It makes a nice change to be able to compliment an official government report.
|
Ever since the House of Lords report in 2000, the government has been vacillating about what should be done about herbalists. At the moment both western herbalists and traditional Chinese medicine (TCM) are essentially unregulated. Many (but not all) herbalists have been pushing for statutory regulation, which they see as government endorsement. It would give them a status like the General Medical Council. |
|
A new report has ruled out this possibility, for very good reasons [download local copy].
Back story (abridged!)
My involvement began with the publication in 2008 of a report on the Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine . That led to my post, A very bad report: gamma minus for the vice-chancellor. The report was chaired by the late Professor Michael Pittilo BSc PhD CBiol FIBiol FIBMS FRSH FLS FRSA, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The membership of the group consisted entirely of quacks and the vice -chancellor’s university ran a course in homeopathy (now closed).
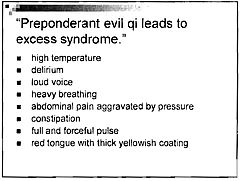
The Pittilo report recommended statutory regulation and "The threshold entry route to the register will normally be through a Bachelor degree with Honours". It ignored entirely the little problem that you can’t run a BSc degree in a subject that’s almost entirely devoid of evidence. It said, for example that acupuncturists must understand " yin/yang, 5 elements/phases, eight principles, cyclical rhythms, qi ,blood and body fluids". But of course there is nothing to "understand"! They are all pre-scientific myths. This “training dilemma” was pointed out in one of my earliest posts, You’d think it was obvious, but nonetheless the then Labour government seemed to take this absurd report seriously.
In 2009 a consultation was held on the Pittilo report. I and many of my friends spent a lot of time pointing out the obvious. Eventually the problem was again kicked into the long grass.
The THR scheme
Meanwhile European regulations caused the creation of the Traditional Herbal Registration (THR) scheme. It’s run by the Medicines and Healthcare products Regulatory Authority (MHRA). This makes it legal to put totally misleading claims on labels of herbal concoctions, as long as they are registered with THR, They also get an impressive-looking certification mark. All that’s needed to get THR registration is that the ‘medicines’ are not obviously toxic and they have been in use for 30 years. There is no need to supply any information whatsoever about whether they work or not. This appears to contradict directly the MHRA’s brief:
"”We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
After much effort, I elicited an admission from the MHRA that there was no reason to think that any herbal concoctions were effective, and that there was nothing to prevent them from adding a statement to say so on the label. They just chose not to do so. That’s totally irresponsible in my opinion. See Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. Over 300 herbal products have been registered under the THR scheme (a small percentage of the number of products being used). So far only one product of Tibetan medicine and one traditional Chinese medicine have been registered under THR. These are the only ones that can be sold legally now, because no herbs whatsoever have achieved full marketing authorisation -that requires good evidence of efficacy and that doesn’t exist for any herb.
The current report
Eventually, in early 2014, the Tory-led government set up yet another body, "Herbal Medicines and Practitioners Working Group " (HMPWG). My heart sank when I saw its membership (Annex A.2). The vice-chair was none other that the notorious David Tredinnick MP (Con, Bosworth). It was stuffed with people who had vested interests. I wrote to the chair and to the few members with scientific credentials to put my views to them.
But my fears were unfounded, because the report of the HMPWG was not written by the group, but by its chair only. David Walker is deputy chief medical officer and he had clearly listened. Here are some quotations.
The good thing about the European laws is that
"This legislation effectively banned the importation and sale of large-scale manufactured herbal medicine products. This step severely limited the scope of some herbal practitioners to continue practising, particularly those from the Traditional Chinese Medicine (TCM) and Ayurvedic traditions."
The biggest loophole is that
"At present under UK law it is permitted for a herbal practitioner to see individual patients, offer diagnoses and prepare herbal treatments on their own premises, as long as these preparations do not contain banned or restricted substances. This is unchanged by the Traditional Herbal Medicinal Products Directive. "
Walker recognised frankly that there is essentially no good evidence that any herb, western or Chinese, works well enough to make an acceptable treatment. And importantly he, unlike Pittilo, realised that this precludes statutory regulation.
