Department of Health
On 23rd May 2009, the Financial Times magazine published a six-page cover story about pseudo-scientific degrees by Richard Tomkins. The online version has the text but doesn’t do justice to the prominence that it was given. The print version had a much better title too, The Retreat from Reason. This article, which was some time in gestation, appeared shortly afte the last degree in homeopathy in the UK closed its doors. So perhaps it should have been called The Return of Reason. What’s interesting is that it has become commonplace for the mainstream newspapers to print articles like this and to dump some of their whackier lifestyle articles.
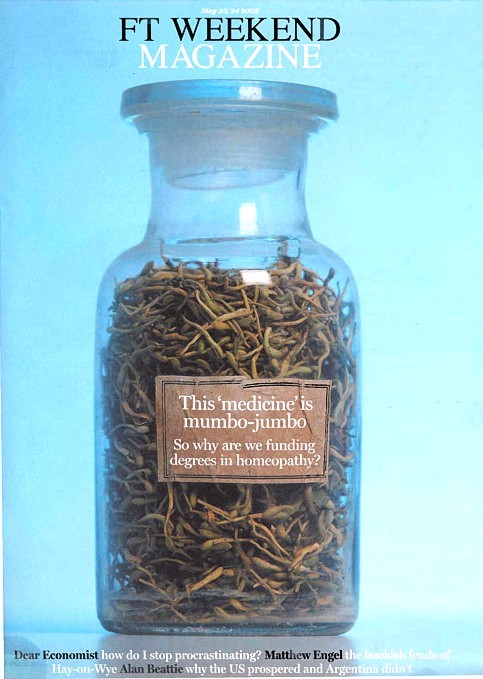
The print version had a much better title too, The Retreat from Reason, with a two-page spread..
They published the entire ‘Patients’ Guide to Magic Medicine‘ as a sidebar on page 4.
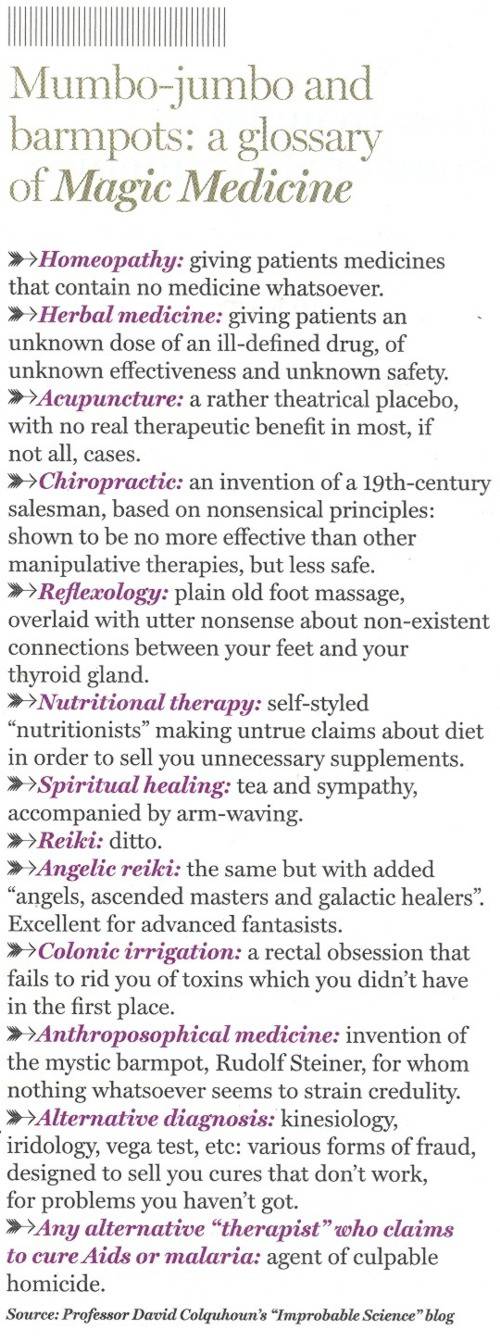
To these has now been added, inspired by Jack of Kent,
Libel: A very expensive remedy, to be used only when you have no evidence. Appeals to alternative practitioners because truth is irrelevant
One part of the article that I particularly enjoyed is this.
George Lewith, professor of health research at the University of Southampton’s medical school, is also director of the Centre for Complementary and Integrated Medicine, a private practice with clinics in Southampton and London’s West End, so it is no surprise that he is ready to speak out in support of complementary therapies. In fact, Southampton University – a member of the elite Russell Group – does not offer degree courses in complementary medicine, but Lewith defends the idea of offering them in principle, on the basis that, done properly, they produce better-trained practitioners. “Without the new universities’ involvement we might be faced with the quackery we saw in the 1940s and 1950s, when these people were outside medicine and were practising in an alternative fringe culture,” he says.
Sorry George, you are still an “alternative fringe culture”. And universities are realising that, and shutting down courses all over the place.
A response in the Finacial Times
The FT published one response in its letter column, A bilious attack on complementary medicine.
“Sir, Like many journalists, Richard Tomkins has been over-impressed by the scientific credentials of Professors David Colquhoun and Edzard Ernst as they carry on their absurdly over-stated, arrogant and irresponsible campaign against complementary medicine (“The retreat of reason”, May 23)”
and then the trump card
“Absence of evidence is not evidence of absence”
That’s the line used by quacks again and again and again (see, for example, integrative baloney @ Yale). I guess they have never heard of type 1 and type 2 errors. But that is a bit technical for homeopaths, so put it more simply. There is a quite remarkable absence of evidence for tooth fairies. So they must exist. Get it?
The letter is from Allen Parrott of Yeovil. Could that be the Allen Parrott of the British Acupuncture Accreditation Board? If so he is “is an adult educationist who was Dean of Adult and Community Education at Yeovil College and a lecturer in the School of Education at Exeter University. As well as his work for the Board, he is currently working as an educational adviser for the Kent, Surrey and Sussex Deanery in the NHS.”. So no reason to worry about the standards of education in Yeovil, then.
| The Prince of Wales’ Foundation for Integrated Health (FiH) is a propaganda organisation that aims to persuade people, and politicians, that the Prince’s somewhat bizarre views about alternative medicine should form the basis of government health policy.
His attempts are often successful, but they are regarded by many people as being clearly unconstitutional. |
 |
The FiH’s 2009 AnnualConferen ce conference was held at The King’s Fund, London 13 – 14 May 2009. It was, as always, an almost totally one-sided affair devoted to misrepresentation of evidence and the promotion of magic medicine. But according to the FiH, at least, it was a great success. The opening speech by the Quacktitioner Royal can be read here. It has already been analysed by somebody who knows rather more about medicine than HRH. He concludes
“It is a shocking perversion of the real issues driven by one man; unelected, unqualified and utterly misguided”.
We are promised some movie clips of the meeting. They might even make a nice UK equivalent of “Integrative baloney @ Yale“.
This post is intended to provide some background information about the speakers at the symposium. But let’s start with what seems to me to be the real problem. The duplicitous use of the word “integrated” to mean two quite different things.
The problem of euphemisms: spin and obfuscation
One of the problems of meetings like this is the harm done by use of euphemisms. After looking at the programme, it becomes obvious that there is a rather ingenious bit of PR trickery going on. It confuses (purposely?) the many different definitions of the word “integrative” . One definition of “Integrative medicine” is this (my emphasis).
” . . . orienting the health care process to engage patients and caregivers in the full range of physical, psychological, social, preventive, and therapeutic factors known to be effective and necessary for the achievement of optimal health.”
That is a thoroughly admirable aim. And that, I imagine, is the sense in which several of the speakers (Marmot, Chantler etc) used the term. Of course the definition is rather too vague to be very helpful in practice, but nobody would dream of objecting to it.
But another definition of the same term ‘integrative medicine’ is as a PR-friendly synonym for ‘alternative medicine’, and that is clearly the sense in which it is used by the Prince of Wales’ Foundation for Integrated Health (FIH), as is immediately obvious from their web site.
The guide to the main therapies supports everything from homeopathy to chiropractic to naturopathy, in a totally uncritical way. Integrated service refers explicitly to integration of ‘complementary’ medicine, and that itself is largely a euphemism for alternative medicine. For example, the FIH’s guide to homeopathy says
“What is homeopathy commonly used for?
Homeopathy is most often used to treat chronic conditions such as asthma; eczema; arthritis; fatigue disorders like ME; headache and migraine; menstrual and menopausal problems; irritable bowel syndrome; Crohn’s disease; allergies; repeated ear, nose, throat and chest infections or urine infections; depression and anxiety.”
But there is not a word about the evidence, and perhaps that isn’t surprising because the evidence that it works in any of these conditions is essentially zero.
The FIH document Complementary Health Care: A Guide for Patients appears to have vanished from the web after its inaccuracy received a very bad press, e.g. in the Times, and also here. It is also interesting that the equally widely criticised Smallwood report (also sponsored by the Prince of Wales) seems to have vanished too).
The programme for the meeting can be seen here, for Day 1, and Day 2
Conference chair Dr Phil Hammond, GP, comedian and health service writer. Hammond asked the FIH if I could speak at the meeting to provide a bit of balance. Guess what? They didn’t want balance.
09:30 Opening session
Dr Michael Dixon OBE
09:30 Introduction: a new direction for The Prince’s Foundation for Integrated Health and new opportunities in integrated health and care. Dr Michael Dixon, Medical Director, FIH
Michael Dixon is devoted to just about every form of alternative medicine. As well as being medical director of the Prince’s Foundation he also runs the NHS Alliance. Despite its name, the NHS Alliance is nothing to do with the NHS and acts, among other things, as an advocate of alternative medicine on the NHS, about which it has published a lot.
Dr Dixon is also a GP at College Surgery, Cullompton, Devon, where his “integrated practice” includes dozens of alternative practitioners. They include not only disproven things like homeopathy and acupuncture, but also even more bizarre practitioners in ‘Thought Field Therapy‘ and ‘Frequencies of Brilliance‘.
To take only one of these, ‘Frequencies of Brilliance’ is bizarre beyond belief. One need only quote its founder and chief salesperson.
“Frequencies of Brilliance is a unique energy healing technique that involves the activation of energetic doorways on both the front and back of the body.”
“These doorways are opened through a series of light touches. This activation introduces high-level Frequencies into the emotional and physical bodies. It works within all the cells and with the entire nervous system which activates new areas of the brain.”
“Frequencies of Brilliance is a 4th /5th dimensional work. The process is that of activating doorways by lightly touching the body or working just above the body.”
“Each doorway holds the highest aspect of the human being and is complete in itself. This means that there is a perfect potential to be accessed and activated throughout the doorways in the body.”
Best of all, it can all be done at a distance (that must help sales a lot). One is reminded of the Skills for Health “competence” in distant healing (inserted on a government web site at the behest (you guessed it) of the Prince’s Foundation, as related here)
“The intent of a long distance Frequencies of Brilliance (FOB) session is to enable a practitioner to facilitate a session in one geographical location while the client is in another.
A practitioner of FOB that has successfully completed a Stage 5 Frequency workshop has the ability to create and hold a stable energetic space in order to work with a person that is not physically present in the same room.
The space that is consciously created in the Frequencies of Brilliance work is known as the “Gap”. It is a space of nonlinear time. It contains ”no time and no space” or respectively “all time and all space”. Within this “Gap” a clear transfer of the energies takes place and is transmitted to an individual at a time and location consciously intended. Since this dimensional space is in non-linear time the work can be performed and sent backward or forward in time as well as to any location.
The Frequencies of Brilliance work cuts through the limitations of our physical existence and allows us to experience ourselves in other dimensional spaces. Therefore people living in other geographic locations than a practitioner have an opportunity to receive and experience the work.
The awareness of this dimensional space is spoken about in many indigenous traditions, meditation practices, and in the world of quantum physics. It is referred to by other names such as the void, or vacuum space, etc.”
This is, of course, preposterous gobbledygook. It, and other things in Dr Dixon’s treatment guide, seem to be very curious things to impose on patients in the 21st century.
Latest news. The Mid-Devon Star announces yet more homeopathy in Dr Dixon’s Cullompton practice. This time it comes in the form of a clinic run from the Bristol Homeopathic Hospital. I guess they must be suffering from reduced commissioning like all the other homeopathic hospitals, but Dr Dixon seems to have come to their rescue. The connection seems to be with Bristol’s homeopathic consultant, Dr Elizabeth A Thompson. On 11 December 2007 I wrote to Dr Thompson, thus
|
In March 2006, a press release http://www.ubht.nhs.uk/press/view.asp?257 announced a randomised trial for homeopathic treatment of asthma in children. This was reported also on the BBC http://news.bbc.co.uk/1/hi/england/bristol/4971050.stm . I’d be very grateful if you could let me know when results from this trial will become available. Yours sincerely David Colquhoun |
The reply, dated 11 December 2007, was unsympathetic
|
I have just submitted the funders report today and we have set ourselves the deadline to publish two inter-related papers by March 1st 2007. Can I ask why you are asking and what authority you have to gain this information. I shall expect a reply to my questions, |
I answered this question politely on the same day but nevertheless my innocent enquiry drew forth a rather vitriolic complaint from Dr Thompson to the Provost of UCL (dated 14 December 2007). In this case, the Provost came up trumps. On 14 January 2008 he replied to Thompson: “I have looked at the email that you copied to me, and I must say that it seems an entirely proper and reasonable request. It is not clear to me why Professor Colquhoun should require some special authority to make such direct enquiries”. Dr Thompson seems to be very sensitive. We have yet to see the results of her trial in which I’m still interested.
Not surprisingly, Dr Dixon has had some severe criticism for his views, not least from the UK’s foremost expert on the evidence for efficacy, Prof Edzard Ernst. Accounts of this can be found in Pulse,
and on Andrew Lewis’s blog.
