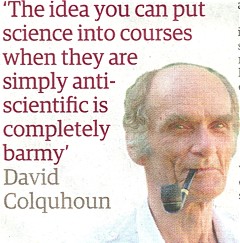
antiscience
On 23rd May 2008 a letter was sent to the vice-chancellor of the University of Westminster, Professor Geoffrey Petts
|
 |
Despite reminders, we were never afforded the courtesy of a reply to this, or any other letter.
Professor Petts has, however, replied to a letters sent to him recently by the Nightingale Collaboration. He said
“Whilst I understand your concerns, colleagues of the School of Life Sciences where these courses are offered do not share them. They are not teaching pseudo-science, as you claim,…”.
Neither of thse claims is true.I know at least two members of the Life Sciences Faculty who are very worried. One has now left and one has retired. The rest are presumably too scared to speak out.
It is most certainly not true to say they "are not teaching pseudo-science". Both the vice-chancellor and the Dean of Life Sciences, Jane Lewis, have been made aware of what;s happening repeatedly over several years, I can think of no other way to put it but to say Professor Petts is lying. Tha is not a good thing for vice-chancellors to do.
Much of what is taught at Westminster has now been revealed. This seems like a good moment to summarise what we know. Searching this blog for "University of Westminster" yields 39 hits. Of these, 11 show what’s taught at Westminster, so I’ll summarise them here for easy reference.
March 26th, 2007
The day after “Science degrees without the Science“ appeared in Nature, the University of Westminster issued a statement (now vanished, but see debate in THE). In my view, their statement provides the strongest grounds so far to believe that the BSc is inappropriate.
Let’s take a look at it.
|
“The BSc (Hons) Health Sciences: Homeopathy is a fully validated degree that satisfies internal and external quality assurance standards.”
|
Since that time, the university has closed down the BSc in Homeopathy. I have now seen many such validation documents and they are mostly box ticking exercises, not worth the paper they are written on. The worst offender is the University or Wales.
Westminster University BSc: “amethysts emit high yin energy”
April 23rd, 2008
http://dcscience.net/vib-therapies-43s.jpg
|
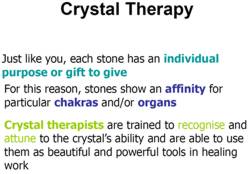
This shows the first set of slides that I got from Westminster (leaked by an angry insider). It has slides on crystal healing and dowsing, things that are at the lunatic fringe even by the standards of alternative medicine. it also relates that an academic who invited me to give a talk at the University of Westminster on the evidence for alternative medal was leaned on heavily by “VC, Provosts and Deans” to prevent that talk taking place. |
|
Crystal balls. Professor Petts in Private Eye
February 19th, 2009
Professor Petts makes an appearance in Private Eye. It could held that this counts as bringing your university into disrepute.
February 24th, 2009
BSc courses in homeopathy are closing. Is it a victory for campaigners, or just the end of the Blair/Bush era?
|
Professor Petts of Westminster seems to think that the problem can be solved by putting more science into the courses The rest of the world realises that as soon as you apply science to homeopathy or naturopathy, the whole subject vanishes in a puff of smoke, I fear that Professor Petts will have to do better,
|
 |
The Guardian carries a nice article by Anthea Lipsett, The Opposite of Science (or download pdf of print version).
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
March 30th, 2009
In March 2007 I wrote a piece in Nature on Science degrees without the science. At that time there were five “BSc” degrees in homeopathy. A couple of weeks ago I checked the UCAS site for start in 2009, and found there was only one full “BSc (hons)” left and that was at Westminster University.
Today I checked again and NOW THERE ARE NONE.
A phone call to the University of Westminster tonight confirmed that they have suspended entry to their BSc (Hons) homeopathy degree.
Then I revealed another set of slides, showing a misunderstanding (by the teacher) of statistics, but most chillingly,some very dangerous ideas conveyed to students by Westminster’s naturopaths, and in the teaching of Traditional Chinese Medicine, and the great “detox” scam.
“if you get tuberculosis, it isn’t caused by Mycobacterium tuberculosis? And the symptoms are “constructive”? So you don’t need to do anything. It’s all for the best really.
This isn’t just nonsense. It’s dangerous nonsense.”
“Remember when shopping to favour fruits and vegetables which are in season and locally grown (and ideally organic) as they are more vibrationally compatible with the body.”
Locally grown vegetables are “more vibrationally compatible with the body”? Pure mystical gobbledygook. Words fail me.
More make-believe from the University of Westminster. This time it’s Naturopathy
June 25th, 2009
|
Some truly mind-boggling stuff that’s taught to students at Westminster, It includes "Emotrance". A primer on Emotrance says |
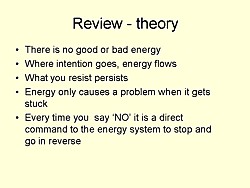 |
"And then I thought of the lady in the supermarket whose husband had died, and I spend the following time sending her my best wishes, and my best space time quantum healing efforts for her void."
Then there are slides on pendulum diagnosis and “kinesiology”, a well-known fraudulent method of diagnosis. It is all perfectly mad.
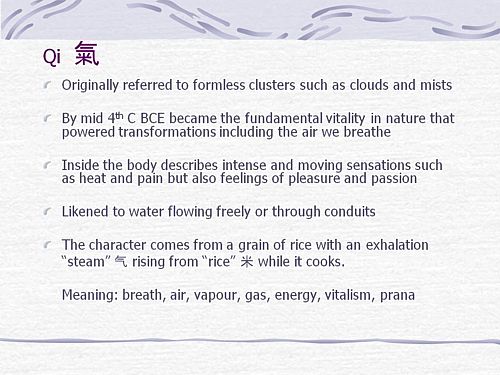
Why degrees in Chinese medicine are a danger to patients
August 10th, 2009
More lunatic fantasies from Westminster, this time about Chinese medicine.
“Teaching students that the brain is made of marrow is not just absurd, but desperately dangerous for anyone unlucky (or stupid) enough to go to such a person when they are ill.”
|
There is a lot of stuff about cancer that is potentially homicidal.
|
 |
This is outrageous and very possibly illegal under the Cancer Act (1939). It certainly poses a huge danger to patients. It is a direct incentive to make illegal, and untrue claims by using weasel words in an attempt to stay just on the right side of the law. But that, of course, is standard practice in alternative medicine,
Emergent Chinese Omics at the University of Westminster/p>
August 27th, 2010
Systems biology is all the rage, No surprise then, to see the University of Westminster advertising a job for a systems biologist in the The Department of Molecular and Applied Biosciences. Well, no surprise there -until you read the small print.
Much has been written here about the University of Westminster, which remains the biggest provider of junk science degrees in the UK, despite having closed two of them.
If there is one thing more offensive than the use of meaningless mystical language, it is the attempt to hijack the vocabulary of real science to promote nonsense. As soon as a quack uses the words "quantum", "energy", "vibration", or now, "systems biology", you can be sure that it’s pretentious nonsense.
Hot of the press. Within a few hours of posting this, I was told that Volker Scheid, the man behind the pretentious Chinese medidine omics nonsense has been promoted to a full chair, And the Dean, Jane Lewis has congratulated him for speaking at a Chines Medicine symposium. Even quite sensible people like Lewis are being corrupted. The buck stops with Petts.
May 3rd, 2011
|
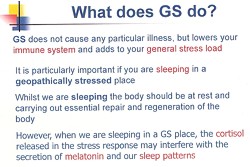
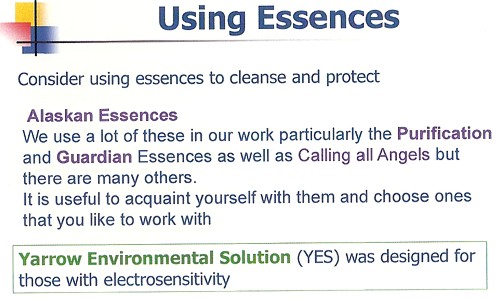
Yet more ghastly slides that are inflicted on Westminster students. How’s this for sheer barminess, taught as part of a Bachelor of Science degree? |
|
And
" Just in case you happen to have run out of Alaskan Calling All Angels Essence, you can buy it from Baldwin’s for £19.95. It’s “designed to invoke the nurturing, uplifting and joyful qualities of the angelic kingdom.”, and what’s more “can also use them any time to cleanse, energize, and protect your auric field.” Well that’s what it says.in the ad.
June 20th, 2011
This post gives details of two complaints, one from a student and one from a lecturer. The vice-chancellor certainly knows about them. So why, I wonder, did he say "“Whilst I understand your concerns, colleagues of the School of Life Sciences where these courses are offered do not share them.". He must know that this simply isn’t true. It is over a year now ( 10 July 2009 ) that a lecturer wrote to the vice-chancellor and Dean
|
“I expect that were the Department of Health to be aware of the unscientific teaching and promotion of practices like dowsing, (and crystals, iridology, astrology, and tasting to determine pharmacological qualities of plant extracts) on the Wmin HM [Westminster Herbal Medicine] Course, progress towards the Statutory Regulation of Herbal Medicine could be threatened.”
|
There’s only one thing wrong with this. The lecturer underestimated the stupidiity of the Department of Health which went ahead with statutory regulation despite being made aware of what was going on.
The latest example to come to light is cited by Andy Lewis on his Quackometer blog
“There are some even odder characters too, such as Roy Riggs B.Sc who describes himself as a “Holistic Geobiologist” and is “an “professional Earth Energy dowser”. He guest lectures at the London Westminster University’s School of Integrative Medicine and The Baltic Dowser’s Association of Lithuania.”
I do wonder who Professor Petts thinks he’s fooling. His denial of the obvious fact that his university is teaching pseudo-science serves only to discredit further the University of Westminster and his own integrity.
Follow-up
13 August 2011 I’m intrigued to notice that two days after posting this summary, googling “Geoffrey Petts” brings up this post as #3 on the first page. Actions have consequences.
Almost all the revelations about what’s taught on university courses in alternative medicine have come from post-1992 universities. (For readers not in the UK, post-1992 universities are the many new univerities created in 1992, from former polytechnics etc, and Russell group universities are the "top 20" research-intensive universities)
It is true that all the undergraduate courses are in post-1992 universities, but the advance of quackademia is by no means limited to them. The teaching at St Bartholomew’s Hospital Medical School, one of the oldest, was pretty disgraceful for example, though after protests from their own students, and from me, it is now better, I believe.

Quackery creeps into all universities to varying extents. The good ones (like Southampton) don’t run "BSc" degrees, but it still infiltrates through two main sources,
The first is via their HR departments, which are run by people who tend to be (I quote) "credulous and moronic" when it comes to science.
The other main source is in teaching to medical students. The General Medical Council says that medical students must know something about alterantive medicine and that’s quite right, A lot of their patients will use it. The problem is that the guidance is shockingly vague .
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
In many medical schools, the information that medical students get is quite accurate. At UCL and at King’s (London) I have done some of the familiarisation myself. In other good medical schools, the students get some shocking stuff. St Bartholomew’s Hospital medical School was one example. Edinburgh University was another.
But there is one Russell group university where alternative myths are propagated more than any other that I know about. That is the University of Southampton.
In general, Southampton is a good place, I worked there for three years myself (1972 – 1975). The very first noise spectra I measured were calculated on a PDP computer in their excellent Institute of Sound and Vibration Research, before I wrote my own programs to do it.
But Southanpton also has a The Complementary and Integrated Medicine Research Unit . Oddly the unit’s web site, http://www.cam-research-group.co.uk, is not a university address, and a search of the university’s web site for “Complementary and Integrated Medicine Research Unit” produces no result. Nevertheless the unit is “within the School of Medicine at the University of Southampton”
Notice the usual euphemisms ‘complementary’ and ‘integrated’ in the title: the word ‘alternative’ is never used. This sort of word play is part of the bait and switch approach of alternative medicine.
