Richard Eastell
This is a web version of a review of Peter Gotzsche’s book. It appeared in the April 2014 Healthwatch Newsletter. Read the whole newsletter. It has lots of good stuff. Their newsletters are here. Healthwatch has been exposing quackery since 1989. Their very first newsletter is still relevant.
|
Most new drugs and vaccines are developed by the pharmaceutical industry. The industry has produced huge benefits for mankind. But since the Thatcherite era it has come to be dominated by marketing people who appear to lack any conscience. That’s what gave rise to the Alltrials movement. It was founded in January 2013 with the aim of ensuring that all past and present clinical trials are registered before they start and that and their results are published The industry has been dragged, kicking and screaming, towards a new era of transparency, with two of the worst offenders, GSK and Roche, now promising to release all data. Let’s hope this is the beginning of real open science. |
|
This version is not quite identical with the published version in which several changes were enforced by Healthwatch’s legal adviser. They weren’t very big changes, but here is the original.
Deadly Medicines and Organised Crime
By Peter Gøtzsche, reviewed by David Colquhoun
Published by Radcliffe Publishing Ltd on 1 August 2013. RRP £24.99 (320 pages, paperback)
ISBN-10: 1846198844 ISBN-13: 978-1846198847
As someone who has spent a lifetime teaching pharmacology, this book is a bitter pill to swallow. It makes Goldacre’s Bad Pharma seem quite mild.
In fairness, the bits of pharmacology that I’ve taught concern mostly drugs that do work quite well. Things like neuromuscular blocking agents, local anaesthetics, general anaesthetics, anticoagulants, cardiac glycosides and thyroid drugs all do pretty much what is says on the label.
Peter Gøtzsche is nothing if not evidence man. He directs the Nordic Cochrane group, and he talks straight. His book is about drugs that don’t work as advertised. There is no doubt whatsoever that the pharmaceutical industry has behaved very badly indeed in the last couple of decades. You don’t have to take my word for it, nor Peter Gotzche’s, nor Ben Goldacre’s. They have told us about it themselves. Not voluntarily of course, but in internal emails that have been revealed during court proceedings, and from whistleblowers.
Peter Rost was vice president marketing for the huge pharmaceutical company, Pfizer, until he was fired after the company failed to listen to his complaints about illegal marketing of human growth hormone as an anti-ageing drug. After this he said:
“It is scary how many similarities there are between this industry and the mob. The mob makes obscene amounts of money, as does this industry. The side effects of organized crime are killings and deaths, and the side effects are the same in this industry. The mob bribes politicians and others, and so does the drug industry … “
The pharmaceutical industry is the biggest defrauder of the US federal government under the False Claims Act. Roche led a cartel that, according to the US Justice Department’s antitrust division, was the most pervasive and harmful criminal antitrust conspiracy ever uncovered. Multibillion dollar fines have been levied on all of the big companies (almost all in the USA, other countries have been supine), though the company’s profits are so huge they are regarded as marketing expenses.
It’s estimated that adverse effects of drugs kill more people than anything but cancer and heart disease, roughly half as many as cigarettes. This horrifying statistic is announced at the beginning of the book, though you have to wait until Chapter 21 to find the data. I’d have liked to see a more critical discussion of the problems of causality in deciding why someone died, which are just as big as those in deciding why somebody recovered. Nevertheless, nobody seems to deny that the numbers who are killed by their treatments are alarmingly high.
Gøtzsche’s book deals with a wide range of drugs that don’t do what it says on the label, but which have made fortunes because of corruption of the scientific process. These include non-steroidal anti-inflammatory drugs (NSAIDs), an area described as “a horror story filled with extravagant claims, bending of the rules, regulatory inaction, . . .”. Other areas where there has been major misbehaviour include diabetes (Avandia), and the great Tamiflu scandal. and the great Tamiflu scandal. It took five years of pressure before Roche released the hidden data about Tamiflu trials. It barely works. Goldacre commented “government’s Tamiflu stockpile wouldn’t have done us much good in the event of a flu epidemic”
But the worst single area is psychiatry.
Two of the chapters in the book deal with psychiatry. Nobody has the slightest idea how the brain works (don’t believe the neuroscience hype) or what causes depression or psychosis. Treatments are no more than guesses and none of them seems to work very well.
The problems with the SSRI antidepressant, paroxetine (Seroxat in UK, Paxil in USA) were brought to public attention, not by a regulator, but by a BBC Panorama television programme. The programme revealed that a PR company, which worked for GSK, had written
"Originally we had planned to do extensive media relations surrounding this study until we actually viewed the results. Essentially the study did not really show it was effective in treating adolescent depression, which is not something we want to publicise."
This referred to the now-notorious study 329. It was intended to show that paroxetine should be recommended for adolescent depression. The paper that eventually appeared in 2001 grossly misrepresented the results. The conclusions stated “Paroxetine is generally well tolerated and effective for major depression in adolescents”, despite the fact that GSK already knew this wasn’t true. The first author of this paper was Martin Keller, chair of psychiatry at Brown University, RI, with 21 others.
