MHRA
The bulletin of the British Pharmacological Society, Pharmacology Matters, declined to publish the following article. Sadly the Society seems to be more interested in "reputation management" than in truth. Luckily, it is not easy to suppress criticism these days. A version of the article has appeared in Research Fortnight where it will be seen by far more people than it would have been in Pharmacology Matters. This is the original version that I submitted to them. They would not allow me to quote Lewis’s comment (apropos of the sale of homeopathic meningitis vaccine)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
If a child were to die of whooping cough or meningitis as a result of buying the fraudulent "vaccines", that would be true. It’s a sad reflection on the state of defamation law that journals are not willing to say so. Blogs are fast becoming the best source of reliable information.

|

|
Stop press. The BPS has now signed up to Alltrials (too late for the printed version)
Pharmacology society does little to defend its subject
David Colquhoun
Over the past few years a courageous group of writers, researchers and activists has worked to expose the truth about the medicines we are sold, be they conventional or alternative.
Thanks, above all, to Ben Goldacre (1), more people than ever know that the big pharma companies have been concealing evidence of the harm that their products do, or the good they fail to do. Thanks to a small army of bloggers the preposterous claims made by peddlers of homeopathic remedies and other quackery are less likely to go unchallenged.
And yet, the organization charged with safeguarding the good name of pharmacology in this country, the British Pharmacological Society (BPS), has remained silent throughout.
The pharmaceutical industry
The BPS, rather than helping, became actively complicit when, along with much of the medical establishment, it signed an agreement with the ABPI (2). This document, developed under the aegis of the Ethical Standards in Health & Life Sciences Group (ESHLSG), contained two objectionable clauses:
“Industry plays a valid and important role in the provision of medical education”
And
“Medical representatives can be a useful resource for healthcare professionals”
Given that clinical “education” has long been part of Pharma’s marketing strategy, this seems disgraceful. And most of the doctors I know and respect refuse to see reps altogether. It is hopelessly optimistic to think that can an industry person can teach clinical pharmacology without bias in favour of his own company’s products. The BPS has many members who teach pharmacology. Can they really cope so badly that we need to have industry to educate clinicians?
It’s fine, and sometimes desirable, for academics and industry to work together on drug development. But only as long as the industry partner has no say in how, or whether, the results are published. Without that proviso we can expect more corruption of the sort that’s been seen at the University of Sheffield (3).
This is very sad, because I have great reason to like the drug industry. I’ve benefitted from several of their products myself. But the industry is in trouble. Many of its products provide only marginal benefits. Furthermore, some of the things that seemed to be useful, like SSRI antidepressants, have turned out to be next to useless once hidden trials were revealed (4). The MHRA’s learning module on SSRIs doesn’t seem to have caught up with this yet.
Sadly, the reaction of industry has been to resort to dishonesty, to hide unfavourable data and to increase yet more what it spends on marketing. Between 2009 and 2012, fines of at least 10 billion dollars (5) have been imposed on some of the most eminent companies. They include Lilly, Pfizer, AstraZeneca, Merck, Abbott and GlaxoSmithKline (GSK). The biggest fine of all ($3 bn, in July 2012) went to a British company, GSK. This succession of large fines seems to be regarded by the companies as mere marketing expenses.
All these fines were levied in the USA. Where, one might ask, are the regulators in the UK? Why have there been no fines here? Why, indeed, are some of the senior managers of these companies not in jail? Why has the BPS remained silent about the prostitution of its subject? And why have the MHRA done so little to stop it?
I suggest that you support the petition for release of the results of all trials (6). It’s been supported by many individuals and a lot of organisations, including the BMJ and the Royal Statistical Society. But, disgracefully, not by the BPS.
Quackery
At least in the case of the pharmaceutical industry some of its products work. But pharmacologists should also be concerned about the quackery industry, worth about 60 billion dollars per year (as opposed to $600 bn for the pharmaceutical industry). Virtually none of their products work (7). Why has the BPS said so little about it? It has, along with most of the medical and university establishment, shrugged its shoulders about the fact that students at Westminster University have been shown dowsing with a pendulum as a method for selection of herbal “remedies”, as part of a Bachelor or “Science” degree. It is an area in which every regulatory agency has failed to ensure even minimal levels of honesty (8). And the BPS has just shrugged.
The MHRA has been worse than useless in this area: it has been actively unhelpful (9). The senior staff of the MHRA are members of the BPS which has, as usual, said next to nothing. The MHRA’s herbal medicine committee has allowed misleading labels that give indications to be put on herbal potions, and these labels fail to make it clear that no evidence whatsoever of efficacy is required to get the MHRA kitemark. The wording was suggested (not required) by European law, but that law does not prevent the MHRA from saying, as it should, “there is no reason to think that this product is effective for any of the indications on the label” (10). Arguably, the MHRA is in breach of Consumer Protection law (11, 12).
At the time, the BPS did make some objection to the labelling (13), but only under great pressure from me (indeed I wrote it) . That has not been followed up, and I can no longer find it on the BPS web site. Indeed Philip Routledge, one of the people who is responsible for the misinformation in his capacity as chair of the MHRA Herbal Medicines Advisory Committee, is, at present the president of the BPS.
The MHRA has also been responsible for misleading labelling of the products of the most obviously fraudulent products of the lot: homeopathic pills, the medicines that contain no medicine. Most of the pills (anything beyond 12x dilution) contain not a single molecule of the substance on the label. Yet they have been given a get-out clause that enables them to evade prosecution by Trading Standards (an organisation that consistently fails to apply consumer protection laws. Rose et al (2011) (12) concluded
"EU directive 200s5/29/EC is largely ineffective in preventing misleading health claims for consumer products in the UK".
It is simply bizarre that the people at the MHRA, many of who are BPS members, have sat round a table and approved the following label. This example is for Arnica 30C pills, which, of course, contain no trace of arnica (14, 8). The outcome of their deliberations is simply surreal (see the actual labels here).
"Used within the homeopathic tradition for the symptomatic relief of sprains, muscular ache; and bruising or swelling after contusions."
This will deceive the naïve into thinking that it will have some effect on sprains etc. It won’t. And the MHRA have declined to test how the label is perceived by the public, though it took some effort to get them to admit it.
"If you are allergic to any of the ingredients in this medicine, consult your doctor before taking this medicine."
The ingredients aren’t stated apart from “contains lactose and sucrose”. That’s all they contain. No arnica.
"If pregnant or breastfeeding consult your doctor before use."
Why should a few mg of lactose and sucrose have the slightest effect on a pregnant or breast-feeding mother. This is pure make-believe
"If you forget to take this product, continue to take your usual dose at the usual time, it does not matter if you have missed a dose. Do not take a double dose to make up for a missed dose."
This statement is even more bizarre. There is nothing in the pills.
"If you take too much of this product (overdose) speak to a doctor or pharmacist and take this label with you."
And this is the ultimate in nonsense. The 1023 campaign regularly swallows whole bottles, and of course nothing happens. You can’t overdose on nothing. The fact that the MHRA can insist on this label, with a straight face, is the ultimate betrayal of science and reason.
"When asked to comment, as part of the consultation on these rules, this was the response from the BPS."
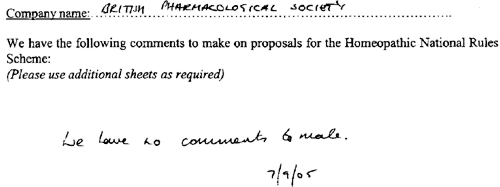
This is extracted from page 16 of the “selected response” provided by the MHRA under a Freedom of Information Act request [download all]
Things have changed little since A.J. Clark wrote his book on Patent Medicines in 1938 (15). And the BPS has done next to nothing to help. Neither has the MHRA. In fact both have colluded in the failures of both honesty and reason.
A BBC South West program recently revealed that a pharmacist was selling “homeopathic vaccines” for whooping cough and meningitis (16). The MHRA have know about his homicidal practice for years, but have done nothing. The General Pharmaceutical Council let him off with a rap on the knuckles. It has been left to bloggers and TV reporters to focus attention on these scoundrels. The well-respected blogger, Andy Lewis, wrote (17)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
And the full clinical data for Tamiflu are still being concealed by Roche (18).
I think that is rather shameful.
I have been a member of the BPS for all my working life. I was happy when they made me an honorary fellow. But I now find myself asking if I can remain a member of an organisation that has done so little to defend honest scientific behaviour.
References
(1) Ben Goldacre’s Bad Pharma. Buy it now. Then do something. https://www.dcscience.net/?p=5538
(2) ABPI 2012 Guidance on collaboration between healthcare professionals and the pharmaceutical industry. http://www.abpi.org.uk/our-work/library/guidelines/Pages/collaboration-guidance.aspx
(3) Colquhoun, D. (2007) The Corporate Corruption of Higher Education: part 2 https://www.dcscience.net/?p=193
(4) Kirsch,I., B.J.Deacon, T.B.Huedo-Medina, A.Scoboria, T.J.Moore, and B.T.Johnson. 2008. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS. Med. 5:e45. http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0050045
(5) Groeger, L. (2012) Big Pharma’s Big Fines http://www.propublica.org/special/big-pharmas-big-fines
(6) All trials registered. All results reported, http://www.alltrials.net/supporters/
(7) Singh,S. and E.Ernst. 2009. Trick or Treatment. Corgi. http://en.wikipedia.org/wiki/Trick_or_Treatment
(8) Colquhoun, D. (2012) Regulation of alternative medicine: why it doesn’t work, and never can. https://www.dcscience.net/?p=5562
(9) Colquhoun, D, (2006) The MHRA breaks its founding principle: it is an intellectual disgrace. https://www.dcscience.net/?p=32
(10) Colquhoun, D. (2011). Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. https://www.dcscience.net/?p=4269
(11) Colquhoun, D. (2009) Most alternative medicine is illegal. https://www.dcscience.net/?p=30
(12) Rose,L.B., P.Posadzki, and E.Ernst. 2012. Spurious claims for health-care products: an experimental approach to evaluating current UK legislation and its implementation. Med. Leg. J. 80:13-18. https://www.dcscience.net/Rose-medico-legal-2012.pdf
(13) Colquhoun, D. (2006) Learned Societies speak out against CAM, and the MHRA. https://www.dcscience.net/?p=30
(14) MHRA Arnicare Arnica 30c pillules NR 01175/0181 http://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con049307.pdf
(15) Colquhoun, D. (2008) Patent medicines in 1938 and now: A.J.Clark’s book. https://www.dcscience.net/?p=257
(16) BBC South West on the evils of homeopathic "vaccines" http://www.youtube.com/watch?v=TZf9mUzI4RI
(17) Why Does the MHRA Not Close Down these Homeopaths? The regulators have known of serious problems for years, Nothing is done. http://www.quackometer.net/blog/2013/01/why-does-the-mhra-not-close-down-these-homeopaths.html
(18) Payne, D. (2012). Tamiflu: the battle for secret drug data http://www.bmj.com/content/345/bmj.e7303
Follow-up
25 February 2013 This post has some follow-up even before it appeared on Research Research. I noticed on the BPS web site a press release “BPS announces intention to sign All Trials Petition“. It was dated 20th February, but I didn’t notice it until after the printed edition went to press. It was expressed as a future intention to sign, though in fact they signed almost straight away (though over 100 organisations had already done so). That’s good. I suspect that when my old friend, Humphrey Rang, who is president elect of the BPS, takes charge, the Society may start to take its responsibilities to the public more seriously than it has in the past.
|
The MHRA, on the other hand, is still evading its self-declared job of ensuring the public that drugs work. |

|
13 March 2013. A reply to this piece appeared in red on Research Research, The British Pharmacological Society champions its science. It was written by Humphrey Rang who, as president elect of the BPS naturally felt obliged to defend its record. He defends the BPS membership of ESHLSG, but fails to mention that first the Lancet and then the BMA withdrew their support. Nor does he mention that medical students and doctors launched a campaign, BadGuidelines.org, against the agreement. The Medical Schools Council, which also signed the agreement, said "the scrutiny of the guidance has ‘identified deficiencies in the current statement". Didn’t they read it before signing? Rang says that the BPS is also working to improve the joint statement with the ABPI. That’s good, but one must wonder why the BPS signed up to the original form.
On the points about quackery, Rang sites the BPS statement on homeopathy (now vanished) but fails to mention that that statement was written by me in an attempt to wake the BPS from it’s slumbers on the matter of medicines that don’t work. But he doesn’t mention at all the matter of mislabelling of both homeopathic and herbal preparations.
Of course, the BPS does many good things. But like most organisations, it is too reluctant to speak out when it sees wrongdoing, and too reluctant to say "sorry we made a cock-up that time".
Which? Magazine (the UK equivalent of Consumer Reports in the USA) has done it again. They published an excellent article, Health products you don’t need. It’s a worthy successor to their recent debunking of “nutritional therapists”. Most of the products in question, apart from Bach Rescue Remedy Spray, were not outright quackery like homeopathy or "detox" products. Rather they were old-fashioned pharmaceutical products that were quite respectable in the 1950s but which have subsequently been found not to work.
