I’m bored stiff with that barmiest of all the widespread forms of alternative medicine, homeopathy. It is clearly heading back to where it was in 1960, a small lunatic fringe of medicine. Nevertheless it’s worth looking at a recent development.
A paper has appeared by that arch defender of all things alternative, George Lewith.
The paper in question is “Homeopathy has clinical benefits in rheumatoid arthritis patients that are attributable to the
consultation process but not the homeopathic remedy: a randomized controlled clinical trial”, Sarah Brien, Laurie Lachance, Phil Prescott, Clare McDermott and George Lewith. [read it here]. It was published in Rheumatology.
Conclusion. Homeopathic consultations but not homeopathic remedies are associated with clinically relevant benefits for patients with active but relatively stable RA.
So yet another case where the homeopathic pills turn out the same as placebos, Hardly surprising since the pills are the same as the placebos, but it’s always good to hear it from someone whose private practice sells homeopathy for money.
The conclusion isn’t actually very novel, because Fisher & Scott (2001) had already found nine years ago that homeopathy was ineffective in reducing the symptoms if joint inflammation in RA. That is Peter Fisher, the Queens’ homeopathic physician, and Clinical Director of the Royal Hospital for Integrated Medicine (recently renamed to remove ‘homeopathy’ from its title). That paper ends with the remarkable statement [download the paper]
- "Over these years we have come to believe that conventional RCTs [randomised controlled trials] are unlikely to capture the possible benefits of homeopathy . . . . It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response."
That seemed to me at the time to amount to an admission that it was all ‘placebo effect’, though Fisher continues to deny that this is the case.
"Homeopathy has clinical benefits in rheumatoid arthritis patients" -the title says. But does it?
In fact this is mere spin. What the paper actually shows is that an empathetic consultation has some benefit (and even this is inconsistent). This is hardly surprising, but there is really not the slightest reason to suppose that the benefit, such as it is, has anything whatsoever to do with homeopathy.
Homeopathy, non-specific effects and good medicine is the title of an excellent editorial, in the same issue of Rheumatology, by Edzard Ernst. He points out that "The recognition of the therapeutic value of an empathetic consultation is by no means a new insight". Any therapy that provides only non-specific effects is unacceptable. Any good doctor provides that and, when it exists, real effective treatments too.
Lewith’s private clinic

The Centre for Complementary and Integrated Medicine is run by Drs Nick Avery and George Lewith. It is always a bit galling to real scientists, who often work 60 hours a week or more to get results, that people like Lewith get a professorial salary (in his case from the University of Southampton) but still have time to make more money by doing another job at the same time.
Avery is a homeopath. I wonder whether we can now look forward to the web site being changed in the near future so that there is a clear statement that the pills have no effect?
There is, at least, now no longer any mention of the Vega test on Lewith’s site. That is a test for food allergy that has been shown again and again to be fraudulent. The Environmental medicine page is brief, and avoids making any claims at all. It now contains the somewhat coy statement
“Specific food avoidance regimes are a controversial area and one in which there may be conflict between conventionally trained allergists and CAM practitioners.”
However the page about fibromyalgia still mentions homeopathy favourably. And it still fails to refer to my reanalysis of one of the positive trials which revealed a simple statistical mistake.
The front page of their web site boasts that "Dr George Lewith is now one of The Lifestyle 50!". " The Times, in an article on September 6th 2008, included George Lewith in The Lifestyle 50, this newspaper’s listing of the “top 50 people who influence the way we eat, exercise and think about ourselves”. Dr Lewith is included in the Alternatives category". It doesn’t mention that this is an honour he shares with such medical luminaries as Gillian ("I’m not a doctor") McKeith, Jennifer Ariston and the Pope,
But let’s end this on a happier note. There is one thing that I agree with wholeheartedly. Lewith says
"The use of bottled water seems to me to be a multi-billion pound industry, based on some of the cleverest marketing that I have ever encountered. There is absolutely no evidence that bottled water is any safer, better, or more “energising” than the water you get from the tap."
No connection of course with the multi-million pound industry of selling homeopathic water by clever marketing.
Some limitations of the paper by Brien et al.
Like any good trial, this one defined in advance a primary and secondary outcome.
The primary outcome was ACR20. which means the propertion of patients that showed an improvement of at least 20% of the number of tender and swollen joint counts and 20% improvement in 3 of the 5 remaining ACR core set measures (see Felsen 1995). Although it isn’t stressed in the paper, there was no detectable difference between consultation vs no consultation for this primary outcome.
