined thresholds for clinical relevance, and are probably due at least partially to placebo effects from incomplete blinding.
This conclusion is much the same as has been reached for acupuncture treatments of almost everything. Two major meta-analyses come to similar conclusions. Madsen Gøtzsche & Hróbjartsson (2009) and Vickers et al (2012) both conclude that if there is an effect at all (dubious) then it is too small to be noticeable to the patient. (Be warned that in the case of Vickers et al. you need to read the paper itself because of the spin placed on the results in the abstract.). These papers are discussed in detail in our recent paper.
Why is Connect Physical Health not aware of this?
Their head of operations told me (see above) that
"Connect does not wish to be drawn into a debate [about acupuncture and craniosacral therapy]".
That outlook was confirmed when I left a comment on their osteoarthritis post. This is what it looked like almost a month later.
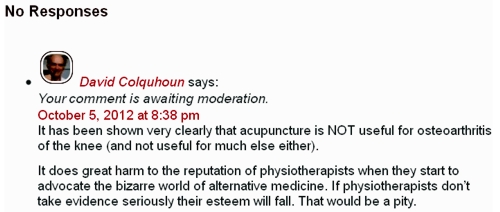
Guess what? The comment has never appeared..
The attitude of Connect Physical Health to evidence is simply to ignore it if it gets in the way of making money, and to censor any criticism.
What have Camden NHS done about it?
The patient and I both complained to Camden NHS in August 2012. At first, they simply forwarded the complaints to Connect Physical Health with the unsatisfactory results shown above. It took until May 2013 to get any sort of reasonable response. That seems a very long time. In fact by the time the response arrived the PCT had been renamed a Clinical Commissioning Group (CCG) because of the vast top-down reorganisation inposed by Lansley’s Health and Social Care Act.
On 8 May 2013, this response was sent to the patient, Here is part of it.
|
I have received your email of complaint from the NHSNCL complaints department regarding your care. You raise some very clear concerns and I will attempt to address these in order. 1) The fact that you felt pressurised into having acupuncture is a concern as everybody should be given a choice. As part of the informed consent relating to acupuncture you should have been told about the treatment, it’s [sic] benefits and risks and then you sign to confirm you are happy to proceed. I understand that this was the case in your situation but I have reinforced that the consent is important and must be adhered to by the provider Connect Physical Health. There are clear standards of clinical practice that all Chartered Physiotherapists must follow which I will discuss further with the Connect Camden team Manager Nick Downing. I do disagree with you around acupuncture; there is no conclusive evidence for acupuncture in frozen shoulder but I have referenced a systematic review which concludes the studies were too small to draw any conclusions although shoulder function was significantly improved at 4 weeks (Green S et al. Acupuncture for shoulder pain. Cochrane Database Syst Rev 2005; 18: CD005319). There is a growing body of evidence supporting the use of acupuncture and until such time as there is specific evidence against it I don’t think we would be absolutely against the practice of this modality alongside other treatments. .Best wishes Strategy and Planning Directorate |
This response raises more questions than it answers.
For example, what is "informed consent" worth if the therapist is his/herself misinformed about the treatment? It is the eternal dilemma of alternative medicine that it is no use referring to well-trained practitioners, when their training has inculcated myths and untruths.
There is not a "growing body of evidence supporting the use of acupuncture". Precisely the opposite is true.
And the statement "until such time as there is specific evidence against it I don’t think we would be absolutely against the practice of this modality alongside" betrays a basic misunderstanding of the scientific process.
So I sent the writer of this letter a reprint of our paper, "Acupuncture is a theatrical placebo: the end of a myth" (the blog version alone has had over 12,000 page views). A few days later we had an amiable lunch together and we had a constructive discussion about the problems of deciding what should be commissioned and what shouldn’t.
It seems to me to be clear that CCGs should take better advice before boasting that they commission evidence-based treatments.
Postscript
Stories like this are worrying to the majority of physiotherapists who don’t go in for mystical mumbo-jumbo of acupuncture. One of the best is Neil O’Connell who blogs at BodyInMind. He tweeted
Physio fail, sigh RT@david_colquhoun: Yet more #acupuncture. Sold to the NHS by private contractor @ConnectPHC http://t.co/HylkwMCVTh
— Neil O'Connell (@NeilOConnell) June 10, 2013
It isn’t clear how many physiotherapists embrace nonsense, but the Acupuncture Association of Chartered Physiotherapists has around 6000 members, compared with 47,000 chartered physiotherapists (AACP), so it’s a smallish minority. The AACP claims that it is “Integrating Evidence-Based Acupuncture into Physiotherapy”. Like most politicians, the term “evidence-based” is thrown around with gay abandon. Clearly they don’t understand evidence.
Follow-up
12 June 2013
The Advertising Standards Authority has, one again, upheld complaints against the UCLH Trust, for making false claims in its advertising. This time, appropriately, it’s about acupuncture. Just about everything in their advertising leaflets was held to be unjustifiable. They’ve been in trouble before about false claims for homeopathy, hypnosis and craniosacral "therapy".
Of course all of these embarrassments come from one very small corner of the UCLH Trust, the Royal London Hospital for Integrated Medicine (previously known as the Royal London Homeopathic Hospital).
Why is it tolerated in an otherwise excellent NHS Trust? Well, the patron is the Queen herself (not Charles, aka the Quacktitioner Royal), She seems to exert more power behind the scenes than is desirable in In a constitutional monarchy
29 June 2013
I wrote to Dr Gill Gaskin about the latest ASA judgement against RLHIM. She is the person at the UCLH Trust who has responsibility for the quack hospital. She previously refused to do anything about the craniosacral nonsense that is promoted there. This time the ASA seems to have stung them into action at long last. I was told
|
In response to your question about proposed action: All written information for patients relating to the services offered by the Royal London Hospital for Integrated Medicine are being withdrawn for review in the light of the ASA’s rulings (and the patient leaflets have already been withdrawn). It will be reviewed and modified where necessary item by item, and only reintroduced after sign-off through the Queen Square divisional clinical governance processes and the Trust’s patient information leaflet team. With best wishes Gill Gaskin Dr Gill Gaskin |
It remains to be seen whether the re-written information is accurate or not.
The rules for advertising
The Advertising Standards Authority gives advice for advertisers about what’s permitted and what isn’t.
Acupuncture The CAP advice
Craniosacral therapy The CAP advice
Homeopathy The CAP advice and 2013 update
Chiropractic The CAP advice.
|
“In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established”. . . “. . . they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.” David Mattin, lately of NHS Choices |
NHS Choices is usually a good source of information for the public. But there is one exception: the information they provide about alternative medicine is poor. A Freedom of Information Act request has revealed that the attempt of NHS Choices to rewrite their pages more accurately was censored by the Department of Health in conjunction with the late Prince’s Foundation for Integrated Health. The Department of Health (DH) has misled the public.
The earliest version of the homeopathy information page recorded by the Wayback Machine was November 12 2007. It was still there on December 5 2010. The comments were mostly critical. One said, quite correctly,
|
I find it most regrettable that the way NHS has covered this subject is to give uncritical voice to the claims of homoeopathy without giving readers the information they need to evaluate those claims. To refer readers to the websites of the British Homeopathy Association is like settling the question of the shape of planet by a reference to the website of the Flat Earth Society |
There were a lot of complaints, and to the credit of NHS Choices, the page vanished. Throughout 2011, and up to October 2012 the information page on homeopathy read
|
Introduction Content on homeopathy has been removed from the website pending a review by the Department of Health policy team responsible for complementary and alternative medicines. Homeopathy is not part of mainstream medicine. Instead it is defined as a complementary or alternative medicine. If you are considering using homeopathy, talk to your GP first. For more information about homeopathy see the House of Commons Science and Technology Committee report on homeopathy published on 8 February 2010 and the Department of Health response to that report published in July 2010 (PDF, 69KB). |
Then, at the end of 2012, the page reappeared. It was a bit better than the original, but not much. Many of the comments criticise the misleading nature of the information (as well as the usual “it worked for me” comments). The “useful links” still has six links to flat-earth organisations like the Society of Homeopaths, and only one to a sensible source, the excellent pamphlet from Sense about Science. They do link at the end to the 2010 Science and Technology Committee Report: Evidence Check 2: Homeopathy (PDF, 1.61Mb), and to the Government Response to the Science and Technology Committee Report, Evidence Check 2: Homeopathy (PDF, 69kb) but no comment is made on the findings.
Policy-based evidence
I wondered why the NHS Choices page, after an absence of almost two years, had returned in such an unsatisfactory form. So I asked them. After a reminder, I was told that my queries were being dealt with not by NHS Choices, but had been referred to Dr Sunjai Gupta “the DH official with responsibility for this area”. Dr Sunjai Gupta OBE is Deputy Director of Public Health Strategy and Social Marketing, Department of Health.
Dr Gupta is not obviously sympathetic to woo. It’s hard to tell since he doesn’t seem to have published much. But one is not reassured by an article that he wrote for the Journal of Holistic Healthcare. It appears straight after an article by fantasy herbalist, Simon Mills.
Despite assurances that I’d hear from Dr Gupta shortly, nothing happened. So I sent a request for the correspondence under the Freedom of Information Act (2000). Although the request was addressed to NHS Choices, a public body, strenuous efforts were made to divert it to the Department of Health. These were resisted. Nevertheless when, after a long delay, the material arrived, it came not from NHS Choices, but from DH, who had evidently vetted it,. The emails were rather shocking [download all].
A mail dated 1 December 2009 said
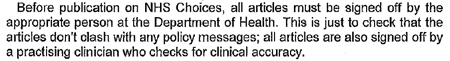
This is the most direct statement I’ve seen that, in the Department of Health, policy dictates evidence. NHS Choices is meant to provide evidence, but what they say has to be checked by DH to make sure they “don’t clash with any policy messages”.
The re-written page
The original version of the re-written page was sent to me by David Mattin, who worked for NHS Choices until September 2012. You can download the whole draft here. It is an enormous improvement on the original page. For example, it says
|
“Does it work?
Many independent experts would respond to this question ‘no, homeopathy does not work’ There is no good quality clinical evidence to show that homeopathy is more successful than placebo in the treatment of any type of condition. Furthermore, if the principles of homeopath were true it would violate all the existing theories of science that we make use of today; not just our theory of medicine, but also chemistry, biology and physics. |
This original draft was sent to Mattin on 29 January 2010. After editing it for length Mattin sent it to DH for approval. Over the next two years, DH removed much of the accurate content. Mattin’s own comments on this evisceration are reproduced below.
