Pittilo
The long-awaited government decision concerning statutory regulation of herbalists, traditional Chinese medicine (TCM) and acupuncture came out today.
Get the Department of Health (DH) report [pdf]
It is not good news. They have opted for statutory regulation by the Health Professions Council (HPC). This is much what was recommended by the disgraceful Pittilo report, about which I wrote a commentary in the Times (or free version here), and A very bad report: gamma minus for the vice-chancellor.
The DH report is merely an analysis of responses to the consultation, but the MHRA says
"The Health Professions Council (HPC) has now been asked to establish a statutory register for practitioners supplying unlicensed herbal medicines. The proposal is, following creation of this register, to make use of a derogation in European medicines legislation (Article 5 (1) of Directive 2001/83/EC) that allows national arrangements to permit those designated as “authorised healthcare professionals” to commission unlicensed medicines to meet the special needs of their patients."
The MHRA points out that this started 11 years ago with the publication of the House of Lords report (2000). Both that report, and the government’s response to it, set the following priorities. Both state clearly
“… we recommend that three important questions should be addressed in the following order . .
- (1) does the treatment offer therapeutic benefits greater than placebo?
- (2) is the treatment safe?
- (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?
The report of DH and the MHRA’s response have ignored totally two of these three requirements. There is no consideration whatsoever of whether treatments work better than placebo (point one) and there is no consideration whatsoever of cost-effectiveness (point 3). These two important recommendations in the Houss of Lords report have simply been brushed under the carpet.
Needless to say, herbalists are head over heels with joy at this sign of official endorsement (here is one reaction)
Here are my first reactions. The post will be updated soon.
The DH report is, in a sense, democratic. They have simply counted the responses, for and against each proposal. They seem to be quite unaware that most of the responses come from High Street herbailsts whose main aim is to gain respectability. The response of the Academy of Royal Medical Colleges counts as one vote, just the same as the owner of a Chinese medicine shop. This is not how health policy should be determined. Some intervention of the brain is needed, but that isn’t apparent in the report.
At present the HPC regulates Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists. I shudder to think what all these good people will think about being lumped together with people who practice evidence-free medicine (or, worse, forms of medicine where there is good evidence that they don’t work).
The vast majority of herbalists, traditional Chinese medicine (TCM) and acupuncture has no good evidence that it works, In the case of soem herbal medicines and acupuncture, there is good evidence that they don’t work. Yet the HPC has, as one of its criteria, that aspiring to be regulated by them requires
"practise based on evidence of efficacy"
The Department of Health seems to have quietly forgotten about this criterion. It cannot possibly be met. The HPC has already expressed its willingness to go along with this two-faced approach (see Health Professions Council ignores its own rules: the result is nonsense )
Another mistake made by the Department of Health regards the value of "training". The report (page 11) says
Would statutory regulation lessen the risk of harm? (Q2)
Again, the vast majority of respondents thought it would. Reasons given were that statutory regulation would ensure that herbal practitioners and acupuncturists are carefully and thoroughly trained. That training is subject to accreditation, evaluation and periodic review by independent educational and training professionals, and disciplinary oversight by a regulating body. Incompetent or unscrupulous practitioners could be struck off the register and prevented from practising.
Although it is pointed out to them in several responses, the Department of Health seems quite incapable of understanding a simple and obvious truth. Spending three years training people to learn things that are not true, safeguards nobody. On the contrary, it endangers the public. Training in nonsense is obviously a nonsense.
At the end of the report is a list of organisations who responded, As expected, they are predominantly trade bodies that have a vested interest in allowing thinks to be sold freely regardless of whether they work or not. The first four are Alliance of Herbal Medicine Practitioners. European herbal and Traditional Medicine Practitioners Association (ETMPA), Association Chinese Medicine Practitioners (UK) (ACMP) and Acupuncture Society. And so on.
More coming soon.
Follow-up
16 February 2011. Later the same day, we see one reason why Michael Mcintyre, chair of the European Herbal Practitioners Association, got what he wanted to promote his trade. They had evidently hired a PR Agency, Cogitamus, to push their case. Now they are crowing about their victory. And of course his profits were not harmed by the free publicity that was given to his cause by the BBC,
The pinheads in the Department of Health are more easily persuaded by a PR agency than by any number of people who know a lot more about it, and who have no profit motive.
17 February 2011.
The herbal problem was front page news in the London free paper, the Metro: Chinese medicine and herbal ban to see Britain defy EU laws
The Daily Telegraph covered the story: Herbal medicine to be regulated, says Andrew Lansley. The comments featured some pretty mad rants from herbalists, to which I tried to reply.
The Metro article elicited a fine bit of abuse from a Lynda Kane. I’m constantly amazed at the downright viciousness of cuddly holistic therapists when they get found out. I guess it is just another bad case of cognitive dissonance. I can’t resist a few quotations.
Sir,
“I have just come across your asinine comments quoted in the London Metro newspaper re the EU herbal medicine directive. For a supposed scientist your mis-informed, closed-minded, unsubstantiated bigotry leaves me speechless”
“As a scientist myself, I abide by the virtues of open-minded neutrality and accepting the hypothesis until proven otherwise by null-hypothesis based research.”
“How many of the innumerable studies on the efficacy of herbal medicine have you read? “
“Perhaps in your ‘day’ professors could say whatever they liked and be listened to. That day is long gone, as you must know from the various law-suits you have been party to.”
I love the idea that statistics allow you to accept any hypothesis whatsoever until someone shows it to be wrong.
This would be funny if it were not so sad (and rather painful). As always I replied politely and referred her to NCCAM’s Guide to Herbs, so she can check up on that plethora of evidence that she seems to think exists.
This is Lynda Kane of energyawareness.org. I can recommend her web site, if you want some truly jaw-dropping woo. She’ll sell you a “White Jade Energy Egg – may provide up to 5 times as much protection from wifi and from other peoples’ energies – costs £47.00”. Hmm, sounds good. How does it work? Easy.
“The human energy or “qi” field is shaped like an egg. It is being attacked by many forms of natural and man-made environmental stress 24 hours a day.”
I guess that’s OK according to Ms Kane’s interpretation of statistics which allows you to accept any hypothesis whatsoever until someone shows it to be wrong.
Anyone for Trading Standards or the ASA?
17 February 2011. The excellent Andy Lewis has posted on similar problems “How to Spot Bad Regulation of Alternative Medicine“
.20 July 2013
Nothing visible happened after this announcement. Until the government’s resident medical loon, David Tredinnick MP forced a debate on the matter. His introduction to the debate was his usual make-believe. Sadly it made much of an exhibit at the Royal Society Summer Science exhibition -a bit of bait and swich by aromatherapists.
After ploughing your way through pages of nonsense, you get to the interesting bit. At 10.38 am, The Parliamentary Under-Secretary of State for Health, Dr Daniel Poulter, announced what was happening. It seems that there may, after all, have been some effect of all the sensible submissions which pointed out the impossibility of regulating nonsense. The question of regulation has, yet again, been postponed.
"To ensure that we take forward the matter effectively, we want to bring together experts and interested parties from all sides of the debate to form a working group that will gather evidence and consider all the viable options in more detail,"
One wonders who will be on this working group? If they don’t choose the right people, it could be as bad as the Pittilo report. It wasn’t reassuring to read
" we want to set up a working group and to work with my hon. Friend [Tredinnick], and herbalists and others, to ensure that the legislation is fit for purpose."
Every single request for information about course materials in quack medicine that I have ever sent has been turned down by universities,
It is hardly as important as as refusal of FoI requests to see climate change documents, but it does indicate that some vice-chancellors are not very interested in openness. This secretiveness is exactly the sort of thing that leads to lack of trust in universities and in science as a whole.
The one case that I have won took over three years and an Information Tribunal decision against the University of Central Lancashire (UCLAN) before I got anything.
UCLAN spent £80,307.95.(inc VAT at 17.5%) in legal expenses alone (plus heaven knows how much in staff time) to prevent us from seeing what was taught on their now defunct “BSc (Hons) homeopathy”. This does not seem to me to be good use of taxpayers’ money. A small sample of what was taught has already been posted (more to come). It is very obvious why the university wanted to keep it secret, and equally obvious that it is in the public interest that it should be seen.
UCLAN had dropped not only its homeopathy "degree" before the information was revealed, They also set up an internal inquiry into all the rest of their courses in magic medicine which ended with the dumping of all of them.
Well, not quite all, There was one left. An “MSc” in homeopathy by e-learning. Why this was allowed to continue after the findings of UCLAN’s internal review, heaven only knows. It is run by the same Kate Chatfield who ran the now defunct BSc. Having started to defend the reputation against the harm done to it by offering this sort of rubbish, I thought I should finish. So I asked for the contents of this course too. It is, after all, much the same title as the course that UCLAN had just been ordered to release. But no, this request too was met with a refusal
Worse still, the refusal was claimed under section 43(2) if the Freedom of Information Act 2000. That is the public interest defence, The very defence that was dismissed in scathing terms by the Information Tribunal less than two months ago,
To add insult to injury, UCLAN said that it would make available the contents of the 86 modules in the course under its publication scheme, at a cost of £20 per module, That comes to £1,720 for the course, Some freedom of information.
Because this was a new request, it now has to go through the process of an internal reviw of the decision before it can ne referred to the Information Commissioner. That will be requested, and since internal reviews have, so far, never changed the initial judgment. the appeal to the Information Commissioner should be submitted within the month. I have been promised that the Information Commissioner will deal with it much faster this time than the two years it took last time.
And a bit more unfreedom
Middlesex University
I first asked Middlesex for materials from their homeopathy course on 1 Oct 2008. These courses are validated by Middlesex university (MU) but actually run by the Centre for Homeopathic Education. Thw MU site barely mentions homeopathy and all I got was the usual excuse that the uninsersity did not possess the teaching materials. As usual, the validation had been done without without looking at what was actually being taught. The did send me the validation document though [download it] As usual, the validation document shows no sign at all of the fact that the usbject of the "BSc" is utter nonsense. One wonderful passage says
“. . . the Panel were assured that the Team are clearly producing practitioners but wanted to explore what makes these students graduates? The Team stated that the training reflects the professional standards that govern the programme and the graduateness is achieved through developing knowledge by being able to access sources and critically analyse these sources . . . “
Given that the most prominent characteristic of homeopaths (and other advocates of magic medicine) is total lack of critical ability, this is hilarious. If they had critical ability they wouldn’t be homeopaths. Hilarious is not quite the right word, It is tragic that nonsense like this can be found in an official university document.
