acupuncture
The much-delayed public consultation on the Pittilo report has just opened.
It is very important that as many people as possible respond to it. It’s easy to say that the consultation is sham. It will be if it is left only to acupuncturists and Chinese medicine people to respond to it. Please write to them before the closing date, November 2nd 2009. The way to send your evidence is here.
There is a questionnaire that you can complete, with the usual leading questions. Best do it anyway, but I’d suggest also sending written evidence as attachment too. I just got from DoH the email address where you can send it. They said
| if you have material you wish to send which you can’t easily “shoehorn” into the questionnaire, please send it to the following mailbox:
HRDListening@dh.gsi.gov.uk |
Here are three documents that I propose to submit in response to the consultation.I ‘d welcome criticisms that might make it more convincing. Use any parts of them you want in your own response.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
|
I’ve written quite a lot about the Pittilo report already, in particular A very bad report: gamma minus for the vice-chancellor, and in The Times (see also the blog version).
Intriguingly, these posts are at number 2 in a Google search for “Michael Pittilo”. |
 |
Briefly, the back story is this.
It is now over a year since the Report to Ministers from “The Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK” [download the report].
The chair of the steering group was Professor R. Michael Pittilo, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The reason thet the report is so disastrously bad in its assessment of evidence is that it was written entirely by people with vested interests.
The committee consisted of five acupuncturists, five herbalists and five representatives of traditional Chinese medicine (plus eleven observers). There was not a single scientist or statistician to help in the assessment of evidence. And it shows: The assessment of the evidence in the report was execrable. Every one of the committee members would have found themselves out of work if they had come to any conclusion other than that their treatment works, Disgracefully, these interests were not declared in the report, though they are not hard to find. The university of which the chair is vice-chancellor runs a course in homeopathy, the most discredited of the popular forms of alternative medicine. That tells you all you need to know about the critical faculties of Michael Pittilo.
The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register normally be through a Bachelor degree with Honours
Let’s consider the virtue of these two recommendations.
Regulation by the Health Professions Council (HPC) breaks their own rules
For a start, this should be ruled out by the HPC’s own rules, which require “Practise based on evidence of efficacy” as a condition for registration. Since there is practically no “evidence of efficacy”, it follows that the HPC can’t regulate acupuncture, herbal and Chinese medicine as Pittilo recommends. Or so you’d think. But the official mind seems to have an infinite capacity for doublespeak. The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
In other words, the HPC simply decided to ignore its own rules, Its excuse for doing so is that regulation would protect “public safety” . But it simply would not do that. It is ell known that some Chinese herbs are adulterated with dangerous substances, but laws against that already exist. Trading Standards are much more likely to take appropriate action than the HPC. The Medicines and Health Regulatory Authority (MHRA) already deals with the licensing of herbal medicines. and, despite the fact that it recently betrayed its trust by allowing them to be labelled in a misleading way, they are the people to do it, not the HPC.
The Pittilo report (page 11) says
In future, it is hoped that more Government funding can be allocated to research into traditional/herbal medicines and acupuncture and that grants will become available to encourage practitioners to undertake postgraduate research work.
So they are asking for more government money.
In March 2007, the Chinese Government pledged to spend over $130 million over the next five years on research into the effectiveness of traditional Chinese medicine. It is to be hoped that this money will be targeted effectively to evaluate TCM.
It seems to have escaped the notice of Pittilo that roughly 100 percent of trials of Chinese medicine done in China come out positive. Elsewhere, very few come out positive,(see Vickers et al., 1998, Controlled Clinical Trials, 19, 159-166: download reprint) The Department of Health would be unwise to rely on Chinese research. Remember that modern acupuncture was not so much a product of ancient wisdom, but rather it stems from nationalist propaganda by Mao Tse-Tung, who needed a cheap way to keep the peasants quiet, though he was too sensible to use it himself.
The HPC report (page 5) cites these with the words
” . . . a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base.”
This sentence seems to assume that the outcomes of research will be to strengthen the evidence base. Thus far, precisely the opposite has been the case. The Pittilo group has apparently not noticed that the US National Institutes of Health has already spent a billion dollars on research in alternative medicine and failed to come up with a single effective treatment. There are better ways to spend money on health. See, for example $2.5B Spent, No Alternative Med Cures found. .An enornous amount of research has already been done and the outcomes have produced no good treatments,
The proposed regulation would endanger the public, not protect it.
The excuse given by the HPC for breaking its own rules is that it should do so to protect the public.
Likewise Ann Keen, Health Minister, said:
“Patient safety is paramount, whether people are accessing orthodox health service treatments or using alternative treatments”
So first we need to identify what dangers are posed by acupuncture, herbal medicine and traditional Chinese medicine.
- Acupuncture is fairly safe. Its biggest danger lies in the unjustified claims that are routinely made for what can be achieved by being impaled by needles. This poses a danger that people may use acupuncture in place of treatments that work
- Herbal medicines are unstandardised, so even the very few that may work are dangerous to patients because the dose of active principle is unknown and varies from one batch to another. Taking a herbal medicine is a bit like swallowing a random number of tablets, False health claims pose a danger to patients too, when they cause patients to avoid treatments that work.
- Traditional Chinese Medicine is probably the most dangerous. Like the other two, the medicines are unstandardised so the dose is never known. False health claims abound. And in addition to these dangers, many cases have been found of Chinese medicines being adulterated with poisonous substances or with conventional drugs.
The form of regulation proposed by Pittilo would do little or nothing to protect the public from any of these dangers.
The proposals accept the herbal and Chinese medicine as traditionally practised. Nothing would be done about one of the major dangers, the lack of standardisation. That is a problem that was solved by pharmacologists in the 1930s, when international standards were set for the biological activity of things like tincture of digitalis, and assays were devised so that different batches could be adjusted to the same potency. Now, 80 years later, it is being proposed by Pittilo that we should return to the standards of safety that existed at the beginning of the last century. That is a threat to public safety., but the proposed regulation would do nothing whatsoever to protect the public from this dangerous practice. On the contrary, it would give official government sanction to it.
The other major danger is that patients are deceived by false health claims. This is dangerous (as well as dishonest) because it can cause patients to avoid treatments that work better, The internet abounds with claims that herbs can cure anything from diabetes to cancer. Many are doubtless illegal, but regulators like the HPC have traditionally ignored such claims: they are left to Trading Standards, Advertising Standards and the Medicines and Health Regulatory Authority (MHRA) to deal with. The MHRA already also has responsibility for monitoring side effects. The HPC would not do this.
The analogy with chiropractic and the GCC
The foolishness of allowing statutory regulation for unproven treatments has recently been illustrated quite dramatically by the case of chiropractic. Chiropractors have had statutory regulation by the General Chiropractic Council, which was established by the Chiropractors Act of 1994. The British Chiropractic Association (BCA) recently decided to sue the science writer, Simon Singh, for defamation when he cast doubt on some of the claims made by chiropractors, in particular their claims to be able to cure colic and asthma in children. That led to close examination of the claims. In fact there is no reason to think that spinal manipulation works for asthma, or that it works for colic. In fact there is quite good evidence that the claims are false. The result was that about 600 well-justified complaints have been lodged with the GCC (enough to bankrupt the GCC if the complaints are dealt with properly).
The point of this story is that the statutory regulator had nothing whatsoever to prevent these false health claims being made. Two of the complaints concern practices run by the chair of the GCC. Worse, the GCC actually endorsed such claims. The statutory regulator saw its duty to defend chiropractic (apart from a handful of cases of sexual misdemeanours), not to protect the patient from false health claims. The respectability conferred by statutory regulation made false health claims easier and endangered the public. It would be a disaster if the same mistake were made again.
On 11th December 2008 I got a letter form the HPC which said
in our opinion a lack of evidence of efficacy would not impede our ability to set standards or deal with complaints we receive. The vast majority of cases we consider are related to conduct.
But perhaps that is because they haven’t tried “regulating” quacks before. Now that the public is far more conscious about health fraud than it used to be, one can predict confidently that the HPC would be similarly overwhelmed by a deluge of complaints about the unjustified health claims made by acupuncturists, herbal medicine and traditional Chinese medicine practitioners. There is no shortage of them to complain about.
The education problem
The Pittilo report recommends that the entry level for registration should be a bachelors degree with honours. At first sight it seems reasonable to ask that practitioners should be ‘properly qualified’, but when one looks at what is actually taught on these degrees it becomes clear that they endanger, rather than protect, the public,
There are two very big problems with this recommendation.
Firstly, you can’t have a bachelors degree with honours until after you have decided whether or not there is anything useful to teach. If and when any of the subjects under consideration and shown to work to a useful extent, then it would be quite reasonable to establish degrees in them. Even the report does not pretend seriously that that stage has been reached. The proposal to set up degrees in subjects, at least some of which are quite likely to have no more than placebo value, is self-evidently nonsense,
The time for degrees, and the time for government endorsement by statutory regulation, is after the therapies have been shown to work, not before.
The absurdity of thinking that the public will be protected because a practitioner has a degree in, say, acupuncture, is shown with startling clarity by a recently revealed examination paper in acupuncture’
You can download the entire exam paper. Here are a few highlights from it.

So students, in 2009, are being taught the crudest form of vitalism.

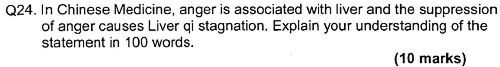
Teaching of traditional Chinese medicine is just as bad. Here are two slides from a course run by the University of Westminster.
The first ‘explains’ the mysterious and entirly mythical “Qi”.

So “Qi” means breath, air, vapour, gas, energy, vitalism. This is meaningless nonsense.
The second slide shows the real dangers posed by the way Chinese medicine is taught, The symptoms listed at the top could easily be a clue to serious illness, yat students are taught to treat them with ginger. Degrees like this endanger the public.

There are more mind-boggling slides from lectures on Chinese medicine and cancer: they show that what students are being taught is terrifyingly dangerous to patients.
It is entirely unacceptable that students are being taught these ancient myths as though they were true, and being encouraged to treat sick people on their basis. The effect of the Pittilo recommendations would be to force new generations of students to have this sort of thing forced on them. In fact the course for which this exam was set has already closed its doors. That is the right thing to do.
Here’s another example. The course leader for “BSc (Hons) Herbal Medicine” at the Univsrsity of Central Lancashire is Graeme Tobyn BA. But Tobyn is not only a herbalist but also an astrologer. In an interview he said
“At the end I asked her if I could cast her horoscope. She threw up her hands and said, ‘I knew this would happen if I came to an alternative practitioner.”
“I think the ruler of the ascendant was applying to Uranus in the ninth house, which was very pertinent.”
This would be preposterous even in the life style section of a downmarket women’s magazine, The Pittilo report wants to make degrees run my people like this compulsory. Luckily the Univerity of Central Lancashire is much more sensible and the course is being closed.
The matter is, in any case, being taken out of the hands of the government by the fact that universities are closing degrees in complementary medicine, including courses in some of those under discussion here, The University of Salford and the University of Central Lancashire have recently announced the closure of all the degree programmes in complementary and alternative medicine. The largest provider of such degrees, the University of Westminster has already shut down two of them, and the rest are being assessed at the moment. It is likely that the rest will be closed in the future.
The revelation that Westminster had been teaching its first year students that “amethysts emit high yin energy” and that students had been taught to diagnose disease and choose treatments by means of a dowsing pendulum, showed very clearly the sort of utter nonsense that undergraduates were being forced to learn to get a ‘bachelors degree with honours’. It stretches credulity to its limits to imagine that the public is protected by degrees like this. Precisely the opposite is true. The universities have recognised this, and shut the degrees. One exception is Professor Pittilo’s own university which continues to run a course in homeopathy, the most discredited of all the popular types alternative medicine.
A simpler, more effective and cheaper way to protect the public
I must certainly agree with the minister that protection of the public is an important matter. Having established that the Pittllo recommendations are more likely to endanger the public than protect them, it is essential to suggest alternative proposals that would work better.
Luckily, that is easy, because mechanisms already exist for dealing with the dangers that were listed above. The matter of adulteration, which is serious in traditional Chinese medicine, is a matter that is already the responsibility of the Office of Trading Standards. The major problem of false claims being made for treatment is also the responsibility of the Office of Trading Standards, which has a statutory duty to enforce the Unfair Trading Consumer Protection Regulations of May 2008. These laws state, for example, that
“One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”
The monitoring of false claims, and of side effects of treatments, is also the responsibility of the Medicines and Health Regulatory Authority (MHRA).
Rather than setting up complicated, expensive and ineffective ‘regulation’ by the HPC, all that need to be done is to ensure that the MHRA and/or Trading Standards have the funds to enforce existing laws. At the moment, they are not being implemented effectively, so I’d recommend that responsibility for enforcing the law against false health claims be transferred entirely to the MHRA, which has much more expertise in such matters than Trading Standards This would be both cheaper and more effective than the present system in which the responsibility is divided between the two organisations in an unclear way.
This proposal would protect the public against unsafe and adulterated treatments, and it would protect the public against false and fraudulent claims. That is what matters. It would do so more effectively,
more cheaply and more honestly than the Pittilo recommendations. There would be no reduction in patient choice either, There is no proposal to ban acupuncture, herbal medicine or traditional Chinese medicine. All that is necessary is to ensure that they don’t endanger the public.
Since the root of the problem lies in the fact that the evidence for the effectiveness is very weak. the question of efficacy, and cost-benefit ratio, should be referred to NICE. This was recommended by the House of Lords Report (2000). It is recommended again by the Smallwood report (sponsored by the Prince of Wales Foundation). It is baffling that this has not been done already. It does not seem wise to spend large amounts of money on new research at the moment, in the light of the fact that the US National Institutes of Health has already spent over $1 billion on such research without finding a single useful treatment.
The results of all this research has been to show that hardly any alternative treatment are effective. That cannot be ignored.
Conclusion
Recent events show that the halcyon days for alternative medicine are over. When the Pittilo report first appeared, it was greeted with derision in the media. For example, in The Times Alice Miles wrote
“This week came the publication of the Report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK. Otherwise known as twaddle.”
In the Independent, Dominic Lawson wrote
So now we will have degrees in quackery.
What, really, is the difference between acupuncture and psychic surgery?
People will no doubt continue to use it and that is their right and their responsibility. But if the government were to accept the recommendations of the Pittilo report it would be seen, quite rightly, as being anti-scientific and of posing a danger to the public.
Fortunately there is a better, and cheaper, way to protect the public.
Follow-up
Margaret McCartney’s blog in the Financial Times puts rhw view of a GP with her usual sense, humour and incisiveness.
“This report would, if implemented, create lots more nonsense exam papers funded by a lot more public money – and would produce practitioners without the absolutely crucial skill of how to assess evidence and reject or use it appropriately”
The Times has covered the story (with some interesting comments) Consultation on how to regulate complementary and alternative therapies
Times Higher Education UK-wide consultation on CAM regulation is launched Excellent response from Andy Lewis.
The Sun has by far the best coverage up to now, Jane Symons writes “Regulating quacks helps them prey on gullible patients“
Acupuncture has been in the news since, in a moment of madness, NICE gave it some credence,
Some people still seem to think that acupuncture is somehow more respectable than, say, homeopathy and crystal healing. If you think that, read Barker Bausell’s book ot Trick or Treatment. It is now absolutely clear that ‘real’ acupuncture is indistinguishable from sham, whether the sham control uses retractable needles, or real needles in the ‘wrong’ places. There has been no clear demonstration of long-lived benefits in any condition, and it is likely that it is no more than a theatrical placebo.
In particular, the indistinguishability of ‘real’ and sham acupuncture shows, beyond reasonable doubt that all the stuff about “energy flow in meridians” is so much hokum.
There is a small group of ‘medical acupuncturists‘ that believes that it is hokum. but who nonetheless maintain that acupuncture works, despite the evidence to the contrary. But most acupuncturists go for the wholesale gobbledygook.
If you don’t believe that, take a look at the exam paper that has come into my possession. It is this year’s exam from the University of Salford. Salford has, very sensibly, now decided to stop all its degrees in alternative medicine, so don’t hold this against the university too much.
You can download the entire exam paper. Here are a few highlights.
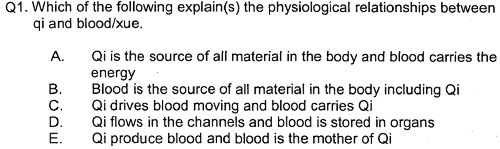
So students, in 2009, are being taught the crudest form of vitalism.
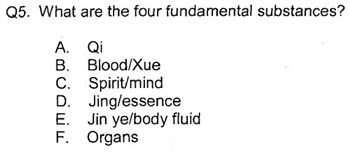
Oh really. Perhaps protons neutrons and electrons?
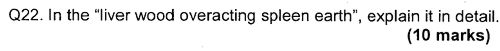
OK I’d fail that one because the words have no obvious meaning at all.
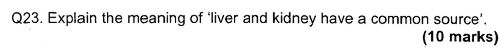
Perhaps an elementary textbook of embryology would help?
How one would love to see a set of model answers for these questions.
All this is ancient hokum being taugh to hapless students in the 21st century as though it were fact. The University of Salford has understood that and closed the course. All we need now is for NICE and the Department of Health to understand what it is that they are promoting.
NICE neglected the cultural cost of their guidance
When National Institute for Health and Clinical Excellence (NICE) included an acupuncture option on their low back pain guidance, they quite forget that one effect of their decision would be to ensure that new generations of students would have their minds poisoned with intellectual junk like this. That is why NICE really must think again. . See also
NICE falls for bait and switch by acupuncturists and chiropractors
NICE fiasco part 2 Rawlins should withdraw guidance and start again
NICE fiasco Part 3. Too many vested interests, not enough honesty
Pittilo and statutory regulation
Public consultation is due to open shortly on the appalling report of the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK (see also, The Times)
One of the recommendations is that acupuncture and Chinese herbal medicine should have statutory regulation by the Health Professions Council (HPC), despite the fact that that would involve the HPC breaking its own rules. Another recommendation of Pittilo is that entry to the “profession” (his word, not mine) should be by means of honours degree only. So he wants to impose on students exams like this one in order to “protect the public”? The absurdity of that proposal should be obvious now. This exam paper will form part of my evidence to the consultation.
And there is one other small problem. Universities are busy shutting down their degrees in alternative medicine, now that the ridiculousness of what is taught has been exposed. They have shut down entirely at the University of Salford and at the University of Central Lancashire, And even the University of Westminster is working on closing them.
All we need now is for the common sense and integrity that has been shown by these universities to spread to the Department of Health (and NICE).
Follow-up
|
.The University of Central Lancashire (UCLAN) is the first place I asked to see teaching materials that were used on its homeopathy “BSc” course. The request was refused, and subsequent internal appeals were refused too, Clearly UCLAN had something to hide. |

