Academia
There have been some really excellent books about quackery this year. This isn’t one of them, because
 |
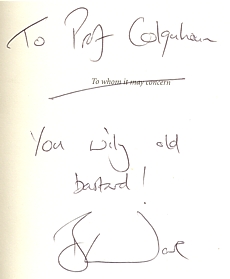
Nice dedication uh? |
it is about a lot more than quackery It is about the scientific method in general. and in particular about how often it is misunderstood by journalists. Abuse of evidence by the pharmaceutical industry is treated just as harshly as abuse of evidence by homeopaths and you get the low-down on both.
“More importantly, you will also see how a health myth can be created, fostered and maintained by the alternative medicine industry using all the same tricks on you, the public, which big pharma uses on doctors. This is about something much bigger than homeopathy.” (p.28)
Sir Iain Chalmers, a founder of the Cochrane Collaboration , co-author of the best lay text on evidence says: “Bad Science introduces the basic scientific principles to help everyone become a more effective bullshit detector”. And there is no more invaluable skill than being a bullshit detector.
Chalmers says also “Ben Goldacre has succeeded where the ‘public engagement in science’ organisations have so signally failed.” That is exactly right. ‘Public engagement’ has rapidly become bureaucratised, and at its worst, is no better than a branch of the university’s marketing department. This sort of public engagement corrupts as much as it enlightens. Goldacre enlightens, and he also makes you laugh.
In the introduction, Goldacre says
“You cannot reason people out of positions that they didn’t reason themselves into.” (p xii)
It’s a nice point, but the rest of the book makes a magnificent attempt to do just that.
There is quite a lot about medicine, of course, that’s his job, after all. But it isn’t all quackery by a long chalk Quackery is merely a good hook to hang the arguments on about how you distinguish what’s true from what isn’t. That’s partly because quacks make every mistake known to mankind (sometimes through ignorance, sometimes just to boost sales), and partly just because it is a topic that interests people, and with which they are bombarded every day I feel exactly the same. If I were to talk about the statistics of single ion channels, nobody would read it (big mistake -it’s fascinating), but if one can use the case of honey versus cough medicine to explain the analysis of variance, there is a chance that someone might find it interesting.
As much as anything, Goldacre’s book is about C.P. Snow’s two cultures. The chapters on the distortion and trivialisation of science in the media are just terrific.
“My basic hypothesis is this: the people who run the media are humanities graduates with little understanding of science, who wear their ignorance as a badge of honour. Secretly, deep down, perhaps they resent the fact that they have denied themselves access to the most significant developments in the history of Western thought from the past two hundred years.” Chapter 11, p. 207
“.. . . here is the information I would like from a newspaper to help me make decisions about my health, when reporting on a risk: I want to know who you’re talking about (e.g. men in their fifties): I want to know what the baseline risk is (e.g. four men out of a hundred will have a heart attack over ten years); and I want to know what the increase in risk is , as a natural frequency [not as relative risk] (two extra men out of that hundred will have a heart attack over ten years). I also want to know exactly what’s causing that increase in risk -an occasional headache pill or a daily tub full of pain-relieving medication for arthritis. Then I will consider reading your newspapers again, instead of blogs which are written by people who understand research , and which link reliably back to the original academic paper, so that I can double check their précis when I wish. ” (p. 242)
I detect some ambiguity in references to things that aren’t true. Sometimes there is magnanimity. At other times he is a grade one kick-ass ninja. For example
I can very happily view posh cosmetics -and other forms of quackery -as a special, self-administered, voluntary tax on people who don’t understand science properly (p. 26)
Of course nobody wants to ban cosmetics, or even homeopathy. But a lot of bad consequences flow from being over-tolerant of lies if you take it too far (he doesn’t). The lying dilemma and the training dilemma are among them. Some unthinking doctors will refer troublesome patients to a reflexologist. That gets the worried-well out of their surgery but neglects the inevitable consequence that Human Resources box-ticking zombies will then insist on having courses that teach the big toe is connected to the kidney (or whatever) so that reflexologists can have an official qualification in mystical mumbo-jumbo.
Is there anything missing from the book? Well inevitably. There are plenty of villains among the peddlers of nutri-bollocks, and in the media. But there isn’t much about the people who seem to me to be in some ways even worse. What about the black-suited men and women in the Ministry of Health and in some vice-chancellors’ chairs who betray their institutions and betray the public through some unfathomable
mixture of political correctness, scientific ignorance and greed? What about the ludicrous behaviour of quangos like Skills for Health? You have to wait right to the end of the book to hear about universities. But when it comes, it is well worth the wait.
“I’m not surprised that there are people with odd ideas about medicine, or that they sell those ideas. But I am spectacularly, supremely, incandescently unimpressed when a a university starts to offer BSc science courses in them.” (p. 317)
It’s almost worth buying Ben Goldacre’s book for that sentence alone.
This book is a romp through the folly, greed and above all the ignorance of much in our society. It’s deeply educational. And it makes you laugh. What more could you want?
The publication of Gilbey’s paper and my editorial in the New Zealand Medical Journal (NZMJ) led to a threat of legal action by the NZ Chiropractors’ Association Inc for alleged defamation. After publishing a defiant editorial, the editor of the NZMJ offered chiropractors the chance to put their case.
In the last issue of NZMJ (22 Aug 2008) three letters appeared. One was from Brian Kelly, (President, New Zealand College of Chiropractic) [download letter]. One was from Karl Bale (CEO/Registrar, Chiropractic Board New Zealand) [download letter], and one was from Simon Roughan (Registered Chiropractor and Acting President of the New Zealand Chiropractors’ Association) [download letter].
In the current issue (5 September 2008) Gilbey, Ernst and I responded.{download Gilbey response] [download Ernst response].
Here’s mine. The printed version differs in minor ways [download pdf]
| I’m grateful for the opportunity to reply to the defences of chiropractic from Kelly1, Roughan2 and Bale3 in your last issue.
I’d like first to deal with the minor matter of titles, before getting on to the more important question of vidence. I notice that Brian Kelly signs his letter “Dr Brian Kelly B App Sci (Chiro)” in his letter to NZMJ. He seems to be a bit less careful in his use of titles on his own school’s web site where his president’s welcome4 is signed simply “Dr Brian Kelly”, a title he adopts in at least three other places. Karl Bale3 (CEO/Registrar, Chiropractic Board New Zealand) points out that “Failure to qualify the use of the title ‘Doctor’ may contravene the provisions of the Medical Practitioners Act 1995”. One wonders whether Bale has done anything to stop Kelly’s apparent breaches of this rule? This example makes on wonder whether the Chiropractic Board take its responsibilities seriously? It seems often to be the case that ‘voluntary self-regulation’ doesn’t work, because there are too many vested interests. Karl Bale points out that some ruthless sales methods characteristic of chiropractic are also contrary to the Chiropractic Board’s code of ethics. One would hope their well-known antipathy to vaccination and to medicine as a whole were also considered unethical. These practices seem to continue so the the code of ethics It seems to me quite remarkable that none of the letters mentions the ‘subluxation’ that lies at the heart of their subject6. Could that be because they are reluctant to admit openly that it is a mere metaphysical concept, that no one can see or define? It is sad that so many patients are subjected to X-rays in search of this phantom idea. It is this metaphysical nature of chiropractic that separates it quite clearly from science. Brian Kelly says “How can any reader take seriously, anything suggested by a writer who opines that a 19th Century journalist possessed superior “intellectual standards” to “the UK’s Department of Health” and “several university vice chancellors”. The views of the Davenport Leader on chiropractic were mild compared with those of the great H.L. Mencken (1924)7 who wrote “This preposterous quackery flourishes lushly in the back reaches of the Republic, and begins to conquer the less civilized folk of the big cities….” The problem is that the Department of Health is full of arts graduates who may be very good at classics but can’t understand the nature of evidence. And the UK has one vice-chancellor, a geomorphologist, who defends a course in his university that teaches that “amethysts emit high yin energy”8 I’ll admit, though, that perhaps ‘intellect’ is not what’s deficient in this case, but rather honesty. Your correspondents seem to confuse the duration of a course with its intellectual content. You can study homeopathy for years too, but after all that they are still treating sick people with medicines that contain no medicine. Anyone who works in a university knows that you can easily get accreditation for anything whatsoever if you choose the right people to sit on the committee. I have seen only too many of these worthless pieces of paper. “Amethysts emit high yin energy”8 was part of an accredited course (at the University of Westminster) too. Need I say more? Now to the real heart of the problem, namely the question of evidence. Brian Kelly says that the book by Singh and Ernst9 shows “extreme bias”, but what that book actually shows is an extremely scrupulous regard for evidence, Ernst is in a better position to do this than just about anyone else. He has qualified and practised both regular and alternative medicine, and he was appointed to his present position, as professor of complementary and alternative medicine to assess the evidence. Perhaps most importantly of all, his position allows him to do that assessment with complete lack of bias because, unlike Kelly, his livelihood does not depend on any particular outcome of the assessment. I’m afraid that what Kelly describes as “extreme bias” is simply a display of pique because it has turned out that when all the evidence is examined dispassionately, the outcome is not what chiropractors hoped. The fact of the matter is that when you look at all of the evidence, as Singh & Ernst do, it is perfectly clear that chiropractic is at best no better than conventional treatments even for back pain. For all other conditions its benefits fail to outweigh its risks – contrary to the many claims by chiropractors. Both the New Zealand and the UK governments have got themselves into an impossible position by giving official recognition to chiropractic before the evidence was in. Since the conventional manipulative treatments are cheaper, and may be well be safer, and because they involve no quasi-religious ideas like “subluxation” or “innate intelligence”, the only reasonable conclusion is that there is no need for chiropractic to exist at all. They do nothing they do that could not be done as well by medical practitioners and physiotherapists. What will governments do about that, I wonder? David Colquhoun 1. Kelly, B. New Zealand College of Chiropractic response to 2. Roughan, S. Setting the record straight: New Zealand Chiropractors’ Association response letter. NZMJ 22 3. Bale, 4. http://www.nzchiro.co.nz/about_president.php 6. http://www.chirobase.org/01General/chirosub.html 7. http://www.geocities.com/healthbase/mencken_chiro.html 8. http://dcscience.net/?p=227 9. Singh S, Ernst E. Trick or Treatment. Bantam Press; 2008 |
The wars within chiropractic
Although the chiropractors seem to be rather upset by the criticisms that have been levelled against them, the most interesting war is not between chiropractors and people who think that medicine should not be based on metaphysics. It’s the war within chiropractic itself.
The internecine wars within chiropractic have been going almost from the day it was invented. The (ex-)insider’s view gives us a rare insight into what chiropractic schools actually do. Now support has come from a rather unexpected quarter. An article by five chiropractors has just appeared by Murphy et al. (Chiropractic & Osteopathy, 2008, 16:10).
Although the authors declare that they have “a financial interest in the success” of chiropractic, the changes that they propose are so drastic that, if implemented, tthey would leave little left to distinguish chiropractic from, say, physiotherapy. The authors ask the very pertinent question, ‘why is it that podiatry (chiropody in the UK) is well accepted and chiropractic remains on the controversial fringe of medicine?.. Here are some quotations.
“It is also vital that those chiropractors who dogmatically oppose common public health practices, such as immunization [15] and public water fluoridation, cease such unfounded activity.”
“We are concerned that the common perception (which is well supported, in our experience) that chiropractors are only interested in “selling” a lifetime of chiropractic visits may be one of the primary factors behind our low standing in the minds of members of the public [2].”
“One of the problems that we encounter frequently in our interaction with chiropractic educational institutions is the perpetuation of dogma and unfounded claims. Examples include the concept of spinal subluxation as the cause of a variety of internal diseases and the metaphysical, pseudo-religious idea of “innate intelligence” flowing through spinal nerves, with spinal subluxations impeding this flow. These concepts are lacking in a scientific foundation [27] [28] [29] and should not be permitted to be taught at our chiropractic institutions as part of the standard curriculum. Much of what is passed off as “chiropractic philosophy” is simply dogma [30], or untested (and, in some cases, untestable) theories [27] which have no place in an institution of higher learning, except perhaps in an historical context.”
“The Council on Chiropractic Education requirement of 250 adjustments forces interns to use manipulation on patients whether they need it or not, and the radiographic requirement forces interns to take radiographs on patients whether they need them or not.”
“They [podiatrists] did not invent a “lesion” and a “philosophy” and try to force it on the public. They certainly did not claim that all disease arose from the foot, without any evidence to support this notion. The podiatric medical profession simply did what credible and authoritative professions do [32] – they provided society with services that people actually wanted and needed.”
“In the beginning, DD Palmer invented a lesion, and a theory behind this lesion, and developed a profession of individuals who would become champions of that lesion. This is not what credible professions do.”
“In the interim it [chiropractic] has seen its market share dwindle from 10% of the population [4] to 7.5% [3] [42]. Even amongst patients with back pain, the proportion of patients seeing chiropractors dropped significantly between 1987 and 1997, a period of time in which the proportion seeing both medical doctors and physical therapists increased [43].”
“When an individual consults a member of any of the medical professions, it is reasonably expected that the advice and treatment that he or she receives is based in science, not metaphysics or pseudoscience.”
“The chiropractic profession has an obligation to actively divorce itself from metaphysical explanations of health and disease as well as to actively regulate itself in refusing to tolerate fraud, abuse and quackery, which are more rampant in our profession than in other healthcare professions [46].”
“Podiatric medicine is a science-based profession dedicated to the diagnosis and treatment of foot disorders. Foot reflexology is a metaphysically-based group consisting of non-physicians who believe that many physical disorders arise from the foot. Podiatrists have rejected foot reflexology as an unproven and unscientific practice, and do not consider it part of mainstream podiatric practice.”
“We must finally come to the painful realization that the chiropractic concept of spinal subluxation as the cause of “dis-ease” within the human body is an untested hypothesis [27]. It is an albatross around our collective necks that impedes progress.”
All this, remember, comes from five chiropractors. That looks like all out war between their view of chiropractic and that taught in New Zealand College of Chiropractic, and, in the UK by the three chiropractic colleges in the UK.
Follow-up
A report in the New Zealand Herald (18 September 2008) is rather relevant to all this.
Chiropractor to apologise after patient has stroke
A chiropractor has been recommended to apologise to a woman patient who suffered a stroke after he treated her.
The case report is here.
The Advertising Standards Authority has had a bit to say about chiropractors too.
After the announcement that the University of Central Lancashire (Uclan) was suspending its homeopathy “BSc” course, it seems that their vice chancellor has listened to the pressure, both internal and external, to stop bringing his university into disrepute.
An internal review of all their courses in alternative medicine was announced shortly after the course closure. Congratulations to Malcolm McVicar for grasping the nettle at last. Let’s hope other universities follow his example soon.
I have acquired, indirectly, a copy of the announcement of the welcome news.
| Homeopathy, Herbalism and cupuncture Concern has been expressed by some colleagues as to whether the University should offer courses in homeopathy, Herbalism and Acupuncture. Therefore, to facilitate proper discussion on this matter I have set up a working party to review the issues. I have asked Eileen Martin, Pro Vice-Chancellor and Dean of the Faculty of Health, to lead this working party and report to me as soon as possible. Whilst the review is taking place, we need to recognise that there are students and staff studying and teaching on these courses which have satisfied the University’s quality assurance procedures and been duly validated. I would therefore ask that colleagues would refrain from comment or speculation which would cause concern to these students and staff. Staff who wish to express their views on this issue should direct these to Eileen Martin, by the end of September. Regards Malcolm McVicar Vice-Chancellor |
Times Higher Education today reports
“The University of Central Lancashire is to review all its courses in homoeopathy, herbalism and acupuncture after some staff said it should not be offering degrees in “quackery”, Times Higher Education has learnt.
A university spokesman said: “As a university we value and practise transparency and tolerance and welcome all academic viewpoints.”
(Later, an almost identical version of the story ran on the Times Online.)
So far, so good. But of course the outcome of a committee depends entirely on who is appointed to it. Quite often such committees do no more than provide an internal whitewash.
