CAM
Back to my old interest in medicine that doesn’t work. And the fact that there is such a huge market for medicine that doesn’t work is, in large part, a result of regulators who fail to regulate.
One example of a regulator that fails to protect the public from health fraud is the Complementary and Natural Healthcare Council -the CNHC (known colloquially as OfQuack). I have history with them, having offered my services to them, and, astonishingly, been accepted. There I found a lot of well-meaning but poorly-educated people: they had no idea about what constituted evidence, and very little interest in finding out. Of course, I was asked to resign and when I declined to do so, I was fired.
AI reports on health claims
That’s one reason that I was happy to play a small part in a recent study of the health claims made by people who are registered with the CNHC. [link to the paper -it’s open access]. Registration is voluntary: anyone can practise as a naturopath or reflexologist with no need for qualifications and no check on their activities. But if they do choose to register with the CNHC they’ll appear on their website, and that confers on them a (spurious) sort of respectablity.
In the study, artificial intelligence was asked to identify false or misleading claims made on the web sites of practitioners who were registered with the CNHC. Only the practitioners of the most obviously pseudoscientific subjects were included (Alexander Technique, Aromatherapy, Bowen Therapy, Colon Hydrotherapy, Craniosacral Therapy, Healing, Kinesiology, Microsystems Acupuncture, Naturopathy, Reflexology, Reiki and Shiatsu).
The AI assessed text from 11,771 web pages, scraped from 725 web sites. It identified false or misleading claims in 704 (97%) of the websites. The complete list of 23,307 claims identified by AI, with the reasons that AI provided, can be downloaded at https://osf.io/hnuqs (better not try printing it out -it has 2370 pages).
A few of the web pages were read by four humans, and the humans identified a comparable number of false or misleading claims to that found by the AI.
What does this mean for AI?
It seems that the AI did a good job in identifying false and misleading claims. That surprised me because AI has to learn from what it finds on the web. And the information on the web about reflexology, craniosacral therapy and naturopathy etc, is almost all nonsense -just sales talk. The fact that AI wasn’t fooled by this shows that the information that was used to train the AI came, almost entirely, from reliable sources, The sources of training material are a human choice. So the finding that AI can judge that reflexology is nonsense is actually a result of the human intelligence that decided which sources were reliable and which were not.
I’ve tried asking AI several real science questions and I’ve been very disappointed by the answers. The AI showed no ability to judge between different, but legitimate, points of view. For example there is a lot of good material on the web about statistical inference (but also quite a lot of mediocre stuff).
When I asked about the interpretation of p values, the first answers were quite accurate but entirely frequentist. When I pointed out that likelihood and Bayesian approaches are often critical of the frequentist interpretation, the AI apologised and tried again (the mock humility of the apology was particularly horrid). After a few more prompts, the AI came to a view of the problem which was quite close to mine. That doesn’t mean that my view is right. It means that, with helpful prompts, AI can be led to almost any conclusion you wish.
Once again, the biggest influence is the human intelligence that guides the AI. The computer algorithm showed NO understanding of the problems. It spat out a version of the material that was used to train it. It was at the level of a mediocre undergraduate. The only way to detect that it was AI was that it answered in better English, with fewer spelling mistakes than most undergraduates can manage. That makes its use doubly dangerous.
Implications for regulation of alternative medicine
It’s been obvious for a long time that the regulators of alternative medicine fail totally to protect the public from false and misleading claims being made about the products that are being sold to the public. That is shown abundantly by this paper. The number of false or misleading claims that were found on the web is inevitably an underestimate of the real number. AI could count only claims that were made in public, on the web. It couldn’t count the number of false claims that are made in private conversations, nor the number made in printed advertisements.
It’s clear from the huge number of false claims made by CNHC registrants that it would take a lot of time and effort for the CNHC to fulfil its duty to protect the public from them. The benefit of using AI is not that it’s any better than humans at detecting false and misleading claims. The benefit lies entirely in the speed with which it can do the job. That’s why the senior author of the paper, Simon Perry, offered the use of his methods to the CNHC. So far they have shown little interest in accepting that help. All that I can infer from this is that the CNHC has little interest in the false claims made by its registrants, as long as they keep paying the registration fees. It hasn’t changed much since I was part if it, 14 years ago.
Conclusions
AI looks quite promising for some problems where the task is limited and the rules are clear. Learning to spot cancerous tissue in radiographs, when trained on enough radiographs in which the human diagnosis turned out to be accurate. AI also did a good job in detecting false or misleading claims by practitioners of various sorts of alternative medicine, though this reflects the (human) choice of reliable sources of information. The speed with which this can be done should be useful to regulators who are interested in stopping the spread of misinformation. Sadly most regulators show very little interest in doing that part of their job.
Ai seems to have done a good job in predicting protein folding. That is a very restricted task, and there is a lot of (mostly) reliable information to train on. There is a lot of hype about its use for drug discovery, but the training data for that job is often crude and inaccurate.
But general-AI has a long way to go. It has no understanding of what it says. At the moment it’s mainly a tool for crooks, fraudsters and charlatans whose intent is to deceive.
This piece is almost identical with today’s Spectator Health article.
This week there has been enormously wide coverage in the press for one of the worst papers on acupuncture that I’ve come across. As so often, the paper showed the opposite of what its title and press release, claimed. For another stunning example of this sleight of hand, try Acupuncturists show that acupuncture doesn’t work, but conclude the opposite: journal fails, published in the British Journal of General Practice).
Presumably the wide coverage was a result of the hyped-up press release issued by the journal, BMJ Acupuncture in Medicine. That is not the British Medical Journal of course, but it is, bafflingly, published by the BMJ Press group, and if you subscribe to press releases from the real BMJ. you also get them from Acupuncture in Medicine. The BMJ group should not be mixing up press releases about real medicine with press releases about quackery. There seems to be something about quackery that’s clickbait for the mainstream media.
As so often, the press release was shockingly misleading: It said
Acupuncture may alleviate babies’ excessive crying Needling twice weekly for 2 weeks reduced crying time significantly
This is totally untrue. Here’s why.
|
Luckily the Science Media Centre was on the case quickly: read their assessment. The paper made the most elementary of all statistical mistakes. It failed to make allowance for the jelly bean problem. The paper lists 24 different tests of statistical significance and focusses attention on three that happen to give a P value (just) less than 0.05, and so were declared to be "statistically significant". If you do enough tests, some are bound to come out “statistically significant” by chance. They are false postives, and the conclusions are as meaningless as “green jelly beans cause acne” in the cartoon. This is called P-hacking and it’s a well known cause of problems. It was evidently beyond the wit of the referees to notice this naive mistake. It’s very doubtful whether there is anything happening but random variability. And that’s before you even get to the problem of the weakness of the evidence provided by P values close to 0.05. There’s at least a 30% chance of such values being false positives, even if it were not for the jelly bean problem, and a lot more than 30% if the hypothesis being tested is implausible. I leave it to the reader to assess the plausibility of the hypothesis that a good way to stop a baby crying is to stick needles into the poor baby. If you want to know more about P values try Youtube or here, or here. |
One of the people asked for an opinion on the paper was George Lewith, the well-known apologist for all things quackish. He described the work as being a "good sized fastidious well conducted study ….. The outcome is clear". Thus showing an ignorance of statistics that would shame an undergraduate.
On the Today Programme, I was interviewed by the formidable John Humphrys, along with the mandatory member of the flat-earth society whom the BBC seems to feel obliged to invite along for "balance". In this case it was professional acupuncturist, Mike Cummings, who is an associate editor of the journal in which the paper appeared. Perhaps he’d read the Science media centre’s assessment before he came on, because he said, quite rightly, that
"in technical terms the study is negative" "the primary outcome did not turn out to be statistically significant"
to which Humphrys retorted, reasonably enough, “So it doesn’t work”. Cummings’ response to this was a lot of bluster about how unfair it was for NICE to expect a treatment to perform better than placebo. It was fascinating to hear Cummings admit that the press release by his own journal was simply wrong.
Listen to the interview here
Another obvious flaw of the study is that the nature of the control group. It is not stated very clearly but it seems that the baby was left alone with the acupuncturist for 10 minutes. A far better control would have been to have the baby cuddled by its mother, or by a nurse. That’s what was used by Olafsdottir et al (2001) in a study that showed cuddling worked just as well as another form of quackery, chiropractic, to stop babies crying.
Manufactured doubt is a potent weapon of the alternative medicine industry. It’s the same tactic as was used by the tobacco industry. You scrape together a few lousy papers like this one and use them to pretend that there’s a controversy. For years the tobacco industry used this tactic to try to persuade people that cigarettes didn’t give you cancer, and that nicotine wasn’t addictive. The main stream media obligingly invite the representatives of the industry who convey to the reader/listener that there is a controversy, when there isn’t.
Acupuncture is no longer controversial. It just doesn’t work -see Acupuncture is a theatrical placebo: the end of a myth. Try to imagine a pill that had been subjected to well over 3000 trials without anyone producing convincing evidence for a clinically useful effect. It would have been abandoned years ago. But by manufacturing doubt, the acupuncture industry has managed to keep its product in the news. Every paper on the subject ends with the words "more research is needed". No it isn’t.
Acupuncture is pre-scientific idea that was moribund everywhere, even in China, until it was revived by Mao Zedong as part of the appalling Great Proletarian Revolution. Now it is big business in China, and 100 percent of the clinical trials that come from China are positive.
if you believe them, you’ll truly believe anything.
Follow-up
29 January 2017
Soon after the Today programme in which we both appeared, the acupuncturist, Mike Cummings, posted his reaction to the programme. I thought it worth posting the original version in full. Its petulance and abusiveness are quite remarkable.
I thank Cummings for giving publicity to the video of our appearance, and for referring to my Wikipedia page. I leave it to the reader to judge my competence, and his, in the statistics of clinical trials. And it’s odd to be described as a "professional blogger" when the 400+ posts on dcscience.net don’t make a penny -in fact they cost me money. In contrast, he is the salaried medical director of the British Medical Acupuncture Society.
It’s very clear that he has no understanding of the error of the transposed conditional, nor even the mulltiple comparison problem (and neither, it seems, does he know the meaning of the word ‘protagonist’).
I ignored his piece, but several friends complained to the BMJ for allowing such abusive material on their blog site. As a result a few changes were made. The “baying mob” is still there, but the Wikipedia link has gone. I thought that readers might be interested to read the original unexpurgated version. It shows, better than I ever could, the weakness of the arguments of the alternative medicine community. To quote Upton Sinclair:
“It is difficult to get a man to understand something, when his salary depends upon his not understanding it.”
It also shows that the BBC still hasn’t learned the lessons in Steve Jones’ excellent “Review of impartiality and accuracy of the BBC’s coverage of science“. Every time I appear in such a programme, they feel obliged to invite a member of the flat earth society to propagate their make-believe.
Acupuncture for infantile colic – misdirection in the media or over-reaction from a sceptic blogger?26 Jan, 17 | by Dr Mike Cummings So there has been a big response to this paper press released by BMJ on behalf of the journal Acupuncture in Medicine. The response has been influenced by the usual characters – retired professors who are professional bloggers and vocal critics of anything in the realm of complementary medicine. They thrive on oiling up and flexing their EBM muscles for a baying mob of fellow sceptics (see my ‘stereotypical mental image’ here). Their target in this instant is a relatively small trial on acupuncture for infantile colic.[1] Deserving of being press released by virtue of being the largest to date in the field, but by no means because it gave a definitive answer to the question of the efficacy of acupuncture in the condition. We need to wait for an SR where the data from the 4 trials to date can be combined. So what about the research itself? I have already said that the trial was not definitive, but it was not a bad trial. It suffered from under-recruiting, which meant that it was underpowered in terms of the statistical analysis. But it was prospectively registered, had ethical approval and the protocol was published. Primary and secondary outcomes were clearly defined, and the only change from the published protocol was to combine the two acupuncture groups in an attempt to improve the statistical power because of under recruitment. The fact that this decision was made after the trial had begun means that the results would have to be considered speculative. For this reason the editors of Acupuncture in Medicine insisted on alteration of the language in which the conclusions were framed to reflect this level of uncertainty. DC has focussed on multiple statistical testing and p values. These are important considerations, and we could have insisted on more clarity in the paper. P values are a guide and the 0.05 level commonly adopted must be interpreted appropriately in the circumstances. In this paper there are no definitive conclusions, so the p values recorded are there to guide future hypothesis generation and trial design. There were over 50 p values reported in this paper, so by chance alone you must expect some to be below 0.05. If one is to claim statistical significance of an outcome at the 0.05 level, ie a 1:20 likelihood of the event happening by chance alone, you can only perform the test once. If you perform the test twice you must reduce the p value to 0.025 if you want to claim statistical significance of one or other of the tests. So now we must come to the predefined outcomes. They were clearly stated, and the results of these are the only ones relevant to the conclusions of the paper. The primary outcome was the relative reduction in total crying time (TC) at 2 weeks. There were two significance tests at this point for relative TC. For a statistically significant result, the p values would need to be less than or equal to 0.025 – neither was this low, hence my comment on the Radio 4 Today programme that this was technically a negative trial (more correctly ‘not a positive trial’ – it failed to disprove the null hypothesis ie that the samples were drawn from the same population and the acupuncture intervention did not change the population treated). Finally to the secondary outcome – this was the number of infants in each group who continued to fulfil the criteria for colic at the end of each intervention week. There were four tests of significance so we need to divide 0.05 by 4 to maintain the 1:20 chance of a random event ie only draw conclusions regarding statistical significance if any of the tests resulted in a p value at or below 0.0125. Two of the 4 tests were below this figure, so we say that the result is unlikely to have been chance alone in this case. With hindsight it might have been good to include this explanation in the paper itself, but as editors we must constantly balance how much we push authors to adjust their papers, and in this case the editor focussed on reducing the conclusions to being speculative rather than definitive. A significant result in a secondary outcome leads to a speculative conclusion that acupuncture ‘may’ be an effective treatment option… but further research will be needed etc… Now a final word on the 3000 plus acupuncture trials that DC loves to mention. His point is that there is no consistent evidence for acupuncture after over 3000 RCTs, so it clearly doesn’t work. He first quoted this figure in an editorial after discussing the largest, most statistically reliable meta-analysis to date – the Vickers et al IPDM.[2] DC admits that there is a small effect of acupuncture over sham, but follows the standard EBM mantra that it is too small to be clinically meaningful without ever considering the possibility that sham (gentle acupuncture plus context of acupuncture) can have clinically relevant effects when compared with conventional treatments. Perhaps now the best example of this is a network meta-analysis (NMA) using individual patient data (IPD), which clearly demonstrates benefits of sham acupuncture over usual care (a variety of best standard or usual care) in terms of health-related quality of life (HRQoL).[3] |
30 January 2017
I got an email from the BMJ asking me to take part in a BMJ Head-to-Head debate about acupuncture. I did one of these before, in 2007, but it generated more heat than light (the only good thing to come out of it was the joke about leprechauns). So here is my polite refusal.
|
Hello Thanks for the invitation, Perhaps you should read the piece that I wrote after the Today programme Why don’t you do these Head to Heads about genuine controversies? To do them about homeopathy or acupuncture is to fall for the “manufactured doubt” stratagem that was used so effectively by the tobacco industry to promote smoking. It’s the favourite tool of snake oil salesman too, and th BMJ should see that and not fall for their tricks. Such pieces night be good clickbait, but they are bad medicine and bad ethics. All the best David |
‘We know little about the effect of diet on health. That’s why so much is written about it’. That is the title of a post in which I advocate the view put by John Ioannidis that remarkably little is known about the health effects if individual nutrients. That ignorance has given rise to a vast industry selling advice that has little evidence to support it.
The 2016 Conference of the so-called "College of Medicine" had the title "Food, the Forgotten Medicine". This post gives some background information about some of the speakers at this event. I’m sorry it appears to be too ad hominem, but the only way to judge the meeting is via the track record of the speakers.