Middlesex, though it doesn’t advertise homeopathy, does advertise degrees in Traditional Chinese Medicine, Herbal Medicine and Ayurveda. On 2nd February 2010 I asked for teaching materials from these courses. Guess what? The request was refused. In this case the exemptions under FOIA were not even invoked but I was told that "All these materials are presently available only in one format at the University – via a student-only accessed virtual learning environment. ". Seems that they can’t print out the bits that I asked for, The internal review has been requested, then we shall see what the Information Commissioner has to say.
Two other cases are at present being considered by the Information Commissioner (Scotland), after requests under the Scottish FoIA were refused. They are interesting cases because they bear on the decision, currently being considered by the government, about whether they should implement the recommendations of the execrable Pittilo report.
Napier University Edinburgh. The first was for teaching material form the herbal medicine course at Napier University Edinburgh. I notice that this course no longer appears in UCAS or on Napier’s own web site, so maybe the idea that its contents might be disclosed has been sufficient to make the university do the sensible thing.
Robert Gordon University Aberdeen The second request was for teaching material from the “Introduction to Homeopathy” course at the Robert Gordon University Aberdeen. The particular interest that attaches to this is that the vice-chancellor of Robert Gordon university is Michael Pittilo. The fact that he is willing to tolerate such a course in his own university seems to me to disqualify him from expressing any view on medical subjects.
Michael Pittilo, Crohn’s disease and Andrew Wakefield
Michael Pittilo has not been active in science for some time now, but Medline does show scientiifc publications for Pittilo RM, between 1979 anf 1998. Between 1989 and 1995 there are five papers published jointly with one Andrew Wakefield. These papers alleged a relationship between measles virus and Crohn’s disease. The papers were published before tha infamous 1998 paper by Wakefield in the Lancet (now retracted) that brought disgrace on Wakefield and probably caused unnecessary deaths.. The link between measles and Crohn’s disease is now equally disproved.
The subject has been reviewed by Korzenik (2005) in Past and Current Theories of Etiology of IBD. Toothpaste, Worms, and Refrigerators
“Wakefield et al proposed that Crohn’s results from a chronic infection of submucosal endothelium of the intestines with the measles virus [Crohn’s disease: pathogenesis and persistent measles virus infection. Wakefield AJ, Ekbom A, Dhillon AP, Pittilo RM, Pounder RE., Gastroenterology, 1995, 108(3):911-6]”
"This led to considerable media interest and< public concern over use of live measles vaccine as well as other vaccines. A number of researchers countered these claims, with other studies finding that titers to measles were not increased in Crohn’s patients, granulomas were not associated with endothelium 49 , measles were not in granulomas50 and the measles vaccine is not associated with an increased risk of Crohn’s disease51–55 "
This bit of history is not strictly relevant to the Pittilo report, but I do find quite puzzling how the government chooses people from whom it wishes to get advice about medical problems.
Follow-up
I notice that the Robert Gordon university bulletin has announced that
“Professor Mike Pittilo, Principal of the University, has been made an MBE in the New Year Honours list for services to healthcare”.
That is a reward for writing a very bad report that has not yet been implemented, and one hopes, for the sake of patients, will never be implemented. I do sometimes wonder about the bizarre honours system in the UK.
Postcript.
On 16th February, the death of Michael Pittilo was announced. He had been suffeing from cancer and was only 55 years old. I wouldn’t wish that fate on my worst enemy.
The Yuletide edition of the BMJ carries a lovely article by Jeffrey Aronson, Patent medicines and secret remedies. (BMJ 2009;339:b5415).
I was delighted to be asked to write an editorial about it, In fact it proved quite hard work, because the BMJ thought it improper to be too rude about the royal family, or about the possibility of Knight Starvation among senior medics. The compromise version that appeared in the BMJ is on line (full text link).
The changes were sufficient that it seems worth posting the original version (with links embedded for convenience).
The cuts are a bit ironic, since the whole point of the article is to point out the stifling political correctness that has gripped the BMA, the royal colleges, and the Department of Health when it comes to dealing with evidence-free medicine. It has become commonplace for people to worry about the future of the print media, The fact of the matter is you can often find a quicker. smarter amd blunter response to the news on blogs than you can find in the dead tree media. I doubt that the BMJ is in any danger of course. It has a good reputation for its attitude to improper drug company influence (a perpetual problem for clinical journals) as well as for clinical and science articles. It’s great to see its editor, Fiona Godlee, supporting the national campaign for reform of the libel laws (please sign it yourself).
The fact remains that when it comes to the particular problem of magic medicine, the action has not come from the BMA, the royal colleges, and certainly not from the Department of Health, It has come from what Goldacre called the “intrepid, ragged band of bloggers”. They are the ones who’ve done the investigative journalism, sent complaints and called baloney wherever they saw it. This article was meant to celebrate their collective efforts and to celebrate the fact that those efforts are beginning to percolate upwards to influence the powers that be.
It seems invidious to pick on one example, but if you want an example of beautiful and trenchant writing on one of the topics dealt with here, you’d be better off reading Andrew Lewis’s piece "Meddling Princes, Medical Regulation and Licenses to Kill” than anything in a print journal.
I was a bit disappointed by removal of the comment about the Prince of Wales. In fact I’m not particularly republican compared with many of my friends. The royal family is clearly good for the tourist industry and that’s important. Since Mrs Thatcher (and her successors) destroyed large swathes of manufacturing and put trust in the vapourware produced by dishonest and/or incompetent bankers, it isn’t obvious how the UK can stay afloat. If tourists will pay to see people driving in golden coaches, that’s fine. We need the money. What is absolutely NOT acceptable is for royals to interfere in the democratic political process. That is what the Prince of Wales does incessantly. No doubt he is well-meaning, but that is not sufficient. If I wanted to know the winner of the 2.30 at Newmarket, it might make sense to ask a royal. In medicine it makes no sense at all. But the quality of the advice is irrelevant anyway. The royal web site itself says “As a constitutional monarch, the Sovereign must remain politically neutral.”. Why does she not apply that rule to her son? Time to put him over your knee Ma’am?
Two of the major bits that were cut out are shown in bold, The many other changes are small.
BMJ editorial December 2009
Secret remedies: 100 years onTime to look again at the efficacy of remedies Jeffrey Aronson in his article [1] gives a fascinating insight into how the BMA, BMJ and politicians tried, a century ago, to put an end to the marketing of secret remedies. They didn’t have much success. The problems had not improved 40 years later when A.J. Clark published his book on patent medicines [2]. It is astounding to see how little has changed since then. He wrote, for example, “On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”> Clark himself was sued for libel after he’d written in a pamphlet “ ‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”. Although he initially tried to fight the case, impending destitution eventually forced him to apologise [3]. If that happened today, the accusation would have been repeated on hundreds of web sites round the world within 24 hours, and the quack would, with luck, lose [4]. As early as 1927, Clark had written “Today some travesty of physical science appears to be the most popular form of incantation” [5]. That is even more true today. Homeopaths regularly talk utter nonsense about quantum theory [6] and ‘nutritional therapists’ claim to cure AIDS with vitamin pills or even with downloaded music files. Some of their writing is plain delusional, but much of it is a parody of scientific writing. The style, which Goldacre [7] calls ‘sciencey’, often looks quite plausible until you start to check the references. A 100 years on from the BMA’s efforts, we need once again to look at the efficacy of remedies. Indeed the effort is already well under way, but this time it takes a rather different form. The initiative has come largely from an “intrepid, ragged band of bloggers” and some good journalists, helped by many scientific societies, but substantially hindered by the BMA, the Royal Colleges, the Department of Health and a few vice-chancellors. Even NICE and the MHRA have not helped much. The response of the royal colleges to the resurgence in magic medicine that started in the 1970s seems to have been a sort of embarrassment. They pushed the questions under the carpet by setting up committees (often populated with known sympathizers) so as to avoid having to say ‘baloney’. The Department of Health, equally embarrassed, tends to refer the questions to that well-known medical authority, the Prince of Wales (it is his Foundation for Integrated Health that was charged with drafting National Occupational Standards in make-believe subjects like naturopathy [8]. Two recent examples suffice to illustrate the problems. The first example is the argument about the desirability of statutory regulation of acupuncture, herbal and traditional Chinese medicine (the Pittilo recommendations) [9]. Let’s start with a definition, taken from ‘A patients’ guide to magic medicine’ [10]. “Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety”. It seems to me to be self-evident that you cannot start to think about a sensible form of regulation unless you first decide whether what you are trying to regulate is nonsense, though this idea does not seem to have penetrated the thinking of the Department of Health or the authors of the Pittilo report. The consultation on statutory regulation has had many submissions [11] that point out the danger to patients of appearing to give official endorsement of treatments that don’t work. The good news is that there seems to have been a major change of heart at the Royal College of Physicians. Their submission points out with admirable clarity that the statutory regulation of things that don’t work is a danger to patients (though they still have a blank spot about the evidence for acupuncture, partly as a result of the recent uncharacteristically bad assessment of the evidence by NICE [12]). Things are looking up. Nevertheless, after the public consultation on the report ended on November 16th, the Prince of Wales abused his position to make a well-publicised intervention on behalf of herbalists [13]. Sometimes I think his mother should give him a firm lesson in the meaning of the term ‘constitutional monarchy’, before he destroys it. The other example concerns the recent ‘evidence check: homeopathy’ conducted by the House of Commons Science and Technology Select Committee (SCITECH). First the definition [10]: “Homeopathy: giving patients medicines that contain no medicine whatsoever”. When homeopathy was dreamt up, at the end of the 18th century, regular physicians were lethal blood-letters, and it’s quite likely that giving nothing saved people from them. By the mid-19th century, discoveries about the real causes of disease had started, but homeopaths remain to this day stuck in their 18th century time warp. In 1842 Oliver Wendell Holmes said all that needed to be said about medicine-free medicine [14]. It is nothing short of surreal that the UK parliament is still discussing it in 2009. Nevertheless it is worth watching the SCITECH proceedings [15]. The first two sessions are fun, if only for the statement by the Professional Standards Director of Boots that they sell homeopathic pills while being quite aware that they don’t work. I thought that was rather admirable honesty. Peter Fisher, clinical director of the Royal Homeopathic Hospital, went through his familiar cherry-picking of evidence, but at least repeated his condemnation of the sale of sugar pills for the prevention of malaria. But for pure comedy gold, there is nothing to beat the final session. The health minister, Michael O’Brien, was eventually cajoled into admitting that there was no good evidence that homeopathy worked but defended the idea that the taxpayer should pay for it anyway. It was much harder to understand the position of the chief scientific advisor in the Department of Health, David Harper. He was evasive and ill-informed. Eventually the chairman, Phil Willis, said “No, that is not what I am asking you. You are the Department’s Chief Scientist. Can you give me one specific reference which supports the use of homeopathy in terms of Government policy on health?”