quackademia
‘We know little about the effect of diet on health. That’s why so much is written about it’. That is the title of a post in which I advocate the view put by John Ioannidis that remarkably little is known about the health effects if individual nutrients. That ignorance has given rise to a vast industry selling advice that has little evidence to support it.
The 2016 Conference of the so-called "College of Medicine" had the title "Food, the Forgotten Medicine". This post gives some background information about some of the speakers at this event. I’m sorry it appears to be too ad hominem, but the only way to judge the meeting is via the track record of the speakers.

Quite a lot has been written here about the "College of Medicine". It is the direct successor of the Prince of Wales’ late, unlamented, Foundation for Integrated Health. But unlike the latter, its name is disguises its promotion of quackery. Originally it was going to be called the “College of Integrated Health”, but that wasn’t sufficently deceptive so the name was dropped.
For the history of the organisation, see
Don’t be deceived. The new “College of Medicine” is a fraud and delusion
The College of Medicine is in the pocket of Crapita Capita. Is Graeme Catto selling out?
The conference programme (download pdf) is a masterpiece of bait and switch. It is a mixture of very respectable people, and outright quacks. The former are invited to give legitimacy to the latter. The names may not be familiar to those who don’t follow the antics of the magic medicine community, so here is a bit of information about some of them.
The introduction to the meeting was by Michael Dixon and Catherine Zollman, both veterans of the Prince of Wales Foundation, and both devoted enthusiasts for magic medicne. Zollman even believes in the battiest of all forms of magic medicine, homeopathy (download pdf), for which she totally misrepresents the evidence. Zollman works now at the Penny Brohn centre in Bristol. She’s also linked to the "Portland Centre for integrative medicine" which is run by Elizabeth Thompson, another advocate of homeopathy. It came into being after NHS Bristol shut down the Bristol Homeopathic Hospital, on the very good grounds that it doesn’t work.
Now, like most magic medicine it is privatised. The Penny Brohn shop will sell you a wide range of expensive and useless "supplements". For example, Biocare Antioxidant capsules at £37 for 90. Biocare make several unjustified claims for their benefits. Among other unnecessary ingredients, they contain a very small amount of green tea. That’s a favourite of "health food addicts", and it was the subject of a recent paper that contains one of the daftest statistical solecisms I’ve ever encountered
"To protect against type II errors, no corrections were applied for multiple comparisons".
If you don’t understand that, try this paper.
The results are almost certainly false positives, despite the fact that it appeared in Lancet Neurology. It’s yet another example of broken peer review.
It’s been know for decades now that “antioxidant” is no more than a marketing term, There is no evidence of benefit and large doses can be harmful. This obviously doesn’t worry the College of Medicine.
Margaret Rayman was the next speaker. She’s a real nutritionist. Mixing the real with the crackpots is a standard bait and switch tactic.
Eleni Tsiompanou, came next. She runs yet another private "wellness" clinic, which makes all the usual exaggerated claims. She seems to have an obsession with Hippocrates (hint: medicine has moved on since then). Dr Eleni’s Joy Biscuits may or may not taste good, but their health-giving properties are make-believe.
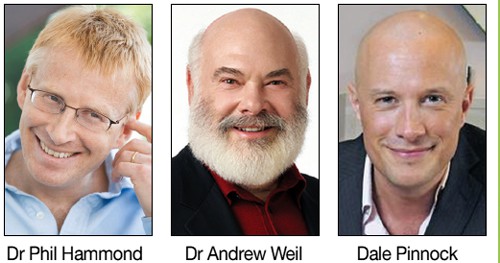
Andrew Weil, from the University of Arizona
gave the keynote address. He’s described as "one of the world’s leading authorities on Nutrition and Health". That description alone is sufficient to show the fantasy land in which the College of Medicine exists. He’s a typical supplement salesman, presumably very rich. There is no excuse for not knowing about him. It was 1988 when Arnold Relman (who was editor of the New England Journal of Medicine) wrote A Trip to Stonesville: Some Notes on Andrew Weil, M.D..
“Like so many of the other gurus of alternative medicine, Weil is not bothered by logical contradictions in his argument, or encumbered by a need to search for objective evidence.”
This blog has mentioned his more recent activities, many times.
Alex Richardson, of Oxford Food and Behaviour Research (a charity, not part of the university) is an enthusiast for omega-3, a favourite of the supplement industry, She has published several papers that show little evidence of effectiveness. That looks entirely honest. On the other hand, their News section contains many links to the notorious supplement industry lobby site, Nutraingredients, one of the least reliable sources of information on the web (I get their newsletter, a constant source of hilarity and raised eyebrows). I find this worrying for someone who claims to be evidence-based. I’m told that her charity is funded largely by the supplement industry (though I can’t find any mention of that on the web site).
Stephen Devries was a new name to me. You can infer what he’s like from the fact that he has been endorsed byt Andrew Weil, and that his address is "Institute for Integrative Cardiology" ("Integrative" is the latest euphemism for quackery). Never trust any talk with a title that contains "The truth about". His was called "The scientific truth about fats and sugars," In a video, he claims that diet has been shown to reduce heart disease by 70%. which gives you a good idea of his ability to assess evidence. But the claim doubtless helps to sell his books.
Prof Tim Spector, of Kings College London, was next. As far as I know he’s a perfectly respectable scientist, albeit one with books to sell, But his talk is now online, and it was a bit like a born-again microbiome enthusiast. He seemed to be too impressed by the PREDIMED study, despite it’s statistical unsoundness, which was pointed out by Ioannidis. Little evidence was presented, though at least he was more sensible than the audience about the uselessness of multivitamin tablets.
Simon Mills talked on “Herbs and spices. Using Mother Nature’s pharmacy to maintain health and cure illness”. He’s a herbalist who has featured here many times. I can recommend especially his video about Hot and Cold herbs as a superb example of fantasy science.
Annie Anderson, is Professor of Public Health Nutrition and
Founder of the Scottish Cancer Prevention Network. She’s a respectable nutritionist and public health person, albeit with their customary disregard of problems of causality.
Patrick Holden is chair of the Sustainable Food Trust. He promotes "organic farming". Much though I dislike the cruelty of factory farms, the "organic" industry is largely a way of making food more expensive with no health benefits.
The Michael Pittilo 2016 Student Essay Prize was awarded after lunch. Pittilo has featured frequently on this blog as a result of his execrable promotion of quackery -see, in particular, A very bad report: gamma minus for the vice-chancellor.
Nutritional advice for patients with cancer. This discussion involved three people.
Professor Robert Thomas, Consultant Oncologist, Addenbrookes and Bedford Hospitals, Dr Clare Shaw, Consultant Dietitian, Royal Marsden Hospital and Dr Catherine Zollman, GP and Clinical Lead, Penny Brohn UK.
Robert Thomas came to my attention when I noticed that he, as a regular cancer consultant had spoken at a meeting of the quack charity, “YestoLife”. When I saw he was scheduled tp speak at another quack conference. After I’d written to him to point out the track records of some of the people at the meeting, he withdrew from one of them. See The exploitation of cancer patients is wicked. Carrot juice for lunch, then die destitute. The influence seems to have been temporary though. He continues to lend respectability to many dodgy meetings. He edits the Cancernet web site. This site lends credence to bizarre treatments like homeopathy and crystal healing. It used to sell hair mineral analysis, a well-known phony diagnostic method the main purpose of which is to sell you expensive “supplements”. They still sell the “Cancer Risk Nutritional Profile”. for £295.00, despite the fact that it provides no proven benefits.
Robert Thomas designed a food "supplement", Pomi-T: capsules that contain Pomegranate, Green tea, Broccoli and Curcumin. Oddly, he seems still to subscribe to the antioxidant myth. Even the supplement industry admits that that’s a lost cause, but that doesn’t stop its use in marketing. The one randomised trial of these pills for prostate cancer was inconclusive. Prostate Cancer UK says "We would not encourage any man with prostate cancer to start taking Pomi-T food supplements on the basis of this research". Nevertheless it’s promoted on Cancernet.co.uk and widely sold. The Pomi-T site boasts about the (inconclusive) trial, but says "Pomi-T® is not a medicinal product".
There was a cookery demonstration by Dale Pinnock "The medicinal chef" The programme does not tell us whether he made is signature dish "the Famous Flu Fighting Soup". Needless to say, there isn’t the slightest reason to believe that his soup has the slightest effect on flu.
In summary, the whole meeting was devoted to exaggerating vastly the effect of particular foods. It also acted as advertising for people with something to sell. Much of it was outright quackery, with a leavening of more respectable people, a standard part of the bait-and-switch methods used by all quacks in their attempts to make themselves sound respectable. I find it impossible to tell how much the participants actually believe what they say, and how much it’s a simple commercial drive.
The thing that really worries me is why someone like Phil Hammond supports this sort of thing by chairing their meetings (as he did for the "College of Medicine’s" direct predecessor, the Prince’s Foundation for Integrated Health. His defence of the NHS has made him something of a hero to me. He assured me that he’d asked people to stick to evidence. In that he clearly failed. I guess they must pay well.
Follow-up
|
“Statistical regression to the mean predicts that patients selected for abnormalcy will, on the average, tend to improve. We argue that most improvements attributed to the placebo effect are actually instances of statistical regression.”
“Thus, we urge caution in interpreting patient improvements as causal effects of our actions and should avoid the conceit of assuming that our personal presence has strong healing powers.” |
In 1955, Henry Beecher published "The Powerful Placebo". I was in my second undergraduate year when it appeared. And for many decades after that I took it literally, They looked at 15 studies and found that an average 35% of them got "satisfactory relief" when given a placebo. This number got embedded in pharmacological folk-lore. He also mentioned that the relief provided by placebo was greatest in patients who were most ill.
Consider the common experiment in which a new treatment is compared with a placebo, in a double-blind randomised controlled trial (RCT). It’s common to call the responses measured in the placebo group the placebo response. But that is very misleading, and here’s why.
The responses seen in the group of patients that are treated with placebo arise from two quite different processes. One is the genuine psychosomatic placebo effect. This effect gives genuine (though small) benefit to the patient. The other contribution comes from the get-better-anyway effect. This is a statistical artefact and it provides no benefit whatsoever to patients. There is now increasing evidence that the latter effect is much bigger than the former.
How can you distinguish between real placebo effects and get-better-anyway effect?
The only way to measure the size of genuine placebo effects is to compare in an RCT the effect of a dummy treatment with the effect of no treatment at all. Most trials don’t have a no-treatment arm, but enough do that estimates can be made. For example, a Cochrane review by Hróbjartsson & Gøtzsche (2010) looked at a wide variety of clinical conditions. Their conclusion was:
“We did not find that placebo interventions have important clinical effects in general. However, in certain settings placebo interventions can influence patient-reported outcomes, especially pain and nausea, though it is difficult to distinguish patient-reported effects of placebo from biased reporting.”
In some cases, the placebo effect is barely there at all. In a non-blind comparison of acupuncture and no acupuncture, the responses were essentially indistinguishable (despite what the authors and the journal said). See "Acupuncturists show that acupuncture doesn’t work, but conclude the opposite"
So the placebo effect, though a real phenomenon, seems to be quite small. In most cases it is so small that it would be barely perceptible to most patients. Most of the reason why so many people think that medicines work when they don’t isn’t a result of the placebo response, but it’s the result of a statistical artefact.
Regression to the mean is a potent source of deception
The get-better-anyway effect has a technical name, regression to the mean. It has been understood since Francis Galton described it in 1886 (see Senn, 2011 for the history). It is a statistical phenomenon, and it can be treated mathematically (see references, below). But when you think about it, it’s simply common sense.
You tend to go for treatment when your condition is bad, and when you are at your worst, then a bit later you’re likely to be better, The great biologist, Peter Medawar comments thus.
|
"If a person is (a) poorly, (b) receives treatment intended to make him better, and (c) gets better, then no power of reasoning known to medical science can convince him that it may not have been the treatment that restored his health"
(Medawar, P.B. (1969:19). The Art of the Soluble: Creativity and originality in science. Penguin Books: Harmondsworth). |
This is illustrated beautifully by measurements made by McGorry et al., (2001). Patients with low back pain recorded their pain (on a 10 point scale) every day for 5 months (they were allowed to take analgesics ad lib).
The results for four patients are shown in their Figure 2. On average they stay fairly constant over five months, but they fluctuate enormously, with different patterns for each patient. Painful episodes that last for 2 to 9 days are interspersed with periods of lower pain or none at all. It is very obvious that if these patients had gone for treatment at the peak of their pain, then a while later they would feel better, even if they were not actually treated. And if they had been treated, the treatment would have been declared a success, despite the fact that the patient derived no benefit whatsoever from it. This entirely artefactual benefit would be the biggest for the patients that fluctuate the most (e.g this in panels a and d of the Figure).
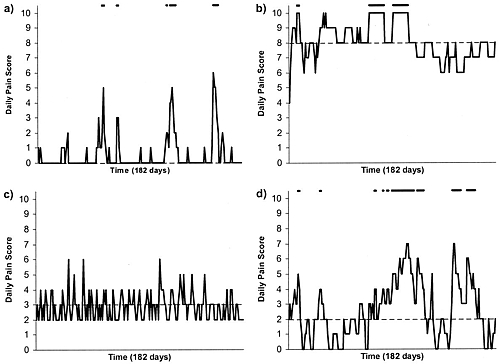
Figure 2 from McGorry et al, 2000. Examples of daily pain scores over a 6-month period for four participants. Note: Dashes of different lengths at the top of a figure designate an episode and its duration.
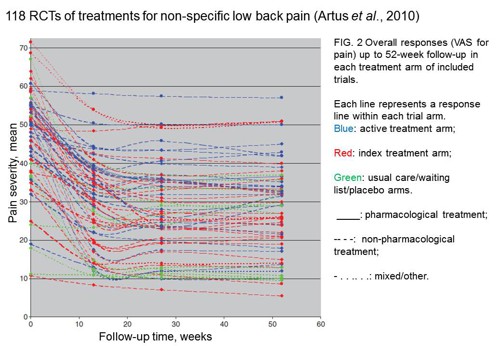
The effect is illustrated well by an analysis of 118 trials of treatments for non-specific low back pain (NSLBP), by Artus et al., (2010). The time course of pain (rated on a 100 point visual analogue pain scale) is shown in their Figure 2. There is a modest improvement in pain over a few weeks, but this happens regardless of what treatment is given, including no treatment whatsoever.
FIG. 2 Overall responses (VAS for pain) up to 52-week follow-up in each treatment arm of included trials. Each line represents a response line within each trial arm. Red: index treatment arm; Blue: active treatment arm; Green: usual care/waiting list/placebo arms. ____: pharmacological treatment; – – – -: non-pharmacological treatment; . . .. . .: mixed/other.
The authors comment
"symptoms seem to improve in a similar pattern in clinical trials following a wide variety of active as well as inactive treatments.", and "The common pattern of responses could, for a large part, be explained by the natural history of NSLBP".
In other words, none of the treatments work.
This paper was brought to my attention through the blog run by the excellent physiotherapist, Neil O’Connell. He comments
"If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery."
O’Connell has discussed the matter in recent paper, O’Connell (2015), from the point of view of manipulative therapies. That’s an area where there has been resistance to doing proper RCTs, with many people saying that it’s better to look at “real world” outcomes. This usually means that you look at how a patient changes after treatment. The hazards of this procedure are obvious from Artus et al.,Fig 2, above. It maximises the risk of being deceived by regression to the mean. As O’Connell commented
"Within-patient change in outcome might tell us how much an individual’s condition improved, but it does not tell us how much of this improvement was due to treatment."
In order to eliminate this effect it’s essential to do a proper RCT with control and treatment groups tested in parallel. When that’s done the control group shows the same regression to the mean as the treatment group. and any additional response in the latter can confidently attributed to the treatment. Anything short of that is whistling in the wind.
Needless to say, the suboptimal methods are most popular in areas where real effectiveness is small or non-existent. This, sad to say, includes low back pain. It also includes just about every treatment that comes under the heading of alternative medicine. Although these problems have been understood for over a century, it remains true that
|
"It is difficult to get a man to understand something, when his salary depends upon his not understanding it."
Upton Sinclair (1935) |
Responders and non-responders?
One excuse that’s commonly used when a treatment shows only a small effect in proper RCTs is to assert that the treatment actually has a good effect, but only in a subgroup of patients ("responders") while others don’t respond at all ("non-responders"). For example, this argument is often used in studies of anti-depressants and of manipulative therapies. And it’s universal in alternative medicine.
There’s a striking similarity between the narrative used by homeopaths and those who are struggling to treat depression. The pill may not work for many weeks. If the first sort of pill doesn’t work try another sort. You may get worse before you get better. One is reminded, inexorably, of Voltaire’s aphorism "The art of medicine consists in amusing the patient while nature cures the disease".
There is only a handful of cases in which a clear distinction can be made between responders and non-responders. Most often what’s observed is a smear of different responses to the same treatment -and the greater the variability, the greater is the chance of being deceived by regression to the mean.
For example, Thase et al., (2011) looked at responses to escitalopram, an SSRI antidepressant. They attempted to divide patients into responders and non-responders. An example (Fig 1a in their paper) is shown.