|
An appeal to the information commissioner took almost two years to be judged, but the case was won. The eventual decision by the Information
Commissioner rejected all the grounds that UClan had used to evade the Freedom of Information Act.
UClan appealed against the judgement and I still haven’t got the stuff but that hardly matters now, because the course in question shut its doors. In any case, plenty of stuff from similar courses has leaked out already.
Meanwhile, in September 2008, UCLAN announced an internal review of all its courses in magic medicine, The review seemed to be genuine. For a start they asked me to give evidence to the review (something that no other university has done). They also asked Michael Eslea to give evidence. He is the UCLAN psychologist, whose magnificent open letter probably tipped the authorities into holding the review.
Just in case it is useful to anyone, here is a copy of the written evidence that I sent [download pdf],
|
Report of the Working Party on the Review of issues associated with Homeopathy, Acupuncture and Chinese Herbal Medicine
1. Introduction As a consequence of concerns expressed by some colleagues within the University of Central Lancashire (UCLan) Dr Malcolm McVicar, Vice Chancellor appointed a working party to review the issues associated with the University offering courses in Homeopathy, Acupuncture and Chinese Herbal Medicine. MEMBERSHIP: Eileen Martin (Chair) Pro-Vice Chancellor and Dean of Faculty of Health and Social Care |
The report was the subject of a special meeting of UCLAN’s Academic Board on 9th July 2009. The following resolutions were passed.
|
Resolutions R1 That further minor revisions be made to the report prior to publication on the University’s website; R2 That the University refrain from offering any practitioner-qualifying courses in Homeopathy, Acupuncture and Chinese Herbal Medicine until such disciplines have achieved statutory regulation status; R3 That the University consider offering a limited number of postgraduate research studentships (leading to Masters by Research of PhD) to suitably qualified UCLan students and staff in these disciplines. They should have interdisciplinary supervisory teams to facilitate development of a broad range of research skills and to contribute to the generation of knowledge in CAM; R4 That the University consider how more interdisciplinary teaching can be achieved, where appropriate, within both undergraduate and postgraduate teaching to facilitate greater exposure to subject expertise and different paradigms. |
Resolutions 1, 3 and 4 say very little. Resolution 4 sounds thoroughly relativist. We are talking about medicine, about treating sick patients. There is only one “paradigm”. That is to find treatments that are as effective and safe as possible. There aren’t two sorts of medicine, regular and alternative. There is just medicine that works and medicine that doesn’t work. It’s a good illustration of DC’s rule number 2, “never trust anyone who uses the word paradigm”.
Resolution 2 is the really interesting one, because none if the topics, Homeopathy, Acupuncture and Chinese Herbal Medicine, is subject to statutory regulation.
If taken literally, resolution 2 means that all the UCLan courses in alternative medicine will close their doors. Bafflingly, this inevitable conclusion is not stated explicitly.
At least resolution 2 means that homeopathy, already closed, will stay closed. It is never likely to get statutory regulation.
For practical purposes, we can ignore for the moment the obvious fact that statutory regulation of nonsense subjects results only in nonsense. The only forms of alternative medicine that have got “statutory regulation” at the moment are chiropractic and osteopathy. The public has not been safeguarded by the General Chiropractic Council (GCC). The GCC, on the contrary, has endangered the public by allowing false health claims to be made with impunity. Perhaps the members of the review committee had not noticed that the Simon SIngh affair has resulted in almost 600 complaints being made to the GCC? The faith of the review in statutory regulation is clearly misplaced.
The Pittilo report is critical for what happens next
Acupuncture and Chinese Herbal Medicine are not subject to statutory regulation at present, so one would suppose that these degrees will close their doors too. However the infamous Pittilo report has proposed that they should become regulated by the Health Professions Council (HPC). The many problems of the Pittilo report have been documented here, in “A very bad report: gamma minus for the vice-chancellor“. There was also a high-profile critique of the report in The Times (and on this blog).
The HPC has, as one of its criteria for regulation, “evidence-based practice”. Disgracefully, the HPC has already shown its willingness to ignore its own rules and to act as statutory regulator for Acupuncture and Chinese Herbal medicine. This rather disgraceful behaviour is documented in “Health Professions Council ignores its own rules: the result is nonsense“.
The UCLAN report seems to assume that the recommendations of the Pittilo report will be accepted. But the long-awaited consultation has still not opened. We can be sure that when it does, the opposition to it will be very strong indeed.
The report in full
Here are a few comments on the report itself. Download the full report (as of July 15th).
i have to say that when I visited Preston to give evidence, my views seem to be treated seriously, even sympathetically, so it was a great disappointment to see the outcome. So what’s wrong? The major disaster is declared early in the report.
Section 2, Context
The debate is centred on a number of key themes which relate to:-
1. The quality of and/or absence of an evidence base to support claims of the efficacy and benefits of such treatments, linked to issues of public safety/protection and professional regulation.
Sounds good. What matters about any sort of medicine is whether or not it works and whether it is safe. It therefore verges on the incredible that we read in section 4.1
“conclusions from research into the efficacy of the various CAM’s are outside the remit of this report.”
The whole point about CAM is that there is very little evidence that any of it works. So the review committee decided to ignore the most important problem of the lot. I can’t see how any rational decision can be made without first deciding whether the treatment is better than placebo. That, surely, is the main question, and it was dodged.
UCLAN has failed to grasp the nettle, just as the Department of Health has also consistently failed to do so.
Section 4,1 Efficacy This section repeats the assertion, absurd to my mind, that it is possible to judge CAM courses while declining to assess whether they work or not.
Section 4.2 Role of Universities in Society.
There is universal agreement that critical thinking is crucial to the idea of a university, but the judgement of whether CAM teaches critical thinking is simply fudged. Again the report fails to grasp the nettle.
“Disagreements about critical thinking within CAMs arises because some will argue that such substantiation and assessment can occur within the discipline, whilst others will argue that the methodology for substantiation, that is evidence provision, is universal. As a result, the latter will demand that evidence is provided using methods from one field (e.g. randomised controlled trials) for use in another.”
Sadly, the report dodged the crucial judgement once again. The most obvious characteristic of every form of alternative medicine is their total lack of critical self-appraisal. It is very sad that the review committee could not bring itself to say so.
Section 4.4 Nomenclature of degrees
Recommendation
The nomenclature of courses, leading to a professional as well as an academic award, should reflect the professional route; for example Bachelor with Honours in Complementary Medicine, B Comp. Med.(Hons) or B Acupuncture (Hons).
This sounds to me like another truly pathetic fudge. What on earth is solved by changing the name of the degree? You’d still be teaching students the same load of gobbledygook and then letting them loose on sick people, whether you call it a Bachelor of Science, a Bachelor of Arts, or, as is recommended here, a Bachelor of nothing whatsoever.
Well, I suppose there is a (doubtless unintended) irony in calling CAM degrees “Bachelor of nothing whatsoever”.
Section 4.4 Ethical, non-harm and economic considerations
This section list a lot of reasons why teaching alternative medicine should be unethical. but nevertheless manages to conclude that
” . . . it is not unethical to offer courses in Homeopathy, Acupuncture and Chinese Herbal Medicine at a university.”
I find the logic by which this bizarre conclusion was reached quite impossible to follow. Like much of the rest of the report this conclusion seems to stem from a reluctance to grapple with the really important questions, like ‘does it work or not?’.
Despite this the recommendation is perhaps the most interesting of all.
“Recommendation
• The University refrains from offering any CAM courses until such disciplines have achieved statutory regulation status.”
This recommendation was accepted, and passed as a resolution at Academic Board. If it is implemented now, than there will be no more alternative medicine degrees next year at the University of Central Lancashire. If and when this happens, the University must be congratulated on its return to rational medicine.
Follow-up
Michael Eslea, UCLAN’s hero in resisting nonsense from the inside, has posted on this topic.
17 July 2009. It seemed odd that that no announcement was made about the future if the remaining CAM courses at UCLAN. So I asked deputy Vice-Chancellor Patrick McGhee for clarification. After a couple of days, I got this response.
|
From: CTheobald@uclan.ac.uk To: d.colquhoun@ucl.ac.uk Hi David, I have been asked to respond to your question below on the running of acupuncture and Chinese herbal medicine at UCLan. It is correct to assume that UCLan will not be taking any new entrants onto these programmes until further notice. Best Wishes Chris Chris Theobald |
So the report may have been disappointing, but it has done the job. As several people have pointed out in comments, it would be asking too much to expect a university to say “sorry we just noticed that we have been running junk-science courses for years”. But they have done the right thing anyway.
The first post was NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself.
That was followed by NICE fiasco, part 2. Rawlins should withdraw guidance and start again.
Since then, something of a maelstrom has engulfed NICE, so it’s time for an update.
It isn’t only those who are appalled that NHS should endorse voodoo medicine on the basis of very slim evidence who are asking NICE to rethink their guidance on low back pain. Pain specialists are up in arms too, and have even started a blog, ‘Not Nearly as NICE as you think …‘, to express their views. Equally adverse opinions are being expressed in the Britsh Medical Journal. A letter there is signed by over 50 specialists in pain medicine. It ends thus
“Because of these new guidelines patients will continue to experience unnecessary pain and suffering and their rights to appropriately individually tailored treatment have been removed on the basis of a flawed analysis of available evidence. We believe the guidelines do not reflect best practice, remove patient choice and are not in our patients’ best interests.”
In a contribution headed “NICE misguidance”. Dr Michel Vagg ends
It seems to me that this guideline has been used as a propaganda vehicle to allow cherry-picked evidence to be enshrined as doctrine. This is an abuse of the guideline development process . . . ”
I have to say, though, that it seems to me that some of these people are promoting their own interests as much as chiropractors and acupuncturists. The evidence that spinal injections produce worthwhile benefits seems to be as thin as the evidence that chiropractic and acupuncture produce worthwhile benefits. But no doubt the injections are good for the budgets of PCTs or private practice doctors.. Could it perhaps be the case that some of the clinicians’ anger is being generated by doctors who are rushing to defend their own favourite ineffective treatment?
Why, oh why, can’t either NICE or the pain consultants bring themselves to state the obvious, that nothing works very well. The only thing that can be said for most of the regular treatments is that although they may not be much more effective than acupuncture or chiropractic, at least they don’t come with the intellectually-offensive hokum that accompanies the latter. Very sensible attempts have been made to identify the cause of low back pain [reviewed here], Occasionally they succeed. Mostly they don’t.
One clinician’s letter deserves special attention because it goes into the evidence, and the costs, in some detail. Its conclusions are very different from those in the NICE guidance.
The letter, a Review of NICE guidance, is from Dr C.J.D. Wells [download the whole letter]. He is a pain relief consultant from Liverpool.
Let’s look at some highlights.
Wells points out the absurdity of the cost estimates
“In the pricing section, they estimate that this will require an increase of facilities so that 3,500 patients can be treated instead of 1,000 at present (again see comments on pricing). This is not many treatments for the 20 million sufferers, of whom we can estimate that at least 2 million will have significant long-term disability and psychological distress”
And that is without even costing all the secondary costs of miseducating a new generation of students in fables about “Qi”, meridians, energy flow, subluxations and innate intelligence.
“The abysmal ignorance of the committee is reflected in the poor overall advice. So if you have a committee with special interests in Exercise, Manipulation, PMP’s, and Surgery, and you call an expert on Acupuncture, you get advice to use Exercise, Manipulation, Acupuncture, PMP’s and Surgery. Amazing.”
Another pain consutant, Charles Guaci, says in a comment in the Daily Mail.
I am a Pain Consultant of 30 years experience, have published two books (one translated into different languages).
NICE never asked me for my opinion.
This is the most ridicuculous pseudo-scientific document I have ever seen.
The panel consisted of a surgeon, psychologist, osteopath, acupuncturist a physiotherapist and an academic; not one pain consultant! The conclusions are simply a means of increasing the employment of their friends!
All evidence submitted to NICE was ignored.
It is almost certain than unless NICE rethink their ideas that Pain Consultants will be seeking a judicial review as well as full disclosure of how the panel arrived at their bizarre findings under the Freedom of information act.
Patients should realise that they are being taken for a ride.
Despite the outcry from opponents of magic medicine and from pain specialists, the assessment by the normally excellent NHS Choices site was disappointing. It made no mention at all of the secondary consequences of recommending CAM and described the assertions of the guidance group quite uncritically.
The reputation of NICE
NICE has been criticised before, though usually unjustly. In the past I have often supported them. For example. when NICE said that treatment of dementia with anticholinesterase drugs like galantamine was ineffective, there was a great outcry, but NICE were quite right. There is little or no rationale for such treatments, and more importantly, very little evidence that they work. But patients, especially when they are desperate, have greater faith in drug treatments than most pharmacologists, They want to clutch at straws. A bit like the NICE guidance committee, faced with a bunch of treatments most of which are almost ineffective, clutched at the straws of acupuncture and chiropractic. But this time it isn’t only the patients who are cross. It is most of the medical and scientific world too.
One interpretation of these bizarre events is that they represent a case of medical/scientific arrogance. Ben Goldacre wrote of another aspect of the same problem thus week, in Dodgy academic PR [download the paper on which this is based].
The first job of a scientist is to say openly when the answer to a question is not known. But scientists are under constant pressure to exaggerate the importance of their results. Last year we published an article which I feel may, if verified, turn out to be the second most important that I have ever been an author on. Because it happened to be published in Nature (not because of its quality), a press release was written (by an arts graduate!). It took some argument to prevent the distorted and exaggerated account being imposed on the public. This is typical of the sort of thing reported in Goldacre’s column. I reported a similar case a while ago, Why honey isn’t a wonder cough cure: more academic spin.
If NICE does not reconsider this guidance, it is hard to see how it can be taken seriously in the future. I hope that when NICE’s director, Professor Sir Michael Rawlins, returns from his trips abroad, he will find time to look at the case himself.
Indirectly, then, it can be argued that NICE’s bizarre guidance is just another manifestation of the management of science being passed from the hands of scientists into the hands of administrators and spin experts. It is yet another example of DC’s rule
Never trust anyone who uses the word ‘stakeholder’
Some bone-headed bureaucrat decides that any charlatan or quack is a ‘stakeholder’ in the provision of NHS care and gives them a quite disproportionate say in how taxpayers’ money is spent. The bureaucrats are so busy following processes and procedures, ticking boxes, and so deficient in scientific education, that they failed to notice that they’ve been caught out by the old trick of used car salesmen, bait and switch.
The consequences
The expected consequences have already started to materialise. The Prince of Wales’ Foundation for Magic Medicine is jubilant about having been endorsed by NICE. And I’m told that “The chiropractors have now just written letters to all health boards in Scotland asking for contracts for their services to deal with back pain”.
