chiropractic
This is my version of a post which I was asked to write for the Independent. It’s been published, though so many changes were made by the editor that I’m posting the original here (below).
Superstition is rife in all sports. Mostly it does no harm, and it might even have a placebo effect that’s sufficient to make a difference of 0.01%. That might just get you a medal. But what does matter is that superstition has given rise to an army of charlatans who are only to willing to sell their magic medicine to athletes, most of whom are not nearly as rich as Phelps.
So much has been said about cupping during the last week
that it’s hard to say much that’s original. Yesterday I did six radio interviews and two for TV, and today Associated Press TV came to film a piece about it. Everyone else must have been on holiday. The only one I’ve checked was the piece on the BBC News channel. That one didn’t seem to go too badly, so it’s here
BBC news coverage
It starts with the usual lengthy, but uninformative, pictures of someone being cupped, The cupper in this case was actually a chiropractor, Rizwhan Suleman. Chiropractic is, of course a totally different form of alternative medicine and its value has been totally discredited in the wake of the Simon Singh case. It’s not unusual for people to sell different therapies with conflicting beliefs. Truth is irrelevant. Once you’ve believed one impossible thing, it seems that the next ones become quite easy.
The presenter, Victoria Derbyshire, gave me a fair chance to debunk it afterwards.
Nevertheless, the programme suffered from the usual pretence that there is a controversy about the medical value of cupping. There isn’t. But despite Steve Jones’ excellent report to the BBC Trust, the media insist on giving equal time to flat-earth advocates. The report, (Review of impartiality and accuracy of the BBC’s coverage of science) was no doubt commissioned with good intentions, but it’s been largely ignored.
Still worse, the BBC News Channel, when it repeated the item (its cycle time is quite short) showed only Rizwhan Suleman and cut out my comments altogether. This is not false balance. It’s no balance whatsoever. A formal complaint has been sent. It is not the job of the BBC to provide free advertising to quacks.
After this, a friend drew my attention to a much worse programme on the subject.
The Jeremy Vine show on BBC Radio 2, at 12.00 on August 10th, 2016. This was presented by Vanessa Feltz. It was beyond appalling. There was absolutely zero attempt at balance, false or otherwise. The guest was described as being am "expert" on cupping. He was Yusef Noden, of the London Hijama Clinic, who "trained and qualified with the Hijama & Prophetic Medicine Institute". No doubt he’s a nice bloke, but he really could use a first year course in physiology. His words were pure make-believe. His repeated statements about "withdrawing toxins" are well know to be absolutely untrue. It was embarrassing to listen to. If you really want to hear it, here is an audio recording.
The Jeremy Vine show
This programme is one of the worst cases I’ve heard of the BBC mis-educating the public by providing free advertising for quite outrageous quackery. Another complaint will be submitted. The only form of opposition was a few callers who pointed out the nonsense, mixed with callers who endorsed it. That is not, by any stretch of the imagination, fair and balanced.
It’s interesting that, although cupping is often associated with Traditional Chinese Medicine, neither of the proponents in these two shows was Chinese, but rather they were Muslim. This should not be surprising as neither cupping nor acupuncture are exclusively Chinese. Similar myths have arisen in many places. My first encounter with this particular branch of magic medicine was when I was asked to make a podcast for “Things Unseen”, in which I debated with a Muslim hijama practitioner and an Indian Ayurvedic practitioner. It’s even harder to talk sense to practitioners of magic medicine who believe that god is on their side, as well as believing that selling nonsense is a good way to make a living.
An excellent history of the complex emergence of similar myths in different parts of the world has been published by Ben Kavoussi, under the title "Acupuncture is astrology with needles".
Now the original version of my blog for the Independent.
Cupping: Michael Phelps and Gwyneth Paltrow may be believers, but the truth behind it is what really sucks
The sight of Olympic swimmer, Michael Phelps, with bruises on his body caused by cupping resulted in something of a media feeding-frenzy this week. He’s a great athlete so cupping must be responsible for his performance, right? Just as cupping must be responsible for the complexion of an earlier enthusiast, Gwyneth Paltrow.
The main thing in common between Phelps and Paltrow is that they both have a great deal of money, and neither has much interest in how you distinguish truth from myth. They can afford to indulge any whim, however silly.
And cupping is pretty silly. It’s a pre-scientific medical practice that started in a time when there was no understanding of physiology, much like bloodletting. Indeed one version does involve a bit of bloodletting. Perhaps bloodletting is the best argument against the belief that it’s ancient wisdom, so it must work. It was a standard part of medical treatment for hundreds of years, and killed countless people.
It is desperately implausible that putting suction cups on your skin would benefit anything, so it’s not surprising that there is no worthwhile empirical evidence that it does. The Chinese version of cupping is related to acupuncture and, unlike cupping, acupuncture has been very thoroughly tested. Over 3000 trials have failed to show any benefit that’s big enough to benefit patients. Acupuncture is no more than a theatrical placebo. And even its placebo effects are too small to be useful.
At least it’s likely that cupping usually does no lasting damage.. We don’t know for sure because in the world of alternative medicine there is no system for recording bad effects (and there is a vested interest in not reporting them). In extreme cases, it can leave holes in your skin that pose a serious danger of infection, but most people probably end up with just broken capillaries and bruises. Why would anyone want that?
The answer to that question seems to be a mixture of wishful thinking about the benefits and vastly exaggerated claims made by the people who sell the product.
It’s typical that the sales people can’t even agree on what the benefits are alleged to be. If selling to athletes, the claim may be that it relieves pain, or that it aids recovery, or that it increases performance. Exactly the same cupping methods are sold to celebs with the claim that their beauty will be improved because cupping will “boost your immune system”. This claim is universal in the world of make-believe medicine, when the salespeople can think of nothing else. There is no surer sign of quackery. It means nothing whatsoever. No procedure is known to boost your immune system. And even if anything did, it would be more likely to cause inflammation and blood clots than to help you run faster or improve your complexion.
It’s certainly most unlikely that sucking up bits of skin into evacuated jars would have any noticeable effect on blood flow in underlying muscles, and so increase your performance. The salespeople would undoubtedly benefit from a first year physiology course.
Needless to say, they haven’t tried to actually measuring blood flow, or performance. To do that might reduce sales. As Kate Carter said recently “Eating jam out of those jars would probably have a more significant physical impact”.
The problem with all sports medicine is that tiny effects could make a difference. When three hour endurance events end with a second or so separating the winner from the rest, that is an effect of less than 0.01%. Such tiny effects will never be detectable experimentally. That leaves the door open to every charlatan to sell miracle treatments that might just work. If, like steroids, they do work, there is a good chance that they’ll harm your health in the long run.
You might be better off eating the jam.
Here is a very small selection of the many excellent accounts of cupping on the web.
There have been many good blogs. The mainstream media have, on the whole, been dire. Here are three that I like,
|
In July 2016, Orac posted in ScienceBlogs. "What’s the harm? Cupping edition". He used his expertise as a surgeon to explain the appalling wounds that can be produced by excessive cupping. |
 Photo from news,com.au |
Timothy Caulfield, wrote "Olympic debunk!". He’s Chair in Health Law and Policy at the University of Alberta, and the author of Is Gwyneth Paltrow Wrong about Everything.
“The Olympics are a wonderful celebration of athletic performance. But they have also become an international festival of sports pseudoscience. It will take an Olympic–sized effort to fight this bunk and bring a win to the side of evidence-based practice.”
Jennifer Raff wrote Pseudoscience is common among elite athletes outside of the Olympics too…and it makes me furious. She works on the genomes of modern and ancient people at the University of Kansas, and, as though that were not a full-time job for most people, she writes blogs, books and she’s also "training (and occasionally competing) in Muay Thai, boxing, BJJ, and MMA".
"I’m completely unsurprised to find that pseudoscience is common among the elite athletes competing in the Olympics. I’ve seen similar things rampant in the combat sports world as well."
What she writes makes perfect sense. Just don’t bother with the comments section which is littered with Trump-like post-factual comments from anonymous conspiracy theorists.
Follow-up
|
“Statistical regression to the mean predicts that patients selected for abnormalcy will, on the average, tend to improve. We argue that most improvements attributed to the placebo effect are actually instances of statistical regression.”
“Thus, we urge caution in interpreting patient improvements as causal effects of our actions and should avoid the conceit of assuming that our personal presence has strong healing powers.” |
In 1955, Henry Beecher published "The Powerful Placebo". I was in my second undergraduate year when it appeared. And for many decades after that I took it literally, They looked at 15 studies and found that an average 35% of them got "satisfactory relief" when given a placebo. This number got embedded in pharmacological folk-lore. He also mentioned that the relief provided by placebo was greatest in patients who were most ill.
Consider the common experiment in which a new treatment is compared with a placebo, in a double-blind randomised controlled trial (RCT). It’s common to call the responses measured in the placebo group the placebo response. But that is very misleading, and here’s why.
The responses seen in the group of patients that are treated with placebo arise from two quite different processes. One is the genuine psychosomatic placebo effect. This effect gives genuine (though small) benefit to the patient. The other contribution comes from the get-better-anyway effect. This is a statistical artefact and it provides no benefit whatsoever to patients. There is now increasing evidence that the latter effect is much bigger than the former.
How can you distinguish between real placebo effects and get-better-anyway effect?
The only way to measure the size of genuine placebo effects is to compare in an RCT the effect of a dummy treatment with the effect of no treatment at all. Most trials don’t have a no-treatment arm, but enough do that estimates can be made. For example, a Cochrane review by Hróbjartsson & Gøtzsche (2010) looked at a wide variety of clinical conditions. Their conclusion was:
“We did not find that placebo interventions have important clinical effects in general. However, in certain settings placebo interventions can influence patient-reported outcomes, especially pain and nausea, though it is difficult to distinguish patient-reported effects of placebo from biased reporting.”
In some cases, the placebo effect is barely there at all. In a non-blind comparison of acupuncture and no acupuncture, the responses were essentially indistinguishable (despite what the authors and the journal said). See "Acupuncturists show that acupuncture doesn’t work, but conclude the opposite"
So the placebo effect, though a real phenomenon, seems to be quite small. In most cases it is so small that it would be barely perceptible to most patients. Most of the reason why so many people think that medicines work when they don’t isn’t a result of the placebo response, but it’s the result of a statistical artefact.
Regression to the mean is a potent source of deception
The get-better-anyway effect has a technical name, regression to the mean. It has been understood since Francis Galton described it in 1886 (see Senn, 2011 for the history). It is a statistical phenomenon, and it can be treated mathematically (see references, below). But when you think about it, it’s simply common sense.
You tend to go for treatment when your condition is bad, and when you are at your worst, then a bit later you’re likely to be better, The great biologist, Peter Medawar comments thus.
|
"If a person is (a) poorly, (b) receives treatment intended to make him better, and (c) gets better, then no power of reasoning known to medical science can convince him that it may not have been the treatment that restored his health"
(Medawar, P.B. (1969:19). The Art of the Soluble: Creativity and originality in science. Penguin Books: Harmondsworth). |
This is illustrated beautifully by measurements made by McGorry et al., (2001). Patients with low back pain recorded their pain (on a 10 point scale) every day for 5 months (they were allowed to take analgesics ad lib).
The results for four patients are shown in their Figure 2. On average they stay fairly constant over five months, but they fluctuate enormously, with different patterns for each patient. Painful episodes that last for 2 to 9 days are interspersed with periods of lower pain or none at all. It is very obvious that if these patients had gone for treatment at the peak of their pain, then a while later they would feel better, even if they were not actually treated. And if they had been treated, the treatment would have been declared a success, despite the fact that the patient derived no benefit whatsoever from it. This entirely artefactual benefit would be the biggest for the patients that fluctuate the most (e.g this in panels a and d of the Figure).
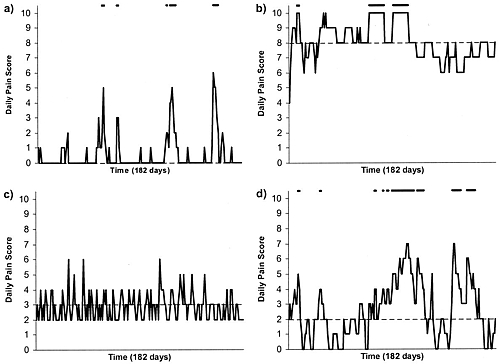
Figure 2 from McGorry et al, 2000. Examples of daily pain scores over a 6-month period for four participants. Note: Dashes of different lengths at the top of a figure designate an episode and its duration.
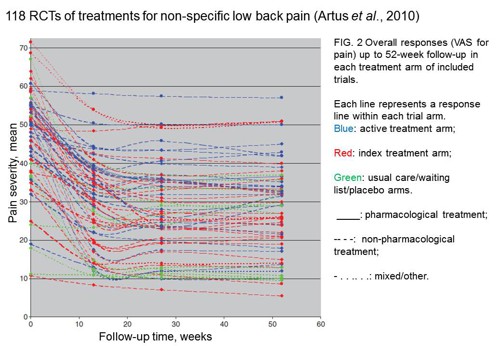
The effect is illustrated well by an analysis of 118 trials of treatments for non-specific low back pain (NSLBP), by Artus et al., (2010). The time course of pain (rated on a 100 point visual analogue pain scale) is shown in their Figure 2. There is a modest improvement in pain over a few weeks, but this happens regardless of what treatment is given, including no treatment whatsoever.
FIG. 2 Overall responses (VAS for pain) up to 52-week follow-up in each treatment arm of included trials. Each line represents a response line within each trial arm. Red: index treatment arm; Blue: active treatment arm; Green: usual care/waiting list/placebo arms. ____: pharmacological treatment; – – – -: non-pharmacological treatment; . . .. . .: mixed/other.
The authors comment
"symptoms seem to improve in a similar pattern in clinical trials following a wide variety of active as well as inactive treatments.", and "The common pattern of responses could, for a large part, be explained by the natural history of NSLBP".
In other words, none of the treatments work.
This paper was brought to my attention through the blog run by the excellent physiotherapist, Neil O’Connell. He comments
"If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery."
O’Connell has discussed the matter in recent paper, O’Connell (2015), from the point of view of manipulative therapies. That’s an area where there has been resistance to doing proper RCTs, with many people saying that it’s better to look at “real world” outcomes. This usually means that you look at how a patient changes after treatment. The hazards of this procedure are obvious from Artus et al.,Fig 2, above. It maximises the risk of being deceived by regression to the mean. As O’Connell commented
"Within-patient change in outcome might tell us how much an individual’s condition improved, but it does not tell us how much of this improvement was due to treatment."
In order to eliminate this effect it’s essential to do a proper RCT with control and treatment groups tested in parallel. When that’s done the control group shows the same regression to the mean as the treatment group. and any additional response in the latter can confidently attributed to the treatment. Anything short of that is whistling in the wind.
Needless to say, the suboptimal methods are most popular in areas where real effectiveness is small or non-existent. This, sad to say, includes low back pain. It also includes just about every treatment that comes under the heading of alternative medicine. Although these problems have been understood for over a century, it remains true that
|
"It is difficult to get a man to understand something, when his salary depends upon his not understanding it."
Upton Sinclair (1935) |
Responders and non-responders?
One excuse that’s commonly used when a treatment shows only a small effect in proper RCTs is to assert that the treatment actually has a good effect, but only in a subgroup of patients ("responders") while others don’t respond at all ("non-responders"). For example, this argument is often used in studies of anti-depressants and of manipulative therapies. And it’s universal in alternative medicine.
There’s a striking similarity between the narrative used by homeopaths and those who are struggling to treat depression. The pill may not work for many weeks. If the first sort of pill doesn’t work try another sort. You may get worse before you get better. One is reminded, inexorably, of Voltaire’s aphorism "The art of medicine consists in amusing the patient while nature cures the disease".
There is only a handful of cases in which a clear distinction can be made between responders and non-responders. Most often what’s observed is a smear of different responses to the same treatment -and the greater the variability, the greater is the chance of being deceived by regression to the mean.
For example, Thase et al., (2011) looked at responses to escitalopram, an SSRI antidepressant. They attempted to divide patients into responders and non-responders. An example (Fig 1a in their paper) is shown.
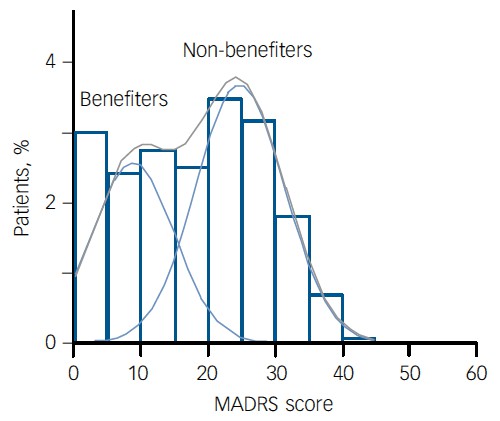
The evidence for such a bimodal distribution is certainly very far from obvious. The observations are just smeared out. Nonetheless, the authors conclude
"Our findings indicate that what appears to be a modest effect in the grouped data – on the boundary of clinical significance, as suggested above – is actually a very large effect for a subset of patients who benefited more from escitalopram than from placebo treatment. "
I guess that interpretation could be right, but it seems more likely to be a marketing tool. Before you read the paper, check the authors’ conflicts of interest.