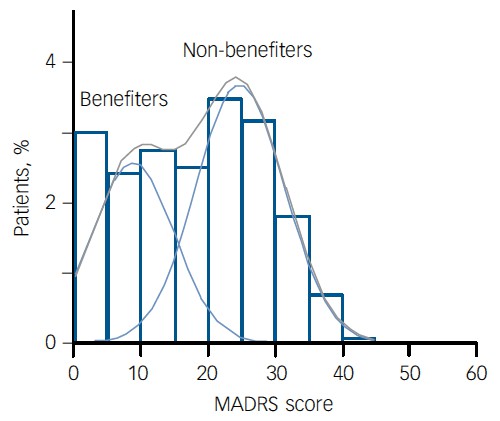
The evidence for such a bimodal distribution is certainly very far from obvious. The observations are just smeared out. Nonetheless, the authors conclude
"Our findings indicate that what appears to be a modest effect in the grouped data – on the boundary of clinical significance, as suggested above – is actually a very large effect for a subset of patients who benefited more from escitalopram than from placebo treatment. "
I guess that interpretation could be right, but it seems more likely to be a marketing tool. Before you read the paper, check the authors’ conflicts of interest.
The bottom line is that analyses that divide patients into responders and non-responders are reliable only if that can be done before the trial starts. Retrospective analyses are unreliable and unconvincing.
Some more reading
Senn, 2011 provides an excellent introduction (and some interesting history). The subtitle is
"Here Stephen Senn examines one of Galton’s most important statistical legacies – one that is at once so trivial that it is blindingly obvious, and so deep that many scientists spend their whole career being fooled by it."
The examples in this paper are extended in Senn (2009), “Three things that every medical writer should know about statistics”. The three things are regression to the mean, the error of the transposed conditional and individual response.
You can read slightly more technical accounts of regression to the mean in McDonald & Mazzuca (1983) "How much of the placebo effect is statistical regression" (two quotations from this paper opened this post), and in Stephen Senn (2015) "Mastering variation: variance components and personalised medicine". In 1988 Senn published some corrections to the maths in McDonald (1983).
The trials that were used by Hróbjartsson & Gøtzsche (2010) to investigate the comparison between placebo and no treatment were looked at again by Howick et al., (2013), who found that in many of them the difference between treatment and placebo was also small. Most of the treatments did not work very well.
Regression to the mean is not just a medical deceiver: it’s everywhere
Although this post has concentrated on deception in medicine, it’s worth noting that the phenomenon of regression to the mean can cause wrong inferences in almost any area where you look at change from baseline. A classical example concern concerns the effectiveness of speed cameras. They tend to be installed after a spate of accidents, and if the accident rate is particularly high in one year it is likely to be lower the next year, regardless of whether a camera had been installed or not. To find the true reduction in accidents caused by installation of speed cameras, you would need to choose several similar sites and allocate them at random to have a camera or no camera. As in clinical trials. looking at the change from baseline can be very deceptive.
Statistical postscript
Lastly, remember that it you avoid all of these hazards of interpretation, and your test of significance gives P = 0.047. that does not mean you have discovered something. There is still a risk of at least 30% that your ‘positive’ result is a false positive. This is explained in Colquhoun (2014),"An investigation of the false discovery rate and the misinterpretation of p-values". I’ve suggested that one way to solve this problem is to use different words to describe P values: something like this.
|
P > 0.05 very weak evidence
P = 0.05 weak evidence: worth another look P = 0.01 moderate evidence for a real effect P = 0.001 strong evidence for real effect |
But notice that if your hypothesis is implausible, even these criteria are too weak. For example, if the treatment and placebo are identical (as would be the case if the treatment were a homeopathic pill) then it follows that 100% of positive tests are false positives.
Follow-up
12 December 2015
It’s worth mentioning that the question of responders versus non-responders is closely-related to the classical topic of bioassays that use quantal responses. In that field it was assumed that each participant had an individual effective dose (IED). That’s reasonable for the old-fashioned LD50 toxicity test: every animal will die after a sufficiently big dose. It’s less obviously right for ED50 (effective dose in 50% of individuals). The distribution of IEDs is critical, but it has very rarely been determined. The cumulative form of this distribution is what determines the shape of the dose-response curve for fraction of responders as a function of dose. Linearisation of this curve, by means of the probit transformation used to be a staple of biological assay. This topic is discussed in Chapter 10 of Lectures on Biostatistics. And you can read some of the history on my blog about Some pharmacological history: an exam from 1959.
This article has appeared, in nearly identical form, on the UK Conversation . You can leave comments there or here.
A constitutional monarch is purely ceremonial and plays no part in politics. Well actually in the UK it isn’t quite as simple as that. The first problem is that we have no constitution. Things haven’t changed much since the 19th century when Walter Bagehot said "the Sovereign has, under a constitutional monarchy… three rights—the right to be consulted, the right to encourage, the right to warn."
These are not inconsiderable powers in a country which is meant to be run by elected representatives. But nobody knows how these powers are used: it is all done in secret. Well, almost all. Charles, Prince of Wales, has been unusually public in expressing his views. He told a conference at St James’s Palace “I was accused once of being the enemy of the Enlightenment” “I felt proud of that.” That’s a remarkable point of view for someone who, if he succeeds, will become the patron of that product of the age of enlightenment, the Royal Society.
I have no doubt that Prince Charles means well. He can’t be blamed for his lack of education. But his views on medicine date from a few centuries ago, and he has lost no opportunity to exploit his privileged position to proclaim them.
Euphemisms for quackery
He set up the Prince’s Foundation for Integrated Health (PFIH) to promote his views. ( “Integrated”, in this context, is, of course, just the latest euphemism for “alternative” or “quack”.) When the Foundation collapsed because of a financial scandal in 2010, it was replaced by the “College of Medicine”. The name changed, but not the people behind it. Initially this phoenix was to be named the “College of Integrated Health”, but by this time the prince’s views on medicine had become sufficiently discredited that the word “integrated” was quickly dropped. This might be thought less than frank, but it is just employment of the classic bait and switch technique, beloved by used car salesmen.
His views were well publicised in a PFIH publication, “Complementary Healthcare: a Guide for Patients”. That volume either omitted or misrepresented the evidence about the one question that matters most to patients – does the treatment work or not? It caused me to write a much shorter, but more accurate, version, the Patients’ Guide to Magic Medicine. The PFIH guide was arguably a danger to public health. When, very properly, it was criticised by Edzard Ernst, a letter was sent from from the prince’s private secretary to Ernst’s vice-chancellor, Steve Smith. Instead of defending Ernst’s public spirited action, Smith instituted disciplinary proceedings against Ernst that lasted for a year. The prince had intervened directly in the affairs of the university. Steve Smith was rewarded with a knighthood in 2011.
None of this criticism has dimmed the prince’s enthusiasm for barmy medical ideas. He is well known to write many letters to government ministers to try to persuade them to adopt his ideas in a whole range of areas. In July 2013, the Minister of Health, Jeremy Hunt, visited the prince at Clarence House. The visit was reported to be to persuade the minister to defend homeopathy, though it was more likely to have been to press the case to confer a government stamp of approval on herbalists and traditional Chinese Medicine practitioners by giving them statutory regulation. This is a matter that was recently raised again in parliament by Charles’ greatest ally, David Tredinnick MP (Con, Bosworth) who got into trouble for charging astrology software to expenses. We shall never know what pressure was applied. A ruling of the Information Commissioner judged, reasonably enough, that there was public interest in knowing what influences were being brought to bear on public policy. But the Attorney General overruled the judgement on the grounds that “Disclosure of the correspondence could damage The Prince of Wales’ ability to perform his duties when he becomes King.” That, of course, is exactly what we are worried about.
Influence on politics
The prince’s influence seems to be big in the Department of Health (DH). He was given £37,000 of taxpayers’ money to produce his guide, and an astonishing £900,000 to prepare the ground for the setting up of the hapless self-regulator, the Complementary and Natural Healthcare Council (CNHC, also known as Ofquack). When NHS Choices (itself set up by DH to assess evidence) tried to rewrite its web page about that most discredited of all forms of quackery, homeopathy, officials in DH referred the new advice to Michael Dixon, the medical director of the Prince’s Foundation and, were it not for the Freedom of Information act, the DH would have caused inaccurate information to be provided. The DH has a chief medical officer and two scientific advisors, but prefers to take the advice of the Prince of Wales.
The Prince of Wales’ business, Duchy Originals, has been condemned by the Daily Mail, (of all places) for selling unhealthy foods. And when his business branched into selling quack “detox” and herbal nonsense he found himself censured by both the MHRA and the Advertising Standards Authority (ASA) for making unjustifiable medical claims for these products.
Ainsworth’s homeopathic pharmacy is endorsed by both Prince Charles and the Queen: it has two Royal Warrants. They sell “homeopathic vaccines” for meningitis, measles, rubella and whooping cough. These “vaccines” contain nothing whatsoever so they are obviously a real danger to public health. Despite the fact that Ainsworth’s had already been censured by the ASA in 2011 for selling similar products, Ainsworth’s continued to recommend them with a “casual disregard for the law”. The regulator (the MHRA) failed to step in to stop them until it was eventually stirred into action by a young BBC reporter, Sam Smith, made a programme for BBC South West. Then, at last, the somnolent regulator was stirred into action. The MHRA “told Ainsworths to stop advertising a number of products” (but apparently not to stop making them or selling them). They still sell Polonium metal 30C and Swine Meningitis 36C, and a booklet that recommends homeopathic “vaccination”. Ainsworth’s sales are no doubt helped by the Royal Warrants. The consequence is that people may die of meningitis. In 2011, the MHRA Chief Executive Professor Kent Woods, was knighted.
It runs in the family
The Prince of Wales is not the only member of the royal family to be obsessed with bizarre forms of medicine. The first homeopath to the British royal family, Frederick Quin, was a son of the Duchess of Devonshire (1765-1824). Queen Mary (1865-1953), wife of King George V, headed the fundraising efforts to move and expand the London Homeopathic Hospital.
King George VI was so enthusiastic that in 1948 conferred the royal title on the London Homeopathic Hospital. The Queen Mother loved homeopathy too (there is no way to tell whether this contributed to her need for a colostomy in the 1960s).
The present Queen’s homeopathic physician is Peter Fisher, who is medical director of what, until recently was called the Royal London Homeopathic Hospital (RLHH). In 2010 that hospital was rebranded as the Royal London Hospital for Integrated Medicine (RLHIM) in another unsubtle bait and switch move.
|
The RLHIM is a great embarrassment to the otherwise excellent UCLH Trust. It has been repeatedly condemned by the Advertising Standards Authority for making false claims. As a consequence, it has been forced to withdraw all of its patient information. The patron of the RLHIM is the Queen, not the Prince of Wales. It is hard to imagine that this anachronistic institution would still exist if it were not for the influence, spoken or unspoken, of the Queen. Needless to say we will never be told. |
 The Queen and Peter Fisher Observer 8 April 2007 |
The attorney general, while trying to justify the secrecy of Charles’ letters, said
“It is a matter of the highest importance within our constitutional framework that the Monarch is a politically neutral figure”.
Questions about health policy are undoubtedly political, and the highly partisan interventions of the prince in the political process make his behaviour unconstitutional. They endanger the monarchy itself. Whether that matters depends on how much you value tradition and how much you value the tourist business generated by the Gilbert & Sullivan flummery at which royals excel.
The least that one can ask of the royal family is that they should not endanger the health of the nation. If I wanted to know the winner of the 2.30 at Ascot, I’d ask a royal. For any question concerning science or medicine I’d ask someone with more education.
Here is some more interesting reading
Michael Baum’s “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong”
Gerald Weissman’s essay Homeopathy: Holmes, Hogwarts, and the Prince of Wales.
Channel 4 TV documentary HRH “meddling in politics”
Observer April 2007 "Royals’ favoured hospital at risk as homeopathy backlash gathers pace. The Queen loves it. But alternative medicine centre’s future looks uncertain as more NHS trusts axe funding"
Follow-up
Anesthesia & Analgesia is the official journal of the International Anesthesia Research Society. In 2012 its editor, Steven Shafer, proposed a head-to-head contest between those who believe that acupuncture works and those who don’t. I was asked to write the latter. It has now appeared in June 2013 edition of the journal [download pdf]. The pro-acupuncture article written by Wang, Harris, Lin and Gan appeared in the same issue [download pdf].
Acupuncture is an interesting case, because it seems to have achieved greater credibility than other forms of alternative medicine, despite its basis being just as bizarre as all the others. As a consequence, a lot more research has been done on acupuncture than on any other form of alternative medicine, and some of it has been of quite high quality. The outcome of all this research is that acupuncture has no effects that are big enough to be of noticeable benefit to patients, and it is, in all probablity, just a theatrical placebo.
After more than 3000 trials, there is no need for yet more. Acupuncture is dead.

Acupuncture is a theatrical placebo
David Colquhoun (UCL) and Steven Novella (Yale)
Anesthesia & Analgesia, June 2013 116:1360-1363.
Pain is a big problem. If you read about pain management centres you might think it had been solved. It hasn’t. And when no effective treatment exists for a medical problem, it leads to a tendency to clutch at straws. Research has shown that acupuncture is little more than such a straw.
Although it is commonly claimed that acupuncture has been around for thousands of years, it hasn’t always been popular even in China. For almost 1000 years it was in decline and in 1822 Emperor Dao Guang issued an imperial edict stating that acupuncture and moxibustion should be banned forever from the Imperial Medical Academy.
Acupuncture continued as a minor fringe activity in the 1950s. After the Chinese Civil War, the Chinese Communist Party ridiculed traditional Chinese medicine, including acupuncture, as superstitious. Chairman Mao Zedong later revived traditional Chinese Medicine as part of the Great Proletarian Cultural Revolution of 1966 (Atwood, 2009). The revival was a convenient response to the dearth of medically-trained people in post-war China, and a useful way to increase Chinese nationalism. It is said that Chairman Mao himself preferred Western medicine. His personal physician quotes him as saying “Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine” Li {Zhisui Li. Private Life Of Chairman Mao: Random House, 1996}.
The political, or perhaps commercial, bias seems to still exist. It has been reported by Vickers et al. (1998) (authors who are sympathetic to alternative medicine) that
"all trials [of acupuncture] originating in China, Japan, Hong Kong, and Taiwan were positive"(4).
Acupuncture was essentially defunct in the West until President Nixon visited China in 1972. Its revival in the West was largely a result of a single anecdote promulgated by journalist James Reston in the New York Times, after he’d had acupuncture in Beijing for post-operative pain in 1971. Despite his eminence as political journalist, Reston had no scientific background and evidently didn’t appreciate the post hoc ergo propter hoc fallacy, or the idea of regression to the mean.
After Reston’s article, acupuncture quickly became popular in the West. Stories circulated that patients in China had open heart surgery using only acupuncture (Atwood, 2009). The Medical Research Council (UK) sent a delegation, which included Alan Hodgkin, to China in 1972 to investigate these claims , about which they were skeptical. In 2006 the claims were repeated in 2006 in a BBC TV program, but Simon Singh (author of Fermat’s Last Theorem) discovered that the patient had been given a combination of three very powerful sedatives (midazolam, droperidol, fentanyl) and large volumes of local anaesthetic injected into the chest. The acupuncture needles were purely cosmetic.
Curiously, given that its alleged principles are as bizarre as those on any other sort of pre-scientific medicine, acupuncture seemed to gain somewhat more plausibility than other forms of alternative medicine. The good thing about that is that more research has been done on acupuncture than on just about any other fringe practice.
The outcome of this research, we propose, is that the benefits of acupuncture, if any, are too small and too transient to be of any clinical significance. It seems that acupuncture is little or no more than a theatrical placebo. The evidence for this conclusion will now be discussed.
Three things that are not relevant to the argument
There is no point in discussing surrogate outcomes such as fMRI studies or endorphine release studies until such time as it has been shown that patients get a useful degree of relief. It is now clear that they don’t.
There is also little point in invoking individual studies. Inconsistency is a prominent characteristic of acupuncture research: the heterogeneity of results poses a problem for meta-analysis. Consequently it is very easy to pick trials that show any outcome whatsoever. Therefore we shall consider only meta-analyses.
The argument that acupuncture is somehow more holistic, or more patient-centred, than medicine seems us to be a red herring. All good doctors are empathetic and patient-centred. The idea that empathy is restricted to those who practice unscientific medicine seems both condescending to doctors, and it verges on an admission that empathy is all that alternative treatments have to offer.
There is now unanimity that the benefits, if any, of acupuncture for analgesia, are too small to be helpful to patients.
Large multicenter clinical trails conducted in Germany {Linde et al., 2005; Melchart et, 2005; Haake et al, 2007, Witt et al, 2005), and in the United States {Cherkin et al, 2009) consistently revealed that verum (or true) acupuncture and sham acupuncture treatments are no different in decreasing pain levels across multiple chronic pain disorders: migraine, tension headache, low back pain, and osteoarthritis of the knee.
If, indeed, sham acupuncture is no different from real acupuncture the apparent improvement that may be seen after acupuncture is merely a placebo effect. Furthermore it shows meridians don’t exist, so the "theory" memorized by qualified acupuncturists is just myth. All that remains to be discussed is whether or not the placebo effect is big enough to be useful, and whether it is ethical to prescribe placebos.
Some recent meta-analyses have found that there may be a small difference between sham and real acupuncture. Madsen Gøtzsche & Hróbjartsson {2009) looked at thirteen trials with 3025 patients, in which acupuncture was used to treat a variety of painful conditions. There was a small difference between ‘real’ and sham acupuncture (it didn’t matter which sort of sham was used), and a somewhat bigger difference between the acupuncture group and the no-acupuncture group. The crucial result was that even this bigger difference corresponded to only a 10 point improvement on a 100 point pain scale. A consensus report (Dworkin, 2009) that a change of this sort should be described as a “minimal” change or “little change”. It isn’t big enough for the patient to notice much effect.
