Trading Standards
This post recounts a complicated story that started in January 2009, but has recently come to what looks like a happy ending. The story involves over a year’s writing of letters and meetings, but for those not interested in the details, I’ll start with a synopsis.
Synopsis of the synopsis
In January 2009, a course in "integrated medicine" was announced that, it was said, would be accredited by the University of Buckingham. The course was to be led by Drs Rosy Daniel and Mark Atkinson. So I sent an assessment of Rosy Daniel’s claims to "heal" cancer to Buckingham’s VC (president), Terence Kealey, After meeting Karol Sikora and Rosy Daniel, I sent an analysis of the course tutors to Kealey who promptly demoted Daniel, and put Prof Andrew Miles in charge of the course. The course went ahead in September 2009. Despite Miles’ efforts, the content was found to be altogether too alternative. The University of Buckingham has now terminated its contract with the "Faculty of Integrated Medicine", and the course will close. Well done.Buckingham.
Synopsis
- January 2009. I saw an announcement of a Diploma in Integrated Medicine, to be accredited by the University of Buckingham (UB). The course was to be run by Drs Rosy Daniel and Mark Atkinson of the College of Integrated Medicine, under the nominal directorship of Karol Sikora (UB’s Dean of Medicine). I wrote to Buckingham’s vice-chancellor (president), Terence Kealey, and attached a reprint of Ernst’s paper on carctol, a herbal cancer ‘remedy’ favoured by Daniiel.
- Unlike most vice-chancellors, Kealey replied at once and asked me to meet Sikora and Daniel. I met first Sikora alone, and then, on March 19 2009, both together. Rosy Daniel gave me a complete list of the speakers she’d chosen. Most were well-known alternative people, some, in my view, the worst sort of quack. After discovering who was to teach on the proposed course, I wrote a long document about the proposed speakers and sent it to the vice-chancellor of the University of Buckingham, Terence Kealey on March 23rd 2009.. Unlike most VCs, he took it seriously. At the end of this meeting I asked Sikora, who was in nominal charge of the course, how many of the proposed tutors he’d heard of. The answer was "none of them"
- Shortly before this meeting, I submitted a complaint to Trading Standards about Rosy Daniel’s commercial site, HealthCreation, for what seemed to me to be breaches of the Cancer Act 1939, by claims made for Carctol. Read the complaint.
- On 27th April 2009, I heard from Kealey that he’d demoted Rosy Daniel from being in charge of the Diploma and appointed Andrew Miles, who had recently been appointed as Buckingham’s Professor of Public Health Education and Policy &Associate Dean of Medicine (Public Health). Terence Kealey said "You’ve done us a good turn, and I’m grateful". Much appreciated. Miles said the course “needs in my view a fundamental reform of content. . . “
- Although Rosy Daniel had been demoted, she was still in charge of delivering the course at what had, by this time, changed its name to the Faculty of Integrated Medicine which, despite its name, is not part of the university.
- Throughout the summer I met Miles (of whom more below) several times and exchanged countless emails, but still didn’t get the revised list of speakers. The course went ahead on 30 September 2009. He also talked with Michael Baum and Edzard Ernst.
- By January 2010, Miles came to accept that the course was too high on quackery to be a credit to the university, and simply fired The Faculty of Integrated Medicine. Their contract was not renewed. Inspection of the speakers, even after revision of the course, shows why.
- As a consequence, it is rumoured that Daniel is trying to sell the course to someone else. The University of Middlesex, and unbelievably, the University of Bristol, have been mentioned, as well as Thames Valley University, the University of Westminster, the University of Southampton and the University of East London. Will the VCs of these institutions not learn something from Buckingham’s experience? It is to be hoped that they would at the very least approach Buckingham to ask pertinent questions? But perhaps a more likely contender for an organisation with sufficient gullibility is the Prince of Wales newly announced College of Integrated Medicine. [but see stop press]
The details of the story
The University of Buckingham (UB) is the only private university in the UK. Recently it announced its intention to start a school of medicine (the undergraduate component is due to start in September 2011). The dean of the new school is Karol Sikora.
Karol Sikora shot to fame after he appeared in a commercial in the USA. The TV commercial was sponsored by a far-right Republican campaign group, “Conservatives for Patients’ Rights” It designed to prevent the election of Barack Obama, by pouring scorn on the National Health Serrvice. A very curious performance. Very curious indeed. And then there was a bit of disagreement about the titles that he claimed to have.
As well as being dean of medicine at UB. Karol Sikora is also medical research director of CancerPartnersUK. a private cancer treatment company. He must be a very busy man.
Karol Sikora’s attitude to quackery is a mystery wrapped in an enigma. As well as being a regular oncologist, he is also a Foundation Fellow of that well known source of unreliable information, The Prince of Wales Foundation for Integrated Health. He spoke at their 2009 conference.
In the light of that, perhaps it is not, after all, so surprising thet the first action of UB’s medical school was to accredit a course a Diploma in Integrated Medicine. This course has been through two incarnations. The first prospectus (created 21 January 2009) advertised the course as being run by the British College of Integrated Medicine.But by the time that UB issued a press release in July 2009, the accredited outfit had changed its name to the Faculty of Integrated Medicine That grand title makes it sound like part of a university. It isn’t.

Rosy Daniel runs a company, Health Creation which, among other things, recommended a herbal concoction. Carctol. to "heal" cancer, . I wrote to Buckingham’s vice-chancellor (president), Terence Kealey, and attached a reprint of Ernst’s paper on Carctol. . Unlike most university vice-chancellors, he took it seriously. He asked me to meet Karol Sikora and Rosy Daniel to discuss it. After discovering who was teaching on this course, I wrote a document about their backgrounds and sent it to Terence Kealey. The outcome was that he removed Rosy Daniel as course director and appointed in her place Andrew Miles, with a brief to reorganise the course. A new prospectus, dated 4 September 2009, appeared. The course is not changed as much as I’d have hoped, although Miles assures me that while the lecture titles themselves may not have changed, he had ordered fundamental revisions to the teaching content and the teaching emphases.
In the new prospectus the British College of Integrated Medicine has been renamed as the Faculty of Integrated Medicine, but it appears to be otherwise unchanged. That’s a smart bit of PR. The word : “Faculty” makes it sound as though the college is part of a university. It isn’t. The "Faculty" occupies some space in the Apthorp Centre in Bath, which houses, among other things, Chiropract, Craniopathy (!) and a holistic vet,
The prospectus now starts thus.

The Advisory Board consists largely of well-know advocates of alternative medicine (more information about them below).

Most of these advisory board members are the usual promoters of magic medicine. But three of them seem quite surprising,Stafford Lightman, Nigel Sparrow and Nigel Mathers.
Stafford Lightman? Well actually I mentioned to him in April that his name was there and he asked for it to be removed, on the grounds that he’d had nothing to do with the course. It wasn’t removed for quite a while, but the current advisory board has none of these people. Nigel Sparrow and Nigel Mathers, as well as Lightman, sent letters of formal complaint to Miles and Terence Kealey, the VC of Buckingham, to complain that their involvement in Rosy Daniel’s set-up had been fundamentally misrepresented by Daniel. With these good scientists having extricated themselves from Daniel’s organisation, the FIM has only people who are firmly in the alternative camp (or quackery, as i’d prefer to call it). For example, people like Andrew Weil and George Lewith.
Andrew Weil, for example, while giving his address as the University of Arizona, is primarily a supplement salesman. He was recently reprimanded by the US Food and Drugs Administration
“Advertising on the site, the agencies said in the Oct. 15 letter, says “Dr. Weil’s Immune Support Formula can help maintain a strong defense against the flu” and claims it has “demonstrated both antiviral and immune-boosting effects in scientific investigation.”