The bottom line is that analyses that divide patients into responders and non-responders are reliable only if that can be done before the trial starts. Retrospective analyses are unreliable and unconvincing.
Some more reading
Senn, 2011 provides an excellent introduction (and some interesting history). The subtitle is
"Here Stephen Senn examines one of Galton’s most important statistical legacies – one that is at once so trivial that it is blindingly obvious, and so deep that many scientists spend their whole career being fooled by it."
The examples in this paper are extended in Senn (2009), “Three things that every medical writer should know about statistics”. The three things are regression to the mean, the error of the transposed conditional and individual response.
You can read slightly more technical accounts of regression to the mean in McDonald & Mazzuca (1983) "How much of the placebo effect is statistical regression" (two quotations from this paper opened this post), and in Stephen Senn (2015) "Mastering variation: variance components and personalised medicine". In 1988 Senn published some corrections to the maths in McDonald (1983).
The trials that were used by Hróbjartsson & Gøtzsche (2010) to investigate the comparison between placebo and no treatment were looked at again by Howick et al., (2013), who found that in many of them the difference between treatment and placebo was also small. Most of the treatments did not work very well.
Regression to the mean is not just a medical deceiver: it’s everywhere
Although this post has concentrated on deception in medicine, it’s worth noting that the phenomenon of regression to the mean can cause wrong inferences in almost any area where you look at change from baseline. A classical example concern concerns the effectiveness of speed cameras. They tend to be installed after a spate of accidents, and if the accident rate is particularly high in one year it is likely to be lower the next year, regardless of whether a camera had been installed or not. To find the true reduction in accidents caused by installation of speed cameras, you would need to choose several similar sites and allocate them at random to have a camera or no camera. As in clinical trials. looking at the change from baseline can be very deceptive.
Statistical postscript
Lastly, remember that it you avoid all of these hazards of interpretation, and your test of significance gives P = 0.047. that does not mean you have discovered something. There is still a risk of at least 30% that your ‘positive’ result is a false positive. This is explained in Colquhoun (2014),"An investigation of the false discovery rate and the misinterpretation of p-values". I’ve suggested that one way to solve this problem is to use different words to describe P values: something like this.
|
P > 0.05 very weak evidence
P = 0.05 weak evidence: worth another look P = 0.01 moderate evidence for a real effect P = 0.001 strong evidence for real effect |
But notice that if your hypothesis is implausible, even these criteria are too weak. For example, if the treatment and placebo are identical (as would be the case if the treatment were a homeopathic pill) then it follows that 100% of positive tests are false positives.
Follow-up
12 December 2015
It’s worth mentioning that the question of responders versus non-responders is closely-related to the classical topic of bioassays that use quantal responses. In that field it was assumed that each participant had an individual effective dose (IED). That’s reasonable for the old-fashioned LD50 toxicity test: every animal will die after a sufficiently big dose. It’s less obviously right for ED50 (effective dose in 50% of individuals). The distribution of IEDs is critical, but it has very rarely been determined. The cumulative form of this distribution is what determines the shape of the dose-response curve for fraction of responders as a function of dose. Linearisation of this curve, by means of the probit transformation used to be a staple of biological assay. This topic is discussed in Chapter 10 of Lectures on Biostatistics. And you can read some of the history on my blog about Some pharmacological history: an exam from 1959.
It makes a nice change to be able to compliment an official government report.
|
Ever since the House of Lords report in 2000, the government has been vacillating about what should be done about herbalists. At the moment both western herbalists and traditional Chinese medicine (TCM) are essentially unregulated. Many (but not all) herbalists have been pushing for statutory regulation, which they see as government endorsement. It would give them a status like the General Medical Council. |
|
A new report has ruled out this possibility, for very good reasons [download local copy].
Back story (abridged!)
My involvement began with the publication in 2008 of a report on the Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine . That led to my post, A very bad report: gamma minus for the vice-chancellor. The report was chaired by the late Professor Michael Pittilo BSc PhD CBiol FIBiol FIBMS FRSH FLS FRSA, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The membership of the group consisted entirely of quacks and the vice -chancellor’s university ran a course in homeopathy (now closed).
The Pittilo report recommended statutory regulation and "The threshold entry route to the register will normally be through a Bachelor degree with Honours". It ignored entirely the little problem that you can’t run a BSc degree in a subject that’s almost entirely devoid of evidence. It said, for example that acupuncturists must understand " yin/yang, 5 elements/phases, eight principles, cyclical rhythms, qi ,blood and body fluids". But of course there is nothing to "understand"! They are all pre-scientific myths. This “training dilemma” was pointed out in one of my earliest posts, You’d think it was obvious, but nonetheless the then Labour government seemed to take this absurd report seriously.
In 2009 a consultation was held on the Pittilo report. I and many of my friends spent a lot of time pointing out the obvious. Eventually the problem was again kicked into the long grass.
The THR scheme
Meanwhile European regulations caused the creation of the Traditional Herbal Registration (THR) scheme. It’s run by the Medicines and Healthcare products Regulatory Authority (MHRA). This makes it legal to put totally misleading claims on labels of herbal concoctions, as long as they are registered with THR, They also get an impressive-looking certification mark. All that’s needed to get THR registration is that the ‘medicines’ are not obviously toxic and they have been in use for 30 years. There is no need to supply any information whatsoever about whether they work or not. This appears to contradict directly the MHRA’s brief:
"”We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
After much effort, I elicited an admission from the MHRA that there was no reason to think that any herbal concoctions were effective, and that there was nothing to prevent them from adding a statement to say so on the label. They just chose not to do so. That’s totally irresponsible in my opinion. See Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me. Over 300 herbal products have been registered under the THR scheme (a small percentage of the number of products being used). So far only one product of Tibetan medicine and one traditional Chinese medicine have been registered under THR. These are the only ones that can be sold legally now, because no herbs whatsoever have achieved full marketing authorisation -that requires good evidence of efficacy and that doesn’t exist for any herb.
The current report
Eventually, in early 2014, the Tory-led government set up yet another body, "Herbal Medicines and Practitioners Working Group " (HMPWG). My heart sank when I saw its membership (Annex A.2). The vice-chair was none other that the notorious David Tredinnick MP (Con, Bosworth). It was stuffed with people who had vested interests. I wrote to the chair and to the few members with scientific credentials to put my views to them.
But my fears were unfounded, because the report of the HMPWG was not written by the group, but by its chair only. David Walker is deputy chief medical officer and he had clearly listened. Here are some quotations.
The good thing about the European laws is that
"This legislation effectively banned the importation and sale of large-scale manufactured herbal medicine products. This step severely limited the scope of some herbal practitioners to continue practising, particularly those from the Traditional Chinese Medicine (TCM) and Ayurvedic traditions."
The biggest loophole is that
"At present under UK law it is permitted for a herbal practitioner to see individual patients, offer diagnoses and prepare herbal treatments on their own premises, as long as these preparations do not contain banned or restricted substances. This is unchanged by the Traditional Herbal Medicinal Products Directive. "
Walker recognised frankly that there is essentially no good evidence that any herb, western or Chinese, works well enough to make an acceptable treatment. And importantly he, unlike Pittilo, realised that this precludes statutory regulation.
"There are a small number of studies indicating benefit from herbal medicine in a limited range of conditions but the majority of herbal medicine practice is not supported by good quality evidence. A great deal of international, primary research is of poor quality. "
"ts. Herbal medicine practice is therefore currently based upon traditional practice rather than science. It is difficult to differentiate good practice from poor practice on the basis of this evidence in a way that could establish standards for statutory regulation"
The second problem was the harms done by herbs. Herbalists, western and Chinese, have no satisfactory way of reporting side effects
" . . . there is very limited understanding of the risks to patient safety from herbal medicines and herbal practice. A review of safety data was commissioned from HMAC as part of this review. This review identified many anecdotal reports and case studies but little systematically collected data. Most herbal medicine products have not been through the rigorous licensing process that is required of conventional pharmaceutical products to establish their safety and efficacy. Indeed, only a small proportion have even been subject to the less rigorous Traditional Herbal Registration (THR) process. "
"The anecdotal evidence of risk to patients from herbal products in the safety review highlighted the prominence of manufactured herbal medicines in the high profile serious incidents which have been reported in recent years. Many of these reports relate to harm thought to be caused by industrially manufactured herbal products which contained either dangerous herbs, the wrong constituents, toxic contaminants or adulterants. All such industrially manufactured products are now only available under European regulations if their safety is assured through MHRA licensing or THR
accreditation; and specific dangerous herbs have been banned under UK law. This has weakened the case for introduction of statutory regulation as a further safety measure. "
Then Walker identified correctly the training dilemma. Although it seems obvious, this is a big advance for a government document. Degrees that teach nonsense are not good training: they are miseducation.
"The third issue is the identification of educational standards for training practitioners and the benchmarking of standards for accrediting practitioners. With no good data on efficacy or safety, it is difficult for practitioners and patients to understand or quantify the potential benefits and risks of a proposed therapeutic intervention. Training programmes could accredit knowledge and skills in some areas including pharmacology and physiology, professional ethics and infection control but without a credible evidence base relating to the safety and effectiveness of herbal medicine it is hard to see how they could form the basis of accreditation in this field of practice.
There are a number of educational university programmes offering courses in herbal medicine although the number has declined in recent years. Some of these courses are accredited by practitioner organisations which is a potential governance risk as the accreditation may be based on benchmarks established by tradition and custom rather than science.
"
"The herbal medicine sector is in a dilemma" is Walker’s conclusion.
"Some practitioners would like to continue to practise as
they do now, with no further regulation, and accept that their practice is based on tradition and personal experience rather than empirical science. The logical consequence of adopting this form of practice is that we should take a precautionary approach in order to ensure public safety. The public should be protected through consumer legislation to prevent false claims, restricting the use of herbal products which are known to be hazardous to health"
The problem with this is, if course, is that although there is plenty of law, it’s rarely enforced : see Most alternative medicine is illegal Trading Standards very rarely enforce the Consumer Protection Regulations (2008) but Walker is too diplomatic to mention that fact.
"The herbals sector must recognise that its overall approach (including the rationale for use of products and methods of treatment, education and training, and interaction with the NHS) needs to be more science and evidence based if in order to be established as a profession on the same basis as other groups that are statutorily regulated."
So what happens next?
In the short term nothing will happen.
The main mistake has been avoided: there wil be no statutory regulation.
The other options are (a) do nothing, or (b) go for accreditation of a voluntary register (AR) by the Professional Standards Authority for Health and Social Care (PSA). Walker ends up recommending the latter, but only after a lot more work (see pages 28-29 of report). Of particular interest is recommendation 5.
"As a first step it would be helpful for the sector organisations to develop an umbrella voluntary register that could support the development of standards and begin to collaborate on the collection of safety data and the establishment of an academic infrastructure to develop training and research. This voluntary register could in due course seek accreditation from the Professional Standards Authority for Health and Social Care (PSA)."
So it looks as though nothing will happen for a long time, and herbalists and TCM may end up with the utterly ineffectual PSA. After all, the PSA have accredited voluntary registers of homeopaths, so clearly nothing is too delusional for them. It’s very obvious that, unlike Walker, the PSA are quite happy to ignore the training dilemma.
Omissions from the report
Good though this report is, by Department of Health standards, it omits some important points.
Endangered species and animal cruelty aren’t mentioned in the report. Traditional Chinese medicine, and its variants, are responsible for the near-extinction of rhinoceros, tiger and other species because of the superstitious belief that they have medicinal value. It’s not uncommon to find animal parts in Chinese medicines sold in the UK despite it being illegal
And the unspeakably cruel practice of farming bears to collect bile is a direct consequence of TCM.

A bile bear in a “crush cage” on Huizhou Farm, China (Wikipedia)
Statutory regulation of Chiropractors
The same arguments used in Walker’s report to deny statutory regulation of herbalism, would undoubtedly lead to denial of statutory regulation of chiropractors. The General Chiropractic Council was established in 1994, and has a status that’s the same as the General Medical Council. That was a bad mistake. The GCC has not protected the public, in fact it has acted as an advertising agency for chiropractic quackery.
Perhaps Prof. Walker should be asked to review the matter.
Follow-up
You can also read minutes of the HMPWG meetings (and here). But, as usual, all the interesting controversies have been sanitised.
Edzard Ernst has also commented on this topic: Once again: the regulation of nonsense will generate nonsense – the case of UK herbalists.
A constant theme of this blog is that the NHS should not pay for useless treatments. By and large, NICE does a good job of preventing that. But NICE has not been allowed by the Department of Health to look at quackery.
I have the impression that privatisation of many NHS services will lead to an increase in the provision of myth-based therapies. That is part of the "bait and switch" tactic that quacks use in the hope of gaining respectability. A prime example is the "College of Medicine", financed by Capita and replete with quacks, as one would expect since it is the reincarnation of the Prince’s Foundation for Integrated Health.
One such treatment is acupuncture. Having very recently reviewed the evidence, we concluded that "Acupuncture is a theatrical placebo: the end of a myth". Any effects it may have are too small to be useful to patients. That’s the background for an interesting case study.
A colleague got a very painful frozen shoulder. His GP referred him to the Camden & Islington NHS Trust physiotherapy service. That service is now provided by a private company, Connect Physical Health.
That proved to be a big mistake. The first two appointments were not too bad, though they resulted in little improvement. But at the third appointment he was offered acupuncture. He hesitated, but agreed, in desperation to try it. It did no good. At the next appointment the condition was worse. After some very painful manipulation, the physiotherapist offered acupuncture again. This time he refused on the grounds that "I hadn’t noticed any effect the first time, because there is no evidence that it works and that I was concerned by her standards of hygiene". The physiotherapist then became "quite rude" and said that she would put down that the patient had refused treatment.
The lack of response was hardly surprising. NHS Evidence says
"There is no clinical evidence to show that other treatments, such as transcutaneous electrical nerve stimulation (TENS), Shiatsu massage or acupuncture are effective in treating frozen shoulder."
In fact it now seems beyond reasonable doubt that acupuncture is no more than a theatrical placebo.
According to Connect’s own web site “Our services are evidence-based”. That is evidently untrue in this case, so I asked them for the evidence that acupuncture was effective.
I’d noticed that in other places, Connect Physical Health also offers the obviously fraudulent craniosacral therapy (for example, here) and discredited chiropractic quackery. So I asked them about the evidence for their effectiveness too.
This is what they said.
|
Many thanks for your comments via our web site. In response, we thought you might like to access the sources for some of the evidence which underpins our MSK services: Integrating Evidence-Based Acupuncture into Physiotherapy for the Benefit of the Patient – you can obtain the information you require from www.aacp.org.uk The General Chiropractic Council www.gcc-uk.org/page.cfm We have also attached a copy of the NICE Guidelines. |
So, no Cochrane reviews, no NHS Evidence. Instead I was referred to the very quack organisations that promote the treatments in question, the Acupuncture Association of Chartered Physiotherapists, and the totally discredited General Chiropractic Council.
The NICE guidelines that they sent were nothing to do with frozen shoulder. They were the guidelines for low back pain which caused such a furore when they were first issued (and which, in any case, don’t recommend chiropractic explicitly).
When I pointed out these deficiencies I got this.
|
Your email below has been forwarded to me. I am sorry if you feel that that that information we pointed you towards to enable you to make your own investigations into the evidence base for the services provided by Connect Physical Health and your hospital did not meet with your expectations. ‘ ‘ ‘ Please understand that our NHS services in Camden were commissioned by the Primary Care Trust. The fully integrated MSK service model included provision for acupuncture and other manual therapy provided by our experienced Chartered Physiotherapists. If you have any problems with the evidence base for the use of acupuncture or manual therapy within the service, which has been commissioned on behalf of the GPs in Camden Borough, then I would politely recommend that you direct your observations to the clinical commissioning authorities and other professional bodies who do spend time evidencing best practice and representing the academic arguments. I am sure they will be pleased to pick up discussions with you about the relative merits of the interventions being procured by the NHS. Yours sincerely, Mark Mark Philpott BSc BSc MSc MMACP MCSP
Head of Operations, Community MSK Services Connect Physical Health 35 Apex Business Village Cramlington Northumberland NE23 7BF |
So, "don’t blame us, blame the PCT". A second letter asked why they were shirking the little matter of evidence.
|
In response to your last email, I would like to say that Connect does not wish to be drawn into a debate over two therapeutic options (acupuncture and craniosacral therapy) that are widely practiced [sic] within and outside the NHS by very respectable practitioners. You will be as aware, as Connect is, that there are lots of treatments that don’t have a huge evidence base that are practiced in mainstream medicine. Connect has seen many carefully selected patients helped by acupuncture and manual therapy (craniosacral therapy / chiropractic) over many years. Lack of evidence doesn’t mean they don’t work, just that benefit is not proven. Furthermore, nowhere on our website do we state that ALL treatments / services / modalities that Connect offer are ‘Evidence Based’. We do however offer many services that are evidence based, where the evidence exists. We aim to offer ‘choice’ to patients, from a range of services that are safe and delivered by suitably trained professionals and practitioners in line with Codes of Practice and Guidelines from the relevant governing bodies. Connect’s service provision in Camden is meticulously assessed and of a high standard and we are proud of the services provided. |
This response is so wrong, on so many levels, that I gave up on Mr Philpott at this point. At least he admitted implicitly that all of their treatments are not evidence-based. In that case their web site needs to change that claim.