The acupuncture and no-acupuncture groups were, of course, not blind to the patients and neither were they blind to the practitioner giving the treatment. It isn’t possible to say whether the observed difference is a real physiological action or whether it’s a placebo effect of a rather dramatic intervention. Interesting though it would be to know this, it matters not a jot, because the effect just isn’t big enough to produce any tangible benefit.
Publication bias is likely to be an even greater problem for alternative medicine than it is for real medicine, so it is particularly interesting that the result just described has been confirmed by authors who practise, or sympathise with, acupuncture. Vickers et al. (2012) did a meta-analysis for 29 RCTs, with 17,922 patients. The patients were being treated for a variety of chronic pain conditions. The results were very similar to those of Madsen et al.{2009). Real acupuncture was better than sham, but by a tiny amount that lacked any clinical significance. Again there was a somewhat larger difference in the non-blind comparison of acupuncture and no-acupuncture, but again it was so small that patients would barely notice it.
Comparison of these two meta-analyses shows how important it is to read the results, not just the summaries. Although the outcomes were similar for both, the spin on the results in the abstracts (and consequently the tone of media reports) was very different.
An even more extreme example of spin occurred in the CACTUS trial of acupuncture for " ‘frequent attenders’ with medically unexplained symptoms” (Paterson et al., 2011). In this case, the results showed very little difference even between acupuncture and no-acupuncture groups, despite the lack of blinding and lack of proper controls. But by ignoring the problems of multiple comparisons the authors were able to pick out a few results that were statistically significant, though trivial in size. But despite this unusually negative outcome, the result was trumpeted as a success for acupuncture. Not only the authors, but also their university’s PR department and even the Journal editor issued highly misleading statements. This gave rise to a flood of letters to the British Journal of General Practice and much criticism on the internet.
From the intellectual point of view it would be interesting to know if the small difference between real and sham acupuncture found in some, but not all, recent studies is a genuine effect of acupuncture or whether it is a result of the fact that the practitioners are never blinded, or of publication bias. But that knowledge is irrelevant for patients. All that matters for them is whether or not they get a useful degree of relief.
There is now unanimity between acupuncturists and non-acupuncturists that any benefits that may exist are too small to provide any noticeable benefit to patients. That being the case it’s hard to see why acupuncture is still used. Certainly such an accumulation of negative results would result in the withdrawal of any conventional treatment.
Specific conditions
Acupuncture should, ideally, be tested separately for effectiveness for each individual condition for which it has been proposed (like so many other forms of alternative medicine, that’s a very large number). Good quality trials haven’t been done for all of them. It’s unlikely that acupuncture works for rheumatoid arthritis, stopping smoking, irritable bowel syndrome or for losing weight. And there is no good reason to think it works for addictions, asthma, chronic pain, depression, insomnia, neck pain, shoulder pain or frozen shoulder, osteoarthritis of the knee, sciatica, stroke or tinnitus and many other conditions (Ernst et al., 2011).
In 2009, the UK’s National Institute for Clinical Excellence (NICE) did recommend both acupuncture and chiropractic for back pain. This exercise in clutching at straws caused something of a furore. In the light of NICE’s judgement the Oxford Centre for Evidence-based medicine updated its analysis of acupuncture for back pain. Their verdict was
“Clinical bottom line. Acupuncture is no better than a toothpick for treating back pain.”
The paper by Artus et al. (2010) is of particular interest for the problem of back pain. Their Fig 2 shows that there is a modest improvement in pain scores after treatment, but much the same effect, with the same time course is found regardless of what treatment is given, and even with no treatment at all. They say
“we found evidence that these responses seem to follow a common trend of early rapid improvement in symptoms that slows down and reaches a plateau 6 months after the start of treatment, although the size of response varied widely. We found a similar pattern of improvement in symptoms following any treatment, regardless of whether it was index, active comparator, usual care or placebo treatment”.
It seems that most of what’s being seen is regression to the mean. And that is very likely to be the main reason why acupuncture sometimes appears to work when it doesn’t.
Although the article by Wang et al (2012) was written to defend the continued use of acupuncture, the only condition for which they claim that there is any reasonably strong evidence is for post-operative nausea and vomiting (PONV). It would certainly be odd if a treatment that had been advocated for such a wide variety of conditions turned out to work only for PONV. Nevertheless, let’s look at the evidence.
The main papers that are cited to support the efficacy of acupuncture in alleviation of PONV are all from the same author: Lee & Done (1999), and two Cochrane reviews, Lee & Done (2004), updated in Lee & Fan (2009). We need only deal with this latest updated meta-analysis.
Although the authors conclude “P6 acupoint stimulation prevented PONV”, closer examination shows that this conclusion is very far from certain. Even taken at face value, a relative risk of 0.7 can’t be described as “prevention”. The trials that were included were not all tests of acupuncture but included several other more or less bizarre treatments (“acupuncture, electro-acupuncture, transcutaneous nerve stimulation, laser stimulation, capsicum plaster, an acu-stimulation device, and acupressure”). The number needed to treat varied from a disastrous 34 to a poor 5 for patients with control rates of PONV of 10% and 70% respectively.
The meta-analysis showed, on average, similar effectiveness for acupumcture and anti-emetic drugs. The problem is that the effectiveness of drugs is in doubt because an update to the Cochrane review has been delayed (Carlisle, 2012) by the discovery of major fraud by a Japanese anesthetist, Yoshitaka Fujii (Sumikawa, 2012). It has been suggested that metclopramide barely works at all (Bandolier, 2012; Henzi, 1999).
Of the 40 trials (4858 participants) that were included; only four trials reported adequate allocation concealment. Ninety percent of trials were open to bias from this source. Twelve trials did not report all outcomes. The opportunities for bias are obvious. The authors themselves describe all estimates as being of “Moderate quality” which is defined this: “Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate”. That being the case, perhaps the conclusion should have been “more research needed”. In fact almost all trials of alternative medicines seem to end up with the conclusion that more research is needed.
Conclusions
It is clear from meta-analyses that results of acupuncture trials are variable and inconsistent, even for single conditions. After thousands of trials of acupuncture, and hundreds of systematic reviews (Ernst et al., 2011), arguments continue unabated. In 2011, Pain carried an editorial which summed up the present situation well.
“Is there really any need for more studies? Ernst et al. (2011) point out that the positive studies conclude that acupuncture relieves pain in some conditions but not in other very similar conditions. What would you think if a new pain pill was shown to relieve musculoskeletal pain in the arms but not in the legs? The most parsimonious explanation is that the positive studies are false positives. In his seminal article on why most published research findings are false, Ioannidis (2005) points out that when a popular but ineffective treatment is studied, false positive results are common for multiple reasons, including bias and low prior probability.”
Since it has proved impossible to find consistent evidence after more than 3000 trials, it is time to give up. It seems very unlikely that the money that it would cost to do another 3000 trials would be well-spent.
A small excess of positive results after thousands of trials is most consistent with an inactive intervention. The small excess is predicted by poor study design and publication bias. Further, Simmons et al (2011) demonstrated that exploitation of "undisclosed flexibility in data collection and analysis" can produce statistically positive results even from a completely nonexistent effect. With acupuncture in particular there is documented profound bias among proponents (Vickers et al., 1998). Existing studies are also contaminated by variables other than acupuncture – such as the frequent inclusion of "electroacupuncture" which is essentially transdermal electrical nerve stimulation masquerading as acupuncture.
The best controlled studies show a clear pattern – with acupuncture the outcome does not depend on needle location or even needle insertion. Since these variables are what define "acupuncture" the only sensible conclusion is that acupuncture does not work. Everything else is the expected noise of clinical trials, and this noise seems particularly high with acupuncture research. The most parsimonious conclusion is that with acupuncture there is no signal, only noise.
The interests of medicine would be best-served if we emulated the Chinese Emperor Dao Guang and issued an edict stating that acupuncture and moxibustion should no longer be used in clinical practice.
No doubt acupuncture will continue to exist on the High Streets where they can be tolerated as a voluntary self-imposed tax on the gullible (as long as they don’t make unjustified claims).
|
REFERENCES
|
|
|
1. Acupuncture Centre. . About Acupuncture. Available at: http://www.acupuncturecentre.org/aboutacupuncture.html. Accessed March 30, 2013 |
|
|
2. Atwood K. “Acupuncture Anesthesia”: a Proclamation from Chairman Mao (Part IV). Available at: http://www.sciencebasedmedicine.org/index.php/acupuncture-anesthesia-a-proclamation-from-chairman-mao-part-iv/. Accessed September 2, 2012 |
|
|
3. Li Z Private Life of Chairman Mao: The Memoirs of Mao’s Personal Physician. 1996 New York: Random House |
|
|
4. Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials. 1998;19:159–66 Available at: http://bit.ly/WqVGWN. Accessed September 2, 2012 |
|
|
5. Reston J. Now, About My Operation in Peking; Now, Let Me Tell You About My Appendectomy in Peking … The New York Times. 1971 Available at: http://select.nytimes.com/gst/abstract.html?res=FB0D11FA395C1A7493C4AB178CD85F458785F9. Accessed March 30, 2013 |
|
|
6. Atwood K. “Acupuncture anesthesia”: a proclamation from chairman Mao (part I). Available at: http://www.sciencebasedmedicine.org/index.php/acupuncture-anesthesia-a-proclamation-of-chairman-mao-part-i/. Accessed September 2, 2012 |
|
|
7. Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes MG, Weidenhammer W, Willich SN, Melchart D. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293:2118–25 |
|
|
8. Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes M, Hummelsberger J, Irnich D, Weidenhammer W, Willich SN, Linde K. Acupuncture in patients with tension-type headache: randomised controlled trial. BMJ. 2005;331:376–82 |
|
|
9. Haake M, Müller HH, Schade-Brittinger C, Basler HD, Schäfer H, Maier C, Endres HG, Trampisch HJ, Molsberger A. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–8 |
|
|
10. Witt C, Brinkhaus B, Jena S, Linde K, Streng A, Wagenpfeil S, Hummelsberger J, Walther HU, Melchart D, Willich SN. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366:136–43 |
|
|
11. Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, Delaney K, Hawkes R, Hamilton L, Pressman A, Khalsa PS, Deyo RA. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169:858–66 |
|
|
12. Madsen MV, Gøtzsche PC, Hróbjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ. 2009;338:a3115 |
|
|
13. Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S, Burke LB, Cowan P, Farrar JT, Hertz S, Raja SN, Rappaport BA, Rauschkolb C, Sampaio C. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–44 |
|
|
14. Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, Sherman KJ, Witt CM, Linde K. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–53 |
|
|
15. Paterson C, Taylor RS, Griffiths P, Britten N, Rugg S, Bridges J, McCallum B, Kite G. Acupuncture for ‘frequent attenders’ with medically unexplained symptoms: a randomised controlled trial (CACTUS study). Br J Gen Pract. 2011;61:e295–e305 |
|
|
16. . Letters in response to Acupuncture for ‘frequent attenders’ with medically unexplained symptoms. Br J Gen Pract. 2011;61 Available at: http://www.ingentaconnect.com/content/rcgp/bjgp/2011/00000061/00000589. Accessed March 30, 2013 |
|
|
17. Colquhoun D. Acupuncturists show that acupuncture doesn’t work, but conclude the opposite: journal fails. 2011 Available at: https://www.dcscience.net/?p=4439. Accessed September 2, 2012 |
|
|
18. Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011;152:755–64 |
|
|
19. Colquhoun D. NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself. 2009 Available at: https://www.dcscience.net/?p=1516. Accessed September 2, 2012 |
|
|
20. Colquhoun D. The NICE fiasco, part 3. Too many vested interests, not enough honesty. 2009 Available at: https://www.dcscience.net/?p=1593. Accessed September 2, 2012 |
|
|
21. Bandolier. . Acupuncture for back pain—2009 update. Available at: http://www.medicine.ox.ac.uk/bandolier/booth/painpag/Chronrev/Other/acuback.html. Accessed March 30, 2013 |
|
|
22. Artus M, van der Windt DA, Jordan KP, Hay EM. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology (Oxford). 2010;49:2346–56 |
|
|
23. Wang S-M, Harris RE., Lin Y-C, Gan TJ. Acupuncture in 21st century anesthesia: is there a needle in the haystack? Anesth Analg. 2013;116:1356–9 |
|
|
24. Lee A, Done ML. The use of nonpharmacologic techniques to prevent postoperative nausea and vomiting: a meta-analysis. Anesth Analg. 1999;88:1362–9 |
|
|
25. Lee A, Done ML. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2004:CD003281 |
|
|
26. Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2009:CD003281 |
|
|
27. Carlisle JB. A meta-analysis of prevention of postoperative nausea and vomiting: randomised controlled trials by Fujii etal. compared with other authors. Anaesthesia. 2012;67:1076–90 |
|
|
28. Sumikawa K. The results of investigation into Dr.Yoshitaka Fujii’s papers. Report of the Japanese Society of Anesthesiologists Special Investigation Committee. http://www.anesth.or.jp/english/pdf/news20120629.pdf |
|
|
29. Bandolier. . Metoclopramide is ineffective in preventing postoperative nausea and vomiting. Available at: http://www.medicine.ox.ac.uk/bandolier/band71/b71-8.html. Accessed March 30, 2013 |
|
|
30. Henzi I, Walder B, Tramèr MR. Metoclopramide in the prevention of postoperative nausea and vomiting: a quantitative systematic review of randomized, placebo-controlled studies. Br J Anaesth. 1999;83:761–71 |
|
|
31. Hall H. Acupuncture’s claims punctured: not proven effective for pain, not harmless. Pain. 2011;152:711–2 |
|
|
32. Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2:e124 |
|
|
33. Simmons JP, Leif DN, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol Sci. 2011;22:1359–66 |
Follow-up
30 May 2013 Anesthesia & Analgesia has put the whole paper on line. No paywall now!
9 June 2013. Since this page was posted on May 30, it has had over 20,000 page views. Not bad.
26 July 2013. The Observer had a large double-page spread about acupuncture. It was written by David Derbyshire, largely on the basis of this article.
26 December 2013
Over christmas the flow of stuff that misrepresents the "thousands of years" of Chinese medicine has continued unabated. Of course one expects people who are selling Chinese herbs and acupuncture to lie. All businesses do. One does not expect such misrepresentation from British Columbia, Cardiff University School of medicine, or from Yale University. I left a comment on the Yale piece. Whether it passes moderation remains to be seen. Just in case, here it is.
One statement is undoubtedly baseless ““If it’s still in use after a thousand years there must be something right,” It’s pretty obvious to the most casual observer that many beliefs that have been round for a thousand years have proved to be utterly wrong.
In any case, it’s simply not true that most “Traditional” Chinese medicine has been around for thousands of years. Acupuncture was actually banned by the Emperor Dao Guang in 1822. The sort of Chinese medicine that is sold (very profitably) to the west was essentially dead in China until it was revived by Mao as part of the great proletarian cultural revolution (largely to stir up Chinese nationalism at that time). Of course he didn’t use it himself.
This history has been documented in detail now, and it surprises me to see it misrepresented, yet again, from a Yale academic.
Of course there might turn out to be therapeutically useful chemicals in Chinese herbs (it has happened with artemesinin). But it is totally irresponsible to pretend that great things are coming in the absence of good RCTs in human patients.
Yale should be ashamed of PR like this. And so should Cardiff University. It not only makes the universities look silly. It corrupts the whole of the rest of these institutions. Who knows how much more of their PR is mere puffery.
18 January 2014. I checked the Yale posting and found that the comment, above, had indeed been deleted. There is little point in having comments if you are going to delete anything that’s mildly critical. It is simply dishonest.
The College of Medicine is well known to be the reincarnation of the late unlamented Prince of Wales Foundation for Integrated Health. I labelled it as a Fraud and Delusion, but that was perhaps over-generous. It seems to be morphing into a major operator in the destruction of the National Health Service through its close associations with the private health industry.
Their 2012 Conference was held on 3rd May. It has a mixture of speakers, some quite sound, some outright quacks. It’s a typical bait and switch event. You can judge its quality by the fact that the picture at the top of the page that advertises the conference shows Christine Glover, a homeopathic pharmacist who makes a living by selling sugar pills to sick people (and a Trustee of the College of Medicine).
Her own company’s web site says
The approaches are, of course, based on sugar pills. The claim is untrue and dangerous. My name for that is fraud. |
 |
When the "College of Medicine" started it was a company, but on January 30th 2012, it was converted to being a charity. But the Trustees of the charity are the same people as the directors of the company. They are all advocates of ineffective quack medicine. The contact is named as Linda Leung, who was Operations Director of the Prince’s Foundation until it closed, and then became Company Secretary for the “College of Medicine”.
The trustees of the charity are the same people who were directors of the company
- Dr Michael Dixon, general practitioner. Michael Dixon was Medical Director of the Prince’s Foundation until it closed down.
- Professor George Lewith, is Professor of Health Research in the Complementary Medicine Research Unit, University of Southampton. He was a Foundation Fellow of the Prince’s Foundation until it closed down. Much has been written about him here.
- Professor David Peters. is Professor of Integrated Healthcare and Clinical Director at the University of Westminster’s School of Integrated Health; He’s famous for allowing dowsing with a pendulum as a method of diagnosis for treatment with unproven herbal medicines,
He was a Foundation Fellow of the Prince’s Foundation until it closed down. - Mrs Christine Glover is a pharmacist who sells homeopathic pills. She was a Foundation Fellow of the Prince’s Foundation until it closed down.
The involvement of Capita
According to their web site
"A Founder of the College of Medicine is Capita."
Still more amazingly, the CEO of the College of Medicine is actually an employee of Capita too.
"Mark Ratnarajah is interim CEO of the College of Medicine as well as Business Director at Capita Health and Wellbeing."