But the paper wasn’t written by them, but by ghost authors working for GSK. Keller admitted that he hadn’t checked the results properly.
That’s not all. Gøtzsche comments thus.
“Keller is some character. He double- billed his travel expenses, which were reimbursed both by his university and the drug sponsor. Further, the Massachusetts Department of Mental Health had paid Brown’s psychiatry department, which Keller chaired, hundreds of thousands of dollars to fund research that wasn’t being conducted. Keller himself received hundreds of thousands of dollars from drug companies every year that he didn’t disclose.”
His department received $50 million in research funding. Brown University has never admitted that there was a problem. It still boasts about this infamous paper
The extent of corruption at Brown University rivals the mob.
The infamous case of Richard Eastell at Sheffield university is no better. He admitted in print to lying about who’d seen the data. The university did nothing but fire the whistleblower.
Another trial, study 377, also showed that paroxetine didn’t work. GSK suppressed it.
“There are no plans to publish data from Study 377” (Seroxat/Paxil Adolescent Depression. Position piece on the phase III clinical studies. GlaxoSmithKline document. 1998 Oct.)
Where were the regulatory agencies during all this? The MHRA did ban use of paroxetine in adolescents in 2003, but their full investigation didn’t report until 2008. It came to much the same conclusions as the TV programme six years earlier about the deceit. But despite that, no prosecution was brought. GSK got away with a deferential rap on the knuckles.
Fiona Godlee (editor of the BMJ, which had turned down the paper) commented
“We shouldn’t have to rely on investigative journalists to ask the difficult questions”
Now we can add bloggers to that list of people who ask difficult questions. The scam operated by the University of Wales, in ‘validating’ external degrees was revealed by my blog and by BBC TV Wales. The Quality Assurance Agency came in only at the last moment. Regulators regularly fail to regulate.
|
Despite all this, the current MHRA learning module on SSRIs contains little hint that SSRIs simply don’t work for mild or moderate depression. Neither does the current NICE guidance. Some psychiatrists still think they do work, despite there being so many negative trials. |
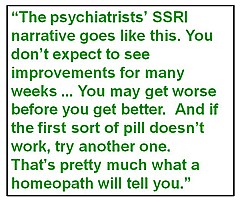 |
The psychiatrists’ narrative goes like this. You don’t expect to see improvements for many weeks (despite the fact that serotonin uptake is stopped immediately). You may get worse before you get better. And if the first sort of pill doesn’t work, try another one. That’s pretty much identical with what a homeopath will tell you. The odds are that its meaning is, wait a while and you’ll get better eventually, regardless of treatment.
It’s common to be told that they must work because when you stop taking them, you get worse. But, perhaps more likely, when you stop taking them you get withdrawal symptoms, because the treatment itself caused a chemical imbalance. Gøtzsche makes a strong case that most psychiatric drugs do more harm than good, if taken for any length of time. Marcia Angell makes a similar case in The Illusions of Psychiatry.
Gøtzsche will inevitably be accused of exaggerating. Chapter 14 ends thus.
“Merck stated only 6 months before it withdrew Vioxx that ‘MSD is fully committed to the highest standards of scientific integrity, ethics, and protection of patient’s wellbeing in our research. We have a tradition of partnership with leaders in the academic research community. Great. Let’s have some more of such ethical partnerships. They often kill our patients while everyone else prospers.
Perhaps Hells Angels should consider something similar in their PR: We are fully committed to the highest standards of integrity, ethics and protection of citizens’ well- being when we push narcotic drugs. We have a tradition of partnership with leaders in the police force”.
But the evidence is there. The book has over 900 references. Much of the wrongdoing has been laid bare by legal actions. I grieve for the state of my subject.
The wrongdoing by pharma is a disgrace.
The corruption of universities and academics is even worse, because they are meant to be our defence against commercial corruption.
All one can do is to take consolation from the fact that academics, like Gøtzsche and Goldacre, and a host of bloggers, are the people who are revealing what’s wrong. As a writer for the business magazine, Fortune, said
“For better or worse, the drug industry is going to have to get used to Dr. Peter Rost – and others like him.”
At a recent meeting I said that it was tragic that medicine, the caring profession, was also the most corrupt (though I’m happy to admit that other jobs might be as bad if offered as much money).
At present there is little transparency. There is no way that I can tell whether my doctor is taking money from pharma, data are still hidden from public scrutiny by regulatory agencies (which are stuffed with people who take pharma money) as well as by companies. Governments regard business as more important than patients. In the UK, the Government continued promotion of the fake bomb detector for many years after they’d been told it was fake. Their attitude to fake medicines is not much different. Business is business, right?