The DH emails
All the names have been redacted. Needless to say, nobody is willing to take responsibility. But the number of people who support magic medicine is really quite small so the main players were easy to identify.
During the nearly 2 year absence of the homeopathy page, dozens of changes were made by DH. It seems that the policy message with which the NHS Choices draft failed to comply were those of the Prince’s Foundation for Integrated Health, and its successor (after April 2010), the College of Integrated Health, now known as the College of Medicine.
NHS Choices sought advice about their redrafted pages from the right person, Sir Iain Chalmers, one of the founders of the Cochrane Collaboration. On 3 Nov 2009, Chalmers advised
The most reliable source in the country - and one of the most reliable in the world - is Professor Edzard Ernst, professor of Complementary Medicine at the Peninsular Medical School, |
Ernst returned his suggestions in July 2010, but it seems that few of them survived the subsequent 18 months of revisions by DH.
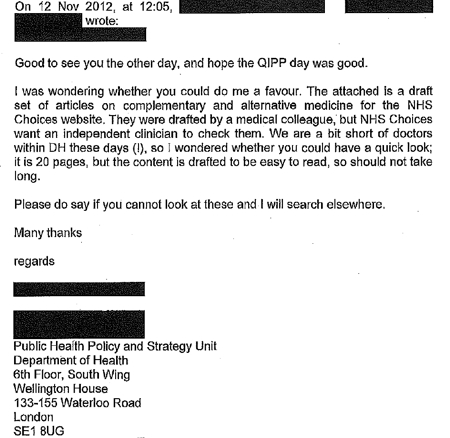
On 2 December 2009, a mail from the NHS headquarters (Quarry House, Leeds) was sent to NHS Choices
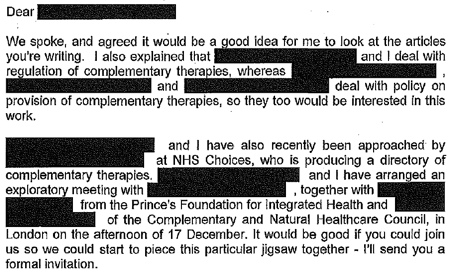
This makes it perfectly clear that DH regards the Prince’s Foundation, and the equally flaky Complementary and Natural Healthcare Council (CNHC: known on the web as Ofquack) as appropriate guides for public health policy. The fact of the matter is that regulation of magic medicine by the government has been a total disaster, because, it seems, DH regards the Prince of Wales as a reliable source.
On 29 December 2009, the Prince’s Foundation went on the attack.
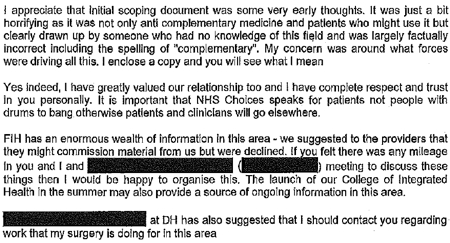
On 10th January 2010, two more letters were sent to DH by the Prince’s Foundation. At 13.48 they wrote
And at 22.14 on the same day, it was followed up with
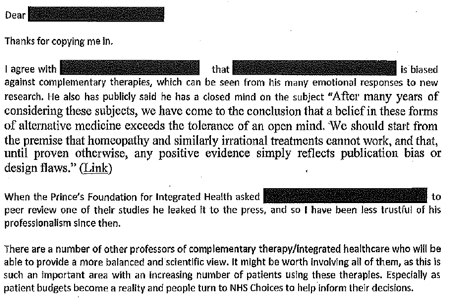
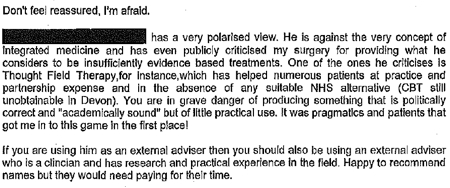
The references to Devon and to Thought Field Therapy, make it very obvious that these letters were written by Dr Michael Dixon OBE, who was medical director of the Prince’s Foundation, and who is now a director of the “College of Medicine”. And the object of Dixon’s bile is obviously Edzard Ernst (the quotation is from his book, Trick or Treatment).
I find it fascinating to see just how venomous quacks become when the evidence contradicts their views. The cuddly “holistic” veneer quickly vanishes.
It gets worse. On 21 January 2010, a mail from NHS Choices to DH said
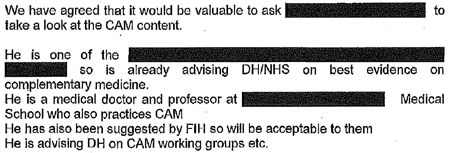
The only person in the country who fits this description is the (in)famous George Lewith. It is simply mind-boggling that DH regards him as an appropriate person to advise on anything.
After that, NHS Choices kept asking DH to sign off the documents, and changes continued to be made. Almost two years later, DH were still stalling.
The admission that “We are a bit short of doctors within DH these days” is interesting.
A bit short of anyone capable of critical thinking would be more accurate.
The most interesting document that I got from DH was an intermediate draft of the rewritten page on homeopathy (undated). Download the document. Here are a couple of extracts.
It’s a story of two years of meddling and procrastination. The end result misinforms the public.
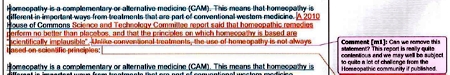
Right at the start, the NHS Choices draft says, reasonably enough
A House of Commons Science and Technology Committee report said that homeopathic remedies perform no better than placebos and that the principles on which homeopathv is based are “scientifically implausible”.
But a comment, added apparently by DH, says
Can we remove this statement? This report is really quite contentious and we may well be subject to quite a lot of challenge from the Homeopathic community if published.
What on earth? The DH seems to think that that its job is not to present the evidence, but to avoid challenges from the homeopathic community! And true enough, this piece is missing from the final version.
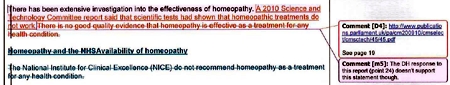
A bit later, the NHS Choices draft was censored again
“A 2010 Science and Technology Committee report said that scientific tests had shown that homeopathic treatments don’t work”
But again this doesn’t appear in the final version. The comment, apparently from DH, says
“The DH response to this report (point 24) doesn’t support this statement though”
That’s a gross distortion of point 24, which actually concludes
“The Government Chief Scientific Adviser cannot envisage scientifically credible proposals for funding for research into homeopathy in the future”
NHS Choices was not happy with the result
Shortly before the revised page was published, Paul Nuki, Editor in Chief of NHS Choicea, sent an email to DH.
|
Date: 7th September 2011 Time: 3:33:42 pm Hi I’ve been through the CAM articles and asked that we publish them asap as requested. For the record, we will be publishing these pieces outside of the normal editorial process. Although originally signed off by a suitably qualified clinician, the time lapse and policy changes have been so substantial as to render that null and void. We also don’t have a formal |
It doesn’t need much reading between the lines to see that he was unhappy with the result. It will be interesting to see whether the Information Standard people at the Royal Society for Public Health do anything about it.
The Department of Health has not just ignored evidence but actively opposed it.
That’s the only possible conclusion from the documents that I was sent. And it’s pretty shocking that the DH has preferred advice from the Prince’s Foundation and its handful of acolytes (in particular Michael Dixon and George Lewith) to the findings of the Science and Technology Select Committee and the views of the Chief Scientific Advisor.
In January this year, the Chief medical Officer, Dame Sally Davies, said, in a rare outburst of candour
|
‘I’m very concerned when homeopathic practitioners try to peddle this way of life to prevent malaria or other infectious disease,” she said. “I am perpetually surprised that homeopathy is available on the NHS.” Dame Sally, who is England’s most senior doctor, concluded by remarking that homeopathy “is rubbish”. |
 |
So one part of DH is working to contradict another part. the Chief Medical Officer. Perhaps Sally Davies should have a word with Dr Gupta.
This all predates the advent of Jeremy Hunt (and known defender of homeopathy) as health minister. But the sympathies of some DH people are made obvious by the presence on the DH web site of an article “Personal health budgets: A new way of accessing complementary therapies?”. This astonishing piece confirms the worst fears that quacks will see personal health budgets as a commercial opportunity to peddle their wares. The article is by Jim Rogers of Lincoln University. What his paper does not mention is Rogers’ conflict of interest. He’s a homeopath, and he has a paper in the International Journal of High Dilution Research (yes, there is a journal for every form of make-believe). You can download a reprint of this paper. It advocates more research into homeopathic provings, something that even George Lewith seems to have given up on.
It’s about time that the DH started to listen to the Chief Medical Officer. As it is, some people at DH seem to prefer the advice of the Prince’s Foundation, and to actively suppress employees who prefer evidence to anecdote.
One thing is clear. The DH is an unholy mess. Parts of it are intent on producing policy-based evidence.
Comment by David Mattin, who edited the first draft for NHS Choices
David Mattin left NHS Choices in September, 2012. He edited the new version and lived through the two years of wrangling with DH during which much of the best content was eviscerated. He sent me this statement about the affair.
|
As an editor at NHS Choices, I viewed it as my job to present evidence-based information to the public. The article we prepared on homeopathy stayed true to that central purpose: it made clear to readers that there is no good quality evidence that homeopathy is an effective treatment for any health condition, and also presented the broad scientific consensus that the supposed method of action of homeopathy is implausible.
What followed was a two year story of delay, and eventual suppression, of that article. My strong impression was of DH civil servants who lacked the courage, and, frankly, the energy to stand up to the criticism from special interest groups that they anticipated would arise because of the article; and that did indeed arise when a draft of the article and other draft content on complementary and alternative medicines fell into the hands of the Prince’s Foundation and other CAM groups.
The attitude of DH civil servants, broadly, was simply to tell us ‘we can’t say this about homeopathy, people will complain’. They seemed to have no interest in making an appraisal of the evidence on homeopathy themselves to see if what we were saying was actually true or not. We repeatedly pushed back with the message: ‘some people may very well complain, but if what we are saying about the evidence base is true – and it is – then we must simply weather those complaints, and stand by our content. Our duty is to supply our readers with the best information, not to please the homeopathy community.’ But these arguments were disregarded. The DH civil servants were almost entirely concerned with the politics of the situation – that is, the politics as they saw them – and the possibility that this article may create new work for them, and very little concerned with the evidence itself, or the presentation of this evidence to the public.