The unit is quite big: ten research staff, four PhD students and two support staff It is headed by George Lewith.
Teaching about alternative medicine to Southampton medical students.
The whole medical class seems to get quite a lot compared with other places I know about. That’s 250 students (210 on the 5-year course plus another 40 from the 4-year graduate-entry route).
Year 1: Lecture by David Owen on ‘holism’ within the Foundation Course given to all 210 medical students doing the standard (5-year) course.
Year 2: Lecture by Lewith (on complementary medicine, focusing on acupuncture for pain) given within the nervous systems course to the whole medical student year-group (210 students).
Year 3 SBOM (scientific basis of medicine) symposium: The 3-hour session (“Complementary or Alternative Medicine: You Decide”). I’m told that attendance at this symposium is often pretty low, but many do turn up and all of them are officially ‘expected’ to attend.
There is also an optional CAM special study module chosen by 20 students in year 3, but also a small number of medical students (perhaps 2 – 3 each year?) choose to do a BMedSci research project supervised by the CAM research group and involving 16-18 weeks of study from October to May in Year 4. The CAM research group also supervise postgraduate students doing PhD research.
As always, a list of lectures doesn’t tell you much. What we need to know is what’s taught to the students and something about the people who teach it. The other interesting question is how it comes about that alternative medicine has been allowed to become so prominent in a Russell group university. It must have support from on high. In this case it isn’t hard to find out where it comes from. Here are some details.
Year 1 Dr David Owen
David Owen is not part of Lewith’s group, but a member of the Division of Medical Education headed by Dr Faith Hill (of whom, more below). He’s one of the many part-time academics in this area, being also a founder of The Natural Practice .
Owen is an advocate of homeopathy (a past president of the Faculty of Homeopathy). Homeopathy is, of course, the most barmy and discredited of all the popular sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes it).
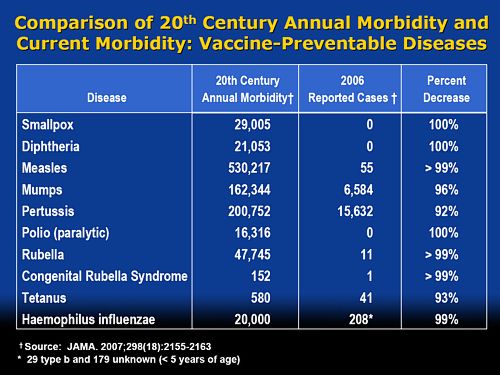
And he’s also a member of the British Society of Environmental Medicine (BSEM). That sounds like a very respectable title, but don’t be deceived. It is an organisation that promotes all sorts of seriously fringe ideas. All you have to do is notice that the star speaker at their 2011 conference was none other than used-to-be a doctor, Andrew Wakefield, a man who has been responsible for the death of children from measles by causing an unfounded scare about vaccination on the basis of data that turned out to have been falsified. There is still a letter of support for Wakefield on the BSEM web site.
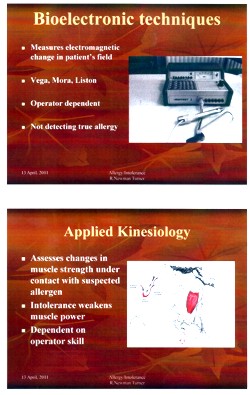
The BSEM specialises in exaggerated claims about ‘environmental toxins’ and uses phony allergy tests like kinesiology and the Vega test that misdiagnose allergies, but provide en excuse to prescribe expensive but unproven nutritional supplements, or expensive psychobabble like "neuro-linguistic programming".
Other registered "ecological physicians" include the infamous Dr Sarah Myhill, who, in 2010, was the subject of a damning verdict by the GMC, and Southampton’s George Lewith.
If it is wrong to expose medical students to someone who believes that dose-response curves have a negative slope (the smaller the dose the bigger the effect -I know, it’s crazy), then it is downright wicked to expose students to a supporter of Andrew Wakefield.
David Owen’s appearance on Radio Oxford, with the indomitable Andy Lewis appears on his Quackometer blog.
Year 2 Dr George Lewith
Lewith is a mystery wrapped in an enigma. He’s participated in some research that is quite good by the (generally pathetic) standards of the world of alternative medicine.
In 2001 he showed that the Vega test did not work as a method of allergy diagnosis. "Conclusion Electrodermal testing cannot be used to diagnose environmental allergies", published in the BMJ .[download reprint].
In 2003 he published "A randomized, double-blind, placebo-controlled proving trial of Belladonna 30C” [download reprint] that showed homeopathic pills with no active ingredients had no effects: The conclusion was "”Ultramolecular homeopathy has no observable clinical effects" (the word ultramolecular, in this context, means that the belladonna pills contained no belladonna).
In 2010 he again concluded that homeopathic pills were no more than placebos, as described in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). [download reprint]
What i cannot understand is that, despite his own findings, his private practice continues to prescribe the Vega machine and continues to prescribe homeopathic pills. And he continues to preach this subject to unfortunate medical students.
Lewith is also one of the practitioners recommended by BSEM. He’s a director of the "College of Medicine". And he’s also an advisor to a charity called Yes To Life. (see A thoroughly dangerous charity: YesToLife promotes nonsense cancer treatments).
3rd year Student Selected Unit
The teaching team includes:
- David Owen – Principal Clinical Teaching Fellow SoM, Holistic Physician
- George Lewith – Professor of Health Research and Consultant Physician
- Caroline Eyles – Homeopathic Physician
- Susan Woodhead – Acupuncturist
- Elaine Cooke – Chiropractic Practitioner
- Phine Dahle – Psychotherapist
- Keith Carr – Reiki Master
- Christine Rose – Homeopath and GP
- David Nicolson – Nutritionalist
- Shelley Baker – Aromatherapist
- Cheryl Dunford – Hypnotherapist
- Dedj Leibbrandt – Herbalist
More details of the teaching team here. There is not a single sceptic among them, so the students don’t get a debate, just propaganda.
In this case. there’s no need for the Freedom of Information Act. The handouts. and the powerpoints are on their web site. They seem to be proud of them
Let’s look at some examples
Chiropractic makes an interesting case, because, in the wake of the Singh-BCA libel case, the claims of chiropractors have been scrutinised as never before and most of their claims have turned out to be bogus. There is a close relationship between Lewith’s unit and the Anglo-European Chiropractic College (the 3rd year module includes a visit there). In fact the handout provided for students, Evidence for Chiropractic Care , was written by the College. It’s interesting because it provides no real evidence whatsoever for the effectiveness of chiropractic care. It’s fairly honest in stating that the view at present is that, for low back pain, it isn’t possible to detect any difference between the usefulness of manipulation by a physiotherapist, by an osteopath or by a chiropractor. Of course it does not draw the obvious conclusion that this makes chiropractic and osteopathy entirely redundant -you can get the same result without all the absurd mumbo jumbo that chiropractors and osteopaths love, or their high-pressure salesmanship and superfluous X-rays. Neither does it mention the sad, but entirely possible, outcome that none of the manipulations are effective for low back pain. There is, for example, no mention of the fascinating paper by Artus et al [download reprint]. This paper concludes
"symptoms seem to improve in a similar pattern in clinical trials following a wide
variety of active as well as inactive treatments."
This paper was brought to my attention through the blog run by the exellent physiotherapist, Neil O’Connell. He comments
“If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery.”
This sort of critical thinking is conspicuously absent from this (and all the other) Southampton handouts. The handout is a superb example of bait and switch: No nonsense about infant colic, innate energy or imaginary subluxations appears in it.
Acupuncture is another interesting case because there is quite a lot of research evidence, in stark contrast to the rest of traditional Chinese medicine, for which there is very little research.
|
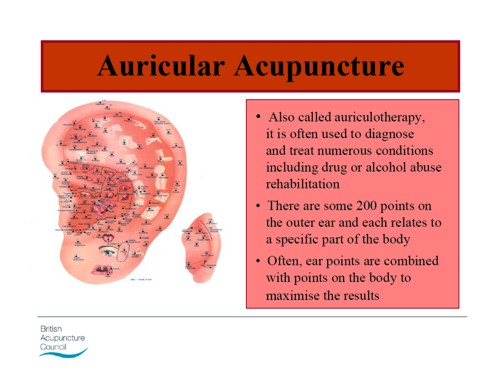
There is a powerpoint show by Susan Woodhead (though it is labelled British Acupuncture Council). The message is simple and totally uncritical. It works. |

|
In fact there is now a broad consensus about acupuncture.
(1) Real acupuncture and sham acupuncture have been found to be indistinguishable in many trials. This is the case regardless of whether the sham is a retractable needle (or even a toothpick) in the "right" places, or whether it is real needles inserted in the "wrong" places. The latter finding shows clearly that all that stuff about meridians and flow of Qi is sheer hocus pocus. It dates from a pre-scientific age and it was wrong.
(2) A non-blind comparison of acupuncture versus no acupuncture shows an advantage for acupuncture. But the advantage is usually too small to be of any clinical significance. In all probability it is a placebo effect -it’s hard to imagine a more theatrical event than having someone in a white coat stick long needles into you, like a voodoo doll. Sadly, the placebo effect isn’t big enough to be of much use.
Needless to say, none of this is conveyed to the medical students of Southampton. Instead they are shown crude ancient ideas that date from long before anything was known about physiology as though they were actually true. These folks truly live in some alternative universe. Here are some samples from the acupuncture powerpoint show by Susan Woodhead.
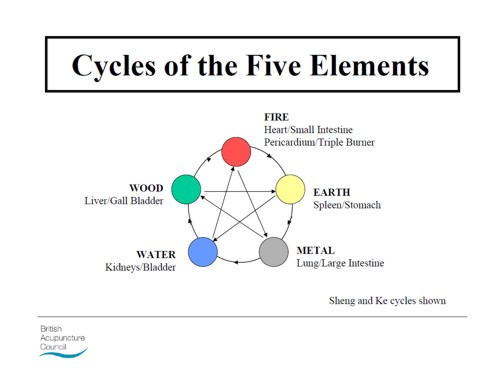
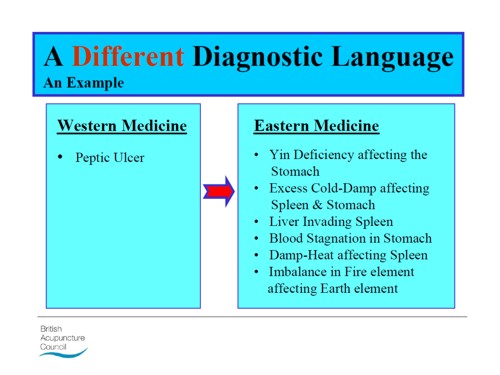
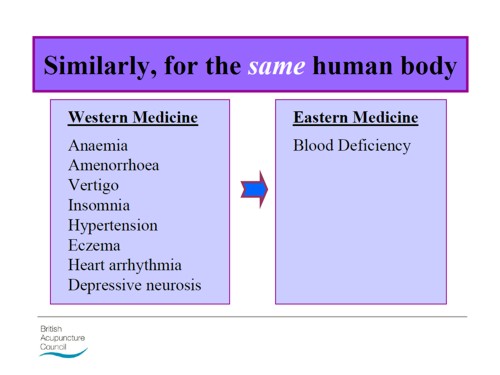
Well this is certainly a "different diagnostic language", but no attempt is made to say which one is right. In the mind of the acupuncurist it seems both are true. It is a characteristic of alternative medicine advocates that they have no difficulty in believing simultaneously several mutually contradictory propositions.