The claims are not true, the letter said, noting the “product has not been approved, cleared, or otherwise authorized by FDA for use in the diagnosis, mitigation, prevention, treatment, or cure of the H1N1 flu virus.”
This isn’t the first time I’ve come across people’s names being used to support alternative medicine without the consent of the alleged supporter. There was, for example, the strange case of Dr John Marks and Patrick Holford.
Misrepresentation of this nature seems to be the order of the day. Could it be that people like Rosy Daniel are so insecure or, indeed, so unimportant within the Academy in real terms (where is there evidence of her objective scholarly or clinical stature?), that they seek to attach themselves, rather like limpets to fishing boats, to people of real stature and reputation, in order to boost their own or others’ view of themselves by a manner of proxy?
The background
When the course was originally proposed, a brochure appeared. It said accreditation by the University of Buckingham was expected soon.
Not much detail appeared in the brochure, Fine words are easy to write but what matters is who is doing th teaching. So I wrote to the vice-chancellor of Buckingham, Terence Kealey. I attached a reprint of Ernst’s paper on carctol, a herbal cancer ‘remedy’ favoured by Daniel (download the cached version of her claims, now deleted).
Terence Kealey
Kealey is regarded in much of academia as a far-right maverick, because he advocates ideas such as science research should get no public funding,and that universities should charge full whack for student fees. He has, in fact, publicly welcomed the horrific cuts being imposed on the Academy by Lord Mandelson. His piece in The Times started
“Wonderful news. The Government yesterday cut half a billion pounds from the money it gives to universities”
though the first comment on it starts
"Considerable accomplishment: to pack all these logical fallacies and bad metaphors in only 400 words"
He and I are probably at opposite ends of the political spectrum. Yet he is the only VC who has been willing to talk about questions like this. Normally letters to vice-chancellors about junk degrees go unanswered. Not so with Kealey. I may disagree with a lot of his ideas, but he is certainly someone you can do business with.
Kealey responded quickly to my letter, sent in January 2009, pointing out that Rosy Daniel’s claims about Carctol could not be supported and were possibly illegal. He asked me to meet Sikora and Daniel. I met first Sikora alone, and then, on March 19 2009, both together. Rosy Daniel gave me a complete list of the speakers she’d chosen to teach on this new Diploma on IM.
After discovering who was to teach on the proposed course, I wrote a long document about the proposed speakers and sent it to Terence Kealey on March 23rd 2009. It contained many names that will be familiar to anyone who has taken an interest in crackpot medicine, combined with a surprisingly large element of vested financial interests. Unlike most VCs, Kealey took it seriously.
The remarkable thing about this meeting was that I asked Sikora how many names where familiar to him on the list of people who had been chosen by Rosy Daniel to teach on the course. His answer was "none of them". Since his name and picture feature in all the course descriptions, this seemed like dereliction of duty to me.
After seeing my analysis of the speakers, Terence Kealey reacted with admirable speed. He withdrew the original brochure, demoted Rosy Daniel (in principle anyway) and brought in Prof Andrew Miles to take responsibility for the course. This meant that he had to investigate the multiple conflicts of interests of the various speakers and to establish some sort of way forward in the ‘mess’ of what had been agreed before Miles’ appointment to Buckingham
Andrew Miles.
Miles is an interesting character, a postdoctoral neuroendocrinologist, turned public health scientist. I’d come across him before as editor-in-chief of the Journal of Evaluation in Clinical Practice This is a curious journal that is devoted mainly to condemning Evidence Based Medicine. Much of its content seems to be in a style that I can only describe as post-modernist-influenced libertarian.
The argument turns on what you mean by ‘evidence’ and, in my opinion, Miles underestimates greatly the crucial problem of causality, a problem that can be solved only by randomisation, His recent views on the topic can be read here.
An article in Miles’ journal gives its flavour: "Andrew Miles, Michael Loughlin and Andreas Polychronis, Medicine and evidence: knowledge and action in clinical practice". Journal of Evaluation in Clinical Practice 2007, 13, 481–503 [download pdf]. This paper launches an attack on Ben Goldacre, in the following passage.
“Loughlin identifies Goldacre [36] as a particularly luminous example of a commentator who is able not only to combine audacity with outrage, but who in a very real way succeeds in manufacturing a sense of having been personally offended by the article in question. Such moralistic posturing acts as a defence mechanism to protect cherished assumptions from rational scrutiny and indeed to enable adherents to appropriate the ‘moral high ground’, as well as the language of ‘reason’ and ‘science’ as the exclusive property of their own favoured approaches. Loughlin brings out the Orwellian nature of this manoeuvre and identifies a significant implication.”
"If Goldacre and others really are engaged in posturing then their primary offence, at least according to the Sartrean perspective adopted by Murray et al. is not primarily intellectual, but rather it is moral. Far from there being a moral requirement to ‘bend a knee’ at the EBM altar, to do so is to violate one’s primary duty as an autonomous being.”
This attack on one of my heroes was occasioned because he featured one of the most absurd pieces of post-modernist bollocks ever, in his Guardian column in 2006. I had a go at the same paper on this blog, as well as an earlier one by Christine Barry, along the same lines. There was some hilarious follow-up on badscience.net. After this, it is understandable that I had not conceived a high opinion of Andrew Miles. I feared that Kealey might have been jumping out of the frying pan into the fire.
After closer acquaintance I have changed my mind, In the present saga Andrew Miles has done an excellent job. He started of sending me links to heaven knows how many papers on medical epistemology, to Papal Encyclicals on the proposed relationship between Faith and Reason and on more than one occasion articles from the Catholic Herald (yes, I did read it). This is not entirely surprising, as Miles is a Catholic priest as well as a public health academic, so has two axes to grind. But after six months of talking, he now sends me links to junk science sites of the sort that I might get from, ahem, Ben Goldacre.
Teachers on the course
Despite Andrew Miles best efforts, he came in too late to prevent much of the teaching being done in the parallel universe of alternative medicine, The University of Buckingham had a pre-Miles, legally-binding contract (now terminated) with the Faculty of Integrated Medicine, and the latter is run by Dr Rosy Daniel and Dr Mark Atkinson. Let’s take a look at their record.
Rosy Daniel BSc, MBBCh
Dr Rosy Daniel first came to my attention through her commercial web site, Health Creation. This site, among other things, promoted an untested herbal concoction, Carctol, for "healing" cancer.
Carctol: Profit before Patients? is a review by Edzard Ernst of the literature, such as it is, and concludes
Carctol and the media hype surrounding it must have given many cancer patients hope. The question is whether this is a good or a bad thing. On the one hand, all good clinicians should inspire their patients with hope [6]. On the other hand, giving hope on false pretences is cruel and unethical. Rosy Daniel rightly points out that all science begins with observations [5]. But all science then swiftly moves on and tests hypotheses. In the case of Carctol, over 20 years of experience in India and almost one decade of experience in the UK should be ample time to do this. Yet, we still have no data. Even the small number of apparently spectacular cases observed by Dr. Daniel have not been published in the medical literature.
On this basis I referred Health Creation to Trading Standards officer for a prima facie breach of the Cancer Act 1939. ]Download the complaint document]. Although no prosecution was brought by Trading Standards, they did request changes in the claims that were being made. Here is an example.
A Google search of the Health Creation site for “Carctol” gives a link
Dr Daniel has prescribed Carctol for years and now feels she is seeing a breakthrough. Dr Daniel now wants scientists to research the new herbal medicine
But going to the link produces
Access denied.
You are not authorized to access this page.
