TCM
This piece is almost identical with today’s Spectator Health article.
This week there has been enormously wide coverage in the press for one of the worst papers on acupuncture that I’ve come across. As so often, the paper showed the opposite of what its title and press release, claimed. For another stunning example of this sleight of hand, try Acupuncturists show that acupuncture doesn’t work, but conclude the opposite: journal fails, published in the British Journal of General Practice).
Presumably the wide coverage was a result of the hyped-up press release issued by the journal, BMJ Acupuncture in Medicine. That is not the British Medical Journal of course, but it is, bafflingly, published by the BMJ Press group, and if you subscribe to press releases from the real BMJ. you also get them from Acupuncture in Medicine. The BMJ group should not be mixing up press releases about real medicine with press releases about quackery. There seems to be something about quackery that’s clickbait for the mainstream media.
As so often, the press release was shockingly misleading: It said
Acupuncture may alleviate babies’ excessive crying Needling twice weekly for 2 weeks reduced crying time significantly
This is totally untrue. Here’s why.
|
Luckily the Science Media Centre was on the case quickly: read their assessment. The paper made the most elementary of all statistical mistakes. It failed to make allowance for the jelly bean problem. The paper lists 24 different tests of statistical significance and focusses attention on three that happen to give a P value (just) less than 0.05, and so were declared to be "statistically significant". If you do enough tests, some are bound to come out “statistically significant” by chance. They are false postives, and the conclusions are as meaningless as “green jelly beans cause acne” in the cartoon. This is called P-hacking and it’s a well known cause of problems. It was evidently beyond the wit of the referees to notice this naive mistake. It’s very doubtful whether there is anything happening but random variability. And that’s before you even get to the problem of the weakness of the evidence provided by P values close to 0.05. There’s at least a 30% chance of such values being false positives, even if it were not for the jelly bean problem, and a lot more than 30% if the hypothesis being tested is implausible. I leave it to the reader to assess the plausibility of the hypothesis that a good way to stop a baby crying is to stick needles into the poor baby. If you want to know more about P values try Youtube or here, or here. |
One of the people asked for an opinion on the paper was George Lewith, the well-known apologist for all things quackish. He described the work as being a "good sized fastidious well conducted study ….. The outcome is clear". Thus showing an ignorance of statistics that would shame an undergraduate.
On the Today Programme, I was interviewed by the formidable John Humphrys, along with the mandatory member of the flat-earth society whom the BBC seems to feel obliged to invite along for "balance". In this case it was professional acupuncturist, Mike Cummings, who is an associate editor of the journal in which the paper appeared. Perhaps he’d read the Science media centre’s assessment before he came on, because he said, quite rightly, that
"in technical terms the study is negative" "the primary outcome did not turn out to be statistically significant"
to which Humphrys retorted, reasonably enough, “So it doesn’t work”. Cummings’ response to this was a lot of bluster about how unfair it was for NICE to expect a treatment to perform better than placebo. It was fascinating to hear Cummings admit that the press release by his own journal was simply wrong.
Listen to the interview here
Another obvious flaw of the study is that the nature of the control group. It is not stated very clearly but it seems that the baby was left alone with the acupuncturist for 10 minutes. A far better control would have been to have the baby cuddled by its mother, or by a nurse. That’s what was used by Olafsdottir et al (2001) in a study that showed cuddling worked just as well as another form of quackery, chiropractic, to stop babies crying.
Manufactured doubt is a potent weapon of the alternative medicine industry. It’s the same tactic as was used by the tobacco industry. You scrape together a few lousy papers like this one and use them to pretend that there’s a controversy. For years the tobacco industry used this tactic to try to persuade people that cigarettes didn’t give you cancer, and that nicotine wasn’t addictive. The main stream media obligingly invite the representatives of the industry who convey to the reader/listener that there is a controversy, when there isn’t.
Acupuncture is no longer controversial. It just doesn’t work -see Acupuncture is a theatrical placebo: the end of a myth. Try to imagine a pill that had been subjected to well over 3000 trials without anyone producing convincing evidence for a clinically useful effect. It would have been abandoned years ago. But by manufacturing doubt, the acupuncture industry has managed to keep its product in the news. Every paper on the subject ends with the words "more research is needed". No it isn’t.
Acupuncture is pre-scientific idea that was moribund everywhere, even in China, until it was revived by Mao Zedong as part of the appalling Great Proletarian Revolution. Now it is big business in China, and 100 percent of the clinical trials that come from China are positive.
if you believe them, you’ll truly believe anything.
Follow-up
29 January 2017
Soon after the Today programme in which we both appeared, the acupuncturist, Mike Cummings, posted his reaction to the programme. I thought it worth posting the original version in full. Its petulance and abusiveness are quite remarkable.
I thank Cummings for giving publicity to the video of our appearance, and for referring to my Wikipedia page. I leave it to the reader to judge my competence, and his, in the statistics of clinical trials. And it’s odd to be described as a "professional blogger" when the 400+ posts on dcscience.net don’t make a penny -in fact they cost me money. In contrast, he is the salaried medical director of the British Medical Acupuncture Society.
It’s very clear that he has no understanding of the error of the transposed conditional, nor even the mulltiple comparison problem (and neither, it seems, does he know the meaning of the word ‘protagonist’).
I ignored his piece, but several friends complained to the BMJ for allowing such abusive material on their blog site. As a result a few changes were made. The “baying mob” is still there, but the Wikipedia link has gone. I thought that readers might be interested to read the original unexpurgated version. It shows, better than I ever could, the weakness of the arguments of the alternative medicine community. To quote Upton Sinclair:
“It is difficult to get a man to understand something, when his salary depends upon his not understanding it.”
It also shows that the BBC still hasn’t learned the lessons in Steve Jones’ excellent “Review of impartiality and accuracy of the BBC’s coverage of science“. Every time I appear in such a programme, they feel obliged to invite a member of the flat earth society to propagate their make-believe.
Acupuncture for infantile colic – misdirection in the media or over-reaction from a sceptic blogger?26 Jan, 17 | by Dr Mike Cummings So there has been a big response to this paper press released by BMJ on behalf of the journal Acupuncture in Medicine. The response has been influenced by the usual characters – retired professors who are professional bloggers and vocal critics of anything in the realm of complementary medicine. They thrive on oiling up and flexing their EBM muscles for a baying mob of fellow sceptics (see my ‘stereotypical mental image’ here). Their target in this instant is a relatively small trial on acupuncture for infantile colic.[1] Deserving of being press released by virtue of being the largest to date in the field, but by no means because it gave a definitive answer to the question of the efficacy of acupuncture in the condition. We need to wait for an SR where the data from the 4 trials to date can be combined. So what about the research itself? I have already said that the trial was not definitive, but it was not a bad trial. It suffered from under-recruiting, which meant that it was underpowered in terms of the statistical analysis. But it was prospectively registered, had ethical approval and the protocol was published. Primary and secondary outcomes were clearly defined, and the only change from the published protocol was to combine the two acupuncture groups in an attempt to improve the statistical power because of under recruitment. The fact that this decision was made after the trial had begun means that the results would have to be considered speculative. For this reason the editors of Acupuncture in Medicine insisted on alteration of the language in which the conclusions were framed to reflect this level of uncertainty. DC has focussed on multiple statistical testing and p values. These are important considerations, and we could have insisted on more clarity in the paper. P values are a guide and the 0.05 level commonly adopted must be interpreted appropriately in the circumstances. In this paper there are no definitive conclusions, so the p values recorded are there to guide future hypothesis generation and trial design. There were over 50 p values reported in this paper, so by chance alone you must expect some to be below 0.05. If one is to claim statistical significance of an outcome at the 0.05 level, ie a 1:20 likelihood of the event happening by chance alone, you can only perform the test once. If you perform the test twice you must reduce the p value to 0.025 if you want to claim statistical significance of one or other of the tests. So now we must come to the predefined outcomes. They were clearly stated, and the results of these are the only ones relevant to the conclusions of the paper. The primary outcome was the relative reduction in total crying time (TC) at 2 weeks. There were two significance tests at this point for relative TC. For a statistically significant result, the p values would need to be less than or equal to 0.025 – neither was this low, hence my comment on the Radio 4 Today programme that this was technically a negative trial (more correctly ‘not a positive trial’ – it failed to disprove the null hypothesis ie that the samples were drawn from the same population and the acupuncture intervention did not change the population treated). Finally to the secondary outcome – this was the number of infants in each group who continued to fulfil the criteria for colic at the end of each intervention week. There were four tests of significance so we need to divide 0.05 by 4 to maintain the 1:20 chance of a random event ie only draw conclusions regarding statistical significance if any of the tests resulted in a p value at or below 0.0125. Two of the 4 tests were below this figure, so we say that the result is unlikely to have been chance alone in this case. With hindsight it might have been good to include this explanation in the paper itself, but as editors we must constantly balance how much we push authors to adjust their papers, and in this case the editor focussed on reducing the conclusions to being speculative rather than definitive. A significant result in a secondary outcome leads to a speculative conclusion that acupuncture ‘may’ be an effective treatment option… but further research will be needed etc… Now a final word on the 3000 plus acupuncture trials that DC loves to mention. His point is that there is no consistent evidence for acupuncture after over 3000 RCTs, so it clearly doesn’t work. He first quoted this figure in an editorial after discussing the largest, most statistically reliable meta-analysis to date – the Vickers et al IPDM.[2] DC admits that there is a small effect of acupuncture over sham, but follows the standard EBM mantra that it is too small to be clinically meaningful without ever considering the possibility that sham (gentle acupuncture plus context of acupuncture) can have clinically relevant effects when compared with conventional treatments. Perhaps now the best example of this is a network meta-analysis (NMA) using individual patient data (IPD), which clearly demonstrates benefits of sham acupuncture over usual care (a variety of best standard or usual care) in terms of health-related quality of life (HRQoL).[3] |
30 January 2017
I got an email from the BMJ asking me to take part in a BMJ Head-to-Head debate about acupuncture. I did one of these before, in 2007, but it generated more heat than light (the only good thing to come out of it was the joke about leprechauns). So here is my polite refusal.
|
Hello Thanks for the invitation, Perhaps you should read the piece that I wrote after the Today programme Why don’t you do these Head to Heads about genuine controversies? To do them about homeopathy or acupuncture is to fall for the “manufactured doubt” stratagem that was used so effectively by the tobacco industry to promote smoking. It’s the favourite tool of snake oil salesman too, and th BMJ should see that and not fall for their tricks. Such pieces night be good clickbait, but they are bad medicine and bad ethics. All the best David |
It’s hard to know what to make of David Tredinnick MP (Cons, Bosworth). He is certainly an extreme example of the scientific ignorance of our parliamentary representatives, but he isn’t alone in that. Our present minister of Education, Michael Gove, memorably referred to Newton’s Laws of Thermodynamics, blissfully unaware that thermodynamics was a 19th century development. And our present Minister of Health seems to think that magic water cures diseases.
But Mr Treddinick breaks every record for anti-scientific nonsense. That, no doubt, is why he was upset by the recent revision of come NHS Choices web pages, so that they now give a good account of the evidence (that’s their job, of course). They did that despite two years of obstruction by the Department of Health. which seemed to think that it was appropriate to take advice from Michael Dixon of the Prince’s Foundation for integrated Health. That shocking example of policy based evidence was revealed on this blog, and caused something of a stir.
Treddinick’s latest letter
A copy of a letter from Mr Tredinnick to the Minister of Health, Jeremy Hunt, has some into my possession by a tortuous route [download the letter]. It’s a corker. Here are a few quotations.
"1. UKIP moving onto our ground
Attached is an extract from a recent UKIP policy statement. The position which UKIP has taken is one with which most of our Daily Mail reading supporters of complementary medicine would agree."
It seems that Treddinick’s preferred authority on medicine is now Nigel Farage, leader of the UK’s far right party. UKIP’s policy on health is appended to the letter, and it’s as barmy as most of the other things they say.
"2. Herbal Medicine
. . .there is very real concern that the Government will not regulate Herbal Medicine and Traditional Chinese Medicine. The current situation is unacceptable, because herbal practitioners need regulation and cannot function as herbal therapists, nor can they cannot obtain stocks of their herbal remedies, without it.
This refers to a saga that has been running for at least 10 years. Herbalists are desperate to get a government stamp of approval by getting statutory regulation, much like real doctors have, despite the fact that they make money by selling sick people "an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety" (as quoted recently in the House of Lords).
Even the US National Center for Complementary and Alternative Medicine (NCCAM) doesn’t claim that a single herbal treatment is useful. The saga of herbal regulation is long and tedious. The short version is that a very bad report, The Pittilo report, recommended regulation of herbalists. After years of prevarication, Andrew Lansley ignored the impartial scientific advice and yielded to the pressure from the herbal industry to accept the Pittilo report. But still nothing has happened.
Could it be that even Jeremy Hunt realises, deep down, that the regulation of nonsense is a nonsense that would harm the public?
We can only hope that a letter from Mr Tredinnick is the kiss of death. Perhaps his continuous pestering will only reinforce the doubts that seem to exist at the Department of Health.
Then Tredinnick returns (yawn) to his obsession with magic water. He vents his rage at the now excellent NHS Choices page on homeopathy.
3. Homeopathy
"Recently this wording has been removed and instead a comment by the Chief Medical Officer that homeopathy is placebo inserted in its place, as well as links to external organisations which campaign against homeopathy. For instance, there is a link to the Sense About Science website, and Caroline Finucane, who is Editor of new content at NHS Choices, also writes for the Sense About Science website. This is an organisation which has no expertise in homeopathy and traces its roots back to the ultra-left Revolutionary Communist Party (RCP)."
"I respectfully suggest that the original wording be reinstated and these links to external organisations be removed or changed to ensure a balanced view.".
So it seems that he prefers the medical views of Nigel Farage and the Prince of Wales to those of the Chief Medical Officer and the government’s chief scientist. Disgracefully, Tredinnick picks out one particular employee of NHS Choices among many, and one who does an excellent job. And he raises the hoary old myth that Sense About Science is a communist organisation. Odd, since others accuse it of being neo-libertarian. The actual history is here. The organisation that is a bit too libertarian for my taste is Spiked Online. I haven’t agreed with every word that Sense about Science has printed, but they have a totally honest belief in evidence.
To drag in the name of one person out of many, and to justify it by a false history shows, once again, how very venomous and vindictive the advocates of delusional medicine can be when they feel cornered.
A bit more information about Mr Treddinick
This is what the BBC News profile says about him.
|
David Tredinnick is an old style Conservative MP, being an Eton-educated former Guards officer, who has sat in the Commons since 1987. However, his ambition for high office was thwarted by his role in one of the sleaze stories which helped to sink the Major government. He accepted £1,000 from an undercover reporter to ask parliamentary questions about a fictitious drug. He was obliged to resign from his role as a PPS and was suspended from the Commons for 20 sitting days. He has not sat on the frontbench since. He is an orthodox Conservative loyalist, though he is more supportive of the European Union than many of his colleagues. He has, however, carved himself a niche as the Commons’ most enthusiastic supporter of complementary medicine. He has wearied successive health secretaries with his persistent advocacy of any and all homeopathic remedies. He has also supported their use in prisons and even suggested them as an aid in alleviating the foot and mouth crisis. |
|
Tredinnick has also asserted that he was aware of a psychiatric hospital that doubled its staff at full moon (this is an old urban myth, and is, of course, quite untrue). His advocacy of homeopathic borax as a way to control the 2001 epidemic of foot and mouth diease can be read here. Luckily it was ignored by the government. I hope his latest letter will be treated similarly. Picture of David Tredinnick MP from the Conservative Party |
 |
Follow-up
The Scottish Universities Medical Journal asked me to write about the regulation of alternative medicine. It’s an interesting topic and not easy to follow because of the veritable maze of more than twenty overlapping regulators and quangos which fail utterly to protect the public against health fraud. In fact they mostly promote health fraud. The paper is now published, and here is a version with embedded links (and some small updates).