|
That isn’t the end of it. The vice-president of the College of Medicine is Dr Harry Brunjes. There is an article about him in the May 2012 issue of Director Magazine. It has to be said that he doesn’t sound like a man with much interest in the National Health Service.. |
Within 9 years of graduating he set up in private practice in Harley Street. Five years later he set up Premier Medical, which, after swallowing a couple of rivals, he sold to Capita for £60 million. He is now recorded in a Companies House document as Dr Henry Otto Brunjes, a director of Capita Health Holdings Limited. This company owns all the shares in Capita Health and Wellbeing Limited, and it is, in turn, owned by Capita Business Services Limited. And they are owned by Capita Holdings Limited. I do hope that this baroquely complicated array of companies with no employees has nothing to do with tax avoidance.
Capita is, of course, a company with a huge interest in the privatisation of health care. It also has a pretty appalling record for ripping off the taxpayer.
It has long been known in Private Eye, as “Crapita” and “the world’s worst outsourcing firm”.
Capita were responsible for of the multimillion pound failed/delayed IT project for the NHS and HMRC. They messed up on staff administration services at Leicester Hospitals NHS Trust and the BBC where staff details were lost. They failed to provide sufficient computing systems for the Criminal Records Bureau, which caused lengthy delays. Capita were also involved in the failure of the Individual Learning Accounts following a £60M over-spend. And most recently, they have caused the near collapse of court translation services after their acquisition of Applied Language Services.
With allies like that, perhaps the College of Medicine hardly needs enemies. No doubt Capita will be happy to provide the public with quackery for an enormous fee from the taxpayer.
 |
One shouldn’t be surprised that the College is involved in Andrew Lansley’s attempts to privatise healthcare. Michael Dixon, Chair of the College of Medicine, also runs the "NHS Alliance", almost the only organisation that supported the NHS Bill. The quackery at his own practice defies belief (some it is described here). |
One would have thought that such a close association with a company with huge vested interests would not be compatible with charitable status. I’ve asked the Charity Commission about that. The Charity commission, sadly, makes no judgements about the worthiness of the objects of the charities it endorses. All sorts of dangerous quack organisations are registered charities, like, for example, Yes to Life.
Secrecy at the College of Medicine
One of the big problems about the privatisation of medicine and education is that you can’t use the Freedom of Information Act to discover what they are up to. A few private companies try to abide by that act, despite not being obliged to do so. But the College of Medicine is not one of them.
Capita They refuse to disclose anything about their relationship with Capita. I asked I asked Graeme Catto, who is a friend (despite the fact that I think he’s wrong). I got nothing.
"Critical appraisal" I also asked Catto for the teaching materials used on a course that they ran about "critical appraisal". Any university is obliged, by the decision of the Information Tribunal, to produce such material on request. The College of Medicine refused, point blank. What, one wonders, have they got to hide? Their refusal strikes me as deeply unethical.
The course (costing £100) on Critical Appraisal, ran on February 2nd 2012. The aims are "To develop introductory skills in the critical appraisal of randomised controlled trials (RCTs) and systematic reviews (SRs)". That sounds good. Have they had a change of heart about testing treatments?
But, as always, you have to look at who is running the course. Is it perhaps a statistician with expertise in clinical trials? Or is it a clinician with experience in running trials? There are plenty of people with this sort of expertise. But no, It is being run by a pharmacist, Karen Pilkington, from that hotbed of unscientific medicine, the University of Westminster.
Pilkington originally joined the University of Westminster as manager for a 4-year project to review the evidence on complementary therapies (funded by the Department of Health). All of her current activities centre round alternative medicine and most of her publications are in journals that are dedicated to alternative medicine. She teaches "Critical Appraisal" at Westminster too, so I should soon have the teaching materials, despite the College’s attempts to conceal them.
Three people who ought to know better
Ore has to admire, however grudgingly, the way that the quacks who run the College of Medicine have managed to enlist the support of several people who really should know better. I suppose they have been duped by that most irritating characteristic of quacks, the tendency to pretend they have the monopoly on empathetic treatment of patients. We all agree that empathy is good, but every good doctor has it. One problem seems to be that senior medical people are not very good at using Google. They don’t do their homework.

|
Professor Sir Graeme Catto MD DSc FRCP FMedSci FRSE is president of the College of Medicine. He’s Emeritus Professor of Medicine at the University of Aberdeen. He was President of the General Medical Council from 2002 to 2009, Pro Vice-Chancellor, University of London and Dean of Guy’s, King’s and St Thomas’ medical school between 2000 and 2005. He’s nice and well-meaning chap, but he doesn’t seem to know much about what’s going on in the College. |

|
Professor Sir Ian Kennedy LLD, FBA, FKC, FUCL, Hon.DSc(Glasgow), Hon.FRCP is vice-president of the College. Among many other things he is Emeritus Professor of Health Law, Ethics and Policy at University College London. He was Chair of the Healthcare Commission until 2003, when it merged with other regulators to form the Care Quality Commission. No doubt he can’t be blamed for the recent parlous performence of the CQC. |

|
Professor Aidan Halligan MA, MD, FRCOG, FFPHM, MRCPI Since March 200y he has been Director of Education at University College London Hospitals. From 2003 until 2005, he was Deputy Chief Medical Officer for England, with responsibility for issues of clinical governance, patient safety and quality of care. He’s undoubtedly a well-meaning man, but so focussed on his (excellent) homelessness project that he seems immune to the company he keeps. Perhaps the clue lies in the fact that when I asked him what he thought of Lansely’s health bill, he seemed to quite like it. |
It seems to me to be incomprehensible that these three people should be willing to sign a letter in the British Medical Journal in defence of the College, with co-signatories George Lewith (about whom much has been written here) and the homeopath Christine Glover. In so doing, they betray medicine, they betray reason, and most important of all, they betray patients. Perhaps they have spent too much time sitting on very important committees and not enough time with patients.
The stated aims of the College sound good.
"A force that combines scientific knowledge, clinical expertise and the patient’s own perspective. A force that will re-define what good medicine means − renewing the traditional values of service, commitment and compassion and creating a more holistic, patient-centred, preventative approach to healthcare."
But what they propose to do about it is, with a few exceptions, bad. They try to whip up panic by exaggerating the crisis in the NHS. There are problems of course, but they result largely from under-funding (we still spend less on healthcare than most developed countries), and from the progressive involvement of for-profit commercial companies, like Capita. The College has the wrong diagnosis and the wrong solution. How do they propose to take care of an aging population? Self-care and herbal medicines seem to be their solution.
|
The programme for the College’s workshop shows it was run by herbalist Simon Mills and by Dick Middleton an employee of the giant herbal company, Schwabe. You can see Middleton attempting to defend misleading labelling of herbal products on YouTube, opposed by me. |
|
It seems that the College of Medicine are aiding and abetting the destruction of the National Health Service. That makes me angry.(here’s why)
I can end only with the most poignant tweet in the run up to the passing of the Health and Social Care Act. It was from someone known as @HeardInLondon, on March 15th
"For a brief period during 20th century, people gave a fuck & looked after each other. Unfortunately this proved unprofitable." #SaveOurNHS
— HeardinLondon (@HeardinLondon) March 13, 2012
"For a brief period during 20th century, people gave a fuck and looked after each other. Unfortunately this proved unprofitable."
Unprofitable for Crapita, that is.
Follow-up
5 May 2012. Well well, if there were any doubt about the endarkenment values of the College, I see that the Prince of Wales, the Quacktitioner Royal himself, gave a speech at the College’s conference.
"”I have been saying for what seems a very long time that until we develop truly integrated systems – not simply treating the symptoms of disease, but actively creating health, putting the patient at the heart of the process by incorporating our core human elements of mind, body and spirit – we shall always struggle, in my view, with an over-emphasis on mechanistic, technological approaches.”
Of course we all want empathy. The speech, as usual, contributes precisely nothing.
12 June 2012. Oh my, how did I manage to miss the fact the the College’s president, Professor Sir Graeme Catto, is also a Crapita eployee. It’s over a year since he was apponted to Capita’s clinical governance board he says "  In a rapidly growing health and wellbeing marketplace, delivering best practice in clinical governance is of utmost importance. I look forward to working with the team at Capita to assist them with continuing to adopt a best in class approach.". The operative word is "marketplace".
In a rapidly growing health and wellbeing marketplace, delivering best practice in clinical governance is of utmost importance. I look forward to working with the team at Capita to assist them with continuing to adopt a best in class approach.". The operative word is "marketplace".
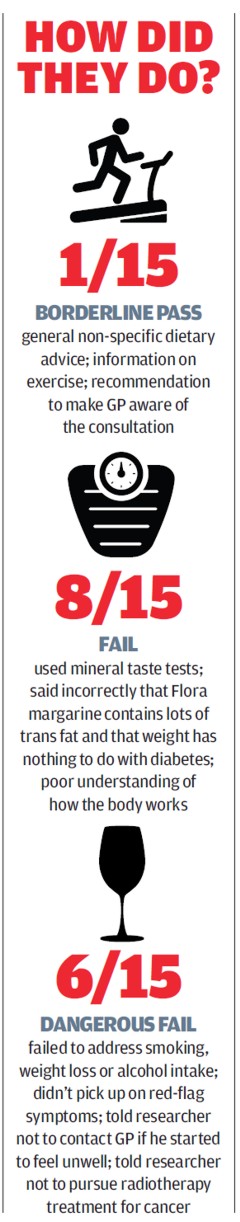
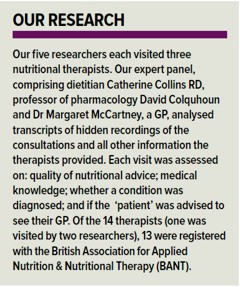
Our undercover investigation finds evidence of nutritional therapists giving out advice that could seriously harm patients’ health
That’s the title of an article in February’s Which? magazine. (That’s similar to Consumer Reports in the USA).
“When Which? sent researchers to investigate the quality of advice from nutritional therapists, some was so bad that patients’ health was put at risk. One nutritional therapist advised against surgery and radiotherapy to treat cancer, while another ‘diagnosed’ a problem with adrenal glands without any blood-test results. Some also used unproven testing, such as iridology or mineral testing, to identify problems or diagnose conditions.”
"We sent five undercover researchers to visit three nutritional therapists each. Every researcher was equipped with a specific health-related scenario: Helen (46) and Sarah (40), recently diagnosed with Ductal Carcinoma In Situ (DCIS), the most common type of non-invasive breast cancer; Mark (56) and Linda (52), suffering with serious fatigue for the past three months; and Emily (31), trying unsuccessfully to conceive for more than a year."
|
Sarah, posing as a patient diagnosed with DCIS, visited a nutritional therapist who advised her to delay treatment recommended by her oncologist (a lumpectomy and a course of radiotherapy). The therapist suggested that Sarah follow a no-sugar diet for three to six months and told her, ‘cancer lives off sugar; if you feed it sugar it’s going to thrive. If we starve the cancer of sugar then you have a better opportunity of the cancer going away’. When Sarah asked whether the cancer could progress during this time the therapist said it was a ‘gamble’. Dr Margaret McCartney, from our panel of experts, says: ‘If cancer treatment were as simplistic as cutting out sugar, surely we would have discovered a cure. This advice is highly irresponsible.’ Our experts rated this consultation as a ‘dangerous fail’." The Patients’ Guide to magic medicine defined “Nutritional therapy: self-styled ‘nutritionists’ making untrue claims about diet in order to sell you unnecessary supplements”. That turned out to be pretty accurate. They are part of the alternative medicine fringe. The Universities Admission Service (UCAS) no longer lists any BSc/MSc degrees in "Nutritional Therapy" or "Nutritional medicine". Westminster University closed its BSc Nutritional Therapy during last year. We still don’t know the fate of the notorious (or should I say hilarious) course run at the Northern College of Acupuncture and validated (after a fashion) by the late University of Wales, but it isn’t listed for entry in 2012. [We do now: see follow-up‘] But there are a large number of university courses called "Nutrition". How many of them teach properly, and how many of them teach the nonsense that prevails in "nutritional therapy", I don’t know. The term ‘nutrition’ has turned into a dangerous minefield. It can mean almost anything, because the term is undefined. Anyone can, and does, describe themselves as a nutritionist. At one extreme you have slick pills salesman like ‘not-a-Dr’ Gillian McKeith and Patrick Holford. At the other extreme you have a fascinating and respectable subject for study. The one thing that you need to get clear is that if you want advice about nutrition, go to a dietitian not a "nutritionist". Dietitians are the properly qualified people who work in the NHS, and who are (mostly) free of crackpot ideas. |
I suppose that one should not be surprised at the poor, and sometimes dangerous, advice that was given by nutritional therapists. Their training contains much nonsense so it isn’t surprising that they did so badly. Some of it has been revealed here. See, for example,
Another worthless validation: the University of Wales and nutritional therapy
Nutritional Fairy Tales from Thames Valley University
College of Natural Nutrition: bizarre teaching revealed
Nutriprofile: useful aid or sales scam?
Response to a threatening letter from Mr Holford
Food for the Brain: Child Survey. A proper job?
Teaching bad science to children: OfQual and Edexcel are to blame
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
The level of knowledge of both physiology and chemistry shown my some of the therapists was shocking. One recommended avoiding margarine, because it’s “two chemical bonds away from pure plastic”. Another said that Flora margarine contains lots of trans fat, which has not been true for a long time.
One graduate ot the late Thames Valley University course said “”advantage of the wholemeal or the wholegrain … is that they contain more fibre and the fibre stops the sugars being absorbed quite as quickly”. Not so. Brown and white bread have much the same glycaemic index (60 – 70).
Quack diagnosis
One alarming fact was that several therapists offered methods of diagnosis for allergy and for deficiencies that have been known for many years not to work. There isn’t anything controversial about iridology, hair mineral analysis, taste tests. kinesiology. or the Vega test. They are pure quackery.
“Professor David Colquhoun, from our panel of experts, said: ‘Sadly, nutritional therapy is plagued by “diagnostic tests” that are little more than quackery; they are tools to aid sales, rather than tools to diagnose deficiencies. Iridology and hair analysis simply don’t work.”
Unnecessary treatments
One therapist advised a researcher to have an optimum nutritional evaluation test, costing £312, and a cellular nutrition profile, costing £156. Apparently, these would allow the therapist to give a
more targeted service by establishing what vitamin and mineral deficiencies he had.
Our experts were not convinced by these tests and certainly didn’t think they were worth the money; any necessary testing
could be done by a GP for free.
In 12 of the 15 consultations, researchers were prescribed a huge range of supplements, costing up to £70 per month. It was not revealed whether or not the prescriber made money from this, but usually you were asked to give the prescriber’s name "to get a discount". So it’s a fair guess that they got kickbacks.
British Association for Applied Nutrition & Nutritional Therapy (BANT)
Despite the low standards of advice, 13 out of the 14 therapists who were visited were registered with BANT, the British Association for Applied Nutrition & Nutritional Therapy. This is what passes for a professional association for nutritional therapists, though like all such bodies in alternative medicine, it is entirely ineffective as a regulator. Rather it serves to protect whatever untrue claims they make. BANT’s code of practice says that its members won’t diagnose, but in fact many of the therapists diagnosed conditions and created treatment plans. You can be confident that BANT will do nothing to stop this bad practice.
You can find out a lot about BANT from these sources:
British Association for Nutritional Therapy – when an organisation looks like a regulator, quacks like a regulator, but isn’t a regulator
Why it is easy to get the incorrect impression that BANT is a regulator
Nutritional Therapists Fail to Join Ofquack
BANT: A Profile
Matthias Rath drops his million pound legal case against me and the Guardian.
Only 3 of the 14 therapists were registered with the Complementary and Natural Healthcare Council (the CNHC, more commonly know as Ofquack). They are meant to be the official regulator, launched with a good chunk of taxpayers’ money, but registration is voluntary and not many have volunteered. As a requlator, Ofquack is a bad joke.
Conclusion
|
"Dr Margaret McCartney says: ‘This investigation appears to show that high street nutritional therapists are a waste of money. If you have symptoms please see your GP, not someone who can’t diagnose accurately.’ If you’re looking for tailored dietary advice, visit a registered dietitian.
" |
There is a discussion of this topic on the Which? magazine site.
Follow-up
The excellent Quackometer has posted simultaneously on the great nutritional therapy scam.
16 January 2012 The British Dietetic Association issued a press release that describes very clearly the many differences between a real dietitian and a "nutritional therapist". Download Leading UK Nutrition Association Urges Awareness Between Dietitians and Nutritionists (pdf).
16 January 2012 BANT issued a press release. Download Are Nutritional Therapists Gambling with Your Health?. It answers none of the serious questions raised by the Which? investigation. BANT moans that that Which? “did not provide all the promised transcripts/questionnaires in a timely fashion”. In fact they got them before Christmas and were given until January 15th to respond.
16 January 2012. BBC Radio 4 programme, You and Yours, had an item with Jenny Driscoll from Which? magazine and BANT chairperson, Catherine Honeywell. She did, inter alia, admit that some of the behaviour of the therapists were irresponsible. It remains to be seen if they do anything about it. don’t hold your breath. Hear it on BBC iPlayer.
16 January 2012. There was pretty god coverage of the story, even in the Daily Mail.
17 January 2012 Another question answered. I just learned that the ludicrous course in Nutritional Therapy, previously validated by the University of Wales (and a contributor to its downfall), is now being validated by, yes, you guessed, Middlesex University. Professor Driscoll seems determined to lead his univerity to the bottom of the academic heap. His new partnership with the Northern college of Acupuncture is just one of a long list of validations that almost rivals that of the late University of Wales. The course has, of course, an enthusiastic testimonial, from a student. It starts
I work full time as a team leader for a pension company but I am also a kinesiologist and work in my spare time doing kinesiology, reiki and Indian head massage.
