Jane Lewis
There’s been no official announcement, but four more of Westminster’s courses in junk medicine have quietly closed.
For entry in 2011 they offer
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Complementary Medicine (B255) | 3FT Hon BSc |
| Complementary Medicine (B301) | 4FT Hon MHSci |
| Complementary Medicine: Naturopathy (B391) | 3FT Hon BSc |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSci |
| Nutritional Therapy (B400) | 3FT Hon BSc |
But for entry in 2012
| University of Westminster (W50) | qualification |
| Chinese Medicine: Acupuncture (B343) | 3FT Hon BSc |
| Chinese Medicine: Acupuncture with Foundation (B341) | 4FT/5FT Hon BSc/MSci |
| Herbal Medicine (B342) | 3FT Hon BSc |
| Herbal Medicine with Foundation Year (B340) | 4FT/5FT Hon BSc/MSc |
At the end of 2006, Westminster was offering 14 different BSc degrees in seven flavours of junk medicine. In October 2008, it was eleven. This year it’s eight, and next year only four degrees in two subjects. Since "Integrated Health" was ‘merged’ with Biological Sciences in May 2010, two of the original courses have been dropped each year. This September there will be a final intake for Nutrition Therapy and Naturopathy. That leaves only two, Chinese Medicine (acupuncture and (Western) Herbal Medicine.
The official reason given for the closures is always that the number of applications has fallen. I’m told that the number of applications has halved over the last five or six years. If that’s right, it counts as a big success for the attempts of skeptics to show the public the nonsense that’s taught on these degrees. Perhaps it is a sign that we are emerging from the endarkenment.
Rumour has it that the remaining degrees will eventually close too. Let’s hope so. Meanwhile, here is another helping hand.
There is already quite a bit here about the dangers of Chinese medicine, e.g. here and, especially, here. A submission to the Department of Health gives more detail. There has been a lot on acupuncture here too. There is now little doubt that it’s no more than a theatrical, and not very effective, placebo. So this time I’ll concentrate on Western herbal medicine.
Western Herbal Medicine
Herbal medicine is just a branch of pharmacology and it could be taught as such. But it isn’t. It comes overlaid with much superstitious nonsense. Some of it can be seen in slides from Edinburgh Napier University (the difference being that Napier closed that course, and Westminster hasn’t)
Even if it were taught properly, it wouldn’t be appropriate for a BSc for several reasons.
First, there isn’t a single herbal that has full marketing authorisation from the MHRA. In other words, there isn’t a single herb for which there is good evidence that it works to a useful extent.
Second, the fact that the active principals in plants are virtually always given in an unknown dose makes them potentially dangerous. This isn’t 1950s pharmacology. It’s 1920s pharmacology, dating from a time before methods were worked out for standardising the potency of natural products (see Plants as Medicines).
Third, if you are going to treat illness with chemicals, why restrict yourself to chemicals that occur in plants?
It was the herbal medicine course that gave rise to the most virulent internal complaints at the University of Westminster. These complaints revealed the use of pendulum dowsing by some teachers on the course and the near-illegal, and certainly dangerous, teaching about herbs in cancer.
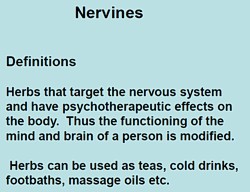
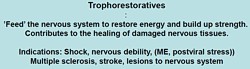
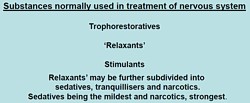
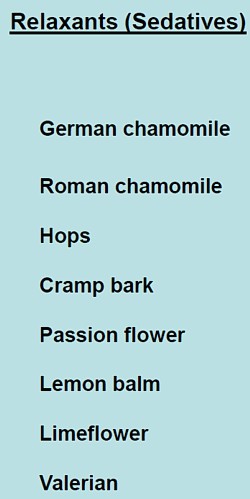
Here are a few slides from Principles of Herbal Medicine(3CT0 502). The vocabulary seems to be stuck in a time warp. When I first started in the late 1950s, words like tonic, carminative, demulcent and expectorant were common Over the last 40 years all these words have died out in pharmacology, for the simple reason that it became apparent that there were no such actions. But these imaginary categories are still alive and well in the herbal world.