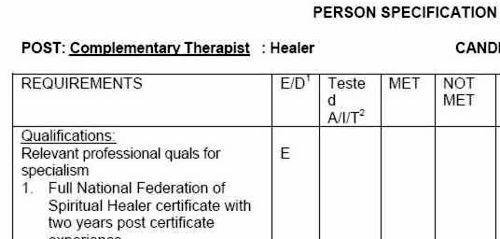
We are witnessing an increasing commercialisation of medicine. It’s really taken off since the passage of the Health and Social Security Bill into law. Not only does that mean having NHS hospitals run by private companies, but it means that “any qualified provider” can bid for just about any service. The problem lies, of course, in what you consider “qualified” to mean. Any qualified homeopath or herbalist will, no doubt, be eligible. University College London Hospital advertised for a spiritual healer. The "person specification" specified a "quallfication", but only HR people think that a paper qualification means that spiritual healing is anything but a delusion.
The vocabulary of bait and switch
First, a bit of vocabulary. Alternative medicine is a term that is used for medical treatments that don’t work (or at least haven’t been shown to work). If they worked, they’d be called “medicine”. The anti-malarial, artemesinin, came originally from a Chinese herb, but once it had been purified and properly tested, it was no longer alternative. But the word alternative is not favoured by quacks. They prefer their nostrums to be described as “complementary” –it sounds more respectable. So CAM (complementary and alternative medicine became the politically-correct euphemism. Now it has gone a stage further, and the euphemism in vogue with quacks at the moment is “integrated” or “integrative” medicine. That means, very often, integrating things that don’t work with things that do. But it sounds fashionable. In reality it is designed to confuse politicians who ask for, say, integrated services for old people.
Put another way, the salespeople of quackery have become rather good at bait and switch. The wikepedia definition is as good as any.
Bait-and-switch is a form of fraud, most commonly used in retail sales but also applicable to other contexts. First, customers are “baited” by advertising for a product or service at a low price; second, the customers discover that the advertised good is not available and are “switched” to a costlier product.
As applied to the alternative medicine industry, the bait is usually in the form of some nice touchy-feely stuff which barely mentions the mystical nonsense. But when you’ve bought into it you get the whole panoply of nonsense. Steven Novella has written eloquently about the use of bait and switch in the USA to sell chiropractic, acupuncture, homeopathy and herbal medicine: "The bait is that CAM offers legitimate alternatives, the switch is that it primarily promotes treatments that don’t work or are at best untested and highly implausible.".
The "College of Medicine" provides a near-perfect example of bait and switch. It is the direct successor of the Prince of Wales’ Foundation for Integrated Health. The Prince’s Foundation was a consistent purveyor of dangerous medical myths. When it collapsed in 2010 because of a financial scandal, a company was formed called "The College for Integrated Health". A slide show, not meant for public consumption, said "The College represents a new strategy to take forward the vision of HRH Prince Charles". But it seems that too many people have now tumbled to the idea that "integrated", in this context, means barmpottery. Within less than a month, the new institution was renamed "The College of Medicine". That might be a deceptive name, but it’s a much better bait. That’s why I described the College as a fraud and delusion.
Not only did the directors, all of them quacks, devise a respectable sounding name, but they also succeeded in recruiting some respectable-sounding people to act as figureheads for the new organisation. The president of the College is Professor Sir Graham Catto, emeritus professor of medicine at the University of Aberdeen. Names like his make the bait sound even more plausible. He claims not to believe that homeopathy works, but seems quite happy to have a homeopathic pharmacist, Christine Glover, on the governing council of his college. At least half of the governing Council can safely be classified as quacks.
So the bait is clear. What about the switch? The first thing to notice is that the whole outfit is skewed towards private medicine: see The College of Medicine is in the pocket of Crapita Capita. The founder, and presumably the main provider of funds (they won’t say how much) is the huge outsourcing company, Capita. This is company known in Private Eye as Crapita. Their inefficiency is legendary. They are the folks who messed up the NHS computer system and the courts computer system. After swallowing large amounts of taxpayers’ money, they failed to deliver anything that worked. Their latest failure is the court translation service.. The president (Catto), the vice president (Harry Brunjes) and the CEO (Mark Ratnarajah) are all employees of Capita.
The second thing to notice is that their conferences and courses are a bizarre mixture of real medicine and pure quackery. Their 2012 conference had some very good speakers, but then it had a "herbal workshop" with Simon Mills (see a video) and David Peters (the man who tolerates dowsing as a way to diagnose which herb to give you). The other speaker was Dick Middleton, who represents the huge herbal company, Schwabe (I debated with him on BBC Breakfast), In fact the College’s Faculty of Self-care appears to resemble a marketing device for Schwabe.
Why regulation isn’t working, and can’t work
There are various levels of regulation. The "highest" level is the statutory regulation of osteopathy and chiropractic. The General Chiropractic Council (GCC) has exactly the same legal status as the General Medical Council (GMC). This ludicrous state of affairs arose because nobody in John Major’s government had enough scientific knowledge to realise that chiropractic, and some parts of osteopathy, are pure quackery,
The problem is that organisations like the GCC function more to promote chiropractic than to regulate them. This became very obvious when the British Chiropractic Association (BCA) decided to sue Simon Singh for defamation, after he described some of their treatments as “bogus”, “without a jot of evidence”.
In order to support Singh, several bloggers assessed the "plethora of evidence" which the BCA said could be used to justify their claims. When, 15 months later, the BCA produced its "plethora" it was shown within 24 hours that the evidence was pathetic. The demolition was summarised by lawyer, David Allen Green, in The BCA’s Worst Day.
In the wake of this, over 600 complaints were made to the GCC about unjustified claims made by chiropractors, thanks in large part to heroic work by two people, Simon Perry and Allan Henness. Simon Perry’s Fishbarrel (browser plugin) allows complaints to be made quickly and easily -try it). The majority of these complaints were rejected by the GCC, apparently on the grounds that chiropractors could not be blamed because the false claims had been endorsed by the GCC itself.
My own complaint was based on phone calls to two chiropractors, I was told such nonsense as "colic is down to, er um, faulty movement patterns in the spine". But my complaint never reached the Conduct and Competence committee because it had been judged by a preliminary investigating committee that there was no case to answer. The impression one got from this (very costly) exercise was that the GCC was there to protect chiropractors, not to protect the public.
The outcome was a disaster for chiropractors, wno emerged totally discredited. It was also a disaster for the GCC which was forced to admit that it hadn’t properly advised chiropractors about what they could and couldn’t claim. The recantation culminated in the GCC declaring, in August 2010, that the mythical "subluxation" is a "historical concept " "It is not supported by any clinical research evidence that would allow claims to be made that it is the cause of disease.". Subluxation was a product of the fevered imagination of the founder of the chiropractic cult, D.D. Palmer. It referred to an imaginary spinal lesion that he claimed to be the cause of most diseases. .Since ‘subluxation’ is the only thing that’s distinguished chiropractic from any other sort of manipulation, the admission by the GCC that it does not exist, after a century of pretending that it does, is quite an admission.
The President of the BCA himself admitted in November 2011
“The BCA sued Simon Singh personally for libel. In doing so, the BCA began one of the darkest periods in its history; one that was ultimately to cost it financially,”
As a result of all this, the deficiencies of chiropractic, and the deficiencies of its regulator were revealed, and advertisements for chiropractic are somewhat less misleading. But this change for the better was brought about entirely by the unpaid efforts of bloggers and a few journalists, and not at all by the official regulator, the GCC. which was part of the problem. not the solution. And it was certainly not helped by the organisation that is meant to regulate the GCC, the Council for Health Regulatory Excellence (CHRE) which did nothing whatsoever to stop the farce.
At the other end of the regulatory spectrum, voluntary self-regulation, is an even worse farce than the GCC. They all have grand sounding "Codes of Practice" which, in practice, the ignore totally.
The Society of Homeopaths is just a joke. When homeopaths were caught out recommending sugar pills for prevention of malaria, they did nothing (arguably such homicidal advice deserves a jail sentence).
The Complementary and Natural Healthcare Council (CNHC) is widely know in the blogosphere as Ofquack. I know about them from the inside, having been a member of their Conduct and Competence Committee, It was set up with the help of a £900,000 grant from the Department of Health to the Prince of Wales, to oversee voluntary self-regulation. It fails utterly to do anything useful.. The CNHC code of practice, paragraph 15 , states
“Any advertising you undertake in relation to your professional activities must be accurate. Advertisements must not be misleading, false, unfair or exaggerated”.
When Simon Perry made a complaint to the CNHC about claims being made by a CNHC-registered reflexologist, the Investigating Committee upheld all 15 complaints. But it then went on to say that there was no case to answer because the unjustified claims were what the person had been taught, and were made in good faith.
This is precisely the ludicrous situation which will occur again and again if reflexologists (and many other alternative therapies) are “accredited”. The CNHC said, correctly, that the reflexologist had been taught things that were not true, but then did nothing whatsoever about it apart from toning down the advertisements a bit. They still register reflexologists who make outrageously false claims.
Once again we see that no sensible regulation is possible for subjects that are pure make-believe.
The first two examples deal (or rather, fail to deal) with regulation of outright quackery. But there are dozens of other quangos that sound a lot more respectable.
European Food Standards Agency (EFSA). One of the common scams is to have have your favourite quack treatment classified as a food not as a medicine. The laws about what you can claim have been a lot laxer for foods. But the EFSA has done a pretty good job in stopping unjustified claims for health benefits from foods. Dozens of claims made by makers of probiotics have been banned. The food industry, needless to say, objects very strongly to be being forced to tell the truth. In my view, the ESFA has not gone far enough. They recently issued a directive about claims that could legally be made. Some of these betray the previously high standards of the EFSA. For example you are allowed to say that "Vitamin C contributes to the reduction of tiredness and fatigue" (as long as the product contains above a specified amount of Vitamin C. I’m not aware of any trials that show vitamin C has the slightest effect on tiredness or fatigue, Although these laws do not come into effect until December 2012, they have already been invoked by the ASA has a reason not to uphold a complaint about a multivitamin pill which claimed that it “Includes 8 nutrients that can contribute to the reduction in tiredness and fatigue”
The Advertising Standards Authority (ASA). This is almost the only organisation that has done a good job on false health claims. Their Guidance on Health Therapies & Evidence says
"Whether you use the words ‘treatment’, ‘treat’ or ‘cure’, all are likely to be seen by members of the public as claims to alleviate effectively a condition or symptom. We would advise that they are not used"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
They are spot on.
The ASA’s Guidance for Advertisers of Homeopathic Services is wonderful.
"In the simplest terms, you should avoid using efficacy claims, whether implied or direct,"
"To date, the ASA has have not seen persuasive evidence to support claims that homeopathy can treat, cure or relieve specific conditions or symptoms."
That seems to condemn the (mis)labelling allowed by the MHRA as breaking the rules.. Sadly, though, the ASA has no powers to enforce its decisions and only too often they are ignored. The Nightingale collaboration has produced an excellent letter that you can hand to any pharmacist who breaks the rules
The ASA has also judged against claims made by "Craniosacral therapists" (that’s the lunatic fringe of osteopathy). They will presumably uphold complaints about similar claims made (I’m ashamed to say) by UCLH Hospitals.
The private examination company Edexcel sets exams in antiscientific subjects, so miseducating children. The teaching of quackery to 16 year-olds has been approved by a maze of quangos, none of which will take responsibility, or justify their actions. So far I’ve located no fewer than eight of them. The Office of the Qualifications and Examinations Regulator (OfQual), Edexcel, the Qualifications and Curriculum Authority (QCA), Skills for Health, Skills for Care, National Occupational Standards (NOS), private exam company VTCT and the schools inspectorate, Ofsted.. Asking any of these people why they approve of examinations in imaginary subjects meets with blank incomprehension. They fail totally to protect tha public from utter nonsense.
The Department of Education has failed to do anything about the miseducation of children in quackery. In fact it has encouraged it by, for the first time, giving taxpayers’ money to a Steiner (Waldorf) school (at Frome, in Somerset). Steiner schools are run by a secretive and cult-like body of people (read about it). They teach about reincarnation, karma, gnomes, and all manner of nonsense, sometimes with unpleasant racial overtones. The teachers are trained in Steiner’s Anthroposophy, so if your child gets ill at school they’ll probably get homeopathic sugar pills. They might well get measles or mumps too, since Steiner people don’t believe in vaccination.
Incredibly, the University of Aberdeen came perilously close to appointing a chair in anthroposophical medicine. This disaster was aborted by bloggers, and a last minute intervention from journalists. Neither the university’s regulatory mechanisms. nor any others, seemed to realise that a chair in mystical barmpottery was a bad idea.
Trading Standards offices and the Office of Fair Trading.
It is the statutory duty of Trading Standards to enforce the Consumer Protection Regulations (2008) This European legislation is pretty good. it caused a lawyer to write " Has The UK Quietly Outlawed “Alternative” Medicine?". Unfortunately Trading Standards people have consistently refused to enforce these laws. The whole organisation is a mess. Its local office arrangement fails totally to deal with the age of the internet. The situation is so bad that a group of us decided to put them to the test. The results were published in the Medico-Legal Journal, Rose et al., 2012. "Spurious Claims for Health-care Products: An Experimental Approach to Evaluating Current UK Legislation and its Implementation". They concluded "EU directive 2005/29/EC is
largely ineffective in preventing misleading health claims for consumer products in
the UK"
Skills for Health is an enormous quango which produces HR style "competences" for everything under the son. They are mostly quite useless. But those concerned with alternative medicine are not just useless. They are positively harmful. Totally barmy. There are competences and National Occupational Standards for every lunatic made-up therapy under the sun. When I phoned them to discover who’d written them, I learned that the had been drafted by the Prince of Wales’ Foundation for Magic Medicine. And when I joked by asking if they had a competence for talking to trees, I was told, perfectly seriously, “You’d have to talk to LANTRA, the land-based organisation for that.”
That was in January 2008. A lot of correspondence with the head of Skills for Health got nowhere at all. She understood nothing and it hasn’t improved a jot.
This organisation costs a lot of taxpayers’ money and it should have been consigned to the "bonfire of the quangos" (but of course there was no such bonfire in reality). It is a disgrace.
The Quality Assurance Agency (QAA) is supposed to ensure the quality of university courses. In fact it endorses courses in nonsense alternative medicine and so does more harm than good. The worst recent failure of the QAA was in the case of the University of Wales: see Scandal of the University of Wales and the Quality Assurance Agency. The university was making money by validating thousands of external degrees in everything from fundamentalist theology to Chinese Medicine. These validations were revealed as utterly incompetent by bloggers, and later by BBC Wales journalist Ciaran Jenkins (now working for Channel 4).
The mainstream media eventually caught up with bloggers. In 2010, BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. The programme can be seen on YouTube (Part 1, and Part 2). The programme also exposed, incidentally, the uselessness of the Quality Assurance Agency (QAA) which did nothing until the scam was exposed by TV and blogs. Eventually the QAA sent nine people to Malaysia to investigate a dodgy college that had been revealed by the BBC. The trip cost £91,000. It could have been done for nothing if anyone at the QAA knew how to use Google.
The outcome was that the University of Wales stopped endorsing external courses, and it was soon shut down altogether (though bafflingly, its vice-chancellor, Marc Clement was promoted). The credit for this lies entirely with bloggers and the BBC. The QAA did nothing to help until the very last moment.
Throughout this saga Universities UK (UUK), has maintained its usual total passivity. They have done nothing whatsoever about their members who give BSc degrees in anti-scientific subjects. (UUK used to known as the Committee of Vice-Chancellors and Principals).