As a final exmple of barminess, just look at the acupuncture points (allegedly) on the ear The fact that it is a favoured by some people in the Pentagon as battlefield acupuncture, is more reminiscent of the mad general, Jack D. Ripper, in Dr Strangelove than it is of science.
There is an equally uncritical handout on acupuncture by Val Hopwood. It’s dated March 2003, a time before some of the most valuable experiments were done.
The handout says "sham acupuncture
is generally less effective than true acupuncture", precisely the opposite of what’s known now. And there are some bits that give you a good laugh, always helpful in teaching. I like
“There is little doubt that an intact functioning nervous system is required for acupuncture to produce
analgesia or, for that matter, any physiological changes”
and
Modern techniques: These include hybrid techniques such as electro-acupuncture . . . and Ryadoraku [sic] therapy and Vega testing.
Vega testing!! That’s been disproved dozens of times (not least by George Lewith). And actually the other made-up nonsense is spelled Ryodoraku.
It’s true that there is a short paragraph at the end of the handout headed "Scientific evaluation of acupuncture" but it doesn’t cite a single reference and reads more like excuses for why acupuncture so often fails when it’s tested properly.
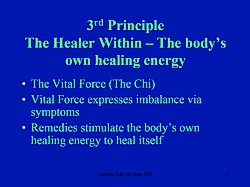
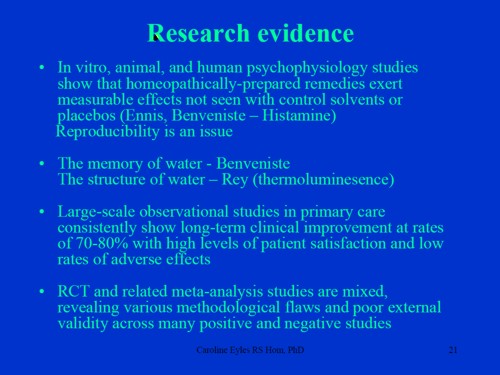
Homeopathy. Finally a bit about that most boring of topics, the laughable medicine that contains no medicine, homeopathy. Caroline Eyles is a member for the Society of Homeopaths, the organisation that did nothing when its members were caught out in the murderous practice of recommending homeopathy for prevention of malaria. The Society of Homeopaths also endorses Jeremy Sherr, a man so crazy that he believes he can cure AIDS and malaria with sugar pills.
The homeopathy handout given to the students has 367 references, but somehow manages to omit the references to their own boss’s work showing that the pills are placebos. The handout has all the sciencey-sounding words, abused by people who don’t understand them.
"The remedy will be particularly effective if matched to the specific/particular characteristics of the individual (the ‘totality’ of the patient) on all levels, including the emotional and mental levels, as well as just the physical symptoms. ‘Resonance’ with the remedy’s curative power will then be at it’s [sic] best."
The handout is totally misleading about the current state of research. It says
"increasing clinical research confirms it’s [sic] clinical effectiveness in treating patients, including babies and animals (where a placebo effect would be hard to justify)."
|
The powerpont show by Caroline Eyles shows all the insight of a mediaeval vitalist |
|
Anyone who has to rely on the utterly discredited Jacques Benveniste as evidence is clearly clutching at straws. What’s more interesting about this slide the admission that "reproducibility is a problem -oops, an issue" and that RCTs (done largely by homeopaths of course) have "various methodological flaws and poor external validity". You’d think that if that was the best that could be produced after 200 yours, they’d shut up shop and get another job. But, like aging vicars who long since stopped believing in god, but are damned if they’ll give up the nice country rectory, they struggle on, sounding increasingly desperate.
How have topics like this become so embedded in a medical course at a Russell group university?
The details above are a bit tedious and repetitive. It’s already established that hardly any alternative medicine works. Don’t take my word for it. Check the web site of the US National Center for Complementary and Alternative Medicine (NCCAM) who, at a cost of over $2 billion have produced nothing useful.
A rather more interesting question is how a good university like Southampton comes to be exposing its medical students to teaching like this. There must be some powerful allies higher up in the university. In this case it’s pretty obvious who thay are.
Professor Stephen Holgate MD DSc CSc FRCP FRCPath FIBiol FBMS FMed Sci CBE has to be the primary suspect, He’s listed as one of Southampton’s Outstanding Academics. His work is nothing to do with alternative medicine but he’s been a long term supporter of the late unlamented Prince of Wales’ Foundation, and he’s now on the advisory board of it’s successor, the so called "College of Medicine" (for more information about that place see the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health, and also Don’t be deceived. The new “College of Medicine” is a fraud and delusion ). His description on that site reads thus.
"Stephen Holgate is MRC Clinical Professor of Immunopharmacology at the University of Southampton School of Medicine and Honorary Consultant Physician at Southampton University Hospital Trust. He is also chair of the MRC’s Populations and Systems Medicine Board. Specialising in respiratory medicine, he is the author of over 800 peer-reviewed papers and contributions to scientific journals and editor of major textbooks on asthma and rhinitis. He is Co-Editor of Clinical and Experimental Allergy, Associate Editor of Clinical Science and on the editorial board of 25 other scientific journals."
Clearly a busy man. Personally I’m deeply suspicious of anyone who claims to be the author of over 800 papers. He graduated in medicine in 1971, so that is an average of over 20 papers a year since then, one every two or three weeks. I’d have trouble reading that many, never mind writing them.
Holgate’s long-standing interest in alternative medicine is baffling. He’s published on the topic with George Lewith, who, incidentally, is one of the directors of the "College of Medicine"..
It may be unkind to mention that, for many years now, I’ve been hearing rumours that Holgate is suffering from an unusually bad case of Knight starvation.
The Division of Medical Education appears to be the other big source of support for. anti-scientific medicine. That is very odd, I know, but it was also the medical education people who were responsible for mis-educating medical students at. St. Bartholomew’s and at Edinburgh university. Southampton’s Division of Medical Education has a mind-boggling 60 academic and support staff. Two of them are of particular interest here.
Faith Hill is director of the division. Her profile doesn’t say anything about alternative medicine, but her interest is clear from a 2003 paper, Complementary and alternative medicine: the next generation of health promotion?. The research consisted of reporting anecdotes from interviews of 52 unnamed people (this sort of thing seems to pass for research in the social sciences). It starts badly by misrepresenting the conclusions of the House of Lords report (2000) on CAM. Although it comes to no useful conclusions, it certainly shows a high tolerance of nonsensical treatments.
Chris Stephens is Associate Dean of Medical Education & Student Experience. His sympathy is shown by a paper he wrote In 2001, with David Owen (the homeopath, above) and George Lewith: Can doctors respond to patients’ increasing interest in complementary and alternative medicine?. Two of the conclusions of this paper were as follows.
"Doctors are training in complementary and alternative medicine and report benefits both for their patients and themselves"
Well, no actually. It wasn’t true then, and it’s probably even less true now. There’s now a lot more evidence and most of it shows alternative medicine doesn’t work.
"Doctors need to address training in and practice of complementary and alternative medicine within their own organisations"
Yes they certainly need to do that.
And the first thing that Drs Hill and Stephens should do is look a bit more closely about what’s taught in their own university, I hope that this post helps them,
Follow-up
4 July 2011. A correspondent has just pointed out that Chris Stephens is a member of the General Chiropractic Council. The GCC is a truly pathetic pseudo-regulator. In the wake of the Simon Singh affair it has been kept busy fending off well-justified complaints against untrue claims made by chiropractors. The GCC is a sad joke, but it’s even sadder to see a Dean of Medical Education at the University of Southampton being involved with an organisation that has treated little matters of truth with such disdain.
A rather unkind tweet from (ex)-chiropractor @RichardLanigan.
“Chris is just another light weight academic who likes being on committees. Regulatory bodies are full of them”
One of my first posts about nonsense taught in universities was about the University of Westminster (April 2008): Westminster University BSc: “amethysts emit high yin energy”. since then, there have been several more revelations.
 Professor Petts |
The vice-cnancellor of Westminster, Professor Geoffrey Petts, with whom the buck stops, did have an internal review but its report was all hot air and no action resulted (see A letter to the Times, and Progress at Westminster). That earned Professor Petts an appearence in Private Eye Crystal balls. Professor Petts in Private Eye (and it earned me an invitation to a Private Eye lunch, along with Francis Wheen, Charlie Booker, Ken Livingstone . . ). It also earned Petts an appearence in the Guardian (The opposite of science). |
By that time Salford University had closed down all its CAM, and the University of Central Lancashire was running an honest internal review which resulted in closure of (almost) all of their nonsense degrees. But Westminster proved more resistant to sense and, although they closed down homeopathy, they still remain the largest single provider of degrees in junk medicine. See, for example More make-believe from the University of Westminster. This time it’s Naturopathy, and
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
It’s interesting that Westminster always declined to comply with Freedom of Information requests, yet I had more from them than from most places. All the information about what’s taught at Westminster came from leaks from within the university. Westminster has more moles than a suburban garden. They were people with conscience who realised that the university was harming itself. They would claim that they were trying to save the university from some remarkably bad management. I claim also that I’m working in the interests of the university.
In the wake of the victory at the Information Tribunal, I sent a Freedom of Information Act (FOIA) request for for samples of teaching materials from all of their courses. This time they couldn’t legally refuse. The first batch has just arrived, so here are a few selected gems of utter nonsense. Well, it is worse than nonsense because it endangers the health of sick people.
A letter to the university from a student
Before getting on to the slides, here’s a letter that was supplied under FOIA. It was sent anonymously to the university. I was told that this was the only letter of complaint but I happen to know that’s not true so I’ve asked again. This one was forwarded to the vice-chancellor in 2008, and to the review committee. Both seem to have ignored it. Judging from the wording, one would guess that it came from one of their own undergraduates. :Here are some extracts.[download whole letter]
|
It is a flagrant contradiction of a ‘science’ in the BSc to have these practices, but it also jeopardises our profession, which is under DoH review and being constantly attacked in the media Gustifiable I suggest). We are taught that simply tasting plant tinctures can tell us which part of the body they work. on and what they do in the body. We are given printed charts with an outline of the body on to record our findings on. This is both nonsense, but is dangerous as it implies that the pharmacology of plant tinctures can be divined by taste alone. In class we are taught that we can divine the drug actions or use of an unknown plant simply by tasting an alcohol extract. Science? or dangerous fantasy. There are lecturers taking clinics who allow students to dowse and partake themselves in dowsing or pendulums to diagnose and even to test suitability of plant drugs. Dowsing is taught to us by some lecturers and frowned upon by others but we feel it brings the herbal medicine into a poor light as it is unscientific and bogus nonsense. We are concerned that we have seen the course leader brush over this practice as though she is frightened to make a stand. |
The letter seems to refer to a course in herbal medicine. That is a subject that could be studied scientifically, though to do so would leave students unemployed because so few herbal treatments have been shown to work. It obviously is not being studied scientifically: but even teaching students about dowsing and pendulums does not seem to have stirred the vice-chancellor into action.
David Peters: wishful thinking?
David Peters is a nice man. He’s the Clinical Director of Westminster’s School of Integrated Health. I debated with him on the excellent Radio 4 Programme, Material World.
His lecture on "Complementary Healthcare in the NHS" showed some fine wishful thinking.
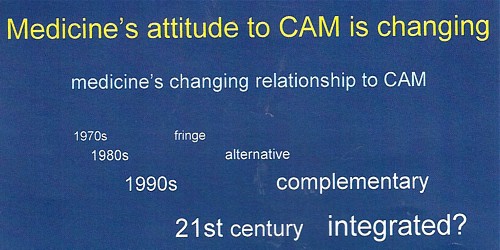
It shows the progress of the euphemisms that quacks use to try to gain respectability, but little else. Interestingly, later slides show a bit more realism.
