Traditional Chinese medicine
|
It seems that bits of good news don’t come singly. First honours degrees in acupuncture vanish, Now a big chain of shops selling Chinese herbs and acupuncture has gone into administration. It seems that, at last, people are getting fed up with being conned out of their hard-earned money |
 Herbmedic Barking |
A local newspaper, The North Herts Comet reported thus.
Customers of Herbmedic, which trades under the name Herbs and Acupuncture, on Queensway in Stevenage have been left counting the cost after shelling out hundreds of pounds for treatment they never received.
The company, which has practices across the country, is now in the hands of receivers, Macintyre Hudson.
Sandra Emery, of The Paddocks in Stevenage, paid £350 for 10 treatment sessions, but only received one before the practice closed.
She said: “A standard course of treatment is 10 sessions, so most customers will have bought this package.
Claudia Gois, of Walden End in Stevenage, paid £240 for 12 treatment sessions but only received four before the practice closed.
She said: “I went there on Friday and it was closed. There was no warning or anything.
“I got in touch with head office and they said it’s very unlikely I will get money back.
This report was on 1st April, The company’s web site shows no sign of any problems, In fact they are still advertising jobs. So was this an April Fool joke?
No it wasn’t. A visit to Companies House soon settled the matter. The whole company is insolvent, as of 27 March 2009..
Download the whole administration notice and the company report.
Criticisms of Herbmedic
This chain of shops was investigated by the BBC’s
Inside Out programme. (September 25th 2006).
“We sent an undercover reporter to branches of the Herbmedic chain in southern England.
On each occasion, the reporter claimed to be suffering from tiredness and was prescribed herbal remedies after a consultation lasting less than five minutes.
The herbalists, who describe themselves as “doctors”, didn’t ask any questions about the patient’s medical history or take any notes.”
This is so bad that even Andrew Fowler, a past President of the Register of Chinese Herbal Medicine, described it as “malpractice”.
“Herbmedic has been investigated by the authorities in the past.
In 2002, trading standards officers prosecuted the branch in Southampton for selling herbal remedies with 26 times the permitted legal limit of lead.
And in October 2003, the Advertising Standards Authority banned Herbmedic from describing its practitioners as “doctors”.
Despite the ban, all three of the stores visited by Inside Out referred to the herbalist as the doctor.”
See also the BBC report Herbalists’ customers ‘at risk’, and a report in the Sunday Times, Herbmedic accused of high-pressure selling.
Read the Advertising Standards report. Seven different complaints against Herbmedic were upheld.
This is entirely consistent with my own experience. I went into one of their shops and asked about a cure for diabetes (hoping the be able to refer them to Trading Standards, but the young lady behind the counter had such a poor grasp of English that her reply was incomprehensible. She just kept trying to push me into having a consultation with “the doctor” who appeared to speak no English at all. I left.
The chequered history of Herbmedic
The company that his just gone into administration is Herbmedic Centre Ltd. It has been in existence for only two years. Its predecessor, known simply as Herbmedic, was dissolved on 13 March 2007, Companies House said
Company Filing History Type Date Description Order GAZ2(A) 13/03/2007 FINAL GAZETTE: DISSOLVED VIA VOLUNTARY STRIKE-OFF GAZ1(A) 28/11/2006 FIRST GAZETTE NOTICE FOR VOLUNTARY STRIKE-OFF 652a 16/10/2006 APPLICATION FOR STRIKING-OFF
Another Chinese medicine chain seems to be having a few problems too
Harmony Medical Distribution Ltd (“specialists in acupuncture and holistic medicine”) seems to be still in business(web site here), but several very similar companies have been dissolved, Harmomy Medics Ltd (dissolved 19 Sep 2006) ,, Harmony Medical Services (UK ) Ltd. (dissolved 6 May 2008) and Harmony Medical Services Ltd (dissolved 17 Oct 2008)
Given this history of companies that dissolve every couple of years and then mysteriously reincarnate with a slightly different name, one wonders if this really is the end of herbmedic, or it is just a device for shedding bad debts. Is this just another “pre-pack administration“?
Watch this space for more.
What’s the latest evidence on acupuncture anyway?
A correspondent drew my attention to the 2009 Annual Evidence Update on acupuncture complied by the NHS Complementary and Alternative Medicine Specialist Library. This includes no fewer than 56 systematic reviews and meta-analyses. Although the reviews are complied by alternative medicine sympathisers, they seem mostly to be pretty fair. Well apart form one thing.
Almost all of the reviews fail to come up with any positive evidence that acupuncture works well enough to be clinically useful. Only two come close, and they are the two singled out as “editor’s picks”. Perhaps that’s not entirely surprising given that the editor is Dr Mike Cummings.
Again and again, the results are inconclusive: #8 is pretty typical
Acupuncture for tension-type headache: a meta-analysis of randomized, controlled trials.
This meta-analysis suggests that acupuncture compared with sham for tension-type headache has limited efficacy for the reduction of headache frequency. There exists a lack of standardization of acupuncture point selection and treatment course among randomized, controlled trials. More research is needed to investigate the treatment of specific tension-type headache subtypes.
Vast effort and a lot of money is being put into trials, yet there are very few (if any) positive results. Very often there are no results at whatsoever. All we hear, again and again, is “more research is needed”.
At some point someone will have to decide it is all a charade and start to spend time and money on investigating things that are more promising.
Follow-up
A correspondent checked with Companies House to discover more about two of the directors of Herbmedic, Mr. Li Mao and Mr Xiao Xuan Chen. They have a chequered history indeed. [download the complete list]
Mr. Li Mao is, or has been, on the board of 31 different companies. Of these 6 are active, 5 are in administration, 14 were dissolved, 4 were liquidated and 2 are active with proposal to strike off. Not only is Her Medic centre Ltd in administration, but so is Dr China (UK) Ltd, and Great Chinese Herbal Medicine Ltd
With record like that, my correspondent wonders whether they should be disqualified.
In March 2007 I wrote a piece in Nature on Science degrees without the science. At that time there were five “BSc” degrees in homeopathy. A couple of weeks ago I checked the UCAS site for start in 2009, and found there was only one full “BSc (hons)” left and that was at Westminster University.
Today I checked again and NOW THERE ARE NONE.
A phone call to the University of Westminster tonight confirmed that they have suspended entry to their BSc (Hons) homeopathy degree.
They say that they have done so because of “poor recruitment”. It was a purely financial decision. Nothing to do with embarrasment. Gratifying though it is that recruits for the course are vanishing, that statement is actually pretty appalling It says that the University of Westminster doesn’t care whether it’s nonsense, but only about whether it makes money.
Nevertheless the first part of this post is not entirely outdated before it even appeared, because homeopathy will still be taught as part of Complementary Therapies. And Naturopathy and “Nutritional Therapy” are still there..
According to their ‘School of Integrated Health‘, “The University of Westminster has a vision of health care for the 21st Century”. Yes, but it is what most people would call a vision of health care in the 18th century.
The revelation that the University of Westminster teaches that Amethysts emit high Yin energy caused something of a scandal.
Since then I have acquired from several sources quite a lot more of their teaching material, despite the fact that the university has refused to comply with the Freedom of Information Act.
In view of the rather silly internal review conducted by Westminster’s Vice-Chancellor, Professor Geoffrey Petts, this seems like a good moment to make a bit more of it public,
I think that revelation of the material is justified because it is in the
public interest to know how the University if Westminster is spending taxpayers’ money. Another motive is to defend the reputation of the post-1992 universities. I have every sympathy with the ex-polytechnics in their efforts to convert themselves into universities. In many ways they have succeeded. That effort
is impeded by teaching mystical versions of medicine.