It does seem a bit odd to appoint as chair the dean of the faculty where all these course are run, and presumably generate income. Eileen Martin has often appeared to be proud of them in the past. Furthermore, the whole investigation will (or should) turn on the assessment of evidence. It needs some knowledge of the design of clinical trials and their statistical analysis, As far as I can see, Ms Martin has essentially no research publications whatsoever.
I also worry about a bit about “satisfied the University’s quality assurance procedures and been duly validated”. One point of the investigation should be recognise frankly that the validation process is entirely circular, and consequently worth next to nothing. It must be hard for a vice-chancellor to admit that, but it will be an essential step in restoring confidence in Uclan.
Let’s not prejudge though. If there are enough good scientists on the committee, the result will be good.
I hope that transparency extends to letting us know who will be doing the judging. Everything depends on that.
Follow-up
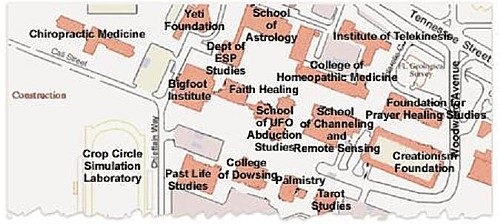
Well well, there’s a coincidence, Once again, the week after a there is an announcement about degrees in witchcraft, what should pop up again in the column of the inimitable Laurie Taylor in THE. The University of Poppleton’s own Department of Palmistry.
| Letter to the editor
Dear Sir I was shocked to see yet another scurrilous attack upon the work of my department in The Poppletonian. Although Palmistry is in its early days as an academic discipline it cannot hope to progress while there are people like your correspondent who insist on referring to it as “a load of superstitious nonsense which doesn’t deserve a place on the end of the pier let alone in a university”. A large number of people claim to have derived considerable benefit from learning about life lines, head lines and heart lines and the role of the six major mounts in predicting their future. All of us in the Palmistry Department believe it vitally important that these claims are rigorously examined. How else can science advance? Yours sincerely, |
The Times today has given s good showing for my comment piece. It gives the case against following the advice of the Pittilo report. It simply makes no sense to have government regulation of acupuncture, herbal medicine, traditional Chinese medicine until such time as there is evidence that they work. It makes even less sense to have BSc degrees in them. The Department of Health should have more sense that to use the Prince of Wales as its scientific advisor.
Let’s hope that the recent example set by the University of Central Lancashire is the start of trend for vice-chancellors to appreciate that running such degrees brings their universities into disrepute.
I can only apologise for the dreadful title that The Times’ sub-editors put on the piece, My original title was
A bad report for the vice chancellor
The Pittilo report to the Department of Health will endanger the public and corrupt universities. There is a better way.
I like that much better than “Regulate quack nedicine? I feel sick”.
But, oh dear, the picture that I sent them is on the left, but what appeared is on the right. Spot the difference.
 |
 |
Well now, at least, I can feel I have something in common with Isambard Kingdom Brunel.
Follow-up
It so happens that Professor Pittilo wrote a letter to Times Higher Education this week. I fear that it provided a yet more evidence that he hasn’t really quite got the hang of evidence.
The Lancashire Evening Post catches up with the UCLan story, two days after you read it here.
A reply from Professor Pittilo
This response to the op-ed of 29th August appeared as a letter
in the Times on Sept 2.
| Public health needs protection
Regulation of acupuncture and herbal medicine has been subject to much scrutiny Sir, Professor Colquhoun’s campaign to discredit our report (“Regulate quack medicine? I feel sick,” Aug 29) is in danger of placing public health at risk. He is entitled to challenge existing evidence for the effectiveness of complementary and alternative medicine (CAM) but fails to acknowledge the key recommendation from the steering group on the essential need to demonstrate efficacy, safety and quality assurance as a prerequisite for NHS funding. Professor Colquhoun dismisses CAM because of the absence of a rigorous scientific foundation and he asserts that to teach and practise it is unethical. Survey data consistently demonstrates very high demand for CAM with one report estimating that 22 million visits involving 10.6 per cent of the population in England alone occurred in 2008. This demand is one reason why his alternative model of trade law enforcement will not work. He may argue that these people are uncritical recipients of nonsense, but data from the Medicines and Healthcare products Regulatory Agency confirm that they are at significant risk from poor practice. It is essential that we protect the public by implementing statutory regulation alongside demanding evidence of efficacy. Professor Colquhoun’s resistance to the teaching of science to CAM practitioners will do little to help them to critically evaluate effectiveness. Professor Michael Pittilo Chair of the Department of Health Steering Group |
And Pittilo wrote in similar vein to Times Higher Education.
Science vital to health study28 August 2008 Your feature on some members of staff at the University of Central Lancashire attacking science degrees in complementary and alternative medicine (“Staff attack science degrees in alternative health”, 7 August) raises a number of concerns. It is up to any university, taking account of the expert views of staff and external peer review, to determine the appropriate title and award for any degree. It is encouraging to note from the feature that new courses The recent report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and other Traditional Medicine There is no doubt that courses that provide a solid scientific foundation will greatly assist CAM practitioners in establishing evidence-based practice. It would be most unfortunate if the reported resistance to degree titles led to those wishing to practise acupuncture or herbal medicine receiving less hard science than they might have. To say that acupuncture and herbal medicine degrees have no academic justification appears arrogant in the extreme. Although it is certainly true that some content may not be scientific, this does not invalidate the legitimacy of these courses at degree level, a fact borne out by their successful validation in a number of universities. R. Michael Pittilo, Principal and vice-chancellor, The Robert Gordon University. |
This one got excellent responses from Kevin Smith (University of Abertay, Dundee), and from Peter J. Brophy (Professor of veterinary anatomy and cell biology University of Edinburgh). This was my comment to THE
There are a few very obvious responses to Professor Pittilo’s letter
For many alternative therapies the “philosophy” is simply incompatible with science. One obvious example is homeopathy. On Mondays and Wednesdays (science days) the students will be required to learn that response increases with dose. On Tuesdays and Thursdays will be taught the opposite. But for the exam they must reproduce only the latter (nonsensical) idea because their aim is to get a job as a homeopath. That makes nonsense of the idea of a university.
This seems to constitute a recognition that the evidence is still very inadequate. The time to start degrees, and the time to give official government recognition, is after the evidence is in, not before. What happens if you start degrees and then find that the subject is so much nonsense? Well, that has already happened in several areas of course. But the people who accredit the course and who act as external examiners just happen to be fervent believers in that nonsense, so all appears to be well (to bean counters anyway).
There is, as it happens, a great deal of evidence now about acupuncture, but the authors of the report do not seem to be aware of it. I recommend Barker Bausell’s book on the topic. If students are educated science, like what constitutes evidence, and our current understanding of words like “energy”, they would have to disavow the subject that there are supposed to training to practise
No, it is not a matter of arrogance, just a matter of careful attention to the evidence. Attention to evidence was notably absent in Prof Pittilo’s report, perhaps because his committee consisted entirely of people who earn their living from the subjects they were supposed to be assessing.
I have had the misfortune to have waded through a mound of such validation documents. The one thing they never consider is whether the treatment works. Sad to say, these validations are not worth the paper they are written on. |
My original piece on Integrative Baloney@Yale was posted on May 16th, after I got back from a visit there. The talk I gave there included a short video. My movie, Integrative baloney@Yale, was made entirely from clips taken from Yale’s own YouTube movies which showed something approaching three hours of its “1st Annual Scientific [sic] symposium”, entitled “Complementary and Alternative Medicine: Evidence for Integration”. I had merely interspersed a few titles to show the worst scientific absurdities of that rather pathetic event. YouTube removed the movie last week.
You can download the movie here [15.8 Mb, wmv file].
It should soon reappear on YouTube (actually it took over a month and several reminders, but eventually they kept their word in the end).
Yale’s lawyers had written to YouTube, to have my movie removed. I guess if you have no evidence, all you can do is resort to law to suppress the views of those who have the temerity to point out that the emperor is naked. Last week it was New Zealand Chiropractors’ Association Inc. This week the rather more substantial Yale University. We live in interesting times.
This is what I got on 15th August.
| Dear Member
This is to notify you that we have removed or disabled access to the following material as a result of a third-party notification by Yale University, Yale School of Medicine (CME) claiming that this material is infringing: Integrative baloney@Yale: http://uk.youtube.com/watch?v=HEl2fhfGBdI Please Note: Repeated incidents of copyright infringement will result in the deletion of your account and all videos uploaded to that account. In order to prevent this from happening |
If you clicked on the link you saw
“This video is no longer available due to a copyright claim by Yale University, Yale School of Medicine (CME)”
It seems that Yale’s Continuing Medical Education (CME) department was responsible.
Of course Yale is correct. I expect they own the copyright of their original movies, but they are not what I posted. I would argue that selecting 6 minutes from a 3 hour original amounts to “fair quotation”, no different from when one cites a short passage from somebody else’s book or paper. Perhaps Yale was just a bit jealous that my movie was getting viewed a lot more times than theirs. Or perhaps they were a bit peeved that a Google search for “Yale Integrative Medicine” produced my movie as #2 (add the word movie and I was #1).
My movie seems to me to be fair comment from someone who is a pharmacologist by trade. Apparently it didn’t seem that way to the apparatchiks of Yale Medical School, who seem to think that academic arguments should be settled by paying lawyers to suppress views they don’t like, rather than by rational discussion.
It’s interesting that the three hours of Yale’s own movie have also vanished from YouTube. Could that be because they realise that the remarks made at the meeting are so embarrassing intellectually that it would be better not to make them public? Actually, no.
What does Yale CME say?
Rather than publishing this straight away, I thought it better to delve a bit further into what had happened. I lodged an appeal with YouTube and I wrote to Ronald J. Vender, MD (Associate Dean, YSM Clinical Affairs, CMO, Yale Medical Group, Medical Director, Yale CME ). The outcome was rather interesting.
First, it turned out that the original posting of the three hours of the symposium proceedings on YouTube was itself unauthorised, which is why it suffered the same fate as my movie.
Dr Vender told me that he is new to the job, and didn’t know about the incident. What’s more surprising, he said he “did not know an Integrative Program even existed at Yale”. That does seem a bit odd indeed for an Associate Dean of Clinical Affairs.
However, Dr Vender turned out to be a very reasonable man,.After some amiable correspondence over the weekend, it took him only a day and a half to sort the matter out. After talking to Yale’s attorney, he wrote on 19th August, thus
“The University attorney believes that there is in fact a difference between the initial unauthorized filming of an entire conference as opposed to quoting from that conference. Therefore, she has agreed to withdraw the injunction that has been imposed on your use of the material. YouTube will be contacted.”
That’s good for me, but it isn’t the main thing. The movie would doubtless have been seen by more people if Yale had tried to maintain the ban. Much more impressively, Dr Vender also said
“As for this particular program, I will be speaking with Dr Belitsky and the program directors to encourage them to adopt a more critical view of the scientific basis for claims made by proponents of CAM. They will also be encouraged to develop a future program that includes faculty who have opposing points of view.”
It remains to be seen what actually happens, but so far, so good.
What next?
The removal of the original videos of the meeting is understandable because they were pretty embarrassing to Yale. But can that be the real reason? I was told that it is simply because their posting was “unauthorised”. But Yale Continuing Medical Education still boasts about the meeting on their own web site. They describe the meeting as “successful”, but if they are so proud of it, why remove the video from YouTube whether it was authorised or not? We are told
“The symposium, accredited for 7.5 AMA PRA Category 1 Credits, began what is hoped to be a long tradition at the Yale School of Medicine.”
They give credits for such miseducation?
Dr Katz’s phrase “we need a more fluid concept of evidence” now gets about 148 hits in Google, since I first helped him to publicise it.
Two of the six “learning objectives” that Yale CME lists for this symposium are particularly revealing.
- Describe therapeutic benefits and recent scientific evidence supporting a wide range of safe and practical complementary treatments, including acupuncture, massage, yoga, meditation, nutrition and exercise
- Identify and discuss barriers to CAM use, practice and research, as well as propose ways of overcoming these barriers
‘Describe the evidence supporting complementary treatments’? But don’t on any account describe the much more substantial evidence that does not support them? A question (or “learning objective”) put in this loaded way is the very antithesis of education.
Equally the second ‘learning objective’ carries with it the assumption that CAM works, otherwise why would anyone want to overcome the barriers to it?
This is indoctrination, not education. It betrays everything that a university should stand for.
Let’s hope the new head of CME, the admirable Dr Vender, succeeds in doing something about it
Follow-up
Success!. Well I think it is success. On 26 November 2008, the admirable Dr Vender wrote to me as follows.
“I do not know if another CAM/Integrative Medicine program is planned at Yale. However, based on the new ACCME standards, this program does not fulfil the standards for receiving CME accreditation (by my interpretation of the standards). At least one of last year’s program directors has been notified already.”
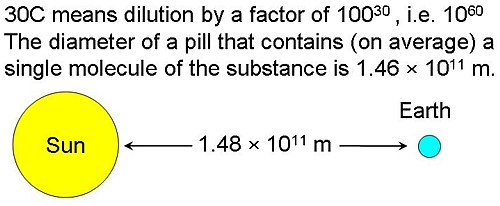
Samuel Hahnemann (1755 – 1843) was the originator of homeopathy. He was clearly a well-intentioned man.. There is good reason to believe that he thought dilution could not go on for ever, but he died 22 years before it became possible to calculate that his favourite 30C dilution already contained nothing at all.
| The bible of homeopaths is Hahnemann’s Organon der rationellen Heilkunde, “Organon of the Medical Art”. His views on dosage, as expressed in the six editions of this book are almost as self-contradictory as the other bible. Hahnemann’s writing about ‘vital spirits’ sounds very silly now, but it is language that was quite common at the end of the 18th century, before much was known about medicine or physiology. But his interest in chemistry was entirely sensible. | 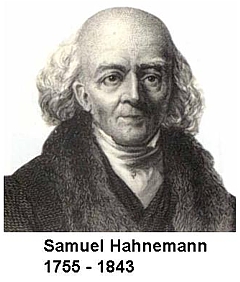 |
Before 1800 Hahnemann started out with the very high doses that were conventional at the time. Unlike most of his contemporaries, he was smart enough to realise that giving 50 g of antimony was killing people so he kept reducing the dose until it was no longer toxic. Unfortunately he (like almost everyone else at the time) didn’t know about controls so he mistook lack of toxicity (because the dose was zero) for a beneficial effect. Nonetheless, for most of his life he did not advocate the extreme dilutions that many modern homeopaths use routinely.
In The Life and Letters of Dr Samuel Hahnemann by Thomas Lindsley Bradford, M.D.(or see Google books edition of the Organon), there is an interesting passage. According to the edition here pp. 237 – 238), this was a note attached to para. #283 in the first edition of the Organon.
| ” The doctrine of the divisibility of matter teaches us that we cannot make a part so small that it shall cease to be something, and that it shall not share all the properties of the whole.” |
Here Hahnemann refers to the doctrine of divisibility, but appears to be saying that dilution can go on for ever. But he also says something that directly contradicts this view (Organon, Dudgeon’s translation see also here, page 239 ). The emphasis is mine.
| “I must say that these procedures seem to show chiefly how high one can go with the potentized attenuation of medicines without their action on the human health becoming nil.“ |
Although this claims that you can dilute a lot, it also admits that if the dilution goes too far the effect would eventually vanish, contrary to the usual homeopathic “principle” that it should keep getting stronger and stronger. and contrary to Hahnemann’s suggestions in other places that he thought matter was infinitely divisible.
This passage shows quite clearly that Hahnemann did not believe that his medicines would work if they were diluted so much that that there were no molecules left. That he believed this is confirmed by a letter that Hahnemann wrote in a letter to a Dr Schreter dated September 13th, 1829. This letter reprimanded Schreter for advocating extremely high dilutions.
| “there must be some limit to the thing. It cannot go on to infinity” The original German version was “Es muss ein Ende geben, es kann nicht bis ins Unendliche weitergehen” |
This confirms that Hahnemann was aware of, and accepted, that matter was not infinitely divisible and his medicines would not work if they contained nothing of the original material.