Evidently she’s a believer in the barmiest and totally disproved forms of magic medicine. And Middlesex University will give her a Master of Science degree. I have to say I find it worrying that she’s a team leader for a pension company. Does she also believe in the value of worthless derivatives. I wonder?
17 January 2012 The discussion is going on at the Which? web site. A Chris James cast doubt on the reaults because ot the small sample size, and asked for confidence limits, so I gave them.
Chris James
It is easy enough to calculate limits yourself -you don’t even need to be able to do the maths -there are web calculators that do it for you, e.g. http://www.causascientia.org/math_stat/ProportionCI.html
14/15 = 93% failed. 95% confidence limits for this are 69.8% to 98.4%
6/15 = 40% gave dangerous advice 95% confidence limits 19.7% to 64.6%
So despite the small sample size we can say that it’s likely that at least 70% (and possibly 98%) of nutritional therapists fail.
And it is likely that at least 20% (and possibly 65%) of nutritional therapists give dangerous advice.
These results give real cause for concern, despite the small sample size.
For statistical enthusiasts, these limits are Bayesian with a uniform prior. Very much the same result is given by the standard analysis which is explained in section 7.7 of Lectures on Biostatistics [download pdf 10.5 Mb]
18 January 2012. BANT has, at last, produced an “updated response”. The good thing is that it starts by saying
” . . it is completely outside the BANT Code of Practice to advise a client to withhold any treatment for cancer for any period of time in order to follow a nutritional approach. Were a client to be advised in such a way we would expect to receive a complaint against the practitioner.”
I hope that this will happen. This statement, the only admission of guilt in BANT’s response, is rather spoiled by a later suggestion that no such recommendation was made. It looked very clear to both Which? magazine and to the three members of the expert panel.
The rest of the response admits no fault of any sort.
I’m sorry to say that the response by BANT shows very clearly what is wrong in nutritional therapy. Any organisation which can see nothing wrong in the advice given in 14 of the 15 consultations is, I’d argue, a threat to the health of the nation. Rather than saying we’ll try to improve, they just deny everything.
The response seems to show that the professional organisation for nutritional therapists is not part of the solution. Rather it is part of the problem.
There’s been no official announcement, but four more of Westminster’s courses in junk medicine have quietly closed.
For entry in 2011 they offer
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Complementary Medicine (B255) | 3FT Hon BSc |
| Complementary Medicine (B301) | 4FT Hon MHSci |
| Complementary Medicine: Naturopathy (B391) | 3FT Hon BSc |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSci |
| Nutritional Therapy (B400) | 3FT Hon BSc |
But for entry in 2012
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSc |
At the end of 2006, Westminster was offering 14 different BSc degrees in seven flavours of junk medicine. In October 2008, it was eleven. This year it’s eight, and next year only four degrees in two subjects. Since "Integrated Health" was ‘merged’ with Biological Sciences in May 2010, two of the original courses have been dropped each year. This September there will be a final intake for Nutrition Therapy and Naturopathy. That leaves only two, Chinese Medicine (acupuncture and (Western) Herbal Medicine.
The official reason given for the closures is always that the number of applications has fallen. I’m told that the number of applications has halved over the last five or six years. If that’s right, it counts as a big success for the attempts of skeptics to show the public the nonsense that’s taught on these degrees. Perhaps it is a sign that we are emerging from the endarkenment.
Rumour has it that the remaining degrees will eventually close too. Let’s hope so. Meanwhile, here is another helping hand.
There is already quite a bit here about the dangers of Chinese medicine, e.g. here and, especially, here. A submission to the Department of Health gives more detail. There has been a lot on acupuncture here too. There is now little doubt that it’s no more than a theatrical, and not very effective, placebo. So this time I’ll concentrate on Western herbal medicine.
Western Herbal Medicine
Herbal medicine is just a branch of pharmacology and it could be taught as such. But it isn’t. It comes overlaid with much superstitious nonsense. Some of it can be seen in slides from Edinburgh Napier University (the difference being that Napier closed that course, and Westminster hasn’t)
Even if it were taught properly, it wouldn’t be appropriate for a BSc for several reasons.
First, there isn’t a single herbal that has full marketing authorisation from the MHRA. In other words, there isn’t a single herb for which there is good evidence that it works to a useful extent.
Second, the fact that the active principals in plants are virtually always given in an unknown dose makes them potentially dangerous. This isn’t 1950s pharmacology. It’s 1920s pharmacology, dating from a time before methods were worked out for standardising the potency of natural products (see Plants as Medicines).
Third, if you are going to treat illness with chemicals, why restrict yourself to chemicals that occur in plants?
It was the herbal medicine course that gave rise to the most virulent internal complaints at the University of Westminster. These complaints revealed the use of pendulum dowsing by some teachers on the course and the near-illegal, and certainly dangerous, teaching about herbs in cancer.
Here are a few slides from Principles of Herbal Medicine(3CT0 502). The vocabulary seems to be stuck in a time warp. When I first started in the late 1950s, words like tonic, carminative, demulcent and expectorant were common Over the last 40 years all these words have died out in pharmacology, for the simple reason that it became apparent that there were no such actions. But these imaginary categories are still alive and well in the herbal world.
There was a lecture on a categories of drugs so old-fashioned that I’ve never even heard the words: "nervines". and "adaptogens".
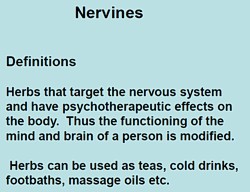 |
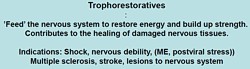 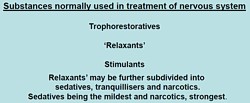 |
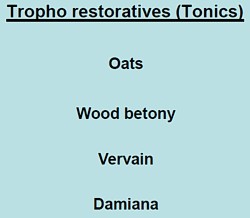 |
The "tonics" listed here seem quite bizarre. In the 1950s, “tonics” containing nux vomica (a small dose of strychnine) and gentian (tastes nasty) were common, but they vanished years ago, because they don’t work. None of those named here even get a mention in NCCAM’s Herbs-at-a-glance. Oats? Come on! |
|
The only ‘relaxant’ here for which there is the slightest evidence is Valerian. I recall tincture of Valerian in a late 1950s pharmacy. It smells terrible, According to NCCAM
Not much, for something that’s been around for centuries. And for chamomile
None of this near-total lack of evidence is mentioned on the slides. |
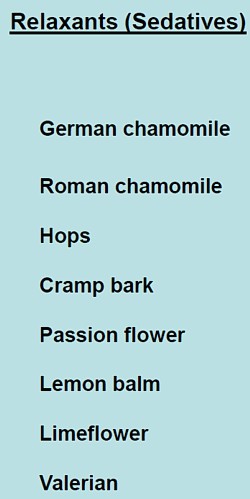 |
What about the ‘stimulants‘? Rosemary? No evidence at all. Tea and coffee aren’t medicine (and not very good stimulants for me either).
|
Ginseng, on the other hand, is big business. That doesn’t mean it works of course. NCCAM says of Asian ginseng (Panax Ginseng).
|
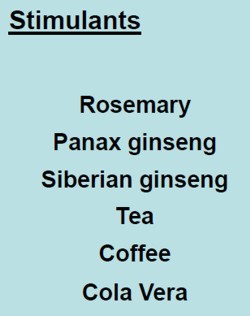 |
Thymoleptics – antidepressants are defined as "herbs that engender a feeling of wellbeing. They uplift the spirit, improve the mood and counteract depression".
Oats, Lemon balm, Damiana, Vervain. Lavender and Rosemary are just old bits of folklore
|
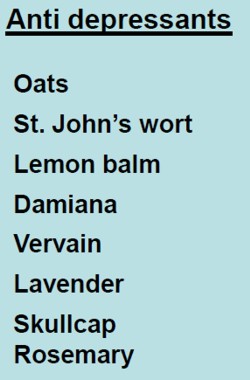 |
The only serious contender here is St John’s Wort. At one time this was the prize exhibit for herbalists. It has been shown to be as good as the conventional SSRIs for treatment of mild to moderate depression. Sadly it has turned out that the SSRIs are themselves barely better than placebos. NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
"Adaptogens" are another figment of the herbalists’ imaginations. They are defined in the lecture thus.
|
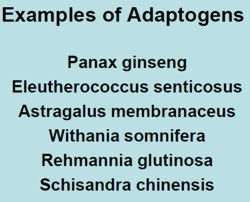
|
Well, it would be quite nice if such drugs existed. Sadly they don’t.
- The evidence for using astragalus for any health condition is limited. High-quality clinical trials (studies in people) are generally lacking.
Another lecture dealt with "stimulating herbs". No shortage of them, it seems.
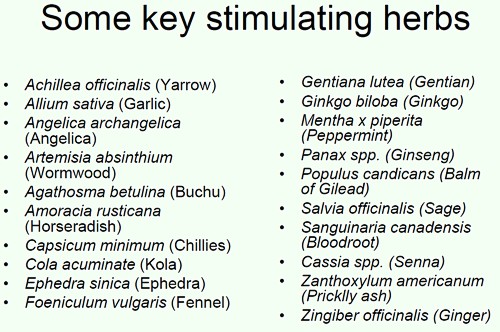
Well at least one of these has quite well-understood effects in pharmacology, ephedrine, a sympathomimetic amine. It isn’t used much because it can be quite dangerous, even with the controlled dose that’s used in real medicine. In the uncontrolled dose in herbal medicines it is downright dangerous.
|
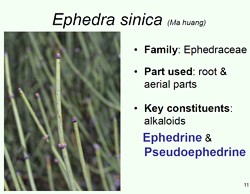
|
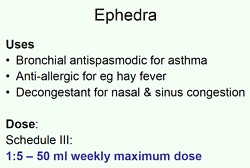
|
|
This is what NCCAM says about Ephedra
- An NCCAM-funded study that analyzed phone calls to poison control centers found a higher rate of side effects from ephedra, compared with other herbal products.
- Other studies and systematic reviews have found an increased risk of heart, psychiatric, and gastrointestinal problems, as well as high blood pressure and stroke, with ephedra use.
- According to the U.S. Food and Drug Administration (FDA), there is little evidence of ephedra’s effectiveness, except for short-term weight loss. However, the increased risk of heart problems and stroke outweighs any benefits.
It seems that what is taught in the BSc Herbal Medicine degree consists largely of folk-lore and old wives’ tales. Some of it could be quite dangerous for patients.
A problem for pharmacognosists
While talking about herbal medicine, it’s appropriate to mention a related problem, though it has nothing to do with the University of Westminster.
My guess is that not many people have even heard of pharmacognosy. If it were not for my humble origins as an apprentice pharmacist in Grange Road, Birkenhead (you can’t get much more humble than that) I might not know either.
Pharmacognosy is a branch of botany, the study of plant drugs. I recall inspecting powered digitalis leaves under a microscope. In Edinburgh, in the time of the great pharmacologist John Henry Gaddum, medical students might be presented in the oral exam with a jar of calabar beans and required to talk about their anticholinesterase effects of the physostigmine that they contain.
The need for pharmacognosy has now all but vanished, but it hangs on in the curriculum for pharmacy students. This has engendered a certain unease about the role of pharmacognists. They often try to justify their existence by rebranding themselves as "phytotherapists". There are even journals of phytotherapy. It sounds a lot more respectable that herbalism. At its best, it is more respectable, but the fact remains that there no herbs whatsoever that have well-documented medical uses.
The London School of Pharmacy is a case in point. Simon Gibbons (Professor of Phytochemistry, Department of Pharmaceutical and Biological Chemistry). The School of Pharmacy) has chosen, for reasons that baffle me, to throw in his lot with the reincarnated Prince of Wales Foundation known as the “College of Medicine“. That organisation exists largely (not entirely) to promote various forms of quackery under the euphemism “integrated medicine”. On their web site he says "Western science is now recognising the extremely high value of herbal medicinal products . . .", despite the fact that there isn’t a single herbal preparation with efficacy sufficient for it to get marketing authorisation in the UK. This is grasping at straws, not science.
The true nature of the "College of Medicine" is illustrated, yet again, by their "innovations network". Their idea of "innovation" includes the Bristol Homeopathic Hospital and the Royal London Hospital for Integrated medicine, both devoted to promoting the utterly discredited late-18th century practice of giving people pills that contain no medicine. Some "innovation".
It baffles me that Simon Gibbons is willing to appear on the same programme as Simon Mills and David Peters, and George Lewith. Mills’ ideas can be judged by watching a video of a talk he gave in which he ‘explains’ “hot and cold herbs”. It strikes me as pure gobbledygook. Make up your own mind. He too has rebranded himself as "phytotherapist" though in fact he’s an old-fashioned herbalist with no concern for good evidence. David Peters is the chap who, as Clinical Director of the University of Westminster’s ever-shrinking School of Quackery, tolerates dowsing as a way to select ‘remedies’.
The present chair of Pharmacognosy at the School of Pharmacy is Michael Heinrich. He, with Simon Gibbons, has written a book Fundamentals of pharmacognosy and phytotherapy. As well as much good chemistry, it contains this extraordinary statement
“TCM [traditional Chinese medicine] still contains very many remedies which were selected by their symbolic significance rather than their proven effects; however this does not mean that they are all ‘quack’remedies! There may even be some value in medicines such as tiger bone, bear gall, turtle shell, dried centipedes, bat dung and so on. The herbs, however, are well researched and are becoming increasingly popular as people become disillusioned with Western Medicine.”
It is irresponsible to give any solace at all to the wicked industries that kill tigers and torture bears to extract their bile. And it is simple untrue that “herbs are well-researched”. Try the test,
A simple test for herbalists. Next time you encounter a herbalist, ask them to name the herb for which there is the best evidence of benefit when given for any condition. Mostly they refuse to answer, as was the case with Michael McIntyre (but he is really an industry spokesman with few scientific pretensions). I asked Michael Heinrich, Professor of Pharmacognosy at the School of Pharmacy. Again I couldn’t get a straight answer. Usually, when pressed, the two things that come up are St John’s Wort and Echinacea. Let’s see what The National Center for Complementary and Alternative Medicine (NCCAM) has to say about them. NCCAM is the branch of the US National Institutes of Health which has spent around a billion dollars of US taxpayers’ money on research into alternative medicine, For all that effort they have failed to come up with a single useful treatment. Clearly they should be shut down. Nevertheless, as an organisation that is enthusiastic about alternative medicine, their view can only be overoptimistic.
For St John’s Wort . NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
For Echinacea NCCAM says
- Study results are mixed on whether echinacea can prevent or effectively treat upper respiratory tract infections such as the common cold. For example, two NCCAM-funded studies did not find a benefit from echinacea, either as Echinacea purpurea fresh-pressed juice for treating colds in children, or as an unrefined mixture of Echinacea angustifolia root and Echinacea purpurea root and herb in adults. However, other studies have shown that echinacea may be beneficial in treating upper respiratory infections.
If these are the best ones, heaven help the rest.
Follow-up
On 23rd May 2008 a letter was sent to the vice-chancellor of the University of Westminster, Professor Geoffrey Petts
|
 |
Despite reminders, we were never afforded the courtesy of a reply to this, or any other letter.
Professor Petts has, however, replied to a letters sent to him recently by the Nightingale Collaboration. He said
“Whilst I understand your concerns, colleagues of the School of Life Sciences where these courses are offered do not share them. They are not teaching pseudo-science, as you claim,…”.
Neither of thse claims is true.I know at least two members of the Life Sciences Faculty who are very worried. One has now left and one has retired. The rest are presumably too scared to speak out.
It is most certainly not true to say they "are not teaching pseudo-science". Both the vice-chancellor and the Dean of Life Sciences, Jane Lewis, have been made aware of what;s happening repeatedly over several years, I can think of no other way to put it but to say Professor Petts is lying. Tha is not a good thing for vice-chancellors to do.
Much of what is taught at Westminster has now been revealed. This seems like a good moment to summarise what we know. Searching this blog for "University of Westminster" yields 39 hits. Of these, 11 show what’s taught at Westminster, so I’ll summarise them here for easy reference.
March 26th, 2007
The day after “Science degrees without the Science“ appeared in Nature, the University of Westminster issued a statement (now vanished, but see debate in THE). In my view, their statement provides the strongest grounds so far to believe that the BSc is inappropriate.
Let’s take a look at it.
|
“The BSc (Hons) Health Sciences: Homeopathy is a fully validated degree that satisfies internal and external quality assurance standards.”
|
Since that time, the university has closed down the BSc in Homeopathy. I have now seen many such validation documents and they are mostly box ticking exercises, not worth the paper they are written on. The worst offender is the University or Wales.
Westminster University BSc: “amethysts emit high yin energy”
April 23rd, 2008
http://dcscience.net/vib-therapies-43s.jpg
|
This shows the first set of slides that I got from Westminster (leaked by an angry insider). It has slides on crystal healing and dowsing, things that are at the lunatic fringe even by the standards of alternative medicine. it also relates that an academic who invited me to give a talk at the University of Westminster on the evidence for alternative medal was leaned on heavily by “VC, Provosts and Deans” to prevent that talk taking place. |
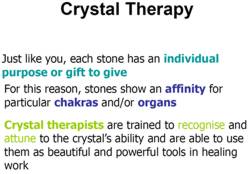
|
Crystal balls. Professor Petts in Private Eye
February 19th, 2009
Professor Petts makes an appearance in Private Eye. It could held that this counts as bringing your university into disrepute.