If the University of Westminster is being brought into disrepute, blame its vice-chancellor, not me.
Homeopathic spiders
Here are a few slides from a lecture on how good spider venom is for you. It is from Course 3CTH502 Homeopathic Materia Medica II. No need to worry though, because they are talking about homeopathic spider venom, so there is nothing but sugar in the pills. The involvement of spiders is pure imagination. No more than mystical gobbledygook.
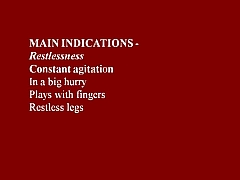
You are in hurry, or play with your fingers? You need spider venom pills (that contain no spider venom).
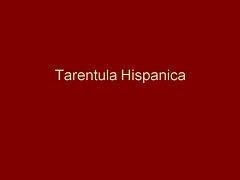

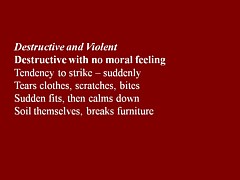
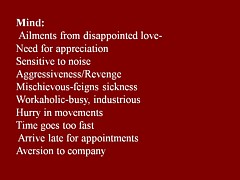
You break furniture? Time goes too fast for you? Try the tarantula-free tarantula pills.
You are preoccupied with sex? You play with ropes? What you need is Mygale (which contains no Mygale)

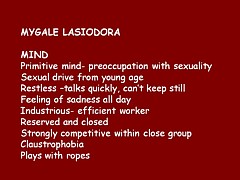
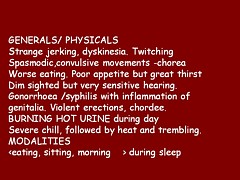
Much more seriously, the same sugar pills are recommended for serious conditions, chorea, ‘dim sight’, gonorrhoea, syphilis and burning hot urine.
This isn’t just preposterous made-up stuff. It is dangerous.
There is a whole lot more fantasy stuff in the handouts for Homeopathy Materia Medica II (3CTH502). Here are a couple of examples.
Aurum metallicum (metallic gold) [Download the whole handout]
Affinities MIND, VASCULAR SYSTEM, Nerves, Heart, Bones, Glands, Liver, Kidneys, RIGHT SIDE, Left side.
Causations Emotions. Ailments from disappointed love and grief, offence or unusual responsibility, abuse of mercury or allopathic drugs.
Aurum belongs to the syphilitic miasm but has elements of sycosis (Aur-Mur).
Potassium salts are the subject of some fine fantasy, in “The Kali’s” [sic]. (there is much more serious stuff to worry about here than a few misplaced apostrophes.). [Download the whole handout]
“The radioactive element of potassium emits negative electrons from the atom nucleus and is thought to be significant in the sphere of cell processes especially in relation to functions relating to automatism and rhythmicity.”
“Kali people are very conscientious with strong principles. They have their rules and they stick to them, ‘a man of his word’.”
“Potassium acts in a parasympathetic way, tending towards depression”
“They [“Kali people=] are not melancholic like the Natrum’s but rather optimistic.”
Radioactive potassium is involved in automaticity? Total nonsense.
Where is the science?
Yes, it is true that the students get a bit of real science. There isn’t the slightest trace that I can find of any attempt to resolve the obvious fact that what they are taught in the science bits contradict directly what they are told in the other bits. Sounds like a recipe for stress to me.
They even get a bit of incredibly elementary statistics. But they can’t even get that right. This slide is from PPP – Res Quant data analysis.
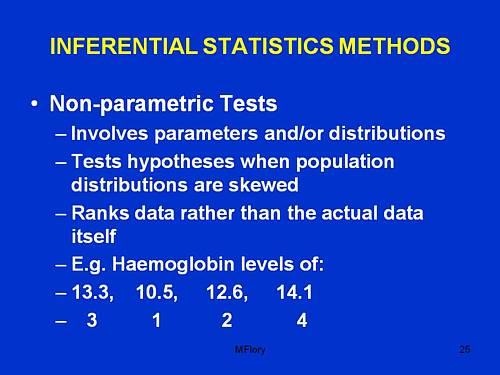
“Involves parameters and/or distributions”. This has no useful meaning whatsoever, that I can detect.
“Tests hypotheses when population distributions are skewed”. Well yes, though nothing there about forms of non-Gaussian properties other than skew, nothing about normalising transformations, and nothing about the Central Limit theorem.
“Ranks data rather than the actual data itself”. This is plain wrong. Randomisation tests on the original data are generally the best (uniformly most powerful) sort of non-parametric test. It seems to have escaped the attention of the tutor that ranking is a short-cut approximation that allowed tables to be constructed, before we had computers.
The students are told about randomised controlled trials. But amazingly in the lecture PPP-RCTs, the little matter of blinding is barely mantioned. And the teacher’s ideas about randomisation are a bit odd too.
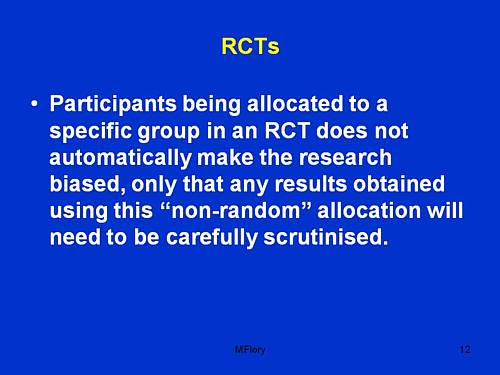
Sorry, but if you fiddle the randomisation, no amount of “careful scrutiny” will rescue you from bias.
An Introduction to Naturopathic Philosophy
Naturopathy is just about as barmy as homeopathy. You can see something about it at the University of Wales. How about this slide from Westminster’s An Introduction to Naturopathic Philosophy.
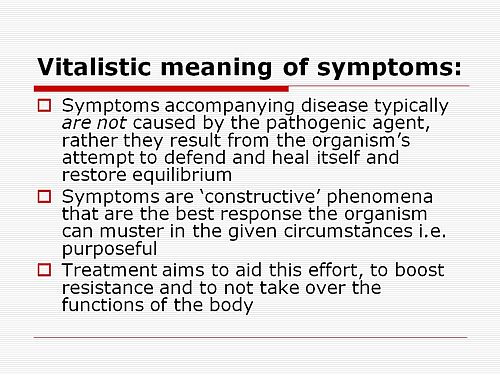
So if you get tuberculosis, it isn’t caused by Mycobacterium tuberculosis? And the symptoms are “constructive”? So you don;t need to do anything. It’s all for the best really.
This isn’t just nonsense. It’s dangerous nonsense.
Traditional Chinese Medicine
Ever wondered what the mysterious “Qi” is? Worry no more. All is explained on this slide.
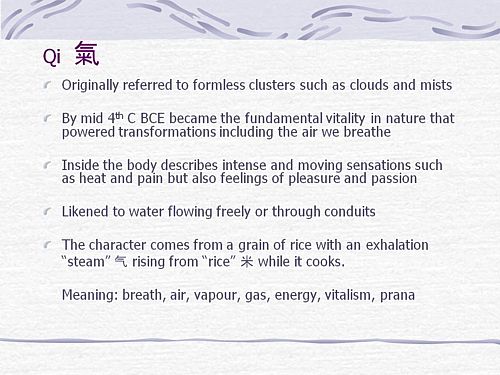
It means breath, air, vapour, gas, energy, vitalism. Or perhaps prana? Is that quite clear now?
