Royal Pharmaceutical Society

The General Pharmaceutical Council (GPhC) has been the statutory body responsible for the regulation of pharmacy since 2010. It’s status is similar to that of the GMC and. heaven help us, the GCC. Before that the regulator was the same as the professional body, the Royal Pharmaceutical Society of Great Britain (RPS). The RPS proved to be as useless as most other regulators, as documented in detail in my 2008 post, At around the time it stopped being a regulator, the RPS started to condemn quackery more effectively, but by then it had lost the power to do much about it (I hope the latter wasn’t the cause of the former). The body that could do something, the GPhC has done essentially nothing. as described in this post.
I did a 2 year apprenticeship in Timothy White’s and Taylor’s Homeopathic (yes, really) Chemists in the 1950s.
My first degree was in pharmacy. I got my interest in pharmacology from reading Martindale’s Extra Pharmacopoeia in the shop. I soon decided that I didn’t really want to spend the rest of my life selling lipstick and Durex. The latter was quite a big seller because the Boots across the road didn’t sell contraceptives (they changed their minds in the 1960s).
In those days, we spent quite a lot of time making up (almost entirely ineffective) ‘tonics’ and ‘cough mixtures’. Now the job consists largely of counting pills. This has exacerbated the ‘chip on the shoulder’ attitude that was present even in the 1950s. For a long time now, pharmacists have wanted to become the a ‘third tier’ in the NHS, alongside GP practices and hospitals., after hospitals and doctors". . Here are a few comments on this proposition.
First let me say that I’ve met some very good and ethical pharmacists. I did a vacation job in a hospital pharmacy where the boss had an encyclopaedic knowledge of the effects and side effects of drugs, and of their dosage. His advice was often sought by doctors, and rightly so. He had no way of knowing at the time that his advice to replace barbiturates with thalidomide would lead to such a tragedy, because the evidence had been concealed by the manufacturer. Some of the problems alluded to here have already been highlighted by two excellent pharmacists, Anthony Cox and @SparkleWildfire, neither of whom work in pharmacists shops. They are absolutely spot on but they seem to be in a minority among pharmacists.
The problems seem to lie mostly in retail shops. Their shelves are laden with ineffective pills and potions. And the pharmacist has every incentive to sell them. His/her income depends on it directly if it’s a privately owned pharmacy. And his/her standing with head office depends on it in chain store pharmacies. This conflict of financial interest is the prime reason why pharmacists are not qualified to form a third tier of healthcare. The avoidance of conflicts of interest among doctors was one of the great accomplishments of the NHS. In the USA there are huge scandals when, as happens repeatedly, doctors order expensive and unnecessary treatments from which they profit. It’s no consolation that such problems are creeping back in the UK as a result of the government’s vigorous efforts to sell it off.
Here are few examples of things that have gone wrong, and who is to blame. Then I’ll consider what can be done.
Ineffective medicines
In any pharmacy you can see ineffective ‘tonics’ and ‘cough medicines’, unnecessary supplements with dishonest claims and even, heaven help us, the ultimate scam, homeopathic pills.
What’s worse, if you ask a pharmacist for advice, it’s quite likely that they’ll recommend you to buy them.
|
I was amazed to discover that a number of old-fashioned ‘tonics’ and ‘cough medicines’ still have full marketing authorisation. That’s the fault of the Medicines and Healthcare Regulatory Auhority (MHRA) who are supposed to assess efficacy and totally failed to do so, Read about that in “Some medicines that don’t work. Why doesn’t the MHRA tell us honestly?” . It’s hard to blame a pharmacist for the bad advice given by the MHRA, but a good one would tell patients to save their money. |
|
Big corporate pharmacies
Companies like Boots seem to have no interest whatsoever in ethical behaviour. All that matters is sales. They provide “(mis)educational” materials that promote nonsense They advertise ridiculous made-up claims in the newspapers, which get shot down regularly by the Advertising Standards Authority, but by that time the promotion is over so they don’t give a damn. See for example, CoQ10 scam and the ASA verdict on it. And "Lactium: more rubbish from Boots the Chemists. And a more serious problem". And "The Vitamin B scam. Don’t trust Boots"
Recently the consumer magazine Which? checked 122 High Street pharmacies. They got unsatisfactory advice from 43% of them, a disastrously bad performance for people who want to be the third tier of healthcare.