The whole episode is an insight into the way special interest groups can influence the workings of government and the public sector simply by making a lot of noise, and having a few powerful friends. In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established, and that they fund. They have sold out the NHS Choices editorial team, who work tirelessly to fulfil their remit. And, most seriously, they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.
|
Follow-up
13 February 2013 The Guardian version of this story, written by Sarah Boseley, is Prince’s charity lobbied government to water down homeopathy criticism. It’s fine as far as it goes but it doesn’t name any names. There are some good comments though.
14 February 2013. The printed Guardian gave the story full 5 column-width coverage. [download print version]
And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
On 14 February, the Guardian version was Editor’s Choice by lunchtime, and the Guardian web version already had 414 comments, mostly sensible (though this blog got far more referrals from twitter than from the Guardian)

And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
15 February 2013. The Daily Mail had very fair coverage of the story.

The Guardian closed the comments on the story when it had got 642 comments, most of them very sensible. And this page got almost 6000 hits in 24 hours. The majority of the referrals came from Twitter rather than from the Guardian, despite the direct link to the page from the Guardian.
18 February 2013. The affair featured in BMJ News [download the reprint]. The item featured prominently on the BMJ news page.

19 February 2013 Only six days of this post, the NHS Choices page has been re-written again, in a much improved form. That looks like bloggers 1, DH 0. It is baffling that it’s left to bloggers, working for nothing, to extract a bit of sense from the highly-paid civil servants at the Department of Health. But at least they listened this time, which is a lot more than happens often. Paul Nuki, who runs NHS Choices, deserves congratulations. Of course the revised page still doesn’t call a spade a spade, but it gets close at times. I like the way it starts "Homeopathy is a ‘treatment’ based". Notice the quotation marks.
Reputation management?
Incidentally, NHS Choices is outsourced to the (in)famous company, Capita. And the moderation of the comments on their site is outsourced again to Tempero, which describes itself as a "reputation management" company. Each of them creams off money meant of patient care. This discovery might explain why I and others have had comments rejected by NHS Choices several times. "Reputation management" is the antithesis of evidence. It is public relations, i.e. paid lying. That is quite wrong for a site that is meant to provide dispassionate information.
21 February 2013. Sadly a step backwards. Part of the improved page was removed. This bit.
The Chief Medical Officer, Professor Dame Sally Davies, has said there is no scientifically plausible way that homeopathy can prevent or cure diseases. She has made it clear she is particularly concerned about the use of homeopathy in developing countries as a so-called cure for malaria.
We can only speculate why this was removed, because it was true. In fact she accurately described homeopathy as "rubbish". Why she should not be quoted beats me.
[Use Firefox if embedded videos do not show in Chrome]
Andrew Lansley’s Health Bill (HASSB) aims to change the NHS into something more like the US system, which gives worse results at twice the cost.
The only possible reason for wanting to do that is simple far-right ideology. No wonder that no hint was given of its intentions before the election.
On the contrary, David Cameron stated repeatedly that there would be no top-down reorganisation of the NHS. That turned out to be a straight lie.
“First let me tell you what we are not going to do. There will be no more of those pointless reorganisations that aim for change, but instead bring chaos.” [David Cameron speaking to Royal College of Nursing in 2009, before election].
We all know that money must be saved. But the two major disasters of the coalition government don’t save any money.
On the contrary, both tuition fees and NHS-wrecking will cost taxpayers’ money. The tuition fees are done (for the time being) but there is still time to save the NHS.
The best simple explanation that I’ve found is by Dr Max Pemberton in the Telegraph: Read this – and prepare to fight for your NHS. The Bill is three times longer than the 1946 Bill that brought the NHS into existence.
“The power to determine the services that make up the NHS will be transferred from the Secretary of State to newly created Clinical Commissioning Groups (CCGs), which are unelected. Members will include GPs but also company chief executives who can, if they wish, outsource decisions about the appropriate level of services offered to companies with commercial interests. This is what the Government means when it says it is handing GPs £60 billion of NHS money. ”
“Monitor. This quango is composed of unelected and unaccountable individuals. It will not have overarching responsibility – which the Government does currently – to ensure that everyone’s health needs are met.” “It will have the power to decide, on purely financial grounds, if an area loses its existing range of hospital services, such as A&E departments, with no duty to consider alternative provision.
“With so many different providers of health care created under this Bill, those with complex health care needs may not receive the joined-up medical care that the NHS now works hard to provide.”
“Less profitable patients – those requiring complex levels of care from multiple individuals and areas of expertise, for example – may be sidelined by these private companies. ”
“the Bill allows CCGs to contract out commissioning functions to private accountancy, health insurance and management consultant firms, which will be able to decide what care is provided free at the point of use through the NHS and what is not. This means that profit-making companies will be able to provide your clinical care and also decide what you’re entitled to under the NHS and from which care providers.” “There is the potential for commercial conflicts when the needs of shareholders come between doctors and patients. ”
“Providers, too, can reduce levels of service provision and entitlement to NHS-funded care and there are no restrictions on charging for non-NHS care.”
“Now, up to 49 per cent of income can be generated from private income. This means that almost half the beds currently used for NHS care could be given over to private patients.” “This could create a two-tier system in hospitals” and “create a conflict of interest, with hospitals having a clear incentive to encourage as many patients as possible to use the private half of their facilities. Moreover, hospitals can decide when to discharge patients. The requirement for coordinated discharge and aftercare of patients between health and social care is abolished in the Bill. “
Why is the bill needed at all?
Most people believe that there is no need for a bill. The real aim appears to be in part 3, which proposes a vast increase in private providers. Oliver Huitson says
“A US report comparing the health services of 7 major economies ranked the NHS 1st in terms of efficiency, and 2nd overall. The US, which has vast private sector involvement and much greater use of GP commissioning, was ranked last despite spending more than twice as much per head as the UK”
” Despite being ranked as one of the most efficient and equitable health services in the developed world, the Conservatives are determined to remodel it in the image of one of the least efficient – all in the name of “improving efficiency”.”
Although most GPs are in favour of having more say in what happens, even the first parts of the bill are a mess. They are advertised as reducing bureaucracy and reducing costs. According to the Financial Times, they do exactly the opposite.
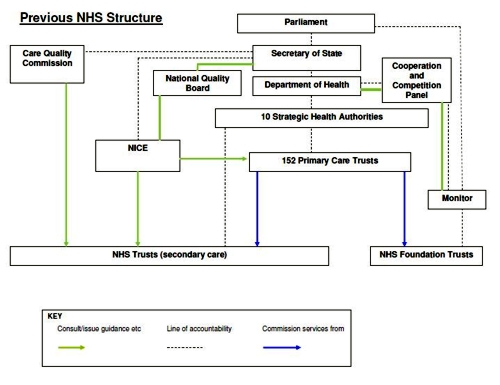
“Here was the original NHS bureaucracy in graphic form”
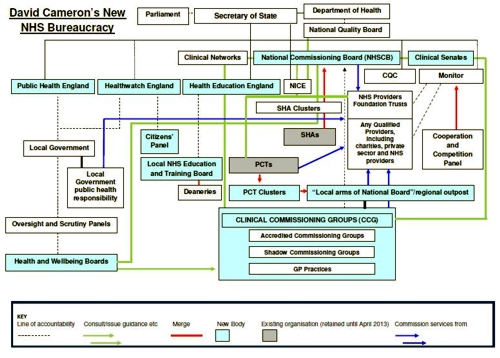
Here is the new NHS bureaucracy in graphic form
Ed Miliband pointed out that the number of NHS statutory organisations was growing from 163 to 521 – including “health and wellbeing committees,” “national commissioning boards”, “clinical networks”, “clinical senates” and so on.
So much for reduced bureaucracy.
Who thinks this is not a good idea?
Almost everyone. Not just the BMA which Lansley dismisses as a Trade Union, despite the fact that now (unlike in 1948) the BMA is voting against the financial interests of its members.
The Royal College of General Practitioners says Drop the Bill. So do Royal College of Nursing. Royal College of Midwives, Faculty of Public Health, Chartered Society of Physiotherapists, the Patients’ Association, among others. Almost the only support left is from the NHS Alliance, a tiny organisation run by Michael Dixon, friend of the Prince of Wales and advocate of quack medicine. The NHS alliance ran its own poll. A total of 100 people have voted so far, 99 of them against the Alliance’s policy. Some support. A rather good infographic shows how the balance lies.
The BMA’s General Practitioners Committee, which represents all GPs in the UK says [read full letter]
“1. Formally reaffirms its opposition to the NHS Health and Social Care Bill;
2. Believes that if passed the Bill will be irreversibly damaging to the NHS as a public service, converting it into a competitive marketplace that will widen health inequalities and be detrimental to patient care; . . . .”
In contrast, the e-petition to the government, started by Dr Kailash Chand OBE, states simply that it “Calls on the Government to drop its Health and Social Care Bill.”. It now has over 167,000 signatories. But despite the fact that petitions with over 100,000 signatures are meant to trigger a debate in the House of Commons, the backbench business committee of MPs has decided not to debate the e-petition.
So many people have rallied to oppose the daftness that it’s invidious to single out names. Nonetheless special mentions must go to Clare Gerada (@clarercgp on Twitter) (chair of the RCGP), and to Clive Peedell (@cpeedell) (oncologist and co-chair NHS Consultants’ Association) -read his Bevan’s Run blog. Among academics, Allyson Pollock and Martin McKee have done superb work on the details.
Most telling of all, some of the people who started by supporting Lansley have changed their minds. One concern about the “any qualified provider” idea is that it could open the door to quackery. Any “qualified” homeopath could bid for business at a competitive rate -sugar pills don’t cost much. Michael Dixon is one such.
Dr Sam Everington of Tower Hamlets is another. Services provided by his practice include “referrals to Inside Out Health and Wellbeing Ltd“. This private company will sell you fraudulent scams like homeopathy and kinesiology at £50 per session, among other nonsense (according to Companies House, it was wound up on 17 January 2012). He’s also associated with the “College of Medicine” (the reincarnation of the Prince of Wales’ Foundation). See also, Dr Margaret McCartney’s blog. As chair of the first Clinical Commissioning Group (CCG) he was embraced by Cameron. His Bromley-by-Bow surgery was host for Andrew Lansley’s first speech as health secretary after the 2010 election, and also host to the Prince of Wales..
But now even Everington has turned against the Bill (read the full letter).
“Dear Prime Minister
The Board of NHS Tower Hamlets Clinical Commissioning Group ask you to reflect and to withdraw the Health and Social Care Bill.”
“We care deeply about the patients that we see every day and we believe the improvements we all want to see in the NHS can be achieved without the bureaucracy generated by the Bill.