February 24th, 2009
BSc courses in homeopathy are closing. Is it a victory for campaigners, or just the end of the Blair/Bush era?
|
Professor Petts of Westminster seems to think that the problem can be solved by putting more science into the courses The rest of the world realises that as soon as you apply science to homeopathy or naturopathy, the whole subject vanishes in a puff of smoke, I fear that Professor Petts will have to do better,
|
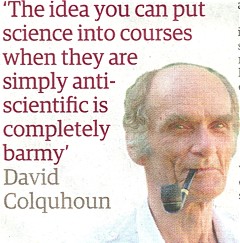 |
The Guardian carries a nice article by Anthea Lipsett, The Opposite of Science (or download pdf of print version).
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
March 30th, 2009
In March 2007 I wrote a piece in Nature on Science degrees without the science. At that time there were five “BSc” degrees in homeopathy. A couple of weeks ago I checked the UCAS site for start in 2009, and found there was only one full “BSc (hons)” left and that was at Westminster University.
Today I checked again and NOW THERE ARE NONE.
A phone call to the University of Westminster tonight confirmed that they have suspended entry to their BSc (Hons) homeopathy degree.
Then I revealed another set of slides, showing a misunderstanding (by the teacher) of statistics, but most chillingly,some very dangerous ideas conveyed to students by Westminster’s naturopaths, and in the teaching of Traditional Chinese Medicine, and the great “detox” scam.
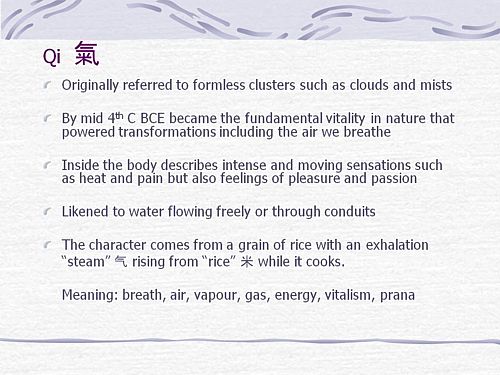
“if you get tuberculosis, it isn’t caused by Mycobacterium tuberculosis? And the symptoms are “constructive”? So you don’t need to do anything. It’s all for the best really.
This isn’t just nonsense. It’s dangerous nonsense.”
“Remember when shopping to favour fruits and vegetables which are in season and locally grown (and ideally organic) as they are more vibrationally compatible with the body.”
Locally grown vegetables are “more vibrationally compatible with the body”? Pure mystical gobbledygook. Words fail me.
More make-believe from the University of Westminster. This time it’s Naturopathy
June 25th, 2009
|
Some truly mind-boggling stuff that’s taught to students at Westminster, It includes "Emotrance". A primer on Emotrance says |
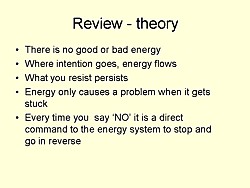 |
"And then I thought of the lady in the supermarket whose husband had died, and I spend the following time sending her my best wishes, and my best space time quantum healing efforts for her void."
Then there are slides on pendulum diagnosis and “kinesiology”, a well-known fraudulent method of diagnosis. It is all perfectly mad.
Why degrees in Chinese medicine are a danger to patients
August 10th, 2009
More lunatic fantasies from Westminster, this time about Chinese medicine.
“Teaching students that the brain is made of marrow is not just absurd, but desperately dangerous for anyone unlucky (or stupid) enough to go to such a person when they are ill.”
|
There is a lot of stuff about cancer that is potentially homicidal.
|
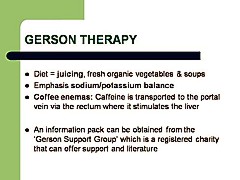 |
This is outrageous and very possibly illegal under the Cancer Act (1939). It certainly poses a huge danger to patients. It is a direct incentive to make illegal, and untrue claims by using weasel words in an attempt to stay just on the right side of the law. But that, of course, is standard practice in alternative medicine,
Emergent Chinese Omics at the University of Westminster/p>
August 27th, 2010
Systems biology is all the rage, No surprise then, to see the University of Westminster advertising a job for a systems biologist in the The Department of Molecular and Applied Biosciences. Well, no surprise there -until you read the small print.
Much has been written here about the University of Westminster, which remains the biggest provider of junk science degrees in the UK, despite having closed two of them.
If there is one thing more offensive than the use of meaningless mystical language, it is the attempt to hijack the vocabulary of real science to promote nonsense. As soon as a quack uses the words "quantum", "energy", "vibration", or now, "systems biology", you can be sure that it’s pretentious nonsense.
Hot of the press. Within a few hours of posting this, I was told that Volker Scheid, the man behind the pretentious Chinese medidine omics nonsense has been promoted to a full chair, And the Dean, Jane Lewis has congratulated him for speaking at a Chines Medicine symposium. Even quite sensible people like Lewis are being corrupted. The buck stops with Petts.
May 3rd, 2011
|
Yet more ghastly slides that are inflicted on Westminster students. How’s this for sheer barminess, taught as part of a Bachelor of Science degree? |
|
And
" Just in case you happen to have run out of Alaskan Calling All Angels Essence, you can buy it from Baldwin’s for £19.95. It’s “designed to invoke the nurturing, uplifting and joyful qualities of the angelic kingdom.”, and what’s more “can also use them any time to cleanse, energize, and protect your auric field.” Well that’s what it says.in the ad.
June 20th, 2011
This post gives details of two complaints, one from a student and one from a lecturer. The vice-chancellor certainly knows about them. So why, I wonder, did he say "“Whilst I understand your concerns, colleagues of the School of Life Sciences where these courses are offered do not share them.". He must know that this simply isn’t true. It is over a year now ( 10 July 2009 ) that a lecturer wrote to the vice-chancellor and Dean
|
“I expect that were the Department of Health to be aware of the unscientific teaching and promotion of practices like dowsing, (and crystals, iridology, astrology, and tasting to determine pharmacological qualities of plant extracts) on the Wmin HM [Westminster Herbal Medicine] Course, progress towards the Statutory Regulation of Herbal Medicine could be threatened.”
|
There’s only one thing wrong with this. The lecturer underestimated the stupidiity of the Department of Health which went ahead with statutory regulation despite being made aware of what was going on.
The latest example to come to light is cited by Andy Lewis on his Quackometer blog
“There are some even odder characters too, such as Roy Riggs B.Sc who describes himself as a “Holistic Geobiologist” and is “an “professional Earth Energy dowser”. He guest lectures at the London Westminster University’s School of Integrative Medicine and The Baltic Dowser’s Association of Lithuania.”
I do wonder who Professor Petts thinks he’s fooling. His denial of the obvious fact that his university is teaching pseudo-science serves only to discredit further the University of Westminster and his own integrity.
Follow-up
13 August 2011 I’m intrigued to notice that two days after posting this summary, googling “Geoffrey Petts” brings up this post as #3 on the first page. Actions have consequences.
Almost all the revelations about what’s taught on university courses in alternative medicine have come from post-1992 universities. (For readers not in the UK, post-1992 universities are the many new univerities created in 1992, from former polytechnics etc, and Russell group universities are the "top 20" research-intensive universities)
It is true that all the undergraduate courses are in post-1992 universities, but the advance of quackademia is by no means limited to them. The teaching at St Bartholomew’s Hospital Medical School, one of the oldest, was pretty disgraceful for example, though after protests from their own students, and from me, it is now better, I believe.

Quackery creeps into all universities to varying extents. The good ones (like Southampton) don’t run "BSc" degrees, but it still infiltrates through two main sources,
The first is via their HR departments, which are run by people who tend to be (I quote) "credulous and moronic" when it comes to science.
The other main source is in teaching to medical students. The General Medical Council says that medical students must know something about alterantive medicine and that’s quite right, A lot of their patients will use it. The problem is that the guidance is shockingly vague .
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
In many medical schools, the information that medical students get is quite accurate. At UCL and at King’s (London) I have done some of the familiarisation myself. In other good medical schools, the students get some shocking stuff. St Bartholomew’s Hospital medical School was one example. Edinburgh University was another.
But there is one Russell group university where alternative myths are propagated more than any other that I know about. That is the University of Southampton.
In general, Southampton is a good place, I worked there for three years myself (1972 – 1975). The very first noise spectra I measured were calculated on a PDP computer in their excellent Institute of Sound and Vibration Research, before I wrote my own programs to do it.
But Southanpton also has a The Complementary and Integrated Medicine Research Unit . Oddly the unit’s web site, http://www.cam-research-group.co.uk, is not a university address, and a search of the university’s web site for “Complementary and Integrated Medicine Research Unit” produces no result. Nevertheless the unit is “within the School of Medicine at the University of Southampton”
Notice the usual euphemisms ‘complementary’ and ‘integrated’ in the title: the word ‘alternative’ is never used. This sort of word play is part of the bait and switch approach of alternative medicine.
The unit is quite big: ten research staff, four PhD students and two support staff It is headed by George Lewith.
Teaching about alternative medicine to Southampton medical students.
The whole medical class seems to get quite a lot compared with other places I know about. That’s 250 students (210 on the 5-year course plus another 40 from the 4-year graduate-entry route).
Year 1: Lecture by David Owen on ‘holism’ within the Foundation Course given to all 210 medical students doing the standard (5-year) course.
Year 2: Lecture by Lewith (on complementary medicine, focusing on acupuncture for pain) given within the nervous systems course to the whole medical student year-group (210 students).
Year 3 SBOM (scientific basis of medicine) symposium: The 3-hour session (“Complementary or Alternative Medicine: You Decide”). I’m told that attendance at this symposium is often pretty low, but many do turn up and all of them are officially ‘expected’ to attend.
There is also an optional CAM special study module chosen by 20 students in year 3, but also a small number of medical students (perhaps 2 – 3 each year?) choose to do a BMedSci research project supervised by the CAM research group and involving 16-18 weeks of study from October to May in Year 4. The CAM research group also supervise postgraduate students doing PhD research.
As always, a list of lectures doesn’t tell you much. What we need to know is what’s taught to the students and something about the people who teach it. The other interesting question is how it comes about that alternative medicine has been allowed to become so prominent in a Russell group university. It must have support from on high. In this case it isn’t hard to find out where it comes from. Here are some details.
Year 1 Dr David Owen
David Owen is not part of Lewith’s group, but a member of the Division of Medical Education headed by Dr Faith Hill (of whom, more below). He’s one of the many part-time academics in this area, being also a founder of The Natural Practice .
Owen is an advocate of homeopathy (a past president of the Faculty of Homeopathy). Homeopathy is, of course, the most barmy and discredited of all the popular sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes it).
And he’s also a member of the British Society of Environmental Medicine (BSEM). That sounds like a very respectable title, but don’t be deceived. It is an organisation that promotes all sorts of seriously fringe ideas. All you have to do is notice that the star speaker at their 2011 conference was none other than used-to-be a doctor, Andrew Wakefield, a man who has been responsible for the death of children from measles by causing an unfounded scare about vaccination on the basis of data that turned out to have been falsified. There is still a letter of support for Wakefield on the BSEM web site.
The BSEM specialises in exaggerated claims about ‘environmental toxins’ and uses phony allergy tests like kinesiology and the Vega test that misdiagnose allergies, but provide en excuse to prescribe expensive but unproven nutritional supplements, or expensive psychobabble like "neuro-linguistic programming".
Other registered "ecological physicians" include the infamous Dr Sarah Myhill, who, in 2010, was the subject of a damning verdict by the GMC, and Southampton’s George Lewith.
If it is wrong to expose medical students to someone who believes that dose-response curves have a negative slope (the smaller the dose the bigger the effect -I know, it’s crazy), then it is downright wicked to expose students to a supporter of Andrew Wakefield.
David Owen’s appearance on Radio Oxford, with the indomitable Andy Lewis appears on his Quackometer blog.
Year 2 Dr George Lewith
Lewith is a mystery wrapped in an enigma. He’s participated in some research that is quite good by the (generally pathetic) standards of the world of alternative medicine.
In 2001 he showed that the Vega test did not work as a method of allergy diagnosis. "Conclusion Electrodermal testing cannot be used to diagnose environmental allergies", published in the BMJ .[download reprint].
In 2003 he published "A randomized, double-blind, placebo-controlled proving trial of Belladonna 30C” [download reprint] that showed homeopathic pills with no active ingredients had no effects: The conclusion was "”Ultramolecular homeopathy has no observable clinical effects" (the word ultramolecular, in this context, means that the belladonna pills contained no belladonna).
In 2010 he again concluded that homeopathic pills were no more than placebos, as described in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). [download reprint]
What i cannot understand is that, despite his own findings, his private practice continues to prescribe the Vega machine and continues to prescribe homeopathic pills. And he continues to preach this subject to unfortunate medical students.
Lewith is also one of the practitioners recommended by BSEM. He’s a director of the "College of Medicine". And he’s also an advisor to a charity called Yes To Life. (see A thoroughly dangerous charity: YesToLife promotes nonsense cancer treatments).
3rd year Student Selected Unit
The teaching team includes:
- David Owen – Principal Clinical Teaching Fellow SoM, Holistic Physician
- George Lewith – Professor of Health Research and Consultant Physician
- Caroline Eyles – Homeopathic Physician
- Susan Woodhead – Acupuncturist
- Elaine Cooke – Chiropractic Practitioner
- Phine Dahle – Psychotherapist
- Keith Carr – Reiki Master
- Christine Rose – Homeopath and GP
- David Nicolson – Nutritionalist
- Shelley Baker – Aromatherapist
- Cheryl Dunford – Hypnotherapist
- Dedj Leibbrandt – Herbalist
More details of the teaching team here. There is not a single sceptic among them, so the students don’t get a debate, just propaganda.
In this case. there’s no need for the Freedom of Information Act. The handouts. and the powerpoints are on their web site. They seem to be proud of them
Let’s look at some examples
Chiropractic makes an interesting case, because, in the wake of the Singh-BCA libel case, the claims of chiropractors have been scrutinised as never before and most of their claims have turned out to be bogus. There is a close relationship between Lewith’s unit and the Anglo-European Chiropractic College (the 3rd year module includes a visit there). In fact the handout provided for students, Evidence for Chiropractic Care , was written by the College. It’s interesting because it provides no real evidence whatsoever for the effectiveness of chiropractic care. It’s fairly honest in stating that the view at present is that, for low back pain, it isn’t possible to detect any difference between the usefulness of manipulation by a physiotherapist, by an osteopath or by a chiropractor. Of course it does not draw the obvious conclusion that this makes chiropractic and osteopathy entirely redundant -you can get the same result without all the absurd mumbo jumbo that chiropractors and osteopaths love, or their high-pressure salesmanship and superfluous X-rays. Neither does it mention the sad, but entirely possible, outcome that none of the manipulations are effective for low back pain. There is, for example, no mention of the fascinating paper by Artus et al [download reprint]. This paper concludes
"symptoms seem to improve in a similar pattern in clinical trials following a wide
variety of active as well as inactive treatments."
This paper was brought to my attention through the blog run by the exellent physiotherapist, Neil O’Connell. He comments
“If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery.”
This sort of critical thinking is conspicuously absent from this (and all the other) Southampton handouts. The handout is a superb example of bait and switch: No nonsense about infant colic, innate energy or imaginary subluxations appears in it.
Acupuncture is another interesting case because there is quite a lot of research evidence, in stark contrast to the rest of traditional Chinese medicine, for which there is very little research.
|
There is a powerpoint show by Susan Woodhead (though it is labelled British Acupuncture Council). The message is simple and totally uncritical. It works. |

|
In fact there is now a broad consensus about acupuncture.
(1) Real acupuncture and sham acupuncture have been found to be indistinguishable in many trials. This is the case regardless of whether the sham is a retractable needle (or even a toothpick) in the "right" places, or whether it is real needles inserted in the "wrong" places. The latter finding shows clearly that all that stuff about meridians and flow of Qi is sheer hocus pocus. It dates from a pre-scientific age and it was wrong.
(2) A non-blind comparison of acupuncture versus no acupuncture shows an advantage for acupuncture. But the advantage is usually too small to be of any clinical significance. In all probability it is a placebo effect -it’s hard to imagine a more theatrical event than having someone in a white coat stick long needles into you, like a voodoo doll. Sadly, the placebo effect isn’t big enough to be of much use.
Needless to say, none of this is conveyed to the medical students of Southampton. Instead they are shown crude ancient ideas that date from long before anything was known about physiology as though they were actually true. These folks truly live in some alternative universe. Here are some samples from the acupuncture powerpoint show by Susan Woodhead.
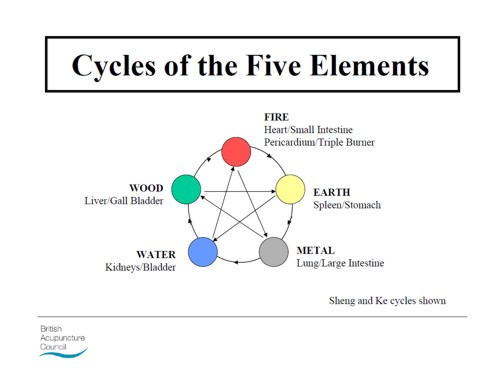
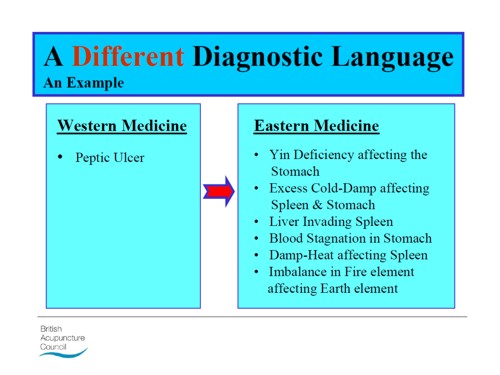
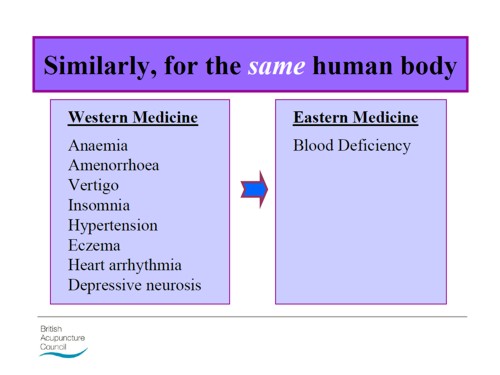
Well this is certainly a "different diagnostic language", but no attempt is made to say which one is right. In the mind of the acupuncurist it seems both are true. It is a characteristic of alternative medicine advocates that they have no difficulty in believing simultaneously several mutually contradictory propositions.
