herbal medicine
|
It seems that bits of good news don’t come singly. First honours degrees in acupuncture vanish, Now a big chain of shops selling Chinese herbs and acupuncture has gone into administration. It seems that, at last, people are getting fed up with being conned out of their hard-earned money |
 Herbmedic Barking |
A local newspaper, The North Herts Comet reported thus.
Customers of Herbmedic, which trades under the name Herbs and Acupuncture, on Queensway in Stevenage have been left counting the cost after shelling out hundreds of pounds for treatment they never received.
The company, which has practices across the country, is now in the hands of receivers, Macintyre Hudson.
Sandra Emery, of The Paddocks in Stevenage, paid £350 for 10 treatment sessions, but only received one before the practice closed.
She said: “A standard course of treatment is 10 sessions, so most customers will have bought this package.
Claudia Gois, of Walden End in Stevenage, paid £240 for 12 treatment sessions but only received four before the practice closed.
She said: “I went there on Friday and it was closed. There was no warning or anything.
“I got in touch with head office and they said it’s very unlikely I will get money back.
This report was on 1st April, The company’s web site shows no sign of any problems, In fact they are still advertising jobs. So was this an April Fool joke?
No it wasn’t. A visit to Companies House soon settled the matter. The whole company is insolvent, as of 27 March 2009..
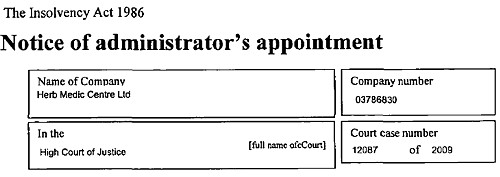
Download the whole administration notice and the company report.
Criticisms of Herbmedic
This chain of shops was investigated by the BBC’s
Inside Out programme. (September 25th 2006).
“We sent an undercover reporter to branches of the Herbmedic chain in southern England.
On each occasion, the reporter claimed to be suffering from tiredness and was prescribed herbal remedies after a consultation lasting less than five minutes.
The herbalists, who describe themselves as “doctors”, didn’t ask any questions about the patient’s medical history or take any notes.”
This is so bad that even Andrew Fowler, a past President of the Register of Chinese Herbal Medicine, described it as “malpractice”.
“Herbmedic has been investigated by the authorities in the past.
In 2002, trading standards officers prosecuted the branch in Southampton for selling herbal remedies with 26 times the permitted legal limit of lead.
And in October 2003, the Advertising Standards Authority banned Herbmedic from describing its practitioners as “doctors”.
Despite the ban, all three of the stores visited by Inside Out referred to the herbalist as the doctor.”
See also the BBC report Herbalists’ customers ‘at risk’, and a report in the Sunday Times, Herbmedic accused of high-pressure selling.
Read the Advertising Standards report. Seven different complaints against Herbmedic were upheld.
This is entirely consistent with my own experience. I went into one of their shops and asked about a cure for diabetes (hoping the be able to refer them to Trading Standards, but the young lady behind the counter had such a poor grasp of English that her reply was incomprehensible. She just kept trying to push me into having a consultation with “the doctor” who appeared to speak no English at all. I left.
The chequered history of Herbmedic
The company that his just gone into administration is Herbmedic Centre Ltd. It has been in existence for only two years. Its predecessor, known simply as Herbmedic, was dissolved on 13 March 2007, Companies House said
Company Filing History Type Date Description Order GAZ2(A) 13/03/2007 FINAL GAZETTE: DISSOLVED VIA VOLUNTARY STRIKE-OFF GAZ1(A) 28/11/2006 FIRST GAZETTE NOTICE FOR VOLUNTARY STRIKE-OFF 652a 16/10/2006 APPLICATION FOR STRIKING-OFF
Another Chinese medicine chain seems to be having a few problems too
Harmony Medical Distribution Ltd (“specialists in acupuncture and holistic medicine”) seems to be still in business(web site here), but several very similar companies have been dissolved, Harmomy Medics Ltd (dissolved 19 Sep 2006) ,, Harmony Medical Services (UK ) Ltd. (dissolved 6 May 2008) and Harmony Medical Services Ltd (dissolved 17 Oct 2008)
Given this history of companies that dissolve every couple of years and then mysteriously reincarnate with a slightly different name, one wonders if this really is the end of herbmedic, or it is just a device for shedding bad debts. Is this just another “pre-pack administration“?
Watch this space for more.
What’s the latest evidence on acupuncture anyway?
A correspondent drew my attention to the 2009 Annual Evidence Update on acupuncture complied by the NHS Complementary and Alternative Medicine Specialist Library. This includes no fewer than 56 systematic reviews and meta-analyses. Although the reviews are complied by alternative medicine sympathisers, they seem mostly to be pretty fair. Well apart form one thing.
Almost all of the reviews fail to come up with any positive evidence that acupuncture works well enough to be clinically useful. Only two come close, and they are the two singled out as “editor’s picks”. Perhaps that’s not entirely surprising given that the editor is Dr Mike Cummings.
Again and again, the results are inconclusive: #8 is pretty typical
Acupuncture for tension-type headache: a meta-analysis of randomized, controlled trials.