Your government has interpreted our commitment to our patients as support for the bill. It is not.”
And, on 1st March, another request to drop the bill, from the East London Integrated Care (ELIC is a not-for-profit social enterprise which is owned and run by local people and health professionals”). Read the full letter.
“Thursday, 1 March 2012 N1 5LZ
Dear Prime Minister,
The Board of City & Hackney Clinical Commissioning Group (CCG) join Tower Hamlets
and most other GPs and nurses and ask you to withdraw the Health and Social Care Bill.”
Is it really privatisation?
If you feel reassured by Lansley’s assurances that his measures aren’t de facto privatisation, just watch this video. It reveals some of the network of lobby groups that are circling the NHS, eager to take your money. For example, the lobby group, Policy Exchange, “Cameron’s favourite”, co-founded by Francis Maude, a member of Cameron’s cabinet, and is lobbying for more private sector provision of NHS services. One of the companies that it’s taken money from is called Tribal, which wants to take over commissioning from GPs. One of the directors of Tribal has described Andrew Lansley’s reforms as being “denationalisation of health services in England”.
So you don’t need to listen to left-wingers. The industry itself is in no doubt that it’s privatisation, and it’s ready and waiting to grab our money..
And of all unlikely allies, the vice chair of the British Holistic Medical Association has written a powerful letter about how the bill really would result in privatisation.
The likely consequences have been put well by Ben Goldacre in his What will happen with the NHS bill, in 5 tweets. The following points are based partly on this.
- GPs know they’re being set up to fail by being given commissioning powers, which they have neither the time nor the expertise to do properly.
- After GPs fail, private commissioning expertise will be needed. Large private companies will be given the job and they will come to operate like health insurers.
- These large bodies, like public/private insurance companies, will be able to pick and choose patients. They will naturally prefer the ones from whom they can make the most money (and not the sick or the old). Note that there is no geographical responsibility in the bill
- Small differences will gradually emerge in what services they offer. Top up plans will become available. And that will be the end of the NHS in the form in which we know it.
The only way that the proposals make any sense at all is if the underlying aim is to destroy the NHS, in anything like its present form. I believe that Lansley’s aims are much more to do with his personal political ideologies than anything to do with health. Those ideologies are far to the right of anything envisaged by Margaret Thatcher.
The politics. Where are the Lib Dems?
I voted Lib Dem in 2010, and I said precisely why. Of course I didn’t expect they’d get a majority. They were just the party that I found least objectionable. Like so many others I watched with horror as the numbers came out. There was no other option but to form a coalition with Conservatives. Well, I’d have been happier with no coalition, but the danger of that producing an overall majority for Conservatives after a year or so made that a very risky option.
When the coalition formed I was alarmed by the prospects for both education and for the NHS. I was less alarmed by the latter, because Cameron had said so many times that he had no intention of messing with the NHS. That turned out to be a direct lie. I could scarcely believe it when Lansley produced a plan after the election for the biggest reorganisation ever in the NHS, something that had not been foreshadowed in any way in the Conservative manifesto. This was one of the most dishonest bits of political manoeuvring that I’ve ever encountered.
Clearly we were spending more than we could afford. What’s unforgivable is to do things that actually cost the taxpayer more than before. Such actions are quite the opposite of cuts. Yet they are being done in the two areas, than any others, that have got Lib Dem voters angry.
(a) The £9k tuition fees cost the taxpayer more than the £3k fees did, because of the financing arrangements. I can see no conceivable reason for spending more taxpayers’ money than before apart from (Conservative) political ideology. That’s done (for now) so back to the main topic of this post, the NHS.
(b) It seems inevitable that Lansley’s proposals will cost money, not save money. Presumably that was predicted in the risk register, the concealment of which is a disgrace. See Liberal Conspiracy and the Green Benches blogs. The Information Commissioner ordered the release of the risk register, but the coalition refused (so much for transparent government). They appealed so now it goes to an Information Tribunal.
An Early Day Motion in the House of Commons urged release. It was signed by only 16 Lib Dems.
The bill started to fall apart in a major way when, on February 6th, The Times reported that
“Andrew Lansley should be taken out and shot,” says a Downing Street source. “He’s messed up both the communication and the substance of the policy.”
But Cameron, instead of grasping the chance, decided to back a loser.
Some Lib Dems have stuck to their principles. For example
John Pugh MP, Co-Chair of the Lib Dem Parliamentary Health Committee, re-established the Beveridge group, and wrote a letter to parliamentarians to explain why.
Andrew George MP wrote Health Bill has no friends. Dignified withdrawal would be best.
On 13 February, hearts soared when Lib Dem peer Shirley Williams spoke out at last. She urged Lansley to drop part 3 of the bill, the part that deals with privatisation. The elation didn’t last long though. Nick Clegg told the BBC: “Andrew Lansley is the architect of the NHS bill. He cares passionately about the NHS. He’s the right man for the job and he must see it through.”. Yes, I know about Cabinet solidarity, but it’s hard to think of any surer way to lose elections than to make statements like that. Even many Conservatives don’t believe it: see, for example, Dr Rachel Joyce on Conservative Home.
On 24th February, the Lib Dem president, Tim Farron MP, spoke up at last. “Mr Farron told ITV the bill should have been “massively changed” or dropped earlier and he wanted plans for more competition in the NHS to be dropped”.
On 26 February, Nigel Crisp, described the bill as a confusing mess that risks setting the NHS back. Crisp was formerly NHS chief executive and the permanent secretary at the Department of Health from 2000 to 2006, and is now a crossbench peer. Like everyone else, he was ignored.
The elation about Shirley Williams intervention didn’t last long. On 27th February a joint letter from Williams and Clegg claimed that they’d fixed the bill. The letter was quickly subjected to a bullshitometer analysis, by Health Policy Insight. Bafflingly, Lansley declared in public that he’d “changed his mind” about the privatisation, while at the same time Lansley and Cameron claimed that nothing much had changed: see Downing Street in knots as it plays down Nick Clegg’s NHS concessions, and Paul Corrigan’s blog.
March 1st saw two more blows for Clegg and Lansley. First, as reported thus in the Independent.
“Graham Winyard, the former deputy Chief Medical Officer, resigned from the party in protest at the leadership’s backing for the Bill. Dr Winyard, who was chairman of Winchester Liberal Democrats until last year, told Mr Clegg in a letter: “It is just not sensible to impose this top-down reorganisation on an NHS struggling to meet the biggest financial challenge in its history. To continue to do so in the face of near unanimous opposition from patient, staff and professional organisations simply invites slow motion disaster both for the NHS and for the party.” He said that he had no option but to resign “with great sadness”. “
Then, also on 1st March, Dr Laurence Buckman, chairman of the BMA’s GPs committee, wrote to 22,000 GPs. [full letter]
- Believes the bill will compromise the role of GPs, and could cause irreparable damage to the relationship between GPs and their patients.
- Believes the bill to be complex, incoherent and not fit for purpose, and almost impossible to implement successfully, given widespread opposition across the NHS workforce.
- Believes that passing the bill will be an irresponsible waste of taxpayers’ money, which will be spent on unnecessary reorganisation rather than on patient care, as well as increasing the running costs of the NHS from the processes of competition, and transaction costs
The chaos that the Lib Dems now find themselves in is illustrated clearly by a post on Liberal Democrat Voice by Andrew Tennant. He’s apparently an unreconstructed 19th century Whig, masquerading as a 21st century liberal. The comments on the post reveal the mess the party has got itself into by refusing to drop the bill.
More to the point, look at the proper detailed analyses done by people who are a lot more knowledgeable than Andrew Tennant, or Andrew Lansley.
- RCGP Report Stage Briefing – Health and Social Care Bill February 2012
- Allyson Pollock explains, line by line, a lot of problems that “Recent amendments put forward by the Liberal Democrats do not address”.
- Statement on Liberal Democrat amendments
Prof Allyson Pollock, David Price, Peter Roderick, and Tim Treuherz
28 February 2012 - Royal College of Physicians, in The Lancet “What began as a ham-fisted attempt to modernise the NHS has become a grotesque political disaster for government.”
- The NHS bill could finish the health service – and David Cameron Polly Toynbee says it as it is.
- A big document by SOSNHS -great source of links Breaking the NHS.
There is one last chance for the Lib Dems to restore their reputation. Lib Dems hope to finally kill health reforms. “Liberal Democrat activists will defy Nick Clegg over the Government’s controversial health reforms by seeking to “kill” them at a party policy-making conference next week.”
Good luck to them. They could save the Lib Dems if they win. Much more importantly, they could save the NHS.
Follow-up
Sunday 4 March. Yet another story of corruption, this time in the Mail on Sunday.
“The head of the NHS regulator that is meant to ensure fairness when private-sector firms bid for public contracts is also the chairman of a huge company whose Health Service business is worth £80 million a year – and set to increase massively.
As the chairman of the NHS Co-operation and Competition Panel (CCP), Lord Carter of Coles is paid £57,000 for two days’ work each week. But his other role, as chairman of the UK branch of the American healthcare firm McKesson, is more generously rewarded. Last year it paid him £799,000.”
“Dr Clare Gerada, chairman of the Royal College of General Practitioners, said: ‘He cannot have any credibility when he is also heading a company with such huge interests in the very contracts his organisation is meant to police.”
See also Conflicts of Interest and NHS reform.
According to a tweet from James Ball
“Politics of the #NHSbill awful for lib dems: only 17% of their current supporters back it – and only 9% of their 2010 voters.”
Sounds plausible. Are you listening, Nick Clegg?
5 March 2012. The emergency motion for the Lib Dem Spring Conference (March 10 -11) has been published. See also the blog of the heroic Dr Charles West for more details. If Clegg manages to defeat this excellent motion, the last chance to save the NHS will be gone.
10 March 2012
Bitterly disappointed by vote at Lib Dem conference, not to debate the motion to drop the NHS bill. Who do I vote for now?