This attitude is actually not at all surprising, because Hahnemann was an educated man and he had a particular interest in chemistry. He cannot have failed to be aware of Dalton’s atomic theory, which was published between 1805 – 1810, while Hahnemann was writing the first edition of the Organon.
Peter Morrell, in Hahnemann and Homeopathy, says
“These were obviously developments that Hahnemann could not have failed to know about and indeed, was thoroughly excited about, It is clear from many of his asides that he regarded chemistry as the most important science.”
What is astonishing is that I can find no example of Hahnemann ever having mentioned Dalton or Avogadro. Perhaps he was a bit scared by the implications of their suggestions that molecules could not be divided without changing their nature.
The first edition of the Organon was published in 1810. but in the 5th edition appeared 1833, ten years before his death, These dates turn out to be important.
John Dalton (1776 – 1844) was able to estimate relative atomic masses of various molecules, the smallest unit that a chemical can exist in without losing irs identity. His values were soon improved by Amadeo
Avogadro (1776 – 1856), in 1811. Avogadro made the very important proposal that the volume of a gas (strictly, of an ideal gas ) is proportional to the number of atoms or molecules that are present. More precisely, the relationship between the masses of the same volume of different gases (at the same temperature and pressure) corresponds to the relationship between their respective molecular weights. Hence, the relative molecular mass of a gas can be calculated from the mass of a sample of known volume.
BUT neither Avogadro nor Dalton knew how many molecules there were in a given mass of a substance
This is absolutely crucial because it means that, although Hahnemann realised that there was a limit to the dilutions that could be used, he had no way of knowing what that limit was,
The answer to that question was discovered only in 1865, 22 years after the death of Hahnemann. It was discovered not by Avogadro, but by Johann Josef Loschmidt (1821 – 1895). It is Loschmidt, not Avogadro, who discovered the crucial numerical value of ‘Avogadro’s number‘, and in the German literature it is known, properly, as Loschmidt’sche Zahl.
This number is 6.022 x 1023 molecules per mole. One mole of a pure compound is its molecular mass in grams. The molecular mass of carbon (relative to hydrogen) is 12, so 12 grams of carbon contain 6.022 x 1023 carbon atoms. The molecular mass of of strychnine is 334.4 so 334.4 grams of strychnine contain 6.022 x 1023 strychnine molecules.
Armed with the numerical value of Avogadro’s number, it is easy to calculate that a 30 C homeopathic dilution contains nothing whatsoever. More precisely, it would contain, on average, a single molecule in spherical pill with a diameter equal to the distance from the earth to the sun.
But Hahnemann could not have known that. If had lived another 25 years he would almost certainly have renounced the idea of using 30 C dilutions.
He had a good excuse for getting it wrong. He was dead before the knowledge existed to do the calculation
But modern homeopaths have no excuse whatsoever for believing the impossible.
Hahnemann would have thought they were nuts, I suspect. He was too intelligent to believe that medicines that contain no medicine could be effective. In his words, “It cannot go on to infinity”.
Acknowledgement
I very grateful to ‘ Lindy’ for help in checking the references that are cited here, and for helpful discussions.
The article below is an editorial that I was asked to write for the New Zealand Medical Journal, as a comment on article in today’s edition about the misuse of the title ‘doctor’ by chiropractors [download pdf]. Titles are not the only form of deception used by chiropractors, so the article looks at some of the others too. For a good collection of articles that reveal chiropractic for what it is, look at Chirobase
THE NEW ZEALAND
MEDICAL JOURNAL
Journal of the New Zealand Medical Association
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716

URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Doctor Who?
Inappropriate use of titles by some alternative “medicine” practitioners
David Colquhoun
Who should use the title ‘doctor’? The title is widely abused as shown by Gilbey1 in this issue of the NZMJ in an article entitled Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. Meanwhile, Evans and colleagues 2, also in this issue, discuss usage and attitudes to alternative treatments.
Gilbey finds that the abuse of the title doctor is widespread and that chiropractors are the main culprits. An amazing 82% of 146 chiropractics used the title Doctor, andL most of them used the title to imply falsely that they were registered medical practitioners.
Although it is illegal in New Zealand to do that, it seems clear that the law is not being enforced and it is widely flouted. This is perhaps not surprising given the history of chiropractic. It has had a strong element of ruthless salesmanship since it was started in Davenport, Iowa by D.D. Palmer (1845–1913). His son, B.J. Palmer, said that their chiropractic school was founded on “a business, not a professional basis. We manufacture chiropractors. We teach them the idea and then we show them how to sell” (Shapiro 2008)3 It is the same now. You can buy advice on how to build “build high-volume, subluxation-based, cash-driven, lifetime family wellness practices”
In her recent book3 , Rose Shapiro comments on the founder of chiropractic as follows.
“By the 1890s Palmer had established a magnetic healing practice in Davenport, Iowa, and was styling himself “doctor”. Not everyone was convinced, as a piece about him in an 1894 edition of the local paper, the Davenport Leader, shows.
A crank on magnetism has a crazy notion hat he can cure the sick and crippled with his magnetic hands. His victims are the weak-minded, ignorant and superstitious,those foolish people who have been sick for years and have become tired of the regular physician and want health by the short-cut method he has certainly profited by the ignorance of his victim. His increase in business shows what can be done in Davenport, even by a quack.”
D.D. Palmer was a curious mixture: grocer, spiritual healer, magnetic therapist, fairground huckster, religious cult leader—and above all, a salesman. He finally found a way to get rich by removing entirely imaginary “subluxations”.
Over 100 years later, it seems that the “weak-minded, ignorant, and superstitious” include the UK’s Department of Health, who have given chiropractics a similar status to the General Medical Council.
The intellectual standards of a 19th Century Mid-Western provincial newspaper journalist are rather better than the intellectual standards of the UK’s Department of Health, and of several university vice-chancellors in 2007.
Do the treatments work?
Neither Gilbey nor Evans et al. really grasp the nettle of judging efficacy. The first thing one wants to know about any treatment —alternative or otherwise — is whether it works. Until that is decided, all talk of qualifications, regulation, and so on is just vacuous bureaucratese. No policy can be framed sensibly until the question of efficacy has been addressed honestly.
It is one good effect of the upsurge of interest in alternative treatments that there are now quite a lot of good trials of the most popular forms of treatments (as well as many more bad trials). Some good summaries of the results are now available too. Cochrane reviews set the standard for good assessment of evidence. New Zealand’s Ministry of Health commissioned the Complementary and Alternative Medicine
website to assess the evidence, and that seems to have done a good job too. Their assessment of chiropractic treatment of low back pain is as follows:
There appears to be some evidence from one systematic review and four other studies, although not conclusive, that chiropractic treatment is as effective as other therapies but this may be due to chance. There is very little evidence that chiropractic is more effective than other therapies.
And two excellent summaries have been published as books this year. Both are by people who have had direct experience of alternative treatments, but who have no financial interest in the outcome of their assessment of evidence. The book by Singh and Ernst4 summarises the evidence on all the major alternative treatments, and the book by Bausell5 concentrates particularly on acupuncture, because the author was for 5 years involved in research in that area, Both of these books come to much the same conclusion about chiropractic. It is now really very well-established that chiropractic is (at best) no more effective than conventional treatment. But it has the disadvantage of being surrounded by gobbledygook about “subluxations” and, more importantly, it kills the occasional patient.
Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
The chiropractors of Alberta (Canada) and the Alberta Government are now facing a class-action lawsuit8. The lead plaintiff is Sandra Nette. Formerly she was a fit 41 year old. Now she is tetraplegic. Immediately
after neck manipulation by a chiropractor she had a massive stroke as a result of a torn vertebral artery.
Acupuncture comes out of the assessments equally badly. Bausell (2007) concludes that it is no more than a theatrical placebo.
Are the qualifications even real?
It is a curious aspect of the alternative medicine industry that they often are keen to reject conventional science, yet they long for academic respectability. One aspect of this is claiming academic titles on the flimsiest of grounds. You can still be held to have misled the public into thinking you are a medical
practitioner, even if you have a real doctorate. But often pays to look into where the qualifications come from.
A celebrated case in the UK concerned the ‘lifestyle nutritionist’, TV celebrity and multi-millionaire, Dr Gillian McKeith, PhD. A reader of Ben Goldacre’s excellent blog, badscience.net did a little investigation. The results appeared in Goldacre’s Bad Science column in the Guardian9.
She claimed that her PhD came from the American College of Nutrition, but it turned out to come from a correspondence course from a non-accredited US ‘college’. McKeith also boasted of having “professional membership” of the American Association of Nutritional Consultants, for which she provided proof of her degree and three professional references.
The value of this qualification can be judged by the fact that Goldacre sent an application and $60 and as a result “My dead cat Hettie is also a “certified professional member” of the AANC. I have the certificate hanging in my loo”.
Is the solution government regulation?
In New Zealand the law about misleading the public into believing you are a medical practitioner already exists. The immediate problem would be solved if that law were taken seriously, but it seems that it is not.
It is common in both the UK and in New Zealand to suggest that some sort of official government regulation is the answer. That solution is proposed in this issue of NZMJ by Evans et al2. A similar thing has been proposed recently in the UK by a committee headed by Michael Pittilo, vice-chancellor of Robert Gordon’s University, Aberdeen.
I have written about the latter under the heading A very bad report. The Pittilo report recommends both government regulation and more degrees in alternative medicine. Given that we now know that most alternative medicine doesn’t work, the idea of giving degrees in such subjects must be quite ludicrous to any thinking person.
The magazine Nature7 recently investigated the 16 UK universities who run such degrees. In the UK, first-year students at the University of Westminster are taught that “amethysts emit high yin energy” . Their vice chancellor, Professor Geoffrey Petts, describes himself a s a geomorphologist, but he cannot be tempted to express an opinion about the curative power of amethysts.
There has been a tendency to a form of grade inflation in universities—higher degrees for less work gets bums on seats. For most of us, getting a doctorate involves at least 3 years of hard experimental research in a university. But in the USA and Canada you can get a ‘doctor of chiropractic’ degree and most chiropractic (mis)education is not even in a university but in separate colleges.
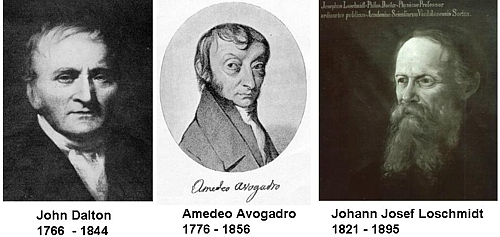
Florida State University famously turned down a large donation to start a chiropractic school because they saw, quite rightly, that to do so would damage their intellectual reputation. This map, now widely distributed on the Internet, was produced by one of their chemistry professors, and it did the trick.
Other universities have been less principled. The New Zealand College of Chiropractic [whose President styles himself “Dr Brian Kelly”,though his only qualification is B. App Sci (chiro)] is accredited by the New Zealand Qualifications Authority (NZQA). Presumably they, like their UK equivalent (the QAA), are not allowed to take into account whether what is being taught is nonsense or not. Nonsense courses are accredited by experts in nonsense. That is why much accreditation is not worth the paper it’s written on.
Of course the public needs some protection from dangerous or fraudulent practices, but that can be done better (and more cheaply) by simply enforcing existing legislation on unfair trade practices, and on false advertising. Recent changes in the law on unfair trading in the UK have made it easier to take legal action against people who make health claims that cannot be justified by evidence, and that seems the best
way to regulate medical charlatans.
Conclusion
For most forms of alternative medicine—including chiropractic and acupuncture—the evidence is now in. There is now better reason than ever before to believe that they are mostly elaborate placebos and, at best, no better than conventional treatments. It is about time that universities and governments recognised the evidence and stopped talking about regulation and accreditation.
Indeed, “falsely claiming that a product is able to cure illnesses, dysfunction, or malformations” is illegal in Europe10.
Making unjustified health claims is a particularly cruel form of unfair trading practice. It calls for prosecutions, not accreditation.
Competing interests: None.
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716
URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Author information: David Colquhoun, Research Fellow, Dept of Pharmacology, University College London, United Kingdom (http://www.ucl.ac.uk/Pharmacology/dc.html)
Correspondence: Professor D Colquhoun, Dept of Pharmacology, University College London, Gower Street, London WC1E 6BT, United Kingdom. Fax: +44(0)20 76797298; email: d.colquhoun@ucl.ac.uk
References:
1. Gilbey A. Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. N Z Med J. 2008;121(1278). [pdf]
2. Evans A, Duncan B, McHugh P, et al. Inpatients’ use, understanding, and attitudes towards traditional, complementary and alternative therapies at a provincial New Zealand hospital. N Z Med J. 2008;121(1278).
3 Shapiro. Rose. Suckers. How Alternative Medicine Makes Fools of Us All Random House, London 2008. (reviewed here)
4. Singh S, Ernst E. Trick or Treatment. Bantam Press; 2008 (reviewed here)
5. Bausell RB. Snake Oil Science. The Truth about Complementary and Alternative Medicine. (reviewed here)
Oxford University Press; 2007
6. Colquhoun D. Science degrees without the Science, Nature 2007;446:373–4. See also here.
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10.
8. Libin K. Chiropractors called to court. Canadian National Post; June21, 2008.
9. Goldacre B. A menace to science. London: Guardian; February 12, 2007/
10. Department for Business Enterprise & Regulatory Reform (BERR). Consumer Protection from Unfair Trading Regulations 2008. UK: Office of Fair Trading.
This, I fear, is pure plagiarism, Robert Shrimsley’s piece in today’s Financial Times was so funny that it just begged to be quoted. Here it is.
|
Surely this is a call to action. The news that Radovan Karadzic has been hiding out as some kind of homeopath has confirmed all prejudices about alternative medicine. I have had my doubts about this vicious breed ever since we were gulled into giving the kids valerian and hops to calm them down on an overnight flight and they went absolutely wild. Talk about a crime against humanity. Incidentally old Rad is not exactly an advert for homeopathy if this week’s photographs are anything to go by. Before he got into all this complementary healing, he was a sprightly, globally-feared warlord and international criminal. Now, after a decade of mixing his own marjoram, he is a strangely bearded hippy, blathering on about the need to nurture your inner self. Of course with hindsight health shops of the world were an obvious hiding place for genocidal maniacs. Remember all that talk of cleansing impurities? Well, I think we now know what that was all about. Some of you may be thinking that Karadzic was an aberration in an otherwise harmless community. But I ask you, how likely is it that the butcher of Belgrade could have kept up the pretence for so long without ever giving himself away. Were no suspicions aroused by the publication of his first book Radovan’s Remedies . Did no one notice that his patented treatment for stress prescribed ground echinacea root, essence of basil and the blood of a thousand Bosnians. Anyway, now that these collected homeopaths, herbologists and healers have finally been exposed as nothing more than a front organisation for the world’s most wanted, we will doubtless see swift action. How long can it be until the National Security Agency, operating undercover in Greenwich Village, finally pinpoints the precise location of Osama bin Laden’s reiki parlour? Crack teams of CIA operatives will surely be rounding up reflexologists in their search for Ratko Mladic. We can be confident that even now special rendition flights, crammed full of ayurvedic surgeons are en route to Guantánamo, where skilled interrogators will rearrange their chakras at no extra charge. Homeopaths will be forced to take two Disprins every four hours until they crack. US authorities have, however, pledged not to use the cruel practice of water-boarding – except perhaps on hydrotherapists. Of course we may snare a few, genuinely innocent aromatherapists on the way but as they say in the trade, you can’t make a poultice without grinding some ginger. |
During the last year, there has been a very welcome flurry of good and informative books about alternative medicine. They are all written in a style that requires little scientific background, even the one that is intended for medical students.
CAM, Cumming | Trick or Treatment | Snake Oil Science |
Testing treatments | Suckers | Healing, Hype or Harm
I’ll start with the bad one, which has not been mentioned on this blog before.