This meta-analysis suggests that acupuncture compared with sham for tension-type headache has limited efficacy for the reduction of headache frequency. There exists a lack of standardization of acupuncture point selection and treatment course among randomized, controlled trials. More research is needed to investigate the treatment of specific tension-type headache subtypes.
Vast effort and a lot of money is being put into trials, yet there are very few (if any) positive results. Very often there are no results at whatsoever. All we hear, again and again, is “more research is needed”.
At some point someone will have to decide it is all a charade and start to spend time and money on investigating things that are more promising.
Follow-up
A correspondent checked with Companies House to discover more about two of the directors of Herbmedic, Mr. Li Mao and Mr Xiao Xuan Chen. They have a chequered history indeed. [download the complete list]
Mr. Li Mao is, or has been, on the board of 31 different companies. Of these 6 are active, 5 are in administration, 14 were dissolved, 4 were liquidated and 2 are active with proposal to strike off. Not only is Her Medic centre Ltd in administration, but so is Dr China (UK) Ltd, and Great Chinese Herbal Medicine Ltd
With record like that, my correspondent wonders whether they should be disqualified.
The Health Professions Council (HPC) is yet another regulatory quango.
The HPC’s strapline is
|
 |
At present the HPC regulates; Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists.
These are thirteen very respectable jobs. With the possible exception of art therapists, nobody would doubt for a moment that they are scientific jobs, based on evidence. Dietitians, for example, are the real experts on nutrition (in contrast to “nutritional therapists” and the like, who are part of the alternative industry). That is just as well because the ten criteria for registration with the HPC say that aspirant groups must have
“Practise based on evidence of efficacy”
But then came the Pittilo report, about which I wrote a commentary in the Times, and here, A very bad report: gamma minus for the vice-chancellor, and here.
Both the Pittilo report, the HPC, and indeed the Department of Health itself (watch this space), seem quite unable to grasp the obvious fact that you cannot come up with any sensible form of regulation until after you have decided whether the ‘therapy’ works or whether it is so much nonsense.
In no sense can “the public be protected” by setting educational standards for nonsense. But this obvioua fact seems to be beyond the intellectual grasp of the quangoid box-ticking mentality.
That report recommended that the HPC should regulate also Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners. Even more absurdly, it recommended degrees in these subjects, just at the moment that those universities who run them are beginning to realise that they are anti-scientific subjects and closing down degrees in them.
How could these three branches of the alternative medicine industry possibly be eligible to register with the HPC when one of the criteria for registration is that there must be “practise based on evidence of efficacy”?
Impossible, I hear you say. But if you said that, I fear you may have underestimated the capacity of the official mind for pure double-speak.
The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
But the last conclusion contradicts directly the requirement for “practise based on evidence of efficacy”. I was curious about how this contradiction
could be resolved so I sent a list of questions. The full letter is here.
The letter was addressed to the president of the HPC, Anna van der Gaag, but with the customary discourtesy of such organisations, it was not answered by her but by Michael Guthrie, Head of Policy and Standards He said
“Our Council considered the report at its meeting in July 2008 and decided that the regulation of these groups was necessary on the grounds of public protection. The Council decided to make a recommendation to the Secretary of State for Health that these groups be regulated.
http://www.hpc-uk.org/assets/documents/100023FEcouncil_20080911_enclosure07.pdf “.
This, of course, doesn’t answer any of my questions. It does not explain how the public is protected by insisting on formal qualifications, if the qualifications
happen to teach mythical nonsense. Later the reply got into deeper water.
“I would additionally add that the new professions criteria are more focused on the process and structures of regulation, rather than the underlying rationale for regulation – the protection of members of the public. The Council considered the group’s report in light of a scoring against the criteria. The criteria on efficacy was one that was scored part met. As you have outlined in your email (and as discussed in the report itself) the evidence of efficacy (at least to western standards) is limited overall, particularly in the areas of herbal medicines and traditional Chinese medicine. However, the evidence base is growing and there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs.”
Yes, based on process and structures (without engaging the brain it seems). Rather reminiscent of the great scandal in UK Social Services. It is right in one respect though.
The evidence base is indeed growing, But it is almost all negative evidence. Does the HPC not realise that? And what about “at least by Western standards”? Surely the HPC is not suggesting that UK health policy should be determined by the standards of evidence of Chinese herbalists? Actually it is doing exactly that since its assessment of evidence was based on the Pittilo report in which the evidence was assessed (very badly) by herbalists.
One despairs too about the statement that
“there was a recognition in the report that the individualised approach to practice in these areas did not lend themselves to traditional RCT research designs”
Yes of course the Pittilo report said that, because it was written by herbalists! Had the HPC bothered to read Ben Goldacre’s column in the Guardian they would have realised that there is no barrier at all to doing proper tests. It isn’t rocket science, though it seems that it is beyond the comprehension of the HPC.
So I followed the link to try again to find out why the HPC had reached the decision to breach its own rules. Page 10 of the HPC Council report says
3. The occupation must practise based on evidence of efficacy This criterion covers how a profession practises. The Council recognizes the centrality of evidence-based practice to modern health care and will assess applicant occupations for evidence that demonstrates that:
- Their practice is subject to research into its effectiveness. Suitable evidence would include publication in journals that are accepted as
learned by the health sciences and/or social care communities- There is an established scientific and measurable basis for measuring outcomes of their practice. This is a minimum—the Council welcomes
evidence of there being a scientific basis for other aspects of practice and the body of knowledge of an applicant occupation- It subscribes to the ethos of evidence-based practice, including being open to changing treatment strategies when the evidence is in favour
of doing so.