If, by "governing bodies" he means jokes like the GCC or the CNHC then I suppose the behaviour of their employees is not surprising. Mr Philpott is evidently not aware that "craniosacral therapy" has been censured by the Advertising Standards Authority. Well he is now, but evidently doesn’t seem to give a damn.
Next I wrote to the PCT and it took several mails to find out who was responsible for the service. Three mails produced no response so I sent a Freedom of Information Act request. In the end I got some
"Connect PHC provide the Community musculoskeletal service for Camden. The specification for the service specifically asks for the provision of evidence based management and treatments see paragraph on Governance page 14 of attached.. Patients are treated with acupuncture as per the NICE Guidelines (May 2009) for the management of low back pain … . .. Chiropractors are not employed in the service and craniosacral therapy is not provided as part of the service either."
Another letter, pointing out that they were using acupuncture for things other than low back pain got no more information. They did send a copy of the contract with Connect. It makes no mention whatsoever of alternative treatments. It should have done, so part of the responsibility for the failure must lie with the PCT.
The contract does, however, say (page 18)
The service to be led by a lead clinician/manager who can effectively demonstrate ongoing and evidence-based development of clinical guidelines, policies and protocols for effective working practices within the service
In my opinion, Connect Physical Health are in breach of contract
Another example of Connect ignoring evidence
The Connect Physical Health web site has an article about osteoarthritis of the knee
Physiotherapy can be extremely beneficial to help to reduce the symptoms of OA. Treatments such as mobilizations, rehab exercises, acupuncture and taping can help to reduce pain, increase range of movement, increase muscle strength and aid return to functional activities and sports.
There is little enough evidence that physiotherapy does any of these things, but at least it is free of mystical mumbo-jumbo. Although at one time the claim for acupuncture was thought to have some truth, the 2010 Cochrane review concludes otherwise
Sham-controlled trials show statistically significant benefits; however, these benefits are small, do not meet our pre-defined thresholds for clinical relevance, and are probably due at least partially to placebo effects from incomplete blinding.
This conclusion is much the same as has been reached for acupuncture treatments of almost everything. Two major meta-analyses come to similar conclusions. Madsen Gøtzsche & Hróbjartsson (2009) and Vickers et al (2012) both conclude that if there is an effect at all (dubious) then it is too small to be noticeable to the patient. (Be warned that in the case of Vickers et al. you need to read the paper itself because of the spin placed on the results in the abstract.). These papers are discussed in detail in our recent paper.
Why is Connect Physical Health not aware of this?
Their head of operations told me (see above) that
"Connect does not wish to be drawn into a debate [about acupuncture and craniosacral therapy]".
That outlook was confirmed when I left a comment on their osteoarthritis post. This is what it looked like almost a month later.
Guess what? The comment has never appeared..
The attitude of Connect Physical Health to evidence is simply to ignore it if it gets in the way of making money, and to censor any criticism.
What have Camden NHS done about it?
The patient and I both complained to Camden NHS in August 2012. At first, they simply forwarded the complaints to Connect Physical Health with the unsatisfactory results shown above. It took until May 2013 to get any sort of reasonable response. That seems a very long time. In fact by the time the response arrived the PCT had been renamed a Clinical Commissioning Group (CCG) because of the vast top-down reorganisation inposed by Lansley’s Health and Social Care Act.
On 8 May 2013, this response was sent to the patient, Here is part of it.
|
I have received your email of complaint from the NHSNCL complaints department regarding your care. You raise some very clear concerns and I will attempt to address these in order. 1) The fact that you felt pressurised into having acupuncture is a concern as everybody should be given a choice. As part of the informed consent relating to acupuncture you should have been told about the treatment, it’s [sic] benefits and risks and then you sign to confirm you are happy to proceed. I understand that this was the case in your situation but I have reinforced that the consent is important and must be adhered to by the provider Connect Physical Health. There are clear standards of clinical practice that all Chartered Physiotherapists must follow which I will discuss further with the Connect Camden team Manager Nick Downing. I do disagree with you around acupuncture; there is no conclusive evidence for acupuncture in frozen shoulder but I have referenced a systematic review which concludes the studies were too small to draw any conclusions although shoulder function was significantly improved at 4 weeks (Green S et al. Acupuncture for shoulder pain. Cochrane Database Syst Rev 2005; 18: CD005319). There is a growing body of evidence supporting the use of acupuncture and until such time as there is specific evidence against it I don’t think we would be absolutely against the practice of this modality alongside other treatments. .Best wishes Strategy and Planning Directorate |
This response raises more questions than it answers.
For example, what is "informed consent" worth if the therapist is his/herself misinformed about the treatment? It is the eternal dilemma of alternative medicine that it is no use referring to well-trained practitioners, when their training has inculcated myths and untruths.
There is not a "growing body of evidence supporting the use of acupuncture". Precisely the opposite is true.
And the statement "until such time as there is specific evidence against it I don’t think we would be absolutely against the practice of this modality alongside" betrays a basic misunderstanding of the scientific process.
So I sent the writer of this letter a reprint of our paper, "Acupuncture is a theatrical placebo: the end of a myth" (the blog version alone has had over 12,000 page views). A few days later we had an amiable lunch together and we had a constructive discussion about the problems of deciding what should be commissioned and what shouldn’t.
It seems to me to be clear that CCGs should take better advice before boasting that they commission evidence-based treatments.
Postscript
Stories like this are worrying to the majority of physiotherapists who don’t go in for mystical mumbo-jumbo of acupuncture. One of the best is Neil O’Connell who blogs at BodyInMind. He tweeted
Physio fail, sigh RT@david_colquhoun: Yet more #acupuncture. Sold to the NHS by private contractor @ConnectPHC http://t.co/HylkwMCVTh
— Neil O'Connell (@NeilOConnell) June 10, 2013
It isn’t clear how many physiotherapists embrace nonsense, but the Acupuncture Association of Chartered Physiotherapists has around 6000 members, compared with 47,000 chartered physiotherapists (AACP), so it’s a smallish minority. The AACP claims that it is “Integrating Evidence-Based Acupuncture into Physiotherapy”. Like most politicians, the term “evidence-based” is thrown around with gay abandon. Clearly they don’t understand evidence.
Follow-up
12 June 2013
The Advertising Standards Authority has, one again, upheld complaints against the UCLH Trust, for making false claims in its advertising. This time, appropriately, it’s about acupuncture. Just about everything in their advertising leaflets was held to be unjustifiable. They’ve been in trouble before about false claims for homeopathy, hypnosis and craniosacral "therapy".
Of course all of these embarrassments come from one very small corner of the UCLH Trust, the Royal London Hospital for Integrated Medicine (previously known as the Royal London Homeopathic Hospital).
Why is it tolerated in an otherwise excellent NHS Trust? Well, the patron is the Queen herself (not Charles, aka the Quacktitioner Royal), She seems to exert more power behind the scenes than is desirable in In a constitutional monarchy
29 June 2013
I wrote to Dr Gill Gaskin about the latest ASA judgement against RLHIM. She is the person at the UCLH Trust who has responsibility for the quack hospital. She previously refused to do anything about the craniosacral nonsense that is promoted there. This time the ASA seems to have stung them into action at long last. I was told
|
In response to your question about proposed action: All written information for patients relating to the services offered by the Royal London Hospital for Integrated Medicine are being withdrawn for review in the light of the ASA’s rulings (and the patient leaflets have already been withdrawn). It will be reviewed and modified where necessary item by item, and only reintroduced after sign-off through the Queen Square divisional clinical governance processes and the Trust’s patient information leaflet team. With best wishes Gill Gaskin Dr Gill Gaskin |
It remains to be seen whether the re-written information is accurate or not.
The rules for advertising
The Advertising Standards Authority gives advice for advertisers about what’s permitted and what isn’t.
Acupuncture The CAP advice
Craniosacral therapy The CAP advice
Homeopathy The CAP advice and 2013 update
Chiropractic The CAP advice.
The Scottish Universities Medical Journal asked me to write about the regulation of alternative medicine. It’s an interesting topic and not easy to follow because of the veritable maze of more than twenty overlapping regulators and quangos which fail utterly to protect the public against health fraud. In fact they mostly promote health fraud. The paper is now published, and here is a version with embedded links (and some small updates).
We are witnessing an increasing commercialisation of medicine. It’s really taken off since the passage of the Health and Social Security Bill into law. Not only does that mean having NHS hospitals run by private companies, but it means that “any qualified provider” can bid for just about any service. The problem lies, of course, in what you consider “qualified” to mean. Any qualified homeopath or herbalist will, no doubt, be eligible. University College London Hospital advertised for a spiritual healer. The "person specification" specified a "quallfication", but only HR people think that a paper qualification means that spiritual healing is anything but a delusion.
The vocabulary of bait and switch
First, a bit of vocabulary. Alternative medicine is a term that is used for medical treatments that don’t work (or at least haven’t been shown to work). If they worked, they’d be called “medicine”. The anti-malarial, artemesinin, came originally from a Chinese herb, but once it had been purified and properly tested, it was no longer alternative. But the word alternative is not favoured by quacks. They prefer their nostrums to be described as “complementary” –it sounds more respectable. So CAM (complementary and alternative medicine became the politically-correct euphemism. Now it has gone a stage further, and the euphemism in vogue with quacks at the moment is “integrated” or “integrative” medicine. That means, very often, integrating things that don’t work with things that do. But it sounds fashionable. In reality it is designed to confuse politicians who ask for, say, integrated services for old people.
Put another way, the salespeople of quackery have become rather good at bait and switch. The wikepedia definition is as good as any.
Bait-and-switch is a form of fraud, most commonly used in retail sales but also applicable to other contexts. First, customers are “baited” by advertising for a product or service at a low price; second, the customers discover that the advertised good is not available and are “switched” to a costlier product.
As applied to the alternative medicine industry, the bait is usually in the form of some nice touchy-feely stuff which barely mentions the mystical nonsense. But when you’ve bought into it you get the whole panoply of nonsense. Steven Novella has written eloquently about the use of bait and switch in the USA to sell chiropractic, acupuncture, homeopathy and herbal medicine: "The bait is that CAM offers legitimate alternatives, the switch is that it primarily promotes treatments that don’t work or are at best untested and highly implausible.".
The "College of Medicine" provides a near-perfect example of bait and switch. It is the direct successor of the Prince of Wales’ Foundation for Integrated Health. The Prince’s Foundation was a consistent purveyor of dangerous medical myths. When it collapsed in 2010 because of a financial scandal, a company was formed called "The College for Integrated Health". A slide show, not meant for public consumption, said "The College represents a new strategy to take forward the vision of HRH Prince Charles". But it seems that too many people have now tumbled to the idea that "integrated", in this context, means barmpottery. Within less than a month, the new institution was renamed "The College of Medicine". That might be a deceptive name, but it’s a much better bait. That’s why I described the College as a fraud and delusion.
Not only did the directors, all of them quacks, devise a respectable sounding name, but they also succeeded in recruiting some respectable-sounding people to act as figureheads for the new organisation. The president of the College is Professor Sir Graham Catto, emeritus professor of medicine at the University of Aberdeen. Names like his make the bait sound even more plausible. He claims not to believe that homeopathy works, but seems quite happy to have a homeopathic pharmacist, Christine Glover, on the governing council of his college. At least half of the governing Council can safely be classified as quacks.
So the bait is clear. What about the switch? The first thing to notice is that the whole outfit is skewed towards private medicine: see The College of Medicine is in the pocket of Crapita Capita. The founder, and presumably the main provider of funds (they won’t say how much) is the huge outsourcing company, Capita. This is company known in Private Eye as Crapita. Their inefficiency is legendary. They are the folks who messed up the NHS computer system and the courts computer system. After swallowing large amounts of taxpayers’ money, they failed to deliver anything that worked. Their latest failure is the court translation service.. The president (Catto), the vice president (Harry Brunjes) and the CEO (Mark Ratnarajah) are all employees of Capita.
The second thing to notice is that their conferences and courses are a bizarre mixture of real medicine and pure quackery. Their 2012 conference had some very good speakers, but then it had a "herbal workshop" with Simon Mills (see a video) and David Peters (the man who tolerates dowsing as a way to diagnose which herb to give you). The other speaker was Dick Middleton, who represents the huge herbal company, Schwabe (I debated with him on BBC Breakfast), In fact the College’s Faculty of Self-care appears to resemble a marketing device for Schwabe.
Why regulation isn’t working, and can’t work
There are various levels of regulation. The "highest" level is the statutory regulation of osteopathy and chiropractic. The General Chiropractic Council (GCC) has exactly the same legal status as the General Medical Council (GMC). This ludicrous state of affairs arose because nobody in John Major’s government had enough scientific knowledge to realise that chiropractic, and some parts of osteopathy, are pure quackery,
The problem is that organisations like the GCC function more to promote chiropractic than to regulate them. This became very obvious when the British Chiropractic Association (BCA) decided to sue Simon Singh for defamation, after he described some of their treatments as “bogus”, “without a jot of evidence”.
In order to support Singh, several bloggers assessed the "plethora of evidence" which the BCA said could be used to justify their claims. When, 15 months later, the BCA produced its "plethora" it was shown within 24 hours that the evidence was pathetic. The demolition was summarised by lawyer, David Allen Green, in The BCA’s Worst Day.
In the wake of this, over 600 complaints were made to the GCC about unjustified claims made by chiropractors, thanks in large part to heroic work by two people, Simon Perry and Allan Henness. Simon Perry’s Fishbarrel (browser plugin) allows complaints to be made quickly and easily -try it). The majority of these complaints were rejected by the GCC, apparently on the grounds that chiropractors could not be blamed because the false claims had been endorsed by the GCC itself.
My own complaint was based on phone calls to two chiropractors, I was told such nonsense as "colic is down to, er um, faulty movement patterns in the spine". But my complaint never reached the Conduct and Competence committee because it had been judged by a preliminary investigating committee that there was no case to answer. The impression one got from this (very costly) exercise was that the GCC was there to protect chiropractors, not to protect the public.
The outcome was a disaster for chiropractors, wno emerged totally discredited. It was also a disaster for the GCC which was forced to admit that it hadn’t properly advised chiropractors about what they could and couldn’t claim. The recantation culminated in the GCC declaring, in August 2010, that the mythical "subluxation" is a "historical concept " "It is not supported by any clinical research evidence that would allow claims to be made that it is the cause of disease.". Subluxation was a product of the fevered imagination of the founder of the chiropractic cult, D.D. Palmer. It referred to an imaginary spinal lesion that he claimed to be the cause of most diseases. .Since ‘subluxation’ is the only thing that’s distinguished chiropractic from any other sort of manipulation, the admission by the GCC that it does not exist, after a century of pretending that it does, is quite an admission.
The President of the BCA himself admitted in November 2011
“The BCA sued Simon Singh personally for libel. In doing so, the BCA began one of the darkest periods in its history; one that was ultimately to cost it financially,”
As a result of all this, the deficiencies of chiropractic, and the deficiencies of its regulator were revealed, and advertisements for chiropractic are somewhat less misleading. But this change for the better was brought about entirely by the unpaid efforts of bloggers and a few journalists, and not at all by the official regulator, the GCC. which was part of the problem. not the solution. And it was certainly not helped by the organisation that is meant to regulate the GCC, the Council for Health Regulatory Excellence (CHRE) which did nothing whatsoever to stop the farce.
At the other end of the regulatory spectrum, voluntary self-regulation, is an even worse farce than the GCC. They all have grand sounding "Codes of Practice" which, in practice, the ignore totally.
The Society of Homeopaths is just a joke. When homeopaths were caught out recommending sugar pills for prevention of malaria, they did nothing (arguably such homicidal advice deserves a jail sentence).
The Complementary and Natural Healthcare Council (CNHC) is widely know in the blogosphere as Ofquack. I know about them from the inside, having been a member of their Conduct and Competence Committee, It was set up with the help of a £900,000 grant from the Department of Health to the Prince of Wales, to oversee voluntary self-regulation. It fails utterly to do anything useful.. The CNHC code of practice, paragraph 15 , states
“Any advertising you undertake in relation to your professional activities must be accurate. Advertisements must not be misleading, false, unfair or exaggerated”.
When Simon Perry made a complaint to the CNHC about claims being made by a CNHC-registered reflexologist, the Investigating Committee upheld all 15 complaints. But it then went on to say that there was no case to answer because the unjustified claims were what the person had been taught, and were made in good faith.