You can download the cached version of this page, which shows the sort of claims that were being made before Trading Standards Officers stepped in. There are now only a few oblique references to Carctol on the Health Creation site, e.g. here..
Both Rosy Daniel and Karol Sikora were speakers at the 2009 Princes’s Foundation Conference, in some odd company.
Mark Atkinson MBBS BSc (Hons) FRIPH
Dr Mark Atkinson is co-leader of the FiM course. He is also a supplement salesman, and he has promoted the Q-link pendant. The Q-link pendant is a simple and obvious fraud designed to exploit paranoia about WiFi killing you. When Ben Goldacre bought one and opened it. He found
“No microchip. A coil connected to nothing. And a zero-ohm resistor, which costs half a penny, and is connected to nothing.”
Nevertheless, Mark Atkinson has waxed lyrical about this component-free device.
“As someone who used to get tired sitting in front of computers and used to worry about the detrimental effects of external EMF’s, particularly as an avid user of mobile phones, I decided to research the various devices and technologies on the market that claim to strengthen the body’s subtle energy fields. It was Q Link that came out top. As a Q link wearer, I no longer get tired whilst at my computer, plus I’m enjoying noticeably higher energy levels and improved mental performance as a result of wearing my Q Link. I highly recommend it.” Dr Mark Atkinson, Holistic Medical Physician
Mark Atkinson is also a fan of Emo-trance. He wrote, In Now Magazine,
"I wanted you to know that of all the therapies I’ve trained in and approaches that I have used (and there’s been a lot) none have excited me and touched me so deeply than Emotrance."
"Silvia Hartmann’s technique is based on focusing your thoughts on parts of your body and guiding energy. It can be used for everything from insomnia to stress. The good news is that EmoTrance shows you how to free yourself from these stuck emotions and release the considerable amounts of energy that are lost to them."
Aha so this particular form of psychobabble is the invention of Silvia Hartmann. Silvia Hartmann came to my attention because her works feature heavily in on of the University of Westminster’s barmier “BSc” degrees, in ‘naturopaths’, described here. She is fanous, apart from Emo-trance, for her book Magic, Spells and Potions
“Dr Hartmann has created techniques that will finally make magic work for you in ways you never believed to be possible.”
Times Higher Education printed a piece with the title ‘Energy therapy’ project in school denounced as ‘psychobabble’. They’d phoned me a couple of days earlier to see whether I had an opinion about “Emotrance”. As it happens, I knew a bit about it because it had cropped up in a course given at, guess where, the University of Westminster . It seems that a secondary school had bought this extreme form of psychobabble. The comments on the Times Higher piece were unusually long and interesting.
It turned out that the inventor of “Emotrance”, Dr Silvia Hartmann PhD., not only wrote books about magic spells and potions, but also that her much vaunted doctorate had been bought from the Universal Life Church, current cost $29.99.
The rest of the teachers
The rest of the teachers on the course, despite valiant attempts at vetting by Andrew Miles, includes many names only too well-known to anybody who has taken and interest in pseudo-scientific medicine. Here are some of them.
Damien Downing:, even the Daily Mail sees through him. Enough said.
Kim Jobst, homoepath and endorser of the obviously fraudulent Q-link
pendant. His Plaxo profile says
About Kim A. Jobst
Consultant, Wholystic Care Physician [sic!] , Medical Homoeopath, Specialist in Neurodegeneration and Dementia, using food state nutrition, diet and lifestyle to facilitate Healing and Growth;
Catherine Zollman, Well known ally of HRH and purveyer of woo.
Harald Walach, another homeopath, fond of talking nonsense about "quantum effects".
Nicola Hembry, a make-believe nutritionist and advocate of vitamin C and laetrile for cancer
Simon Mills, a herbalist who is inclined to diagnoses like “hot damp”, ro be treated with herbs that tend to “cool and dry.”
David Peters, of the University of Westminster. Enough said.
Nicola Robinson of Thames Valley University. Advocate of unevidenced treatmsnts.
Michael Dixon, of whom more here.
And last but not least,
Karol Sikora.
The University of Buckingham removes accreditation of the Faculty of Integrated Medicine
The correspondence has been long and, at times, quite blunt. Here are a few quotations from it, The University of Buckingham, being private, is exempt from the Freedom of Information Act (2000) but nevertheless they have allowed me to reproduce the whole of the correspondence. The University, through its VC, Terence Keeley, has been far more open than places that are in principle subject to FOIA, but which, in practice, always try to conceal material. I may post the lot, as time permits, but meanwhile here are some extracts. They make uncomfortable reading for advocates of magic medicine.
Miles to Daniel, 8 Dec 2009
” . . . now that the University has taken his [Sikora’s] initial advice in trialing the DipSIM and has found it cost-ineffective, the way forward is therefore to alter that equation through more realistic financial contribution from IHT/FIM at Bath or to view the DipSIM as an experiment that has failed and which must give way to other more viable initiatives."
"The University is also able to confirm that we hold no interest in jointly developing any higher degrees on the study of IM with IHT/FIM at Bath. This is primarily because we are developing our own Master’s degree in Medicine of the Person in collaboration with various leading international societies and scholars including the WHO and which is based on a different school of thought. "
Miles to Daniel 15 Dec 2009
"Dear Rosy
It appears that you have not fully assimilated the content of my earlier e-mails and so I will reiterate the points I have already made to you and add to them.
The DipSIM is an external activity – in fact, it is an external collaboration and nothing more. It is not an internal activity and neither is it in any way part of the medical school and neither will it become so and so the ‘normal rules’ of academic engagement and scholarly interchange do not apply. Your status is one of external collaborator and not one of internal or even visiting academic colleague. There is no “joint pursuit” of an academically rigorous study of IM by UB and IHT/FIM beyond the DipSIM and there are no plans, and never have been, for the “joint definition of research priorities” in IM. The DipSIM has been instituted on a trial basis and this has so far shown the DipSIM to be profoundly cost-ineffective for the University. You appear to misunderstand this – deliberately or otherwise."
Daniel to Miles 13 Jan 2010
"However, I am aware that weather permitting you and Karol will be off to the Fellows meeting for the newly forming National College (for which role I nominated you to Dr Michael Dixon and Prof David Peters.)
I have been in dialogue with Michael and Boo Armstrong from FIH and they are strongly in favour of forming a partnership with FIM so that we effectively become one of many new faculties within the College (which is why we change our name to FIM some months ago).
I have told Michael about the difficulties we are having and he sincerely hopes that we can resolve them so that we can all move forward as one. "
Miles to Daniel 20 Jan 2010
"Congratulations on the likely integration of your organisation into the new College of Integrative Health which will develop out of the Prince’s Foundation for Integrated Health. This
will make an entirely appropriate home for you for the longer term.Your image of David Colquhoun "alive and kicking" as the Inquisitor General, radiating old persecutory energy and believing "priestess healers" (such as you describe youself) to be best "tortured, drowned and even burnt alive", will remain with me, I suspect, for many years to come (!). But then, as the Inquisitor General did say, ‘better to burn in this life than in the next’ (!). Overall, then, I reject your conclusion on the nature of the basis of my decision making and playfully suggest that it might form part of the next edition of Frankfurt’s recent volume ["On Bullshit] http://press.princeton.edu/titles/7929.html I hope you will forgive my injection of a little academic humour in an otherwise formal and entirely serious communication.
The nature of IM, with its foundational philosophy so vigorously opposed by mainstream medicine and the conitnuing national and international controversies which engulf homeopaths, acupuncturists, herbalists, naturopaths, transcendental meditators, therapeutic touchers, massagers, reflexologists, chiropractors, hypnotists, crystal users, yoga practitioners, aromatherapists, energy channelers, chinese medicine practitioners et al, can only bring the University difficulties as we seek to establish a formal and internationally recognised School of Medicine and School of Nursing.