So that sounds fine. Except that research is rarely published in “journals that are accepted as learned by the health sciences”. And of course most of the good evidence is negative anyway. Nobody with the slightest knowledge of the literature could possibly think that these criteria are satisfied by Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
So what does the HPC make of the evidence? Appendix 2 tells us. It goes through the criteria for HPS registration.
“Defined body of knowledge: There is a defined body of knowledge, although approaches to practice can vary within each area.”
There is no mention that the “body of knowledge” is, in many cases, nonsensical gobbledygook and, astonishingly this criterion was deemed to be “met”!.
This shows once again the sheer silliness of trying to apply a list of criteria without first judging whether the subject is based in reality,
Evidence of efficacy. There is limited widely accepted evidence of efficacy, although this could be partly explained by the nature of the professions in offering bespoke treatments to individual patients. This criterion is scored part met overall.
Sadly we are not told who deemed this criterion to be “part met”. But it does say that “This scoring has been undertaken based on the information outlined in the [Pittilo] report”. Since the assessment of evidence in that report was execrably bad (having been made by people who would lose their jobs if
they said anything negative). it is no wonder that the judgement is overoptimistic!
Did the HPC not notice the quality of the evidence presented in the Pittilo report? Apparently not. That is sheer incompetence.
Nevertheless the criterion was not “met”, so they can’t join HPC, right? Not at all. The Council simply decided to ignore its own rules.
On page 5 of the Council’s report we see this.
The Steering Group [Pittilo] argues that a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base (p.11, p. 32, p.34).
This question can be a controversial area and the evidence base of these professions was the focus of some press attention following the report’s publication. An often raised argument against regulation in such circumstances is that it would give credibility in the public’s eyes to treatments that are not proven to be safe or efficacious.
This second point is dead right, but it is ignored. The Council then goes on to say
In terms of the HPC’s existing processes, a lack of ‘accepted’ evidence of efficacy is not a barrier to producing standards of proficiency or making decisions about fitness to practise cases.
This strikes me as ludicrous, incompetent, and at heart, dishonest.
There will be no sense in policy in this area until the question of efficacy is referred to NICE. Why didn’t the HPC recommend that? Why has it not been done?
One possible reason is that I discovered recently that, although there are two scientific advisers in the Department of Health,. both of them claim that it is “not their role” to give scientific advice in this area. So the questions get referred instead to the Prince of Wales Foundation. That is no way to run a ship.
The fact of the matter is that the HPC, like so many other regulatory agencies, fails utterly to protect the public from fraudulent and incompetent practitioners. In fact it actually protects them, in the same way that the financial ‘regulators’ protected fraudulent bankers. They all seem to think that ticking boxes and passing exams is an effective process. Even if the exams require you to memorise that amethysts “emit high Yin energy so transmuting lower energies and clearing and aligning energy disturbance as all levels of being”.
It’s only a matter of weeks since a lot of young scientists produced a rather fine pamphlet pointing out that the “detox” industry is simply fraud. They concluded
“There is little or no proof that these products work, except to part people from their cash.”
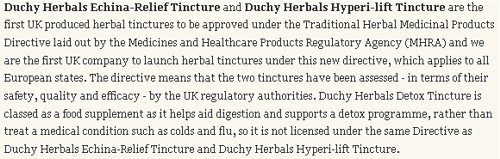
With impeccable timing, Duchy Originals has just launched a “detox” product.
Duchy Originals is a company that was launched in 1990 by the Prince of Wales, Up to now, it has limited itself to selling overpriced and not particularly healthy stuff like Chocolate Butterscotch Biscuits and Sandringham Strawberry Preserve. Pretty yummy if you can afford them.
The move of HRH into herbal concoctions was first noted in the blogosphere (as usual) in December, by Quackometer. It was reported recently in the Daily Telegraph (23rd January).
Expect a media storm.

Aha so it is a “food supplement” not a drug. Perhaps Duchy Originals have not noticed that there are now rather strict regulations about making health claims for foods?
And guess who’s selling it? Yes our old friend, for which no deception is too gross, Boots the Chemists.
That’s £10 for 50 ml. Or £200 per litre.
And what’s in it?

Problem 1. The word detox has no agreed meaning. It is a marketing word, designed to separate the gullible from their money
Problem 2. There isn’t the slightest reason to think that either artichoke or dandelion will help with anything at all. Neither appears at all in the Cochrane reviews. So let’s check two sources that are both compiled by CAM sympathisers (just so I can’t be accused of prejudice).
National Electronic Library of CAM (NELCAM) reveals nothing useful.
- There is no good evidence that artichoke leaf extract works for lowering cholesterol. No other indications are mentioned.
- Dandelion doesn’t get any mention at all.
The US National Center for Complementary and Alternative Medicine (NCCAM) has spent almost $1 billion on testing alternative treatments So far they have produced no good new remedies (see also Integrative baloney @ Yale).They publish a database of knowledge about herbs. This is what they say.