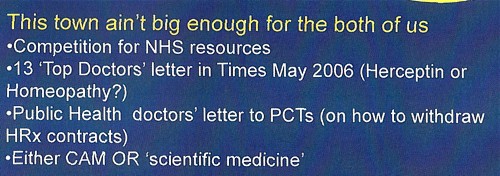
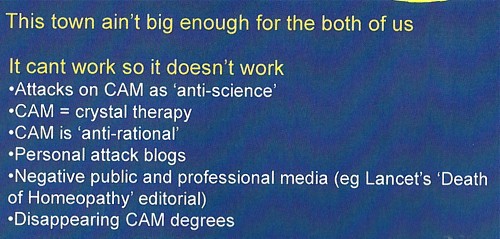
So he has noticed that the tide has turned and that a lot of people are no longer willing to be palmed off with new age gobbledygook. And yes, courses are shutting. Perhaps his course will be the next to shut?
According to an internal Westminster email that found its way to me,
The following courses have been closed/identified for closure due to poor recruitment :
- BSc degrees in Homeopathy and Remedial Massage & Neuromuscular Therapy, students completing by September 2011
- MA degrees in International Community development, Community development and Faith-based Community development, students completing by September 2011
- BSc degree Complementary Medicine
- Graduate diploma BMS
The following courses have been identified as ‘at risk’ (School definition) and will be discussed at the APRG and University Review Group2, due to poor recruitment and high cost of delivery:
- Integrated Health Scheme: BSc Complementary Medicine, Naturopathy; BSc Chinese Medicine; BSc Nutritional Therapy; BSc Herbal Medicine
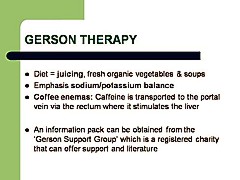
The BSc (Hons) degree in naturopathy
Naturopathy us pretty bizarre, because it consists largely of doing nothing at all, beyond eating vegetables . Being ill is good for you.
Perhaps the best source to judge claims is the US National Center for Complementary and Alternive Medicine (NCCAM), a branch of the National Institutes of Health. This is the outfit that has spent over a billion dollars of US taxpayers’ money testing alternative medicines and for all that money has not come up with a single useful treatment. They never link to any sort of critical comment, and are nothing if not biassed towards all things alternative. If they can’t come up with evidence. nobody can. Two useful links to NCCAM are Herbs at a glance, and Health Topics A – Z.
Uses of herbal teas in naturopathic dietary care
I was sent a set of over 50 slides on "Herbal Teas/Decoctions (3CMWS03, 1/02, Uses of herbal teas in naturopathic dietary care). About half of them amount to little more than ‘how to make a cup of tea’. but then we get onto uses, but then a lot of fantasy ensues.
What NNCAM says about dandelion. There is no compelling scientific evidence for using dandelion as a treatment for any medical condition.
What Westminster says
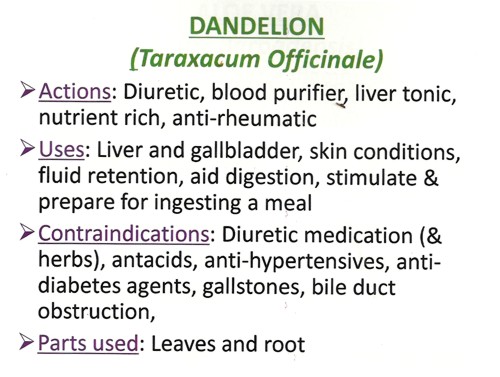
Well I know what a diuretic is, but "blood purifier" and "liver tonic" are meaningless gobbledygook. We’ve been through this before with Red Clover (see Michael Quinion’s .look at the term "blood cleanser"). Using words like them is the very opposite of education.
What NCCAM says.about chamomile: Chamomile has not been well studied in people so there is little evidence to support its use for any condition.
What Westminster says
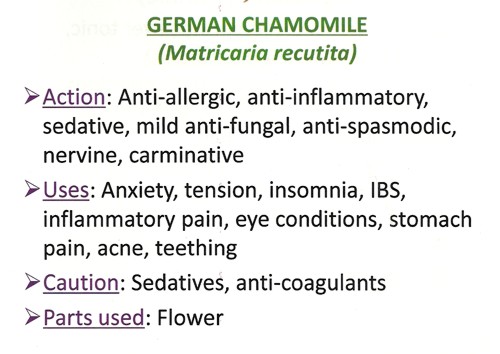
So, judging by NCCAM, these claims are unjustified. It’s teaching folk-lore as though it meant something.
More dangerous advice comes when we get to the ‘repertories’.
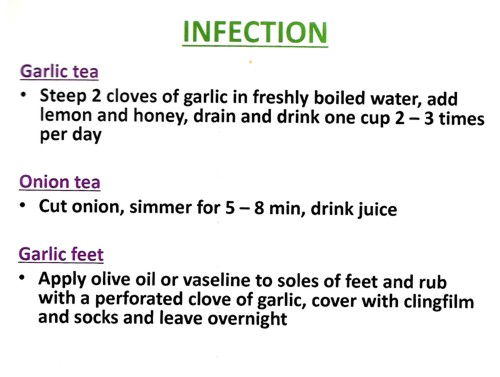
Infections can kill you, They are one of the modest number of things that pharmacology can usually cure, rather than treat symptomatically. If you go to a Westminster-trained naturopath with a serious infection and follow their advice to put garlic in your socks, you will not just be smelly, You could die.
Allergy and Intolerance 3CMwS03 18/02
|
Treating allergies, misdiagnosed by fraudulent tests, is very big business for the ‘health food industry’, This lecture, by R. Newman Turner ND, DO, BAc, started tolerably but descended to a nadir when it mentions, apparently seriously, two of the best known fraudulent methods of allergy diagnosis, the Vega test and "Applied Kinesiology". Kinesiology Sounds sort of sciencey, but Applied Kinesiology is actually a fraudulent and totally ineffective diagnostic method invented by (you guessed) a chiropractor. It has been widely used by alternative medicine to misdiagnose food allergies. It does not work (Garrow, 1988: download reprint). |
|
Could this be the same R Newman Turner who wrote a book on Naturopathic First Aid? The mind boggles.
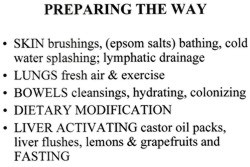
Naturopathic Detoxification 23 CMES03 25/02 Detox Myth of Fact
|
This lecture was the responsibility of Irving S Boxer ND DO MRN LCH, a naturopath, homeopath and osteopath in private practice. Don’t be fooled by the implied question in the title. It might have been taken to suggest a critical approach. Think again. There is all the usual make-believe about unspecified and imaginary toxins that you must get rid of with enemas and vegetables. |
|
|
The skin brushing does not quite plumb the depths of Jacqueline Young’s Taking an air bath , but presumably it is something similar. "Liver activation" by castor oil packs is pure unadulterated gobblydygook. The words mean nothing. Their attempt to divide all foods into those that cleanse and those that clog sounds reminiscent of the Daily Mail’s ontological oncology project. |
|
The practice of healing (3CMSS01 2/12)
Next we retreat still further into fantasy land
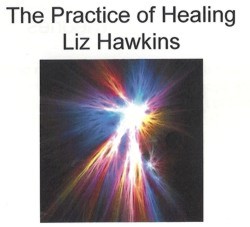
|
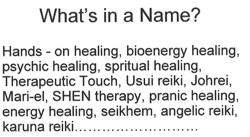
|
All pure hokum, of course’ She could have added "craniosacral therapy" (at present the subject of a complaint against the UCL Hospitals Trust (that’s the NHS, not UCL) to the Advertising Standards Authority,
 |
 |
Is that definition quite clear?
In fact this sort of nonsense about rays coming from your hands was disproved experimentally, in a rather famous paper, the only paper in the Journal of the American Medical Association to have been written by a 9-year old. Emily Rosa. She (with some help from her parents) devised a simple test for her 4th (US) grade science fair project. It was later repeated under more controlled conditions and written up for JAMA [download reprint] . It showed that the claims of ‘therapeutic touch" practitioners to be able to detect "auras" were totally false. No subsequent work has shown otherwise. Why, then, does the University of Westminster teach it as part of a Bachelor of Science degree?
You can see Emily Rosa herself explain why “therapeutic touch is bullshit” with Penn and Teller, in Penn and Teller Expose Therapeutic Touch.
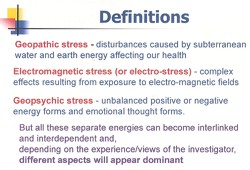
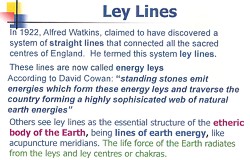
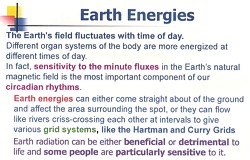
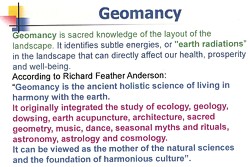
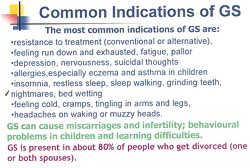
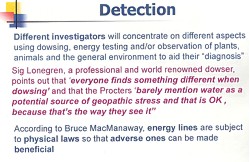
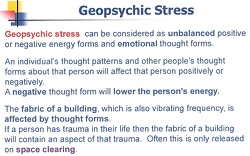
Environmental stress
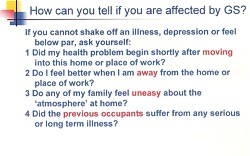
The last bit of hokum (for the moment) is one of the best. This one has every myth under the sun (including some I hadn’t heard of).
|
The lecturer, Val Bullen, was also responsible for the infamous "Amethysts emit high Yin energy" slide. One of her own students desribes her as "sweet but deluded". I have nothing against Ms Bullen, She can believe whatever she wants. My problem is with the vice-chancellor, Prof Geoffrey Petts, who seems to think that this sort of stuff is appropriate for a BSc. |
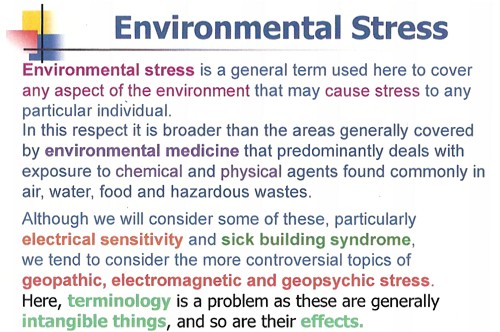
|
Everything barmy is here. Mobile phones, power lines, underwater streams, ley lines, sick building syndrome, are all reasons why you don’t feel 100 percent, Actually my reason is having to read this junk. The "definitions" are, as always, just meaningless words.
|
But don’t despair. Help is at hand.
Just in case you happen to have run out of Alaskan Calling All Angels Essence, you can buy it from Baldwin’s for £19.95. It’s "designed to invoke the nurturing, uplifting and joyful qualities of the angelic kingdom.", and what’s more "can also use them any time to cleanse, energize, and protect your auric field." Well that’s what it says.in the ad.
Yarrow Environmental Solution looks like good stuff too. Only £7.95 for 7.5 ml. For that you get a lot. It will
" . . strengthen and protect against toxic environmental influences, geopathic stress, and other hazards of technology-dominated modern life. This includes the disruptive effects of radiation on human energy fields from X-rays, televisions, computer monitors, electromagnetic fields, airplane flights or nuclear fall-out."
OK stop giggling. This is serious stuff, taught in a UK university as part of a BSc degree, and awarded a high score by the Quality Assurance Agency (QAA).
Professor Petts, are you listening? I believe it is you, not I, who is bringing your university into disrepute.
The slides shown here are copyright of the University of Westminster or of the author of the lecture. They are small sample of what I was sent and are reproduced under the “fair quotation” provision, in the public interest.