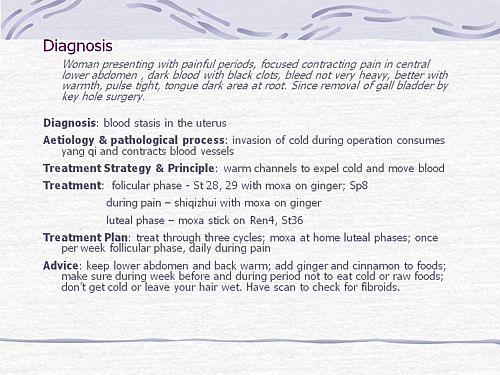
What can we make of this one? Anyone can see that the description is barely written in English and that vital information is missing (such as the age of the woman). And it’s nonsense to suggest that “invasion of cold” (during keyhole surgery!) would cause prolonged constriction of blood vessels (never mind that it would “consume yang qi”). Not being a clinician, I showed it to an oncologist friend. He said that it was impossible to tell from the description whether the problem was serious or not, but that any abdominal pain should be investigated properly. There isn’t anything here about referral for proper investigation. Just a lot of stuff about ginger and cinnamon. Anyone who was taught in this way could be a real danger to the public. It isn’t harmless nonsense It’s potentially harmful nonsense.
And finally, it’s DETOX
Surely everyone knows by now that ‘detox’ is no more than a marketing word? Well not at the University of Westminster. They have a long handout that tells you all the usual myths and a few new ones.
It is written by Jennifer Harper-Deacon, who describes herself modestly, thus.
Jennifer Harper-Deacon is a qualified and registered Naturopath and acupuncturist who holds a PhD in Natural Health and MSc in Complementary Therapies. She is a gifted healer and Reiki Master who runs her own clinic in Surrey where she believes in treating the ‘whole’ person by using a combination of Chinese medicine and naturopathic techniques that she has qualified in, including nutritional medicine, Chinese and Western herbalism, homoeopathy, applied kinesiology, reflexology, therapeutic massage, aromatherapy and flower remedies.
It seems that there is no limit on the number of (mutually incompatible) forms of nuttiness that she believes. Here are a few quotations from her handout for Westminster students.
“Detoxification is the single most powerful tool used by natural health professionals to prevent and reverse disease”
What? To “prevent and reverse” malaria? tuberculosis? Parkinson’s disease? AIDS? cancer?
“When you go on to a raw food only diet, especially fruit, the stored toxins are brought up from the deep organs such as the liver and kidneys, to the superficial systems of elimination.”;
Very odd. I always though that kidneys were a system of elimination.
“The over-use and mis-use of antibiotics has weakened the body’s ability to attack and destroy new strains of resistant bacteria, virulent viruses, which have led to our immune system becoming compromised.”
Certainly over-use and mis-use are problems. But I always thought it was the bacteria that became resistant.
“The beauty about detoxification therapy is that it addresses the very causative issues of health problems”
That is another dangerous and silly myth. Tuberculosis is not caused by mythical and un-named “toxins”. It is caused by Mycobacterium tuberculosis.
“Naturopathy follows the logic of cause and effect therefore believes that we simply need pure food and water, sunshine, air, adequate rest and sleep coupled with the right amount of exercise for health.”
Try telling that to someone with AIDS.
“Colon cleansing is one of the most important parts of any detoxification programme.”
The strange obsession with enemas in the alternative world is always baffling.
“Frankincense: holds the capacity to physically strengthen our defence system and can rebuild energy levels when our immune system is weak. Revered as a herb of protection, frankincense can also strengthen our spiritual defences when our Wei qi is low, making us more susceptible to negative energies. This calming oil has the ability to deepen the breath, helping us to let go of stale air and emotions, making it ideal oil to use inhale prior to meditating.”
This is so much hot air. There is a bit of evidence that frankincense might have some anti-inflammatory action and that’s it.
But this has to be my favourite.
“Remember when shopping to favour fruits and vegetables which are in season and locally grown (and ideally organic) as they are more vibrationally compatible with the body.”
Locally grown vegetables are “more vibrationally compatible with the body”? Pure mystical gobbledygook. Words fail me.
OK there’s a whole lot more, but that will do for now.
It’s good that Westminster is shutting down its Homeopathy BSc, but it seems they have a bit further to go.
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
Congratulations to the vice-chancellor of the University of Salford, Michael Harloe.
Times Higher Education announced on 15th January 2009 Salford to shut complementary medicine BSc.
“The University of Salford is to stop offering undergraduate degrees in acupuncture and complementary medicine because they are no longer considered “a sound academic fit”.”
This is the first time that a University has decided to stop teaching quackery altogether. The university’s press officer told me (22 January 2009)
| “all the University’s programmes associated with complementary medicine within the School of Community, Health Sciences & Social Care will be run out. This includes the Homeopathy in Practice programme. “ |
| Salford, before it became a university, was home to the great L.S. Lowry |

Salford’s Peel building, where L.S.Lowry worked |
“Managers concluded last year that the BSc traditional Chinese medicine and other degrees with a complementary medicine element “cannot really be held to be a good fit with the strategic direction of the school, and resource and energy would be better directed elsewhere”.
There are more than 70 students registered on the Chinese medicine degree course.
The university will continue to offer these subjects at postgraduate level, as short courses and as part of continuing professional development programmes. Traditional Chinese medicine work will also be linked to the university’s allied
health professions courses.”
Another report appeared in the Manchester Evening News: “Needle over acupuncture course”. “A UNIVERSITY has scrapped a course in acupuncture and aromatherapy branded `anti-science’ by critics.
Salford University said the three-year degree in traditional Chinese medicine didn’t fit with the `strategic direction’ bosses want to adopt.
The move is part of wider cuts which will see 150 teaching and support staff jobs axed.”
One of their students raised the question that the university must dread.
“First-year student Gary Leese, who is organising a petition, said: “Why did the university launch the course if they didn’t think it was good enough?”
The comments left by the readers of the Manchester Evening News were mostly very sensible. The first to come in, from someone with the beautifully Lancastrian name, Gladys Rowbotham, said “Some common sense at last!”.
A brief report appeared also in the Manchester Confidential
Why now?
This is rather an interesting development. On 19th April 2007, I sent a Freedom of Information request to Salford to ask for course validation documents for their courses in Homeopathy and in Traditional Chinese Medicine. I also asked for course materials for specified courses. This request was even less successful than usual. Not only were the course materials refused (as they always are), but, unusually, the validation documents were refused too. The excuse for this was more pathetic than usual too. They claimed it would cost more than £450 to email a few documents and powerpoints, and claimed exemption under Section 21 of the Freedom of Information Act, “Information Reasonably Accessible to the Applicant by Other Means”, rather than the more usual excuse (Section 43, “Commercial interests”).
It was never explained what “other means” were meant to be available. Perhaps they thought I should pay £3000 in fees and enrol for the course?
On 6th April 2007, Times Higher Education (THE) ran an opinion piece “Credible endeavour or pseudoscience?“. In this, I wrote, as follows.
“Clearly the buck stops with university vice-chancellors who award the degrees. Two weeks ago, after the publication of my opinion article and a special report on university homoeopathy courses in the journal Nature , the BBC tried to get one of the vice-chancellors to defend themselves. They did not succeed. Letters to vice-chancellors on this go unanswered. Requests to see course materials have repeatedly been refused. The QAA is exempt from the Freedom of Information Act. Teaching materials and the names of examiners are kept secret. This I find incomprehensible and indefensible.”
After this appeared, I was sent by the University of Salford a copy of Michael Harloe’s defence of their position at that time, as sent to THE. It relied heavily on validation by the Quality Assurance Agency. But the QAA is merely a box-ticking organisation that would give top marks to a course in astrology, given a sufficient mound of paperwork, as I pointed out in Nature, “Their own rules prevent them from doing anything useful”.