One side effect of the horrific corruption is that it’s used as a stick by the alternative medicine industry. That’s silly of them, because their business is more or less 100% mendacious marketing of ineffective treatments. At least half of pharma products really do work.
Fines are useless. Nothing will change until a few CEOs, a few professors and a few vice-chancellors spend time in jail for corruption.
Read this book. Get angry. Do something.
Follow-up
The bulletin of the British Pharmacological Society, Pharmacology Matters, declined to publish the following article. Sadly the Society seems to be more interested in "reputation management" than in truth. Luckily, it is not easy to suppress criticism these days. A version of the article has appeared in Research Fortnight where it will be seen by far more people than it would have been in Pharmacology Matters. This is the original version that I submitted to them. They would not allow me to quote Lewis’s comment (apropos of the sale of homeopathic meningitis vaccine)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
If a child were to die of whooping cough or meningitis as a result of buying the fraudulent "vaccines", that would be true. It’s a sad reflection on the state of defamation law that journals are not willing to say so. Blogs are fast becoming the best source of reliable information.

|

|
Stop press. The BPS has now signed up to Alltrials (too late for the printed version)
Pharmacology society does little to defend its subject
David Colquhoun
Over the past few years a courageous group of writers, researchers and activists has worked to expose the truth about the medicines we are sold, be they conventional or alternative.
Thanks, above all, to Ben Goldacre (1), more people than ever know that the big pharma companies have been concealing evidence of the harm that their products do, or the good they fail to do. Thanks to a small army of bloggers the preposterous claims made by peddlers of homeopathic remedies and other quackery are less likely to go unchallenged.
And yet, the organization charged with safeguarding the good name of pharmacology in this country, the British Pharmacological Society (BPS), has remained silent throughout.
The pharmaceutical industry
The BPS, rather than helping, became actively complicit when, along with much of the medical establishment, it signed an agreement with the ABPI (2). This document, developed under the aegis of the Ethical Standards in Health & Life Sciences Group (ESHLSG), contained two objectionable clauses:
“Industry plays a valid and important role in the provision of medical education”
And
“Medical representatives can be a useful resource for healthcare professionals”
Given that clinical “education” has long been part of Pharma’s marketing strategy, this seems disgraceful. And most of the doctors I know and respect refuse to see reps altogether. It is hopelessly optimistic to think that can an industry person can teach clinical pharmacology without bias in favour of his own company’s products. The BPS has many members who teach pharmacology. Can they really cope so badly that we need to have industry to educate clinicians?
It’s fine, and sometimes desirable, for academics and industry to work together on drug development. But only as long as the industry partner has no say in how, or whether, the results are published. Without that proviso we can expect more corruption of the sort that’s been seen at the University of Sheffield (3).
This is very sad, because I have great reason to like the drug industry. I’ve benefitted from several of their products myself. But the industry is in trouble. Many of its products provide only marginal benefits. Furthermore, some of the things that seemed to be useful, like SSRI antidepressants, have turned out to be next to useless once hidden trials were revealed (4). The MHRA’s learning module on SSRIs doesn’t seem to have caught up with this yet.
Sadly, the reaction of industry has been to resort to dishonesty, to hide unfavourable data and to increase yet more what it spends on marketing. Between 2009 and 2012, fines of at least 10 billion dollars (5) have been imposed on some of the most eminent companies. They include Lilly, Pfizer, AstraZeneca, Merck, Abbott and GlaxoSmithKline (GSK). The biggest fine of all ($3 bn, in July 2012) went to a British company, GSK. This succession of large fines seems to be regarded by the companies as mere marketing expenses.
All these fines were levied in the USA. Where, one might ask, are the regulators in the UK? Why have there been no fines here? Why, indeed, are some of the senior managers of these companies not in jail? Why has the BPS remained silent about the prostitution of its subject? And why have the MHRA done so little to stop it?
I suggest that you support the petition for release of the results of all trials (6). It’s been supported by many individuals and a lot of organisations, including the BMJ and the Royal Statistical Society. But, disgracefully, not by the BPS.
Quackery
At least in the case of the pharmaceutical industry some of its products work. But pharmacologists should also be concerned about the quackery industry, worth about 60 billion dollars per year (as opposed to $600 bn for the pharmaceutical industry). Virtually none of their products work (7). Why has the BPS said so little about it? It has, along with most of the medical and university establishment, shrugged its shoulders about the fact that students at Westminster University have been shown dowsing with a pendulum as a method for selection of herbal “remedies”, as part of a Bachelor or “Science” degree. It is an area in which every regulatory agency has failed to ensure even minimal levels of honesty (8). And the BPS has just shrugged.