Quite a lot has been written here about the "College of Medicine". It is the direct successor of the Prince of Wales’ late, unlamented, Foundation for Integrated Health. But unlike the latter, its name is disguises its promotion of quackery. Originally it was going to be called the “College of Integrated Health”, but that wasn’t sufficently deceptive so the name was dropped.
For the history of the organisation, see
Don’t be deceived. The new “College of Medicine” is a fraud and delusion
The College of Medicine is in the pocket of Crapita Capita. Is Graeme Catto selling out?
The conference programme (download pdf) is a masterpiece of bait and switch. It is a mixture of very respectable people, and outright quacks. The former are invited to give legitimacy to the latter. The names may not be familiar to those who don’t follow the antics of the magic medicine community, so here is a bit of information about some of them.
The introduction to the meeting was by Michael Dixon and Catherine Zollman, both veterans of the Prince of Wales Foundation, and both devoted enthusiasts for magic medicne. Zollman even believes in the battiest of all forms of magic medicine, homeopathy (download pdf), for which she totally misrepresents the evidence. Zollman works now at the Penny Brohn centre in Bristol. She’s also linked to the "Portland Centre for integrative medicine" which is run by Elizabeth Thompson, another advocate of homeopathy. It came into being after NHS Bristol shut down the Bristol Homeopathic Hospital, on the very good grounds that it doesn’t work.
Now, like most magic medicine it is privatised. The Penny Brohn shop will sell you a wide range of expensive and useless "supplements". For example, Biocare Antioxidant capsules at £37 for 90. Biocare make several unjustified claims for their benefits. Among other unnecessary ingredients, they contain a very small amount of green tea. That’s a favourite of "health food addicts", and it was the subject of a recent paper that contains one of the daftest statistical solecisms I’ve ever encountered
"To protect against type II errors, no corrections were applied for multiple comparisons".
If you don’t understand that, try this paper.
The results are almost certainly false positives, despite the fact that it appeared in Lancet Neurology. It’s yet another example of broken peer review.
It’s been know for decades now that “antioxidant” is no more than a marketing term, There is no evidence of benefit and large doses can be harmful. This obviously doesn’t worry the College of Medicine.
Margaret Rayman was the next speaker. She’s a real nutritionist. Mixing the real with the crackpots is a standard bait and switch tactic.
Eleni Tsiompanou, came next. She runs yet another private "wellness" clinic, which makes all the usual exaggerated claims. She seems to have an obsession with Hippocrates (hint: medicine has moved on since then). Dr Eleni’s Joy Biscuits may or may not taste good, but their health-giving properties are make-believe.
Andrew Weil, from the University of Arizona
gave the keynote address. He’s described as "one of the world’s leading authorities on Nutrition and Health". That description alone is sufficient to show the fantasy land in which the College of Medicine exists. He’s a typical supplement salesman, presumably very rich. There is no excuse for not knowing about him. It was 1988 when Arnold Relman (who was editor of the New England Journal of Medicine) wrote A Trip to Stonesville: Some Notes on Andrew Weil, M.D..
“Like so many of the other gurus of alternative medicine, Weil is not bothered by logical contradictions in his argument, or encumbered by a need to search for objective evidence.”
This blog has mentioned his more recent activities, many times.
Alex Richardson, of Oxford Food and Behaviour Research (a charity, not part of the university) is an enthusiast for omega-3, a favourite of the supplement industry, She has published several papers that show little evidence of effectiveness. That looks entirely honest. On the other hand, their News section contains many links to the notorious supplement industry lobby site, Nutraingredients, one of the least reliable sources of information on the web (I get their newsletter, a constant source of hilarity and raised eyebrows). I find this worrying for someone who claims to be evidence-based. I’m told that her charity is funded largely by the supplement industry (though I can’t find any mention of that on the web site).
Stephen Devries was a new name to me. You can infer what he’s like from the fact that he has been endorsed byt Andrew Weil, and that his address is "Institute for Integrative Cardiology" ("Integrative" is the latest euphemism for quackery). Never trust any talk with a title that contains "The truth about". His was called "The scientific truth about fats and sugars," In a video, he claims that diet has been shown to reduce heart disease by 70%. which gives you a good idea of his ability to assess evidence. But the claim doubtless helps to sell his books.
Prof Tim Spector, of Kings College London, was next. As far as I know he’s a perfectly respectable scientist, albeit one with books to sell, But his talk is now online, and it was a bit like a born-again microbiome enthusiast. He seemed to be too impressed by the PREDIMED study, despite it’s statistical unsoundness, which was pointed out by Ioannidis. Little evidence was presented, though at least he was more sensible than the audience about the uselessness of multivitamin tablets.
Simon Mills talked on “Herbs and spices. Using Mother Nature’s pharmacy to maintain health and cure illness”. He’s a herbalist who has featured here many times. I can recommend especially his video about Hot and Cold herbs as a superb example of fantasy science.
Annie Anderson, is Professor of Public Health Nutrition and
Founder of the Scottish Cancer Prevention Network. She’s a respectable nutritionist and public health person, albeit with their customary disregard of problems of causality.
Patrick Holden is chair of the Sustainable Food Trust. He promotes "organic farming". Much though I dislike the cruelty of factory farms, the "organic" industry is largely a way of making food more expensive with no health benefits.
The Michael Pittilo 2016 Student Essay Prize was awarded after lunch. Pittilo has featured frequently on this blog as a result of his execrable promotion of quackery -see, in particular, A very bad report: gamma minus for the vice-chancellor.
Nutritional advice for patients with cancer. This discussion involved three people.
Professor Robert Thomas, Consultant Oncologist, Addenbrookes and Bedford Hospitals, Dr Clare Shaw, Consultant Dietitian, Royal Marsden Hospital and Dr Catherine Zollman, GP and Clinical Lead, Penny Brohn UK.
Robert Thomas came to my attention when I noticed that he, as a regular cancer consultant had spoken at a meeting of the quack charity, “YestoLife”. When I saw he was scheduled tp speak at another quack conference. After I’d written to him to point out the track records of some of the people at the meeting, he withdrew from one of them. See The exploitation of cancer patients is wicked. Carrot juice for lunch, then die destitute. The influence seems to have been temporary though. He continues to lend respectability to many dodgy meetings. He edits the Cancernet web site. This site lends credence to bizarre treatments like homeopathy and crystal healing. It used to sell hair mineral analysis, a well-known phony diagnostic method the main purpose of which is to sell you expensive “supplements”. They still sell the “Cancer Risk Nutritional Profile”. for £295.00, despite the fact that it provides no proven benefits.
Robert Thomas designed a food "supplement", Pomi-T: capsules that contain Pomegranate, Green tea, Broccoli and Curcumin. Oddly, he seems still to subscribe to the antioxidant myth. Even the supplement industry admits that that’s a lost cause, but that doesn’t stop its use in marketing. The one randomised trial of these pills for prostate cancer was inconclusive. Prostate Cancer UK says "We would not encourage any man with prostate cancer to start taking Pomi-T food supplements on the basis of this research". Nevertheless it’s promoted on Cancernet.co.uk and widely sold. The Pomi-T site boasts about the (inconclusive) trial, but says "Pomi-T® is not a medicinal product".
There was a cookery demonstration by Dale Pinnock "The medicinal chef" The programme does not tell us whether he made is signature dish "the Famous Flu Fighting Soup". Needless to say, there isn’t the slightest reason to believe that his soup has the slightest effect on flu.
In summary, the whole meeting was devoted to exaggerating vastly the effect of particular foods. It also acted as advertising for people with something to sell. Much of it was outright quackery, with a leavening of more respectable people, a standard part of the bait-and-switch methods used by all quacks in their attempts to make themselves sound respectable. I find it impossible to tell how much the participants actually believe what they say, and how much it’s a simple commercial drive.
The thing that really worries me is why someone like Phil Hammond supports this sort of thing by chairing their meetings (as he did for the "College of Medicine’s" direct predecessor, the Prince’s Foundation for Integrated Health. His defence of the NHS has made him something of a hero to me. He assured me that he’d asked people to stick to evidence. In that he clearly failed. I guess they must pay well.
Follow-up
|
“Statistical regression to the mean predicts that patients selected for abnormalcy will, on the average, tend to improve. We argue that most improvements attributed to the placebo effect are actually instances of statistical regression.”
“Thus, we urge caution in interpreting patient improvements as causal effects of our actions and should avoid the conceit of assuming that our personal presence has strong healing powers.” |
In 1955, Henry Beecher published "The Powerful Placebo". I was in my second undergraduate year when it appeared. And for many decades after that I took it literally, They looked at 15 studies and found that an average 35% of them got "satisfactory relief" when given a placebo. This number got embedded in pharmacological folk-lore. He also mentioned that the relief provided by placebo was greatest in patients who were most ill.
Consider the common experiment in which a new treatment is compared with a placebo, in a double-blind randomised controlled trial (RCT). It’s common to call the responses measured in the placebo group the placebo response. But that is very misleading, and here’s why.
The responses seen in the group of patients that are treated with placebo arise from two quite different processes. One is the genuine psychosomatic placebo effect. This effect gives genuine (though small) benefit to the patient. The other contribution comes from the get-better-anyway effect. This is a statistical artefact and it provides no benefit whatsoever to patients. There is now increasing evidence that the latter effect is much bigger than the former.
How can you distinguish between real placebo effects and get-better-anyway effect?
The only way to measure the size of genuine placebo effects is to compare in an RCT the effect of a dummy treatment with the effect of no treatment at all. Most trials don’t have a no-treatment arm, but enough do that estimates can be made. For example, a Cochrane review by Hróbjartsson & Gøtzsche (2010) looked at a wide variety of clinical conditions. Their conclusion was:
“We did not find that placebo interventions have important clinical effects in general. However, in certain settings placebo interventions can influence patient-reported outcomes, especially pain and nausea, though it is difficult to distinguish patient-reported effects of placebo from biased reporting.”
In some cases, the placebo effect is barely there at all. In a non-blind comparison of acupuncture and no acupuncture, the responses were essentially indistinguishable (despite what the authors and the journal said). See "Acupuncturists show that acupuncture doesn’t work, but conclude the opposite"
So the placebo effect, though a real phenomenon, seems to be quite small. In most cases it is so small that it would be barely perceptible to most patients. Most of the reason why so many people think that medicines work when they don’t isn’t a result of the placebo response, but it’s the result of a statistical artefact.
Regression to the mean is a potent source of deception
The get-better-anyway effect has a technical name, regression to the mean. It has been understood since Francis Galton described it in 1886 (see Senn, 2011 for the history). It is a statistical phenomenon, and it can be treated mathematically (see references, below). But when you think about it, it’s simply common sense.
You tend to go for treatment when your condition is bad, and when you are at your worst, then a bit later you’re likely to be better, The great biologist, Peter Medawar comments thus.
|
"If a person is (a) poorly, (b) receives treatment intended to make him better, and (c) gets better, then no power of reasoning known to medical science can convince him that it may not have been the treatment that restored his health"
(Medawar, P.B. (1969:19). The Art of the Soluble: Creativity and originality in science. Penguin Books: Harmondsworth). |
This is illustrated beautifully by measurements made by McGorry et al., (2001). Patients with low back pain recorded their pain (on a 10 point scale) every day for 5 months (they were allowed to take analgesics ad lib).
The results for four patients are shown in their Figure 2. On average they stay fairly constant over five months, but they fluctuate enormously, with different patterns for each patient. Painful episodes that last for 2 to 9 days are interspersed with periods of lower pain or none at all. It is very obvious that if these patients had gone for treatment at the peak of their pain, then a while later they would feel better, even if they were not actually treated. And if they had been treated, the treatment would have been declared a success, despite the fact that the patient derived no benefit whatsoever from it. This entirely artefactual benefit would be the biggest for the patients that fluctuate the most (e.g this in panels a and d of the Figure).

Figure 2 from McGorry et al, 2000. Examples of daily pain scores over a 6-month period for four participants. Note: Dashes of different lengths at the top of a figure designate an episode and its duration.
The effect is illustrated well by an analysis of 118 trials of treatments for non-specific low back pain (NSLBP), by Artus et al., (2010). The time course of pain (rated on a 100 point visual analogue pain scale) is shown in their Figure 2. There is a modest improvement in pain over a few weeks, but this happens regardless of what treatment is given, including no treatment whatsoever.
FIG. 2 Overall responses (VAS for pain) up to 52-week follow-up in each treatment arm of included trials. Each line represents a response line within each trial arm. Red: index treatment arm; Blue: active treatment arm; Green: usual care/waiting list/placebo arms. ____: pharmacological treatment; – – – -: non-pharmacological treatment; . . .. . .: mixed/other.
The authors comment
"symptoms seem to improve in a similar pattern in clinical trials following a wide variety of active as well as inactive treatments.", and "The common pattern of responses could, for a large part, be explained by the natural history of NSLBP".
In other words, none of the treatments work.
This paper was brought to my attention through the blog run by the excellent physiotherapist, Neil O’Connell. He comments
"If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery."
O’Connell has discussed the matter in recent paper, O’Connell (2015), from the point of view of manipulative therapies. That’s an area where there has been resistance to doing proper RCTs, with many people saying that it’s better to look at “real world” outcomes. This usually means that you look at how a patient changes after treatment. The hazards of this procedure are obvious from Artus et al.,Fig 2, above. It maximises the risk of being deceived by regression to the mean. As O’Connell commented
"Within-patient change in outcome might tell us how much an individual’s condition improved, but it does not tell us how much of this improvement was due to treatment."
In order to eliminate this effect it’s essential to do a proper RCT with control and treatment groups tested in parallel. When that’s done the control group shows the same regression to the mean as the treatment group. and any additional response in the latter can confidently attributed to the treatment. Anything short of that is whistling in the wind.
Needless to say, the suboptimal methods are most popular in areas where real effectiveness is small or non-existent. This, sad to say, includes low back pain. It also includes just about every treatment that comes under the heading of alternative medicine. Although these problems have been understood for over a century, it remains true that
|
"It is difficult to get a man to understand something, when his salary depends upon his not understanding it."
Upton Sinclair (1935) |
Responders and non-responders?
One excuse that’s commonly used when a treatment shows only a small effect in proper RCTs is to assert that the treatment actually has a good effect, but only in a subgroup of patients ("responders") while others don’t respond at all ("non-responders"). For example, this argument is often used in studies of anti-depressants and of manipulative therapies. And it’s universal in alternative medicine.
There’s a striking similarity between the narrative used by homeopaths and those who are struggling to treat depression. The pill may not work for many weeks. If the first sort of pill doesn’t work try another sort. You may get worse before you get better. One is reminded, inexorably, of Voltaire’s aphorism "The art of medicine consists in amusing the patient while nature cures the disease".
There is only a handful of cases in which a clear distinction can be made between responders and non-responders. Most often what’s observed is a smear of different responses to the same treatment -and the greater the variability, the greater is the chance of being deceived by regression to the mean.
For example, Thase et al., (2011) looked at responses to escitalopram, an SSRI antidepressant. They attempted to divide patients into responders and non-responders. An example (Fig 1a in their paper) is shown.

The evidence for such a bimodal distribution is certainly very far from obvious. The observations are just smeared out. Nonetheless, the authors conclude
"Our findings indicate that what appears to be a modest effect in the grouped data – on the boundary of clinical significance, as suggested above – is actually a very large effect for a subset of patients who benefited more from escitalopram than from placebo treatment. "
I guess that interpretation could be right, but it seems more likely to be a marketing tool. Before you read the paper, check the authors’ conflicts of interest.
The bottom line is that analyses that divide patients into responders and non-responders are reliable only if that can be done before the trial starts. Retrospective analyses are unreliable and unconvincing.
Some more reading
Senn, 2011 provides an excellent introduction (and some interesting history). The subtitle is
"Here Stephen Senn examines one of Galton’s most important statistical legacies – one that is at once so trivial that it is blindingly obvious, and so deep that many scientists spend their whole career being fooled by it."
The examples in this paper are extended in Senn (2009), “Three things that every medical writer should know about statistics”. The three things are regression to the mean, the error of the transposed conditional and individual response.
You can read slightly more technical accounts of regression to the mean in McDonald & Mazzuca (1983) "How much of the placebo effect is statistical regression" (two quotations from this paper opened this post), and in Stephen Senn (2015) "Mastering variation: variance components and personalised medicine". In 1988 Senn published some corrections to the maths in McDonald (1983).
The trials that were used by Hróbjartsson & Gøtzsche (2010) to investigate the comparison between placebo and no treatment were looked at again by Howick et al., (2013), who found that in many of them the difference between treatment and placebo was also small. Most of the treatments did not work very well.
Regression to the mean is not just a medical deceiver: it’s everywhere
Although this post has concentrated on deception in medicine, it’s worth noting that the phenomenon of regression to the mean can cause wrong inferences in almost any area where you look at change from baseline. A classical example concern concerns the effectiveness of speed cameras. They tend to be installed after a spate of accidents, and if the accident rate is particularly high in one year it is likely to be lower the next year, regardless of whether a camera had been installed or not. To find the true reduction in accidents caused by installation of speed cameras, you would need to choose several similar sites and allocate them at random to have a camera or no camera. As in clinical trials. looking at the change from baseline can be very deceptive.
Statistical postscript
Lastly, remember that it you avoid all of these hazards of interpretation, and your test of significance gives P = 0.047. that does not mean you have discovered something. There is still a risk of at least 30% that your ‘positive’ result is a false positive. This is explained in Colquhoun (2014),"An investigation of the false discovery rate and the misinterpretation of p-values". I’ve suggested that one way to solve this problem is to use different words to describe P values: something like this.
|
P > 0.05 very weak evidence
P = 0.05 weak evidence: worth another look P = 0.01 moderate evidence for a real effect P = 0.001 strong evidence for real effect |
But notice that if your hypothesis is implausible, even these criteria are too weak. For example, if the treatment and placebo are identical (as would be the case if the treatment were a homeopathic pill) then it follows that 100% of positive tests are false positives.
Follow-up
12 December 2015
It’s worth mentioning that the question of responders versus non-responders is closely-related to the classical topic of bioassays that use quantal responses. In that field it was assumed that each participant had an individual effective dose (IED). That’s reasonable for the old-fashioned LD50 toxicity test: every animal will die after a sufficiently big dose. It’s less obviously right for ED50 (effective dose in 50% of individuals). The distribution of IEDs is critical, but it has very rarely been determined. The cumulative form of this distribution is what determines the shape of the dose-response curve for fraction of responders as a function of dose. Linearisation of this curve, by means of the probit transformation used to be a staple of biological assay. This topic is discussed in Chapter 10 of Lectures on Biostatistics. And you can read some of the history on my blog about Some pharmacological history: an exam from 1959.
This post was written for the Spectator Health section, at short notice after the release of the spider letters. The following version is almost the same as appeared there, with a few updates. Some of the later sections are self-plagiarised from earlier posts.

Picture: Getty
The age of enlightenment was a beautiful thing. People cast aside dogma and authority. They started to think for themselves. Natural science flourished. Understanding of the natural world increased. The hegemony of religion slowly declined. Eventually real universities were created and real democracy developed. The modern world was born.
People like Francis Bacon, Voltaire and Isaac Newton changed the world for the better. Well, that’s what most people think. But not Charles, Prince of Wales and Duke of Cornwall.
In 2010 he said
"I was accused once of being the enemy of the Enlightenment,” he told a conference at St James’s Palace. “I felt proud of that.” “I thought, ‘Hang on a moment’. The Enlightenment started over 200 years ago. It might be time to think again and review it and question whether it is really effective in today’s conditions."
It seems that the Prince preferred things as they were before 1650. That’s a remarkable point of view for someone who, if he succeeds, will become the patron of that product of the age of enlightenment, the Royal Society, a venture that got its Royal Charter from King Charles II in1622.
I suppose that the Prince cannot be blamed for his poor education. He may have been at Trinity College Cambridge, his 2.2 degree is the current euphemism for a fail (it seems that he even failed to learn the dates of the enlightenment).
His behaviour has brought to the fore the question of the role of the monarchy.
A constitutional monarch is purely ceremonial and plays no part in politics. Well actually in the UK it isn’t quite as simple as that. The first problem is that we have no constitution. Things haven’t changed much since the 19th century when Walter Bagehot said “the Sovereign has, under a constitutional monarchy… three rights—the right to be consulted, the right to encourage, the right to warn.”.
These are real powers in a country which is meant to be run by elected representatives. But nobody knows how these powers are used: it is all done in secret. Well, almost all. The Prince of Wales has been unusually public in expressing his views. His views bear directly on government policy in many areas: medicine, architecture, agriculture and the environment. These are mostly areas that involve at least an elementary knowledge of science. But that is something that he lacks. Worse still, he seems to have no consciousness of his ignorance.
The Royal family should clearly have no influence whatsoever on government policies in a democracy. And they should be seen to have no influence. The Queen is often praised for her neutrality, but the fact is that nobody has the slightest idea what happens at the weekly meetings between the Prime Minister and the Queen. I doubt that she advises the prime minister to create a National Health Service, or to tax the rich. We shall never know that. We should do.
Almost the only light that has been thrown on the secret activities of Charles was the release, on 13 May, of 27 letters that the Prince wrote to government ministers in the Blair government between 2004 and 2005. It has take 10 years of effort by the Guardian to get hold of the letters. It was ike getting blood from a stone. When the Information Commissioner ruled that the letters should be made public, the decision was vetoed by the Conservative attorney general, Dominic Grieve. He said. of the "particularly frank" letters,
" Disclosure of the correspondence could damage The Prince of Wales’ ability to perform his duties when he becomes King."
That, of course, is precisely why the documents should be revealed.
If Charles’ ability to perform his duty as King is damaged, should his subjects be kept unaware of that fact? Of course not.
In this case, the law prevailed over the attorney general. After passing through the hands of 16 different judges, the Supreme Court eventually ruled, in March, that the government’s attempts to block release were unlawful. The government spent over £400,000 in trying, and failing, to conceal what we should know. The Freedom of Information Act (2000) is the best thing that Tony Blair did, though he, and Jack Straw, thought it was the worst. I expect they are afraid of what it might reveal about their own records. Transparency is not favoured by governments of any hue.
What do the letters say?
You can read all the letters on the Guardian web site. They give the impression of being written by a rather cranky old man with bees in his bonnet and too much time on his hands. The problem is that not all cranky old men can write directly to the prime minister, and get an answer.
Not all the letters are wrong headed. But all attempt to change government policy. They represent a direct interference in the political process by the heir to the throne. That is unacceptable in a democracy. It disqualifies him from becoming king.
Some letters verged on the bizarre.
|
21 October 2004 I particularly hope that the illegal fishing of the Patagonian Toothfish will be high on your list of priorities because until the trade is stopped, there is little hope for the poor old albatross. |
No doubt illegal fishing is a problem, but not many people would write directly to a minister about the Patagonian Toothfish.
Others I agree with. But they are still attempts to influence the policies of the elected government. This one was about the fact that supermarkets pay so little to dairy farmers for milk that sometimes it’s cheaper than bottled water.
|
To Tony Blair 8 September 2004 ". . . unless United Kingdom co-operatives can grow sufficiently the processors and retailers will continue to have the farmers in an arm lock and we will continue to shoot ourselves in the foot! You did kindly say that you would look at this . . . ". Yours ever, Charles |
He wrote to the minister of education to try to influence education policy.
|
22 February 2005 "I understand from your predecessor, Charles Clarke, that he has spoken to you about my most recent letter of 24th November, and specifically about the impact of my Education Summer School for teachers of English and History. This Programme, which involves up to ninety state school teachers each year, has been held over the past three years in Dartington, Devon, at Dunston, in Norfolk and at Buxton, in Derbyshire. I believe that they have added fresh inspiration to the national debate about the importance of English Literature and History in schools." Despite having made substantial progress, as you may be aware I remain convinced that the correct approaches to teaching and learning need to be challenged |
It’s interesting that the meeting was in Dartington. That’s near Totnes ("twinned with Narnia") and it’s a centre for the bizarre educational cult promoted by the mystic and racist, Rudolf Steiner.
Then we get a reference to one of Charles’ most bizarre beliefs, alternative medicine.
|
24 February 2005 Dear Prime Minister, We briefly mentioned the European Union Directive on Herbal Medicines, which is having such a deleterious effect on complementary medicine sector in this country by effectively outlawing the use of certain herbal extracts. I think we both agreed this was using a sledgehammer to crack a nut. You rightly asked me what could be done about it and I am asking the Chief Executive of my Foundation for Integrated Health to provide a more detailed briefing which I hope to be able to send shortly so that your advisers can look at it. Meanwhile, I have given Martin Hurst a note suggesting someone he could talk to who runs the Herbal Practitioner’s Association. Yours ever, Charles |
In this he opposes the EU Directive on Herbal Medicines. All this directive did was to insist that there was some anecdotal evidence for the safety of things that are sold to you. It asked for no evidence at all that they work, and it allowed very misleading labels. It provided the weakest form of protection from the deluded and charlatans. It was put into effect in the UK by the Medicines and Healthcare Products Regulatory Authority (MHRA). They even allowed products that were registered under this scheme to display an impressive-looking “kite-mark”. Most people would interpret this as a government endorsement of herbal medicines.
This got a sympathetic response from Tony Blair, someone who, along with his wife, was notoriously sympathetic to magic medicine.
|
30 March 2005 Dear Prince Charles Thanks too for your contacts on herbal medicines who have been sensible and constructive. They feel that the directive itself is sound and the UK regulators excellent, but are absolutely correct in saying that the implementation as it is currently planned is crazy. We can do quite a lot here: we will delay implementation for all existing products to 2011; we will take more of the implementation upon ourselves; and I think we can sort out the problems in the technical committee – where my European experts have some very good ideas. We will be consulting with your contacts and others on the best way to do this we simply cannot have burdensome regulation here. Yours ever, Tony |
Note "absolutely correct in saying that the implementation as it is currently planned is crazy. We can do quite a lot here: we will delay implementation for all existing products to 2011".
Government support for acupuncture and herbal medicine was made explicit in a letter from Health Secretary, John Reid (February 2005). He assures the prince that government is taking action to "enhance the status of the herbal medicine and acupuncture professions".