|
Even that’s probably better than my own experience. Recently, when I asked a Sainsbury’s pharmacist about a herbal treatment for prostate problems, he pointed to the MHRA’s kite mark and said it must work because the MHRA approved it -he was quite unaware that you get the THR kite mark without having to present any evidence at all about efficacy. |

|
Of course that is partly the fault of the MHRA for allowing misleading labels, but nevertheless, he should have known. See “Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me” for more on how the MHRA has betrayed its own standards.
When I’ve asked Boots’ pharmacists advice about persistent diarrhoea in an infant, saying I wanted a natural remedy, I’ve usually been guided to the homeopathic display. Only once was I told firmly that I should use rehydration not homeopathy (something every good parent knows) and when I asked that good pharmacist where she’d been educated, she said in Germany (mildly surprising given the amount of junk available in German pharmacies)
Regulators
Anthony Cox, a pharmacist who has been consistently on the side of right, says
"This is something that needs to be dealt with at a regulatory and professional body by the whole profession, and I am certain we have the majority of the UK pharmacy profession on side."
But the regulator has done nothing, and it isn’t even clear that there is a majority on his side.
At a 2009 meeting of Branch Representatives of the RPS a motion was proposed:
“…registration as a pharmacist and practice as a homeopath are not compatible, and that premises registered with the Society should not be used for the promotion of homeopathy”
Although that is obviously sensible to most people, the proposal was followed by a speaker from Leicester who thought it right to keep an open mind about Avogadro’s number and the motion was defeated. So much for the "scientists on the High Street" aspiration.
There have been two major scandals surrounding homeopathy recently. Both were revealed first by bloggers, and both came to wide notice through television programs. None were noticed by the regulators, and when they were brought to the attention of the regulator, nothing effective was done.
The malaria scandal
A lot has been wriitten about this here and on other blogs e.g. here and here. The idea that sugar pills can prevent or cure malaria is so mind-bogglingly dangerous that it was condemned by the Queen’s Homeopathic Physician, Peter Fisher. It was exposed on a BBC Newsnight programme in 2006. Watch the video.
The Gentle Art of Homeopathic Killing was an article that originally appeared on the excellent Quackometer blog produced by Andy Lewis. "The Society of Homeopaths were so outraged about one of their members flouting the code of ethics so blatantly that they took immediate action. That action was, as expected, not to do anything about the ethics breach but to threaten Andy and his hosting ISP with legal action for defamation. The article is reproduced here as a public service".
Some of the people involved in this bad advice were pharmacists, Very properly they were referred to the RPS in 2006 qnd 2009, the regulator at that time. They sat on the complaint so long that eventually the RPS was replaced by the GPhC as regulator. Nothing much has happened.
The GPhC did precisely nothing. Read their pathetic response.
Homeopathy for meningitis
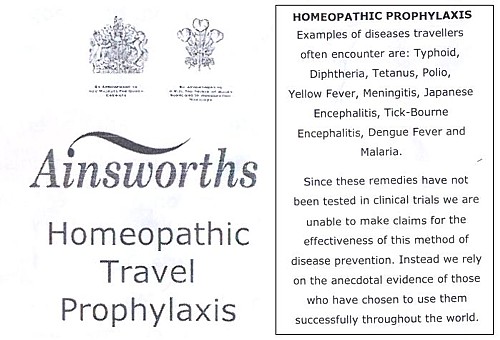
An equally murderous fraud, "homeopathic vaccines" by Ainsworth’s has long been targeted by bloggers. In January 2013, Samantha Smith made an excellent BBC South West programme about it. Watch it and get angry.