This is precisely the ludicrous situation which will occur again and again if reflexologists (and many other alternative therapies) are “accredited”. The CNHC said, correctly, that the reflexologist had been taught things that were not true, but then did nothing whatsoever about it apart from toning down the advertisements a bit. They still register reflexologists who make outrageously false claims.
Once again we see that no sensible regulation is possible for subjects that are pure make-believe.
The first two examples deal (or rather, fail to deal) with regulation of outright quackery. But there are dozens of other quangos that sound a lot more respectable.
European Food Standards Agency (EFSA). One of the common scams is to have have your favourite quack treatment classified as a food not as a medicine. The laws about what you can claim have been a lot laxer for foods. But the EFSA has done a pretty good job in stopping unjustified claims for health benefits from foods. Dozens of claims made by makers of probiotics have been banned. The food industry, needless to say, objects very strongly to be being forced to tell the truth. In my view, the ESFA has not gone far enough. They recently issued a directive about claims that could legally be made. Some of these betray the previously high standards of the EFSA. For example you are allowed to say that "Vitamin C contributes to the reduction of tiredness and fatigue" (as long as the product contains above a specified amount of Vitamin C. I’m not aware of any trials that show vitamin C has the slightest effect on tiredness or fatigue, Although these laws do not come into effect until December 2012, they have already been invoked by the ASA has a reason not to uphold a complaint about a multivitamin pill which claimed that it “Includes 8 nutrients that can contribute to the reduction in tiredness and fatigue”
The Advertising Standards Authority (ASA). This is almost the only organisation that has done a good job on false health claims. Their Guidance on Health Therapies & Evidence says
"Whether you use the words ‘treatment’, ‘treat’ or ‘cure’, all are likely to be seen by members of the public as claims to alleviate effectively a condition or symptom. We would advise that they are not used"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
They are spot on.
The ASA’s Guidance for Advertisers of Homeopathic Services is wonderful.
"In the simplest terms, you should avoid using efficacy claims, whether implied or direct,"
"To date, the ASA has have not seen persuasive evidence to support claims that homeopathy can treat, cure or relieve specific conditions or symptoms."
That seems to condemn the (mis)labelling allowed by the MHRA as breaking the rules.. Sadly, though, the ASA has no powers to enforce its decisions and only too often they are ignored. The Nightingale collaboration has produced an excellent letter that you can hand to any pharmacist who breaks the rules
The ASA has also judged against claims made by "Craniosacral therapists" (that’s the lunatic fringe of osteopathy). They will presumably uphold complaints about similar claims made (I’m ashamed to say) by UCLH Hospitals.
The private examination company Edexcel sets exams in antiscientific subjects, so miseducating children. The teaching of quackery to 16 year-olds has been approved by a maze of quangos, none of which will take responsibility, or justify their actions. So far I’ve located no fewer than eight of them. The Office of the Qualifications and Examinations Regulator (OfQual), Edexcel, the Qualifications and Curriculum Authority (QCA), Skills for Health, Skills for Care, National Occupational Standards (NOS), private exam company VTCT and the schools inspectorate, Ofsted.. Asking any of these people why they approve of examinations in imaginary subjects meets with blank incomprehension. They fail totally to protect tha public from utter nonsense.
The Department of Education has failed to do anything about the miseducation of children in quackery. In fact it has encouraged it by, for the first time, giving taxpayers’ money to a Steiner (Waldorf) school (at Frome, in Somerset). Steiner schools are run by a secretive and cult-like body of people (read about it). They teach about reincarnation, karma, gnomes, and all manner of nonsense, sometimes with unpleasant racial overtones. The teachers are trained in Steiner’s Anthroposophy, so if your child gets ill at school they’ll probably get homeopathic sugar pills. They might well get measles or mumps too, since Steiner people don’t believe in vaccination.
Incredibly, the University of Aberdeen came perilously close to appointing a chair in anthroposophical medicine. This disaster was aborted by bloggers, and a last minute intervention from journalists. Neither the university’s regulatory mechanisms. nor any others, seemed to realise that a chair in mystical barmpottery was a bad idea.
Trading Standards offices and the Office of Fair Trading.
It is the statutory duty of Trading Standards to enforce the Consumer Protection Regulations (2008) This European legislation is pretty good. it caused a lawyer to write " Has The UK Quietly Outlawed “Alternative” Medicine?". Unfortunately Trading Standards people have consistently refused to enforce these laws. The whole organisation is a mess. Its local office arrangement fails totally to deal with the age of the internet. The situation is so bad that a group of us decided to put them to the test. The results were published in the Medico-Legal Journal, Rose et al., 2012. "Spurious Claims for Health-care Products: An Experimental Approach to Evaluating Current UK Legislation and its Implementation". They concluded "EU directive 2005/29/EC is
largely ineffective in preventing misleading health claims for consumer products in
the UK"
Skills for Health is an enormous quango which produces HR style "competences" for everything under the son. They are mostly quite useless. But those concerned with alternative medicine are not just useless. They are positively harmful. Totally barmy. There are competences and National Occupational Standards for every lunatic made-up therapy under the sun. When I phoned them to discover who’d written them, I learned that the had been drafted by the Prince of Wales’ Foundation for Magic Medicine. And when I joked by asking if they had a competence for talking to trees, I was told, perfectly seriously, “You’d have to talk to LANTRA, the land-based organisation for that.”
That was in January 2008. A lot of correspondence with the head of Skills for Health got nowhere at all. She understood nothing and it hasn’t improved a jot.
This organisation costs a lot of taxpayers’ money and it should have been consigned to the "bonfire of the quangos" (but of course there was no such bonfire in reality). It is a disgrace.
The Quality Assurance Agency (QAA) is supposed to ensure the quality of university courses. In fact it endorses courses in nonsense alternative medicine and so does more harm than good. The worst recent failure of the QAA was in the case of the University of Wales: see Scandal of the University of Wales and the Quality Assurance Agency. The university was making money by validating thousands of external degrees in everything from fundamentalist theology to Chinese Medicine. These validations were revealed as utterly incompetent by bloggers, and later by BBC Wales journalist Ciaran Jenkins (now working for Channel 4).
The mainstream media eventually caught up with bloggers. In 2010, BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. The programme can be seen on YouTube (Part 1, and Part 2). The programme also exposed, incidentally, the uselessness of the Quality Assurance Agency (QAA) which did nothing until the scam was exposed by TV and blogs. Eventually the QAA sent nine people to Malaysia to investigate a dodgy college that had been revealed by the BBC. The trip cost £91,000. It could have been done for nothing if anyone at the QAA knew how to use Google.
The outcome was that the University of Wales stopped endorsing external courses, and it was soon shut down altogether (though bafflingly, its vice-chancellor, Marc Clement was promoted). The credit for this lies entirely with bloggers and the BBC. The QAA did nothing to help until the very last moment.
Throughout this saga Universities UK (UUK), has maintained its usual total passivity. They have done nothing whatsoever about their members who give BSc degrees in anti-scientific subjects. (UUK used to known as the Committee of Vice-Chancellors and Principals).
Council for Health Regulatory Excellence (CHRE), soon to become the PSAHSC,
Back now to the CHRE, the people who failed so signally to sort out the GCC. They are being reorganised. Their consultation document says
"The Health and Social Care Act 20122 confers a new function on the Professional Standards Authority for Health and Social Care (the renamed Council for Healthcare Regulatory Excellence). From November 2012 we will set standards for organisations that hold voluntary registers for people working in health and social care occupations and we will accredit the register if they meet those standards. It will then be known as an ‘Accredited Register’. "
They are trying to decide what the criteria should be for "accreditation" of a regulatory body. The list of those interested has some perfectly respectable organisations, like the British Psychological Society. It also contains a large number of crackpot organisations, like Crystal and Healing International, as well as joke regulators like the CNHC.
They already oversee the Health Professions Council (HPC) which is due to take over Herbal medicine and Traditional Chinese Medicine, with predictably disastrous consequences.
Two of the proposed criteria for "accreditation" appear to be directly contradictory.
Para 2.5 makes the whole accreditation pointless from the point of view of patients
2.5 It will not be an endorsement of the therapeutic validity or effectiveness of any particular discipline or treatment.
Since the only thing that matters to the patient is whether the therapy works (and is safe), accrediting of organisations that ignore this will merely give the appearance of official approval of crystal healing etc etc. This appears to contradict directly
A.7 The organisation can demonstrate that there either is a sound knowledge base underpinning the profession or it is developing one and makes that explicit to the public.
A "sound knowledge base", if it is to mean anything useful at all, means knowledge that the treatment is effective. If it doesn’t mean that, what does it mean?
It seems that the official mind has still not grasped the obvious fact that there can be no sensible regulation of subjects that are untrue nonsense. If it is nonsense, the only form of regulation that makes any sense is the law.
Please fill in the consultation. My completed return can be downloaded as an example, if you wish.
Medicines and Healthcare products Regulatory Agency (MHRA) should be a top level defender of truth. Its strapline is
"We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
The MHRA did something (they won’t tell me exactly what) about one of the most cruel scams that I’ve ever encountered, Esperanza Homeopathic Neuropeptide, peddled for multiple sclerosis, at an outrageous price ( £6,759 for 12 month’s supply). Needless to say there was not a jot of evidence that it worked (and it wasn’t actually homeopathic).
Astoundingly, Trading Standards officers refused to do anything about it.
The MHRA admit (when pushed really hard) that there is precious little evidence that any of the herbs work, and that homeopathy is nothing more than sugar pills. Their answer to that is to forget that bit about "ensuring that medicines … work"
Here’s the MHRA’s Traditional Herbal Registration Certificate for devils claw tablets.

The wording "based on traditional use only" has to be included because of European legislation. Shockingly, the MHRA have allowed them to relegate that to small print, with all the emphasis on the alleged indications. The pro-CAM agency NCCAM rates devil’s claw as "possibly effective" or "insufficient evidence" for all these indications, but that doesn’t matter because the MHRA requires no evidence whatsoever that the tablets do anything. They should, of course, added a statement to this effect to the label. They have failed in their duty to protect and inform the public by allowing this labelling.
But it gets worse. Here is the MHRA’s homeopathic marketing authorisation for the homeopathic medicinal product Arnicare Arnica 30c pillules
It is nothing short of surreal.
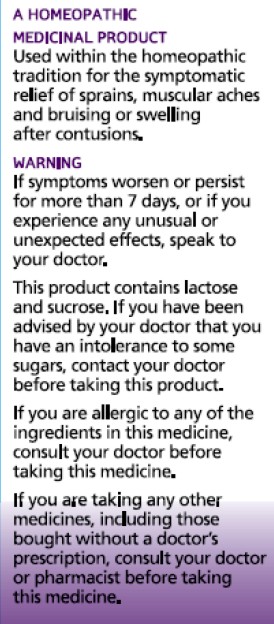
|
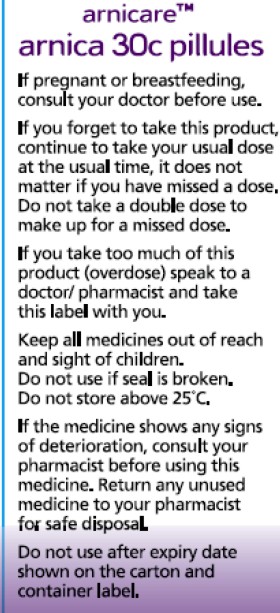
|
Since the pills contain nothing at all, they don’t have the slightest effect on sprains, muscular aches or bruising. The wording on the label is exceedingly misleading.
If you "pregnant or breastfeeding" there is no need to waste you doctor’s time before swallowing a few sugar pills.
"Do not take a double dose to make up for a missed one". Since the pills contain nothing, it doesn’t matter a damn.
"If you overdose . . " it won’t have the slightest effect because there is nothing in them
And it gets worse. The MHRA-approved label specifies ACTIVE INGREDIENT. Each pillule contains 30c Arnica Montana
No, they contain no arnica whatsoever.
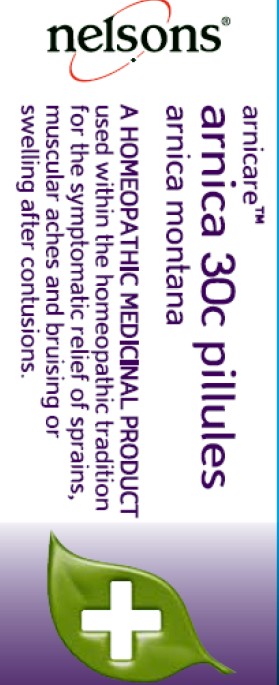
|
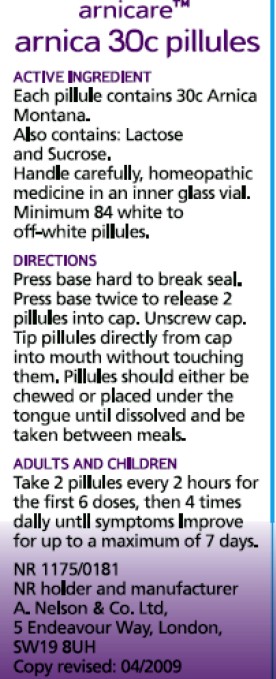
|
It truly boggles the mind that men with dark suits and lots of letters after their names have sat for hours only to produce dishonest and misleading labels like these.
When this mislabeling was first allowed, it was condemned by just about every scientific society, but the MHRA did nothing.
The Nightingale Collaboration.
This is an excellent organisation, set up by two very smart skeptics, Alan Henness and Maria MacLachlan. Visit their site regularly, sign up for their newsletter Help with their campaigns. Make a difference.
Conclusions
The regulation of alternative medicine in the UK is a farce. It is utterly ineffective in preventing deception of patients.
Such improvements as have occurred have resulted from the activity of bloggers, and sometime the mainstream media. All the official regulators have, to varying extents, made things worse.
The CHRE proposals promise to make matters still worse by offering "accreditation" to organisations that promote nonsensical quackery. None of the official regulators seem to be able to grasp the obvious fact that is impossible to have any sensible regulation of people who promote nonsensical untruths. One gets the impression that politicians are more concerned to protect the homeopathic (etc, etc) industry than they are to protect patients.
Deception by advocates of alternative medicine harms patients. There are adequate laws that make such deception illegal, but they are not being enforced. The CHRE and its successor should restrict themselves to real medicine. The money that they spend on pseudo-regulation of quacks should be transferred to the MHRA or a reformed Trading Standards organisation so they can afford to investigate and prosecute breaches of the law. That is the only form of regulation that makes sense.
Follow-up
The shocking case of the continuing sale of “homeopathic vaccines” for meningitis, rubella, pertussis etc was highlighted in an excellent TV programme by BBC South West. The failure of the MHRA and the GPC do take any effective action is a yet another illustration of the failure of regulators to do their job. I have to agree with Andy Lewis when he concludes
“Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator.”
We all know that chiropractors feel pretty desperate, after their job has been revealed as baseless (much more information at ebm-first). Nonetheless it was very surprising when I was alerted by Twitter to the fact that the London Chiropractors were claiming to have been chosen by UCL as a "Centre of Excellence".

That was the heading in the whole page devoted to crowing about this designation. The page, as it was on18th April, can be seen on freezepage.com. They even boast about our 21 Nobel prizewinners, as though they had endorsed chiropractic.
"London Chiropractor has recently been designated as a “Centre of Excellence” by University College London. The University is among the world’s leading universities as can be seen by its ranking in a variety of performance areas. Twenty-one Nobel prizewinners have come from the University’s community".
The triumphalist crowing goes on
"The designation of London Chiropractor as a Centre of Excellence is something that we are sincerely proud of. It distinguishes our clinic while providing impetus to carry on with our multi-disciplinary and evidence based treatment strategies while looking for new ways in which to improve on all aspects of our clinic at the same time and in a continuous manner."
But chiropractic is undoubtedly in deep trouble, after more that 600 complaints were submitted to the General Chiropractic Council (GCC). The GCC was forced to renounce what has always been a central myth of chiropractic, the "subluxation". The fact that most of the complaints have been rejected has revealed huge deficiencies in the GCC (some of which it recently admitted). It also reveals the uselessness of the Council for Health Regulatory Excellence (CHRE).which is meant to supervise them. More details at quackometer, Chiropractors at War with their Regulator, the GCC.
In the words of Richard Brown (president of the BCA) himself,
"The BCA sued Simon Singh personally for libel. In doing so, the BCA began one of the darkest periods in its history; one that was ultimately to cost it financially,"
Needless to say, chiropractors are trying to cash in on the Olympic games, sadly, with a little success. I suppose that invoking UCL. was part of that attempt. Like so many of chiropractors’ attempts to defend themselves, it misfired badly.
The inspection of evidence that followed the attempt by the British Chiropractic Association (BCA) to sue Simon Singh showed that he was entirely justified to describe many of their treatments as “bogus” and “without a jot of evidence”.