I do not believe my comments in relation to governance at Bath are "offensive". They are, on the contrary, entirely accurate and of concern to the University. There have been resignations at senior level from your Board due to misrepresentation of your position and there has been a Trading Standards Authority investigation into further instances of misrepresentation. I am advised that an audit is underway of your compliance with the Authority’s instructions. You have therefore not dealt with my concerns, you have merely described them as "offensive".
I note from your e-mail that you are now in discussions with other universities and given the specific concerns of the University of Buckingham which I have dealt with exhaustively in this and other correspondences and the incompatibility of the developments at UB with the DipSIM and your own personal ambitions, etc., I believe you to have taken a very wise course and I wish you well in your negotiations. In these circumstances I feel it appropriate to enhance those negotiations by confirming that the University of Buckingham will not authorise the intake of a second cohort of students and that the relationship between IHT and the University will cease following the graduation of those members of the current course that are successful in their studies – the end of February 2011."
From Miles 2 Feb 2010
"Here is the list of teachers – you can subtract me (I withdrew from teaching when the antics ay Bath started) and also Professor John Cox (Former President of The Royal College of Psychiatrists and Former Secretary General of the World Psychiatric Association) who withdrew when he learned of some of the stuff going on…. Karol Sikora continues to teach. Michael Loughlin and Carmel Martin are both good colleagues of mine and, I can assure you – taught the students solid stuff! Michael taught medical epistemology and Carmel the emerging field of systems complexity in health services (Both of them have now withdrawn from teaching commitments).
The tutors shown are described by Rosy as the finest minds in IM teaching in the country. I interviewed tham all personally on (a) the basis of an updated CV & (b) via a 30 min telephone interview with me personally. Some were excluded from teaching because they were not qualified to do so academically (e.g. Boo Armstrong, Richard Falmer, not even a first degree, etc, etc., but gave a short presentation in a session presided over by an approved teacher) and others were approved because of their academic qualifications, PhD, MD, FRCP etc etc etc) and activity within the IM field. Each approved teacher was issued with highly specific teaching guidance form me (no bias, reference to opposing schools of thought, etc etc) and each teacher was required to complete and sign a Conflicts of Interest form. All of these documentations are with me here. Short of all this governance it’s impossible to bar them from teaching because who else would then do it?! Anyway, the end is in sight – Hallelujah! "
From Miles 19 Feb 2010
"Dear David
Just got back to the office after an excellent planning meeting for the new Master’s Degree in Person-centred Medicine and a hearty (+ alcoholic) lunch at the Ath! Since I shall never be a FRS, the Ath seems to me the next best ‘club’ (!). Michael Baum is part of the steering committee and you might like to take his thoughts on the direction of the programme. Our plans may even find their way into your Blog as an example of how to do things (vs how not to do things, i.e. CAM, IM, etc!). This new degree will sit well alongside the new degrees in Public Health – i.e. the population/utilitarian outlook of PH versus the individual person-centred approach., etc. "
And an email from a senior UB spokesperson
"Rumour has it that now that Buckingham has dismissed the ‘priestess healer of Bath’, RD [Rosy Daniel] , explorations are taking place with other universities, most of which are subject to FoI request from DC at the time of writing. Will these institutions have to make the same mistakes Buckingham did before taking the same action? Rumour also has it that RD changed the name of her institution to FIM in order to fit neatly into the Prince’s FIH, a way, no doubt, of achieving ‘protection’ and ‘accreditation’ in parallel with particularly lucrative IM ‘education’ (At £9,000 a student and with RD’s initial course attracting 20 mainly GPs, that’s £180,00 – not bad business…. And Buckingham’s ‘share of this? £12,000!”
The final bombshell; even the Prince of Wales’ FIH rejects Daniel and Atkinson?
Only today (31 March) I was sent, from a source that I can’t reveal, an email which comes from someone who "represent the College and FIH . . . ".. This makes it clear that the letter comes from the Prince of Wales’ Foundation for Integrated Health
|
Dr Rosy Daniel BSc MBBCh Director of the Faculty of Integrated Medicine Medical Director Health Creation 30th March 2010 RE: Your discussion paper and recent correspondence Thank you for meeting with [XXXXXX] and myself this evening to discuss your proposals concerning a future relationship between your Faculty of Integrated Medicine and the new College. As you know, he and I have been asked to represent the College and FIH in this matter. We are aware of difficulties facing your organisations and the FIM DipSIM course. As a consequence of these, it is not possible for the College to enter into an association with you, any of your organisations nor the DipSIM course at the present time. It would, therefore, be wrong to represent to others that any such association has been agreed. You will appreciate that, in these circumstances, you will not receive an invitation to the meeting of 15th April 2010 nor to other planned events. I am sorry to disappoint you in this matter. Yours sincerely |
Conclusions
I’ll confess to feeling almost a little guilty for having appeared to persecute the particular individuals involved in thie episode. But patients are involved and so is the law, and both of these are more important than individuals, The only unfair aspect is that, while it seems that even the Prince of Wales’ Foundation for Integrated Health has rejected Daniel and Atkinson, that Foundation embraces plenty of people who are just as deluded, and potentially dangerous, as those two. The answer to that problem is for the Prince to stop endorsing treatments that don’t work.
As for the University of Buckingham. Well, despite the ‘right wing maverick’ Kealey and the ‘anti-evidence’ Miles, I really think they’ve done the right thing. They’ve listened, they’ve maintained academic rigour and they’ve released all information for which I asked and a lot more. Good for them, I say.
Follow-up
15 April 2010. This story was reported by Times Higher Education, under the title “It’s terminal for integrated medicine diploma“. That report didn’t attract comments. But on 25th April Dr Rosy Daniel replied with “‘Terminal’? We’ve only just begun“. This time there were some feisty responses. Dr Daniel really should check her facts before getting into print.
3 March 2011. Unsurprisingly, Dr Daniel is up and running again, under the name of the British College of Integrated Medicine. The only change seems to be that Mark Atkinson has jumped ship altogether, and, of course, she is now unable to claim endorsement by Buckingham, or any other university. Sadly, though, Karol Sikora seems to have learned nothing from the saga related above. He is still there as chair of the Medical Advisory Board, along with the usual suspects mentioned above.
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
More boring politics, but it matters. The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register should normally be through a Bachelor degree with Honours
For the background on this appalling report, see earlier posts.
A very bad report: gamma minus for the vice-chancellor
The Times (blame subeditor for the horrid title), and some follow up on the Times piece
The Health Professions Council breaks its own rules: the result is nonsense
Chinese medicine -acupuncture gobbledygook revealed
Consultation opens on the Pittilo report: help stop the Department of Health making a fool of itself
Why degrees in Chinese medicine are a danger to patients
The Department of Health consultation shuts on November 2nd. If you haven’t responded yet, please do. It would be an enormous setback for reason and common sense if the government were to give a stamp of official approval to people who are often no more than snake-oil salesman.
Today I emailed my submission to the Pittilo consultation to the Department of Health, at HRDListening@dh.gsi.gov.uk
The submission
I sent the following documents, updated versions of those already posted earlier.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
- An example of dangerous (and probably illegal) claims that are routinely made by TCM practitioners [download pdf]f
I also completed their questionnaire, despite its deficiencies. In case it is any help to anyone, this is what I said:
The questionnaire
Q1: What evidence is there of harm to the public currently as a result of the activities of acupuncturists, herbalists and traditional Chinese medicine practitioners? What is its likelihood and severity?