There was a lecture on a categories of drugs so old-fashioned that I’ve never even heard the words: "nervines". and "adaptogens".
 |
  |
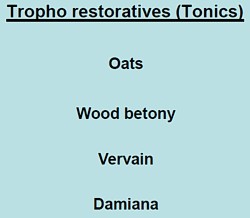 |
The "tonics" listed here seem quite bizarre. In the 1950s, “tonics” containing nux vomica (a small dose of strychnine) and gentian (tastes nasty) were common, but they vanished years ago, because they don’t work. None of those named here even get a mention in NCCAM’s Herbs-at-a-glance. Oats? Come on! |
|
The only ‘relaxant’ here for which there is the slightest evidence is Valerian. I recall tincture of Valerian in a late 1950s pharmacy. It smells terrible, According to NCCAM
Not much, for something that’s been around for centuries. And for chamomile
None of this near-total lack of evidence is mentioned on the slides. |
 |
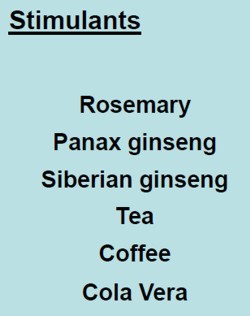
What about the ‘stimulants‘? Rosemary? No evidence at all. Tea and coffee aren’t medicine (and not very good stimulants for me either).
|
Ginseng, on the other hand, is big business. That doesn’t mean it works of course. NCCAM says of Asian ginseng (Panax Ginseng).
|
 |
Thymoleptics – antidepressants are defined as "herbs that engender a feeling of wellbeing. They uplift the spirit, improve the mood and counteract depression".
Oats, Lemon balm, Damiana, Vervain. Lavender and Rosemary are just old bits of folklore
|
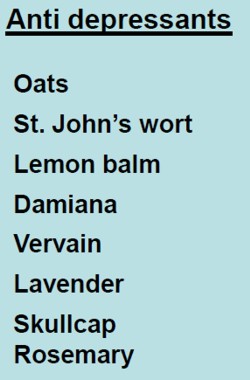 |
The only serious contender here is St John’s Wort. At one time this was the prize exhibit for herbalists. It has been shown to be as good as the conventional SSRIs for treatment of mild to moderate depression. Sadly it has turned out that the SSRIs are themselves barely better than placebos. NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
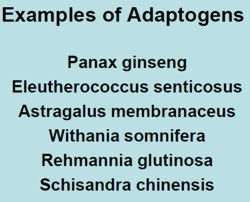
"Adaptogens" are another figment of the herbalists’ imaginations. They are defined in the lecture thus.
|
|
Well, it would be quite nice if such drugs existed. Sadly they don’t.
- The evidence for using astragalus for any health condition is limited. High-quality clinical trials (studies in people) are generally lacking.
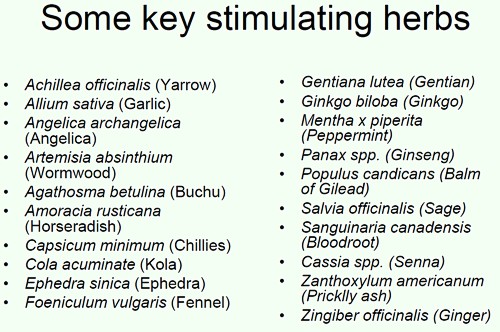
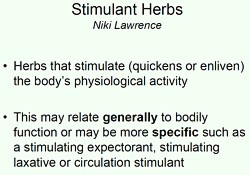
Another lecture dealt with "stimulating herbs". No shortage of them, it seems.
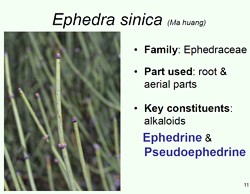
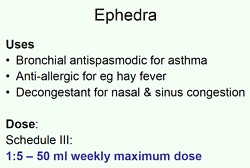
Well at least one of these has quite well-understood effects in pharmacology, ephedrine, a sympathomimetic amine. It isn’t used much because it can be quite dangerous, even with the controlled dose that’s used in real medicine. In the uncontrolled dose in herbal medicines it is downright dangerous.
|
|
|
|
This is what NCCAM says about Ephedra
- An NCCAM-funded study that analyzed phone calls to poison control centers found a higher rate of side effects from ephedra, compared with other herbal products.
- Other studies and systematic reviews have found an increased risk of heart, psychiatric, and gastrointestinal problems, as well as high blood pressure and stroke, with ephedra use.
- According to the U.S. Food and Drug Administration (FDA), there is little evidence of ephedra’s effectiveness, except for short-term weight loss. However, the increased risk of heart problems and stroke outweighs any benefits.
It seems that what is taught in the BSc Herbal Medicine degree consists largely of folk-lore and old wives’ tales. Some of it could be quite dangerous for patients.
A problem for pharmacognosists
While talking about herbal medicine, it’s appropriate to mention a related problem, though it has nothing to do with the University of Westminster.
My guess is that not many people have even heard of pharmacognosy. If it were not for my humble origins as an apprentice pharmacist in Grange Road, Birkenhead (you can’t get much more humble than that) I might not know either.
Pharmacognosy is a branch of botany, the study of plant drugs. I recall inspecting powered digitalis leaves under a microscope. In Edinburgh, in the time of the great pharmacologist John Henry Gaddum, medical students might be presented in the oral exam with a jar of calabar beans and required to talk about their anticholinesterase effects of the physostigmine that they contain.
The need for pharmacognosy has now all but vanished, but it hangs on in the curriculum for pharmacy students. This has engendered a certain unease about the role of pharmacognists. They often try to justify their existence by rebranding themselves as "phytotherapists". There are even journals of phytotherapy. It sounds a lot more respectable that herbalism. At its best, it is more respectable, but the fact remains that there no herbs whatsoever that have well-documented medical uses.