There could hardly have been a worse time for NICE to endorse chiropractic. We are in the middle of a storm about free speech because of the disgraceful action of the British Chiropractic Associaton in suing one of our best science writers, Simon Singh, for defamation because he had the temerity to express an opinion, Of course, even if the BCA wins in court, it will be the overall loser, because chiropractic claims are now being scrutinised as never before (just look at what they told me).
Follow-up
A much-cited paper. The paper that is most often cited by chiropractors who claim to be able to cure colic by spinal manipulation is Klougart N, Nilsson N and Jacobsen J (1989) Infantile Colic Treated by Chiropractors: A Prospective Study of 316 Cases, J Manip Physiol Ther,12:281-288. This is not easy to get hold of but Steve Vogel has sent me s scanned copy which you can download here. As evidence it is about as useless as the infamous Spence study so beloved of homeopaths. There was no control group at all. It simply follows 316 babies and found that most of them eventually got better. Well, they do, don’t they? It is a sign of the pathetic standard of reaearch in chiropractic that anyone should think this paper worth mentioning at all.
June 6 2009. More flak for NICE from the Royal College of Anaesthetists, and more adverse comment in the BMJ. And of course the blogs. for example, “If this is “evidence based medicine” I want my old job back“.
“Acupuncture on the NHS: a dangerous precedent”: a good analysis at counterknowledge.com.
June 6 2009, Comment sent to the BMJ. The comment was submitted, as below, early on Friday 5th June. The BMJ said it was a “sensitive issue” and for the next five days lawyers pondered over it.
Underwood and Littlejohns describe their guidance as being a “landmark”. I can only agree with that description. It is the first time that NICE has ever endorsed alternative medicine in the face of all the evidence. The guidance group could hardly have picked a worse moment to endorse chiropractic. Chiropractors find it so hard to find evidence for their practices that, when one of our finest science writers, Simon Singh, asked to see the evidence they sued him for defamation. I suggest that the guidance group should look at the formidable list of people who are supporting Singh, after his brave decision to appeal against this iniquitous persecution.
Of course I’m sure this bizarre decision has nothing to do with the presence on the guidance group of Peter Dixon, chair of the General Chiropractic Council. Nevertheless, I am curious to know why it is that when I telephoned two of the practices belonging to Peter Dixon Associates, I was told that they could probably treat infantile colic and asthma. Such claims have just been condemned by the Advertising Standards Authority.
The low back pain guidance stands a good chance of destroying NICE’s previously excellent reputation for dispassionate assessment of benefits and costs. Yes, that is indeed a landmark of sorts.
If NICE is ever to recover its reputation, I think that it will have to start again. Next time it will have to admit openly that none of the treatments work very well in most cases. And it will have to recognise properly the disastrous cultural consequences of giving endorsement to people who, when asked to produce evidence, resort to legal intimidation.
Eventually, on Wednesday 10 June the comment appeared in the BMJ, and it wasn’t greatly changed. Nevertheless if is yet another example of legal chill. This is the final version.
Underwood and Littlejohns describe their guidance as being a “landmark”. I can only agree with that description. It is the first time that NICE has ever endorsed alternative medicine in the face of all the evidence. The guidance group could hardly have picked a worse moment to endorse chiropractic. Chiropractors are so sensitive about criticisms of their practices that, when one of our finest science writers, Simon Singh, queried the evidence-base for their therapeutic claims they sued him for defamation. I suggest that the guidance group should look at the formidable list of people who are supporting Singh, after his brave decision to appeal against an illiberal court ruling in this iniquitous persecution.
One wonders whether this bizarre decision by NICE has anything to do with the presence on the guidance group of Peter Dixon, chair of the General Chiropractic Council. I am also curious to know why it is that when I telephoned two of the practices belonging to Peter Dixon Associates, I was told that chiropractic could be effective in the treatment of infantile colic and asthma. Similar claims about treating colic have just been condemned by the Advertising Standards Authority.
The low back pain guidance stands a good chance of destroying NICE’s previously excellent reputation for dispassionate assessment of benefits and costs. Yes, that is indeed a landmark of sorts.
If NICE is ever to recover its reputation, I think that it will have to start again. Next time it will have to admit openly that none of the treatments works very well in most cases. And it will have to recognise properly the disastrous cultural consequences of giving endorsement to people who, instead of engaging in scientific debate, resort to legal intimidation.
Bait and switch. Oh dear, oh dear. Just look at this. British Chiropractic Association tell their members to hide their sins from prying eyes.
Excellent round-up of the recent outburst of writing about “chiroquacktic” (Tut, tut, is there no respect?).
Dr Crippen writes “NICE recommends a cure for all known disease” [Ed some exaggeration, surely]
Two days ago I wrote NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself
Now the official ‘guidance’ is out, and it is indeed quite as bad as the draft.
The relevant bits now read thus.
- Offer one of the following treatment options, taking into account patient preference: an exercise programme, a course of manual therapy or a course of acupuncture. Consider offering another of these options if the chosen treatment does not result in satisfactory improvement.
- Consider offering a structured exercise programme tailored to the person:
- This should comprise of up to a maximum of 8 sessions over a period of up to 12 weeks.
- Offer a group supervised exercise programme, in a group of up to 10 people.
- A one-to-one supervised exercise programme may be offered if a group programme is not suitable for a particular person.
- Consider offering a course of manual therapy, including spinal manipulation, comprising up to a maximum of nine sessions over a period of up to 12 weeks
- Consider offering a course of acupuncture needling comprising up to a maximum of 10 sessions over a period of up to 12 weeks.
The summary guidance still doesn’t mention chiropractic explicitly, just a coy reference to “spinal manipulation”. At a time when the British Chiropractic Association is busy trying to suppress free speech via the law courts, I guess it isn’t surprising that they don’t like to use the word.
The bias in the recommendations is perhaps not surprising because the guidance development group had a heavy representation from alternative medicine advocates, and of people with a record of what, is, in my view, excessive tolerance of mumbo-jumbo.
Royal College of General Practitioners (RCGP) played a large part in writing the guidance. That is an organisation thar has steadfastly refused to make any sort of sensible statement of policy about magic medicine. It isn’t long since I was told by a senior person at the RCGP that there was nothing odd about neuro-linguistic programming. That does not bode well.
Professor Martin Underwood, Professor of Primary Care Research Warwick Medical School, University of Warwick. Underwood chaired the guidance development group. Martin Underwood is also a GP in Coventry See also the British Osteopathic Association. Underwood was lead author of the BEAM trial (download reprint). It is well worth reading the comments on this trial too. It was a randomised trial (though not, of course, blind).
|
Our main aim was to estimate, for patients consulting their general practitioner with back pain, the effectiveness of adding the following to best care in general practice: a class based exercise programme (“back to fitness”), a package of treatment by a spinal manipulator (chiropractor, osteopath, or physiotherapist), or manipulation followed by exercise Conclusions |
In other words, none of them worked very well. The paper failed to distinguish between manipulation by physiotherapists, chiropractors and osteopaths and so missed a valuable chance to find out whether there is an advantage to employing people from alternative medicine (the very problem that this NICE guidance should have dealt with)
Steve Vogel, another member of the guidance development group, is an osteopath. Osteopathy has cast off its shady origins better than chiropractic, but it remains a largely evidence-free zone, and is still usually classified as alternative medicine.
Peter Dixon DC FCC FBCA is chairman of the General Chiropractic Council and founder of Peter Dixon Associates. They run six chiropractic clinics. The claims made by these clinics on their web site are mostly related to musculo-skeletal conditions (not, all spine-related however). But they also include
“Chiropractic is also suitable for relieving the symptoms of stress, and optimizing the way the body works is one of the best ways of enhancing health and wellbeing.”
I wonder how they could justify that claim? Then we get
A chiropractor is always willing to discuss individual conditions or answer questions in order to assess whether chiropractic may be of benefit.
Thanks for the invitation. I accepted it. After the first two phone calls, I had learned all I needed.
The first of Peter Dixon’s clinics that I called, was asked about my son who was suffeiing from perpetual colic. I asked for advice. I was put through to the chiropractor. Here are some extracts from the conversation.
“I think now it’s termed irritable baby syndrome. . . . . We’ve found chiropractic is very effective for colic . . . . £50 up to 3/4 hour which would involve taking a case history, examining the baby, with regard to seeing how the joints in the spine work because often colic is down to, er um, faulty movement patterns in the spine. We deal with an awful lot of things to do with the frame -how the spine moves -and it’s often problems with the way that the bones of the spine move in infants and babies that is the underlying cause in colicky symptoms. . . usually on the whole, I’ve shot myself in the foot by saying this in the past, if there are -um when I say back problems they’re usually temporary issues -when they are there the response for most babies is quite quick . . . it depends on how it’s related to what’s gone on in the birth process -there is usually some traumatic cause and it usually sets up a problem in the upper neck or the mid-back and that will drive those colic symptoms. . . . Yes it’s quite a straightforward thing we just check the baby’s spine and see if it’s problem we can deal with or not.”
Yes, I think you just shot yourself in the foot again. I have no idea in what fraction of cases a chiropractor would fail to claim that it was a case that they could deal with. At least that possibility was envisaged. But when I asked where he’d refer me to in such case I was told it might be a result of bottle feeding -“what they consume”. So I expect it would have been sent to some sort of “nutritional therapist” who would have used one of their usual battery of unreliable tests for food allergies.
I tried a second clinic in Peter Dixon’s empire and asked if chiropractic could help with asthma.”It can do, depending on what type of asthma you have". After some questions I was asked
“Do you have any general aches and pains otherwise, any tension .problems round the rib cage or thoracic spine . . . There are two things we’d look as chiropractors as to whether we could help or not and that would include the tension round the rib cage -in any type of asthma you’ll become tight round the rib cage and merely by keeping that area loose you’d help to stop the asthma from becoming quite as bad. And the second part is we’d look at the neck area with you to see if there is any restriction there -which houses the nerve supply to the lungs which can be indicated in some asthma cases also.”
I was invited to come for a free screen, so I asked if it usually worked quickly, “It depends what the problem is but you’d need a course I suspect”. £45 for the first appointment then £28 per session. “In most cases you’d need to look at a six to eight session course”.
Would anyone with experience of crying babies or of asthma like to comment on these proposed treatments? They are not my idea of evidence-based treatments and I find it quite surprising that someone who sponsors them is thought appropriate to write guidance for NICE.
This sort of ‘sting’ always makes me feel a bit uneasy, but it seems to be the only way to find out what actually goes on. And what goes on has all the appearance of classic bait and switch. You go in for your backache, and before you know where you are you are being sold a course of treatment to stop your baby crying.
Media follow-up after the NICE announcement
Sadly, I heard that the Today programme (my favourite news programme) was pretty wet. if only their science reporting was as good as their politics reporting.
The 27th May was certainly pretty busy for me, Apart from a couple of local paper interviews, this is what happened,
Sky News TV. Richard Suchet and two cameraman came to UCL and filmed a lot of stuff out of which a 20 second clip was used. And then they grumble that they don’t make money.
BBC TV 6 o’clock News. Similar, but at least only two people this time. Both TV stations spent ages showing pictures of people having needles pushed into them and very little time discussing the problems. A pathetically bad attempt at science reporting. Radio, on the whole, did much better
BBC Three Counties Radio (09.20) Host Ronnie Barbour, The daytime talk shows may be appalling to some of us, but the hosts did a far better job of airing the problems than TV [download the mp3].
Radio 5 Live Victoria Derbyshire [download the mp3]
BBC Radio Sheffield (12.05) was the best talk show by far. First speaker was Steve Vogel, the osteopath from the guidance development group. Although invited by the rather sensible host, Rony, to respond to the idea that a secondary consequence of the guidance would be to introduce hocus-pocus, he steadfastly refused to answer the question. At the end a rather sensible GP summed up the view from the coalface. [play the mp3]
Radio 4 PM programme This excellent early evening news programme is run by Eddie Mair. It was the best interview yet. The other side was put by Martin Underwood, chair of the guidance development group [play the mp3]
Underwood said “the evidence shows that it [acupuncture] works”. I disagree. The evidence shows that acupuncture, in a non-blind comparison with no acupuncture shows a small, variable additional effect that doesn’t last and is of marginal clinical significance, That is not what I call “works”. Underwood then indulges in the subgroup analysis fallacy by asserting that a few people get a large benefit from acupuncture. Or perhaps a few people just happen to get better that day. I was not convinced.
More 4 News TV 20.20 was an interview, with the other side being put by my old friend, George Lewith.
During the introduction, an acupuncturist. Lisa Sherman, ‘explained’ acupuncture in the usual sort of utterly meaningless words that illustrate perfectly the problem.
George Lewith said that “we don’t have a good pretend form of acupuncture”. “We don’t have a good placebo and we can demonstrate that acupuncture is literally twice as effective as conventional care”. The first is simply nonsense: huge efforts have gone into developing good controls in acupuncture studies (see, for example, Barker Bausell’s book, Snake Oil Science). And I hope that George will send the references for his “twice as effective” claim. It seems to me to be nothing short of preposterous.
My conclusions
So what went wrong?
One problem could be regarded as medical arrogance. The fact is that the problem of low back pain has not been solved, either by drugs or anything else. It is a failure of medicine (and of pharmacology). That should be the premise of all discussions, and it smacks of arrogance not to tell people straight out. Of course there are some cases when causes can be identified, and perhaps remedied, usually by surgery, but these are the exceptions not the rule.
One consequence of the inability of medicine to help much is that patients get desperate, and willing to try anything. And of course if they happen to have a remission, that is attributed to the treatment, however preposterous that treatment may have been. Conditions like back pain that come and go unpredictable are a gift for quacks.
Another consequence, for researchers rather than patients, is to clutch at straws. Even small and inconsistent effects are seized on as ‘successes’. This phenomenon seems to be part of the reason for the NICE guidance. Another reason is, almost certainly, the grinding of axes by some of the people who wrote it.
What should be done now?
Professor Sir Michael Rawlins is a sensible chap. He cares about evidence, But it does seem that in this case, he might have taken his eye off the ball, for once. In my opinion, he should restore the reputation of NICE by withdrawing this guidance and starting again.
Follow-up
An interesting document has come my way. It shows the responses of the guidance group to the consultation on the draft guidance. Many people made comments not unlike mone, but they were all brushed aside in a way that looks to me rather partisan. The document appears to have vanished from NICE’s web site, but you can download it here.
Friday 29th May. The Times prints a letter from two consultants in pain medicine, Joan Hestor and Stephen Ward. It says, inter alia
“As experienced pain specialists we feel that NICE has lost its way in publishing these guidelines.”
“We are saddened that NICE has chosen to ignore our important role and promote seemingly unworkable and for the most part clinically ineffective treatments”
Friday 29th May. NICE has had a good reputation in the USA for its important, and usually high-quality, attempts to assess what works and what doesn’t. That makes it all the sadder to see it condemned already from the USA for its latest effort. The excellent Yale neurologist, Steven Novella, has written about it on his Neurologica blog.
Friday 29th May. A correspondent points out that the costings of the guidance can be found on the NICE web site. Table 1 has a strong air of make-believe.