A quick email to the UCL authorities quickly determined that the claimed endorsement was not true. Attempting to access this page now leads to “page not found". The page vanished on Sunday 22nd April, and a near identical page for the Broadgate Spine and Joint Clinic had already vanished on Friday 20th April. While it is true that two surgeons from UCL’s Institute of Sports Medicine have worked in the same building, they neither use chiropractic nor endorse it.
I’m assured that the alleged endorsement never happened. London Chiropractors won’t say where it came from. It seems that it was simply made up. I think that’s called a lie. I presume it is a sign of the desperation of chiropractors.
Follow-up
Almost all the revelations about what’s taught on university courses in alternative medicine have come from post-1992 universities. (For readers not in the UK, post-1992 universities are the many new univerities created in 1992, from former polytechnics etc, and Russell group universities are the "top 20" research-intensive universities)
It is true that all the undergraduate courses are in post-1992 universities, but the advance of quackademia is by no means limited to them. The teaching at St Bartholomew’s Hospital Medical School, one of the oldest, was pretty disgraceful for example, though after protests from their own students, and from me, it is now better, I believe.

Quackery creeps into all universities to varying extents. The good ones (like Southampton) don’t run "BSc" degrees, but it still infiltrates through two main sources,
The first is via their HR departments, which are run by people who tend to be (I quote) "credulous and moronic" when it comes to science.
The other main source is in teaching to medical students. The General Medical Council says that medical students must know something about alterantive medicine and that’s quite right, A lot of their patients will use it. The problem is that the guidance is shockingly vague .
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
In many medical schools, the information that medical students get is quite accurate. At UCL and at King’s (London) I have done some of the familiarisation myself. In other good medical schools, the students get some shocking stuff. St Bartholomew’s Hospital medical School was one example. Edinburgh University was another.
But there is one Russell group university where alternative myths are propagated more than any other that I know about. That is the University of Southampton.
In general, Southampton is a good place, I worked there for three years myself (1972 – 1975). The very first noise spectra I measured were calculated on a PDP computer in their excellent Institute of Sound and Vibration Research, before I wrote my own programs to do it.
But Southanpton also has a The Complementary and Integrated Medicine Research Unit . Oddly the unit’s web site, http://www.cam-research-group.co.uk, is not a university address, and a search of the university’s web site for “Complementary and Integrated Medicine Research Unit” produces no result. Nevertheless the unit is “within the School of Medicine at the University of Southampton”
Notice the usual euphemisms ‘complementary’ and ‘integrated’ in the title: the word ‘alternative’ is never used. This sort of word play is part of the bait and switch approach of alternative medicine.
The unit is quite big: ten research staff, four PhD students and two support staff It is headed by George Lewith.
Teaching about alternative medicine to Southampton medical students.
The whole medical class seems to get quite a lot compared with other places I know about. That’s 250 students (210 on the 5-year course plus another 40 from the 4-year graduate-entry route).
Year 1: Lecture by David Owen on ‘holism’ within the Foundation Course given to all 210 medical students doing the standard (5-year) course.
Year 2: Lecture by Lewith (on complementary medicine, focusing on acupuncture for pain) given within the nervous systems course to the whole medical student year-group (210 students).
Year 3 SBOM (scientific basis of medicine) symposium: The 3-hour session (“Complementary or Alternative Medicine: You Decide”). I’m told that attendance at this symposium is often pretty low, but many do turn up and all of them are officially ‘expected’ to attend.
There is also an optional CAM special study module chosen by 20 students in year 3, but also a small number of medical students (perhaps 2 – 3 each year?) choose to do a BMedSci research project supervised by the CAM research group and involving 16-18 weeks of study from October to May in Year 4. The CAM research group also supervise postgraduate students doing PhD research.
As always, a list of lectures doesn’t tell you much. What we need to know is what’s taught to the students and something about the people who teach it. The other interesting question is how it comes about that alternative medicine has been allowed to become so prominent in a Russell group university. It must have support from on high. In this case it isn’t hard to find out where it comes from. Here are some details.
Year 1 Dr David Owen
David Owen is not part of Lewith’s group, but a member of the Division of Medical Education headed by Dr Faith Hill (of whom, more below). He’s one of the many part-time academics in this area, being also a founder of The Natural Practice .
Owen is an advocate of homeopathy (a past president of the Faculty of Homeopathy). Homeopathy is, of course, the most barmy and discredited of all the popular sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes it).
And he’s also a member of the British Society of Environmental Medicine (BSEM). That sounds like a very respectable title, but don’t be deceived. It is an organisation that promotes all sorts of seriously fringe ideas. All you have to do is notice that the star speaker at their 2011 conference was none other than used-to-be a doctor, Andrew Wakefield, a man who has been responsible for the death of children from measles by causing an unfounded scare about vaccination on the basis of data that turned out to have been falsified. There is still a letter of support for Wakefield on the BSEM web site.
The BSEM specialises in exaggerated claims about ‘environmental toxins’ and uses phony allergy tests like kinesiology and the Vega test that misdiagnose allergies, but provide en excuse to prescribe expensive but unproven nutritional supplements, or expensive psychobabble like "neuro-linguistic programming".
Other registered "ecological physicians" include the infamous Dr Sarah Myhill, who, in 2010, was the subject of a damning verdict by the GMC, and Southampton’s George Lewith.
If it is wrong to expose medical students to someone who believes that dose-response curves have a negative slope (the smaller the dose the bigger the effect -I know, it’s crazy), then it is downright wicked to expose students to a supporter of Andrew Wakefield.
David Owen’s appearance on Radio Oxford, with the indomitable Andy Lewis appears on his Quackometer blog.
Year 2 Dr George Lewith
Lewith is a mystery wrapped in an enigma. He’s participated in some research that is quite good by the (generally pathetic) standards of the world of alternative medicine.
In 2001 he showed that the Vega test did not work as a method of allergy diagnosis. "Conclusion Electrodermal testing cannot be used to diagnose environmental allergies", published in the BMJ .[download reprint].
In 2003 he published "A randomized, double-blind, placebo-controlled proving trial of Belladonna 30C” [download reprint] that showed homeopathic pills with no active ingredients had no effects: The conclusion was "”Ultramolecular homeopathy has no observable clinical effects" (the word ultramolecular, in this context, means that the belladonna pills contained no belladonna).
In 2010 he again concluded that homeopathic pills were no more than placebos, as described in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). [download reprint]
What i cannot understand is that, despite his own findings, his private practice continues to prescribe the Vega machine and continues to prescribe homeopathic pills. And he continues to preach this subject to unfortunate medical students.
Lewith is also one of the practitioners recommended by BSEM. He’s a director of the "College of Medicine". And he’s also an advisor to a charity called Yes To Life. (see A thoroughly dangerous charity: YesToLife promotes nonsense cancer treatments).
3rd year Student Selected Unit
The teaching team includes:
- David Owen – Principal Clinical Teaching Fellow SoM, Holistic Physician
- George Lewith – Professor of Health Research and Consultant Physician
- Caroline Eyles – Homeopathic Physician
- Susan Woodhead – Acupuncturist
- Elaine Cooke – Chiropractic Practitioner
- Phine Dahle – Psychotherapist
- Keith Carr – Reiki Master
- Christine Rose – Homeopath and GP
- David Nicolson – Nutritionalist
- Shelley Baker – Aromatherapist
- Cheryl Dunford – Hypnotherapist
- Dedj Leibbrandt – Herbalist
More details of the teaching team here. There is not a single sceptic among them, so the students don’t get a debate, just propaganda.
In this case. there’s no need for the Freedom of Information Act. The handouts. and the powerpoints are on their web site. They seem to be proud of them
Let’s look at some examples
Chiropractic makes an interesting case, because, in the wake of the Singh-BCA libel case, the claims of chiropractors have been scrutinised as never before and most of their claims have turned out to be bogus. There is a close relationship between Lewith’s unit and the Anglo-European Chiropractic College (the 3rd year module includes a visit there). In fact the handout provided for students, Evidence for Chiropractic Care , was written by the College. It’s interesting because it provides no real evidence whatsoever for the effectiveness of chiropractic care. It’s fairly honest in stating that the view at present is that, for low back pain, it isn’t possible to detect any difference between the usefulness of manipulation by a physiotherapist, by an osteopath or by a chiropractor. Of course it does not draw the obvious conclusion that this makes chiropractic and osteopathy entirely redundant -you can get the same result without all the absurd mumbo jumbo that chiropractors and osteopaths love, or their high-pressure salesmanship and superfluous X-rays. Neither does it mention the sad, but entirely possible, outcome that none of the manipulations are effective for low back pain. There is, for example, no mention of the fascinating paper by Artus et al [download reprint]. This paper concludes
"symptoms seem to improve in a similar pattern in clinical trials following a wide
variety of active as well as inactive treatments."
This paper was brought to my attention through the blog run by the exellent physiotherapist, Neil O’Connell. He comments
“If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery.”
This sort of critical thinking is conspicuously absent from this (and all the other) Southampton handouts. The handout is a superb example of bait and switch: No nonsense about infant colic, innate energy or imaginary subluxations appears in it.
Acupuncture is another interesting case because there is quite a lot of research evidence, in stark contrast to the rest of traditional Chinese medicine, for which there is very little research.
|
There is a powerpoint show by Susan Woodhead (though it is labelled British Acupuncture Council). The message is simple and totally uncritical. It works. |

|
In fact there is now a broad consensus about acupuncture.
(1) Real acupuncture and sham acupuncture have been found to be indistinguishable in many trials. This is the case regardless of whether the sham is a retractable needle (or even a toothpick) in the "right" places, or whether it is real needles inserted in the "wrong" places. The latter finding shows clearly that all that stuff about meridians and flow of Qi is sheer hocus pocus. It dates from a pre-scientific age and it was wrong.
(2) A non-blind comparison of acupuncture versus no acupuncture shows an advantage for acupuncture. But the advantage is usually too small to be of any clinical significance. In all probability it is a placebo effect -it’s hard to imagine a more theatrical event than having someone in a white coat stick long needles into you, like a voodoo doll. Sadly, the placebo effect isn’t big enough to be of much use.
Needless to say, none of this is conveyed to the medical students of Southampton. Instead they are shown crude ancient ideas that date from long before anything was known about physiology as though they were actually true. These folks truly live in some alternative universe. Here are some samples from the acupuncture powerpoint show by Susan Woodhead.
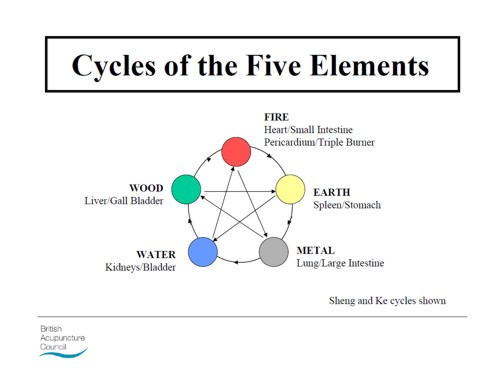
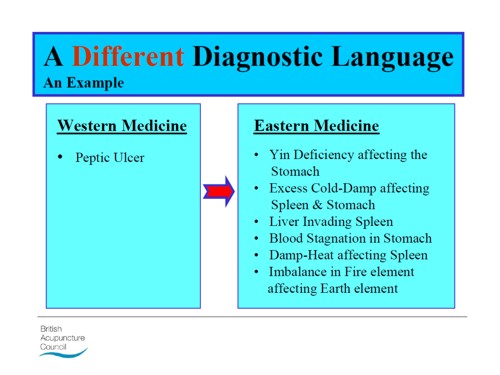
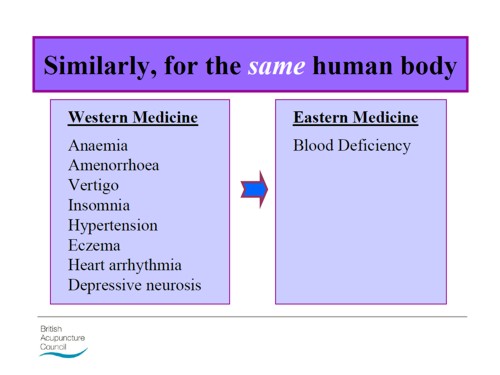
Well this is certainly a "different diagnostic language", but no attempt is made to say which one is right. In the mind of the acupuncurist it seems both are true. It is a characteristic of alternative medicine advocates that they have no difficulty in believing simultaneously several mutually contradictory propositions.
As a final exmple of barminess, just look at the acupuncture points (allegedly) on the ear The fact that it is a favoured by some people in the Pentagon as battlefield acupuncture, is more reminiscent of the mad general, Jack D. Ripper, in Dr Strangelove than it is of science.
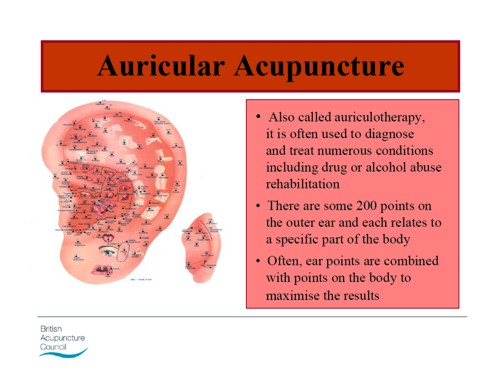
There is an equally uncritical handout on acupuncture by Val Hopwood. It’s dated March 2003, a time before some of the most valuable experiments were done.
The handout says "sham acupuncture
is generally less effective than true acupuncture", precisely the opposite of what’s known now. And there are some bits that give you a good laugh, always helpful in teaching. I like
“There is little doubt that an intact functioning nervous system is required for acupuncture to produce
analgesia or, for that matter, any physiological changes”
and
Modern techniques: These include hybrid techniques such as electro-acupuncture . . . and Ryadoraku [sic] therapy and Vega testing.
Vega testing!! That’s been disproved dozens of times (not least by George Lewith). And actually the other made-up nonsense is spelled Ryodoraku.
It’s true that there is a short paragraph at the end of the handout headed "Scientific evaluation of acupuncture" but it doesn’t cite a single reference and reads more like excuses for why acupuncture so often fails when it’s tested properly.
Homeopathy. Finally a bit about that most boring of topics, the laughable medicine that contains no medicine, homeopathy. Caroline Eyles is a member for the Society of Homeopaths, the organisation that did nothing when its members were caught out in the murderous practice of recommending homeopathy for prevention of malaria. The Society of Homeopaths also endorses Jeremy Sherr, a man so crazy that he believes he can cure AIDS and malaria with sugar pills.
The homeopathy handout given to the students has 367 references, but somehow manages to omit the references to their own boss’s work showing that the pills are placebos. The handout has all the sciencey-sounding words, abused by people who don’t understand them.
"The remedy will be particularly effective if matched to the specific/particular characteristics of the individual (the ‘totality’ of the patient) on all levels, including the emotional and mental levels, as well as just the physical symptoms. ‘Resonance’ with the remedy’s curative power will then be at it’s [sic] best."
The handout is totally misleading about the current state of research. It says
"increasing clinical research confirms it’s [sic] clinical effectiveness in treating patients, including babies and animals (where a placebo effect would be hard to justify)."
|
The powerpont show by Caroline Eyles shows all the insight of a mediaeval vitalist |
|
Anyone who has to rely on the utterly discredited Jacques Benveniste as evidence is clearly clutching at straws. What’s more interesting about this slide the admission that "reproducibility is a problem -oops, an issue" and that RCTs (done largely by homeopaths of course) have "various methodological flaws and poor external validity". You’d think that if that was the best that could be produced after 200 yours, they’d shut up shop and get another job. But, like aging vicars who long since stopped believing in god, but are damned if they’ll give up the nice country rectory, they struggle on, sounding increasingly desperate.
How have topics like this become so embedded in a medical course at a Russell group university?
The details above are a bit tedious and repetitive. It’s already established that hardly any alternative medicine works. Don’t take my word for it. Check the web site of the US National Center for Complementary and Alternative Medicine (NCCAM) who, at a cost of over $2 billion have produced nothing useful.
A rather more interesting question is how a good university like Southampton comes to be exposing its medical students to teaching like this. There must be some powerful allies higher up in the university. In this case it’s pretty obvious who thay are.
Professor Stephen Holgate MD DSc CSc FRCP FRCPath FIBiol FBMS FMed Sci CBE has to be the primary suspect, He’s listed as one of Southampton’s Outstanding Academics. His work is nothing to do with alternative medicine but he’s been a long term supporter of the late unlamented Prince of Wales’ Foundation, and he’s now on the advisory board of it’s successor, the so called "College of Medicine" (for more information about that place see the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health, and also Don’t be deceived. The new “College of Medicine” is a fraud and delusion ). His description on that site reads thus.
"Stephen Holgate is MRC Clinical Professor of Immunopharmacology at the University of Southampton School of Medicine and Honorary Consultant Physician at Southampton University Hospital Trust. He is also chair of the MRC’s Populations and Systems Medicine Board. Specialising in respiratory medicine, he is the author of over 800 peer-reviewed papers and contributions to scientific journals and editor of major textbooks on asthma and rhinitis. He is Co-Editor of Clinical and Experimental Allergy, Associate Editor of Clinical Science and on the editorial board of 25 other scientific journals."