Dixon is now (in)famous in the USA too. The excellent Yale neurologist, Steven Novella, has written an analysis of his views on Science Based Medicine. He describes Dr. Michael Dixon as “A Pyromaniac In a Field of (Integrative) Straw Men”
Peter Hain
09:40 Politics and people: can integrated health and care take centre stage in 2009/2010? Rt Hon Peter Hain MP
It seems that Peter Hain was converted to alternative medicine when his first baby, Sam, was born with eczema. After (though possibly not because of) homeopathic treatment and a change in diet, the eczema got better. This caused Hain, while Northern Ireland Secretary to spend £200,000 of taxpayers’ money to set up a totally uninformative customer satisfaction survey, which is being touted elsewhere in this meeting as though it were evidence (see below). I have written about this episode before: see Peter Hain and Get Well UK: pseudoscience and privatisation in Northern Ireland.
I find it very sad that a hero of my youth (for his work in the anti-apartheid movement) should have sunk to promoting junk science, and even sadder that he does so at my expense.
There has been a report on Hain’s contribution in Wales Online.
09:55 Why does the Health Service need a new perspective on health and healing? Sir Cyril Chantler, Chair, King’s Fund, previous Dean, Guy’s Hospital and Great Ormond Street
Cyril Chantler is a distinguished medical administrator. He also likes to talk and we have discussed the quackery problem several times. He kindly sent me the slides that he used. Slide 18 says that in order to do some good we “need to demonstrate that the treatment is clinically effective and cost effective for NHS use”. That’s impeccable, but throughout the rest of the slides he talks of integrating with complementary” therapies, the effectiveness of which is either already disproved or simply not known.
I remain utterly baffled by the reluctance of some quite sensible people to grasp the nettle of deciding what works. Chantler fails to grasp the nettle, as does the Department of Health. Until they do so, I don’t see how they can be taken seriously.
10.05 Panel discussion
The Awards
10:20 Integrated Health Awards 2009 Introduction: a review of the short-listed applications
10:45 Presentations to the Award winners by the special guest speaker
11:00 Keynote address by special guest speaker
Getting integrated
Dr David Peters
12:00 Integration, long term disease and creating a sustainable NHS. Professor David Peters, Clinical Director and Professor of Integrated Healthcare, University of Westminster
I first met David Peters after Nature ran my article, Science Degrees without the Science. .One of the many media follow-ups of that article was on Material World (BBC Radio 4). This excellent science programme, presented by Quentin Cooper, had a discussion between me and David Peters ( listen to the mp3 file).
There was helpful intervention from Michael Marmot who had talked, in the first half of the programme, about his longitudinal population studies.
Marmot stressed the need for proper testing. In the case of
homeopathy and acupuncture, that proper testing has largely been done. The tests were failed.
The University of Westminster has, of course, gained considerable notoriety as the university that runs more degree programmes in anti-scientific forms of medicine than any other. Their lecture on vibrational medicine teaches students that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbances at all levels of being”. So far their vice-chancellor, Professor Geoffrey Petts, has declined to answer enquiries about whether he thinks such gobbledygook is appropriate for a BSc degree.
But he did set up an internal enquiry into the future of their alternative activities. Sadly that enquiry seems to have come to the nonsensical conclusion that the problem can be solved by injection of good science into the courses, as reported here and in the Guardian.
It seems obvious that if you inject good science into their BSc in homeopathy the subject will simply vanish in a puff of smoke.
In 2007, the University of Westminster did respond to earlier criticism in Times Higher Education, but their response seemed to me to serve only to dig themselves deeper into a hole.
Nevertheless, Westminster has now closed down its homeopathy degree (the last in the country to go) and there is intense internal discussion going on there. I have the impression that Dr Peters’ job is in danger. The revelation of more slides from their courses on homeopathy, naturopathy and Chinese herbal medicine shows that these courses are not only barmy, but also sometimes dangerous.
Professor Chris Fowler
12:10 Educating tomorrow’s integrated doctors. Professor Chris Fowler, Dean for Education, Barts and The London School of Medicine and Dentistry
I first came across Dr Fowler when I noticed him being praised for his teaching of alternative medicine to students at Barts and the London Medical School on the web site of the Prince’s Foundation. I wrote him a polite letter to ask if he really thought that the Prince of Wales was the right person to consult about the education of medical students. The response I got was, ahem, unsympathetic. But a little while later I noticed that two different Barts students had set up public blogs that criticised strongly the nonsense that was being inflicted on them.
At that point, I felt it was necessary to support the students who, it seemed to me, knew more about medical education than Professor Fowler. It didn’t take long to uncover the nonsense that was being inflicted on the students: read about it here.
There is a follow-up to this story here. Fortunately, Barts’ Director of Research, and, I’m told, the Warden of Barts, appear to agree with my view of the harm that this sort of thing can do to the reputation of Barts, so things may change soon,
Dame Donna Kinnair
12:30 Educating tomorrow’s integrated nurses.
Dame Donna Kinnair, Director of Nursing, Southwark PCT
As far as I can see, Donna Kinnair has no interest in alternative medicine. She is director of nursing at Southwark primary care trust and was an adviser to Lord Laming throughout his inquiry into the death of Victoria Climbié. I suspect that her interest is in integrating child care services (they need it, judging by the recent death of ‘Baby P’). Perhaps her presence shows the danger of using euphemisms like ‘integrated medicine’ when what you really mean is the introduction of unproven or disproved forms of medicine.
Michael Dooley
12:40 Integrating the care of women: an example of the new paradigm. Michael Dooley, Consultant Obstetrician and Gynecologist
DC’s rule 2. Never trust anyone who uses the word ‘paradigm’. It is a sure-fire sign of pseudoscience. In this case, the ‘new paradigm’ seems to be the introduction of disproven treatment. Dooley is a gynaecologist and Medical Director of the Poundbury Clinic. His clinic offers a whole range of unproven and disproved treatments. These include acupuncture as an aid to conception in IVF. This is not recommended by the Cochrane review, and one report suggests that it hinders conception rather than helps.
12.40 Discussion
13.00 – 14.00 Lunch and Exhibition
15.30 Tea
Boo Armstrong and Get Well UK
16.00 Integrated services in action: The Northern
Ireland experience: what has it shown us and what are its implications?
Boo Armstrong of Get Well UK with a team from the NI study
I expect that much will be made of this “study”, which, of course, tells you absolutely nothing whatsoever about the effectiveness of the alternative treatments that were used in it. This does not appear to be the view of Boo Armstrong, On the basis of the “study”, her company’s web site proclaims boldly
“Complementary Medicine Works
Get Well UK ran the first government-backed complementary therapy project in the UK, from February 2007 to February 2008″
This claim appears, prima facie, to breach the Unfair Trading Regulations of May 2008. The legality of the claim is, at the moment, being judged by a Trading Standards Officer. In any case, the “study” was not backed by the government as a whole, but just by Peter Hain’s office. It is not even clear that it had ethical approval.
The study consisted merely of asking people who had seen an alternative medicine practitioner whether they felt better or worse. There was no control group; no sort of comparison was made. It is surely obvious to the most naive person that a study like this cannot even tell you if the treatment has a placebo effect, never mind that it has any genuine effects of its own. To claim that it does so seems to be simply dishonest. There is no reason at all to think that the patients would not have got better anyway.
It is not only Get Well UK who misrepresent the evidence. The Prince’s
Foundation itself says
“Now a new, year long trial supported by the Northern Ireland health service has . . . demonstrated that integrating complementary and conventional medicine brings measurable benefits to patients’ health.”
That is simply not true. It is either dishonest or stupid. Don’t ask me which, I have no idea.
This study is no more informative than the infamous Spence (2005) ‘study’ of the same type, which seems to be the only thing that homeopaths can produce to support their case.
There is an excellent analysis of the Northern Ireland ‘study’ by Andy Lewis, The Northern Ireland NHS Alternative Medicine ‘Trial’. He explains patiently, yet again, what constitutes evidence and why studies like this are useless.
His analogy starts
” . . . the Apple Marketing Board approach the NHS and ask for £200,000 to do a study to show the truth behind the statement ‘An apple a day keeps the doctor away’. The Minister, being particularly fond of apples, agrees and the study begins.”
16.30 Social enterprise and whole systems integrated care. Dee Kyne, Sandwell PCT and a GP. Developing an integrated service in secondary care
Dee Kyne appears to be CEO of KeepmWell Ltd (a financial interest that is not mentioned).
Peter Mackereth, Clinical Lead, Supportive Services, Christie Hospital NHS Foundation Trust
I had some correspondence with Mackereth when the Times (7 Feb 2007) published a picture of the Prince of Wales inspecting an “anti-MRSA aromatherapy inhaler” in his department at the Christie. It turned out that the trial they were doing was not blind No result has been announced anyway, and on enquiry, I find that the trial has not even started yet. Surprising, then to find that the FIH is running the First Clinical Aromatherapy Conference at the Christie Hospital, What will there be to talk about?
Much of what they do at the Christie is straightforward massage, but they also promote the nonsensical principles of “reflexology” and acupuncture.
The former is untested. The latter is disproven.
Parallel Sessions
Developing a PCT funded musculoskeletal service Dr Roy Welford, Glastonbury Health Centre
Roy Welford is a Fellow of the Faculty of Homeopathy, and so promotes disproven therapies. The Glastonbury practice also advertises acupuncture (disproven), osteopathy and herbal medicine (largely untested so most of it consists of giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety).
Making the best of herbal self-prescription in integrated practice: key remedies and principles. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon
Simon Mills is a herbalist who now describes himself as a “phytotherapist” (it sounds posher, but the evidence, or lack of it, is not changed by the fancy name). Mills likes to say things like “there are herbs for heating and drying”, “hot and cold” remedies, and to use meaningless terms like “blood cleanser”, but he appears to be immune to the need for good evidence that herbs work before you give them to sick people. He says, at the end of a talk, “The hot and the cold remain the trade secret of traditional medicine”. And this is the 21st Century.
Practical ways in which complementary approaches can improve the treatment of cancer. Professor Jane Plant, Author of “Your life in your hands” and Chief Scientist, British Geological Society and Professor Karol Sikora, Medical Director, Cancer Partners UK
Jane Plant is a geologist who, through her own unfortunate encounter with breast cancer, became obsessed with the idea that a dairy-free diet cured her. Sadly there is no good evidence for that idea, according to the World Cancer Research Fund Report, led by Professor Sir Michael Marmot. No doubt her book on the subject sells well, but it could be held that it is irresponsible to hold out false hopes to desperate people. She is a supporter of the very dubious CancerActive organisation (also supported by Michael Dixon OBE –see above) as well as the notorious pill salesman, Patrick Holford (see also here).
Karol Sikora, formerly an oncologist at the Hammersmith Hospital, is now Dean of Medicine at the University of Buckingham (the UK’s only private university). He is also medical director at CancerPartners UK, a private cancer company.
He recently shot to fame when he appeared in a commercial in the USA sponsored by “Conservatives for Patients’ Rights”, to pour scorn on the NHS, and to act as an advocate for the USA’s present health system. A very curious performance. Very curious indeed.
His attitude to quackery is a mystery wrapped in an enigma. One was somewhat alarmed to see him sponsoring a course at what was, at first, called the British College of Integrated Medicine, and has now been renamed the Faculty of Integrated Medicine That grand title makes it sound like part of a university. It isn’t.

The alarm was as result of the alliance with Dr Rosy Daniel (who promotes an untested herbal conconction, Carctol, for ‘healing’ cancer) and Dr Mark Atkinson (a supplement salesman who has also promoted the Qlink pendant. The Qlink pendant is a simple and obvious fraud designed to exploit paranoia about WiFi killing you.
The first list of speakers on the proposed diploma in Integrated Medicine was an unholy alliance of outright quacks and commercial interests. It turned out that, although Karol Sikora is sponsoring the course, he knew nothing about the speakers. I did and when I pointed this out to Terence Kealey, vice-chancellor of Buckingham, he immediately removed Rosy Daniel from directing the Diploma. At the moment the course is being revamped entirely by Andrew Miles. There is hope that he’ll do a better job. It has not yet been validated by the University of Buckingham. Watch this space for developments.
Stop press It is reported in the Guardian that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear. More developments in the follow-up.
The role of happy chickens in healing: farms as producers of health as well as food – the Care Farm Initiative Jonathan Dover, Project Manager, Care Farming, West Midlands.
“Care farming is a partnership between farmers, participants and health & social care providers. It combines the care of the land with the care of people, reconnecting people with nature and their communities.”
Sounds lovely, I wonder how well it works?
What can the Brits learn from the Yanks when it comes to integrated health? Jack Lord, Chief Executive Humana Europe
It is worth noticing that the advisory board of Humana Europe includes Micheal Dixon OBE, a well known advocate of alternative medicine (see
above). Humana Europe is a private company, a wholly owned subsidiary of Humana Inc., a health benefits company with 11 million members and 22,000 employees and headquarters in Louisville, Kentucky. In 2005 it entered into a business partnership with Virgin Group. Humana was mentioned in the BBC Panorama programme “NHS for Sale”. The company later asked that it be pointed out that they provide commissioning services, not clinical services [Ed. well not yet anyway].
Humana’s document “Humana uses computer games to help people lead healthier lives” is decidedly bizarre. Hang on, it was only a moment ago that we were being told that computer games rewired your brain.
Day 2 Integrated health in action
09.00 Health, epidemics and the search for new solutions. Sir Michael Marmot, Professor of Epidemiology and Public Health, Royal Free and University College Medical School
It is a mystery to me that a distinguished epidemiologist should be willing to keep such dubious company. Sadly I don’t know what he said, but judging my his publications and his appearence on Natural World, I can’t imagine he’d have much time for homeopaths.