Nothing could reveal more clearly the clueless attitude of the then government to quackery. In fact, after 15 years of wrangling, the promised recognition of herbalism by statutory regulation never happened. One is reminded of the time that an equally-clueless minister, Lord (Phillip) Hunt, referred to ‘psychic surgery’ as a “profession”.
We got a preview of the Prince’s letters a month before the release when Max Hastings wrote in the Spectator
I have beside me a copy of a letter allegedly written by him some years ago to a cultural institution, asserting the conviction that ‘there is a DIVINE Source which is ultimate TRUTH… that this Truth can be expressed by means of numbers… and that, if followed correctly, these principles can be expressed with infinite variety to produce Beauty’.
You can’t get much barmier than that.
Are the letters harmless?
That has been the reaction on the BBC. I can’t agree. In one sense they so trivial that it’s amazing that the government thought it was a good use of £400,000 to conceal them. But they are all the evidence that we’ll get of the Prince’s very direct attempts to influence the political process.
The Prince of Wales is more than just a crank. He has done real harm. Here are some examples.
When the generally admirable NHS Choices re-wrote their advice on homeopathy (the medicines that contain no medicine) the new advice took two years to appear. It was held up in the Department of Health while consultations were made with the Prince’s Foundation for Integrated Health. That’s Charles’ lobby organisation for crackpot medicine. (The word "integrated" is the euphemism for alternative medicine that’s in favour with its advocates.) If it were not for the fact that I used the Freedom of Information Act to find out what was going on, the public would have been given bad advice as a direct result of the Prince’s political interference.
The Prince’s Foundation for Integrated Health (FIH) folded in 2010 as a result of a financial scandal, but it was quickly reincarnated as the "College of Medicine". It was originally going to be named the College of Integrated Medicine, but it was soon decided that this sounded too much like quackery, so it was given the deceptive name, College of Medicine. It appears to be financed by well-known outsourcing company Capita. It’s closely connected with Dr Michael Dixon, who was medical advisor to the FIH, and who tried to derail the advice given by NHS Choices.
Perhaps the worst example of interference by the Prince of Wales, was his attempt to get an academic fired. Prof Edzard Ernst is the UK’s foremost expert on alternative medicine. He has examined with meticulous care the evidence for many sorts of alternative medicine.Unfortunately for its advocates, it turned out that there is very little evidence that any of it works. This attention to evidence annoyed the Prince, and a letter was sent from Clarence House to Ernst’s boss, the vice-chancellor of the University of Exeter, Steve Smith. Shamefully, Smith didn’t tell the prince to mind his ow business, but instead subjected Ernst to disciplinary proceedings, After subjecting him to a year of misery, he was let off with a condescending warning letter, but Ernst was forced to retire early. In 2011and the vice-chancellor was rewarded with a knighthood. His university has lost an honest scientist but continues to employ quacks.
Not just interfering but costing taxpayers’ money
The Prince’s influence seems to be big in the Department of Health (DH). He was given £37,000 of taxpayers’ money to produce his Patients’ Guide (I produced a better version for nothing). And he was paid an astonishing £900,000 by DH to prepare the ground for the setting up of the hapless self-regulator, the Complementary and Natural Healthcare Council (CNHC, also known as Ofquack).
The Prince of Wales’ business, Duchy Originals, has been condemned by the Daily Mail, (of all places) for selling unhealthy foods. And when his business branched into selling quack “detox” and herbal nonsense he found himself censured by both the MHRA and the Advertising Standards Authority (ASA) for making unjustifiable medical claims for these products.
It runs in the family
The Prince of Wales is not the only member of the royal family to be obsessed with bizarre forms of medicine. The first homeopath to the British royal family, Frederick Quin, was a son of the Duchess of Devonshire (1765-1824). Queen Mary (1865-1953), wife of King George V, headed the fundraising efforts to move and expand the London Homeopathic Hospital. King George VI was so enthusiastic that in 1948 he conferred the royal title on the London Homeopathic Hospital.
The Queen Mother loved homeopathy too (there is no way to tell whether this contributed to her need for a colostomy in the 1960s).
The present Queen’s homeopathic physician is Peter Fisher, who is medical director of what, until recently was called the Royal London Homeopathic Hospital (RLHH). In 2010 that hospital was rebranded as the Royal London Hospital for Integrated medicine (RLHIM) in another unsubtle bait and switch move.
The RLHIM is a great embarrassment to the otherwise excellent UCLH Trust. It has been repeatedly condemned by the Advertising Standards Authority for making false claims. As a consequence, it has been forced to withdraw all of its patient information.
The patron of the RLHIM is the Queen, not the Prince of Wales. It is hard to imagine that this anachronistic institution would still exist if it were not for the influence, spoken or unspoken, of the Queen. Needless to say we will never be told.
The royal warrant for a firm that sells "meningitis vaccine" that contains nothing
Ainsworth’s homeopathic pharmacy is endorsed by both Prince Charles and the Queen: it has two Royal Warrants, one from each of them. They sell “homeopathic vaccines” for meningitis, measles, rubella and whooping cough. These “vaccines” contain nothing whatsoever so they are obviously a real danger to public health.
Despite the fact that Ainsworth’s had already been censured by the ASA in 2011 for selling similar products, Ainsworth’s continued to recommend them with a “casual disregard for the law”.
The regulator (the MHRA) failed to step in to stop them until it was eventually stirred into action by a young BBC reporter, Sam Smith who made a programme for BBC South West. Then, at last, the somnolent regulator was stirred into action. The MHRA “told Ainsworths to stop advertising a number of products” (but apparently not to stop making them or selling them).
They still sell Polonium metal 30C and Swine Meningitis 36C, and a booklet that recommends homeopathic “vaccination”.
Ainsworth’s sales are no doubt helped by the Royal Warrants. The consequence is that people may die of meningitis. In 2011, the MHRA Chief Executive Professor Kent Woods, was knighted. It was commented, justly, that
"Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator "
But the regulator has to fight the political influence of the Queen and Prince Charles. They lost.
The attorney general, while trying to justify the secrecy of Charles’ letters, said
“It is a matter of the highest importance within our constitutional framework that the Monarch is a politically neutral figure”.
Questions about health policy are undoubtedly political, and the highly partisan interventions of the Prince in the political process make his behaviour unconstitutional.
The Prince’s petulant outbursts not only endanger patients. They endanger the monarchy itself. Whether that matters depends on how much you value the tourist business generated by the Gilbert & Sullivan flummery at which royals excel.
The least that one can ask of the royal family is that they should not endanger the health of the nation. It would help if they refrained from using their influence on matters that are beyond their intellectual grasp..
If I wanted to know the winner of the 2.30 at Ascot, I’d ask a royal. For any other question I’d ask someone with more education.
Follow-up
The letters have made headlines in just about every newspaper. The Guardian had extensive coverage, of course.
The Times had a front page story "Revealed: how Charles got Blair to alter health policy" [pdf]
The British Medical Journal wrote "Prince Charles delayed regulation of herbal medicines" [pdf]
For me, the most shocking item was an interview given by Jack Straw, on Radio 4’s Today Programme. He was Home Secretary from 1997 to 2001 and Foreign Secretary from 2001 to 2006 under Tony Blair. From 2007 to 2010 he was Lord Chancellor. His response to the letters sounded like that of a right-wing conservative.
Like Blair. he deplored the Freedom of Information Act that his own government passed. He defended the secrecy, and supported the Conservative attorney-general’s attempt to veto the release of the letters. Perhaps his defence of secrecy is not surprising, He has a lot to hide, His involvement in the mendacity that led to the Iraq war, the dodgy dossier, his role in covering up torture (the "rendition" scandal). And He was suspended by the Labour party in February 2015 due to allegation of cash bribes.
He is certainly a man with plenty of things to hide.
|
Maurice Nathan Saatchi, Baron Saatchi is an advertising man who, with his brother, Charles Saatchi ("‘why tell the truth when a good lie will do?), became very rich by advertising cigarettes and the Conservative party. After his second wife died of cancer he introduced a private members bill in the House of Lords in 2012. The Medical Innovation Bill came back to the Lords for its second reading on 24 October 2014. |
 |
The debate was deeply depressing: very pompous and mostly totally uninformed. You would never have guessed that the vast majority of those who understand the problem are against the bill. The Bill has failed to win the support of The British Medical Association, The Motor Neurone Disease Association, the Royal College of Physicians, the Royal College of Surgeons, the Medical Research Society, the Royal College of Radiologists, The Medical Defence Union, the Academy of Medical Sciences, the Royal College of Pathologists, the Royal College of General Practitioners, the Academy for Healthcare Science, the Wellcome Trust, Action Against Medical Accidents, and patient advocacy charities Health Watch and the Nightingale Collaboration, and others. Conservative MP Sarah Wollaston, a former GP, has “very serious concerns” about it.
Grief is not a good basis for legislation. In the Daily Telegraph, Lord Saatchi attributes the lack of a "cure for cancer" to fear of litigation.
“Any deviation by a doctor is likely to result in a verdict of guilt for medical negligence. The law defines medical negligence as deviation from that standard procedure. But as innovation is deviation, non-deviation is non-innovation. This is why there is no cure for cancer.”
This statement is utterly bizarre. Evidently Lord Saatchi knows much more about how to sell cigarettes than he does about how to discover new drugs. The reason there is no cure is that it’s a very difficult problem. It has nothing to do with litigation
Almost every medical organisation, and many lawyers, have pointed out the flaws in his ideas,. But slick, and often mendacious, advertising of his cure has deceived many of our scientifically-illiterate parliamentarians, and the bill is making progress
Lord Saatchi’s Bill would allow uncontrolled testing of treatments on any patient. It is not limited to cancer, nor to terminally ill patients (though some amendments, yet to be accepted, might change that). This sort of uncontrolled experimentation is likely to impede advances in treatment rather than to help them. And the vagueness of the wording of the bill could lead to an increase in litigation, rather than the intended decrease.
It is no coincidence that the legion of cancer quacks is in favour of the bill. It opens the door to their nonsense. Big pharma is likely to benefit too, because they will be able to sell improperly tested drugs with little or no effectiveness and immunity from prosecution if they do harm.
For more information about the Bill, see the excellent site, Stop the Saatchi Bill. There are sections on Dispelling Myths, on Professional Concerns, and on the many good articles and blogs that have pointed out the many problems with the bill.
Two recent articles are well worth reading
Saatchi’s ‘Medical Innovation Bill’ will benefit lawyers and charlatans, not patients, by neurologist David Nicholl. And it’s particularly interesting that the Telegraph’s arch-conservative, Peter Oborne has come out strongly against the bill, in The ‘Saatchi Bill’ is dangerous and will bring nothing but harm. I can’t agree with his opening words ("Lord Saatchi is rightly regarded as a national treasure. In his early days he was the advertising genius who played a fundamental role in selling the Thatcherite message"), but I agree entirely with
“The PR campaign distorts the facts, exploiting ignorance and desperation to plant false hope in the rich soil of multiple fallacies.”
“Quacks will be given free rein. No “treatment” is so loopy (or potentially dangerous) that the Saatchi Bill won’t protect doctors who prescribe or administer it from prosecution.”
“The propagation of falsehoods and fallacies surrounding and arising from this Bill will have a corrosive effect on medical ethics and society as a whole.”
Lord Saatchi, who proposed the bill said “To prevent more needless cancer deaths, doctors must be free to innovate”. This statement shows he has no idea of the efforts that go into cancer research. We are doing our best, but it is a very hard problem. In some areas (like breast cancer) there have been big advances. In others areas (e.g. pancreatic or ovarian cancer) there has not yet been any perceptible progress. It will take many more years of hard scientific work. Individual doctors tinkering with speculative untested treatments will not solve the problem.
- The only people who will benefit from the bill will be lawyers, quacks and big pharma.
- “Innovation” is undefined –the bill is based on the myth that there exists a miraculous cure waiting to be found. Sadly, the probability of this happening is vanishingly small.
- To some extent, medicine is victim of its own hype. The public feels it has a right to demand the latest miracle cure. Too often, they don’t exist.
- There is no need for the bill because doctors can already prescribe whatever they want. The Medical Defence Union says it has no reason to think that doctors are deterred from innovating by the fear of litigation.
- The bill won’t help to discover new cures –in fact it is more likely to hinder it, especially if it deters people from joining properly organised clinical trials. The bill will generate many separate anecdotes which may or may not be published. That’s the worst possible way to do research.
- The bill removes protections from patients and is more likely to increase litigation than reduce it.
- Anyone unlucky enough to get cancer is immediately a target for a legion of quacks trying to sell you crazy “treatments”. There is nothing to stop even the lunatic fringe of alternative medicine, homeopaths, promoting their sugar pills. There are, disgracefully, several hundred homeopaths with medical degrees –all a quack has to do is to ask another quack doctor to endorse their daft ideas.
- For untested treatments there is, by definition, no reason to think they’ll do more good than harm. The cancer surgeon, Michael Baum said, rightly, that in cases of terminal cancer "there will be many patients we can’t help. but none we can’t harm".
As a result of tweeting about the bill, I got a call on 21 October from RT TV (UK) asking me speak on the Saatchi Bill. That was a pleasure. Here it is (done from home, on Skype).
And on the day of the Lords debate (24 October 2014) I was asked to talk again about the Saatchi Bill, on the flagship Radio 4 morning news programme, Today. It was only a 3 minute interview with Mishal Husain, but it was unopposed so I managed to get in the main points.
![]() Click to play interview
Click to play interview
This is the Today Programme studio.

The BBC doesn’t pay you, but it’s good at driving you to/from the studio, though the cars are unnecessarily posh. On the way home, I had my first ever ride in an all-electric Tesla. It does 0 – 60 in 4.2 seconds but costs £50k -more than twice the price of a Prius.

|

|
Follow-up
25 October 2014 A summary of the misunderstandings in yesterday’s House of Lords debate: What the Lords Missed.