The London School of Pharmacy is a case in point. Simon Gibbons (Professor of Phytochemistry, Department of Pharmaceutical and Biological Chemistry). The School of Pharmacy) has chosen, for reasons that baffle me, to throw in his lot with the reincarnated Prince of Wales Foundation known as the “College of Medicine“. That organisation exists largely (not entirely) to promote various forms of quackery under the euphemism “integrated medicine”. On their web site he says "Western science is now recognising the extremely high value of herbal medicinal products . . .", despite the fact that there isn’t a single herbal preparation with efficacy sufficient for it to get marketing authorisation in the UK. This is grasping at straws, not science.
The true nature of the "College of Medicine" is illustrated, yet again, by their "innovations network". Their idea of "innovation" includes the Bristol Homeopathic Hospital and the Royal London Hospital for Integrated medicine, both devoted to promoting the utterly discredited late-18th century practice of giving people pills that contain no medicine. Some "innovation".
It baffles me that Simon Gibbons is willing to appear on the same programme as Simon Mills and David Peters, and George Lewith. Mills’ ideas can be judged by watching a video of a talk he gave in which he ‘explains’ “hot and cold herbs”. It strikes me as pure gobbledygook. Make up your own mind. He too has rebranded himself as "phytotherapist" though in fact he’s an old-fashioned herbalist with no concern for good evidence. David Peters is the chap who, as Clinical Director of the University of Westminster’s ever-shrinking School of Quackery, tolerates dowsing as a way to select ‘remedies’.
The present chair of Pharmacognosy at the School of Pharmacy is Michael Heinrich. He, with Simon Gibbons, has written a book Fundamentals of pharmacognosy and phytotherapy. As well as much good chemistry, it contains this extraordinary statement
“TCM [traditional Chinese medicine] still contains very many remedies which were selected by their symbolic significance rather than their proven effects; however this does not mean that they are all ‘quack’remedies! There may even be some value in medicines such as tiger bone, bear gall, turtle shell, dried centipedes, bat dung and so on. The herbs, however, are well researched and are becoming increasingly popular as people become disillusioned with Western Medicine.”
It is irresponsible to give any solace at all to the wicked industries that kill tigers and torture bears to extract their bile. And it is simple untrue that “herbs are well-researched”. Try the test,
A simple test for herbalists. Next time you encounter a herbalist, ask them to name the herb for which there is the best evidence of benefit when given for any condition. Mostly they refuse to answer, as was the case with Michael McIntyre (but he is really an industry spokesman with few scientific pretensions). I asked Michael Heinrich, Professor of Pharmacognosy at the School of Pharmacy. Again I couldn’t get a straight answer. Usually, when pressed, the two things that come up are St John’s Wort and Echinacea. Let’s see what The National Center for Complementary and Alternative Medicine (NCCAM) has to say about them. NCCAM is the branch of the US National Institutes of Health which has spent around a billion dollars of US taxpayers’ money on research into alternative medicine, For all that effort they have failed to come up with a single useful treatment. Clearly they should be shut down. Nevertheless, as an organisation that is enthusiastic about alternative medicine, their view can only be overoptimistic.
For St John’s Wort . NCCAM says
- There is scientific evidence that St. John’s wort may be useful for short-term treatment of mild to moderate depression. Although some studies have reported benefits for more severe depression, others have not; for example, a large study sponsored by NCCAM found that the herb was no more effective than placebo in treating major depression of moderate severity.
For Echinacea NCCAM says
- Study results are mixed on whether echinacea can prevent or effectively treat upper respiratory tract infections such as the common cold. For example, two NCCAM-funded studies did not find a benefit from echinacea, either as Echinacea purpurea fresh-pressed juice for treating colds in children, or as an unrefined mixture of Echinacea angustifolia root and Echinacea purpurea root and herb in adults. However, other studies have shown that echinacea may be beneficial in treating upper respiratory infections.
If these are the best ones, heaven help the rest.
Follow-up
Universities, like most businesses, cite glowing testimonials from grateful students, I doubt whether universities are any more honest than anyone else in their choice of what to publish. When I asked to see any letters that had been sent to the university, I was sent only one and extracts from it appear in the last post on Westminster. More dangerous nonsense from the University of Westminster: when will Professor Geoffrey Petts do something about it? But I knew (don’t ask how) that there had been more than that, and a slightly widened FOIA request produced some interesting results (though I’m aware of other letters that were not supplied -not good).
As always, the information came with the caveat
"Copyright in our response to your request belongs to the University of Westminster. All rights are reserved. This document is for personal use only and may not be copied, or stored in any electronic form, or reproduced in any other way or used for any other purpose, either in whole or in part, without the prior written consent of the University of Westminster.".