The MHRA has been worse than useless in this area: it has been actively unhelpful (9). The senior staff of the MHRA are members of the BPS which has, as usual, said next to nothing. The MHRA’s herbal medicine committee has allowed misleading labels that give indications to be put on herbal potions, and these labels fail to make it clear that no evidence whatsoever of efficacy is required to get the MHRA kitemark. The wording was suggested (not required) by European law, but that law does not prevent the MHRA from saying, as it should, “there is no reason to think that this product is effective for any of the indications on the label” (10). Arguably, the MHRA is in breach of Consumer Protection law (11, 12).
At the time, the BPS did make some objection to the labelling (13), but only under great pressure from me (indeed I wrote it) . That has not been followed up, and I can no longer find it on the BPS web site. Indeed Philip Routledge, one of the people who is responsible for the misinformation in his capacity as chair of the MHRA Herbal Medicines Advisory Committee, is, at present the president of the BPS.
The MHRA has also been responsible for misleading labelling of the products of the most obviously fraudulent products of the lot: homeopathic pills, the medicines that contain no medicine. Most of the pills (anything beyond 12x dilution) contain not a single molecule of the substance on the label. Yet they have been given a get-out clause that enables them to evade prosecution by Trading Standards (an organisation that consistently fails to apply consumer protection laws. Rose et al (2011) (12) concluded
"EU directive 200s5/29/EC is largely ineffective in preventing misleading health claims for consumer products in the UK".
It is simply bizarre that the people at the MHRA, many of who are BPS members, have sat round a table and approved the following label. This example is for Arnica 30C pills, which, of course, contain no trace of arnica (14, 8). The outcome of their deliberations is simply surreal (see the actual labels here).
"Used within the homeopathic tradition for the symptomatic relief of sprains, muscular ache; and bruising or swelling after contusions."
This will deceive the naïve into thinking that it will have some effect on sprains etc. It won’t. And the MHRA have declined to test how the label is perceived by the public, though it took some effort to get them to admit it.
"If you are allergic to any of the ingredients in this medicine, consult your doctor before taking this medicine."
The ingredients aren’t stated apart from “contains lactose and sucrose”. That’s all they contain. No arnica.
"If pregnant or breastfeeding consult your doctor before use."
Why should a few mg of lactose and sucrose have the slightest effect on a pregnant or breast-feeding mother. This is pure make-believe
"If you forget to take this product, continue to take your usual dose at the usual time, it does not matter if you have missed a dose. Do not take a double dose to make up for a missed dose."
This statement is even more bizarre. There is nothing in the pills.
"If you take too much of this product (overdose) speak to a doctor or pharmacist and take this label with you."
And this is the ultimate in nonsense. The 1023 campaign regularly swallows whole bottles, and of course nothing happens. You can’t overdose on nothing. The fact that the MHRA can insist on this label, with a straight face, is the ultimate betrayal of science and reason.
"When asked to comment, as part of the consultation on these rules, this was the response from the BPS."
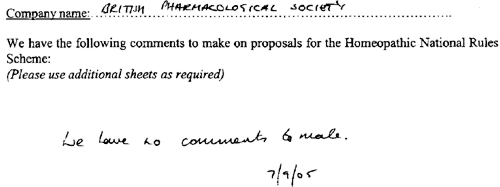
This is extracted from page 16 of the “selected response” provided by the MHRA under a Freedom of Information Act request [download all]
Things have changed little since A.J. Clark wrote his book on Patent Medicines in 1938 (15). And the BPS has done next to nothing to help. Neither has the MHRA. In fact both have colluded in the failures of both honesty and reason.
A BBC South West program recently revealed that a pharmacist was selling “homeopathic vaccines” for whooping cough and meningitis (16). The MHRA have know about his homicidal practice for years, but have done nothing. The General Pharmaceutical Council let him off with a rap on the knuckles. It has been left to bloggers and TV reporters to focus attention on these scoundrels. The well-respected blogger, Andy Lewis, wrote (17)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
And the full clinical data for Tamiflu are still being concealed by Roche (18).
I think that is rather shameful.
I have been a member of the BPS for all my working life. I was happy when they made me an honorary fellow. But I now find myself asking if I can remain a member of an organisation that has done so little to defend honest scientific behaviour.