Harm
No Harm
Unsure
Comment
The major source of harm is the cruel deception involved in making false claims of benefit to desperate patients. This applies to all three.
In the case of herbal and TCM there is danger from toxicity because herbal preparations are unstandardised so those that do contain an active ingredient are given in an unknown dose. This is irresponsible and dangerous (but would not be changed by the proposals for regulation).
In addition TCM suffers from recurrent problems of contamination with heavy metals, prescription drugs and so on. Again this would not be the business of the proposed form of regulation.
Q2: Would this harm be lessened by statutory regulation? If so, how?
Yes
No
Unsure
The proposed form of regulation would be no help at all. The HPC has already said that it is not concerned with whether or not the drug works, and, by implication, does not see itself as preventing false health claims (just as the GCC doesn’t do this). False claims are the responsibility of Trading Standards who are meant to enforce the Consumer Protection Unfair Trading Regulations (May 2008), though they do not at present enforce them very effectively. Also Advertisng Standards. The proposed regulation would not help, and could easily hinder public safety as shown by the fact that the GCC has itself been referred to the Advertisng Standards Authority.
The questions of toxicity and contamination are already the responsibility of Trading Standards and the MHRA. Regulation by the HPC would not help at all. The HPC is not competent to deal with such questions.
Q3: What do you envisage would be the benefit to the public, to practitioners and to businesses, associated with introducing statutory regulation?
Significant benefit
Some benefit
No benefit
Unsure
This question is badly formulated because the answer is different according to whether you are referring to the public, to practitioners or to businesses.
The public would be endangered by the form of regulation that is proposed, as is shown very clearly by the documents that I have submitted separately.
In the case of practitioners and businesses, there might be a small benefit, if the statutory regulation gave the impression that HM and TCM had government endorsement and must therefore be safe and effective.
There is also one way that the regulation could harm practitioners and businesses. If the HPC received a very large number of complaints about false health claims, just as the GCC has done recently, not only would it cost a large amount of money to process the claims, but the attendant bad publicity could harm practitioners. It is quite likely that this would occur since false claims to benefit sick people are rife in the areas of acupuncture, HM and TCM.
Q4: What do you envisage would be the regulatory burden and financial costs to the public, to practitioners, and to businesses, associated with introducing statutory regulation? Are these costs justified by the benefits and are they proportionate to the risks? If so, in what way?
Justified
Not Justified
Unsure
Certainly not justified. Given that I believe that the proposed form of regulation would endanger patients, no cost at all would be justified. But even if there were a marginal benefit, the cost would be quite unjustified. The number of practitioners involved is very large. It would involve a huge expansion of an existing quango, at a time when the government is trying to reduce the number of quangos. Furthermore, if the HPC were flooded with complaints about false health claims, as the GCC has been, the costs in legal fees could be enormous.
Q5: If herbal and TCM practitioners are subject to statutory regulation, should the right to prepare and commission unlicensed herbal medicines be restricted to statutorily regulated practitioners?
Yes
No
Unsure
I don’t think it would make much difference. The same (often false) ideas are shared by all HM people and that would continue to be the same with or without SR.
Q6: If herbal and TCM practitioners are not statutorily regulated, how (if at all) should unlicensed herbal medicines prepared or commissioned by these practitioners be regulated?
They could carry on as now, but the money that would have been spent on SR should instead be used to give the Office of Trading Standards and the MHRA the ability to exert closer scrutiny and to enforce more effectively laws that already exist. Present laws, if enforced, are quite enough to protect the public.
Q7: What would be the effect on public, practitioners and businesses if, in order to comply with the requirements of European medicines legislation, practitioners were unable to supply manufactured unlicensed herbal medicines commissioned from a third party?
Significant effect
Some effect
No effect
Unsure
European laws,especialliy in food area, are getting quite strict about the matters of efficacy. The proposed regulation, which ignores efficacy, could well be incompatible with European law, if not now, then soon. This would do no harm to legitimate business though it might affect adversely businesses which make false claims (and there are rather a lot of the latter).
Q8: How might the risk of harm to the public be reduced other than by orthodox statutory regulation? For example by voluntary self-regulation underpinned by consumer protection legislation and by greater public awareness, by accreditation of voluntary registration bodies, or by a statutory or voluntary licensing regime?
Voluntary self-regulation
Accreditation of voluntary bodies
Statutory or voluntary licensing
Unsure
I disagree with the premise, for reasons given in detail in separate documents. I believe that ‘orthodox statutory regulation’, if that means the Pittilo proposals, would increase, not decrease, the risk to the public. Strengthening the powers of Trading Standards, the MHRA and such consumer protection legislation would be far more effective in reducing risk to the public than the HPC could ever be. Greater public awareness of the weakness of the evidence for the efficacy of these treatments would obviously help too, but can’t do the job on its own.
Q10: What would you envisage would be the benefits to the public, to practitioners, and to businesses, for the alternatives to statutory regulation outlined at Question 8?
It depends on which alternative you are referring to. The major benefit of enforcement of existing laws by Trading Standards and/or the MHRA would be (a) to protect the public from risk, (b) to protect the public from health fraud and (c) almost certainly lower cost to the tax payer.
Q11: If you feel that not all three practitioner groups justify statutory regulation, which group(s) does/do not and please give your reasons why/why not?
Acupuncture
Herbal Medicine
TCM
Unsure
None of them. The differences are marginal. In the case of acupuncture there has been far more good research than for HM or TCM. But the result of that research is to show that in most cases the effects are likely to be no more than those expected of a rather theatrical placebo. Furthermore the extent to which acupuncture has a bigger effect than no-acupuncture in a NON-BLIND comparison, is usually too small and transient to offer any clinical advantage (so it doesn’t really matter whether the effect is placebo or not, it is too small to be useful).
In the case of HM, and even more of TCM, there is simply not enough research to give much idea of their usefulness, with a small handful of exceptions.
This leads to a conclusion that DH seems to have ignored in the past. It makes absolutely no sense to talk about “properly trained practitioners” without first deciding whether the treatments work or not. There can be no such thing as “proper training” in a discipline that offers no benefit over placebo. It is a major fault of the Pittilo recommendations that they (a) ignore this basic principle and (b) are very over-optimistic about the state of the evidence.
Q12: Would it be helpful to the public for these practitioners to be regulated in a way which differentiates them from the regulatory regime for mainstream professions publicly perceived as having an evidence base of clinical effectiveness? If so, why? If not, why not?
Yes
No
Unsure
It might indeed be useful if regulation pointed out the very thin evidence base for HM and TCM but it would look rather silly. The public would say how can it be that the DH is granting statutory regulation to things that don’t work?
Q13: Given the Government’s commitment to reducing the overall burden of unnecessary statutory regulation, can you suggest which areas of healthcare practice present sufficiently low risk so that they could be regulated in a different, less burdensome way or de-regulated, if a decision is made to statutorily regulate acupuncturists, herbalists and traditional Chinese medicine practitioners?
Yes
No
Unsure
As stated above, the.only form of regulation that is needed, and the only form that would protect the public, is through consumer protection regulations, most of which already exist (though they are enforced in a very inconsistent way). Most statutory regulation is objectionable, not on libertarian grounds, but because it doesn’t achieve the desired ends (and is expensive). In this case of folk medicine, like HM and TCM, the effect would be exactly the opposite of that desired as shown in separate documents that I have submitted to the consultation.
Q14: If there were to be statutory regulation, should the Health Professions Council (HPC) regulate all three professions? If not, which one(s) should the HPC not regulate?
Yes
No
Unsure
The HPC should regulate none of them. It has never before regulated any form of alternative medicine and it is ill-equipped to do so. Its statement that it doesn’t matter that there is very little evidence that the treatments work poses a danger to patients (as well as being contrary to its own rules).