Why else would anyone ask for information but to make it public? And since the letter was sent in electronic form, it would be hard to comply with the second part. As always, I rely on the fair quotation and public interest defences to quote parts of the letters.
The main players here are Peter Davies (Head of herbal medicine and nutritional therapy), Julie Whitehouse (Course Leader for MSci Herbal Medicine and the BSc Honours Health Sciences), David Peters (Clinical director of Westminster’s School of Integrated Health), and the dean of the School of Life Sciences. Jane Lewis. There’s no woo about Jane Lewis. I suspect she’d have got rid of all the nonsense, given a chance. Who, I wonder, is stopping her?
Julie Whitehouse is, I see, a co-author of Brock et al. (2010) American skullcap (Scutellaria lateriflora): an ancient remedy for today’s anxiety, British Journal of Wellbeing1 (4), 25-30. I had no idea there was such a journal. UCL does not subscribe so if anyone has a reprint I’d love to see it. Judging by the abstract it’s yet more ‘preliminary work’. That’s very typical. Next to no CAM research gets past the preliminary report.
Some testimonials
Here are some quotations from “a part-time student on the herbal medicine (HM) BSc course, currently in my 3rd year of study. I have first class honours degree in ecology, am a qualified staff nurse, and am an experienced performance and business manager."
|
cc Professor Jane Lewis, Dean of School: Biosciences "Dear Professor Petts, I hope you do not mind me writing to you personally. I am a part-time student on the herbal medicine (HM) BSc course, currently in my 3rd year of study. I have first class honours degree in ecology, am a qualified staff nurse, and am an experienced performance and business manager. I regard myself as scientist." "I would like to express to you my disappointment and frustration with my own studies at Westminster. I thought (erroneously, I have since discovered) that I was paying for a Bachelor of Science degree, and that science and scientific thinking would underpin my studies. How wrong I have been. Based on my experience at Westminster, two things really need to be done to restore credibility in the herbal medicine degree, viz. removing the antiscience and pseudoscience, and strengthening the scientific basis of both our core and herbal medicine modules. The current degree is confusing and infuriating in that it really does not know what it is." "Here is a quote from a handout (on ‘The Galenic Constitutional System in Practice’) given to 3rd year herbalists last semester: ‘Treating particular disease/conditions is more successful if the disease can be analysed in terms on hot, cold, wet and dry’. If I showed this to any modern (not 17th century) doctor they would be rolling around on the floor in hysterics and condemning this type of nonsense in the strongest possible language. I am ashamed to tell anybody what we are being taught. Is this clandestine teaching or is the University actually sanctioning this pre-scientific view of medicine?" Anti-science ideas need to be, not only banished from teaching material, but also robustly challenged every time they are raised by students (or lecturers) in the polyclinic or the classroom. But, constantly challenging anti-scientific and erroneous ideas is very wearing and wearying for me as a student, as I am sure it is for scientists on your staff. (I should say here that there are some excellent scientists who have supported and encouraged me in my studies at Westminster; Dr Gillian Shine in the core modules and Christopher Robbins in HM, leap to mind). academic institution. I should not feel threatened by challenging what I am taught when it is plainly pseudoscience or antiscience and my University should be supporting me in my challenge, which I am sure you will. |
And from the same student, this time addressed to Julie Whitehouse and copied to the dean, Jane Lewis (in 2009) [some details removed to preserve patient confidentiality].
|
… a patient attended who had been treated with a Reiki [typo for Reishi] mushroom tincture and another herbal tincture (about 6 herbs) by an HM clinic supervisor. The patient had also been advised to do ‘body brushing’ which I understand was for ‘detoxification’. This lady is being treated by an oncologist for [***] cancer and is currently undergoing chemotherapy. I do not believe her oncology team were informed before we initiated treatment and the bottles of tincture were not labelled with what they contained. I have serious ethical problems with treating anyone with cancer with herbs, but someone in the middle of chemotherapy? Not only are patients’ lives being put at risk, but students are not getting clear messages about the limitations of HM or the professional ethics involved in treating someone with cancer. I have seen patient files with ‘anti-mitotic’ or ‘anti-cancer’ herbs written in the notes. I question whether this is also bordering on the illegal. At the very least it betrays a naive belief that herbs can treat cancer. I was ignored earlier this year when I queried students being encouraged to go to a herbalist’s cancer seminars in Bristol (and she claimed to cure cancer) and this case highlights to me the dangers of Wmin condoning and teaching the ‘we treat people not diseases’ mantra. |
This second letter elicited a response from the university, and the response is worth looking at.