Anthony Pinkus, pharmacist at Ainsworths, has been referred to the then regulator, the RPS, in 2006 and 2009. It’s said that he took "remedial action", though there is little obvious change judged by the video above. No doubt some of the most incriminating stuff has been removed from his web site to hide it from the ASA. It’s safer to mislead people by word of mouth. Since the last video more complaints have been made to the GPhC. So far, nothing but silence.
Why doesn’t the regulator regulate?
This pamphlet is reproduced from the July 2011 Quackometer post, “Ainsworths Pharmacy: Casual Disregard for the Law“
|
It’s almost as though those royal warrants, enlarged on right, acted as a talisman that puts this dangerous company outside the grasp of regulators. I hope that the GPhC Council , and Duncan Rudkin (its chief executive and registrar), are not so worried about their knighthoods that they won’t risk upsetting the royal family, just to save patients from malaria and meningitis. Their CEO, Robert Nicholls is only a CBE so far. |
|
Another reason for their inaction might be that the GPhC Council members, and Duncan Rudkin (its chief executive and registrar), lack critical faculties. Perhaps they have not been very well educated? Many of them aren’t even pharmacists, but that curious breed of professional administrators who inhabit the vast number of quangos, tick their boxes and do harm. Or perhaps they are just more interested in protecting the income of pharmacists than in protecting their customers?
Education
The solution to most problems is education. But there is no real knowledge of how many pharmacists in the UK are educated in the critical assessment of evidence. A recent paper from the USA did not give cause for optimism. It’s discussed by the excellent US pharmacist, Scott Gavura, at Science-based medicine. The results are truly horrifying.
“Few students disagreed with any CAM therapy. There was the greatest support for vitamins and minerals (94%, mean 4.29) which could include the science-based use these products. But there was strong support for demonstrably ineffective treatments like acupuncture, with 64% agreeing it was acceptable. Even homeopathy, which any pharmacy student with basic medicinal chemistry skills ought to know is absurd, was supported by over 40% of students.”
If the numbers are similar in the UK, the results of the Which? magazine survey are not so surprising. And if they are held by the GPhC Council. their inaction is to be expected. We just don’t know, and perhaps someone should find out.
I suspect that sympathy for quackery may sometimes creep in through that old-fashioned discipline known as pharmacognosy. It is about the botany of medicinal plants, and it’s still taught, despite the fact that very few drugs are now extracted from plants. At times, it gets dangerously close to herbalism. For example, at the School of Pharmacy (now part of UCL) a book is used Fundamentals of Pharmacognosy and Phytotherapy by Michael Heinrich, Joanne Barnes, Simon Gibbons and Elizabeth M. Williamson, ot the Centre for Pharmacognosy and Phytotherapy at the School of Pharmacy. The introductory chapter says.
“TRADITIONAL CHINESE MEDICINE (TCM) The study of TCM is a mixture of myth and fact, stretching back well over 5000 years. At the time, none of the knowledge was written down, apart from primitive inscriptions of prayers for the sick on pieces of tortoise carapace and animal bones, so a mixture of superstition, symbolism and fact was passed down by word of mouth for centuries. TCM still contains very many remedies, which were selected by their symbolic significance rather than proven effects; however, this does not necessarily mean that they are all ‘quack’ remedies!”
Well, not necessarily. But as in most such books, there are good descriptions of the botany, more or less good accounts of the chemical constituents followed by uncritical lists of things that the herb might (or might not) do. The fact that even the US National Institutes of Health quackery branch, NCCAM, doesn’t claim that a single herbal treatment is useful tells you all you need to know.