The statement also said that the courses teach critical thinking about alternative medicine. But it has been pointed out over and over again that what alternative medicine advocates lack, above anything else, is any faculty of critical self-appraisal.
One has to have some sympathy with a vice chancellor who is put on the spot and forced to defend courses in which he probably does not really believe himself. Perhaps it is not surprising that letters so often go unanswered. What can they say? There really is no answer that doesn’t leave the hapless VC with egg on his face.
If there is one lesson from this, it is not to be discouraged if you get no answer from a vice-chancellor. It has probably been read and may well get acted on eventually. Shutting down a course is no easy matter. It takes time.
I said the buck stops with the vice chancellor. Professor Harloe has grasped the nettle and done the right thing. Let’s hope a few more now follow his excellent lead..
What does this mean for the Pittilo report?
The gamma-minus Pittilo report (see also. The Times) recommended more degrees in alternative medicine, but there seems to be something of a trend developing in exactly the opposite direction.
The University of Central Lancashire has closed the first year entry to its “BSc” in Homeopathy, and announced a review of all its activities in the area of alternative medicine. Now we have Salford. There are stirrings among the good scientists even at the University of Westminster which has a new Dean and VC.
This rather absurd situation has arisen because of the adamant refusal of the government, and of a dozen or more quangos, to grasp the nettle of whether or not the alternative treatments work. Time and time again, the one important question that you want to know about any sort of treatment, namely, is it effective, has been pushed under the carpet.
The sort of absurd political correctness that leads to the fraudulent conjurers known as ‘psychic surgeons’ being referred to as a “profession” by the Department of Health has obscured reality. Even the MHRA was persuaded to allow misleading labelling of homeopathic and herbal “remedies”. thus betraying its job. In its own words “The MHRA is the government agency that is responsible for ensuring that medicines and medical devices work, . . .”.
There is a lesson here. You can’t go on avoiding reality for ever. One consolation is that, in the end, it is the universities who are leading the way, albeit slowly.
All we need now is for the Department of Health, the MHRA and the endless box-ticking quangos to wake up too.
I’m perfectly happy to think of alternative medicine as being a voluntary, self-imposed tax on the gullible (to paraphrase Goldacre again). But only as long as its practitioners do no harm and only as long as they obey the law of the land. Only too often, though, they do neither.
When I talk about law, I don’t mean lawsuits for defamation. Defamation suits are what homeopaths and chiropractors like to use to silence critics. heaven knows, I’ve becomes accustomed to being defamed by people who are, in my view. fraudsters, but lawsuits are not the way to deal with it.
I’m talking about the Trading Standards laws Everyone has to obey them, and in May 2008 the law changed in a way that puts the whole health fraud industry in jeopardy.
The gist of the matter is that it is now illegal to claim that a product will benefit your health if you can’t produce evidence to justify the claim.
I’m not a lawyer, but with the help of two lawyers and a trading standards officer I’ve attempted a summary. The machinery for enforcing the law does not yet work well, but when it does, there should be some very interesting cases.
The obvious targets are homeopaths who claim to cure malaria and AIDS, and traditional Chinese Medicine people who claim to cure cancer.
But there are some less obvious targets for prosecution too. Here is a selection of possibilities to savour..
- Universities such as Westminster, Central Lancashire and the rest, which promote the spreading of false health claims
- Hospitals, like the Royal London Homeopathic Hospital, that treat patients with mistletoe and marigold paste. Can they produce any real evidence that they work?
- Edexcel, which sets examinations in alternative medicine (and charges for them)
- Ofsted and the QCA which validate these exams
- Skills for Health and a whole maze of other unelected and unaccountable quangos which offer “national occupational standards” in everything from distant healing to hot stone therapy, thereby giving official sanction to all manner of treatments for which no plausible evidence can be offered.
- The Prince of Wales Foundation for Integrated Health, which notoriously offers health advice for which it cannot produce good evidence
- Perhaps even the Department of Health itself, which notoriously referred to “psychic surgery” as a profession, and which has consistently refused to refer dubious therapies to NICE for assessment.
The law, insofar as I’ve understood it, is probably such that only the first three or four of these have sufficient commercial elements for there to be any chance of a successful prosecution. That is something that will eventually have to be argued in court.
But lecanardnoir points out in his comment below that The Prince of Wales is intending to sell herbal concoctions, so perhaps he could end up in court too.
The laws
We are talking about The Consumer Protection from Unfair Trading Regulations 2008. The regulations came into force on 26 May 2008. The full regulations can be seen here, or download pdf file. They can be seen also on the UK Statute Law Database.
The Office of Fair Trading, and Department for Business, Enterprise & Regulatory Reform (BERR) published Guidance on the Consumer Protection from Unfair Trading Regulations 2008 (pdf file),
Statement of consumer protection enforcement principles (pdf file), and
The Consumer Protection from Unfair Trading Regulations: a basic guide for business (pdf file).
Has The UK Quietly Outlawed “Alternative” Medicine?
On 26 September 2008, Mondaq Business Briefing published this article by a Glasgow lawyer, Douglas McLachlan. (Oddly enough, this article was reproduced on the National Center for Homeopathy web site.)
“Proponents of the myriad of forms of alternative medicine argue that it is in some way “outside science” or that “science doesn’t understand why it works”. Critical thinking scientists disagree. The best available scientific data shows that alternative medicine simply doesn’t work, they say: studies repeatedly show that the effect of some of these alternative medical therapies is indistinguishable from the well documented, but very strange “placebo effect” ”
“Enter The Consumer Protection from Unfair Trading Regulations 2008(the “Regulations”). The Regulations came into force on 26 May 2008 to surprisingly little fanfare, despite the fact they represent the most extensive modernisation and simplification of the consumer protection framework for 20 years.”
The Regulations prohibit unfair commercial practices between traders and consumers through five prohibitions:-
- General Prohibition on Unfair Commercial
Practices (Regulation 3)- Prohibition on Misleading Actions (Regulations 5)
- Prohibition on Misleading Omissions (Regulation 6)
- Prohibition on Aggressive Commercial Practices (Regulation 7)
- Prohibition on 31 Specific Commercial Practices that are in all Circumstances Unfair (Schedule 1). One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. The definition of “product” in the Regulations includes services, so it does appear that all forms medical products and treatments will be covered.
Just look at that!
| One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations” |
Section 5 is equally powerful, and also does not contain the contentious word “cure” (see note below)
Misleading actions
5.—(1) A commercial practice is a misleading action if it satisfies the conditions in either paragraph (2) or paragraph (3).
(2) A commercial practice satisfies the conditions of this paragraph—
(a) if it contains false information and is therefore untruthful in relation to any of the matters in paragraph (4) or if it or its overall presentation in any way deceives or is likely to deceive the average consumer in relation to any of the matters in that paragraph, even if the information is factually correct; and
(b) it causes or is likely to cause the average consumer to take a transactional decision he would not have taken otherwise.
These laws are very powerful in principle, But there are two complications in practice.
One complication concerns the extent to which the onus has been moved on to the seller to prove the claims are true, rather than the accuser having to prove they are false. That is a lot more favourable to the accuser than before, but it’s complicated.
The other complication concerns enforcement of the new laws, and at the moment that is bad.
Who has to prove what?
That is still not entirely clear. McLachlan says
“If we accept that mainstream evidence based medicine is in some way accepted by mainstream science, and alternative medicine bears the “alternative” qualifier simply because it is not supported by mainstream science, then where does that leave a trader who seeks to refute any allegation that his claim is false?
Of course it is always open to the trader to show that his the alternative therapy actually works, but the weight of scientific evidence is likely to be against him.”