These are the things that were looked at.
- Benylin Chesty Coughs (Non-Drowsy)
- Benylin Tickly Coughs (Non-Drowsy)
- Covonia Herbal Mucus
Cough Syrup - Boots Cold and Flu Relief
Tablets - Adios Slimming Tablets
- Bio-Oil
- Seven Seas Jointcare Be Active
- Bach Rescue Remedy
Spray
It’s an interesting and large category, and its one that I grew up with. My first job, in the 1950s was as an apprentice in Timothy Whites & Taylors Homeopathic Chemists in Grange Road, Birkenhead (you can’t have a much humbler start than that). Don’t worry about he homeopathic bit. We had one homeopathic prescription in two years, which was made up with great hilarity. These were the days before the endarkenment.
We did, however, sell a lot of "tonics" and "cough medicines". Two popular brands were Metatone Tonic and Minadex Tonic. I was quite surprised to discover that they are still on sale. Even in the 1950s I was a bit sceptical about what a "tonic" was supposed to achieve. The term soon became extinct as it was slowly realised that no examples existed.
Here is the bad news. It is scarcely an exaggeration to assert the following.
- Nothing is known that alters the time course of a cold.
- There is nothing that you can buy that will suppress a cough*.
- There is no such thing as a "demulcent" or an "expectorant"
- There is no such thing as a "tonic".
- It would be nice if these things existed, but they are figments of the imagination. Nonetheless they sell by the truckload and vast amounts of money are made by selling them.
[*morphine may have a modest effect, but you can’t buy it]
How can this happen? We have the Medicines and Healthcare products Regulatory Agency (MHRA) is the government agency which is responsible for ensuring that medicines and medical devices work, and are acceptably safe.
Demulcents
In the 1950s this was a more or less respectable term. If you google it now, almost all the references come from herbalists, It is, almost entirely, part of the world of quackery. Apart, that is, from the MHRA. And NHS Evidence. It was surprising to find, in a 2009 document from the MHRA
"Simple cough mixtures containing a demulcent, for example glycerin, and syrup can have a soothing effect by coating the throat and relieving the irritation which causes the cough"
No reference is given, and I’m not aware of the slightest reason to think that there is any such effect. Syrup in your respiratory tract is a bit of a disaster.
But the same document says
There are severe limitations to the efficacy studies given that many of the products were first introduced decades ago. There has been no co-ordinated development program to establish efficacy. What trials there are have not been carried out to current standards.
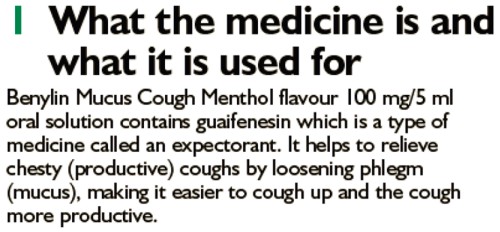
There isn’t much detail about these old ‘remedies’ on the MHRA site. I did find a Publiic Assessment Report for Benylin Mucus Cough Menthol Flavour Oral Solution. The main ingredient is Guaifenesin
The assessment says this.
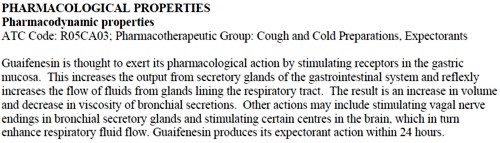
And the approved label says this.
The Public Assessment Report also says
Efficacy
Guaifenesin . . . is a well-established medicinal product with well-known efficacy and safety profiles
This appears to be pure make-believe. There is no credible evidence for any such effect. The report may be dated 2012, but it is a carry-over from a previous age.
In 1976, it was pointed out that none of these things worked (Ziment, 1976), and the situation hasn’t changed. Ziment’s review concludes
"Perhaps this is the one disease that could truly benefit from that oft-touted panacea of therapeutics, the overworked nostrum of materia medica—namely, chicken soup"
A 2012 Cochrane review agrees: "Over-the-counter (OTC) medications for acute cough". This review concludes
"We found no good evidence for or against the effectiveness of over-the-counter (OTC) medications in acute cough, which confirms the findings of two previous reviews (Anonymous 1999; Smith 1993)."
What the MHRA tell me
I was puzzled by the apparently unjustified statements on the MHRA site so I asked them about the eight products that were investigated by Which? magazine (see above). I asked them also about Metatone and Minadex "tonics"
The questions, and the responses can be downloaded here. (I merely asked some reasonable questions, but the MHRA chose to treat them as a request under the Freedom of Information Act).
The first five items all have full marketing authorisation, as do Metatone and Minadex "tonics".
"Metatone (PL-02855/0017), Covonia Herbal Mucus Cough Syrup, Cold and Flu Relief Tablets and Adios Tablets originally held Product Licences of Right. These products were on the market before the Medicines Act 1968 came into force in 1971. These licences were reviewed in the 1980s to ensure that the products were safe, of suitable quality and have evidence of efficacy. Because of the length of time that the products had been on the market they were considered to have well established use and original clinical data to today’s standards was not necessarily available."
The MHRA tell me that they have no copies of the reviews conducted in the 1980s, apart from one. They sent a scanned copy of the August 1988 expert review of Covania syrup (the ingredients have changed since than).
The document is like an antique. It simply repeats the old myths. The names of the "expert reviewers" have been hidden. Given the quality of the review, perhaps that isn’t surprising, but the MHRA should not be so secretive.
There is no such thing as a "tonic", so I asked the MHRA about that too.
Q.5 Can you tell me what criteria the MHRA uses when allowing a product to be advertised as a "tonic"?
R.5 The MHRA assesses proposed product names on a case by case basis. On the basis of the well established use of Minadex Tonic it was decided that the use of the word tonic in the product name was acceptable. For the same reason, it was accepted that Metatone could be referred to as a tonic in the Product Information Leaflet and product labels
In other words, we let them get away with it because it’s old.
I had always understood that when the MHRA grants "Marketing authorisation", that meant there was some guarantee that the product worked. You’d infer that from the MHRA’s own definition.(my emphasis)
"Medicines which meet the standards of safety, quality and efficacy are granted a marketing authorisation (previously a product licence),"
Sadly, it seems that this isn’t true, at least for old-established products, those that were on the market before the Medicines Act (1968) came into force in 1971.
Conclusion
Although old products which were on the market before 1971 were supposed to be reviewed for efficacy and safety. This hasn’t been done efficiently. The make-believe has simply been perpetuated. I have no objection to people buying benylin etc, but they should not have full marketing authorisation and they should be labelled accurately so that it is clear that there is very little evidence that they’ll do you much good. The MHRA has let down the public, just as it did when it allowed misleading labels on homeopathic and herbal potions.
Postscript
After writing this, I discovered a very recent paper about guaifenesin (Seagrave et al, 2012), This paper shows some effects on mucus secretion in cultured human cells (not in humans) with prolonged exposure to concentrations of 30 and 100 µM. This is an order of magnitude greater than the peak blood concentration (7 µM. = 1.4 µg/ml) that is achieved (transiently) in man (Maynard & Bruce, 1970). This is not mentioned in the paper. I’m sure that has nothing to do with what we read at the end of the paper.
Competing interest
JS has received research funds from Reckitt Benckiser. HHA is a consultant to Reckitt Benckiser and is the co-author of a Mucinex sustained-release guaifenesin) patent. DBH has received research funds and consultancy payments from Reckitt Benckiser. DFR has received consultancy payments from Reckitt Benckiser. GS is an employee of Reckitt Benckiser and is also a co-author of a Mucinex (sustained-release guaifenfesin) patent.Acknowledgements
This study was funded by Reckitt Benckiser Healthcare International Ltd. Assistance with manuscript submission was provided by Elements Communications Ltd, supported by Reckitt Benckiser Healthcare International Ltd.
On 15 October 2010, Reckitt Benckiser was fined £10.2 m by the Office of Fair Trading after the company admitted anti-competitive behaviour.
Follow-up
Shortly after this post went up. I was attacked on twitter by @iHealthP. That’s a company, http://www.ihealthpartnership.com (the tweeter declined to reveal their identity). It started thus.
Your article asserts that “There is nothing that will suppress a cough.” This is bollocks, pure & simple.
The interchange was one of those less pleasant Twitter moments (I’ve Storifed some of it in case anyone is interested). The discussion did throw up a few useful references though. @LeCanardNoir pointed out a 2007 paper which concludes
"Clearly the widespread notion that codeine is an effective cough suppressant is not supported by the available evidence."
One of the papers cited by @iHealthP in support of his/her contention that pholcodine and codeine work was Recommendations for the management of cough in adults (from the British Thoracic Society Cough Guideline Group). This paper actually concludes
“There are no effective treatments controlling the cough response per se with an acceptable therapeutic ratio.”
That, of course, is exactly what I said.
There was, however, one reference produced by @iHealthP for which I’m grateful. It doesn’t concern over-the-counter cough treatments (which is what this post is about), but morphine. It does, though, produce some evidence that morphine does work to some extent as a cough suppressant. Amazingly this "well-known truth" was not demonstrated until 2006. The paper, Opiate Therapy in Chronic Cough, by Morice et al., 2006. shows a convincing effect of morphine (5 or 10 mg twice a day) on chronic cough. The main caveat lies in the reported side effects: constipation (40%) and drowsiness (25%). Obvious side-effects can make the trial non-blind. In any case, none of this is relevant to the present post (though I altered the blog to refer to it).
Since writing about anti-scientific degrees in Nature (March 2007), much has been revealed about the nonsense that is taught on these degrees. New Year’s day seems like a good time to assess how far we’ve got, five years on.
At the beginning of 2007 UCAS (the universities central admission service) offered 45 different BSc degrees in quackery, at 16 universities.
Now there are only 24 such degrees.
If you exclude chiropractic and osteopathy, which all run at private colleges, with some sort of "validation" from a university, there are now only 18 BSc/MSc courses being offered in eight universities.
Degrees in homeopathy, naturopathy and "nutritional therapy", reflexology and aromatherapy have vanished altogether from UCAS.
In the race to provide BScs in anti-science, Middlesex University has now overhauled the long-standing leader, Westminster, by a short head.
 Michael Driscoll, vice-chancellor of Middlesex |
|
Let’s see what’s gone.
The University of Central Lancashire (UCLAN) was the first to see sense. In August 2008 they announced closure of their “BSc” degree in homeopathy. On September 2008 they announced an internal review of their courses in homeopathy. herbalism and acupuncture. The report of this review closed down all of them in July 2009. I first asked for their teaching materials in July 2006. I finally got them in December 2010, after winning an appeal to the Information Commissioner, and then winning an appeal against that decision at an Information tribunal . By the time I got them, the course had been closed for over two years. That is just as well, because it turned out that UCLAN’s students were being taught dangerous nonsense. No wonder they tried so hard to conceal it.
Salford University was the next to go. They shut down their courses in complementary medicine, homeopathy and acupuncture. In January 2009 they announced " they are no longer considered “a sound academic fit” ". Shortly afterwards. a letter appeared in The Times from three heavyweights (plus me) congratulating the vice-chancellor on his decision.
University of Westminster
For many years, Westminster was the biggest supplier of BSc degrees in quackery. At the beginning of 2007 they offered 14 different BSc degrees in homeopathy, naturopathy, nutritional therapy, "complementary therapies", (western) herbal medicine and traditional Chinese medicine with acupuncture. Some of their courses were so bizarre that some of the students and even staff sent me slides which taught things like "amethysts emit high Yin energy". Like UCLAN, Westminster also held an internal review. Unlike UCLAN it came to the absurd conclusion that all would be well if they injected more science into the courses. The incompetence of the review meant that those who wrote it hadn’t noticed that if you try to put science into homeopathy or naturopathy, the whole subject vanishes in a puff of smoke. Nevertheless Westminster closed down entry to BSc homeopathy in March 2009 (though the subject remained as part of other courses).
Three years after the Nature article, all five BSc homeopathy degrees had shut their doors.
During 2011, Westminster shut down Naturopathy, Nutritional therapy, Therapeutic bodywork and Complementary Medicine. See, for example,
More dangerous nonsense from the University of Westminster: when will Professor Geoffrey Petts do something about it?
Now Westminster has only four courses in two subjects. They still teach some dangerous and untrue things, but I suspect the writing is on the wall for these too.
I have seen a document, dated 11 April 2011, which states
“The following courses have been identified as ‘at risk’ (School definition) and will be discussed at the APRG and University Review Group2, due to poor recruitment and high cost of delivery:
Integrated Health Scheme: BSc Complementary Medicine, Naturopathy; BSc Chinese Medicine; BSc Nutritional Therapy; BSc Herbal Medicine”
All but Chinese medicine and Herbal medicine have already gone. Almost there.