The Daily Mail (29 May 2009). Their article quotes serious criticisms of NICE.
Dr Ron Cooper, past chairman of the group and a consultant pain specialist in Northern Ireland, said: ‘I have never known so many pain medicine specialists to be so furious. More patients will end up having more expensive surgery, which is unnecessary, risky and has worse results.
‘NICE made it difficult for us to submit evidence to a committee on which there was not one experienced pain physician.
‘The guidelines will make us the laughing stock of Europe, Australia and the U.S. where pain specialists will continue to have full access to a wide range of treatments.’
Chirowatch suspended. 30 May 2009. The invaluable chiro-watch site, http://www.chirowatch.com, run by Dr Canadian physician, Dr Tom Polevoy, has been “suspended”. In fact the whole of his domain, healthwatcher.net, has been disabled. It seems that this was the result of a legal threat to his ISP, not by chiropractors this time, but by William O’Neill of the Canadian Cancer Research Group, which is far from being what the respectable-sounding title suggests, according to Dr Stephen Barrett. The site will be back soon, I’m told. Meanwhile you can read the suspended page here, and the only result of their hamfisted bullying will be to vastly increase the number of people who read it. You can read lots more at Quackwatch’s chirobase and at ebm-first.
A new blog, Not as NICE as you think appeared on May 30th. It is written by a pain physician, Stephen Ward. and is devoted to pointing out the serious problems raised by NICE’s guidance. It starts with the (very critical) World Institute of Pain Press Release.
British Medical Journal has more flak for the NICE guidelines
And the BMJ has published a letter signed by 50 consultants in pain medicine, NICE guidelines on low back pain are flawed.(this will probably appear as a letter in the print edition of the BMJ).
First the MHRA lets down the public by allowing deceptive labelling of sugar pills (see here, and this this blog). Now it is the turn of NICE to betray its own principles.
The National Institute for Health and Clinical Excellence (NICE) describes its job thus
“NICE is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health.”
Its Guidance document on Low Back Pain will be published on Wednesday 27 May 2009, but the newspapers have already started to comment, presumably on the assumption that it will have changed little from the Draft Guidance of September 2008. These comments may have to be changed as soon as the final version becomes available.
The draft guidance, though mostly sensible, has two recommendations that I believe to be wrong and dangerous. The recommendations include (page 7) these three.
- Consider offering a course of manual therapy including spinal manipulation of up to 9 sessions over up to 12 weeks.
- Consider offering a course of acupuncture needling comprising up to 10 sessions over a period of up to 12 weeks.
- Consider offering a structured exercise programme tailored to the individual.
All three of this options are accompanied by a footnote that reads thus.
“A choice of any of these therapies may be offered, taking into account patient preference.”
On the face if it, this might seem quite reasonable. All three choices seem to be about as effective (or ineffective) as each other, so why not let patients choose between them?
Actually there are very good reasons, but NICE does not seem to have thought about them. In the past I have had a high opinion of NICE but it seems that even they are now getting bogged down in the morass of political correctness and officialdom that is the curse of the Department of Health. It is yet another example of DC’s rule number one.
Never trust anyone who uses the word ‘stakeholder’.
They do use it, often.
So what is so wrong?
For a start, I take it that the reference to “spinal manipulation” in the first recommendation is a rather cowardly allusion to chiropractic. Why not say so, if that’s whar you mean? Chiropractic is mentioned in the rest of the report but the word doesn’t seem to occur in the recommendations. Is NICE perhaps nervous that it would reduce the credibility of the report if the word chiropractic were said out loud?
Well, they have a point, I suppose. It would.
That aside, here’s what’s wrong.
The Evidence
I take as my premise that the evidence says that no manipulative therapy has any great advantage over the others. They are all more or less equally effective. Perhaps I should say, more or less equally ineffective, because anyone who claims to have the answer to low back pain is clearly deluded (and I should know: nobody has fixed mine yet). So for effectiveness there are no good grounds to choose between exercise, physiotherapy, acupuncture or chiropractic. There is, though, an enormous cultural difference. Acupuncture and chiropractic are firmly in the realm of alternative medicine. They both invoke all sorts of new-age nonsense for which there isn’t the slightest good evidence. That may not poison your body, but it certainly poisons your mind.
Acupuncturists talk about about “Qi”, “meridians”, “energy flows”. The fact that “sham” and “real” acupuncture consistently come out indistinguishable is surely all the evidence one needs to dismiss such nonsense. Indeed there is a small group of medical acupuncturists who do dismiss it. Most don’t. As always in irrational subjects, acupuncture is riven by internecine strife between groups who differ in the extent of their mystical tendencies,
Chiropractors talk of “subluxations”, an entirely imaginary phenomenon (but a cause of much unnecessary exposure to X-rays). Many talk of quasi-religious things like “innate energy”. And Chiropractic is even more riven by competing factions than acupuncture. See, for example, Chiropractic wars Part 3: internecine conflict.
The bait and switch trick
This is the basic trick used by ‘alternative therapists’ to gain respectability.
There is a superb essay on it by the excellent Yale neurologist Steven Novella: The Bait and Switch of Unscientific Medicine. The trick is to offer some limited and reasonable treatment (like back manipulation for low back pain). This, it seems, is sufficient to satisfy NICE. But then, once you are in the showroom, you can be exposed to all sorts of other nonsense about “subluxations” or “Qi”. Still worse, you will also be exposed to the claims of many chiropractors and acupuncturists to be able to cure all manner of conditions other than back pain. But don’t even dare to suggest that manipulation of the spine is not a cure for colic or asthma or you may find yourself sued for defamation. The shameful legal action of the British Chiropractic Association against Simon Singh (follow it here) led to an addition to DC’s Patients’ Guide to Magic Medicine.
(In the face of such tragic behaviour, one has to be able to laugh).
Libel: A very expensive remedy, to be used only when you have no evidence. Appeals to alternative practitioners because truth is irrelevant.
NICE seems to have fallen for the bait and switch trick, hook line and sinker.
The neglected consequences
Once again, we see the consequences of paying insufficient attention to the Dilemmas of Alternative Medicine.
The lying dilemma
If acupuncture is recommended we will have acupuncturists telling patients about utterly imaginary things like “Qi” and “meridians”. And we will have chiropractors telling them about subluxations and innate energy. It is my opinion that these things are simply make-believe (and that is also the view of a minority of acupuncturist and chiropractors). That means that you have to decide whether the supposed benefits of the manipulation are sufficient to counterbalance the deception of patients.
Some people might think that it was worth it (though not me). What is unforgivable is not to consider even the question. The NICE guidance says not a word about this dilemma. Why not?
The training dilemma
The training dilemma is even more serious. Once some form of alternative medicine has successfully worked the Bait and Switch trick and gained a toehold in the NHS, there will be an army of box-ticking HR zombies employed to ensure that they have been properly trained in “subluxations” or “Qi”. There will be quangos set up to issue National Occupational Standards in “subluxations” or “Qi”. Skills for Health will issue “competences” in “subluxations” or “Qi” (actually they already do). There will be courses set up to teach about “subluxations” or “Qi”, some even in ‘universities’ (there already are).
The respectability problem
But worst of all, it will become possible for aupuncturists and chiropractors to claim that they now have official government endorsement from a prestigious evidence-based organisation like NICE for “subluxations” or “Qi”. Of course this isn’t true. In fact the words “subluxations” or “Qi” are not even mentioned in the draft report. That is the root of the problem. They should have been. But omitting stuff like that is how the Bait and Switch trick works.
Alternative medicine advocates crave, above all, respectability and acceptance. It is sad that NICE seems to have given them more credibility and acceptance without having considered properly the secondary consequences of doing so,
How did this failure of NICE happen?
It seems to have been a combination of political correctness, failure to consider secondary consequences, and excessive influence of the people who stand to make money from the acceptance of alternative medicine.
Take, for example, the opinion of the British Pain Society. This organisation encompasses not just doctors. It
includes “doctors, nurses, physiotherapists, scientists, psychologists, occupational therapists and other healthcare professionals actively engaged in the diagnosis and treatment of pain and in pain research for the benefit of patients”. Nevertheless, their response to the draft guidelines pointed out that the manipulative therapies as a whole were over-represented.
|
Manipulation The guidelines assess 9 large groups of interventions of which manual therapies are only one part. The full GDG members panel of 13 individuals included two proponents of spinal manipulation/mobilisation (P Dixon and S Vogel). In addition, the chair of the panel (M Underwood) is the lead author of the UKBEAM trial on which the positive recommendation for |
It seems that the Pain Society were quite right.
LBC 97.3 Breakfast Show (25 May 2009) had a quick discussion on acupuncture (play mp3 file). After I had my say, the other side was put by Rosey Grandage. She has (among other jobs) a private acupuncture practice so she is not quite as unbiassed as me). As usual, she misrepresents the evidence by failing to distinguish between blind and non-blind studies. She also misrepresented what I said by implying that I was advocating drugs. That was not my point and I did not mention drugs (they, like all treatments, have pretty limited effectiveness, and they have side effects too). She said “there is very good evidence to show they (‘Qi’ and ‘meridians’] exist”. That is simply untrue.
There can’t be a better demonstration of the consequences of falling for bait and switch than the defence mounted by Rosey Grandage. NICE may not mention “Qi” and “meridians”; but the people they want to allow into the NHS have no such compunctions.
I first came across Rosey Grandage when I discovered her contribution to the Open University/BBC course K221. That has been dealt with elsewhere. A lot more information about acupuncture has appeared since then. She doesn’t seem to have noticed it. Has she not seen the Nordic Cochrane Centre report? Nor read Barker Bausell, or Singh & Ernst? Has she any interest in evidence that might reduce her income? Probably not.
Where to find out more
An excellent review of chiropractic can be found at the Layscience site. It was written by the indefatigable ‘Blue Wode’ who has provided enormous amounts of information at the admirable ebm-first site (I am authorised to reveal that ‘Blue Wode’ is the author of that site). There you will also find much fascinating information about both acupuncture and about chiropractic.
I’m grateful to ‘Blue Wode’ for some of the references used here.
Follow-up
| The Prince of Wales’ Foundation for Integrated Health (FiH) is a propaganda organisation that aims to persuade people, and politicians, that the Prince’s somewhat bizarre views about alternative medicine should form the basis of government health policy.
His attempts are often successful, but they are regarded by many people as being clearly unconstitutional. |
 |
The FiH’s 2009 AnnualConferen ce conference was held at The King’s Fund, London 13 – 14 May 2009. It was, as always, an almost totally one-sided affair devoted to misrepresentation of evidence and the promotion of magic medicine. But according to the FiH, at least, it was a great success. The opening speech by the Quacktitioner Royal can be read here. It has already been analysed by somebody who knows rather more about medicine than HRH. He concludes
“It is a shocking perversion of the real issues driven by one man; unelected, unqualified and utterly misguided”.
We are promised some movie clips of the meeting. They might even make a nice UK equivalent of “Integrative baloney @ Yale“.
This post is intended to provide some background information about the speakers at the symposium. But let’s start with what seems to me to be the real problem. The duplicitous use of the word “integrated” to mean two quite different things.
The problem of euphemisms: spin and obfuscation
One of the problems of meetings like this is the harm done by use of euphemisms. After looking at the programme, it becomes obvious that there is a rather ingenious bit of PR trickery going on. It confuses (purposely?) the many different definitions of the word “integrative” . One definition of “Integrative medicine” is this (my emphasis).
” . . . orienting the health care process to engage patients and caregivers in the full range of physical, psychological, social, preventive, and therapeutic factors known to be effective and necessary for the achievement of optimal health.”
That is a thoroughly admirable aim. And that, I imagine, is the sense in which several of the speakers (Marmot, Chantler etc) used the term. Of course the definition is rather too vague to be very helpful in practice, but nobody would dream of objecting to it.
But another definition of the same term ‘integrative medicine’ is as a PR-friendly synonym for ‘alternative medicine’, and that is clearly the sense in which it is used by the Prince of Wales’ Foundation for Integrated Health (FIH), as is immediately obvious from their web site.
The guide to the main therapies supports everything from homeopathy to chiropractic to naturopathy, in a totally uncritical way. Integrated service refers explicitly to integration of ‘complementary’ medicine, and that itself is largely a euphemism for alternative medicine. For example, the FIH’s guide to homeopathy says
“What is homeopathy commonly used for?
Homeopathy is most often used to treat chronic conditions such as asthma; eczema; arthritis; fatigue disorders like ME; headache and migraine; menstrual and menopausal problems; irritable bowel syndrome; Crohn’s disease; allergies; repeated ear, nose, throat and chest infections or urine infections; depression and anxiety.”
But there is not a word about the evidence, and perhaps that isn’t surprising because the evidence that it works in any of these conditions is essentially zero.
The FIH document Complementary Health Care: A Guide for Patients appears to have vanished from the web after its inaccuracy received a very bad press, e.g. in the Times, and also here. It is also interesting that the equally widely criticised Smallwood report (also sponsored by the Prince of Wales) seems to have vanished too).
The programme for the meeting can be seen here, for Day 1, and Day 2
Conference chair Dr Phil Hammond, GP, comedian and health service writer. Hammond asked the FIH if I could speak at the meeting to provide a bit of balance. Guess what? They didn’t want balance.
09:30 Opening session
Dr Michael Dixon OBE
09:30 Introduction: a new direction for The Prince’s Foundation for Integrated Health and new opportunities in integrated health and care. Dr Michael Dixon, Medical Director, FIH
Michael Dixon is devoted to just about every form of alternative medicine. As well as being medical director of the Prince’s Foundation he also runs the NHS Alliance. Despite its name, the NHS Alliance is nothing to do with the NHS and acts, among other things, as an advocate of alternative medicine on the NHS, about which it has published a lot.
Dr Dixon is also a GP at College Surgery, Cullompton, Devon, where his “integrated practice” includes dozens of alternative practitioners. They include not only disproven things like homeopathy and acupuncture, but also even more bizarre practitioners in ‘Thought Field Therapy‘ and ‘Frequencies of Brilliance‘.
To take only one of these, ‘Frequencies of Brilliance’ is bizarre beyond belief. One need only quote its founder and chief salesperson.
“Frequencies of Brilliance is a unique energy healing technique that involves the activation of energetic doorways on both the front and back of the body.”
“These doorways are opened through a series of light touches. This activation introduces high-level Frequencies into the emotional and physical bodies. It works within all the cells and with the entire nervous system which activates new areas of the brain.”
“Frequencies of Brilliance is a 4th /5th dimensional work. The process is that of activating doorways by lightly touching the body or working just above the body.”
“Each doorway holds the highest aspect of the human being and is complete in itself. This means that there is a perfect potential to be accessed and activated throughout the doorways in the body.”
Best of all, it can all be done at a distance (that must help sales a lot). One is reminded of the Skills for Health “competence” in distant healing (inserted on a government web site at the behest (you guessed it) of the Prince’s Foundation, as related here)
“The intent of a long distance Frequencies of Brilliance (FOB) session is to enable a practitioner to facilitate a session in one geographical location while the client is in another.
A practitioner of FOB that has successfully completed a Stage 5 Frequency workshop has the ability to create and hold a stable energetic space in order to work with a person that is not physically present in the same room.
The space that is consciously created in the Frequencies of Brilliance work is known as the “Gap”. It is a space of nonlinear time. It contains ”no time and no space” or respectively “all time and all space”. Within this “Gap” a clear transfer of the energies takes place and is transmitted to an individual at a time and location consciously intended. Since this dimensional space is in non-linear time the work can be performed and sent backward or forward in time as well as to any location.
The Frequencies of Brilliance work cuts through the limitations of our physical existence and allows us to experience ourselves in other dimensional spaces. Therefore people living in other geographic locations than a practitioner have an opportunity to receive and experience the work.
The awareness of this dimensional space is spoken about in many indigenous traditions, meditation practices, and in the world of quantum physics. It is referred to by other names such as the void, or vacuum space, etc.”
This is, of course, preposterous gobbledygook. It, and other things in Dr Dixon’s treatment guide, seem to be very curious things to impose on patients in the 21st century.
Latest news. The Mid-Devon Star announces yet more homeopathy in Dr Dixon’s Cullompton practice. This time it comes in the form of a clinic run from the Bristol Homeopathic Hospital. I guess they must be suffering from reduced commissioning like all the other homeopathic hospitals, but Dr Dixon seems to have come to their rescue. The connection seems to be with Bristol’s homeopathic consultant, Dr Elizabeth A Thompson. On 11 December 2007 I wrote to Dr Thompson, thus
|
In March 2006, a press release http://www.ubht.nhs.uk/press/view.asp?257 announced a randomised trial for homeopathic treatment of asthma in children. This was reported also on the BBC http://news.bbc.co.uk/1/hi/england/bristol/4971050.stm . I’d be very grateful if you could let me know when results from this trial will become available. Yours sincerely David Colquhoun |
The reply, dated 11 December 2007, was unsympathetic
|
I have just submitted the funders report today and we have set ourselves the deadline to publish two inter-related papers by March 1st 2007. Can I ask why you are asking and what authority you have to gain this information. I shall expect a reply to my questions, |
I answered this question politely on the same day but nevertheless my innocent enquiry drew forth a rather vitriolic complaint from Dr Thompson to the Provost of UCL (dated 14 December 2007). In this case, the Provost came up trumps. On 14 January 2008 he replied to Thompson: “I have looked at the email that you copied to me, and I must say that it seems an entirely proper and reasonable request. It is not clear to me why Professor Colquhoun should require some special authority to make such direct enquiries”. Dr Thompson seems to be very sensitive. We have yet to see the results of her trial in which I’m still interested.
Not surprisingly, Dr Dixon has had some severe criticism for his views, not least from the UK’s foremost expert on the evidence for efficacy, Prof Edzard Ernst. Accounts of this can be found in Pulse,
and on Andrew Lewis’s blog.
Dixon is now (in)famous in the USA too. The excellent Yale neurologist, Steven Novella, has written an analysis of his views on Science Based Medicine. He describes Dr. Michael Dixon as “A Pyromaniac In a Field of (Integrative) Straw Men”
Peter Hain
09:40 Politics and people: can integrated health and care take centre stage in 2009/2010? Rt Hon Peter Hain MP
It seems that Peter Hain was converted to alternative medicine when his first baby, Sam, was born with eczema. After (though possibly not because of) homeopathic treatment and a change in diet, the eczema got better. This caused Hain, while Northern Ireland Secretary to spend £200,000 of taxpayers’ money to set up a totally uninformative customer satisfaction survey, which is being touted elsewhere in this meeting as though it were evidence (see below). I have written about this episode before: see Peter Hain and Get Well UK: pseudoscience and privatisation in Northern Ireland.
I find it very sad that a hero of my youth (for his work in the anti-apartheid movement) should have sunk to promoting junk science, and even sadder that he does so at my expense.
There has been a report on Hain’s contribution in Wales Online.
09:55 Why does the Health Service need a new perspective on health and healing? Sir Cyril Chantler, Chair, King’s Fund, previous Dean, Guy’s Hospital and Great Ormond Street
Cyril Chantler is a distinguished medical administrator. He also likes to talk and we have discussed the quackery problem several times. He kindly sent me the slides that he used. Slide 18 says that in order to do some good we “need to demonstrate that the treatment is clinically effective and cost effective for NHS use”. That’s impeccable, but throughout the rest of the slides he talks of integrating with complementary” therapies, the effectiveness of which is either already disproved or simply not known.
I remain utterly baffled by the reluctance of some quite sensible people to grasp the nettle of deciding what works. Chantler fails to grasp the nettle, as does the Department of Health. Until they do so, I don’t see how they can be taken seriously.
10.05 Panel discussion
The Awards
10:20 Integrated Health Awards 2009 Introduction: a review of the short-listed applications
10:45 Presentations to the Award winners by the special guest speaker
11:00 Keynote address by special guest speaker
Getting integrated
Dr David Peters
12:00 Integration, long term disease and creating a sustainable NHS. Professor David Peters, Clinical Director and Professor of Integrated Healthcare, University of Westminster
I first met David Peters after Nature ran my article, Science Degrees without the Science. .One of the many media follow-ups of that article was on Material World (BBC Radio 4). This excellent science programme, presented by Quentin Cooper, had a discussion between me and David Peters ( listen to the mp3 file).
There was helpful intervention from Michael Marmot who had talked, in the first half of the programme, about his longitudinal population studies.
Marmot stressed the need for proper testing. In the case of
homeopathy and acupuncture, that proper testing has largely been done. The tests were failed.
The University of Westminster has, of course, gained considerable notoriety as the university that runs more degree programmes in anti-scientific forms of medicine than any other. Their lecture on vibrational medicine teaches students that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbances at all levels of being”. So far their vice-chancellor, Professor Geoffrey Petts, has declined to answer enquiries about whether he thinks such gobbledygook is appropriate for a BSc degree.
But he did set up an internal enquiry into the future of their alternative activities. Sadly that enquiry seems to have come to the nonsensical conclusion that the problem can be solved by injection of good science into the courses, as reported here and in the Guardian.
It seems obvious that if you inject good science into their BSc in homeopathy the subject will simply vanish in a puff of smoke.
In 2007, the University of Westminster did respond to earlier criticism in Times Higher Education, but their response seemed to me to serve only to dig themselves deeper into a hole.
Nevertheless, Westminster has now closed down its homeopathy degree (the last in the country to go) and there is intense internal discussion going on there. I have the impression that Dr Peters’ job is in danger. The revelation of more slides from their courses on homeopathy, naturopathy and Chinese herbal medicine shows that these courses are not only barmy, but also sometimes dangerous.
Professor Chris Fowler
12:10 Educating tomorrow’s integrated doctors. Professor Chris Fowler, Dean for Education, Barts and The London School of Medicine and Dentistry
I first came across Dr Fowler when I noticed him being praised for his teaching of alternative medicine to students at Barts and the London Medical School on the web site of the Prince’s Foundation. I wrote him a polite letter to ask if he really thought that the Prince of Wales was the right person to consult about the education of medical students. The response I got was, ahem, unsympathetic. But a little while later I noticed that two different Barts students had set up public blogs that criticised strongly the nonsense that was being inflicted on them.
At that point, I felt it was necessary to support the students who, it seemed to me, knew more about medical education than Professor Fowler. It didn’t take long to uncover the nonsense that was being inflicted on the students: read about it here.
There is a follow-up to this story here. Fortunately, Barts’ Director of Research, and, I’m told, the Warden of Barts, appear to agree with my view of the harm that this sort of thing can do to the reputation of Barts, so things may change soon,
Dame Donna Kinnair
12:30 Educating tomorrow’s integrated nurses.
Dame Donna Kinnair, Director of Nursing, Southwark PCT
As far as I can see, Donna Kinnair has no interest in alternative medicine. She is director of nursing at Southwark primary care trust and was an adviser to Lord Laming throughout his inquiry into the death of Victoria Climbié. I suspect that her interest is in integrating child care services (they need it, judging by the recent death of ‘Baby P’). Perhaps her presence shows the danger of using euphemisms like ‘integrated medicine’ when what you really mean is the introduction of unproven or disproved forms of medicine.
Michael Dooley
12:40 Integrating the care of women: an example of the new paradigm. Michael Dooley, Consultant Obstetrician and Gynecologist
DC’s rule 2. Never trust anyone who uses the word ‘paradigm’. It is a sure-fire sign of pseudoscience. In this case, the ‘new paradigm’ seems to be the introduction of disproven treatment. Dooley is a gynaecologist and Medical Director of the Poundbury Clinic. His clinic offers a whole range of unproven and disproved treatments. These include acupuncture as an aid to conception in IVF. This is not recommended by the Cochrane review, and one report suggests that it hinders conception rather than helps.
12.40 Discussion
13.00 – 14.00 Lunch and Exhibition
15.30 Tea
Boo Armstrong and Get Well UK
16.00 Integrated services in action: The Northern
Ireland experience: what has it shown us and what are its implications?
Boo Armstrong of Get Well UK with a team from the NI study
I expect that much will be made of this “study”, which, of course, tells you absolutely nothing whatsoever about the effectiveness of the alternative treatments that were used in it. This does not appear to be the view of Boo Armstrong, On the basis of the “study”, her company’s web site proclaims boldly
“Complementary Medicine Works
Get Well UK ran the first government-backed complementary therapy project in the UK, from February 2007 to February 2008″
This claim appears, prima facie, to breach the Unfair Trading Regulations of May 2008. The legality of the claim is, at the moment, being judged by a Trading Standards Officer. In any case, the “study” was not backed by the government as a whole, but just by Peter Hain’s office. It is not even clear that it had ethical approval.
The study consisted merely of asking people who had seen an alternative medicine practitioner whether they felt better or worse. There was no control group; no sort of comparison was made. It is surely obvious to the most naive person that a study like this cannot even tell you if the treatment has a placebo effect, never mind that it has any genuine effects of its own. To claim that it does so seems to be simply dishonest. There is no reason at all to think that the patients would not have got better anyway.
It is not only Get Well UK who misrepresent the evidence. The Prince’s
Foundation itself says
“Now a new, year long trial supported by the Northern Ireland health service has . . . demonstrated that integrating complementary and conventional medicine brings measurable benefits to patients’ health.”
That is simply not true. It is either dishonest or stupid. Don’t ask me which, I have no idea.
This study is no more informative than the infamous Spence (2005) ‘study’ of the same type, which seems to be the only thing that homeopaths can produce to support their case.
There is an excellent analysis of the Northern Ireland ‘study’ by Andy Lewis, The Northern Ireland NHS Alternative Medicine ‘Trial’. He explains patiently, yet again, what constitutes evidence and why studies like this are useless.
His analogy starts
” . . . the Apple Marketing Board approach the NHS and ask for £200,000 to do a study to show the truth behind the statement ‘An apple a day keeps the doctor away’. The Minister, being particularly fond of apples, agrees and the study begins.”
16.30 Social enterprise and whole systems integrated care. Dee Kyne, Sandwell PCT and a GP. Developing an integrated service in secondary care
Dee Kyne appears to be CEO of KeepmWell Ltd (a financial interest that is not mentioned).
Peter Mackereth, Clinical Lead, Supportive Services, Christie Hospital NHS Foundation Trust
I had some correspondence with Mackereth when the Times (7 Feb 2007) published a picture of the Prince of Wales inspecting an “anti-MRSA aromatherapy inhaler” in his department at the Christie. It turned out that the trial they were doing was not blind No result has been announced anyway, and on enquiry, I find that the trial has not even started yet. Surprising, then to find that the FIH is running the First Clinical Aromatherapy Conference at the Christie Hospital, What will there be to talk about?
Much of what they do at the Christie is straightforward massage, but they also promote the nonsensical principles of “reflexology” and acupuncture.
The former is untested. The latter is disproven.
Parallel Sessions
Developing a PCT funded musculoskeletal service Dr Roy Welford, Glastonbury Health Centre
Roy Welford is a Fellow of the Faculty of Homeopathy, and so promotes disproven therapies. The Glastonbury practice also advertises acupuncture (disproven), osteopathy and herbal medicine (largely untested so most of it consists of giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety).
Making the best of herbal self-prescription in integrated practice: key remedies and principles. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon
Simon Mills is a herbalist who now describes himself as a “phytotherapist” (it sounds posher, but the evidence, or lack of it, is not changed by the fancy name). Mills likes to say things like “there are herbs for heating and drying”, “hot and cold” remedies, and to use meaningless terms like “blood cleanser”, but he appears to be immune to the need for good evidence that herbs work before you give them to sick people. He says, at the end of a talk, “The hot and the cold remain the trade secret of traditional medicine”. And this is the 21st Century.
Practical ways in which complementary approaches can improve the treatment of cancer. Professor Jane Plant, Author of “Your life in your hands” and Chief Scientist, British Geological Society and Professor Karol Sikora, Medical Director, Cancer Partners UK
Jane Plant is a geologist who, through her own unfortunate encounter with breast cancer, became obsessed with the idea that a dairy-free diet cured her. Sadly there is no good evidence for that idea, according to the World Cancer Research Fund Report, led by Professor Sir Michael Marmot. No doubt her book on the subject sells well, but it could be held that it is irresponsible to hold out false hopes to desperate people. She is a supporter of the very dubious CancerActive organisation (also supported by Michael Dixon OBE –see above) as well as the notorious pill salesman, Patrick Holford (see also here).
Karol Sikora, formerly an oncologist at the Hammersmith Hospital, is now Dean of Medicine at the University of Buckingham (the UK’s only private university). He is also medical director at CancerPartners UK, a private cancer company.
He recently shot to fame when he appeared in a commercial in the USA sponsored by “Conservatives for Patients’ Rights”, to pour scorn on the NHS, and to act as an advocate for the USA’s present health system. A very curious performance. Very curious indeed.
His attitude to quackery is a mystery wrapped in an enigma. One was somewhat alarmed to see him sponsoring a course at what was, at first, called the British College of Integrated Medicine, and has now been renamed the Faculty of Integrated Medicine That grand title makes it sound like part of a university. It isn’t.