9.25 Improving health in the workplace. Dame Carol Black, National Director, Health and Work, Department of Health
This is not the first time that Dame Carol has been comtroversial.
9.45 Integrated health in focus: defeating obesity. Professor Chris Drinkwater, President, NHS Alliance.
The NHS Alliance was mentioned above. Enough said.
10.00 Integrated healthcare in focus: new approaches to managing asthma, eczema and allergy. Professor Stephen Holgate, Professor of Immunopharmacology, University of Southampton
10.15 Using the natural environment to increase activity. The Natural England Project: the results from year one. Dr William Bird and Ruth Tucker, Natural England.
10.30 Panel discussion
10.45 Coffee
Self help in action
11.10 Your health, your way: supporting self care through care planning and the use of personal budgets. Angela Hawley, Self Care Lead, Department of Health
11.25 NHS Life Check: providing the signposts to
integrated health. Roy Lambley, Project Director, NHS LifeCheck Programme
This programme was developed with the University of Westminster’s “Health and Well-being Network”. This group, with one exception, is separate from Westminster’s extensive alternative medicine branch (it’s mostly psychologists).
11.45 The agony and the ecstasy of helping patients to help themselves: tips for clinicians, practices and PCTs. Professor
Ruth Chambers, FIH Foundation Fellow.
11.55 Providing self help in practice: Department of Health Integrated Self Help Information Project. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon and Dr Sam Everington, GP, Bromley by Bow.
The Culm Valley Integrated Centre for health is part of the College Surgery Partnership, associated with Michael Dixon OBE (yes, again!).
Simon Mills is the herbalist who says “The hot and the cold remain the trade secret of traditional medicine” .
Sam Everington, in contrast, seems to be interested in ‘integration’ in the real sense of the word, rather than quackery.
Integrated health in action
How to make sense of the evidence on complementary approaches: what works? What might work? What doesn’t work?
Dr Hugh MacPherson, Senior Research Fellow in Health Sciences, York University and Dr Catherine Zollman, Bravewell Fellow
Hugh MacPherson‘s main interest is in acupuncture and he publishes in alternative medicine journals. Since the recent analysis in the BMJ from the Nordic Cochrane Centre (Madsen et al., 2009) it seems that acupuncture is finally dead. Even its placebo effect is too small to be useful. Catherine Zollman is a Bristol GP who is into homeopathy as well as acupuncture. She is closely connected with the Prince’s Foundation via the Bravewell Fellowship. That fellowship is funded by the Bravewell Collaboration, which is run by Christie Mack, wife of John Mack (‘Mack the Knife’), head of Morgan Stanley (amazingly, they still seem to have money). This is the group which, by sheer wealth, has persuaded so many otherwise respectable US universities to embrace every sort of quackery (see, for example, Integrative baloney @ Yale)
The funding of integrated services
14.15 How to get a PCT or practice- based commissioner to fund your integrated service. A PCT Chief Executive and a Practice-Based Commissioning lead.
14.30 How I succeeded: funding an integrated service. Dr John Ribchester, Whitstable
14.45 How we created an acupuncture service in St Albans and Harpenden PBC group. Mo Girach, Chief Executive, STAHCOM
Uhuh Acupunture again. Have these people never read Bausell’s
book? Have they not read the BMJ? Acupuncture is now ell-established to be based on fraudulent principles, and not even to have a worthwhile placeobo effect. STAHCOM seem to be more interested in money than in what works.
Dragon’s Den. Four pitchers lay out their stall for the commissioning dragons
And at this stage there is no prize for guessing that all four are devoted to trying to get funds for discredited treatments
- An acupuncture service for long-term pain. Mike Cummings Chair, Medical Acupuncture Association
- Manipulation for the treatment of back pain Simon Fielding, Founder Chairman of the General Osteopathic Council
- Nigel Clarke, Senior Partner, Learned Lion Partners Homeopathy for long term conditions
- Peter Fisher, Director, Royal Homeopathic Hospital
Sadly it is not stated who the dragons are. One hopes they will be more interested in evidence than the supplicants.
Mike Cummings at least doesn’t believe the nonsense about meridians and Qi. It’s a pity he doesn’t look at the real evidence though.
You can read something about him and his journal at BMJ Group promotes acupuncture: pure greed.
Osteopathy sounds a bit more respectable than the others, but in fact it has never shaken off its cult-like origins. Still many osteopaths make absurd claims to cure all sorts of diseases. Offshoots of osteopathy like ‘cranial osteopathy’ are obvious nonsense. There is no reason to think that osteopathy is any better than any other manipulative therapy and it is clear that all manipulative therapies should be grouped into one.
Osteopathy and chiropractic provide the best ever examples of the folly of giving official government recognition to a branch of alternative medicine before the evidence is in.
Learned Lion Partners is a new one on me. It seems it is
part of Madsen Gornall Ashe Chambers (‘MGA Chambers’) “a grouping of top level, independent specialists who provide a broad range of management consultancy advice to the marketing community”. It’s a management consultant and marketing outfit. So don’t expect too much when it comes to truth and evidence. The company web site says nothing about alternative medicine, but only that Nigel Clarke
“. . . has very wide experience of public affairs issues and campaigns, having worked with clients in many sectors in Europe, North America and the Far East. He has particular expertise in financial, competition and healthcare issues. “
However, all is revealed when we see that he is a Trustee of the Prince’s Foundation where his entry says
“Nigel Clarke is senior partner of Learned Lion Partners. He is a director of Vidapulse Ltd, Really Easy Ltd, Newscounter Ltd and Advanced Transport Systems Ltd. He has worked on the interfaces of public policy for 25 years. He has been chair of the General Osteopathic Council since May 2001, having been a lay member since it was formed. He is now a member of the Council for Healthcare Regulatory Excellence”
The Council for Healthcare Regulatory Excellence is yet another quango that ticks boxes and fails absolutely to grasp the one important point, does it work?. I came across them at the Westminster Forum, and they seemed a pretty pathetic way to spend £2m per year.
Peter Fisher is the last supplicant to the Dragons. He is clinical director of the Royal London Homeopathic Hospital (RLHH), and Queen’s homeopathic physician, It was through him that I got an active interest in quackery. The TV programme QED asked me to check the statistics in a paper of his that claimed that homeopathy was good for fibrositis (there was an elementary mistake and no evidence for an effect). Peter Fisher is also remarkable because he agreed with me that BSc degrees in homeopathy were not justified (on TV –see the movie). And he condemned homeopaths who were caught out recommending their sugar pills for malaria. To that extent Fisher represents the saner end of the homeopathic spectrum. Nevertheless he still maintains that sugar pills work and have effects of their own, and tries to justify the ‘memory of water’ by making analogies with a memory stick or CD. This is so obviously silly that no more comment is needed.
Given Fisher’s sensible condemnation of the malaria fiasco, I was rather surprised to see that he appeared on the programme of a conference at the University of Middlesex, talking about “A Strategy To Research The Potential Of Homeopathy In Pandemic Flu”. The title of the conference was Developing Research Strategies in CAM. A colleague, after seeing the programme, thought it was more like “a right tossers’ ball”.
Much of the homeopathy has now vanished from the RLHH as a result of greatly reduced commissioning by PCTs (read about it in Fisher’s own words). And the last homeopathy degree in the UK has closed down. It seems an odd moment for the FIH to be pushing it so hard.
Follow-up
Stop press It is reported in the Guardian (22 May 2009) that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear, oh dear.
This fascinating fact seems to have been unearthed first by the admirable NHS Blog Doctor, in his post ‘Imperial College confirm that Karol Sikora does not work for them and does not speak on their behalf‘.
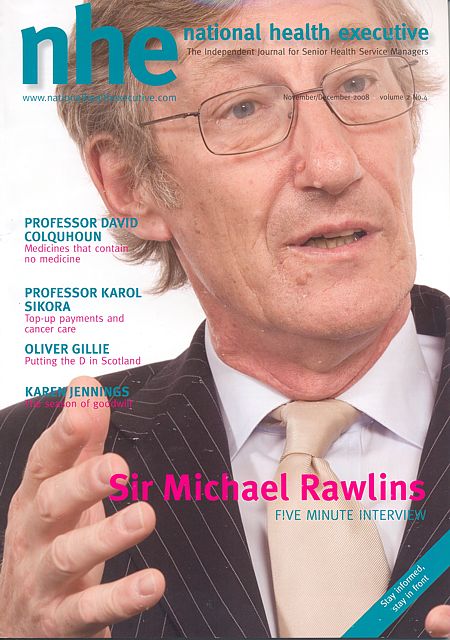
Recently I wrote a piece for the National Health Executive (“the Independent Journal for Senior Health Service Managers”), with the title Medicines that contain no medicine and other follies
In the interests of what journalists call balance (but might better be called equal time for the Flat Earth Society), an article appeared straight after mine, Integrating Homeopathy into Primary Care. It was by Rachel Roberts “Research consultant for the Society of Homeopaths”.
This defence was so appalling that I sent them a response (after first doing a bit of checking on its author). To my surprise, they published the response in full [download pdf of printed version]. Their title was

As always, the first step is to Google the author, to find out a bit more. It seems that Rachel Roberts runs a business Integrated Homeopathic Training. (a financial interest that was not mentioned in her article). She will sell you flash cards (‘Matmedcards’) for £70 (+£9 p&p) for 120 cards (yes, seriously). The card for Conium maculatum is remarkable. It says on the reverse side
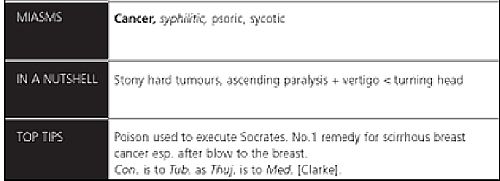
Yes, it says (my emphasis)
“The poison used to execute Socrates. No 1 remedy for scirrhous breast cancer. Esp after blow to the breast”
No doubt she would claim that the word “remedy” was a special weasel word of homeopaths that did not imply any therapeutic efficacy. But its use in this context seems to me to be cruel deception, even murderous. It also appears to breach the Cancer Act 1939, as well as the Unfair Trading laws.
I asked the Bristol Trading Standards Office, and got a reply remarkably quickly. It ended thus.
“. . . . the use of the card for “hemlock” as an example amounts to advice in connection with the treatment (of cancer)”. I will initially write to IHT and require that they remove this, and any other, reference to cancer treatment from their website.
When I checked again a couple of weeks later, the hemlock sample card had been been replaced by one about chamomile (it is described as the opium of homeopathy. Luckily the pills contain no opium (and no chamomile either) or that would be breaking another law. Bafflingly, it is not (yet) against the law to sell pills that contain no trace of the ingredient on the label, if they are labelled ‘homeopathic’.
Presumably the packs still contain a claim to cure cancer. And what is said in the privacy of the consulting room will never be known.
Political correctness is a curious thing. I felt slightly guilty when I reported this breach of the Cancer Act. It felt almost sneaky. The feeling didn’t last long though. We are talking about sick people here.
It isn’t hard to imagine a desperate woman suffering from cancer reading that Ms Roberts knows the “No 1 remedy for scirrhous breast cancer”. She might actually believe it. She might buy some hemlock pills that contain no hemlock (or anything else). She might die as a result. It is not a joke. It is, literally, deadly serious.
It is also deadly serious that the Department of Health and some NHS managers are so stifled by political correctness that they refer to homeopaths as “professionals” and pay them money.
Ms Roberts, in her article, is at pains to point out that
|
 |
Well it is already well known that the the Code of Ethics of the Society of Homeopaths is something of a joke. This is just one more example.
The Code of Ethics, para 72 says homeopaths have a legal obligation
“To avoid making claims (whether explicit or implied; orally or in writing) implying cure of any named disease.”
Like, perhaps, claiming to have the “No 1 remedy for scirrhous breast cancer”?
Obviously voluntary self-regulation isn’t worth the paper it’s written on.
You don’t need to go to her web site to find “claims . . . implying cure of any named disease”. In her article she says
“Conditions which responded well to homeopathy included childhood eczema and asthma, migraine, menopausal problems, inflammatory bowel disease, irritable bowel syndrome, arthritis, depression and chronic fatigue syndrome.”
No doubt they will say that the claim that asthma and migraine “responded well” to their sugar pills carries no suggestion that they can cure a named disease. And if you believe that, you’ll believe anything.
I have to say that I find Ms Robert’s article exceedingly puzzling. It comes with 29 references, so it looks, to use Goldacre’s word, ‘sciencey’. If you read the references, and more importantly, know about all the work that isn’t referred to, you see it is the very opposite of science. I see only two options.
Either it is deliberate deception designed to make money, or it shows, to a mind-boggling extent, an inability to understand what constitutes evidence.
The latter, more charitable, view is supported by the fact that Ms Roberts trots out, yet again, the infamous 2005 Spence paper, as though it constituted evidence for anything at all. In this paper 6544 patients at the Bristol Homeopathic Hospital were asked if the felt better after attending the out-patient department. Half of them reported that the felt ‘better’ or ‘much better’. Another 20% said they were ‘slightly better’ (but that is what you say to be nice to the doctor). The patients were not compared with any other group at all. What could be less surprising than that half of the relatively minor complaints that get referred for homeopathy get ‘better or much better’ on their own?
This sort of study can’t even tell you if homeopathic treatment has a placebo effect, never mind that it has a real effect of its own. It is a sign of the desperation of homeopaths that they keep citing this work.
Whatever the reason, the conclusion is clear. Never seek advice from someone who has a financial interest in the outcome. Ms Roberts makes her living from homeopathy. If she were to come to the same conclusion as the rest of the world, that it is a placebo and a fraud, her income would vanish. It is asking too much of anyone to do that.
| This is the mistake made time and time again by the Department of Health and by the NHS. The Pittilo report does the same thing The execrably bad assessment of evidence in that report is, one suspects, not unrelated to the fact that it was done entirely by people who would lose their jobs if they were to come to any conclusion other than their treatments work. |  |
At present , the regulation of alternative medicine is chaotic because the government and the dozen or so different quangos involved are trying to regulate while avoiding the single most important question – do the treatments work?
