There’s been no official announcement, but four more of Westminster’s courses in junk medicine have quietly closed.
For entry in 2011 they offer
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Complementary Medicine (B255) | 3FT Hon BSc |
| Complementary Medicine (B301) | 4FT Hon MHSci |
| Complementary Medicine: Naturopathy (B391) | 3FT Hon BSc |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSci |
| Nutritional Therapy (B400) | 3FT Hon BSc |
But for entry in 2012
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSc |
At the end of 2006, Westminster was offering 14 different BSc degrees in seven flavours of junk medicine. In October 2008, it was eleven. This year it’s eight, and next year only four degrees in two subjects. Since "Integrated Health" was ‘merged’ with Biological Sciences in May 2010, two of the original courses have been dropped each year. This September there will be a final intake for Nutrition Therapy and Naturopathy. That leaves only two, Chinese Medicine (acupuncture and (Western) Herbal Medicine.
The official reason given for the closures is always that the number of applications has fallen. I’m told that the number of applications has halved over the last five or six years. If that’s right, it counts as a big success for the attempts of skeptics to show the public the nonsense that’s taught on these degrees. Perhaps it is a sign that we are emerging from the endarkenment.
Rumour has it that the remaining degrees will eventually close too. Let’s hope so. Meanwhile, here is another helping hand.
There is already quite a bit here about the dangers of Chinese medicine, e.g. here and, especially, here. A submission to the Department of Health gives more detail. There has been a lot on acupuncture here too. There is now little doubt that it’s no more than a theatrical, and not very effective, placebo. So this time I’ll concentrate on Western herbal medicine.
Western Herbal Medicine
Herbal medicine is just a branch of pharmacology and it could be taught as such. But it isn’t. It comes overlaid with much superstitious nonsense. Some of it can be seen in slides from Edinburgh Napier University (the difference being that Napier closed that course, and Westminster hasn’t)
Even if it were taught properly, it wouldn’t be appropriate for a BSc for several reasons.
First, there isn’t a single herbal that has full marketing authorisation from the MHRA. In other words, there isn’t a single herb for which there is good evidence that it works to a useful extent.
Second, the fact that the active principals in plants are virtually always given in an unknown dose makes them potentially dangerous. This isn’t 1950s pharmacology. It’s 1920s pharmacology, dating from a time before methods were worked out for standardising the potency of natural products (see Plants as Medicines).
Third, if you are going to treat illness with chemicals, why restrict yourself to chemicals that occur in plants?
It was the herbal medicine course that gave rise to the most virulent internal complaints at the University of Westminster. These complaints revealed the use of pendulum dowsing by some teachers on the course and the near-illegal, and certainly dangerous, teaching about herbs in cancer.
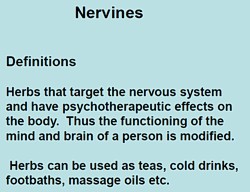
Here are a few slides from Principles of Herbal Medicine(3CT0 502). The vocabulary seems to be stuck in a time warp. When I first started in the late 1950s, words like tonic, carminative, demulcent and expectorant were common Over the last 40 years all these words have died out in pharmacology, for the simple reason that it became apparent that there were no such actions. But these imaginary categories are still alive and well in the herbal world.
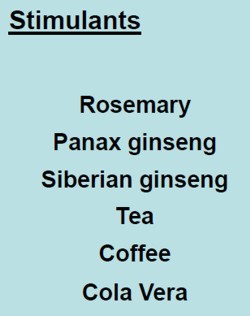
There was a lecture on a categories of drugs so old-fashioned that I’ve never even heard the words: "nervines". and "adaptogens".
 |
  |
 |
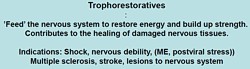
The "tonics" listed here seem quite bizarre. In the 1950s, “tonics” containing nux vomica (a small dose of strychnine) and gentian (tastes nasty) were common, but they vanished years ago, because they don’t work. None of those named here even get a mention in NCCAM’s Herbs-at-a-glance. Oats? Come on! |
|
The only ‘relaxant’ here for which there is the slightest evidence is Valerian. I recall tincture of Valerian in a late 1950s pharmacy. It smells terrible, According to NCCAM
Not much, for something that’s been around for centuries. And for chamomile
None of this near-total lack of evidence is mentioned on the slides. |
 |
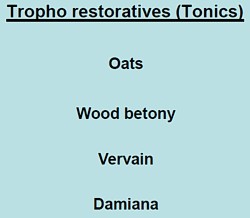
What about the ‘stimulants‘? Rosemary? No evidence at all. Tea and coffee aren’t medicine (and not very good stimulants for me either).
|
Ginseng, on the other hand, is big business. That doesn’t mean it works of course. NCCAM says of Asian ginseng (Panax Ginseng).
|
 |
Thymoleptics – antidepressants are defined as "herbs that engender a feeling of wellbeing. They uplift the spirit, improve the mood and counteract depression".