. But answer came there none (well, there were words, but they made no sense). Then at the end of the session Harper said “homeopathic practitioners would argue that the way randomised clinical trials are set up they do not lend themselves necessarily to the evaluation and demonstration of efficacy of homeopathic remedies, so to go down the track of having more randomised clinical trials, for the time being at least, does not seem to be a sensible way forward.” Earlier, Kent Woods (CEO of the MHRA) had said “the underlying theory does not really give rise to many testable hypotheses”. These two eminent people seemed to have been fooled by the limp excuses offered by homeopaths. The hypotheses are testable and homeopathy, because it involves pills, is particularly well suited to being tested by proper RCTs (they have been, and when done properly, they fail). If you want to know how to do it, all you have to do is read Goldacre in the Guardian [16]. It really isn’t vert complicated. “Imagine going to an NHS hospital for treatment and being sent away with nothing but a bottle of water and some vague promises.” “And no, it’s not a fruitcake fantasy. This is homeopathy and the NHS currently spends around £10million on it.” That was written by health journalist Jane Symons, in The Sun [17]. A Murdoch tabloid has produced a better account of homeopathy than anything that could be managed by the chief scientific advisor to the Department of Health. And it isn’t often that one can say that. These examples serve to show that the medical establishment is slowly being dragged, from the bottom up, into realising that matters of truth and falsehood are more important than their knighthoods. It is all very heartening, both for medicine and for democracy itself. David Colquhoun. Declaration of interests. I was A.J. Clark chair of pharmacology at UCL, 1985 – 2004. 1. Aronson, JK BMJ 2009;339:b5415 2. Clark, A,J, (1938) Patent Medicines FACT series 14, London. See also Patent medicines in 1938 and now https://www.dcscience.net/?p=257 3. David Clark “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3) 4. Lewis, A. (2007) The Gentle Art of Homeopathic Killing 5. A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927 6. Chrastina, D (2007) Quantum theory isn’t that weak, (response to Lionel Milgrom). 7 Goldacre, B. (2008) Bad Science. HarperCollins 8. Skills for Health web site 9. A very bad report: gamma minus for the vice-chancellor 10. A Patients’ Guide to Magic Medicine, and also in the Financial Times. 12. NICE fiasco, part 2. Rawlins should withdraw guidance and start again 13. BBC news 1 December 2009 Prince Charles: ‘Herbal medicine must be regulated’. 14. Oliver Wendell Holmes (1842) Homeopathy and Its Kindred Delusions. 15. House of Commons Science and technology committee. Evidence check: homeopathy. Videos and transcripts available at http://www.viewista.com/s/fywlp2/ez/1 16. Goldacre, B. A Kind of Magic Guardian 16 November 2007. 17. Homeopathy is resources drain says |
Follow-up
There is a good account of the third SCITECH session by clinical science consultant, Majikthyse, at The Three Amigos.
16 December 2009.. Recorded an interview for BBC Radio 5 Live. It was supposed to go out early on 17th.
17 December 2009. The editorial is mentioned in Editor’s Choice, by deputy editor Tony Delamothe. I love his way of putting the problem "too many at the top of British medicine seem frozen in the headlights of the complementary medicine bandwagon". He sounds remarkably kind given that I was awarded (by the editor, Fiona Godlee, no less) a sort of booby prize at the BMJ party for having generated a record number of emails during the editing of a single editorial (was it really 24?). Hey ho.
17 December 2009. More information on very direct political meddling by the Prince of Wales in today’s Guardian, and in Press Association report.
17 December 2009. Daily Telegraph reports on the editorial, under the heading “ ‘Nonsense’ alternative medicines should not be regulated“. Not a bad account for a non-health journalist.
17 December 2009. Good coverage in the excellent US blog, Neurologica, by the superb Steven Novella.’ “Intrepid, Ragged Band of Bloggers” take on CAM‘ provides a chance to compare and contrast the problems in the UK and the USA.’
18 December 2009. Article in The Times by former special advisor, Paul Richards. “The influence of Prince Charles the lobbyist is out of hand. Our deference stops us asking questions.”
“A good starting point might be publication of all correspondence over the past 30 years. Then we will know the extent, and influence, of Prince Charles the lobbyist.”
Comments in the BMJ Quite a lot of comments had appeared by January 8th, though sadly they were mostly from the usual suspects who appear every time one suggests evidence matters. A reply was called for, so I sent this (the version below has links).
After a long delay, this response eventually appeared in the BMJ on January 15 2010.
It’s good to see so many responses, though somewhat alarming to see that several of them seem to expect an editorial to provide a complete review of the literature. I ‘ll be happy to provide references for any assertion that I made.
I also find it a bit odd that some people think that an editorial is not the place to express an opinion robustly. That view seems to me to be a manifestation of the very sort of political correctness that I was deploring. It’s a bit like the case when the then health minister, Lord Hunt, referred to psychic surgery as a “profession” when he should have called it a fraudulent conjuring trick. Anything I write is very mild compared with what Thomas Wakley wrote in the Lancet, a journal which he founded around the time UCL came into existence. For example (I quote)
“[We deplore the] “state of society which allows various sets of mercenary, goose-brained monopolists and charlatans to usurp the highest privileges…. This is the canker-worm which eats into the heart of the medical body.” Wakley, T. The Lancet 1838-9, 1
I don’t think it is worth replying to people who cite Jacques Benveniste or Andrew Wakefield as authorities. Neither is it worth replying to people who raise the straw man argument about wicked pharmaceutical companies (about which I am on record as being as angry as anyone). But I would like to reply directly to some of the more coherent comments.
Sam Lewis and Robert Watson. [comment] Thank you for putting so succinctly what I was trying to say.
Peter Fisher [comment]. I have a lot of sympathy for Peter Fisher. He has attempted to do some good trials of homeopathy (they mostly had negative outcomes). He said he was "very angry" when the non-medical homeopaths were caught out recommending their sugar pills for malaria prevention (not that this as stopped such dangerous claims which are still commonplace). He agreed with me that there was not sufficient scientific basis for BSc degrees in homeopathy. I suppose that it isn’t really surprising that he continues to cherry pick the evidence. As clinical director of the Royal London Homeopathic Hospital and Homeopathic physician to the Queen, just imagine the cognitive dissonance that would result if he were to admit publicly that is all placebo after all. He has come close though. His (negative) trial for homeopathic treatment of rheumatoid arthritis included the words "It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response” [2]. [download
the paper]. When it comes to malaria, it matters a lot.
Adrian White [comment] seems to be cross because I cited my own blog. I did that simply because if he follows the links there he will find the evidence. In the case of acupuncture it has been shown time after time that "real" acupuncture does not differ perceptibly from sham. That is true whether the sham consists of retractable needles or real needles in the "wrong" places. A non-blind comparison between acupuncture and no acupuncture usually shows some advantage for the former but it is, on average, too small to be of much clinical significance [3]. I agree that there is no way to be sure that this advantage is purely placebo effect but since it is small and transient it really doesn’t matter much. Nobody has put it more clearly than Barker Bausell in his book, Snake Oil Science [4]
White also seems to have great faith in peer review. I agree that in real science it is probably the best system we have. But in alternative medicine journals the "peers" are usually other true believers in whatever hocus pocus is being promoted and peer reveiw breaks down altogether.
R. M. Pittilo [comment] I’m glad that Professor Pittilo has replied in person because I did single out his report for particular criticism. I agree that his report said that NHS funding should be available to CAM only where there is evidence of efficacy. That was not my criticism. My point was that in his report, the evidence for efficacy was assessed by representatives of Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Every one of them would have been out of work if they had found their subjects were nonsense and that, no doubt, explains why the assessment was so bad. To be fair, they did admit that the evidence was not all that it might be and recommended (as always) more research I’d like to ask Professor Pittilo how much money should be spent on more research in the light of the fact that over a billion dollars has been spent in the USA on CAM research without producing a single useful treatment. Pittilo says "My own view is that both statutory regulation and the quest for evidence should proceed together" but he seems to neglect the possibility that the quest for evidence might fail. Experience in the USA suggests that is exactly what has, to a large extent, already happened.
I also find it quite absurd that the Pittilo report should recommend, despite a half-hearted admission that the evidence is poor, that entry to these subjects should be via BSc Honours degrees. In any case he is already thwarted in that ambition because universities are closing down degrees in these subjects having realised that the time to run a degree is after, not before, you have some evidence that the subject is not nonsense. I hope that in due course Professor Pittilo may take the same action about the courses in things like homeopathy that are run by the university of which he is vice-chancellor. That could only enhance the academic reputation of Robert Gordon’s University.