Joanna Barnes is Associate Professor in Herbal Medicines, School of Pharmacy, University of Auckland, New Zealand. She has written a book, Herbal Medicines (“A useful book for learning holistic medicine”) that is desperately uncritical about the alleged theraputic effectiveness of plants. ("Simon Gibbons is on the editorial board of The Chinese Journal of Natural Medicine. Elizabeth Williamson is editor of the Journal of Phytotherapy Research, a journal that has a strong flavour of herbalism (take the infamous snoring remedy). These people aren’t quacks but they are dangerously tolerant of quacks.
The warning is in the title. "Phytotherapy" is the current euphemism for herbalism. It’s one of those red light words that tells you that what follows is unlikely to be critical. Exeter’s fantasy herbalist, Simon Mills, now describes himself as a phytotherapist. What more warning could you need?
Perhaps this explains why so many pharmacists are unworried by selling things that don’t work. Pharmacy education seems not to include much about the critical assessment of evidence. It should do.
Chemist and Druggist magazine certainly doesn’t help. It continually reinforces the idea that there is a debate about homepathy. There isn’t. And in one of its CPD modules Katherine Gascoigne says
"Homeopathic remedies are available, but are best prescribed by a homeopath"
Ms Gascoigne must be living on another planet.
Conclusions
The main conclusion from all of this is that the General Pharmaceutical Council is almost criminally negligent. It continues to allow pharmacists, Anthony Pinkus among them, to endanger lives. It fails to apply its own declared principles. The members of its Council, and Duncan Rudkin (its chief executive and registrar), are not doing their job.
Individual pharmacists vary a lot, from the superb to those who believe in quackery. Some, perhaps many, are embarrassed by the fact that their employer compels them to sell rubbish. It’s too much to expect that they’ll endanger their mortgage payments by speaking out about it, but the best ones will take you aside and explain that they can’t recommend it.
The GPhC itself is regulated by the Professional Standards Authority, the subject of my last post. We can’t expect anything sensible from them.
In the USA there is a shocking number of pharmacists who seem to believe in quackery. In the UK. nobody knows, though judging by their failure to vote against the daftest of all scams, homeopathy, there is no cause for complacency here.
It seems that there will have to be big improvements in pharmacy education before you can have much confidence in the quality of the advice that you get in a pharmacy.
Follow-up
Yesterday a talk was given at the School of Pharmacy, organised by the “The Centre for Homeopathic Education” (an oxymoron if there ever was one). The flyer had all the usual nonsense. Its mention of “Remedies & Tonics for Cancer Recovery” might well have breached the Cancer Act (1939). When I asked whether the amount received in room rental was sufficient to offest the damage to the reputation of the School of Pharmacy resulting from hosting a nutty (and possible illegal) event, I had the greatest difficulty in extracting any sort of response from the school’s director, Duncan Craig. I’m told that he considers “the policy on space rental to be a UCL management issue, rather than a matter of discussion on scientific ethics with a colleague”. Oh dear.
We have often had cause to criticise Boots Alliance, the biggest retail pharmacist in the UK, because of its deeply unethical approach to junk medicine. Click here to read the shameful litany. The problem of Boots was raised recently also by Edzard Ernst at the Hay Literary Festival. He said
“The population at large trusts Boots more than any other pharmacy, but when you look behind the smokescreen, when it comes to alternative medicines, that trust is not justified.”

Ernst accused Boots of breaching ethical guidelines drawn up by the Royal Pharmaceutical Society of Great Britain, by failing to tell customers that its homeopathic medicines contain no active ingredients and are ineffective in clinical trials.
Another chain, Lloyds Pharmacy, are just as bad. Many smaller pharmacies are no more honest when it comes to selling medicines that are known to be ineffective.