The response
|
2 What was done following the complaint 021209 Clinical Director met with the tutor. Reviewed notes. No indication that the patient was seeking ‘alternatives’ to chemo, nor that she was led to believe the prescription was designed to do other than support her coping with chemo which in her experience had previously been physically demanding and distressing. Procedures regarding communication with oncologists, informed consent, labeling of medicines need reviewing and reinforcing. Action by Course leader/herbal team. Report back to PC Exec 210110 151209 The student who (though she had not been present during this session, had objected to way this case was handled met with the course leader in the presence of the Senior Clinical supervisor and another tutor. The meeting was supportive rather than confrontational. The student was asked to reflect on the consequences of her (frequent) impulsive emailing and the time and effort she demands of others – and to consider the Code of Conduct she has signed. |
So the whistle-blowing student seems to have been patted on the head and told to shut up. Nevertheless the complaint had some effect, though not much.
|
050110 Course leader proposed to review current Polyclinic policies and procedures, and discuss current practice in cases of serious disease and how doctors are informed and patients consented
|
The response included "Extracts from Smith J, Rowan N & Sullivan (2000) Medicinal Mushrooms: Their therapeutic properties and current medical usage with special emphasis on cancer treatment” from Cancer Research UK."
|
In almost all the examples that will be discussed in this chapter the polysaccharides act mainly as immune- stimulants with little or no adverse drug reactions. Furthermore, several of these extracts have been shown to stimulate apoptosis in cancer cells (e.g. Fullerton et al., 2000). While there are examples where the mushroom polysaccharides have shown efficacy against specific types of cancer as monotherapy, the overwhelming successes have been demonstrated when they function together with proven and accepted chemotherapeutic agents.
|
I could not find that document at Cancer Research UK though there is a similar report, dated May 2002, "Medicinal Mushrooms: Their therapeutic properties and current medical usage with special emphasis on cancer treatments" by Smith, Rowan and Sullivan. It can be downloaded at the Cancer Research UK page, Medicinal Mushrooms and Cancer. That page, last updated 7 August 2006, lists John Smith BSc MSc PhD DSc FIBiol FRSE as Emeritus Professor of Applied Microbiology, University of Strathclyde. amd Chief Scientific Officer, MycoBiotech Ltd, Singapore, and Richard Sullivan BSc MD PhD as Head of Clinical Programmes, Cancer Research UK (a job he left in 2008). Professor John Smith is still Chief Scientific Advisor to Mycobiotech Inc, based in Singapore. This company sells various mushroom products. They are all marketed as “nutriceuticals” or “functional foods”, not as pharmaceuticals. These descriptions are a very common way of making medicinal claims for products, while describing them as foods to avoid the strict regulations about claims made for medicines.
It does not seem to me to be a good idea for Cancer Research UK to have advice on its web site from someone with a very obvious financial interest.
The quotations from the Smith report are obviously intended to defend the practice of prescribing mushrooms to people on chemotherapy. But the fact that in 2011, five years after the CRUK page, Mycobiotech still has no approved medicine approved for cancer speaks for itself. They sell Shiitake Herbal Soups. They also sell Essence of Shiitake which, they say, contains Lentinan, “which has been confirmed through research, to be an immuno-enhancer. Lentinan has been found to reduce tumour growth and to prolong the life of cancer patients”. That sounds to me like a rather strong medicinal claim for a “food”. Even Nutra-ingredients, the industry site for nutriceuticals, doesn’t claim much for it.
Now back to Westminster’s response to the student’s complaint.
|
I have found no evidence that herbal practitioners in the Polyclinic are making explicit claims to treat cancer. |
And, from David Peters.
|
DP**There is one item in the notes however which I think we need to comment on. While the paper-trail in all other respects shows that the herbal prescription was supportive, one herb in the prescription is categorised as ‘anti-tumour’. Although I am convinced after reviewing the notes and talking with the tutor involved, that the aim was to support the patient through her chemotherapy, this part of the prescription nonetheless signifies some ambivalence at least, about whether the aim was or was not to treat cancer
|
But then, from Julie Whitehouse
|
JW Yes there is antitumour as an action for many herbs and nutritional components – and several relevant actions including anything as general as anti- oxidant even – it doesn’t mean we are suggesting they are being used as treatment
|
It doesn’t take much reading between the lines to see the tension between Whitehouse and Peters. The former is very reluctant to give up the myths, the latter is slightly more cautious about claims to treat cancer.
Let’s be clear about one thing. The student was dead right. There is so little reliable information about mushrooms that neither Cochrane Reviews nor NCCAM has anything relevant to say about them. Antioxidants are a myth, much beloved by marketing people and "boosting the immune system" is the universal mantra of every advocate of magic medicine when they can’t think of anything else to make up. Why can’t Peters and Whitehouse admit it?