Complementary and Alternative medicine. An illustrated text.
by Allan D. Cumming, Karen R. Simpson and David Brown (and 12 others). 94 pages, Churchill Livingstone; 1 edition (8 Dec 2006).
| The authors of this book sound impressive
Allan Cumming, BSc(Hons), MBChB, MD, FRCP(E), Professor of Medical Education and Director of Undergraduate Learning and Teaching, and Honorary Consultant Physician, College of Medicine and Veterinary Medicine, University of Edinburgh, Edinburgh, UK; Karen Simpson, BA(Hons), RN, RNT, Fellow in Medical Education, College of Medicine and Veterinary Medicine David Brown, MBChB, DRCOG, General Practitioner, The Murrayfield Medical Centre, and Honorary Clinical Tutor, University of Edinburgh |
 |
Sadly, this is a book so utterly stifled by political correctness that it ends up saying nothing useful at all. The slim volume is, I have to say, quite remarkably devoid of useful information. Partly that is a result of out-of-date and selective references (specially in the chapters written by alternative practitioners),
But the lack of information goes beyond the usual distortions and wishful thinking. I get the strong impression is that it results not so much for a strong commitment to alternative medicine (at least by Cumming) as from the fact that the first two authors are involved with medical education. It seems that they belong to that singularly barmy fringe of educationalists who hold that the teacher must not give information to s student for fear of imparting bias. Rather the student must be told how to find out the information themselves. There is just one little problem with this view. It would take about 200 years to graduate in medicine.
There is something that worries me about medical education specialists. Just look at the welcome given by Yale’s Dean of Medical Education, Richard Belitsky, to Yale’s own division of “fluid concepts of evidence”, as described at Integrative baloney @ Yale, and as featured on YouTube. There are a lot of cryptic allusions to alternative forms of evidence in Cumming’s book too, but nothing in enough detail to be useful to the reader.
What should a book about Alternative medicine tell you? My list would look something like this.
- Why people are so keen to deceive themselves about the efficacy of a treatment
- Why it is that are so often deceived into thinking that something works when it doesn’t
- How to tell whether a medicine works better than placebo or not,
- Summaries of the evidence concerning the efficacy and safety of the main types of alternative treatments.
The Cumming book contains chapters with titles like these. It asks most of the right questions, but fails to answer any of them. There is, time and time again, the usual pious talk about the importance of evidence, but then very little attempt to tell you what the evidence says. When an attempt is made to mention evidence, it is usually partial and out of date. Nowhere are you told clearly about the hazards that will be encountered when trying to find out whether a treatment works.
| The usual silly reflexology diagram is reproduced in Cumming’s introductory chapter, but with no comment at all, The fact that it is obviously total baloney is carefully hidden from the reader.. What is the poor medical student meant to think when they perceive that it is totally incompatible with all the physiology they have learned? No guidance is offered. | 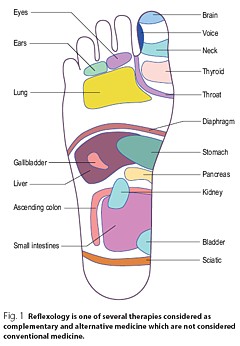 |
| You will look in vain for a decent account of how to do a good randomised controlled trial, though you do get a rather puerile cartoon, The chapter about evidence is written by a librarian. Since the question of evidence is crucial, this is a fatal omission. |  |
Despite the lack of presentation of evidence that any of it works, there seems to be an assumption throughout the book that is is desirable to integrate alternative medicine into clinical practice. In Cumming’s chapter (page 6) we see
Since it would not be in the interests of patients to integrate treatments that don’t work with treatments that do work, I see only two ways to explain this attitude. Either the authors have assumed than most alternative methods work (in which case they haven’t read the evidence), or they think integration is a good idea even if the treatment doesn’t work. Neither case strikes me as good medical education.
The early chapters are merely vague and uninformative. Some of the later chapters are simply a disgrace.
Most obviously the chapter on homeopathy is highly selective and inaccurate, That is hardly surprising because it is was written by Thomas Whitmarsh, a consultant physician at Glasgow Homeopathic Hospital (one that has still survived). It has all the usual religious zeal of the homeopath. I honestly don’t know whether people like Whitmarsh are incapable of understanding what constitutes evidence, or are simply too blinded by faith to even try. Since the only other possibility is that they are dishonest, I suppose it must be one of the former.
The chapter on “Nutritional therapy” is also written by a convert and is equally misleading piece of special pleading.
The same is true of the chapter on Prayer and Faith Healing. This chapter reproduces the header of the Cochrane Review on “Intercessory prayer for the alleviation of Ill Health”, but then proceeds to ignore entirely its conclusion “Most of the studies show no real differences”).
If you want to know about alternative medicine, don’t buy this book. Although this book was written for medical students, you will learn a great deal more from any of the following books, all of which were written for the general public.
Trick or Treatment
by Simon Singh and Edzard Ernst, Bantam Press, 2008
| Simon Singh is the author of many well-known science books, like Fermat’s Last Theorem. Edzard Ernst is the UK’s first professor of complementary and alternative medicine.
Ernst, unlike Cumming et. al is a real expert in alternative medicine. He practised it at an early stage in his career and has now devoted all his efforts to careful, fair and honest assessment of the evidence. That is what this book is about. It is a very good account of the subject and it should be read by everyone, and certainly by every medical student. |
 |
Singh and Ernst follow the sensible pattern laid out above, The first chapter goes in detail into how you distinguish truth from fiction (a little detail often forgotten in this area).
The authors argue, very convincingly, that the development of medicine during the 19th and 20th century depended very clearly on the acceptance of evidence not anecdote. There is a fascinating history of clinical trials, from James Lind (lemons and scurvy), John Snow and the Broad Street pump, Florence Nightingale’s contribution not just to hygiene, but also to the statistical analysis that was needed to demonstrate the strength of her conclusions (she became the first female member of the Royal Statistical Society, and had studied under Cayley and Sylvester, pioneers of matrix algebra).
There are detailed assessments of the evidence for acupuncture, homeopathy, chiropractic and herbalism, and shorter synopses for dozens of others. The assessments are fair, even generous in marginal cases.
Acupunture. Like the other good books (but not Cumming’s), it is pointed out that acupuncture in the West is not so much the product of ancient wisdom (which is usually wrong anyway), but rather a product of Chinese nationalist propaganda engineered by Mao Tse-tung after 1949. It spread to the West after Nixon’s visit Their fabricated demonstrations of open heart surgery under acupuncture have been known since the 70s but quite recently they managed again to deceive the BBC It was Singh who revealed the deception. The conclusion is ” . . . this chapter demonstrates that acupuncture is very likely to be acting as nothing more than a placebo . . . ”
Homeopathy. “hundreds of trials have failed to deliver significant or convincing evidence to support the use of homeopathy for the treatment of any particular ailment. On the contrary, it would be to say that there is a mountain of evidence to suggest that homeopathic remedies simply do not work”.
Chiropractic. Like the other good books (but not Cumming’s) there is a good account of the origins of chiropractic (see, especially, Suckers). D.D. Palmer, grocer, spiritual healer, magnetic therapist and fairground quack, finally found a way to get rich by removing entirely imaginary ‘subluxations’. They point out the dangers of chiropractic (the subject of court action), and they point out that physiotherapy is just as effective and safer.
Herbalism. There is a useful table that summarises the evidence. They conclude that a few work and most don’t Unlike homeopathy, there is nothing absurd about herbalism, but the evidence that most of them do any good is very thin indeed.
| “We argue that it is now the time for the tricks to stop, and for the real treatments to take priority. In the name of honesty, progress and good healthcare, we call for scientific standards, evaluation and regulation to be applied to all types of medicine, so that patients can be confident that they are receiving treatments that demonstrably generate more harm than good.” |
Snake Oil Science, The Truth about Complementary and Alternative Medicine.
R. Barker Bausell, Oxford University Press, 2007
Another wonderful book from someone who has been involved himself in acupuncture research, Bausell is a statistician and experimental designer who was Research Director of a Complementary and Alternative Medicine Specialised Research Center at the University of Maryland.
This book gives a superb account of how you find out the truth about medicines, and of how easy it is to be deceived about their efficacy.
I can’t do better than quote the review by Robert Park of the American Physical Society (his own book, Voodoo Science, is also excellent)
| “Hang up your lantern, Diogenes, an honest man has been found. Barker Bausell, a biostatistician, has stepped out of the shadows to give us an insider’s look at how clinical evidence is manipulated to package and market the placebo effect. Labeled as ‘Complementary and Alternative Medicine’, the placebo effect is being sold, not just to a gullible public, but to an increasing number of health professionals as well. Bausell knows every trick and explains each one in clear language” |  |
Bausell’s conclusion is stronger than that of Singh and Ernst.
“There is no compelling, credible scientific evidence to suggest that any CAM therapy benefits any medical condition or reduces any medical symptom (pain or otherwise) better than a placebo”.
Here are two quotations from Bausell that I love.
[Page 22] ” seriously doubt, however, that there is a traditional Chinese medicine practitioner anywhere who ever stopped performing acupuncture on an afflicted body in the presence of similarly definitive negative evidence. CAM therapists simply do not value (and most cases, in my experience, do not understand) the scientific process”
And even better,
[Page39] “But why should nonscientists care one iota about something as esoteric as causal inference? I believe that the answer to this question is because the making of causal inferences is part of our job description as Homo Sapiens.”
Testing Treatments: Better Research for Better Healthcare
by Imogen Evans, Hazel Thornton, Iain Chalmers, British Library, 15 May 2006
You don’t even need to pay for this excellent book (but buy it anyway, eg from Amazon). If you can’t afford, £15 then download it from the James Lind Library.
| This book is a unlike all the others, because it is barely mentions alternative medicine. What it does, and does very well, is to describe he harm that can be done to patients when they are treated on the basis of guesswork or ideology, rather than on the basis of proper tests. This, of course, is true whether or not the treatment is labelled ‘alternative’.
It is worth noting that one of the authors of this book is someone who has devoted much of his life to the honest assessement of evidence, Sir Iain Chalmers, one of the founders of the Cochrane Collaboration , and Editor of the James Lind Library . |
 |
A central theme is that randomised double blind trial are essentially the only way to be sure you have the right answer. One of the examples that the authors use to illustrate this is Hormone Replacement Therapy (HRT). For over 20 years, women were told that HRT would reduce their risk of heart attacks and strokes. But when, eventually, proper randomised trials were done, it was found that precisely the opposite was true. The lives of many women were cut short because the RCT had not been done,
The reason why the observational studies gave the wrong answer is pretty obvious. HRT was used predominantly by the wealthier and better-educated women. Income is just about the best predictor of longevity. The samples were biassed, and when a proper RCT was done it was revealed that the people who used HRT voluntarily lived longer despite the HRT, not because of it. It is worth remembering that there are very few RCTs that test the effects of diet. And diet differs a lot between rich and poor people. That, no doubt, is why there are so many conflicting recommendations about diet. And that is why “nutritional therapy” is little more than quackery. Sadly, the media just love crap epidemiology. One of the best discussions of this topics was in Radio 4 Programme. “The Rise of the Lifestyle Nutritionists“, by Ben Goldacre.
One of the big problems in all assessment is the influence of money, in other words corruption, The alternative industry is entirely corrupt of course, but the pharmaceutical industry has been increasingly bad. Testing Treatments reproduces this trenchant comment.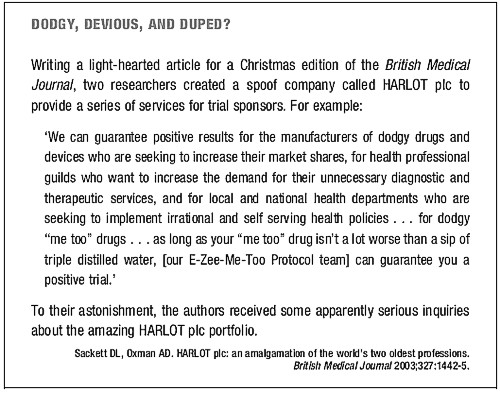
Suckers. How Alternative Medicine Makes Fools of Us All
Rose Shapiro, Random House, London 2008
| I love this book. It is well-researched, feisty and a thoroughly good read.
It was put well in the review by George Monbiot.
The chapters on osteopathy and chiropractic are particularly fascinating. |
 |
This passage describes the founder of the chiropractic religion.
“By the 1890s Palmer had established a magnetic healing practice in Davenport, Iowa, and was styling himself ‘doctor’. Not everyone was convinced as a piece about him in an 1894 edition of the local paper, the Davenport Leader, shows.”
A crank on magnetism has a crazy notion hat he can cure the sick and crippled with his magnetic hands. His victims are the eak-minded, ignorant and superstitious, those foolish people who have been sick for years and have become tired of the regular physician and want health by the short-cut method . . . he has certainly profited by the ignorance of his victims . . . His increase in business shows what can be done in Davenport, even by a quack”
Over 100 years later, it seems that the “weak-minded, ignorant and superstitious” include the UK’s Department of Health, who have given these quacks a similar status to the General Medical Council.
The intellectual standards of a 19th Century mid-western provincial newspaper leader writer are rather better than the intellectual standards of the Department of Health, and of several university vice-chancellors in 2007.
Healing Hype or Harm
Edited by Imprint Academic (1 Jun 2008)
Download the contents page
My own chapter in this compilation of essays, “Alternative medicine in UK Universities” is an extended version of what was published in Nature last year (I don’t use the term CAM because I don’t believe anything can be labelled ‘complementary’ until it has been shown to work). Download a copy if the corrected proof of this chapter (pdf).
| Perhaps the best two chapters, though, are “CAM and Politics” by Rose and Ernst, and “CAM in Court” by John Garrow.
CAM and politics gives us some horrifiying examples of the total ignorance of almost all politicians and civil servants about the scientific method (and their refusal to listen to anyone who does understand it). CAM in Court has some fascinating examples of prosecutions for defrauding the public. Recent changes in the law mean we may be seeing a lot more of these soon. Rational argument doesn’t work well very well with irrational people. But a few homeopaths in jail for killing people with malaria would probably be rather effective. |
 |
Follow-up
Healing, Hype or Harm has had some nice reviews, That isn’t so surprising from the excellent Harriet Hall at Science-Based Medicine. The introduction to my chapter was a fable about the replacemment of the Department of Physics and Astronomy by the new Department of Alternative Physics and Astrology. It was an unashamedly based on Laurie Taylor’e University of Poppleton column. Hall refers to it as “Crislip-style”, a new term to me. I guess the incomparable Laurie Taylor is not well-known in the USA, Luckily Hall gives a link to Mark Crislip’s lovely article, Alternative Flight,
“Americans want choice. Americans are increasingly using alternative aviation. A recent government study suggests that 75% of Americans have attempted some form of alternative flight, which includes everything from ultralights to falling, tripping and use of bungee cords.”
“Current airplane design is based upon a white male Western European model of what powered flight should look like. Long metal tubes with wings are a phallic design that insults the sensibilities of women, who have an alternative, more natural, emotional, way of understanding airplane design. In the one size fits all design of allopathic airlines, alternative designs are ignored and airplane design utilizing the ideas and esthetics of indigenous peoples and ancient flying traditions are derided as primitive and unscientific, despite centuries of successful use.”
Metapsychology Online Reviews doesn’t sound like a promising title for a good review of Healing, Hype or Harm, but in fact their review by Kevin Purday is very sympathetic. I like the ending.
“One may not agree with everything that is written in this book but it is wonderful that academic honesty is still alive and well.”
| A report has appeared on Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine. The report is written by people all of whom have vested interests in spreading quackery. It shows an execrable ability to assess evidence, and it advocates degrees in antiscience It would fail any examination. Sorry, Prof Pittilo, but it’s gamma minus.[Download the report] |  |
Alice Miles put it well in The Times, today.
“This week came the publication of the “Report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK”. Otherwise known as twaddle.” . . .
“Regulate the practitioners – for safety, note, not for efficacy, as that is impossible to prove – and you give them official recognition. From recognition it is but a short hop to demand and then prescription: packet of Prozac, bit of yoga and a bag of dodgy herbs for you, sir.” . . .