As a final exmple of barminess, just look at the acupuncture points (allegedly) on the ear The fact that it is a favoured by some people in the Pentagon as battlefield acupuncture, is more reminiscent of the mad general, Jack D. Ripper, in Dr Strangelove than it is of science.
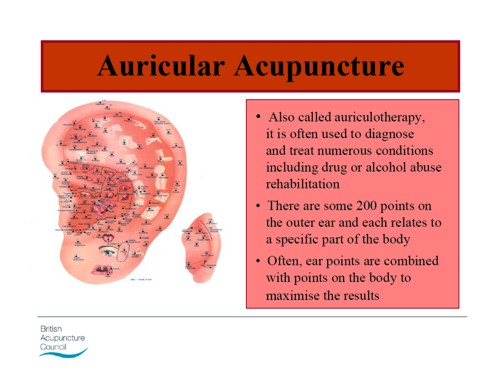
There is an equally uncritical handout on acupuncture by Val Hopwood. It’s dated March 2003, a time before some of the most valuable experiments were done.
The handout says "sham acupuncture
is generally less effective than true acupuncture", precisely the opposite of what’s known now. And there are some bits that give you a good laugh, always helpful in teaching. I like
“There is little doubt that an intact functioning nervous system is required for acupuncture to produce
analgesia or, for that matter, any physiological changes”
and
Modern techniques: These include hybrid techniques such as electro-acupuncture . . . and Ryadoraku [sic] therapy and Vega testing.
Vega testing!! That’s been disproved dozens of times (not least by George Lewith). And actually the other made-up nonsense is spelled Ryodoraku.
It’s true that there is a short paragraph at the end of the handout headed "Scientific evaluation of acupuncture" but it doesn’t cite a single reference and reads more like excuses for why acupuncture so often fails when it’s tested properly.
Homeopathy. Finally a bit about that most boring of topics, the laughable medicine that contains no medicine, homeopathy. Caroline Eyles is a member for the Society of Homeopaths, the organisation that did nothing when its members were caught out in the murderous practice of recommending homeopathy for prevention of malaria. The Society of Homeopaths also endorses Jeremy Sherr, a man so crazy that he believes he can cure AIDS and malaria with sugar pills.
The homeopathy handout given to the students has 367 references, but somehow manages to omit the references to their own boss’s work showing that the pills are placebos. The handout has all the sciencey-sounding words, abused by people who don’t understand them.
"The remedy will be particularly effective if matched to the specific/particular characteristics of the individual (the ‘totality’ of the patient) on all levels, including the emotional and mental levels, as well as just the physical symptoms. ‘Resonance’ with the remedy’s curative power will then be at it’s [sic] best."
The handout is totally misleading about the current state of research. It says
"increasing clinical research confirms it’s [sic] clinical effectiveness in treating patients, including babies and animals (where a placebo effect would be hard to justify)."
|
The powerpont show by Caroline Eyles shows all the insight of a mediaeval vitalist |
|
Anyone who has to rely on the utterly discredited Jacques Benveniste as evidence is clearly clutching at straws. What’s more interesting about this slide the admission that "reproducibility is a problem -oops, an issue" and that RCTs (done largely by homeopaths of course) have "various methodological flaws and poor external validity". You’d think that if that was the best that could be produced after 200 yours, they’d shut up shop and get another job. But, like aging vicars who long since stopped believing in god, but are damned if they’ll give up the nice country rectory, they struggle on, sounding increasingly desperate.
How have topics like this become so embedded in a medical course at a Russell group university?
The details above are a bit tedious and repetitive. It’s already established that hardly any alternative medicine works. Don’t take my word for it. Check the web site of the US National Center for Complementary and Alternative Medicine (NCCAM) who, at a cost of over $2 billion have produced nothing useful.
A rather more interesting question is how a good university like Southampton comes to be exposing its medical students to teaching like this. There must be some powerful allies higher up in the university. In this case it’s pretty obvious who thay are.
Professor Stephen Holgate MD DSc CSc FRCP FRCPath FIBiol FBMS FMed Sci CBE has to be the primary suspect, He’s listed as one of Southampton’s Outstanding Academics. His work is nothing to do with alternative medicine but he’s been a long term supporter of the late unlamented Prince of Wales’ Foundation, and he’s now on the advisory board of it’s successor, the so called "College of Medicine" (for more information about that place see the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health, and also Don’t be deceived. The new “College of Medicine” is a fraud and delusion ). His description on that site reads thus.
"Stephen Holgate is MRC Clinical Professor of Immunopharmacology at the University of Southampton School of Medicine and Honorary Consultant Physician at Southampton University Hospital Trust. He is also chair of the MRC’s Populations and Systems Medicine Board. Specialising in respiratory medicine, he is the author of over 800 peer-reviewed papers and contributions to scientific journals and editor of major textbooks on asthma and rhinitis. He is Co-Editor of Clinical and Experimental Allergy, Associate Editor of Clinical Science and on the editorial board of 25 other scientific journals."
Clearly a busy man. Personally I’m deeply suspicious of anyone who claims to be the author of over 800 papers. He graduated in medicine in 1971, so that is an average of over 20 papers a year since then, one every two or three weeks. I’d have trouble reading that many, never mind writing them.
Holgate’s long-standing interest in alternative medicine is baffling. He’s published on the topic with George Lewith, who, incidentally, is one of the directors of the "College of Medicine"..
It may be unkind to mention that, for many years now, I’ve been hearing rumours that Holgate is suffering from an unusually bad case of Knight starvation.
The Division of Medical Education appears to be the other big source of support for. anti-scientific medicine. That is very odd, I know, but it was also the medical education people who were responsible for mis-educating medical students at. St. Bartholomew’s and at Edinburgh university. Southampton’s Division of Medical Education has a mind-boggling 60 academic and support staff. Two of them are of particular interest here.
Faith Hill is director of the division. Her profile doesn’t say anything about alternative medicine, but her interest is clear from a 2003 paper, Complementary and alternative medicine: the next generation of health promotion?. The research consisted of reporting anecdotes from interviews of 52 unnamed people (this sort of thing seems to pass for research in the social sciences). It starts badly by misrepresenting the conclusions of the House of Lords report (2000) on CAM. Although it comes to no useful conclusions, it certainly shows a high tolerance of nonsensical treatments.
Chris Stephens is Associate Dean of Medical Education & Student Experience. His sympathy is shown by a paper he wrote In 2001, with David Owen (the homeopath, above) and George Lewith: Can doctors respond to patients’ increasing interest in complementary and alternative medicine?. Two of the conclusions of this paper were as follows.
"Doctors are training in complementary and alternative medicine and report benefits both for their patients and themselves"
Well, no actually. It wasn’t true then, and it’s probably even less true now. There’s now a lot more evidence and most of it shows alternative medicine doesn’t work.
"Doctors need to address training in and practice of complementary and alternative medicine within their own organisations"
Yes they certainly need to do that.
And the first thing that Drs Hill and Stephens should do is look a bit more closely about what’s taught in their own university, I hope that this post helps them,
Follow-up
4 July 2011. A correspondent has just pointed out that Chris Stephens is a member of the General Chiropractic Council. The GCC is a truly pathetic pseudo-regulator. In the wake of the Simon Singh affair it has been kept busy fending off well-justified complaints against untrue claims made by chiropractors. The GCC is a sad joke, but it’s even sadder to see a Dean of Medical Education at the University of Southampton being involved with an organisation that has treated little matters of truth with such disdain.
A rather unkind tweet from (ex)-chiropractor @RichardLanigan.
“Chris is just another light weight academic who likes being on committees. Regulatory bodies are full of them”
The Atlantic is an American magazine founded (as The Atlantic Monthly) in Boston, Massachusetts, in 1857. It is a literary and cultural magazine with a very distinguished history. Its contributors include Mark Twain and Martin Luther King. So it was pretty exciting to be asked to write something for it, even with a 12 hour deadline.

Sadly though, in recent years, the coverage of science in The Atlantic has been less than good The inimitable David Gorski has explained the problem in Blatant pro-alternative medicine propaganda in The Atlantic. The immediate cause of the kerfuffle was the publication of an article, The Triumph of New-Age Medicine. It was written by a journalist, David Freedman. It is very long and really not very good. It has been deconstructed also by Steven Novella.
Freedman’s article is very long, but it boils down to saying I know it doesn’t work but isn’t it nice. The article was followed up with Fix or Fraud: a ‘debate’., The debate is rather disappointing. It suffers from the problem, not unknown at the BBC, of thinking that ‘balance’ means giving equal time to people who think the earth is flat as it gives to people who think it is a oblate spheroid. The debate consists of 800 word contributions from seven people, six of whom are flat earthers, and one of which is very good. Try Steven Salzberg, A ‘triumph’ of hype over reality for some real sense. One of the flat earthers is director of a National Institutes of Health institute, NCCAM.
And this is a magazine that published not only Mark Twain, but Abraham Flexner, the man who, in 1910, put US medical education on a firm scientific footing, You can read Flexner in their archive. Mark Twain said
[A reply to letters recommending remedies]:
Dear Sir (or Madam):–I try every remedy sent to me. I am now on No. 67. Yours is 2,653. I am looking forward to its beneficial results. – quoted in My Father Mark Twain, by Clara Clemens
"allopathy is good for the sane and homeopathy for the insane"
So here is the piece, produced rather rapidly, for the debate. This is the original unedited version, slightly longer than appears in The Atlantic.
The title for The Atlantic piece, America, Land of the Health Hucksters, was theirs not mine. There is no shortage of health hucksters in the UK. but at least they mostly haven’t become as embedded within univerities and hospitals as much as in the USA.
|
David Freeman’s article, “The Triumph of New Age Medicine” starts by admitting that most alternative treatments don’t work, and ends by recommending them. He takes a lot more words to say it, but that seems a fair synopsis. It is the sort of thing you might expect in a cheap supermarket magazine, not in Atlantic. The article is a prime example of rather effective sales technique, much beloved of used car salesmen and health hucksters. It’s called bait and switch. It’s true that medicine can’t cure everything. That’s hardly surprising given that serious research has been going on for barely 100 years, and it turns out that the humans are quite complicated. But the answer to the limitations of medicine is not to invent fairy stories, which is what the alternative medicine industry does. There is no sensible option but to keep the research going and to test its results honestly. It’s sad but true that Big Pharma has at times corrupted medicine, by concealing negative results. But that corruption has been revealed by real scientists, not by health hucksters. In the end, science is self-correcting and the truth emerges. Health hucksters, on the other hand, seem incapable of giving up their beliefs whatever the evidence says. The idea of patient-centered care is fashionable and care is great, if you can’t cure. But there’s a whole spectrum in the wellbeing industry, from serious attempts to make people happier, to the downright nuts. The problem is that caring for patients make a very good bait, and the switch to woo tends to follow not far behind. I write from the perspective of someone who lives in a country that achieves health care for all its citizens at half the cost of the US system, and gets better outcomes in life expectancy and infant mortality. The view from outside is that US medicine rather resembles US religion. It has been taken over by fundamentalists who become very rich by persuading a gullible public to believe things that aren’t true. One of Freedman’s problems is, I think, that he vastly overestimates the power of the placebo effect. It exists, for sure, but in most cases, it seems to be small, erratic and transient. Acupuncture is a good example. It’s quite clear now that real acupuncture and sham acupuncture are indistinguishable, so it’s also quite clear that the ‘principles’ on which it’s based are simply hokum. If you do a non-blind comparison of acupuncture with no acupuncture, there is in some trials (not all) a small advantage for the acupuncture group. But it is too small to be of much benefit to the patient. By far the more important reason why ineffective voodoo like acupuncture appears to work is the “get better anyway” effect (known technically as regression to the mean). You take the needles or pills when you are at your worst, the next day you feel better. It’s natural to attribute the fact that you feel better to the needles or pills, when all you are seeing is natural fluctuations in the condition. It’s like Echinacea will cure your cold in only seven days when otherwise it would have taken a week. If the article itself was naïve and uncritical, the follow up was worse. It is rather surprising to me that a magazine like Atlantic should think it worth printing an advertorial for Andrew Weil’s business. Surely, though, Josephine Briggs, as director of an NIH institute is more serious? Sadly, no. Her piece is a masterpiece of clutching at straws. The fact is that her institute has spent over $ 2 billion of US taxpayers’ money and, for all that money it has produced not a single useful treatment. All that NCCAM has done is to show that several things do not work, something we pretty much knew already. If I were a US taxpayer, I’d be somewhat displeased by that. It should be shut down now. At first sight Dean Ornish sounds more respectable. He bases his arguments on diet and life style changes, which aren’t alternative at all. He’s done some research too. The problem is that it’s mostly preliminary and inconclusive research, on the basis of which he vastly exaggerates the strength of the evidence for what can be achieved by diet alone. It’s classical bait and switch again. The respectable, if ill-founded, arguments get you the foot in the door, and the woo follows later. This is all very sad for a country that realized quite early that the interests of patients were best served by using treatments that had been shown to work. The Flexner report of 1910 led the world in the rational education of physicians. But now even places like Yale and Harvard peddle snake oil to their students through their "integrative medicine" departments. It’s hard to see why the USA is in the vanguard of substituting wishful thinking for common sense and reason. The main reason, I’d guess, is money. Through NCCAM and the Bravewell Collaborative, large amounts of money have been thrown to the winds and businesses like Yale and Harvard have been quick to abandon their principles and grab the money. Another reason for the popularity of alternative medicine in parts of academia is that it’s a great deal easier to do ‘science’ when you are allowed to make up the answers. The "integrative medicine" symposium held at Yale in 2008 boggled the mind. Dr David Katz listed a lot of things he’d tried and which failed to work, His conclusion was not that they should be abandoned, but that we needed a "more fluid concept of evidence". You can see it on YouTube, Senator Tom Harkin’s promotion of NCCAM has done for the U.S. reputation in medicine what Dick Cheney did for the U.S. reputation in torture. It is hard to look at the USA from outside without thinking of the decline and fall of the Roman Empire. One had hoped that era was over with the election of Obama, but the hucksters won’t give up without a fight. They are making too much money to do that. |
Follow-up
The comments that appeared in The Atlantic on this piece were mostly less than enlightening -not quite what one expected of an intellectual magazine. Nevertheless I tried to answer all but the plain abusive comments.
More interesting, though, was an editorial by Jennie Rothenberg Gritz, the Atlantic Senior Editor who asked me to contribute. The Man Who Invented Medical School. It picked up on my mention of Abraham Flexner, and his famous 1910 report [download from Carnegie Foundation] which first put US medial education on a form rational footing. based on science. Now, 100 years later that’s being unpicked both in the USA and here. ms Gritz seemed to think that Flexner would have approved of Dean Ornish. In a response I begged to differ. I’m pretty sure that Felxner would have been furious of he could have seen the reecent march of quackademia, particularly, but not exclusively, in the USA. It is exactly the sort of thing his report set out, successfully, to abolish. He wrote, for example,
“the practitioner is subjected, year in, year out, to the steady bombardment of the unscrupulous manufacturer, persuasive to the uncritical, on the principle that “what I tell you three times is true.” Against bad example and persistent asseveration, only precise scientific concepts and a critical
appreciation of the nature and limits of actual demonstration can protect the young physician.” (Flexner report, 1910, pp 64-65)
It is this very “appreciation of the nature and limits of actual demonstration” that is now being abandoned by the alternative medicine industry. despite the fact that real medicine was in its infancy at the time he w as writing, he was very perceptive about the problems. Perhaps Freedman should read the report.
David Katz seems to have spotted my piece in The Atlantic, and has responded at great length in the Huffington Post (quite appropriate, given the consistent support of HuffPo for nonsense medicine). HuffPo allows only short comments with no links so I’ll reply to him here.
I fear that Dr Katz doth protest a great deal too much. He seems to object to a comment that I made about him in The Atlantic.
“… [He] listed a lot of things he’d tried and which failed to work. His conclusion was not that they should be abandoned, but that we needed a ‘a more fluid concept of evidence.'”
You don’t have to take my word for it. You can take it from the words of Dr Katz.
"What do we do when the evidence we have learned, or if we care to be more provocative, with which we have been indoctrinated, does now fully meet the needs of our patients"
It seems odd to me to regard teaching about how you distinguish what;s true and what isn’t as "indoctrination", though I can understand that knowledge of that subject could well diminish the income of alternative practitioners. You went on to say
"Some years ago the CDC funded us with a million dollars to do what they referred to initially as a systematic review of the evidence base for complementary and alternative medicine, Anybody who’s ever been involved in systematic reviews knows that’s a very silly thing. . . . Well we knew it was silly but a million dollars sounded real [mumbled] took the money and then we figurered we’d figure out what to do with it [smiles broadly]. That’s what we did ". . .