George Lewith [comment] You must be aware that the proposed regulatory body, the Health Professions Council, has already broken its own rules about "evidence-based practice" by agreeing to take on, if asked, practitioners of Herbal Medicine, Chinese Medicine and Acupuncture. They have (shamefully) excluded the idea that claims of efficacy would be regulated. In other word they propose to provide exactly the sort of pseudo-regulation which would endanger patients They are accustomed to the idea that regulation is to do only with censoring practitioners who are caught in bed with patients. However meritorious that may be, it is not the main problem with pseudo-medicine, an area in which they have no experience. I’m equally surprised that Lewith should recommend that Chinese evaluation of Traditional Chinese medicine should be included in meta-analyses, in view of the well-known fact that 99% of evaluations from China are positive: “No trial published in China or Russia/USSR found a test treatment to be ineffective” [5]. He must surely realise that medicine in China is a branch of politics. In fact the whole resurgence in Chinese medicine and acupuncture in post-war times has less to do with ancient traditions than with Chinese nationalism, in particular the wish of Mao Tse-Tung to provide the appearance of health care for the masses (though it is reported that he himself preferred Western Medicine).
1. Lord Hunt thinks “psychic surgery” is a “profession”. https://www.dcscience.net/?p=258
2. Fisher, P. Scott, DL. 2001 Rheumatology 40, 1052 – 1055. [pdf file]
3. Madsen et al, BMJ 2009;338:a3115 [pdf file]
4. R, Barker Bausell, Snake Oil Science, Oxford University Press, 2007
5. Vickers, Niraj, Goyal, Harland and Rees (1998, Controlled Clinical Trials, 19, 159-166) “Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials”. [pdf file]
15 January 2010. During the SciTech hearings, Kent Woods (CEO of the MHRA) made a very feeble attempt to defend the MHRA’s decision to allow misleading labelling of homeopathic products. Now they have published their justification for this claim. It is truly pathetic, as explained by Martin at LayScience: New Evidence Reveals the MHRA’s Farcical Approach to Homeopathy. This mis-labelling cause a great outcry in 2006, as documented in The MHRA breaks its founding principle: it is an intellectual disgrace, and Learned Societies speak out against CAM, and the MHRA.
22 January 2010 Very glad to see that the minister himself has chosen to respond in the BMJ to the editorial
|
Rt Hon. Mike O’Brien QC MP, Minister of State for Health Services I am glad that David Colquhoun was entertained by my appearance before the Health Select Committee on Homeopathy. But he is mistaken when he says, “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense.” Regulation is about patient safety. Acupuncture, herbal and traditional Chinese medicine involve piercing the skin and/or the ingestion of potentially harmful substances and present a possible risk to patients. The Pittilo Report recommends statutory regulation and we have recently held a public consultation on whether this is a sensible way forward. Further research into the efficacy of therapies such as Homeopathy is unlikely to settle the debate, such is the controversy surrounding the subject. That is why the Department of Health’s policy towards complementary and alternative medicines is neutral. Whether I personally think Homeopathy is nonsense or not is besides the point. As a Minister, I do not decide the correct treatment for patients. Doctors do that. I do not propose on this occasion to interfere in the doctor-patient relationship. |
Here is my response to the minister
|
I am very glad that the minister himself has replied. I think he is wrong in two ways, one relatively trivial but one very important. First, he is wrong to refer to homeopathy as controversial. It is not. It is quite the daftest for the common forms of magic medicine and essentially no informed person believes a word of it. Of course, as minister, he is free to ignore scientific advice, just as the Home Secretary did recently. But he should admit that that is what he is doing, and not hide behind the (imagined) controversy. Second, and far more importantly, he is wrong, dangerously wrong, to say it I was mistaken to claim that “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense". According to that view it would make sense to grant statutory regulation to voodoo and astrology. The Pittilo proposals would involve giving honours degrees in nonsense if one took the minister’s view that it doesn’t matter whether the subjects are nonsense or not. Surely he isn’t advocating that? The minister is also wrong to suppose that regulation, in the form proposed by Pittilo, would do anything to help patient safety. Indeed there is a good case to be made that it would endanger patients (not to mention endangering tigers and bears). The reason for that is that the main danger to patients arises from patients being given “remedies” that don’t work. The proposed regulatory body, the Health Professions Council, has already declared that it is not interested in whether the treatments work or not. That in itself endangers patients. In the case of Traditional Chinese Medicine, there is also a danger to patients from contaminated medicines. The HPC is not competent to deal with that either. It is the job of the MHRA and/or Trading Standards. There are much better methods of ensuring patient safety that those proposed by Pittilo. In order to see the harm that can result from statutory regulation, it is necessary only to look at the General Chiropractic Council. Attention was focussed on chiropractic when the British Chiropractic Association decided, foolishly, to sue Simon Singh for defamation. That led to close inspection of the strength of the evidence for their claims to benefit conditions like infant colic and asthma. The evidence turned out to be pathetic, and the result was that something like 600 complaints were made to the GCC about the making of false health claims (including two against practices run by the chair of the GCC himself). The processing of these complaints is still in progress, but what is absolutely clear is that the statutory regulatory body, the GCC, had done nothing to discourage these false claims. On the contrary it had perpetrated them itself. No doubt the HPC would be similarly engulfed in complaints if the Pittilo proposals went ahead. It is one thing to say that the government chooses to pay for things like homeopathy, despite it being known that they are only placebos, because some patients like them. It is quite another thing to endanger patient safety by advocating government endorsement in the form of statutory regulation, of treatments that don’t work. I would be very happy to meet the minister to discuss the problems involved in ensuring patient safety. He has seen herbalists and other with vested interests. He has been lobbied by the Prince of Wales. Perhaps it is time he listened to the views of scientists too. |
Both the minister’s response, and my reply, were reformatted to appear as letters in the print edition of the BMJ, as well as comments on the web..
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
More boring politics, but it matters. The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register should normally be through a Bachelor degree with Honours
For the background on this appalling report, see earlier posts.
A very bad report: gamma minus for the vice-chancellor
The Times (blame subeditor for the horrid title), and some follow up on the Times piece
The Health Professions Council breaks its own rules: the result is nonsense
Chinese medicine -acupuncture gobbledygook revealed
Consultation opens on the Pittilo report: help stop the Department of Health making a fool of itself
Why degrees in Chinese medicine are a danger to patients
The Department of Health consultation shuts on November 2nd. If you haven’t responded yet, please do. It would be an enormous setback for reason and common sense if the government were to give a stamp of official approval to people who are often no more than snake-oil salesman.
Today I emailed my submission to the Pittilo consultation to the Department of Health, at HRDListening@dh.gsi.gov.uk
The submission
I sent the following documents, updated versions of those already posted earlier.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
- An example of dangerous (and probably illegal) claims that are routinely made by TCM practitioners [download pdf]f
I also completed their questionnaire, despite its deficiencies. In case it is any help to anyone, this is what I said:
The questionnaire
Q1: What evidence is there of harm to the public currently as a result of the activities of acupuncturists, herbalists and traditional Chinese medicine practitioners? What is its likelihood and severity?
Harm
No Harm
Unsure
Comment
The major source of harm is the cruel deception involved in making false claims of benefit to desperate patients. This applies to all three.
In the case of herbal and TCM there is danger from toxicity because herbal preparations are unstandardised so those that do contain an active ingredient are given in an unknown dose. This is irresponsible and dangerous (but would not be changed by the proposals for regulation).
In addition TCM suffers from recurrent problems of contamination with heavy metals, prescription drugs and so on. Again this would not be the business of the proposed form of regulation.
Q2: Would this harm be lessened by statutory regulation? If so, how?
Yes
No
Unsure
The proposed form of regulation would be no help at all. The HPC has already said that it is not concerned with whether or not the drug works, and, by implication, does not see itself as preventing false health claims (just as the GCC doesn’t do this). False claims are the responsibility of Trading Standards who are meant to enforce the Consumer Protection Unfair Trading Regulations (May 2008), though they do not at present enforce them very effectively. Also Advertisng Standards. The proposed regulation would not help, and could easily hinder public safety as shown by the fact that the GCC has itself been referred to the Advertisng Standards Authority.
The questions of toxicity and contamination are already the responsibility of Trading Standards and the MHRA. Regulation by the HPC would not help at all. The HPC is not competent to deal with such questions.
Q3: What do you envisage would be the benefit to the public, to practitioners and to businesses, associated with introducing statutory regulation?
Significant benefit
Some benefit
No benefit
Unsure
This question is badly formulated because the answer is different according to whether you are referring to the public, to practitioners or to businesses.
The public would be endangered by the form of regulation that is proposed, as is shown very clearly by the documents that I have submitted separately.
In the case of practitioners and businesses, there might be a small benefit, if the statutory regulation gave the impression that HM and TCM had government endorsement and must therefore be safe and effective.
There is also one way that the regulation could harm practitioners and businesses. If the HPC received a very large number of complaints about false health claims, just as the GCC has done recently, not only would it cost a large amount of money to process the claims, but the attendant bad publicity could harm practitioners. It is quite likely that this would occur since false claims to benefit sick people are rife in the areas of acupuncture, HM and TCM.
Q4: What do you envisage would be the regulatory burden and financial costs to the public, to practitioners, and to businesses, associated with introducing statutory regulation? Are these costs justified by the benefits and are they proportionate to the risks? If so, in what way?
Justified
Not Justified
Unsure
Certainly not justified. Given that I believe that the proposed form of regulation would endanger patients, no cost at all would be justified. But even if there were a marginal benefit, the cost would be quite unjustified. The number of practitioners involved is very large. It would involve a huge expansion of an existing quango, at a time when the government is trying to reduce the number of quangos. Furthermore, if the HPC were flooded with complaints about false health claims, as the GCC has been, the costs in legal fees could be enormous.
Q5: If herbal and TCM practitioners are subject to statutory regulation, should the right to prepare and commission unlicensed herbal medicines be restricted to statutorily regulated practitioners?
Yes
No
Unsure
I don’t think it would make much difference. The same (often false) ideas are shared by all HM people and that would continue to be the same with or without SR.
Q6: If herbal and TCM practitioners are not statutorily regulated, how (if at all) should unlicensed herbal medicines prepared or commissioned by these practitioners be regulated?
They could carry on as now, but the money that would have been spent on SR should instead be used to give the Office of Trading Standards and the MHRA the ability to exert closer scrutiny and to enforce more effectively laws that already exist. Present laws, if enforced, are quite enough to protect the public.
Q7: What would be the effect on public, practitioners and businesses if, in order to comply with the requirements of European medicines legislation, practitioners were unable to supply manufactured unlicensed herbal medicines commissioned from a third party?