More complaints
This one is from a member of staff who teaches on the herbal medicine course. It was addressed to Julie Whitehouse and copied to the dean and vice-chancellor.(10 July 2009).
|
"During last week (5-9th May) I witnessed a member of the Herbal Team and a student dowsing with a pendulum to divine herbal drugs to prescribe for the student. When I approached and spoke, they defensively hid the pendulum and were clearly embarrassed. I discussed what they were doing. They freely said they were prescribing herbal medicine and cited other staff as their ‘authority’ and ‘instructors’. Diagnosing or prescribing by pendulum has no scientific credibility. Further, it is dangerous for prescribing as it both fails to identify any appropriate drugs (except by chance) and may select dangerous drugs for a patient. I know other staff have raised with you the teaching or use of such mediaeval and unscientific practices on the Wmin HM course." "I feel that such practice in the HM Course teaching or in the Polyclinic should be proscribed. I would like to suggest that you address and resolve this matter urgently. Dowsing is in conflict with the VC’s recent letter to SIH staff, specifically expecting more evidence of science within the teaching of CT Courses." "I expect that were the Department of Health to be aware of the unscientific teaching and promotion of practices like dowsing, (and crystals, iridology, astrology, and tasting to determine pharmacological qualities of plant extracts) on the Wmin HM Course, progress towards the Statutory Regulation of Herbal Medicine could be threatened." |
The writer seems to have overestimated the sense in the Department of Health. They were aware of these practices (I told them) but nevertheless went ahead with a silly form of statutory regulation.
The same lecturer wrote on 27 July 2009
|
"This happened with a supervisor, students and patient in the consultation room. The patient was invited to dowse her own "remedies" using a pendulum. A set of Bach Flower remedies (also proscribed in the HM Clinics) was placed in front of the patient and a pendulum was produced. On the basis of the dowsing, a prescription of ‘remedies’ was dispensed." "Although Julie says dowsing has been proscribed, she has been unable to present and document saying as such. Bach Flower Remedies have been proscribed for HM Clinics." |
Some of the replies were sent to me. Julie Whitehouse replied to the lecturer and Peter Davies on 10 August 2009
|
“I have written and circulated the text to be put into the handbook and have had approval from most members of the herbal team – but [the lecturer who complained] was not there at the time – hope he approves of the statement. It does not specifically say we do not dowse – but it does I think state clearly what we do – we surely do not want a list of what we don’t do – where would it end – there could be many things in a list of what we don’t do.”
|
So she explicitly refused to ban the use of dowsing in Westminster’s clinic. The lecturer replied, pointing out the unreasonableness of this attitude.
|
Dear Julie, I am afraid that I have not received any copy (home or University) of your ‘statement’ so cannot comment. Please resend me another copy. I don’t understand your not wanting ‘a list of what we don’t do – where would it end’. It is commonplace to have proscribed activities in both social and professional activities, and these are usually for clear reasons of safety and public good. Eg.: Herbal practice is constrained by the prohibitions in the Medicines Act 1968 and following, the maximum dosages under Schedule III of that Act, the prohibited herbal drugs under the MCA, Trading Standards regulations, etc. |
It seems that, despite the vice-chancellor’s assurance that the courses would become more scientific, there are still apologists for diagnosis with a pendulum, and for treating cancer with mushrooms at Westminster University.
This saga sounds only top characteristic. Complaints through official channels usually get you nowhere with big organisations. Sadly, the only way to get change is public embarrassment.
Some action from Vice-chancellor Geoftrey Petts is long overdue.
Follow-up
A kind reader sent me a copy of Brock, Whitehouse, Tewfik & Towell,. (2010) American skullcap (Scutellaria lateriflora): an ancient remedy for today’s anxiety, British Journal of Wellbeing1 (4), 25-30.. This is the paper that I described above, on the basis of the abstract, as "preliminary study".. Now that I’ve seen it I realise it isn’t study at all. They simply emailed 377 members of the National Institute of Medical Herbalists to ask what they thought of S. laterifloria. Only 62 replied (16%) and their anecdotes are listed in the paper. It is this sort of worthless information that gets herbal medicine a bad name.
10 August 2011. I notice that Professor Petts has replied to a letters sent to him by the Nightingale Collaboration. He said “Whilst I understand your concerns, colleagues of the School of Life Sciences where these courses are offered do not share them. They are not teaching pseudo-science, as you claim,…”. Well I know at least two member of the Life Sciences department who are very worried. One has now left and one has retired. The rest are presumably too scared to speak out. How he has the nerve to claim that they don’t teach pseudo-science all the teaching materials that have been revealed on this blog is hard to imagine. It is simply not true and he must know it. I find it deeply worrying when vice-chancellors say things which they know to be untrue.
The latest example to come to light is cited by Andy Lewis on his Quackometer blog
“There are some even odder characters too, such as Roy Riggs B.Sc who descibes himself as a “Holistic Geobiologist” and is “an “professional Earth Energy dowser”. He guest lectures at the London Westminster University’s School of Integrative Medicine and The Baltic Dowser’s Association of Lithuania.”
I do wonder who Professor Petts thinks he’s fooling.
Systems biology is all the rage, No surprise then, to see the University of Westminster advertising a job for a systems biologist in the The Department of Molecular and Applied Biosciences. Well, no surprise there -until you read the small print.
Much has been wriiten here about the University of Westminster, which remains the biggest provider of junk sciencne degrees in the UK, despite having closed two of them.