University of Wales
Since my first post in 2008 about the validation scam operated by the University of Wales, and some good investigations by BBC Wales TV, the outcome was the most spectacular so far. The entire institution collapsed. They no longer "validate" external degrees at dodgy business colleges, loony religious colleges or magic medicine colleges.
Another worthless validation: the University of Wales and nutritional therapy (October 2008) This is a ‘degree’ in nutrtional therapy. It is even more hilarious than usual, but it passed the validation anyway.
Scandal of the University of Wales and the Quality Assurance Agency (November 2010). This post followed the BBC Wales TV programme. At last the QAA began to notice, yet further confirmation of its utter ineptitude.
The University of Wales disgraced (but its vice chancellor is promoted) (October, 2011) The eventual collapse of the university was well-deserved. But it is very weird that the people who were responsible for it have still got their jobs. In fact the vice-chancellor, Marc Clement, was promoted despite his mendacious claim to be unaware of what was going on.
It remains to be seen how many of the many quack courses that were validated by the University of Wales will be taken on by other universities. The McTimoney College of Chiropractic is owned by BPP University (so much for their quality control, as explained in Private Eye). but still claims to be validated by Wales until 2017.
Some of the more minor players
Edinburgh Napier University. After an FOI request (rejected), Napier closed their herbal medicine degree in 2010.
Hot and cold herbal nonsense from Napier University Edinburgh: another course shuts. (June 2010)
As expected, the Scottish Information Commissioner agreed with that for England and Wales and ordered material to be sent. Edinburgh Napier University teaches reflexology, aromatherapy and therapeutic touch. Scottish Information Commissioner says you should know. Some of the horrors so discovered appeared in Yet more dangerous nonsense inflicted on students by Edinburgh Napier University. The embarrassment seems to have worked. Their remaining degrees in aromatherapy and reflexology have now vanished from UCAS too. All that remains is a couple of part time “Certificates of Credit” for aromatherapy and reflexology
Anglia Ruskin Univerity Not only have BSc degrees gone in aromatherapy and reflexology, but their midwifery degree now states "We are unable to accept qualifications in aromatherapy, massage and reflexology."
University of Derby Reflexology and aromatherapy have gone, though doubtless Spa management therapies have much nonsense left
University of Greenwich. BSc in Complementary Therapies (Nutritional Health) and BSc in Complementary Therapies (Nutritional Health) have been shut. The BSc Acupuncture is listed on their web site but it is under review, and is not listed in UCAS for 2012. (Acupuncture is run at International College of Oriental medicine, validated by Greenwich.). Only osteopathy (MOst) is still running, and that is a validation of an external course run at The European School of Osteopathy, in Maidstone
Thames Valley University was renamed the University of West London in 2010. The nonsense that was run there (e.g. Nutritional Fairy Tales from Thames Valley University) seems to have vanished. Their previous alt med guru, Nicola Robinson, appears now to be at London South Bank University (ranked 116 out of the 116 UK universities)
What’s left?
Chiropractic Surprisingly, given the total discreditation of chiropractic in the wake of the Simon Singh affair, and the internecine warfare that followed it, none of the chiropractic courses have shut yet. Some are clearly in trouble, so watch this space.
Osteopathy has also had no course closures since 2007. Like chiropractic it also suffers from internecine warfare. The General Osteopathic Council refuses to disown the utter nonsense of "craniosacral" osteopathy. But the more sensible practitioners do so and are roughly as effective as physiotherapists (though there are real doubts about how effective that is).
Excluding chiropractic and osteopathy, this is all that’s left. It now consists almost entirely of Chinese medicine and a bit of herbal.
Glyndwr university (Known as North East Wales Institute until 2008) Ranked 104 out of 116 UK universities
BSc Acupuncture (B341) BSc
BSc Complementary Therapies for Healthcare (B343)
Cardiff Metropolitan University (UWIC) (Known as University of Wales Institute Cardiff (UWIC) until Nov 2011.) The vice-chancellor of Cardiff Metropolitan, Antony Chapman, is in the QAA’s board of directors, so perhaps it isn’t surprising that the QAA has done nothing.
BSc Complementary Therapies (3 years) (B390)
BSc Complementary Therapies (4 yrs inc Foundation) (B300)
University of Lincoln
Acupuncture (B343) 3FT Hon BSc
Herbal Medicine (B342) 3FT Hon BSc
University of East London Ranked 113 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
London South Bank University Ranked 116 out of 116 UK universities
Acupuncture (B343) 4FT Deg MCM
The Manchester Metropolitan University Ranked 93 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
Middlesex University
Acupuncture (B348) 3FT Hon BSc
Ayurvedic Medicine (A900) 4FT Oth MCM
Herbal Medicine (B347) 3FT Hon BSc
Traditional Chinese Medicine (BT31) 4FT Hon BSc
University of Westminster
Chinese Medicine: Acupuncture (B343) 3FT Hon BSc
Chinese Medicine: Acupuncture with Foundation (B341) 4FT/5FT Hon BSc/MSci
Herbal Medicine (B342) 3FT Hon BSc
Herbal Medicine with Foundation Year (B340) 4FT/5FT Hon BSc/MSci
It seems that acupuncture hangs on in universities that are right at the bottom of the rankings.
Manchester Metropolitan gets the booby prize for actually starting a new course, just as all around are closing theirs. Dr Peter Banister, who was on the committee that approved the course (but now retired), has told me ” I am sceptical in the current economic climate whether it will prove to be successful”. Let’s hope he’s right.
But well done Westminster. Your position as the leader in antiscientific degrees has now been claimed by Middlesex University. Their "degrees" in Ayurveda mark out Middlesex University as the new King of Woo.
Over to you, Professor Driscoll. As vice-chancellor of Middlesex University, the buck stops with you.
Both still teach Chinese and herbal medicine, which are potentially dangerous. There is not a single product from either that has marketing authorisation from the MHRA, though the MHRA has betrayed its trust by allowing misleading labelling of herbal medicines without requiring any evidence whatsoever that they work, see, for example
Why degrees in Chinese medicine are a danger to patients
More quackedemia. Dangerous Chinese medicine taught at Middlesex University
Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me
Sub-degree courses
In contrast to the large reduction in the number of BSc and MSc degrees, there has actually been an increase in two year foundation degrees and HND courses in complementary medicine, at places right near the bottom of the academic heap. The subject is sinking to the bottom. With luck it will vanish entirely from universities before too long.
Research-intensive Universities
Although all of the degrees in magic medicine are from post-1992 universities, the subject has crept into more prestigious universities. Of these, the University of Southampton is perhaps the worst, because of the presence of George Lewith, and his defender, Stephen Holgate. Others have staunch defenders of quackery, including the University of Warwick, University of Edinburgh and St Batholomew’s.
Why have all these courses closed?
One reason is certainly the embarrassment caused by exposure of what’s taught on the courses. Professors Petts (Westminster) and Driscoll (Middlesex) must be aware that googling their names produces references to this and other skeptical blogs on the front page. Thanks to some plain brown emails, and, after a three year battle, the Freedom of Information Act, it has been possible to show here the nonsense that has been foisted on students by some universities. Not only is this a burden on the taxpayer, but, more importantly, some of it is a danger to patients.
When a course closes, it is often said that it is because of falling student numbers (though UCLAN and Salford did not use that excuse). Insofar as that is true, the credit must go to the whole of the skeptical movement that has grown so remarkably in the last few years. Ben Goldacre’s "ragged band of bloggers" have produced a real change in universities and in society as a whole.
The people who should have done the job have either been passive or an active hindrance. The list is long. Vice-chancellors and Universities UK (UUK), the Quality Assurance Agency (QAA), the Hiigher Education Funding Council England (HEFCE), Skills for Health, the Medicines and Health Regulatory Authority ( MHRA) , the Health Professions Council (HPC), the Department of Health, the Prince of Wales and his reincarnated propaganda organisation, the "College of Medicine", the King’s Fund, the Universities and Colleges Union (UCU), OfQual, Edexcel, National Occupational Standards and Qualifications and the Curriculum Authority (QCA).
Whatever happened to that "bonfire of the quangos"?
Follow-up
2 January 2012 The McTimoney College of Chiropractic (owned by BPP University) claims that its “validation” by the University of Wales will continue until 2017. This contradicts the statement from UoW. Watch this space.
3 January 2012. Thanks to Neil O’Connell for drawing my attention to a paper in Pain. The paper is particularly interesting because it comes from the Southampton group which has previously been sympathetic to acupuncture. Its authors include George Lewith. It shows, yet again that there is no detectable difference between real and sham acupuncture treatment. It also shows that the empathy of the practitioner has little effect: in fact the stern authoritarian practitioner may have been more effective.
Patients receiving acupuncture demonstrated clinically important improvements from baseline (i.e., a 29.5% reduction in pain), but despite this, acupuncture has no specific efficacy over placebo for this group of patients. The clinical effect of acupuncture treatment and associated controls is not related to the use of an acupuncture needle, nor mediated by empathy, but is practitioner related and may be linked to the perceived authority of the practitioner.”
Sadly. the trial didn’t include a no-treatment group, so it is impossible to say how much of the improvement is regression to the mean and how much is a placebo effect. The authors admit that it could be mostly the former.
Surely now the misplaced confidence in acupuncture shown by some medical and university people must be in tatters.
In yet another sign that even acupuncture advovates are beginning to notice that it doesn’t work, a recent article Paradoxes in Acupuncture Research: Strategies for Moving Forward, shows some fascinating squirming.
3 January 2012. The Daily Telegraph has carried a piece about closure of university courses, written by Michael Hanlon. On 31 January they carried a much longer piece.
3 January 2012. It is a great pity that some physiotherapists seem to have fallen hook, line and sinker for the myths of acupuncture. Physiotherapists are, by and large, the respectable face of manipulative therapy. Their evidence base is certainly not all one would wish, but at least they are free of the outrageous mumbo humbo of chiropractors. Well, most of them are, but not the Acupuncture Association of Chartered Physiotherapists (AACP), or, still worse, The Association of Chartered Physiotherapists in Energy Medicine, a group that is truly away with the fairies. These organisations are bringing a very respectable job into disrepute. And the Health Professions Council, which is meant to be their regulator, has, like most regulators, done nothing whatsoever to stop it.
5 January 2012. Times Higher Education gives a history of the demise of the University of Wales, Boom or Bust. It’s a useful timeline, but like so many journalists, it’s unwilling to admit that bloggers were on to the problem long before the BBC, never mind the QAA.
There was also a leader on the same topic, Perils of the export business. It again fails to take the QAA to task for its failures.
Interviews for Deutsche Welle and Middle East Broadcasting Center TV.
17 January 2012 Another question answered. I just learned that the ludicrous course in Nutritional Therapy, previously validated by the University of Wales (and a contributor to its downfall), is now being validated by, yes, you guessed, Middlesex University. Professor Driscoll seems determined to lead his univerity to the bottom of the academic heap. His new partnership with the Northern college of Acupuncture is just one of a long list of validations that almost rivals that of the late University of Wales. The course has, of course, an enthusiastic testimonial, from a student. It starts
I work full time as a team leader for a pension company but I am also a kinesiologist and work in my spare time doing kinesiology, reiki and Indian head massage.
Evidently she’s a believer in the barmiest and totally disproved forms of magic medicine. And Middlesex University will give her a Master of Science degree. I have to say I find it worrying that she’s a team leader for a pension company. Does she also believe in the value of worthless derivatives. I wonder?
18 January 2012. the story has gone international, with an interview that I did for Deutsche Welle, UK universities drop alternative medicine degree programs. I’m quoted as saying “They’re dishonest, they teach things that aren’t true, and things that are dangerous to patients in some cases”. That seems fair enough.
There is also an interesting item from July 2010 about pressure to drop payment for homeopathy by German health insurance
31 January 2012
The Daily Telegraph carried a prominent 1200 word account (the title wasn’t mine). The published version was edited slightly.
The absurdness of allowing statutory regulation of herbal medicines, both Western and Chinese has already been pointed out here, in Government lends credibility to quacks and charlatans, and by Andrew Lewis in “How to Spot Bad Regulation of Alternative Medicine“
The harm done by the government’s endorsement of herbal products could be ameliorated if they were labelled honestly. The labelling is a matter for the Medicines and Healthcare products Regulatory Authority (MHRA), and for a while I have been writing to the head of the MRH, Kent Woods, and to Richard Woodfield (head of MHRA herbal medicine policy), in an attempt to work out their reasons for not telling the consumer the simple truth.
A similar (but even worse) problem arises in the labels that have been allowed by the MHRA for homeopathic pills. That has been discussed in Pseudo-regulation: another chance to save the MHRA from looking idiotic . The matter is not yet decided, but on past performance, I’m pessimistic about whether the MHRA will listen to scientists.