On the other hand, I’m advised by a Trading Standards Officer that “He doesn’t have to refute anything! The prosecution have to prove the claims are false”. This has been confirmed by another Trading Standards Officer who said
“It is not clear (though it seems to be) what difference is implied between “cure” and “treat”, or what evidence is required to demonstrate that such a cure is false “beyond reasonable doubt” in court. The regulations do not provide that the maker of claims must show that the claims are true, or set a standard indicating how such a proof may be shown.”
The main defence against prosecution seems to be the “Due diligence defence”, in paragraph 17.
Due diligence defence
17. —(1) In any proceedings against a person for an offence under regulation 9, 10, 11 or 12 it is a defence for that person to prove—
(a) that the commission of the offence was due to—
(i) a mistake;
(ii) reliance on information supplied to him by another person;
(iii) the act or default of another person;
(iv) an accident; or
(v) another cause beyond his control; and
(b) that he took all reasonable precautions and exercised all due diligence to avoid the commission of such an offence by himself or any person under his control.
If “taking all reasonable precautions” includes being aware of the lack of any good evidence that what you are selling is effective, then this defence should not be much use for most quacks.
Douglas McLachlan has clarified, below, this difficult question
False claims for health benefits of foods
A separate bit of legislation, European regulation on nutrition and health claims made on food, ref 1924/2006, in Article 6, seems clearer in specifying that the seller has to prove any claims they make.
Article 6
Scientific substantiation for claims
1. Nutrition and health claims shall be based on and substantiated by generally accepted scientific evidence.
2. A food business operator making a nutrition or health claim shall justify the use of the claim.
3. The competent authorities of the Member States may request a food business operator or a person placing a product on the market to produce all relevant elements and data establishing compliance with this Regulation.
That clearly places the onus on the seller to provide evidence for claims that are made, rather than the complainant having to ‘prove’ that the claims are false.
On the problem of “health foods” the two bits of legislation seem to overlap. Both have been discussed in “Trading regulations and health foods“, an editorial in the BMJ by M. E. J. Lean (Professor of Human Nutrition in Glasgow).
“It is already illegal under food labelling regulations (1996) to claim that food products can treat or prevent disease. However, huge numbers of such claims are still made, particularly for obesity ”
“The new regulations provide good legislation to protect vulnerable consumers from misleading “health food” claims. They now need to be enforced proactively to help direct doctors and consumers towards safe, cost effective, and evidence based management of diseases.”
In fact the European Food Standards Agency (EFSA) seems to be doing a rather good job at imposing the rules. This, predictably, provoked howls of anguish from the food industry There is a synopsis here.
“Of eight assessed claims, EFSA’s Panel on Dietetic Products, Nutrition and Allergies (NDA) rejected seven for failing to demonstrate causality between consumption of specific nutrients or foods and intended health benefits. EFSA has subsequently issued opinions on about 30 claims with seven drawing positive opinions.”
“. . . EFSA in disgust threw out 120 dossiers supposedly in support of nutrients seeking addition to the FSD’s positive list.
If EFSA was bewildered by the lack of data in the dossiers, it needn’t hav been as industry freely admitted it had in many cases submitted such hollow documents to temporarily keep nutrients on-market.”
Or, on another industry site, “EFSA’s harsh health claim regime”
“By setting an unworkably high standard for claims substantiation, EFSA is threatening R&D not to mention health claims that have long been officially approved in many jurisdictions.”
Here, of course,”unworkably high standard” just means real genuine evidence. How dare they ask for that!
Enforcement of the law
Article 19 of the Unfair Trading regulations says
19. —(1) It shall be the duty of every enforcement authority to enforce these Regulations.
(2) Where the enforcement authority is a local weights and measures authority the duty referred to in paragraph (1) shall apply to the enforcement of these Regulations within the authority’s area.
Nevertheless, enforcement is undoubtedly a weak point at the moment. The UK is obliged to enforce these laws, but at the moment it is not doing so effectively.
A letter in the BMJ from Rose & Garrow describes two complaints under the legislation in which it appears that a Trading Standards office failed to enforce the law. They comment
” . . . member states are obliged not only to enact it as national legislation but to enforce it. The evidence that the government has provided adequate resources for enforcement, in the form of staff and their proper training, is not convincing. The media, and especially the internet, are replete with false claims about health care, and sick people need protection. All EU citizens have the right to complain to the EU Commission if their government fails to provide that protection.”
This is not a good start. A lawyer has pointed out to me
“that it can sometimes be very difficult to get Trading Standards or the OFT to take an interest in something that they don’t fully understand. I think that if it doesn’t immediately leap out at them as being false (e.g “these pills cure all forms of cancer”) then it’s going to be extremely difficult. To be fair, neither Trading Standards nor the OFT were ever intended to be medical regulators and they have limited resources available to them. The new Regulations are a useful new weapon in the fight against quackery, but they are no substitute for proper regulation.”
Trading Standards originated in Weights and Measures. It was their job to check that your pint of beer was really a pint. Now they are being expected to judge medical controversies. Either they will need more people and more training, or responsibility for enforcement of the law should be transferred to some more appropriate agency (though one hesitates to suggest the MHRA after their recent pathetic performance in this area).
Who can be prosecuted?
Any “trader”, a person or a company. There is no need to have actually bought anything, and no need to have suffered actual harm. In fact there is no need for there to be a complainant at all. Trading standards officers can act on their own. But there must be a commercial element. It’s unlikely that simply preaching nonsense would be sufficient to get you prosecuted, so the Prince of Wales is, sadly, probably safe.
Universities who teach that “Amethysts emit high Yin energy” make an interesting case. They charge fees and in return they are “falsely claiming that a product is able to cure illnesses”.
In my view they are behaving illegally, but we shan’t know until a university is taken to court. Watch this space.
The fact remains that the UK is obliged to enforce the law and presumably it will do so eventually. When it does, alternative medicine will have to change very radically. If it were prevented from making false claims, there would be very little of it left apart from tea and sympathy
Follow-up
New Zealand must have similar laws.
Just as I was about to post this I found that in New Zealand a
“couple who sold homeopathic remedies claiming to cure bird flu, herpes and Sars (severe acute respiratory syndrome) have been convicted of breaching the Fair Trading Act.”
They were ordered to pay fines and court costs totalling $23,400.
A clarification form Douglas McLachlan
On the difficult question of who must prove what, Douglas McLachlan, who wrote Has The UK Quietly Outlawed “Alternative” Medicine?, has kindly sent the following clarification.
“I would agree that it is still for the prosecution to prove that the trader committed the offence beyond a reasonable doubt, and that burden of proof is always on the prosecution at the outset, but I think if a trader makes a claim regarding his product and best scientific evidence available indicates that that claim is false, then it will be on the trader to substantiate the claim in order to defend himself. How will the trader do so? Perhaps the trader might call witness after witness in court to provide anecdotal evidence of their experiences, or “experts” that support their claim – in which case it will be for the prosecution to explain the scientific method to the Judge and to convince the Judge that its Study evidence is to be preferred.
Unfortunately, once human personalities get involved things could get clouded – I could imagine a small time seller of snake oil having serious difficulty, but a well funded homeopathy company engaging smart lawyers to quote flawed studies and lead anecdotal evidence to muddy the waters just enough for a Judge to give the trader the benefit of the doubt. That seems to be what happens in the wider public debate, so it’s easy to envisage it happening a courtroom.”
The “average consumer”.
(3) A commercial practice is unfair if—
(a) it contravenes the requirements of professional diligence; and
(b) it materially distorts or is likely to materially distort the economic behaviour of the average consumer with regard to the product.