Significant effect
Some effect
No effect
Unsure
European laws,especialliy in food area, are getting quite strict about the matters of efficacy. The proposed regulation, which ignores efficacy, could well be incompatible with European law, if not now, then soon. This would do no harm to legitimate business though it might affect adversely businesses which make false claims (and there are rather a lot of the latter).
Q8: How might the risk of harm to the public be reduced other than by orthodox statutory regulation? For example by voluntary self-regulation underpinned by consumer protection legislation and by greater public awareness, by accreditation of voluntary registration bodies, or by a statutory or voluntary licensing regime?
Voluntary self-regulation
Accreditation of voluntary bodies
Statutory or voluntary licensing
Unsure
I disagree with the premise, for reasons given in detail in separate documents. I believe that ‘orthodox statutory regulation’, if that means the Pittilo proposals, would increase, not decrease, the risk to the public. Strengthening the powers of Trading Standards, the MHRA and such consumer protection legislation would be far more effective in reducing risk to the public than the HPC could ever be. Greater public awareness of the weakness of the evidence for the efficacy of these treatments would obviously help too, but can’t do the job on its own.
Q10: What would you envisage would be the benefits to the public, to practitioners, and to businesses, for the alternatives to statutory regulation outlined at Question 8?
It depends on which alternative you are referring to. The major benefit of enforcement of existing laws by Trading Standards and/or the MHRA would be (a) to protect the public from risk, (b) to protect the public from health fraud and (c) almost certainly lower cost to the tax payer.
Q11: If you feel that not all three practitioner groups justify statutory regulation, which group(s) does/do not and please give your reasons why/why not?
Acupuncture
Herbal Medicine
TCM
Unsure
None of them. The differences are marginal. In the case of acupuncture there has been far more good research than for HM or TCM. But the result of that research is to show that in most cases the effects are likely to be no more than those expected of a rather theatrical placebo. Furthermore the extent to which acupuncture has a bigger effect than no-acupuncture in a NON-BLIND comparison, is usually too small and transient to offer any clinical advantage (so it doesn’t really matter whether the effect is placebo or not, it is too small to be useful).
In the case of HM, and even more of TCM, there is simply not enough research to give much idea of their usefulness, with a small handful of exceptions.
This leads to a conclusion that DH seems to have ignored in the past. It makes absolutely no sense to talk about “properly trained practitioners” without first deciding whether the treatments work or not. There can be no such thing as “proper training” in a discipline that offers no benefit over placebo. It is a major fault of the Pittilo recommendations that they (a) ignore this basic principle and (b) are very over-optimistic about the state of the evidence.
Q12: Would it be helpful to the public for these practitioners to be regulated in a way which differentiates them from the regulatory regime for mainstream professions publicly perceived as having an evidence base of clinical effectiveness? If so, why? If not, why not?
Yes
No
Unsure
It might indeed be useful if regulation pointed out the very thin evidence base for HM and TCM but it would look rather silly. The public would say how can it be that the DH is granting statutory regulation to things that don’t work?
Q13: Given the Government’s commitment to reducing the overall burden of unnecessary statutory regulation, can you suggest which areas of healthcare practice present sufficiently low risk so that they could be regulated in a different, less burdensome way or de-regulated, if a decision is made to statutorily regulate acupuncturists, herbalists and traditional Chinese medicine practitioners?
Yes
No
Unsure
As stated above, the.only form of regulation that is needed, and the only form that would protect the public, is through consumer protection regulations, most of which already exist (though they are enforced in a very inconsistent way). Most statutory regulation is objectionable, not on libertarian grounds, but because it doesn’t achieve the desired ends (and is expensive). In this case of folk medicine, like HM and TCM, the effect would be exactly the opposite of that desired as shown in separate documents that I have submitted to the consultation.
Q14: If there were to be statutory regulation, should the Health Professions Council (HPC) regulate all three professions? If not, which one(s) should the HPC not regulate?
Yes
No
Unsure
The HPC should regulate none of them. It has never before regulated any form of alternative medicine and it is ill-equipped to do so. Its statement that it doesn’t matter that there is very little evidence that the treatments work poses a danger to patients (as well as being contrary to its own rules).
Q15: If there were to be statutory regulation, should the Health Professions Council or the General Pharmaceutical Council/Pharmaceutical Society of Northern Ireland regulate herbal medicine and traditional Chinese medicine practitioners?
HPC
GPC/PSNI
Unsure
Neither. The GPC is unlikely to care about whether the treatments work any more than the RPSGB did, or the GCC does now. The problems would be exactly the same whichever body did it.
Q16: If neither, who should and why?
As I have said repeatedly, it should be left to Trading Standards, the MHRA and other consumer protection regulation.
Q17:
a) Should acupuncture be subject to a different form of regulation from that for herbalism and traditional Chinese medicine? If so, what?
Yes
No
Unsure
b) Can acupuncture be adequately regulated through local means, for example through Health and Safety legislation, Trading Standards legislation and Local Authority licensing?
Yes
No
Unsure
(a) No -all should be treated the same. Acupuncture is part of TCM
(b) Yes
Q18.
a) Should the titles acupuncturist, herbalist and [traditional] Chinese medicine practitioner be protected?
b) If your answer is no which ones do you consider should not be legally protected?
Yes
No
Unsure
No. It makes no sense to protect titles until such time as it has been shown that the practitioners can make a useful contribution to medicine (above placebo effect). That does not deny that placebos may be useful at times. but if that is all they are doing, the title should be ‘placebo practitioners’.
Q19: Should a new model of regulation be tested where it is the functions of acupuncture, herbal medicine and TCM that are protected, rather than the titles of acupuncturist, herbalist or Chinese medicine practitioner?
Yes
No
Unsure
No. This makes absolutely no sense when there is so little knowledge about what is meant by the ” functions of acupuncture, herbal medicine and TCM”.Insofar as they don’t work (better than placebo), there IS no function. Any attempt to define function when there is so little solid evidence (at least for HM and TCM) is doomed to failure.
Q20: If statutory professional self-regulation is progressed, with a model of protection of title, do you agree with the proposals for “grandparenting” set out in the Pittilo report?
Yes
No
Unsure
No. I believe the Pittilo report should be ignored entirely. The whole process needs to be thought out again in a more rational way.
Q22: Could practitioners demonstrate compliance with regulatory requirements and communicate effectively with regulators, the public and other healthcare professionals if they do not achieve the standard of English language competence normally required for UK registration? What additional costs would occur for both practitioners and regulatory authorities in this case?
Yes
No
Unsure
No. It is a serious problem, in TCM especially, that many High Street practitioners speak hardly any English at all. That adds severely to the already considerable risks. There would be no reliable way to convey what was expected of them. it would be absurd for the taxpayer to pay for them to learn English for the purposes of practising TCM (of course there might be the same case as for any other immigrant for teaching English on social grounds).
Q23: What would the impact be on the public, practitioners and businesses (financial and regulatory burden) if practitioners unable to achieve an English language IELTS score of 6.5 or above are unable to register in the UK?
Significant impact
Some impact
No impact
Unsure
The question is not relevant. The aim of regulation is to protect the public from risk (and it should be, but isn’t, an aim to protect them from health fraud). It is not the job of regulation to promote businesses
Q24: Are there any other matters you wish to draw to our attention?
I have submitted three documents via HRDListening@dh.gsi.gov.uk. The first of these puts the case against the form of regulation proposed by Pittilo, far more fluently than is possible in a questionnaire.
Another shows examples of what is actually taught in degrees in acupuncture, HM and TCM. They show very graphically the extent to which the Pittilo proposals would endanger the public, if they were to be implemented..
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
Acupuncture in the BMJ
A new review appeared in the BMJ today. It is by Madsen et al., from the Nordic Cochrane Centre, Copenhagen. Here are the conclusions.
- The analgesic effect of acupuncture is small and cannot be distinguished from bias resulting from incomplete blinding.
- The analgesic effect of placebo acupuncture is moderate but very variable as some large trials report substantial effects.
- The effect of acupuncture seems to be unrelated to the type of placebo acupuncture used as control.
The results confirm, yet again, that there is essentially no difference between “real” acupuncture and sham acupuncture. All that talk about meridians and Qi really is so much mumbo jumbo.
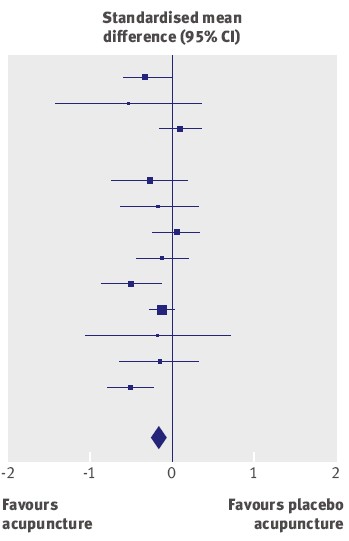
The average effect (the diamond at the bottom) is essentially zero.
It has often been supposed that acupuncture is a theatrical placebo, but because of the placebo effect it produces more pain relief than (non-blind) controls. This study confirms that there is likely to be such an effect, but it also finds that the size of the placebo effect is too small to be useful to patients. Here is the comparison between sham acupuncture and no acupuncture at all.
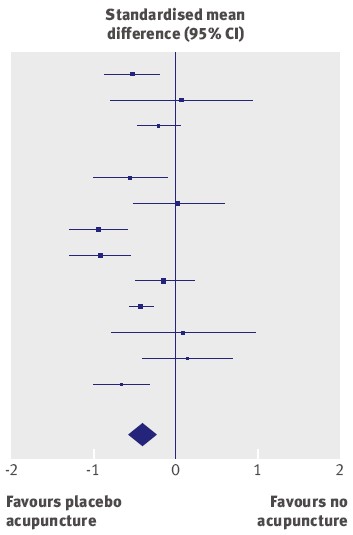
The results of different trials are very variable, but the average effect (diamond at the bottom) favours sham acupuncture over no acupuncture at all.