Council for Health Regulatory Excellence (CHRE), soon to become the PSAHSC,
Back now to the CHRE, the people who failed so signally to sort out the GCC. They are being reorganised. Their consultation document says
"The Health and Social Care Act 20122 confers a new function on the Professional Standards Authority for Health and Social Care (the renamed Council for Healthcare Regulatory Excellence). From November 2012 we will set standards for organisations that hold voluntary registers for people working in health and social care occupations and we will accredit the register if they meet those standards. It will then be known as an ‘Accredited Register’. "
They are trying to decide what the criteria should be for "accreditation" of a regulatory body. The list of those interested has some perfectly respectable organisations, like the British Psychological Society. It also contains a large number of crackpot organisations, like Crystal and Healing International, as well as joke regulators like the CNHC.
They already oversee the Health Professions Council (HPC) which is due to take over Herbal medicine and Traditional Chinese Medicine, with predictably disastrous consequences.
Two of the proposed criteria for "accreditation" appear to be directly contradictory.
Para 2.5 makes the whole accreditation pointless from the point of view of patients
2.5 It will not be an endorsement of the therapeutic validity or effectiveness of any particular discipline or treatment.
Since the only thing that matters to the patient is whether the therapy works (and is safe), accrediting of organisations that ignore this will merely give the appearance of official approval of crystal healing etc etc. This appears to contradict directly
A.7 The organisation can demonstrate that there either is a sound knowledge base underpinning the profession or it is developing one and makes that explicit to the public.
A "sound knowledge base", if it is to mean anything useful at all, means knowledge that the treatment is effective. If it doesn’t mean that, what does it mean?
It seems that the official mind has still not grasped the obvious fact that there can be no sensible regulation of subjects that are untrue nonsense. If it is nonsense, the only form of regulation that makes any sense is the law.
Please fill in the consultation. My completed return can be downloaded as an example, if you wish.
Medicines and Healthcare products Regulatory Agency (MHRA) should be a top level defender of truth. Its strapline is
"We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
The MHRA did something (they won’t tell me exactly what) about one of the most cruel scams that I’ve ever encountered, Esperanza Homeopathic Neuropeptide, peddled for multiple sclerosis, at an outrageous price ( £6,759 for 12 month’s supply). Needless to say there was not a jot of evidence that it worked (and it wasn’t actually homeopathic).
Astoundingly, Trading Standards officers refused to do anything about it.
The MHRA admit (when pushed really hard) that there is precious little evidence that any of the herbs work, and that homeopathy is nothing more than sugar pills. Their answer to that is to forget that bit about "ensuring that medicines … work"
Here’s the MHRA’s Traditional Herbal Registration Certificate for devils claw tablets.

The wording "based on traditional use only" has to be included because of European legislation. Shockingly, the MHRA have allowed them to relegate that to small print, with all the emphasis on the alleged indications. The pro-CAM agency NCCAM rates devil’s claw as "possibly effective" or "insufficient evidence" for all these indications, but that doesn’t matter because the MHRA requires no evidence whatsoever that the tablets do anything. They should, of course, added a statement to this effect to the label. They have failed in their duty to protect and inform the public by allowing this labelling.
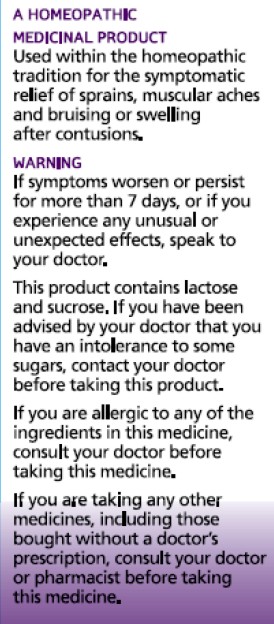
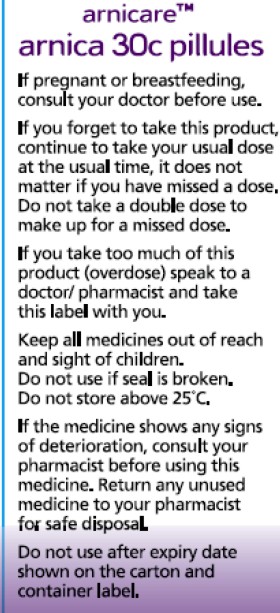
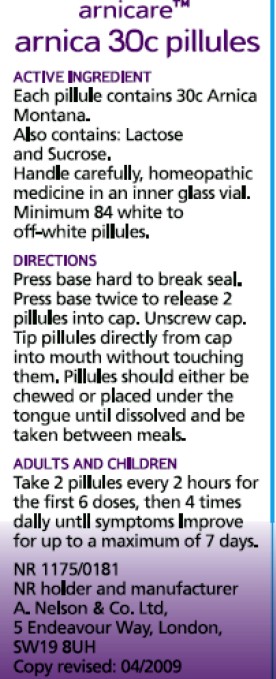
But it gets worse. Here is the MHRA’s homeopathic marketing authorisation for the homeopathic medicinal product Arnicare Arnica 30c pillules
It is nothing short of surreal.
|
|
Since the pills contain nothing at all, they don’t have the slightest effect on sprains, muscular aches or bruising. The wording on the label is exceedingly misleading.
If you "pregnant or breastfeeding" there is no need to waste you doctor’s time before swallowing a few sugar pills.
"Do not take a double dose to make up for a missed one". Since the pills contain nothing, it doesn’t matter a damn.
"If you overdose . . " it won’t have the slightest effect because there is nothing in them
And it gets worse. The MHRA-approved label specifies ACTIVE INGREDIENT. Each pillule contains 30c Arnica Montana
No, they contain no arnica whatsoever.
|
|
It truly boggles the mind that men with dark suits and lots of letters after their names have sat for hours only to produce dishonest and misleading labels like these.
When this mislabeling was first allowed, it was condemned by just about every scientific society, but the MHRA did nothing.
The Nightingale Collaboration.
This is an excellent organisation, set up by two very smart skeptics, Alan Henness and Maria MacLachlan. Visit their site regularly, sign up for their newsletter Help with their campaigns. Make a difference.
Conclusions
The regulation of alternative medicine in the UK is a farce. It is utterly ineffective in preventing deception of patients.
Such improvements as have occurred have resulted from the activity of bloggers, and sometime the mainstream media. All the official regulators have, to varying extents, made things worse.
The CHRE proposals promise to make matters still worse by offering "accreditation" to organisations that promote nonsensical quackery. None of the official regulators seem to be able to grasp the obvious fact that is impossible to have any sensible regulation of people who promote nonsensical untruths. One gets the impression that politicians are more concerned to protect the homeopathic (etc, etc) industry than they are to protect patients.
Deception by advocates of alternative medicine harms patients. There are adequate laws that make such deception illegal, but they are not being enforced. The CHRE and its successor should restrict themselves to real medicine. The money that they spend on pseudo-regulation of quacks should be transferred to the MHRA or a reformed Trading Standards organisation so they can afford to investigate and prosecute breaches of the law. That is the only form of regulation that makes sense.
Follow-up
The shocking case of the continuing sale of “homeopathic vaccines” for meningitis, rubella, pertussis etc was highlighted in an excellent TV programme by BBC South West. The failure of the MHRA and the GPC do take any effective action is a yet another illustration of the failure of regulators to do their job. I have to agree with Andy Lewis when he concludes
“Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator.”
One wonders about the standards of peer review at the British Journal of General Practice. The June issue has a paper, "Acupuncture for ‘frequent attenders’ with medically unexplained symptoms: a randomised controlled trial (CACTUS study)". It has lots of numbers, but the result is very easy to see. Just look at their Figure.
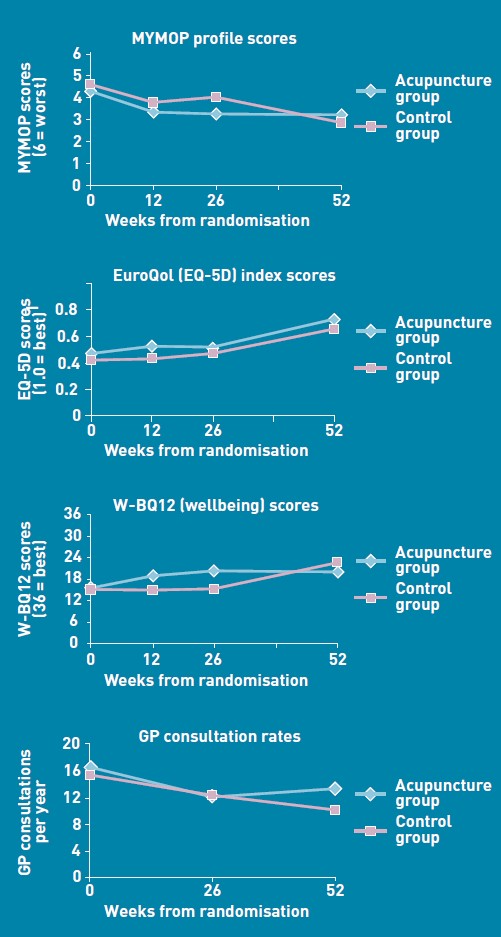
There is no need to wade through all the statistics; it’s perfectly obvious at a glance that acupuncture has at best a tiny and erratic effect on any of the outcomes that were measured.
But this is not what the paper said. On the contrary, the conclusions of the paper said
|
Conclusion The addition of 12 sessions of five-element acupuncture to usual care resulted in improved health status and wellbeing that was sustained for 12 months. |
How on earth did the authors manage to reach a conclusion like that?
The first thing to note is that many of the authors are people who make their living largely from sticking needles in people, or advocating alternative medicine. The authors are Charlotte Paterson, Rod S Taylor, Peter Griffiths, Nicky Britten, Sue Rugg, Jackie Bridges, Bruce McCallum and Gerad Kite, on behalf of the CACTUS study team. The senior author, Gerad Kite MAc , is principal of the London Institute of Five-Element Acupuncture London. The first author, Charlotte Paterson, is a well known advocate of acupuncture. as is Nicky Britten.
The conflicts of interest are obvious, but nonetheless one should welcome a “randomised controlled trial” done by advocates of alternative medicine. In fact the results shown in the Figure are both interesting and useful. They show that acupuncture does not even produce any substantial placebo effect. It’s the authors’ conclusions that are bizarre and partisan. Peer review is indeed a broken process.
That’s really all that needs to be said, but for nerds, here are some more details.
How was the trial done?
The description "randomised" is fair enough, but there were no proper controls and the trial was not blinded. It was what has come to be called a "pragmatic" trial, which means a trial done without proper controls. They are, of course, much loved by alternative therapists because their therapies usually fail in proper trials. It’s much easier to get an (apparently) positive result if you omit the controls. But the fascinating thing about this study is that, despite the deficiencies in design, the result is essentially negative.
The authors themselves spell out the problems.
“Group allocation was known by trial researchers, practitioners, and patients”
So everybody (apart from the statistician) knew what treatment a patient was getting. This is an arrangement that is guaranteed to maximise bias and placebo effects.
"Patients were randomised on a 1:1 basis to receive 12 sessions of acupuncture starting immediately (acupuncture group) or starting in 6 months’ time (control group), with both groups continuing to receive usual care."
So it is impossible to compare acupuncture and control groups at 12 months, contrary to what’s stated in Conclusions.
"Twelve sessions, on average 60 minutes in length, were provided over a 6-month period at approximately weekly, then fortnightly and monthly intervals"
That sounds like a pretty expensive way of getting next to no effect.
"All aspects of treatment, including discussion and advice, were individualised as per normal five-element acupuncture practice. In this approach, the acupuncturist takes an in-depth account of the patient’s current symptoms and medical history, as well as general health and lifestyle issues. The patient’s condition is explained in terms of an imbalance in one of the five elements, which then causes an imbalance in the whole person. Based on this elemental diagnosis, appropriate points are used to rebalance this element and address not only the presenting conditions, but the person as a whole".
Does this mean that the patients were told a lot of mumbo jumbo about “five elements” (fire earth, metal, water, wood)? If so, anyone with any sense would probably have run a mile from the trial.
"Hypotheses directed at the effect of the needling component of acupuncture consultations require sham-acupuncture controls which while appropriate for formulaic needling for single well-defined conditions, have been shown to be problematic when dealing with multiple or complex conditions, because they interfere with the participative patient–therapist interaction on which the individualised treatment plan is developed. 37–39 Pragmatic trials, on the other hand, are appropriate for testing hypotheses that are directed at the effect of the complex intervention as a whole, while providing no information about the relative effect of different components."
Put simply that means: we don’t use sham acupuncture controls so we can’t distinguish an effect of the needles from placebo effects, or get-better-anyway effects.
"Strengths and limitations: The ‘black box’ study design precludes assigning the benefits of this complex intervention to any one component of the acupuncture consultations, such as the needling or the amount of time spent with a healthcare professional."
"This design was chosen because, without a promise of accessing the acupuncture treatment, major practical and ethical problems with recruitment and retention of participants were anticipated. This is because these patients have very poor self-reported health (Table 3), have not been helped by conventional treatment, and are particularly desperate for alternative treatment options.".
It’s interesting that the patients were “desperate for alternative treatment”. Again it seems that every opportunity has been given to maximise non-specific placebo, and get-well-anyway effects.
There is a lot of statistical analysis and, unsurprisingly, many of the differences don’t reach statistical significance. Some do (just) but that is really quite irrelevant. Even if some of the differences are real (not a result of random variability), a glance at the figures shows that their size is trivial.
My conclusions
(1) This paper, though designed to be susceptible to almost every form of bias, shows staggeringly small effects. It is the best evidence I’ve ever seen that not only are needles ineffective, but that placebo effects, if they are there at all, are trivial in size and have no useful benefit to the patient in this case..
(2) The fact that this paper was published with conclusions that appear to contradict directly what the data show, is as good an illustration as any I’ve seen that peer review is utterly ineffective as a method of guaranteeing quality. Of course the editor should have spotted this. It appears that quality control failed on all fronts.
Follow-up
In the first four days of this post, it got over 10,000 hits (almost 6,000 unique visitors).
Margaret McCartney has written about this too, in The British Journal of General Practice does acupuncture badly.
The Daily Mail exceeds itself in an article by Jenny Hope whch says “Millions of patients with ‘unexplained symptoms’ could benefit from acupuncture on the NHS, it is claimed”. I presume she didn’t read the paper.
The Daily Telegraph scarcely did better in Acupuncture has significant impact on mystery illnesses. The author if this, very sensibly, remains anonymous.
Many “medical information” sites churn out the press release without engaging the brain, but most of the other newspapers appear, very sensibly, to have ignored ther hyped up press release. Among the worst was Pulse, an online magazine for GPs. At least they’ve publish the comments that show their report was nonsense.
The Daily Mash has given this paper a well-deserved spoofing in Made-up medicine works on made-up illnesses.
“Professor Henry Brubaker, of the Institute for Studies, said: “To truly assess the efficacy of acupuncture a widespread double-blind test needs to be conducted over a series of years but to be honest it’s the equivalent of mapping the DNA of pixies or conducting a geological study of Narnia.” ”
There is no truth whatsoever in the rumour being spread on Twitter that I’m Professor Brubaker.
Euan Lawson, also known as Northern Doctor, has done another excellent job on the Paterson paper: BJGP and acupuncture – tabloid medical journalism. Most tellingly, he reproduces the press release from the editor of the BJGP, Professor Roger Jones DM, FRCP, FRCGP, FMedSci.
"Although there are countless reports of the benefits of acupuncture for a range of medical problems, there have been very few well-conducted, randomised controlled trials. Charlotte Paterson’s work considerably strengthens the evidence base for using acupuncture to help patients who are troubled by symptoms that we find difficult both to diagnose and to treat."
Oooh dear. The journal may have a new look, but it would be better if the editor read the papers before writing press releases. Tabloid journalism seems an appropriate description.
Andy Lewis at Quackometer, has written about this paper too, and put it into historical context. In Of the Imagination, as a Cause and as a Cure of Disorders of the Body. “In 1800, John Haygarth warned doctors how we may succumb to belief in illusory cures. Some modern doctors have still not learnt that lesson”. It’s sad that, in 2011, a medical journal should fall into a trap that was pointed out so clearly in 1800. He also points out the disgracefully inaccurate Press release issued by the Peninsula medical school.