One thing that one can still do is to email all Lib Dem MPs give your views. Here is a list of their email addresses (via Lindy).
bakern@parliament.uk, danny.alexander.mp@parliament.uk, alan.beith.mp@parliament.uk, gordon.birtwistle.mp@parliament.uk, brookea@parliament.uk, braket@parliament.uk, brownej@parliament.uk, hernandeza@parliament.uk, burstowp@parliament.uk, lorely.burt.mp@parliament.uk, cablev@parliament.uk, menzies.campbell.mp@parliament.uk, carmichaela@parliament.uk, nick.clegg.mp@parliament.uk, mike.crockart.mp@parliament.uk, farront@parliament.uk, daveye@parliament.uk, simon.wright.mp@parliament.uk, willottj@parliament.uk, featherstonel@parliament.uk, fosterd@parliament.uk, andrew.george.mp@parliament.uk, duncan.hames.mp@parliament.uk, stephen.gilbert.mp@parliament.uk, stephenwilliamsmp@parliament.uk, kennedyc@parliament.uk, jo.swinson.mp@parliament.uk, julian.huppert.mp@parliament.uk,hunterm@parliament.uk, simon@simonhughes.org.uk, chris.huhne.mp@parliament.uk, martin.horwood.mp@parliament.uk, hemmingj@parliament.uk, david.heath.mp@parliament.uk, hancockm@parliament.uk, pagep@parliament.uk, lambn@parliament.uk, lawsd@parliament.uk, john.leech.mp@parliament.uk, stephen.lloyd.mp@parliament.uk, michaelmooremp@parliament.uk, greg.mulholland.mp@parliament.uk, teathers@parliament.uk, tessa.munt.mp@parliament.uk, john.thurso.mp@parliament.uk, david.ward.mp@parliament.uk, webbs@parliament.uk, williamsmf@parliament.uk, williamsr@parliament.uk, pughj@parliament.uk, reida@parliament.uk, contact@danrogerson.org, susan.hislop@parliament.uk, robert.smith.mp@parliament.uk, stunella@parliament.uk, ian.swales.mp@parliament.uk
And here are email addresses for (most) Lib Dem peers)
williamss@parliament.uk, walmsleyj@parliament.uk, wallacej@parliament.uk, wallacew@parliament.uk, tordoffg@parliament.uk, topeg@parliament.uk, thomascm@parliament.uk, thomass@parliament.uk, stephenn@parliament.uk, smitht@parliament.uk, shipleyj@parliament.uk, shuttd@parliament.uk, sharpm@parliament.uk, scottrc@parliament.uk, robertsr@parliament.uk, rennardc@parliament.uk, randersonj@parliament.uk, palmerm@parliament.uk, oakeshottm@parliament.uk, northoverl@parliament.uk, newbyr@parliament.uk, millers@parliament.uk, methuenr@parliament.uk, methuenr@parliament.uk, maddockd@parliament.uk, maddockd@parliament.uk, maclennanr@parliament.uk, loombar@parliament.uk, linklaterv@parliament.uk, lestera@parliament.uk, leej@parliament.uk, kramers@parliament.uk, jonesn@parliament.uk, ecem@parliament.uk, harrisa@parliament.uk, hamwees@parliament.uk, greavesa@parliament.uk, goodhartw@parliament.uk, germanm@parliament.uk, gardens@parliament.uk, falknerk@parliament.uk, ezrad@parliament.uk, dholakian@parliament.uk, cotterb@parliament.uk, clementjonest@parliament.uk, chidgeyd@parliament.uk, carlilea@parliament.uk, brintons@parliament.uk, willisg@parliament.uk, addingtond@parliament.uk , alderdicej@parliament.uk, allanr@parliament.uk, ashdownp@parliament.uk, barkere@parliament.uk, benjaminf@parliament.uk , bonhamcarterj@parliament.uk
13 March 2012. This is really last chance day. At 11 am, the Lords debate third reading of health bill and at 2 pm the Commons have emergency debate, triggered by the e-petition, which now has more than 173,000 signatures. I sent the following email to all Lib Dem peers and MPs this morning.
|
The idea that the changes to the health bill have solved its problems is simply wrong. Before you vote, please read http://abetternhs.wordpress.com/2012/03/11/40points/ ,
That is written by a working GP who knows what he’s talking about. For the truth about the 49% disaster, read this. There are 27 professional organisations who are against the bill (see here). Do you really understand the implications better than they do? The vote at the lib dem conference gives you the mandate to vote according to your conscience. Please vote to drop the bill and start again. I voted Lib Dem at every election from 2001. If you let us down on the health bill, I will certainly not do so again. David Colquhoun |
16 March 2012. I have learned ( from Lord Shutt) that there will be a 3-line whip on Lib Dem peers to vote against Lord Owen’s amendment. And this despite the vote against the Clegg-Williams motion at the Lib Dem conference last week. This makes the much vaunted party democracy look like a bit of a joke. The only hope now is the bishops. Here is a list of their email addresses. You can also contact them through Dr Éoin Clarke’s site (from where I got the addresses)
bishop@bathwells.anglican.org, bishop@birmingham.anglican.org, chaplain@bishopofblackburn.org.uk, bishop@bristoldiocese.org, bpchester@chester.anglican.org, bishchichester@diochi.org.uk, bishop@bishopofderby.org, durham@durham.anglican.org, langrishm@parliament.uk, bshpglos@glosdioc.org.uk, bishop.christopher@cofeguildford.org.uk, bishop@hereford.anglican.org, bishop.tim@leccofe.org, bishop.lichfield@lichfield.anglican.org, bishopslodge@liverpool.anglican.org, bishop@londin.clara.co.uk, bishop@bishopscourt.manchester.anglican.org, bishop@newcastle.anglican.org, bishop@norwich.anglican.org, bishop@riponleeds-diocese.org.uk, bishop.nigel@stedmundsbury.anglican.org, bishop@bishopofwakefield.org.uk, contact@lambethpalace.org.uk, office@archbishopofyork.org
This is what I sent to them today.
|
Dear Bishop,
You will be aware of the widespread concerns about the commercialisation of the NHS. No fewer than 27 medical organisations have now come out strongly against the bill and it’s clear that, despite (or because of?) over 1000 amendments, it is a real mess. Despite the vote at the Lib Dems conference against the bill, I hear that there will be a 3-line whip in the Lords to force Lib Dem peers to vote against the very sensible proposal by Lord Owen to delay passing of the bill until the government release the assessment of the risks of passing it. This means that the Bishops will be crucial. I would like to ask you seriously to consider voting for Lord Owen’s motion on Monday. The future of the National Health Service lies in your hands Best regards |
18 March 2012. Tomorrow is last hope for stopping the bill in the Lords. The 3-line whip will, I expect, ensure the defeat of Lord David Owen’s excellent amendment. The bill will probably become law. Two tweets express the impending death of the NHS quite poignantly. On 15 March @Heardin London wrote
"For a brief period during 20th century, people gave a fuck and looked after each other. Unfortunately this proved unprofitable."
and today, from @thewritertype,
"Years from now you’ll have to explain to children what the NHS was. Then you’ll have to explain what a LibDem was."
Poetry in 140 characters.
20 March 2012.
|
The hated bill was rammed through in the House of Commons, thanks to support from Lib Dems. .The list of the peers and MPs who will make money out of privatisation is truly scary and deeply corrupt. |
|
This is a slightly-modified version of the article that appeared in BMJ blogs yesterday, but with more links to original sources, and a picture. There are already some comments in the BMJ.
The original article, diplomatically, did not link directly to UCL’s Grand Challenge of Human Wellbeing, a well-meaning initiative which, I suspect, will not prove to be value for money when it comes to practical action.
Neither, when referring to the bad effects of disempowerment on human wellbeing (as elucidated by, among others, UCL’s Michael Marmot), did I mention the several ways in which staff have been disempowered and rendered voiceless at UCL during the last five years. Although these actions have undoubtedly had a bad effect on the wellbeing of UCL’s staff, it seemed a litlle unfair to single out UCL since similar things are happening in most universities. Indeed the fact that it has been far worse at Imperial College (at least in medicine) has probably saved UCL from being denuded. One must be thankful for small mercies.
There is, i think, a lesson to be learned from the fact that formal initiatives in wellbeing are springing up at a time when university managers are set on taking actions that have exactly the opposite effect. A ‘change manager’ is not an adequate substitute for a vote. Who do they imagine is being fooled?
The A to Z of the wellbeing industry
From angelic reiki to patient-centred care
Nobody could possibly be against wellbeing. It would be like opposing motherhood and apple pie. There is a whole spectrum of activities under the wellbeing banner, from the undoubtedly well-meaning patient-centred care at one end, to downright barmy new-age claptrap at the other end. The only question that really matters is, how much of it works?
Let’s start at the fruitcake end of the spectrum.
One thing is obvious. Wellbeing is big business. And if it is no more than a branch of the multi-billion-dollar positive-thinking industry, save your money and get on with your life.
In June 2010, Northamptonshire NHS Foundation Trust sponsored a “Festival of Wellbeing” that included a complementary therapy taster day. In a BBC interview one practitioner used the advertising opportunity, paid for by the NHS, to say “I’m an angelic reiki master teacher and also an angel therapist.” “Angels are just flying spirits, 100 percent just pure light from heaven. They are all around us. Everybody has a guardian angel.” Another said “I am a member of the British Society of Dowsers and use a crystal pendulum to dowse in treatment sessions. Sessions may include a combination of meditation, colour breathing, crystals, colour scarves, and use of a light box.” You couldn’t make it up.
The enormous positive-thinking industry is no better. Barbara Ehrenreich’s book, Smile Or Die: How Positive Thinking Fooled America and the World, explains how dangerous the industry is, because, as much as guardian angels, it is based on myth and delusion. It simply doesn’t work (except for those who make fortunes by promoting it). She argues that it fosters the sort of delusion that gave us the financial crisis (and pessimistic bankers were fired for being right). Her interest in the industry started when she was diagnosed with cancer. She says
”When I was diagnosed, what I found was constant exhortations to be positive, to be cheerful, to even embrace the disease as if it were a gift. If that’s a gift, take me off your Christmas list,”
It is quite clear that positive thinking does nothing whatsoever to prolong your life (Schofield et al 2004; Coyne et al 2007; 2,3), any more than it will cure tuberculosis or cholera. “Encouraging patients to “be positive” only may add to the burden of having cancer while providing little benefit” (Schofield et al 2004). Far from being helpful, it can be rather cruel.
Just about every government department, the NHS, BIS, HEFCE, and NICE, has produced long reports on wellbeing and stress at work. It’s well known that income is correlated strongly with health (Marmot, M., 2004). For every tube stop you go east of Westminster you lose a year of life expectancy (London Health Observatory). It’s been proposed that what matters is inequality of income (Wilkinson & Pickett, 2009). The nature of the evidence doesn’t allow such a firm conclusion (Lynch et al. 2004), but that isn’t really the point. The real problem is that nobody has come up with good solutions. Sadly the recommendations at the ends of all these reports don’t amount to a hill of beans. Nobody knows what to do, partly because pilot studies are rarely randomised so causality is always dubious, and partly because the obvious steps are either managerially inconvenient, ideologically unacceptable, or too expensive.