- Dandelion. There is no compelling scientific evidence for using dandelion as a treatment for any medical condition.
- Artichoke isn’t even mentioned anywhere.
If “detox” is meant to be a euphemism for hangover cure, then look at the review by Pittler et al (2005), ‘Interventions for preventing or treating alcohol hangover: systematic review of randomised controlled trials’.
“Conclusion No compelling evidence exists to suggest that any conventional or complementary intervention is effective for preventing or treating alcohol hangover. The most effective way to avoid the symptoms of alcohol induced hangover is to practise abstinence or moderation.”
Problem 3. The claim that the product is “cleansing and purifying” is either meaningless or false. Insofar as it is meaningless, it is marketing jargon that is designed to deceive. The claim that it supports “the body’s natural elimination and detoxification processes, and helps maintain healthy digestion” is baseless. It is a false health claim that, prima facie, is contrary to the Unfair Trading law, and/or European regulation on nutrition and health claims made on food, ref 1924/2006 , and which therefore should result in prosecution.
Two more Duchy herbals
Duchy are selling also Echinacea and Hypericum (St John’s Wort).
The evidence that Echinacea helps with colds is, to put it mildly, very marginal.
Of St John’s Wort, NCCAM says
“There is some scientific evidence that St. John’s wort is useful for treating mild to moderate depression. However, two large studies, one sponsored by NCCAM, showed that the herb was no more effective than placebo in treating major depression of moderate severity.”
As well as having dubious effectiveness it is well known that St John’s Wort can interact with many other drugs, a hazard that is not mentioned by Duchy Originals
These two are slightly different because they appear to have the blessing of the MHRA.
The behaviour of the MHRA in ignoring the little question of whether the treatment works or not has been condemned widely. But at least the MHRA are quite explicit. This is what the MHRA says of St. John’s Wort (my emphasis).
“This registration is based exclusively upon evidence of traditional use of Hypericum perforatum L. as a herbal medicine and not upon data generated from clinical trials.. There is no requirement under the Traditional Herbal Registration scheme to prove scientifically that the product works.“
But that bit about “There is no requirement under the Traditional Herbal Registration scheme to prove scientifically that the product works” does not appear in the Duchy Originals advertisement. On the contrary, this is what they say.
Yes, they claim that “the two tinctures [echinacea and hypericum] -in terms of their safety, quality and efficacy -by the UK regulatory authorities”
That is simply not true.
On the contrary, anyone without specialist knowledge would interpret bits like these as claims that there will be a health benefit.
![]()
That is claim to benefit your health. So are these.
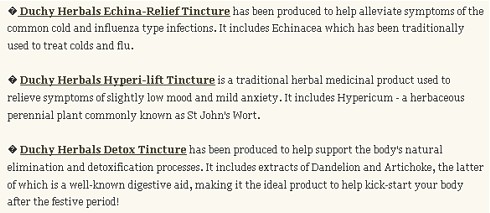
Who makes them?
Michael McIntyre is certainly a high profile herbalist.
He was founder president of the European Herbal Practitioners Association and a trustee of the Prince of Wales’s Foundation for Integrated Medicine. It seems that he a great believer in the myth of “detox”, judging by his appearance on the Firefly tonics web site. They will sell you
“Natural healthy energy” in a drink
That’s what we wanted…
A Wake up for that drowsy afternoon… Detox for a dodgy Friday morning…
Sharpen up for that interminable meeting.
We left the herbs to our wonderful herbalists.
Their De-tox contains lemon, lime, ginger, sarsparilla and angelica. I expect it tastes nice. All the rest is pure marketing rubbish. It does not speak very well of Michael McIntyre that he should lend his name to such promotions.
Nelsons, who actually make the stuff, is better known as a big player in the great homeopathic fraud business. They will sell you 30C pills of common salt at £4.60 for 84. Their main health-giving virtue is that they’re salt free.
If you want to know what use they are, you are referred here, where it is claimed that it is “used to treat watery colds, headaches, anaemia, constipation, and backache”. Needless to say there isn’t a smidgeon of reason to believe it does the slightest good for them.
And remember what Nelson’s advisor at their London pharmacy told BBC TV while recommending sugar pills to prevent malaria?
“They make it so your energy doesn’t have a malaria-shaped hole in it so the malarial mosquitos won’t come along and fill that in.”
You couldn’t make it up.
The Prince of Wales has some sensible things to say in other areas, such as the world’s over-reliance on fossil fuels. Even his ideas about medicine are, no doubt, well-intentioned. It does seem a shame that he just can’t get the hang of the need for evidence. Wishful thinking just isn’t enough.
Follow-up
Some more interesting reading about the Prince of Wales.
Michael Baum’s An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong”
Gerald Weissman’s essay Homeopathy: Holmes, Hogwarts, and the Prince of Wales.
Channel 4 TV documentary HRH “meddling in politics”
11 March 2009 The MHRA have censured Duchy Originals for the claims made for these products. and in May 2009, two complaints to the Advertising Standards Authority were upheld.
Herbal medicine is, unlike homeopathy, not ridiculous, It is merely Pharmacology, as practised up to circa 1900. Whereas good trials have now shown acupuncture to be sham and homeopathy to be a placebo, there has been very little good research on herbs.