"There are a small number of studies indicating benefit from herbal medicine in a limited range of conditions but the majority of herbal medicine practice is not supported by good quality evidence. A great deal of international, primary research is of poor quality. "
"ts. Herbal medicine practice is therefore currently based upon traditional practice rather than science. It is difficult to differentiate good practice from poor practice on the basis of this evidence in a way that could establish standards for statutory regulation"
The second problem was the harms done by herbs. Herbalists, western and Chinese, have no satisfactory way of reporting side effects
" . . . there is very limited understanding of the risks to patient safety from herbal medicines and herbal practice. A review of safety data was commissioned from HMAC as part of this review. This review identified many anecdotal reports and case studies but little systematically collected data. Most herbal medicine products have not been through the rigorous licensing process that is required of conventional pharmaceutical products to establish their safety and efficacy. Indeed, only a small proportion have even been subject to the less rigorous Traditional Herbal Registration (THR) process. "
"The anecdotal evidence of risk to patients from herbal products in the safety review highlighted the prominence of manufactured herbal medicines in the high profile serious incidents which have been reported in recent years. Many of these reports relate to harm thought to be caused by industrially manufactured herbal products which contained either dangerous herbs, the wrong constituents, toxic contaminants or adulterants. All such industrially manufactured products are now only available under European regulations if their safety is assured through MHRA licensing or THR
accreditation; and specific dangerous herbs have been banned under UK law. This has weakened the case for introduction of statutory regulation as a further safety measure. "
Then Walker identified correctly the training dilemma. Although it seems obvious, this is a big advance for a government document. Degrees that teach nonsense are not good training: they are miseducation.
"The third issue is the identification of educational standards for training practitioners and the benchmarking of standards for accrediting practitioners. With no good data on efficacy or safety, it is difficult for practitioners and patients to understand or quantify the potential benefits and risks of a proposed therapeutic intervention. Training programmes could accredit knowledge and skills in some areas including pharmacology and physiology, professional ethics and infection control but without a credible evidence base relating to the safety and effectiveness of herbal medicine it is hard to see how they could form the basis of accreditation in this field of practice.
There are a number of educational university programmes offering courses in herbal medicine although the number has declined in recent years. Some of these courses are accredited by practitioner organisations which is a potential governance risk as the accreditation may be based on benchmarks established by tradition and custom rather than science.
"
"The herbal medicine sector is in a dilemma" is Walker’s conclusion.
"Some practitioners would like to continue to practise as
they do now, with no further regulation, and accept that their practice is based on tradition and personal experience rather than empirical science. The logical consequence of adopting this form of practice is that we should take a precautionary approach in order to ensure public safety. The public should be protected through consumer legislation to prevent false claims, restricting the use of herbal products which are known to be hazardous to health"
The problem with this is, if course, is that although there is plenty of law, it’s rarely enforced : see Most alternative medicine is illegal Trading Standards very rarely enforce the Consumer Protection Regulations (2008) but Walker is too diplomatic to mention that fact.
"The herbals sector must recognise that its overall approach (including the rationale for use of products and methods of treatment, education and training, and interaction with the NHS) needs to be more science and evidence based if in order to be established as a profession on the same basis as other groups that are statutorily regulated."
So what happens next?
In the short term nothing will happen.
The main mistake has been avoided: there wil be no statutory regulation.
The other options are (a) do nothing, or (b) go for accreditation of a voluntary register (AR) by the Professional Standards Authority for Health and Social Care (PSA). Walker ends up recommending the latter, but only after a lot more work (see pages 28-29 of report). Of particular interest is recommendation 5.
"As a first step it would be helpful for the sector organisations to develop an umbrella voluntary register that could support the development of standards and begin to collaborate on the collection of safety data and the establishment of an academic infrastructure to develop training and research. This voluntary register could in due course seek accreditation from the Professional Standards Authority for Health and Social Care (PSA)."
So it looks as though nothing will happen for a long time, and herbalists and TCM may end up with the utterly ineffectual PSA. After all, the PSA have accredited voluntary registers of homeopaths, so clearly nothing is too delusional for them. It’s very obvious that, unlike Walker, the PSA are quite happy to ignore the training dilemma.
Omissions from the report
Good though this report is, by Department of Health standards, it omits some important points.
Endangered species and animal cruelty aren’t mentioned in the report. Traditional Chinese medicine, and its variants, are responsible for the near-extinction of rhinoceros, tiger and other species because of the superstitious belief that they have medicinal value. It’s not uncommon to find animal parts in Chinese medicines sold in the UK despite it being illegal
And the unspeakably cruel practice of farming bears to collect bile is a direct consequence of TCM.

A bile bear in a “crush cage” on Huizhou Farm, China (Wikipedia)
Statutory regulation of Chiropractors
The same arguments used in Walker’s report to deny statutory regulation of herbalism, would undoubtedly lead to denial of statutory regulation of chiropractors. The General Chiropractic Council was established in 1994, and has a status that’s the same as the General Medical Council. That was a bad mistake. The GCC has not protected the public, in fact it has acted as an advertising agency for chiropractic quackery.