The General Pharmaceutical Council (GPhC) has been the statutory body responsible for the regulation of pharmacy since 2010. It’s status is similar to that of the GMC and. heaven help us, the GCC. Before that the regulator was the same as the professional body, the Royal Pharmaceutical Society of Great Britain (RPS). The RPS proved to be as useless as most other regulators, as documented in detail in my 2008 post, At around the time it stopped being a regulator, the RPS started to condemn quackery more effectively, but by then it had lost the power to do much about it (I hope the latter wasn’t the cause of the former). The body that could do something, the GPhC has done essentially nothing. as described in this post.
I did a 2 year apprenticeship in Timothy White’s and Taylor’s Homeopathic (yes, really) Chemists in the 1950s.
My first degree was in pharmacy. I got my interest in pharmacology from reading Martindale’s Extra Pharmacopoeia in the shop. I soon decided that I didn’t really want to spend the rest of my life selling lipstick and Durex. The latter was quite a big seller because the Boots across the road didn’t sell contraceptives (they changed their minds in the 1960s).
In those days, we spent quite a lot of time making up (almost entirely ineffective) ‘tonics’ and ‘cough mixtures’. Now the job consists largely of counting pills. This has exacerbated the ‘chip on the shoulder’ attitude that was present even in the 1950s. For a long time now, pharmacists have wanted to become the a ‘third tier’ in the NHS, alongside GP practices and hospitals., after hospitals and doctors". . Here are a few comments on this proposition.
First let me say that I’ve met some very good and ethical pharmacists. I did a vacation job in a hospital pharmacy where the boss had an encyclopaedic knowledge of the effects and side effects of drugs, and of their dosage. His advice was often sought by doctors, and rightly so. He had no way of knowing at the time that his advice to replace barbiturates with thalidomide would lead to such a tragedy, because the evidence had been concealed by the manufacturer. Some of the problems alluded to here have already been highlighted by two excellent pharmacists, Anthony Cox and @SparkleWildfire, neither of whom work in pharmacists shops. They are absolutely spot on but they seem to be in a minority among pharmacists.
The problems seem to lie mostly in retail shops. Their shelves are laden with ineffective pills and potions. And the pharmacist has every incentive to sell them. His/her income depends on it directly if it’s a privately owned pharmacy. And his/her standing with head office depends on it in chain store pharmacies. This conflict of financial interest is the prime reason why pharmacists are not qualified to form a third tier of healthcare. The avoidance of conflicts of interest among doctors was one of the great accomplishments of the NHS. In the USA there are huge scandals when, as happens repeatedly, doctors order expensive and unnecessary treatments from which they profit. It’s no consolation that such problems are creeping back in the UK as a result of the government’s vigorous efforts to sell it off.
Here are few examples of things that have gone wrong, and who is to blame. Then I’ll consider what can be done.
Ineffective medicines
In any pharmacy you can see ineffective ‘tonics’ and ‘cough medicines’, unnecessary supplements with dishonest claims and even, heaven help us, the ultimate scam, homeopathic pills.
What’s worse, if you ask a pharmacist for advice, it’s quite likely that they’ll recommend you to buy them.
|
I was amazed to discover that a number of old-fashioned ‘tonics’ and ‘cough medicines’ still have full marketing authorisation. That’s the fault of the Medicines and Healthcare Regulatory Auhority (MHRA) who are supposed to assess efficacy and totally failed to do so, Read about that in “Some medicines that don’t work. Why doesn’t the MHRA tell us honestly?” . It’s hard to blame a pharmacist for the bad advice given by the MHRA, but a good one would tell patients to save their money. |
|
Big corporate pharmacies
Companies like Boots seem to have no interest whatsoever in ethical behaviour. All that matters is sales. They provide “(mis)educational” materials that promote nonsense They advertise ridiculous made-up claims in the newspapers, which get shot down regularly by the Advertising Standards Authority, but by that time the promotion is over so they don’t give a damn. See for example, CoQ10 scam and the ASA verdict on it. And "Lactium: more rubbish from Boots the Chemists. And a more serious problem". And "The Vitamin B scam. Don’t trust Boots"
Recently the consumer magazine Which? checked 122 High Street pharmacies. They got unsatisfactory advice from 43% of them, a disastrously bad performance for people who want to be the third tier of healthcare.
|
Even that’s probably better than my own experience. Recently, when I asked a Sainsbury’s pharmacist about a herbal treatment for prostate problems, he pointed to the MHRA’s kite mark and said it must work because the MHRA approved it -he was quite unaware that you get the THR kite mark without having to present any evidence at all about efficacy. |

|
Of course that is partly the fault of the MHRA for allowing misleading labels, but nevertheless, he should have known. See “Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me” for more on how the MHRA has betrayed its own standards.
When I’ve asked Boots’ pharmacists advice about persistent diarrhoea in an infant, saying I wanted a natural remedy, I’ve usually been guided to the homeopathic display. Only once was I told firmly that I should use rehydration not homeopathy (something every good parent knows) and when I asked that good pharmacist where she’d been educated, she said in Germany (mildly surprising given the amount of junk available in German pharmacies)
Regulators
Anthony Cox, a pharmacist who has been consistently on the side of right, says
"This is something that needs to be dealt with at a regulatory and professional body by the whole profession, and I am certain we have the majority of the UK pharmacy profession on side."
But the regulator has done nothing, and it isn’t even clear that there is a majority on his side.
At a 2009 meeting of Branch Representatives of the RPS a motion was proposed:
“…registration as a pharmacist and practice as a homeopath are not compatible, and that premises registered with the Society should not be used for the promotion of homeopathy”
Although that is obviously sensible to most people, the proposal was followed by a speaker from Leicester who thought it right to keep an open mind about Avogadro’s number and the motion was defeated. So much for the "scientists on the High Street" aspiration.
There have been two major scandals surrounding homeopathy recently. Both were revealed first by bloggers, and both came to wide notice through television programs. None were noticed by the regulators, and when they were brought to the attention of the regulator, nothing effective was done.
The malaria scandal
A lot has been wriitten about this here and on other blogs e.g. here and here. The idea that sugar pills can prevent or cure malaria is so mind-bogglingly dangerous that it was condemned by the Queen’s Homeopathic Physician, Peter Fisher. It was exposed on a BBC Newsnight programme in 2006. Watch the video.
The Gentle Art of Homeopathic Killing was an article that originally appeared on the excellent Quackometer blog produced by Andy Lewis. "The Society of Homeopaths were so outraged about one of their members flouting the code of ethics so blatantly that they took immediate action. That action was, as expected, not to do anything about the ethics breach but to threaten Andy and his hosting ISP with legal action for defamation. The article is reproduced here as a public service".
Some of the people involved in this bad advice were pharmacists, Very properly they were referred to the RPS in 2006 qnd 2009, the regulator at that time. They sat on the complaint so long that eventually the RPS was replaced by the GPhC as regulator. Nothing much has happened.
The GPhC did precisely nothing. Read their pathetic response.
Homeopathy for meningitis
An equally murderous fraud, "homeopathic vaccines" by Ainsworth’s has long been targeted by bloggers. In January 2013, Samantha Smith made an excellent BBC South West programme about it. Watch it and get angry.
Anthony Pinkus, pharmacist at Ainsworths, has been referred to the then regulator, the RPS, in 2006 and 2009. It’s said that he took "remedial action", though there is little obvious change judged by the video above. No doubt some of the most incriminating stuff has been removed from his web site to hide it from the ASA. It’s safer to mislead people by word of mouth. Since the last video more complaints have been made to the GPhC. So far, nothing but silence.
Why doesn’t the regulator regulate?
This pamphlet is reproduced from the July 2011 Quackometer post, “Ainsworths Pharmacy: Casual Disregard for the Law“
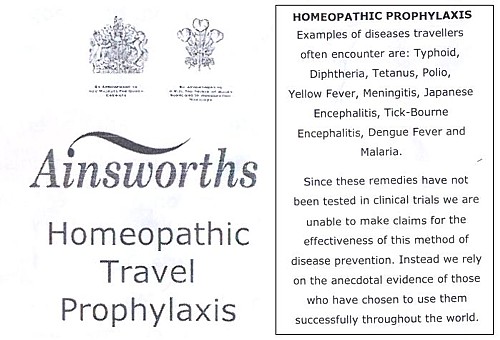
|
It’s almost as though those royal warrants, enlarged on right, acted as a talisman that puts this dangerous company outside the grasp of regulators. I hope that the GPhC Council , and Duncan Rudkin (its chief executive and registrar), are not so worried about their knighthoods that they won’t risk upsetting the royal family, just to save patients from malaria and meningitis. Their CEO, Robert Nicholls is only a CBE so far. |
|
Another reason for their inaction might be that the GPhC Council members, and Duncan Rudkin (its chief executive and registrar), lack critical faculties. Perhaps they have not been very well educated? Many of them aren’t even pharmacists, but that curious breed of professional administrators who inhabit the vast number of quangos, tick their boxes and do harm. Or perhaps they are just more interested in protecting the income of pharmacists than in protecting their customers?
Education
The solution to most problems is education. But there is no real knowledge of how many pharmacists in the UK are educated in the critical assessment of evidence. A recent paper from the USA did not give cause for optimism. It’s discussed by the excellent US pharmacist, Scott Gavura, at Science-based medicine. The results are truly horrifying.
“Few students disagreed with any CAM therapy. There was the greatest support for vitamins and minerals (94%, mean 4.29) which could include the science-based use these products. But there was strong support for demonstrably ineffective treatments like acupuncture, with 64% agreeing it was acceptable. Even homeopathy, which any pharmacy student with basic medicinal chemistry skills ought to know is absurd, was supported by over 40% of students.”
If the numbers are similar in the UK, the results of the Which? magazine survey are not so surprising. And if they are held by the GPhC Council. their inaction is to be expected. We just don’t know, and perhaps someone should find out.
I suspect that sympathy for quackery may sometimes creep in through that old-fashioned discipline known as pharmacognosy. It is about the botany of medicinal plants, and it’s still taught, despite the fact that very few drugs are now extracted from plants. At times, it gets dangerously close to herbalism. For example, at the School of Pharmacy (now part of UCL) a book is used Fundamentals of Pharmacognosy and Phytotherapy by Michael Heinrich, Joanne Barnes, Simon Gibbons and Elizabeth M. Williamson, ot the Centre for Pharmacognosy and Phytotherapy at the School of Pharmacy. The introductory chapter says.
“TRADITIONAL CHINESE MEDICINE (TCM) The study of TCM is a mixture of myth and fact, stretching back well over 5000 years. At the time, none of the knowledge was written down, apart from primitive inscriptions of prayers for the sick on pieces of tortoise carapace and animal bones, so a mixture of superstition, symbolism and fact was passed down by word of mouth for centuries. TCM still contains very many remedies, which were selected by their symbolic significance rather than proven effects; however, this does not necessarily mean that they are all ‘quack’ remedies!”
Well, not necessarily. But as in most such books, there are good descriptions of the botany, more or less good accounts of the chemical constituents followed by uncritical lists of things that the herb might (or might not) do. The fact that even the US National Institutes of Health quackery branch, NCCAM, doesn’t claim that a single herbal treatment is useful tells you all you need to know.
Joanna Barnes is Associate Professor in Herbal Medicines, School of Pharmacy, University of Auckland, New Zealand. She has written a book, Herbal Medicines (“A useful book for learning holistic medicine”) that is desperately uncritical about the alleged theraputic effectiveness of plants. ("Simon Gibbons is on the editorial board of The Chinese Journal of Natural Medicine. Elizabeth Williamson is editor of the Journal of Phytotherapy Research, a journal that has a strong flavour of herbalism (take the infamous snoring remedy). These people aren’t quacks but they are dangerously tolerant of quacks.
The warning is in the title. "Phytotherapy" is the current euphemism for herbalism. It’s one of those red light words that tells you that what follows is unlikely to be critical. Exeter’s fantasy herbalist, Simon Mills, now describes himself as a phytotherapist. What more warning could you need?
Perhaps this explains why so many pharmacists are unworried by selling things that don’t work. Pharmacy education seems not to include much about the critical assessment of evidence. It should do.
Chemist and Druggist magazine certainly doesn’t help. It continually reinforces the idea that there is a debate about homepathy. There isn’t. And in one of its CPD modules Katherine Gascoigne says
"Homeopathic remedies are available, but are best prescribed by a homeopath"
Ms Gascoigne must be living on another planet.
Conclusions
The main conclusion from all of this is that the General Pharmaceutical Council is almost criminally negligent. It continues to allow pharmacists, Anthony Pinkus among them, to endanger lives. It fails to apply its own declared principles. The members of its Council, and Duncan Rudkin (its chief executive and registrar), are not doing their job.
Individual pharmacists vary a lot, from the superb to those who believe in quackery. Some, perhaps many, are embarrassed by the fact that their employer compels them to sell rubbish. It’s too much to expect that they’ll endanger their mortgage payments by speaking out about it, but the best ones will take you aside and explain that they can’t recommend it.
The GPhC itself is regulated by the Professional Standards Authority, the subject of my last post. We can’t expect anything sensible from them.
In the USA there is a shocking number of pharmacists who seem to believe in quackery. In the UK. nobody knows, though judging by their failure to vote against the daftest of all scams, homeopathy, there is no cause for complacency here.
It seems that there will have to be big improvements in pharmacy education before you can have much confidence in the quality of the advice that you get in a pharmacy.
Follow-up
Yesterday a talk was given at the School of Pharmacy, organised by the “The Centre for Homeopathic Education” (an oxymoron if there ever was one). The flyer had all the usual nonsense. Its mention of “Remedies & Tonics for Cancer Recovery” might well have breached the Cancer Act (1939). When I asked whether the amount received in room rental was sufficient to offest the damage to the reputation of the School of Pharmacy resulting from hosting a nutty (and possible illegal) event, I had the greatest difficulty in extracting any sort of response from the school’s director, Duncan Craig. I’m told that he considers “the policy on space rental to be a UCL management issue, rather than a matter of discussion on scientific ethics with a colleague”. Oh dear.
The consistent failure of ‘regulators’ to do their job has been a constant theme on this blog. There is a synopsis of dozens of them at Regulation of alternative medicine: why it doesn’t work, and never can. And it isn’t only quackery where this happens. The ineptitude (and extravagance) of the Quality Assurance Agency (QAA) was revealed starkly when the University of Wales’ accreditation of external degrees was revealed (by me and by BBC TV Wales, not by the QAA) to be so bad that the University had to shut down.
Here is another example that you couldn’t make up.
 |
 |
Yes, the Professional Standards Authority (PSA) has agreed to accredit that bad-joke pseudo-regulator, the Complementary & Natural Healthcare Council (CNHC, more commonly known as Ofquack)
Ofquack was created at the instigation of HRH the Prince of Wales, at public expense, as a means of protecting the delusional beliefs of quacks from criticism. I worked for them for a while, and know from the inside that their regulation is a bad joke.
When complaints were made about untrue claims made by ‘reflexologists’, the complaints were upheld but they didn’t even reach the Conduct and Competence committee, on the grounds that the reflexologists really believed the falsehoods that they’d been taught. Therefore, by the Humpty Dumpty logic of the CNHC, their fitness to practise was not affected by their untrue claims. You can read the account of this bizarre incident by the person who submitted the complaints, Simon Perry.
In fact in the whole history of the CNHC, it has received a large number of complaints, but only one has ever been considered by their Conduct and Competence Committee. The rest have been dismissed before they were considered properly. That alone makes their claim to be a regulator seem ridiculous.
The CNHC did tell its registrants to stop making unjustified claims, but it has been utterly ineffective in enforcing that ruling. In May 2013, another 100 complaints were submitted and no doubt they will be brushed aside too: see Endemic problems with CNHC registrants..
As I said at the time
It will be fascinating to see how the CNHC tries to escape from the grave that it has dug for itself.
If the CNHC implements properly its own code of conduct, few people will sign up and the CNHC will die. If it fails to implement its own code of conduct it would be shown to be a dishonest sham.
In February of this year (2013), I visited the PSA with colleagues from the Nightingale Collaboration. We were received cordially enough, but they seemed to be bureaucrats with no real understanding of science. We tried to explain to them the fundamental dilemma of the regulation of quacks, namely that no amount of training will help when the training teaches things that aren’t true. They were made aware of all of the problems described above. But despite that, they ended up endorsing the CNHC.
How on earth did the PSA manage to approve an obviously ineffective ‘regulator’?
The job of the PSA is said to be “. . . protecting users of health and social care services and the public”. They (or at least their predecessor, the CHRE), certainly didn’t do that during the saga of the General Chiropractic Council.
The betrayal of reason is catalogued in a PSA document [get local copy]. Here is some nerdy detail.
It is too tedious to go through the whole document, so I’ll deal with only two of its many obvious flaws, the sections that deal with the evidence base, and with training.
The criteria for accreditation state
Standard 6: the organisation demonstrates that there is a defined knowledge base underpinning the health and social care occupations covered by its register or, alternatively, how it is actively developing one. The organisation makes the defined knowledge base or its development explicit to the public.
The Professional Standards Authority recognises that not all disciplines are underpinned by evidence of proven therapeutic value. Some disciplines are subject to controlled randomized trials, others are based on qualitative evidence. Some rely on anecdotes. Nevertheless, these disciplines are legal and the public choose to use them. The Authority requires organisations to make the knowledge base/its development clear to the public so that they may make informed decisions.
Since all 15 occupations that are “regulated” by the CNHC fall into the last category. they “rely on anecdotes”, you would imagine the fact that “The Authority requires organisations to make the knowledge base/its development clear to the public” would mean that the CNHC was required to make a clear statement that reiki, reflexology etc are based solely on anecdote. Of course the CNHC does no such thing. For example, the CNHC’s official definition of reflexology says
Reflexology is a complementary therapy based on the belief that there are reflex areas in the feet and hands which are believed to correspond to all organs and parts of the body
There is, of course, not the slightest reason to think such connections exist, but the CNHC gives no hint whatsoever of that inconvenient fact. The word “anecdote” is used by the PSA but occurs nowhere on the CNHC’s web site.
It is very clear that the CNHC fails standard 6.
But the PSA managed to summon up the following weasel words to get around this glaring failure:
“The professional associations (that verify eligibility for CNHC registration) were actively involved in defining the knowledge base for each of the 15 professions. The Panel further noted that Skills for Health has lead responsibility for writing and reviewing the National Occupational Standards (NOS) for the occupations CNHC registers and that all NOS have to meet the quality criteria set by the UK Commission for Employment and Skills (UKCES), who are responsible for the approval of all NOS across all industry sectors. The Panel considered evidence provided and noted that the applicant demonstrated that there is a defined knowledge base underpinning the occupations covered by its registers. The knowledge base was explicit to the public”.
The PSA, rather than engaging their own brains, simply defer to two other joke organisations, Skills for Health and National Occupational Standards. But it is quite obvious that for things like reiki, reflexology and craniosacral therapy, the “knowledge base” consists entirely of made-up nonsense. Any fool can see that (but not, it seems, the PSA).
Skills for Health lists made-up, HR style, “competencies” for everything under the sun. When I got them to admit that their efforts on distance-healing etc had been drafted by the Prince of Wales’ Foundation, the conversation with Skills for Health became surreal (recorded in January 2008)
DC. Well yes the Prince of Wales would like that. His views on medicine are well known, and they are nothing if not bizarre. Haha are you going to have competencies in talking to trees perhaps?
“You’d have to talk to LANTRA, the land-based organisation for that.”
DC. I’m sorry, I have to talk to whom?
“LANTRA which is the sector council for the land-based industries uh, sector, not with us sorry . . . areas such as horticulture etc.”
DC. We are talking about medicine aren’t we? Not horticulture.
“You just gave me an example of talking to trees, that’s outside our remit ”
You couldn’t make it up, but it’s true. And the Professional Standards Authority rely on what these jokers say.
The current Skills for Health entry for reflexology says
“Reflexology is the study and practice of treating reflex points and areas in the feet and hands that relate to corresponding parts of the body. Using precise hand and finger techniques a reflexologist can improve circulation, induce relaxation and enable homeostasis. These three outcomes can activate the body’s own healing systems to heal and prevent ill health.”
This is crass, made-up nonsense. Of course there are no connections between “areas in the feet and hands that relate to corresponding parts of the body” and no reason to think that reflexology is anything more than foot massage. That a very expensive body, paid for by you and me, can propagate such preposterous nonsense is worrying. That the PSA should rely on them is even more worrying.
National Occupational Standards is yet another organisation that is utterly dimwitted about medical matters, but if you look up reflexology you are simply referred to Skills for Health, as above.
UK Commission for Employment and Skills
(UKCES) is a new one on me. The PSA says that “the UK Commission for Employment and Skills (UKCES), who are responsible for the approval of all NOS across all industry sectors” It is only too obvious that the UKCES leadership team have failed utterly to do their job when it comes to made-up medicine. None of them know much about medicine. It’s true that their chairman did once work for SmithKline Beecham, but as a marketer of Lucozade, a job which anyone with much knowledge of science would not find comfortable..
You don’t need to know much medicine to spot junk. I see no excuse for their failure.
The training problem.
The PSA’s criteria for accreditation say
Standard 9: education and training
The organisation:
9a) Sets appropriate educational standards that enable its registrants to practise competently the occupation(s) covered by its register. In setting its standards the organisation takes account of the following factors:
- The nature and extent of risk to service users and the public
- The nature and extent of knowledge, skill and experience required to provide
service users and the public with good quality careand later
9b) Ensures that registrants who assess the health needs of service users and provide any form of care and treatment are equipped to:
- Recognise and interpret clinical signs of impairment
- Recognise where a presenting problem may mask underlying pathologies
- Have sufficient knowledge of human disease and social determinants of health to identify where service users may require referral to another health or social care professional.
Anyone who imagines for a moment that a reflexologist or a craniosacral therapist is competent to diagnose a subarachnoid haemorrhage or malaria must need their head examining. In any case, the CNHC has already admitted that their registrants are taught things that aren’t true, so more training presumably means more inculcation of myths.
So how does the PSA wriggle out of this? Their response started
“The Panel noted that practitioners must meet, as a minimum, the National Occupational Standards for safe and competent practice. This is verified by the professional associations, who have in turn provided written undertakings to CNHC affirming that there are processes in place to verify the training and skills outcomes of their members to the NOS”
Just two problems there. The NOS standards themselves are utterly delusional. And checking them is left to the quacks themselves. To be fair, the PSA weren’t quite happy with this, but after an exchange of letters, minor changes enabled the boxes to be ticked and the PSA said “The Panel was now satisfied from the evidence provided, that this Standard had been
met”.
What’s wrong with regulators?
This saga is typical of many other cases of regulators doing more harm than good. Regulators are sometimes quacks themselves, in which case one isn’t surprised at their failure to regulate.
But organisations like the Professional Standards Authority and Skills for Health are not (mostly) quacks themselves. So how do they end up giving credence to nonsense? I find that very hard to comprehend, but here are a few ideas.
(1) They have little scientific education and are not really capable of critical thought
(2) Perhaps even more important, they lack all curiosity. It isn’t very hard to dig under the carapace of quack organisations, but rather than finding out for themselves, the bureaucrats of the PSA are satisfied by reassuring letters that allow them to tick their boxes and get home.
(3) A third intriguing possibility is that people like the PSA yield to political pressure. The Department of Health is deeply unscientific and clearly has no idea what to do about alternative medicine. They have still done nothing at all about herbal medicine, traditional Chinese medicine or homeopathy, after many years of wavering. My guess is that they see the CNHC as an organisation that gives the appearance that they’ve done something about reiki etc. I wonder whether they applied pressure to the PSA to accredit CNHC, despite it clearly breaking their own rules. I have sent a request under the Freedom of Information Act in an attempt to discover if the Department of Health has misbehaved in the way it did when it attempted to override NHS Choices.
The responsibility for this cock-up has to rest squarely on the shoulders of the PSA’s director, Harry Cayton. He was director of the CHRE from which PSA evolved and is the person who so signally failed to do anything about the General Chiropractic Council fiasco,
What can be done?
This is just the latest of many examples of regulators who not only fail to help but actually do harm by giving their stamp of approval to mickey mouse organisations like the CNHC. Most of the worst quangos survived the “bonfire of the quangos”.. The bonfire should have started with the PSA, CNHC and Skills for Health. They cost a lot and do harm.
There is a much simpler answer. There is a good legal case that much of alternative medicine is illegal. All one has to do is to enforce the existing law. Nobody would object to quacks if they stopped making false claims (though whether they could stay in business if they stopped exaggerating is debatable). There is only one organisation that has done a good job when it comes to truthfulness. That is the Advertising Standards Authority. But the ASA can do nothing apart from telling people to change the wording of their advertisements, and even that is often ignored.
The responsibility for enforcing the Consumer Protection Law is Trading Standards. They have consistently failed to do their job (see Medico-Legal Journal, Rose et al., 2012. “Spurious Claims for Health-care Products“.
If they did their job of prosecuting people who defraud the public with false claims, the problem would be solved.
But they don’t, and it isn’t.
Follow-up
The indefatigable Quackometer has wriiten an excellent account of the PSA fiasco
Here is a record of a couple of recent newspaper pieces. Who says the mainstream media don’t matter any longer? Blogs may be in the lead now when it comes to critical analysis. The best blogs have more expertise and more time to read the sources than journalists. But the mainstream media get the message to a different, and much larger, audience.
The Observer ran a whole page interview with me as part of their “Rational Heroes” series. I rather liked their subtitle [pdf of article]
“Professor of pharmacology David Colquhoun is the take-no-prisoners debunker of pseudoscience on his unmissable blog”
It was pretty accurate apart from the fact that the picture was labelled as “DC in his office”. Actually it was taken (at the insistence of the photographer) in Lucia Sivilotti’s lab.