Most herbalism could fairly be described giving to sick patients an unknown dose of a substance with unknown efficacy and unknown safety.
How odd, then, to visit the Royal Society of Medicine to be greeted thus.
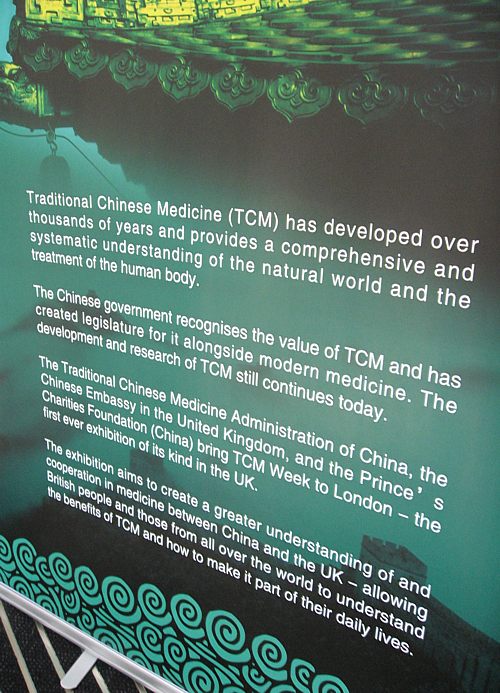
Just look at the words!
“Traditional Chinese Medicine (TCM) has developed over thousands of years”
That’s partly true
“and provides a comprehensive and systematic understanding of the natural world and the treatment of the human body.”
and that is total nonsense. TCM provides no understanding and virtually none of it is known to be useful for treating anything.
| Another poster at the RSM exhibition provides some of the explanation. What on earth, one wonders, do they mean by “making efforts to modernise TCM “? So far, the idea of modernising TCM doesn’t seem to include any great effort to find out if it works. Much of the promotion of TCM seems to be not so much ‘ancient wisdom’, but modern nationalist propaganda by the Chinese government. |
 |
The history is fascinating, but you won’t learn it from the posters on display at the exhibition.
“The Daoguang emperor though it [acupuncture] was a barrier to medical progress and removed it from the curriculum of the Imperial Medical Institute,”
“By the start of the twentieth century, acupuncture was extinct in the West and dormant in the East. It might have fallen out of favour permanently, but it suddenly experienced a revival in 1949 as a direct result of the communist revolution and the establishment of the People’s Republic of China. Chairman Mao Tse-tung engineered a resurgence in traditional Chinese medicine, which included not just acupuncture but also Chinese herbal medicine and other therapies ”
“His motivation was partly ideological, inasmuch as he wanted to reinforce a sense of national pride in Chinese medicine. However he was also driven by necessity. He had promised to deliver affordable healthcare .. . . ”
“Mao did not care whether traditional Chinese medicine worked, as long as he could keep the masses contented. In fact, his personal physician, Zhisui Li, wrote a memoir entitled ‘The Private Life of Chairman Mao’, in which he quoted Mao as saying”
“Even though I believe we should promote Chinese medicine, I personally do not believe in it. I don’t take Chinese medicine.” “
Singh & Ernst Trick or Treatmant, page 46.
Or, as put more succinctly by Shapiro
“You would never know that TCM was fashioned in the twentieth century, as we shall see, from a ragbag of therapies in post-revolutionary China.”
Rose Shapiro, Suckers, how alternative medicine makes fools of us all.
Why is the Royal Society of Medicine allowing such mendacious posters? As it happens, I and a friend were visiting the RSM to see their Academic Dean, with a view to finding out why the RSM had failed to take any public position on alternative medicine. The answer appeared to be money, and that was the answer to why the TCM exhibition was being held on their premises too. The Dean no more believed in TCM than we did, but, well, they need the income. He pointed out (looking suitably sheepish) that the address given for the exhibition was not the RSM, but Number 1 Wimpole Street (that, of course, is also the address of the RSM).
Ah, so that’s OK then.
It has to be said that the RSM isn’t alone in its spineless attitude. Both the British Medical Association (BMA) and the Royal College of General Practitioners (RCGP) have failed to make any clear condemnation of mystical medicine. This is in stark contrast to just about every relevant scientific society (here is a summary).
It is a mystery to me why much of medicine should still be dominated by a mindset that seems to have lagged 200 years behind every other science. Perhaps medicine is just too complicated.
UCL Hospitals’ skeleton in the cupboard
Make no mistake, University College London Hospital is top class. The UCLH Trust. runs seven hospitals All but one of them are excellent. But in 2002 the Royal London Homeopathic Hospital was acquired as part of the UCLH group, to the intense embarrassment of UCL scientists.
Let’s start with the good bit. Usually I don’t like anecdotes, so just think of this as a vote of thanks, not evidence.
A personal history of UCH
I owe UCLH a lot personally. On December 13th 1984, my wife had
a subarachnoid haemorrhage when she was seven months pregnant. After misdiagnosis at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millilmetre from the pituitary on the other. It was a bit tricky but I think we got it”.
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds).. Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. | 
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album.. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. Heaven knows what it would have cost in the USA.