The alarm was as result of the alliance with Dr Rosy Daniel (who promotes an untested herbal conconction, Carctol, for ‘healing’ cancer) and Dr Mark Atkinson (a supplement salesman who has also promoted the Qlink pendant. The Qlink pendant is a simple and obvious fraud designed to exploit paranoia about WiFi killing you.
The first list of speakers on the proposed diploma in Integrated Medicine was an unholy alliance of outright quacks and commercial interests. It turned out that, although Karol Sikora is sponsoring the course, he knew nothing about the speakers. I did and when I pointed this out to Terence Kealey, vice-chancellor of Buckingham, he immediately removed Rosy Daniel from directing the Diploma. At the moment the course is being revamped entirely by Andrew Miles. There is hope that he’ll do a better job. It has not yet been validated by the University of Buckingham. Watch this space for developments.
Stop press It is reported in the Guardian that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear. More developments in the follow-up.
The role of happy chickens in healing: farms as producers of health as well as food – the Care Farm Initiative Jonathan Dover, Project Manager, Care Farming, West Midlands.
“Care farming is a partnership between farmers, participants and health & social care providers. It combines the care of the land with the care of people, reconnecting people with nature and their communities.”
Sounds lovely, I wonder how well it works?
What can the Brits learn from the Yanks when it comes to integrated health? Jack Lord, Chief Executive Humana Europe
It is worth noticing that the advisory board of Humana Europe includes Micheal Dixon OBE, a well known advocate of alternative medicine (see
above). Humana Europe is a private company, a wholly owned subsidiary of Humana Inc., a health benefits company with 11 million members and 22,000 employees and headquarters in Louisville, Kentucky. In 2005 it entered into a business partnership with Virgin Group. Humana was mentioned in the BBC Panorama programme “NHS for Sale”. The company later asked that it be pointed out that they provide commissioning services, not clinical services [Ed. well not yet anyway].
Humana’s document “Humana uses computer games to help people lead healthier lives” is decidedly bizarre. Hang on, it was only a moment ago that we were being told that computer games rewired your brain.
Day 2 Integrated health in action
09.00 Health, epidemics and the search for new solutions. Sir Michael Marmot, Professor of Epidemiology and Public Health, Royal Free and University College Medical School
It is a mystery to me that a distinguished epidemiologist should be willing to keep such dubious company. Sadly I don’t know what he said, but judging my his publications and his appearence on Natural World, I can’t imagine he’d have much time for homeopaths.
9.25 Improving health in the workplace. Dame Carol Black, National Director, Health and Work, Department of Health
This is not the first time that Dame Carol has been comtroversial.
9.45 Integrated health in focus: defeating obesity. Professor Chris Drinkwater, President, NHS Alliance.
The NHS Alliance was mentioned above. Enough said.
10.00 Integrated healthcare in focus: new approaches to managing asthma, eczema and allergy. Professor Stephen Holgate, Professor of Immunopharmacology, University of Southampton
10.15 Using the natural environment to increase activity. The Natural England Project: the results from year one. Dr William Bird and Ruth Tucker, Natural England.
10.30 Panel discussion
10.45 Coffee
Self help in action
11.10 Your health, your way: supporting self care through care planning and the use of personal budgets. Angela Hawley, Self Care Lead, Department of Health
11.25 NHS Life Check: providing the signposts to
integrated health. Roy Lambley, Project Director, NHS LifeCheck Programme
This programme was developed with the University of Westminster’s “Health and Well-being Network”. This group, with one exception, is separate from Westminster’s extensive alternative medicine branch (it’s mostly psychologists).
11.45 The agony and the ecstasy of helping patients to help themselves: tips for clinicians, practices and PCTs. Professor
Ruth Chambers, FIH Foundation Fellow.
11.55 Providing self help in practice: Department of Health Integrated Self Help Information Project. Simon Mills, Project Lead: Integrated Self Care in Family Practice, Culm Valley Integrated Centre for Health, Devon and Dr Sam Everington, GP, Bromley by Bow.
The Culm Valley Integrated Centre for health is part of the College Surgery Partnership, associated with Michael Dixon OBE (yes, again!).
Simon Mills is the herbalist who says “The hot and the cold remain the trade secret of traditional medicine” .
Sam Everington, in contrast, seems to be interested in ‘integration’ in the real sense of the word, rather than quackery.
Integrated health in action
How to make sense of the evidence on complementary approaches: what works? What might work? What doesn’t work?
Dr Hugh MacPherson, Senior Research Fellow in Health Sciences, York University and Dr Catherine Zollman, Bravewell Fellow
Hugh MacPherson‘s main interest is in acupuncture and he publishes in alternative medicine journals. Since the recent analysis in the BMJ from the Nordic Cochrane Centre (Madsen et al., 2009) it seems that acupuncture is finally dead. Even its placebo effect is too small to be useful. Catherine Zollman is a Bristol GP who is into homeopathy as well as acupuncture. She is closely connected with the Prince’s Foundation via the Bravewell Fellowship. That fellowship is funded by the Bravewell Collaboration, which is run by Christie Mack, wife of John Mack (‘Mack the Knife’), head of Morgan Stanley (amazingly, they still seem to have money). This is the group which, by sheer wealth, has persuaded so many otherwise respectable US universities to embrace every sort of quackery (see, for example, Integrative baloney @ Yale)
The funding of integrated services
14.15 How to get a PCT or practice- based commissioner to fund your integrated service. A PCT Chief Executive and a Practice-Based Commissioning lead.
14.30 How I succeeded: funding an integrated service. Dr John Ribchester, Whitstable
14.45 How we created an acupuncture service in St Albans and Harpenden PBC group. Mo Girach, Chief Executive, STAHCOM
Uhuh Acupunture again. Have these people never read Bausell’s
book? Have they not read the BMJ? Acupuncture is now ell-established to be based on fraudulent principles, and not even to have a worthwhile placeobo effect. STAHCOM seem to be more interested in money than in what works.
Dragon’s Den. Four pitchers lay out their stall for the commissioning dragons
And at this stage there is no prize for guessing that all four are devoted to trying to get funds for discredited treatments
- An acupuncture service for long-term pain. Mike Cummings Chair, Medical Acupuncture Association
- Manipulation for the treatment of back pain Simon Fielding, Founder Chairman of the General Osteopathic Council
- Nigel Clarke, Senior Partner, Learned Lion Partners Homeopathy for long term conditions
- Peter Fisher, Director, Royal Homeopathic Hospital
Sadly it is not stated who the dragons are. One hopes they will be more interested in evidence than the supplicants.
Mike Cummings at least doesn’t believe the nonsense about meridians and Qi. It’s a pity he doesn’t look at the real evidence though.
You can read something about him and his journal at BMJ Group promotes acupuncture: pure greed.
Osteopathy sounds a bit more respectable than the others, but in fact it has never shaken off its cult-like origins. Still many osteopaths make absurd claims to cure all sorts of diseases. Offshoots of osteopathy like ‘cranial osteopathy’ are obvious nonsense. There is no reason to think that osteopathy is any better than any other manipulative therapy and it is clear that all manipulative therapies should be grouped into one.
Osteopathy and chiropractic provide the best ever examples of the folly of giving official government recognition to a branch of alternative medicine before the evidence is in.
Learned Lion Partners is a new one on me. It seems it is
part of Madsen Gornall Ashe Chambers (‘MGA Chambers’) “a grouping of top level, independent specialists who provide a broad range of management consultancy advice to the marketing community”. It’s a management consultant and marketing outfit. So don’t expect too much when it comes to truth and evidence. The company web site says nothing about alternative medicine, but only that Nigel Clarke
“. . . has very wide experience of public affairs issues and campaigns, having worked with clients in many sectors in Europe, North America and the Far East. He has particular expertise in financial, competition and healthcare issues. “
However, all is revealed when we see that he is a Trustee of the Prince’s Foundation where his entry says
“Nigel Clarke is senior partner of Learned Lion Partners. He is a director of Vidapulse Ltd, Really Easy Ltd, Newscounter Ltd and Advanced Transport Systems Ltd. He has worked on the interfaces of public policy for 25 years. He has been chair of the General Osteopathic Council since May 2001, having been a lay member since it was formed. He is now a member of the Council for Healthcare Regulatory Excellence”
The Council for Healthcare Regulatory Excellence is yet another quango that ticks boxes and fails absolutely to grasp the one important point, does it work?. I came across them at the Westminster Forum, and they seemed a pretty pathetic way to spend £2m per year.
Peter Fisher is the last supplicant to the Dragons. He is clinical director of the Royal London Homeopathic Hospital (RLHH), and Queen’s homeopathic physician, It was through him that I got an active interest in quackery. The TV programme QED asked me to check the statistics in a paper of his that claimed that homeopathy was good for fibrositis (there was an elementary mistake and no evidence for an effect). Peter Fisher is also remarkable because he agreed with me that BSc degrees in homeopathy were not justified (on TV –see the movie). And he condemned homeopaths who were caught out recommending their sugar pills for malaria. To that extent Fisher represents the saner end of the homeopathic spectrum. Nevertheless he still maintains that sugar pills work and have effects of their own, and tries to justify the ‘memory of water’ by making analogies with a memory stick or CD. This is so obviously silly that no more comment is needed.
Given Fisher’s sensible condemnation of the malaria fiasco, I was rather surprised to see that he appeared on the programme of a conference at the University of Middlesex, talking about “A Strategy To Research The Potential Of Homeopathy In Pandemic Flu”. The title of the conference was Developing Research Strategies in CAM. A colleague, after seeing the programme, thought it was more like “a right tossers’ ball”.
Much of the homeopathy has now vanished from the RLHH as a result of greatly reduced commissioning by PCTs (read about it in Fisher’s own words). And the last homeopathy degree in the UK has closed down. It seems an odd moment for the FIH to be pushing it so hard.
Follow-up
Stop press It is reported in the Guardian (22 May 2009) that Professor Sikora has been describing his previous job at Imperial College with less than perfect accuracy. Oh dear, oh dear.
This fascinating fact seems to have been unearthed first by the admirable NHS Blog Doctor, in his post ‘Imperial College confirm that Karol Sikora does not work for them and does not speak on their behalf‘.
|
It seems that bits of good news don’t come singly. First honours degrees in acupuncture vanish, Now a big chain of shops selling Chinese herbs and acupuncture has gone into administration. It seems that, at last, people are getting fed up with being conned out of their hard-earned money |
 Herbmedic Barking |
A local newspaper, The North Herts Comet reported thus.
Customers of Herbmedic, which trades under the name Herbs and Acupuncture, on Queensway in Stevenage have been left counting the cost after shelling out hundreds of pounds for treatment they never received.
The company, which has practices across the country, is now in the hands of receivers, Macintyre Hudson.
Sandra Emery, of The Paddocks in Stevenage, paid £350 for 10 treatment sessions, but only received one before the practice closed.
She said: “A standard course of treatment is 10 sessions, so most customers will have bought this package.
Claudia Gois, of Walden End in Stevenage, paid £240 for 12 treatment sessions but only received four before the practice closed.
She said: “I went there on Friday and it was closed. There was no warning or anything.
“I got in touch with head office and they said it’s very unlikely I will get money back.
This report was on 1st April, The company’s web site shows no sign of any problems, In fact they are still advertising jobs. So was this an April Fool joke?
No it wasn’t. A visit to Companies House soon settled the matter. The whole company is insolvent, as of 27 March 2009..
Download the whole administration notice and the company report.
Criticisms of Herbmedic
This chain of shops was investigated by the BBC’s
Inside Out programme. (September 25th 2006).
“We sent an undercover reporter to branches of the Herbmedic chain in southern England.
On each occasion, the reporter claimed to be suffering from tiredness and was prescribed herbal remedies after a consultation lasting less than five minutes.
The herbalists, who describe themselves as “doctors”, didn’t ask any questions about the patient’s medical history or take any notes.”
This is so bad that even Andrew Fowler, a past President of the Register of Chinese Herbal Medicine, described it as “malpractice”.
“Herbmedic has been investigated by the authorities in the past.
In 2002, trading standards officers prosecuted the branch in Southampton for selling herbal remedies with 26 times the permitted legal limit of lead.
And in October 2003, the Advertising Standards Authority banned Herbmedic from describing its practitioners as “doctors”.
Despite the ban, all three of the stores visited by Inside Out referred to the herbalist as the doctor.”
See also the BBC report Herbalists’ customers ‘at risk’, and a report in the Sunday Times, Herbmedic accused of high-pressure selling.
Read the Advertising Standards report. Seven different complaints against Herbmedic were upheld.
This is entirely consistent with my own experience. I went into one of their shops and asked about a cure for diabetes (hoping the be able to refer them to Trading Standards, but the young lady behind the counter had such a poor grasp of English that her reply was incomprehensible. She just kept trying to push me into having a consultation with “the doctor” who appeared to speak no English at all. I left.
The chequered history of Herbmedic
The company that his just gone into administration is Herbmedic Centre Ltd. It has been in existence for only two years. Its predecessor, known simply as Herbmedic, was dissolved on 13 March 2007, Companies House said
Company Filing History Type Date Description Order GAZ2(A) 13/03/2007 FINAL GAZETTE: DISSOLVED VIA VOLUNTARY STRIKE-OFF GAZ1(A) 28/11/2006 FIRST GAZETTE NOTICE FOR VOLUNTARY STRIKE-OFF 652a 16/10/2006 APPLICATION FOR STRIKING-OFF
Another Chinese medicine chain seems to be having a few problems too
Harmony Medical Distribution Ltd (“specialists in acupuncture and holistic medicine”) seems to be still in business(web site here), but several very similar companies have been dissolved, Harmomy Medics Ltd (dissolved 19 Sep 2006) ,, Harmony Medical Services (UK ) Ltd. (dissolved 6 May 2008) and Harmony Medical Services Ltd (dissolved 17 Oct 2008)
Given this history of companies that dissolve every couple of years and then mysteriously reincarnate with a slightly different name, one wonders if this really is the end of herbmedic, or it is just a device for shedding bad debts. Is this just another “pre-pack administration“?
Watch this space for more.
What’s the latest evidence on acupuncture anyway?
A correspondent drew my attention to the 2009 Annual Evidence Update on acupuncture complied by the NHS Complementary and Alternative Medicine Specialist Library. This includes no fewer than 56 systematic reviews and meta-analyses. Although the reviews are complied by alternative medicine sympathisers, they seem mostly to be pretty fair. Well apart form one thing.
Almost all of the reviews fail to come up with any positive evidence that acupuncture works well enough to be clinically useful. Only two come close, and they are the two singled out as “editor’s picks”. Perhaps that’s not entirely surprising given that the editor is Dr Mike Cummings.
Again and again, the results are inconclusive: #8 is pretty typical
Acupuncture for tension-type headache: a meta-analysis of randomized, controlled trials.
This meta-analysis suggests that acupuncture compared with sham for tension-type headache has limited efficacy for the reduction of headache frequency. There exists a lack of standardization of acupuncture point selection and treatment course among randomized, controlled trials. More research is needed to investigate the treatment of specific tension-type headache subtypes.
Vast effort and a lot of money is being put into trials, yet there are very few (if any) positive results. Very often there are no results at whatsoever. All we hear, again and again, is “more research is needed”.
At some point someone will have to decide it is all a charade and start to spend time and money on investigating things that are more promising.
Follow-up
A correspondent checked with Companies House to discover more about two of the directors of Herbmedic, Mr. Li Mao and Mr Xiao Xuan Chen. They have a chequered history indeed. [download the complete list]
Mr. Li Mao is, or has been, on the board of 31 different companies. Of these 6 are active, 5 are in administration, 14 were dissolved, 4 were liquidated and 2 are active with proposal to strike off. Not only is Her Medic centre Ltd in administration, but so is Dr China (UK) Ltd, and Great Chinese Herbal Medicine Ltd
With record like that, my correspondent wonders whether they should be disqualified.
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
Acupuncture in the BMJ
A new review appeared in the BMJ today. It is by Madsen et al., from the Nordic Cochrane Centre, Copenhagen. Here are the conclusions.
- The analgesic effect of acupuncture is small and cannot be distinguished from bias resulting from incomplete blinding.
- The analgesic effect of placebo acupuncture is moderate but very variable as some large trials report substantial effects.
- The effect of acupuncture seems to be unrelated to the type of placebo acupuncture used as control.
The results confirm, yet again, that there is essentially no difference between “real” acupuncture and sham acupuncture. All that talk about meridians and Qi really is so much mumbo jumbo.
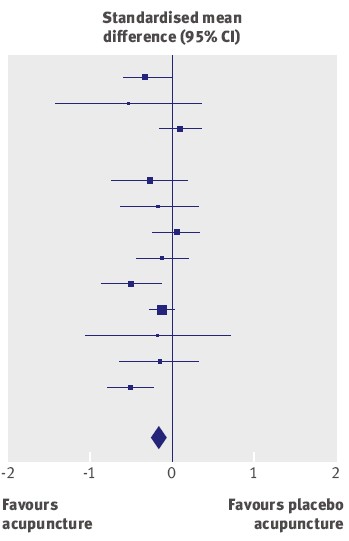
The average effect (the diamond at the bottom) is essentially zero.
It has often been supposed that acupuncture is a theatrical placebo, but because of the placebo effect it produces more pain relief than (non-blind) controls. This study confirms that there is likely to be such an effect, but it also finds that the size of the placebo effect is too small to be useful to patients. Here is the comparison between sham acupuncture and no acupuncture at all.
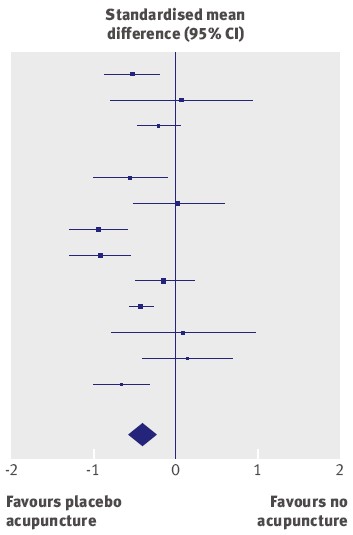
The results of different trials are very variable, but the average effect (diamond at the bottom) favours sham acupuncture over no acupuncture at all.
But how big is the effect? The numbers along the bottom of the graph are ‘standardised mean differences’. The average value of -0.42 (95% confidence limits -0.6 to -0.23) between ‘no acupuncture’ and ‘sham acupuncture’ corresponds to a difference of about 10 points on a 100 point scale. This difference is big enough to be real, in the sense that it isn’t just chance. But is it big enough to be useful to the patient? Probably not. Madsen et al conclude
“a consensus report characterised a 10mm reduction on a 100 mm visual analogue scale as representing a “minimal” change or “little change”. Thus, the apparent analgesic effect of acupuncture seems to be below a clinically relevant pain improvement.”
This makes nonsense of the Pittilo report. Notice that these results, yet again, make nonsense of the proposals in the gamma-minus Pittilo report, to pseudo-regulate acupuncture, and to have degrees in the subject.
Cochrane reviews of Acupuncture : and a bad report from BBC
Two new Cochrane reviews appeared last week, Acupuncture for tension-type headache, and Acupuncture for migraine prophylaxis.
You can’t blame subeditors for the appalling title of the BBC’s report on Acupuncture ‘works for headaches’. The content is pretty misleading too. (The link is to a version saved at 19.35 on 21 January 2009.). Furthermore, like far too many of the BBC reports, it is anonymous. One has no idea to blame This is important, if only because the BBC news site is so influential. Twelve hours after posting the misleading title has been copied all round the world.
In the Guardian, Ian Sample had a much better report, Even’fake’ acupuncture reduces the severity of headaches and migraines. Sadly the print edition had the title “Acupuncture aids migraines, researchers
find”, but that can be blamed on subeditors who have a problem with reading (in fact Sample had seen neither title).
The BBC report seemed to call for a complaint. This is what I sent.
| I wish to complain about the report on acupuncture at http://news.bbc.co.uk/1/hi/health/7838231.stm
The title itself was highly misleading “Acupuncture works for headaches” is precisely the opposite of what was shown, namely that it is no better than sham acupuncture controls. The article goes on to say
It is not said that there isn’t the slightest reason to think this is true (or even means anything) , and that the work which is being reported is strong evidence that it’s not true
That is wrong. University of Salford , for example has just closed its acupuncture course after a number of us have pointed out that it is teaching things that aren’t true
It is exactly the opposite of an endorsement. It is one more nail in the coffin of acupuncture as generally understood. This article, I contend, is partial and misleading. Unfortunately it is anonymous. |
Follow-up
Today’s BBC report on the BMJ paper is almost as partisan as the one that I just complained about. “Confusion on acupuncture benefit ” exaggerates greatly the amount of confusion. Worse still, it quotes only two well-known advocates of acupuncture, people who make their living from it. No independent scientific voice is to be heard.
One of those cited is Adrian White. He is described as “a researcher into acupuncture at the Peninsula Medical School”. There is no mention of the fact that he is also Editor in Chief of the journal Acupuncture in Medicine. The other person who is quoted is Mike O’Farrell, the chief executive of the British Acupuncture Council. What do you expect him to say?
I’ve just sent another complaint, about today’s BBC report. The more the merrier.
The BMJ itself published an editorial on the Madsen paper. It seems very odd that they should have chosen the editors of the BMJ-group journal, Acupuncture in Medicine, to comment on a paper that sounds the death knell for the subject from which they make their living. Needless to say, the editorial attempted to wriggle out of the obvious conclusions. Worse still, the Health editor of the BBC web site referred to the editorial in his defence, in response to my complaint.
Channel 4 News does a lot better than the BBC, or the BMJ editorial, with its report Acupuncture ‘fails to relieve pain’
“Claims that acupuncture can relieve pain have been undermined by the results of a new study.”
“senior researcher Asbjorn Hrobjartsson said: “Our findings question both the traditional foundation of acupuncture…and the prevailing theory that acupuncture has an important effect on pain in general”. “
The Daily Telegraph also, like almost everyone else, did better than the BBC, with “Acupuncture ‘has almost no effect in relieving pain’”
“The pain relieving effects of acupuncture are so small that they may be clinically irrelevant, according to a review of research into the treatment.”
Even Metro, the free London Newspaper, is more accurate then the BBC. They carry a short report “Acupuncture ‘has no medical point’.”
“The pain-relieving effects of acupuncture compared with a placebo are so small they may be clinically irrelevant.”
New review puts in doubt traditional foundation of acupuncture. Believe it or not, that is the title of the report on Madsen et al from the Prince’s Foundation for Integretad Health! Don’t get too excited though. They haven’t even bothered to look at the original paper, but merely cite the dreadful BBC report. Much prominence is given to the acupuncturists, White and O’Farrell, and the important finding isn’t mentioned at all. Another gamma minus.
Congratulations to the vice-chancellor of the University of Salford, Michael Harloe.
Times Higher Education announced on 15th January 2009 Salford to shut complementary medicine BSc.
“The University of Salford is to stop offering undergraduate degrees in acupuncture and complementary medicine because they are no longer considered “a sound academic fit”.”
This is the first time that a University has decided to stop teaching quackery altogether. The university’s press officer told me (22 January 2009)
| “all the University’s programmes associated with complementary medicine within the School of Community, Health Sciences & Social Care will be run out. This includes the Homeopathy in Practice programme. “ |
| Salford, before it became a university, was home to the great L.S. Lowry |