Pharmacists are fond of referring to themselves as “professionals” who are regulated by a professional body, the Royal Pharmaceutical Society of Great Britain (RPSGB). It’s natural to ask where their regulatory body stands on the question of junk medicine. So I asked them, and this is what I found.
| 17 April, 2008
I am writing an article about the role of pharmacists in giving advice about (a) alternative medicines and (b) nutritional supplements. I can find no clear statements about these topics on the RPSGB web site. Please can you give me a statement on the position of the Royal Pharmaceutical Society on these two topics. In particular, have you offered guidance to pharmacists about how to deal with the conflict of interest that arises when they can make money by selling something that they know to have no good evidence for efficacy? This question has had some publicity recently in connection with Boots’ promotion of CCoQ10 to give you “energy”, and only yesterday when the bad effects of some nutritional supplements were in the news. |
Here are some extracts from the first reply that I got from the RPSGB’s Legal and Ethical Advisory Service (emphasis is mine).
| 28 April 2008
Pharmacists must comply with the Code of Ethics and its supporting documents. Principle 5 of the Code of Ethics requires pharmacists to develop their professional knowledge and competence whilst Principle 6 requires pharmacists to be honest and trustworthy. The Code states: 5. DEVELOP YOUR PROFESSIONAL KNOWLEDGE AND COMPETENCE At all stages of your professional working life you must ensure that your knowledge, skills and performance are of a high quality, up to date and relevant to your field of practice. You must: 5.1 Maintain and improve the quality of your work by keeping your knowledge and skills up to date, evidence-based and relevant to your role and responsibilities. 5.2 Apply your knowledge and skills appropriately to your professional responsibilities. 5.3 Recognise the limits of your professional competence; practise only in those areas in which you are competent to do so and refer to others where necessary. 5.4 Undertake and maintain up-to-date evidence of continuing professional development relevant to your field of practice. 6. BE HONEST AND TRUSTWORTHY Patients, colleagues and the public at large place their trust in you as a pharmacy professional. You must behave in a way that justifies this trust and maintains the reputation of your profession. You must: 6.2 Ensure you do not abuse your professional position or exploit the vulnerability or lack of knowledge of others. 6.3 Avoid conflicts of interest and declare any personal or professional interests to those who may be affected. Do not ask for or accept gifts, inducements, hospitality or referrals that may affect, or be perceived to affect, your professional judgement. 6.4 Be accurate and impartial when teaching others and when providing or publishing information to ensure that you do not mislead others or make claims that cannot be justified. |
And, on over-the counter prescribing
| In addition the “Professional Standards and Guidance for the Sale and Supply of Medicines” document which supports the Code of Ethics states:
“2. SUPPLY OF OVER THE COUNTER (OTC) MEDICINES STANDARDS When purchasing medicines from pharmacies patients expect to be provided with high quality, relevant information in a manner they can easily understand. You must ensure that: 2.1 procedures for sales of OTC medicines enable intervention and professional advice to be given whenever this can assist the safe and effective use of medicines. Pharmacy medicines must not be accessible to the public by self-selection. |
Evidence-based? Accurate and impartial? High quality information? Effective use?
These words don’t seem to accord with Boots’ mendacious advertisements for CoQ10 (which were condemned by the ASA).
Neither does it accord with the appalling advice that I got from a Boots pharmacist about Vitamin B for vitality.
Or their bad advice on childhood diarrhoea.
Or the unspeakable nonsense of the Boots (mis)-education web site.
Then we get to the nub. This is what I was told by the RPSGB about alternative medicine (the emphasis is mine).
| 8. COMPLEMENTARY THERAPIES AND MEDICINES
STANDARDS You must ensure that you are competent in any area in which you offer advice on treatment or medicines. If you sell or supply homoeopathic or herbal medicines, or other complementary therapies, you must: 8.1 assist patients in making informed decisions by providing them with necessary and relevant information. 8.2 ensure any stock is obtained from a reputable source. 8.3 recommend a remedy only where you can be satisfied of its safety and quality, taking into account the Medicines and Healthcare products Regulatory Agency registration schemes for homoeopathic and herbal remedies.” Therefore pharmacists are required to keep their knowledge and skills up to date and provide accurate and impartial information to ensure that you do not mislead others or make claims that cannot be justified. |
It does seem very odd that “accurate and impartial information” about homeopathic pills does not include mentioning that they contain no trace of the ingredient on the label. and have been shown in clinical trials to be ineffective. These rather important bits of information are missing from both advertisements and from (in my experience) the advice given by pharmacists in the shop.