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew playing cricket in Bangladesh, Feb 2005. |
But now the the less desirable side of UCLH
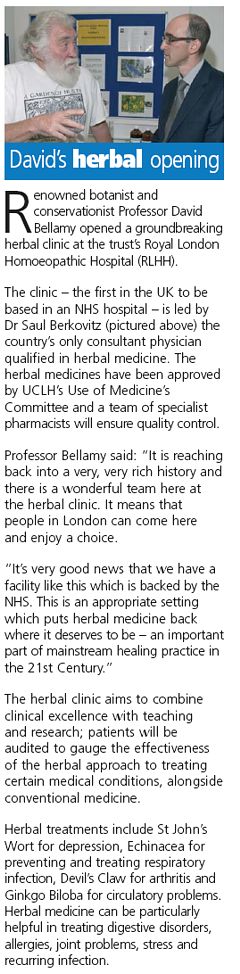
Herbs and homeopaths at UCLH
| Recently I was sent the UCLH Annual Review 2007 – 2008. There was a lot of good stuff in it and worth a read despite there being too much hyperbole and too many pictures of men in dark suits. But buried among all the high tech stuff, what do we find but an advertisement for 1900-style pharmacology in the form of the herbal clinic at the Royal London Homeopathic Hospital, accompanied by a load of utterly inaccurate information from the TV botanist, David Bellamy. Take, for example, the claim about Devil’s Claw for osteoarthritis. Even alternative medicine advocates said “The authors concluded that there are insufficient high-quality trials to determine the safety and efficacy of Devil’s Claw (Harpagophytum procumbens) in the treatment of osteoarthritis, and that definitive trials are needed.”
Reading between the lines, I’d guess that the opening of this clinic has a subtext. It is well known that funding for homeopathy has dried up (partly as a result of our letter to NHS Trusts that appeared in the There have been problems before with the herbal activities at the RLHH before (see Conflicts of Interest at the Homeopathic Hospital). It appeared that the Khans, who run the Marigold homeopathic podiatry clinic (no, seriously, it is real) were largely prescribing a herbal product that was made by their own company. without even the hospital trust, never mind the patients, being made aware of it. In normal medicine this would be regarded as a rather serious offence, but as far as I know, nothing was ever done about it. |
 |
The ethics of alternative medicine are truly one of life’s great mysteries.
Reading further in the annual review, we come to the page about the RLHH. The homeopathy side must really have run down because it seems to have diversified into selling cosmetics and groceries. That sounds like desperation.

Good heavens, they sell “chemical-free sun cream”. One wonders what it can be made of, if not chemicals. This is the language of low-grade advertising agencies, not what one expects from an NHS hospital trust.
But next to this there is a much more interesting item. Just look at the last sentence.
I wonder if this could possibly have anything to do with the fact that Michael Baum and I visited the Trust headquarters in August 2006 to propose that the RLHH might be turned into a centre of supportive and palliative care? It would be nice to think so. But it seems they haven’t gone nearly far enough yet. If all they do is replace the waning homeopathy We know they are under pressure from their royal patrons, but that, in a constitutional monarchy, is simply not acceptable. |
 |
Michael Baum is a cancer surgeon who has taken a particular interest in palliative and supportive care. He is someone whose views should be taken seriously. He is also the author of the magnificent “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong” Here is a quotation from that letter. The UCLH Trust should bear it in mind.
| The power of my authority comes with a knowledge built on 40 years of study and 25 years of active involvement in cancer research. I’m sensitive to the danger of abusing this power and, as a last resort, I know that the General Medical Council (GMC) is watching over my shoulder to ensure I respect a code of conduct with a duty of care that respects patients’ dignity and privacy and reminds me that my personal beliefs should not prejudice my advice. Your power and authority rest on an accident of birth. Furthermore, your public utterances are worthy of four pages, whereas, if lucky, I might warrant one. I don’t begrudge you that authority and we probably share many opinions about art and architecture, but I do beg you to exercise your power with extreme caution when advising patients with life threatening diseases to embrace unproven therapies. There is no equivalent of the GMC for the monarchy, so it is left either to sensational journalism or, more rarely, to the quiet voice of loyal subjects such as myself to warn you that you may have overstepped the mark. It is in the nature of your world to be surrounded by sycophants (including members of the medical establishment hungry for their mention in the Queen’s birthday honours list) who constantly reinforce what they assume are your prejudices. Sir, they patronise you! Allow me this chastisement. |
Follow-up
The photo album chronicling the birth of my son, is really just for family and friends, but at least one blog picked up on the wider significance.
The Times today has given s good showing for my comment piece. It gives the case against following the advice of the Pittilo report. It simply makes no sense to have government regulation of acupuncture, herbal medicine, traditional Chinese medicine until such time as there is evidence that they work. It makes even less sense to have BSc degrees in them. The Department of Health should have more sense that to use the Prince of Wales as its scientific advisor.
Let’s hope that the recent example set by the University of Central Lancashire is the start of trend for vice-chancellors to appreciate that running such degrees brings their universities into disrepute.
I can only apologise for the dreadful title that The Times’ sub-editors put on the piece, My original title was
A bad report for the vice chancellor
The Pittilo report to the Department of Health will endanger the public and corrupt universities. There is a better way.
I like that much better than “Regulate quack nedicine? I feel sick”.