I do hope you told the CDC that you did not spend the million dollars for the sensible purpose for which it was awarded.
This infusion of calcium, magnesium and D vitamins and vitamin C ameliorates the symptoms of fibromyalgia. . . . We did typical placebo controlled randomized double-blind trial for several months . . . we saw an improvement in both our treatment and placebo groups . . .
You then describe how you tested yoga for asthma and homeopathy for attention deficit hyperactivity disorder, Neither of them worked either. Your reaction to this string of failures was just to say “we need a more fluid concept of evidence”
After telling an anecdote about one patient who got better after taking homeopathic treatment you said £I don’t care to get into a discussion of how, or even whether, homeopathy works”. Why not? It seems it doesn’t matter much to you whether the things you sell to patients work or not.
You then went on to describe quite accurately that anti-oxidants don’t work and neither do multivitamin supplements for prevention of cardiovascular problems, And once again you fail to accept the evidence, even evidence you have found yourself. Your response was
“So here too is an invitation to think more fluidly about of evidence. Absence of evidence is not evidence of absence.”
That last statement is the eternal cry of every quack. It’s true, of course, but that does not mean that absence of evidence gives you a licence to invent the answer. But inventing the answer is what you do, time after time, You seem quite incapable of saying the most important thing that anyone in your position should. I don’t know the answer.
Systems biology is all the rage, No surprise then, to see the University of Westminster advertising a job for a systems biologist in the The Department of Molecular and Applied Biosciences. Well, no surprise there -until you read the small print.
Much has been wriiten here about the University of Westminster, which remains the biggest provider of junk sciencne degrees in the UK, despite having closed two of them.
Senior Lecturer in Systems BiologyUniversity of Westminster – Department of Molecular and Applied Biosciences, School of Life SciencesCavendish Site Salary £37,886 – £50,751 (Inc. LWA) The Department of Molecular and Applied Biosciences wishes to appoint a Senior Lecturer in Systems Biology. The post-holder will teach on the undergraduate and postgraduate degree programmes within the School of Life Sciences, particularly in the areas of Molecular Biology, Bioinformatics and/or statistics, establish their own and participate in ongoing research programmes and undertake external income generation activities. The candidate should have an active interest in bridging the gap between western life sciences and Chinese medicine using emerging systems biology approaches, specifically in metabolomics and proteomics with a goal of developing novel diagnostic technologies facilitating the creation of a personalised approach to medical care. They should therefore be willing to work closely with colleagues in the life sciences as well as with clinicians and clinical researchers from within the East Asian medical tradition. The post is available from 1st October 2010 or as soon as possible thereafter. The closing date for applications, together with a short statement on why you believe you are suitable for the position and a description of your research plans, is Monday 6th September 2010. Interviews are expected to be held later in September. Administrative contact (for queries only): Tayjal Tailor (t.tailor1@wmin.ac.uk) Reference Number: 50000360 Closing Date: Friday 3 September 2010 |
A note about systems biology
Systems biology is about about how whole organs behave, as opposed to single cells or single molecules, It has to be the ultimate aim of biology. There is one case in which this has been done with some success, That is the modelling of the behaviour of the whole heart by Denis Noble and his colleagues in the Phyiology department (now gone) in Oxford. They adopted a bottom up approach. They measured the currents that flow though many sorts of ion channels in single cells from various parts of the heart, and how individual cells communicate with each other. Starting from this solid basis, together with a lot of computer power, they were able to model successfully a lot of phenomena that occur in the whole heart, but can’t be investigated in single cells. For example their work cast light on abnormal heart rhythms like ventricular fibrillation, and on the effect of drugs on heart rhythm.
This work was mostly done before the term ‘systems biology" thought of. It was called physiology. It is impressive work, and systems biology became a fashionable buzzword among research administrators and funding agencies. Despite the amount of money thrown at the problem, I’m not aware of any success that remotely approaches Noble’s.. One reason for that is that people have not been willing to put in the groundwork. In the case of the heart, the models were built on -many years of basic research on the electrophysiology of single heart cells. People have tried to model from the top down, without doing the spade work first. There has developed a perception that computing power can compensate for lack of basic knowledge about things work. It can’t. The usual aphorism applies: garbage in, garbage out.
Here’s an example, which eas noted in the diary pages for 29 June, 2008. While in Edinbuurgh, to give a talk to the European Conference on Mathematical and Theoretical Biology, I noticed a poster. It described an attempt to model on a computer the entire metabolic network of yeast.
“81 of the 662 intracellular concentrations were defined . . . The remainder were set to the median concentration of c. 0.2 mM.”
Ahem. We didn’t know the concentrations so we just made them up so we could run the program.
It’s interesting that even people in the business seem to realise that even that it isn’t living up to the hype. The Fixing proteomics web site shows why.
Put another way, if you try to run before you can walk, you risk falling falling on your face.
For these reasons, it seems to me that that most attempts at system biology have been disappointing (please correct me if I’m wrong)
Systems biology for Chinese medicine
If systems biology suffers from trying to run before it can walk in regular biology, where at least something is known about the functions of cells, how much more true that must be of Chinese medicine. In Chinese medicine almost all the treatments have never been tested properly in man. The odds are that most don’t work at all, and some are very poisonous (not to mention the cruelty and destruction of endangered species that is involved in making some of their more bizarre medicines). The idea that you can explain it with systems biology, is ludicrous in the extreme.
One can’t imagine any vaguely competent biologist who’d want to touch a project as bizarre as this with a bargepole.
Eastmedicine
This advertisement stems presumably from EASTmedicine is the University of Westminster’s research centre for East Asian Sciences and Traditions in Medicine. The proclaimed aims are to focus on “understanding, development and evaluation of East Asian medicines as living traditions”. The director of EASTmedicine, Volker Scheid, is a herbalist and acupuncturist and, as such, a firm believer in alternative medicine. When he isn’t at the University he has a private practice, the Traditional Acupuncture Centre, in London.
The website of his private practice makes some astonishing claims
"Acupuncture is effective in the treatment of numerous conditions including headache, migraine, digestive problems, menstrual disorders, indeterminate aches and pains, asthma, hayfever, stress, tiredness, depression and anxiety. Also commonly treated are chronic conditions such as arthritis, back pain, ulcerative colitis, irritable bowel syndrome, eczema, sinusitis, high blood pressure and repetitive strain injuries."
These claims simply cannot be justified by any worthwhile evidence. It will be interesting to see what Trading Standards make of them.
Dr Scheid describes himself as a "scholar physician". Physician seems a rather pretentious description for someone whose qualifications are stated to be PhD, MBAcC, FRCHM. But in similar vein he describes himself thus "I am one of the West’s leading experts on Chinese medical formulas and treatment strategies".
Although Scheid sells acupuncture treatments to patients, he seems ro be more anthropologist than medical. In a discussion of two acupuncture papers
"From the Perspective of the Anthropologist –
Volker Scheid, London, UK
From a perspective anchored in the cultural studies of science, technology and medicine my main interest in these papers is their status as cultural artifacts that provide access to the lifeworlds of a particular research community. If any, life-world debate and argument marks sites of contestation." Forsch Komplementärmed 2007;14:371–375
Scheid shows not the slightest interest in whether acupuncture works other than as a placebo. Since he is selling acupuncture, he presumably starts from the premise that it works.
Volker Scheid has had a £205,000 Wellcome Trust for the History of Medicine Project Grant: 2009 2012; Treating the Liver: Towards a Transnational History of East Asian Medicine; There’s nothing wrong with writing the history of long-outdated systems of medicine, though one could hardly imagine that the history would be very impartial, when it is written by a true believer. Another taste of his style can be found in his paper on Globalising Chinese Medical Understandings of Menopause. There is lots of rather pretentious stuff about culture, but very little about what actually works, Towards the end of the paper we come to the usual feeble excuse.
" . . once traditional medicines allow themselves to be evaluated by biomedical research methods, the odds against receiving fair treatment are heavily stacked against them."
The translation of that into plain English is something like ‘when we test our treatments properly we find they don’t work, so we blame the methods and carry on with selling them anyway’.
Judging from its web site, EASTmedicine does not to do any serious clinical trials to test whether the treaments work in man, They just know that they do. But they are hoping to add some spurious scientific background to their dubious claims by hiring someone to do compuations that will cast no light whatsoever on the question that really matters, Do they work or not?
The agenda is made clear by the statement
EASTmedicine seeks to describe and analyse the dynamics of these transformations with a specific view of managing their integration into contemporary health care.
So it is just yet another group of people pushing to have unproven and disproved treatments accepted by real medicine.
The University of Westminster appears to be determined to make itself the laughing stock by persisting in promoting junk science at a time when most other universities have realise that the harm done to their reputations is not worth the income it generates, Plenty of it has been revealed here.
The vice-chancellor of Westminster, Prof Geoffrey Petts, made into the pages of Private Eye (see Crystal balls. Professor Petts in Private Eye when he announced that he wouldn’t get rid of the junk, but would make it more ‘scientific’. Well, credit where it’s due, They have dropped homeopathy. see The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University For 2010 they still off ten different “BSc (Hons)” degrees in pre-scientific forms of medicine. It will take more than a bit od talk about systems biology to make anyone believe that these courses have anything to do with science.
For example, look at some slides from their lectures on “energy medicine”, Westminster University BSc: “amethysts emit high yin energy”
More make-believe from the University of Westminster. This time it’s Naturopathy , or
Why degrees in Chinese medicine are a danger to patients
The Dean of the School of the Life Sciences, Jane Lewis, is an entirely respectable marine biologist. She has had the thankless task of merging the real science with the alternative medicine in a single school. I phoned her to get a reaction
" outcome of merger of the school and trying to bring various parts of the school together" " "things are much more rigorous than they were".
DC: "Why don’t you just phase it out?"
"I’m not in a poition to do that. i move things forward as seems best -for the whole school I have to say". We’re retaining those bits thatI think have some good standing -I see NICE has approved the use of acupuncture for lower back pain and some other bits and pieces so I see acupuncture as something that does have some standing, andwe make sure it rigorously taught"
"DCHave you looked at the stuff on naturopathy?" "Are amethysts emit high Yin energy still taught?" " i don’t think so".
It seems, as so often in this case, that the senior people don’t really know what’s being taught under their noses. Prof
Lewis says she has not read about the background
to the (unusually) daft advice from NICE. Neither has she read Barker Bausell’s book on acupuncture research. If she had done any of these things,I suspect she would not have such a high opinion of it as appears to be the case.
Bait and switch. Astonishingly there is a now a whole organisation devoted to the respectabalisation of Traditional Chinese Medicine Good Practice in Traditional Chinese Medicine Research in the Post-genomic Era It sounds nice and sciencey but, as usual, they are trying to run before they can walk. The first thing has to be to do good clinical trials to find out if there is anything there to be investigated. If, and only if, this is the case, would there be any case for fancy talk about "proteomics"
and "the post-genomic era".
I do hope that no funding agency would be fooled into parting with money on the basis of the present vacuous rhetoric.
Professor Lewis said that I have I have quoted things like "amethysts emit high Yin energy" out of context. There is a simple solution to that. I have asked Westminster to make available the entire contents of the courses. Then we shall all be able to see the context of what their sudents are being taught.
Follow up
A brief report of this matter has appeared in Times Higher Education. In a statement, the University of Westminster says “its research into Chinese medicine is following the lead of “top research institutions”. I’m not aware of anyhting quite like this from anywhere else. In any case, Westminster should be able to think for themselves.
This post was one of the earliest on my old improbable science page (late 2002). It has been reproduced here because of the interest attached to Stephen Senn’s analysis of what appears to be a rather dubious trial, and because the subject purports to be regular medicine rather than alternative quackery. It is unlikely that all of the links will still be valid.
During research for a talk on quack medicines. I came across several web sites that were selling the common co-enzyme, NADH, for a whole variety of ailments. One of these sites, Wizards Gate, no longer sells NADH (“because the profit is too small”). but continues to carry the following advertisement for it.
| A recent Georgetown University Medical Center clinical pilot study among CFS patients reports that participants taking ENADA® were four times more likely than those taking a placebo to experience a reduction in symptoms.
Please click on the links below for more information. |
 |
What this does NOT mention is that the huge column on the left represents eight people out of 26, and the tiny one on the right represents two people (out of 26)!
The reader is then referred to ImmuneSupport.com, who describe NADH as follows (with my comments in italics).
- Improves cellular energy [This, as it stands, is meaningless]
- Elevates mental clarity [There is no evidence that this is true]
Promotes mental alertness and concentration [Again, there is no evidence that this is true]
The ImmuneSupport site goes on to say
“NADH is proven to trigger energy production through ATP generation [true].
A naturally occurring coenzyme found in all living cells, NADH helps supply cells with energy.[true].
Thus, as NADH levels rise in the body, the cells become more energized, helping the body feel stronger and more vitalized. [This sentence confuses energy in the technical sense that is used in physics, with the everyday use of the term to describe a mental and physical state, In fact there is no reason to think that NADH “helps the body feel stronger” to any greater extent than a placebo].
Other sites that promote NADH heavily are Enada.com, and the Menuco Corporation, of which more below
The clinical trial referred to in all of these advertisements is Forsyth, L. M., Preuss, H. G., MacDowell, A. L., Chiazze, L., Jr., Birkmayer, G. D., & Bellanti, J. A. (1999). Therapeutic effects of oral NADH on the symptoms of patients with chronic fatigue syndrome. Ann.Allergy Asthma Immunol. 82, 185-191.
It is very clear from the letter below that this trial is flawed, but it is impossible to see exactly how flawed it is because the authors, in breach of all guidelines on such matters, have refused, for over a year, to make available the raw data that would allow a correct analysis to be done.
|
Annals of Allergy, Asthma, & Immunology ©2000;84:639-640 To the Editor: We should like to comment on the paper by Forsyth et al. 1 This paper claims, on the basis of a randomized double-blind clinical trial, that NADH is effective in the treatment of chronic fatigue syndrome. It seems that there are several problems with the work described in this paper.
Drs Forsythe and Bellanti were asked in June 1999 to provide the raw data, in particular the crucial information on sequences that would allow re-analysis of their results. Despite several further requests we have not had any response. This is made all the more disturbing in view of fact that their paper is being used to justify vigorous marketing 3 of NADH as a treatment that “Enhances energy naturally, elevates mental clarity, improves alertness, and concentration,” which treatment is also being claimed by some to be useful for everything from improving athletic performance to Alzheimer’s disease. In view of this it seems that the least that it is owed the readers of your journal is for the authors to produce the original data so that their claims can be verified. David Colquhoun Professor of Pharmacology, University College London, Hon, Director Wellcome Laboratory for Molecular Pharmacology, Dept of Pharmacology, University College London, London, United Kingdom and , Professor of Pharmaceutical and Health Statistics, Department of Epidemiology & Public Health, REFERENCES1. Forsythe LM, Preuss HG, MacDowell AL, et al. Ann Allergy Asthma Immunol 2. Senn SJ. Cross-over trials in clinical research. Wiley, Chichester, 3. See, for example, http://www.enada.com/,http://www.wizardsgate.com/ |
Professor Bellanti’s response:
|
We have reviewed the two “Letters to the Editor” from Professors Colquhoun and Senn and from Professor Lorden and wish to respond to both. Recognizing that there are various methods and points of view concerning statistical analyses, since this was a preliminary study and not a definitive one, we chose to analyze the data in the manner described. This was done to determine whether there was a basis for the therapeutic efficacy of NADH in chronic fatigue syndrome and, if so, then to proceed to a larger, more definitive study. We feel that we have accomplished this goal in obtaining sufficient evidence to proceed further. We are grateful for the constructive elements of the readers’ comments and we shall take these into consideration as we plan the definitive studies. Joseph A Bellanti, MD |
This reply from Professor Bellanti stands in contrast to his own statement in a recent report presented to Annual Meeting of American College of Allergy, Asthma and Immunology in which he says “We have recently demonstrated the clinical effectiveness of reduced nicotinamide adenine dinucleotide (NADH) in a group of 26 patients with CFS in a double-blinded, placebo-controlled, crossover study”.
There is no mention here (or in any of the advertisements) of the study being “preliminary” or “not definitive”. (The measurement of 5-HIAA urinary concentration as a possible predictive marker of disease activity and therapeutic efficay of NADH in the chronic fatigue syndrome. Joseph A Bellanti MD; Linda M Forsyth MD; Ana Luiza MacDowell-Carneiro MD; Dawn B. Wallerstedt, MSN, FNP; Harry G Preuss MD and Georg D Birkmayer MD. PhD ).
This reply gives no reason at all for refusing to disclose the raw data, to allow others to check the conclusions. It does say that “there are various methods and points of view concerning statistical analyses”, but does not (unsurprisingly) refer to anyone who thinks that a test of difference between two independent estimates of a binomial proportion is an appropriate way to analyse a cross over trial.
Financial interests
The editor of Annals of Allergy, Asthma, & Immunology, Dr Edward O’Connell, tells me that the journal requires authors to disclose any financial interest in the work, and that no such interests were declared in the case of Forsyth et al. This seems very odd, since the address of one of the authors, Dr G.D Birkmayer is given as Birkmayer Pharmaceuticals (Vienna), who market the ENADA brand of NADH, on which Dr Birkmayer holds patents. Birkmayer Pharmacuticals supported the work by a grant, and analysed the data
Latest news The case of the Bellanti paper was referred to the Georgetown University’s Research Integrity Committee for review, in February 2001. That committee has reported that “no violation within the purview of the Code has been committed”. In the light of the facts concerning (a) improperly analysed data, (b) non-disclosure of financial interest and (c) the refusal to allow independent analysis of the data, it seems the the University has a novel view of what constitutes research integrity!