Oats, Lemon balm, Damiana, Vervain. Lavender and Rosemary are just old bits of folklore
|
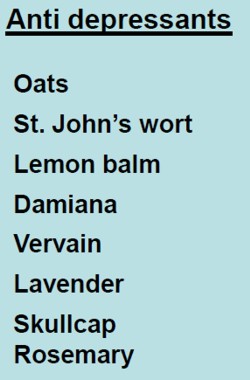 |
The only serious contender here is St John’s Wort. At one time this was the prize exhibit for herbalists. It has been shown to be as good as the conventional SSRIs for treatment of mild to moderate depression. Sadly it has turned out that the SSRIs are themselves barely better than placebos. NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
"Adaptogens" are another figment of the herbalists’ imaginations. They are defined in the lecture thus.
|
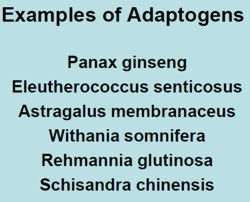
|
Well, it would be quite nice if such drugs existed. Sadly they don’t.
- The evidence for using astragalus for any health condition is limited. High-quality clinical trials (studies in people) are generally lacking.
Another lecture dealt with "stimulating herbs". No shortage of them, it seems.
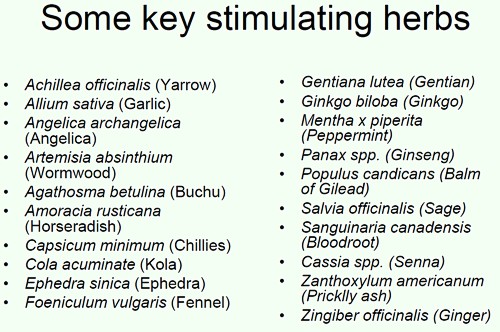
Well at least one of these has quite well-understood effects in pharmacology, ephedrine, a sympathomimetic amine. It isn’t used much because it can be quite dangerous, even with the controlled dose that’s used in real medicine. In the uncontrolled dose in herbal medicines it is downright dangerous.
|
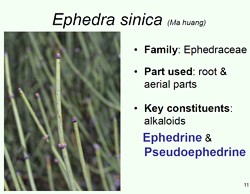
|
|
|
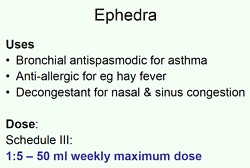
This is what NCCAM says about Ephedra
- An NCCAM-funded study that analyzed phone calls to poison control centers found a higher rate of side effects from ephedra, compared with other herbal products.
- Other studies and systematic reviews have found an increased risk of heart, psychiatric, and gastrointestinal problems, as well as high blood pressure and stroke, with ephedra use.
- According to the U.S. Food and Drug Administration (FDA), there is little evidence of ephedra’s effectiveness, except for short-term weight loss. However, the increased risk of heart problems and stroke outweighs any benefits.
It seems that what is taught in the BSc Herbal Medicine degree consists largely of folk-lore and old wives’ tales. Some of it could be quite dangerous for patients.
A problem for pharmacognosists
While talking about herbal medicine, it’s appropriate to mention a related problem, though it has nothing to do with the University of Westminster.
My guess is that not many people have even heard of pharmacognosy. If it were not for my humble origins as an apprentice pharmacist in Grange Road, Birkenhead (you can’t get much more humble than that) I might not know either.
Pharmacognosy is a branch of botany, the study of plant drugs. I recall inspecting powered digitalis leaves under a microscope. In Edinburgh, in the time of the great pharmacologist John Henry Gaddum, medical students might be presented in the oral exam with a jar of calabar beans and required to talk about their anticholinesterase effects of the physostigmine that they contain.