“The Government responded on Monday – with a three-month consultation. So join in. Write to the Health Minister Ben Bradshaw at Richmond House, 79 Whitehall, SW1A 2NS. Write, on behalf of the NHS: “What I want for my 60th birthday is… the chance to provide medical, dental, and nursing care to all. And absolutely nothing else.”
Judging by Ben Bradshaw’s speech to the Prince’s Foundation, there may be a problem in conveying to him the evidence, but one can and must try.
Why is it that a health joutnalist can do so much better than a university head? Yes, the chair of the steering group is Professor R. Michael Pittilo BSc PhD CBiol FIBiol FIBMS FRSH FLS FRSA, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. Despite all those impressive-lookin initials after his name, I believe that this is a very bad report.
Here is something about Prof Pittilo from his university’s web site (the emphasis is mine).
Professor Michael Pittilo joined The Robert Gordon University, Aberdeen, as Principal and Vice-Chancellor on 5th September, 2005.
After postdoctoral research on arterial disease at the University of London, he was appointed to Kingston University where he became Head of Life Sciences. In 1995 he became Foundation Dean of the Faculty of Health and Social Care Sciences at Kingston University and St George’s Medical School (University of London). He was appointed Pro Vice Chancellor at the University of Hertfordshire in 2001.
Professor Pittilo has held a number of additional roles, including chairing Department of Health working groups, and as a trustee for the Prince of Wales’s Foundation for Integrated Health. “
Notice that Prof Pittilo is a Trustee of the Prince’s Foundation for Integrated Health, source of some of the least reliable information about alternative medicine to be found anywhere.
This steering group is, as so often, a nest of vested interests. It does not seem to have on it any regular medical or clinical scientist whatsoever. Why not? They just might produce some embarrassing facts perhaps? Like most government committees its members seem to have been chosen to produce the desired outcome.
For a start, the university run by Prof Pittilo, Robert Gordon’s University, is itself involved in a few antiscientific courses. Since his report recommends that degrees in quackery should become mandatory, I expect he’d welcome the chance to run more. Amazingly, Robert Gordon’s University runs an Introduction to Homeopathy, just about the daftest of all the common sorts of magic medicine.
Most of the the members of the steering group represent vested interests, though strangely this is not made clear in the list of members. An earlier report, in 2006, from the steering group was more open about this. Twelve of the members of the group represent Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Most of the rest are lay members or bureaucrats. With membership like that it is, I suppose, not surprising that the assessment of evidence is, to put it kindly, grossly distorted and woefully inadequate.
The report starts badly by failing to mention that the House of Lords report (2000), and the government’s response to it, set the following priorities. Both state clearly
“… we recommend that three important questions should be addressed in the following order . .
- (1) does the treatment offer therapeutic benefits greater than placebo?
- (2) is the treatment safe?
- (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?
The word ‘placebo’ does not occur a single time in the main report (and only twice in the text of the seven appendices). But they do say (page 11):
“We recommend that public funding from the NHS should be used to fund CAM therapies where there is evidence of efficacy, safety and quality assurance.”
The evidence
The problem is that the assessment of the evidence for efficacy in the report is pathetically poor. The report, sad to say, consists essentially of 161 pages of special pleading by the alternative medicine industry, served up with the usual large dose of HR gobbledygook.
There is really no excuse for this utterly incompetent assessment. There have been plenty of books this year alone that make excellent summaries of the evidence, mostly written for the lay public. They should, therefore, be understandable by any university vice-chancellor (president). The one benefit of the upsurge in public interest in magic medicine is that there are now quite a lot of good clinical trials, and when the trials are done properly, they mostly confirm what we thought before: in most cases the effects are no more than placebo.
Here is one example. Annexe1 concerns “Developing Research and Providing an Evidence Base for Acupuncture and Herbal/Traditional Medicine Treatment”. The wording of the title itself suggests, rightly, that this evidence base does not exist, in which case why on earth are we talking about them as “professions”? The discussion of the evidence in Annexe 1 is nothing if not partial. But what do you expect if you ask herbalists to assess herbal medicine? An honest assessment would put them out of business. The eternal mantra of the alternative industry appears as usual, “Absence of evidence is, of course, not evidence of absence”. True of course, but utterly irrelevant. Annexe 1 says
“Acupuncture is a complex intervention and lack of a suitable placebo control has hindered efforts to evaluate efficacy”
This is simply untrue, In recent years enormous efforts have been put into devising controls for assessment of acupuncture, but they are entirely ignored here. One thing that has been established quite clearly is that it makes no difference where you put the needles, so all the talk of Qi and meridians is obvious mumbo-jumbo.
Have the authors of Annexe 1, and Professor Pittilo, not read the relevant studies? Two books this year have dealt with the question of evidence with great care. They are both by people who have been involved personally with acupuncture research, Prof Edzard Ernst and Dr Barker Bausell. Edzard Ernst is the UK’s first Professor of Complementary Medicine. Barker Bausell was research director of an NIH-funded Complementary and Alternative Medicine Specialized Research Center at the University of Maryland.
 |
 |
Singh and Ernst discuss thoroughly the question of controls and assess all the evidence carefully. Their conclusions include the following.
- The traditional principles of acupuncture are deeply flawed, as there is no evidence at all to demonstrate the existence of Ch’i [Qi] or meridians.
- By focussing on the increasing number of high-quality research papers, reliable conclusions from systematic reviews make it clear that acupuncture does not work for a whole range of conditions, except as a placebo.
- In short, the evidence is neither consistent nor convincing. It is borderline.
Barker Bausell was himself involved in designing and analysing trialsof acupuncture. His conclusions are even less positive.
“There is no compelling, credible scientific evidence to suggest that any CAM therapy benefits any medical condition or reduces any medical symptom (pain or otherwise) better than a placebo”.
These are serious authors with direct experience in CAM research, which is more than can be said of anyone on the steering group. Why are their conclusions ignored entirely? That is sheer incompetence.
Degrees in anti-science
One conclusion of the report is that
“The threshold entry route to the register will normally be through a Bachelor degree with Honours”
This is utter nonsense. It is quite obvious surely that you can’t award honours degrees until after you have the evidence. You can read on page 55 of the report
“3a: Registrant acupuncturists must:
understand the following aspects and concepts for traditional East-Asian acupuncture:
– yin/yang, /5 elements/phases, eight principles, cyclical rhythms, qi ,blood and body fluids, different levels of qi, pathogenic factors, 12 zang fu and 6 extraordinary fu, jing luo/ meridians, the major acupuncture points, East-Asian medicine disease categorisation, the three burners, the 4 stages/levels and 6 divisions
– causes of disharmony/disease causation
– the four traditional diagnostic methods: questioning, palpation, listening and observing”
This is utter baloney. Anyone who advocates giving honours degrees in such nonsense deserves to be fired for bringing his university into disrepute (and, in the process, bringing all universities and science itself into disrepute).
That includes also degrees that teach that “amethysts emit high yin energy“.
So what should be done?
If making peole do degrees in mumbo-jumbo is not the answer, what is? Clearly it would be far too draconian to try to ban quackery (and it would only increase its popularity anyway).
The answer seems to me to be quite simple. All that needs to done is to enforce existing laws. It is already illegal to sell contaminated and poisonous goods to the public. It is already illegal to make fraudulent advertisemants and to sell goods that are not as described on the label.
The only problem is that the agencies that enforce these rules are toothless and that there are a lot of loopholes and exceptions that work in favour of quackery. I have tried myself to complain about mislabelling of homeopathic pills to the Office of Fair Trading on the grounds that are labelled Arnica 30C but contain no Arnica. They solemnly bought a bottle and sent it to an analyst and of course they found no arnica, But nothing happened, because an exception to the usual law applies to homeopathic pills.
The Advertising Standards Authority is good as far as it goes. They quickly told Boots Pharmacies to withdraw advertisements that claimed CoQ10 “increased vitality”. But they can exact no penalties and they can’t deal with lies that are told to you orally, or with anything at all on the web.
The Health Professions Council (HPC) says that one of the criteria for registering new professions is aspirant groups must “Practise based on evidence of efficacy”. If that were actually applied, none of this process would occur anyway. No doubt the HPC will fail to apply its own criteria. On past form, it can be expected to adopt a “fluid concept of evidence“.,
One more thing, New European legislation was described recently in the BMJ
“Consumers in the United Kingdom are to receive stronger legal safeguards against products that claim, without any identifiable scientific evidence, to provide physical and mental health benefits such as tackling obesity or depression.”
“The scope of the legislation is deliberately wide and is the biggest shake up in consumer law for decades. It targets any unfair selling to consumers by any business.”
Politicians seem to be immune to rational argument when it comes to quackery. But a few legal actions under these laws could bring the house of cards tumbling so fast that this gamma-minus report would become rapidly irrelevant. There will be no shortage of people to bring the actions. I can’t wait.
Follow up
Dominic Lawson, 24 June 2008. An excellent column appeared today in the Independent. Dominic Lawson writes about the Pittilo report: “So now we will have degrees in quackery. What, really, is the difference between acupuncture and psychic surgery?“. The reference to that well known conjuring trick, “psychic surgery” as a “profession”, revealed here, causes Lawson to say
“It makes it clear that the lunatics have taken over the asylum. For a start, how could Philip Hunt, previously director of the National Association of Health Authorities and Trusts, possibly have thought that “psychic healing” constituted a “profession” – let alone one which would “develop its own system of voluntary self-regulation?”
“One can see how this might fit in with the Government’s “never mind the quality, feel the width” approach to university education. One can also see how established practitioners of such therapies might see this as a future source of income – how pleasant it might be to become Visiting Professor of Vibrational Medicine at the University of Westminster.
Thus garlanded with the laurels of academic pseudo-science, the newly professionalised practitioners of “alternative medicine” can look down on such riff-raff as the “psychic surgeons”
Once again I have to ask, how is it that we have to rely on journalists to prevent vice-chancellors eroding academic standards; indeed eroding simple common sense? I guess it is just another sign of the delusional thinking engendered by the culture of managerialism that grips universities.
We have often had cause to criticise Boots Alliance, the biggest retail pharmacist in the UK, because of its deeply unethical approach to junk medicine. Click here to read the shameful litany. The problem of Boots was raised recently also by Edzard Ernst at the Hay Literary Festival. He said
“The population at large trusts Boots more than any other pharmacy, but when you look behind the smokescreen, when it comes to alternative medicines, that trust is not justified.”

Ernst accused Boots of breaching ethical guidelines drawn up by the Royal Pharmaceutical Society of Great Britain, by failing to tell customers that its homeopathic medicines contain no active ingredients and are ineffective in clinical trials.
Another chain, Lloyds Pharmacy, are just as bad. Many smaller pharmacies are no more honest when it comes to selling medicines that are known to be ineffective.
Pharmacists are fond of referring to themselves as “professionals” who are regulated by a professional body, the Royal Pharmaceutical Society of Great Britain (RPSGB). It’s natural to ask where their regulatory body stands on the question of junk medicine. So I asked them, and this is what I found.
| 17 April, 2008
I am writing an article about the role of pharmacists in giving advice about (a) alternative medicines and (b) nutritional supplements. I can find no clear statements about these topics on the RPSGB web site. Please can you give me a statement on the position of the Royal Pharmaceutical Society on these two topics. In particular, have you offered guidance to pharmacists about how to deal with the conflict of interest that arises when they can make money by selling something that they know to have no good evidence for efficacy? This question has had some publicity recently in connection with Boots’ promotion of CCoQ10 to give you “energy”, and only yesterday when the bad effects of some nutritional supplements were in the news. |
Here are some extracts from the first reply that I got from the RPSGB’s Legal and Ethical Advisory Service (emphasis is mine).
| 28 April 2008
Pharmacists must comply with the Code of Ethics and its supporting documents. Principle 5 of the Code of Ethics requires pharmacists to develop their professional knowledge and competence whilst Principle 6 requires pharmacists to be honest and trustworthy. The Code states: 5. DEVELOP YOUR PROFESSIONAL KNOWLEDGE AND COMPETENCE At all stages of your professional working life you must ensure that your knowledge, skills and performance are of a high quality, up to date and relevant to your field of practice. You must: 5.1 Maintain and improve the quality of your work by keeping your knowledge and skills up to date, evidence-based and relevant to your role and responsibilities. 5.2 Apply your knowledge and skills appropriately to your professional responsibilities. 5.3 Recognise the limits of your professional competence; practise only in those areas in which you are competent to do so and refer to others where necessary. 5.4 Undertake and maintain up-to-date evidence of continuing professional development relevant to your field of practice. 6. BE HONEST AND TRUSTWORTHY Patients, colleagues and the public at large place their trust in you as a pharmacy professional. You must behave in a way that justifies this trust and maintains the reputation of your profession. You must: 6.2 Ensure you do not abuse your professional position or exploit the vulnerability or lack of knowledge of others. 6.3 Avoid conflicts of interest and declare any personal or professional interests to those who may be affected. Do not ask for or accept gifts, inducements, hospitality or referrals that may affect, or be perceived to affect, your professional judgement. 6.4 Be accurate and impartial when teaching others and when providing or publishing information to ensure that you do not mislead others or make claims that cannot be justified. |
And, on over-the counter prescribing
| In addition the “Professional Standards and Guidance for the Sale and Supply of Medicines” document which supports the Code of Ethics states:
“2. SUPPLY OF OVER THE COUNTER (OTC) MEDICINES STANDARDS When purchasing medicines from pharmacies patients expect to be provided with high quality, relevant information in a manner they can easily understand. You must ensure that: 2.1 procedures for sales of OTC medicines enable intervention and professional advice to be given whenever this can assist the safe and effective use of medicines. Pharmacy medicines must not be accessible to the public by self-selection. |
Evidence-based? Accurate and impartial? High quality information? Effective use?
These words don’t seem to accord with Boots’ mendacious advertisements for CoQ10 (which were condemned by the ASA).
Neither does it accord with the appalling advice that I got from a Boots pharmacist about Vitamin B for vitality.
Or their bad advice on childhood diarrhoea.
Or the unspeakable nonsense of the Boots (mis)-education web site.
Then we get to the nub. This is what I was told by the RPSGB about alternative medicine (the emphasis is mine).
| 8. COMPLEMENTARY THERAPIES AND MEDICINES
STANDARDS You must ensure that you are competent in any area in which you offer advice on treatment or medicines. If you sell or supply homoeopathic or herbal medicines, or other complementary therapies, you must: 8.1 assist patients in making informed decisions by providing them with necessary and relevant information. 8.2 ensure any stock is obtained from a reputable source. 8.3 recommend a remedy only where you can be satisfied of its safety and quality, taking into account the Medicines and Healthcare products Regulatory Agency registration schemes for homoeopathic and herbal remedies.” Therefore pharmacists are required to keep their knowledge and skills up to date and provide accurate and impartial information to ensure that you do not mislead others or make claims that cannot be justified. |
It does seem very odd that “accurate and impartial information” about homeopathic pills does not include mentioning that they contain no trace of the ingredient on the label. and have been shown in clinical trials to be ineffective. These rather important bits of information are missing from both advertisements and from (in my experience) the advice given by pharmacists in the shop.
If you look carefully, though, the wording is a bit sneaky. Referring to over-the-counter medicines, the code refers to “safe and effective use of medicines”, but when it comes to alternative medicines, all mention of ‘effectiveness’ has mysteriously vanished.
So I wrote again to get clarification.
| 29 April, 2008
Thanks for that information. I’d appreciate clarification of two matters in what you sent. (1) Apropros of complementary and alternative medicine, the code says 8.3 recommend a remedy only where you can be satisfied of its safety and quality I notice that this paragraph mentions safety and quality but does not mention efficacy. Does this mean that it is considered ethical to recommend a medicine when there is no evidence of its efficacy? Apparently it does. This gets to the heart of my question and I’d appreciate a clear answer. |
This enquiry was followed by a long silence. Despite several reminders by email and by telephone nothing happened until eventually got a phone call over a month later (May 3) from David Pruce, Director of Practice & Quality Improvement, Royal Pharmaceutical Society of Great Britain. The question may be simple, but the RPSGB evidently it hard, or more likely embarrassing, to answer.