Perhaps Prof. Walker should be asked to review the matter.
Follow-up
You can also read minutes of the HMPWG meetings (and here). But, as usual, all the interesting controversies have been sanitised.
Edzard Ernst has also commented on this topic: Once again: the regulation of nonsense will generate nonsense – the case of UK herbalists.


[…] By David Colquhoun […]
“Herbalists, western and Chinese, have no satisfactory way of reporting side effects.” There is no reason why any prescriber (e.g. a herbalist) or a patient should not report a suspected adverse reaction, for example (in the UK) to the MHRA on a yellow card (https://yellowcard.mhra.gov.uk). The MHRA specifically invites reports on medicines, vaccines, and herbal and homoeopathic remedies, medical devices, defective medicines, and counterfeit or fake medicines or medical devices. There are other ways; for example, writing a report for a case reports journal. Whether prescribers of herbal medicines or their patients will take these opportunities, even if they recognize adverse events as suspected adverse reactions, is another matter.
It would be worth mentioning in this sort of discussion the case of the aristolochia, not only because of the ancient and instructive historical background, but also because the fatal risks of mis-identification and cross-contamination should make suspect any herb that hasn’t gone through extensive chemical quality control.
There’s an iarc monograph http://monographs.iarc.fr/ENG/Monographs/vol82/index.php. There is also plenty of information on the web about the dreadful Balkan ‘epidemic’ and how difficult it was to find the cause. The aristolochic acids are also good examples of how nasty natural chemicals can be; they look like the sort of thing you might get by nitrating coal tar.
Yes the MHRAhas issued many warnings about the dangers of Chinese herbs, apart from Aristolochia, others are dangerous too, for example those that contain lei gong teng (tripterygium wilfordii), which carry risks of serious side effects on fertility, the liver, kidneys, immune system, blood, and heart.
And there have also been many reports of contamination of herbs with lead, arsenic as well as with normal prescription drugs (in totally unknown doses)
. If you buy herbs from the many Chinese medicine shops that have strung up on every high street, you are taking your life in your hands.
“good evidence of efficacy and that doesn’t exist for any herb”
That’s going a bit far, I think. What I would agree is that such evidence is not to be found within herbalism, but rather in pharmacognosy and phytotherapy.
Luke Devlin
I’m afraid that it isn’t going too far. I suggest that you look at the NIH site that deals with question
https://nccih.nih.gov/health/herbsataglance.htm
That is written by people who are sympathetic to alternative medicine, but if you look at the “what the science says” section, you’ll find that none of them can be recommended. That’s why not a single herbal preparation has marketing authorisation in the UK.
Pharmacognosy (or phytotherapy as it has been re-branded) is a branch of botany. It doesn’t deal with efficacy and has always been over-optimistic about what can be achieved with herbs.
David Colquhoun,
That looks like a useful reference.
To provide a balanced view that illustrates why eating the plants as such is not the way to go, we could also do with a list of the numerous plant constituents and other natural products that have made it into medical practice, and perhaps another list of those that have been tested and rejected. Useful information would include safe dosage limits and the consequences of exceeding them, as well as reasons why synthetic replacements are preferred in some cases.
In a public debate it’s important to recall of the historical context; until a century or so ago people who could afford them had only plant products and some more or less toxic inorganics.
Yes exactly. And until a century ago people died young. There was nothing curative until the sulphonamides in the 1930s, and shortly afterwords, antibiotics. It’s a chastening thought that most effective medicines have been invented in my lifetime.
I’m not aware of any herb that has been used with much benefit. I can just remember tincture if digitalis but this was standardised by biological assay, so you knew what dose was being given, So it wasn’t just eating the plant. That would be incredibly dangerous because the cardiac glycosides contained in foxgloves have a narrow margin of safety. Much safer to use the accurate dose in a tablet that contains pure digoxin. You might be interested in a bit that I wrote about this in 2006 http://www.dcscience.net/2006/02/24/plants-as-medicines/
Atropine (from Belladonna) and tubocurarine (from arrow poison) and cocaine (for local anaesthesia) have been used in medicine, but all have both are now replaced by better and safer synthetic alternatives.
The history is fascinating, but it’s largely a history of early death. There is, sad to day, much truth in my Patients’ Guide, which defined
[…] In fact, after 15 years of wrangling, the promised recognition of herbalism by statutory regulation never happened. One is reminded of the time that an equally-clueless minister, Lord (Phillip) Hunt, referred to […]