The need for pharmacognosy has now all but vanished, but it hangs on in the curriculum for pharmacy students. This has engendered a certain unease about the role of pharmacognists. They often try to justify their existence by rebranding themselves as "phytotherapists". There are even journals of phytotherapy. It sounds a lot more respectable that herbalism. At its best, it is more respectable, but the fact remains that there no herbs whatsoever that have well-documented medical uses.
The London School of Pharmacy is a case in point. Simon Gibbons (Professor of Phytochemistry, Department of Pharmaceutical and Biological Chemistry). The School of Pharmacy) has chosen, for reasons that baffle me, to throw in his lot with the reincarnated Prince of Wales Foundation known as the “College of Medicine“. That organisation exists largely (not entirely) to promote various forms of quackery under the euphemism “integrated medicine”. On their web site he says "Western science is now recognising the extremely high value of herbal medicinal products . . .", despite the fact that there isn’t a single herbal preparation with efficacy sufficient for it to get marketing authorisation in the UK. This is grasping at straws, not science.
The true nature of the "College of Medicine" is illustrated, yet again, by their "innovations network". Their idea of "innovation" includes the Bristol Homeopathic Hospital and the Royal London Hospital for Integrated medicine, both devoted to promoting the utterly discredited late-18th century practice of giving people pills that contain no medicine. Some "innovation".
It baffles me that Simon Gibbons is willing to appear on the same programme as Simon Mills and David Peters, and George Lewith. Mills’ ideas can be judged by watching a video of a talk he gave in which he ‘explains’ “hot and cold herbs”. It strikes me as pure gobbledygook. Make up your own mind. He too has rebranded himself as "phytotherapist" though in fact he’s an old-fashioned herbalist with no concern for good evidence. David Peters is the chap who, as Clinical Director of the University of Westminster’s ever-shrinking School of Quackery, tolerates dowsing as a way to select ‘remedies’.
The present chair of Pharmacognosy at the School of Pharmacy is Michael Heinrich. He, with Simon Gibbons, has written a book Fundamentals of pharmacognosy and phytotherapy. As well as much good chemistry, it contains this extraordinary statement
“TCM [traditional Chinese medicine] still contains very many remedies which were selected by their symbolic significance rather than their proven effects; however this does not mean that they are all ‘quack’remedies! There may even be some value in medicines such as tiger bone, bear gall, turtle shell, dried centipedes, bat dung and so on. The herbs, however, are well researched and are becoming increasingly popular as people become disillusioned with Western Medicine.”
It is irresponsible to give any solace at all to the wicked industries that kill tigers and torture bears to extract their bile. And it is simple untrue that “herbs are well-researched”. Try the test,
A simple test for herbalists. Next time you encounter a herbalist, ask them to name the herb for which there is the best evidence of benefit when given for any condition. Mostly they refuse to answer, as was the case with Michael McIntyre (but he is really an industry spokesman with few scientific pretensions). I asked Michael Heinrich, Professor of Pharmacognosy at the School of Pharmacy. Again I couldn’t get a straight answer. Usually, when pressed, the two things that come up are St John’s Wort and Echinacea. Let’s see what The National Center for Complementary and Alternative Medicine (NCCAM) has to say about them. NCCAM is the branch of the US National Institutes of Health which has spent around a billion dollars of US taxpayers’ money on research into alternative medicine, For all that effort they have failed to come up with a single useful treatment. Clearly they should be shut down. Nevertheless, as an organisation that is enthusiastic about alternative medicine, their view can only be overoptimistic.
For St John’s Wort . NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
For Echinacea NCCAM says
- Study results are mixed on whether echinacea can prevent or effectively treat upper respiratory tract infections such as the common cold. For example, two NCCAM-funded studies did not find a benefit from echinacea, either as Echinacea purpurea fresh-pressed juice for treating colds in children, or as an unrefined mixture of Echinacea angustifolia root and Echinacea purpurea root and herb in adults. However, other studies have shown that echinacea may be beneficial in treating upper respiratory infections.
If these are the best ones, heaven help the rest.


Gentian tastes nasty?
Not a fan of Angostura bitters or Suze then?