When I asked Pruce why para 8.3 does not mention effectiveness, his reply, after some circumlocution, was as follows.
Pruce: “You must assist patients in making informed decisions by providing necessary and relevant information . . . we would apply this to any medicine, the pharmacist needs to help the patient assess the risks and benefits.”
DC: “and would that include saying it doesn’t work better than placebo?”
Pruce “if there is good evidence to show that it may, but it depends on what the evidence is, what the level of evidence is, and the pharmacist’s assessment of the evidence”
DC “What’s your assessment of the evidence?”
Pruce, “I don’t think my personal assessment is relevant. I wouldn’t want to be drawn on my personal assessment”. “If a pharmacist is selling homeopathic medicines they have to assist the patient in making informed decisions”
“I don’t think we specifically talk about the efficacy of any other medicine” [DC: not true, see para 2.1, above]
“We would expect pharmacists to be making sure that what they are providing to a patient is safe and efficacious”
DC “So why doesn’t it mention efficacious in para 8.3”
Pruce “What we are trying to do with the Code of Ethics is not go down to the nth degree of detail ” . . . “there are large areas of medicine where there is an absence of data”
DC “Yes, actually homeopathy isn’t one of them. It used to be.”
Pruce. “uh, that’s again a debatable point”
DC I don’t think it’s debatable at all, if you’ve read the literature
Pruce. “well many people would debate that point” “This [homeopathy] is a controversial area where opinions are divided on it”
DC “Not informed opinions”
Pruce “Well . . . there are also a large number of people that do believe in it. We haven’t come out with a categorical statement either way.”
I came away from this deeply unsatisfactory conversation with a strong impression that the RPSGB’s Director of Practice & Quality Improvement was either not familiar with the evidence, or had been told not to say anything about it, in the absence of any official statement about alternative medicine.
I do hope that the RPSGB does not really believe that “there are also a large number of people that do believe in it” constitutes any sort of evidence.
It is high time that the RPSGB followed its own code of ethics and required, as it does for over-the-counter sales, that accurate advice should be given about “the safe and effective use of medicines”.
“The scientist on the High Street”
The RPS publishes a series of factsheets for their “Scientist in the High Street” campaign. One of these “factsheets” concerns homeopathy, [download pdf from the RPSGB]. Perhaps we can get an answer there?
Well not much. For the most part the “factsheet” just mouths the vacuous gobbledygook of homeopaths. It does recover a bit towards the end, when it says
“The methodologically “best” trials showed no effect greater than that of placebo”.
But there is no hint that this means pharmacists should not be selling homeopathic pills to sick people..
That is perhaps not surprising, because the Science Committee of the RPSGB copped out of their responsibility by getting the factsheet written by a Glasgow veterinary homeopath, Steven Kayne. You can judge his critical attitude by a paper (Isbell & Kayne, 1997) which asks whether the idea that shaking a solution increases its potency. The paper is a masterpiece of prevarication, it quotes only homeopaths and fails to come to the obvious conclusion. And it is the same Steven Kayne who wrote in Health and Homeopathy (2001)
“Homeopathy is not very good for treating bacterial infections directly, apart from cystitis that often responds to a number of medicines, including Berberis or Cantharis”.
So there is a bacterial infection that can be cured by pills that contain no medicine? Is this dangerous nonsense what the RPSGB really believes?
More unreliable advice
While waiting for the train to Cardiff on April 16th (to give a seminar at the Welsh School of Pharmacy), I amused myself by dropping into the Boots store on Paddington station.
| DC I’ve seen your advertisements for CoQ10. Can you tell me more? Will they really make me more energetic?
Boots: Yes they will, but you may have to take them for several weeks. DC. Several weeks? Boots: yes the effect develops only slowly Peers at the label and reads it out to me DC I see. Can you tell me whether there have been any trials that show it works? Boots. I don’t know. I’d have to ask. But there must be or they wouldn’t be allowed to sell it. DC. Actually there are no trials, you know Boots. Really? I didn’t think that was allowed. But people have told me that they feel better after taking it. DC You are a pharmacist? Boots. Yes |
Sadly, this abysmal performance is only too typical in my experience, Try it yourself.
The malaria question
After it was revealed that pharmacists were recommending, or tolerating recommendations, of homeopathic treatment of malaria, the RPSGB did, at last. speak out. It was this episode that caused Quackometer to write his now famous piece on ‘The gentle art of homeopathic killing‘ (it shot to fame when the Society of Homeopaths tried to take legal action to ban it) Recommending pills that contain no medicine for the treatment or prevention or treatment of malaria is dangerous. If it is not criminal it ought to be [watch the Neals Yard video]. .
The RPSGB says it is investigating the role of pharmacists in the Newsnight sting (see the follow-up here). That was in July 2006, but they are stlll unwilling to say if any action will be taken. Anyone want to bet that it will be swept under the carpet?
The statement issued by the RPSGB, 5 months after the malaria sting is just about the only example that I can find of them speaking out against dangerous and fraudulent homeopathic practices. Even in this case, it is pretty mild and restricted narrowly to malaria prevention.
The RPSGB and the Quacktioner Royal
The RPSGB submitted a response to the ‘consultation’ held by the Prince’s Foundation for Integrated Health, about their Complementary Healthcare; a guide for patients.
| Response by the Royal Pharmaceutical Society of Great Britain Dr John Clements, Science Secretary “We believe that more emphasis should be given to the need for members of the public who are purchasing products (as opposed to services) to ask for advice about the product. Pharmacists are trained as experts on medicines and the public, when making purchases in pharmacies, would expect to seek advice from pharmacists” |
So plenty of puffery for the role of pharmacists. But there is not a word of criticism about the many barmy treatments that are included in the “Guide for Patients”. Not just homeopathy and herbalism, but also Craniosacral therapy, Laying on of Hands, chiropractic, Reiki, Shiatsu –every form of barminess under the sun drew no comment from the RPS.
I can’t see how a response like this is consistent with the RPS’s own code of ethics.
A recent president of the RPSGB was a homeopath
| Christine Glover provides perhaps the most dramatic reason of all for thinking thst, despite all the fine words, the RPSGB cares little for evidence and truth The NHS Blogdoctor published “Letter from an angry pharmacist”. |  |
Mrs Glover was president of the RPSGB from 1999 to 2001, vice-president in 1997-98, and a member of the RPSGB Council until May 2005. She is not just a member, but a Fellow. (Oddly, her own web site says President from 1998 – 2001.)
So it is relevant to ask how the RPSGB’s own ex-president obeys their code of ethics. Here are some examples on how Ms Glover helps to assist the safe and effective use of medicines. . Much of her own web site seems to have vanished (I wonder why) so I’ll have to quote the “Letter from an angry pharmacist”., as revealed by NHS Blogdoctor,
“What has Christine got to offer?
- “We offer a wide range of Homeopathic remedies (over 3000 different remedies and potencies) as well as Bach flower remedies, Vitamins, Supplements, some herbal products and Essential Oils.”
- Jetlag Tablets highly recommended in ‘Wanderlust’ travel magazine. Suitable for all ages.
- Wind Remedy useful for wind particularly in babies. In can be supplied in powder form for very small babies. Granules or as liquid potency.
- Udder Care 100ml £80.00 One capful in sprayer filled with water. Two jets to be squirted on inner vulva twice daily for up to 4 days until clots reduced. Discard remainder. Same dose for high cell-counting cows detected.
Udder Care? Oh! I forgot to say, “Glover’s Integrated Healthcare” does cows as well as people. Dr Crippen would not suggest to a woman with sore breasts that she sprayed something on her inner vulva. But women are women and cows are cows and Dr Crippen is not an expert on bovine anatomy and physiology. But, were he a farmer, he would need some persuasion to spend £80.00 on 100 mls of a liquid to squirt on a cow’s vulva. Sorry, inner vulva.”
Nothing shows more clearly that the RPSGB will tolerate almost any quackery than the fact that they think Glover is an appropriate person to be president. Every item on the quotation above seems to me to be in flagrant breach of the RPSGB’s Code of Ethics. Just like the Society of Homeopaths, the code seems to be there merely for show, at least in the case of advice about junk medicine..
A greater role for pharmacists?
This problem has become more important now that the government proposes to give pharmacists a greater role in prescribing. Needless to say the RPSGB is gloating about their proposed new role. Other people are much less sure it is anything but a money–saving gimmick and crypto-privatisation.
I have known pharmacists who have a detailed knowledge of the actions of drugs, and I have met many more who haven’t. The main objection, though, is that pharmacists have a direct financial interest in their prescribing. Conflicts of interest are already rife in medicine, and we can’t afford them.
Conclusion
The Royal Pharmaceutical Society is desperately evasive about a matter that is central to their very existence, giving good advice to patients about which medicines work and which don’t. Pharmacists should be in the front line in education of the public, about medicines, the ‘scientist on the High Street’. Some of them are, but their professional organisation is letting them down badly.
Until such time as the RPSGB decides to take notice of evidence, and clears up some of the things described here, it is hard to see how they can earn the respect of pharmacists, or of anyone else.
Follow-up
Stavros Isaiadis’ blog, Burning Mind, has done a good piece on “More on Quack Medicine in High Street Shops“.
The Chemist and Druggist reports that the RPSGB is worried about the marketing of placebo pills (‘obecalp’ -geddit?). It does seem very odd that the RPSGB should condemn honest placebos, but be so very tolerant about dishonest placebos. You couldn’t make it up.
A complaint to the RPSGB is rejected
Just to see what happened, I made a complaint to thr RPSGB about branches of their own Code of Ethics at Boots in Hexham and in Evesham. Both of them supported Homeopathy Awareness Week These events had been publicised in those particularly unpleasent local ‘newspapers’ that carry paid advertising disguised as editorial material. In this case it was the Evesham Journal and the Hexham Courant.
Guess what? The RPSGB replied thus
“Your complaint has been reviewed bt Mrs Jill Williams and Mr David Slater who are both Regional Lead Inspectors. Having carried out a review they have concluded that support of homeopathic awareness week does not constitute a breach of the Society’s Code of Ethics or Professional Standards.”
In case you have forgotten, the Professional Standards say
2.1 procedures for sales of OTC medicines enable intervention and professional advice to be given whenever this can assist the safe and effective use of medicines.
The RPSGB has some very quaint ideas on how to interpret their own code of ethics
The extent to which irrationality has become established in US Medicine is truly alarming I wrote about Quackademics in the USA and Canada on my last trip to the USA, and on my May trip I visited Yale, where I decided to try a full frontal attack. [download the poster]

Several US blogs have written about this phenomenon. For example the incomparable Orac at the The Academic Woo Aggregator , and Dr RW (R.W. Donnell) , see particularly his articles on How did pseudoscience get admitted to medical school? and What is happening to our medical schools? Abraham Flexner is turning over in his grave. Excellent US stuff too at Science-based Medicine (try this and this). There is also a good analysis of what’s happening at Yale by Sandy Szwarc at Junkfood Science.
Remember that the terms ‘integrative’ and ‘complementary’ are euphemisms coined by quacks to make their wares sound more respectable, There is no point integrating treatments that don’t work with treatments that do work.
‘Integrative Medicine’ at Yale says, like all the others on the roll of shame, says “we aim to improve awareness and access to the best in evidence-based, comprehensive medical care available worldwide”. They all pay lip service to being “evidence based”, but there is just one snag. It is untrue. In almost all cases, the evidence is either negative or absent. But this does not put them off for a moment. The whole process is simply dishonest.
The evidence
The evidence has been summarised in several books recently, The following books are particularly interesting because they are all ‘views from the inside. Edzard Ernst is the UK’s first Professor of Complementary Medicine. Barker Bausell was research director of an NIH funded Complementary and Alternative Medicine Specialized Research Center at the University of Maryland.
The first two books go through the evidence fairly and carefully. They show no bias against alternative treatments (if anything, I’d say they are rather generous in cases of doubt).
 |
 |
For a first class US account try Barker Bausell’s Snake Oil Science
Bausell’s book gives an excellent account of how to test treatments properly, and of all the ways you can be fooled into thinking something works when it doesn’t. Bausell concludes
|
 |
| For an excellent account of how to find the truth, try Testing Treatments (Evans. Thornton and Chalmers). One of the authors, Iain Chalmers, is a founder of the Cochrane library and a world authotity on how to separate medical fact from medical myth. |  |
It can now be said with some certainty that the number of alternative treatments that have been shown to work better than placebo is very small, and quite possibly zero,
With that settled, what’s going on at Yale (and many others on the roll of shame)?
David L. Katz, MD, MPH, FACPM, FACP, is founder and director of the Integrative Medicine Center (IMC) at Griffin Hospital in Derby, Connecticut. He is also an associate professor, adjunct, of Public Health and director of the Prevention Research Center (PRC) at the Yale University School of Medicine in New Haven, Connecticut.
That sounds pretty respectable. But he is into not just good nutrition, exercise, relaxation and massage, but also utterly barmy and disproved things like homeopathy and ‘therapeutic touch’.
| Watch the movie
It so happens that Yale recently held an “Integrative Medicine Scientific Symposium”. Can we find the much vaunted evidence base there? That is easy to answer because three hours of this symposium have appeared on YouTube. So this is the public face of Yale medical school. There’s some interesting history and a great deal of bunkum and double-speak. To save you time, I’ve cut out about 6 minutes from the movies. |
 |
View or download the movie here > [18.5 Mb, flv file].
Dean of education Richard Belitsky and Dr David Katz
Pretty remarble uh? Dr Katz goes through several different trials, all of which come out negative. And what is his conclusion? You guessed.
His conclusion is not that the treatments don’t work but that we need a “more fluid concept of evidence” .
It’s equally bizarre to hear Richard Belitsky, Dean of Medical Education at Yale saying he is “very proud” of this betrayal of enlightenment values. If this is what Yale now considers to be education, it might be better to go somewhere else.
This is not science. It isn’t even common sense. It is a retreat to the dark ages of medicine when a physician felt free to guess the answer. In fact it’s worse. In the old days there was no evidence to assess. Now there is a fair amount of evidence, but Dr Katz feels free to ignore it and guess anyway. He refers to teaching about evidence as ‘indoctrination’, a pretty graphic illustration of his deeply anti-scientific approach to knowledge. And he makes a joke about having diverted a $1m grant from CDC, for much needed systematic reviews, into something that fits his aims better.
Katz asks, as one must, what should we do if there is no treatment that is known to help a patient. That is only too frequent a problem. The reasonable thing to say is “there is no treatment that is known to help”. But Dr Katz thinks it’s better to guess an answer. There is nothing wrong with placebo effects but there is everything wrong with trying to pretend that you are doing more than give placebos. Perhaps he should consider the dilemmas of alternative medicine.
You can read about more about Yale’s activities here and in interviews here. Dr Katz says “The founding approach—and I think Andrew Weil, MD, gets the lion’s share of credit for establishing the concept —is training conventional practitioners in complementary disciplines”. Let’s take a look at this hero. Try, for example, Arnold Relman’s “A trip to Stonesville“.
“According to Weil, many of his basic insights about the causes of disease and the nature of healing come from what he calls “stoned thinking,” that is, thoughts experienced while under the influence of psychedelic agents or during other states of “altered consciousness” induced by trances, ritual, magic, hypnosis, meditation, and the like.”
“To the best of my knowledge, Weil himself has published nothing in the peer-reviewed medical literature to document objectively his personal experiences with allegedly cured patients or to verify his claims for the effectiveness of any of the unorthodox remedies he uses.”
Here is the advertisment for Andrew Weil’s nutrition symposium.

Not only does this yet again propagate the great antioxidant myth, but a few moments with Google show that it is riddled with vested interests, as already pointed out on Quackademics in USA and Canada.
What has brought medical schools down to this level?