Some tweets
Twitter info 426 clicks on http://bit.ly/mgIQ6e alone at 15.30 on 1 June (and that’s only the hits via twitter). By July 8th this had risen to 1,655 hits via Twitter, from 62 different countries,
@followthelemur Selina
MASSIVE peer review fail by the British Journal of General Practice http://bit.ly/mgIQ6e (via @david_colquhoun)
@david_colquhoun David Colquhoun
Appalling paper in Brit J Gen Practice: Acupuncturists show that acupuncture doesn’t work, but conclude the opposite http://bit.ly/mgIQ6e
Retweeted by gentley1300 and 36 others
@david_colquhoun David Colquhoun.
I deny the Twitter rumour that I’m Professor Henry Brubaker as in Daily Mash http://bit.ly/mt1xhX (just because of http://bit.ly/mgIQ6e )
@brunopichler Bruno Pichler
http://tinyurl.com/3hmvan4 Made-up medicine works on made-up illnesses (me thinks Henry Brubaker is actually @david_colquhoun)
@david_colquhoun David Colquhoun,
HEHE RT @brunopichler: http://tinyurl.com/3hmvan4 Made-up medicine works on made-up illnesses
@psweetman Pauline Sweetman
Read @david_colquhoun’s take on the recent ‘acupuncture effective for unexplained symptoms’ nonsense: bit.ly/mgIQ6e
@bodyinmind Body In Mind
RT @david_colquhoun: ‘Margaret McCartney (GP) also blogged acupuncture nonsense http://bit.ly/j6yP4j My take http://bit.ly/mgIQ6e’
@abritosa ABS
Br J Gen Practice mete a pata na poça: RT @david_colquhoun […] appalling acupuncture nonsense http://bit.ly/j6yP4j http://bit.ly/mgIQ6e
@jodiemadden Jodie Madden
amusing!RT @david_colquhoun: paper in Brit J Gen Practice shows that acupuncture doesn’t work,but conclude the opposite http://bit.ly/mgIQ6e
@kashfarooq Kash Farooq
Unbelievable: acupuncturists show that acupuncture doesn’t work, but conclude the opposite. http://j.mp/ilUALC by @david_colquhoun
@NeilOConnell Neil O’Connell
Gobsmacking spin RT @david_colquhoun: Acupuncturists show that acupuncture doesn’t work, but conclude the opposite http://bit.ly/mgIQ6e
@euan_lawson Euan Lawson (aka Northern Doctor)
Aye too right RT @david_colquhoun @iansample @BenGoldacre Guardian should cover dreadful acupuncture paper http://bit.ly/mgIQ6e
@noahWG Noah Gray
Acupuncturists show that acupuncture doesn’t work, but conclude the opposite, from @david_colquhoun: http://bit.ly/l9KHLv
8 June 2011 I drew the attention of the editor of BJGP to the many comments that have been made on this paper. He assured me that the matter would be discussed at a meeting of the editorial board of the journal. Tonight he sent me the result of this meeting.
|
Subject: BJGP Dear Prof Colquhoun We discussed your emails at yesterday’s meeting of the BJGP Editorial Board, attended by 12 Board members and the Deputy Editor The Board was unanimous in its support for the integrity of the Journal’s peer review process for the Paterson et al paper – which was accepted after revisions were made in response to two separate rounds of comments from two reviewers and myself – and could find no reason either to retract the paper or to release the reviewers’ comments Some Board members thought that the results were presented in an overly positive way; because the study raises questions about research methodology and the interpretation of data in pragmatic trials attempting to measure the effects of complex interventions, we will be commissioning a Debate and Analysis article on the topic. In the meantime we would encourage you to contribute to this debate throught the usual Journal channels Roger Jones Professor Roger Jones MA DM FRCP FRCGP FMedSci FHEA FRSA |
It is one thing to make a mistake, It is quite another thing to refuse to admit it. This reply seems to me to be quite disgraceful.
20 July 2011. The proper version of the story got wider publicity when Margaret McCartney wrote about it in the BMJ. The first rapid response to this article was a lengthy denial by the authors of the obvious conclusion to be drawn from the paper. They merely dig themselves deeper into a hole. The second response was much shorter (and more accurate).
|
Thank you Dr McCartney Richard Watson, General Practitioner The fact that none of the authors of the paper or the editor of BJGP have bothered to try and defend themselves speaks volumes. Like many people I glanced at the report before throwing it away with an incredulous guffaw. You bothered to look into it and refute it – in a real journal. That last comment shows part of the problem with them publishing, and promoting, such drivel. It makes you wonder whether anything they publish is any good, and that should be a worry for all GPs. |
30 July 2011. The British Journal of General Practice has published nine letters that object to this study. Some of them concentrate on problems with the methods. others point out what I believe to be the main point, there us essentially no effect there to be explained. In the public interest, I am posting the responses here [download pdf file]
Thers is also a response from the editor and from the authors. Both are unapologetic. It seems that the editor sees nothing wrong with the peer review process.
I don’t recall ever having come across such incompetence in a journal’s editorial process.
Here’s all he has to say.
|
The BJGP Editorial Board considered this correspondence recently. The Board endorsed the Journal’s peer review process and did not consider that there was a case for retraction of the paper or for releasing the peer reviews. The Board did, however, think that the results of the study were highlighted by the Journal in an overly-positive manner. However,many of the criticisms published above are addressed by the authors themselves in the full paper.
|
If you subscribe to the views of Paterson et al, you may want to buy a T-shirt that has a revised version of the periodic table.
5 August 2011. A meeting with the editor of BJGP
Yesterday I met a member of the editorial board of BJGP. We agreed that the data are fine and should not be retracted. It’s the conclusions that should be retracted. I was also told that the referees’ reports were "bland". In the circumstances that merely confirmed my feeling that the referees failed to do a good job.
Today I met the editor, Roger Jones, himself. He was clearly upset by my comment and I have now changed it to refer to the whole editorial process rather than to him personally. I was told, much to my surprise, that the referees were not acupuncturists but “statisticians”. That I find baffling. It soon became clear that my differences with Professor Jones turned on interpretations of statistics.
It’s true that there were a few comparisons that got below P = 0.05, but the smallest was P = 0.02. The warning signs are there in the Methods section: "all statistical tests were …. deemed to be statistically significant if P < 0.05". This is simply silly -perhaps they should have read Lectures on Biostatistics. Or for a more recent exposition, the XKCD cartoon in which it’s proved that green jelly beans are linked to acne (P = 0.05). They make lots of comparisons but make no allowance for this in the statistics. Figure 2 alone contains 15 different comparisons: it’s not surprising that a few come out "significant", even if you don’t take into account the likelihood of systematic (non-random) errors when comparing final values with baseline values.
Keen though I am on statistics, this is a case where I prefer the eyeball test. It’s so obvious from the Figure that there’s nothing worth talking about happening, it’s a waste of time and money to torture the numbers to get "significant" differences. You have to be a slavish believer in P values to treat a result like that as anything but mildly suggestive. A glance at the Figure shows the effects, if there are any at all, are trivial.
I still maintain that the results don’t come within a million miles of justifying the authors’ stated conclusion “The addition of 12 sessions of five-element acupuncture to usual care resulted in improved health status and wellbeing that was sustained for 12 months.” Therefore I still believe that a proper course would have been to issue a new and more accurate press release. A brief admission that the interpretation was “overly-positive”, in a journal that the public can’t see, simply isn’t enough.
I can’t understand either, why the editorial board did not insist on this being done. If they had done so, it would have been temporarily embarrassing, certainly, but people make mistakes, and it would have blown over. By not making a proper correction to the public, the episode has become a cause célèbre and the reputation oif the journal will suffer permanent harm. This paper is going to be cited for a long time, and not for the reasons the journal would wish.
Misinformation, like that sent to the press, has serious real-life consequences. You can be sure that the paper as it still stands, will be cited by every acupuncturist who’s trying to persuade the Department of Health that he’s a "qualified provider".
There was not much unanimity in the discussion up to this point, Things got better when we talked about what a GP should do when there are no effective options. Roger Jones seemed to think it was acceptable to refer them to an alternative practitioner if that patient wanted it. I maintained that it’s unethical to explain to a patient how medicine works in terms of pre-scientific myths.
I’d have love to have heard the "informed consent" during which "The patient’s condition is explained in terms of imbalance in the five elements which then causes an imbalance in the whole person". If anyone had tried to explain my conditions in terms of my imbalance in my Wood, Water, Fire, Earth and Metal. I’d think they were nuts. The last author. Gerad Kite, runs a private clinic that sells acupuncture for all manner of conditions. You can find his view of science on his web site. It’s condescending and insulting to talk to patients in these terms. It’s the ultimate sort of paternalism. And paternalism is something that’s supposed to be vanishing in medicine. I maintained that this was ethically unacceptable, and that led to a more amicable discussion about the possibility of more honest placebos.
It was good of the editor to meet me in the circumstances. I don’t cast doubt on the honesty of his opinions. I simply disagree with them, both at the statistical level and the ethical level.
30 March 2014
I only just noticed that one of the authors of the paper, Bruce McCallum (who worked as an acupuncturist at Kite’s clinic) appeared in a 2007 Channel 4 News piece. I was a report on the pressure to save money by stopping NHS funding for “unproven and disproved treatments”. McCallum said that scientific evidence was needed to show that acupuncture really worked. Clearly he failed, but to admit that would have affected his income.
Watch the video (McCallum appears near the end).
|
The Science Museum is a wonderful place. As a child it seemed magical. So all the more disappointing to find that it houses an exhibition that promotes quackery. The exhibition is uncritical and sometimes downright dangerous. It does not teach you anything about science, it teaches anti-science and uncritical thinking. It was not originally like this. Most of the objects in the exhibition were originally part of Henry Wellcome’s Wellcome Museum of Medical History, based at 183 Euston Road. It was moved on permanent loan to the Science Museum in 1977 where it was known as The Wellcome Museum of the History of Medicine. |
|
Recently the Wellcome-Trust sponsored exhibition was the subject of a blog post at Purely a figment of your imagination, written by Alex Davenport. That reminded me that last June I was sent a lot of pictures of the exhibition but never got round to finishing writing them up. Here, somewhat tardily, is some of what I got.
It seems that the Wellcome Trust is not to blame, The free advertising for quacks was something added to the Wellcome collection by the Science Museum itself.
At the time, I wrote to the Science Museum to find out what was going on. The response was very disappointing, merely bland PR stuff. I was told that the person responsible for the display was Lisa O’Sullivan, Senior Curator of Medicine, but she was on sabbatical, so no response from her.
The clue to what went wrong came in a letter from Dr. Tim Boon, the Science Museum’s Chief Curator. The letter was relayed via the Museum’s Press Officer. A subsequent letter to Boon himself was not answered.
"Therefore, in addition to the overwhelming majority of the Upper Wellcome gallery that tells the story of the history of Western medicine since the rise of Civilisation up to the modern era, we devote a small section to these more anthropological concerns in our display called ‘Living Medical Traditions’.
Our message in this display is that these traditions are not ‘alternative’ systems in some parts of the world. Instead they are often the only choice of medical care to those communities. We do not make any claims for the validity of these traditions. For example, we include the use of acupuncture but do not say that acupuncture ‘works’. "
Unfortunately this is really not true: the tone is very much that it does work. The reason is clear in the next paragraph.
"As with all Science Museum galleries independent experts were consulted when developing this gallery. In this instance advice was sought from leading academics in the history of non-western medical traditions as well as practitioners and users of these traditions. We maintained editorial control throughout.”
Aha they asked "experts", but of course it is always possible to find some ‘expert’ to advocate any view, however barmy. The only experts that were consulted, we are told, is historians and practitioners of anti-scientific medicine. No scientists. Clearly the Museum allowed the quacks to write their own script, with no supervision from anyone who understands the science, It is meant to be a Science Museum, not a museum of anthropology.
The nonsense of quack medicine provides an excellent opportunity to explain simply how science tries to separate truth from falsehood. The Museum has not only missed that opportunity but it has actively promoted anti-science.
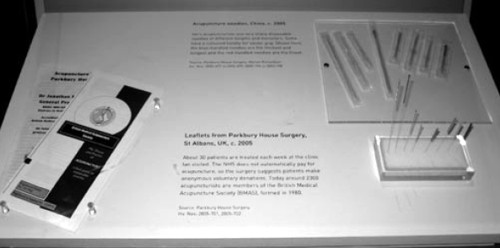
The Museum declined to name these mystery experts, but one of them is revealed in the 2006 newsletter of the British Medical Acupuncture Society [download the newsletter]. An article by Jonathan Freedman shows the delight of acupuncturists.
"The BMAS were approached by the Museum last Summer and asked if any members would be able to contribute a case study about acupuncture to feature in the ‘personal stories’ section of the exhibition."
"I think the final product has worked extremely well and shows Western Medical Acupuncture in a positive light. A selection of needles is displayed along with the BMAS leaflet and my own practice acupuncture leaflet."
In fact the Science Museum’s good name is used by Freedman to advertise his private practice.
Here is the free advertising in the Science Museum.
Traditional Chinese Medicine
There is plenty of this and it is totally uncritical. All it does is repeat the gobbledygook used by practitioners. In fact it was largely written by them.
There are recorded commercials too. Listen to this one.
Advertising for cupping at the Asanté Clinic.
In the recording, Dr Ke diagnoses an asthma patient as having mucus in the lungs -by looking at his tongue (no kidding) -and recommends cupping. He says
“We need to clear this mucus, or the phlegm, in the chest by using cupping, It’s improving, sort of, the flow of the water, and flow out, in other words, suck out the badness from the body”
This, needless to say, is total rubbish.
The recording took place at the Asanté Clinic, on the Archway campus of the University of Middlesex. Ah yes, Middlesex. Take a look at ‘More quackedemia. Dangerous Chinese medicine taught at Middlesex University‘.
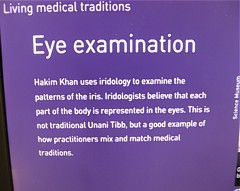
Unani medicine, Another advertisement for a private clinic.
|
|
|
Listen to a diagnosis being made by looking at the iris.
Iridology is, of course, total bunk Just one of the many phoney methods of diagnosis used by alternative practitioners, as an aid to selling you an expensive treatment.
Ayervedic medicine
Listen to another advertisement, for private Ayurveda clinic
The display that accompanies the recording is totally uninformative. The practitioners have been allowed to advertise their wares with no trace of critical thought. No trace of science.
|
|
|
|
|
|
|
|
|
The power of blogs
I guess this incident is yet another example of the power of blogs. My own letters to the science museum produced precisely nothing, as is usually the case if you go through the “proper channels”. Alex Davenport’s blog,on the other hand, stung the Science Museum into a public response. It’s true that the response is much the same as the patronising PR junk that was sent to me last year, though it was labelled as being by Susannah Shute, Web Content Coordinator. The response even linked to a picture of the homeopathy exhibit.
It seems a bit more pressure is needed to persuade the museum to change this particular exhibition into science, rather than its present anti-science.
Follow-up
13 April 2011. Simon Singh arranged a meeting with the new director of the Science Museum, Ian Blatchford, and deputy director Heather Mayfield Our deputation consisted of Simon Singh, Alex Davenport, Marianne Baker and me. It was Alex’s blog on the science museum exhibit, and my post on the museum which followed it shortly, that caused the meeting. Alex had a follow-up blog too. I hadn’t realised that Simon had resigned as a trustee of the museum five years ago, in protest about the (dreadful) alternative medicine exhibit. I had various stonewalling responses to my attempts to pursue the matter out of the limelight, so eventually went public. After the blogs appeared, the Science Museum published a response which was, sadly, entirely vacuous. We had an excellent discussion, during which Ian Blatchford said he regretted the official response and changes to the exhibit are promised. there is an account of the meeting here.