Take two examples:
Sir Michael Marmot’s famous Whitehall study (Marmot, M., 2004) has shown that a major correlate of illness is lack of control over one’s own fate: disempowerment. What has been done about it?
In universities it has proved useful to managers to increase centralisation and to disempower academics, precisely the opposite of what Marmot recommends.
|
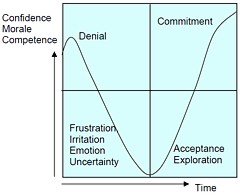
As long as it’s convenient to managers they are not going to change policy. Rather, they hand the job to the HR department which appoints highly paid “change managers,” who add to the stress by sending you stupid graphs that show you emerging from the slough of despond into eternal light once you realise that you really wanted to be disempowered after all. Or they send you on some silly “resilience” course. |
|
A second example comes from debt. According to a BIS report (Mental Capital and Wellbeing), debt is an even stronger risk factor for mental disorder than low income. So what is the government’s response to that? To treble tuition fees to ensure that almost all graduates will stay in debt for most of their lifetime. And this was done despite the fact that the £9k fees will save nothing for the taxpayer: in fact they’ll cost more than the £3k fees. The rise has happened, presumably, because the ideological reasons overrode the government’s own ideas on how to make people happy.
Nothing illustrates better the futility of the wellbeing industry than the response that is reported to have been given to a reporter who posed as an applicant for a “health, safety, and wellbeing adviser” with a local council. When he asked what “wellbeing” advice would involve, a member of the council’s human resources team said: “We are not really sure yet as we have only just added that to the role. We’ll want someone to make sure that staff take breaks, go for walks — that kind of stuff.”
The latest wellbeing notion to re-emerge is the happiness survey. Jeremy Bentham advocated “the greatest happiness for the greatest number,” but neglected to say how you measure it. A YouGov poll asks, “what about your general well-being right now, on a scale from 1 to 10.” I have not the slightest idea about how to answer such a question. As always some things are good, some are bad, and anyway wellbeing relative to whom? Writing this is fun. Trying to solve an algebraic problem is fun. Constant battling with university management in order to be able to do these things is not fun. The whole exercise smacks of the sort of intellectual arrogance that led psychologists in the 1930s to claim that they could sum up a person’s intelligence in a single number. That claim was wrong and it did great social harm.
HEFCE has spent a large amount of money setting up “pilot studies” of wellbeing in nine universities. Only one is randomised, so there will be no evidence for causality. The design of the pilots is contracted to a private company, Robertson Cooper, which declines to give full details but it seems likely that the results will be about as useless as the notorious Durham fish oil “trials”(Goldacre, 2008).
Lastly we get to the sensible end of the spectrum: patient-centred care. Again this has turned into an industry with endless meetings and reports and very few conclusions. Epstein & Street (2011) say
“Helping patients to be more active in consultations changes centuries of physician-dominated dialogues to those that engage patients as active participants. Training physicians to be more mindful, informative, and empathic transforms their role from one characterized by authority to one that has the goals of partnership, solidarity, empathy, and collaboration.”
That’s fine, but the question that is constantly avoided is what happens when a patient with metastatic breast cancer expresses a strong preference for Vitamin C or Gerson therapy, as advocated by the YesToLife charity. The fact of the matter is that the relationship can’t be equal when one party, usually (but not invariably) the doctor, knows a lot more about the problem than the other.
What really matters above all to patients is getting better. Anyone in their right mind would prefer a grumpy condescending doctor who correctly diagnoses their tumour, to an empathetic doctor who misses it. It’s fine for medical students to learn social skills but there is a real danger of so much time being spent on it that they can no longer make a correct diagnosis. Put another way, there is confusion between caring and curing. It is curing that matters most to patients. It is this confusion that forms the basis of the bait and switch tactics (see also here) used by magic medicine advocates to gain the respectability that they crave but rarely deserve.
If, as is only too often the case, the patient can’t be cured, then certainly they should be cared for. That’s a moral obligation when medicine fails in its primary aim. There is a lot of talk about individualised care. It is a buzzword of quacks and also of the libertarian wing which says NICE is too prescriptive. It sounds great, but it helps only if the individualised treatment actually works.
Nobody knows how often medicine fails to be “patient-centred.”. Even less does anyone know whether patient-centred care can improve the actual health of patients. There is a strong tendency to do small pilot trials that are as likely to mislead as inform. One properly randomised trial (Kinmonth et al., 1998) concluded
“those committed to achieving the benefits of patient centred consulting should not lose the focus on disease management.”
Non-randomised studies may produce more optimistic conclusions (e.g. Hojat et al, 2011), but there is no way to tell if this is simply because doctors find it easy to be empathetic with patients who have better outcomes.
Obviously I’m in favour of doctors being nice to patients and to listening to their wishes. But there is a real danger that it will be seen as more important than curing. There is also a real danger that it will open the doors to all sorts of quacks who claim to provide individualised empathic treatment, but end up recommending Gerson therapy for metastatic breast cancer. The new College of Medicine, which in reality is simply a reincarnation of the late unlamented Prince’s Foundation for Integrated Health, lists as its founder Capita, the private healthcare provider that will, no doubt, be happy to back the herbalists and homeopaths in the College of Medicine, and, no doubt, to make a profit from selling their wares to the NHS.
In my own experience as a patient, there is not nearly as much of a problem with patient centred care as the industry makes out. Others have been less lucky, as shown by the mid-Staffordshire disaster (Delamothe, 2010), That seems to have resulted from PR being given priority over patients. Perhaps all that’s needed is to save money on all the endless reports and meetings (“the best substitute for work”), ban use of PR agencies (paid lying) and to spend the money on more doctors and nurses so they can give time to people who need it. This is a job that will be hindered considerably by the government’s proposals to sell off NHS work to private providers who will be happy to make money from junk medicine.
Reference
Wilkinson. R & Pickett, K. 2009 , The Spirit Level, ISBN 978 1 84614 039 6
A footnote on Robertson Cooper and "resilience"
I took up the offer of Robertson Cooper to do their free "resilience" assessment, the company to which HEFCE has paid an undisclosed amount of money.
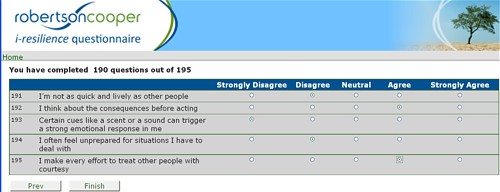
The first problem arose when it asked about your job. There was no option for scientist, mathematician, university or research, so I was forced to choose "education and training". (a funny juxtaposition since training is arguably the antithesis of education). It had 195 questions. mostly as unanswerable as in the YouGov happiness survey. I particularly liked question 124 "I see little point in many of the theoretical models I come across". The theoretical models that I come across most are Markov models for the intramolecular changes in a receptor molecule when it binds a ligand (try, for example, Joint distributions of apparent open and shut times of single-ion channels and maximum likelihood fitting of mechanisms). I doubt the person who wrote the question has ever heard of a model of that sort. The answer to that question (and most of the others) would not be worth the paper they are written on.
The whole exercise struck me as the worst sort of vacuous HR psychobabble. It is worrying that HEFCE thinks it is worth spending money on it.
Follow-up
Having recently been fired from Ofquack, the Complementary and Natural Healthcare Council (CNHC). I found I was missing the constant dribble of double-speak, Then, as luck would have it, a friend emailed me to draw my attention to a lucrative job at Ninewells Hospital, Dundee. On August 11th I put out a tweet, just in case any of my friends were interested.
How to save money. NHS Scorland (Tayside) advertises for homeopathic doctor http://bit.ly/9Ou9Yo Pathetic #fail
After the story appeared in the Daily Express it occurred to me that I should apply. It seems that NHS Scotland
Tayside) is determined to look idiotic in the eyes of the world. They advertised for a homeopathic doctor, The upper level of salary, £68,000 for two sessions a week, is a great deal more than I ever got paid as holder of the established chair of pharmacology at UCL, Then I discovered that a crystallographer, David Briggs (@xtaldave on twitter) had applied for the job. If he can, why not I? I found it hard to match the wit of his supporting statement, but just in case others want to apply, here’s my attempt. The more the merrier.
.
|
As a Fellow of the Royal Society for the last 25 years, and author of a textbook on statistics, I feel sure that I am capable of dealing with the intellectual rigours of handing out placebos to patients. I feel that my academic qualifications, and my authorship of many research papers, including several articles about homeopathy, should more than make up for my lack of formal qualifications in medicine or homeopathy. Indeed I have spent more time than I care to remember on reading the extensive literature on homeopathy. Having some expertise in the statistical analysis of clinical trials, my reading of the literature has equipped me well to impress gullible patients with sciencey sounding words like “succussion”, “energy medicine” and “quantum theory”. As an additional qualification, I have read widely about crystal healing, magnetic bracelets, aura photography and other such fairground paraphernalia which are designed, like homeopathy, to impress those with no knowledge of science or medicine. I have had over two years’ experience of serving on the Conduct and Competence Committee of the Complementary and Natural Healthcare Council, which has provided me with valuable insights into the world of alternative medicine. Indeed I have been told that my name is well known in Clarence House itself. If appointed to this job, I should like to combine it with research in homeopathy. I would approach this by using systems biology, in the hope that proteomics and metabolomics would be able to explain the still mysterious ability of medicines that contain no medicine to satisfy patients. People whom I know at the University of Westminster have proposed to use systems biology to explain Traditional Chinese Medicine, and I imagine that its application to homeopathy will be every bit as successful as theirs. To have cutting edge research of this sort will, I believe, give NHS Scotland a reputation that will spread around the world. I would also propose to save the Tayside PCT a lot of money, something not to be ignored in these hard times. At present, homeopathic pharmacies stock many thousands of sorts of pill. Recognising that the majority of them contain nothing at all, I’d retain the labels but fill all the bottles with sugar pills. This would save huge amounts of time and money, while having no effect at all on the outcome for patients. Despite my lack of formal qualifications, I hope you will agree that I’m qualified intellectually to meet the rigours of your job. |
Follow-up
I was not the only person to follow the example of David Briggs (@xtaldave). So far I’ve seen Dean Burnett (@garboy) on Science Digestive, Peter Harrison on Reality is My Religion, and Torgwen.
Three days on, there are at least eleven applications, and the three earliest ones have been read something like 12.000 times.