[…] Improbable Science reports that a public, tax-supported university in the UK has shut down only half of their woo-woo […]
[…] his own university, and he has a pretty good take down. The other is the University of Westminster where alternative ‘medicine’ degrees have been getting phased out over the years: At the end of 2006, Westminster was offering 14 different BSc degrees in seven flavours of junk […]
I would also be very worried if your sample is representative of UK courses on herbal medicine. However, I think your account of “western herbal medicine” is filled with prejudices. It is actually rather strange coming from a pharmacologist. The difference between herbal medicine and stuff like homeopathy is that herbal medicine is based on the same principles of pharmacology: many plant metabolites are active substances. There are several herbs that have been submitted to clinical trials, systematic reviews and meta-analysis. New analytical methods are overcoming the difficult problems associated with the quality control of herbal medicines. Yes, its true that many of these products are no better than placebo, but so is many of mainstream synthetic medicines like antidepressants. Your account of pharmacognosists is also very prejudicious. You say that the need for pharmacognosy has vanished, but all of those working on the chemistry of natural products and many of those working on the development of new drugs would think otherwise. Many of the marvels of synthetic organic chemistry that make the arsenal of medicine are still based on a natural product pharmacophore. Rational drug design would not have many medals to exhibit if we remove the sometimes distant natural product template that was the starting point for drug development. You should as a pharmacologist be a little more humble towards the science that gave you what to work with…
@Eddie
You say
If you were really worried, you’d have spent as much time as I have trying to discover what’s taught. Have you any reason to think it isn’t representative? The content shown here is very similar to that at the (now-closed) course at Edinburgh Napier University, and similar to many textbooks and videos that are easily available. Westminster is probably exceptional in using dowsing, but it’s hard to discover if that’s so because universities are very reluctant to admit that sort of thing. That apart, I suspect this course is entirely typical.
So it seems we are in agreement that courses like this one are a disgrace to any thinking person, never mind to a “university”.
You seem more critical of my comments about the history and about pharrnacognosy. Of course I am well aware of the important part that plants have played in the history of pharmacology.. I’m also aware that no plants are used in their raw form in medicine, for good reasons that I’ve outlined. Working out what active principles are in plants, phytochemistry, has been, and still is, an important source of ideas, and occasionally produces a winner. Artemisinin comes to mind, but that isn’t used as a raw herb of course (by anyone in their right mind).
What I was criticisng was not phytochemistry, but "phytotherapy". More often than not, that term is simply a rebranding of herbalism, in an effort to make it sound more respectable. Just watch the video by Simon Mills if you don’t believe that As it happens I recently stumbled on a PhD thesis written between 1997 and 2002, "Re-presenting herbal medicine as phytotherapy: a strategy of professionalisation through formation of a ‘scientific’ medicine", by Edmond VanMarie [pdf file]. The hyphenation and scare quotes convey the message. It’s a bit like the rebranding of alternative medicine as ‘complementary’ and then as ‘integrated’. It is a crude and dishonest public relations exercise that does nothing to change the reality.
I have nothing against pharmacognosists as long as they stick to botany, or to phytochemistry. The problem arises when they try to justify their existence by means of exaggerated claims for efficacy, and when they sell their souls to the fantasists in the "College of Medicine". That can only destroy their reputation.
[…] was reading about problems with universities endorsing ‘science’ degrees in homeopathy and other […]
[…] University of Westminster shuts down naturopathy, nutritional therapy, but keeps Acupuncture and Her… […]
[…] (herbal) and other dietary supplements, acupuncture, massage, and yoga. NCCAM Featured ContentPeople with cancer want to do everything they can to combat the disease, manage its symptoms, and co…k" rel="nofollow" href="http://nccam.nih.gov/health/cancer/camcancer.htm?nav=rss">NCCAM Featured […]
It is interesting to see you applauding the closure of the so called “junk medicine” courses at Westminister, while obesity, diabetes mellitus, cancer and cardiovascular disease abound. The bottom line is that drugs and present day medicine are not stemming the tide. The simple reason for this is that these fields are not well equipped enough to do so. Until they are, we will continue to see the rising pandemic of chronic disease worldwide. By the way, medicine has been, and will always be an art as well as a science. Science itself is all about inspired ideas gained from observation and testing put to further observation and testing until a repeatable pattern emerges. Which is exactly what should happen in nutritional courses – this will not happen when they are closed down. The only long term solution to obesity, diabetes etc is a nutritional one. Drugs, surgery etc are at best adjuncts in the battle. Do you really think the general public are clued up on nutrition? If they are, why do we have an avalanche of chronic disease spreading worldwide? Are doctors and the pharmaceutical industry teaching proper nutrition and lifestyle choices?