That isn’t hard to see, The main thing is simply money. Very few university administrators have the intellectual integrity to turn down money, whatever the level of dishonesty that is required by its acceptance. You can buy a lot of silence for $100m
The US Taxpayer has given almost a billion dollars, via NIH.
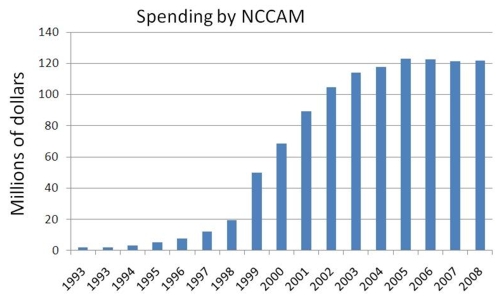
Wallace Sampson, MD says of NCCAM
“. . it has not proved effectiveness for any ‘alternative’ method. It has added evidence of ineffectiveness of some methods that we knew did not work before NCCAM was formed”
“Its major accomplishment has been to ensure the positions of medical school faculty who might become otherwise employed in more productive pursuits.”
“Special commercial interests and irrational, wishful thinking created NCCAM. It is the only entity in the NIH devoted to an ideological approach to health.”
NCCAM has given money from some very dubious trials too, Both Orac on Respectful Insolence and Dr RW (R.W. Donnell) have written recently about the NCCAM-funded trial of “chelation therapy”, as first exposed in a devastating article by Kimball C. Atwood IV, MD; Elizabeth Woeckner, AB, MA; Robert S. Baratz, MD, DDS, PhD; Wallace I. Sampson, MD on Medscape Today. This is a $30 million, 5-year, phase 3 Trial to Assess Chelation Therapy (TACT) for coronary artery disease.
“But how did such a crappy study ever come to be, much less be funded by the NIH to the tune of $30 million? The answer, not surprisingly, involves one of the foremost promoters of quackery in the federal government, Representative Dan Burton (R-IN).”
“We conclude that the TACT is unethical, dangerous, pointless, and wasteful. It should be abandoned.”
Orac comments
“TACT is not the only example of an unethical and scientifically worthless trial being funded not because the science is compelling but because powerful lobbies and legislators who are true believers in woo applied pressure to the NIH to do them”
The Bravewell Collaboration is the other major source of money. Forbes Business says “Bravewell is not some flaky New Age group”. Well dead wrong there, That is precisely what it is.
This group of ultra-rich people, according to its boss, Christy Mack, has a
So Bravewell is corrupting the search for real knowledge and real cures with big bucks. You can buy a lot of hokum for $100m. |
 |
The money comes from Morgan Stanley,
|
 |
Bravewell is run by his wife, Christy Mack (Mack-the-wife?) Vice-President, The C.J. Mack Foundation, Member, Board of Directors, The Bravewell Collaborative.
The Flexner report.
The story of Bravewell stands in chilling contrast to another case of philanthropy. Andrew Carnegie’s foundation financed the report by Abraham Flexner, “Medical Education in the United States and Canada” (1910) [download, 15 Mb] . That report was responsible for dragging medical education out of the dark ages
almost a century ago. It resulted in creation of some of the best medical schools anywhere (including Yale).
“By educational patriotism I mean this: a university has a mission greater than the formation of a large student body or the attainment of institutional completeness, namely, the duty of loyalty to the standards of common honesty, of intellectual sincerity, of scientific accuracy.”
“The tendency to build a system out of a few partially apprehended facts, deductive inference filling in the rest, has not indeed been limited to medicine, but it has nowhere else had more calamitous consequences.”
Flexner (1910).
Now another philanthropist is using big bucks to reverse the process and push medicine back into the 19th century.
Flexner would have thought it quite inconceivable that in 2007 medical schools would be offering Continuing Medical Education in homeopathy.
Why are Yale’s academics so quiet about this?
Perhaps they don’t even know it’s happening. If they say firmly that they don’t want it, it will go,
It’s been done before
Florida State University, allegedly under political pressure, proposed to set up a school of Chiropractic. That would have made it Florida State school of snake-oil salesmanship. What a sad fate. [ Science magazine comment] [comment form Paul Lee] [Comment in St Petersburg Times]
But the academics stopped it. An FSU professor, Albert Stiegman, predicted the future campus map.
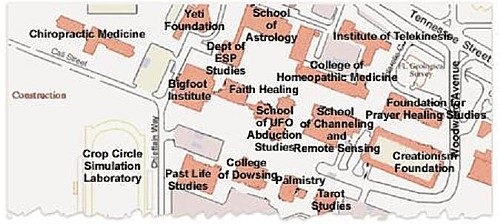
According to FSUnews
“The Florida Board of Governors voted 10-3 Thursday to deny Florida State University’s request to build a chiropractic school.”
“However, the passage of the bill for the chiropractic school by the Legislature seemingly bypassed the Board of Governors.”
In the end, reason won. Let’s hope that Yale follows their example.
Follow up
The problem of Yale has been taken up with great eloquence by some US commentators
Dr RW (R.W, Donnell): “Quackademic Medicine at Yale”
“By the way, where’s the AAMC in all this? Aren’t they supposed to be guardians of integrity and professionalism in medical education? Are they asleep at the switch or is money silencing them too?”
Orac (Respectful Insolence): “Integrative” medicine at Yale: A more “fluid” concept of evidence?”
“after the Dean of the Yale School Medicine embarrassed himself in the introduction by saying he’s proud of how far this nonsense has come, Dr. Katz takes the stage and demonstrates the sort of hostile attitude towards science that, if allowed to take root will be the death of scientific medicine in any meaningful form at U.S. medical schools”
Junkfood Science. Sandy Szwarc on “Quote of the day: ;We need a more fluid concept of evidence’”
“Will healthcare professionals and consumers . . . . speak out against these wellness programs being enacted by government agencies, insurers and employers? Or is the money too good?”
Science-based Medicine. Steven Novella writes on “Changing the rules of evidence“. When alternative medicine people do not like the evidence, they change the rules to get the outcome that they want, as seen so graphically in this post. They have always done this, but it is only recently that this sort of behaviour has been endorsed by places like Yale.
The Macho Response, another US blog, comments bluntly, in “Yale wants a more fluid concept of evidence”
This is beyond embarrassing – it’s a fucking crime – and it’s happening at Yale University and many others.
If you’re in the medical profession (and I know many of my readers are) you need to go here – now.
Kiosque Médias writes as follows
Pour ceux qui s’intéressent à la médecine et à la santé, le blog de David Colquhoun vaut probablement le détour. Ce professeur-chercheur au département de neurosciences, de physiologie et de pharmacologie de l’University College London y décrypte les résultats d’études médicales, en mettant l’accent sur les médecines alternatives. Et il est rarement tendre!
James Randi Newsletter. The hit rate soars after a recommendation this piece by the amazing Randi.
Hokum-Balderdash Assay. Edwardson writes
“Yale University is going to the ducks. It now has an Integrative Medicine program and in April held its first annual Integrative Medicine Scientific Symposium. I think there must’ve been a typo there. They must’ve meant “Ist Annual I.M. Pseudoscientific Symposium.” There! Now we’ve done away with the oxymoron.”
Why is Yale so secretive about its quackery department?,
Most universities are only to keen to boast about their grant income. Not in this case though. When I asked how they funded their quackery, all I got was a letter that had very obviously been drafted by a lawyer.
“As a private institution, Yale University is not generally subject to the U.S. Freedom of Information Act. We therefore respectfully decline to compile and provide the information you have requested.”
So pretty clear signs of guiltiness there.
Dr David Katz, yes, he of the “fluid concept of evidence”, has posted an article, Health Hazards of rhe Blogoshere. If it quacks like a duck . . .
It seems that he has been a bit alarmed by the reaction of the bloggers. It starts, rather pompously, thus.
“Being well educated does not guarantee you’ll always be right, and it certainly doesn’t guarantee everyone will agree with you. But it still matters. Or at least it used to “
But the rest if it reads less like a defence than as an admission of guilt, thus prompting the next item.
Paul Hutchinson’s blog
| A quack who admits it picks out a quotation from Dr Katz’s response and turned into a cartoon, released to the public domain, So here it is. | 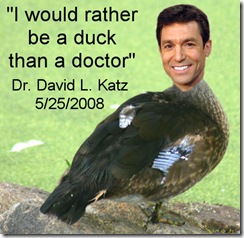 |
Respectful Insolence.
Orac comments too, in “Fluid evidence” strikes back: Dr. Katz versus the skeptical blogsophere”. He does a terrific job in taking apart the response from the hapless Dr Katz.
“No, Dr. Katz does not like his first encounter with the medical blogosphere at all. Indeed, he is so unhappy that apparently a few weeks ago he tried t answer the bloggers who had raked him over the coals for blatantly advocating “integrating” unscientific woo like homeopathy with scientific medicine. Unfortunately for him, he did not do a particularly good job of it. Indeed, what most stood out as I read his rejoinder was that he does not answer a single substantive criticism leveled at his comments. Not one. Instead, he does what pretty much all woo-meisters do when criticized for shifting goalposts and appealing to other ways of knowing besides science as a means of “proving” that their preferred fairy dust works; he wraps himself in the mantle of the brave iconoclast willing to challenge accepted dogma and whines about the peons who criticized him, heaping contempt on the bloggers who had the temerity to criticize his advocacy for pseudoscience because to him they have not earned the right to criticize his (at least in his opinion, apparently) greatness in comparison to him.”
| Last year, Nature published a pretty forthright condemnation of the award of Bachelor of Science degrees in subjects that are not science: in fact positively anti-science. This topic has come up again in Times Higher Education (24 April 2008). A league table shows that the largest number of anti-science courses is run by the University of Westminster [download paper version]. |
 |
Vice chancellors have consistently refused to answer letters, from me, from the Times Higher Education or from the BBC, asking them to defend their practices.
The vice chancellors union, Universities UK, has simply refused to consider this very basic threat to academic standards.
It is particularly amazing that vice-chancellors continue to support courses in homeopathy when they have been condemned by no less a person than the head honcho of homeopathy in the UK, Dr Peter Fisher. He is clinical director of the Royal London Homeopathic Hospital and Homeopathic Physician to the Queen. Peter Fisher and I were interviewed on BBC London News after publication of the Nature article. At the end, Fisher was asked by the presenter, Riz Lateef, about whether homeopathy was a suitable subject for a science degree.[Watch the movie]
| Riz Lateef (presenter): “Dr Fisher, could you ever see it [homeopathy] as a science degree in the future? Dr Peter Fisher: “I would hope so. I wouldn’t deny that a lot of scientific research needs to be done, and I would hope that in the future it would have a scientific basis. I have to say that at the moment that basis isn’t comprehensive. To that extent I would agree with Professor Colquhoun.” |
The one exception was a response, of sorts, that I got from Westminster University.
I can interpret this lack of response only as a sign of guilt on the part of the vice chancellors of the 16 or so universities who teach this stuff. That interpretation is reinforced by the refusal of two of them to release their teaching materials, despite requests under the Freedom of Information Act 2000. Both the University of Central Lancashire and the University of Westminster have turned down appeals, and refused to hand over anything. The former case has been with the Information Commissioner for some time now, and if the ruling goes as a hope, the taxpayer may soon be able to see how their money is being spent.
But the wonderful thing about the electronic age is that it has become really quite difficult to keep secrets. Last year I managed to find an exam paper set by the University of Westminster in Homeopathic Materia Medica, and a question from that paper has already appeared in Nature.
I recently acquired copies of a course handbook. and of the powerpoint slides used for the lecture on ‘Vibrational Medicine’ by the University of Westminster. This appears to be from a course in Complementary Therapies, part of “Health Sciences: Complementary Therapies BSc Honours”, according to Westminster’s web site. A lot of people have access to this first year course material, so Westminster needn’t bother trying to guess how I got hold of this interesting material
In the public interest, here are a few quotations. Taxpayers should know how their money is being spent.
According to the handbook
“Complementary Therapies is a core module for the Therapeutic Bodywork, Herbal Medicine, Homœopathy, Nutritional Therapy and Complementary Therapies courses. Therefore all students of these degree courses are required to take this module.”
The University of Central Lancashire also has “Vitalistic Medicine” as part of its BSc Homeopathy (but, like Westminster, has some excellent people too).
There is a rather good Wikipedia entry on Vitalism, a topic that is now largely the preserve of cranks.

The handbook is wonderful. The word ‘evidence’. in the context of ‘does it work?’, does not occur a single time. There is plenty of the usual edu-bollocks jargon that is so beloved by bureaucrats, but not the slightest hint of critical thinking about assessment of the ‘therapies’.
The course seems to be a romp through almost every form of battiness known to humankind. Not just homeopathy, traditional Chinese medicine and nutritional therapy, but also dowsing, crystal healing and other forms of advanced delusional thinking. Before somebody grumbles, let me emphasise that ‘nutrition’ is to be distinguished from ‘nutritional therapy’: the latter involves imaginative claims that buying expensive supplements can prevent or cure almost anything. There’s a lot more about that here, and here.
Here are just 5 days from the timetable.
| 9am-1.00pm : Homœopathy (group work and video) |
| 9am-1.00pm : Traditional Chinese Medicine |
| 9am-10.45pm : BODYWORK THERAPIES |
| 11.15-1.00pm : Nutritional Therapy |
| 9am-1.00pm : Vibrational Medicine/Energy Concepts (L&P) |
All this can be yours -at a cost.
Full-time UK/EU fee – £3,145
Full-time Overseas fee – £9,450
The slides for the last of these lectures show some of the most glorious examples of the abuse of sciencey-sounding words that I’ve seen in a while.
 |
 |
Sigh. All this is sheer imagination. It is ancient vitalism dressed up pretentiously in sciencey words.Then a bit later we come to the general theory -“energy concepts”.
 |
 |
More plausible-sounding, but utterly meaningless words about vibrations. And then on to old superstitions about dowsing with rods and pendulums.
 |
 |
.
Not a single word of scepticism appears about any of this mumbo jumbo. Can it get worse? Yes it can. CRYSTAL HEALING comes next.
 |
 |
Are you having difficulty in understanding what all these words mean? I certainly hope so, because they have no meaning to understand. Don’t worry too much though, There are some helpful diagrams.
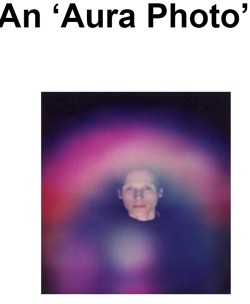 |
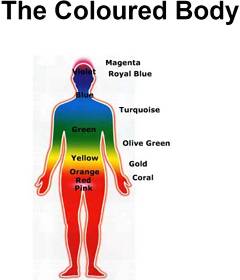 |
Aura photographs? They are just fairground conjuring tricks. Well, that is what you thought. But here we see them presented, apparently in all seriousness, as part of a vocational bachelor of science degree in a UK
university.Never mind, it is all assessed properly, with all the right box-ticking jargon. The course handbook says
| Learning Outcomes On successful completion of this module you will be able to: • describe the theoretical basis and classification of a range of complementary therapies |
What theoretical basis? There isn’t any theoretical basis, just a meaningless jumble of words.
You just couldn’t make it up.
Westminster University is not all like this
This post is not intended as an attack on the University of Westminster as a whole. Last year I had an invitation from their biomedical people to give a talk there. They asked for a talk on “What is is the evidence for Alternative Medicine?”. But then I got an email from them saying
“I was surprised to be sat on heavily on return from said trip by the VC, Provosts and Deans (including Peter Davies the leader of the Alt Med School !) once news of your talk leaked out. Could you give a talk on your research instead- yep I know its pusillanimous of me and yep I know unis stand for freedom of speech and yep I know that fellow members of staff suggested you come and others were keen to listen to your views on quackery.”
So on November 2nd 2007 I gave a seminar about single ion channel work (our new ideas about partial agonists). Of course all the excellent staff whom I met agreed with me about the embarrassment that having degrees in homeopathy etc. The fault lies not with their academic staff, but with their administration. Freedom of speech does not seem to be high on their agenda.
Postscript I recently learned that when Times Higher Education asked Westminster about my seminar, they were given the following statement.