18 August 2010. Astonished to receive by snail-mail a straight-faced acknowledgment of my application from NHS Tayside [download pdf]. They ask me to send four copies of my CV and fill in forms for Equal Opportunities and Fitness to Practise. Does this mean I’ve been short-listed? This gets more surreal by the minute.
This is a post about Markovian queuing theory. But hang on, don’t run away. It isn’t so hard.
|
The idea came from my recent experience. On Friday 23 October, I was supposed to have a kidney removed at the Royal Marsden Hospital. At the very last minute the operation was cancelled. That is more irritating than serious. A delay of a few weeks poses no great risk for me. . |

|
The cancellation arose because there was no bed available in the High Dependency Unit (HDU), which is where nephrectomy patients go for a while after the operation. Was this a failure of the NHS? I think not and here’s why
The first reaction of a neighbour to this news was to say "that’s why I have private insurance". Well, wrong actually. For a start, at the Marsden private patients and NHS patients get identical treatment (the only difference on the NHS is that "you don’t get hot and cold running margaritas at your bedside", my surgeon said). And secondly, the provision of emergency beds poses a really difficult problem, which I’ll attempt to explain.
Bed provision raises a fascinating statistical question. How many beds must be available to make sure nobody is ever turned away? The answer, in principle, is an infinite number. In practice it is more than anyone can afford.
The HDU has eleven beds but let’s think about a simpler case to start with. If patients arrived regularly at a fixed rate, and each patient stayed for a fixed length of time. there would be no problem. Say, for example, that a patient arrived regularly at 10 am and 4 pm each day, and suppose that each patient stayed for exactly 46 hours. It’s pretty obvious that you’d need four beds. Each bed could take a patient every two days and there are two patients per day coming in. Allowing two hours for changing beds, all four beds would be occupied for essentially 100 percent of the time, actually 95% = 46 hours/48 hours).
Random arrivals
The problem arises because patients don’t arrive regularly and they don’t stay for a fixed length of time. What happens if patients arrive at random and stay for a random length of time? (We’ll get back to the meaning of ‘random’ in this context later.)
Suppose again that two patients per day arrive on average, and that each patient stays in the HDU for 46 hours on average. So the mean arrival rate, and the mean length of stay in the HDU are the same as in the first example. When there was no randomness, four beds coped perfectly.
But with random arrivals and random length of stay the situation is very different. With four beds, if a queue were allowed to build up, the average number of patients in the queue would be 21 and the average length of time a patient would spend waiting to get a bed would be 10.5 days. This would be an efficient use of resources because every time a bed was vacated it would be filled straight away from the queue. The resources would be used to the maximum possible extent:, 95%. But it would be terrible for patients. The length of the queue would, of course, fluctuate, as shown by this distribution (see below) of the queue length. Occasionally it might reach 100 or more.
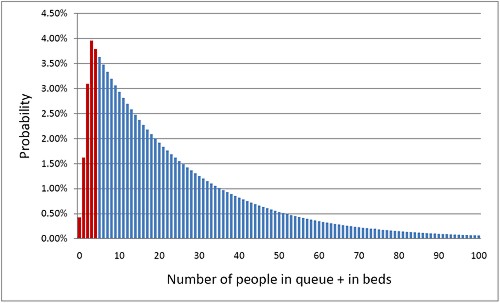
The histogram shows the total number of people in the system.The first five bins (red) represent the probabilities of 0, 1, 2, 3 or 4 beds being occupied. All the rest are in the queue.
What if you can’t queue?
For a High Dependency Unit or an Intensive Care Unit you can’t have a queue. If there is no bed, you are turned away. In the example just described, 91% of patients would have to wait, and that’s impossible in an HDU or ICU. The necessary statistical theory has been done for this case too (it is described as having zero queue capacity). Let’s look at the same case, with 4 beds, mean time between arrival of patients, 0.5 days, mean length of stay 1.917 days (46 hours).
|
In this case there is no queue so the only possibilities are that 0, 1, 2, 3 or all 4 beds are occupied. The relative probabilities of these cases are shown on the right (they add up to 100% because there are no other possibilities). |
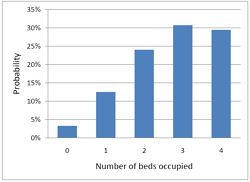
|
Despite the pressure on the unit, the randomness ensures that beds are by no means always occupied. All four are occupied for only 29% of the time and the average occupancy is 2.7 so the resources are used only 68% of the time (rather than 95% when a queue was allowed to form). Worse still, there is a 29% chance of the system being full, so you would be turned away.
So how many beds do you need? Clearly the more beds you have, the smaller the chance of anyone being turned away. But more beds means more cost and less efficiency. This is how it works out in our case.
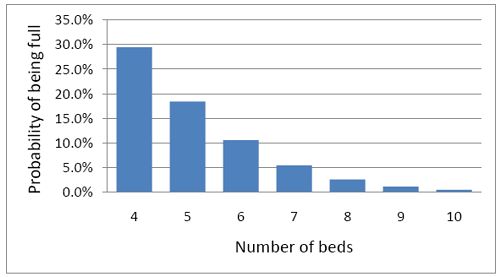
To get the chance of being turned away below 5%, rather than 29%, you’d have to double the number of beds from 4 to 8. But in doing so the beds would not be in use 68% of the time as with 4 beds, but for only 47% of the time.
|
Looked at another way, if you try to increase the utilisation of beds, above 50 or 60%, then the rate at which patients get turned away goes shooting up exponentially. |
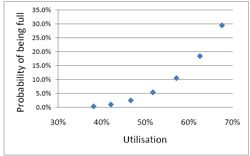
|
This isn’t inefficiency. It is an inevitable consequence of randomness in arrival times and lengths of stay.
A real life example
McManus et al. (2004) looked at all admissions to the medical–surgical Intensive Care Unit (ICU) of a large, urban children’s hospital in the USA during a 2-year period. (Anesthesiology 2004; 100:1271–6. Download pdf). Their Figure 2 shows the monthly average rejection rates mostly vary between 10 and 20%, so there is nothing unusual in there being no bed available in the private US medical system. For a period the rate of rejection reaches disastrous values, up to 47%. This happens, unsurprisingly, at times when the utilisation of beds was high.
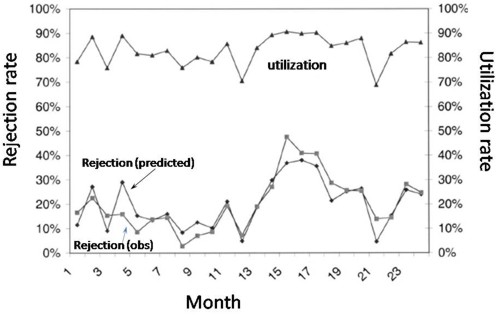
The observed relationship (McManus, Fig. 3) is very much as predicted above.with a very steep (roughly exponential) rise in rejection rate when the beds are in use for more than half the time.
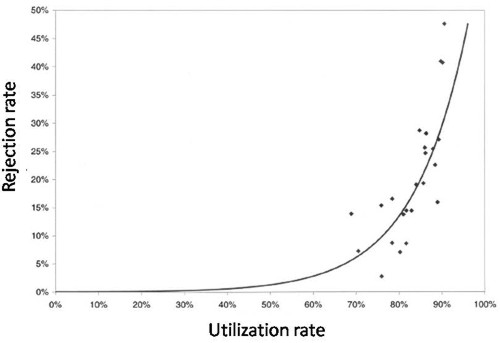
How to do the calculations
You can get the message without reading this section. It’s included for those who want to know a bit more about what we mean when we say that patients arrive at random rather than at fixed intervals, and that durations of stay in the unit have random rather than fixed durations.
Consider the durations of stay in the unit. They are variable in length and the usual way to represent variability is to plot a distribution of the variable quantity. The best known sort of probability distribution is the bell-shaped curve known as the Gaussian distribution. This is shown at the top of the Figure (note that pdf stands for probability density function, not portable document format).
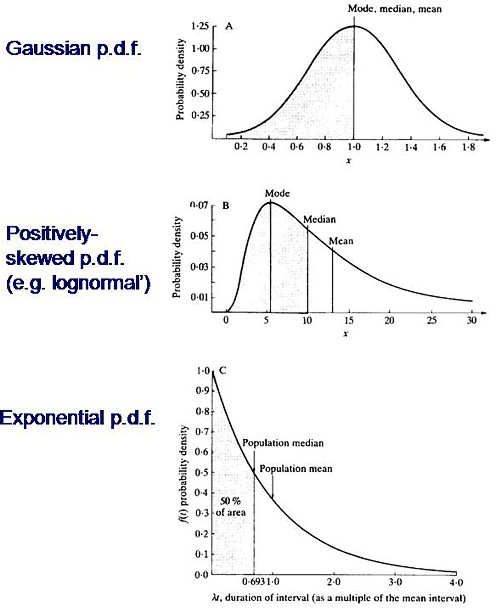
Not every sort of variability is described by a symmetrical bell-shaped curve. Quite often distributions with a positive skew are seen, like the middle example in the Figure. The distribution of incomes in the population have this sort of shape. Notice that more people earn less than average than earn more than average (the median is less than the mean). This can happen because those that earn less than average can’t get much less than average (unless we allow negative incomes), whereas bankers can earn (or at least be paid) a great deal more than average. The most frequent income (the peak of the distribution) is still smaller than the median.
An extreme form of a positively-skewed distribution is shown at the bottom. It is called the exponential distribution (because it has the shape of a decaying exponential curve). If this described personal incomes (and we are heading that way) it would mean that the most frequent income was zero and 63.2% of people earn less than average.