The Traditional Herbal Registration (THR) scheme allows herbal medicines that are registered on this scheme to be sold if they are safe, and have been in use for 30 years. There is need to supply any information whatsoever about whether they work or not. That itself is very odd, given that the MHRA’s strap line says
"We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
In the case of herbals, the bit about ensuring that medicines work has been brushed under the carpet.
A typical dishonest label
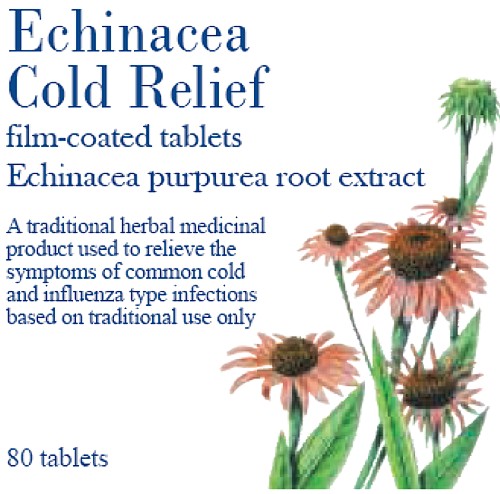
Take "Echina Cold Relief". The Traditional Herbal Regulation document specifies the label.
Note, first of all, the therapeutic claim in the brand name itself. This is blatant practice for most herbals and appears to be unregulated. The label says
|
It is my contention that most people would interpret this label as a claim that the tablets would have a beneficial effect on the symptoms of "common cold and influenza type infections". The impression is reinforced by the government stamp of approval on the package. The MHRA tell me that no tests have been done to discover how shoppers interpret these words. They should have been done.
|

|
Why is there nothing on the label that tells the plain, unvarnished truth? Perhaps something like this
"There is no evidence that this product works for the indications mentioned".
Or
"Clinical trials have shown this product to be ineffective for xxx "
or, at a minimum
"The MHRA kite mark does not imply that this product is effective".
Some Evidence
Echinacea is a generous choice of example because, unlike most herbs, there is a bit of evidence about its effectiveness. A Cochrane review says
Sixteen trials including a total of 22 comparisons of Echinacea preparations and a control group (19 placebo, 2 no treatment, 1 another herbal preparation) met the inclusion criteria. All trials except one were double-blinded. The majority had reasonable to good methodological quality. Three comparisons investigated prevention; 19 comparisons investigated treatment of colds. A variety of different Echinacea preparations were used. None of the prevention trials showed an effect over placebo. Comparing an Echinacea preparation with placebo as treatment, a significant effect was reported in nine comparisons, a trend in one, and no difference in six. Evidence from more than one trial was available only for preparations based on the aerial parts of Echinacea purpurea (E. purpurea).
“It seems that some preparations based on the herb of Echinacea purpurea might be effective for this purpose in adults, while there is no clear evidence that other preparations are effective or that children benefit. Side effects were infrequent but rashes were reported in one trial in children.”
The US agency NCCAM has spent over a billion dollars on testing various sorts of alternative treatment, and has failed to find a single useful treatment, They say
"Two NCCAM-funded studies did not find a benefit from echinacea, either as Echinacea purpurea fresh-pressed juice for treating colds in children, or as an unrefined mixture of Echinacea angustifolia root and Echinacea purpurea root and herb in adults."
So the evidence is a mess. There is no evidence that Echinacea can prevent colds, and, at the very best, it might shorten slightly the time for which cold symptoms last. The most likely interpretation of the mixture of contradictory results, many negative trials with a handful of small positive effects, is that for practical purposes, echinacea is useless. There is NO treatment known that affects the duration of a cold to any useful extent.
I wrote to Kent Woods in February 2011
|
Hello
Sorry to bother you again, but recent events have caused me to think about a rather fundamental question, and I have never seen it discussed in any official documents. I suspect it needs to be answered at the highest level. Question, Do you make any distinction between (a) herbs that have unknown efficacy (most of them). and (b) herbs that have been shown in good trials to have no useful effect (like echinacea)? It is one thing to say “traditionally used for …” when you don’t know whether it is true or not. It is quite another thing to say “traditionally used for. . . ” when you know it is untrue No such distinction seems to be made at the moment. Is that because the distinction has never been considered by the MHRA? Or is it because it has been considered, but dismissed as unimportant? Or is it considered important but you are prevented from doing anything about it (and, if this is the case, what prevents you?) Best wishes |
His reply was, essentially, that herbs come in so many different forms that they can’t all be tested so it is never possible to say that a herb “does not work to any useful extent”
|
. . . Based on our experience of regulating herbal medicines, we think it unlikely for the foreseeable future that there would be available for particular herbs a comprehensive body of published studies that meet medicines regulatory standards and cover systematically the numerous possible permutations as to type of extract, plant species and part of plant. Consequently, it is unlikely that evidence would be available for MHRA to know that a traditional herbal product did not have efficacy. In summary, you suggest an interesting scenario the handling of which would be worthy of further consideration in the event of major advances in the range and quality of clinical trials of herbal medicines – but for the foreseeable future we would see the dilemma as largely a theoretical one.
Regards Kent Woods
|
This strikes me as a cop-out. It amounts to saying that it’s impossible ever to say that a treatment us useless. If NICE took the same view, no medicine would ever be ruled out as having no useful effect.
Then I asked about a press release from the MHRA, dated 18 March 2011.
|
Hello It says (my emphasis)
Since the main sort of information that people want about a medicine is whether it works, and you have explicitly ruled out any information about that, the description "informed choice" seems to me to be exaggerated to the point of dishonesty. This raises another question. Many people think that the wording that you approve is deceptive. can you tell me whether you have yet done tests to discover whether or not the average consumer interprets your wording as suggesting effectiveness? This was raised (apropos oh homeopathics) with Kent Woods at the SciTech enquiry and they were assured such tests had been done. Still nobody has seen the result of such tests. Please will you let me know if they have been done, and, if they have, what the results were? if they have not been done, why not? Best regards |
The legal requirement
In response to my letter, Richard Woodfield said
"Specifically on the question of wording affecting efficacy, we have to comply with the requirements of the herbals Directive which specifies the required product information about the traditional basis of the registration. We have not user tested the required statement in the Directive.
"
The European Herbals directive 2004/24/EC [download it] does make it mandatory to include the words used by the MHRA
“In addition to the requirements of Articles 86 to 99, any advertisement for a medicinal product registered under this chapter shall contain the following statement: Traditional herbal medicinal product for use in specified indication( s) exclusively based upon long-standing use.”
Telling the truth on the label
I asked the MHRA whether there was any legal reason why they could not add the following notice to the wording required by the European Directive. I had to ask the question several times before I got a straight answer, but the answer eventually turned out to be that there is no legal reason that bars honest labels. Eventually Richard Woodfield told me there was no legal reason.
|
Dear Prof Colquhoun There is no specific bar in the European Directive that would definitely preclude requiring additional statements that were consistent with the Directive. Obviously one would have to look at the specifics of what was proposed.
The main bar is that of Government policy. Under the previous Administration when the scheme was set up there was a strong policy of avoiding gold plating of European legislation – and this would clearly be a case of gold plating. Under the new Government that policy of avoiding gold plating has been strengthened further. And added to that there is now a presumption that wherever possible Directives should be transposed by “copy out” of the text rather than elaborating upon the requirements of the Directive.
The onus would be on those seeking gold plating to demonstrate that it was necessary. In the present absence of evidence of significant detriment under the THR scheme to consumers who for example choose to take a THR to help with a condition such as mild indigestion we have no present plans to propose the introduction of a form of retrospective gold plating of this legislation. As recognised in your last email, I think that is about as far as we can usefully comment on the issue for the time being. Regards
Richard Woodfield |
So, at last we have the answer. And pretty pathetic it is. “Gold-plating” is a term that is used by the anti-European lobby to describe the process of not simply implementing European law but making it more strict that is essential. In this case, I would claim that making the label honest was the opposite of gold-plating, The European law is obviously designed to encourage the herbal industry by disguising the lack of evidence for the herbs. The MHRA should correct that deficiency but has declined to do so.
Safety
The herbal medicine business, especially the Chinese Traditional medicine, is riddled with impure, contaminated and sometimes lethally toxic rubbish. Of course it is right that the public should be protected from this. Probably it is a job that should be done by Trading Standards officers, but sadly they have shown themselves time and time again to be incompetent and unwilling to enforce the law when it comes to false health claims. The MHRA make a reasonably good job on this front, but that is no reason for them to endorse misleading labels. Statutory regulation by the HPC will do nothing to help: on the contrary it will endorse courses that teach dangerous nonsense.
The Herbal Medicines Advisory Committee
The MHRA’s Herbal Medicines Advisory Committee should have resisted this misleading labelling, but they do not seem to have not done so (it’s hard to tell because the published minutes are totally free of any useful information). The chairman of that committee is Professor Philip A Routledge OBE MB BS MD FRCP FRCPE. If I had been in his position, I would have resigned. I believe that he has let down honest science, and potentially endangered patients by not insisting on honest labels. I do hope that this was not a result of pressure from the Prince of Wales. We know he has lobbied Kent Woods and Philip Routledge. Incidentally, Routledge is president elect of the British Pharmacological Society. Quackery has crept in even there.
What can be done
There us no reason why, even now, the MHRA could not change the labels to something honest. I expect the government is pressing them to support the herbal industry, and big business usually wins over regulators (as with banks).
Freedom of choice by consumers was mentioned several times by the MHRA. That’s fine. Nobody wants to ban echinacea. The whole point of labels is to ensure that it is informed choice. Labels that mislead do not help anyone. They hurt the consumer and they are disastrous for the reputation for integrity of the MHRA.
We should keep up the pressure on the MHRA. Here are a couple of my recent efforts, on BBC Breakfast TV.
The second interview was joint with Dick Middleton. It should have been made clear that Middleton is a pharmacist who is technical director of Schwabe Pharma, a company that sells expensive herbal pills, so has a vested financial interest in disguising the lack of evidence for efficacy,
Follow-up
1 May 2011. The new herbal regulations have come into effect. Radio 5 put me up against the herbal industry representative, Michael McIntyre (chair of the European Herbal & Traditional Medicine Practitioners Association). I was pleased to get the chance to debate directly with him, because he has been misrpresenting the evidence for years. See, for example, Some truly appalling reporting of science by the BBC. and Government lends credibility to quacks and charlatans. I was able, at last, to ask him directly, which herb had the best evidence for its efficacy. He repeatedly refused to answer: “I’m not going to get into detail”. Eventually he resorted to the argument that herbalists treat people not diseases. I pointed out that the MHRA-approved labels list all sorts of diseases. No response. He then misquotes Sackett, who did NOT say that experience was as good as RCTs.
McIntyre goes on to misrepresent the BMJ Clinical Evidence paper which, he says, shows that 46% of all treatments are not proven to be effective. It is hard to be believe that McIntyre is really unaware that a large proportion of those that were not shown to be effective are CAM treatments, herbal medicine and the like. Professor John Garrow has pointed this out (see, also Healthwatch). Either he doesn’t read the literature or he deliberately misrepresents it.
Then a caller came in to swear that Chinese Medicine had cured his prostate problem and his wife’s hair. Of course he hadn’t any idea of how is prostate would have progressed if he hadn’t taken the Chinese medicine. Luckily for him, he didn’t have prostate cancer (the people who take Chinese medicine for cancer are probably dead so they can’t appear on the radio). These people are difficult to deal with without appearing rude, by saying they are gullible and deceived. I tried. Interestingly McIntyre did not leap to the defence of Chinese herbs.
I hate to be forced to return to the world’s most boring delusion, homeopathy. It is boring because the battle to inform people how daft it is has been almost won. Now not a single Bachelors degree in homeopathy appears in UCAS, compared with at least five in 2007. But the battle is not quite won with the UK Government. This post is not so much about homeopathy as about the failures of the Government and the MHRA.
The Medicines and Health Regulatory Authority (MHRA), has just launched yet another consultation and I have felt obliged to waste an entire Sunday writing a response to it, I can’t imagine that any scientist would disagree much with what I have written, but most of them have far better ways to spend their time than bothering about the lunatic fringes of medicine. No doubt most of the responses will come from people who make money from homeopathy, Not just the homeopaths on the High Street, but also the very rich companies like Boiron and Weleda who make enormous profits from selling pills that contain nothing but a bit of sugar.
The documents
The consultation concerns what should be done, about homeopathy in the wake of the scarifying report of the House of Commons Select Committee [get pdf], and the governments response to that report [get pdf].
The MHRA’s request for consultation is here. Download the consultation document. You can download my full response [get pdf], Please write your own response and send it to andreafarmer@mhra.gsi.gov.uk before February 17th. Feel free to plagiarise anything you find here.
Another good response is from Healthwatch, [download pdf]
And an excellent response by Prof John C. McLachlan [download pdf].
Now I’ll filll in some of the background and outline why I think the MHRA still hasn’t understood.