But how big is the effect? The numbers along the bottom of the graph are ‘standardised mean differences’. The average value of -0.42 (95% confidence limits -0.6 to -0.23) between ‘no acupuncture’ and ‘sham acupuncture’ corresponds to a difference of about 10 points on a 100 point scale. This difference is big enough to be real, in the sense that it isn’t just chance. But is it big enough to be useful to the patient? Probably not. Madsen et al conclude
“a consensus report characterised a 10mm reduction on a 100 mm visual analogue scale as representing a “minimal” change or “little change”. Thus, the apparent analgesic effect of acupuncture seems to be below a clinically relevant pain improvement.”
This makes nonsense of the Pittilo report. Notice that these results, yet again, make nonsense of the proposals in the gamma-minus Pittilo report, to pseudo-regulate acupuncture, and to have degrees in the subject.
Cochrane reviews of Acupuncture : and a bad report from BBC
Two new Cochrane reviews appeared last week, Acupuncture for tension-type headache, and Acupuncture for migraine prophylaxis.
You can’t blame subeditors for the appalling title of the BBC’s report on Acupuncture ‘works for headaches’. The content is pretty misleading too. (The link is to a version saved at 19.35 on 21 January 2009.). Furthermore, like far too many of the BBC reports, it is anonymous. One has no idea to blame This is important, if only because the BBC news site is so influential. Twelve hours after posting the misleading title has been copied all round the world.
In the Guardian, Ian Sample had a much better report, Even’fake’ acupuncture reduces the severity of headaches and migraines. Sadly the print edition had the title “Acupuncture aids migraines, researchers
find”, but that can be blamed on subeditors who have a problem with reading (in fact Sample had seen neither title).
The BBC report seemed to call for a complaint. This is what I sent.
| I wish to complain about the report on acupuncture at http://news.bbc.co.uk/1/hi/health/7838231.stm
The title itself was highly misleading “Acupuncture works for headaches” is precisely the opposite of what was shown, namely that it is no better than sham acupuncture controls. The article goes on to say
It is not said that there isn’t the slightest reason to think this is true (or even means anything) , and that the work which is being reported is strong evidence that it’s not true
That is wrong. University of Salford , for example has just closed its acupuncture course after a number of us have pointed out that it is teaching things that aren’t true
It is exactly the opposite of an endorsement. It is one more nail in the coffin of acupuncture as generally understood. This article, I contend, is partial and misleading. Unfortunately it is anonymous. |
Follow-up
Today’s BBC report on the BMJ paper is almost as partisan as the one that I just complained about. “Confusion on acupuncture benefit ” exaggerates greatly the amount of confusion. Worse still, it quotes only two well-known advocates of acupuncture, people who make their living from it. No independent scientific voice is to be heard.
One of those cited is Adrian White. He is described as “a researcher into acupuncture at the Peninsula Medical School”. There is no mention of the fact that he is also Editor in Chief of the journal Acupuncture in Medicine. The other person who is quoted is Mike O’Farrell, the chief executive of the British Acupuncture Council. What do you expect him to say?
I’ve just sent another complaint, about today’s BBC report. The more the merrier.
The BMJ itself published an editorial on the Madsen paper. It seems very odd that they should have chosen the editors of the BMJ-group journal, Acupuncture in Medicine, to comment on a paper that sounds the death knell for the subject from which they make their living. Needless to say, the editorial attempted to wriggle out of the obvious conclusions. Worse still, the Health editor of the BBC web site referred to the editorial in his defence, in response to my complaint.
Channel 4 News does a lot better than the BBC, or the BMJ editorial, with its report Acupuncture ‘fails to relieve pain’
“Claims that acupuncture can relieve pain have been undermined by the results of a new study.”
“senior researcher Asbjorn Hrobjartsson said: “Our findings question both the traditional foundation of acupuncture…and the prevailing theory that acupuncture has an important effect on pain in general”. “
The Daily Telegraph also, like almost everyone else, did better than the BBC, with “Acupuncture ‘has almost no effect in relieving pain’”
“The pain relieving effects of acupuncture are so small that they may be clinically irrelevant, according to a review of research into the treatment.”
Even Metro, the free London Newspaper, is more accurate then the BBC. They carry a short report “Acupuncture ‘has no medical point’.”
“The pain-relieving effects of acupuncture compared with a placebo are so small they may be clinically irrelevant.”
New review puts in doubt traditional foundation of acupuncture. Believe it or not, that is the title of the report on Madsen et al from the Prince’s Foundation for Integretad Health! Don’t get too excited though. They haven’t even bothered to look at the original paper, but merely cite the dreadful BBC report. Much prominence is given to the acupuncturists, White and O’Farrell, and the important finding isn’t mentioned at all. Another gamma minus.
The Times today has given s good showing for my comment piece. It gives the case against following the advice of the Pittilo report. It simply makes no sense to have government regulation of acupuncture, herbal medicine, traditional Chinese medicine until such time as there is evidence that they work. It makes even less sense to have BSc degrees in them. The Department of Health should have more sense that to use the Prince of Wales as its scientific advisor.
Let’s hope that the recent example set by the University of Central Lancashire is the start of trend for vice-chancellors to appreciate that running such degrees brings their universities into disrepute.
I can only apologise for the dreadful title that The Times’ sub-editors put on the piece, My original title was
A bad report for the vice chancellor
The Pittilo report to the Department of Health will endanger the public and corrupt universities. There is a better way.
I like that much better than “Regulate quack nedicine? I feel sick”.
But, oh dear, the picture that I sent them is on the left, but what appeared is on the right. Spot the difference.
 |
 |
Well now, at least, I can feel I have something in common with Isambard Kingdom Brunel.
Follow-up
It so happens that Professor Pittilo wrote a letter to Times Higher Education this week. I fear that it provided a yet more evidence that he hasn’t really quite got the hang of evidence.
The Lancashire Evening Post catches up with the UCLan story, two days after you read it here.
A reply from Professor Pittilo
This response to the op-ed of 29th August appeared as a letter
in the Times on Sept 2.
| Public health needs protection
Regulation of acupuncture and herbal medicine has been subject to much scrutiny Sir, Professor Colquhoun’s campaign to discredit our report (“Regulate quack medicine? I feel sick,” Aug 29) is in danger of placing public health at risk. He is entitled to challenge existing evidence for the effectiveness of complementary and alternative medicine (CAM) but fails to acknowledge the key recommendation from the steering group on the essential need to demonstrate efficacy, safety and quality assurance as a prerequisite for NHS funding. Professor Colquhoun dismisses CAM because of the absence of a rigorous scientific foundation and he asserts that to teach and practise it is unethical. Survey data consistently demonstrates very high demand for CAM with one report estimating that 22 million visits involving 10.6 per cent of the population in England alone occurred in 2008. This demand is one reason why his alternative model of trade law enforcement will not work. He may argue that these people are uncritical recipients of nonsense, but data from the Medicines and Healthcare products Regulatory Agency confirm that they are at significant risk from poor practice. It is essential that we protect the public by implementing statutory regulation alongside demanding evidence of efficacy. Professor Colquhoun’s resistance to the teaching of science to CAM practitioners will do little to help them to critically evaluate effectiveness. Professor Michael Pittilo Chair of the Department of Health Steering Group |
And Pittilo wrote in similar vein to Times Higher Education.
Science vital to health study28 August 2008 Your feature on some members of staff at the University of Central Lancashire attacking science degrees in complementary and alternative medicine (“Staff attack science degrees in alternative health”, 7 August) raises a number of concerns. It is up to any university, taking account of the expert views of staff and external peer review, to determine the appropriate title and award for any degree. It is encouraging to note from the feature that new courses The recent report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and other Traditional Medicine There is no doubt that courses that provide a solid scientific foundation will greatly assist CAM practitioners in establishing evidence-based practice. It would be most unfortunate if the reported resistance to degree titles led to those wishing to practise acupuncture or herbal medicine receiving less hard science than they might have. To say that acupuncture and herbal medicine degrees have no academic justification appears arrogant in the extreme. Although it is certainly true that some content may not be scientific, this does not invalidate the legitimacy of these courses at degree level, a fact borne out by their successful validation in a number of universities. R. Michael Pittilo, Principal and vice-chancellor, The Robert Gordon University. |
This one got excellent responses from Kevin Smith (University of Abertay, Dundee), and from Peter J. Brophy (Professor of veterinary anatomy and cell biology University of Edinburgh). This was my comment to THE
There are a few very obvious responses to Professor Pittilo’s letter
For many alternative therapies the “philosophy” is simply incompatible with science. One obvious example is homeopathy. On Mondays and Wednesdays (science days) the students will be required to learn that response increases with dose. On Tuesdays and Thursdays will be taught the opposite. But for the exam they must reproduce only the latter (nonsensical) idea because their aim is to get a job as a homeopath. That makes nonsense of the idea of a university.
This seems to constitute a recognition that the evidence is still very inadequate. The time to start degrees, and the time to give official government recognition, is after the evidence is in, not before. What happens if you start degrees and then find that the subject is so much nonsense? Well, that has already happened in several areas of course. But the people who accredit the course and who act as external examiners just happen to be fervent believers in that nonsense, so all appears to be well (to bean counters anyway).
There is, as it happens, a great deal of evidence now about acupuncture, but the authors of the report do not seem to be aware of it. I recommend Barker Bausell’s book on the topic. If students are educated science, like what constitutes evidence, and our current understanding of words like “energy”, they would have to disavow the subject that there are supposed to training to practise
No, it is not a matter of arrogance, just a matter of careful attention to the evidence. Attention to evidence was notably absent in Prof Pittilo’s report, perhaps because his committee consisted entirely of people who earn their living from the subjects they were supposed to be assessing.
I have had the misfortune to have waded through a mound of such validation documents. The one thing they never consider is whether the treatment works. Sad to say, these validations are not worth the paper they are written on. |
The article below is an editorial that I was asked to write for the New Zealand Medical Journal, as a comment on article in today’s edition about the misuse of the title ‘doctor’ by chiropractors [download pdf]. Titles are not the only form of deception used by chiropractors, so the article looks at some of the others too. For a good collection of articles that reveal chiropractic for what it is, look at Chirobase
THE NEW ZEALAND
MEDICAL JOURNAL
Journal of the New Zealand Medical Association
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716

URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Doctor Who?