We were sent a revised version, which was improved, but not, we said improved enough.
10 May 2011. Got an email from the person who originally brought the problem to my attention.
“Visited Science museum yesterday , wonderful news – all offensive material gone, and different ok stuff there”.
Well done, Science Museum.
There is something very offensive about the idea that a ‘bachelor of science’ degree can be awarded by a university, as a prize for memorising gobbledygook.
Once the contents of the ‘degrees’ has been exposed to public ridicule, many universities have stopped doing it. All (or nearly all) of these pseudo-degrees have closed at the University of Salford, the University of Central Lancashire, Robert Gordon University, the University of Buckingham, and even at the University of Westminster (the worst offender), one course has closed (with rumours of more to follow).
|
I’ve already written about the course in Traditional Chinese Medicine at the University of Salford (Chinese medicine -acupuncture gobbledygook revealed) and at the University of Westminster: see Why degrees in Chinese medicine are a danger to patients. The former has closed, but not the latter. Here is another one. One place that has yet to come under close scrutiny is Middlesex University. |

Michael Driscoll, VC of Middlesex University. The buck stops with him. |
Their “Complementary Health” courses are as follows (April 2010).
- Complementary Health Sciences (Ayurveda) Degree, BSc Honours
- Herbal Medicine Degree, BSc Honours
- Traditional Chinese Acupuncture Degree, BSc Honours
- Traditional Chinese Medicine Degree, BSc Honours
and also two postgraduate courses
I asked Middlesex University for samples of their teaching materials under the Freedom of Information Act, and, as usual, the request was refused. As usual, I then asked for the mandatory internal review of the decision, and this time, most unusually, the internal review did not confirm the initial refusal and I was sent a bundle of teaching materials about Chinese Herbal Medicine, It was not all I asked for, but it is quite enough to show the absurd ideas that are still being taught as part of bachelor of Science degree in a UK University.
Not only are the ideas absurd, pre-scientific, indeed antiscientific. They are also dangerous. People who have been taught this nonsense are going out and being let loose on sick people.
The vice-chancellor of Middlesex University, Professor Michael Driscoll, is an economist, not a biologist. Surely you don’t need to be a scientist to feel a bit suspicious when you read on the Middlesex web site about
Traditional Chinese Acupuncture and Moxibustion including distribution of meridians-collaterals and location of acupoints; needling and moxibustion techniques;
Have any of the members of the Executive ever thought to ask about what goes on in these courses? Even if it is beyond an economist to see through the nonsense, surely it should be possible for Professor Margaret House, Deputy Vice-Chancellor Academic, whose interests lie in water quality, should be able to, though as Dean of the School of Health and Social Sciences she appears to sponsor the nonsense. And Professor Waqar Ahmad, Deputy Vice-Chancellor Research and Enterprise, who has written a s book on Ethnicity, Health and Health Care, should surely be able to distinguish sense from nonsense in health care? In that respect, I’d have less confidence in Katie Bell, Chief Marketing Officer, who joined Middlesex University in 2009 following a career in brand marketing for Nestlé UK and GlaxoSmithKline Consumer Healthcare. Marketing people seldom have much regard for truth.
Have any of the University’s Governors ever asked what is going on in their name? It’s true that none of the long list of distinguished-sounding governors is a scientist. Surely you don’t need to be to question whether or not what follows can be described as ‘science’.
My guess is that none of these distinguished people has ever bothered to look at the dangerous nonsense that is being taught in their University. It is not in the nature of ‘managers’ to look far beyond ticked-boxes and profit, They should have done of course, but to make it easier for them, here is a small selection of the slides that I was sent (the copyright for them lies with the university: these few slides come under the heading ‘ ‘fair quotation’ and it is undoubtedly in the public interest to show them).
Course CMH 1211
e 
Uhuh, my spleen qi is well and truly knotted already though when I learned physiology it was not thought that the spleen had much to do with emotions.
Ah so at least the problem of heavy breathers is solved. But high temperature, abdominal pain and abnormal pulse can be signs of serious illness. If your only explanation for them is “preponderant evil Qi”, you are a menace to public health.
All these symptoms could be the result of a serious disease. It is not only antiquated nonsense to talk about them in terms of Yin, Yang and Qi. It endangers people,
Course CMH 2212
Chinese materia medica. Some of the herbs are likely to contain active ingredients (indeed some are very dangerous). It would be quite possible to study the ingredients of these herbs and to investigate how they work in the light of what has been learned about physiology and pharmacology in the last 200 years. Pharmacology has a long history of doing that, But is seems to play no part in this course. Herbs are “cold” or “hot” and may “check the exuberance of yang”.
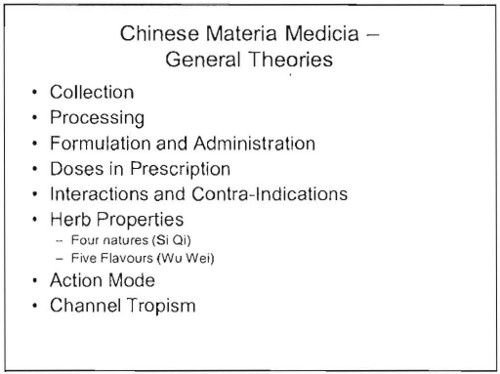
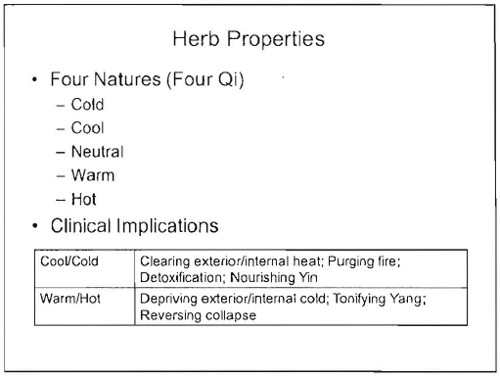
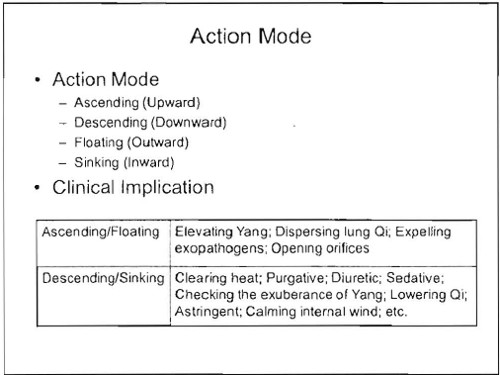
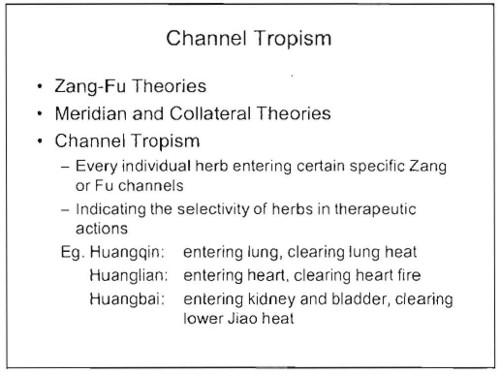
and so on, just preposterous, made-up nonsense from another era.
If it were taught as cultural history, it might be interesting. But it is being taught as though it were true, and an appropriate way to treat sick people.
Course CMH 3214
Would you trust your child to someone who’d been taught that “causes of paediatric diseases are relatively simple”, and “children are pure yang”?
Now some Chinese recipes
Course CMH 3100
![]()
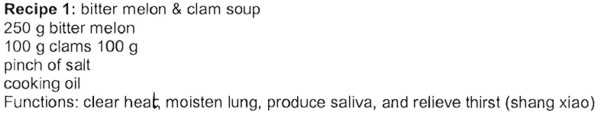
This may or may not taste good, but to recommend it for diabetes is seriously irresponsible.
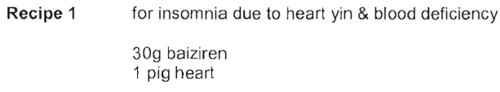
The programme specification for the “BSc (Hons) Traditonal Chinese medicine” can be found here. [local copy download]
It is written with all the official trappings, just as though the degree was about science. It isn’t. It is a danger to public health.
I have asked the vice-chancellor, Michael Driscoll, to express his view of these comments
Follow-up
A rather unexpected comment from a London acupuncturist.
“At least,I knew that Professor David Colquhoun is very skeptical about Chinese medicine. he comment Chinese medicine study”not only are the ideas absurd, pre-scientific, indeed antiscientific. They are also dangerous. People who have been taught this nonsense are going out and being let loose on sick people.” “
“But,I still like to read his blog as His article very is respectable. I think. Look this…”
The skeptic blog featured this post in its weekly roundup.
27 May 2010. Times Higher Education reported the decision of Middlesex University to close its philosophy department. This department seems to have a remarkable reputation, not least for a post-1992 university. Three academics and four students have been suspended and gagged in classical bullying style.
This has happened while they continue to teach dangerous rubbish like that described above.
I left a comment at Times Higher, as follows.
It is a reflection on the quality of university management that Middlesex has chosen to shut its philosophy department while continuing to run degrees in quackery. These courses not only offer an Hons BSc for memorising chunks of anti-scientific nonsense. They also pose a real danger to patients. See https://www.dcscience.net/?p=2923
I can think of no better illustration than this of the crass nature of the judgements made by Middlesex’s management. They are either ignorant of what constitutes science, or they are corrupt. I see no other possibilities. In either case they should not be running a university.
I think Prof Michael Driscoll owes the world an explanation.
Every single request for information about course materials in quack medicine that I have ever sent has been turned down by universities,
It is hardly as important as as refusal of FoI requests to see climate change documents, but it does indicate that some vice-chancellors are not very interested in openness. This secretiveness is exactly the sort of thing that leads to lack of trust in universities and in science as a whole.
The one case that I have won took over three years and an Information Tribunal decision against the University of Central Lancashire (UCLAN) before I got anything.
UCLAN spent £80,307.95.(inc VAT at 17.5%) in legal expenses alone (plus heaven knows how much in staff time) to prevent us from seeing what was taught on their now defunct “BSc (Hons) homeopathy”. This does not seem to me to be good use of taxpayers’ money. A small sample of what was taught has already been posted (more to come). It is very obvious why the university wanted to keep it secret, and equally obvious that it is in the public interest that it should be seen.
UCLAN had dropped not only its homeopathy "degree" before the information was revealed, They also set up an internal inquiry into all the rest of their courses in magic medicine which ended with the dumping of all of them.
Well, not quite all, There was one left. An “MSc” in homeopathy by e-learning. Why this was allowed to continue after the findings of UCLAN’s internal review, heaven only knows. It is run by the same Kate Chatfield who ran the now defunct BSc. Having started to defend the reputation against the harm done to it by offering this sort of rubbish, I thought I should finish. So I asked for the contents of this course too. It is, after all, much the same title as the course that UCLAN had just been ordered to release. But no, this request too was met with a refusal
Worse still, the refusal was claimed under section 43(2) if the Freedom of Information Act 2000. That is the public interest defence, The very defence that was dismissed in scathing terms by the Information Tribunal less than two months ago,
To add insult to injury, UCLAN said that it would make available the contents of the 86 modules in the course under its publication scheme, at a cost of £20 per module, That comes to £1,720 for the course, Some freedom of information.
Because this was a new request, it now has to go through the process of an internal reviw of the decision before it can ne referred to the Information Commissioner. That will be requested, and since internal reviews have, so far, never changed the initial judgment. the appeal to the Information Commissioner should be submitted within the month. I have been promised that the Information Commissioner will deal with it much faster this time than the two years it took last time.
And a bit more unfreedom
Middlesex University
I first asked Middlesex for materials from their homeopathy course on 1 Oct 2008. These courses are validated by Middlesex university (MU) but actually run by the Centre for Homeopathic Education. Thw MU site barely mentions homeopathy and all I got was the usual excuse that the uninsersity did not possess the teaching materials. As usual, the validation had been done without without looking at what was actually being taught. The did send me the validation document though [download it] As usual, the validation document shows no sign at all of the fact that the usbject of the "BSc" is utter nonsense. One wonderful passage says
“. . . the Panel were assured that the Team are clearly producing practitioners but wanted to explore what makes these students graduates? The Team stated that the training reflects the professional standards that govern the programme and the graduateness is achieved through developing knowledge by being able to access sources and critically analyse these sources . . . “
Given that the most prominent characteristic of homeopaths (and other advocates of magic medicine) is total lack of critical ability, this is hilarious. If they had critical ability they wouldn’t be homeopaths. Hilarious is not quite the right word, It is tragic that nonsense like this can be found in an official university document.
Middlesex, though it doesn’t advertise homeopathy, does advertise degrees in Traditional Chinese Medicine, Herbal Medicine and Ayurveda. On 2nd February 2010 I asked for teaching materials from these courses. Guess what? The request was refused. In this case the exemptions under FOIA were not even invoked but I was told that "All these materials are presently available only in one format at the University – via a student-only accessed virtual learning environment. ". Seems that they can’t print out the bits that I asked for, The internal review has been requested, then we shall see what the Information Commissioner has to say.
Two other cases are at present being considered by the Information Commissioner (Scotland), after requests under the Scottish FoIA were refused. They are interesting cases because they bear on the decision, currently being considered by the government, about whether they should implement the recommendations of the execrable Pittilo report.
Napier University Edinburgh. The first was for teaching material form the herbal medicine course at Napier University Edinburgh. I notice that this course no longer appears in UCAS or on Napier’s own web site, so maybe the idea that its contents might be disclosed has been sufficient to make the university do the sensible thing.
Robert Gordon University Aberdeen The second request was for teaching material from the “Introduction to Homeopathy” course at the Robert Gordon University Aberdeen. The particular interest that attaches to this is that the vice-chancellor of Robert Gordon university is Michael Pittilo. The fact that he is willing to tolerate such a course in his own university seems to me to disqualify him from expressing any view on medical subjects.
Michael Pittilo, Crohn’s disease and Andrew Wakefield
Michael Pittilo has not been active in science for some time now, but Medline does show scientiifc publications for Pittilo RM, between 1979 anf 1998. Between 1989 and 1995 there are five papers published jointly with one Andrew Wakefield. These papers alleged a relationship between measles virus and Crohn’s disease. The papers were published before tha infamous 1998 paper by Wakefield in the Lancet (now retracted) that brought disgrace on Wakefield and probably caused unnecessary deaths.. The link between measles and Crohn’s disease is now equally disproved.
The subject has been reviewed by Korzenik (2005) in Past and Current Theories of Etiology of IBD. Toothpaste, Worms, and Refrigerators
“Wakefield et al proposed that Crohn’s results from a chronic infection of submucosal endothelium of the intestines with the measles virus [Crohn’s disease: pathogenesis and persistent measles virus infection. Wakefield AJ, Ekbom A, Dhillon AP, Pittilo RM, Pounder RE., Gastroenterology, 1995, 108(3):911-6]”
"This led to considerable media interest and< public concern over use of live measles vaccine as well as other vaccines. A number of researchers countered these claims, with other studies finding that titers to measles were not increased in Crohn’s patients, granulomas were not associated with endothelium 49 , measles were not in granulomas50 and the measles vaccine is not associated with an increased risk of Crohn’s disease51–55 "
This bit of history is not strictly relevant to the Pittilo report, but I do find quite puzzling how the government chooses people from whom it wishes to get advice about medical problems.
Follow-up
I notice that the Robert Gordon university bulletin has announced that
“Professor Mike Pittilo, Principal of the University, has been made an MBE in the New Year Honours list for services to healthcare”.
That is a reward for writing a very bad report that has not yet been implemented, and one hopes, for the sake of patients, will never be implemented. I do sometimes wonder about the bizarre honours system in the UK.
Postcript.
On 16th February, the death of Michael Pittilo was announced. He had been suffeing from cancer and was only 55 years old. I wouldn’t wish that fate on my worst enemy.