They should now grasp that nettle and refer the question to NICE.
Follow-up
I’m perfectly happy to think of alternative medicine as being a voluntary, self-imposed tax on the gullible (to paraphrase Goldacre again). But only as long as its practitioners do no harm and only as long as they obey the law of the land. Only too often, though, they do neither.
When I talk about law, I don’t mean lawsuits for defamation. Defamation suits are what homeopaths and chiropractors like to use to silence critics. heaven knows, I’ve becomes accustomed to being defamed by people who are, in my view. fraudsters, but lawsuits are not the way to deal with it.
I’m talking about the Trading Standards laws Everyone has to obey them, and in May 2008 the law changed in a way that puts the whole health fraud industry in jeopardy.
The gist of the matter is that it is now illegal to claim that a product will benefit your health if you can’t produce evidence to justify the claim.
I’m not a lawyer, but with the help of two lawyers and a trading standards officer I’ve attempted a summary. The machinery for enforcing the law does not yet work well, but when it does, there should be some very interesting cases.
The obvious targets are homeopaths who claim to cure malaria and AIDS, and traditional Chinese Medicine people who claim to cure cancer.
But there are some less obvious targets for prosecution too. Here is a selection of possibilities to savour..
- Universities such as Westminster, Central Lancashire and the rest, which promote the spreading of false health claims
- Hospitals, like the Royal London Homeopathic Hospital, that treat patients with mistletoe and marigold paste. Can they produce any real evidence that they work?
- Edexcel, which sets examinations in alternative medicine (and charges for them)
- Ofsted and the QCA which validate these exams
- Skills for Health and a whole maze of other unelected and unaccountable quangos which offer “national occupational standards” in everything from distant healing to hot stone therapy, thereby giving official sanction to all manner of treatments for which no plausible evidence can be offered.
- The Prince of Wales Foundation for Integrated Health, which notoriously offers health advice for which it cannot produce good evidence
- Perhaps even the Department of Health itself, which notoriously referred to “psychic surgery” as a profession, and which has consistently refused to refer dubious therapies to NICE for assessment.
The law, insofar as I’ve understood it, is probably such that only the first three or four of these have sufficient commercial elements for there to be any chance of a successful prosecution. That is something that will eventually have to be argued in court.
But lecanardnoir points out in his comment below that The Prince of Wales is intending to sell herbal concoctions, so perhaps he could end up in court too.
The laws
We are talking about The Consumer Protection from Unfair Trading Regulations 2008. The regulations came into force on 26 May 2008. The full regulations can be seen here, or download pdf file. They can be seen also on the UK Statute Law Database.
The Office of Fair Trading, and Department for Business, Enterprise & Regulatory Reform (BERR) published Guidance on the Consumer Protection from Unfair Trading Regulations 2008 (pdf file),
Statement of consumer protection enforcement principles (pdf file), and
The Consumer Protection from Unfair Trading Regulations: a basic guide for business (pdf file).
Has The UK Quietly Outlawed “Alternative” Medicine?
On 26 September 2008, Mondaq Business Briefing published this article by a Glasgow lawyer, Douglas McLachlan. (Oddly enough, this article was reproduced on the National Center for Homeopathy web site.)
“Proponents of the myriad of forms of alternative medicine argue that it is in some way “outside science” or that “science doesn’t understand why it works”. Critical thinking scientists disagree. The best available scientific data shows that alternative medicine simply doesn’t work, they say: studies repeatedly show that the effect of some of these alternative medical therapies is indistinguishable from the well documented, but very strange “placebo effect” ”
“Enter The Consumer Protection from Unfair Trading Regulations 2008(the “Regulations”). The Regulations came into force on 26 May 2008 to surprisingly little fanfare, despite the fact they represent the most extensive modernisation and simplification of the consumer protection framework for 20 years.”
The Regulations prohibit unfair commercial practices between traders and consumers through five prohibitions:-
- General Prohibition on Unfair Commercial
Practices (Regulation 3)- Prohibition on Misleading Actions (Regulations 5)
- Prohibition on Misleading Omissions (Regulation 6)
- Prohibition on Aggressive Commercial Practices (Regulation 7)
- Prohibition on 31 Specific Commercial Practices that are in all Circumstances Unfair (Schedule 1). One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”. The definition of “product” in the Regulations includes services, so it does appear that all forms medical products and treatments will be covered.
Just look at that!
| One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations” |
Section 5 is equally powerful, and also does not contain the contentious word “cure” (see note below)
Misleading actions
5.—(1) A commercial practice is a misleading action if it satisfies the conditions in either paragraph (2) or paragraph (3).
(2) A commercial practice satisfies the conditions of this paragraph—
(a) if it contains false information and is therefore untruthful in relation to any of the matters in paragraph (4) or if it or its overall presentation in any way deceives or is likely to deceive the average consumer in relation to any of the matters in that paragraph, even if the information is factually correct; and
(b) it causes or is likely to cause the average consumer to take a transactional decision he would not have taken otherwise.
These laws are very powerful in principle, But there are two complications in practice.
One complication concerns the extent to which the onus has been moved on to the seller to prove the claims are true, rather than the accuser having to prove they are false. That is a lot more favourable to the accuser than before, but it’s complicated.
The other complication concerns enforcement of the new laws, and at the moment that is bad.
Who has to prove what?
That is still not entirely clear. McLachlan says
“If we accept that mainstream evidence based medicine is in some way accepted by mainstream science, and alternative medicine bears the “alternative” qualifier simply because it is not supported by mainstream science, then where does that leave a trader who seeks to refute any allegation that his claim is false?
Of course it is always open to the trader to show that his the alternative therapy actually works, but the weight of scientific evidence is likely to be against him.”
On the other hand, I’m advised by a Trading Standards Officer that “He doesn’t have to refute anything! The prosecution have to prove the claims are false”. This has been confirmed by another Trading Standards Officer who said
“It is not clear (though it seems to be) what difference is implied between “cure” and “treat”, or what evidence is required to demonstrate that such a cure is false “beyond reasonable doubt” in court. The regulations do not provide that the maker of claims must show that the claims are true, or set a standard indicating how such a proof may be shown.”
The main defence against prosecution seems to be the “Due diligence defence”, in paragraph 17.
Due diligence defence
17. —(1) In any proceedings against a person for an offence under regulation 9, 10, 11 or 12 it is a defence for that person to prove—
(a) that the commission of the offence was due to—
(i) a mistake;
(ii) reliance on information supplied to him by another person;
(iii) the act or default of another person;
(iv) an accident; or
(v) another cause beyond his control; and
(b) that he took all reasonable precautions and exercised all due diligence to avoid the commission of such an offence by himself or any person under his control.
If “taking all reasonable precautions” includes being aware of the lack of any good evidence that what you are selling is effective, then this defence should not be much use for most quacks.
Douglas McLachlan has clarified, below, this difficult question
False claims for health benefits of foods
A separate bit of legislation, European regulation on nutrition and health claims made on food, ref 1924/2006, in Article 6, seems clearer in specifying that the seller has to prove any claims they make.
Article 6
Scientific substantiation for claims
1. Nutrition and health claims shall be based on and substantiated by generally accepted scientific evidence.
2. A food business operator making a nutrition or health claim shall justify the use of the claim.
3. The competent authorities of the Member States may request a food business operator or a person placing a product on the market to produce all relevant elements and data establishing compliance with this Regulation.
That clearly places the onus on the seller to provide evidence for claims that are made, rather than the complainant having to ‘prove’ that the claims are false.
On the problem of “health foods” the two bits of legislation seem to overlap. Both have been discussed in “Trading regulations and health foods“, an editorial in the BMJ by M. E. J. Lean (Professor of Human Nutrition in Glasgow).
“It is already illegal under food labelling regulations (1996) to claim that food products can treat or prevent disease. However, huge numbers of such claims are still made, particularly for obesity ”
“The new regulations provide good legislation to protect vulnerable consumers from misleading “health food” claims. They now need to be enforced proactively to help direct doctors and consumers towards safe, cost effective, and evidence based management of diseases.”
In fact the European Food Standards Agency (EFSA) seems to be doing a rather good job at imposing the rules. This, predictably, provoked howls of anguish from the food industry There is a synopsis here.
“Of eight assessed claims, EFSA’s Panel on Dietetic Products, Nutrition and Allergies (NDA) rejected seven for failing to demonstrate causality between consumption of specific nutrients or foods and intended health benefits. EFSA has subsequently issued opinions on about 30 claims with seven drawing positive opinions.”
“. . . EFSA in disgust threw out 120 dossiers supposedly in support of nutrients seeking addition to the FSD’s positive list.
If EFSA was bewildered by the lack of data in the dossiers, it needn’t hav been as industry freely admitted it had in many cases submitted such hollow documents to temporarily keep nutrients on-market.”
Or, on another industry site, “EFSA’s harsh health claim regime”
“By setting an unworkably high standard for claims substantiation, EFSA is threatening R&D not to mention health claims that have long been officially approved in many jurisdictions.”
Here, of course,”unworkably high standard” just means real genuine evidence. How dare they ask for that!
Enforcement of the law
Article 19 of the Unfair Trading regulations says
19. —(1) It shall be the duty of every enforcement authority to enforce these Regulations.
(2) Where the enforcement authority is a local weights and measures authority the duty referred to in paragraph (1) shall apply to the enforcement of these Regulations within the authority’s area.
Nevertheless, enforcement is undoubtedly a weak point at the moment. The UK is obliged to enforce these laws, but at the moment it is not doing so effectively.
A letter in the BMJ from Rose & Garrow describes two complaints under the legislation in which it appears that a Trading Standards office failed to enforce the law. They comment
” . . . member states are obliged not only to enact it as national legislation but to enforce it. The evidence that the government has provided adequate resources for enforcement, in the form of staff and their proper training, is not convincing. The media, and especially the internet, are replete with false claims about health care, and sick people need protection. All EU citizens have the right to complain to the EU Commission if their government fails to provide that protection.”
This is not a good start. A lawyer has pointed out to me
“that it can sometimes be very difficult to get Trading Standards or the OFT to take an interest in something that they don’t fully understand. I think that if it doesn’t immediately leap out at them as being false (e.g “these pills cure all forms of cancer”) then it’s going to be extremely difficult. To be fair, neither Trading Standards nor the OFT were ever intended to be medical regulators and they have limited resources available to them. The new Regulations are a useful new weapon in the fight against quackery, but they are no substitute for proper regulation.”
Trading Standards originated in Weights and Measures. It was their job to check that your pint of beer was really a pint. Now they are being expected to judge medical controversies. Either they will need more people and more training, or responsibility for enforcement of the law should be transferred to some more appropriate agency (though one hesitates to suggest the MHRA after their recent pathetic performance in this area).
Who can be prosecuted?
Any “trader”, a person or a company. There is no need to have actually bought anything, and no need to have suffered actual harm. In fact there is no need for there to be a complainant at all. Trading standards officers can act on their own. But there must be a commercial element. It’s unlikely that simply preaching nonsense would be sufficient to get you prosecuted, so the Prince of Wales is, sadly, probably safe.
Universities who teach that “Amethysts emit high Yin energy” make an interesting case. They charge fees and in return they are “falsely claiming that a product is able to cure illnesses”.
In my view they are behaving illegally, but we shan’t know until a university is taken to court. Watch this space.
The fact remains that the UK is obliged to enforce the law and presumably it will do so eventually. When it does, alternative medicine will have to change very radically. If it were prevented from making false claims, there would be very little of it left apart from tea and sympathy
Follow-up
New Zealand must have similar laws.
Just as I was about to post this I found that in New Zealand a
“couple who sold homeopathic remedies claiming to cure bird flu, herpes and Sars (severe acute respiratory syndrome) have been convicted of breaching the Fair Trading Act.”
They were ordered to pay fines and court costs totalling $23,400.
A clarification form Douglas McLachlan
On the difficult question of who must prove what, Douglas McLachlan, who wrote Has The UK Quietly Outlawed “Alternative” Medicine?, has kindly sent the following clarification.
“I would agree that it is still for the prosecution to prove that the trader committed the offence beyond a reasonable doubt, and that burden of proof is always on the prosecution at the outset, but I think if a trader makes a claim regarding his product and best scientific evidence available indicates that that claim is false, then it will be on the trader to substantiate the claim in order to defend himself. How will the trader do so? Perhaps the trader might call witness after witness in court to provide anecdotal evidence of their experiences, or “experts” that support their claim – in which case it will be for the prosecution to explain the scientific method to the Judge and to convince the Judge that its Study evidence is to be preferred.
Unfortunately, once human personalities get involved things could get clouded – I could imagine a small time seller of snake oil having serious difficulty, but a well funded homeopathy company engaging smart lawyers to quote flawed studies and lead anecdotal evidence to muddy the waters just enough for a Judge to give the trader the benefit of the doubt. That seems to be what happens in the wider public debate, so it’s easy to envisage it happening a courtroom.”
The “average consumer”.
(3) A commercial practice is unfair if—
(a) it contravenes the requirements of professional diligence; and
(b) it materially distorts or is likely to materially distort the economic behaviour of the average consumer with regard to the product.
It seems,therefore, that what matters is whether the “average consumer” would infer from what is said that a claim was being made to cure a disease. The legal view cited by Mojo (comment #2, below) is that expressions such as “can be used to treat” or “can help with” would be considered by the average consumer as implying successful treatment or cure.
The drugstore detox delusion. A nice analysis “detox” at .Science-based Pharmacy
The National Health Executive (“the Independent Journal for Senior Health Service Managers) asked for an article about quackery. This is a version of that article with live links.