Salford’s Peel building, where L.S.Lowry worked |
“Managers concluded last year that the BSc traditional Chinese medicine and other degrees with a complementary medicine element “cannot really be held to be a good fit with the strategic direction of the school, and resource and energy would be better directed elsewhere”.
There are more than 70 students registered on the Chinese medicine degree course.
The university will continue to offer these subjects at postgraduate level, as short courses and as part of continuing professional development programmes. Traditional Chinese medicine work will also be linked to the university’s allied
health professions courses.”
Another report appeared in the Manchester Evening News: “Needle over acupuncture course”. “A UNIVERSITY has scrapped a course in acupuncture and aromatherapy branded `anti-science’ by critics.
Salford University said the three-year degree in traditional Chinese medicine didn’t fit with the `strategic direction’ bosses want to adopt.
The move is part of wider cuts which will see 150 teaching and support staff jobs axed.”
One of their students raised the question that the university must dread.
“First-year student Gary Leese, who is organising a petition, said: “Why did the university launch the course if they didn’t think it was good enough?”
The comments left by the readers of the Manchester Evening News were mostly very sensible. The first to come in, from someone with the beautifully Lancastrian name, Gladys Rowbotham, said “Some common sense at last!”.
A brief report appeared also in the Manchester Confidential
Why now?
This is rather an interesting development. On 19th April 2007, I sent a Freedom of Information request to Salford to ask for course validation documents for their courses in Homeopathy and in Traditional Chinese Medicine. I also asked for course materials for specified courses. This request was even less successful than usual. Not only were the course materials refused (as they always are), but, unusually, the validation documents were refused too. The excuse for this was more pathetic than usual too. They claimed it would cost more than £450 to email a few documents and powerpoints, and claimed exemption under Section 21 of the Freedom of Information Act, “Information Reasonably Accessible to the Applicant by Other Means”, rather than the more usual excuse (Section 43, “Commercial interests”).
It was never explained what “other means” were meant to be available. Perhaps they thought I should pay £3000 in fees and enrol for the course?
On 6th April 2007, Times Higher Education (THE) ran an opinion piece “Credible endeavour or pseudoscience?“. In this, I wrote, as follows.
“Clearly the buck stops with university vice-chancellors who award the degrees. Two weeks ago, after the publication of my opinion article and a special report on university homoeopathy courses in the journal Nature , the BBC tried to get one of the vice-chancellors to defend themselves. They did not succeed. Letters to vice-chancellors on this go unanswered. Requests to see course materials have repeatedly been refused. The QAA is exempt from the Freedom of Information Act. Teaching materials and the names of examiners are kept secret. This I find incomprehensible and indefensible.”
After this appeared, I was sent by the University of Salford a copy of Michael Harloe’s defence of their position at that time, as sent to THE. It relied heavily on validation by the Quality Assurance Agency. But the QAA is merely a box-ticking organisation that would give top marks to a course in astrology, given a sufficient mound of paperwork, as I pointed out in Nature, “Their own rules prevent them from doing anything useful”.
The statement also said that the courses teach critical thinking about alternative medicine. But it has been pointed out over and over again that what alternative medicine advocates lack, above anything else, is any faculty of critical self-appraisal.
One has to have some sympathy with a vice chancellor who is put on the spot and forced to defend courses in which he probably does not really believe himself. Perhaps it is not surprising that letters so often go unanswered. What can they say? There really is no answer that doesn’t leave the hapless VC with egg on his face.
If there is one lesson from this, it is not to be discouraged if you get no answer from a vice-chancellor. It has probably been read and may well get acted on eventually. Shutting down a course is no easy matter. It takes time.
I said the buck stops with the vice chancellor. Professor Harloe has grasped the nettle and done the right thing. Let’s hope a few more now follow his excellent lead..
What does this mean for the Pittilo report?
The gamma-minus Pittilo report (see also. The Times) recommended more degrees in alternative medicine, but there seems to be something of a trend developing in exactly the opposite direction.
The University of Central Lancashire has closed the first year entry to its “BSc” in Homeopathy, and announced a review of all its activities in the area of alternative medicine. Now we have Salford. There are stirrings among the good scientists even at the University of Westminster which has a new Dean and VC.
This rather absurd situation has arisen because of the adamant refusal of the government, and of a dozen or more quangos, to grasp the nettle of whether or not the alternative treatments work. Time and time again, the one important question that you want to know about any sort of treatment, namely, is it effective, has been pushed under the carpet.
The sort of absurd political correctness that leads to the fraudulent conjurers known as ‘psychic surgeons’ being referred to as a “profession” by the Department of Health has obscured reality. Even the MHRA was persuaded to allow misleading labelling of homeopathic and herbal “remedies”. thus betraying its job. In its own words “The MHRA is the government agency that is responsible for ensuring that medicines and medical devices work, . . .”.
There is a lesson here. You can’t go on avoiding reality for ever. One consolation is that, in the end, it is the universities who are leading the way, albeit slowly.
All we need now is for the Department of Health, the MHRA and the endless box-ticking quangos to wake up too.
Herbal medicine is, unlike homeopathy, not ridiculous, It is merely Pharmacology, as practised up to circa 1900. Whereas good trials have now shown acupuncture to be sham and homeopathy to be a placebo, there has been very little good research on herbs.
Most herbalism could fairly be described giving to sick patients an unknown dose of a substance with unknown efficacy and unknown safety.
How odd, then, to visit the Royal Society of Medicine to be greeted thus.
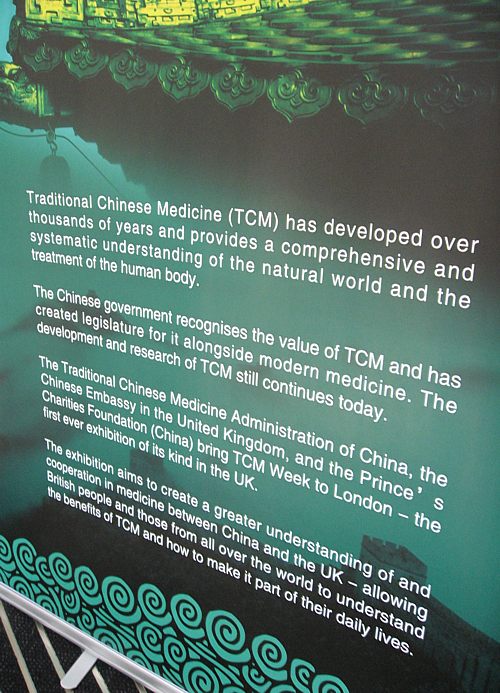
Just look at the words!
“Traditional Chinese Medicine (TCM) has developed over thousands of years”
That’s partly true
“and provides a comprehensive and systematic understanding of the natural world and the treatment of the human body.”
and that is total nonsense. TCM provides no understanding and virtually none of it is known to be useful for treating anything.
| Another poster at the RSM exhibition provides some of the explanation. What on earth, one wonders, do they mean by “making efforts to modernise TCM “? So far, the idea of modernising TCM doesn’t seem to include any great effort to find out if it works. Much of the promotion of TCM seems to be not so much ‘ancient wisdom’, but modern nationalist propaganda by the Chinese government. |
 |
The history is fascinating, but you won’t learn it from the posters on display at the exhibition.
“The Daoguang emperor though it [acupuncture] was a barrier to medical progress and removed it from the curriculum of the Imperial Medical Institute,”
“By the start of the twentieth century, acupuncture was extinct in the West and dormant in the East. It might have fallen out of favour permanently, but it suddenly experienced a revival in 1949 as a direct result of the communist revolution and the establishment of the People’s Republic of China. Chairman Mao Tse-tung engineered a resurgence in traditional Chinese medicine, which included not just acupuncture but also Chinese herbal medicine and other therapies ”
“His motivation was partly ideological, inasmuch as he wanted to reinforce a sense of national pride in Chinese medicine. However he was also driven by necessity. He had promised to deliver affordable healthcare .. . . ”
“Mao did not care whether traditional Chinese medicine worked, as long as he could keep the masses contented. In fact, his personal physician, Zhisui Li, wrote a memoir entitled ‘The Private Life of Chairman Mao’, in which he quoted Mao as saying”
“Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine.” “
Singh & Ernst Trick or Treatmant, page 46.
Or, as put more succinctly by Shapiro
“You would never know that TCM was fashioned in the twentieth century, as we shall see, from a ragbag of therapies in post-revolutionary China.”
Rose Shapiro, Suckers, how alternative medicine makes fools of us all.
Why is the Royal Society of Medicine allowing such mendacious posters? As it happens, I and a friend were visiting the RSM to see their Academic Dean, with a view to finding out why the RSM had failed to take any public position on alternative medicine. The answer appeared to be money, and that was the answer to why the TCM exhibition was being held on their premises too. The Dean no more believed in TCM than we did, but, well, they need the income. He pointed out (looking suitably sheepish) that the address given for the exhibition was not the RSM, but Number 1 Wimpole Street (that, of course, is also the address of the RSM).
Ah, so that’s OK then.
It has to be said that the RSM isn’t alone in its spineless attitude. Both the British Medical Association (BMA) and the Royal College of General Practitioners (RCGP) have failed to make any clear condemnation of mystical medicine. This is in stark contrast to just about every relevant scientific society (here is a summary).
It is a mystery to me why much of medicine should still be dominated by a mindset that seems to have lagged 200 years behind every other science. Perhaps medicine is just too complicated.
UCL Hospitals’ skeleton in the cupboard
Make no mistake, University College London Hospital is top class. The UCLH Trust. runs seven hospitals All but one of them are excellent. But in 2002 the Royal London Homeopathic Hospital was acquired as part of the UCLH group, to the intense embarrassment of UCL scientists.
Let’s start with the good bit. Usually I don’t like anecdotes, so just think of this as a vote of thanks, not evidence.
A personal history of UCH
I owe UCLH a lot personally. On December 13th 1984, my wife had
a subarachnoid haemorrhage when she was seven months pregnant. After misdiagnosis at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millilmetre from the pituitary on the other. It was a bit tricky but I think we got it”.
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds).. Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. | 
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album.. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. Heaven knows what it would have cost in the USA.
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew playing cricket in Bangladesh, Feb 2005. |
But now the the less desirable side of UCLH
Herbs and homeopaths at UCLH
| Recently I was sent the UCLH Annual Review 2007 – 2008. There was a lot of good stuff in it and worth a read despite there being too much hyperbole and too many pictures of men in dark suits. But buried among all the high tech stuff, what do we find but an advertisement for 1900-style pharmacology in the form of the herbal clinic at the Royal London Homeopathic Hospital, accompanied by a load of utterly inaccurate information from the TV botanist, David Bellamy. Take, for example, the claim about Devil’s Claw for osteoarthritis. Even alternative medicine advocates said “The authors concluded that there are insufficient high-quality trials to determine the safety and efficacy of Devil’s Claw (Harpagophytum procumbens) in the treatment of osteoarthritis, and that definitive trials are needed.”
Reading between the lines, I’d guess that the opening of this clinic has a subtext. It is well known that funding for homeopathy has dried up (partly as a result of our letter to NHS Trusts that appeared in the There have been problems before with the herbal activities at the RLHH before (see Conflicts of Interest at the Homeopathic Hospital). It appeared that the Khans, who run the Marigold homeopathic podiatry clinic (no, seriously, it is real) were largely prescribing a herbal product that was made by their own company. without even the hospital trust, never mind the patients, being made aware of it. In normal medicine this would be regarded as a rather serious offence, but as far as I know, nothing was ever done about it. |
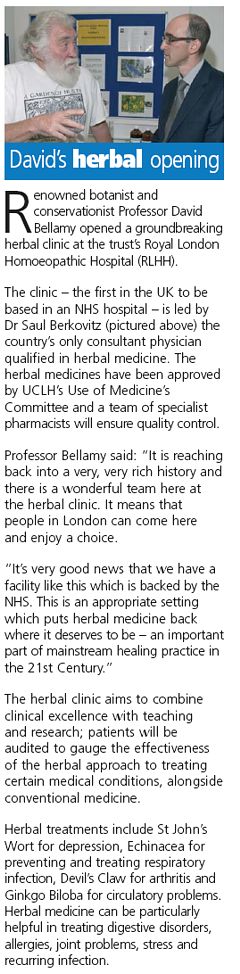 |
The ethics of alternative medicine are truly one of life’s great mysteries.
Reading further in the annual review, we come to the page about the RLHH. The homeopathy side must really have run down because it seems to have diversified into selling cosmetics and groceries. That sounds like desperation.