Clearly a busy man. Personally I’m deeply suspicious of anyone who claims to be the author of over 800 papers. He graduated in medicine in 1971, so that is an average of over 20 papers a year since then, one every two or three weeks. I’d have trouble reading that many, never mind writing them.
Holgate’s long-standing interest in alternative medicine is baffling. He’s published on the topic with George Lewith, who, incidentally, is one of the directors of the "College of Medicine"..
It may be unkind to mention that, for many years now, I’ve been hearing rumours that Holgate is suffering from an unusually bad case of Knight starvation.
The Division of Medical Education appears to be the other big source of support for. anti-scientific medicine. That is very odd, I know, but it was also the medical education people who were responsible for mis-educating medical students at. St. Bartholomew’s and at Edinburgh university. Southampton’s Division of Medical Education has a mind-boggling 60 academic and support staff. Two of them are of particular interest here.
Faith Hill is director of the division. Her profile doesn’t say anything about alternative medicine, but her interest is clear from a 2003 paper, Complementary and alternative medicine: the next generation of health promotion?. The research consisted of reporting anecdotes from interviews of 52 unnamed people (this sort of thing seems to pass for research in the social sciences). It starts badly by misrepresenting the conclusions of the House of Lords report (2000) on CAM. Although it comes to no useful conclusions, it certainly shows a high tolerance of nonsensical treatments.
Chris Stephens is Associate Dean of Medical Education & Student Experience. His sympathy is shown by a paper he wrote In 2001, with David Owen (the homeopath, above) and George Lewith: Can doctors respond to patients’ increasing interest in complementary and alternative medicine?. Two of the conclusions of this paper were as follows.
"Doctors are training in complementary and alternative medicine and report benefits both for their patients and themselves"
Well, no actually. It wasn’t true then, and it’s probably even less true now. There’s now a lot more evidence and most of it shows alternative medicine doesn’t work.
"Doctors need to address training in and practice of complementary and alternative medicine within their own organisations"
Yes they certainly need to do that.
And the first thing that Drs Hill and Stephens should do is look a bit more closely about what’s taught in their own university, I hope that this post helps them,
Follow-up
4 July 2011. A correspondent has just pointed out that Chris Stephens is a member of the General Chiropractic Council. The GCC is a truly pathetic pseudo-regulator. In the wake of the Simon Singh affair it has been kept busy fending off well-justified complaints against untrue claims made by chiropractors. The GCC is a sad joke, but it’s even sadder to see a Dean of Medical Education at the University of Southampton being involved with an organisation that has treated little matters of truth with such disdain.
A rather unkind tweet from (ex)-chiropractor @RichardLanigan.
“Chris is just another light weight academic who likes being on committees. Regulatory bodies are full of them”
The mainstream media eventually catch up with bloggers. BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. It also exposed the uselessness of the Quality Assurance Agency (QAA). Both these things have been written about repeatedly here for some years. It was good to see them getting wider publicity.
Watch the video of the programme (Part 1, and Part 2) "Week In Week Out – University Challenged." “The programme examines how pop stars and evangelical Christians are running colleges offering courses validated by the University of Wales.” (I make a brief appearance, talking about validation of degrees in Chinese Medicine).

In October 2008 I posted Another worthless validation: the University of Wales and nutritional therapy. With the help of the Freedom of Information Act, it was possible to reveal the mind-boggling incompetence of the validation process used by the University of Wales.
McTimoney College of Chiropractic
The Chiropractic “degrees” from the McTimoney College of Chiropractic are also validated by the University of Wales by an equally incompetent, or perhaps I should say bogus, procedure. More details can be found at The McTimoney Chiropractic Association would seem to believe that chiropractic is “bogus”, and in a later post, Not much Freedom of Information at University of Wales, University of Kingston, Robert Gordon University or Napier University.
Andy Lewis has also written about chiropractic in The University of Wales is Responsible for Enabling Bogus* Chiropractic Claims to be Made.
Sadly the BBC programme did not have much to say about these domestic courses, but otherwise it was excoriating. In particular it had extensive interviews with Nigel Palastanga, whose astonishing admission that courses were validated withour seeing what was taught on them was revealed here two years ago. After that revelation, the vice-chancellor of UoW, Marc Clement BSc PhD CEng CPhys FIET FInstP, promoted Palastanga to be pro-vice-chancellor in charge of Learning, Teaching and Enhancement (I know, you couldn’t make it up).

In the documentary Palastanga said
"It’s a major business. We earn a considerable amount of money."
That was obvious two years ago, but it’s good to hear it from the horse’s mouth.
After a section that revealed a bit about what goes on at two very fundamentalist bible colleges which gave University of Wales degrees, A. C. Grayling commented thus.
"They are there to train advocates for the biblical message and that is absolutely not, by a very very long chalk, what a university should be doing.. . . A respectable British Higher education institution like the University of Wales shouldn’t be touching them with a bargepole."
Undaunted, Palastanga responded
“That’s his opinion. I would say they are validated to the highest standards. They match what are called QAA benchmark. We have serious academics looking at them, and their academic standards are established at the very highest level.”
And if you believe that, you will truly believe anything.
You can download here one of many moderator’s reports obtained under the Freedom of Information Act. This one is for the BSc (Hons) Chiropractic. It is entirely typical of theuncritical boxticking approach to validation, Nowhere does it say "subluxation is nonsense", though even the GCC now admit that.
Traditional Chinese Medicine
The University of Wales validates several courses in what almost everyone but them classifies as quackery. As well as chiropractic and “nutritional therapy”, there is herbalism. For example a course at a college in Barcelona issues University of Wales degrees in Traditional Chinese medicine, a subject that is a menace to public health.. I was asked to comment on the course, and on a bag of herbs that the presenter had been sold to treat depression.
|
Radix Bupleuri Chinensis
Radix Angelicae Sinensis Radix Paeoniae Lactiflorae Rhizoma Atractylodis Macrocephalae Sclerotium Poriae Cocos Radix Glycyrrhizae Uralensis Cortex Moutan Radicis (Paeonia Suffruticosa) Fructus Gardeniae Jasminoidis Herba Menthae Haplocalycis Zingiber officinale rhizome-fresh |
 Ingredients of a custom mixture. |
There is no good evidence that any of the ingredients help depression, in fact next to nothing is known about most of them, apart from liquorice and ginger. Swallowing them would be rather reckless. They fall right into the description of any herbal medicine, in the Patients’ Guide, "Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety. "
Of the degrees, I said
"There’s no evidence that it [the herbs] does you any good. It may be dangerous because you have no idea of the dose. Degrees in Chinese Medicine consist of three years spent memorising myths and pre-scientific, er, untruths. That isn’t a degree, it’s a travesty."
Palastanga. responded
"We’ve had long debates in the Health Committee about where we would draw the line about what we validate. They have to demonstrate to us that there is some scientific basis for the practice, that there is an established curriculum, that there is an established safe practice."
The presenter asked him "So you are confident that Chinese medicine works? Palastanga replied
" I didn’t say that. I said that there is evidence that it does work . . We are trying to enforce these professions to undertake effective research."
That statement is simply not true, as shown by the response of the validation committee to the application for validation of the course in “Nutritional Therapy” at the Northern College of Acupuncture, documented previously. The fact of the matter is that the validation proceeded without looking at what was actually taught, and without even a detailed timetable of lectures. The committee looked only at the official documents presented to it and was totally negligent in failing to discover some of the bizarre beliefs of the people who were giving the course.
Palastanga went on to raise the usual straw man argument, about how little regular medicine is based on good evidence (though admittedly that is certainly true in his own field -he is a physiotherapist).
Fazley International College Kuala Lumpur
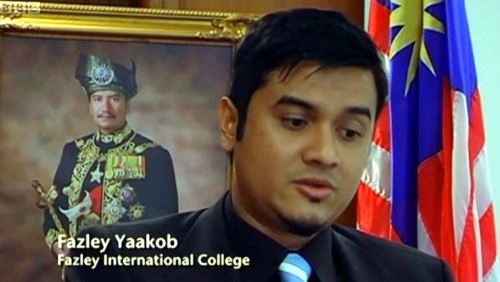
This business college in Kuala Lumpur offered University of Wales degrees. Its 32-year old president is a part time pop star with impressive looking qualifications
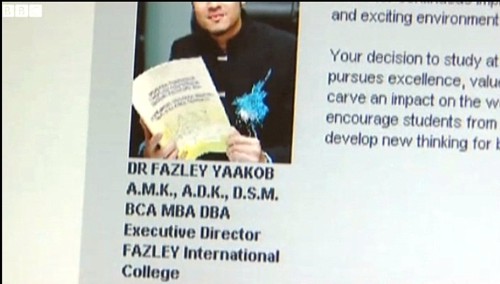
The presenter pointed out that
" His doctorate and his MBA were awarded in that citadel of education, Cambridge. Here he is, pictured at the city’s prestigious business school. He was there for all of four days and walked away with a doctorate. But the degree was not from the University of Cambridge, but from the now defunct "European Business School Cambridge". It never had the right to award degrees."
Neither the University of Wales nor the QAA had noticed this unfortunate fact. Once the TV team had done their job for them, the UoW withdrew support. though, as of 15 November 2010, that is not obvious from Fazley’s web site.
Mr (not Dr) Fazley seemed rather pleased about how students were attracted by the connection with the Prince of Wales. The fact that he is Chancellor of the University of Wales seems not inappropriate, given the amount of quackery they promote.
Quality Assurance Agency (QAA)
In 2007, I wrote, in Nature (see also here),
“Why don’t regulators prevent BSc degrees in anti-science? The Quality Assurance Agency for Higher Education (QAA) claims that “We safeguard and help to improve the academic standards and quality of higher education in the UK.” It costs taxpayers £11.5 million (US$22 million) annually. It is, of course, not unreasonable that governments should ask whether universities are doing a good job. But why has the QAA not noticed that some universities are awarding BSc degrees in subjects that are not, actually, science? The QAA report on the University of Westminster courses awards a perfect score for ‘curriculum design, content and organization,’ despite this content consisting largely of what I consider to be early-nineteenth-century myths, not science. It happens because the QAA judges courses only against the aims set by those who run the QAA, and if their aims are to propagate magic as science, that’s fine.”
That was illustrated perfectly in the documentary when Dr Stephen Jackson of the QAA appeared to try to justify the fact that the QAA had, like the University of Wales, failed entirely to spot any of the obvious problems. He had a nice dark suit, tie and poppy, but couldn’t disguise the fact that the QAA had given high ratings to some very dubious courses.
The QAA sent nine people to the other side of the globe, at a cost of £91,000. They could have done a lot better if they’d spent 10 minutes with Google at home.
Universities UK (UUK)
Needless to say, the Committee of Vice-Chancellors and Principals has said nothing at all. As usual, Laurie Taylor had it all worked out in Times Higher Education (4th November).
Speaking to our reporter Keith Ponting (30), he commended UUK’s decision to say absolutely nothing whatsoever about the abolition of all public funding for the arts and humanities.
He also praised UUK’s total silence on Lord Browne’s view that student courses should primarily be evaluated by their employment returns.
When pressed by Ponting for his overall view of UUK’s failure to respond in any way at all to any aspect of the Browne Review, he described it as “welcome evidence, in a world of change, of UUK’s consistent commitment over the years to ineffectual passivity”.
Meanwhile, a University of Wales video on YouTube
Caveat emptor
Follow-up
A couple of days later, a search of Google news for the “University of Wales” shows plenty of fallout. The vice-chancellor claims that ““The Minister’s attack came as a complete and total surprise to me”. That can’t be true. It is over two years since I told him what was going on, and if he was unaware of it, that is dereliction of duty. It is not the TV programme that brought the University into disrepute, it was the vice-chancellor.


Snow on December 18th Roaring fire
Lindy contributes acute comments regularly here. She is also an accomplished musician. She has kindly allowed me to post here four of her re-written carols.
Adam lay ybounden | Hark the Herald | Holly and the Ivy | Merry Gentlemen
Adam lay ybounden
The Middle English dialect is not easy to follow. In fact Wikipedia reveals that it is oit even standard Middle English, but Macaronic English. The original words are reproduced in the right hand column. The original, sung by choir of King’s College Chapel, is on YouTube.
| Atoms lay y’bounden In primordial soup; Six billion years did pass A’fore they could regroup. For first had bin a big bang The universe was shook; Though through milennia For god it was mistook. Then particles of light did shine, ema- -nating from the sun. Out of soup arose archaea And so life was begun. Thanks be to the man This mystery did solve; Through him we celebrate how we Did from the bugs evolve. |
Adam lay ybounden, Bounden in a bond: Four thousand winter Thought he not too long. And all was for an apple, An appil that he took, As clerkè finden Written in their book. Ne had the apple taken been, The appil taken been, Ne had never our lady Abeen heavenè queen. Blessèd be the time That appil taken was, Therefore we moun singen, Deo gracias! . |
Hark the Herald Angels sing.
This version is for Simon Singh. If you haven’t yet signed the new peition, please do it here.
Mark this very dang’rous thing,
Story is of Simon Singh.
He got chiropractors riled,
“Sod it! We have been defiled!
Ployful all ye woosters rise,
Join us to defend our lies,
With us loudly please proclaim,
Subluxations are our game”
Christ, they all with one accord
Took young Simon off to court.
“We’ll put you before a judge,
Since we always bear a grudge
‘Gainst all those who say our modus
Operandi is all bogus;
Mark the words of justice Eady,
Gave his ruling oh so speedy.
Mark the case of Simon Singh
With support the web does ring.
Ditch draconian libel laws,
Without which they’d have no cause
To sue those who would speak freely,
Truth, opinion-and reason really
Should prevail o’er all such things,
Surely he his case must win.
The Holly and the Ivy
Dedicated to the Prince of Wales, certain vice-chancellors and other champions of the endarkenment.
The folly and the lies, see
How they’ve become full-blown;
The braying of th’quackti’tioner Roy-
Al, th’enlightenment has flown.
Refrain: For deriding all the data
(Such stunning stuff we hear)!
The displaying of such cherry pick-
-Ing, beats bringing in Chi square.
The folly hears no critics
It makes you quite struck dumb,
Just put a poison substance in,
And dilute to kingdom come.
For deriding all the data etc.
The folly so does blossom,
Beguiles you with its charm,
Just make some movements with your wrist
And it will do no harm.
For deriding all the data etc.
The folly’s given credence
If you are qualified
With a BSc in pseudosci-
-Ence, th’endarkenment is nigh!
For deriding all the data etc.
The folly bears a burden
Now it has fallen down;
F.O.I requests and publicity
Have giv’n D.C. the crown.
For deriding all the data etc.
The folly is so fickle,
How did they have the gall
To tell us how their remedies
Were here to treat us all?
For deriding all the data etc.
The folly and the lies, see
How they must surely fail
We’ll drink a toast to good evidence
And let real science prevail!
Alternative refrain:
Oh the rising of the Reiki,
Of acupuncture too,
All Rolfering* and Tuina-ish,
They all amount to woo.
*The names Rolf and Roger seem remarkably similar in some circumstances so I get a little confused.
Merry gentlemen.
Here is Lindy’s version of "god rest ye merry gentleman", composed in the wake of the admission by the Professional Standards director of Boots the Chemists that they sell homeopathic pills despite being aware of the fact that there is no reason to think they work.
I arrest you merry gentlemen,
Please kindly step this way.
For you are selling sugar pills
For which the people pay;
We’re from the Trading Standards and through courts we’ll find a way
To stop your profit-making ploy, Profiting ploy,
We’ll stop your profiteering ploy”!
The chemists calmly did defend
Themselves though they were riled;
“The people do demand these pills
Because they’re not defiled
With molecules (nor ‘owt at all), despite the claims so wild;
We’ll continue our profiteering ploy, Profiting ploy,
We’ll continue our profiteering ploy”.
So Trading Standards did respond
“We understand your aim
To make more money, though if you
Persist with bogus claim
To cure disease with sugar pills,
We’ll put you all to shame!
We are stopping your profiteering ploy, Profiting ploy,
We are stopping your profiteering ploy”.
“You breach the regulations by selling pills, you see,
Which claim to contain ‘aqua’ (dilute to 30C),
Or ‘dolphin song’ or ‘canine testes’ – even ‘ATP’!
So you’ll stop all this profiteering ploy, profiting ploy,
So you’ll stop all this profiteering ploy”.
The Dept of Health bangs on and on
About a patient’s choice,
But all good people must condemn
These lies with one great voice.
We dream of days when fibs are gone and we can all rejoice
‘Cos they’ve stopped all their profiteering ploy, Profiting ploy,
‘Cos they’ve stopped all their profiteering ploy
Chiropractors are getting very touchy indeed, all over the world. And no wonder, because their claims are being exposed as baseless as never before, in the wake of their attempts to stifle criticism by legal action..
In March, Shaun Holt appeared on Breakfast TV in New Zealand. Holt has done a lot of good work on TV in debunking some of the preposterous claims made by quacks. See him on YouTube.