Follow-up
5 May 2011. By sheer coincidence, Emily and Linda Rosa were passing through London. They called for lunch and here’s a picture (with Ben Goldacre) in UCL’s (endangered) Housman room. Linda kindly gave me a copy of her book Attachment Therapy on Trial: The Torture and Death of Candace Newmaker. [Download reprint of Rosa’s paper..]

.
6 May 2011. Talking of the “vibrational medicine” fantasy, I had an email that pointed out a site that plumbs new depths in fantasy physics. It’s on the PositiveHealthOnline website: A post there, Spirals and Energy in Nature, was written by Robert McCoy. He claims to have worked on microprocessor layout design, but anyone with school physics could tell that the article is sheer nonsense. In a way it is much more objectionable that the silly slides with coloured rays used in the Westminster course. McCoy’s post seeks to blind with sciencey-sounding language, that in fact makea no sense at all. Luckily my retweet of the site attracted the attention of a real physicist, A.P. Gaylard, who made a very welcome return to blogging with Fantasy physics and energy medicine. He dismantles the physics, line-by-line, in a devastating critique. This sort of junk physics is far more dangerous than the perpetual motion pundits and the cold-fusion fantasists. At PositiveHealthOnline it is being used to push pills that do you no good and may harm you. It is a danger to public health.
This is a slightly-modified version of the article that appeared in BMJ blogs yesterday, but with more links to original sources, and a picture. There are already some comments in the BMJ.
The original article, diplomatically, did not link directly to UCL’s Grand Challenge of Human Wellbeing, a well-meaning initiative which, I suspect, will not prove to be value for money when it comes to practical action.
Neither, when referring to the bad effects of disempowerment on human wellbeing (as elucidated by, among others, UCL’s Michael Marmot), did I mention the several ways in which staff have been disempowered and rendered voiceless at UCL during the last five years. Although these actions have undoubtedly had a bad effect on the wellbeing of UCL’s staff, it seemed a litlle unfair to single out UCL since similar things are happening in most universities. Indeed the fact that it has been far worse at Imperial College (at least in medicine) has probably saved UCL from being denuded. One must be thankful for small mercies.
There is, i think, a lesson to be learned from the fact that formal initiatives in wellbeing are springing up at a time when university managers are set on taking actions that have exactly the opposite effect. A ‘change manager’ is not an adequate substitute for a vote. Who do they imagine is being fooled?
The A to Z of the wellbeing industry
From angelic reiki to patient-centred care
Nobody could possibly be against wellbeing. It would be like opposing motherhood and apple pie. There is a whole spectrum of activities under the wellbeing banner, from the undoubtedly well-meaning patient-centred care at one end, to downright barmy new-age claptrap at the other end. The only question that really matters is, how much of it works?
Let’s start at the fruitcake end of the spectrum.
One thing is obvious. Wellbeing is big business. And if it is no more than a branch of the multi-billion-dollar positive-thinking industry, save your money and get on with your life.
In June 2010, Northamptonshire NHS Foundation Trust sponsored a “Festival of Wellbeing” that included a complementary therapy taster day. In a BBC interview one practitioner used the advertising opportunity, paid for by the NHS, to say “I’m an angelic reiki master teacher and also an angel therapist.” “Angels are just flying spirits, 100 percent just pure light from heaven. They are all around us. Everybody has a guardian angel.” Another said “I am a member of the British Society of Dowsers and use a crystal pendulum to dowse in treatment sessions. Sessions may include a combination of meditation, colour breathing, crystals, colour scarves, and use of a light box.” You couldn’t make it up.
The enormous positive-thinking industry is no better. Barbara Ehrenreich’s book, Smile Or Die: How Positive Thinking Fooled America and the World, explains how dangerous the industry is, because, as much as guardian angels, it is based on myth and delusion. It simply doesn’t work (except for those who make fortunes by promoting it). She argues that it fosters the sort of delusion that gave us the financial crisis (and pessimistic bankers were fired for being right). Her interest in the industry started when she was diagnosed with cancer. She says
”When I was diagnosed, what I found was constant exhortations to be positive, to be cheerful, to even embrace the disease as if it were a gift. If that’s a gift, take me off your Christmas list,”
It is quite clear that positive thinking does nothing whatsoever to prolong your life (Schofield et al 2004; Coyne et al 2007; 2,3), any more than it will cure tuberculosis or cholera. “Encouraging patients to “be positive” only may add to the burden of having cancer while providing little benefit” (Schofield et al 2004). Far from being helpful, it can be rather cruel.
Just about every government department, the NHS, BIS, HEFCE, and NICE, has produced long reports on wellbeing and stress at work. It’s well known that income is correlated strongly with health (Marmot, M., 2004). For every tube stop you go east of Westminster you lose a year of life expectancy (London Health Observatory). It’s been proposed that what matters is inequality of income (Wilkinson & Pickett, 2009). The nature of the evidence doesn’t allow such a firm conclusion (Lynch et al. 2004), but that isn’t really the point. The real problem is that nobody has come up with good solutions. Sadly the recommendations at the ends of all these reports don’t amount to a hill of beans. Nobody knows what to do, partly because pilot studies are rarely randomised so causality is always dubious, and partly because the obvious steps are either managerially inconvenient, ideologically unacceptable, or too expensive.
Take two examples:
Sir Michael Marmot’s famous Whitehall study (Marmot, M., 2004) has shown that a major correlate of illness is lack of control over one’s own fate: disempowerment. What has been done about it?
In universities it has proved useful to managers to increase centralisation and to disempower academics, precisely the opposite of what Marmot recommends.
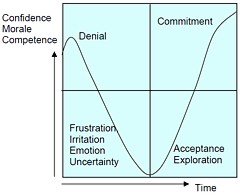
|
As long as it’s convenient to managers they are not going to change policy. Rather, they hand the job to the HR department which appoints highly paid “change managers,” who add to the stress by sending you stupid graphs that show you emerging from the slough of despond into eternal light once you realise that you really wanted to be disempowered after all. Or they send you on some silly “resilience” course. |
|
A second example comes from debt. According to a BIS report (Mental Capital and Wellbeing), debt is an even stronger risk factor for mental disorder than low income. So what is the government’s response to that? To treble tuition fees to ensure that almost all graduates will stay in debt for most of their lifetime. And this was done despite the fact that the £9k fees will save nothing for the taxpayer: in fact they’ll cost more than the £3k fees. The rise has happened, presumably, because the ideological reasons overrode the government’s own ideas on how to make people happy.
Nothing illustrates better the futility of the wellbeing industry than the response that is reported to have been given to a reporter who posed as an applicant for a “health, safety, and wellbeing adviser” with a local council. When he asked what “wellbeing” advice would involve, a member of the council’s human resources team said: “We are not really sure yet as we have only just added that to the role. We’ll want someone to make sure that staff take breaks, go for walks — that kind of stuff.”
The latest wellbeing notion to re-emerge is the happiness survey. Jeremy Bentham advocated “the greatest happiness for the greatest number,” but neglected to say how you measure it. A YouGov poll asks, “what about your general well-being right now, on a scale from 1 to 10.” I have not the slightest idea about how to answer such a question. As always some things are good, some are bad, and anyway wellbeing relative to whom? Writing this is fun. Trying to solve an algebraic problem is fun. Constant battling with university management in order to be able to do these things is not fun. The whole exercise smacks of the sort of intellectual arrogance that led psychologists in the 1930s to claim that they could sum up a person’s intelligence in a single number. That claim was wrong and it did great social harm.
HEFCE has spent a large amount of money setting up “pilot studies” of wellbeing in nine universities. Only one is randomised, so there will be no evidence for causality. The design of the pilots is contracted to a private company, Robertson Cooper, which declines to give full details but it seems likely that the results will be about as useless as the notorious Durham fish oil “trials”(Goldacre, 2008).
Lastly we get to the sensible end of the spectrum: patient-centred care. Again this has turned into an industry with endless meetings and reports and very few conclusions. Epstein & Street (2011) say
“Helping patients to be more active in consultations changes centuries of physician-dominated dialogues to those that engage patients as active participants. Training physicians to be more mindful, informative, and empathic transforms their role from one characterized by authority to one that has the goals of partnership, solidarity, empathy, and collaboration.”
That’s fine, but the question that is constantly avoided is what happens when a patient with metastatic breast cancer expresses a strong preference for Vitamin C or Gerson therapy, as advocated by the YesToLife charity. The fact of the matter is that the relationship can’t be equal when one party, usually (but not invariably) the doctor, knows a lot more about the problem than the other.
What really matters above all to patients is getting better. Anyone in their right mind would prefer a grumpy condescending doctor who correctly diagnoses their tumour, to an empathetic doctor who misses it. It’s fine for medical students to learn social skills but there is a real danger of so much time being spent on it that they can no longer make a correct diagnosis. Put another way, there is confusion between caring and curing. It is curing that matters most to patients. It is this confusion that forms the basis of the bait and switch tactics (see also here) used by magic medicine advocates to gain the respectability that they crave but rarely deserve.
If, as is only too often the case, the patient can’t be cured, then certainly they should be cared for. That’s a moral obligation when medicine fails in its primary aim. There is a lot of talk about individualised care. It is a buzzword of quacks and also of the libertarian wing which says NICE is too prescriptive. It sounds great, but it helps only if the individualised treatment actually works.
Nobody knows how often medicine fails to be “patient-centred.”. Even less does anyone know whether patient-centred care can improve the actual health of patients. There is a strong tendency to do small pilot trials that are as likely to mislead as inform. One properly randomised trial (Kinmonth et al., 1998) concluded
“those committed to achieving the benefits of patient centred consulting should not lose the focus on disease management.”
Non-randomised studies may produce more optimistic conclusions (e.g. Hojat et al, 2011), but there is no way to tell if this is simply because doctors find it easy to be empathetic with patients who have better outcomes.
Obviously I’m in favour of doctors being nice to patients and to listening to their wishes. But there is a real danger that it will be seen as more important than curing. There is also a real danger that it will open the doors to all sorts of quacks who claim to provide individualised empathic treatment, but end up recommending Gerson therapy for metastatic breast cancer. The new College of Medicine, which in reality is simply a reincarnation of the late unlamented Prince’s Foundation for Integrated Health, lists as its founder Capita, the private healthcare provider that will, no doubt, be happy to back the herbalists and homeopaths in the College of Medicine, and, no doubt, to make a profit from selling their wares to the NHS.
In my own experience as a patient, there is not nearly as much of a problem with patient centred care as the industry makes out. Others have been less lucky, as shown by the mid-Staffordshire disaster (Delamothe, 2010), That seems to have resulted from PR being given priority over patients. Perhaps all that’s needed is to save money on all the endless reports and meetings (“the best substitute for work”), ban use of PR agencies (paid lying) and to spend the money on more doctors and nurses so they can give time to people who need it. This is a job that will be hindered considerably by the government’s proposals to sell off NHS work to private providers who will be happy to make money from junk medicine.
Reference
Wilkinson. R & Pickett, K. 2009 , The Spirit Level, ISBN 978 1 84614 039 6
A footnote on Robertson Cooper and "resilience"
I took up the offer of Robertson Cooper to do their free "resilience" assessment, the company to which HEFCE has paid an undisclosed amount of money.
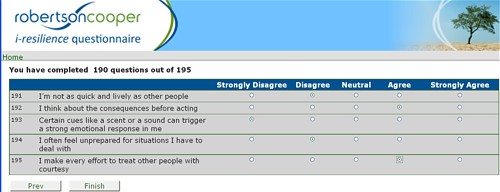
The first problem arose when it asked about your job. There was no option for scientist, mathematician, university or research, so I was forced to choose "education and training". (a funny juxtaposition since training is arguably the antithesis of education). It had 195 questions. mostly as unanswerable as in the YouGov happiness survey. I particularly liked question 124 "I see little point in many of the theoretical models I come across". The theoretical models that I come across most are Markov models for the intramolecular changes in a receptor molecule when it binds a ligand (try, for example, Joint distributions of apparent open and shut times of single-ion channels and maximum likelihood fitting of mechanisms). I doubt the person who wrote the question has ever heard of a model of that sort. The answer to that question (and most of the others) would not be worth the paper they are written on.