References
(1) Ben Goldacre’s Bad Pharma. Buy it now. Then do something. https://www.dcscience.net/?p=5538
(2) ABPI 2012 Guidance on collaboration between healthcare professionals and the pharmaceutical industry. http://www.abpi.org.uk/our-work/library/guidelines/Pages/collaboration-guidance.aspx
(3) Colquhoun, D. (2007) The Corporate Corruption of Higher Education: part 2 https://www.dcscience.net/?p=193
(4) Kirsch,I., B.J.Deacon, T.B.Huedo-Medina, A.Scoboria, T.J.Moore, and B.T.Johnson. 2008. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS. Med. 5:e45. http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0050045
(5) Groeger, L. (2012) Big Pharma’s Big Fines http://www.propublica.org/special/big-pharmas-big-fines
(6) All trials registered. All results reported, http://www.alltrials.net/supporters/
(7) Singh,S. and E.Ernst. 2009. Trick or Treatment. Corgi. http://en.wikipedia.org/wiki/Trick_or_Treatment
(8) Colquhoun, D. (2012) Regulation of alternative medicine: why it doesn’t work, and never can. https://www.dcscience.net/?p=5562
(9) Colquhoun, D, (2006) The MHRA breaks its founding principle: it is an intellectual disgrace. https://www.dcscience.net/?p=32
(10) Colquhoun, D. (2011). Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. https://www.dcscience.net/?p=4269
(11) Colquhoun, D. (2009) Most alternative medicine is illegal. https://www.dcscience.net/?p=30
(12) Rose,L.B., P.Posadzki, and E.Ernst. 2012. Spurious claims for health-care products: an experimental approach to evaluating current UK legislation and its implementation. Med. Leg. J. 80:13-18. https://www.dcscience.net/Rose-medico-legal-2012.pdf
(13) Colquhoun, D. (2006) Learned Societies speak out against CAM, and the MHRA. https://www.dcscience.net/?p=30
(14) MHRA Arnicare Arnica 30c pillules NR 01175/0181 http://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con049307.pdf
(15) Colquhoun, D. (2008) Patent medicines in 1938 and now: A.J.Clark’s book. https://www.dcscience.net/?p=257
(16) BBC South West on the evils of homeopathic "vaccines" http://www.youtube.com/watch?v=TZf9mUzI4RI
(17) Why Does the MHRA Not Close Down these Homeopaths? The regulators have known of serious problems for years, Nothing is done. http://www.quackometer.net/blog/2013/01/why-does-the-mhra-not-close-down-these-homeopaths.html
(18) Payne, D. (2012). Tamiflu: the battle for secret drug data http://www.bmj.com/content/345/bmj.e7303
Follow-up
25 February 2013 This post has some follow-up even before it appeared on Research Research. I noticed on the BPS web site a press release “BPS announces intention to sign All Trials Petition“. It was dated 20th February, but I didn’t notice it until after the printed edition went to press. It was expressed as a future intention to sign, though in fact they signed almost straight away (though over 100 organisations had already done so). That’s good. I suspect that when my old friend, Humphrey Rang, who is president elect of the BPS, takes charge, the Society may start to take its responsibilities to the public more seriously than it has in the past.
|
The MHRA, on the other hand, is still evading its self-declared job of ensuring the public that drugs work. |

|
13 March 2013. A reply to this piece appeared in red on Research Research, The British Pharmacological Society champions its science. It was written by Humphrey Rang who, as president elect of the BPS naturally felt obliged to defend its record. He defends the BPS membership of ESHLSG, but fails to mention that first the Lancet and then the BMA withdrew their support. Nor does he mention that medical students and doctors launched a campaign, BadGuidelines.org, against the agreement. The Medical Schools Council, which also signed the agreement, said "the scrutiny of the guidance has ‘identified deficiencies in the current statement". Didn’t they read it before signing? Rang says that the BPS is also working to improve the joint statement with the ABPI. That’s good, but one must wonder why the BPS signed up to the original form.
On the points about quackery, Rang sites the BPS statement on homeopathy (now vanished) but fails to mention that that statement was written by me in an attempt to wake the BPS from it’s slumbers on the matter of medicines that don’t work. But he doesn’t mention at all the matter of mislabelling of both homeopathic and herbal preparations.
Of course, the BPS does many good things. But like most organisations, it is too reluctant to speak out when it sees wrongdoing, and too reluctant to say "sorry we made a cock-up that time".
|
Synexus is "The world’s largest multi-national company entirely focused on the recruitment and running of clinical trials company that runs clinical trials and screening programmes". |

|
I should say at the outset that I’m deeply impressed by our local GP practice. I can’t imagine a better GP than mine; he has the ideal mix of knowledge and empathy. I do, however, worry about the fragmentisation of the NHS and its creeping privatisation.
I came across Synexus because my wife had a letter (on our GP practice letterhead) inviting her to go for osteoporosis screening, and possibly to "take part in a study". Download the letter.
Notice that the form gives no idea of what the "study" might be. Notice also, more seriously, the small print on the second page of the form. Here it is in normal size print.
"If you contact Synexus and/or return the attached tear-off slip Synexus may, with your consent, use the data you provide for the purposes of informing you of the study, of medical products and processes that might be of interest to you. Your information will be held by, and access to it limited to, Synexus Ltd and/or companies within the Synexus group of companies and/or third parties acting on their behalf"
You are invited, in near-illegible small print, to allow all your medical data to be handed over to Synexus [see comment, below], and an unspecified number of other companies and third parties. It also gives the company permission to "use the data you provide for the purposes of informing you. . . of medical products and processes that might be of interest to you". This appears to mean that in the future you’ll be pestered with mailings that bypass your GP and advertise (private?) screening etc. For the purposes of screening there should be no need to hand over any data whatsoever (and the practice manager ensures me that they don’t).