If you look carefully, though, the wording is a bit sneaky. Referring to over-the-counter medicines, the code refers to “safe and effective use of medicines”, but when it comes to alternative medicines, all mention of ‘effectiveness’ has mysteriously vanished.
So I wrote again to get clarification.
| 29 April, 2008
Thanks for that information. I’d appreciate clarification of two matters in what you sent. (1) Apropros of complementary and alternative medicine, the code says 8.3 recommend a remedy only where you can be satisfied of its safety and quality I notice that this paragraph mentions safety and quality but does not mention efficacy. Does this mean that it is considered ethical to recommend a medicine when there is no evidence of its efficacy? Apparently it does. This gets to the heart of my question and I’d appreciate a clear answer. |
This enquiry was followed by a long silence. Despite several reminders by email and by telephone nothing happened until eventually got a phone call over a month later (May 3) from David Pruce, Director of Practice & Quality Improvement, Royal Pharmaceutical Society of Great Britain. The question may be simple, but the RPSGB evidently it hard, or more likely embarrassing, to answer.
When I asked Pruce why para 8.3 does not mention effectiveness, his reply, after some circumlocution, was as follows.
Pruce: “You must assist patients in making informed decisions by providing necessary and relevant information . . . we would apply this to any medicine, the pharmacist needs to help the patient assess the risks and benefits.”
DC: “and would that include saying it doesn’t work better than placebo?”
Pruce “if there is good evidence to show that it may, but it depends on what the evidence is, what the level of evidence is, and the pharmacist’s assessment of the evidence”
DC “What’s your assessment of the evidence?”
Pruce, “I don’t think my personal assessment is relevant. I wouldn’t want to be drawn on my personal assessment”. “If a pharmacist is selling homeopathic medicines they have to assist the patient in making informed decisions”
“I don’t think we specifically talk about the efficacy of any other medicine” [DC: not true, see para 2.1, above]
“We would expect pharmacists to be making sure that what they are providing to a patient is safe and efficacious”
DC “So why doesn’t it mention efficacious in para 8.3”
Pruce “What we are trying to do with the Code of Ethics is not go down to the nth degree of detail ” . . . “there are large areas of medicine where there is an absence of data”
DC “Yes, actually homeopathy isn’t one of them. It used to be.”
Pruce. “uh, that’s again a debatable point”
DC I don’t think it’s debatable at all, if you’ve read the literature
Pruce. “well many people would debate that point” “This [homeopathy] is a controversial area where opinions are divided on it”
DC “Not informed opinions”
Pruce “Well . . . there are also a large number of people that do believe in it. We haven’t come out with a categorical statement either way.”
I came away from this deeply unsatisfactory conversation with a strong impression that the RPSGB’s Director of Practice & Quality Improvement was either not familiar with the evidence, or had been told not to say anything about it, in the absence of any official statement about alternative medicine.
I do hope that the RPSGB does not really believe that “there are also a large number of people that do believe in it” constitutes any sort of evidence.
It is high time that the RPSGB followed its own code of ethics and required, as it does for over-the-counter sales, that accurate advice should be given about “the safe and effective use of medicines”.
“The scientist on the High Street”
The RPS publishes a series of factsheets for their “Scientist in the High Street” campaign. One of these “factsheets” concerns homeopathy, [download pdf from the RPSGB]. Perhaps we can get an answer there?
Well not much. For the most part the “factsheet” just mouths the vacuous gobbledygook of homeopaths. It does recover a bit towards the end, when it says
“The methodologically “best” trials showed no effect greater than that of placebo”.
But there is no hint that this means pharmacists should not be selling homeopathic pills to sick people..