This time he talked about chiropractic. Here is the video.
One could argue that he was over generous to chiropractic, especially when talking about their effectiveness in treating low back pain. He said, quite rightly, that chiropractors are no better than physiotherapists at treating low back pain.
But a recent trial suggests that neither are much good. “A randomised controlled trial of spinal manipulative therapy in acute low back pain” (Juni et al., 2009 in the BMJ; see also coverage in Pulse). This trial compared standard care with standard care plus spinal manipulative therapy (SMT). The results were negative, despite the fact that this sort of A + B vs B design is inherently biassed in favour of the treatment (see A trial design that generates only ”positive” results, Ernst & Lee 2008, Postgrad Med J.).
"SMT was performed by a specialist in manual medicine, chiropractice and rheumatology (GH), a specialist in physical medicine (DV) or an osteopath (RvB), all proficient in SMT."
"Conclusions: SMT is unlikely to result in relevant early pain reduction in patients with acute low back pain."
Admittedly, the trial was quite small (104 patients, 52 in each group) so it will need to be confirmed. but the result is entirely in line with what we knew already.
It also adds to the evidence that the recommendation by NICE of SMT by chiropractors constitutes their biggest failure ever to assess evidence properly. If NICE don’t amend this advice soon, they are in danger of damaging their hitherto excellent record.
Despite the moderate tone and accuracy of what Holt said on TV, the New Zealand Chiropractors’ Association made a formal complaint. That is what they like to do, as I learned recently, to my cost. It is so much easier than producing evidence.
Quite absurdly the New Zealand Broadcasting Standards Authority (BSA) has upheld some of the complaints. Their judgement can be read here.
The BSA consists of four people, two lawyers and two journalists. So not a trace of scientific expertise among them. Having people like that judging the claims of chiropractors makes as much sense as having them judged by Mr Justice Eady. They seem to be the sort of people who think that if there is a disagreement, the truth must lie half-way between the opposing views.
One of the BSA members, Tapu Misa, has used her newspaper column to quote approvingly the views of the notorious Dr Mercola web site on flu prevention “Your best defence, it says, is to eat right, get lots of sleep, avoid sugar and stress, load up on garlic, Vitamin D and krill oil”. (Snake oil is said to be good too.) There are some odd attitudes to science in some of her other columns too (e.g. here and here). Not quite the person to be judging the evidence for and against chiropractic, I think.
In fact the TV show in question was more than fair to chiropractors. It adopted the media’s usual interpretation of fair and balanced: equal time for the flat earthers. A Chiropractor was invited to reply to Holt’s piece. Here he is.
The chiropractor, Doug Blackbourn, started very plausibly, though a tendency to omit every third syllable made transcription hard work. He established that if you cut yourself you get better (without any help). He established that nerves run down the spinal cord. So far, so good. But then he quickly moved on to the usual flights of fancy.
"We have two premises. The body heals itself and the nervous system runs the body. Now the nervous system runs the body, travels down through the spinal cord so chiropractic is not based on the belief that, you know, energy flows, it’s based on the fact that your nervous system runs the body and [inaudible] affects the overall health of the body"
This statement is totally vague. It has nothing whatsoever to do with the main question, can chiropractors do anything useful. It is sheer flannel.
We’re seeing people, heck, diabetes. I had a quadriplegic come in one time for adjustment, we’ve got stroke people, we’ve got all sorts of conditions. We’re not treating the condition, We’re allowing, checking the spine to see if there’s any interference there that will slow the body down"
“Interference”? “slowing the body down”? These are utterly meaningless phrases that simply serve to distract from the only question that matters.
"Chiropractice is the most safest [sic] profession to go to to get your spine adjusted"
Hmm I thought it was the only job that uses the word ‘adjustment’.
Worst of all was his response to a question about asthma.
Presenter: "So chiropractors are not out there claiming they will cure asthma for example?". Chiropractor: "No"
This is simply untrue, both in New Zealand and in the UK. For a start, just look at what Blackbourn’s own web site says about asthma.
"The challenge, of course, with allergy and asthma medication is there is no end-point. There is no cure. Asthma and allergies, for the most part, are lifelong conditions requiring lifelong medication. Might there be a better way, an alternative solution?
“Alternative” is the key word. Medical treatment is designed to combat symptoms, and is successful to a certain extent with allergies and asthma. Underlying causes are not addressed, however, and symptoms continue year after year. What else might be done?
Enter chiropractic care. Chiropractic health care, with its unique comprehensive approach, is able to offer positive benefit to a variety of conditions and ailments. In the case of allergies and asthma, these “hypersensitivity conditions” may respond well to therapy designed to normalize the body’s flow of nerve signals. To use a metaphor, chiropractic treatment removes roadblocks to the body’s natural healing abilities. Restoring these imbalances may help reduce such hypersensitivity reactions."
Blackbourn’s web site describes him thus
"As a Doctor of Chiropractic, Dr. Doug Blackbourn . . ."
But the qualifications of “Dr” Blackbourn are B.App.Sc (Chiro) M.N.Z.C.A , the same as those of “Dr” Brian Kelly.
After a performance like this, perhaps someone should submit a complaint to the New Zealand Broadcasting Standards Authority.
After all, I notice that they have dismissed complaints from one chiropractor, Sean Parker, after a TV programme looked at the business practices of his private chiropractic practice, The Spinal Health Foundation. Perhaps the BSA understands business better than it understands science.
Follow-up
Is chiropractic crumbling in New Zealand? The New Zealand College of Chiropractic featured in my editorial in the New Zealand Medical Journal, and in the fallout from that article, It’s principle, “Dr” Brian Kelly (B App Sci (Chiro)) seems to be getting desperate. His college is now canvassing for recruits in Canada. They are promised all the woo.
- Subluxation centered techniques – Gonstead, Toggle Recoil, Thompson, Diversified
- Traditional philosophy featuring vitalism and innate healing – congruent curriculum
Perhaps Canada is a good place to recruit, gven the $500 million class action being brought against chiropractors in Canada, after Sandra Nette became tetraplegic immediately after a chiropractor manipulated her neck, Canadian chiropractors must be looking for somewhere to hide.
Stuff and Nonsense. jdc described this story at the time the complaint was lodged.
Shaun Holt’s own blog follows the action.
New Zealand Doctor covers the story.
Bay of Plenty Times “Bay researcher slams television complaint ruling“
In July 2008 I wrote an editorial in the New Zealand Medical Journal (NZMJ), at the request of its editor.
The title was Dr Who? deception by chiropractors. It was not very flattering and it resulted in a letter from lawyers representing the New Zealand Chiropractic Association. Luckily the editor of the NZMJ, Frank Frizelle, is a man of principle, and the legal action was averted. It also resulted in some interesting discussions with disillusioned chiropractors that confirmed one’s worst fears. Not to mention revealing the internecine warfare between one chiropractor and another.
This all occurred before the British Chiropractic Association sued Simon Singh for defamation. The strength of the reaction to that foolhardy action now has chiropractors wondering if they can survive at all. The baselessness of most of their claims has been exposed as never before. No wonder they are running scared. The whole basis of their business is imploding.
Needless to say chiropractors were very cross indeed. Then in February 2009 I had a polite email from a New Zealand chiropractor, David Owen, asking for help to find one of the references in the editorial. I’d quoted Preston Long as saying
"Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
And I’d given the reference as
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10
I’d found the quotation, and the reference, in Ernst’s 2005 article, The value of Chiropractic, but at the time I couldn’t find the Journal of Quality Healthcare. I did find the same article on the web. At least the article had the same title, the same author and the same quotation. But after finding, and reading, the article, I neglected to change the reference from J Quality Health Care to http://skepticreport.com/sr/?p=88. I should have done so and for that I apologise.
When I asked Ernst about the Journal of Quality Healthcare, he couldn’t find his copy of the Journal either, but he and his secretary embarked on a hunt for it, and eventually it was found.

![]()
|
It turns out that Journal of Quality Healthcare shut down in 2004, without leaving a trace on the web, or even in the British Library. It was replaced by a different journal, Patient Safety and Quality Healthcare (PSQH) A reprint was obtained from them. It is indeed the same as the web version that I’d read, and it highlighted the quotation in question. The reprint of the original article, which proved so hard to find, can be downloaded here. |
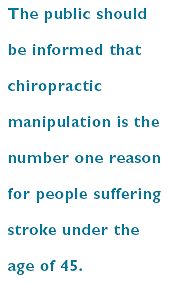
|
The full quotation is this
"Sixty-two clinical neurologists from across Canada, all certified members of the Royal College of Physicians and Surgeons, issued a warning to the Canadian public, which was reported by Brad Stewart, MD. The warning was entitled Canadian Neurologists Warn Against Neck Manipulation. The final conclusion was that endless non-scientific claims are being made as to the uses of neck manipulation(Stewart, 2003). They need to be stopped. The public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45."
I have often condemned the practice of citing papers without reading them (it is, of course, distressingly common), so I feel bad about this, though I had in fact read the paper in question in its web version. I’m writing about it because I feel one should be open about mistakes, even small ones.
I’m also writing about it because one small section of the magic medicine community seems to think they have nailed me because of it. David Owen, the New Zealand chiropractor, wrote to the editor of the NZMJ, thus.
|
The quote [in question] is the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45. Long PH. Stroke and Manipulation. J Quality Health Care. 2004:3:8-10 This quote actually comes from the following blog article http://www.skepticreport.com/medicalquackery/strokespinal.htm [DC the URL is now http://skepticreport.com/sr/?p=88] I have attached all my personal communications with Colquhoun. They demonstrate this is not a citation error. Prof Colquhoun believes the origin of the quote doesn’t matter because Long was quoting from a Canadian Neurologists’ report (this is also incorrect). As you can see he fails to provide any evidence at all to support the existance [sic] of the “J Quality Health Care.” Colquhoun ‘s belief that my forwarding this complaint is me “resorting to threats” is the final nail in the coffin. If he had any leg to stand on where is the threat? This may seem pedantic but it surely reflects a serious ethical breach. Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility? Incidentally, at the end of the article, conflicts of interest are listed as none. As Colquhoun is a Professor of Pharmacology and much of his research funding no doubt comes from the pharmaceutical industry how can he have no conflict of interest with therapies that do not advocate the use of drugs and compete directly against the billions spent on pain medications each year? If I may quote Colquhoun himself in his defence of his article (Journal of the New Zealand Medical Association, 05-September-2008, Vol 121 No 1281) I’ll admit, though, that perhaps ‘intellect’ is not what’s deficient in this case, but rather honesty. David Owen |
Financial interests
Well, here is a threat: I’m exposed as a shill of Big Pharma. ". . . much of his funding no doubt comes from the pharmaceutical industry". I can’t count how many times this accusation has been thrown at me by advocates of magic medicine. Oddly enough none of them has actually taken the trouble to find out where my research funding has come from. None of them even knows enough about the business to realise the extreme improbability that the Pharmaceutical Industry would be interested in funding basic work on the stochastic properties of single molecules. They fund only clinicians who can help to improve their profits,
The matter of funding is already on record, but I’ll repeat it now. The media ‘nutritional therapist’, Patrick Holford, said, in the British Medical Journal
“I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry “
To which my reply was
” Oh dear, Patrick Holford really should check before saying things like “I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry”. Unlike Holford, when I said “no competing interests”, I meant it. My research has never been funded by the drug industry, but always by the Medical Research Council or by the Wellcome Trust. Neither have I accepted hospitality or travel to conferences from them. That is because I would never want to run the risk of judgements being clouded by money. The only time I have ever taken money from industry is in the form of modest fees that I got for giving a series of lectures on the basic mathematical principles of drug-receptor interaction, a few years ago.”
I spend a lot of my spare time, and a bit of my own money, in an attempt to bring some sense into the arguments. The alternative medicine gurus make their livings (in some cases large fortunes) out of their wares.
So who has the vested interest?
Does chiropractic actually cause stroke?
As in the case of drugs and diet, it is remarkably difficult to be sure about causality. A patient suffers a vertebral artery dissection shortly after visiting a chiropractor, but did the neck manipulation cause the stroke? Or did it precipitate the stroke in somebody predisposed to one? Or is the timing just coincidence and the stroke would have happened anyway? There has been a lot of discussion about this and a forthcoming analysis will tackle the problem of causality head-on,
My assessment at the moment, for what it’s worth, is that there are some pretty good reasons to suspect that neck manipulation can be dangerous, but it seems that serious damage is rare.
In a sense, it really doesn’t matter much anyway, because it is now apparent that chiropractic is pretty well discredited without having to resort to arguments about rare (though serious) effects. There is real doubt about whether it is even any good for back pain (see Cochrane review), and good reason to think that the very common claims of chiropractors to be able to cure infant colic, asthma and so on are entirely, ahem, bogus. (See also Steven Novella, ebm-first, and innumerable other recent analyses.)
Chiropractic is entirely discredited, whether or not it may occasionally kill people.
Complaint sent to UCL
I had an enquiry about this problem also from my old friend George Lewith. I told him what had happened. Soon after this, a complaint was sent to Tim Perry and Jason Clarke, UCL’s Director and Deputy Director of Academic Services. The letter came not from Lewith or Owen, but from Lionel Milgom. Milgrom is well known in the magic medicine community for writing papers about how homeopathy can be “explained” by quantum entanglement. Unfortunately for him, his papers have been read by some real physicists and they are no more than rather pretentious metaphors. See, for example, Danny Chrastina’s analysis, and shpalman, here. Not to mention Lewis, AP Gaylard and Orac.
|
Dear Mr Perry and Mr Clark, I would like to bring to your attention an editorial (below) that appeared in the most recent issue of the New Zealand Medical Journal. In it, one of your Emeritus Professors, David Colquhoun, is accused of a serious ethical breach, and I quote – “Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility?” Professor Colquhoun is well-known for writing extensively and publicly excoriating many forms of complementary and alternative medicine, particularly with regard to the alleged unscientific nature and unethical behaviour of its practitioners. Professor Colquhoun is also a voluble champion for keeping the libel laws out of science. While such activities are doubtlessly in accord with the venerable Benthamite liberal traditions of UCL, I am quite certain hypocrisy is not. And though Professor Colquhoun has owned up to his error, as the NZMJ’s editor implies, it leaves a question mark over his credibility. As custodians of the college’s academic quality therefore, you might care to consider the possible damage to UCL’s reputation of perceived professorial cant; emeritus or otherwise. Yours Sincerely Dr Lionel R Milgrom |
So, as we have seen, the quotation was correct, the reference was correct, and I’d read the article from which it came I made a mistake in citing the original paper rather than the web version of the same paper..
I leave it to the reader to judge whether this constitutes a "serious ethical breach", whether I’d slipped in an "unsupported statement", and whether it constitutes "hypocrisy"
Follow-up
It so happens that no sooner was this posted than there appeared Part 2 of the devastating refutation of Lionel Milgrom’s attempt to defend homeopathy, written by AP Gaylard. Thanks to Mojo (comment #2) for pointing this out.
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
Today, 29 July 2009, a large number of magazines and blogs will publish simultaneously Simon Singh’s article. The Guardian was forced to withdraw it, but what he said must be heard (even if the word ‘bogus’ is now missing).
This is an edited version if the article in the Guardian that resulted in the decision of the British Chiropractic Association to sue Singh for libel. That decision was bad for Singh, though its effects could yet be good for the rest of the world, Firstly the decision to use law rather than rational argument stands a good chance of destroying chiropractic entirely because its claims have now come under scrutiny as never before, and they have been found wanting. Secondly, the support for Singh has been so enormous that there must now be a good chance of getting the UK’s iniquitous laws about defamation changed.
I’d rather have reproduced the original article in its entirety, but this bowdlerised version still presents the case very strongly (and the unedited version appears here and here).