Q15: If there were to be statutory regulation, should the Health Professions Council or the General Pharmaceutical Council/Pharmaceutical Society of Northern Ireland regulate herbal medicine and traditional Chinese medicine practitioners?
HPC
GPC/PSNI
Unsure
Neither. The GPC is unlikely to care about whether the treatments work any more than the RPSGB did, or the GCC does now. The problems would be exactly the same whichever body did it.
Q16: If neither, who should and why?
As I have said repeatedly, it should be left to Trading Standards, the MHRA and other consumer protection regulation.
Q17:
a) Should acupuncture be subject to a different form of regulation from that for herbalism and traditional Chinese medicine? If so, what?
Yes
No
Unsure
b) Can acupuncture be adequately regulated through local means, for example through Health and Safety legislation, Trading Standards legislation and Local Authority licensing?
Yes
No
Unsure
(a) No -all should be treated the same. Acupuncture is part of TCM
(b) Yes
Q18.
a) Should the titles acupuncturist, herbalist and [traditional] Chinese medicine practitioner be protected?
b) If your answer is no which ones do you consider should not be legally protected?
Yes
No
Unsure
No. It makes no sense to protect titles until such time as it has been shown that the practitioners can make a useful contribution to medicine (above placebo effect). That does not deny that placebos may be useful at times. but if that is all they are doing, the title should be ‘placebo practitioners’.
Q19: Should a new model of regulation be tested where it is the functions of acupuncture, herbal medicine and TCM that are protected, rather than the titles of acupuncturist, herbalist or Chinese medicine practitioner?
Yes
No
Unsure
No. This makes absolutely no sense when there is so little knowledge about what is meant by the ” functions of acupuncture, herbal medicine and TCM”.Insofar as they don’t work (better than placebo), there IS no function. Any attempt to define function when there is so little solid evidence (at least for HM and TCM) is doomed to failure.
Q20: If statutory professional self-regulation is progressed, with a model of protection of title, do you agree with the proposals for “grandparenting” set out in the Pittilo report?
Yes
No
Unsure
No. I believe the Pittilo report should be ignored entirely. The whole process needs to be thought out again in a more rational way.
Q22: Could practitioners demonstrate compliance with regulatory requirements and communicate effectively with regulators, the public and other healthcare professionals if they do not achieve the standard of English language competence normally required for UK registration? What additional costs would occur for both practitioners and regulatory authorities in this case?
Yes
No
Unsure
No. It is a serious problem, in TCM especially, that many High Street practitioners speak hardly any English at all. That adds severely to the already considerable risks. There would be no reliable way to convey what was expected of them. it would be absurd for the taxpayer to pay for them to learn English for the purposes of practising TCM (of course there might be the same case as for any other immigrant for teaching English on social grounds).
Q23: What would the impact be on the public, practitioners and businesses (financial and regulatory burden) if practitioners unable to achieve an English language IELTS score of 6.5 or above are unable to register in the UK?
Significant impact
Some impact
No impact
Unsure
The question is not relevant. The aim of regulation is to protect the public from risk (and it should be, but isn’t, an aim to protect them from health fraud). It is not the job of regulation to promote businesses
Q24: Are there any other matters you wish to draw to our attention?
I have submitted three documents via HRDListening@dh.gsi.gov.uk. The first of these puts the case against the form of regulation proposed by Pittilo, far more fluently than is possible in a questionnaire.
Another shows examples of what is actually taught in degrees in acupuncture, HM and TCM. They show very graphically the extent to which the Pittilo proposals would endanger the public, if they were to be implemented..
Recently I wrote a piece for the National Health Executive (“the Independent Journal for Senior Health Service Managers”), with the title Medicines that contain no medicine and other follies
In the interests of what journalists call balance (but might better be called equal time for the Flat Earth Society), an article appeared straight after mine, Integrating Homeopathy into Primary Care. It was by Rachel Roberts “Research consultant for the Society of Homeopaths”.
This defence was so appalling that I sent them a response (after first doing a bit of checking on its author). To my surprise, they published the response in full [download pdf of printed version]. Their title was

As always, the first step is to Google the author, to find out a bit more. It seems that Rachel Roberts runs a business Integrated Homeopathic Training. (a financial interest that was not mentioned in her article). She will sell you flash cards (‘Matmedcards’) for £70 (+£9 p&p) for 120 cards (yes, seriously). The card for Conium maculatum is remarkable. It says on the reverse side
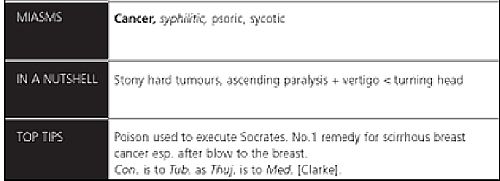
Yes, it says (my emphasis)
“The poison used to execute Socrates. No 1 remedy for scirrhous breast cancer. Esp after blow to the breast”
No doubt she would claim that the word “remedy” was a special weasel word of homeopaths that did not imply any therapeutic efficacy. But its use in this context seems to me to be cruel deception, even murderous. It also appears to breach the Cancer Act 1939, as well as the Unfair Trading laws.
I asked the Bristol Trading Standards Office, and got a reply remarkably quickly. It ended thus.
“. . . . the use of the card for “hemlock” as an example amounts to advice in connection with the treatment (of cancer)”. I will initially write to IHT and require that they remove this, and any other, reference to cancer treatment from their website.
When I checked again a couple of weeks later, the hemlock sample card had been been replaced by one about chamomile (it is described as the opium of homeopathy. Luckily the pills contain no opium (and no chamomile either) or that would be breaking another law. Bafflingly, it is not (yet) against the law to sell pills that contain no trace of the ingredient on the label, if they are labelled ‘homeopathic’.
Presumably the packs still contain a claim to cure cancer. And what is said in the privacy of the consulting room will never be known.
Political correctness is a curious thing. I felt slightly guilty when I reported this breach of the Cancer Act. It felt almost sneaky. The feeling didn’t last long though. We are talking about sick people here.
It isn’t hard to imagine a desperate woman suffering from cancer reading that Ms Roberts knows the “No 1 remedy for scirrhous breast cancer”. She might actually believe it. She might buy some hemlock pills that contain no hemlock (or anything else). She might die as a result. It is not a joke. It is, literally, deadly serious.
It is also deadly serious that the Department of Health and some NHS managers are so stifled by political correctness that they refer to homeopaths as “professionals” and pay them money.
Ms Roberts, in her article, is at pains to point out that
|
 |
Well it is already well known that the the Code of Ethics of the Society of Homeopaths is something of a joke. This is just one more example.
The Code of Ethics, para 72 says homeopaths have a legal obligation
“To avoid making claims (whether explicit or implied; orally or in writing) implying cure of any named disease.”
Like, perhaps, claiming to have the “No 1 remedy for scirrhous breast cancer”?
Obviously voluntary self-regulation isn’t worth the paper it’s written on.
You don’t need to go to her web site to find “claims . . . implying cure of any named disease”. In her article she says
“Conditions which responded well to homeopathy included childhood eczema and asthma, migraine, menopausal problems, inflammatory bowel disease, irritable bowel syndrome, arthritis, depression and chronic fatigue syndrome.”
No doubt they will say that the claim that asthma and migraine “responded well” to their sugar pills carries no suggestion that they can cure a named disease. And if you believe that, you’ll believe anything.
I have to say that I find Ms Robert’s article exceedingly puzzling. It comes with 29 references, so it looks, to use Goldacre’s word, ‘sciencey’. If you read the references, and more importantly, know about all the work that isn’t referred to, you see it is the very opposite of science. I see only two options.