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
More boring politics, but it matters. The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register should normally be through a Bachelor degree with Honours
For the background on this appalling report, see earlier posts.
A very bad report: gamma minus for the vice-chancellor
The Times (blame subeditor for the horrid title), and some follow up on the Times piece
The Health Professions Council breaks its own rules: the result is nonsense
Chinese medicine -acupuncture gobbledygook revealed
Consultation opens on the Pittilo report: help stop the Department of Health making a fool of itself
Why degrees in Chinese medicine are a danger to patients
The Department of Health consultation shuts on November 2nd. If you haven’t responded yet, please do. It would be an enormous setback for reason and common sense if the government were to give a stamp of official approval to people who are often no more than snake-oil salesman.
Today I emailed my submission to the Pittilo consultation to the Department of Health, at HRDListening@dh.gsi.gov.uk
The submission
I sent the following documents, updated versions of those already posted earlier.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
- An example of dangerous (and probably illegal) claims that are routinely made by TCM practitioners [download pdf]f
I also completed their questionnaire, despite its deficiencies. In case it is any help to anyone, this is what I said:
The questionnaire
Q1: What evidence is there of harm to the public currently as a result of the activities of acupuncturists, herbalists and traditional Chinese medicine practitioners? What is its likelihood and severity?
Harm
No Harm
Unsure
Comment
The major source of harm is the cruel deception involved in making false claims of benefit to desperate patients. This applies to all three.
In the case of herbal and TCM there is danger from toxicity because herbal preparations are unstandardised so those that do contain an active ingredient are given in an unknown dose. This is irresponsible and dangerous (but would not be changed by the proposals for regulation).
In addition TCM suffers from recurrent problems of contamination with heavy metals, prescription drugs and so on. Again this would not be the business of the proposed form of regulation.
Q2: Would this harm be lessened by statutory regulation? If so, how?
Yes
No
Unsure
The proposed form of regulation would be no help at all. The HPC has already said that it is not concerned with whether or not the drug works, and, by implication, does not see itself as preventing false health claims (just as the GCC doesn’t do this). False claims are the responsibility of Trading Standards who are meant to enforce the Consumer Protection Unfair Trading Regulations (May 2008), though they do not at present enforce them very effectively. Also Advertisng Standards. The proposed regulation would not help, and could easily hinder public safety as shown by the fact that the GCC has itself been referred to the Advertisng Standards Authority.
The questions of toxicity and contamination are already the responsibility of Trading Standards and the MHRA. Regulation by the HPC would not help at all. The HPC is not competent to deal with such questions.
Q3: What do you envisage would be the benefit to the public, to practitioners and to businesses, associated with introducing statutory regulation?
Significant benefit
Some benefit
No benefit
Unsure
This question is badly formulated because the answer is different according to whether you are referring to the public, to practitioners or to businesses.
The public would be endangered by the form of regulation that is proposed, as is shown very clearly by the documents that I have submitted separately.
In the case of practitioners and businesses, there might be a small benefit, if the statutory regulation gave the impression that HM and TCM had government endorsement and must therefore be safe and effective.
There is also one way that the regulation could harm practitioners and businesses. If the HPC received a very large number of complaints about false health claims, just as the GCC has done recently, not only would it cost a large amount of money to process the claims, but the attendant bad publicity could harm practitioners. It is quite likely that this would occur since false claims to benefit sick people are rife in the areas of acupuncture, HM and TCM.
Q4: What do you envisage would be the regulatory burden and financial costs to the public, to practitioners, and to businesses, associated with introducing statutory regulation? Are these costs justified by the benefits and are they proportionate to the risks? If so, in what way?
Justified
Not Justified
Unsure
Certainly not justified. Given that I believe that the proposed form of regulation would endanger patients, no cost at all would be justified. But even if there were a marginal benefit, the cost would be quite unjustified. The number of practitioners involved is very large. It would involve a huge expansion of an existing quango, at a time when the government is trying to reduce the number of quangos. Furthermore, if the HPC were flooded with complaints about false health claims, as the GCC has been, the costs in legal fees could be enormous.
Q5: If herbal and TCM practitioners are subject to statutory regulation, should the right to prepare and commission unlicensed herbal medicines be restricted to statutorily regulated practitioners?
Yes
No
Unsure
I don’t think it would make much difference. The same (often false) ideas are shared by all HM people and that would continue to be the same with or without SR.
Q6: If herbal and TCM practitioners are not statutorily regulated, how (if at all) should unlicensed herbal medicines prepared or commissioned by these practitioners be regulated?
They could carry on as now, but the money that would have been spent on SR should instead be used to give the Office of Trading Standards and the MHRA the ability to exert closer scrutiny and to enforce more effectively laws that already exist. Present laws, if enforced, are quite enough to protect the public.
Q7: What would be the effect on public, practitioners and businesses if, in order to comply with the requirements of European medicines legislation, practitioners were unable to supply manufactured unlicensed herbal medicines commissioned from a third party?
Significant effect
Some effect
No effect
Unsure
European laws,especialliy in food area, are getting quite strict about the matters of efficacy. The proposed regulation, which ignores efficacy, could well be incompatible with European law, if not now, then soon. This would do no harm to legitimate business though it might affect adversely businesses which make false claims (and there are rather a lot of the latter).
Q8: How might the risk of harm to the public be reduced other than by orthodox statutory regulation? For example by voluntary self-regulation underpinned by consumer protection legislation and by greater public awareness, by accreditation of voluntary registration bodies, or by a statutory or voluntary licensing regime?
Voluntary self-regulation
Accreditation of voluntary bodies
Statutory or voluntary licensing
Unsure
I disagree with the premise, for reasons given in detail in separate documents. I believe that ‘orthodox statutory regulation’, if that means the Pittilo proposals, would increase, not decrease, the risk to the public. Strengthening the powers of Trading Standards, the MHRA and such consumer protection legislation would be far more effective in reducing risk to the public than the HPC could ever be. Greater public awareness of the weakness of the evidence for the efficacy of these treatments would obviously help too, but can’t do the job on its own.
Q10: What would you envisage would be the benefits to the public, to practitioners, and to businesses, for the alternatives to statutory regulation outlined at Question 8?
It depends on which alternative you are referring to. The major benefit of enforcement of existing laws by Trading Standards and/or the MHRA would be (a) to protect the public from risk, (b) to protect the public from health fraud and (c) almost certainly lower cost to the tax payer.
Q11: If you feel that not all three practitioner groups justify statutory regulation, which group(s) does/do not and please give your reasons why/why not?
Acupuncture
Herbal Medicine
TCM
Unsure
None of them. The differences are marginal. In the case of acupuncture there has been far more good research than for HM or TCM. But the result of that research is to show that in most cases the effects are likely to be no more than those expected of a rather theatrical placebo. Furthermore the extent to which acupuncture has a bigger effect than no-acupuncture in a NON-BLIND comparison, is usually too small and transient to offer any clinical advantage (so it doesn’t really matter whether the effect is placebo or not, it is too small to be useful).
In the case of HM, and even more of TCM, there is simply not enough research to give much idea of their usefulness, with a small handful of exceptions.
This leads to a conclusion that DH seems to have ignored in the past. It makes absolutely no sense to talk about “properly trained practitioners” without first deciding whether the treatments work or not. There can be no such thing as “proper training” in a discipline that offers no benefit over placebo. It is a major fault of the Pittilo recommendations that they (a) ignore this basic principle and (b) are very over-optimistic about the state of the evidence.
Q12: Would it be helpful to the public for these practitioners to be regulated in a way which differentiates them from the regulatory regime for mainstream professions publicly perceived as having an evidence base of clinical effectiveness? If so, why? If not, why not?
Yes
No
Unsure
It might indeed be useful if regulation pointed out the very thin evidence base for HM and TCM but it would look rather silly. The public would say how can it be that the DH is granting statutory regulation to things that don’t work?
Q13: Given the Government’s commitment to reducing the overall burden of unnecessary statutory regulation, can you suggest which areas of healthcare practice present sufficiently low risk so that they could be regulated in a different, less burdensome way or de-regulated, if a decision is made to statutorily regulate acupuncturists, herbalists and traditional Chinese medicine practitioners?
Yes
No
Unsure
As stated above, the.only form of regulation that is needed, and the only form that would protect the public, is through consumer protection regulations, most of which already exist (though they are enforced in a very inconsistent way). Most statutory regulation is objectionable, not on libertarian grounds, but because it doesn’t achieve the desired ends (and is expensive). In this case of folk medicine, like HM and TCM, the effect would be exactly the opposite of that desired as shown in separate documents that I have submitted to the consultation.
Q14: If there were to be statutory regulation, should the Health Professions Council (HPC) regulate all three professions? If not, which one(s) should the HPC not regulate?
Yes
No
Unsure
The HPC should regulate none of them. It has never before regulated any form of alternative medicine and it is ill-equipped to do so. Its statement that it doesn’t matter that there is very little evidence that the treatments work poses a danger to patients (as well as being contrary to its own rules).
Q15: If there were to be statutory regulation, should the Health Professions Council or the General Pharmaceutical Council/Pharmaceutical Society of Northern Ireland regulate herbal medicine and traditional Chinese medicine practitioners?
HPC
GPC/PSNI
Unsure
Neither. The GPC is unlikely to care about whether the treatments work any more than the RPSGB did, or the GCC does now. The problems would be exactly the same whichever body did it.
Q16: If neither, who should and why?
As I have said repeatedly, it should be left to Trading Standards, the MHRA and other consumer protection regulation.
Q17:
a) Should acupuncture be subject to a different form of regulation from that for herbalism and traditional Chinese medicine? If so, what?
Yes
No
Unsure
b) Can acupuncture be adequately regulated through local means, for example through Health and Safety legislation, Trading Standards legislation and Local Authority licensing?
Yes
No
Unsure
(a) No -all should be treated the same. Acupuncture is part of TCM
(b) Yes
Q18.
a) Should the titles acupuncturist, herbalist and [traditional] Chinese medicine practitioner be protected?
b) If your answer is no which ones do you consider should not be legally protected?
Yes
No
Unsure
No. It makes no sense to protect titles until such time as it has been shown that the practitioners can make a useful contribution to medicine (above placebo effect). That does not deny that placebos may be useful at times. but if that is all they are doing, the title should be ‘placebo practitioners’.
Q19: Should a new model of regulation be tested where it is the functions of acupuncture, herbal medicine and TCM that are protected, rather than the titles of acupuncturist, herbalist or Chinese medicine practitioner?
Yes
No
Unsure
No. This makes absolutely no sense when there is so little knowledge about what is meant by the ” functions of acupuncture, herbal medicine and TCM”.Insofar as they don’t work (better than placebo), there IS no function. Any attempt to define function when there is so little solid evidence (at least for HM and TCM) is doomed to failure.
Q20: If statutory professional self-regulation is progressed, with a model of protection of title, do you agree with the proposals for “grandparenting” set out in the Pittilo report?
Yes
No
Unsure
No. I believe the Pittilo report should be ignored entirely. The whole process needs to be thought out again in a more rational way.
Q22: Could practitioners demonstrate compliance with regulatory requirements and communicate effectively with regulators, the public and other healthcare professionals if they do not achieve the standard of English language competence normally required for UK registration? What additional costs would occur for both practitioners and regulatory authorities in this case?
Yes
No
Unsure
No. It is a serious problem, in TCM especially, that many High Street practitioners speak hardly any English at all. That adds severely to the already considerable risks. There would be no reliable way to convey what was expected of them. it would be absurd for the taxpayer to pay for them to learn English for the purposes of practising TCM (of course there might be the same case as for any other immigrant for teaching English on social grounds).
Q23: What would the impact be on the public, practitioners and businesses (financial and regulatory burden) if practitioners unable to achieve an English language IELTS score of 6.5 or above are unable to register in the UK?
Significant impact
Some impact
No impact
Unsure
The question is not relevant. The aim of regulation is to protect the public from risk (and it should be, but isn’t, an aim to protect them from health fraud). It is not the job of regulation to promote businesses
Q24: Are there any other matters you wish to draw to our attention?
I have submitted three documents via HRDListening@dh.gsi.gov.uk. The first of these puts the case against the form of regulation proposed by Pittilo, far more fluently than is possible in a questionnaire.
Another shows examples of what is actually taught in degrees in acupuncture, HM and TCM. They show very graphically the extent to which the Pittilo proposals would endanger the public, if they were to be implemented..
In March 2007 I wrote a piece in Nature on Science degrees without the science. At that time there were five “BSc” degrees in homeopathy. A couple of weeks ago I checked the UCAS site for start in 2009, and found there was only one full “BSc (hons)” left and that was at Westminster University.
Today I checked again and NOW THERE ARE NONE.
A phone call to the University of Westminster tonight confirmed that they have suspended entry to their BSc (Hons) homeopathy degree.
They say that they have done so because of “poor recruitment”. It was a purely financial decision. Nothing to do with embarrasment. Gratifying though it is that recruits for the course are vanishing, that statement is actually pretty appalling It says that the University of Westminster doesn’t care whether it’s nonsense, but only about whether it makes money.
Nevertheless the first part of this post is not entirely outdated before it even appeared, because homeopathy will still be taught as part of Complementary Therapies. And Naturopathy and “Nutritional Therapy” are still there..
According to their ‘School of Integrated Health‘, “The University of Westminster has a vision of health care for the 21st Century”. Yes, but it is what most people would call a vision of health care in the 18th century.
The revelation that the University of Westminster teaches that Amethysts emit high Yin energy caused something of a scandal.
Since then I have acquired from several sources quite a lot more of their teaching material, despite the fact that the university has refused to comply with the Freedom of Information Act.
In view of the rather silly internal review conducted by Westminster’s Vice-Chancellor, Professor Geoffrey Petts, this seems like a good moment to make a bit more of it public,
I think that revelation of the material is justified because it is in the
public interest to know how the University if Westminster is spending taxpayers’ money. Another motive is to defend the reputation of the post-1992 universities. I have every sympathy with the ex-polytechnics in their efforts to convert themselves into universities. In many ways they have succeeded. That effort
is impeded by teaching mystical versions of medicine.
If the University of Westminster is being brought into disrepute, blame its vice-chancellor, not me.
Homeopathic spiders
Here are a few slides from a lecture on how good spider venom is for you. It is from Course 3CTH502 Homeopathic Materia Medica II. No need to worry though, because they are talking about homeopathic spider venom, so there is nothing but sugar in the pills. The involvement of spiders is pure imagination. No more than mystical gobbledygook.
You are in hurry, or play with your fingers? You need spider venom pills (that contain no spider venom).

You break furniture? Time goes too fast for you? Try the tarantula-free tarantula pills.
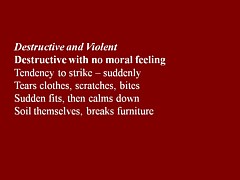
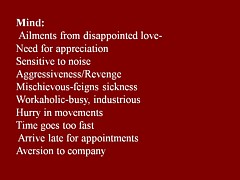
You are preoccupied with sex? You play with ropes? What you need is Mygale (which contains no Mygale)

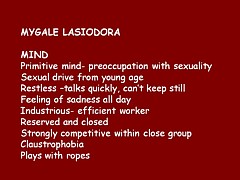
Much more seriously, the same sugar pills are recommended for serious conditions, chorea, ‘dim sight’, gonorrhoea, syphilis and burning hot urine.
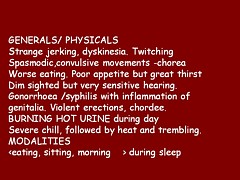
This isn’t just preposterous made-up stuff. It is dangerous.
There is a whole lot more fantasy stuff in the handouts for Homeopathy Materia Medica II (3CTH502). Here are a couple of examples.
Aurum metallicum (metallic gold) [Download the whole handout]
Affinities MIND, VASCULAR SYSTEM, Nerves, Heart, Bones, Glands, Liver, Kidneys, RIGHT SIDE, Left side.