The whole exercise struck me as the worst sort of vacuous HR psychobabble. It is worrying that HEFCE thinks it is worth spending money on it.
Follow-up
Systems biology is all the rage, No surprise then, to see the University of Westminster advertising a job for a systems biologist in the The Department of Molecular and Applied Biosciences. Well, no surprise there -until you read the small print.
Much has been wriiten here about the University of Westminster, which remains the biggest provider of junk sciencne degrees in the UK, despite having closed two of them.
Senior Lecturer in Systems BiologyUniversity of Westminster – Department of Molecular and Applied Biosciences, School of Life SciencesCavendish Site Salary £37,886 – £50,751 (Inc. LWA) The Department of Molecular and Applied Biosciences wishes to appoint a Senior Lecturer in Systems Biology. The post-holder will teach on the undergraduate and postgraduate degree programmes within the School of Life Sciences, particularly in the areas of Molecular Biology, Bioinformatics and/or statistics, establish their own and participate in ongoing research programmes and undertake external income generation activities. The candidate should have an active interest in bridging the gap between western life sciences and Chinese medicine using emerging systems biology approaches, specifically in metabolomics and proteomics with a goal of developing novel diagnostic technologies facilitating the creation of a personalised approach to medical care. They should therefore be willing to work closely with colleagues in the life sciences as well as with clinicians and clinical researchers from within the East Asian medical tradition. The post is available from 1st October 2010 or as soon as possible thereafter. The closing date for applications, together with a short statement on why you believe you are suitable for the position and a description of your research plans, is Monday 6th September 2010. Interviews are expected to be held later in September. Administrative contact (for queries only): Tayjal Tailor (t.tailor1@wmin.ac.uk) Reference Number: 50000360 Closing Date: Friday 3 September 2010 |
A note about systems biology
Systems biology is about about how whole organs behave, as opposed to single cells or single molecules, It has to be the ultimate aim of biology. There is one case in which this has been done with some success, That is the modelling of the behaviour of the whole heart by Denis Noble and his colleagues in the Phyiology department (now gone) in Oxford. They adopted a bottom up approach. They measured the currents that flow though many sorts of ion channels in single cells from various parts of the heart, and how individual cells communicate with each other. Starting from this solid basis, together with a lot of computer power, they were able to model successfully a lot of phenomena that occur in the whole heart, but can’t be investigated in single cells. For example their work cast light on abnormal heart rhythms like ventricular fibrillation, and on the effect of drugs on heart rhythm.
This work was mostly done before the term ‘systems biology" thought of. It was called physiology. It is impressive work, and systems biology became a fashionable buzzword among research administrators and funding agencies. Despite the amount of money thrown at the problem, I’m not aware of any success that remotely approaches Noble’s.. One reason for that is that people have not been willing to put in the groundwork. In the case of the heart, the models were built on -many years of basic research on the electrophysiology of single heart cells. People have tried to model from the top down, without doing the spade work first. There has developed a perception that computing power can compensate for lack of basic knowledge about things work. It can’t. The usual aphorism applies: garbage in, garbage out.
Here’s an example, which eas noted in the diary pages for 29 June, 2008. While in Edinbuurgh, to give a talk to the European Conference on Mathematical and Theoretical Biology, I noticed a poster. It described an attempt to model on a computer the entire metabolic network of yeast.
“81 of the 662 intracellular concentrations were defined . . . The remainder were set to the median concentration of c. 0.2 mM.”
Ahem. We didn’t know the concentrations so we just made them up so we could run the program.
It’s interesting that even people in the business seem to realise that even that it isn’t living up to the hype. The Fixing proteomics web site shows why.
Put another way, if you try to run before you can walk, you risk falling falling on your face.
For these reasons, it seems to me that that most attempts at system biology have been disappointing (please correct me if I’m wrong)
Systems biology for Chinese medicine
If systems biology suffers from trying to run before it can walk in regular biology, where at least something is known about the functions of cells, how much more true that must be of Chinese medicine. In Chinese medicine almost all the treatments have never been tested properly in man. The odds are that most don’t work at all, and some are very poisonous (not to mention the cruelty and destruction of endangered species that is involved in making some of their more bizarre medicines). The idea that you can explain it with systems biology, is ludicrous in the extreme.
One can’t imagine any vaguely competent biologist who’d want to touch a project as bizarre as this with a bargepole.
Eastmedicine
This advertisement stems presumably from EASTmedicine is the University of Westminster’s research centre for East Asian Sciences and Traditions in Medicine. The proclaimed aims are to focus on “understanding, development and evaluation of East Asian medicines as living traditions”. The director of EASTmedicine, Volker Scheid, is a herbalist and acupuncturist and, as such, a firm believer in alternative medicine. When he isn’t at the University he has a private practice, the Traditional Acupuncture Centre, in London.
The website of his private practice makes some astonishing claims
"Acupuncture is effective in the treatment of numerous conditions including headache, migraine, digestive problems, menstrual disorders, indeterminate aches and pains, asthma, hayfever, stress, tiredness, depression and anxiety. Also commonly treated are chronic conditions such as arthritis, back pain, ulcerative colitis, irritable bowel syndrome, eczema, sinusitis, high blood pressure and repetitive strain injuries."
These claims simply cannot be justified by any worthwhile evidence. It will be interesting to see what Trading Standards make of them.
Dr Scheid describes himself as a "scholar physician". Physician seems a rather pretentious description for someone whose qualifications are stated to be PhD, MBAcC, FRCHM. But in similar vein he describes himself thus "I am one of the West’s leading experts on Chinese medical formulas and treatment strategies".
Although Scheid sells acupuncture treatments to patients, he seems ro be more anthropologist than medical. In a discussion of two acupuncture papers
"From the Perspective of the Anthropologist –
Volker Scheid, London, UK
From a perspective anchored in the cultural studies of science, technology and medicine my main interest in these papers is their status as cultural artifacts that provide access to the lifeworlds of a particular research community. If any, life-world debate and argument marks sites of contestation." Forsch Komplementärmed 2007;14:371–375
Scheid shows not the slightest interest in whether acupuncture works other than as a placebo. Since he is selling acupuncture, he presumably starts from the premise that it works.
Volker Scheid has had a £205,000 Wellcome Trust for the History of Medicine Project Grant: 2009 2012; Treating the Liver: Towards a Transnational History of East Asian Medicine; There’s nothing wrong with writing the history of long-outdated systems of medicine, though one could hardly imagine that the history would be very impartial, when it is written by a true believer. Another taste of his style can be found in his paper on Globalising Chinese Medical Understandings of Menopause. There is lots of rather pretentious stuff about culture, but very little about what actually works, Towards the end of the paper we come to the usual feeble excuse.
" . . once traditional medicines allow themselves to be evaluated by biomedical research methods, the odds against receiving fair treatment are heavily stacked against them."
The translation of that into plain English is something like ‘when we test our treatments properly we find they don’t work, so we blame the methods and carry on with selling them anyway’.
Judging from its web site, EASTmedicine does not to do any serious clinical trials to test whether the treaments work in man, They just know that they do. But they are hoping to add some spurious scientific background to their dubious claims by hiring someone to do compuations that will cast no light whatsoever on the question that really matters, Do they work or not?
The agenda is made clear by the statement
EASTmedicine seeks to describe and analyse the dynamics of these transformations with a specific view of managing their integration into contemporary health care.
So it is just yet another group of people pushing to have unproven and disproved treatments accepted by real medicine.
The University of Westminster appears to be determined to make itself the laughing stock by persisting in promoting junk science at a time when most other universities have realise that the harm done to their reputations is not worth the income it generates, Plenty of it has been revealed here.
The vice-chancellor of Westminster, Prof Geoffrey Petts, made into the pages of Private Eye (see Crystal balls. Professor Petts in Private Eye when he announced that he wouldn’t get rid of the junk, but would make it more ‘scientific’. Well, credit where it’s due, They have dropped homeopathy. see The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University For 2010 they still off ten different “BSc (Hons)” degrees in pre-scientific forms of medicine. It will take more than a bit od talk about systems biology to make anyone believe that these courses have anything to do with science.
For example, look at some slides from their lectures on “energy medicine”, Westminster University BSc: “amethysts emit high yin energy”
More make-believe from the University of Westminster. This time it’s Naturopathy , or
Why degrees in Chinese medicine are a danger to patients
The Dean of the School of the Life Sciences, Jane Lewis, is an entirely respectable marine biologist. She has had the thankless task of merging the real science with the alternative medicine in a single school. I phoned her to get a reaction
" outcome of merger of the school and trying to bring various parts of the school together" " "things are much more rigorous than they were".
DC: "Why don’t you just phase it out?"
"I’m not in a poition to do that. i move things forward as seems best -for the whole school I have to say". We’re retaining those bits thatI think have some good standing -I see NICE has approved the use of acupuncture for lower back pain and some other bits and pieces so I see acupuncture as something that does have some standing, andwe make sure it rigorously taught"
"DCHave you looked at the stuff on naturopathy?" "Are amethysts emit high Yin energy still taught?" " i don’t think so".
It seems, as so often in this case, that the senior people don’t really know what’s being taught under their noses. Prof
Lewis says she has not read about the background
to the (unusually) daft advice from NICE. Neither has she read Barker Bausell’s book on acupuncture research. If she had done any of these things,I suspect she would not have such a high opinion of it as appears to be the case.
Bait and switch. Astonishingly there is a now a whole organisation devoted to the respectabalisation of Traditional Chinese Medicine Good Practice in Traditional Chinese Medicine Research in the Post-genomic Era It sounds nice and sciencey but, as usual, they are trying to run before they can walk. The first thing has to be to do good clinical trials to find out if there is anything there to be investigated. If, and only if, this is the case, would there be any case for fancy talk about "proteomics"
and "the post-genomic era".
I do hope that no funding agency would be fooled into parting with money on the basis of the present vacuous rhetoric.
Professor Lewis said that I have I have quoted things like "amethysts emit high Yin energy" out of context. There is a simple solution to that. I have asked Westminster to make available the entire contents of the courses. Then we shall all be able to see the context of what their sudents are being taught.
Follow up
A brief report of this matter has appeared in Times Higher Education. In a statement, the University of Westminster says “its research into Chinese medicine is following the lead of “top research institutions”. I’m not aware of anyhting quite like this from anywhere else. In any case, Westminster should be able to think for themselves.
Suggested twitter tag: #buckgate
|
Number 19 Buckingham Street, London WC2N 6EF.is to be the home of the proposed "College of Medicine" that has arisen from the ashes of the late unlamented Prince’s Foundation for Integrated Health (their last accounts can be seen at Quackometer). Naturally one must ask if the "College of Medicine" will propagate the same sort of barmy ideas as the Prince’s Foundation used to do, A visit to Companies House shows the auguries are not good |
 19 Buckingham Street |
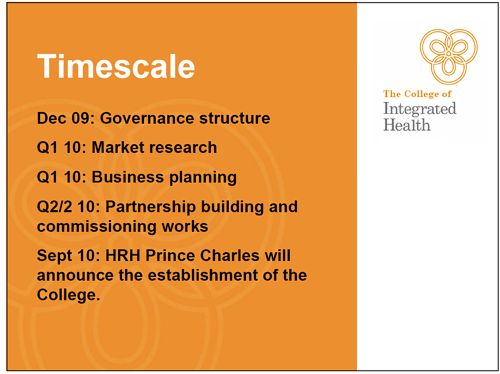
For one thing, the name College of Medicine has existed only since May 2010. The company was registered originally 19th November 2009 as The College of Integrated Health, but after a teleconference on 5th May 2010 it changed its name, presumably to make itself sound more like real medicine. This happened immediately after the closure of the Prince’s Foundation on April 30th.