Photo by Karen Robinson.
The astonishing result of this was that on Sunday the blog got a record 24,305 hits. Normally it gets 1,000-1,400 hits a day . between posts, fewer on Sunday, and the previous record was around 7000/day
A week later it was still twice normal. It remains to be seen whether the eventual plateau stays up.
I also gained around 1000 extra followers on twitter, though some dropped away quite soon, and 100 or so people signed for email updates. The dead tree media aren’t yet dead. I’m happy to say.
3 June 2013
Perhaps as a result of the foregoing piece, I got asked to write a column for The Observer, at barely 48 hours notice. This is the best I could manage in the time. The web version has links.
This attracted the usual "it worked for me" anecdotes in the comments, but I spent an afternoon answering them. It seems important to have a dialogue, not just to lecture the public. In fact when I read a regular scientific paper, I now find myself looking for the comment section. That may say something about the future of scientific publishing.
It is for others to judge how succesfully I engage with the public, but I was quite surprised to discover that UCL’s public engagement unit, @UCL_in_public, has blocked me on twitter. Hey ho. They have 1574 follower and I have 7597. I wish them the best of luck.
Follow-up
Anesthesia & Analgesia is the official journal of the International Anesthesia Research Society. In 2012 its editor, Steven Shafer, proposed a head-to-head contest between those who believe that acupuncture works and those who don’t. I was asked to write the latter. It has now appeared in June 2013 edition of the journal [download pdf]. The pro-acupuncture article written by Wang, Harris, Lin and Gan appeared in the same issue [download pdf].
Acupuncture is an interesting case, because it seems to have achieved greater credibility than other forms of alternative medicine, despite its basis being just as bizarre as all the others. As a consequence, a lot more research has been done on acupuncture than on any other form of alternative medicine, and some of it has been of quite high quality. The outcome of all this research is that acupuncture has no effects that are big enough to be of noticeable benefit to patients, and it is, in all probablity, just a theatrical placebo.
After more than 3000 trials, there is no need for yet more. Acupuncture is dead.

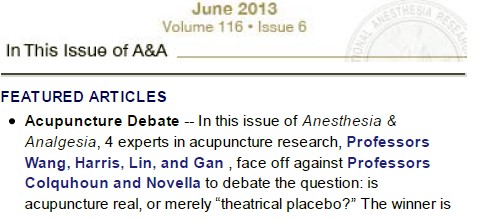
Acupuncture is a theatrical placebo
David Colquhoun (UCL) and Steven Novella (Yale)
Anesthesia & Analgesia, June 2013 116:1360-1363.
Pain is a big problem. If you read about pain management centres you might think it had been solved. It hasn’t. And when no effective treatment exists for a medical problem, it leads to a tendency to clutch at straws. Research has shown that acupuncture is little more than such a straw.
Although it is commonly claimed that acupuncture has been around for thousands of years, it hasn’t always been popular even in China. For almost 1000 years it was in decline and in 1822 Emperor Dao Guang issued an imperial edict stating that acupuncture and moxibustion should be banned forever from the Imperial Medical Academy.
Acupuncture continued as a minor fringe activity in the 1950s. After the Chinese Civil War, the Chinese Communist Party ridiculed traditional Chinese medicine, including acupuncture, as superstitious. Chairman Mao Zedong later revived traditional Chinese Medicine as part of the Great Proletarian Cultural Revolution of 1966 (Atwood, 2009). The revival was a convenient response to the dearth of medically-trained people in post-war China, and a useful way to increase Chinese nationalism. It is said that Chairman Mao himself preferred Western medicine. His personal physician quotes him as saying “Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine” Li {Zhisui Li. Private Life Of Chairman Mao: Random House, 1996}.
The political, or perhaps commercial, bias seems to still exist. It has been reported by Vickers et al. (1998) (authors who are sympathetic to alternative medicine) that
“all trials [of acupuncture] originating in China, Japan, Hong Kong, and Taiwan were positive”(4).
Acupuncture was essentially defunct in the West until President Nixon visited China in 1972. Its revival in the West was largely a result of a single anecdote promulgated by journalist James Reston in the New York Times, after he’d had acupuncture in Beijing for post-operative pain in 1971. Despite his eminence as political journalist, Reston had no scientific background and evidently didn’t appreciate the post hoc ergo propter hoc fallacy, or the idea of regression to the mean.
After Reston’s article, acupuncture quickly became popular in the West. Stories circulated that patients in China had open heart surgery using only acupuncture (Atwood, 2009). The Medical Research Council (UK) sent a delegation, which included Alan Hodgkin, to China in 1972 to investigate these claims , about which they were skeptical. In 2006 the claims were repeated in 2006 in a BBC TV program, but Simon Singh (author of Fermat’s Last Theorem) discovered that the patient had been given a combination of three very powerful sedatives (midazolam, droperidol, fentanyl) and large volumes of local anaesthetic injected into the chest. The acupuncture needles were purely cosmetic.
Curiously, given that its alleged principles are as bizarre as those on any other sort of pre-scientific medicine, acupuncture seemed to gain somewhat more plausibility than other forms of alternative medicine. The good thing about that is that more research has been done on acupuncture than on just about any other fringe practice.
The outcome of this research, we propose, is that the benefits of acupuncture, if any, are too small and too transient to be of any clinical significance. It seems that acupuncture is little or no more than a theatrical placebo. The evidence for this conclusion will now be discussed.
Three things that are not relevant to the argument
There is no point in discussing surrogate outcomes such as fMRI studies or endorphine release studies until such time as it has been shown that patients get a useful degree of relief. It is now clear that they don’t.
There is also little point in invoking individual studies. Inconsistency is a prominent characteristic of acupuncture research: the heterogeneity of results poses a problem for meta-analysis. Consequently it is very easy to pick trials that show any outcome whatsoever. Therefore we shall consider only meta-analyses.
The argument that acupuncture is somehow more holistic, or more patient-centred, than medicine seems us to be a red herring. All good doctors are empathetic and patient-centred. The idea that empathy is restricted to those who practice unscientific medicine seems both condescending to doctors, and it verges on an admission that empathy is all that alternative treatments have to offer.
There is now unanimity that the benefits, if any, of acupuncture for analgesia, are too small to be helpful to patients.
Large multicenter clinical trails conducted in Germany {Linde et al., 2005; Melchart et, 2005; Haake et al, 2007, Witt et al, 2005), and in the United States {Cherkin et al, 2009) consistently revealed that verum (or true) acupuncture and sham acupuncture treatments are no different in decreasing pain levels across multiple chronic pain disorders: migraine, tension headache, low back pain, and osteoarthritis of the knee.
If, indeed, sham acupuncture is no different from real acupuncture the apparent improvement that may be seen after acupuncture is merely a placebo effect. Furthermore it shows meridians don’t exist, so the “theory” memorized by qualified acupuncturists is just myth. All that remains to be discussed is whether or not the placebo effect is big enough to be useful, and whether it is ethical to prescribe placebos.
Some recent meta-analyses have found that there may be a small difference between sham and real acupuncture. Madsen Gøtzsche & Hróbjartsson {2009) looked at thirteen trials with 3025 patients, in which acupuncture was used to treat a variety of painful conditions. There was a small difference between ‘real’ and sham acupuncture (it didn’t matter which sort of sham was used), and a somewhat bigger difference between the acupuncture group and the no-acupuncture group. The crucial result was that even this bigger difference corresponded to only a 10 point improvement on a 100 point pain scale. A consensus report (Dworkin, 2009) that a change of this sort should be described as a “minimal” change or “little change”. It isn’t big enough for the patient to notice much effect.
The acupuncture and no-acupuncture groups were, of course, not blind to the patients and neither were they blind to the practitioner giving the treatment. It isn’t possible to say whether the observed difference is a real physiological action or whether it’s a placebo effect of a rather dramatic intervention. Interesting though it would be to know this, it matters not a jot, because the effect just isn’t big enough to produce any tangible benefit.
Publication bias is likely to be an even greater problem for alternative medicine than it is for real medicine, so it is particularly interesting that the result just described has been confirmed by authors who practise, or sympathise with, acupuncture. Vickers et al. (2012) did a meta-analysis for 29 RCTs, with 17,922 patients. The patients were being treated for a variety of chronic pain conditions. The results were very similar to those of Madsen et al.{2009). Real acupuncture was better than sham, but by a tiny amount that lacked any clinical significance. Again there was a somewhat larger difference in the non-blind comparison of acupuncture and no-acupuncture, but again it was so small that patients would barely notice it.
Comparison of these two meta-analyses shows how important it is to read the results, not just the summaries. Although the outcomes were similar for both, the spin on the results in the abstracts (and consequently the tone of media reports) was very different.
An even more extreme example of spin occurred in the CACTUS trial of acupuncture for ” ‘frequent attenders’ with medically unexplained symptoms” (Paterson et al., 2011). In this case, the results showed very little difference even between acupuncture and no-acupuncture groups, despite the lack of blinding and lack of proper controls. But by ignoring the problems of multiple comparisons the authors were able to pick out a few results that were statistically significant, though trivial in size. But despite this unusually negative outcome, the result was trumpeted as a success for acupuncture. Not only the authors, but also their university’s PR department and even the Journal editor issued highly misleading statements. This gave rise to a flood of letters to the British Journal of General Practice and much criticism on the internet.
From the intellectual point of view it would be interesting to know if the small difference between real and sham acupuncture found in some, but not all, recent studies is a genuine effect of acupuncture or whether it is a result of the fact that the practitioners are never blinded, or of publication bias. But that knowledge is irrelevant for patients. All that matters for them is whether or not they get a useful degree of relief.
There is now unanimity between acupuncturists and non-acupuncturists that any benefits that may exist are too small to provide any noticeable benefit to patients. That being the case it’s hard to see why acupuncture is still used. Certainly such an accumulation of negative results would result in the withdrawal of any conventional treatment.
Specific conditions
Acupuncture should, ideally, be tested separately for effectiveness for each individual condition for which it has been proposed (like so many other forms of alternative medicine, that’s a very large number). Good quality trials haven’t been done for all of them. It’s unlikely that acupuncture works for rheumatoid arthritis, stopping smoking, irritable bowel syndrome or for losing weight. And there is no good reason to think it works for addictions, asthma, chronic pain, depression, insomnia, neck pain, shoulder pain or frozen shoulder, osteoarthritis of the knee, sciatica, stroke or tinnitus and many other conditions (Ernst et al., 2011).
In 2009, the UK’s National Institute for Clinical Excellence (NICE) did recommend both acupuncture and chiropractic for back pain. This exercise in clutching at straws caused something of a furore. In the light of NICE’s judgement the Oxford Centre for Evidence-based medicine updated its analysis of acupuncture for back pain. Their verdict was
“Clinical bottom line. Acupuncture is no better than a toothpick for treating back pain.”
The paper by Artus et al. (2010) is of particular interest for the problem of back pain. Their Fig 2 shows that there is a modest improvement in pain scores after treatment, but much the same effect, with the same time course is found regardless of what treatment is given, and even with no treatment at all. They say
“we found evidence that these responses seem to follow a common trend of early rapid improvement in symptoms that slows down and reaches a plateau 6 months after the start of treatment, although the size of response varied widely. We found a similar pattern of improvement in symptoms following any treatment, regardless of whether it was index, active comparator, usual care or placebo treatment”.
It seems that most of what’s being seen is regression to the mean. And that is very likely to be the main reason why acupuncture sometimes appears to work when it doesn’t.
Although the article by Wang et al (2012) was written to defend the continued use of acupuncture, the only condition for which they claim that there is any reasonably strong evidence is for post-operative nausea and vomiting (PONV). It would certainly be odd if a treatment that had been advocated for such a wide variety of conditions turned out to work only for PONV. Nevertheless, let’s look at the evidence.
The main papers that are cited to support the efficacy of acupuncture in alleviation of PONV are all from the same author: Lee & Done (1999), and two Cochrane reviews, Lee & Done (2004), updated in Lee & Fan (2009). We need only deal with this latest updated meta-analysis.
Although the authors conclude “P6 acupoint stimulation prevented PONV”, closer examination shows that this conclusion is very far from certain. Even taken at face value, a relative risk of 0.7 can’t be described as “prevention”. The trials that were included were not all tests of acupuncture but included several other more or less bizarre treatments (“acupuncture, electro-acupuncture, transcutaneous nerve stimulation, laser stimulation, capsicum plaster, an acu-stimulation device, and acupressure”). The number needed to treat varied from a disastrous 34 to a poor 5 for patients with control rates of PONV of 10% and 70% respectively.
The meta-analysis showed, on average, similar effectiveness for acupumcture and anti-emetic drugs. The problem is that the effectiveness of drugs is in doubt because an update to the Cochrane review has been delayed (Carlisle, 2012) by the discovery of major fraud by a Japanese anesthetist, Yoshitaka Fujii (Sumikawa, 2012). It has been suggested that metclopramide barely works at all (Bandolier, 2012; Henzi, 1999).
Of the 40 trials (4858 participants) that were included; only four trials reported adequate allocation concealment. Ninety percent of trials were open to bias from this source. Twelve trials did not report all outcomes. The opportunities for bias are obvious. The authors themselves describe all estimates as being of “Moderate quality” which is defined this: “Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate”. That being the case, perhaps the conclusion should have been “more research needed”. In fact almost all trials of alternative medicines seem to end up with the conclusion that more research is needed.
Conclusions
It is clear from meta-analyses that results of acupuncture trials are variable and inconsistent, even for single conditions. After thousands of trials of acupuncture, and hundreds of systematic reviews (Ernst et al., 2011), arguments continue unabated. In 2011, Pain carried an editorial which summed up the present situation well.
“Is there really any need for more studies? Ernst et al. (2011) point out that the positive studies conclude that acupuncture relieves pain in some conditions but not in other very similar conditions. What would you think if a new pain pill was shown to relieve musculoskeletal pain in the arms but not in the legs? The most parsimonious explanation is that the positive studies are false positives. In his seminal article on why most published research findings are false, Ioannidis (2005) points out that when a popular but ineffective treatment is studied, false positive results are common for multiple reasons, including bias and low prior probability.”
Since it has proved impossible to find consistent evidence after more than 3000 trials, it is time to give up. It seems very unlikely that the money that it would cost to do another 3000 trials would be well-spent.
A small excess of positive results after thousands of trials is most consistent with an inactive intervention. The small excess is predicted by poor study design and publication bias. Further, Simmons et al (2011) demonstrated that exploitation of “undisclosed flexibility in data collection and analysis” can produce statistically positive results even from a completely nonexistent effect. With acupuncture in particular there is documented profound bias among proponents (Vickers et al., 1998). Existing studies are also contaminated by variables other than acupuncture – such as the frequent inclusion of “electroacupuncture” which is essentially transdermal electrical nerve stimulation masquerading as acupuncture.
The best controlled studies show a clear pattern – with acupuncture the outcome does not depend on needle location or even needle insertion. Since these variables are what define “acupuncture” the only sensible conclusion is that acupuncture does not work. Everything else is the expected noise of clinical trials, and this noise seems particularly high with acupuncture research. The most parsimonious conclusion is that with acupuncture there is no signal, only noise.
The interests of medicine would be best-served if we emulated the Chinese Emperor Dao Guang and issued an edict stating that acupuncture and moxibustion should no longer be used in clinical practice.
No doubt acupuncture will continue to exist on the High Streets where they can be tolerated as a voluntary self-imposed tax on the gullible (as long as they don’t make unjustified claims).
|
REFERENCES
|
|
| 1. Acupuncture Centre. . About Acupuncture. Available at: http://www.acupuncturecentre.org/aboutacupuncture.html. Accessed March 30, 2013 | |
| 2. Atwood K. “Acupuncture Anesthesia”: a Proclamation from Chairman Mao (Part IV). Available at: http://www.sciencebasedmedicine.org/index.php/acupuncture-anesthesia-a-proclamation-from-chairman-mao-part-iv/. Accessed September 2, 2012 | |
| 3. Li Z Private Life of Chairman Mao: The Memoirs of Mao’s Personal Physician. 1996 New York: Random House | |
| 4. Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials. 1998;19:159–66 Available at: http://bit.ly/WqVGWN. Accessed September 2, 2012 | |
| 5. Reston J. Now, About My Operation in Peking; Now, Let Me Tell You About My Appendectomy in Peking … The New York Times. 1971 Available at: http://select.nytimes.com/gst/abstract.html?res=FB0D11FA395C1A7493C4AB178CD85F458785F9. Accessed March 30, 2013 | |
| 6. Atwood K. “Acupuncture anesthesia”: a proclamation from chairman Mao (part I). Available at: http://www.sciencebasedmedicine.org/index.php/acupuncture-anesthesia-a-proclamation-of-chairman-mao-part-i/. Accessed September 2, 2012 | |
| 7. Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes MG, Weidenhammer W, Willich SN, Melchart D. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293:2118–25 | |
| 8. Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes M, Hummelsberger J, Irnich D, Weidenhammer W, Willich SN, Linde K. Acupuncture in patients with tension-type headache: randomised controlled trial. BMJ. 2005;331:376–82 | |
| 9. Haake M, Müller HH, Schade-Brittinger C, Basler HD, Schäfer H, Maier C, Endres HG, Trampisch HJ, Molsberger A. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–8 | |
| 10. Witt C, Brinkhaus B, Jena S, Linde K, Streng A, Wagenpfeil S, Hummelsberger J, Walther HU, Melchart D, Willich SN. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366:136–43 | |
| 11. Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, Delaney K, Hawkes R, Hamilton L, Pressman A, Khalsa PS, Deyo RA. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169:858–66 | |
| 12. Madsen MV, Gøtzsche PC, Hróbjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ. 2009;338:a3115 | |
| 13. Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S, Burke LB, Cowan P, Farrar JT, Hertz S, Raja SN, Rappaport BA, Rauschkolb C, Sampaio C. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–44 | |
| 14. Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, Sherman KJ, Witt CM, Linde K. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–53 | |
| 15. Paterson C, Taylor RS, Griffiths P, Britten N, Rugg S, Bridges J, McCallum B, Kite G. Acupuncture for ‘frequent attenders’ with medically unexplained symptoms: a randomised controlled trial (CACTUS study). Br J Gen Pract. 2011;61:e295–e305 | |
| 16. . Letters in response to Acupuncture for ‘frequent attenders’ with medically unexplained symptoms. Br J Gen Pract. 2011;61 Available at: http://www.ingentaconnect.com/content/rcgp/bjgp/2011/00000061/00000589. Accessed March 30, 2013 | |
| 17. Colquhoun D. Acupuncturists show that acupuncture doesn’t work, but conclude the opposite: journal fails. 2011 Available at: https://www.dcscience.net/?p=4439. Accessed September 2, 2012 | |
| 18. Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011;152:755–64 | |
| 19. Colquhoun D. NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself. 2009 Available at: https://www.dcscience.net/?p=1516. Accessed September 2, 2012 | |
| 20. Colquhoun D. The NICE fiasco, part 3. Too many vested interests, not enough honesty. 2009 Available at: https://www.dcscience.net/?p=1593. Accessed September 2, 2012 | |
| 21. Bandolier. . Acupuncture for back pain—2009 update. Available at: http://www.medicine.ox.ac.uk/bandolier/booth/painpag/Chronrev/Other/acuback.html. Accessed March 30, 2013 | |
| 22. Artus M, van der Windt DA, Jordan KP, Hay EM. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology (Oxford). 2010;49:2346–56 | |
| 23. Wang S-M, Harris RE., Lin Y-C, Gan TJ. Acupuncture in 21st century anesthesia: is there a needle in the haystack? Anesth Analg. 2013;116:1356–9 | |
| 24. Lee A, Done ML. The use of nonpharmacologic techniques to prevent postoperative nausea and vomiting: a meta-analysis. Anesth Analg. 1999;88:1362–9 | |
| 25. Lee A, Done ML. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2004:CD003281 | |
| 26. Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2009:CD003281 | |
| 27. Carlisle JB. A meta-analysis of prevention of postoperative nausea and vomiting: randomised controlled trials by Fujii etal. compared with other authors. Anaesthesia. 2012;67:1076–90 | |
| 28. Sumikawa K. The results of investigation into Dr.Yoshitaka Fujii’s papers. Report of the Japanese Society of Anesthesiologists Special Investigation Committee. http://www.anesth.or.jp/english/pdf/news20120629.pdf | |
| 29. Bandolier. . Metoclopramide is ineffective in preventing postoperative nausea and vomiting. Available at: http://www.medicine.ox.ac.uk/bandolier/band71/b71-8.html. Accessed March 30, 2013 | |
| 30. Henzi I, Walder B, Tramèr MR. Metoclopramide in the prevention of postoperative nausea and vomiting: a quantitative systematic review of randomized, placebo-controlled studies. Br J Anaesth. 1999;83:761–71 | |
| 31. Hall H. Acupuncture’s claims punctured: not proven effective for pain, not harmless. Pain. 2011;152:711–2 | |
| 32. Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2:e124 | |
| 33. Simmons JP, Leif DN, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol Sci. 2011;22:1359–66 |
Follow-up
30 May 2013 Anesthesia & Analgesia has put the whole paper on line. No paywall now!
9 June 2013. Since this page was posted on May 30, it has had over 20,000 page views. Not bad.
26 July 2013. The Observer had a large double-page spread about acupuncture. It was written by David Derbyshire, largely on the basis of this article.
26 December 2013
Over christmas the flow of stuff that misrepresents the “thousands of years” of Chinese medicine has continued unabated. Of course one expects people who are selling Chinese herbs and acupuncture to lie. All businesses do. One does not expect such misrepresentation from British Columbia, Cardiff University School of medicine, or from Yale University. I left a comment on the Yale piece. Whether it passes moderation remains to be seen. Just in case, here it is.
One statement is undoubtedly baseless ““If it’s still in use after a thousand years there must be something right,” It’s pretty obvious to the most casual observer that many beliefs that have been round for a thousand years have proved to be utterly wrong.
In any case, it’s simply not true that most “Traditional” Chinese medicine has been around for thousands of years. Acupuncture was actually banned by the Emperor Dao Guang in 1822. The sort of Chinese medicine that is sold (very profitably) to the west was essentially dead in China until it was revived by Mao as part of the great proletarian cultural revolution (largely to stir up Chinese nationalism at that time). Of course he didn’t use it himself.
This history has been documented in detail now, and it surprises me to see it misrepresented, yet again, from a Yale academic.
Of course there might turn out to be therapeutically useful chemicals in Chinese herbs (it has happened with artemesinin). But it is totally irresponsible to pretend that great things are coming in the absence of good RCTs in human patients.
Yale should be ashamed of PR like this. And so should Cardiff University. It not only makes the universities look silly. It corrupts the whole of the rest of these institutions. Who knows how much more of their PR is mere puffery.
18 January 2014. I checked the Yale posting and found that the comment, above, had indeed been deleted. There is little point in having comments if you are going to delete anything that’s mildly critical. It is simply dishonest.
It’s hard to know what to make of David Tredinnick MP (Cons, Bosworth). He is certainly an extreme example of the scientific ignorance of our parliamentary representatives, but he isn’t alone in that. Our present minister of Education, Michael Gove, memorably referred to Newton’s Laws of Thermodynamics, blissfully unaware that thermodynamics was a 19th century development. And our present Minister of Health seems to think that magic water cures diseases.
But Mr Treddinick breaks every record for anti-scientific nonsense. That, no doubt, is why he was upset by the recent revision of come NHS Choices web pages, so that they now give a good account of the evidence (that’s their job, of course). They did that despite two years of obstruction by the Department of Health. which seemed to think that it was appropriate to take advice from Michael Dixon of the Prince’s Foundation for integrated Health. That shocking example of policy based evidence was revealed on this blog, and caused something of a stir.
Treddinick’s latest letter
A copy of a letter from Mr Tredinnick to the Minister of Health, Jeremy Hunt, has some into my possession by a tortuous route [download the letter]. It’s a corker. Here are a few quotations.
"1. UKIP moving onto our ground
Attached is an extract from a recent UKIP policy statement. The position which UKIP has taken is one with which most of our Daily Mail reading supporters of complementary medicine would agree."
It seems that Treddinick’s preferred authority on medicine is now Nigel Farage, leader of the UK’s far right party. UKIP’s policy on health is appended to the letter, and it’s as barmy as most of the other things they say.
"2. Herbal Medicine
. . .there is very real concern that the Government will not regulate Herbal Medicine and Traditional Chinese Medicine. The current situation is unacceptable, because herbal practitioners need regulation and cannot function as herbal therapists, nor can they cannot obtain stocks of their herbal remedies, without it.
This refers to a saga that has been running for at least 10 years. Herbalists are desperate to get a government stamp of approval by getting statutory regulation, much like real doctors have, despite the fact that they make money by selling sick people "an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety" (as quoted recently in the House of Lords).
Even the US National Center for Complementary and Alternative Medicine (NCCAM) doesn’t claim that a single herbal treatment is useful. The saga of herbal regulation is long and tedious. The short version is that a very bad report, The Pittilo report, recommended regulation of herbalists. After years of prevarication, Andrew Lansley ignored the impartial scientific advice and yielded to the pressure from the herbal industry to accept the Pittilo report. But still nothing has happened.
Could it be that even Jeremy Hunt realises, deep down, that the regulation of nonsense is a nonsense that would harm the public?
We can only hope that a letter from Mr Tredinnick is the kiss of death. Perhaps his continuous pestering will only reinforce the doubts that seem to exist at the Department of Health.
Then Tredinnick returns (yawn) to his obsession with magic water. He vents his rage at the now excellent NHS Choices page on homeopathy.
3. Homeopathy
"Recently this wording has been removed and instead a comment by the Chief Medical Officer that homeopathy is placebo inserted in its place, as well as links to external organisations which campaign against homeopathy. For instance, there is a link to the Sense About Science website, and Caroline Finucane, who is Editor of new content at NHS Choices, also writes for the Sense About Science website. This is an organisation which has no expertise in homeopathy and traces its roots back to the ultra-left Revolutionary Communist Party (RCP)."
"I respectfully suggest that the original wording be reinstated and these links to external organisations be removed or changed to ensure a balanced view.".
So it seems that he prefers the medical views of Nigel Farage and the Prince of Wales to those of the Chief Medical Officer and the government’s chief scientist. Disgracefully, Tredinnick picks out one particular employee of NHS Choices among many, and one who does an excellent job. And he raises the hoary old myth that Sense About Science is a communist organisation. Odd, since others accuse it of being neo-libertarian. The actual history is here. The organisation that is a bit too libertarian for my taste is Spiked Online. I haven’t agreed with every word that Sense about Science has printed, but they have a totally honest belief in evidence.
To drag in the name of one person out of many, and to justify it by a false history shows, once again, how very venomous and vindictive the advocates of delusional medicine can be when they feel cornered.
A bit more information about Mr Treddinick
This is what the BBC News profile says about him.
|
David Tredinnick is an old style Conservative MP, being an Eton-educated former Guards officer, who has sat in the Commons since 1987. However, his ambition for high office was thwarted by his role in one of the sleaze stories which helped to sink the Major government. He accepted £1,000 from an undercover reporter to ask parliamentary questions about a fictitious drug. He was obliged to resign from his role as a PPS and was suspended from the Commons for 20 sitting days. He has not sat on the frontbench since. He is an orthodox Conservative loyalist, though he is more supportive of the European Union than many of his colleagues. He has, however, carved himself a niche as the Commons’ most enthusiastic supporter of complementary medicine. He has wearied successive health secretaries with his persistent advocacy of any and all homeopathic remedies. He has also supported their use in prisons and even suggested them as an aid in alleviating the foot and mouth crisis. |
|
Tredinnick has also asserted that he was aware of a psychiatric hospital that doubled its staff at full moon (this is an old urban myth, and is, of course, quite untrue). His advocacy of homeopathic borax as a way to control the 2001 epidemic of foot and mouth diease can be read here. Luckily it was ignored by the government. I hope his latest letter will be treated similarly. Picture of David Tredinnick MP from the Conservative Party |
 |
Follow-up
The bulletin of the British Pharmacological Society, Pharmacology Matters, declined to publish the following article. Sadly the Society seems to be more interested in "reputation management" than in truth. Luckily, it is not easy to suppress criticism these days. A version of the article has appeared in Research Fortnight where it will be seen by far more people than it would have been in Pharmacology Matters. This is the original version that I submitted to them. They would not allow me to quote Lewis’s comment (apropos of the sale of homeopathic meningitis vaccine)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
If a child were to die of whooping cough or meningitis as a result of buying the fraudulent "vaccines", that would be true. It’s a sad reflection on the state of defamation law that journals are not willing to say so. Blogs are fast becoming the best source of reliable information.