Download the pdf version.
There is a Russian translation here (obviously I can’t vouch for its accuracy).
On May 23 th 2006 a letter was sent to the chief executives of 467 NHS Trusts. It was reported as a front page story in the Times, and it was the lead item on the Today programme. The letter urged the government not to spend NHS funds on “unproven and disproved treatments”. Who can imagine anything more simple and self-evident than that? But in politics nothing is simple.
It turns out that quite a lot of patients are deeply attached to unproven and disproved treatments. They clamour for them and, since “patient choice” is high on the agenda at the moment, they quite often get them. Unproven and disproved treatments cost quite a lot of money that the NHS should be spending on things that work.
In January 2007, the Association of Directors of Public Health issued its own list of unproven and disproved treatments. It included, among others, tonsillectomy and adenoidectomy, carpal tunnel surgery and homeopathy. They all matter, but here I’ll concentrate on alternative treatments, of which homeopathy is one of the most widespread.
It should be simple. We have a good mechanism for deciding which treatments are cost-effective, in the form of the National Institute for Clinical Excellence (NICE). If homeopathy and herbalism are not good ways to spend NHS money, why has NICE not said so? The answer to that is simple. NICE has not been asked. It can consider only those questions that are referred to it by the Department of Health (DoH).
The government often says that it takes the best scientific advice, but the DoH seems to have something of a blank spot when it comes to alternative medicine. Nobody knows why. Perhaps it is the dire lack of anyone with a scientific education in government. Or could there be something in the rumour that the DoH lives in terror of being at the receiving end of a rant from the general direction of Clarence House if it doesn’t behave? Whatever the reason, the matter has still not been referred to NICE, despite many requests to do so.
A judgement from NICE would be useful, but it is hardly essential. It isn’t hard to understand. At its simplest the whole problem can be summed up very briefly.
- Homeopathy: giving patients medicines that contain no medicine whatsoever.
- Herbal medicine: giving patients an unknown dose of a medicine, of unknown effectiveness and unknown safety.
- Acupuncture: a rather theatrical placebo, with no real therapeutic benefit in most if not all cases.
- Chiropractic: an invention of a 19 th century salesmen, based on nonsensical principles, and shown to be no more effective than other manipulative therapies, but less safe.
- Reflexology: plain old foot massage, overlaid with utter nonsense about non-existent connections between your feet and your thyroid gland.
- Nutritional therapy: self-styled ‘nutritionists’ making unjustified claims about diet to sell unnecessary supplements.
Of these, ‘nutritional therapy’, or ‘nutritional medicine’, is a relative newcomer. At their worst, they claim that Vitamin C can cure AIDS, and have been responsible for many deaths in Africa. There isn’t the slightest need for them since the nutrition area is already covered by registered dietitians who have far better training.
There have been several good honest summaries of the evidence that underlies these interpretations, written in a style quite understandable by humanities graduates. Try, for example, Trick or Treatment (Singh & Ernst, Bantam Press 2008): a copy should be presented to every person in the DoH and every NHS manager. In some areas the evidence is now quite good. Homeopathy, when tested properly, comes out no different from placebo. That is hardly surprising because the ‘treatment’ pill contains no medicine so it is the same as the placebo pill.
Acupuncture has also been tested well in the last 10 years. A lot of ingenuity has been put into designing sham acupuncture to use as a control. There is still a bit of doubt in a few areas, but overwhelmingly the results show that real acupuncture is not distinguishable from sham. Acupuncture, it seems, is nothing more than a particularly theatrical placebo. All the stuff about meridians and “Qi” is so much mumbo-jumbo. In contrast, herbal medicines have hardly been tested at all.
It is quite easy to get an impression that some of these fringe forms of medicine work better than they do. They form efficient lobby groups and they have friends in high places. They long for respectability and they’ve had a surprising amount of success in getting recognised by the NHS. Some (like chiropractic) have even got official government recognition.
One can argue about whether it was money well-spent, but in the USA almost a billion dollars has been spent on research on alternative medicine by their National Center for Complementary and Alternative Medicine (NCCAM), which was set up as a result of political pressure from the (huge) alternative medicine industry. That has produced not a single effective alternative treatment, but at least it has shown clearly that most don’t work.
The letter of 23 May 2006 proved to be remarkably effective. Tunbridge Wells Homeopathic Hospital has closed and commissioning of homeopathic services has fallen drastically. That has released money for treatments that work, and providing treatments that work is the job of the NHS.
It is sometimes asked, what is wrong with placebo effects as long as the patient feels better? First it must be said that much of the apparent benefit of placebos like homeopathy isn’t a placebo effect, but merely spontaneous recovery. Echinacea cures your cold in only seven days when otherwise it would have taken a week. But when there is a genuine psychosomatic placebo effect, it can be a real benefit. As always, though, one must consider the cost as well as the benefit.
And there are a lot of hidden costs in this approach. One cost is the need to lie to patients to achieve a good placebo effect. That contradicts the trend towards more openness in medicine. And there is a major cost to the taxpayer in the training of people. If the NHS employs homeopaths or spiritual healers because they are nice people who can elicit a good placebo effect, the Human Resources department will insist that they are fully-qualified in myths. ““Full National Federation of Spiritual Healer certificate. or a full Reiki Master qualification, and two years post certificate experience” (I quote). That is one reason why you can find in UK universities, undergraduates being taught at taxpayers’ expense, that “amethysts emit high Yin energy”.
There is a solution to all of this. There is room in the NHS for nice, caring people, to hold the hands of sick patients. They might be called ‘healthcare workers in supportive and palliative care’. They could do a good job, without any of the nonsense of homeopathy or spiritualism. Likewise, manipulative therapists could get together to dispense with the nonsense elements in chiropractic, and to make a real attempt to find out what works best.
All that stands in the way of this common sense approach is the rigidity of Human Resources departments which demand formal qualifications in black magic before you can cheer up sick patients. The over-formalisation of nonsense has done great harm. You have only to note that Skills for Health has listed ‘competences’ in Distant Healing (in the presence of the client or in the absence of the client).
When I asked Skills for Health if they would be defining a ‘competence’ in talking to trees, I was told, in all seriousness, ““You’d have to talk to LANTRA, the land-based organisation for that”.
I’m not joking. I wish I were.
Follow-up
Herbal medicine is, unlike homeopathy, not ridiculous, It is merely Pharmacology, as practised up to circa 1900. Whereas good trials have now shown acupuncture to be sham and homeopathy to be a placebo, there has been very little good research on herbs.
Most herbalism could fairly be described giving to sick patients an unknown dose of a substance with unknown efficacy and unknown safety.
How odd, then, to visit the Royal Society of Medicine to be greeted thus.
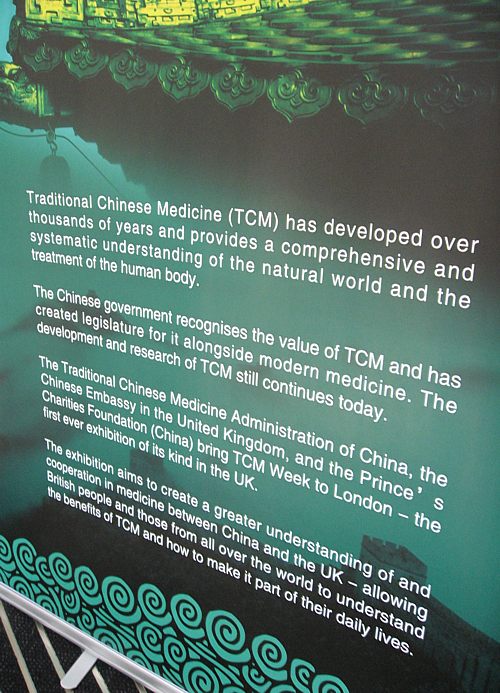
Just look at the words!
“Traditional Chinese Medicine (TCM) has developed over thousands of years”
That’s partly true
“and provides a comprehensive and systematic understanding of the natural world and the treatment of the human body.”
and that is total nonsense. TCM provides no understanding and virtually none of it is known to be useful for treating anything.
| Another poster at the RSM exhibition provides some of the explanation. What on earth, one wonders, do they mean by “making efforts to modernise TCM “? So far, the idea of modernising TCM doesn’t seem to include any great effort to find out if it works. Much of the promotion of TCM seems to be not so much ‘ancient wisdom’, but modern nationalist propaganda by the Chinese government. |
 |
The history is fascinating, but you won’t learn it from the posters on display at the exhibition.
“The Daoguang emperor though it [acupuncture] was a barrier to medical progress and removed it from the curriculum of the Imperial Medical Institute,”
“By the start of the twentieth century, acupuncture was extinct in the West and dormant in the East. It might have fallen out of favour permanently, but it suddenly experienced a revival in 1949 as a direct result of the communist revolution and the establishment of the People’s Republic of China. Chairman Mao Tse-tung engineered a resurgence in traditional Chinese medicine, which included not just acupuncture but also Chinese herbal medicine and other therapies ”
“His motivation was partly ideological, inasmuch as he wanted to reinforce a sense of national pride in Chinese medicine. However he was also driven by necessity. He had promised to deliver affordable healthcare .. . . ”
“Mao did not care whether traditional Chinese medicine worked, as long as he could keep the masses contented. In fact, his personal physician, Zhisui Li, wrote a memoir entitled ‘The Private Life of Chairman Mao’, in which he quoted Mao as saying”
“Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine.” “
Singh & Ernst Trick or Treatmant, page 46.
Or, as put more succinctly by Shapiro
“You would never know that TCM was fashioned in the twentieth century, as we shall see, from a ragbag of therapies in post-revolutionary China.”
Rose Shapiro, Suckers, how alternative medicine makes fools of us all.
Why is the Royal Society of Medicine allowing such mendacious posters? As it happens, I and a friend were visiting the RSM to see their Academic Dean, with a view to finding out why the RSM had failed to take any public position on alternative medicine. The answer appeared to be money, and that was the answer to why the TCM exhibition was being held on their premises too. The Dean no more believed in TCM than we did, but, well, they need the income. He pointed out (looking suitably sheepish) that the address given for the exhibition was not the RSM, but Number 1 Wimpole Street (that, of course, is also the address of the RSM).
Ah, so that’s OK then.
It has to be said that the RSM isn’t alone in its spineless attitude. Both the British Medical Association (BMA) and the Royal College of General Practitioners (RCGP) have failed to make any clear condemnation of mystical medicine. This is in stark contrast to just about every relevant scientific society (here is a summary).
It is a mystery to me why much of medicine should still be dominated by a mindset that seems to have lagged 200 years behind every other science. Perhaps medicine is just too complicated.
UCL Hospitals’ skeleton in the cupboard
Make no mistake, University College London Hospital is top class. The UCLH Trust. runs seven hospitals All but one of them are excellent. But in 2002 the Royal London Homeopathic Hospital was acquired as part of the UCLH group, to the intense embarrassment of UCL scientists.
Let’s start with the good bit. Usually I don’t like anecdotes, so just think of this as a vote of thanks, not evidence.
A personal history of UCH
I owe UCLH a lot personally. On December 13th 1984, my wife had
a subarachnoid haemorrhage when she was seven months pregnant. After misdiagnosis at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millilmetre from the pituitary on the other. It was a bit tricky but I think we got it”.
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds).. Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. | 
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album.. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. Heaven knows what it would have cost in the USA.
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew playing cricket in Bangladesh, Feb 2005. |
But now the the less desirable side of UCLH
Herbs and homeopaths at UCLH
| Recently I was sent the UCLH Annual Review 2007 – 2008. There was a lot of good stuff in it and worth a read despite there being too much hyperbole and too many pictures of men in dark suits. But buried among all the high tech stuff, what do we find but an advertisement for 1900-style pharmacology in the form of the herbal clinic at the Royal London Homeopathic Hospital, accompanied by a load of utterly inaccurate information from the TV botanist, David Bellamy. Take, for example, the claim about Devil’s Claw for osteoarthritis. Even alternative medicine advocates said “The authors concluded that there are insufficient high-quality trials to determine the safety and efficacy of Devil’s Claw (Harpagophytum procumbens) in the treatment of osteoarthritis, and that definitive trials are needed.”
Reading between the lines, I’d guess that the opening of this clinic has a subtext. It is well known that funding for homeopathy has dried up (partly as a result of our letter to NHS Trusts that appeared in the There have been problems before with the herbal activities at the RLHH before (see Conflicts of Interest at the Homeopathic Hospital). It appeared that the Khans, who run the Marigold homeopathic podiatry clinic (no, seriously, it is real) were largely prescribing a herbal product that was made by their own company. without even the hospital trust, never mind the patients, being made aware of it. In normal medicine this would be regarded as a rather serious offence, but as far as I know, nothing was ever done about it. |
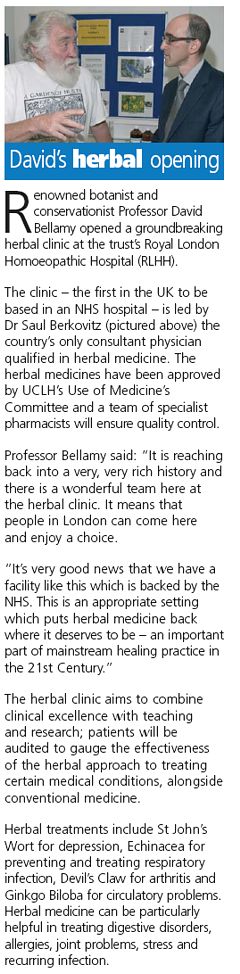 |
The ethics of alternative medicine are truly one of life’s great mysteries.
Reading further in the annual review, we come to the page about the RLHH. The homeopathy side must really have run down because it seems to have diversified into selling cosmetics and groceries. That sounds like desperation.