My wife asked my advice about whether she should sign up for "the study" if invited to do so, so I asked the GP practice what the trial was about. Rather to my surprise, they didn’t know. Neither did Hertfordshire NHS. So I asked the National Osteoporosis Society, and they didn’t know either. After several emails and a phone call, I eventually got the details from Synexus.
I have two concerns about this. One is the argument that’s been raging about the value of indiscrimate screening, The case against it has been put perfectly in Margaret McCartney’s recent book, The Patient Paradox. There’s a good case that too much money is spent on people who are well, and not enough on those who are ill. Of course prevention is better than cure. The problem is that in many cases the screening tests aren’t accurate enough, so many people get diagnosed and treated when they are not actually ill.
On top of that, there is now a serious worry about screening tests promoted by private companies, for profit. Lifeline has been criticised, for good reasons. The men’s health charity, Movember, promotes PSA screening for prostate cancer, one of the most unreliable tests in existence. There is now a web site that collates evidence about private health screening. Many of the tests are available on the NHS, and the NHS advice about them is being re-written so that it gives information about risks as well as benefits.
The NHS advice on screening for osteoporosis is still ambiguous. The evidence for benefit of screening at age 60 is not clear.
The main question, though, is this. If my wife were offered an opportunity to "take part in a study", should she say yes, or no? My first inclination was to say yes. Clinical trials are the only way to find out whether treatments work or not. If people don’t volunteer for trials, we’ll never know. But before saying yes, one would want to know that the trial was organised properly, so that it could answer a relevant question. That’s why I was surprised when I found it so hard to discover the details. Nobody seemed to know even where the trial was registered. It’s no use searching trial registers for "Synexus": you need to know who is paying for it.
Eventually Dr John Robinson of Synexus turned out to be very helpful. The protocol number is 20070337 with a EudraCT number 2011-001456-11. The trial is registered at ClinicalTrails.gov and it has ethical approval. It’s a trial of a new osteoporosis treatment made by Amgen, AMG 785. It’s a monoclonal antibody against sclerostin, a protein that inhibits bone formation. It sounds like a good idea, but we won’t know how well it works until it’s been tested. The allocation of patients to AMG 785 or placebo is randomised and double blind. The patient Information sheet for participants looks pretty good to me.
Nevertheless, I have some reservations about the trial. First, its organisation is odd. “After taking AMG 785 or placebo for one year, all study participants will be taking denosumab for the following year”. Denusomab is another product of the same company, Amgen. It has already been approved by NICE. When I asked Dr Robinson why this arrangement had been chosen, this is what he said.
"Previous studies have shown that the maximal benefit on bone density is seen after 12 months and that treatment after this period shows a lower increase, it is for this reason treatment with AMG 785 is for 12 months in this study.
Other studies have also shown benefit in further improving and maintaining the increase in bone density and reducing fracture risk by subsequently treating patients with Alendronate after 12 months of AMG 785. This study is investigating whether similar or better findings occur with denosumab."
This does not make any sense to me. If the object is to compare AMG 785 with denusomab, they should be compared side by side, not sequentially. That brings us straight to the main problem with the trial design. It asks the wrong question. What the doctor needs to know is whether AMG 785 is more effective than existing treatments, not whether it is better than placebo. When I asked Dr Robinson about this, he said
"To quote from the protocol: A placebo-controlled study was chosen because it permits a minimally confounded demonstration of efficacy and safety of AMG 785 in the treatment of PMO. Using an active control such as a bisphosphonate means that more patients have to be enrolled to show benefit from AMG 785. The study already plans to enrol 6000 women. Increasing this number would add to the time required to complete the study. In addition the use of a placebo control is also within regulatory guidelines. "
What this means, in plain English, is that they are expecting a rather small difference between AMG 785 and existing treatments. It would take a very large number of patients to show this difference. If the difference is indeed small, it would be hard to justify the (doubtless eye-watering) cost of AMG 795 (denusomab costs £185.00 per dose). Testing a new drug against placebo, or against a low dose of something not very effective, is one of the stratagems listed in Chapter 4, Bad trials, in Ben Goldacre’s Bad Pharma. It makes the new drug look good, but it asks the wrong question.
The National Osteoporosis Society should be an organisation to which patients could turn to for advice in cases like this. In this case they were not helpful. They didn’t know much about the trial. I hope that this is not related to the fact that they get a lot of funding from Synexus. I noticed too that one of their advisors is the infamous Professor Richard Eastell, who admitted in print to lying in a paper, about a drug for osteoporosis made by Proctor & Gamble. It’s getting quite hard to find a medical charity that isn’t in the pocket of Big Pharma. or quacks (or even occasionally, both).
Conclusion. The trial asks the wrong question. On those grounds alone, I think that my advice would be not to volunteer for the trial.