|

|
Stop press. The BPS has now signed up to Alltrials (too late for the printed version)
Pharmacology society does little to defend its subject
David Colquhoun
Over the past few years a courageous group of writers, researchers and activists has worked to expose the truth about the medicines we are sold, be they conventional or alternative.
Thanks, above all, to Ben Goldacre (1), more people than ever know that the big pharma companies have been concealing evidence of the harm that their products do, or the good they fail to do. Thanks to a small army of bloggers the preposterous claims made by peddlers of homeopathic remedies and other quackery are less likely to go unchallenged.
And yet, the organization charged with safeguarding the good name of pharmacology in this country, the British Pharmacological Society (BPS), has remained silent throughout.
The pharmaceutical industry
The BPS, rather than helping, became actively complicit when, along with much of the medical establishment, it signed an agreement with the ABPI (2). This document, developed under the aegis of the Ethical Standards in Health & Life Sciences Group (ESHLSG), contained two objectionable clauses:
“Industry plays a valid and important role in the provision of medical education”
And
“Medical representatives can be a useful resource for healthcare professionals”
Given that clinical “education” has long been part of Pharma’s marketing strategy, this seems disgraceful. And most of the doctors I know and respect refuse to see reps altogether. It is hopelessly optimistic to think that can an industry person can teach clinical pharmacology without bias in favour of his own company’s products. The BPS has many members who teach pharmacology. Can they really cope so badly that we need to have industry to educate clinicians?
It’s fine, and sometimes desirable, for academics and industry to work together on drug development. But only as long as the industry partner has no say in how, or whether, the results are published. Without that proviso we can expect more corruption of the sort that’s been seen at the University of Sheffield (3).
This is very sad, because I have great reason to like the drug industry. I’ve benefitted from several of their products myself. But the industry is in trouble. Many of its products provide only marginal benefits. Furthermore, some of the things that seemed to be useful, like SSRI antidepressants, have turned out to be next to useless once hidden trials were revealed (4). The MHRA’s learning module on SSRIs doesn’t seem to have caught up with this yet.
Sadly, the reaction of industry has been to resort to dishonesty, to hide unfavourable data and to increase yet more what it spends on marketing. Between 2009 and 2012, fines of at least 10 billion dollars (5) have been imposed on some of the most eminent companies. They include Lilly, Pfizer, AstraZeneca, Merck, Abbott and GlaxoSmithKline (GSK). The biggest fine of all ($3 bn, in July 2012) went to a British company, GSK. This succession of large fines seems to be regarded by the companies as mere marketing expenses.
All these fines were levied in the USA. Where, one might ask, are the regulators in the UK? Why have there been no fines here? Why, indeed, are some of the senior managers of these companies not in jail? Why has the BPS remained silent about the prostitution of its subject? And why have the MHRA done so little to stop it?
I suggest that you support the petition for release of the results of all trials (6). It’s been supported by many individuals and a lot of organisations, including the BMJ and the Royal Statistical Society. But, disgracefully, not by the BPS.
Quackery
At least in the case of the pharmaceutical industry some of its products work. But pharmacologists should also be concerned about the quackery industry, worth about 60 billion dollars per year (as opposed to $600 bn for the pharmaceutical industry). Virtually none of their products work (7). Why has the BPS said so little about it? It has, along with most of the medical and university establishment, shrugged its shoulders about the fact that students at Westminster University have been shown dowsing with a pendulum as a method for selection of herbal “remedies”, as part of a Bachelor or “Science” degree. It is an area in which every regulatory agency has failed to ensure even minimal levels of honesty (8). And the BPS has just shrugged.
The MHRA has been worse than useless in this area: it has been actively unhelpful (9). The senior staff of the MHRA are members of the BPS which has, as usual, said next to nothing. The MHRA’s herbal medicine committee has allowed misleading labels that give indications to be put on herbal potions, and these labels fail to make it clear that no evidence whatsoever of efficacy is required to get the MHRA kitemark. The wording was suggested (not required) by European law, but that law does not prevent the MHRA from saying, as it should, “there is no reason to think that this product is effective for any of the indications on the label” (10). Arguably, the MHRA is in breach of Consumer Protection law (11, 12).
At the time, the BPS did make some objection to the labelling (13), but only under great pressure from me (indeed I wrote it) . That has not been followed up, and I can no longer find it on the BPS web site. Indeed Philip Routledge, one of the people who is responsible for the misinformation in his capacity as chair of the MHRA Herbal Medicines Advisory Committee, is, at present the president of the BPS.
The MHRA has also been responsible for misleading labelling of the products of the most obviously fraudulent products of the lot: homeopathic pills, the medicines that contain no medicine. Most of the pills (anything beyond 12x dilution) contain not a single molecule of the substance on the label. Yet they have been given a get-out clause that enables them to evade prosecution by Trading Standards (an organisation that consistently fails to apply consumer protection laws. Rose et al (2011) (12) concluded
"EU directive 200s5/29/EC is largely ineffective in preventing misleading health claims for consumer products in the UK".
It is simply bizarre that the people at the MHRA, many of who are BPS members, have sat round a table and approved the following label. This example is for Arnica 30C pills, which, of course, contain no trace of arnica (14, 8). The outcome of their deliberations is simply surreal (see the actual labels here).
"Used within the homeopathic tradition for the symptomatic relief of sprains, muscular ache; and bruising or swelling after contusions."
This will deceive the naïve into thinking that it will have some effect on sprains etc. It won’t. And the MHRA have declined to test how the label is perceived by the public, though it took some effort to get them to admit it.
"If you are allergic to any of the ingredients in this medicine, consult your doctor before taking this medicine."
The ingredients aren’t stated apart from “contains lactose and sucrose”. That’s all they contain. No arnica.
"If pregnant or breastfeeding consult your doctor before use."
Why should a few mg of lactose and sucrose have the slightest effect on a pregnant or breast-feeding mother. This is pure make-believe
"If you forget to take this product, continue to take your usual dose at the usual time, it does not matter if you have missed a dose. Do not take a double dose to make up for a missed dose."
This statement is even more bizarre. There is nothing in the pills.
"If you take too much of this product (overdose) speak to a doctor or pharmacist and take this label with you."
And this is the ultimate in nonsense. The 1023 campaign regularly swallows whole bottles, and of course nothing happens. You can’t overdose on nothing. The fact that the MHRA can insist on this label, with a straight face, is the ultimate betrayal of science and reason.
"When asked to comment, as part of the consultation on these rules, this was the response from the BPS."
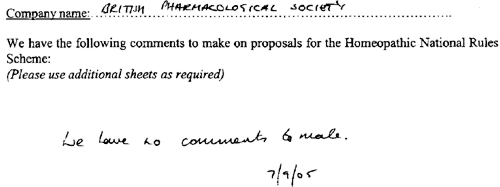
This is extracted from page 16 of the “selected response” provided by the MHRA under a Freedom of Information Act request [download all]
Things have changed little since A.J. Clark wrote his book on Patent Medicines in 1938 (15). And the BPS has done next to nothing to help. Neither has the MHRA. In fact both have colluded in the failures of both honesty and reason.
A BBC South West program recently revealed that a pharmacist was selling “homeopathic vaccines” for whooping cough and meningitis (16). The MHRA have know about his homicidal practice for years, but have done nothing. The General Pharmaceutical Council let him off with a rap on the knuckles. It has been left to bloggers and TV reporters to focus attention on these scoundrels. The well-respected blogger, Andy Lewis, wrote (17)
“Children will be harmed by this inaction. Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator [MHRA].”
And the full clinical data for Tamiflu are still being concealed by Roche (18).
I think that is rather shameful.
I have been a member of the BPS for all my working life. I was happy when they made me an honorary fellow. But I now find myself asking if I can remain a member of an organisation that has done so little to defend honest scientific behaviour.
References
(1) Ben Goldacre’s Bad Pharma. Buy it now. Then do something. https://www.dcscience.net/?p=5538
(2) ABPI 2012 Guidance on collaboration between healthcare professionals and the pharmaceutical industry. http://www.abpi.org.uk/our-work/library/guidelines/Pages/collaboration-guidance.aspx
(3) Colquhoun, D. (2007) The Corporate Corruption of Higher Education: part 2 https://www.dcscience.net/?p=193
(4) Kirsch,I., B.J.Deacon, T.B.Huedo-Medina, A.Scoboria, T.J.Moore, and B.T.Johnson. 2008. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS. Med. 5:e45. http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0050045
(5) Groeger, L. (2012) Big Pharma’s Big Fines http://www.propublica.org/special/big-pharmas-big-fines
(6) All trials registered. All results reported, http://www.alltrials.net/supporters/
(7) Singh,S. and E.Ernst. 2009. Trick or Treatment. Corgi. http://en.wikipedia.org/wiki/Trick_or_Treatment
(8) Colquhoun, D. (2012) Regulation of alternative medicine: why it doesn’t work, and never can. https://www.dcscience.net/?p=5562
(9) Colquhoun, D, (2006) The MHRA breaks its founding principle: it is an intellectual disgrace. https://www.dcscience.net/?p=32
(10) Colquhoun, D. (2011). Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. https://www.dcscience.net/?p=4269
(11) Colquhoun, D. (2009) Most alternative medicine is illegal. https://www.dcscience.net/?p=30
(12) Rose,L.B., P.Posadzki, and E.Ernst. 2012. Spurious claims for health-care products: an experimental approach to evaluating current UK legislation and its implementation. Med. Leg. J. 80:13-18. https://www.dcscience.net/Rose-medico-legal-2012.pdf
(13) Colquhoun, D. (2006) Learned Societies speak out against CAM, and the MHRA. https://www.dcscience.net/?p=30
(14) MHRA Arnicare Arnica 30c pillules NR 01175/0181 http://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con049307.pdf
(15) Colquhoun, D. (2008) Patent medicines in 1938 and now: A.J.Clark’s book. https://www.dcscience.net/?p=257
(16) BBC South West on the evils of homeopathic "vaccines" http://www.youtube.com/watch?v=TZf9mUzI4RI
(17) Why Does the MHRA Not Close Down these Homeopaths? The regulators have known of serious problems for years, Nothing is done. http://www.quackometer.net/blog/2013/01/why-does-the-mhra-not-close-down-these-homeopaths.html
(18) Payne, D. (2012). Tamiflu: the battle for secret drug data http://www.bmj.com/content/345/bmj.e7303
Follow-up
25 February 2013 This post has some follow-up even before it appeared on Research Research. I noticed on the BPS web site a press release “BPS announces intention to sign All Trials Petition“. It was dated 20th February, but I didn’t notice it until after the printed edition went to press. It was expressed as a future intention to sign, though in fact they signed almost straight away (though over 100 organisations had already done so). That’s good. I suspect that when my old friend, Humphrey Rang, who is president elect of the BPS, takes charge, the Society may start to take its responsibilities to the public more seriously than it has in the past.
|
The MHRA, on the other hand, is still evading its self-declared job of ensuring the public that drugs work. |