Good heavens, they sell “chemical-free sun cream”. One wonders what it can be made of, if not chemicals. This is the language of low-grade advertising agencies, not what one expects from an NHS hospital trust.
But next to this there is a much more interesting item. Just look at the last sentence.
I wonder if this could possibly have anything to do with the fact that Michael Baum and I visited the Trust headquarters in August 2006 to propose that the RLHH might be turned into a centre of supportive and palliative care? It would be nice to think so. But it seems they haven’t gone nearly far enough yet. If all they do is replace the waning homeopathy We know they are under pressure from their royal patrons, but that, in a constitutional monarchy, is simply not acceptable. |
 |
Michael Baum is a cancer surgeon who has taken a particular interest in palliative and supportive care. He is someone whose views should be taken seriously. He is also the author of the magnificent “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong” Here is a quotation from that letter. The UCLH Trust should bear it in mind.
| The power of my authority comes with a knowledge built on 40 years of study and 25 years of active involvement in cancer research. I’m sensitive to the danger of abusing this power and, as a last resort, I know that the General Medical Council (GMC) is watching over my shoulder to ensure I respect a code of conduct with a duty of care that respects patients’ dignity and privacy and reminds me that my personal beliefs should not prejudice my advice. Your power and authority rest on an accident of birth. Furthermore, your public utterances are worthy of four pages, whereas, if lucky, I might warrant one. I don’t begrudge you that authority and we probably share many opinions about art and architecture, but I do beg you to exercise your power with extreme caution when advising patients with life threatening diseases to embrace unproven therapies. There is no equivalent of the GMC for the monarchy, so it is left either to sensational journalism or, more rarely, to the quiet voice of loyal subjects such as myself to warn you that you may have overstepped the mark. It is in the nature of your world to be surrounded by sycophants (including members of the medical establishment hungry for their mention in the Queen’s birthday honours list) who constantly reinforce what they assume are your prejudices. Sir, they patronise you! Allow me this chastisement. |
Follow-up
The photo album chronicling the birth of my son, is really just for family and friends, but at least one blog picked up on the wider significance.
Alfred Joseph Clark FRS held the established chair of Pharmacology at UCL from 1919 to 1926, when he left for Edinburgh. In the 1920s and 30s, Clark was a great pioneer in the application of quantitative physical ideas to pharmacology. As well as his classic scientific works, like The Mode of Action of Drugs on Cells (1933) he wrote, and felt strongly, about the fraud perpetrated on the public by patent medicine salesmen. In 1938 (while in Edinburgh) he published a slim volume called Patent Medicines. The parallels with today are astonishing.
Alfred Joseph Clark FRS (1885 – 1941) |
 |
I was lucky to be given a copy of this book by David Clark, A.J. Clark’s eldest son, who is now 88. I visited him in Cambridge on 17 September 2008, because he thought that, as holder of the A.J. Clark chair at UCL from 1985 to 2004, I’d be a good person to look after this and several other books from his father’s library. They would have gone to the Department of Pharmacology if we still had one, but that has been swept away by mindless administrators with little understanding of how to get good science.
Quotations from the book are in italic, and are interspersed with comments from me.
The book starts with a quotation from the House of Commons Select Committee report on Patent Medicines. The report was submitted to the House on 4 August 1914, so there is no need to explain why it had little effect. The report differs from recent ones in that it is not stifled by the sort of political correctness that makes politicians refer to fraudsters as “professions”.
The problem
“2.2 The situation, therefore, as regards the sale and advertisement of proprietary medicines and articles may be summarised as follows:
For all practical purposes British law is powerless to prevent any person from procuring any drug, or making any mixture, whether patent or without any therapeutical activity whatever (as long as it does not contain a scheduled poison), advertising it in any decent terms as a cure for any disease or ailment, recommending it by bogus testimonials and the invented opinions and facsimile signatures of fictitious physicians, and selling it under any name he chooses, on payment of a small stamp duty. For any price he can persuade a credulous public to pay.”
Select Committee on Patent Medicines. 1914
“The writer has endeavoured in the present article to analyse the reasons for the amazing immunity of patent medicines form all attempts to curb their activity, to estimate the results and to suggest the obvious measures of reform that are needed.”
| Clark, writing in 1938, was surprised that so little had changed since 1914. What would he have thought if he had known that now, almost 100 years after the 1914 report, the fraudsters are still getting away with it? Chapter 2 starts thus. |
 |
THE LAW
The Select Committee appointed by the House of Commons in 1914 ‘to consider and inquire into the question of the sale of Patent and Proprietary Medicines’ stated its opinion in 28 pages of terse and uncompromising invective. Its general conclusions were as follows:
That the trade in secret remedies constituted a grave and widespread public evil.
That the existing law was chaotic and had proved inoperative and that consequently the traffic in secret remedies was practically uncontrolled.
In particular it concluded ‘”that this is an intolerable state of things and that new legislation to deal with it, rather than merely the amendment of existing laws, is urgently needed in the public interest.”
The “widespread public evil”continues almost unabated, and rather than introduce sensible legislation to cope with it, the government has instead given a stamp of approval for quackery by introducing utterly ineffective voluntary “self-regulation”.
Another Bill to deal with patent medicines was introduced in 1931, without success, and finally in 1936, a Medical and Surgical Appliances (Advertisement) Bill was introduced. This Bill had a very limited scope. Its purpose was to alleviate some of the worst abuses of the quack medicine trade by prohibiting the advertisement of cures for certain diseases such as blindness, Bright’s disease [nephritis] , cancer, consumption [tuberculosis], epilepsy, fits, locomotor ataxy, fits, lupus or paralysis.
The agreement of many interests was secured for this measure. The president of the Advertising Association stated that the proposed Bill would not affect adversely any legitimate trade interest. Opposition to the Bill was, however, whipped up amongst psychic healers, anti-vivisectionists and other opponents of medicine and at the second reading in March 1936, the Bill was opposed and the House was counted out during the ensuing debate. The immediate reason for this fate was that the Bill came up for second reading on the day of the Grand National! This is only one example of the remarkable luck that has attended the patent medicine vendors.
(Page 14).
The “remarkable luck” of patent medicine vendors continues to this day, Although, in principle, advertisement of cures for venereal diseases was banned in 1917, and for cancer in 1939, it takes only a few minutes with Google to find that these laws are regularly flouted by quacks, In practice quacks get away with selling vitamin pills for AIDS, sugar pills for malaria and homeopathic pills for rabies, polio anthrax and just about anything else you can think of. Most of these advertisements are contrary to the published codes of ethics of the organisations to which the quack in question belongs but nothing ever happens.
Self-regulation simply does not work, and there is still no effective enforcement even of existing laws..
“It has already been stated that British law allows the advertiser of a secret remedy to tell any lie or make any claim that he fancies will sell his goods and the completeness of this licence is best illustrated by the consideration of a few specific points.
Advertisements for secret remedies very frequently contain a list of testimonials from medical men, which usually are in an anonymous form, stating that ………….. M.D., F.R.C.S., has found the remedy infallible. Occasionally, however, the name and address of a doctor is given and anyone unaware of the vagaries of English law would imagine that such use of a doctor’s name and professional reputation could not be made with impunity without his consent. In 1899, however, the Sallyco Mineral Water Company advertised that ‘Dr. Morgan Dochrill, physician to St. John’s Hospital, London and many of the leading physicians are presenting ‘Sallyco’ as an habitual drink. Dr. Dochrill says nothing has done his gout so much good.
Dr. Dochrill, whose name and title were correctly stated above, sued the company but failed in his case. ”
“The statement that the law does not prevent the recommending of a secret remedy by the use of bogus testimonials and facsimile signatures of fictitious physicians is obviously an understatement since it is doubtful how far it interferes with the use of bogus testimonials from real physicians.”
Dodgy testimonials are still a mainstay of dodgy salesman. One is reminded of the unauthorised citation of testimonials from Dr John Marks and Professor Jonathan Waxman by Patrick Holford to aid his sales of unnecessary vitamin supplements. There is more on this at Holfordwatch.
The man in the street knows that the merits of any article are usually exaggerated in advertisements and is in the habit of discounting a large proportion of such claims, but, outside the realm of secret remedies, the law is fairly strict as regards definite misstatements concerning goods offered for sale and hence the everyday experience of the man in the street does not prepare him for dealing with advertisements which are not merely exaggerations but plain straightforward lies from beginning to end.
Scientific training is undoubtedly a handicap in estimating popular gullibility as regards nostrums. One imagines that no one today would be willing to spend money on pills guaranteed to prevent earthquakes but yet the claims of many of the remedies offered appear equally absurd to anyone with an elementary
knowledge of physiology or even of chemistry. A study of the successes and failures suggests that success depends chiefly on not over-rating the public intelligence. (Page 34)
This may have changed a bit since A.J. Clark was writing in 1938. Now the main clients of quacks seem to be the well-off “worried-well”. But it remains as true as ever that “Scientific training is undoubtedly a handicap in estimating popular gullibility as regards nostrums.” In 2008, it is perhaps more a problem of Ben Goldacre’s dictum ““My basic hypothesis is this: the people who run the media are humanities graduates with little understanding of science, who wear their ignorance as a badge of honour.”
Clark refers (page 36) to a successful conviction for fraud in the USA in 1917. The subject was a widely advertised ‘get fat quick’ pill that contained lecithin, proteins and sugar. The BMA analysis (in 1912)
suggested that the cost of the ingredients in a box of 30 tablets sold for 4/6 was 1 1/4 d. [4/6 meant 4 shillings and six pence, or 22.5 pence since 1971, and 1 1/4 old pence, a penny farthing, is 0.52 new pence]. He comments thus.
The trial revealed many interesting facts. The formula was devised after a short consultation with the expert of one of the largest drug manufacturers in the U.S.A. This firm manufactured the tablets and sold them to the proprietary medicine company at about 3/- per 1000, whilst they were retailed to the public at the rate of £7 10s. per 1000. The firm is estimated to have made a profit of about $3,000,000.
These trials in the U.S.A. revealed the fact that in a considerable proportion of cases the ‘private formula’ department of the large and well known drug firm already mentioned had first provided the formula for the nostrum and subsequently had prepared it wholesale.
Nothing much has changed here either. The alternative medicine industry (and it is a very big industry) is fond of denouncing the evils of the pharmaceutical industry, and sadly, occasionally they are right. One of the less honest practices of the pharmaceutical industry (though one never mentioned by quacks) is buying heavily into alternative medicine. Goldacre points out
“there is little difference between the vitamin and pharmaceutical industries. Key players in both include multinationals such as Roche and Aventis; BioCare, the vitamin pill producer that media nutritionist Patrick Holford works for, is part-owned by Elder Pharmaceuticals.”
And then. of course, there is the deeply dishonest promotion by Boots the Chemists of homeopathic miseducation, of vitamins and of CoQ10 supplements.
The manner in which secret remedies can survive repeated exposure is shown by the following summary of the life history of a vendor of a consumption [tuberculosis] cure.
1904, 1906: Convicted of violating the law in South Africa.
1908: Exposed in British Medical Association report and also attacked by Truth.
1910: Sued by a widow. The judge stated: ‘I think this is an intentional and well-considered fraud. It is a scandalous thing that poor people should be imposed upon and led to part with their money, and to hope that those dear to them would be cured by those processes which were nothing but quack remedies and had not the slightest value of any kind.’
1914: A libel action against the British Medical Association was lost.
1915 The cure was introduced into the United States.
1919 The cure was sold in Canada.
1924 Articles by men with medical qualifications appeared in the Swiss medical journal boosting
the cure.
Secret remedies have a vitality that resembles that of the more noxious weeds and the examples mentioned suggest that nothing can do them any serious harm.
Most of the time, quacks get away with claims every bit as outrageous today. But Clark does give one example of a successful prosecution. It resulted from an exposé in the newspapers -wait for it -in the Daily Mail.
There is, however, one example which proves that a proprietary remedy can be squashed by exposure if this is accompanied by adequate publicity.
The preparation Yadil was introduced as an antiseptic and was at first advertised to the medical profession. The proprietor claimed that the remedy was not secret and that the active principle was ‘tri-methenal allylic carbide’. The drug acquired popularity in the influenza epidemic of 1918 and the proprietor became more and more ambitious in his therapeutic claims. The special virtue claimed for Yadil was that it would kill any harmful organism that had invaded the body. A more specific claim was that consumption in the first stage was cured with two or three pints whilst advanced cases might require a little more. Other advertisements suggested that it was a cure for most known diseases from cancer downwards.
These claims were supported by an extraordinarily intense advertising campaign. Most papers, and even magazines circulating amongst the wealthier classes, carried full page and even double page advertisements. The Daily Mail refused these advertisements and in 1924 published a three column article by Sir William Pope, professor of Chemistry in the University of Cambridge. He stated that
the name ‘tri-methenal allylic carbide’ was meaningless gibberish and was not the chemical definition of any known substance. He concluded that Yadil consisted of :
‘About one per cent of the chemical compound formaldehyde.
About four per cent of glycerine.
About ninety-five per cent of water and, lastly, a smell.
He calculated that the materials contained in a gallon cost about 1/6, whilst the mixture was sold at £4 10s. per gallon.
This exposure was completely successful and the matter is of historic interest in that it is the only example of the career of a proprietary medicine being arrested by the action of the Press.
Clark goes on to talk of the law of libel.
“On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”
The law of libel to this day remains a serious risk to freedom of speech of both individuals and the media. Its use by rogues to suppress fair comment is routine. My first encounter was when a couple of herbalists
threatened to sue UCL because I said that the term ‘blood cleanser’ is gobbledygook. The fact that the statement was obviously true didn’t deter them for a moment. The herbalists were bluffing no doubt, but they caused enough nuisance that I was asked to take my pages off UCL’s server. A week later I was invited back but by then I’d set up a much better blog and the publicity resulted in an enormous increase in readership, so the outcome was good for me (but bad for herbalists).