@historian186
I can see you are not a scientist because you refer to
“the simple reason for this . . .”.
There is nothing simple about it. The extent of ignorance about nutrition is amazing. Try, for example, my posts on the risks of eating red meat.
It is arrogant and inaccurate to declare that “The only long term solution to obesity, diabetes etc is a nutritional one”. The fact of the matter is that nobody knows what the long term solution is.
That being said, it’s sensible to eat a mixed diet, and, above all, not to eat too much.
The answer to your last question is that doctors are incessantly trying to teach proper nutrition and lifestyle. We are urged daily by doctors and government agencies to eat our five-a-day.
If you explore this blog, you’ll see that nutritional therapists are taught a lot of new age nonsense, which they then sell to patients. See, for example, Nutritional Fairy Tales from Thames Valley University. They do no serious research and, not infrequently, the give bad advice, as revealed in the recent investigation by Which? magazine. This concluded that “high street nutritional therapists are a waste of money”.
Only too many of them make a living my recommending unnecessary supplements (sometimes with kickbacks from the supplement industry).
The supplement industry is vast an wealthy. It makes false claims for its products regularly. It is at least as dishonest as the pharmaceutical industry, but at least some of the products of the latter work (or do you have teeth extracted without an anaesthetic?).
There a perfectly respectable courses in nutrition, both the science its the practical application.
The people who are experts in practical application are called registered dietitions. Anyone can call themselves a nutritionist.
The courses that were closed were little better than quackery. The world is better off without them.
*My God, this article sounds like something out of the dark ages. My wonderful naturopathic doctor helped me beyond belief – this was mainly due to adopting the theory that many illnesses are linked to the mind and emotions. My GP has also had the brains to think outside the box and offered much natural care advice too, with wonderful results. Personal health care is very individual and i find it incredibly ignorant of you to class natural care with a sweeping statement such as ‘junk’. You have absolutely no idea what you are talking about it, and from i can gather, have absolutely no experience in these fields. I praise all health care professionals that are starting to treat the body as a multi functioning organism, combining mind and emotions too, and also have the sense to use means – such as those taught on naturopathic courses – to locate such areas of dis – ease. Although there will always be arguments for ‘for’ and ‘against’, to generalise and rubbish everything is totally unwise. There is a place for both orthodox and natural medicine – both are valid.
Yes, the documents revealed here are indeed like something out of the dark ages. I expect that is why the course in “naturopathy” has closed now.
Naturopathy consists largely of doing nothing (for a substantial fee). I’m glad you got better. You were lucky not to die. If your symptoms had been caused by a fatal disease, it’s unlikely that a naturopath would have spotted the fact, and by the time you got to a real doctor it could well have been too late.
That’s why it is a great mistake to think that things like homeopathy and naturopathy are safe. The treatments themselves have no effects, good or bad. But if you had pneumonia. septicaemia, meningitis, diabetes are any other life-threatening illness, relying on these ill-educated people could be fatal.
In fact homeopaths in Australia have been jailed for manslaughter, for exactly that reason. Their neglect of proper medical care killed their own daughter.
*David Colguhoun, Sir, are you unaware that a good herbal medicine practitioner will of studied pathology? As such they are able to diagnose disease.
*Eddie, a pharmacologist investigates pharmaceutical chemicals and the effect they have on the body and it’s systems. Herbal medicine can not be patented, and as such carries little interest for pharmaceutical companies and their affiliates. Shall I continue 😉
@Dr J Kanns
Yes. I know that they do some regular physiology and pathology, as well as the sort of nonsense exemplified above. But they have no access to hospitals and so much of it must be theoretical. It would be foolish to trust their diagnostic abilities, in my opinion.
Even if they get the diagnosis right, there is little that they can do about it. You don’t need to believe me. Look at Herbs at a Glance, on the web site of the National Center for Complementary and Alternative Medicine (NCCAM), an organisation that is heavily biassed in favour of alternative medicine. For just about every herb listed there, check the “What the science says” section. Even NCCAM admit there is little or no good evidence for any of them.
And you are, of course, quite wrong to say that pharmaceutical companies are not interested in plants. Take, for example. digoxin or artemesinin. It would be dangerous to give either of them in plant form, because the extracts used by herbalists are, disgracefully, not standardised. See, for example, my post on Plants as medicines.