It seems,therefore, that what matters is whether the “average consumer” would infer from what is said that a claim was being made to cure a disease. The legal view cited by Mojo (comment #2, below) is that expressions such as “can be used to treat” or “can help with” would be considered by the average consumer as implying successful treatment or cure.
The drugstore detox delusion. A nice analysis “detox” at .Science-based Pharmacy
Herbal medicine is, unlike homeopathy, not ridiculous, It is merely Pharmacology, as practised up to circa 1900. Whereas good trials have now shown acupuncture to be sham and homeopathy to be a placebo, there has been very little good research on herbs.
Most herbalism could fairly be described giving to sick patients an unknown dose of a substance with unknown efficacy and unknown safety.
How odd, then, to visit the Royal Society of Medicine to be greeted thus.
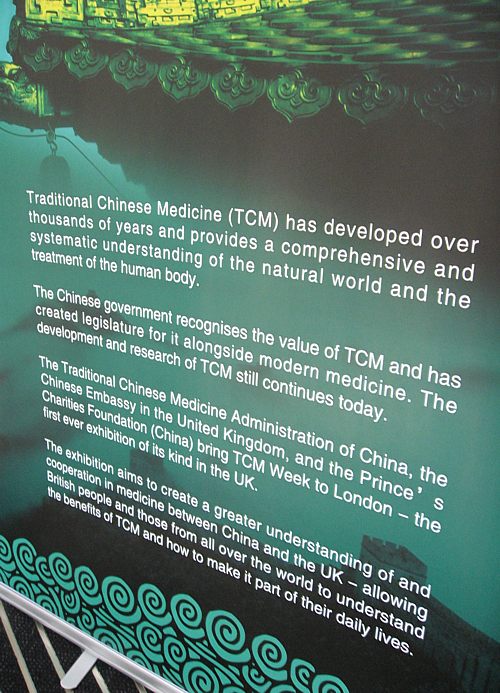
Just look at the words!
“Traditional Chinese Medicine (TCM) has developed over thousands of years”
That’s partly true
“and provides a comprehensive and systematic understanding of the natural world and the treatment of the human body.”
and that is total nonsense. TCM provides no understanding and virtually none of it is known to be useful for treating anything.
| Another poster at the RSM exhibition provides some of the explanation. What on earth, one wonders, do they mean by “making efforts to modernise TCM “? So far, the idea of modernising TCM doesn’t seem to include any great effort to find out if it works. Much of the promotion of TCM seems to be not so much ‘ancient wisdom’, but modern nationalist propaganda by the Chinese government. |
 |
The history is fascinating, but you won’t learn it from the posters on display at the exhibition.
“The Daoguang emperor though it [acupuncture] was a barrier to medical progress and removed it from the curriculum of the Imperial Medical Institute,”
“By the start of the twentieth century, acupuncture was extinct in the West and dormant in the East. It might have fallen out of favour permanently, but it suddenly experienced a revival in 1949 as a direct result of the communist revolution and the establishment of the People’s Republic of China. Chairman Mao Tse-tung engineered a resurgence in traditional Chinese medicine, which included not just acupuncture but also Chinese herbal medicine and other therapies ”
“His motivation was partly ideological, inasmuch as he wanted to reinforce a sense of national pride in Chinese medicine. However he was also driven by necessity. He had promised to deliver affordable healthcare .. . . ”
“Mao did not care whether traditional Chinese medicine worked, as long as he could keep the masses contented. In fact, his personal physician, Zhisui Li, wrote a memoir entitled ‘The Private Life of Chairman Mao’, in which he quoted Mao as saying”
“Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine.” “
Singh & Ernst Trick or Treatmant, page 46.
Or, as put more succinctly by Shapiro
“You would never know that TCM was fashioned in the twentieth century, as we shall see, from a ragbag of therapies in post-revolutionary China.”
Rose Shapiro, Suckers, how alternative medicine makes fools of us all.
Why is the Royal Society of Medicine allowing such mendacious posters? As it happens, I and a friend were visiting the RSM to see their Academic Dean, with a view to finding out why the RSM had failed to take any public position on alternative medicine. The answer appeared to be money, and that was the answer to why the TCM exhibition was being held on their premises too. The Dean no more believed in TCM than we did, but, well, they need the income. He pointed out (looking suitably sheepish) that the address given for the exhibition was not the RSM, but Number 1 Wimpole Street (that, of course, is also the address of the RSM).
Ah, so that’s OK then.
It has to be said that the RSM isn’t alone in its spineless attitude. Both the British Medical Association (BMA) and the Royal College of General Practitioners (RCGP) have failed to make any clear condemnation of mystical medicine. This is in stark contrast to just about every relevant scientific society (here is a summary).
It is a mystery to me why much of medicine should still be dominated by a mindset that seems to have lagged 200 years behind every other science. Perhaps medicine is just too complicated.
UCL Hospitals’ skeleton in the cupboard
Make no mistake, University College London Hospital is top class. The UCLH Trust. runs seven hospitals All but one of them are excellent. But in 2002 the Royal London Homeopathic Hospital was acquired as part of the UCLH group, to the intense embarrassment of UCL scientists.
Let’s start with the good bit. Usually I don’t like anecdotes, so just think of this as a vote of thanks, not evidence.
A personal history of UCH
I owe UCLH a lot personally. On December 13th 1984, my wife had
a subarachnoid haemorrhage when she was seven months pregnant. After misdiagnosis at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millilmetre from the pituitary on the other. It was a bit tricky but I think we got it”.
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds).. Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. | 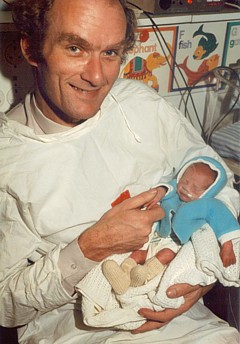
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album.. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. Heaven knows what it would have cost in the USA.
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew playing cricket in Bangladesh, Feb 2005. |
But now the the less desirable side of UCLH
Herbs and homeopaths at UCLH
| Recently I was sent the UCLH Annual Review 2007 – 2008. There was a lot of good stuff in it and worth a read despite there being too much hyperbole and too many pictures of men in dark suits. But buried among all the high tech stuff, what do we find but an advertisement for 1900-style pharmacology in the form of the herbal clinic at the Royal London Homeopathic Hospital, accompanied by a load of utterly inaccurate information from the TV botanist, David Bellamy. Take, for example, the claim about Devil’s Claw for osteoarthritis. Even alternative medicine advocates said “The authors concluded that there are insufficient high-quality trials to determine the safety and efficacy of Devil’s Claw (Harpagophytum procumbens) in the treatment of osteoarthritis, and that definitive trials are needed.”
Reading between the lines, I’d guess that the opening of this clinic has a subtext. It is well known that funding for homeopathy has dried up (partly as a result of our letter to NHS Trusts that appeared in the There have been problems before with the herbal activities at the RLHH before (see Conflicts of Interest at the Homeopathic Hospital). It appeared that the Khans, who run the Marigold homeopathic podiatry clinic (no, seriously, it is real) were largely prescribing a herbal product that was made by their own company. without even the hospital trust, never mind the patients, being made aware of it. In normal medicine this would be regarded as a rather serious offence, but as far as I know, nothing was ever done about it. |
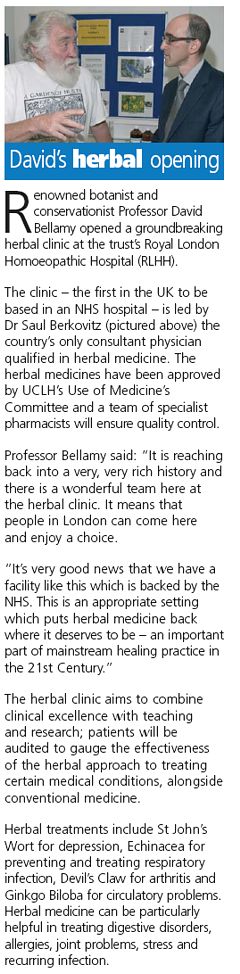 |
The ethics of alternative medicine are truly one of life’s great mysteries.