Senior Lecturer in Systems BiologyUniversity of Westminster – Department of Molecular and Applied Biosciences, School of Life SciencesCavendish Site Salary £37,886 – £50,751 (Inc. LWA) The Department of Molecular and Applied Biosciences wishes to appoint a Senior Lecturer in Systems Biology. The post-holder will teach on the undergraduate and postgraduate degree programmes within the School of Life Sciences, particularly in the areas of Molecular Biology, Bioinformatics and/or statistics, establish their own and participate in ongoing research programmes and undertake external income generation activities. The candidate should have an active interest in bridging the gap between western life sciences and Chinese medicine using emerging systems biology approaches, specifically in metabolomics and proteomics with a goal of developing novel diagnostic technologies facilitating the creation of a personalised approach to medical care. They should therefore be willing to work closely with colleagues in the life sciences as well as with clinicians and clinical researchers from within the East Asian medical tradition. The post is available from 1st October 2010 or as soon as possible thereafter. The closing date for applications, together with a short statement on why you believe you are suitable for the position and a description of your research plans, is Monday 6th September 2010. Interviews are expected to be held later in September. Administrative contact (for queries only): Tayjal Tailor (t.tailor1@wmin.ac.uk) Reference Number: 50000360 Closing Date: Friday 3 September 2010 |
A note about systems biology
Systems biology is about about how whole organs behave, as opposed to single cells or single molecules, It has to be the ultimate aim of biology. There is one case in which this has been done with some success, That is the modelling of the behaviour of the whole heart by Denis Noble and his colleagues in the Phyiology department (now gone) in Oxford. They adopted a bottom up approach. They measured the currents that flow though many sorts of ion channels in single cells from various parts of the heart, and how individual cells communicate with each other. Starting from this solid basis, together with a lot of computer power, they were able to model successfully a lot of phenomena that occur in the whole heart, but can’t be investigated in single cells. For example their work cast light on abnormal heart rhythms like ventricular fibrillation, and on the effect of drugs on heart rhythm.
This work was mostly done before the term ‘systems biology" thought of. It was called physiology. It is impressive work, and systems biology became a fashionable buzzword among research administrators and funding agencies. Despite the amount of money thrown at the problem, I’m not aware of any success that remotely approaches Noble’s.. One reason for that is that people have not been willing to put in the groundwork. In the case of the heart, the models were built on -many years of basic research on the electrophysiology of single heart cells. People have tried to model from the top down, without doing the spade work first. There has developed a perception that computing power can compensate for lack of basic knowledge about things work. It can’t. The usual aphorism applies: garbage in, garbage out.
Here’s an example, which eas noted in the diary pages for 29 June, 2008. While in Edinbuurgh, to give a talk to the European Conference on Mathematical and Theoretical Biology, I noticed a poster. It described an attempt to model on a computer the entire metabolic network of yeast.
“81 of the 662 intracellular concentrations were defined . . . The remainder were set to the median concentration of c. 0.2 mM.”
Ahem. We didn’t know the concentrations so we just made them up so we could run the program.
It’s interesting that even people in the business seem to realise that even that it isn’t living up to the hype. The Fixing proteomics web site shows why.
Put another way, if you try to run before you can walk, you risk falling falling on your face.
For these reasons, it seems to me that that most attempts at system biology have been disappointing (please correct me if I’m wrong)
Systems biology for Chinese medicine
If systems biology suffers from trying to run before it can walk in regular biology, where at least something is known about the functions of cells, how much more true that must be of Chinese medicine. In Chinese medicine almost all the treatments have never been tested properly in man. The odds are that most don’t work at all, and some are very poisonous (not to mention the cruelty and destruction of endangered species that is involved in making some of their more bizarre medicines). The idea that you can explain it with systems biology, is ludicrous in the extreme.
One can’t imagine any vaguely competent biologist who’d want to touch a project as bizarre as this with a bargepole.
Eastmedicine
This advertisement stems presumably from EASTmedicine is the University of Westminster’s research centre for East Asian Sciences and Traditions in Medicine. The proclaimed aims are to focus on “understanding, development and evaluation of East Asian medicines as living traditions”. The director of EASTmedicine, Volker Scheid, is a herbalist and acupuncturist and, as such, a firm believer in alternative medicine. When he isn’t at the University he has a private practice, the Traditional Acupuncture Centre, in London.
The website of his private practice makes some astonishing claims
"Acupuncture is effective in the treatment of numerous conditions including headache, migraine, digestive problems, menstrual disorders, indeterminate aches and pains, asthma, hayfever, stress, tiredness, depression and anxiety. Also commonly treated are chronic conditions such as arthritis, back pain, ulcerative colitis, irritable bowel syndrome, eczema, sinusitis, high blood pressure and repetitive strain injuries."
These claims simply cannot be justified by any worthwhile evidence. It will be interesting to see what Trading Standards make of them.
Dr Scheid describes himself as a "scholar physician". Physician seems a rather pretentious description for someone whose qualifications are stated to be PhD, MBAcC, FRCHM. But in similar vein he describes himself thus "I am one of the West’s leading experts on Chinese medical formulas and treatment strategies".