The secondary outcome was 28-joint DAS (DAS-28), tender and swollen joint count, disease severity, pain, weekly patient
and physician GA and pain, and inflammatory markers (see, for example, Stucki. 1996). It was only on this outcome that an effect was seen between consultation and no consultation. The "effect size" (standardized mean score differences, adjusted for baseline differences) was an improvement of 0.7 in DAS-28 score, which runs on a scale from 0 – 10. Although this improvement is probably real (statistically significant), it is barely bigger than improvement of 0.6 which is said to be the smallest change that is clinically significant (Stucki. 1996).
Not only is the improvement by the consultation small in clinical terms. It is also rather inconsistent. for example Table 6 shows that the consultation seemded to result in a detectable effect on swollen joint count, but not on tender joint count. Neither was there any significant effect of the consultation on the response to “considering all the ways your arthritis affects you, please make a vertical line to show how well you are now”. There appeared to be an improvement on “negative mood score”, but not on “positive mood score”. Effects of the consultation on pain scores was marginal at best.
It seems to me that the conclusion that the consultation process helps patients, though not entirely implausible, gets marginal support from this study. It may be real, but if so it isn’t a large effect.
Like most alternative medicine advocates, the authors of this paper make the mistake of confusing caring and curing. Caring is good if there is nothing else that can be done (as is only too often the case). But what patients really want is cures and they’ll never get that from an empathetic consultation.
The problem of Human Resources
What does all this mean for alternative medicine on the NHS? Nobody denies the desirability of empathy. In fact it is now talked about so much that there is a danger that scientific medical education will be marginalised. My own experience of the NHS is that most doctors are quite good at empathy, without any need to resort to hocus pocus like homeopathy and all the myriad forms of mythical medicine.
It must be said that Drs Avery and Lewith have had proper medical training. Their views on alternative medicine seem bizarre to me, but at least they should do no great harm. Sadly, the same can’t be said for the majority of homeopaths who have no medical training and who continue to andanger the public by recommending sugar pills for anything from malaria to Dengue fever. People like that have no place in the NHS. Indeed some are in jail.
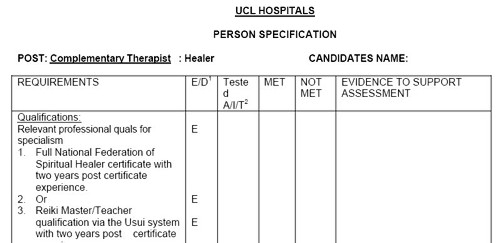
Not long ago, I was invited to tour the oncology wards at UCL hospital with their chief spiritual healer, Angie Buxton-King. Although in her private practice she offers some pretty bizarre services like healing humans and animals at a distance, I had the impression that on the wards she did a pretty good job holding hands with people who were nervous about injections and chatting to people in for their third lot of chemotherapy. I asked if she would object to being called a "supportive health care worker" rather than a spiritual healer. Somewhat reluctantly she said that she wouldn’t mind that. But it can’t be done because of the absurd box-ticking mentality of HR departments. There is no job-description for someone who holds hands with patients, and no formal qualifications. On the other hand, if you are sufficiently brainless, you can tick a box for a healer. Once again I wish that HR departments would not hinder academic integrity.
Follow-up
Steven Novella, at Science-Based medicine, has also written about this paper.


Interesting that you should mention Dr Nick Avery, George Lewith’s colleague, because in the past Dr Avery has been the Consultant Homeopath to Boots the Chemist. One wonders what Dr Avery might have to say to Boots now regarding its selling of homeopathy remedies in the absence of a personalised consultation.
http://forums.randi.org/showpost.php?p=1511328&postcount=22
It needn’t even be a homoeopathic consultation; any “conventional” intervention will invoke the placebo effect just as well, according to a systematic review published in Homeopathy earlier this year (Nuhn T, Lüdtke R, Geraedts M. Placebo effect sizes in homeopathic compared to conventional drugs – a systematic review of randomised controlled trials. Homeopathy. 2010 Jan;99(1):76-82), which concluded that “[p]lacebo effects in RCTs on classical homeopathy did not appear to be larger than placebo effects in conventional medicine.”
The real medicine might even have a real effect to add to the placebo effect.
@Mojo
Thanks for that reference, which I missed. It’s just as one would expect but nice to have it shown anyway.
\Full National Federation of Spiritual Healer Certificate with two years post certificate experience\
Seriously?
@lizhk
Oh yes, entirely serious. That;s part of the “person specification” form that was produced by “Human Resources” at UCLH. That’s what happens you allow people with no knowledge of science or medicine to gain too much influence.