The Medicines Act 1968 and PLRs
The Medicines Act (1968) was passed in the wake of the thalidomide disaster. It required evidence that medicines work and that they are safe. It was not possible to check all existing medicines by the time the Act was implemented in 1971, so, as a temporary measure, many medicines, including homeopathic stuff, were give a "public licence of right" (PLR). Forty years later they have mostly vanished. But not for homeopathy. The PLR is the licence that allows homeopaths to break all the rules. They still exist.
MHRA cocked it up in 2006
The story starts with the National Regulation Scheme for homeopathic junk that was introduced by the MHRA in 2006. This allowed, for the first time, indications to be put on the labels of the bottles of sugar pills. There were howls of outrage from just about every scientific organisation (the medical establishment was, as usual, more pusillanimous, with some honourable exceptions). The history is related here in the following posts.
The MHRA breaks its founding principle: it is an intellectual disgrace
The Royal Society speaks out on CAM
Learned Societies speak out against CAM, and the MHRA
The MHRA loses the plot: it allows mislabelling of Arnica gel
House of Lords slams homeopathy and the MHRA
MHRA admits herbal medicines unproven
The Science and Technology Select Committee report
This was an admirable effort, It extracted, with some difficulty, admissions from Boots’ professional standards director that the sold pills while knowing that they didn’t work. It also squeezed out of the then Health Minister, Mike O’Brien an admission that they don’t work, Less surprisingly, the head of the MHRA agreed that they don’t work. So it is unanimous (apart, of course, from those who make money from selling things that don’t work).
If you want to know more about Boots’ Professional standards, take a look at Mis-education at Boots the Chemist, or The Vitamin B scam. Don’t trust Boots, or Boots reaches new level of dishonesty with CoQ10 promotion, to name but a few. The oral sessions of the committee were notable for the squirming evasiveness of most of the answers to simple questions. An account can be found in Comedy gold in parliament and tragedy from Prince of Wales: editorial in British Medical Journal
The Government’s response to the report was mostly as truly pathetic bit of official waffle, like those letters you get when you write to your Member of Parliament. But it did contain one good thing."In order for the public to make informed choices, it is therefore vitally important that the scientific evidence base for homeopathy is clearly explained and available." (though even that statement is attributed to John Beddington, the Government’s Chief Scientific advisor, rather than something the Government thinks essential).
"“The MHRA will review the labelling requirements under the NRS to ensure that these deliver clarity as to the status of products and their composition."
The proposals in the MHRA Consultation document’
There are a couple of good things in the proposals. The MHRA proposes to end PLRs (decades overdue, but nonetheless welcome).
The MHRA proposes to stop ‘regulating’ (ho ho) “Bach Flower Remedies” as medicines (but seems happy to classify them as food Supplements, another weasel description to evade sensible regulation). That’s sensible because they aren’t medicines. Homeopathic pills most certainly aren’t medicines either but the MHRA seems to have difficulty grasping that, and wants to treat them quite differently from “Flower remedies”
More honest labelling was about the only sensible thing recommended by the Government’s response. On this topic the MHRA proposals verge on the laughable
At present the labelling allowed under the NRS includes
“A homeopathic medicinal product used within the homeopathic tradition for the symptomatic relief of ….”
It is proposed to change this to
“A homeopathic medicinal product licensed only on the basis of safety, quality and use within the homeopathic tradition”
“A homeopathic medicinal product used within the homeopathic tradition for the symptomatic relief of……”
Spot the difference!
The is utterly inadequate. In fact it verges on the pathetic (and on the dishonest). Here is an extract from my full response.
"Sad to say these proposals to remedy the labelling problem are wholly inadequate. They are almost as deceptive as the originals. These labels don‘t come anywhere near to fulfilling the requirement in the government‘s response which said
In order for the public to make informed choices, it is therefore vitally important that the scientific evidence base for homeopathy is clearly explained and available
Why, oh why, cannot the MHRA bring itself to simply tell the truth? It seems to be so stifled by some perversion of political correctness that it is unable to do what it must know is right.
Nothing indicates more clearly the ludicrous state of the NRS than the label approved for Arnica 30C pills.
The approved label says
"ACTIVE INGREDIENT
Each pill contains 30C Arnica Montana
Also contains: lactose and sucrose"
The MHRA must decide whether or not it believes Avogadro‘s number or not.
How many people in the general public realise the ―Each pill contains 30C Arnica Montana‖ means that the ―pills contain no Arnica whatsoever‖? The very mention of the words ―active ingredient‖ will suggest to most people that there is an active ingredient when there is not. This wording alone is both dishonest and deceptive.
The rest of the approved label consists largely of make-believe too.
"If you are pregnant or breastfeeding consult your doctor before use"
What is your doctor meant to advise you about the dangers of taking a few mg of sugar when you are pregnant?
"If you take too much of the product (overdose) speak to a doctor / pharmacist and take this label with you,."
Unless the MHRA has disavowed Avogadro‘s number, an overdose is impossible. To allow a label like this makes the MHRA a laughing stock
https://www.dcscience.net/wp-admin/edit-tags.php?taxonomy=category
Labels should tell the truth in plain language. For example they should say
This product contains no Arnica
There is no evidence that it works for any condition, other than as a placebo
Some comments on regulation of magic medicine
Governments like to regulate things. They should have regulated the banks a bit more. The problem arises when you try to regulate things that are myths. Like homeopathy.
Andy Lewis has recently written a superb account of the problems on his Quackometer blog, When the Regulator Believes in Fairies, Who Protects the Public?
The government appears to believe that "training" will solve all the problems. Training people to believe things that aren’t true can never solve problems. On the contrary, it creates problems. Organisations like the Complementary and Natural Health Care Council (CNHC)do nothing to protect the public, They endanger the public (see Why the CNHC can’t succeed). Their excuse for rejecting complaints that members were making false claims was not to deny that the claims were false, but to say that it didn’t matter because that is what they had been trained to say. That is make-believe regulation.
Follow-up
.This is Andy Lewis’s version of an honest label. It looks quite accurate to me.

27 January 2011
News today makes one despair of the morality of governments. Remember those obviously fraudulent bomb detectors, no more than a dowsing rod? Although they are now the subject of a fraud investigation, they are still being sold. The government has banned their export to Iraq and Afghanistan, but NOT to anywhere else, This suggests not only that the government is (or at least was) quite happy to believe in dowsing. It also implies that even when they realise that it’s fraud they take the view that that business is far more important than even the most basic morality. No doubt they will allow fraudulent labelling of medicines in order to protect the homeopathic industry
Does politics have to be quite so disgusting?
28 January 2011. An excellent post on a similar topic is that referred to in a comment below. The MHRA and the non-regulation of homeopathy explains the European background better that I have done.
11 February 2011. Here is a characteristically beautiful response to the consultation by Prof John C. McLachlan, who has allowed me to post it here [download pdf].
This is another short interruption in the epic self-destruction of chiropractors. In a sense it is more serious. One expects quacks to advocate quackery. What you don’t expect is that the National Institute of Clinical Excellence (NICE) will endorse it. Neither do you expect the Medicines and Healthcare products Regulatory Agency (MHRA) to betray its mandate to make sure that medicines work.
The saga of the NICE low back pain guidance has been the subject of a deluge of criticism, It seems doubtful that the guidance can survive, not least because of its absurd endorsement of chiropractic, at a time when chiropractic is undergoing self-immolation as a consequence of the persecution of Simon Singh by the British Chiropractic Association (see here, and here, and here, and here and thousands of other sites).
The other betrayal has come to the for after the MHRA approved highly misleading labelling of a homeopathic preparation. At the time,
in 2006, when the principle was approved by the MHRA, just about every scientific organisation, even the Royal Society, condemned the action. What was discouraging that the clinical organisations all stayed silent. It is still a mystery why the MHRA made this enormous mistake, Some said that European regulations required it, but that is quite untrue, as Les Rose has shown. It appears to have been the result of a pusillanimous MHRA bowing to pressure from a deeply unscientific Department of Health (a letter from Caroline Flint at the time borders on the surreal).
On 20 May 2009, the British Medical Journal printed an article Drugs agency grants its first licence to homoeopathic product by Deborah Cohen (available free). The comments were mostly highly critical of the MHRA. The BMJ asked, as it does from time to time, for my comment to be converted to a letter
for the print edition. That isn’t freely available, so here it is.
|
Published 9 June 2009, doi:10.1136/bmj.b2333 LettersHomoeopathic product licenceMHRA label seems to be illegalThe strap line for the Medicines and Healthcare products Regulatory Agency (MHRA) is “We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe.” Yet the MHRA has made mockery of its own aims by ignoring the bit about “ensuring that medicines work” and allowing Arnica 30C pills to be labelled: “a homoeopathic medicinal product used within the homoeopathic tradition for the symptomatic relief of sprains, muscular aches, and bruising or swelling after contusions.”1 This label should be illegal anyway because the pills contain no trace of the ingredient on the label, but this deceit has been allowed through a legal loophole for a long time now. If you sold strawberry jam that contained not a trace of strawberry you’d be in trouble. But I can see no legal loophole that allows the manufacturers of Arnica 30C to evade the provisions of the Consumer Protection from Unfair Trading Regulations 2008. One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction, or malformations.” The consumer protection laws apply to the way that “the average consumer” will interpret the label. The average consumer is unlikely to know that “used within the homoeopathic tradition” is a form of weasel words that actually means “there isn’t a jot of evidence that the medicine works.” Since there is not the slightest evidence that Arnica 30C pills provide symptomatic relief of sprains, etc, the labelling that the MHRA has approved seems to be illegal. The MHRA is not selling anything itself, so I presume that it won’t find itself in court, but anyone who follows its advice could well do so. Cite this as: BMJ 2009;338:b2333 David Colquhoun, research professor1 University College London, London WC1E 6BT Competing interests: None declared. References |
It is, I suppose, just a sign of the chaos that reigns in the multiple agencies and quangos responsible for ‘regulation’ that one arm of government proposes action that a different branch would consider illegal. That is an inevitable consequence of trying to regulate something without first deciding whether it is nonsense or not. The Department of Health appears to be quite incapable of grasping this simple and obvious fact.
Follow-up
Health: best treatments. The Guardian seems to the be picking up BMJ stories and ran this one.
First the MHRA lets down the public by allowing deceptive labelling of sugar pills (see here, and this this blog). Now it is the turn of NICE to betray its own principles.
The National Institute for Health and Clinical Excellence (NICE) describes its job thus
“NICE is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health.”
Its Guidance document on Low Back Pain will be published on Wednesday 27 May 2009, but the newspapers have already started to comment, presumably on the assumption that it will have changed little from the Draft Guidance of September 2008. These comments may have to be changed as soon as the final version becomes available.
The draft guidance, though mostly sensible, has two recommendations that I believe to be wrong and dangerous. The recommendations include (page 7) these three.
- Consider offering a course of manual therapy including spinal manipulation of up to 9 sessions over up to 12 weeks.
- Consider offering a course of acupuncture needling comprising up to 10 sessions over a period of up to 12 weeks.
- Consider offering a structured exercise programme tailored to the individual.
All three of this options are accompanied by a footnote that reads thus.
“A choice of any of these therapies may be offered, taking into account patient preference.”
On the face if it, this might seem quite reasonable. All three choices seem to be about as effective (or ineffective) as each other, so why not let patients choose between them?
Actually there are very good reasons, but NICE does not seem to have thought about them. In the past I have had a high opinion of NICE but it seems that even they are now getting bogged down in the morass of political correctness and officialdom that is the curse of the Department of Health. It is yet another example of DC’s rule number one.
Never trust anyone who uses the word ‘stakeholder’.
They do use it, often.
So what is so wrong?
For a start, I take it that the reference to “spinal manipulation” in the first recommendation is a rather cowardly allusion to chiropractic. Why not say so, if that’s whar you mean? Chiropractic is mentioned in the rest of the report but the word doesn’t seem to occur in the recommendations. Is NICE perhaps nervous that it would reduce the credibility of the report if the word chiropractic were said out loud?
Well, they have a point, I suppose. It would.
That aside, here’s what’s wrong.
The Evidence
I take as my premise that the evidence says that no manipulative therapy has any great advantage over the others. They are all more or less equally effective. Perhaps I should say, more or less equally ineffective, because anyone who claims to have the answer to low back pain is clearly deluded (and I should know: nobody has fixed mine yet). So for effectiveness there are no good grounds to choose between exercise, physiotherapy, acupuncture or chiropractic. There is, though, an enormous cultural difference. Acupuncture and chiropractic are firmly in the realm of alternative medicine. They both invoke all sorts of new-age nonsense for which there isn’t the slightest good evidence. That may not poison your body, but it certainly poisons your mind.