Although Scheid sells acupuncture treatments to patients, he seems ro be more anthropologist than medical. In a discussion of two acupuncture papers
"From the Perspective of the Anthropologist –
Volker Scheid, London, UK
From a perspective anchored in the cultural studies of science, technology and medicine my main interest in these papers is their status as cultural artifacts that provide access to the lifeworlds of a particular research community. If any, life-world debate and argument marks sites of contestation." Forsch Komplementärmed 2007;14:371–375
Scheid shows not the slightest interest in whether acupuncture works other than as a placebo. Since he is selling acupuncture, he presumably starts from the premise that it works.
Volker Scheid has had a £205,000 Wellcome Trust for the History of Medicine Project Grant: 2009 2012; Treating the Liver: Towards a Transnational History of East Asian Medicine; There’s nothing wrong with writing the history of long-outdated systems of medicine, though one could hardly imagine that the history would be very impartial, when it is written by a true believer. Another taste of his style can be found in his paper on Globalising Chinese Medical Understandings of Menopause. There is lots of rather pretentious stuff about culture, but very little about what actually works, Towards the end of the paper we come to the usual feeble excuse.
" . . once traditional medicines allow themselves to be evaluated by biomedical research methods, the odds against receiving fair treatment are heavily stacked against them."
The translation of that into plain English is something like ‘when we test our treatments properly we find they don’t work, so we blame the methods and carry on with selling them anyway’.
Judging from its web site, EASTmedicine does not to do any serious clinical trials to test whether the treaments work in man, They just know that they do. But they are hoping to add some spurious scientific background to their dubious claims by hiring someone to do compuations that will cast no light whatsoever on the question that really matters, Do they work or not?
The agenda is made clear by the statement
EASTmedicine seeks to describe and analyse the dynamics of these transformations with a specific view of managing their integration into contemporary health care.
So it is just yet another group of people pushing to have unproven and disproved treatments accepted by real medicine.
The University of Westminster appears to be determined to make itself the laughing stock by persisting in promoting junk science at a time when most other universities have realise that the harm done to their reputations is not worth the income it generates, Plenty of it has been revealed here.
The vice-chancellor of Westminster, Prof Geoffrey Petts, made into the pages of Private Eye (see Crystal balls. Professor Petts in Private Eye when he announced that he wouldn’t get rid of the junk, but would make it more ‘scientific’. Well, credit where it’s due, They have dropped homeopathy. see The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University For 2010 they still off ten different “BSc (Hons)” degrees in pre-scientific forms of medicine. It will take more than a bit od talk about systems biology to make anyone believe that these courses have anything to do with science.
For example, look at some slides from their lectures on “energy medicine”, Westminster University BSc: “amethysts emit high yin energy”
More make-believe from the University of Westminster. This time it’s Naturopathy , or
Why degrees in Chinese medicine are a danger to patients
The Dean of the School of the Life Sciences, Jane Lewis, is an entirely respectable marine biologist. She has had the thankless task of merging the real science with the alternative medicine in a single school. I phoned her to get a reaction
" outcome of merger of the school and trying to bring various parts of the school together" " "things are much more rigorous than they were".
DC: "Why don’t you just phase it out?"
"I’m not in a poition to do that. i move things forward as seems best -for the whole school I have to say". We’re retaining those bits thatI think have some good standing -I see NICE has approved the use of acupuncture for lower back pain and some other bits and pieces so I see acupuncture as something that does have some standing, andwe make sure it rigorously taught"
"DCHave you looked at the stuff on naturopathy?" "Are amethysts emit high Yin energy still taught?" " i don’t think so".
It seems, as so often in this case, that the senior people don’t really know what’s being taught under their noses. Prof
Lewis says she has not read about the background
to the (unusually) daft advice from NICE. Neither has she read Barker Bausell’s book on acupuncture research. If she had done any of these things,I suspect she would not have such a high opinion of it as appears to be the case.
Bait and switch. Astonishingly there is a now a whole organisation devoted to the respectabalisation of Traditional Chinese Medicine Good Practice in Traditional Chinese Medicine Research in the Post-genomic Era It sounds nice and sciencey but, as usual, they are trying to run before they can walk. The first thing has to be to do good clinical trials to find out if there is anything there to be investigated. If, and only if, this is the case, would there be any case for fancy talk about "proteomics"
and "the post-genomic era".
I do hope that no funding agency would be fooled into parting with money on the basis of the present vacuous rhetoric.
Professor Lewis said that I have I have quoted things like "amethysts emit high Yin energy" out of context. There is a simple solution to that. I have asked Westminster to make available the entire contents of the courses. Then we shall all be able to see the context of what their sudents are being taught.
Follow up
A brief report of this matter has appeared in Times Higher Education. In a statement, the University of Westminster says “its research into Chinese medicine is following the lead of “top research institutions”. I’m not aware of anyhting quite like this from anywhere else. In any case, Westminster should be able to think for themselves.