That is perhaps not surprising, because the Science Committee of the RPSGB copped out of their responsibility by getting the factsheet written by a Glasgow veterinary homeopath, Steven Kayne. You can judge his critical attitude by a paper (Isbell & Kayne, 1997) which asks whether the idea that shaking a solution increases its potency. The paper is a masterpiece of prevarication, it quotes only homeopaths and fails to come to the obvious conclusion. And it is the same Steven Kayne who wrote in Health and Homeopathy (2001)
“Homeopathy is not very good for treating bacterial infections directly, apart from cystitis that often responds to a number of medicines, including Berberis or Cantharis”.
So there is a bacterial infection that can be cured by pills that contain no medicine? Is this dangerous nonsense what the RPSGB really believes?
More unreliable advice
While waiting for the train to Cardiff on April 16th (to give a seminar at the Welsh School of Pharmacy), I amused myself by dropping into the Boots store on Paddington station.
| DC I’ve seen your advertisements for CoQ10. Can you tell me more? Will they really make me more energetic?
Boots: Yes they will, but you may have to take them for several weeks. DC. Several weeks? Boots: yes the effect develops only slowly Peers at the label and reads it out to me DC I see. Can you tell me whether there have been any trials that show it works? Boots. I don’t know. I’d have to ask. But there must be or they wouldn’t be allowed to sell it. DC. Actually there are no trials, you know Boots. Really? I didn’t think that was allowed. But people have told me that they feel better after taking it. DC You are a pharmacist? Boots. Yes |
Sadly, this abysmal performance is only too typical in my experience, Try it yourself.
The malaria question
After it was revealed that pharmacists were recommending, or tolerating recommendations, of homeopathic treatment of malaria, the RPSGB did, at last. speak out. It was this episode that caused Quackometer to write his now famous piece on ‘The gentle art of homeopathic killing‘ (it shot to fame when the Society of Homeopaths tried to take legal action to ban it) Recommending pills that contain no medicine for the treatment or prevention or treatment of malaria is dangerous. If it is not criminal it ought to be [watch the Neals Yard video]. .
The RPSGB says it is investigating the role of pharmacists in the Newsnight sting (see the follow-up here). That was in July 2006, but they are stlll unwilling to say if any action will be taken. Anyone want to bet that it will be swept under the carpet?
The statement issued by the RPSGB, 5 months after the malaria sting is just about the only example that I can find of them speaking out against dangerous and fraudulent homeopathic practices. Even in this case, it is pretty mild and restricted narrowly to malaria prevention.
The RPSGB and the Quacktioner Royal
The RPSGB submitted a response to the ‘consultation’ held by the Prince’s Foundation for Integrated Health, about their Complementary Healthcare; a guide for patients.
| Response by the Royal Pharmaceutical Society of Great Britain Dr John Clements, Science Secretary “We believe that more emphasis should be given to the need for members of the public who are purchasing products (as opposed to services) to ask for advice about the product. Pharmacists are trained as experts on medicines and the public, when making purchases in pharmacies, would expect to seek advice from pharmacists” |
So plenty of puffery for the role of pharmacists. But there is not a word of criticism about the many barmy treatments that are included in the “Guide for Patients”. Not just homeopathy and herbalism, but also Craniosacral therapy, Laying on of Hands, chiropractic, Reiki, Shiatsu –every form of barminess under the sun drew no comment from the RPS.
I can’t see how a response like this is consistent with the RPS’s own code of ethics.
A recent president of the RPSGB was a homeopath
| Christine Glover provides perhaps the most dramatic reason of all for thinking thst, despite all the fine words, the RPSGB cares little for evidence and truth The NHS Blogdoctor published “Letter from an angry pharmacist”. |  |
Mrs Glover was president of the RPSGB from 1999 to 2001, vice-president in 1997-98, and a member of the RPSGB Council until May 2005. She is not just a member, but a Fellow. (Oddly, her own web site says President from 1998 – 2001.)