Inappropriate use of titles by some alternative “medicine” practitioners
David Colquhoun
Who should use the title ‘doctor’? The title is widely abused as shown by Gilbey1 in this issue of the NZMJ in an article entitled Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. Meanwhile, Evans and colleagues 2, also in this issue, discuss usage and attitudes to alternative treatments.
Gilbey finds that the abuse of the title doctor is widespread and that chiropractors are the main culprits. An amazing 82% of 146 chiropractics used the title Doctor, andL most of them used the title to imply falsely that they were registered medical practitioners.
Although it is illegal in New Zealand to do that, it seems clear that the law is not being enforced and it is widely flouted. This is perhaps not surprising given the history of chiropractic. It has had a strong element of ruthless salesmanship since it was started in Davenport, Iowa by D.D. Palmer (1845–1913). His son, B.J. Palmer, said that their chiropractic school was founded on “a business, not a professional basis. We manufacture chiropractors. We teach them the idea and then we show them how to sell” (Shapiro 2008)3 It is the same now. You can buy advice on how to build “build high-volume, subluxation-based, cash-driven, lifetime family wellness practices”
In her recent book3 , Rose Shapiro comments on the founder of chiropractic as follows.
“By the 1890s Palmer had established a magnetic healing practice in Davenport, Iowa, and was styling himself “doctor”. Not everyone was convinced, as a piece about him in an 1894 edition of the local paper, the Davenport Leader, shows.
A crank on magnetism has a crazy notion hat he can cure the sick and crippled with his magnetic hands. His victims are the weak-minded, ignorant and superstitious,those foolish people who have been sick for years and have become tired of the regular physician and want health by the short-cut method he has certainly profited by the ignorance of his victim. His increase in business shows what can be done in Davenport, even by a quack.”
D.D. Palmer was a curious mixture: grocer, spiritual healer, magnetic therapist, fairground huckster, religious cult leader—and above all, a salesman. He finally found a way to get rich by removing entirely imaginary “subluxations”.
Over 100 years later, it seems that the “weak-minded, ignorant, and superstitious” include the UK’s Department of Health, who have given chiropractics a similar status to the General Medical Council.
The intellectual standards of a 19th Century Mid-Western provincial newspaper journalist are rather better than the intellectual standards of the UK’s Department of Health, and of several university vice-chancellors in 2007.
Do the treatments work?
Neither Gilbey nor Evans et al. really grasp the nettle of judging efficacy. The first thing one wants to know about any treatment —alternative or otherwise — is whether it works. Until that is decided, all talk of qualifications, regulation, and so on is just vacuous bureaucratese. No policy can be framed sensibly until the question of efficacy has been addressed honestly.
It is one good effect of the upsurge of interest in alternative treatments that there are now quite a lot of good trials of the most popular forms of treatments (as well as many more bad trials). Some good summaries of the results are now available too. Cochrane reviews set the standard for good assessment of evidence. New Zealand’s Ministry of Health commissioned the Complementary and Alternative Medicine
website to assess the evidence, and that seems to have done a good job too. Their assessment of chiropractic treatment of low back pain is as follows:
There appears to be some evidence from one systematic review and four other studies, although not conclusive, that chiropractic treatment is as effective as other therapies but this may be due to chance. There is very little evidence that chiropractic is more effective than other therapies.
And two excellent summaries have been published as books this year. Both are by people who have had direct experience of alternative treatments, but who have no financial interest in the outcome of their assessment of evidence. The book by Singh and Ernst4 summarises the evidence on all the major alternative treatments, and the book by Bausell5 concentrates particularly on acupuncture, because the author was for 5 years involved in research in that area, Both of these books come to much the same conclusion about chiropractic. It is now really very well-established that chiropractic is (at best) no more effective than conventional treatment. But it has the disadvantage of being surrounded by gobbledygook about “subluxations” and, more importantly, it kills the occasional patient.
Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
The chiropractors of Alberta (Canada) and the Alberta Government are now facing a class-action lawsuit8. The lead plaintiff is Sandra Nette. Formerly she was a fit 41 year old. Now she is tetraplegic. Immediately
after neck manipulation by a chiropractor she had a massive stroke as a result of a torn vertebral artery.
Acupuncture comes out of the assessments equally badly. Bausell (2007) concludes that it is no more than a theatrical placebo.
Are the qualifications even real?
It is a curious aspect of the alternative medicine industry that they often are keen to reject conventional science, yet they long for academic respectability. One aspect of this is claiming academic titles on the flimsiest of grounds. You can still be held to have misled the public into thinking you are a medical
practitioner, even if you have a real doctorate. But often pays to look into where the qualifications come from.
A celebrated case in the UK concerned the ‘lifestyle nutritionist’, TV celebrity and multi-millionaire, Dr Gillian McKeith, PhD. A reader of Ben Goldacre’s excellent blog, badscience.net did a little investigation. The results appeared in Goldacre’s Bad Science column in the Guardian9.
She claimed that her PhD came from the American College of Nutrition, but it turned out to come from a correspondence course from a non-accredited US ‘college’. McKeith also boasted of having “professional membership” of the American Association of Nutritional Consultants, for which she provided proof of her degree and three professional references.
The value of this qualification can be judged by the fact that Goldacre sent an application and $60 and as a result “My dead cat Hettie is also a “certified professional member” of the AANC. I have the certificate hanging in my loo”.
Is the solution government regulation?
In New Zealand the law about misleading the public into believing you are a medical practitioner already exists. The immediate problem would be solved if that law were taken seriously, but it seems that it is not.
It is common in both the UK and in New Zealand to suggest that some sort of official government regulation is the answer. That solution is proposed in this issue of NZMJ by Evans et al2. A similar thing has been proposed recently in the UK by a committee headed by Michael Pittilo, vice-chancellor of Robert Gordon’s University, Aberdeen.
I have written about the latter under the heading A very bad report. The Pittilo report recommends both government regulation and more degrees in alternative medicine. Given that we now know that most alternative medicine doesn’t work, the idea of giving degrees in such subjects must be quite ludicrous to any thinking person.
The magazine Nature7 recently investigated the 16 UK universities who run such degrees. In the UK, first-year students at the University of Westminster are taught that “amethysts emit high yin energy” . Their vice chancellor, Professor Geoffrey Petts, describes himself a s a geomorphologist, but he cannot be tempted to express an opinion about the curative power of amethysts.
There has been a tendency to a form of grade inflation in universities—higher degrees for less work gets bums on seats. For most of us, getting a doctorate involves at least 3 years of hard experimental research in a university. But in the USA and Canada you can get a ‘doctor of chiropractic’ degree and most chiropractic (mis)education is not even in a university but in separate colleges.
Florida State University famously turned down a large donation to start a chiropractic school because they saw, quite rightly, that to do so would damage their intellectual reputation. This map, now widely distributed on the Internet, was produced by one of their chemistry professors, and it did the trick.

Other universities have been less principled. The New Zealand College of Chiropractic [whose President styles himself “Dr Brian Kelly”,though his only qualification is B. App Sci (chiro)] is accredited by the New Zealand Qualifications Authority (NZQA). Presumably they, like their UK equivalent (the QAA), are not allowed to take into account whether what is being taught is nonsense or not. Nonsense courses are accredited by experts in nonsense. That is why much accreditation is not worth the paper it’s written on.
Of course the public needs some protection from dangerous or fraudulent practices, but that can be done better (and more cheaply) by simply enforcing existing legislation on unfair trade practices, and on false advertising. Recent changes in the law on unfair trading in the UK have made it easier to take legal action against people who make health claims that cannot be justified by evidence, and that seems the best
way to regulate medical charlatans.
Conclusion
For most forms of alternative medicine—including chiropractic and acupuncture—the evidence is now in. There is now better reason than ever before to believe that they are mostly elaborate placebos and, at best, no better than conventional treatments. It is about time that universities and governments recognised the evidence and stopped talking about regulation and accreditation.
Indeed, “falsely claiming that a product is able to cure illnesses, dysfunction, or malformations” is illegal in Europe10.
Making unjustified health claims is a particularly cruel form of unfair trading practice. It calls for prosecutions, not accreditation.
Competing interests: None.
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716
URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Author information: David Colquhoun, Research Fellow, Dept of Pharmacology, University College London, United Kingdom (http://www.ucl.ac.uk/Pharmacology/dc.html)
Correspondence: Professor D Colquhoun, Dept of Pharmacology, University College London, Gower Street, London WC1E 6BT, United Kingdom. Fax: +44(0)20 76797298; email: d.colquhoun@ucl.ac.uk
References:
1. Gilbey A. Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. N Z Med J. 2008;121(1278). [pdf]
2. Evans A, Duncan B, McHugh P, et al. Inpatients’ use, understanding, and attitudes towards traditional, complementary and alternative therapies at a provincial New Zealand hospital. N Z Med J. 2008;121(1278).
3 Shapiro. Rose. Suckers. How Alternative Medicine Makes Fools of Us All Random House, London 2008. (reviewed here)
4. Singh S, Ernst E. Trick or Treatment. Bantam Press; 2008 (reviewed here)
5. Bausell RB. Snake Oil Science. The Truth about Complementary and Alternative Medicine. (reviewed here)
Oxford University Press; 2007
6. Colquhoun D. Science degrees without the Science, Nature 2007;446:373–4. See also here.
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10.
8. Libin K. Chiropractors called to court. Canadian National Post; June21, 2008.
9. Goldacre B. A menace to science. London: Guardian; February 12, 2007/
10. Department for Business Enterprise & Regulatory Reform (BERR). Consumer Protection from Unfair Trading Regulations 2008. UK: Office of Fair Trading.
| A report has appeared on Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine. The report is written by people all of whom have vested interests in spreading quackery. It shows an execrable ability to assess evidence, and it advocates degrees in antiscience It would fail any examination. Sorry, Prof Pittilo, but it’s gamma minus.[Download the report] |  |
Alice Miles put it well in The Times, today.
“This week came the publication of the “Report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK”. Otherwise known as twaddle.” . . .
“Regulate the practitioners – for safety, note, not for efficacy, as that is impossible to prove – and you give them official recognition. From recognition it is but a short hop to demand and then prescription: packet of Prozac, bit of yoga and a bag of dodgy herbs for you, sir.” . . .