There is no doubt that the "College of Medicine" is the direct descendent of the Prince of Wales’ Foundation. In a powerpoint show dated 9th November 2009 (before the name change) this slide is to be found.
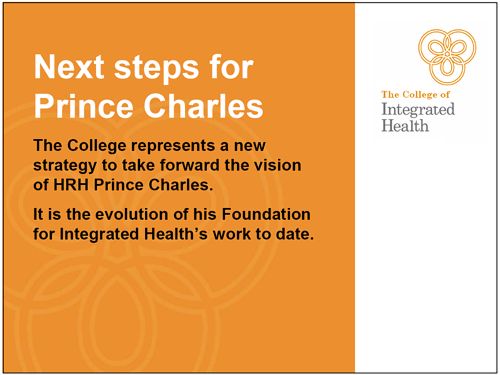
The author of the slide show is specified as "Linda". That, it is a fair bet, must be Linda Leung, who was Operations Director of the Prince’s Foundation until it closed, and is now Company Secretary for the "College of Medicine".
The final form of the "College" is still being argued about, but guess who will open it?
When ask about how Charles’ relationship with the College, The Office of TRH The Prince of Wales and The Duchess of Cornwall declined to make any comment, but simply referred me to Michael Dixon, who, in turn referred me to Pat Goodall.
Recently a statement from Clarence House to the Guardian said that "the Prince of Wales was aware of the college, but “has not been involved with setting-up the college, is not launching it and has no official role with it". That’s the official line anyway.
It is, of course, almost impossible to find out exactly what the relationship is between Prince Charles himself and the new "College". He operates largely out of sight, and the Freedom of Information Act, disgracefully, excludes his interference in the democratic process from public scrutiny.
Who is paying?
Flat 5 at 19 Buckingham Street was recently valued at half a million pounds. There is some serious money behind this venture. The rumour is that it’s from a ‘private donor’. Small prize for anyone who finds out who it is.
Aims of the College
The stated object of the College is "to advance health for the public benefit". Sounds good, but what does it mean? It doesn’t take long to find out. It is laid out in the document from Companies House.
To further its objects the Charity may:
7.1 engage with and develop communities of health professionals, health care providers and patients;
7.2 set standards and promote excellence in the fields of health and care;
7.3 lead, represent, train and support stakeholders so that they are better equipped to serve the public in improving the health ofthe public;
7.4 establish an evidence base for integrated health and for individual complementary modalities;
7.5 promote, foster and advance an integrated approach to health and care;
7.6 raise public, professional and political awareness and cultivate a sentiment in favour of an integrated approach to health and care by publishing and distributing books, pamphlets, reports, leaflets, journals, films, tapes and instructional matter on any media;
and so on, for 36 paragraphs. Already in paragraph 4 to 6 we see their interest is to promote “integrated health” and “complementary modalities. These of course are just what most of the rest of the world calls quackery. The objects don’t differ greatly from the Prince’s Foundation from which this outfit sprang.
What will be taught at the College?
Some information about the preliminary plans can be gleaned from a letter that describes the new College (download the letter). The letter says
“The College is developing two groups of courses. The first is aimed at registered professionals such as doctors, nurses and physiotherapists. It will familiarise them with different aspects of CAM and develop skills they can use in their day to day practice – not least techniques they can pass on to patients to help them manage their own conditions.”
In other words, the only course for doctors will be to teach them about quackery. Final judgement on that must await information about who will teach it.
“The second group of courses is aimed at non-registered practitioners and will focus on developing their understanding of conventional medicine, including ‘red flag’ symptoms, familiarisation with conventional therapeutics and increased awareness of critical appraisal.”
The other course, it seems, will be for quacks, to try to teach them enough real medicine to prevent them from killing too many people. The bit about teaching them about “critical appraisal” is hard to believe. If that were really done the clients would mostly be out of business.
If you were in any doubt at all about the aims of the College, it is necessary only to look at the four directors of the Company
Directors of the College of Medicine.
- Dr Michael Dixon, general practitioner. Michael Dixon was Medical Director of the Prince’s Foundation until it closed down.
- Professor George Lewith, is Professor of Health Research in the Complementary Medicine Research Unit, University of Southampton. He was a Foundation Fellow of the Prince’s Foundation until it closed down.
- Professor David Peters. is Professor of Integrated Healthcare and Clinical Director at the University of Westminster’s School of Integrated Health.
He was a Foundation Fellow of the Prince’s Foundation until it closed down. - Mrs Christine Glover is a pharmacist who sells homeopathic pills. She was a Foundation Fellow of the Prince’s Foundation until it closed down.
The company secretary is named as Linda Leung, who was Operations Director of the Prince’s Foundation until it closed.
A request to Michael Dixon for information was deflected to Mrs Pat Goodall She is yet another connection with PFIH. Mrs Goodall acted as a spokesperson for the Prince’s Foundation until it closed down. Now she is scheduled to become Director of Policy and Communications for the "College of Medicine". Mrs Goodall declined to say where the money came from. But she did say that the College was not the "equivalent of a further education college,. . . or higher education college", That being the case, it seems very odd to use the name "College of Medicine". It is a downright misleading name.
These people are all well know advocates of alternative medicine, It is very obvious that the "College of Medicine", despite its misleadingly innocuous name, is simply a reincarnation of the Prince’s Foundation for Integrated Health.
The term "integrated" is, of course, simply a euphemism for alternative medicine. That means those forms of medicine for which there is little or no evidence that they work. When evidence that something works is found, it is called simply medicine.
It may be useful to give a bit more information about the Directors.
Dr Michael Dixon OBE
Michael Dixon is devoted to just about every form of alternative medicine. As well as being medical director of the Prince’s Foundation he also runs the NHS Alliance. Despite its name, the NHS Alliance is nothing to do with the NHS and acts, among other things, as an advocate of alternative medicine on the NHS, about which it has published a lot.
Dr Dixon is also a GP at College Surgery, Cullompton, Devon, where his “integrated practice” includes dozens of alternative practitioners. They include not only disproven things like homeopathy and acupuncture, but also even more bizarre practitioners in ‘Thought Field Therapy‘ and ‘Frequencies of Brilliance‘.
To take only one of these, ‘Frequencies of Brilliance’ is bizarre beyond belief. One need only quote its founder and chief salesperson.
“Frequencies of Brilliance is a unique energy healing technique that involves the activation of energetic doorways on both the front and back of the body.”
“These doorways are opened through a series of light touches. This activation introduces high-level Frequencies into the emotional and physical bodies. It works within all the cells and with the entire nervous system which activates new areas of the brain.”
“Frequencies of Brilliance is a 4th /5th dimensional work. The process is that of activating doorways by lightly touching the body or working just above the body.”
“Each doorway holds the highest aspect of the human being and is complete in itself. This means that there is a perfect potential to be accessed and activated throughout the doorways in the body.”
Best of all, it can all be done at a distance (that must help sales a lot). One is reminded of the Skills for Health “competence” in distant healing (inserted on a government web site at the behest (you guessed it) of the Prince’s Foundation, as related here)
“The intent of a long distance Frequencies of Brilliance (FOB) session is to enable a practitioner to facilitate a session in one geographical location while the client is in another.
A practitioner of FOB that has successfully completed a Stage 5 Frequency workshop has the ability to create and hold a stable energetic space in order to work with a person that is not physically present in the same room.
The space that is consciously created in the Frequencies of Brilliance work is known as the “Gap”. It is a space of nonlinear time. It contains ”no time and no space” or respectively “all time and all space”. Within this “Gap” a clear transfer of the energies takes place and is transmitted to an individual at a time and location consciously intended. Since this dimensional space is in non-linear time the work can be performed and sent backward or forward in time as well as to any location.
The Frequencies of Brilliance work cuts through the limitations of our physical existence and allows us to experience ourselves in other dimensional spaces. Therefore people living in other geographic locations than a practitioner have an opportunity to receive and experience the work.
The awareness of this dimensional space is spoken about in many indigenous traditions, meditation practices, and in the world of quantum physics. It is referred to by other names such as the void, or vacuum space, etc.”
This is, of course, preposterous gobbledygook. It, and other things in Dr Dixon’s treatment guide, seem to be very curious things to impose on patients in the 21st century.
You can read more about Michael Dixon at Dr Aust’s blog (Dr Michael Dixon is annoyed), and, from the USA, Steven Novella’s analysis in Dr. Michael Dixon – “A Pyromaniac In a Field of (Integrative) Straw Men”
Professor George Lewith,
George Lewith has appeared quite often in this blog. He first came to my attention when I discovered in 2006 that his private clinic was offering a well-known form of fraudulent allergy diagnosis, the Vega test, despite the fact that Lewith himself had written a paper that said it didn’t work.
Lewith is particularly keen on acupuncture and that most discredited form of quackery, homeopathy. On More 4 News, he actually claimed that there was no good sham form of acupuncture. That is simply not true: great ingenuity has gone into devising controls for acupuncture trials and ‘real’ acupuncture always comes out the same as sham.
Professor David Peters
David Peters comes from the University of Westminster, which is famous for offering more degrees than any other in anti-scientific nonsense.
Westminster is home of the quite remarkable teaching that "Amethysts emit high Yin energy". dowsing, aura photography and other such fairground frauds.
Westminster offers also a "BSc degree" in that quite remarkable branch of make-believe known as naturopathy, This teaches students about a totally insane form of psycho-babble called Emo-trance and they are taught (no. seriously) about diagnosis with dowsing and pendulums
Westminster also teaches about kinesiology. Sounds sort of sciencey, but Applied Kinesiology is actually a fraudulent and totally ineffective diagnostic method invented by (you guessed) a chiropractor. It has been widely used by alternative medicine to misdiagnose food allergies. It does not work (Garrow, 1988: download reprint).
Westminster offers “BSc degrees” in Chinese Medicine that are a menace to public health. Their unfortunate students are told "Legally, you cannot claim to cure cancer. This is not a problem because we treat people not diseases". It is hard to imagine anything more irresponsible,
David Peters, as Clinical Director at Westminster must bear responsibility for this load of irresponsible make-believe, I have no doubt that he is well-intentioned but some of the stuff on these courses is a serious danger to public health.
Mrs Christine Glover
Mrs Glover is an Edinburgh pharmacist. She claims
She believes symptoms rarely occur in isolation but are usually linked to a persons circumstancs [sic].
Illness occurs when there are imbalances in any of the physical, emotional and spiritual aspects of their life.
Well, yes and no, Would you really go to her if you had cancer, or tuberculosis, or even atrial flutter? Judging by her website, what you’d get is a bottle of her Liquid Iron & Vitamin Formula (for £16.25 !). Or any one of a range of homeopathic pills.
There is no branch of alternative medicine that is more totally discredited than homeopathy. Yet now it i being proposed to form a College of Medicine with four directors who are all part of the dwindling band that insists you can do magic with pills that contain no medicine.
Who else supports the College?
There are some pretty surprising people who are listed in the letter as supporting the College of Medicine, though it remains to be seen how many are left once the true nature of the College is known.
Some of the supporters were already Foundation Fellows of the Prince’s Foundation, despite having no obvious sympathy with quackery. These include Professor Sir Cyril Chantler, Professor Adrian Eddleston and Professor Simon Gibbons. They also include the notorious Karol Sikora, and the geochemist Professor Jane Plant.