|
13 March 2013. A reply to this piece appeared in red on Research Research, The British Pharmacological Society champions its science. It was written by Humphrey Rang who, as president elect of the BPS naturally felt obliged to defend its record. He defends the BPS membership of ESHLSG, but fails to mention that first the Lancet and then the BMA withdrew their support. Nor does he mention that medical students and doctors launched a campaign, BadGuidelines.org, against the agreement. The Medical Schools Council, which also signed the agreement, said "the scrutiny of the guidance has ‘identified deficiencies in the current statement". Didn’t they read it before signing? Rang says that the BPS is also working to improve the joint statement with the ABPI. That’s good, but one must wonder why the BPS signed up to the original form.
On the points about quackery, Rang sites the BPS statement on homeopathy (now vanished) but fails to mention that that statement was written by me in an attempt to wake the BPS from it’s slumbers on the matter of medicines that don’t work. But he doesn’t mention at all the matter of mislabelling of both homeopathic and herbal preparations.
Of course, the BPS does many good things. But like most organisations, it is too reluctant to speak out when it sees wrongdoing, and too reluctant to say "sorry we made a cock-up that time".
|
“In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established”. . . “. . . they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.” David Mattin, lately of NHS Choices |
NHS Choices is usually a good source of information for the public. But there is one exception: the information they provide about alternative medicine is poor. A Freedom of Information Act request has revealed that the attempt of NHS Choices to rewrite their pages more accurately was censored by the Department of Health in conjunction with the late Prince’s Foundation for Integrated Health. The Department of Health (DH) has misled the public.
The earliest version of the homeopathy information page recorded by the Wayback Machine was November 12 2007. It was still there on December 5 2010. The comments were mostly critical. One said, quite correctly,
|
I find it most regrettable that the way NHS has covered this subject is to give uncritical voice to the claims of homoeopathy without giving readers the information they need to evaluate those claims. To refer readers to the websites of the British Homeopathy Association is like settling the question of the shape of planet by a reference to the website of the Flat Earth Society |
There were a lot of complaints, and to the credit of NHS Choices, the page vanished. Throughout 2011, and up to October 2012 the information page on homeopathy read
|
Introduction Content on homeopathy has been removed from the website pending a review by the Department of Health policy team responsible for complementary and alternative medicines. Homeopathy is not part of mainstream medicine. Instead it is defined as a complementary or alternative medicine. If you are considering using homeopathy, talk to your GP first. For more information about homeopathy see the House of Commons Science and Technology Committee report on homeopathy published on 8 February 2010 and the Department of Health response to that report published in July 2010 (PDF, 69KB). |
Then, at the end of 2012, the page reappeared. It was a bit better than the original, but not much. Many of the comments criticise the misleading nature of the information (as well as the usual “it worked for me” comments). The “useful links” still has six links to flat-earth organisations like the Society of Homeopaths, and only one to a sensible source, the excellent pamphlet from Sense about Science. They do link at the end to the 2010 Science and Technology Committee Report: Evidence Check 2: Homeopathy (PDF, 1.61Mb), and to the Government Response to the Science and Technology Committee Report, Evidence Check 2: Homeopathy (PDF, 69kb) but no comment is made on the findings.
Policy-based evidence
I wondered why the NHS Choices page, after an absence of almost two years, had returned in such an unsatisfactory form. So I asked them. After a reminder, I was told that my queries were being dealt with not by NHS Choices, but had been referred to Dr Sunjai Gupta “the DH official with responsibility for this area”. Dr Sunjai Gupta OBE is Deputy Director of Public Health Strategy and Social Marketing, Department of Health.
Dr Gupta is not obviously sympathetic to woo. It’s hard to tell since he doesn’t seem to have published much. But one is not reassured by an article that he wrote for the Journal of Holistic Healthcare. It appears straight after an article by fantasy herbalist, Simon Mills.
Despite assurances that I’d hear from Dr Gupta shortly, nothing happened. So I sent a request for the correspondence under the Freedom of Information Act (2000). Although the request was addressed to NHS Choices, a public body, strenuous efforts were made to divert it to the Department of Health. These were resisted. Nevertheless when, after a long delay, the material arrived, it came not from NHS Choices, but from DH, who had evidently vetted it,. The emails were rather shocking [download all].
A mail dated 1 December 2009 said
This is the most direct statement I’ve seen that, in the Department of Health, policy dictates evidence. NHS Choices is meant to provide evidence, but what they say has to be checked by DH to make sure they “don’t clash with any policy messages”.
The re-written page
The original version of the re-written page was sent to me by David Mattin, who worked for NHS Choices until September 2012. You can download the whole draft here. It is an enormous improvement on the original page. For example, it says
|
“Does it work?
Many independent experts would respond to this question ‘no, homeopathy does not work’ There is no good quality clinical evidence to show that homeopathy is more successful than placebo in the treatment of any type of condition. Furthermore, if the principles of homeopath were true it would violate all the existing theories of science that we make use of today; not just our theory of medicine, but also chemistry, biology and physics. |
This original draft was sent to Mattin on 29 January 2010. After editing it for length Mattin sent it to DH for approval. Over the next two years, DH removed much of the accurate content. Mattin’s own comments on this evisceration are reproduced below.
The DH emails
All the names have been redacted. Needless to say, nobody is willing to take responsibility. But the number of people who support magic medicine is really quite small so the main players were easy to identify.
During the nearly 2 year absence of the homeopathy page, dozens of changes were made by DH. It seems that the policy message with which the NHS Choices draft failed to comply were those of the Prince’s Foundation for Integrated Health, and its successor (after April 2010), the College of Integrated Health, now known as the College of Medicine.
NHS Choices sought advice about their redrafted pages from the right person, Sir Iain Chalmers, one of the founders of the Cochrane Collaboration. On 3 Nov 2009, Chalmers advised
The most reliable source in the country - and one of the most reliable in the world - is Professor Edzard Ernst, professor of Complementary Medicine at the Peninsular Medical School, |
Ernst returned his suggestions in July 2010, but it seems that few of them survived the subsequent 18 months of revisions by DH.
On 2 December 2009, a mail from the NHS headquarters (Quarry House, Leeds) was sent to NHS Choices
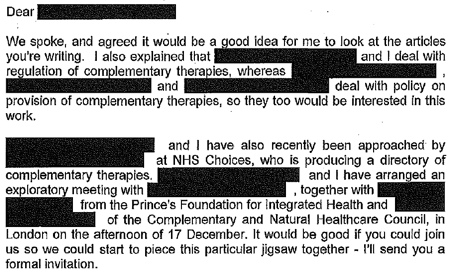
This makes it perfectly clear that DH regards the Prince’s Foundation, and the equally flaky Complementary and Natural Healthcare Council (CNHC: known on the web as Ofquack) as appropriate guides for public health policy. The fact of the matter is that regulation of magic medicine by the government has been a total disaster, because, it seems, DH regards the Prince of Wales as a reliable source.
On 29 December 2009, the Prince’s Foundation went on the attack.
On 10th January 2010, two more letters were sent to DH by the Prince’s Foundation. At 13.48 they wrote
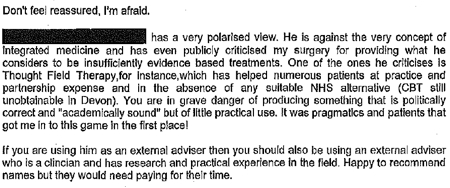
And at 22.14 on the same day, it was followed up with
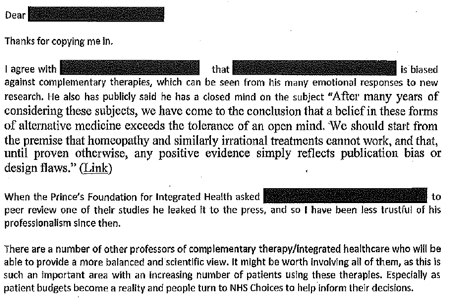
The references to Devon and to Thought Field Therapy, make it very obvious that these letters were written by Dr Michael Dixon OBE, who was medical director of the Prince’s Foundation, and who is now a director of the “College of Medicine”. And the object of Dixon’s bile is obviously Edzard Ernst (the quotation is from his book, Trick or Treatment).
I find it fascinating to see just how venomous quacks become when the evidence contradicts their views. The cuddly “holistic” veneer quickly vanishes.
It gets worse. On 21 January 2010, a mail from NHS Choices to DH said
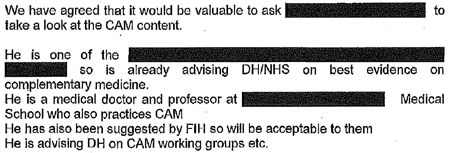
The only person in the country who fits this description is the (in)famous George Lewith. It is simply mind-boggling that DH regards him as an appropriate person to advise on anything.
After that, NHS Choices kept asking DH to sign off the documents, and changes continued to be made. Almost two years later, DH were still stalling.
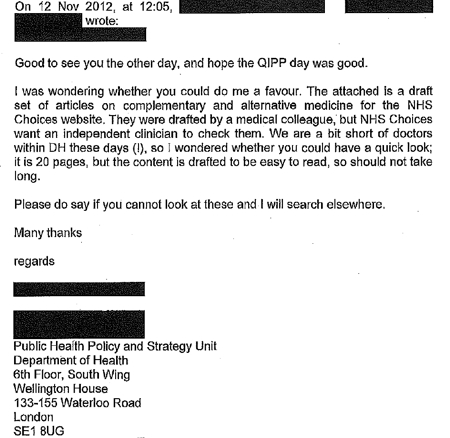
The admission that “We are a bit short of doctors within DH these days” is interesting.
A bit short of anyone capable of critical thinking would be more accurate.
The most interesting document that I got from DH was an intermediate draft of the rewritten page on homeopathy (undated). Download the document. Here are a couple of extracts.
It’s a story of two years of meddling and procrastination. The end result misinforms the public.
Right at the start, the NHS Choices draft says, reasonably enough
A House of Commons Science and Technology Committee report said that homeopathic remedies perform no better than placebos and that the principles on which homeopathv is based are “scientifically implausible”.
But a comment, added apparently by DH, says
Can we remove this statement? This report is really quite contentious and we may well be subject to quite a lot of challenge from the Homeopathic community if published.
What on earth? The DH seems to think that that its job is not to present the evidence, but to avoid challenges from the homeopathic community! And true enough, this piece is missing from the final version.
A bit later, the NHS Choices draft was censored again
“A 2010 Science and Technology Committee report said that scientific tests had shown that homeopathic treatments don’t work”
But again this doesn’t appear in the final version. The comment, apparently from DH, says
“The DH response to this report (point 24) doesn’t support this statement though”
That’s a gross distortion of point 24, which actually concludes
“The Government Chief Scientific Adviser cannot envisage scientifically credible proposals for funding for research into homeopathy in the future”
NHS Choices was not happy with the result
Shortly before the revised page was published, Paul Nuki, Editor in Chief of NHS Choicea, sent an email to DH.
|
Date: 7th September 2011 Time: 3:33:42 pm Hi I’ve been through the CAM articles and asked that we publish them asap as requested. For the record, we will be publishing these pieces outside of the normal editorial process. Although originally signed off by a suitably qualified clinician, the time lapse and policy changes have been so substantial as to render that null and void. We also don’t have a formal |
It doesn’t need much reading between the lines to see that he was unhappy with the result. It will be interesting to see whether the Information Standard people at the Royal Society for Public Health do anything about it.
The Department of Health has not just ignored evidence but actively opposed it.
That’s the only possible conclusion from the documents that I was sent. And it’s pretty shocking that the DH has preferred advice from the Prince’s Foundation and its handful of acolytes (in particular Michael Dixon and George Lewith) to the findings of the Science and Technology Select Committee and the views of the Chief Scientific Advisor.
In January this year, the Chief medical Officer, Dame Sally Davies, said, in a rare outburst of candour
|
‘I’m very concerned when homeopathic practitioners try to peddle this way of life to prevent malaria or other infectious disease,” she said. “I am perpetually surprised that homeopathy is available on the NHS.” Dame Sally, who is England’s most senior doctor, concluded by remarking that homeopathy “is rubbish”. |
 |
So one part of DH is working to contradict another part. the Chief Medical Officer. Perhaps Sally Davies should have a word with Dr Gupta.
This all predates the advent of Jeremy Hunt (and known defender of homeopathy) as health minister. But the sympathies of some DH people are made obvious by the presence on the DH web site of an article “Personal health budgets: A new way of accessing complementary therapies?”. This astonishing piece confirms the worst fears that quacks will see personal health budgets as a commercial opportunity to peddle their wares. The article is by Jim Rogers of Lincoln University. What his paper does not mention is Rogers’ conflict of interest. He’s a homeopath, and he has a paper in the International Journal of High Dilution Research (yes, there is a journal for every form of make-believe). You can download a reprint of this paper. It advocates more research into homeopathic provings, something that even George Lewith seems to have given up on.
It’s about time that the DH started to listen to the Chief Medical Officer. As it is, some people at DH seem to prefer the advice of the Prince’s Foundation, and to actively suppress employees who prefer evidence to anecdote.
One thing is clear. The DH is an unholy mess. Parts of it are intent on producing policy-based evidence.
Comment by David Mattin, who edited the first draft for NHS Choices
David Mattin left NHS Choices in September, 2012. He edited the new version and lived through the two years of wrangling with DH during which much of the best content was eviscerated. He sent me this statement about the affair.
|
As an editor at NHS Choices, I viewed it as my job to present evidence-based information to the public. The article we prepared on homeopathy stayed true to that central purpose: it made clear to readers that there is no good quality evidence that homeopathy is an effective treatment for any health condition, and also presented the broad scientific consensus that the supposed method of action of homeopathy is implausible.
What followed was a two year story of delay, and eventual suppression, of that article. My strong impression was of DH civil servants who lacked the courage, and, frankly, the energy to stand up to the criticism from special interest groups that they anticipated would arise because of the article; and that did indeed arise when a draft of the article and other draft content on complementary and alternative medicines fell into the hands of the Prince’s Foundation and other CAM groups.
The attitude of DH civil servants, broadly, was simply to tell us ‘we can’t say this about homeopathy, people will complain’. They seemed to have no interest in making an appraisal of the evidence on homeopathy themselves to see if what we were saying was actually true or not. We repeatedly pushed back with the message: ‘some people may very well complain, but if what we are saying about the evidence base is true – and it is – then we must simply weather those complaints, and stand by our content. Our duty is to supply our readers with the best information, not to please the homeopathy community.’ But these arguments were disregarded. The DH civil servants were almost entirely concerned with the politics of the situation – that is, the politics as they saw them – and the possibility that this article may create new work for them, and very little concerned with the evidence itself, or the presentation of this evidence to the public.
The whole episode is an insight into the way special interest groups can influence the workings of government and the public sector simply by making a lot of noise, and having a few powerful friends. In causing NHS Choices to publish content that is less than completely frank about the evidence on homeopathy, the DH have compromised the editorial standards of a website that they themselves established, and that they fund. They have sold out the NHS Choices editorial team, who work tirelessly to fulfil their remit. And, most seriously, they have failed the general public, by putting special interests, politics, and the path of least resistance (as they saw it) before the truth about health and healthcare.
|
Follow-up
13 February 2013 The Guardian version of this story, written by Sarah Boseley, is Prince’s charity lobbied government to water down homeopathy criticism. It’s fine as far as it goes but it doesn’t name any names. There are some good comments though.
14 February 2013. The printed Guardian gave the story full 5 column-width coverage. [download print version]
And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
On 14 February, the Guardian version was Editor’s Choice by lunchtime, and the Guardian web version already had 414 comments, mostly sensible (though this blog got far more referrals from twitter than from the Guardian)

And news has reached the USA: there’s an account of the affair on the Neurologica blog: Politics trumping science at the NHS.
15 February 2013. The Daily Mail had very fair coverage of the story.