Beware the spinal trapSome practitioners claim it is a cure-all, but the research suggests chiropractic therapy has mixed results – and can even be lethal, says Simon Singh. You might be surprised to know that the founder of chiropractic therapy, Daniel David Palmer, wrote that “99% of all diseases are caused by displaced vertebrae”. In the 1860s, Palmer began to develop his theory that the spine was involved in almost every illness because the spinal cord connects the brain to the rest of the body. Therefore any misalignment could cause a problem in distant parts of the body. In fact, Palmer’s first chiropractic intervention supposedly cured a man who had been profoundly deaf for 17 years. His second treatment was equally strange, because he claimed that he treated a patient with heart trouble by correcting a displaced vertebra. You might think that modern chiropractors restrict themselves to treating back problems, but in fact some still possess quite wacky ideas. The fundamentalists argue that they can cure anything, including helping treat children with colic, sleeping and feeding problems, frequent ear infections, asthma and prolonged crying – even though there is not a jot of evidence. I can confidently label these assertions as utter nonsense because I have co-authored a book about alternative medicine with the world’s first professor of complementary medicine, Edzard Ernst. He learned chiropractic techniques himself and used them as a doctor. This is when he began to see the need for some critical evaluation. Among other projects, he examined the evidence from 70 trials exploring the benefits of chiropractic therapy in conditions unrelated to the back. He found no evidence to suggest that chiropractors could treat any such conditions. But what about chiropractic in the context of treating back problems? Manipulating the spine can cure some problems, but results are mixed. To be fair, conventional approaches, such as physiotherapy, also struggle to treat back problems with any consistency. Nevertheless, conventional therapy is still preferable because of the serious dangers associated with chiropractic. In 2001, a systematic review of five studies revealed that roughly half of all chiropractic patients experience temporary adverse effects, such as pain, numbness, stiffness, dizziness and headaches. These are relatively minor effects, but the frequency is very high, and this has to be weighed against the limited benefit offered by chiropractors. More worryingly, the hallmark technique of the chiropractor, known as high-velocity, low-amplitude thrust, carries much more significant risks. This involves pushing joints beyond their natural range of motion by applying a short, sharp force. Although this is a safe procedure for most patients, others can suffer dislocations and fractures. Worse still, manipulation of the neck can damage the vertebral arteries, which supply blood to the brain. So-called vertebral dissection can ultimately cut off the blood supply, which in turn can lead to a stroke and even death. Because there is usually a delay between the vertebral dissection and the blockage of blood to the brain, the link between chiropractic and strokes went unnoticed for many years. Recently, however, it has been possible to identify cases where spinal manipulation has certainly been the cause of vertebral dissection. Laurie Mathiason was a 20-year-old Canadian waitress who visited a chiropractor 21 times between 1997 and 1998 to relieve her low-back pain. On her penultimate visit she complained of stiffness in her neck. That evening she began dropping plates at the restaurant, so she returned to the chiropractor. As the chiropractor manipulated her neck, Mathiason began to cry, her eyes started to roll, she foamed at the mouth and her body began to convulse. She was rushed to hospital, slipped into a coma and died three days later. At the inquest, the coroner declared: “Laurie died of a ruptured vertebral artery, which occurred in association with a chiropractic manipulation of the neck.” This case is not unique. In Canada alone there have been several other women who have died after receiving chiropractic therapy, and Edzard Ernst has identified about 700 cases of serious complications among the medical literature. This should be a major concern for health officials, particularly as under-reporting will mean that the actual number of cases is much higher. If spinal manipulation were a drug with such serious adverse effects and so little demonstrable benefit, then it would almost certainly have been taken off the market. Simon Singh is a science writer in London and the co-author, with Edzard Ernst, of Trick or Treatment? Alternative Medicine on Trial. This is an edited version of an article published in The Guardian for which Singh is being personally sued for libel by the British Chiropractic Association. |
That’s a great account of the evidence. Notice the conclusion,
“If spinal manipulation were a drug with such serious adverse effects and so little demonstrable benefit, then it would almost certainly have been taken off the market“.
It is the job of NICE to evaluate critically that sort of thing, which makes it all the odder that the NICE guidance group, very unusually, failed to assess properly the evidence for chiropractic.
If you aren’t one of the 15,000 people who have already signed Singh’s statement, please do it now
Follow-up
Resignation of Pain Society president. While we are on the topic of chiropractic, my comment, The hidden cost of endorsing voodoo, appeared at last on the BMJ article about NICE’s low back pain guidance. The thread came back to life after the British Pain Society voted out its president, Paul Watson, a physiotherapist who was a member of the group that wrote the guidance.
Some of the links Links to some of the many repostings of Singh’s article today are aggregated at Sense about Science. There where over 200 in a single day. The British Chiropractic Association tried to suppress criticism, but they clearly don’t understand the web.
“An intrepid, ragged band of bloggers. Chiropractors may regret choosing to sue Simon Singh, springing online scientists into action”. Ben Goldacre has summed up the reaction of the blogosphere with characteristically fine style in the Guardian. Ragged? Moi? The blog version (with links) is here.
It’s good to see the BMJ joining the campaign for free speech (only a month or two behind the blogs). The suing of Simon Singh for defamation by the British Chiropractic Association has stirred up a hornet’s nest that could (one hopes) change the law of the land, and destroy chiropractic altogether. The BMJ’s editor, Fiona Godlee, has a fine editorial, Keep the libel laws out of science. She starts “I hope all readers of the BMJ are signed up to organised scepticism” and says
“Weak science sheltered from criticism by officious laws means bad medicine. Singh is determined to fight the lawsuit rather than apologise for an article he believes to be sound. He and his supporters have in their sights not only the defence of this case but the reform of England’s libel laws.”
Godlee refers to equally fine articles by the BMJ’s Deputy Editor, Tony Delamothe, Thinking about Charles II“, and by Editor in Chief, Harvey Marcovitch, “Libel law in the UK“.
The comments on Godlee’s editorial, show strong support, (apart from one from the infamous quantum fantasist, Lionel Milgrom). But there was one that slighlty surprised me, from Tricia Greenhalgh, author of the superb book, “How to read a paper”. She comments
“the use of the term ‘bogus’ seems both unprofessional and unscholarly. The argument would be stronger if expressed in more reserved terms”
That set me thinking, not for the first time, about the difference between journalism and scholarship. I can’t imagine ever using a word like ‘bogus’ in a paper about single ion channels. But Singh was writing in a newspaper, not in a scientific paper. Even more to the point, his comments were aimed at people who are not scholars and who, quite explicitly reject the normal standards of science and evidence. The scholarly approach has been tried for centuries, and it just doesn’t work with such people. I’d defend Singh’s language. It is the only way to have any effect. That is why I sent the following comment.
The ultimate irony is that the comment was held up by the BMJ’s lawyers, and has still to appear.
|
Thanks for an excellent editorial. I doubt that it’s worth replying to Lionel Milgrom whose fantasy physics has been totally demolished by real physicists. Trisha Greenhalgh is, though, someone whose views I’d take very seriously. She raises an interesting question when she says “bogus” is an unprofessional word to use. Two things seem relevant. First, there is little point in writing rational scholarly articles for a group of people who do not accept the ordinary rules of evidence or scholarship. We are dealing with fantasists. Worse still, we are dealing with fantasists whose income depends on defending their fantasies. You can point out to your heart’s content that “subluxations” are figment of the chiropractors’ imagination, but they don’t give a damn. They aren’t interested in what’s true and what isn’t. Throughout my lifetime, pharmacologists and others have been writing scholarly articles about how homeopathy and other sorts of alternative medicine are bogus. All this effort had little effect. What made the difference was blogs and investigative journalism. When it became possible to reveal leaked teaching materials that taught students that “amethysts emit high yin energy“, and name and shame the vice-chancellors who allow that sort of thing to happen (in this case Prof Geoffrey Petts of Westminster University), things started to happen. In the last few years all five “BSc” degrees in homeopathy have closed and that is undoubtedly a consequence of the activities of bloggers and can assess evidence but who work more like investigative journalists. When the BCA released, 15 months after the event, its “plethora of evidence” a semi-organised effort by a group of bloggers produced, in less than 24 hours, thoroughly scholarly analyses of all of them (there is a summary here). As the editorial says, they didn’t amount to a hill of beans, They also pointed out the evidence that was omitted by the BCA. The conventional press just followed the bloggers. I find it really rather beautiful that a group of people who have other jobs to do, spent a lot of time doing these analyses, unpaid, in their own time, simply to support Singh, because they believed it is the right thing to do. Simon Singh has analysed the data coolly in his book. But In the case that gave rise to the lawsuit he was writing in a newspaper. It was perfectly clear from the context what ‘bogus’ meant. but Mr Justice Eady (aided by a disastrous law) chose to ignore entirely the context and the question of truth. The description ‘bogus’. as used by Singh, seems to be entirely appropriate for a newspaper article. To criticise him for using “unprofessional” language is inappropriate because we are not dealing with professionals. At the heart of the problem is the sort of stifling political correctness that has resulted in quacks being referred to as “professions” rather than fantasists and fraudsters [of course I use the word fraudster with no implication that it necessarily implies conscious lying]. At least there are some laughs to be had from the whole sorry affair. Prompted by that prince among lawyers known as Jack of Kent there was a new addition to my ‘Patients’ Guide to Magic Medicine‘, as featured in the Financial Times.
|
It is, perhaps, misplaced political correctness that lies at the heart of the problem. Who can forget the letter from Lord Hunt, while he was at the Department of Health, in which he described “psychic surgery” (one of the best known fraudulent conjuring tricks) as a “profession”.
Follow-up
Two days later, the comment has appeared in the BMJ at last. But it has been altered a bit.
|
Unprofessional language is appropriate when dealing with unprofessional people Thanks for an excellent editorial. I doubt that it’s worth replying to Lionel Milgrom whose fantasy physics has been totally demolished by real physicists. Trisha Greenhalgh is, though, someone whose views I’d take very seriously. She raises an interesting question when she says “bogus” is an unprofessional word to use. Two things seem relevant. First, there is little point in writing rational scholarly articles for a group of people who do not seem to accept the ordinary rules of evidence or scholarship. You can point out to your heart’s content that “subluxations” are figment of the chiropractors’ imagination, but they don’t give a damn. Throughout my lifetime, pharmacologists and others have been writing scholarly articles about how homeopathy and other sorts of alternative medicine are bogus. All this effort had little effect. What made the difference was blogs and investigative journalism. When it became possible to reveal leaked teaching materials that taught students that “amethysts emit high yin energy”, and name and shame the vice-chancellors who allow that sort of thing to happen (in this case Prof Geoffrey Petts of Westminster University), things started to happen. In the last few years all five “BSc” degrees in homeopathy have closed and that is undoubtedly a consequence of the activities of bloggers and can assess evidence but who work more like investigative journalists. When the BCA released, 15 months after the event, its “plethora of evidence” a semi-organised effort by a group of bloggers produced, in less than 24 hours, thoroughly scholarly analyses of all of them (there is a summary here). As the editorial says, they didn’t amount to a hill of beans, They also pointed out the evidence that was omitted by the BCA. The conventional press just followed the bloggers. I find it really rather beautiful that a group of people who have other jobs to do, spent a lot of time doing these analyses, unpaid, in their own time, simply to support Singh, because they believed it is the right thing to do. Simon Singh has analysed the data coolly in his book. But In the case that gave rise to the lawsuit he was writing in a newspaper. It was perfectly clear from the context what ‘bogus’ meant. but Mr Justice Eady (aided by a disastrous law) chose to ignore entirely the context. The description ‘bogus’. as used by Singh, seems to be entirely appropriate for a newspaper article. To criticise him for using “unprofessional” language is inappropriate because we are not dealing with professionals. At least there are some laughs to be had from the whole sorry affair. Prompted by that prince among lawyers known as Jack of Kent there was a new addition to my ‘Patients’ Guide to Magic Medicine’, as featured in the Financial Times.
|
Here are the changes that were made. Hmm.very interesting.
On 17th June 2009, 15 months after Singh’s article was published, the British Chiropractic Association (BCA) has finally produced its evidence (though only after enormous pressure from bloggers [download as pdf]..
Jack of Kent has already made some comments from the legal point of view.
As expected, the list of references they give is truly pathetic, The list of 29 references has nine about infantile colic, four about asthma (two of which refer to osteopathy not chiropractic). three about the safety of chiropractic (a contentious matter but not the point here) and three about the safety of non-steroidal anti-inflammatory drugs (an important matter but utterly irrelevant here).
Let’s look at the papers about colic. Most are in obscure alternative medicine journals, not easily available, but the BCA’s own synopsis is sufficient for now.
-
Klougart N, Nilsson N and Jacobsen J (1989) Infantile Colic Treated by Chiropractors: A Prospective Study of 316 Cases, J Manip Physiol Ther,12:281-288. [ download thr reprint]. As evidence it is about as useless as the infamous Spence study so beloved of homeopaths. There was no control group at all. It simply follows 316 babies and found that most of them eventually got better. Well, they do, don’t they? It is a sign of the pathetic standard of research in chiropractic that anyone should think this paper worth mentioning at all.
-
Mercer, C. and Nook, B. in the Proceedings of the 5th Biennial Congress of the World Federation of Chiropractic (1999) (so no peer review, for what that is worth). “Resolution of symptoms [of infantile colic] in 93% of infants treated with spinal manipulation”.. This sounds as useless as Klougart et al. Why only 93% one wonders? Every parent knows that 100 percent of babies stop crying eventually.
-
Wiberg et al. J Manip Physiol Ther, 1999, 242 517 – 522. This one was randomised (but not blind) and showed that spinal manipulation was as effective as dimethicone for colic. [Download pdf]
I expect that all that means is that dimethicone doesn’t work either. -
Hayden & Mullinger (2006) Complementary Ther. clin. Prac. “This preliminary study suggested that cranial osteopathic treatment can benefit infants with colic”. So. (a) preliminary and (b) not chiropractic.
-
Hipperson AJ (2004) Clinical Chiropractic 11, 122 – 129. A report of two case studies, so essentially worthless as evidence The journal isn’t even listed in Pubmed.
-
Browning M. Miller, J. Clinical Chiropractic (2008) 11, 122—129 [download pdf] Comparison of the short-term effects of chiropractic spinal manipulation and occipito-sacral decompression in the treatment of infant colic: A single-blinded, randomised, comparison trial. This paper just compared two different chiropractic methods. It shows that both are equally effective, or equally plausibly, both are equally ineffective.
- Leach RA (2002) J Manip Physiol Ther, 25, 58 -62. Merely two case reports and they refer to usie of a mechanical device, not the usual chiropractic manipulation.
-
Miller J (2007) Clinical Chiropractic 10, 139—146 Cry babies: A framework for chiropractic care [download pdf]. No evidence at all here. It isn’t a research paper.
- Nilsson N. 1985 Eur J Chiropr 33, 264 – 255 Infantile colic and chiropractic. “Respondents to a questionnaire revealed that 91% of of infants improved after 2 – 3 manipulations”. Again, no controls. So, babies stop crying, eventually.
That seems to be the best they can do. What they don’t do is mention any of the papers that contradict their claims. They cite Sackett et al. (1996) as their criterion for what constitutes evidence, That paper says “Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence”. That means all the evidence. So why, for example, is there no mention of Olafsdottir et al. (2001), “Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation”. That is one of the few really good papers in the area. It compared chiropractic treatment of babies for colic with placebo treatment (the nurse just held the baby for 10 minutes (the time the chiropractor took). The conclusion was
Conclusion Chiropractic spinal manipulation is no more effective than placebo in the treatment of infantile colic. This study emphasises the need for placebo controlled and blinded studies when investigating alternative methods to treat unpredictable conditions such as infantile colic.
More on this dishonest selectivity can be found at Holfordwatch.
No doubt there will soon be more analyses of what passes, in the eyes of the BCA, for evidence, The nine papers they cite for colic are truly pathetic. Not a single one of them amounts to anything that would be recognised as evidence in the real world. And papers that do provide real evidence are not mentioned.
Follow-up
As always, the blogs provided a very fast response to a document that appeared only late last night. And, as always, these unpaid people, working in their spare time, have done a far better job than the suits at the BCA (or NICE).
Here are some of them.
“A Review of The BCA’s Evidence for Chiropractic”. Martin on The Lay Scientist.
“The BCA have no evidence that chiropractic can help with ear infections” on Gimpy’s blog.
“Examining the BCA’S ‘Plethora’ of Evidence”. Unity, at Ministry of Truth.
“British Chiropractic Association and The Plethora of Evidence for Paediatric Asthma”. On Evidence Matters
“BCA Statement Baffles Blogger”. James Cole on jdc325’s Weblog
“Careful, BCA, you might slip a disk. The British Chiropractic Association may need to hire a chiropractor to work on themselves: they’re shoveling so hard they’re likely to hurt their backs.” In the US magazine, Discover.
“British Chiropractic Association (BCA) demonstrate what evidence-based medicine isn’t” at Holfordwatch. This one shows nicely how the BCA fail to apply their own standard of evidence, based on Sackett et al. (1996).
“The BCA’s worst day”. “Today has not been a good day for the British Chiropractic Association”. Jack of Kent summarises the demolition, in 24 hours, of the BCA’s ‘evidence’
Laurie Taylor says it all.
Could this bit (dated 18 June) in Laurie Taylor’s saga of the University of Poppleton possibly have been inspired by the Singh affair?
|
Sweet smell of success Our campus burst into colour last week as members of the Department of Aromatherapy, led by Professor Gwendolyn Frisson, paraded round the former administrative block happily waving bunches of wild carrot, devil’s claw, cinnamon leaf and lime blossom. What sparked the herbal celebration was the news of a full retraction from the journalist on the Poppleton Evening News who had described the department in print as “a hotchpotch of untestable propositions and unproven medical interventions”. The journalist in question, Simeon Rainbow, explained in his published retraction that he’d had time to reflect on the department’s reaction to his original article and now fully recognised that there was no better way of deciding upon the scientific validity of practices such as aromatherapy than by threatening anyone who denied such validity with an enormously costly libel action. Professor Frisson said that she welcomed the retraction. She would now be able to return with renewed enthusiasm to her research on the beneficial effects of grated angelica root on patients with advanced encephalitis. |