Causations Emotions. Ailments from disappointed love and grief, offence or unusual responsibility, abuse of mercury or allopathic drugs.
Aurum belongs to the syphilitic miasm but has elements of sycosis (Aur-Mur).
Potassium salts are the subject of some fine fantasy, in “The Kali’s” [sic]. (there is much more serious stuff to worry about here than a few misplaced apostrophes.). [Download the whole handout]
“The radioactive element of potassium emits negative electrons from the atom nucleus and is thought to be significant in the sphere of cell processes especially in relation to functions relating to automatism and rhythmicity.”
“Kali people are very conscientious with strong principles. They have their rules and they stick to them, ‘a man of his word’.”
“Potassium acts in a parasympathetic way, tending towards depression”
“They [“Kali people=] are not melancholic like the Natrum’s but rather optimistic.”
Radioactive potassium is involved in automaticity? Total nonsense.
Where is the science?
Yes, it is true that the students get a bit of real science. There isn’t the slightest trace that I can find of any attempt to resolve the obvious fact that what they are taught in the science bits contradict directly what they are told in the other bits. Sounds like a recipe for stress to me.
They even get a bit of incredibly elementary statistics. But they can’t even get that right. This slide is from PPP – Res Quant data analysis.
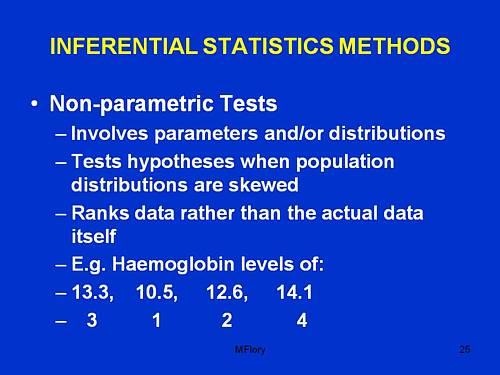
“Involves parameters and/or distributions”. This has no useful meaning whatsoever, that I can detect.
“Tests hypotheses when population distributions are skewed”. Well yes, though nothing there about forms of non-Gaussian properties other than skew, nothing about normalising transformations, and nothing about the Central Limit theorem.
“Ranks data rather than the actual data itself”. This is plain wrong. Randomisation tests on the original data are generally the best (uniformly most powerful) sort of non-parametric test. It seems to have escaped the attention of the tutor that ranking is a short-cut approximation that allowed tables to be constructed, before we had computers.
The students are told about randomised controlled trials. But amazingly in the lecture PPP-RCTs, the little matter of blinding is barely mantioned. And the teacher’s ideas about randomisation are a bit odd too.
Sorry, but if you fiddle the randomisation, no amount of “careful scrutiny” will rescue you from bias.
An Introduction to Naturopathic Philosophy
Naturopathy is just about as barmy as homeopathy. You can see something about it at the University of Wales. How about this slide from Westminster’s An Introduction to Naturopathic Philosophy.
So if you get tuberculosis, it isn’t caused by Mycobacterium tuberculosis? And the symptoms are “constructive”? So you don;t need to do anything. It’s all for the best really.
This isn’t just nonsense. It’s dangerous nonsense.
Traditional Chinese Medicine
Ever wondered what the mysterious “Qi” is? Worry no more. All is explained on this slide.
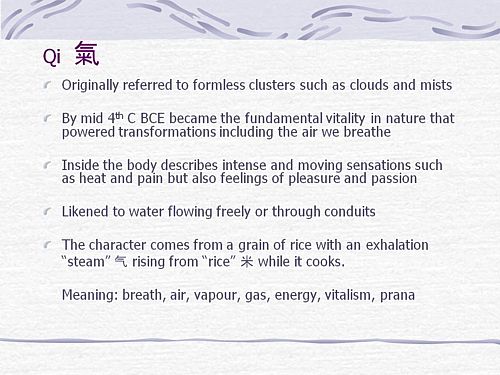
It means breath, air, vapour, gas, energy, vitalism. Or perhaps prana? Is that quite clear now?
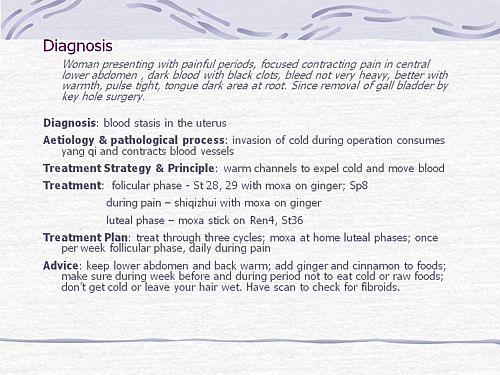
What can we make of this one? Anyone can see that the description is barely written in English and that vital information is missing (such as the age of the woman). And it’s nonsense to suggest that “invasion of cold” (during keyhole surgery!) would cause prolonged constriction of blood vessels (never mind that it would “consume yang qi”). Not being a clinician, I showed it to an oncologist friend. He said that it was impossible to tell from the description whether the problem was serious or not, but that any abdominal pain should be investigated properly. There isn’t anything here about referral for proper investigation. Just a lot of stuff about ginger and cinnamon. Anyone who was taught in this way could be a real danger to the public. It isn’t harmless nonsense It’s potentially harmful nonsense.
And finally, it’s DETOX
Surely everyone knows by now that ‘detox’ is no more than a marketing word? Well not at the University of Westminster. They have a long handout that tells you all the usual myths and a few new ones.
It is written by Jennifer Harper-Deacon, who describes herself modestly, thus.
Jennifer Harper-Deacon is a qualified and registered Naturopath and acupuncturist who holds a PhD in Natural Health and MSc in Complementary Therapies. She is a gifted healer and Reiki Master who runs her own clinic in Surrey where she believes in treating the ‘whole’ person by using a combination of Chinese medicine and naturopathic techniques that she has qualified in, including nutritional medicine, Chinese and Western herbalism, homoeopathy, applied kinesiology, reflexology, therapeutic massage, aromatherapy and flower remedies.
It seems that there is no limit on the number of (mutually incompatible) forms of nuttiness that she believes. Here are a few quotations from her handout for Westminster students.
“Detoxification is the single most powerful tool used by natural health professionals to prevent and reverse disease”
What? To “prevent and reverse” malaria? tuberculosis? Parkinson’s disease? AIDS? cancer?
“When you go on to a raw food only diet, especially fruit, the stored toxins are brought up from the deep organs such as the liver and kidneys, to the superficial systems of elimination.”;
Very odd. I always though that kidneys were a system of elimination.
“The over-use and mis-use of antibiotics has weakened the body’s ability to attack and destroy new strains of resistant bacteria, virulent viruses, which have led to our immune system becoming compromised.”
Certainly over-use and mis-use are problems. But I always thought it was the bacteria that became resistant.
“The beauty about detoxification therapy is that it addresses the very causative issues of health problems”
That is another dangerous and silly myth. Tuberculosis is not caused by mythical and un-named “toxins”. It is caused by Mycobacterium tuberculosis.
“Naturopathy follows the logic of cause and effect therefore believes that we simply need pure food and water, sunshine, air, adequate rest and sleep coupled with the right amount of exercise for health.”
Try telling that to someone with AIDS.
“Colon cleansing is one of the most important parts of any detoxification programme.”
The strange obsession with enemas in the alternative world is always baffling.
“Frankincense: holds the capacity to physically strengthen our defence system and can rebuild energy levels when our immune system is weak. Revered as a herb of protection, frankincense can also strengthen our spiritual defences when our Wei qi is low, making us more susceptible to negative energies. This calming oil has the ability to deepen the breath, helping us to let go of stale air and emotions, making it ideal oil to use inhale prior to meditating.”
This is so much hot air. There is a bit of evidence that frankincense might have some anti-inflammatory action and that’s it.
But this has to be my favourite.
“Remember when shopping to favour fruits and vegetables which are in season and locally grown (and ideally organic) as they are more vibrationally compatible with the body.”
Locally grown vegetables are “more vibrationally compatible with the body”? Pure mystical gobbledygook. Words fail me.
OK there’s a whole lot more, but that will do for now.
It’s good that Westminster is shutting down its Homeopathy BSc, but it seems they have a bit further to go.
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
Congratulations to the vice-chancellor of the University of Salford, Michael Harloe.
Times Higher Education announced on 15th January 2009 Salford to shut complementary medicine BSc.
“The University of Salford is to stop offering undergraduate degrees in acupuncture and complementary medicine because they are no longer considered “a sound academic fit”.”
This is the first time that a University has decided to stop teaching quackery altogether. The university’s press officer told me (22 January 2009)
| “all the University’s programmes associated with complementary medicine within the School of Community, Health Sciences & Social Care will be run out. This includes the Homeopathy in Practice programme. “ |
| Salford, before it became a university, was home to the great L.S. Lowry |

Salford’s Peel building, where L.S.Lowry worked |
“Managers concluded last year that the BSc traditional Chinese medicine and other degrees with a complementary medicine element “cannot really be held to be a good fit with the strategic direction of the school, and resource and energy would be better directed elsewhere”.
There are more than 70 students registered on the Chinese medicine degree course.
The university will continue to offer these subjects at postgraduate level, as short courses and as part of continuing professional development programmes. Traditional Chinese medicine work will also be linked to the university’s allied
health professions courses.”
Another report appeared in the Manchester Evening News: “Needle over acupuncture course”. “A UNIVERSITY has scrapped a course in acupuncture and aromatherapy branded `anti-science’ by critics.
Salford University said the three-year degree in traditional Chinese medicine didn’t fit with the `strategic direction’ bosses want to adopt.
The move is part of wider cuts which will see 150 teaching and support staff jobs axed.”
One of their students raised the question that the university must dread.
“First-year student Gary Leese, who is organising a petition, said: “Why did the university launch the course if they didn’t think it was good enough?”
The comments left by the readers of the Manchester Evening News were mostly very sensible. The first to come in, from someone with the beautifully Lancastrian name, Gladys Rowbotham, said “Some common sense at last!”.
A brief report appeared also in the Manchester Confidential
Why now?
This is rather an interesting development. On 19th April 2007, I sent a Freedom of Information request to Salford to ask for course validation documents for their courses in Homeopathy and in Traditional Chinese Medicine. I also asked for course materials for specified courses. This request was even less successful than usual. Not only were the course materials refused (as they always are), but, unusually, the validation documents were refused too. The excuse for this was more pathetic than usual too. They claimed it would cost more than £450 to email a few documents and powerpoints, and claimed exemption under Section 21 of the Freedom of Information Act, “Information Reasonably Accessible to the Applicant by Other Means”, rather than the more usual excuse (Section 43, “Commercial interests”).
It was never explained what “other means” were meant to be available. Perhaps they thought I should pay £3000 in fees and enrol for the course?
On 6th April 2007, Times Higher Education (THE) ran an opinion piece “Credible endeavour or pseudoscience?“. In this, I wrote, as follows.
“Clearly the buck stops with university vice-chancellors who award the degrees. Two weeks ago, after the publication of my opinion article and a special report on university homoeopathy courses in the journal Nature , the BBC tried to get one of the vice-chancellors to defend themselves. They did not succeed. Letters to vice-chancellors on this go unanswered. Requests to see course materials have repeatedly been refused. The QAA is exempt from the Freedom of Information Act. Teaching materials and the names of examiners are kept secret. This I find incomprehensible and indefensible.”
After this appeared, I was sent by the University of Salford a copy of Michael Harloe’s defence of their position at that time, as sent to THE. It relied heavily on validation by the Quality Assurance Agency. But the QAA is merely a box-ticking organisation that would give top marks to a course in astrology, given a sufficient mound of paperwork, as I pointed out in Nature, “Their own rules prevent them from doing anything useful”.
The statement also said that the courses teach critical thinking about alternative medicine. But it has been pointed out over and over again that what alternative medicine advocates lack, above anything else, is any faculty of critical self-appraisal.
One has to have some sympathy with a vice chancellor who is put on the spot and forced to defend courses in which he probably does not really believe himself. Perhaps it is not surprising that letters so often go unanswered. What can they say? There really is no answer that doesn’t leave the hapless VC with egg on his face.
If there is one lesson from this, it is not to be discouraged if you get no answer from a vice-chancellor. It has probably been read and may well get acted on eventually. Shutting down a course is no easy matter. It takes time.
I said the buck stops with the vice chancellor. Professor Harloe has grasped the nettle and done the right thing. Let’s hope a few more now follow his excellent lead..
What does this mean for the Pittilo report?
The gamma-minus Pittilo report (see also. The Times) recommended more degrees in alternative medicine, but there seems to be something of a trend developing in exactly the opposite direction.
The University of Central Lancashire has closed the first year entry to its “BSc” in Homeopathy, and announced a review of all its activities in the area of alternative medicine. Now we have Salford. There are stirrings among the good scientists even at the University of Westminster which has a new Dean and VC.
This rather absurd situation has arisen because of the adamant refusal of the government, and of a dozen or more quangos, to grasp the nettle of whether or not the alternative treatments work. Time and time again, the one important question that you want to know about any sort of treatment, namely, is it effective, has been pushed under the carpet.
The sort of absurd political correctness that leads to the fraudulent conjurers known as ‘psychic surgeons’ being referred to as a “profession” by the Department of Health has obscured reality. Even the MHRA was persuaded to allow misleading labelling of homeopathic and herbal “remedies”. thus betraying its job. In its own words “The MHRA is the government agency that is responsible for ensuring that medicines and medical devices work, . . .”.
There is a lesson here. You can’t go on avoiding reality for ever. One consolation is that, in the end, it is the universities who are leading the way, albeit slowly.
All we need now is for the Department of Health, the MHRA and the endless box-ticking quangos to wake up too.
Herbal medicine is, unlike homeopathy, not ridiculous, It is merely Pharmacology, as practised up to circa 1900. Whereas good trials have now shown acupuncture to be sham and homeopathy to be a placebo, there has been very little good research on herbs.
Most herbalism could fairly be described giving to sick patients an unknown dose of a substance with unknown efficacy and unknown safety.
How odd, then, to visit the Royal Society of Medicine to be greeted thus.
Just look at the words!
“Traditional Chinese Medicine (TCM) has developed over thousands of years”
That’s partly true
“and provides a comprehensive and systematic understanding of the natural world and the treatment of the human body.”
and that is total nonsense. TCM provides no understanding and virtually none of it is known to be useful for treating anything.
| Another poster at the RSM exhibition provides some of the explanation. What on earth, one wonders, do they mean by “making efforts to modernise TCM “? So far, the idea of modernising TCM doesn’t seem to include any great effort to find out if it works. Much of the promotion of TCM seems to be not so much ‘ancient wisdom’, but modern nationalist propaganda by the Chinese government. |
 |
The history is fascinating, but you won’t learn it from the posters on display at the exhibition.
“The Daoguang emperor though it [acupuncture] was a barrier to medical progress and removed it from the curriculum of the Imperial Medical Institute,”
“By the start of the twentieth century, acupuncture was extinct in the West and dormant in the East. It might have fallen out of favour permanently, but it suddenly experienced a revival in 1949 as a direct result of the communist revolution and the establishment of the People’s Republic of China. Chairman Mao Tse-tung engineered a resurgence in traditional Chinese medicine, which included not just acupuncture but also Chinese herbal medicine and other therapies ”
“His motivation was partly ideological, inasmuch as he wanted to reinforce a sense of national pride in Chinese medicine. However he was also driven by necessity. He had promised to deliver affordable healthcare .. . . ”
“Mao did not care whether traditional Chinese medicine worked, as long as he could keep the masses contented. In fact, his personal physician, Zhisui Li, wrote a memoir entitled ‘The Private Life of Chairman Mao’, in which he quoted Mao as saying”
“Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine.” “
Singh & Ernst Trick or Treatmant, page 46.
Or, as put more succinctly by Shapiro
“You would never know that TCM was fashioned in the twentieth century, as we shall see, from a ragbag of therapies in post-revolutionary China.”