Good heavens, they sell “chemical-free sun cream”. One wonders what it can be made of, if not chemicals. This is the language of low-grade advertising agencies, not what one expects from an NHS hospital trust.
But next to this there is a much more interesting item. Just look at the last sentence.
I wonder if this could possibly have anything to do with the fact that Michael Baum and I visited the Trust headquarters in August 2006 to propose that the RLHH might be turned into a centre of supportive and palliative care? It would be nice to think so. But it seems they haven’t gone nearly far enough yet. If all they do is replace the waning homeopathy We know they are under pressure from their royal patrons, but that, in a constitutional monarchy, is simply not acceptable. |
 |
Michael Baum is a cancer surgeon who has taken a particular interest in palliative and supportive care. He is someone whose views should be taken seriously. He is also the author of the magnificent “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong” Here is a quotation from that letter. The UCLH Trust should bear it in mind.
| The power of my authority comes with a knowledge built on 40 years of study and 25 years of active involvement in cancer research. I’m sensitive to the danger of abusing this power and, as a last resort, I know that the General Medical Council (GMC) is watching over my shoulder to ensure I respect a code of conduct with a duty of care that respects patients’ dignity and privacy and reminds me that my personal beliefs should not prejudice my advice. Your power and authority rest on an accident of birth. Furthermore, your public utterances are worthy of four pages, whereas, if lucky, I might warrant one. I don’t begrudge you that authority and we probably share many opinions about art and architecture, but I do beg you to exercise your power with extreme caution when advising patients with life threatening diseases to embrace unproven therapies. There is no equivalent of the GMC for the monarchy, so it is left either to sensational journalism or, more rarely, to the quiet voice of loyal subjects such as myself to warn you that you may have overstepped the mark. It is in the nature of your world to be surrounded by sycophants (including members of the medical establishment hungry for their mention in the Queen’s birthday honours list) who constantly reinforce what they assume are your prejudices. Sir, they patronise you! Allow me this chastisement. |
Follow-up
The photo album chronicling the birth of my son, is really just for family and friends, but at least one blog picked up on the wider significance.
Today brings a small setback for those of us interested in spreading sensible ideas about science. According to a press release
“The BMJ Group is to begin publishing a medical journal on acupuncture from next year, it was announced today (Tuesday 11 November 2008).
This will be the first complementary medicine title that the BMJ Group has published.”
And they are proud of that? What one earth is going on? The BMJ group is a publishing company which says, of itself,
“Our brand stands for medical credibility. We are one of the world’s best known and most respected medical publishers.”
Well perhaps it used to be.
They have certainly picked a very bad moment for this venture. In the last year there have been at least five good books that assess the evidence carefully and honestly. Of these, the ones that are perhaps the best on the subject of acupuncture are Singh & Ernst’s Trick or Treatment and Barker Bausell’s Snake Oil Science. Both Ernst and Bausell have first hand experience of acupuncture research. And crucially, none of these authors has any financial interest in whether the judgement goes for acupuncture or against it.
Here are quotations from Singh & Ernst’s conclusions
“Reliable conclusions from systematic reviews make it clear that acupuncture does not work for a whole range of conditions, except as a placebo.”
“There are some high quality trials that support the use of acupuncture for some types of pain and nausea, but there are also high quality trials that contradict this conclusion. In short, the evidence is neither consistent nor convincing – it is borderline.”
The House of Lords’ report in 2000 tended to give acupuncture the benefit of the (very considerable) doubt that existed at the time the report was written. Since that time there have been a lot of very well-designed trials of acupuncture.
Now it is quite clear that, for most (and quite possibly all) conditions, acupuncture is no more than a particularly theatrical placebo. Perhaps that is not surprising insofar as the modern western practice of acupuncture owes more to Chinese nationalistic propaganda that started in the time of Mao-Tse Tung than it owes to ancient wisdom (which often turns out to be bunk anyway).
The BMJ Group has decided to endorse acupuncture at a time when it is emerging that the evidence for any specific effect is very thin indeed. Well done.
The journal in question is this.
Acupuncture in Medicine is a quarterly title, which aims to build the evidence base for acupuncture. It is currently self-published by the British Medical Acupuncture Society (BMAS).
One good thing can be said about the Society and the Journal. That is that they don’t espouse all the mumbo-jumbo about ‘meridians’ and ‘Qi’. This, of course, puts them at odds with the vast majority of acupuncture teaching. This sort of internecine warfare between competing sects is characteristic of all sorts of alternative medicine. But that is just ideology. What matters is whether or not sticking needles in you is actually anything more than a placebo.
British Medical Acupuncture Society (BMAS)
The British Medical Acupuncture Society (BMAS). is “a registered charity established to encourage the use and scientific understanding of acupuncture within medicine for the public benefit.”. The phrase “encourage the use” suggests that they do not even envisage the possibility that it might not work. Their web site includes these claims.
Acupuncture can help in a variety of conditions:
- Pain relief for a wide range of painful conditions
- Nausea, especially postoperative nausea and vomiting
- Overactive bladder, also known as bladder detrusor instability
- Menstrual and menopausal problems, eg period pains and hot flushes
- Allergies such as hay fever and some types of allergic rashes
- Some other skin problems such as ulcers, itching and localised rashes
- Sinus problems and more
Presumably the word “help” is chosen carefully to fall just short of “cure”. The claims are vaguely worded, but let’s see what we can find about them from systematic reviews. It appears that the BMAS is being rather optimistic about the evidence.
BMJ Clinical Evidence is considered reliable and is particular interesting because it is owned by the BMJ Publishing Group.
Low Back Pain (chronic) Acupuncture is listed as being of “unknown effectiveness”.
Dysmenorrhoea Acupuncture is listed as being of “unknown effectiveness”.
Osteoarthritis of the knee. Acupuncture is listed as being of “unknown effectiveness”.
Psoriasis (chronic plaque) Acupuncture is listed as being of “unknown effectiveness”.
Neck pain “Acupuncture may be more effective than some types of sham treatment (not further defined) or inactive treatment (not further defined) at improving pain relief at the end of treatment or in the short term (less than 3 months), but not in the intermediate term (not defined) or in the long term (not defined)”
Headache (chronic tension-type) Acupuncture is listed as being of “unknown effectiveness”.
What about the greatest authority, the Cochrane Reviews?
Cochrane Reviews
Low back pain The data do not allow firm conclusions about the effectiveness of acupuncture for acute low-back pain. For chronic low-back pain, acupuncture is more effective for pain relief and functional improvement than no treatment or sham treatment immediately after treatment and in the short-term only. Acupuncture is not more effective than other conventional and “alternative” treatments. The data suggest that acupuncture and dry-needling may be useful adjuncts to other therapies for chronic low-back pain. Because most of the studies were of lower methodological quality, there certainly is a further need for higher quality trials in this area.
Chronic asthma. There is not enough evidence to make recommendations about the value of acupuncture in asthma treatment. Further research needs to consider the complexities and different types of acupuncture.
But most of the vaguely-worded claims made by BMAS have not been the subject of Cochrane reviews. The obvious interpretation of that is that there is not enough evidence to make it worth writing a review. In which case, why does BMAS claim that acupuncture can “help”?
Bandolier is another excellent source of high quality information, This was their view in September 2006
“Large, high-quality randomised trials of acupuncture have been published since the reviews. In fibromyalgia, chemotherapy-induced nausea and vomiting, breech presentation, tension headache, and migraine, all were negative compared with sham acupuncture. One in osteoarthritis of the knee, had statistical improvement over sham acupuncture at three months, but not later. Both large trials and this review of reviews come to the same general conclusion; that over a whole range of conditions and outcomes acupuncture cannot yet be shown to be effective.”
After thousands of years of acupuncture (or at least almost 40 years in the West) there seems to be very little to show for it.
The journal: Acupuncture in Medicine
What about the journal in question? Like all journals devoted to alternative medicine, it claims to be evidence-based. And like all journals devoted to alternative medicine it suffers from a fatal conflict of interest. If this journal were ever to conclude that acupuncture is a placebo, it would destroy the journal and the livelihoods of many of the people who write for it.
Scanning the first three issues of 2008 shows that it is very much like other alternative medicine journals. Most of the papers don’t address the critical question, is it a placebo. And most papers end up rather limply, with a statement along the lines “acupuncture may be useful for ***. More research is needed.”
The editor in chief of the journal is Dr Adrian White, and its editor is Michael Cummings. White is quoted by Ernst in the Guardian in 2004.
“We need to provide hard evidence to support what we all see in our clinics every day: that the modern approach to acupuncture works, and is highly relevant to the new, patient-centred NHS.” .
That means the answer is assumed in advance. That just isn’t science.. ‘We know the answer, all we have to do now is get some evidence’.
Why should the BMJ Group want to do a thing like this?
The press release says
Commenting on the move, BMJ and BMJ Journals Publishing Director, Peter Ashman, said “The journal is a good complement for our existing portfolio of journals and we’re certain that the Society’s members and other subscribers will appreciate the benefits of the decision the BMAS has made on their behalf.”
He continued: “The BMAS is ambitious for its journal to grow and flourish and we’re looking forward to working with the Society to develop an editorial and commercial strategy which will achieve the aims of BMAS and those of its members, while reaching out to the wider global community interested in this fascinating area of medicine.”
Yes, you got it. Money. The same motive that causes some vice-chancellors to bring their university into disrepute by awarding BSc degrees in subjects that are not only not science, but which are oftenly openly anti-science.
Conscience doesn’t seem to bother these people, so let’s put the problem in purely cash terms.
Both the BMJ Group and the vice-chancellors will have to decide whether the cash they gain is sufficient to counterbalance the corrosive effects of their actions on their own reputations.
Follow-up
Only a couple of days later, two new trials show acupuncture is no different from sham controls for helping IVF pregnancy rates. James Randerson in the Guardian writes thus.
“Acupuncture aimed at improving IVF success rates is widely offered by fertility clinics in the UK. In the first of the studies, researchers in Hong Kong split 370 women receiving IVF into two groups. One group received real acupuncture before and after having an IVF embryo implanted into their uterus. The other had the same procedure, except the treatment used retractable needles that did not penetrate the skin.”
“Of the 185 who received the sham treatment, 91 achieved a clinical pregnancy (foetal heartbeat identified using ultrasound) and 71 had a successful delivery. This compared with 72 clinical pregnancies in the true acupuncture group and 55 live births. The differences between the groups were not statistically significant.”
“In a second study, researchers in Chicago used a similar design in which 124 women received true or sham acupuncture. The control group had their skin punctured by real acupuncture needles, but not at genuine “Qi-lines” on the body. In the true acupuncture group, 43.9% achieved a clinical pregnancy, compared with 55.2% of the women given the sham treatment. “
The original paper for the first study can be seen here.
It was a great delight to visit Amsterdam on 25 October to speak at a meeting off the Vereniging tegen de Kwakzalverij (Society against quackery). Unfortunately their excellent web site is in Dutch, so the best you can do at the moment is to use the Google translation, with its frequently hilarious renderings. Better translations coming soon, I hope.
| Symposium
Niet-reguliere geneeswijzen in de 21ste eeuw in internationaal perspectief Non-mainstream medicine in the 21st century in an international perspective |
 |
The Dutch society has 1800 members and is the oldest and biggest such society in the world. I very much hope that their web site will soon have an English version. That is only appropriate since the origin of the word quack is from the Dutch Kwakzalver. (Kwak=Chatterer, salesman, zalf = salve, ointment). (In contrast the noise made by a duck is simply described by the OED as being “imitative”, though the great Michael Quinion thinks the two usages may be connected.