Reading further in the annual review, we come to the page about the RLHH. The homeopathy side must really have run down because it seems to have diversified into selling cosmetics and groceries. That sounds like desperation.

Good heavens, they sell “chemical-free sun cream”. One wonders what it can be made of, if not chemicals. This is the language of low-grade advertising agencies, not what one expects from an NHS hospital trust.
But next to this there is a much more interesting item. Just look at the last sentence.
I wonder if this could possibly have anything to do with the fact that Michael Baum and I visited the Trust headquarters in August 2006 to propose that the RLHH might be turned into a centre of supportive and palliative care? It would be nice to think so. But it seems they haven’t gone nearly far enough yet. If all they do is replace the waning homeopathy We know they are under pressure from their royal patrons, but that, in a constitutional monarchy, is simply not acceptable. |
 |
Michael Baum is a cancer surgeon who has taken a particular interest in palliative and supportive care. He is someone whose views should be taken seriously. He is also the author of the magnificent “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong” Here is a quotation from that letter. The UCLH Trust should bear it in mind.
| The power of my authority comes with a knowledge built on 40 years of study and 25 years of active involvement in cancer research. I’m sensitive to the danger of abusing this power and, as a last resort, I know that the General Medical Council (GMC) is watching over my shoulder to ensure I respect a code of conduct with a duty of care that respects patients’ dignity and privacy and reminds me that my personal beliefs should not prejudice my advice. Your power and authority rest on an accident of birth. Furthermore, your public utterances are worthy of four pages, whereas, if lucky, I might warrant one. I don’t begrudge you that authority and we probably share many opinions about art and architecture, but I do beg you to exercise your power with extreme caution when advising patients with life threatening diseases to embrace unproven therapies. There is no equivalent of the GMC for the monarchy, so it is left either to sensational journalism or, more rarely, to the quiet voice of loyal subjects such as myself to warn you that you may have overstepped the mark. It is in the nature of your world to be surrounded by sycophants (including members of the medical establishment hungry for their mention in the Queen’s birthday honours list) who constantly reinforce what they assume are your prejudices. Sir, they patronise you! Allow me this chastisement. |
Follow-up
The photo album chronicling the birth of my son, is really just for family and friends, but at least one blog picked up on the wider significance.
After the announcement that the University of Central Lancashire (Uclan) was suspending its homeopathy “BSc” course, it seems that their vice chancellor has listened to the pressure, both internal and external, to stop bringing his university into disrepute.
An internal review of all their courses in alternative medicine was announced shortly after the course closure. Congratulations to Malcolm McVicar for grasping the nettle at last. Let’s hope other universities follow his example soon.
I have acquired, indirectly, a copy of the announcement of the welcome news.
| Homeopathy, Herbalism and cupuncture Concern has been expressed by some colleagues as to whether the University should offer courses in homeopathy, Herbalism and Acupuncture. Therefore, to facilitate proper discussion on this matter I have set up a working party to review the issues. I have asked Eileen Martin, Pro Vice-Chancellor and Dean of the Faculty of Health, to lead this working party and report to me as soon as possible. Whilst the review is taking place, we need to recognise that there are students and staff studying and teaching on these courses which have satisfied the University’s quality assurance procedures and been duly validated. I would therefore ask that colleagues would refrain from comment or speculation which would cause concern to these students and staff. Staff who wish to express their views on this issue should direct these to Eileen Martin, by the end of September. Regards Malcolm McVicar Vice-Chancellor |
Times Higher Education today reports
“The University of Central Lancashire is to review all its courses in homoeopathy, herbalism and acupuncture after some staff said it should not be offering degrees in “quackery”, Times Higher Education has learnt.
A university spokesman said: “As a university we value and practise transparency and tolerance and welcome all academic viewpoints.”
(Later, an almost identical version of the story ran on the Times Online.)
So far, so good. But of course the outcome of a committee depends entirely on who is appointed to it. Quite often such committees do no more than provide an internal whitewash.
It does seem a bit odd to appoint as chair the dean of the faculty where all these course are run, and presumably generate income. Eileen Martin has often appeared to be proud of them in the past. Furthermore, the whole investigation will (or should) turn on the assessment of evidence. It needs some knowledge of the design of clinical trials and their statistical analysis, As far as I can see, Ms Martin has essentially no research publications whatsoever.
I also worry about a bit about “satisfied the University’s quality assurance procedures and been duly validated”. One point of the investigation should be recognise frankly that the validation process is entirely circular, and consequently worth next to nothing. It must be hard for a vice-chancellor to admit that, but it will be an essential step in restoring confidence in Uclan.
Let’s not prejudge though. If there are enough good scientists on the committee, the result will be good.
I hope that transparency extends to letting us know who will be doing the judging. Everything depends on that.
Follow-up
Well well, there’s a coincidence, Once again, the week after a there is an announcement about degrees in witchcraft, what should pop up again in the column of the inimitable Laurie Taylor in THE. The University of Poppleton’s own Department of Palmistry.
| Letter to the editor
Dear Sir I was shocked to see yet another scurrilous attack upon the work of my department in The Poppletonian. Although Palmistry is in its early days as an academic discipline it cannot hope to progress while there are people like your correspondent who insist on referring to it as “a load of superstitious nonsense which doesn’t deserve a place on the end of the pier let alone in a university”. A large number of people claim to have derived considerable benefit from learning about life lines, head lines and heart lines and the role of the six major mounts in predicting their future. All of us in the Palmistry Department believe it vitally important that these claims are rigorously examined. How else can science advance? Yours sincerely, |
The Times today has given s good showing for my comment piece. It gives the case against following the advice of the Pittilo report. It simply makes no sense to have government regulation of acupuncture, herbal medicine, traditional Chinese medicine until such time as there is evidence that they work. It makes even less sense to have BSc degrees in them. The Department of Health should have more sense that to use the Prince of Wales as its scientific advisor.
Let’s hope that the recent example set by the University of Central Lancashire is the start of trend for vice-chancellors to appreciate that running such degrees brings their universities into disrepute.
I can only apologise for the dreadful title that The Times’ sub-editors put on the piece, My original title was
A bad report for the vice chancellor
The Pittilo report to the Department of Health will endanger the public and corrupt universities. There is a better way.
I like that much better than “Regulate quack nedicine? I feel sick”.
But, oh dear, the picture that I sent them is on the left, but what appeared is on the right. Spot the difference.
 |
 |
Well now, at least, I can feel I have something in common with Isambard Kingdom Brunel.
Follow-up
It so happens that Professor Pittilo wrote a letter to Times Higher Education this week. I fear that it provided a yet more evidence that he hasn’t really quite got the hang of evidence.
The Lancashire Evening Post catches up with the UCLan story, two days after you read it here.