Acupuncturists talk about about “Qi”, “meridians”, “energy flows”. The fact that “sham” and “real” acupuncture consistently come out indistinguishable is surely all the evidence one needs to dismiss such nonsense. Indeed there is a small group of medical acupuncturists who do dismiss it. Most don’t. As always in irrational subjects, acupuncture is riven by internecine strife between groups who differ in the extent of their mystical tendencies,
Chiropractors talk of “subluxations”, an entirely imaginary phenomenon (but a cause of much unnecessary exposure to X-rays). Many talk of quasi-religious things like “innate energy”. And Chiropractic is even more riven by competing factions than acupuncture. See, for example, Chiropractic wars Part 3: internecine conflict.
The bait and switch trick
This is the basic trick used by ‘alternative therapists’ to gain respectability.
There is a superb essay on it by the excellent Yale neurologist Steven Novella: The Bait and Switch of Unscientific Medicine. The trick is to offer some limited and reasonable treatment (like back manipulation for low back pain). This, it seems, is sufficient to satisfy NICE. But then, once you are in the showroom, you can be exposed to all sorts of other nonsense about “subluxations” or “Qi”. Still worse, you will also be exposed to the claims of many chiropractors and acupuncturists to be able to cure all manner of conditions other than back pain. But don’t even dare to suggest that manipulation of the spine is not a cure for colic or asthma or you may find yourself sued for defamation. The shameful legal action of the British Chiropractic Association against Simon Singh (follow it here) led to an addition to DC’s Patients’ Guide to Magic Medicine.
(In the face of such tragic behaviour, one has to be able to laugh).
Libel: A very expensive remedy, to be used only when you have no evidence. Appeals to alternative practitioners because truth is irrelevant.
NICE seems to have fallen for the bait and switch trick, hook line and sinker.
The neglected consequences
Once again, we see the consequences of paying insufficient attention to the Dilemmas of Alternative Medicine.
The lying dilemma
If acupuncture is recommended we will have acupuncturists telling patients about utterly imaginary things like “Qi” and “meridians”. And we will have chiropractors telling them about subluxations and innate energy. It is my opinion that these things are simply make-believe (and that is also the view of a minority of acupuncturist and chiropractors). That means that you have to decide whether the supposed benefits of the manipulation are sufficient to counterbalance the deception of patients.
Some people might think that it was worth it (though not me). What is unforgivable is not to consider even the question. The NICE guidance says not a word about this dilemma. Why not?
The training dilemma
The training dilemma is even more serious. Once some form of alternative medicine has successfully worked the Bait and Switch trick and gained a toehold in the NHS, there will be an army of box-ticking HR zombies employed to ensure that they have been properly trained in “subluxations” or “Qi”. There will be quangos set up to issue National Occupational Standards in “subluxations” or “Qi”. Skills for Health will issue “competences” in “subluxations” or “Qi” (actually they already do). There will be courses set up to teach about “subluxations” or “Qi”, some even in ‘universities’ (there already are).
The respectability problem
But worst of all, it will become possible for aupuncturists and chiropractors to claim that they now have official government endorsement from a prestigious evidence-based organisation like NICE for “subluxations” or “Qi”. Of course this isn’t true. In fact the words “subluxations” or “Qi” are not even mentioned in the draft report. That is the root of the problem. They should have been. But omitting stuff like that is how the Bait and Switch trick works.
Alternative medicine advocates crave, above all, respectability and acceptance. It is sad that NICE seems to have given them more credibility and acceptance without having considered properly the secondary consequences of doing so,
How did this failure of NICE happen?
It seems to have been a combination of political correctness, failure to consider secondary consequences, and excessive influence of the people who stand to make money from the acceptance of alternative medicine.
Take, for example, the opinion of the British Pain Society. This organisation encompasses not just doctors. It
includes “doctors, nurses, physiotherapists, scientists, psychologists, occupational therapists and other healthcare professionals actively engaged in the diagnosis and treatment of pain and in pain research for the benefit of patients”. Nevertheless, their response to the draft guidelines pointed out that the manipulative therapies as a whole were over-represented.
|
Manipulation The guidelines assess 9 large groups of interventions of which manual therapies are only one part. The full GDG members panel of 13 individuals included two proponents of spinal manipulation/mobilisation (P Dixon and S Vogel). In addition, the chair of the panel (M Underwood) is the lead author of the UKBEAM trial on which the positive recommendation for |
It seems that the Pain Society were quite right.
LBC 97.3 Breakfast Show (25 May 2009) had a quick discussion on acupuncture (play mp3 file). After I had my say, the other side was put by Rosey Grandage. She has (among other jobs) a private acupuncture practice so she is not quite as unbiassed as me). As usual, she misrepresents the evidence by failing to distinguish between blind and non-blind studies. She also misrepresented what I said by implying that I was advocating drugs. That was not my point and I did not mention drugs (they, like all treatments, have pretty limited effectiveness, and they have side effects too). She said “there is very good evidence to show they (‘Qi’ and ‘meridians’] exist”. That is simply untrue.
There can’t be a better demonstration of the consequences of falling for bait and switch than the defence mounted by Rosey Grandage. NICE may not mention “Qi” and “meridians”; but the people they want to allow into the NHS have no such compunctions.
I first came across Rosey Grandage when I discovered her contribution to the Open University/BBC course K221. That has been dealt with elsewhere. A lot more information about acupuncture has appeared since then. She doesn’t seem to have noticed it. Has she not seen the Nordic Cochrane Centre report? Nor read Barker Bausell, or Singh & Ernst? Has she any interest in evidence that might reduce her income? Probably not.
Where to find out more
An excellent review of chiropractic can be found at the Layscience site. It was written by the indefatigable ‘Blue Wode’ who has provided enormous amounts of information at the admirable ebm-first site (I am authorised to reveal that ‘Blue Wode’ is the author of that site). There you will also find much fascinating information about both acupuncture and about chiropractic.
I’m grateful to ‘Blue Wode’ for some of the references used here.
Follow-up
I’m perfectly happy to think of alternative medicine as being a voluntary, self-imposed tax on the gullible (to paraphrase Goldacre again). But only as long as its practitioners do no harm and only as long as they obey the law of the land. Only too often, though, they do neither.
When I talk about law, I don’t mean lawsuits for defamation. Defamation suits are what homeopaths and chiropractors like to use to silence critics. heaven knows, I’ve becomes accustomed to being defamed by people who are, in my view. fraudsters, but lawsuits are not the way to deal with it.
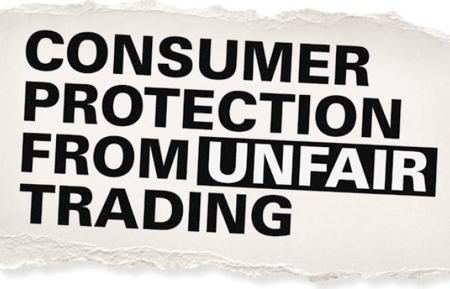
I’m talking about the Trading Standards laws Everyone has to obey them, and in May 2008 the law changed in a way that puts the whole health fraud industry in jeopardy.
The gist of the matter is that it is now illegal to claim that a product will benefit your health if you can’t produce evidence to justify the claim.
I’m not a lawyer, but with the help of two lawyers and a trading standards officer I’ve attempted a summary. The machinery for enforcing the law does not yet work well, but when it does, there should be some very interesting cases.
The obvious targets are homeopaths who claim to cure malaria and AIDS, and traditional Chinese Medicine people who claim to cure cancer.
But there are some less obvious targets for prosecution too. Here is a selection of possibilities to savour..
- Universities such as Westminster, Central Lancashire and the rest, which promote the spreading of false health claims
- Hospitals, like the Royal London Homeopathic Hospital, that treat patients with mistletoe and marigold paste. Can they produce any real evidence that they work?
- Edexcel, which sets examinations in alternative medicine (and charges for them)
- Ofsted and the QCA which validate these exams
- Skills for Health and a whole maze of other unelected and unaccountable quangos which offer “national occupational standards” in everything from distant healing to hot stone therapy, thereby giving official sanction to all manner of treatments for which no plausible evidence can be offered.
- The Prince of Wales Foundation for Integrated Health, which notoriously offers health advice for which it cannot produce good evidence
- Perhaps even the Department of Health itself, which notoriously referred to “psychic surgery” as a profession, and which has consistently refused to refer dubious therapies to NICE for assessment.
The law, insofar as I’ve understood it, is probably such that only the first three or four of these have sufficient commercial elements for there to be any chance of a successful prosecution. That is something that will eventually have to be argued in court.
But lecanardnoir points out in his comment below that The Prince of Wales is intending to sell herbal concoctions, so perhaps he could end up in court too.
The laws
We are talking about The Consumer Protection from Unfair Trading Regulations 2008. The regulations came into force on 26 May 2008. The full regulations can be seen here, or download pdf file. They can be seen also on the UK Statute Law Database.
The Office of Fair Trading, and Department for Business, Enterprise & Regulatory Reform (BERR) published Guidance on the Consumer Protection from Unfair Trading Regulations 2008 (pdf file),
Statement of consumer protection enforcement principles (pdf file), and
The Consumer Protection from Unfair Trading Regulations: a basic guide for business (pdf file).
Has The UK Quietly Outlawed “Alternative” Medicine?
On 26 September 2008, Mondaq Business Briefing published this article by a Glasgow lawyer, Douglas McLachlan. (Oddly enough, this article was reproduced on the National Center for Homeopathy web site.)
“Proponents of the myriad of forms of alternative medicine argue that it is in some way “outside science” or that “science doesn’t understand why it works”. Critical thinking scientists disagree. The best available scientific data shows that alternative medicine simply doesn’t work, they say: studies repeatedly show that the effect of some of these alternative medical therapies is indistinguishable from the well documented, but very strange “placebo effect” ”
“Enter The Consumer Protection from Unfair Trading Regulations 2008(the “Regulations”). The Regulations came into force on 26 May 2008 to surprisingly little fanfare, despite the fact they represent the most extensive modernisation and simplification of the consumer protection framework for 20 years.”
The Regulations prohibit unfair commercial practices between traders and consumers through five prohibitions:-
- General Prohibition on Unfair Commercial
Practices (Regulation 3)- Prohibition on Misleading Actions (Regulations 5)
- Prohibition on Misleading Omissions (Regulation 6)
- Prohibition on Aggressive Commercial Practices (Regulation 7)
- Prohibition on 31 Specific Commercial Practices that are in all Circumstances Unfair (Schedule 1). One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. The definition of “product” in the Regulations includes services, so it does appear that all forms medical products and treatments will be covered.
Just look at that!
| One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations” |
Section 5 is equally powerful, and also does not contain the contentious word “cure” (see note below)
Misleading actions
5.—(1) A commercial practice is a misleading action if it satisfies the conditions in either paragraph (2) or paragraph (3).
(2) A commercial practice satisfies the conditions of this paragraph—
(a) if it contains false information and is therefore untruthful in relation to any of the matters in paragraph (4) or if it or its overall presentation in any way deceives or is likely to deceive the average consumer in relation to any of the matters in that paragraph, even if the information is factually correct; and
(b) it causes or is likely to cause the average consumer to take a transactional decision he would not have taken otherwise.
These laws are very powerful in principle, But there are two complications in practice.
One complication concerns the extent to which the onus has been moved on to the seller to prove the claims are true, rather than the accuser having to prove they are false. That is a lot more favourable to the accuser than before, but it’s complicated.
The other complication concerns enforcement of the new laws, and at the moment that is bad.
Who has to prove what?
That is still not entirely clear. McLachlan says
“If we accept that mainstream evidence based medicine is in some way accepted by mainstream science, and alternative medicine bears the “alternative” qualifier simply because it is not supported by mainstream science, then where does that leave a trader who seeks to refute any allegation that his claim is false?
Of course it is always open to the trader to show that his the alternative therapy actually works, but the weight of scientific evidence is likely to be against him.”
On the other hand, I’m advised by a Trading Standards Officer that “He doesn’t have to refute anything! The prosecution have to prove the claims are false”. This has been confirmed by another Trading Standards Officer who said
“It is not clear (though it seems to be) what difference is implied between “cure” and “treat”, or what evidence is required to demonstrate that such a cure is false “beyond reasonable doubt” in court. The regulations do not provide that the maker of claims must show that the claims are true, or set a standard indicating how such a proof may be shown.”
The main defence against prosecution seems to be the “Due diligence defence”, in paragraph 17.
Due diligence defence
17. —(1) In any proceedings against a person for an offence under regulation 9, 10, 11 or 12 it is a defence for that person to prove—
(a) that the commission of the offence was due to—
(i) a mistake;
(ii) reliance on information supplied to him by another person;
(iii) the act or default of another person;
(iv) an accident; or
(v) another cause beyond his control; and
(b) that he took all reasonable precautions and exercised all due diligence to avoid the commission of such an offence by himself or any person under his control.
If “taking all reasonable precautions” includes being aware of the lack of any good evidence that what you are selling is effective, then this defence should not be much use for most quacks.
Douglas McLachlan has clarified, below, this difficult question
False claims for health benefits of foods
A separate bit of legislation, European regulation on nutrition and health claims made on food, ref 1924/2006, in Article 6, seems clearer in specifying that the seller has to prove any claims they make.