But, oh dear, the picture that I sent them is on the left, but what appeared is on the right. Spot the difference.
 |
 |
Well now, at least, I can feel I have something in common with Isambard Kingdom Brunel.
Follow-up
It so happens that Professor Pittilo wrote a letter to Times Higher Education this week. I fear that it provided a yet more evidence that he hasn’t really quite got the hang of evidence.
The Lancashire Evening Post catches up with the UCLan story, two days after you read it here.
A reply from Professor Pittilo
This response to the op-ed of 29th August appeared as a letter
in the Times on Sept 2.
| Public health needs protection
Regulation of acupuncture and herbal medicine has been subject to much scrutiny Sir, Professor Colquhoun’s campaign to discredit our report (“Regulate quack medicine? I feel sick,” Aug 29) is in danger of placing public health at risk. He is entitled to challenge existing evidence for the effectiveness of complementary and alternative medicine (CAM) but fails to acknowledge the key recommendation from the steering group on the essential need to demonstrate efficacy, safety and quality assurance as a prerequisite for NHS funding. Professor Colquhoun dismisses CAM because of the absence of a rigorous scientific foundation and he asserts that to teach and practise it is unethical. Survey data consistently demonstrates very high demand for CAM with one report estimating that 22 million visits involving 10.6 per cent of the population in England alone occurred in 2008. This demand is one reason why his alternative model of trade law enforcement will not work. He may argue that these people are uncritical recipients of nonsense, but data from the Medicines and Healthcare products Regulatory Agency confirm that they are at significant risk from poor practice. It is essential that we protect the public by implementing statutory regulation alongside demanding evidence of efficacy. Professor Colquhoun’s resistance to the teaching of science to CAM practitioners will do little to help them to critically evaluate effectiveness. Professor Michael Pittilo Chair of the Department of Health Steering Group |
And Pittilo wrote in similar vein to Times Higher Education.
Science vital to health study28 August 2008 Your feature on some members of staff at the University of Central Lancashire attacking science degrees in complementary and alternative medicine (“Staff attack science degrees in alternative health”, 7 August) raises a number of concerns. It is up to any university, taking account of the expert views of staff and external peer review, to determine the appropriate title and award for any degree. It is encouraging to note from the feature that new courses The recent report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and other Traditional Medicine There is no doubt that courses that provide a solid scientific foundation will greatly assist CAM practitioners in establishing evidence-based practice. It would be most unfortunate if the reported resistance to degree titles led to those wishing to practise acupuncture or herbal medicine receiving less hard science than they might have. To say that acupuncture and herbal medicine degrees have no academic justification appears arrogant in the extreme. Although it is certainly true that some content may not be scientific, this does not invalidate the legitimacy of these courses at degree level, a fact borne out by their successful validation in a number of universities. R. Michael Pittilo, Principal and vice-chancellor, The Robert Gordon University. |
This one got excellent responses from Kevin Smith (University of Abertay, Dundee), and from Peter J. Brophy (Professor of veterinary anatomy and cell biology University of Edinburgh). This was my comment to THE
There are a few very obvious responses to Professor Pittilo’s letter
For many alternative therapies the “philosophy” is simply incompatible with science. One obvious example is homeopathy. On Mondays and Wednesdays (science days) the students will be required to learn that response increases with dose. On Tuesdays and Thursdays will be taught the opposite. But for the exam they must reproduce only the latter (nonsensical) idea because their aim is to get a job as a homeopath. That makes nonsense of the idea of a university.
This seems to constitute a recognition that the evidence is still very inadequate. The time to start degrees, and the time to give official government recognition, is after the evidence is in, not before. What happens if you start degrees and then find that the subject is so much nonsense? Well, that has already happened in several areas of course. But the people who accredit the course and who act as external examiners just happen to be fervent believers in that nonsense, so all appears to be well (to bean counters anyway).
There is, as it happens, a great deal of evidence now about acupuncture, but the authors of the report do not seem to be aware of it. I recommend Barker Bausell’s book on the topic. If students are educated science, like what constitutes evidence, and our current understanding of words like “energy”, they would have to disavow the subject that there are supposed to training to practise
No, it is not a matter of arrogance, just a matter of careful attention to the evidence. Attention to evidence was notably absent in Prof Pittilo’s report, perhaps because his committee consisted entirely of people who earn their living from the subjects they were supposed to be assessing.
I have had the misfortune to have waded through a mound of such validation documents. The one thing they never consider is whether the treatment works. Sad to say, these validations are not worth the paper they are written on. |
This was posted originally on the old IMPROBABLE SCIENCE page
UCL felled by a herbalist?
OK this isn’t really bad science, but it’s caused inconvenience to me and to readers. It still puzzles me that UCL has not got the resources to deal with a herbalist (the reason that I was given for the move). The herbalist in question, Ann Walker, got rather angry when I called her use of the term ‘blood cleanser’ as gobbledygook
On Friday 1 June, 2007, when it was announced that the IMPROBABLE SCIENCE page had been moved from the UCL server, several people sent letters to the provost. Here is one of them. I have never met Prof Shafer, but his letter, and other similar ones, lightened an otherwise bad day.
| Dear Dr. Grant:I am very sorry to learn that you have requested Dr. Colquhoun to remove his “Improbable Science” web page from the computer system at University College London. It is particularly disheartening to learn that you made this request after receiving a complaint from a practitioner of nonscientific medicine.