Given that there has to be some way of assessing someone’s quality as a “supportive/compassionate healthcare worker”, how would you suggest it is done?
@hamletsghost
I think the answer is quite easy. The matter of appointments should be taken out of the hands of HR and given to the person who’ll be employing them. Then they will be judged by someone who knows what the job entails. That person should have the power also to end the job after a probationary period if they don’t perform, without having to spend a year filling in forms.
The increase in the number, and the power, of HR people is quite a recent phenomenon and it has caused a decrease in quality and an increase in bureaucracy. Like the QAA it was doubtless done with good intentions but it has failed.
If I was a homeopath what would I do if I was confronted by all the negative publicity emanating from blogs such as this? And the prediction of conventional homeopathy’s demise? Well Darwin’s Laws apply here too……. my technique would evolve.
First I would incorporate a bit of psychotherapy into the treatment regime. It’s possible to measure the amount of arsenic in a C30 homeopathic medicine (zero) but much more difficult to analyse, decode and measure all the parameters involved in a consultation. I would tell potential patients of the efficacy of my potions ordered online (healing at a distance) but would stress that when combined with a consultation with a healer, such as myself, the chances of a cure (and a healthy injection of cash into my bank account) would be greatly enhanced.
I would be sufficiently emboldened in this brazen approach by the rank stupidity of my fellow man and not just ordinary folk but intelligent people (creatives) who make programmes for channel 4. Like the lady who dreamt her horse would die and when she went out the next day it was dead. Then she dreamt that she too would die but she went to a Shaman (an ex-banker inevitably) who undid the dream and she lives to tell the tale, With rich numpties like this at hand the possibilities are endless.
She also consulted a psychoanalyst but that’s another story
“Well Darwin’s Laws apply here too”
… so you have a breeding population of techniques, have you?
What would it take to get the NHS to sponsor little old ladies with tea and bikkies to sit in the waiting rooms of GPs and having nice, long chats with the ill?
OMG have I been infected by the ‘Meme’ meme from reading Chapter 11 of ‘The Selfish Gene’? Damn that guy Dawkins.
[…] This post was mentioned on Twitter by Blue Wode and Alan Henness, Fernando Frias. Fernando Frias said: RT @Blue_Wode: Here's an idea: Replace CAM with little old ladies in GPs' waiting rooms http://bit.ly/baXrKg #winwinsolutions X-DD […]
Excellent point on memes, CrewsControl, though I don’t believe Darwin read very much Dawkins.
Laws according to Darwin: “These laws, taken in the largest sense, being Growth with Reproduction; Inheritance which is almost implied by reproduction; Variability from the indirect and direct action of the external conditions of life, and from use and disuse; a Ratio of Increase so high as to lead to a Struggle for Life, and as a consequence to Natural Selection, entailing Divergence of Character and the Extinction of less-improved forms.”
Crews Control:
An excellent summation of the equivalence of worth of homeopaths & psychoanalysts, who are similarly also bogus promoters of expensive unsupported “therapies”, but sans the added cost of succussion & water bills. Perhaps that makes the pompous psychoanalists even more dilute than the pompous homeopaths?
Crews Control & others:
I’ve long been trying to popularize the term
(or “stealth talking therapy”) as a realistic description of what the homeopaths are selling. Of course, they are not trained in psychotherapy (for whatever you believe the training is worth), but talking therapy is what they actually provide. Retired homeopathic doctor Anthony Campbell (essentially Peter Fisher’s predecessor) makes this point very clearly in his book about homeopathy.
Great paper but sorry, can’t resist, is Jennifer Ariston the women who is always going on and on?
[…] Dr Lewith was in the news again recently when he published a paper that showed (yet again) that homeopathic pills work no better than placebo. No surprise there of course. The paper has been described here, in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). […]
[…] sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes […]
[…] This all predates the advent of Jeremy Hunt (and known defender of homeopathy) as health minister. But the sympathies of some DH people are made obvious by the presence on the DH web site of an article "Personal health budgets: A new way of accessing complementary therapies?". This astonishing piece confirms the worst fears that quacks will see personal health budgets as a commercial opportunity to peddle their wares. The article is my Jim Rogers of Lincoln University. What his paper does not mention is Rogers’ conflict of interest. He’s a homeopath, and he has a paper in the International Journal of High Dilution Research (yes, there is a journal for every form of make-believe). You can download a reprint of this paper. It advocates more research into homeopathic provings, something that even George Lewith seems to have given up on. […]