The Guardian closed the comments on the story when it had got 642 comments, most of them very sensible. And this page got almost 6000 hits in 24 hours. The majority of the referrals came from Twitter rather than from the Guardian, despite the direct link to the page from the Guardian.
18 February 2013. The affair featured in BMJ News [download the reprint]. The item featured prominently on the BMJ news page.

19 February 2013 Only six days of this post, the NHS Choices page has been re-written again, in a much improved form. That looks like bloggers 1, DH 0. It is baffling that it’s left to bloggers, working for nothing, to extract a bit of sense from the highly-paid civil servants at the Department of Health. But at least they listened this time, which is a lot more than happens often. Paul Nuki, who runs NHS Choices, deserves congratulations. Of course the revised page still doesn’t call a spade a spade, but it gets close at times. I like the way it starts "Homeopathy is a ‘treatment’ based". Notice the quotation marks.
Reputation management?
Incidentally, NHS Choices is outsourced to the (in)famous company, Capita. And the moderation of the comments on their site is outsourced again to Tempero, which describes itself as a "reputation management" company. Each of them creams off money meant of patient care. This discovery might explain why I and others have had comments rejected by NHS Choices several times. "Reputation management" is the antithesis of evidence. It is public relations, i.e. paid lying. That is quite wrong for a site that is meant to provide dispassionate information.
21 February 2013. Sadly a step backwards. Part of the improved page was removed. This bit.
The Chief Medical Officer, Professor Dame Sally Davies, has said there is no scientifically plausible way that homeopathy can prevent or cure diseases. She has made it clear she is particularly concerned about the use of homeopathy in developing countries as a so-called cure for malaria.
We can only speculate why this was removed, because it was true. In fact she accurately described homeopathy as "rubbish". Why she should not be quoted beats me.
Nobody could have been more surprised than I when I found myself nominated as an academic role model at UCL. I had to answer a few questions. It is not obvious to me what the object of the stunt is, but the person who asked me to do it seemed to find the answers amusing, so I’ll reproduce here what I said. I apologise for the temporary lapse into narcissism.
The final version has now been printed [download a copy]. Sadly the printed edition was “corrected” by someone who replaced “whom I asked to submit the first theoretical paper by Hawkes and me to the Royal Society” (as written below), with “paper by Hawkes and I”. Aaargh.
Your nomination – Why you were nominated as an Academic Role Model?
"David Colquhoun has made major contributions to our understanding of how ion channels (proteins which allow charged ions to pass across cell membranes) function to mediate electrical signalling in nerve and muscle cells. This work elegantly combines experimental and theoretical aspects, and resulted in David being made a Fellow of the Royal Society. David Colquhoun played a key role in resisting the notion that UCL should merge with Imperial College in 2002, by running a website opposed to the merger. He thus facilitated the continued existence of an independent UCL. He is also well-known for his principled opposition to therapies that are not based on scientific evidence, and for his blog which comments on this issue as well as on university bureaucracy and politics."
Role models’ questions
1. What is your response to being nominated?
Astounded.
We are interested in giving people a very brief ‘snapshot’ description of their career trajectory, to help a broad range of people see how you got to where you are:
2. What has your career path been?
|
My first job (in 1950s) was as an apprentice pharmacist in Timothy Whites & Taylors (Homeopathic Chemists) in Grange Road, Birkenhead. You can’t get a more humble start than that. But it got me interested in drugs, and thanks to my schoolmaster father, I got to the University of Leeds. |
 My father (1907 – 2001), in 1955 |
|
One of the courses involved some statistics, and that interested me. I think I made a semi-conscious decision that it would be sensible to be good at something that others were bad at, so I learned quite a lot of statistics and mathematics. I recall buying a Methuen’s Monograph on Determinants and Matrices in my final year, and, with the help of an Argentinian PhD student in physical chemistry (not my lecturers) I began to make sense of it. |

|
I purposely went into my final viva with it sticking out of my pocket. The examiner was Walter Perry, then professor of Pharmacology in Edinburgh (he later did a great job setting up the Open University). That’s how I came to be a PhD student in Edinburgh.
Although Perry was one of my supervisors, the only time I saw him was when he came into my lab between committee meetings for a cigarette. But he did make me an honorary lecturer so I could join the Staff Club, where I made many friends, including a young physics lecturer called Peter Higgs. The staff club exists no longer, having been destroyed in one of those acts of short-sighted academic vandalism that vice-chancellors seem so fond of.
The great university expansion in the 1960s made it easy to get a job. The most famous pharmacology department in the world was at UCL so I asked someone to introduce me to its then head, Heinz Schild, and asked him if he had a job. While interned during WW2 he had written a paper on the statistics of biological assay and wanted someone to teach it to students, so I got a job (in 1964), and have been at UCL ever since apart from 9 years. Between 1964 and 1970 I published little, but learned a great deal by writing a textbook on statistics.
That sort of statistics is now thought too difficult for undergraduates, and the famous department that attracted me was itself destroyed in another act of academic vandalism, in 2007.
I have spent my life doing things that I enjoy. Such success as I’ve had, I attribute to a liking for spending time with people cleverer than I am, and wasting time drinking coffee. I found a very clever statistician, Alan Hawkes, in the Housman Room in the late 1960s, and we began to collaborate on the theory of single ion channel analysis in a series of papers that still isn’t quite finished. He did the hard mathematics, but I knew enough about it to write it up in a more or less comprehensible form and to write computer programs to evaluate the algebra. When I got stuck, I would often ask Hyman Kestelman (co-author of the famous mathematics textbook, Massie & Kestelman) to explain, usually in what was then the Joint Staff Common Room at lunch time (it is now the Haldane room, the common room having been confiscated by unenlightened management). Before leaving for the USA in 1970, I, in league with the then professor of French, Brian Woledge, eventually got through a motion that allowed women into the Housman room.
I’d also talk as much as I could to Bernard Katz, whom I asked to submit the first theoretical paper by Hawkes and me to the Royal Society. His comments on the first draft led to the published version making a prediction about single ion channel behaviour before channels could be observed.
The next step was sheer luck. As this was going on, two young Germans, Neher & Sakmann, succeeded in observing the tiny currents that flow through single ion channel molecules, so it became possible to test the theory. In series of visits to Göttingen, Sakmann and I did experiments late into the night. Neher & Sakmann got a well-deserved Nobel Prize in 1991, and I expect I benefitted from a bit of reflected glory
The work that I have done is nothing if not basic. It doesn’t fit in with the current vogue for translational research (most of which will fail), although I would regard it as laying the basis for rational drug design. My only regret is that rational drug design has proved to be so difficult that it won’t be achieved in my lifetime (please don’t believe the hype).
We’d also like you to take a slightly more personal view:
3. What have been the highs (and the lows?) of your career so far?
The highs have been the chance to work with brilliant people and write a handful of papers that have a chance of having a lasting influence. Because I have been able to take my time on those projects there haven’t been too many lows, apart from observing the continuous loss of academic integrity caused by the intense pressure to publish or perish, and the progressive decline in collegiality in universities caused by that pressure combined with the rise in power of managerialism. Luckily the advent of blogs has allowed me to do a little about that.
I’m saddened by the fact that the innumeracy of biologists that I noticed as an undergraduate has not really improved at all (though I don’t believe it is worse). Most biologists still have difficulty with even the simplest equations. Worse still, they don’t know enough maths to communicate their problem to a mathematician, so only too often one sees collaborations with mathematicians produce useless results.
The only real failure I’ve had was when, in a fit of vanity, I applied for the chair of Pharmacology in Oxford, in 1984, and failed to get it. But in retrospect that was really a success too. I would have hated the flummery of Oxford, and as head of department (an increasingly unattractive job) I would have spent my time on pushing paper, not ion channels. In retrospect, it was a lucky escape. UCL is my sort of place (most of the time).
We would like to hear what our role models have to say about the next generation:
4. What advice would you give to people finishing off their PhD?
My career course would be almost impossible now. In fact it is very likely that I would have been fired before I got going in the present climate. There were quite long periods when I didn’t publish much. I was learning the tools of my trade, both mathematical and experimental. Now there is no time to do that. You are under pressure to publish a paper a week (for the glory of your PI and your university) and probably rarely find time to leave the lab to talk to inspiring people. If you are given any courses they’ll probably be in some inane HR nonsense, not in algebra. That is one reason we started our summer workshop, though bizarrely that has now been dropped by the graduate school in favour of Advanced Powerpoint.
The plight of recent PhDs is dire. Too many are taken on (for the benefit of the university, not of the student) and there aren’t many academic jobs. If you want to stay in academia, all I can suggest is that you get good at doing something that other people can’t do, and to resist the pressure to publish dozens of trivial papers.
Try to maintain some academic integrity despite the many pressures to do the opposite that are imposed on you by your elders (but not always betters). That may or may not be enough to get you the job that you want, but at least you’ll be able to hold your head high.
Finally, we want to give a balanced impression of our role models because many were nominated for their ability to motivate others, and to balance life and work:
5. How do you keep motivated?
Work-life balance is much talked about by HR, though they are one of the reasons why it is now almost impossible, In the past it wasn’t a great problem. I’m fascinated by the problems that I’m trying to puzzle out. I’ve had periods of a year or two when things haven’t gone well and I’ve felt as though I was a failure, but luckily they haven’t lasted too long, and they occurred in a time before some idiotic performance manager would harass you for failing to publish for a year or two. The climate of “performance management” is doing a lot to kill innovation and creativity.
6. What do you do when are not working in SLMS?
I’ve had various phases. For a while I carried on boxing (which had been compulsory at school). When I was first at UCL in 1964 I bought a 21 foot sloop (and as a consequence could barely afford to eat), and in 1970 (at Yale) I learned to fly. I had a lot of fun sailing right up to the early 1980s, when I found I could not afford a son as well as a boat. That was when running came into fashion and that could be done for the price of a pair of shoes. I did marathons and half marathons for fun (the London in 1988 was great fun). And that was supplanted by walking country trails in the early 2000s.
There is never a clear division between work and play, especially with algebra. You can continue to struggle with a derivation on a boat, or even get a new angle on it while running. That, of course, is why the transparency review is such total nonsense.
The main cause of stress has never been work for me. Stress comes mainly from the imposition of dim-witted managerialism and incompetent HR policies. And that has become progressively worse. I doubt that if I were a young academic now I’d have the time to spend the weekend sailing.
I’m not sure whether the blogging that has taken up something like half my time since my nominal retirement in 2004 counts as work or not. It certainly depends on things that I have learned in my academic work. And it’s fun to have effects in the real world after a life spent on problems that many would regard as esoteric.
If you want a hobby that costs very little, and allows you to say what you want, start a blog.
Follow-up
|
This is a very important book. Buy it now (that link is to Waterstone’s Amazon don’t pay tax in the UK, so don’t use them). When you’ve read it, do something about it. The book has lots of suggestions about what to do. |

Stolen from badscience.net |
Peter Medawar, the eminent biologist, in his classic book Advice to a Young Scientist, said this.
“Exaggerated claims for the efficacy of a medicament are very seldom the consequence of any intention to deceive; they are usually the outcome of a kindly conspiracy in which everybody has the very best intentions. The patient wants to get well, his physician wants to have made him better, and the pharmaceutical company would have liked to have put it into the physician’s power to have made him so. The controlled clinical trial is an attempt to avoid being taken in by this conspiracy of good will.”
There was a lot of truth in that 1979, towards the end of the heyday of small molecule pharmacology. Since then, one can argue, things have gone downhill.
First, though, think of life without general anaesthetics, local anaesthetics, antibiotics, anticoagulants and many others. They work well and have done incalculable good. And they were developed by the drug industry.
But remember also that remarkably little is known about medicine. There are huge areas in which neither causes nor cures are known. Treatments for chronic pain, back problems, many sorts of cancer and almost all mental problems are a mess. It just isn’t known what to do. Nobody is to blame for this. Serious medical research has been going on for little more than 60 years, and it turns out to be very complicated. We are doing our best, but are still ignorant about whole huge areas. That leads to a temptation to make things up. Clutching at straws is very evident when it comes to depression, pain and Alzheimer’s disease, among others.
In order to improve matters, one essential is to do fair tests on treatments that we have. Ben Goldacre’s book is a superb account of how this could be done, and how the process of testing has been subverted for commercial gain and to satisfy the vanities of academics.
Of course there is nothing new in criticisms of Big Pharma. The huge fines levied on them for false advertising are well known. The difference is that Goldacre’s book explains clearly what’s gone wrong in great detail, documents it thoroughly, and makes concrete suggestions for improving matters.
Big Pharma has undoubtedly sometimes behaved appallingly in recent years. Someone should be in jail for crimes against patients. They have behaved in much the same way that bankers have. In any huge globalised industry it is always possible to blame someone in another department for the dishonesty. But they aren’t the only people to blame. None of the problems could have arisen with the complicity of academics, universities, and a plethora of regulatory agencies and professional bodies.
The biggest scandal of all is missing data (chapter 1). Companies, and sometmes academics, have suppressed of trials that don’t favour the drugs that they are trying to sell. The antidepressant drug, reboxetine, appeared at first to be good. It had been approved by the Medicines and Healthcare products Regulatory Agency (MHRA) and there was at least one good randomized placebo-controlled trial (RCT) showing it worked. But it didn’t. The manufacturer didn’t provide a complete list of unpublished trials when asked for them. After much work it was found in 2010 that, as well as the published, favourable trial, there were six more trials which had not been published and all six showed reboxetine to be no better than placebo . In comparisons with other antidepressant drugs three small studies (507 patients) showed reboxetine to be as good as its competitors. These were published. But it came to light that data on 1657 patients had never been published and these showed reboxetine to be worse than its rivals.
When all the data for the SSRI antidepressants were unearthed (Kirsch et al., 2008) it turned out that they were no better than placebo for mild or moderate depression. This selective suppression of negative data has happened time and time again. It harms patients and deceives doctors, but, incredibly, it’s not illegal.
Disgracefully, Kirsch et al. had to use a Freedom of Information Act request to get the data from the FDA.
“The output of a regulator is often simply a crude, brief summary: almost a ‘yes’ or ‘no’ about side effects. This is the opposite of science, which is only reliable because everyone shows their working, explains how they know that something is effective or safe, shares their methods and their results, and allows others to decide if they agree with the way they processed and analysed the data.”
|
“the NICE document discussing whether it’s a good idea to have Lucentis, an extremely expensive drug, costing well over £ 1,000 per treatment, that is injected into the eye for a condition called acute macular degeneration. As you can see, the NICE document on whether this treatment is a good idea is censored. Not only is the data on the effectiveness of the treatment blanked out by thick black rectangles, in case any doctor or patient should see it, but absurdly, even the names of some trials are missing, preventing the reader from even knowing of their existence, or cross referencing information about them.Most disturbing of all, as you can see in the last bullet point, the data on adverse events is also censored.”
|
The book lists all the tricks that are used by both industry and academics. Here are some of them.
- Regulatory agencies like the MHRA, the European Medicines Agency (EMA) and the US Food and Drugs Administration (FDA) set a low bar for approval of drugs.
- Companies make universities sign gagging agreements which allow unfavourable results to be suppressed, and their existence hidden.
- Accelerated approval schemes are abused to get quick approval of ineffective drugs and the promised proper tests often don’t materialise
- Disgracefully, even when all the results have been given to the regulatory agencies (which isn’t always). The MHRA, EMA and FDA don’t make them public. We are expected to take their word.
- Although all clinical trials are meant to be registered before they start, the EMA register, unbelievably, is not public. Furthermore there is no check that the results if trials ever get published. Despite mandates that results must be published within a year of finishing the trial, many aren’t. Journals promise to check this sort of thing, but they don’t.
- When the results are published, it is not uncommon for the primary outcome, specified before it started, to have been changed to one that looks like a more favourable result. Journals are meant to check, but mostly don’t.
- Companies use scientific conferences, phony journals, make-believe “seed trials” and “continuing medical education” for surreptitious advertising.
- Companies invent new diseases, plant papers to make you think you’re abnormal, and try to sell you a “cure”. For example, female sexual dysfunction , restless legs syndrome and social anxiety disorder (i.e. shyness). This is called disease-mongering, medicalisation or over-diagnosis. It’s bad.
- Spin is rife. Companies, and authors, want to talk up their results. University PR departments want to exaggerate benefits. Journal editors want sensational papers. Read the results, not the summary. This is universal (but particularly bad in alternative medicine).
- Companies fund patient groups to lobby for pills even when the pills are known to be ineffective. The lobby that demanded that Herceptin should be available to all on the breast cancer patients on the NHS was organised by a PR company working for the manufacturer, Roche. But Herceptin doesn’t work at all in 80% of patients and gives you at best a few extra months of life in advanced cases.
- Ghostwriting of papers is serious corruption. A company writes the paper and senior academics appear as the authors, though they may never have seen the original data. Even in cases where academics have admitted to lying about whether they have seen the data, they go unpunished by their universities. See for example, the case of Professor Eastell.
- By encouraging the funding of “continuing medical education” by companies, the great and the good of academic medicine have let us down badly.
This last point is where the book ends, and it’s worth amplification.
“So what have the great and good of British medicine done to help patients, in the face of this endemic corruption, and these systematic flaws? In 2012, a collaborative document was produced by senior figures in medicine from across the board, called ‘Guidance on Collaboration Between Healthcare Professionals and the Pharmaceutical Industry’. This document was jointly approved by the ABPI, the Department of Health, the Royal Colleges of Physicians, Nursing, Psychiatrists, GPs, the Lancet, the British Medical Association, the NHS Confederation, and so on. ”
“It contains no recognition of the serious problems we have seen in this book. In fact, quite the opposite: it makes a series of assertions about them that are factually incorrect.”
“It states that drug reps ‘can be a useful resource for healthcare professionals’. Again, I’m not sure why the Royal Colleges, the BMA, the Department of Health and the NHS Confederation felt the need to reassert this to the doctors of the UK, on behalf of industry, when the evidence shows that drug reps actively distort prescribing practices. But that is the battle you face, trying to get these issues taken seriously by the pinnacle of the medical establishment.”
This is perhaps the most shameful betrayal of all. The organisations that should protect patients have sold them out.
You may have been sold out by your “elders and betters”, but you can do something. The “What to do” sections of the book should be produced as a set of flash cards, as a reminder that matters can be improved.
It is shameful that this book was not written by a clinical pharmacologist, or a senior doctor, or a Royal College, or a senior academic. Why has the British Pharmacological Society said nothing?
It is shameful too that this book was not written by one of the quacks who are keen to defend the $60 billion alternative medicine industry (which has cured virtually nothing) and who are strident in their criticism of the 600 billion dollar Pharma industry. They haven’t done the work that Goldacre has to analyse the real problems. All they have done is to advocate unfair tests, because that is the only sort their treatments can pass.
It’s weird that medicine, the most caring profession, is more corrupt than any other branch of science. The reason, needless to say, is money. Well, money and vanity. The publish or perish mentality of senior academics encourages dishonesty. It is a threat to honest science.
Goldacre’s book shows the consequences: harm to patients and huge wastage of public money.
Read it.
Do something.
Follow-up
7 October, 2012, The Observer
Goldacre wrote
"I think it’s really disappointing that nobody, not the Royal Colleges, the Academy of Medical Sciences, the British Pharmacological Society, the British Medical Association, none of these organisations have stood up and said: selective non-publication of unflattering trial data is research misconduct, and if you do it you will be booted out. And I think they really urgently should."
Exactly.