It was also good in the end for Andy Lewis when his immortal page “The gentle art of homoeopathic killing” (about the great malaria scandal) was suppressed. The Society of Homeopaths’ lawyers didn’t go for him personally but for his ISP who gave in shamefully and removed the page. As a result the missing page reappeared in dozens of web sites round the world and shot to the top in a Google search.
Chiropractors are perhaps the group most likely to try to suppress contrary opinions by law not argument. The only lawyers’ letter that has been sent to me personally, alleged defamation in an editorial that I wrote for the New Zealand Medical Journal. That was a little scary, but the journal stuck up for its right to speak and the threat went away after chiropractors were allowed right of reply (but we got the last word).
Simon Singh, one of the best science communicators we have, has not been so lucky. He is going to have to defend in court an action brought by the British Chiropractic Association because of innocent opinions expressed in the Guardian.
Chapter 6 is about “The harm done by patent medicines”. It starts thus.
“The trade in secret remedies obviously represents a ridiculous waste of money but some may argue that, since we are a free country and it pleases people to waste their money in this particular way, there is no call for any legislative interference. The trade in quack medicines cannot, however, be regarded as a harmless one. The Poisons Acts fortunately prevent the sale of a large number of dangerous drugs, but there are numerous other ways in which injury can be produced by these remedies.”
The most serious harm, he thought, resulted from self-medication, and he doesn’t mince his words.
“The most serious objection to quack medicines is however that their advertisements encourage self-medication as a substitute for adequate treatment and they probably do more harm in this than in any other manner.
The nature of the problem can best be illustrated by considering a simple example such as diabetes. In this case no actual cure is known to medicine but, on the other hand, if a patient is treated adequately by insulin combined with appropriate diet, he can be maintained in practically normal health, in spite of his disability, for an indefinite period. The expectation of life of the majority of intelligent diabetics, who make no mistakes in their regime, is not much less than that of normal persons. The regime is both irksome and unpleasant, but anyone who persuades diabetics to abandon it, is committing manslaughter as certainly as if he fired a machine gun into a crowded street.
As regards serious chronic disease the influence of secret remedies may be said to range from murderous to merely harmful.
‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous, since they are likely to cause the death of anyone who is unfortunate enough to believe in their efficacy and thus delay adequate treatment until too late.
The phrase “‘Cures for consumption, cancer and diabetes may fairly be classed as murderous” made Clark himself the victim of suppression of freedom of speech by lawyers. His son, David Clark, wrote of his father in “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3)
“Although tolerant of many human foibles, A. J. had always disapproved fiercely of quacks, particularly the charlatans who sold fraudulent medicines. During his visits to London he met Raymond Postgate, then a crusading left wing journalist, who persuaded A.J. to write a pamphlet which was published in an ephemeral series called ‘Fact‘ in March 1938. It was a lively polemical piece. . To A.J.’s surprise and dismay he was sued for libel by a notorious
rogue who peddled a quack cure for for tuberculosis. This man said that A.J.’s remarks (such as “‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”) were libellous and would damage his business. A.J. was determined to fight, and he and Trixie decided to put their savings at stake if necessary. The B.M.A. and the Medical Defence Union agreed to support him and they all went to lawyers. He was shocked when they advised him that he would be bound to lose for he had damaged the man’s livelihood! Finally, after much heart searching, he made an apology, saying that he had not meant that particular man’s nostrum”
Talk about déjà vu!
On page 68 there is another very familiar story. It could have been written today.
“The fact that the public is acquiring more knowledge of health matters and is becoming more suspicious of the cruder forms of lies is also helping to weed out the worst types of patent medicine advertisements. For example, in 1751 a bottle of oil was advertised as a cure for scurvy, leprosy and consumption but today such claims would not be effective in promoting the sale of a remedy. The modern advertiser would probably claim that the oil was rich in all the vitamins and the elements essential for life and would confine his claims to a statement that it would alleviate all minor forms of physical or mental ill-health.
The average patent medicine advertised today makes plausible rather than absurd claims and in general the advertisements have changed to conform with a change in the level of the public’s knowledge.
It is somewhat misleading, however, to speak of this as an improvement, since the law has not altered and hence the change only means that the public is being swindled in a somewhat more skilful manner.
The ideal method of obtaining an adequate vitamin supply is to select a diet containing an abundant supply of fresh foods, but unfortunately the populace is accustomed to live very largely on preserved or partially purified food stuffs and such processes usually remove most of the vitamins.”
The first part of the passage above is reminiscent of something that A.J Clark wrote in the BMJ in 1927. Nowadays it is almost unquotable and I was told by a journal editor that it was unacceptable even with asterisks. That seems to me a bit silly. Words had different connotations in 1927.
“The less intelligent revert to the oldest form of belief and seek someone who will make strong magic for them and defeat the evil spirits by some potent charm. This is the feeling to which the quack appeals; he claims to be above the laws of science and to possess some charm for defeating disease of any variety.
The nature of the charm changes with the growth of education. A naked n****r howling to the beat of a tom-tom does not impress a European, and most modern Europeans would be either amused or disgusted by the Black mass that was popular in the seventeenth century. Today some travesty of physical science appears to be the most popular form of incantation.”
A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927
Apart from some of the vocabulary, what better description could one have of the tendency of homeopaths to harp on meaninglessly about quantum theory or the “scienciness” and “referenciness” of
modern books on nutritional therapy?
So has anything changed?
Thus far, the outcome might be thought gloomy. Judging by Clark’s account, remarkably little has changed since 1938, or even since 1914. The libel law in the UK is as bad now as it was then. Recently the United Nations Human Rights Committee said UK laws block matters of public interest and encourage libel tourism (report here, see also here). It is unfit for a free society and it should be changed.
But there are positive sides too. Firstly the advent of scientific bloggers has begun to have some real influence. People are no longer reliant on journalists to interpret (or, often, misinterpret) results for them. They can now get real experts and links to original sources. Just one of these, Ben Goldacre’s badscience.net, and his weekly column in the Guardian has worked wonders in educating the public and improving journalism. Young people can, and do, contribute to the debate because they can blog anonymously if they are frightened that their employer might object.
Perhaps still more important, the law changed this year. Now, at last, it may be possible to prosecute successfully those who make fraudulent health claims. Sad to say, this was not an initiative of the UK government, which remains as devoted as ever to supporting quacks. Remember that, quite shamefully, the only reason given by the Medicines and Health Regulatory Authority (MHRA) gave for allowing false labelling of homeopathic pills was to support the “homeopathic industry”. They suggested (falsely) that the EU required them to take this irresponsible step, which was condemned by just about every scientific organisation. But the new unfair trading regulations did come from the EU. After almost 100 years since the 1914 report, we have at last some decent legislation. Let’s hope it’s enforced.
Postcript
The back cover of the series of ‘Fact‘ books in which A.J. Clark’s article appeared is reproduced below, simply because of the historical portrait of the 1930s that it gives.
Follow-up
This post got a lot of hits from Ben Goldacre’s miniblog which read
- Prof David Colquhoun gets into a time machine and meets himself
A truly classic DC post.
Thanks, Ben.
There have been some really excellent books about quackery this year. This isn’t one of them, because
 |
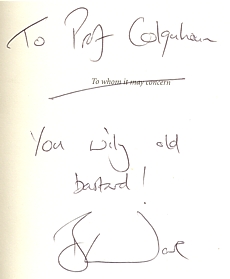
Nice dedication uh? |
it is about a lot more than quackery It is about the scientific method in general. and in particular about how often it is misunderstood by journalists. Abuse of evidence by the pharmaceutical industry is treated just as harshly as abuse of evidence by homeopaths and you get the low-down on both.
“More importantly, you will also see how a health myth can be created, fostered and maintained by the alternative medicine industry using all the same tricks on you, the public, which big pharma uses on doctors. This is about something much bigger than homeopathy.” (p.28)
Sir Iain Chalmers, a founder of the Cochrane Collaboration , co-author of the best lay text on evidence says: “Bad Science introduces the basic scientific principles to help everyone become a more effective bullshit detector”. And there is no more invaluable skill than being a bullshit detector.
Chalmers says also “Ben Goldacre has succeeded where the ‘public engagement in science’ organisations have so signally failed.” That is exactly right. ‘Public engagement’ has rapidly become bureaucratised, and at its worst, is no better than a branch of the university’s marketing department. This sort of public engagement corrupts as much as it enlightens. Goldacre enlightens, and he also makes you laugh.
In the introduction, Goldacre says
“You cannot reason people out of positions that they didn’t reason themselves into.” (p xii)
It’s a nice point, but the rest of the book makes a magnificent attempt to do just that.
There is quite a lot about medicine, of course, that’s his job, after all. But it isn’t all quackery by a long chalk Quackery is merely a good hook to hang the arguments on about how you distinguish what’s true from what isn’t. That’s partly because quacks make every mistake known to mankind (sometimes through ignorance, sometimes just to boost sales), and partly just because it is a topic that interests people, and with which they are bombarded every day I feel exactly the same. If I were to talk about the statistics of single ion channels, nobody would read it (big mistake -it’s fascinating), but if one can use the case of honey versus cough medicine to explain the analysis of variance, there is a chance that someone might find it interesting.
As much as anything, Goldacre’s book is about C.P. Snow’s two cultures. The chapters on the distortion and trivialisation of science in the media are just terrific.
“My basic hypothesis is this: the people who run the media are humanities graduates with little understanding of science, who wear their ignorance as a badge of honour. Secretly, deep down, perhaps they resent the fact that they have denied themselves access to the most significant developments in the history of Western thought from the past two hundred years.” Chapter 11, p. 207
“.. . . here is the information I would like from a newspaper to help me make decisions about my health, when reporting on a risk: I want to know who you’re talking about (e.g. men in their fifties): I want to know what the baseline risk is (e.g. four men out of a hundred will have a heart attack over ten years); and I want to know what the increase in risk is , as a natural frequency [not as relative risk] (two extra men out of that hundred will have a heart attack over ten years). I also want to know exactly what’s causing that increase in risk -an occasional headache pill or a daily tub full of pain-relieving medication for arthritis. Then I will consider reading your newspapers again, instead of blogs which are written by people who understand research , and which link reliably back to the original academic paper, so that I can double check their précis when I wish. ” (p. 242)
I detect some ambiguity in references to things that aren’t true. Sometimes there is magnanimity. At other times he is a grade one kick-ass ninja. For example
I can very happily view posh cosmetics -and other forms of quackery -as a special, self-administered, voluntary tax on people who don’t understand science properly (p. 26)
Of course nobody wants to ban cosmetics, or even homeopathy. But a lot of bad consequences flow from being over-tolerant of lies if you take it too far (he doesn’t). The lying dilemma and the training dilemma are among them. Some unthinking doctors will refer troublesome patients to a reflexologist. That gets the worried-well out of their surgery but neglects the inevitable consequence that Human Resources box-ticking zombies will then insist on having courses that teach the big toe is connected to the kidney (or whatever) so that reflexologists can have an official qualification in mystical mumbo-jumbo.
Is there anything missing from the book? Well inevitably. There are plenty of villains among the peddlers of nutri-bollocks, and in the media. But there isn’t much about the people who seem to me to be in some ways even worse. What about the black-suited men and women in the Ministry of Health and in some vice-chancellors’ chairs who betray their institutions and betray the public through some unfathomable
mixture of political correctness, scientific ignorance and greed? What about the ludicrous behaviour of quangos like Skills for Health? You have to wait right to the end of the book to hear about universities. But when it comes, it is well worth the wait.
“I’m not surprised that there are people with odd ideas about medicine, or that they sell those ideas. But I am spectacularly, supremely, incandescently unimpressed when a a university starts to offer BSc science courses in them.” (p. 317)
It’s almost worth buying Ben Goldacre’s book for that sentence alone.
This book is a romp through the folly, greed and above all the ignorance of much in our society. It’s deeply educational. And it makes you laugh. What more could you want?
The Times today has given s good showing for my comment piece. It gives the case against following the advice of the Pittilo report. It simply makes no sense to have government regulation of acupuncture, herbal medicine, traditional Chinese medicine until such time as there is evidence that they work. It makes even less sense to have BSc degrees in them. The Department of Health should have more sense that to use the Prince of Wales as its scientific advisor.
Let’s hope that the recent example set by the University of Central Lancashire is the start of trend for vice-chancellors to appreciate that running such degrees brings their universities into disrepute.
I can only apologise for the dreadful title that The Times’ sub-editors put on the piece, My original title was
A bad report for the vice chancellor
The Pittilo report to the Department of Health will endanger the public and corrupt universities. There is a better way.
I like that much better than “Regulate quack nedicine? I feel sick”.
But, oh dear, the picture that I sent them is on the left, but what appeared is on the right. Spot the difference.
 |
 |
Well now, at least, I can feel I have something in common with Isambard Kingdom Brunel.
Follow-up
It so happens that Professor Pittilo wrote a letter to Times Higher Education this week. I fear that it provided a yet more evidence that he hasn’t really quite got the hang of evidence.
The Lancashire Evening Post catches up with the UCLan story, two days after you read it here.