De Kwakzalver, Jan Steen (1626-1679) Rijksmuseum Amsterdam. Click to enlarge

The Quack doctor, Jan Steen (1626-1679). Click to enlarge
Translations of some key parts will be posted here soon. My talk was about Support for alternative medicine in government and universities in the U.K
The meeting started with the announcement of the winner of the Meester Kackadorisprijs.
The Master Kackodoris prize
The Meester Kackadorisprijs is awarded to individuals or institutions who promote quackery and who should know better (the quacks themselves are never nominated). The short list for the 2008 prize included the vice chancellor of the Free University of Amsterdam
| Prof. dr. Lex Bouter, rector magnificus Vrije Universiteit
The vice-chancellor was on the short-list for the prize because of his part in a recent paper, “Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: systematic review and meta-analysis.” (Manheimer E, Zhang G, Udoff L, Haramati A, Langenberg P, Berman BM, Bouter LM, Brit Med J 336, 545-9) [Available free] |
 |
This paper has been cited all over the world, but it seems not to have been very good. See for example the magnificent analysis of it in “Yawn, still one more overhyped acupuncture study: Does acupuncture help infertile women conceive?” . See also the Cochrane review (it could all be placebo). The fact that the vice-chancellor appears to have been only a ‘guest author’ anyway does not count as an excuse. The large number of citations received by this paper should, incidentally, be seen as another nail in the coffin of attempts to measure quality by citation rates.
In the event, vice-chancellor Bouter did not win the Kackodoris prize this year. In a speech at the start of the symposium, it emerged that he had been narrowly beaten by the Dutch Christian Radio Association for its assiduous promotion of quackery.
The chair of the Dutch society, Cees Rencken, is doing a great job. I hope that it will soon be better known outside the Netherlands.
And it’s time we had a UK equivalent of the Kackadoris prize. There will be no shortage of worthy candidates.

Frits Van Dam (Secretary) and Cees Renckens (Chair) of VtdK
(photo: Sofie van de Calseijde)

Some pictures of Amsterdam
(meetings photos: Sofie van de Calseijde)
Follow-up
We know all about the sixteen or so universities that run “BSc” degrees in hokum. They are all “post-1992” universities, which used to be polytechnics. That is one reason why it saddens me to see them destroying their own attempts to achieve parity with older universities by running courses that I would regard as plain dishonest.
Older universities do not run degree courses in such nonsense. Academics (insofar as they still have any influence) certainly would not put up with it if they tried. But nevertheless you can find quackery in some of the most respected universities, and it gets there not via academics but (guess what) via Human Resources. It creeps in through two routes. One is the “training courses” that research staff now have to do (the “Roberts agenda”). The other route is through occupational health services.
Quackery in training courses
It isn’t easy to find out what happens elsewhere, but I was certainly surprised to find out that UCL’s own HR department was offering a course that promised to teach you the “core principles” of Brain Gym and Neurolinguistic Programming, both totally discredited bits of psycho-babble, more appropriate to the lifestyle section of a downmarket.women’s magazine than a university. I gather that HR’s reaction after I brought this to light was not to ask what was wrong with it, but just to get angry.
In a spirit of collegiality I offered to run a transferable skills course myself. I even offered to do it for nothing (rather than the rumoured £700 per day charged by the life style consultants). I proposed a course in ‘How to read critically’ (subtitle ‘How to detect bullshit’). This seems to me to be the ultimate transferable skill. Bullshit occurs in every walk of life. My proposal was moderately worded and perfectly serious.
Guess what? Despite several reminders, I have never had any response to my suggestion. Well, I suppose that HR people now regard themselves as senior to mere professors and there is really no need to reply to their
letters.
Quackery in occupational health. Leicester sets a good example
If you work at a university, why not search the university’s web site for “complementary medicice” or complementary therapies”. If it is a real university, you won’t find any degrees in homeopathy, or in amethysts
that emit high yin energy. But some quite surprising places are found to be recommending magic medicine through their Occupational Health service, which usually seems to be part of HR. In fact at one time even UCL was doing it, but no soon had somebody sent me the link than it disappeared. As a matter of historical record, you can see it here (it had all the usual junk, as well as harmless stuff like yoga and pilates).
While looking for something else I stumbled recently some other cases. One was at the University of Leicester, a very good university (and alma mater to the great David Attenborough who must have done more to point out the beauty of science than just about anyone). But we find on their staff wellbeing site, alongside some perfectly sensible stuff, a link to complementary therapies.
The list of ‘therapies’ includes not only the usual placebos, acupuncture, reiki, reflexology, but, even more exotically, a fraudulent Russian device called SCENAR therapy. They have a nice leaflet that explains all these things in words that run the whole gamut from meaningless gobbledygook to plain wrong. Here are some examples from the leaflet.
Reflexology
“In the feet, there are reflex areas corresponding to all the parts of the body and these areas are arranged in such a way as to form a map of the body in the feet”
Reflexology has been shown to be effective for:
- Back Pain
- Migraine
- Infertility
- Arthritis
Well no, there are no such areas in your feet. That is sheer imagination. And reflexology has not “been shown to be effective” for any of those conditions. These claims for therapeutic efficacy are not only lies. They are also illegal.
“Reiki
Each hand position is held for a few minutes, and during this time healing energy will flow into you, balancing your energy system, releasing stress, soothing pain, and promoting your body’s natural ability to heal itself.”
This is sheer idiotic mumbo-jumbo. The “flow of healing energy” is totally imaginary. Such talk is offensive to anyone with half a brain. Insofar as they claim to heal anything, it is also illegal. The comes SCENAR.
“What is SCENAR?
SCENAR is an acronym for Self Controlled Energo- Neuro Adaptive Regulator. It is a reflex biofeedback device which when used by a qualified practitioner, can help to alleviate acute and chronic pain. It is licensed in the UK for pain relief but experience has shown that it is helpful in a wide variety of conditions.”
This is even more seriously nuts than the others. The term “licensed” means merely that it is electrically safe. It certainly does not mean that it works. Pubmed shows only three publications about the SCENAR device, all in Russian,
One sales site (apparently Russian) makes the following modest claim.
“A prime goal of the Russian Space Program was to provide space travelers with a portable medical device that would become their “universal medical assistant” in space. So from the beginning, the SCENAR was designed to replace an entire medical hospital, with all its staff, diagnostic and treatment facilities, even the pharmacy. A universal, non-invasive, portable regulator of body functions (among other things) was envisaged.”
The SCENAR device (right) looks like a TV remote control (perhaps it IS a TV remote control -we aren’t anywhere told in comprehensible terms what’s in the box. The Russian site sells also the rather baffling accessory on the right. The mind boggles.

SCENAR device |

Remote rectal-vaginal electrode for SCENAR |
How does this rubbish get onto the web site of a good university?
I presume that it is just another sign of what happens when universities come to be run by non-academics. No doubt the occupational health people are well meaning and kind, but just scientifically illiterate. What about the HR person in charge of them? They are not known for scientific literacy either (which would not matter if they stuck to their job). But perhaps they just didn’t notice. There is only one way to find out. Ask. So I sent this letter.on 10th September.
| Hello
I am a pharmacologist and I have a side interest in public understanding of science, alternative medicine.and medical fraud I was quite surprised when Google led me unexpectedly to your complementary therapies page at http://www.le.ac.uk/staffwellbeing/complementary_therapy.html There is, sad to say, a great deal of information on these pages that is simply not true. For example it has NOT been shown that reflexology has been shown to be effective in any of the conditions which you list, as far as I know To take only one more example from this page, the SCENAR device is an even more extreme example. It is well known to be fraudulent. and has been investigated by the Washington State Attorney General. This sort of thing is not what one would expect from a very respectable university, and it must be a great embarrassment to your excellent medical scientists. Apart from the many scientific inaccuracies (which greatly impede the efforts of those of us who try to improve public understanding of science), you are, I hope, aware that there is a legal aspect. Since May this year, new regulations have made it illegal to make claims for health benefits if evidence cannot be produced to show that the claims are justified. I would like to put it to you that many of the claims made on this page are not only immoral, but also illegal. I wondered whether you , or your HR department, would like to make any comments Best regards David Colquhoun |
I got an immediate and very sympathetic response from the Director of HR and a week later, on17th September, he wrote
“Hi David,
I have discussed the matter with my manager of Staff Counselling and Welfare and have agreed that it is probably safest that we remove the references to ‘complimentary’[sic] therapies from the site entirely.
Thank you for your helpful input and the recommendations for reading matter.”
So there is a lesson here. If you find this sort or stuff on your own institution’s web site, all that may be needed is a simple letter that points out what nonsense it is. Admittedly the HR man seemed rather more worried about whether the claims were illegal than whether they were true, but either way, it worked.
Only one little snag. As of 6 October the pages still have not been removed.
On the assumption that they eventually will be removed, I have kept copies of the Wellbeing page, of the Complementary Therapies page, and of the ‘explanatory leaflet’. They stand as part of a historical record that
shows, once again, what can happen when scientific matters get into the hands of HR. Fortunately Leicester University has an HR director who is willing to listen to advice.
Follow-up
Something seems to have gone seriously wrong. Despite the rapid response, virtually all the nonsense is still there on 13th October. It seems not to be so simple after all.
And despite several reminders, the advertisement for SCENAR ‘therapy’ is still on the University web site on December 14th. I know that no decision by HR can be made with fewer than 25 meetings and an awayday in Majorca, but this is getting ridiculous.