Either it is deliberate deception designed to make money, or it shows, to a mind-boggling extent, an inability to understand what constitutes evidence.
The latter, more charitable, view is supported by the fact that Ms Roberts trots out, yet again, the infamous 2005 Spence paper, as though it constituted evidence for anything at all. In this paper 6544 patients at the Bristol Homeopathic Hospital were asked if the felt better after attending the out-patient department. Half of them reported that the felt ‘better’ or ‘much better’. Another 20% said they were ‘slightly better’ (but that is what you say to be nice to the doctor). The patients were not compared with any other group at all. What could be less surprising than that half of the relatively minor complaints that get referred for homeopathy get ‘better or much better’ on their own?
This sort of study can’t even tell you if homeopathic treatment has a placebo effect, never mind that it has a real effect of its own. It is a sign of the desperation of homeopaths that they keep citing this work.
Whatever the reason, the conclusion is clear. Never seek advice from someone who has a financial interest in the outcome. Ms Roberts makes her living from homeopathy. If she were to come to the same conclusion as the rest of the world, that it is a placebo and a fraud, her income would vanish. It is asking too much of anyone to do that.
| This is the mistake made time and time again by the Department of Health and by the NHS. The Pittilo report does the same thing The execrably bad assessment of evidence in that report is, one suspects, not unrelated to the fact that it was done entirely by people who would lose their jobs if they were to come to any conclusion other than their treatments work. |  |
At present , the regulation of alternative medicine is chaotic because the government and the dozen or so different quangos involved are trying to regulate while avoiding the single most important question – do the treatments work?
They should now grasp that nettle and refer the question to NICE.
Follow-up
I’m perfectly happy to think of alternative medicine as being a voluntary, self-imposed tax on the gullible (to paraphrase Goldacre again). But only as long as its practitioners do no harm and only as long as they obey the law of the land. Only too often, though, they do neither.
When I talk about law, I don’t mean lawsuits for defamation. Defamation suits are what homeopaths and chiropractors like to use to silence critics. heaven knows, I’ve becomes accustomed to being defamed by people who are, in my view. fraudsters, but lawsuits are not the way to deal with it.
I’m talking about the Trading Standards laws Everyone has to obey them, and in May 2008 the law changed in a way that puts the whole health fraud industry in jeopardy.
The gist of the matter is that it is now illegal to claim that a product will benefit your health if you can’t produce evidence to justify the claim.
I’m not a lawyer, but with the help of two lawyers and a trading standards officer I’ve attempted a summary. The machinery for enforcing the law does not yet work well, but when it does, there should be some very interesting cases.
The obvious targets are homeopaths who claim to cure malaria and AIDS, and traditional Chinese Medicine people who claim to cure cancer.
But there are some less obvious targets for prosecution too. Here is a selection of possibilities to savour..
- Universities such as Westminster, Central Lancashire and the rest, which promote the spreading of false health claims
- Hospitals, like the Royal London Homeopathic Hospital, that treat patients with mistletoe and marigold paste. Can they produce any real evidence that they work?
- Edexcel, which sets examinations in alternative medicine (and charges for them)
- Ofsted and the QCA which validate these exams
- Skills for Health and a whole maze of other unelected and unaccountable quangos which offer “national occupational standards” in everything from distant healing to hot stone therapy, thereby giving official sanction to all manner of treatments for which no plausible evidence can be offered.
- The Prince of Wales Foundation for Integrated Health, which notoriously offers health advice for which it cannot produce good evidence
- Perhaps even the Department of Health itself, which notoriously referred to “psychic surgery” as a profession, and which has consistently refused to refer dubious therapies to NICE for assessment.
The law, insofar as I’ve understood it, is probably such that only the first three or four of these have sufficient commercial elements for there to be any chance of a successful prosecution. That is something that will eventually have to be argued in court.
But lecanardnoir points out in his comment below that The Prince of Wales is intending to sell herbal concoctions, so perhaps he could end up in court too.
The laws
We are talking about The Consumer Protection from Unfair Trading Regulations 2008. The regulations came into force on 26 May 2008. The full regulations can be seen here, or download pdf file. They can be seen also on the UK Statute Law Database.
The Office of Fair Trading, and Department for Business, Enterprise & Regulatory Reform (BERR) published Guidance on the Consumer Protection from Unfair Trading Regulations 2008 (pdf file),
Statement of consumer protection enforcement principles (pdf file), and
The Consumer Protection from Unfair Trading Regulations: a basic guide for business (pdf file).
Has The UK Quietly Outlawed “Alternative” Medicine?
On 26 September 2008, Mondaq Business Briefing published this article by a Glasgow lawyer, Douglas McLachlan. (Oddly enough, this article was reproduced on the National Center for Homeopathy web site.)
“Proponents of the myriad of forms of alternative medicine argue that it is in some way “outside science” or that “science doesn’t understand why it works”. Critical thinking scientists disagree. The best available scientific data shows that alternative medicine simply doesn’t work, they say: studies repeatedly show that the effect of some of these alternative medical therapies is indistinguishable from the well documented, but very strange “placebo effect” ”
“Enter The Consumer Protection from Unfair Trading Regulations 2008(the “Regulations”). The Regulations came into force on 26 May 2008 to surprisingly little fanfare, despite the fact they represent the most extensive modernisation and simplification of the consumer protection framework for 20 years.”
The Regulations prohibit unfair commercial practices between traders and consumers through five prohibitions:-
- General Prohibition on Unfair Commercial
Practices (Regulation 3)- Prohibition on Misleading Actions (Regulations 5)
- Prohibition on Misleading Omissions (Regulation 6)
- Prohibition on Aggressive Commercial Practices (Regulation 7)
- Prohibition on 31 Specific Commercial Practices that are in all Circumstances Unfair (Schedule 1). One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. The definition of “product” in the Regulations includes services, so it does appear that all forms medical products and treatments will be covered.
Just look at that!
| One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations” |
Section 5 is equally powerful, and also does not contain the contentious word “cure” (see note below)
Misleading actions
5.—(1) A commercial practice is a misleading action if it satisfies the conditions in either paragraph (2) or paragraph (3).
(2) A commercial practice satisfies the conditions of this paragraph—
(a) if it contains false information and is therefore untruthful in relation to any of the matters in paragraph (4) or if it or its overall presentation in any way deceives or is likely to deceive the average consumer in relation to any of the matters in that paragraph, even if the information is factually correct; and
(b) it causes or is likely to cause the average consumer to take a transactional decision he would not have taken otherwise.
These laws are very powerful in principle, But there are two complications in practice.
One complication concerns the extent to which the onus has been moved on to the seller to prove the claims are true, rather than the accuser having to prove they are false. That is a lot more favourable to the accuser than before, but it’s complicated.
The other complication concerns enforcement of the new laws, and at the moment that is bad.
Who has to prove what?
That is still not entirely clear. McLachlan says
“If we accept that mainstream evidence based medicine is in some way accepted by mainstream science, and alternative medicine bears the “alternative” qualifier simply because it is not supported by mainstream science, then where does that leave a trader who seeks to refute any allegation that his claim is false?
Of course it is always open to the trader to show that his the alternative therapy actually works, but the weight of scientific evidence is likely to be against him.”
On the other hand, I’m advised by a Trading Standards Officer that “He doesn’t have to refute anything! The prosecution have to prove the claims are false”. This has been confirmed by another Trading Standards Officer who said
“It is not clear (though it seems to be) what difference is implied between “cure” and “treat”, or what evidence is required to demonstrate that such a cure is false “beyond reasonable doubt” in court. The regulations do not provide that the maker of claims must show that the claims are true, or set a standard indicating how such a proof may be shown.”