A reply from Professor Pittilo
This response to the op-ed of 29th August appeared as a letter
in the Times on Sept 2.
| Public health needs protection
Regulation of acupuncture and herbal medicine has been subject to much scrutiny Sir, Professor Colquhoun’s campaign to discredit our report (“Regulate quack medicine? I feel sick,” Aug 29) is in danger of placing public health at risk. He is entitled to challenge existing evidence for the effectiveness of complementary and alternative medicine (CAM) but fails to acknowledge the key recommendation from the steering group on the essential need to demonstrate efficacy, safety and quality assurance as a prerequisite for NHS funding. Professor Colquhoun dismisses CAM because of the absence of a rigorous scientific foundation and he asserts that to teach and practise it is unethical. Survey data consistently demonstrates very high demand for CAM with one report estimating that 22 million visits involving 10.6 per cent of the population in England alone occurred in 2008. This demand is one reason why his alternative model of trade law enforcement will not work. He may argue that these people are uncritical recipients of nonsense, but data from the Medicines and Healthcare products Regulatory Agency confirm that they are at significant risk from poor practice. It is essential that we protect the public by implementing statutory regulation alongside demanding evidence of efficacy. Professor Colquhoun’s resistance to the teaching of science to CAM practitioners will do little to help them to critically evaluate effectiveness. Professor Michael Pittilo Chair of the Department of Health Steering Group |
And Pittilo wrote in similar vein to Times Higher Education.
Science vital to health study28 August 2008 Your feature on some members of staff at the University of Central Lancashire attacking science degrees in complementary and alternative medicine (“Staff attack science degrees in alternative health”, 7 August) raises a number of concerns. It is up to any university, taking account of the expert views of staff and external peer review, to determine the appropriate title and award for any degree. It is encouraging to note from the feature that new courses The recent report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and other Traditional Medicine There is no doubt that courses that provide a solid scientific foundation will greatly assist CAM practitioners in establishing evidence-based practice. It would be most unfortunate if the reported resistance to degree titles led to those wishing to practise acupuncture or herbal medicine receiving less hard science than they might have. To say that acupuncture and herbal medicine degrees have no academic justification appears arrogant in the extreme. Although it is certainly true that some content may not be scientific, this does not invalidate the legitimacy of these courses at degree level, a fact borne out by their successful validation in a number of universities. R. Michael Pittilo, Principal and vice-chancellor, The Robert Gordon University. |
This one got excellent responses from Kevin Smith (University of Abertay, Dundee), and from Peter J. Brophy (Professor of veterinary anatomy and cell biology University of Edinburgh). This was my comment to THE
There are a few very obvious responses to Professor Pittilo’s letter
For many alternative therapies the “philosophy” is simply incompatible with science. One obvious example is homeopathy. On Mondays and Wednesdays (science days) the students will be required to learn that response increases with dose. On Tuesdays and Thursdays will be taught the opposite. But for the exam they must reproduce only the latter (nonsensical) idea because their aim is to get a job as a homeopath. That makes nonsense of the idea of a university.
This seems to constitute a recognition that the evidence is still very inadequate. The time to start degrees, and the time to give official government recognition, is after the evidence is in, not before. What happens if you start degrees and then find that the subject is so much nonsense? Well, that has already happened in several areas of course. But the people who accredit the course and who act as external examiners just happen to be fervent believers in that nonsense, so all appears to be well (to bean counters anyway).
There is, as it happens, a great deal of evidence now about acupuncture, but the authors of the report do not seem to be aware of it. I recommend Barker Bausell’s book on the topic. If students are educated science, like what constitutes evidence, and our current understanding of words like “energy”, they would have to disavow the subject that there are supposed to training to practise
No, it is not a matter of arrogance, just a matter of careful attention to the evidence. Attention to evidence was notably absent in Prof Pittilo’s report, perhaps because his committee consisted entirely of people who earn their living from the subjects they were supposed to be assessing.
I have had the misfortune to have waded through a mound of such validation documents. The one thing they never consider is whether the treatment works. Sad to say, these validations are not worth the paper they are written on. |
The article below is an editorial that I was asked to write for the New Zealand Medical Journal, as a comment on article in today’s edition about the misuse of the title ‘doctor’ by chiropractors [download pdf]. Titles are not the only form of deception used by chiropractors, so the article looks at some of the others too. For a good collection of articles that reveal chiropractic for what it is, look at Chirobase
THE NEW ZEALAND
MEDICAL JOURNAL
Journal of the New Zealand Medical Association
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716

URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Doctor Who?
Inappropriate use of titles by some alternative “medicine” practitioners
David Colquhoun
Who should use the title ‘doctor’? The title is widely abused as shown by Gilbey1 in this issue of the NZMJ in an article entitled Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. Meanwhile, Evans and colleagues 2, also in this issue, discuss usage and attitudes to alternative treatments.
Gilbey finds that the abuse of the title doctor is widespread and that chiropractors are the main culprits. An amazing 82% of 146 chiropractics used the title Doctor, andL most of them used the title to imply falsely that they were registered medical practitioners.
Although it is illegal in New Zealand to do that, it seems clear that the law is not being enforced and it is widely flouted. This is perhaps not surprising given the history of chiropractic. It has had a strong element of ruthless salesmanship since it was started in Davenport, Iowa by D.D. Palmer (1845–1913). His son, B.J. Palmer, said that their chiropractic school was founded on “a business, not a professional basis. We manufacture chiropractors. We teach them the idea and then we show them how to sell” (Shapiro 2008)3 It is the same now. You can buy advice on how to build “build high-volume, subluxation-based, cash-driven, lifetime family wellness practices”
In her recent book3 , Rose Shapiro comments on the founder of chiropractic as follows.
“By the 1890s Palmer had established a magnetic healing practice in Davenport, Iowa, and was styling himself “doctor”. Not everyone was convinced, as a piece about him in an 1894 edition of the local paper, the Davenport Leader, shows.
A crank on magnetism has a crazy notion hat he can cure the sick and crippled with his magnetic hands. His victims are the weak-minded, ignorant and superstitious,those foolish people who have been sick for years and have become tired of the regular physician and want health by the short-cut method he has certainly profited by the ignorance of his victim. His increase in business shows what can be done in Davenport, even by a quack.”
D.D. Palmer was a curious mixture: grocer, spiritual healer, magnetic therapist, fairground huckster, religious cult leader—and above all, a salesman. He finally found a way to get rich by removing entirely imaginary “subluxations”.
Over 100 years later, it seems that the “weak-minded, ignorant, and superstitious” include the UK’s Department of Health, who have given chiropractics a similar status to the General Medical Council.
The intellectual standards of a 19th Century Mid-Western provincial newspaper journalist are rather better than the intellectual standards of the UK’s Department of Health, and of several university vice-chancellors in 2007.
Do the treatments work?
Neither Gilbey nor Evans et al. really grasp the nettle of judging efficacy. The first thing one wants to know about any treatment —alternative or otherwise — is whether it works. Until that is decided, all talk of qualifications, regulation, and so on is just vacuous bureaucratese. No policy can be framed sensibly until the question of efficacy has been addressed honestly.
It is one good effect of the upsurge of interest in alternative treatments that there are now quite a lot of good trials of the most popular forms of treatments (as well as many more bad trials). Some good summaries of the results are now available too. Cochrane reviews set the standard for good assessment of evidence. New Zealand’s Ministry of Health commissioned the Complementary and Alternative Medicine
website to assess the evidence, and that seems to have done a good job too. Their assessment of chiropractic treatment of low back pain is as follows:
There appears to be some evidence from one systematic review and four other studies, although not conclusive, that chiropractic treatment is as effective as other therapies but this may be due to chance. There is very little evidence that chiropractic is more effective than other therapies.
And two excellent summaries have been published as books this year. Both are by people who have had direct experience of alternative treatments, but who have no financial interest in the outcome of their assessment of evidence. The book by Singh and Ernst4 summarises the evidence on all the major alternative treatments, and the book by Bausell5 concentrates particularly on acupuncture, because the author was for 5 years involved in research in that area, Both of these books come to much the same conclusion about chiropractic. It is now really very well-established that chiropractic is (at best) no more effective than conventional treatment. But it has the disadvantage of being surrounded by gobbledygook about “subluxations” and, more importantly, it kills the occasional patient.
Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
The chiropractors of Alberta (Canada) and the Alberta Government are now facing a class-action lawsuit8. The lead plaintiff is Sandra Nette. Formerly she was a fit 41 year old. Now she is tetraplegic. Immediately
after neck manipulation by a chiropractor she had a massive stroke as a result of a torn vertebral artery.
Acupuncture comes out of the assessments equally badly. Bausell (2007) concludes that it is no more than a theatrical placebo.
Are the qualifications even real?
It is a curious aspect of the alternative medicine industry that they often are keen to reject conventional science, yet they long for academic respectability. One aspect of this is claiming academic titles on the flimsiest of grounds. You can still be held to have misled the public into thinking you are a medical
practitioner, even if you have a real doctorate. But often pays to look into where the qualifications come from.
A celebrated case in the UK concerned the ‘lifestyle nutritionist’, TV celebrity and multi-millionaire, Dr Gillian McKeith, PhD. A reader of Ben Goldacre’s excellent blog, badscience.net did a little investigation. The results appeared in Goldacre’s Bad Science column in the Guardian9.
She claimed that her PhD came from the American College of Nutrition, but it turned out to come from a correspondence course from a non-accredited US ‘college’. McKeith also boasted of having “professional membership” of the American Association of Nutritional Consultants, for which she provided proof of her degree and three professional references.
The value of this qualification can be judged by the fact that Goldacre sent an application and $60 and as a result “My dead cat Hettie is also a “certified professional member” of the AANC. I have the certificate hanging in my loo”.
Is the solution government regulation?
In New Zealand the law about misleading the public into believing you are a medical practitioner already exists. The immediate problem would be solved if that law were taken seriously, but it seems that it is not.
It is common in both the UK and in New Zealand to suggest that some sort of official government regulation is the answer. That solution is proposed in this issue of NZMJ by Evans et al2. A similar thing has been proposed recently in the UK by a committee headed by Michael Pittilo, vice-chancellor of Robert Gordon’s University, Aberdeen.
I have written about the latter under the heading A very bad report. The Pittilo report recommends both government regulation and more degrees in alternative medicine. Given that we now know that most alternative medicine doesn’t work, the idea of giving degrees in such subjects must be quite ludicrous to any thinking person.
The magazine Nature7 recently investigated the 16 UK universities who run such degrees. In the UK, first-year students at the University of Westminster are taught that “amethysts emit high yin energy” . Their vice chancellor, Professor Geoffrey Petts, describes himself a s a geomorphologist, but he cannot be tempted to express an opinion about the curative power of amethysts.
There has been a tendency to a form of grade inflation in universities—higher degrees for less work gets bums on seats. For most of us, getting a doctorate involves at least 3 years of hard experimental research in a university. But in the USA and Canada you can get a ‘doctor of chiropractic’ degree and most chiropractic (mis)education is not even in a university but in separate colleges.
Florida State University famously turned down a large donation to start a chiropractic school because they saw, quite rightly, that to do so would damage their intellectual reputation. This map, now widely distributed on the Internet, was produced by one of their chemistry professors, and it did the trick.
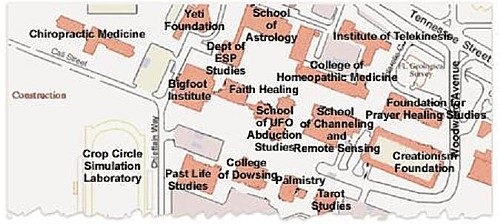
Other universities have been less principled. The New Zealand College of Chiropractic [whose President styles himself “Dr Brian Kelly”,though his only qualification is B. App Sci (chiro)] is accredited by the New Zealand Qualifications Authority (NZQA). Presumably they, like their UK equivalent (the QAA), are not allowed to take into account whether what is being taught is nonsense or not. Nonsense courses are accredited by experts in nonsense. That is why much accreditation is not worth the paper it’s written on.
Of course the public needs some protection from dangerous or fraudulent practices, but that can be done better (and more cheaply) by simply enforcing existing legislation on unfair trade practices, and on false advertising. Recent changes in the law on unfair trading in the UK have made it easier to take legal action against people who make health claims that cannot be justified by evidence, and that seems the best
way to regulate medical charlatans.
Conclusion
For most forms of alternative medicine—including chiropractic and acupuncture—the evidence is now in. There is now better reason than ever before to believe that they are mostly elaborate placebos and, at best, no better than conventional treatments. It is about time that universities and governments recognised the evidence and stopped talking about regulation and accreditation.
Indeed, “falsely claiming that a product is able to cure illnesses, dysfunction, or malformations” is illegal in Europe10.
Making unjustified health claims is a particularly cruel form of unfair trading practice. It calls for prosecutions, not accreditation.
Competing interests: None.
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716
URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Author information: David Colquhoun, Research Fellow, Dept of Pharmacology, University College London, United Kingdom (http://www.ucl.ac.uk/Pharmacology/dc.html)
Correspondence: Professor D Colquhoun, Dept of Pharmacology, University College London, Gower Street, London WC1E 6BT, United Kingdom. Fax: +44(0)20 76797298; email: d.colquhoun@ucl.ac.uk
References:
1. Gilbey A. Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. N Z Med J. 2008;121(1278). [pdf]
2. Evans A, Duncan B, McHugh P, et al. Inpatients’ use, understanding, and attitudes towards traditional, complementary and alternative therapies at a provincial New Zealand hospital. N Z Med J. 2008;121(1278).
3 Shapiro. Rose. Suckers. How Alternative Medicine Makes Fools of Us All Random House, London 2008. (reviewed here)
4. Singh S, Ernst E. Trick or Treatment. Bantam Press; 2008 (reviewed here)
5. Bausell RB. Snake Oil Science. The Truth about Complementary and Alternative Medicine. (reviewed here)
Oxford University Press; 2007
6. Colquhoun D. Science degrees without the Science, Nature 2007;446:373–4. See also here.
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10.
8. Libin K. Chiropractors called to court. Canadian National Post; June21, 2008.
9. Goldacre B. A menace to science. London: Guardian; February 12, 2007/
10. Department for Business Enterprise & Regulatory Reform (BERR). Consumer Protection from Unfair Trading Regulations 2008. UK: Office of Fair Trading.