A reply from Professor Pittilo
This response to the op-ed of 29th August appeared as a letter
in the Times on Sept 2.
| Public health needs protection
Regulation of acupuncture and herbal medicine has been subject to much scrutiny Sir, Professor Colquhoun’s campaign to discredit our report (“Regulate quack medicine? I feel sick,” Aug 29) is in danger of placing public health at risk. He is entitled to challenge existing evidence for the effectiveness of complementary and alternative medicine (CAM) but fails to acknowledge the key recommendation from the steering group on the essential need to demonstrate efficacy, safety and quality assurance as a prerequisite for NHS funding. Professor Colquhoun dismisses CAM because of the absence of a rigorous scientific foundation and he asserts that to teach and practise it is unethical. Survey data consistently demonstrates very high demand for CAM with one report estimating that 22 million visits involving 10.6 per cent of the population in England alone occurred in 2008. This demand is one reason why his alternative model of trade law enforcement will not work. He may argue that these people are uncritical recipients of nonsense, but data from the Medicines and Healthcare products Regulatory Agency confirm that they are at significant risk from poor practice. It is essential that we protect the public by implementing statutory regulation alongside demanding evidence of efficacy. Professor Colquhoun’s resistance to the teaching of science to CAM practitioners will do little to help them to critically evaluate effectiveness. Professor Michael Pittilo Chair of the Department of Health Steering Group |
And Pittilo wrote in similar vein to Times Higher Education.
Science vital to health study28 August 2008 Your feature on some members of staff at the University of Central Lancashire attacking science degrees in complementary and alternative medicine (“Staff attack science degrees in alternative health”, 7 August) raises a number of concerns. It is up to any university, taking account of the expert views of staff and external peer review, to determine the appropriate title and award for any degree. It is encouraging to note from the feature that new courses The recent report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and other Traditional Medicine There is no doubt that courses that provide a solid scientific foundation will greatly assist CAM practitioners in establishing evidence-based practice. It would be most unfortunate if the reported resistance to degree titles led to those wishing to practise acupuncture or herbal medicine receiving less hard science than they might have. To say that acupuncture and herbal medicine degrees have no academic justification appears arrogant in the extreme. Although it is certainly true that some content may not be scientific, this does not invalidate the legitimacy of these courses at degree level, a fact borne out by their successful validation in a number of universities. R. Michael Pittilo, Principal and vice-chancellor, The Robert Gordon University. |
This one got excellent responses from Kevin Smith (University of Abertay, Dundee), and from Peter J. Brophy (Professor of veterinary anatomy and cell biology University of Edinburgh). This was my comment to THE
There are a few very obvious responses to Professor Pittilo’s letter
For many alternative therapies the “philosophy” is simply incompatible with science. One obvious example is homeopathy. On Mondays and Wednesdays (science days) the students will be required to learn that response increases with dose. On Tuesdays and Thursdays will be taught the opposite. But for the exam they must reproduce only the latter (nonsensical) idea because their aim is to get a job as a homeopath. That makes nonsense of the idea of a university.
This seems to constitute a recognition that the evidence is still very inadequate. The time to start degrees, and the time to give official government recognition, is after the evidence is in, not before. What happens if you start degrees and then find that the subject is so much nonsense? Well, that has already happened in several areas of course. But the people who accredit the course and who act as external examiners just happen to be fervent believers in that nonsense, so all appears to be well (to bean counters anyway).
There is, as it happens, a great deal of evidence now about acupuncture, but the authors of the report do not seem to be aware of it. I recommend Barker Bausell’s book on the topic. If students are educated science, like what constitutes evidence, and our current understanding of words like “energy”, they would have to disavow the subject that there are supposed to training to practise
No, it is not a matter of arrogance, just a matter of careful attention to the evidence. Attention to evidence was notably absent in Prof Pittilo’s report, perhaps because his committee consisted entirely of people who earn their living from the subjects they were supposed to be assessing.
I have had the misfortune to have waded through a mound of such validation documents. The one thing they never consider is whether the treatment works. Sad to say, these validations are not worth the paper they are written on. |
The first major victory in the battle for the integrity of universities seems to have been won. This email was sent by Kate Chatfield who is module leader for the “BSc” in homeopathic medicine at the University of Central Lancashire (UCLAN).
| from Kate Chatfield…
Dear All, It’s a sad day for us here at UCLan because we have taken the decision not to run a first year this year due to low recruitment. The course will be put ‘on hold’ for this year and next until we see what happens with the general climate. Fortunately our masters course is thriving and we have been asked to focus upon this area and homeopathy research for the time being. Of late UCLan has been the subject of many attacks by the anti-homeopathy league. Colquhoun et al have kept the university lawyers and us quite fruitlessly busy by making claims for very detailed course information under the Freedom of Information Act. The latest demand is for 32 identified lesson plans with teaching notes, power points, handouts etc. The relentless attacks have taken their toll and it appears that they have won this small victory. The university has been very clear that this decision has been taken solely on the grounds of poor educational experience and is nothing to do with the current furore. They continue to be supportive of us and our efforts. Best wishes Kate and Jean |
There is some background here. In July 2006 I made a request to UCLAN under the Freedom of Information Act 2000, in which I asked to see some of their teaching materials. I appealed to UCLAN but Professor Patrick McGhee, Deputy Vice-Chancellor (Academic), also turned down two appeals. A letter sent directly to Professor Malcolm McVicar, vice-chancellor and president of UCLAN, failed to elicit the courtesy of a reply (standard practice I’m afraid, when a vice chancellor is faced with a difficult question). (Ironically, McVicar lists one of his interests as “health policy”.) So then I appealed to the Office of the Information Commissioner, in November 2006. Recently the case got to the top of the pile, and a judgment is expected any moment now.
Kate Chatfield’s letter to her colleagues is interesting. She describes a request ro see some of her teaching materials as an “attack”. If someone asks to see my teaching materials, I am rather flattered, and I send them. Is she not proud of what she teaches? Why all the secrecy? After all, you, the taxpayer, are paying for this stuff to be taught, so why should you not be able see it? Or is the problem that she feels that the “alternative reality” in which homeopaths live is just too complicated for mortals to grasp? Perhaps this attitude should be interpreted as flattering to the general public, because somewhere deep down she knows that the public will be able to spot gobbledygook when they see it. The revelation that the University of Westminster teaches first year undergraduates the “amethysts emit high yin energy” didn’t help their academic reputation much either.
Much credit for this decision must go also to the pressure from the many good academics at UCLAN. When it was revealed recently that UCLAN intended to open yet more courses in forms of medicine that are disproved or unproven, they naturally felt that their university was being brought into disrepute. Opposition to plans to introduce new “degrees” in acupuncture and Chinese herbal medicine were exposed in Times Higher Education recently. It particular, great credit must go to Dr Michael Eslea from UCLAN’s Psychology department. His open letter to his vice-chancellor is an example of scientific integrity in action.
The abandonment of this degree in medicines that contain no medicine is a small victory for common sense, for science and for the integrity of universities. Sadly, there is still a long way to go.
It is my understanding that ‘bringing the university into disrepute’ is a serious offence. Please note, vice-chancellor.
A few more judgments like that to suspend your homeopathy degree could work wonders for your reputation.
The follow-up
Watch this space.
The Guardian was quick off the mark -this story appeared on their education web site within 3 hours of my posting it “Homeopathy degrees suspended after criticism” by Anthea Lipsett. My comment there disappeared for a while because the Guardian legal people misunderstood the meaning of the last sentence. It’s back now, with blame allocated unambiguously to the vice-chancellors of the 16 or so universities who run this sort of course.
UCLAN’s web site seems to need some updating. The “BSc” in homeopathic medicine is still advertised there. as of 28 August.
UCLAN’s best ally. Dr Michael Eslea, has had some publicity for his attempts to rescue his university’s reputation. The story appeared in the “High Principals” column of Private Eye (Issue 1217, Aug 22, 2008). It also appeared in his local paper, the Lancashire Evening Post.
The Lancashire Evening Post catches up with homeopathy suspension story, two days after you read it here. But the UCLAN web site still advertises it.