Follow-up
I should have mentioned an interesting and relevant Cochrane review, New treatments compared to established treatments in randomized trials (2012), The authors’ conclusions are as follows.
“Society can expect that slightly more than half of new experimental treatments will prove to be better than established treatments when tested in RCTs, but few will be substantially better. This is an important finding for patients (as they contemplate participation in RCTs), researchers (as they plan design of the new trials), and funders (as they assess the ’return on investment’).”
15 May 2013. As noted in the comments, Synexus has been censured by the Advertising Standards Authority, because the ASA judged that they did not give sufficient prominence to the fact that there advertising of free screening was actually a way to recruit people into clinical trials.
|
This is a very important book. Buy it now (that link is to Waterstone’s Amazon don’t pay tax in the UK, so don’t use them). When you’ve read it, do something about it. The book has lots of suggestions about what to do. |

Stolen from badscience.net |
Peter Medawar, the eminent biologist, in his classic book Advice to a Young Scientist, said this.
“Exaggerated claims for the efficacy of a medicament are very seldom the consequence of any intention to deceive; they are usually the outcome of a kindly conspiracy in which everybody has the very best intentions. The patient wants to get well, his physician wants to have made him better, and the pharmaceutical company would have liked to have put it into the physician’s power to have made him so. The controlled clinical trial is an attempt to avoid being taken in by this conspiracy of good will.”
There was a lot of truth in that 1979, towards the end of the heyday of small molecule pharmacology. Since then, one can argue, things have gone downhill.
First, though, think of life without general anaesthetics, local anaesthetics, antibiotics, anticoagulants and many others. They work well and have done incalculable good. And they were developed by the drug industry.
But remember also that remarkably little is known about medicine. There are huge areas in which neither causes nor cures are known. Treatments for chronic pain, back problems, many sorts of cancer and almost all mental problems are a mess. It just isn’t known what to do. Nobody is to blame for this. Serious medical research has been going on for little more than 60 years, and it turns out to be very complicated. We are doing our best, but are still ignorant about whole huge areas. That leads to a temptation to make things up. Clutching at straws is very evident when it comes to depression, pain and Alzheimer’s disease, among others.
In order to improve matters, one essential is to do fair tests on treatments that we have. Ben Goldacre’s book is a superb account of how this could be done, and how the process of testing has been subverted for commercial gain and to satisfy the vanities of academics.
Of course there is nothing new in criticisms of Big Pharma. The huge fines levied on them for false advertising are well known. The difference is that Goldacre’s book explains clearly what’s gone wrong in great detail, documents it thoroughly, and makes concrete suggestions for improving matters.
Big Pharma has undoubtedly sometimes behaved appallingly in recent years. Someone should be in jail for crimes against patients. They have behaved in much the same way that bankers have. In any huge globalised industry it is always possible to blame someone in another department for the dishonesty. But they aren’t the only people to blame. None of the problems could have arisen with the complicity of academics, universities, and a plethora of regulatory agencies and professional bodies.
The biggest scandal of all is missing data (chapter 1). Companies, and sometmes academics, have suppressed of trials that don’t favour the drugs that they are trying to sell. The antidepressant drug, reboxetine, appeared at first to be good. It had been approved by the Medicines and Healthcare products Regulatory Agency (MHRA) and there was at least one good randomized placebo-controlled trial (RCT) showing it worked. But it didn’t. The manufacturer didn’t provide a complete list of unpublished trials when asked for them. After much work it was found in 2010 that, as well as the published, favourable trial, there were six more trials which had not been published and all six showed reboxetine to be no better than placebo . In comparisons with other antidepressant drugs three small studies (507 patients) showed reboxetine to be as good as its competitors. These were published. But it came to light that data on 1657 patients had never been published and these showed reboxetine to be worse than its rivals.
When all the data for the SSRI antidepressants were unearthed (Kirsch et al., 2008) it turned out that they were no better than placebo for mild or moderate depression. This selective suppression of negative data has happened time and time again. It harms patients and deceives doctors, but, incredibly, it’s not illegal.
Disgracefully, Kirsch et al. had to use a Freedom of Information Act request to get the data from the FDA.
“The output of a regulator is often simply a crude, brief summary: almost a ‘yes’ or ‘no’ about side effects. This is the opposite of science, which is only reliable because everyone shows their working, explains how they know that something is effective or safe, shares their methods and their results, and allows others to decide if they agree with the way they processed and analysed the data.”
|
“the NICE document discussing whether it’s a good idea to have Lucentis, an extremely expensive drug, costing well over £ 1,000 per treatment, that is injected into the eye for a condition called acute macular degeneration. As you can see, the NICE document on whether this treatment is a good idea is censored. Not only is the data on the effectiveness of the treatment blanked out by thick black rectangles, in case any doctor or patient should see it, but absurdly, even the names of some trials are missing, preventing the reader from even knowing of their existence, or cross referencing information about them.Most disturbing of all, as you can see in the last bullet point, the data on adverse events is also censored.”
|
The book lists all the tricks that are used by both industry and academics. Here are some of them.