“The Government responded on Monday – with a three-month consultation. So join in. Write to the Health Minister Ben Bradshaw at Richmond House, 79 Whitehall, SW1A 2NS. Write, on behalf of the NHS: “What I want for my 60th birthday is… the chance to provide medical, dental, and nursing care to all. And absolutely nothing else.”
Judging by Ben Bradshaw’s speech to the Prince’s Foundation, there may be a problem in conveying to him the evidence, but one can and must try.
Why is it that a health joutnalist can do so much better than a university head? Yes, the chair of the steering group is Professor R. Michael Pittilo BSc PhD CBiol FIBiol FIBMS FRSH FLS FRSA, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. Despite all those impressive-lookin initials after his name, I believe that this is a very bad report.
Here is something about Prof Pittilo from his university’s web site (the emphasis is mine).
Professor Michael Pittilo joined The Robert Gordon University, Aberdeen, as Principal and Vice-Chancellor on 5th September, 2005.
After postdoctoral research on arterial disease at the University of London, he was appointed to Kingston University where he became Head of Life Sciences. In 1995 he became Foundation Dean of the Faculty of Health and Social Care Sciences at Kingston University and St George’s Medical School (University of London). He was appointed Pro Vice Chancellor at the University of Hertfordshire in 2001.
Professor Pittilo has held a number of additional roles, including chairing Department of Health working groups, and as a trustee for the Prince of Wales’s Foundation for Integrated Health. “
Notice that Prof Pittilo is a Trustee of the Prince’s Foundation for Integrated Health, source of some of the least reliable information about alternative medicine to be found anywhere.
This steering group is, as so often, a nest of vested interests. It does not seem to have on it any regular medical or clinical scientist whatsoever. Why not? They just might produce some embarrassing facts perhaps? Like most government committees its members seem to have been chosen to produce the desired outcome.
For a start, the university run by Prof Pittilo, Robert Gordon’s University, is itself involved in a few antiscientific courses. Since his report recommends that degrees in quackery should become mandatory, I expect he’d welcome the chance to run more. Amazingly, Robert Gordon’s University runs an Introduction to Homeopathy, just about the daftest of all the common sorts of magic medicine.
Most of the the members of the steering group represent vested interests, though strangely this is not made clear in the list of members. An earlier report, in 2006, from the steering group was more open about this. Twelve of the members of the group represent Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Most of the rest are lay members or bureaucrats. With membership like that it is, I suppose, not surprising that the assessment of evidence is, to put it kindly, grossly distorted and woefully inadequate.
The report starts badly by failing to mention that the House of Lords report (2000), and the government’s response to it, set the following priorities. Both state clearly
“… we recommend that three important questions should be addressed in the following order . .
- (1) does the treatment offer therapeutic benefits greater than placebo?
- (2) is the treatment safe?
- (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?
The word ‘placebo’ does not occur a single time in the main report (and only twice in the text of the seven appendices). But they do say (page 11):
“We recommend that public funding from the NHS should be used to fund CAM therapies where there is evidence of efficacy, safety and quality assurance.”
The evidence
The problem is that the assessment of the evidence for efficacy in the report is pathetically poor. The report, sad to say, consists essentially of 161 pages of special pleading by the alternative medicine industry, served up with the usual large dose of HR gobbledygook.
There is really no excuse for this utterly incompetent assessment. There have been plenty of books this year alone that make excellent summaries of the evidence, mostly written for the lay public. They should, therefore, be understandable by any university vice-chancellor (president). The one benefit of the upsurge in public interest in magic medicine is that there are now quite a lot of good clinical trials, and when the trials are done properly, they mostly confirm what we thought before: in most cases the effects are no more than placebo.
Here is one example. Annexe1 concerns “Developing Research and Providing an Evidence Base for Acupuncture and Herbal/Traditional Medicine Treatment”. The wording of the title itself suggests, rightly, that this evidence base does not exist, in which case why on earth are we talking about them as “professions”? The discussion of the evidence in Annexe 1 is nothing if not partial. But what do you expect if you ask herbalists to assess herbal medicine? An honest assessment would put them out of business. The eternal mantra of the alternative industry appears as usual, “Absence of evidence is, of course, not evidence of absence”. True of course, but utterly irrelevant. Annexe 1 says
“Acupuncture is a complex intervention and lack of a suitable placebo control has hindered efforts to evaluate efficacy”
This is simply untrue, In recent years enormous efforts have been put into devising controls for assessment of acupuncture, but they are entirely ignored here. One thing that has been established quite clearly is that it makes no difference where you put the needles, so all the talk of Qi and meridians is obvious mumbo-jumbo.
Have the authors of Annexe 1, and Professor Pittilo, not read the relevant studies? Two books this year have dealt with the question of evidence with great care. They are both by people who have been involved personally with acupuncture research, Prof Edzard Ernst and Dr Barker Bausell. Edzard Ernst is the UK’s first Professor of Complementary Medicine. Barker Bausell was research director of an NIH-funded Complementary and Alternative Medicine Specialized Research Center at the University of Maryland.
 |
 |
Singh and Ernst discuss thoroughly the question of controls and assess all the evidence carefully. Their conclusions include the following.
- The traditional principles of acupuncture are deeply flawed, as there is no evidence at all to demonstrate the existence of Ch’i [Qi] or meridians.
- By focussing on the increasing number of high-quality research papers, reliable conclusions from systematic reviews make it clear that acupuncture does not work for a whole range of conditions, except as a placebo.
- In short, the evidence is neither consistent nor convincing. It is borderline.
Barker Bausell was himself involved in designing and analysing trialsof acupuncture. His conclusions are even less positive.
“There is no compelling, credible scientific evidence to suggest that any CAM therapy benefits any medical condition or reduces any medical symptom (pain or otherwise) better than a placebo”.
These are serious authors with direct experience in CAM research, which is more than can be said of anyone on the steering group. Why are their conclusions ignored entirely? That is sheer incompetence.
Degrees in anti-science
One conclusion of the report is that
“The threshold entry route to the register will normally be through a Bachelor degree with Honours”
This is utter nonsense. It is quite obvious surely that you can’t award honours degrees until after you have the evidence. You can read on page 55 of the report
“3a: Registrant acupuncturists must:
understand the following aspects and concepts for traditional East-Asian acupuncture:
– yin/yang, /5 elements/phases, eight principles, cyclical rhythms, qi ,blood and body fluids, different levels of qi, pathogenic factors, 12 zang fu and 6 extraordinary fu, jing luo/ meridians, the major acupuncture points, East-Asian medicine disease categorisation, the three burners, the 4 stages/levels and 6 divisions
– causes of disharmony/disease causation
– the four traditional diagnostic methods: questioning, palpation, listening and observing”
This is utter baloney. Anyone who advocates giving honours degrees in such nonsense deserves to be fired for bringing his university into disrepute (and, in the process, bringing all universities and science itself into disrepute).
That includes also degrees that teach that “amethysts emit high yin energy“.
So what should be done?
If making peole do degrees in mumbo-jumbo is not the answer, what is? Clearly it would be far too draconian to try to ban quackery (and it would only increase its popularity anyway).
The answer seems to me to be quite simple. All that needs to done is to enforce existing laws. It is already illegal to sell contaminated and poisonous goods to the public. It is already illegal to make fraudulent advertisemants and to sell goods that are not as described on the label.
The only problem is that the agencies that enforce these rules are toothless and that there are a lot of loopholes and exceptions that work in favour of quackery. I have tried myself to complain about mislabelling of homeopathic pills to the Office of Fair Trading on the grounds that are labelled Arnica 30C but contain no Arnica. They solemnly bought a bottle and sent it to an analyst and of course they found no arnica, But nothing happened, because an exception to the usual law applies to homeopathic pills.
The Advertising Standards Authority is good as far as it goes. They quickly told Boots Pharmacies to withdraw advertisements that claimed CoQ10 “increased vitality”. But they can exact no penalties and they can’t deal with lies that are told to you orally, or with anything at all on the web.
The Health Professions Council (HPC) says that one of the criteria for registering new professions is aspirant groups must “Practise based on evidence of efficacy”. If that were actually applied, none of this process would occur anyway. No doubt the HPC will fail to apply its own criteria. On past form, it can be expected to adopt a “fluid concept of evidence“.,
One more thing, New European legislation was described recently in the BMJ
“Consumers in the United Kingdom are to receive stronger legal safeguards against products that claim, without any identifiable scientific evidence, to provide physical and mental health benefits such as tackling obesity or depression.”
“The scope of the legislation is deliberately wide and is the biggest shake up in consumer law for decades. It targets any unfair selling to consumers by any business.”
Politicians seem to be immune to rational argument when it comes to quackery. But a few legal actions under these laws could bring the house of cards tumbling so fast that this gamma-minus report would become rapidly irrelevant. There will be no shortage of people to bring the actions. I can’t wait.
Follow up
Dominic Lawson, 24 June 2008. An excellent column appeared today in the Independent. Dominic Lawson writes about the Pittilo report: “So now we will have degrees in quackery. What, really, is the difference between acupuncture and psychic surgery?“. The reference to that well known conjuring trick, “psychic surgery” as a “profession”, revealed here, causes Lawson to say
“It makes it clear that the lunatics have taken over the asylum. For a start, how could Philip Hunt, previously director of the National Association of Health Authorities and Trusts, possibly have thought that “psychic healing” constituted a “profession” – let alone one which would “develop its own system of voluntary self-regulation?”
“One can see how this might fit in with the Government’s “never mind the quality, feel the width” approach to university education. One can also see how established practitioners of such therapies might see this as a future source of income – how pleasant it might be to become Visiting Professor of Vibrational Medicine at the University of Westminster.
Thus garlanded with the laurels of academic pseudo-science, the newly professionalised practitioners of “alternative medicine” can look down on such riff-raff as the “psychic surgeons”
Once again I have to ask, how is it that we have to rely on journalists to prevent vice-chancellors eroding academic standards; indeed eroding simple common sense? I guess it is just another sign of the delusional thinking engendered by the culture of managerialism that grips universities.