“Prof David Colquhoun was invited to take part in a research seminar series organised by the University’s School of Biosciences last year. As part of this series, on Friday 2 November 2007, he gave a talk on the agreed topic of “Single ion Channel studies suggest a new mechanism for partial agonism” – his area of research.”
Perhaps I am naive, but it truly shocks me that a university can issue such a dishonest account of what happened.
This is a fuller version, with links, of the comment piece published in Times Higher Education on 10 April 2008. Download newspaper version here.
If you still have any doubt about the problems of directed research, look at the trenchant editorial in Nature (3 April, 2008. Look also at the editorial in Science by Bruce Alberts. The UK’s establishment is busy pushing an agenda that is already fading in the USA.
Since this went to press, more sense about “Brain Gym” has appeared. First Jeremy Paxman had a good go on Newsnight. Skeptobot has posted links to the videos of the broadcast, which have now appeared on YouTube.
Then, in the Education Guardian, Charlie Brooker started his article about “Brain Gym” thus
Dr Aust’s cogent comments are at “Brain Gym” loses its trousers. |
 |
The Times Higher’s subeditor removed my snappy title and substituted this.

So here it is.
“HR is like many parts of modern businesses: a simple expense, and a burden on the backs of the productive workers”, “They don’t sell or produce: they consume. They are the amorphous support services” .
So wrote Luke Johnson recently in the Financial Times. He went on, “Training advisers are employed to distract everyone from doing their job with pointless courses”. Luke Johnson is no woolly-minded professor. He is in the Times’ Power 100 list, he organised the acquisition of PizzaExpress before he turned 30 and he now runs Channel 4 TV.
Why is it that Human Resources (you know, the folks we used to call Personnel) have acquired such a bad public image? It is not only in universities that this has happened. It seems to be universal, and worldwide. Well here are a few reasons.
Like most groups of people, HR is intent on expanding its power and status. That is precisely why they changed their name from Personnel to HR. As Personnel Managers they were seen as a service, and even, heaven forbid, on the side of the employees. As Human Resources they become part of the senior management team, and see themselves not as providing a service, but as managing people. My concern is the effect that change is having on science, but it seems that the effects on pizza sales are not greatly different.
The problem with having HR people (or lawyers, or any other non-scientists) managing science is simple. They have no idea how it works. They seem to think that every activity
can be run as though it was Wal-Mart That idea is old-fashioned even in management circles. Good employers have hit on the bright idea that people work best when they are not constantly harassed and when they feel that they are assessed fairly. If the best people don’t feel that, they just leave at the first opportunity. That is why the culture of managerialism and audit. though rampant, will do harm in the end to any university that embraces it.
As it happens, there was a good example this week of the damage that can be inflicted on intellectual standards by the HR mentality. As a research assistant, I was sent the Human Resources Division Staff Development and Training booklet. Some of the courses they run are quite reasonable. Others amount to little more than the promotion of quackery. Here are three examples. We are offered a courses in “Self-hypnosis”, in “Innovations for Researchers” and in “Communication and Learning: Recent Theories and Methodologies”. What’s wrong with them?
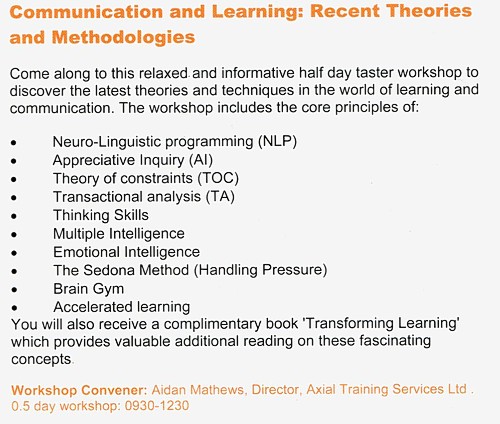
“Self-hypnosis” seems to be nothing more than a pretentious word for relaxation. The person who is teaching researchers to innovate left science straight after his PhD and then did courses in “neurolinguistic programming” and life-coaching (the Carole Caplin of academia perhaps?). How that qualifies him to teach scientists to be innovative in research may not be obvious.
The third course teaches, among other things, the “core principles” of neurolinguistic programming, the Sedona method (“Your key to lasting happiness, success, peace and well-being”), and, wait for it, Brain Gym. This booklet arrived within a day or two of Ben
Goldacre’s spectacular demolition of Brain Gym “Nonsense dressed up as neuroscience”
“Brain Gym is a set of perfectly good fun exercise break ideas for kids, which costs a packet and comes attached to a bizarre and entirely bogus pseudoscientific explanatory framework”
“This ridiculousness comes at very great cost, paid for by you, the taxpayer, in thousands of state schools. It is peddled directly to your children by their credulous and apparently moronic teachers”
And now, it seems, peddled to your researchers by your credulous and
moronic HR department.
Neurolinguistic programming is an equally discredited form of psycho-babble, the dubious status of which was highlighted in a Beyerstein’s 1995 review, from Simon Fraser University.
“ Pop-psychology. The human potential movement and the fringe areas of psychotherapy also harbor a number of other scientifically questionable panaceas. Among these are Scientology, Neurolinguistic Programming, Re-birthing and Primal Scream Therapy which have never provided a scientifically acceptable rationale or evidence to support their therapeutic claims.”
The intellectual standards for many of the training courses that are inflicted on young researchers seem to be roughly on a par with the self-help pages of a downmarket women’s magazine. It is the Norman Vincent Peale approach to education. Uhuh, sorry, not education, but training. Michael O’Donnell defined Education as “Elitist activity. Cost ineffective. Unpopular with Grey Suits . Now largely replaced by Training .”
In the UK most good universities have stayed fairly free of quackery (the exceptions being the sixteen post-1992 universities that give BSc degrees in things like homeopathy). But now it is creeping in though the back door of credulous HR departments. Admittedly UCL Hospitals Trust recently advertised for spiritual healers, but that is the NHS not a university. The job specification form for spiritual healers was, it’s true, a pretty good example of the HR box-ticking mentality. You are in as long as you could tick the box to say that you have a “Full National Federation of Spiritual Healer certificate. or a full Reiki Master qualification, and two years post certificate experience”. To the HR mentality, it doesn’t matter a damn if you have a certificate in balderdash, as long as you have the piece of paper. How would they know the difference?
A lot of the pressure for this sort of nonsense comes, sadly, from a government that is obsessed with measuring the unmeasurable. Again, real management people have already worked this out. The management editor of the Guardian, said
“What happens when bad measures drive out good is strikingly described in an article in the current Economic Journal. Investigating the effects of competition in the NHS, Carol Propper and her colleagues made an extraordinary discovery. Under competition, hospitals improved their patient waiting times. At the same time, the death-rate e emergency heart-attack admissions substantially increased.”
Two new government initiatives provide beautiful examples of the HR mentality in action, They are Skills for Health, and the recently-created Complementary and Natural Healthcare Council.(already dubbed OfQuack).
The purpose of the Natural Healthcare Council .seems to be to implement a box-ticking exercise that will have the effect of giving a government stamp of approval to treatments that don’t work. Polly Toynbee summed it up when she wrote about “ Quackery
and superstition – available soon on the NHS “ . The advertisement for its CEO has already appeared, It says that main function of the new body will be to enhance public protection and confidence in the use of complementary therapists. Shouldn’t it be decreasing confidence in quacks, not increasing it? But, disgracefully, they will pay no attention at all to whether the treatments work. And the advertisement refers you to
the Prince of Wales’ Foundation for Integrated Health for more information (hang on, aren’t we supposed to have a constitutional monarchy?).
Skills for Health, or rather that unofficial branch of government, the Prince of Wales’ Foundation, had been busy making ‘competences’ for distant healing, with a helpful bulletted list.
“This workforce competence is applicable to:
- healing in the presence of the client
- distant healing in contact with the client
- distant healing not in contact with the client”
And they have done the same for homeopathy and its kindred delusions. The one thing they never consider is whether they are writing ‘competences’ in talking gobbledygook. When I phoned them to try to find out who was writing this stuff (they wouldn’t say), I made a passing joke about writing competences in talking to trees. The answer came back, in all seriousness,
“You’d have to talk to LANTRA, the land-based organisation for that”,
“LANTRA which is the sector council for the land-based industries uh, sector, not with us sorry . . . areas such as horticulture etc.”.
Anyone for competences in sense of humour studies?
The “unrepentant capitalist” Luke Johnson, in the FT, said
“I have radically downsized HR in several companies I have run, and business has gone all the better for it.”
Now there’s a thought.
The follow-up
The provost’s newletter for 24th June 2008 could just be a delayed reaction to this piece? For no obvious reason, it starts thus.
“(1) what’s management about?
Human resources often gets a bad name in universities, because as academics we seem to sense instinctively that management isn’t for us. We are autonomous lone scholars who work hours well beyond those expected, inspired more by intellectual curiosity than by objectives and targets. Yet a world-class institution like UCL obviously requires high quality management, a theme that I reflect on whenever I chair the Human Resources Policy Committee, or speak at one of the regular meetings to welcome new staff to UCL. The competition is tough, and resources are scarce, so they need to be efficiently used. The drive for better management isn’t simply a preoccupation of some distant UCL bureaucracy, but an important responsibility for all of us. UCL is a single institution, not a series of fiefdoms; each of us contributes to the academic mission and good management permeates everything we do. I despair at times when quite unnecessary functional breakdowns are brought to my attention, sometimes even leading to proceedings in the Employment Tribunal, when it is clear that early and professional management could have stopped the rot from setting in years before. UCL has long been a leader in providing all newly appointed heads of department with special training in management, and the results have been impressive. There is, to say the least, a close correlation between high performing departments and the quality of their academic leadership. At its best, the ethos of UCL lies in working hard but also in working smart; in understanding that UCL is a world-class institution and not the place for a comfortable existence free from stretch and challenge; yet also a good place for highly-motivated people who are also smart about getting the work-life balance right.”
I don’t know quite what to make of this. Is it really a defence of the Brain Gym mentality?
Of course everyone wants good management. That’s obvious, and we really don’t need a condescending lecture about it. The interesting question is whether we are getting it.
There is nothing one can really object to in this lecture, apart from the stunning post hoc ergo propter hoc fallacy implicit in “UCL has long been a leader in providing all newly appointed heads of department with special training in management, and the results have been impressive.”. That’s worthy of a nutritional therapist.
Before I started writing this response at 08.25 I had already got an email from a talented and hard-working senior postdoc. “Let’s start our beautiful working day with this charging thought of the week:”.
He was obviously rather insulted at the suggestion that it was necessary to lecture academics with words like ” not the place for a comfortable existence free from stretch and challenge; yet also a good place for highly-motivated people who are also smart about getting the work-life balance right.”. I suppose nobody had thought of that until HR wrote it down in a “competence”?
To provoke this sort of reaction in our most talented young scientists could, arguably, be regarded as unfortunate.
I don’t blame the postdoc for feeling a bit insulted by this little homily.
So do I.
Now back to science.
This is an old joke which can be found in many places on the web, with minor variations. I came across it in an article by Gustav Born in 2002 (BIF Futura, 17, 78 – 86) and reproduce what he said. It has never been more relevant, so it’s well worth repeating. The title of the article was British medical education and research in the new century.
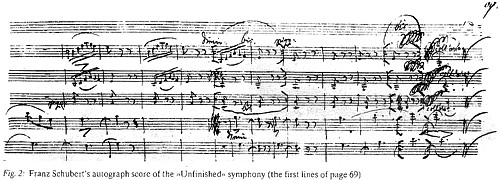
“The other deleterious development in UK research is increased bureaucratic control. Bureaucracy is notoriously bad for all creative activities. The story is told of a company chairman who was given a ticket to a concert in which Schubert’s Unfinished Symphony was to be played. Unable to go himself, he passed the ticket on to his colleague, the director in charge of administration and personnel. The next day the chairman asked, ‘Did you enjoy the concert?’ His colleague replied, ‘My report will be on your desk this afternoon’. This puzzled the chairman, who later received the following:
Report on attendance at a musical concert dated 14 November 1989. Item 3.
Schubert’s Unfinished Symphony.
- The attendance of the orchestra conductor is unnecessary for public performance. The orchestra has obviously practiced and has the prior authorization from the conductor to play the symphony at a predetermined level of quality. Considerable money could be saved by merely having the conductor critique the performance during a retrospective peer-review meeting.
- For considerable periods, the four oboe players had nothing to do. Their numbers should be reduced, and their work spread over the whole orchestra, thus eliminating the peaks and valleys of activity.
- All twelve violins were playing identical notes with identical motions. This was unnecessary duplication. If a larger volume is required, this could be obtained through electronic amplification which has reached very high levels of reproductive quality.
- Much effort was expended in playing sixteenth notes, or semi-quavers. This seems to me an excessive refinement, as listeners are unable to distinguish such rapid playing. It is recommended that all notes be rounded up to the nearest semi-quaver. If this were done, it would be possible to use trainees and lower-grade operatives more extensively.
- No useful purpose would appear to be served by repeating with horns the same passage that has already been handled by the strings. If all such redundant passages were eliminated, as determined by a utilization committee, the concert could have been reduced from two hours to twenty minutes with great savings in salaries and overhead.
- In fact, if Schubert had attended to these matters on a cost containment basis, he probably would have been able to finish his symphony.
In research, as in music, blind bureaucracy has the effect of destroying imaginative creativity. If that is truly valued, it must remain free from bureaucratic excesses. And indeed, the great strength of British science has always been the ability of curiosity-driven individuals to follow up original ideas, and the support that these individuals receive from organizations such as the MRC and the Wellcome Trust. This has given research workers the possibility to twist and turn in following up intuitions and ideas in other fields as well as their own. This freedom has been significantly eroded by job insecurity in universities and in commercial enterprises.”
Later in the article, Born talks about innovation in the pharmaceutical industry
“This ‘urge to merge’, which is affecting the pharmaceutical industry worldwide, is almost always claimed to be justified by the need for a larger research budget to sustain innovation. The actual evidence indicates that such mergers hide -for a while failure of innovation. An almost universal response to this problem has been to ‘streamline’ and ‘commercialize’ the process of research, with ultimate control vested in accountants rather than in pharmaceutically informed scientists. This has meant that the industry’s research and development programmes are being driven by technical novelties, notably computer- aided drug design, combinatorial chemistry, high-throughput screening and genomics. All these techniques are very cost-intensive and, what is worse, are superseding individual scientists with profound appreciation of disease mechanisms and knowledge of biochemical and pharmacological mechanisms. It is they whose ability to ask the crucial, often seemingly simple questions, that have led to blockbuster drugs. Outstanding British examples are James Black’s discovery of the gastric acid secretion inhibitors, and Hans Kosterlitz’s question whether the brain might perhaps contain some analgesic chemical like that in -of all things the poppy plant.”
“The fact is that drug discovery, like all discoveries, is more an individual than a team achievement, at least at the beginning. With a few notable exceptions, the trouble with the industry is summarized by a group research director at one of the leading pharmaceutical companies:
“Creative individuals are being driven out of the industry and being replaced by functionaries wbo parrot strategic maxims. Research is being driven by lawyers, financial experts, salesmen and market strategists who are completely unable to develop new ideas. It is doubtful whether there are any senior executives who understand the problem” (Drews, J., 1999 In quest of tomorrow’s medicine, Springer-Verlag, New York).
And further:
“Partly as a result of mismanagement and partly as a result of a search for solutions which takes no account of disease mechanisms and biomedical complexity, substantial parts of the pharmaceutical industry are failing to innovate at a rate which is needed for their health and for the health of the general public. Research management needs to be rethought with a much greater emphasis on creative individuals with a broad knowledge of biology and medicine, a lower emphasis on market research, and a greater openness to the information to be gained from clinical studies (Horrobin, D.F., 2000, Innovation in the pharmaceutical industry. J. R. Soc. Med. 93, 341 – 345. ).”
For more on keeping univeristies honest, see the excellent new blog, The storm breaking upon the university.