It is this last, rather unusual, sort of distribution that, in the simplest case, describes the lengths of random time intervals. This is getting very close to my day job. If an ion channel has a single open state, the lengths of individual ion channel openings is described by an exponential distribution.
|
The observation of an exponential distribution of durations is what would be predicted for a memoryless process, or Markov process. In the case of an ion channel, memoryless means that the probability of the channel shutting in the next microsecond is the same however long the channel has been open, This is exactly analogous to the fact that the probability of throwing a six with a die is exactly the same at each throw, regardless of how many sixes have been thrown before. |
Andrei A. Markov, 1856-1922 |
It is the simplest definition of a random length of time. For those who have done a bit of statistics, it is worth mentioning that if the number of events per unit time is described by a Poisson distribution, then the interval between events are exponentially-distributed. They are different ways of saying the same thing.
|
The lengths of stays in ICU in the McManus paper were roughly exponentially-distributed (right). The monthly average duration of stay ranged from 2.4 to 5.5 days, and average monthly admission rates to the 18 bed unit ranged from 4.6 to 6.2 patients per day. |
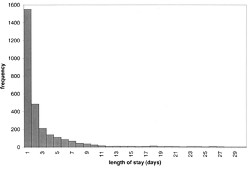
|
The monthly average percentage of patients who were turned away because there were no vacant beds varied widely, ranging from 3% up to a disastrous 47%
A technical note and an analogy with synapses
It’s intriguing to note that, in the simplest case, the time you’d spend waiting in a queue would have a simple exponential distribution (plus a discrete bit for the times when you don’t have to wait at all). The time you have to wait is the sum of all the lengths of stay of the people in front of you, and each of these lengths, in the case we discussing, is exponentially-distributed. If the queue was constant in length you can use a mathematical method known as convolution to show that the distribution of waiting time would follow a gamma distribution, a sort of distribution that goes through a peak, and eventually becomes Gaussian for long queues), However the queue is not fixed in length but its length is random (geometrically-distributed). It turns out that the distribution of the sum of a random number of exponentially distributed times is itself exponential. It is precisely this beautiful theorem that shows why the length of a burst of ion channel openings (which consists of the sum of a random number of exponentially-distributed open times, if you neglect the time spent in short shuttings) is, to a good approximation itself exponential, And that explains why the decay of synaptic currents is often close to following a simple exponential time course.
The calculations
The calculations for these graphs were done with a set of Excel add-in functions, Queueing Toolpak 4.0, which can be downloaded here. If this had been a paper of my own, rather than a blog post written in one weekend, I’d have done the algebra myself, just to be sure, The theory has much in common with that of single ion channels. Transitions between different states of the system can be described by transition rates or probabilities that don’t vary with time. The table, or matrix, of transition probabilities can be used to calculate the results, And if you want to know about the algebra of matrices, you could always apply for our summer workshop. There are some pictures from the workshop here.
Follow-up
Of course it is quite impossible for anyone who was around in the 60s to hear the name of a Russian mathematician without thinking of Tom Lehrer’s totally unjustified slur on another great Russian mathematician, Nicolai Ivanovich Lobachevsky. If you’ve never heard ‘Plagiarize’, you can hear it on Youtube. Sheer genius.
Why the size of the unit matters
This section was added as a result of a comment, below, from a statistician
At first glance one might think that if we quadruple the number of beds to 16 beds rather than 4, and we also quadruple the arrival rate to 8 rather than 2 per day, then the arrival rate per bed is the same and one might expect everything would stay the same.
As you say, it doesn’t.
If queueing was allowed, the mean queue length would be only slightly shorter, 18,7 rather than 20.9, but the mean time spent in the queue would fall from 10.5 days to 2.3 days.
In the more realistic case, with no queuing allowed, the rejection rate would fall from 29.4% to 15.5% and bed utilisation would increase from 68% to 81%. The rejection rate seems to fall roughly as the square root of the number of beds.
Clearly there is an advantage to having a big hospital with a big HDU.
Stochastic processes quite often behave unintuitive ways (unless you’ve spent years developing the right intuition).

Conservatives in the USA have been lying about the NHS on a massive scale. As Simon Hoggart comments today “There are few tribes more loathsome than the American right”.
In the forefront has been a far-right lobby group, Conservatives for Patients’ Rights (CPR). Even I was surprised to read in the Washington Post
“The campaign is being coordinated by CRC Public Relations, the group that masterminded the “Swift boat” attacks against 2004 Democratic presidential candidate, John F. Kerry”
CRC Public Relations is a conservative PR firm previously known as Creative Response Concepts. ‘Creative’ appears to mean ‘lying’, but I guess that is what PR is all about.
The founder of CPR, Rick Scott, has an interesting background. According to Stephen Barrett
“In 1987, he founded and became chief operating officer of a hospital chain that grew into the 23 billion-dollars-a-year Columbia/HCA. In 1997, a few weeks after the FBI raided HCA hospitals in five states, Scott was ousted as CEO and three executives were indicted on charges of Medicare fraud. The FBI’s investigation found that the hospital chain had been overbilling Medicare and giving kickbacks to doctors who steered patients to its hospitals. The overbilling included upcoding lesser procedures to get higher reimbursements and billing for lab tests that were not medically necessary and were not ordered by physicians. The situation was settled with a set of guilty pleas and criminal and civil fines totalling $1.7 billion. The U.S. Department of Justice referred to the matter as the “largest health care fraud case in U.S. history.”
Disgracefully, Karol Sikora, a former oncologist at the Hammersmith Hospital, supported CPR on US television. See Karol Sikora makes a fool of himself at NHSblogdoctor. I quote
“Karol Sikora had been duped by a slick American businessman into providing a “rent-a-quote” service for a notorious right-wing American organisation”
This post was reproduced on the US site, Trusted.MD
Sikora now works for the UK’s only private university and a private cancer treatment company. He is also famous for claiming,
falsely, to be a professor at Imperial College (he has an honorary contract with the Imperial College Hospital Trust but nothing with the University). And for promoting a load of nonsense about
alternative medicine (a lot more on that coming up shortly).
This is why love the NHS
Europe as a whole gets better health care for less money than in the USA. The fact that every US doctor has a financial interest in ordering expensive treatments whether they are needed or not,
is an obscenity. The fact that over 40 million Americans have no insurance is an obscenity (see The brutal truth about America’s healthcare).
Just look at the numbers (Source: WHO/OECD Health Data 2009)
Health spending as a share of GDP.
US 16% UK 8.4%
Public spending on healthcare (% of total spending on healthcare)
US 45% UK 82%
Health spending per head
US $7,290 UK $2,992
Practising physicians (per 1,000 people)
US 2.4 UK 2.5
Nurses (per 1,000 people)
US 10.6 UK 10.0
Acute care hospital beds (per 1,000 people)
US 2.7 UK 2.6
Life expectancy:
US 78 UK 80
Infant mortality (per 1,000 live births)
US 6.7 UK 4.8
My experience
Yes I know this is anecdote, but it matters a lot to me. I already posted a version of this story, but this seems like the time to repeat it.
On December 13th 1984, my wife had a subarachnoid haemorrhage when she was seven months pregnant. After an initial misdiagnosis by an obstetrician at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next morning I was called to see the neurourgeon, the great Alan Crockard. He was sitting surrounded by medical students some of whom I’d taught the previous year. He told me my wife had had a subarachnoid haemorrhage (at 33!) and they would operate straight away. And “I have to ask you, if we can save only the mother or the baby, which shall it be”. It’s as well to write that down because even 24 years later I can’t say it without a lump rising in my throat.
That same day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millimetre from the pituitary on the other. It was a bit tricky but I think we got it”. Obstetricians were in theatre too because all this was done with the baby still in situ
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds). Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. The care was superb. | 
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. She and Andrew were in hospital continuously for more than four months. Not a penny changed hands. Heaven knows what it would have cost in the USA, or even of insurance would have covered such a gargantuan bill.
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew (left) playing cricket in Bangladesh, Feb 2005. |
My own experience is trivial compared with that of Margaret and Andrew, but it has been as near perfect as anyone could wish. I had a lumbar spinal fusion (L3 – L4) in 1995, after several attempts at less drastic solutions. I’ve had two artificial hips. They allowed me to walk across the Alps for my 65th birthday. Then a few trivial things like bilateral hernia and DVT (I had been scanned and was on anticoagulant therapy within 4 hours of walking into UCLH’s Accident and Emergency). And now it looks as though I’ll be getting a partial or total nephrectomy too.
And not a penny has changed hands.
The NHS is a beautiful thing. OK it has has the usual excessive number of managers and HR-bollocks, like most big companies. It isn’t perfect but it is a great deal closer to perfection
than the US system.
 Approaching Seescharte (2600 m) at 08.20, 21 August 2001. Memminger Hütte visible below. With fused vertebrae and right prosthetic hip, thanks to the NHS. (Click for bigger picture.) |
Bush may have gone, but a large fraction of Americans seem to be unrepentant Bush-ites. Almost all of my many friends in the USA think more or less like I do. Even Obama is to the right of most European conservatives, The other 48% are to the right of Attila the Hun. The extent of the polarisation that still exists is nothing short of terrifying.
|
Thanks to the great Aneurin Bevan who established the NHS in 1948 for ordinary people like me, in the face of fierce opposition from the medical establishment.
|
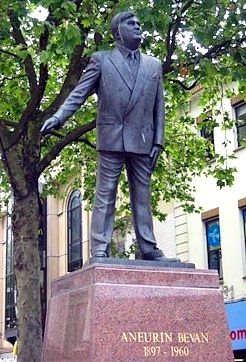 Statue of Bevan in Cardiff |
Ah well, The Daily Mash. is always there when you need a (wry) laugh
Follow-up
Paul Krugman in the New York Times is magnificent as always. In The Swiss Menace he points out that Obama’s scheme is nothing like the NHS anyway, but more like that in Switzerland.
“The plans on the table would, roughly speaking, turn America into Switzerland — which may be occupied by lederhosen-wearing holey-cheese eaters, but wasn’t a socialist hellhole the last time I looked.”
“In Britain, the government itself runs the hospitals and employs the doctors. We’ve all heard scare stories about how that works in practice; these stories are false.”
“So we can do this. At this point, all that stands in the way of universal health care in America are the greed of the medical-industrial complex, the lies of the right-wing propaganda machine, and the gullibility of voters who believe those lies.”
Comparing US and UK cancer statistics . As Ben Goldacre says, “I think you’ll find it’s a bit more complicated than that”. There’s an interesting analysis at Cancer Research UK
The US uses the PSA blood test far more widely than we do in the UK – despite questions over how effective it is at spotting cancers that would actually kill, as opposed to those that cause no symptoms. As a result, the USA has one of the highest recorded rates of prostate cancer in the world.
So although it’s undoubtedly ‘better’ at spotting prostate cancers, it’s also fair to say that some of these Americans will never die from their disease. This ‘overdiagnosis‘ inflates the survival statistics, at the expense of ‘overtreating‘ men – which is expensive and can cause long-term side effects (which can need further treatment).
In fact the age-standardised death rates per 100,000 people are almost the same in the UK (all races) when compared with the USA (whites only). What is different is that far more cases of prostate cancer are diagnosed in the USA. If the rate of ‘real’ (potentially fatal) prostate cancer were similar in both countries then both countries have much the same success in treating it, If, on the other hand, US men had a genuinely higher incidence of real prostate cancer, the US would be doing better, There is no way to distinguish between these two interpretations,