I don’t know how many of your faculty publish in Nature (Colquhoun D. Science degrees without the science. Nature. 2007;446:373-4). However, based on my experience at Stanford, I would guess precious few. You now appear to be attempting to squelch his academic freedom, or at least disassociate UCL from his efforts to educate the public about quack science. Perhaps you were put off by the “unprofessional appearance” of the web page. If so then you have misunderstood its purpose. The public is inundated by junk science, A large portion come from the Internet. There are almost no Internet resources where a lay reader can find a counterweight to the extensive claims of pseudoscientists. Dr. Colquhoun’s blog is a unique resource. The format may put off a scientific reader, but it is exactly the format required to get the message to the web surfer with a 10 second attention span. In my view the Improbable Science web page was among the most important public services made available by the University College London. I don’t know the facts of your decision. Perhaps there are policies, procedures, and regulations that Dr. Colquhoun has violated in creating the Improbable Science web page. However, I do know that any request to remove the page that follows a complaint from an individual offended by the page is entirely inappropriate. Even were your request otherwise reasonable, the mere appearance of academic censorship should have been absolutely unacceptable to you. (Think of it like conflict of interest – there is a need to avoid not only true conflict of interest, but the mere appearance of It is thus with shock, sadness, and disappointment that I have learned of this decision by the University College London. I hope that you will reconsider. The present course makes it appear that UCL has caved in to pseudoscientists and is engaged in academic censorship of possibly the most important public service offered by the UCL. Sincerely, Steve Shafer Steven L. Shafer, MD Editor-in-Chief, Anesthesia & Analgesia Professor, Department of Anesthesia, Stanford University Adjunct Professor, Biopharmaceutical Sciences, UCSF Stanford University Medical Center Stanford, CA 94305 |
No doubt it is an exaggeration to say “the Improbable Science web page was among the most important public services made available by the University College London”. But thanks anyway.
After an unrepentant response, Professor Shafer replied thus.
| Dear Provost Grant:I appreciate your taking the time to respond. I’m sure that as provost you live on the receiving end of a firehose of correspondence, as do I as a professor and a journal Editor-in-Chief. I’m sorry to have added to the e-mail overload. I appreciate your finding time to respond.
It would be my hope that Stanford University would shoulder the responsibility of dealing with whatever harassment would come my way by virtue of my scientific and academic pursuits. Yes, when legal action is threatened, and staff are consumed with processing paperwork, I’m sure my Dean, Provost, and President would prefer to ransfer everything to me. However, the effect would be chilling. Universities are supposed to provide a haven to insulate scientists from harassment. I’ve looked at Dr. You note that Dr. Colquhoun “accepts that he needs to be in a position where he shoulders directly the burden of responding to Dr Lakin.” I applaud his fortitude, but note that are only 24 hours in a day. If the administrative resources of University College London are inadequate to respond to Dr. Lakin, how is Dr. Colquhoun, on his own, without the resources of UCL, expected to survive the harassment, legal hallenges, and other pressures to silence him? As a counter example, the University of California at San Francisco stood solidly behind Stanton Glantz when the cigarette industry tried to destroy him for his efforts to expose their activities. Had he agreed to “shoulder directly the burden”, we would never have known of the extensive research conducted by the cigarette industry over two decades that identified the health risks, and guided their extensive disinformation campaign. I would hope that Stanford University would following the UCSF example, and devote the necessary resources to defend my academic freedom, rather than the UCL Again, I appreciate your responding to my e-mail. I hope that my perspective is a least thought provoking on the complex mutual responsibilities between a prestigious University and an equally prominent faculty member with outspoken views. Thank you for your consideration, Sincerely, Steve Shafer |
The Goldacre effect
Saturday 9 June 2007. The wires (and my hit counter) are melting after Ben Goldacre’s comments on the move of this web site from UCL’s servers. That’s understandable: his excellent badscience.net site gets 12,000 hits a day and 95,000 unique visitors per month.
Like all the other comments, his badscience column in today’s Guardian, was not solicited by me, but it’s wonderful to know that somebody cares. His badscience.net version (“The Mighty David Colquhoun” !) was even more over-the-top. I can’t say I’m feeling very “mighty” at the moment.
Goldacre’s piece starts “I’ve always said you’d get a lot more kids interested in science if you told them it involves fighting – which of course it does.” A correspondent today enlarged on the theme “you have got me thinking and yes my kids would be far more interested in science if a playstation game was created whereby Prof. Colquhoun was zapping disgruntled alternative therapists”. The mind boggles. Making money out of selling mindless violence (in the news again today) must be even worse than making money out of selling useless pills. A university should be one of the few places left where one cannot be accused of knowing the price of everything, and the value of nothing.
Contrary to what some people seem to think, I don’t enjoy rows. They keep me awake at night. But some things are just too important to duck out of them.
Read the provost’s reply.
Goldacre has posted the complete text of the provost’s reply to one of the many people who have written to him. You should read the other side of the story too (click here and search for “letter from provost”). Grant has a real problem. He shouldn’t have to spend time fending off herbalists. Yet if they aren’t fended off, more attacks will occur. Who’d be a provost? That is all sorted out now.