The main defence against prosecution seems to be the “Due diligence defence”, in paragraph 17.
Due diligence defence
17. —(1) In any proceedings against a person for an offence under regulation 9, 10, 11 or 12 it is a defence for that person to prove—
(a) that the commission of the offence was due to—
(i) a mistake;
(ii) reliance on information supplied to him by another person;
(iii) the act or default of another person;
(iv) an accident; or
(v) another cause beyond his control; and
(b) that he took all reasonable precautions and exercised all due diligence to avoid the commission of such an offence by himself or any person under his control.
If “taking all reasonable precautions” includes being aware of the lack of any good evidence that what you are selling is effective, then this defence should not be much use for most quacks.
Douglas McLachlan has clarified, below, this difficult question
False claims for health benefits of foods
A separate bit of legislation, European regulation on nutrition and health claims made on food, ref 1924/2006, in Article 6, seems clearer in specifying that the seller has to prove any claims they make.
Article 6
Scientific substantiation for claims
1. Nutrition and health claims shall be based on and substantiated by generally accepted scientific evidence.
2. A food business operator making a nutrition or health claim shall justify the use of the claim.
3. The competent authorities of the Member States may request a food business operator or a person placing a product on the market to produce all relevant elements and data establishing compliance with this Regulation.
That clearly places the onus on the seller to provide evidence for claims that are made, rather than the complainant having to ‘prove’ that the claims are false.
On the problem of “health foods” the two bits of legislation seem to overlap. Both have been discussed in “Trading regulations and health foods“, an editorial in the BMJ by M. E. J. Lean (Professor of Human Nutrition in Glasgow).
“It is already illegal under food labelling regulations (1996) to claim that food products can treat or prevent disease. However, huge numbers of such claims are still made, particularly for obesity ”
“The new regulations provide good legislation to protect vulnerable consumers from misleading “health food” claims. They now need to be enforced proactively to help direct doctors and consumers towards safe, cost effective, and evidence based management of diseases.”
In fact the European Food Standards Agency (EFSA) seems to be doing a rather good job at imposing the rules. This, predictably, provoked howls of anguish from the food industry There is a synopsis here.
“Of eight assessed claims, EFSA’s Panel on Dietetic Products, Nutrition and Allergies (NDA) rejected seven for failing to demonstrate causality between consumption of specific nutrients or foods and intended health benefits. EFSA has subsequently issued opinions on about 30 claims with seven drawing positive opinions.”
“. . . EFSA in disgust threw out 120 dossiers supposedly in support of nutrients seeking addition to the FSD’s positive list.
If EFSA was bewildered by the lack of data in the dossiers, it needn’t hav been as industry freely admitted it had in many cases submitted such hollow documents to temporarily keep nutrients on-market.”
Or, on another industry site, “EFSA’s harsh health claim regime”
“By setting an unworkably high standard for claims substantiation, EFSA is threatening R&D not to mention health claims that have long been officially approved in many jurisdictions.”
Here, of course,”unworkably high standard” just means real genuine evidence. How dare they ask for that!
Enforcement of the law
Article 19 of the Unfair Trading regulations says
19. —(1) It shall be the duty of every enforcement authority to enforce these Regulations.
(2) Where the enforcement authority is a local weights and measures authority the duty referred to in paragraph (1) shall apply to the enforcement of these Regulations within the authority’s area.
Nevertheless, enforcement is undoubtedly a weak point at the moment. The UK is obliged to enforce these laws, but at the moment it is not doing so effectively.
A letter in the BMJ from Rose & Garrow describes two complaints under the legislation in which it appears that a Trading Standards office failed to enforce the law. They comment
” . . . member states are obliged not only to enact it as national legislation but to enforce it. The evidence that the government has provided adequate resources for enforcement, in the form of staff and their proper training, is not convincing. The media, and especially the internet, are replete with false claims about health care, and sick people need protection. All EU citizens have the right to complain to the EU Commission if their government fails to provide that protection.”
This is not a good start. A lawyer has pointed out to me
“that it can sometimes be very difficult to get Trading Standards or the OFT to take an interest in something that they don’t fully understand. I think that if it doesn’t immediately leap out at them as being false (e.g “these pills cure all forms of cancer”) then it’s going to be extremely difficult. To be fair, neither Trading Standards nor the OFT were ever intended to be medical regulators and they have limited resources available to them. The new Regulations are a useful new weapon in the fight against quackery, but they are no substitute for proper regulation.”
Trading Standards originated in Weights and Measures. It was their job to check that your pint of beer was really a pint. Now they are being expected to judge medical controversies. Either they will need more people and more training, or responsibility for enforcement of the law should be transferred to some more appropriate agency (though one hesitates to suggest the MHRA after their recent pathetic performance in this area).
Who can be prosecuted?
Any “trader”, a person or a company. There is no need to have actually bought anything, and no need to have suffered actual harm. In fact there is no need for there to be a complainant at all. Trading standards officers can act on their own. But there must be a commercial element. It’s unlikely that simply preaching nonsense would be sufficient to get you prosecuted, so the Prince of Wales is, sadly, probably safe.
Universities who teach that “Amethysts emit high Yin energy” make an interesting case. They charge fees and in return they are “falsely claiming that a product is able to cure illnesses”.
In my view they are behaving illegally, but we shan’t know until a university is taken to court. Watch this space.
The fact remains that the UK is obliged to enforce the law and presumably it will do so eventually. When it does, alternative medicine will have to change very radically. If it were prevented from making false claims, there would be very little of it left apart from tea and sympathy
Follow-up
New Zealand must have similar laws.
Just as I was about to post this I found that in New Zealand a
“couple who sold homeopathic remedies claiming to cure bird flu, herpes and Sars (severe acute respiratory syndrome) have been convicted of breaching the Fair Trading Act.”
They were ordered to pay fines and court costs totalling $23,400.
A clarification form Douglas McLachlan
On the difficult question of who must prove what, Douglas McLachlan, who wrote Has The UK Quietly Outlawed “Alternative” Medicine?, has kindly sent the following clarification.
“I would agree that it is still for the prosecution to prove that the trader committed the offence beyond a reasonable doubt, and that burden of proof is always on the prosecution at the outset, but I think if a trader makes a claim regarding his product and best scientific evidence available indicates that that claim is false, then it will be on the trader to substantiate the claim in order to defend himself. How will the trader do so? Perhaps the trader might call witness after witness in court to provide anecdotal evidence of their experiences, or “experts” that support their claim – in which case it will be for the prosecution to explain the scientific method to the Judge and to convince the Judge that its Study evidence is to be preferred.
Unfortunately, once human personalities get involved things could get clouded – I could imagine a small time seller of snake oil having serious difficulty, but a well funded homeopathy company engaging smart lawyers to quote flawed studies and lead anecdotal evidence to muddy the waters just enough for a Judge to give the trader the benefit of the doubt. That seems to be what happens in the wider public debate, so it’s easy to envisage it happening a courtroom.”
The “average consumer”.
(3) A commercial practice is unfair if—
(a) it contravenes the requirements of professional diligence; and
(b) it materially distorts or is likely to materially distort the economic behaviour of the average consumer with regard to the product.
It seems,therefore, that what matters is whether the “average consumer” would infer from what is said that a claim was being made to cure a disease. The legal view cited by Mojo (comment #2, below) is that expressions such as “can be used to treat” or “can help with” would be considered by the average consumer as implying successful treatment or cure.
The drugstore detox delusion. A nice analysis “detox” at .Science-based Pharmacy