- Regulatory agencies like the MHRA, the European Medicines Agency (EMA) and the US Food and Drugs Administration (FDA) set a low bar for approval of drugs.
- Companies make universities sign gagging agreements which allow unfavourable results to be suppressed, and their existence hidden.
- Accelerated approval schemes are abused to get quick approval of ineffective drugs and the promised proper tests often don’t materialise
- Disgracefully, even when all the results have been given to the regulatory agencies (which isn’t always). The MHRA, EMA and FDA don’t make them public. We are expected to take their word.
- Although all clinical trials are meant to be registered before they start, the EMA register, unbelievably, is not public. Furthermore there is no check that the results if trials ever get published. Despite mandates that results must be published within a year of finishing the trial, many aren’t. Journals promise to check this sort of thing, but they don’t.
- When the results are published, it is not uncommon for the primary outcome, specified before it started, to have been changed to one that looks like a more favourable result. Journals are meant to check, but mostly don’t.
- Companies use scientific conferences, phony journals, make-believe “seed trials” and “continuing medical education” for surreptitious advertising.
- Companies invent new diseases, plant papers to make you think you’re abnormal, and try to sell you a “cure”. For example, female sexual dysfunction , restless legs syndrome and social anxiety disorder (i.e. shyness). This is called disease-mongering, medicalisation or over-diagnosis. It’s bad.
- Spin is rife. Companies, and authors, want to talk up their results. University PR departments want to exaggerate benefits. Journal editors want sensational papers. Read the results, not the summary. This is universal (but particularly bad in alternative medicine).
- Companies fund patient groups to lobby for pills even when the pills are known to be ineffective. The lobby that demanded that Herceptin should be available to all on the breast cancer patients on the NHS was organised by a PR company working for the manufacturer, Roche. But Herceptin doesn’t work at all in 80% of patients and gives you at best a few extra months of life in advanced cases.
- Ghostwriting of papers is serious corruption. A company writes the paper and senior academics appear as the authors, though they may never have seen the original data. Even in cases where academics have admitted to lying about whether they have seen the data, they go unpunished by their universities. See for example, the case of Professor Eastell.
- By encouraging the funding of “continuing medical education” by companies, the great and the good of academic medicine have let us down badly.
This last point is where the book ends, and it’s worth amplification.
“So what have the great and good of British medicine done to help patients, in the face of this endemic corruption, and these systematic flaws? In 2012, a collaborative document was produced by senior figures in medicine from across the board, called ‘Guidance on Collaboration Between Healthcare Professionals and the Pharmaceutical Industry’. This document was jointly approved by the ABPI, the Department of Health, the Royal Colleges of Physicians, Nursing, Psychiatrists, GPs, the Lancet, the British Medical Association, the NHS Confederation, and so on. ”
“It contains no recognition of the serious problems we have seen in this book. In fact, quite the opposite: it makes a series of assertions about them that are factually incorrect.”
“It states that drug reps ‘can be a useful resource for healthcare professionals’. Again, I’m not sure why the Royal Colleges, the BMA, the Department of Health and the NHS Confederation felt the need to reassert this to the doctors of the UK, on behalf of industry, when the evidence shows that drug reps actively distort prescribing practices. But that is the battle you face, trying to get these issues taken seriously by the pinnacle of the medical establishment.”
This is perhaps the most shameful betrayal of all. The organisations that should protect patients have sold them out.
You may have been sold out by your “elders and betters”, but you can do something. The “What to do” sections of the book should be produced as a set of flash cards, as a reminder that matters can be improved.
It is shameful that this book was not written by a clinical pharmacologist, or a senior doctor, or a Royal College, or a senior academic. Why has the British Pharmacological Society said nothing?
It is shameful too that this book was not written by one of the quacks who are keen to defend the $60 billion alternative medicine industry (which has cured virtually nothing) and who are strident in their criticism of the 600 billion dollar Pharma industry. They haven’t done the work that Goldacre has to analyse the real problems. All they have done is to advocate unfair tests, because that is the only sort their treatments can pass.
It’s weird that medicine, the most caring profession, is more corrupt than any other branch of science. The reason, needless to say, is money. Well, money and vanity. The publish or perish mentality of senior academics encourages dishonesty. It is a threat to honest science.
Goldacre’s book shows the consequences: harm to patients and huge wastage of public money.
Read it.
Do something.
Follow-up
7 October, 2012, The Observer
Goldacre wrote
"I think it’s really disappointing that nobody, not the Royal Colleges, the Academy of Medical Sciences, the British Pharmacological Society, the British Medical Association, none of these organisations have stood up and said: selective non-publication of unflattering trial data is research misconduct, and if you do it you will be booted out. And I think they really urgently should."
Exactly.