Article 6
Scientific substantiation for claims
1. Nutrition and health claims shall be based on and substantiated by generally accepted scientific evidence.
2. A food business operator making a nutrition or health claim shall justify the use of the claim.
3. The competent authorities of the Member States may request a food business operator or a person placing a product on the market to produce all relevant elements and data establishing compliance with this Regulation.
That clearly places the onus on the seller to provide evidence for claims that are made, rather than the complainant having to ‘prove’ that the claims are false.
On the problem of “health foods” the two bits of legislation seem to overlap. Both have been discussed in “Trading regulations and health foods“, an editorial in the BMJ by M. E. J. Lean (Professor of Human Nutrition in Glasgow).
“It is already illegal under food labelling regulations (1996) to claim that food products can treat or prevent disease. However, huge numbers of such claims are still made, particularly for obesity ”
“The new regulations provide good legislation to protect vulnerable consumers from misleading “health food” claims. They now need to be enforced proactively to help direct doctors and consumers towards safe, cost effective, and evidence based management of diseases.”
In fact the European Food Standards Agency (EFSA) seems to be doing a rather good job at imposing the rules. This, predictably, provoked howls of anguish from the food industry There is a synopsis here.
“Of eight assessed claims, EFSA’s Panel on Dietetic Products, Nutrition and Allergies (NDA) rejected seven for failing to demonstrate causality between consumption of specific nutrients or foods and intended health benefits. EFSA has subsequently issued opinions on about 30 claims with seven drawing positive opinions.”
“. . . EFSA in disgust threw out 120 dossiers supposedly in support of nutrients seeking addition to the FSD’s positive list.
If EFSA was bewildered by the lack of data in the dossiers, it needn’t hav been as industry freely admitted it had in many cases submitted such hollow documents to temporarily keep nutrients on-market.”
Or, on another industry site, “EFSA’s harsh health claim regime”
“By setting an unworkably high standard for claims substantiation, EFSA is threatening R&D not to mention health claims that have long been officially approved in many jurisdictions.”
Here, of course,”unworkably high standard” just means real genuine evidence. How dare they ask for that!
Enforcement of the law
Article 19 of the Unfair Trading regulations says
19. —(1) It shall be the duty of every enforcement authority to enforce these Regulations.
(2) Where the enforcement authority is a local weights and measures authority the duty referred to in paragraph (1) shall apply to the enforcement of these Regulations within the authority’s area.
Nevertheless, enforcement is undoubtedly a weak point at the moment. The UK is obliged to enforce these laws, but at the moment it is not doing so effectively.
A letter in the BMJ from Rose & Garrow describes two complaints under the legislation in which it appears that a Trading Standards office failed to enforce the law. They comment
” . . . member states are obliged not only to enact it as national legislation but to enforce it. The evidence that the government has provided adequate resources for enforcement, in the form of staff and their proper training, is not convincing. The media, and especially the internet, are replete with false claims about health care, and sick people need protection. All EU citizens have the right to complain to the EU Commission if their government fails to provide that protection.”
This is not a good start. A lawyer has pointed out to me
“that it can sometimes be very difficult to get Trading Standards or the OFT to take an interest in something that they don’t fully understand. I think that if it doesn’t immediately leap out at them as being false (e.g “these pills cure all forms of cancer”) then it’s going to be extremely difficult. To be fair, neither Trading Standards nor the OFT were ever intended to be medical regulators and they have limited resources available to them. The new Regulations are a useful new weapon in the fight against quackery, but they are no substitute for proper regulation.”
Trading Standards originated in Weights and Measures. It was their job to check that your pint of beer was really a pint. Now they are being expected to judge medical controversies. Either they will need more people and more training, or responsibility for enforcement of the law should be transferred to some more appropriate agency (though one hesitates to suggest the MHRA after their recent pathetic performance in this area).
Who can be prosecuted?
Any “trader”, a person or a company. There is no need to have actually bought anything, and no need to have suffered actual harm. In fact there is no need for there to be a complainant at all. Trading standards officers can act on their own. But there must be a commercial element. It’s unlikely that simply preaching nonsense would be sufficient to get you prosecuted, so the Prince of Wales is, sadly, probably safe.
Universities who teach that “Amethysts emit high Yin energy” make an interesting case. They charge fees and in return they are “falsely claiming that a product is able to cure illnesses”.
In my view they are behaving illegally, but we shan’t know until a university is taken to court. Watch this space.
The fact remains that the UK is obliged to enforce the law and presumably it will do so eventually. When it does, alternative medicine will have to change very radically. If it were prevented from making false claims, there would be very little of it left apart from tea and sympathy
Follow-up
New Zealand must have similar laws.
Just as I was about to post this I found that in New Zealand a
“couple who sold homeopathic remedies claiming to cure bird flu, herpes and Sars (severe acute respiratory syndrome) have been convicted of breaching the Fair Trading Act.”
They were ordered to pay fines and court costs totalling $23,400.
A clarification form Douglas McLachlan
On the difficult question of who must prove what, Douglas McLachlan, who wrote Has The UK Quietly Outlawed “Alternative” Medicine?, has kindly sent the following clarification.
“I would agree that it is still for the prosecution to prove that the trader committed the offence beyond a reasonable doubt, and that burden of proof is always on the prosecution at the outset, but I think if a trader makes a claim regarding his product and best scientific evidence available indicates that that claim is false, then it will be on the trader to substantiate the claim in order to defend himself. How will the trader do so? Perhaps the trader might call witness after witness in court to provide anecdotal evidence of their experiences, or “experts” that support their claim – in which case it will be for the prosecution to explain the scientific method to the Judge and to convince the Judge that its Study evidence is to be preferred.
Unfortunately, once human personalities get involved things could get clouded – I could imagine a small time seller of snake oil having serious difficulty, but a well funded homeopathy company engaging smart lawyers to quote flawed studies and lead anecdotal evidence to muddy the waters just enough for a Judge to give the trader the benefit of the doubt. That seems to be what happens in the wider public debate, so it’s easy to envisage it happening a courtroom.”
The “average consumer”.
(3) A commercial practice is unfair if—
(a) it contravenes the requirements of professional diligence; and
(b) it materially distorts or is likely to materially distort the economic behaviour of the average consumer with regard to the product.
It seems,therefore, that what matters is whether the “average consumer” would infer from what is said that a claim was being made to cure a disease. The legal view cited by Mojo (comment #2, below) is that expressions such as “can be used to treat” or “can help with” would be considered by the average consumer as implying successful treatment or cure.
The drugstore detox delusion. A nice analysis “detox” at .Science-based Pharmacy
Alfred Joseph Clark FRS held the established chair of Pharmacology at UCL from 1919 to 1926, when he left for Edinburgh. In the 1920s and 30s, Clark was a great pioneer in the application of quantitative physical ideas to pharmacology. As well as his classic scientific works, like The Mode of Action of Drugs on Cells (1933) he wrote, and felt strongly, about the fraud perpetrated on the public by patent medicine salesmen. In 1938 (while in Edinburgh) he published a slim volume called Patent Medicines. The parallels with today are astonishing.
Alfred Joseph Clark FRS (1885 – 1941) |
 |
I was lucky to be given a copy of this book by David Clark, A.J. Clark’s eldest son, who is now 88. I visited him in Cambridge on 17 September 2008, because he thought that, as holder of the A.J. Clark chair at UCL from 1985 to 2004, I’d be a good person to look after this and several other books from his father’s library. They would have gone to the Department of Pharmacology if we still had one, but that has been swept away by mindless administrators with little understanding of how to get good science.
Quotations from the book are in italic, and are interspersed with comments from me.
The book starts with a quotation from the House of Commons Select Committee report on Patent Medicines. The report was submitted to the House on 4 August 1914, so there is no need to explain why it had little effect. The report differs from recent ones in that it is not stifled by the sort of political correctness that makes politicians refer to fraudsters as “professions”.
The problem
“2.2 The situation, therefore, as regards the sale and advertisement of proprietary medicines and articles may be summarised as follows:
For all practical purposes British law is powerless to prevent any person from procuring any drug, or making any mixture, whether patent or without any therapeutical activity whatever (as long as it does not contain a scheduled poison), advertising it in any decent terms as a cure for any disease or ailment, recommending it by bogus testimonials and the invented opinions and facsimile signatures of fictitious physicians, and selling it under any name he chooses, on payment of a small stamp duty. For any price he can persuade a credulous public to pay.”
Select Committee on Patent Medicines. 1914
“The writer has endeavoured in the present article to analyse the reasons for the amazing immunity of patent medicines form all attempts to curb their activity, to estimate the results and to suggest the obvious measures of reform that are needed.”
| Clark, writing in 1938, was surprised that so little had changed since 1914. What would he have thought if he had known that now, almost 100 years after the 1914 report, the fraudsters are still getting away with it? Chapter 2 starts thus. |
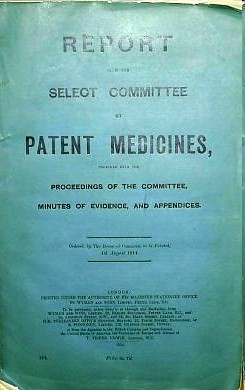 |
THE LAW
The Select Committee appointed by the House of Commons in 1914 ‘to consider and inquire into the question of the sale of Patent and Proprietary Medicines’ stated its opinion in 28 pages of terse and uncompromising invective. Its general conclusions were as follows:
That the trade in secret remedies constituted a grave and widespread public evil.
That the existing law was chaotic and had proved inoperative and that consequently the traffic in secret remedies was practically uncontrolled.
In particular it concluded ‘”that this is an intolerable state of things and that new legislation to deal with it, rather than merely the amendment of existing laws, is urgently needed in the public interest.”
The “widespread public evil”continues almost unabated, and rather than introduce sensible legislation to cope with it, the government has instead given a stamp of approval for quackery by introducing utterly ineffective voluntary “self-regulation”.
Another Bill to deal with patent medicines was introduced in 1931, without success, and finally in 1936, a Medical and Surgical Appliances (Advertisement) Bill was introduced. This Bill had a very limited scope. Its purpose was to alleviate some of the worst abuses of the quack medicine trade by prohibiting the advertisement of cures for certain diseases such as blindness, Bright’s disease [nephritis] , cancer, consumption [tuberculosis], epilepsy, fits, locomotor ataxy, fits, lupus or paralysis.
The agreement of many interests was secured for this measure. The president of the Advertising Association stated that the proposed Bill would not affect adversely any legitimate trade interest. Opposition to the Bill was, however, whipped up amongst psychic healers, anti-vivisectionists and other opponents of medicine and at the second reading in March 1936, the Bill was opposed and the House was counted out during the ensuing debate. The immediate reason for this fate was that the Bill came up for second reading on the day of the Grand National! This is only one example of the remarkable luck that has attended the patent medicine vendors.
(Page 14).
The “remarkable luck” of patent medicine vendors continues to this day, Although, in principle, advertisement of cures for venereal diseases was banned in 1917, and for cancer in 1939, it takes only a few minutes with Google to find that these laws are regularly flouted by quacks, In practice quacks get away with selling vitamin pills for AIDS, sugar pills for malaria and homeopathic pills for rabies, polio anthrax and just about anything else you can think of. Most of these advertisements are contrary to the published codes of ethics of the organisations to which the quack in question belongs but nothing ever happens.
Self-regulation simply does not work, and there is still no effective enforcement even of existing laws..
“It has already been stated that British law allows the advertiser of a secret remedy to tell any lie or make any claim that he fancies will sell his goods and the completeness of this licence is best illustrated by the consideration of a few specific points.
Advertisements for secret remedies very frequently contain a list of testimonials from medical men, which usually are in an anonymous form, stating that ………….. M.D., F.R.C.S., has found the remedy infallible. Occasionally, however, the name and address of a doctor is given and anyone unaware of the vagaries of English law would imagine that such use of a doctor’s name and professional reputation could not be made with impunity without his consent. In 1899, however, the Sallyco Mineral Water Company advertised that ‘Dr. Morgan Dochrill, physician to St. John’s Hospital, London and many of the leading physicians are presenting ‘Sallyco’ as an habitual drink. Dr. Dochrill says nothing has done his gout so much good.
Dr. Dochrill, whose name and title were correctly stated above, sued the company but failed in his case. ”
“The statement that the law does not prevent the recommending of a secret remedy by the use of bogus testimonials and facsimile signatures of fictitious physicians is obviously an understatement since it is doubtful how far it interferes with the use of bogus testimonials from real physicians.”
Dodgy testimonials are still a mainstay of dodgy salesman. One is reminded of the unauthorised citation of testimonials from Dr John Marks and Professor Jonathan Waxman by Patrick Holford to aid his sales of unnecessary vitamin supplements. There is more on this at Holfordwatch.