So it is relevant to ask how the RPSGB’s own ex-president obeys their code of ethics. Here are some examples on how Ms Glover helps to assist the safe and effective use of medicines. . Much of her own web site seems to have vanished (I wonder why) so I’ll have to quote the “Letter from an angry pharmacist”., as revealed by NHS Blogdoctor,
“What has Christine got to offer?
- “We offer a wide range of Homeopathic remedies (over 3000 different remedies and potencies) as well as Bach flower remedies, Vitamins, Supplements, some herbal products and Essential Oils.”
- Jetlag Tablets highly recommended in ‘Wanderlust’ travel magazine. Suitable for all ages.
- Wind Remedy useful for wind particularly in babies. In can be supplied in powder form for very small babies. Granules or as liquid potency.
- Udder Care 100ml £80.00 One capful in sprayer filled with water. Two jets to be squirted on inner vulva twice daily for up to 4 days until clots reduced. Discard remainder. Same dose for high cell-counting cows detected.
Udder Care? Oh! I forgot to say, “Glover’s Integrated Healthcare” does cows as well as people. Dr Crippen would not suggest to a woman with sore breasts that she sprayed something on her inner vulva. But women are women and cows are cows and Dr Crippen is not an expert on bovine anatomy and physiology. But, were he a farmer, he would need some persuasion to spend £80.00 on 100 mls of a liquid to squirt on a cow’s vulva. Sorry, inner vulva.”
Nothing shows more clearly that the RPSGB will tolerate almost any quackery than the fact that they think Glover is an appropriate person to be president. Every item on the quotation above seems to me to be in flagrant breach of the RPSGB’s Code of Ethics. Just like the Society of Homeopaths, the code seems to be there merely for show, at least in the case of advice about junk medicine..
A greater role for pharmacists?
This problem has become more important now that the government proposes to give pharmacists a greater role in prescribing. Needless to say the RPSGB is gloating about their proposed new role. Other people are much less sure it is anything but a money–saving gimmick and crypto-privatisation.
I have known pharmacists who have a detailed knowledge of the actions of drugs, and I have met many more who haven’t. The main objection, though, is that pharmacists have a direct financial interest in their prescribing. Conflicts of interest are already rife in medicine, and we can’t afford them.
Conclusion
The Royal Pharmaceutical Society is desperately evasive about a matter that is central to their very existence, giving good advice to patients about which medicines work and which don’t. Pharmacists should be in the front line in education of the public, about medicines, the ‘scientist on the High Street’. Some of them are, but their professional organisation is letting them down badly.
Until such time as the RPSGB decides to take notice of evidence, and clears up some of the things described here, it is hard to see how they can earn the respect of pharmacists, or of anyone else.
Follow-up
Stavros Isaiadis’ blog, Burning Mind, has done a good piece on “More on Quack Medicine in High Street Shops“.
The Chemist and Druggist reports that the RPSGB is worried about the marketing of placebo pills (‘obecalp’ -geddit?). It does seem very odd that the RPSGB should condemn honest placebos, but be so very tolerant about dishonest placebos. You couldn’t make it up.
A complaint to the RPSGB is rejected
Just to see what happened, I made a complaint to thr RPSGB about branches of their own Code of Ethics at Boots in Hexham and in Evesham. Both of them supported Homeopathy Awareness Week These events had been publicised in those particularly unpleasent local ‘newspapers’ that carry paid advertising disguised as editorial material. In this case it was the Evesham Journal and the Hexham Courant.
Guess what? The RPSGB replied thus
“Your complaint has been reviewed bt Mrs Jill Williams and Mr David Slater who are both Regional Lead Inspectors. Having carried out a review they have concluded that support of homeopathic awareness week does not constitute a breach of the Society’s Code of Ethics or Professional Standards.”
In case you have forgotten, the Professional Standards say
2.1 procedures for sales of OTC medicines enable intervention and professional advice to be given whenever this can assist the safe and effective use of medicines.
The RPSGB has some very quaint ideas on how to interpret their own code of ethics