Rose Shapiro, Suckers, how alternative medicine makes fools of us all.
Why is the Royal Society of Medicine allowing such mendacious posters? As it happens, I and a friend were visiting the RSM to see their Academic Dean, with a view to finding out why the RSM had failed to take any public position on alternative medicine. The answer appeared to be money, and that was the answer to why the TCM exhibition was being held on their premises too. The Dean no more believed in TCM than we did, but, well, they need the income. He pointed out (looking suitably sheepish) that the address given for the exhibition was not the RSM, but Number 1 Wimpole Street (that, of course, is also the address of the RSM).
Ah, so that’s OK then.
It has to be said that the RSM isn’t alone in its spineless attitude. Both the British Medical Association (BMA) and the Royal College of General Practitioners (RCGP) have failed to make any clear condemnation of mystical medicine. This is in stark contrast to just about every relevant scientific society (here is a summary).
It is a mystery to me why much of medicine should still be dominated by a mindset that seems to have lagged 200 years behind every other science. Perhaps medicine is just too complicated.
UCL Hospitals’ skeleton in the cupboard
Make no mistake, University College London Hospital is top class. The UCLH Trust. runs seven hospitals All but one of them are excellent. But in 2002 the Royal London Homeopathic Hospital was acquired as part of the UCLH group, to the intense embarrassment of UCL scientists.
Let’s start with the good bit. Usually I don’t like anecdotes, so just think of this as a vote of thanks, not evidence.
A personal history of UCH
I owe UCLH a lot personally. On December 13th 1984, my wife had
a subarachnoid haemorrhage when she was seven months pregnant. After misdiagnosis at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millilmetre from the pituitary on the other. It was a bit tricky but I think we got it”.
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds).. Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. | 
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album.. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. Heaven knows what it would have cost in the USA.
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew playing cricket in Bangladesh, Feb 2005. |
But now the the less desirable side of UCLH
Herbs and homeopaths at UCLH
| Recently I was sent the UCLH Annual Review 2007 – 2008. There was a lot of good stuff in it and worth a read despite there being too much hyperbole and too many pictures of men in dark suits. But buried among all the high tech stuff, what do we find but an advertisement for 1900-style pharmacology in the form of the herbal clinic at the Royal London Homeopathic Hospital, accompanied by a load of utterly inaccurate information from the TV botanist, David Bellamy. Take, for example, the claim about Devil’s Claw for osteoarthritis. Even alternative medicine advocates said “The authors concluded that there are insufficient high-quality trials to determine the safety and efficacy of Devil’s Claw (Harpagophytum procumbens) in the treatment of osteoarthritis, and that definitive trials are needed.”
Reading between the lines, I’d guess that the opening of this clinic has a subtext. It is well known that funding for homeopathy has dried up (partly as a result of our letter to NHS Trusts that appeared in the There have been problems before with the herbal activities at the RLHH before (see Conflicts of Interest at the Homeopathic Hospital). It appeared that the Khans, who run the Marigold homeopathic podiatry clinic (no, seriously, it is real) were largely prescribing a herbal product that was made by their own company. without even the hospital trust, never mind the patients, being made aware of it. In normal medicine this would be regarded as a rather serious offence, but as far as I know, nothing was ever done about it. |
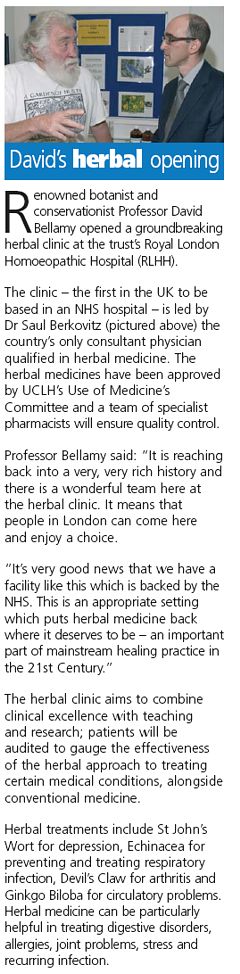 |
The ethics of alternative medicine are truly one of life’s great mysteries.
Reading further in the annual review, we come to the page about the RLHH. The homeopathy side must really have run down because it seems to have diversified into selling cosmetics and groceries. That sounds like desperation.

Good heavens, they sell “chemical-free sun cream”. One wonders what it can be made of, if not chemicals. This is the language of low-grade advertising agencies, not what one expects from an NHS hospital trust.
But next to this there is a much more interesting item. Just look at the last sentence.
I wonder if this could possibly have anything to do with the fact that Michael Baum and I visited the Trust headquarters in August 2006 to propose that the RLHH might be turned into a centre of supportive and palliative care? It would be nice to think so. But it seems they haven’t gone nearly far enough yet. If all they do is replace the waning homeopathy We know they are under pressure from their royal patrons, but that, in a constitutional monarchy, is simply not acceptable. |
 |
Michael Baum is a cancer surgeon who has taken a particular interest in palliative and supportive care. He is someone whose views should be taken seriously. He is also the author of the magnificent “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong” Here is a quotation from that letter. The UCLH Trust should bear it in mind.
| The power of my authority comes with a knowledge built on 40 years of study and 25 years of active involvement in cancer research. I’m sensitive to the danger of abusing this power and, as a last resort, I know that the General Medical Council (GMC) is watching over my shoulder to ensure I respect a code of conduct with a duty of care that respects patients’ dignity and privacy and reminds me that my personal beliefs should not prejudice my advice. Your power and authority rest on an accident of birth. Furthermore, your public utterances are worthy of four pages, whereas, if lucky, I might warrant one. I don’t begrudge you that authority and we probably share many opinions about art and architecture, but I do beg you to exercise your power with extreme caution when advising patients with life threatening diseases to embrace unproven therapies. There is no equivalent of the GMC for the monarchy, so it is left either to sensational journalism or, more rarely, to the quiet voice of loyal subjects such as myself to warn you that you may have overstepped the mark. It is in the nature of your world to be surrounded by sycophants (including members of the medical establishment hungry for their mention in the Queen’s birthday honours list) who constantly reinforce what they assume are your prejudices. Sir, they patronise you! Allow me this chastisement. |
Follow-up
The photo album chronicling the birth of my son, is really just for family and friends, but at least one blog picked up on the wider significance.
The Times today has given s good showing for my comment piece. It gives the case against following the advice of the Pittilo report. It simply makes no sense to have government regulation of acupuncture, herbal medicine, traditional Chinese medicine until such time as there is evidence that they work. It makes even less sense to have BSc degrees in them. The Department of Health should have more sense that to use the Prince of Wales as its scientific advisor.
Let’s hope that the recent example set by the University of Central Lancashire is the start of trend for vice-chancellors to appreciate that running such degrees brings their universities into disrepute.
I can only apologise for the dreadful title that The Times’ sub-editors put on the piece, My original title was
A bad report for the vice chancellor
The Pittilo report to the Department of Health will endanger the public and corrupt universities. There is a better way.
I like that much better than “Regulate quack nedicine? I feel sick”.
But, oh dear, the picture that I sent them is on the left, but what appeared is on the right. Spot the difference.
 |
 |
Well now, at least, I can feel I have something in common with Isambard Kingdom Brunel.
Follow-up
It so happens that Professor Pittilo wrote a letter to Times Higher Education this week. I fear that it provided a yet more evidence that he hasn’t really quite got the hang of evidence.
The Lancashire Evening Post catches up with the UCLan story, two days after you read it here.
A reply from Professor Pittilo
This response to the op-ed of 29th August appeared as a letter
in the Times on Sept 2.
| Public health needs protection
Regulation of acupuncture and herbal medicine has been subject to much scrutiny Sir, Professor Colquhoun’s campaign to discredit our report (“Regulate quack medicine? I feel sick,” Aug 29) is in danger of placing public health at risk. He is entitled to challenge existing evidence for the effectiveness of complementary and alternative medicine (CAM) but fails to acknowledge the key recommendation from the steering group on the essential need to demonstrate efficacy, safety and quality assurance as a prerequisite for NHS funding. Professor Colquhoun dismisses CAM because of the absence of a rigorous scientific foundation and he asserts that to teach and practise it is unethical. Survey data consistently demonstrates very high demand for CAM with one report estimating that 22 million visits involving 10.6 per cent of the population in England alone occurred in 2008. This demand is one reason why his alternative model of trade law enforcement will not work. He may argue that these people are uncritical recipients of nonsense, but data from the Medicines and Healthcare products Regulatory Agency confirm that they are at significant risk from poor practice. It is essential that we protect the public by implementing statutory regulation alongside demanding evidence of efficacy. Professor Colquhoun’s resistance to the teaching of science to CAM practitioners will do little to help them to critically evaluate effectiveness. Professor Michael Pittilo Chair of the Department of Health Steering Group |
And Pittilo wrote in similar vein to Times Higher Education.
Science vital to health study28 August 2008 Your feature on some members of staff at the University of Central Lancashire attacking science degrees in complementary and alternative medicine (“Staff attack science degrees in alternative health”, 7 August) raises a number of concerns. It is up to any university, taking account of the expert views of staff and external peer review, to determine the appropriate title and award for any degree. It is encouraging to note from the feature that new courses The recent report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and other Traditional Medicine There is no doubt that courses that provide a solid scientific foundation will greatly assist CAM practitioners in establishing evidence-based practice. It would be most unfortunate if the reported resistance to degree titles led to those wishing to practise acupuncture or herbal medicine receiving less hard science than they might have. To say that acupuncture and herbal medicine degrees have no academic justification appears arrogant in the extreme. Although it is certainly true that some content may not be scientific, this does not invalidate the legitimacy of these courses at degree level, a fact borne out by their successful validation in a number of universities. R. Michael Pittilo, Principal and vice-chancellor, The Robert Gordon University. |
This one got excellent responses from Kevin Smith (University of Abertay, Dundee), and from Peter J. Brophy (Professor of veterinary anatomy and cell biology University of Edinburgh). This was my comment to THE
There are a few very obvious responses to Professor Pittilo’s letter
For many alternative therapies the “philosophy” is simply incompatible with science. One obvious example is homeopathy. On Mondays and Wednesdays (science days) the students will be required to learn that response increases with dose. On Tuesdays and Thursdays will be taught the opposite. But for the exam they must reproduce only the latter (nonsensical) idea because their aim is to get a job as a homeopath. That makes nonsense of the idea of a university.
This seems to constitute a recognition that the evidence is still very inadequate. The time to start degrees, and the time to give official government recognition, is after the evidence is in, not before. What happens if you start degrees and then find that the subject is so much nonsense? Well, that has already happened in several areas of course. But the people who accredit the course and who act as external examiners just happen to be fervent believers in that nonsense, so all appears to be well (to bean counters anyway).
There is, as it happens, a great deal of evidence now about acupuncture, but the authors of the report do not seem to be aware of it. I recommend Barker Bausell’s book on the topic. If students are educated science, like what constitutes evidence, and our current understanding of words like “energy”, they would have to disavow the subject that there are supposed to training to practise
No, it is not a matter of arrogance, just a matter of careful attention to the evidence. Attention to evidence was notably absent in Prof Pittilo’s report, perhaps because his committee consisted entirely of people who earn their living from the subjects they were supposed to be assessing.
I have had the misfortune to have waded through a mound of such validation documents. The one thing they never consider is whether the treatment works. Sad to say, these validations are not worth the paper they are written on. |
The first major victory in the battle for the integrity of universities seems to have been won. This email was sent by Kate Chatfield who is module leader for the “BSc” in homeopathic medicine at the University of Central Lancashire (UCLAN).
| from Kate Chatfield…
Dear All, It’s a sad day for us here at UCLan because we have taken the decision not to run a first year this year due to low recruitment. The course will be put ‘on hold’ for this year and next until we see what happens with the general climate. Fortunately our masters course is thriving and we have been asked to focus upon this area and homeopathy research for the time being. Of late UCLan has been the subject of many attacks by the anti-homeopathy league. Colquhoun et al have kept the university lawyers and us quite fruitlessly busy by making claims for very detailed course information under the Freedom of Information Act. The latest demand is for 32 identified lesson plans with teaching notes, power points, handouts etc. The relentless attacks have taken their toll and it appears that they have won this small victory. The university has been very clear that this decision has been taken solely on the grounds of poor educational experience and is nothing to do with the current furore. They continue to be supportive of us and our efforts. Best wishes Kate and Jean |
There is some background here. In July 2006 I made a request to UCLAN under the Freedom of Information Act 2000, in which I asked to see some of their teaching materials. I appealed to UCLAN but Professor Patrick McGhee, Deputy Vice-Chancellor (Academic), also turned down two appeals. A letter sent directly to Professor Malcolm McVicar, vice-chancellor and president of UCLAN, failed to elicit the courtesy of a reply (standard practice I’m afraid, when a vice chancellor is faced with a difficult question). (Ironically, McVicar lists one of his interests as “health policy”.) So then I appealed to the Office of the Information Commissioner, in November 2006. Recently the case got to the top of the pile, and a judgment is expected any moment now.
Kate Chatfield’s letter to her colleagues is interesting. She describes a request ro see some of her teaching materials as an “attack”. If someone asks to see my teaching materials, I am rather flattered, and I send them. Is she not proud of what she teaches? Why all the secrecy? After all, you, the taxpayer, are paying for this stuff to be taught, so why should you not be able see it? Or is the problem that she feels that the “alternative reality” in which homeopaths live is just too complicated for mortals to grasp? Perhaps this attitude should be interpreted as flattering to the general public, because somewhere deep down she knows that the public will be able to spot gobbledygook when they see it. The revelation that the University of Westminster teaches first year undergraduates the “amethysts emit high yin energy” didn’t help their academic reputation much either.
Much credit for this decision must go also to the pressure from the many good academics at UCLAN. When it was revealed recently that UCLAN intended to open yet more courses in forms of medicine that are disproved or unproven, they naturally felt that their university was being brought into disrepute. Opposition to plans to introduce new “degrees” in acupuncture and Chinese herbal medicine were exposed in Times Higher Education recently. It particular, great credit must go to Dr Michael Eslea from UCLAN’s Psychology department. His open letter to his vice-chancellor is an example of scientific integrity in action.
The abandonment of this degree in medicines that contain no medicine is a small victory for common sense, for science and for the integrity of universities. Sadly, there is still a long way to go.
It is my understanding that ‘bringing the university into disrepute’ is a serious offence. Please note, vice-chancellor.
A few more judgments like that to suspend your homeopathy degree could work wonders for your reputation.
The follow-up
Watch this space.
The Guardian was quick off the mark -this story appeared on their education web site within 3 hours of my posting it “Homeopathy degrees suspended after criticism” by Anthea Lipsett. My comment there disappeared for a while because the Guardian legal people misunderstood the meaning of the last sentence. It’s back now, with blame allocated unambiguously to the vice-chancellors of the 16 or so universities who run this sort of course.
UCLAN’s web site seems to need some updating. The “BSc” in homeopathic medicine is still advertised there. as of 28 August.
UCLAN’s best ally. Dr Michael Eslea, has had some publicity for his attempts to rescue his university’s reputation. The story appeared in the “High Principals” column of Private Eye (Issue 1217, Aug 22, 2008). It also appeared in his local paper, the Lancashire Evening Post.
The Lancashire Evening Post catches up with homeopathy suspension story, two days after you read it here. But the UCLAN web site still advertises it.

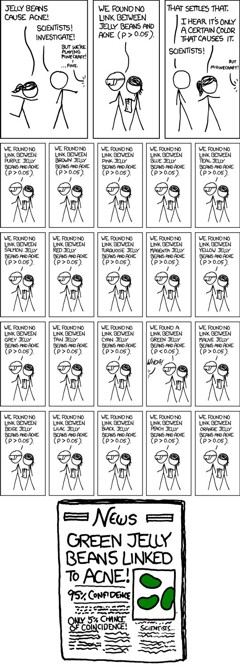
 >
>