The man in the street knows that the merits of any article are usually exaggerated in advertisements and is in the habit of discounting a large proportion of such claims, but, outside the realm of secret remedies, the law is fairly strict as regards definite misstatements concerning goods offered for sale and hence the everyday experience of the man in the street does not prepare him for dealing with advertisements which are not merely exaggerations but plain straightforward lies from beginning to end.
Scientific training is undoubtedly a handicap in estimating popular gullibility as regards nostrums. One imagines that no one today would be willing to spend money on pills guaranteed to prevent earthquakes but yet the claims of many of the remedies offered appear equally absurd to anyone with an elementary
knowledge of physiology or even of chemistry. A study of the successes and failures suggests that success depends chiefly on not over-rating the public intelligence. (Page 34)
This may have changed a bit since A.J. Clark was writing in 1938. Now the main clients of quacks seem to be the well-off “worried-well”. But it remains as true as ever that “Scientific training is undoubtedly a handicap in estimating popular gullibility as regards nostrums.” In 2008, it is perhaps more a problem of Ben Goldacre’s dictum ““My basic hypothesis is this: the people who run the media are humanities graduates with little understanding of science, who wear their ignorance as a badge of honour.”
Clark refers (page 36) to a successful conviction for fraud in the USA in 1917. The subject was a widely advertised ‘get fat quick’ pill that contained lecithin, proteins and sugar. The BMA analysis (in 1912)
suggested that the cost of the ingredients in a box of 30 tablets sold for 4/6 was 1 1/4 d. [4/6 meant 4 shillings and six pence, or 22.5 pence since 1971, and 1 1/4 old pence, a penny farthing, is 0.52 new pence]. He comments thus.
The trial revealed many interesting facts. The formula was devised after a short consultation with the expert of one of the largest drug manufacturers in the U.S.A. This firm manufactured the tablets and sold them to the proprietary medicine company at about 3/- per 1000, whilst they were retailed to the public at the rate of £7 10s. per 1000. The firm is estimated to have made a profit of about $3,000,000.
These trials in the U.S.A. revealed the fact that in a considerable proportion of cases the ‘private formula’ department of the large and well known drug firm already mentioned had first provided the formula for the nostrum and subsequently had prepared it wholesale.
Nothing much has changed here either. The alternative medicine industry (and it is a very big industry) is fond of denouncing the evils of the pharmaceutical industry, and sadly, occasionally they are right. One of the less honest practices of the pharmaceutical industry (though one never mentioned by quacks) is buying heavily into alternative medicine. Goldacre points out
“there is little difference between the vitamin and pharmaceutical industries. Key players in both include multinationals such as Roche and Aventis; BioCare, the vitamin pill producer that media nutritionist Patrick Holford works for, is part-owned by Elder Pharmaceuticals.”
And then. of course, there is the deeply dishonest promotion by Boots the Chemists of homeopathic miseducation, of vitamins and of CoQ10 supplements.
The manner in which secret remedies can survive repeated exposure is shown by the following summary of the life history of a vendor of a consumption [tuberculosis] cure.
1904, 1906: Convicted of violating the law in South Africa.
1908: Exposed in British Medical Association report and also attacked by Truth.
1910: Sued by a widow. The judge stated: ‘I think this is an intentional and well-considered fraud. It is a scandalous thing that poor people should be imposed upon and led to part with their money, and to hope that those dear to them would be cured by those processes which were nothing but quack remedies and had not the slightest value of any kind.’
1914: A libel action against the British Medical Association was lost.
1915 The cure was introduced into the United States.
1919 The cure was sold in Canada.
1924 Articles by men with medical qualifications appeared in the Swiss medical journal boosting
the cure.
Secret remedies have a vitality that resembles that of the more noxious weeds and the examples mentioned suggest that nothing can do them any serious harm.
Most of the time, quacks get away with claims every bit as outrageous today. But Clark does give one example of a successful prosecution. It resulted from an exposé in the newspapers -wait for it -in the Daily Mail.
There is, however, one example which proves that a proprietary remedy can be squashed by exposure if this is accompanied by adequate publicity.
The preparation Yadil was introduced as an antiseptic and was at first advertised to the medical profession. The proprietor claimed that the remedy was not secret and that the active principle was ‘tri-methenal allylic carbide’. The drug acquired popularity in the influenza epidemic of 1918 and the proprietor became more and more ambitious in his therapeutic claims. The special virtue claimed for Yadil was that it would kill any harmful organism that had invaded the body. A more specific claim was that consumption in the first stage was cured with two or three pints whilst advanced cases might require a little more. Other advertisements suggested that it was a cure for most known diseases from cancer downwards.
These claims were supported by an extraordinarily intense advertising campaign. Most papers, and even magazines circulating amongst the wealthier classes, carried full page and even double page advertisements. The Daily Mail refused these advertisements and in 1924 published a three column article by Sir William Pope, professor of Chemistry in the University of Cambridge. He stated that
the name ‘tri-methenal allylic carbide’ was meaningless gibberish and was not the chemical definition of any known substance. He concluded that Yadil consisted of :
‘About one per cent of the chemical compound formaldehyde.
About four per cent of glycerine.
About ninety-five per cent of water and, lastly, a smell.
He calculated that the materials contained in a gallon cost about 1/6, whilst the mixture was sold at £4 10s. per gallon.
This exposure was completely successful and the matter is of historic interest in that it is the only example of the career of a proprietary medicine being arrested by the action of the Press.
Clark goes on to talk of the law of libel.
“On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”
The law of libel to this day remains a serious risk to freedom of speech of both individuals and the media. Its use by rogues to suppress fair comment is routine. My first encounter was when a couple of herbalists
threatened to sue UCL because I said that the term ‘blood cleanser’ is gobbledygook. The fact that the statement was obviously true didn’t deter them for a moment. The herbalists were bluffing no doubt, but they caused enough nuisance that I was asked to take my pages off UCL’s server. A week later I was invited back but by then I’d set up a much better blog and the publicity resulted in an enormous increase in readership, so the outcome was good for me (but bad for herbalists).
It was also good in the end for Andy Lewis when his immortal page “The gentle art of homoeopathic killing” (about the great malaria scandal) was suppressed. The Society of Homeopaths’ lawyers didn’t go for him personally but for his ISP who gave in shamefully and removed the page. As a result the missing page reappeared in dozens of web sites round the world and shot to the top in a Google search.
Chiropractors are perhaps the group most likely to try to suppress contrary opinions by law not argument. The only lawyers’ letter that has been sent to me personally, alleged defamation in an editorial that I wrote for the New Zealand Medical Journal. That was a little scary, but the journal stuck up for its right to speak and the threat went away after chiropractors were allowed right of reply (but we got the last word).
Simon Singh, one of the best science communicators we have, has not been so lucky. He is going to have to defend in court an action brought by the British Chiropractic Association because of innocent opinions expressed in the Guardian.
Chapter 6 is about “The harm done by patent medicines”. It starts thus.
“The trade in secret remedies obviously represents a ridiculous waste of money but some may argue that, since we are a free country and it pleases people to waste their money in this particular way, there is no call for any legislative interference. The trade in quack medicines cannot, however, be regarded as a harmless one. The Poisons Acts fortunately prevent the sale of a large number of dangerous drugs, but there are numerous other ways in which injury can be produced by these remedies.”
The most serious harm, he thought, resulted from self-medication, and he doesn’t mince his words.
“The most serious objection to quack medicines is however that their advertisements encourage self-medication as a substitute for adequate treatment and they probably do more harm in this than in any other manner.
The nature of the problem can best be illustrated by considering a simple example such as diabetes. In this case no actual cure is known to medicine but, on the other hand, if a patient is treated adequately by insulin combined with appropriate diet, he can be maintained in practically normal health, in spite of his disability, for an indefinite period. The expectation of life of the majority of intelligent diabetics, who make no mistakes in their regime, is not much less than that of normal persons. The regime is both irksome and unpleasant, but anyone who persuades diabetics to abandon it, is committing manslaughter as certainly as if he fired a machine gun into a crowded street.
As regards serious chronic disease the influence of secret remedies may be said to range from murderous to merely harmful.
‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous, since they are likely to cause the death of anyone who is unfortunate enough to believe in their efficacy and thus delay adequate treatment until too late.
The phrase “‘Cures for consumption, cancer and diabetes may fairly be classed as murderous” made Clark himself the victim of suppression of freedom of speech by lawyers. His son, David Clark, wrote of his father in “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3)
“Although tolerant of many human foibles, A. J. had always disapproved fiercely of quacks, particularly the charlatans who sold fraudulent medicines. During his visits to London he met Raymond Postgate, then a crusading left wing journalist, who persuaded A.J. to write a pamphlet which was published in an ephemeral series called ‘Fact‘ in March 1938. It was a lively polemical piece. . To A.J.’s surprise and dismay he was sued for libel by a notorious
rogue who peddled a quack cure for for tuberculosis. This man said that A.J.’s remarks (such as “‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”) were libellous and would damage his business. A.J. was determined to fight, and he and Trixie decided to put their savings at stake if necessary. The B.M.A. and the Medical Defence Union agreed to support him and they all went to lawyers. He was shocked when they advised him that he would be bound to lose for he had damaged the man’s livelihood! Finally, after much heart searching, he made an apology, saying that he had not meant that particular man’s nostrum”
Talk about déjà vu!
On page 68 there is another very familiar story. It could have been written today.
“The fact that the public is acquiring more knowledge of health matters and is becoming more suspicious of the cruder forms of lies is also helping to weed out the worst types of patent medicine advertisements. For example, in 1751 a bottle of oil was advertised as a cure for scurvy, leprosy and consumption but today such claims would not be effective in promoting the sale of a remedy. The modern advertiser would probably claim that the oil was rich in all the vitamins and the elements essential for life and would confine his claims to a statement that it would alleviate all minor forms of physical or mental ill-health.
The average patent medicine advertised today makes plausible rather than absurd claims and in general the advertisements have changed to conform with a change in the level of the public’s knowledge.
It is somewhat misleading, however, to speak of this as an improvement, since the law has not altered and hence the change only means that the public is being swindled in a somewhat more skilful manner.
The ideal method of obtaining an adequate vitamin supply is to select a diet containing an abundant supply of fresh foods, but unfortunately the populace is accustomed to live very largely on preserved or partially purified food stuffs and such processes usually remove most of the vitamins.”
The first part of the passage above is reminiscent of something that A.J Clark wrote in the BMJ in 1927. Nowadays it is almost unquotable and I was told by a journal editor that it was unacceptable even with asterisks. That seems to me a bit silly. Words had different connotations in 1927.
“The less intelligent revert to the oldest form of belief and seek someone who will make strong magic for them and defeat the evil spirits by some potent charm. This is the feeling to which the quack appeals; he claims to be above the laws of science and to possess some charm for defeating disease of any variety.
The nature of the charm changes with the growth of education. A naked n****r howling to the beat of a tom-tom does not impress a European, and most modern Europeans would be either amused or disgusted by the Black mass that was popular in the seventeenth century. Today some travesty of physical science appears to be the most popular form of incantation.”
A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927
Apart from some of the vocabulary, what better description could one have of the tendency of homeopaths to harp on meaninglessly about quantum theory or the “scienciness” and “referenciness” of
modern books on nutritional therapy?
So has anything changed?
Thus far, the outcome might be thought gloomy. Judging by Clark’s account, remarkably little has changed since 1938, or even since 1914. The libel law in the UK is as bad now as it was then. Recently the United Nations Human Rights Committee said UK laws block matters of public interest and encourage libel tourism (report here, see also here). It is unfit for a free society and it should be changed.
But there are positive sides too. Firstly the advent of scientific bloggers has begun to have some real influence. People are no longer reliant on journalists to interpret (or, often, misinterpret) results for them. They can now get real experts and links to original sources. Just one of these, Ben Goldacre’s badscience.net, and his weekly column in the Guardian has worked wonders in educating the public and improving journalism. Young people can, and do, contribute to the debate because they can blog anonymously if they are frightened that their employer might object.
Perhaps still more important, the law changed this year. Now, at last, it may be possible to prosecute successfully those who make fraudulent health claims. Sad to say, this was not an initiative of the UK government, which remains as devoted as ever to supporting quacks. Remember that, quite shamefully, the only reason given by the Medicines and Health Regulatory Authority (MHRA) gave for allowing false labelling of homeopathic pills was to support the “homeopathic industry”. They suggested (falsely) that the EU required them to take this irresponsible step, which was condemned by just about every scientific organisation. But the new unfair trading regulations did come from the EU. After almost 100 years since the 1914 report, we have at last some decent legislation. Let’s hope it’s enforced.
Postcript
The back cover of the series of ‘Fact‘ books in which A.J. Clark’s article appeared is reproduced below, simply because of the historical portrait of the 1930s that it gives.
Follow-up
This post got a lot of hits from Ben Goldacre’s miniblog which read
- Prof David Colquhoun gets into a time machine and meets himself
A truly classic DC post.
Thanks, Ben.