Professor Jane Plant is, apparently, a distinguished geochemist, but she developed an obsession with dairy-free diets, after her own experiences with breast cancer. She has written a lot of books and, no doubt, made a lot of money from the desperate. An extracr from one of her books is titled “Why I believe that giving up milk is the key to beating breast cancer”. If you want to see the ‘evidence’ for some of her wild claims, her web site invites to join -at a cost of £30. To get a bit closer to the truth it is only necessary to quote the World Cancer Research Fund (WCRF) Report on diet and cancer, ‘Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective‘. The WCRF is inclined, in my view, to exaggerate the strength of the evidence for a causal link between diet and cancer (see Diet and health. What can you believe: or does bacon kill you?) but nevertheless their assessment of dairy products is very different from Plant’s.
"The strongest evidence, corresponding to judgements of ‘convincing’ and ‘probable’, shows that milk probably protects against colorectal cancer, and that diets high in calcium are a probable cause of prostate cancer."
It seems that Jane Plant’s claims are thoroughly irresponsible.
I’m told that two people who were also Foundation Fellows, and who were originally listed as supporters of the College seem to have already jumped ship, namely Professor Stephen Holgate and Baroness Finlay.
Professor Sir Graeme Catto is to be president, and I’m told, Professor Sir Ian Kennedy has agreed to be vice president.
It is incomprehensible to me why people like this should be willing to lend their names to the Prince’s Foundation in the first place, or to its replacement now..
Other people listed as supporters include Sir Donald Irvine, Professor John Cox, and, on the "scientific advisory committee, Professor Mustafa Djamgoz and Professor Ajit Lalvani.
None of these people has an obvious belief in quackery. sp what are they doing mixed up with a venture like this?
Graeme Catto tells me he “knows very little about CAM”, and Cyril Chantler says the College should deal with evidence-based integrated medicine “but not alternative medicine or homeopathy”. Since, during his time as a Foundation Fellow of the Prince’s Foundation, Cyril Chantler failed totally to shake the advocacy of homeopathy by them, it seems unlikely yhat he’ll be any more successful with the College.
The only member of the "scientific advisory committee" who has answered by invitation to comment on a draft of this post is Professor Mustafa Djamgoz. It seems that he is more gullible that meets the eye He said, for example,
“There are many ‘eastern’ remedies (such as acupuncture that we witnessed dismissed 25 year ago) that work.”
“We ourselves have already shown that natural substances like omega-3 polyunsaturated fatty acids, reseveratrol [sic] etc can produce anti-cancer effects by blocking ion channels.”
Clearly Professor Djamgoz has not been keeping up with research in these areas. Has he never read Barker Bausell’s book on acupuncture, Snake Oil Science.? Apparently not. And there is, of course, not the slightest reason to think that omega-3 or resveratrol help cancer in humans.
It is often said that the reason that eminent people support quackery is that they live in hopes of a peerage. That is, perhaps, a bit uncharitable. I think it more likely that they don’t bother to investigate closely what it is they are signing up to, and that they are fooled by the weasel words of “integrated medicine”.
People like Catto and Chantler seem to think they are supporting caring, human centred, medicine. I fear they have been fooled, They are supporting sheer quackery.
Patient centred medicine
One of the most infuriating characteristics of quacks is their attempt to hi-jack the ‘human side of medicine’. I suppose they have little else to offer, so it’s understandable. But there is nothing human about deceiving desperate patients and the human side of medicine is something that is emphasised in the education of every real doctor.
If you want to know more about it, there is no better exposition than Michael Baum’s Samuel Gee lecture. Baum has been at the forefront of thinking about supportive or spiritual care of cancer patients. His 2009 Samuel Gee lecture is available in video, Concepts of Holism in Orthodox and Alternative Medicine. It is a masterpiece. He ends the lecture thus.
“Alternative versions of “holistic medicine” that offer claims of miracle cures for cancer by impossible dietary regimens, homeopathy or metaphysical manipulation of non-existent energy fields, are cruel and fraudulent acts that deserve to be criminalized.”
A similar distinction has been made with beautiful clarity by Dr James May
“The use of the term ‘integrative medicine’ in your editorial seems to confuse more than clarify the problem of ‘holism’ in medicine. Complementary therapists for example often use the term ‘holistic’ to blur the boundaries between the therapies used and the practitioner’s interpersonal skills. It would be better, however, to keep these distinctions clear. Caring is different from curing.”
“‘Holism’ is not a multifaceted approach to curing, it is a multifaceted approach to caring”
“Effective medicine is best measured with RCTs. Caring is not. ‘Integrative medicine’ therefore risks both damaging how we measure effective medicines (RCTs), as well as reducing caring to measurables. A better term for this might be ‘disintegrative medicine’.Effective medicine is best measured with RCTs. Caring is not. ‘Integrative medicine’ therefore risks both damaging how we measure effective medicines (RCTs), as well as reducing caring to measurables. A better term for this might be ‘disintegrative medicine’.”
I hope that the various eminent people who have lent their name to this mis-named ‘College of Medicine’ will look very carefully at what it actually does. And that will probably mean withdrawing their support.
Follow-up
The Guardian, 2nd August 2010, carried this story, written by their science correspondent, Ian Sample: College of Medicine born from ashes of Prince Charles’s holistic health charity. He quotes Tracey Brown of the Sense about Science charity as saying that the college’s emphasis on merging conventional medicine with unproven complementary therapies “would take society back a century”.
“Despite its mission to promote the integration of alternatives to medicine, this new body has chosen to call itself very grandly the College of Medicine. Perhaps someone thinks this will sound good with Royal in front of it? This wouldn’t be a surprise given the institution’s origins in the Prince of Wales’s efforts to integrate his favoured traditional remedies into medicine.”

Quotation from DC
The term ‘evidence-based medicine’ seemed to me, when I first heard it, utterly ludicrous. It still does. What’s the alternative? Guess-work based medicine?
Quacks are fond of using cuddly words like ‘holistic’ and ‘integrative’, partly, one suspects, in an attempt to gain respectability and to disguise some of their barmier views. See, for example, Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
Advocates of evidence-based medicine are often accused by quacks of being hard-hearted calculators who want to take the soul out of medicine. Nothing could be further from the truth in my view. But I don’t practise medicine so it seemed to me to be worth quoting two of the best definitions I know, both from people at the sharp end of medicine.
James Matthew May
James May is a general practioner in London. He is also chairman of Healthwatch, an organisation that was exposing health fraud long before the recent explosion in the ‘skeptical blogosphere’.
The following passage was written as comment (‘rapid reponse’) to an editorial in the British Medical Journal. The editorial itself was (in my view) silly and misguided (Closing the evidence gap in integrative medicine, by Hugh MacPherson, David Peters, and Catherine Zollman). It is best forgotten as soon as possible. But James May’s comment deserves to be preserved and publicised. The highlights in bold font are mine.
|
The use of the term ‘integrative medicine’ in your editorial seems to confuse more than clarify the problem of ‘holism’ in medicine. Complementary therapists for example often use the term ‘holistic’ to blur the boundaries between the therapies used and the practitioner’s interpersonal skills. It would be better, however, to keep these distinctions clear. Caring is different from curing. The point of RCTs is to establish how much of a treatment’s efficacy is independent of the ideas, concerns, and expectations of either the patient or the clinician. Using ‘multi-modal’ or ‘synergistic’ research methods is likely to confuse this important distinction. ‘Holism’ is not a multifaceted approach to curing, it is a mulitfaceted approach to caring. A truly holistic clinician will ‘cure sometimes, relieve often and comfort always’. Comforting may not produce a positive clinical outcome – but we should still do it. Historically speaking caring pre-existed effective medicine by millenia, but it was a principle motive for finding effective medicine. Caring therefore is not a subset of medicine, instead medicine is one of the tools used for caring. ‘Integrative medicine’ as a concept, however, blurs this boundary. It has been wisely observed that ‘if we keep trying to measure what we value, we will end up only valuing what we can measure.’ This particular ‘evidence gap’ is therefore probably best left; filled instead by caring doctors. Effective medicine is best measured with RCTs. Caring is not. ‘Integrative medicine’ therefore risks both damaging how we measure effective medicines (RCTs), as well as reducing caring to measurables. A better term for this might be ‘disintegrative medicine’. Competing interests: Chairman of HealthWatch |
Michael Baum
Baum is a recently-retired cancer surgeon from UCLH. As well as being s surgeon with a strong interest in scientific medicine, he has been at the forefront of thinking about supportive or spiritual care of cancer patients. His 2009 Samuel Gee lecture is available in video, Concepts of Holism in Orthodox and Alternative Medicine. It is a masterpiece. The conclusion puts his view bluntly (again the emphasis is mine).
|
Conclusion Holism in medicine is an open ended and exquisitely complex understanding of human biology that over time has lead to spectacular improvements in the length and quality of life of patients with cancer. This approach encourages us to consider the transcendental as much as the cell and molecular biology of the human organism. Alternative versions of “holistic medicine” that offer claims of miracle cures for cancer by impossible dietary regimens, homeopathy or metaphysical manipulation of non-existent energy fields, are cruel and fraudulent acts that deserve to be criminalized. Such “alternative” versions of holism are arid and closed belief systems, locked in a time warp, incapable of making progress yet quick to deny progress in the field of scientific medicine. |
Follow-up
There is something very offensive about the idea that a ‘bachelor of science’ degree can be awarded by a university, as a prize for memorising gobbledygook.
Once the contents of the ‘degrees’ has been exposed to public ridicule, many universities have stopped doing it. All (or nearly all) of these pseudo-degrees have closed at the University of Salford, the University of Central Lancashire, Robert Gordon University, the University of Buckingham, and even at the University of Westminster (the worst offender), one course has closed (with rumours of more to follow).
|
I’ve already written about the course in Traditional Chinese Medicine at the University of Salford (Chinese medicine -acupuncture gobbledygook revealed) and at the University of Westminster: see Why degrees in Chinese medicine are a danger to patients. The former has closed, but not the latter. Here is another one. One place that has yet to come under close scrutiny is Middlesex University. |

Michael Driscoll, VC of Middlesex University. The buck stops with him. |
Their “Complementary Health” courses are as follows (April 2010).
- Complementary Health Sciences (Ayurveda) Degree, BSc Honours
- Herbal Medicine Degree, BSc Honours
- Traditional Chinese Acupuncture Degree, BSc Honours
- Traditional Chinese Medicine Degree, BSc Honours
and also two postgraduate courses
I asked Middlesex University for samples of their teaching materials under the Freedom of Information Act, and, as usual, the request was refused. As usual, I then asked for the mandatory internal review of the decision, and this time, most unusually, the internal review did not confirm the initial refusal and I was sent a bundle of teaching materials about Chinese Herbal Medicine, It was not all I asked for, but it is quite enough to show the absurd ideas that are still being taught as part of bachelor of Science degree in a UK University.
Not only are the ideas absurd, pre-scientific, indeed antiscientific. They are also dangerous. People who have been taught this nonsense are going out and being let loose on sick people.
The vice-chancellor of Middlesex University, Professor Michael Driscoll, is an economist, not a biologist. Surely you don’t need to be a scientist to feel a bit suspicious when you read on the Middlesex web site about
Traditional Chinese Acupuncture and Moxibustion including distribution of meridians-collaterals and location of acupoints; needling and moxibustion techniques;
Have any of the members of the Executive ever thought to ask about what goes on in these courses? Even if it is beyond an economist to see through the nonsense, surely it should be possible for Professor Margaret House, Deputy Vice-Chancellor Academic, whose interests lie in water quality, should be able to, though as Dean of the School of Health and Social Sciences she appears to sponsor the nonsense. And Professor Waqar Ahmad, Deputy Vice-Chancellor Research and Enterprise, who has written a s book on Ethnicity, Health and Health Care, should surely be able to distinguish sense from nonsense in health care? In that respect, I’d have less confidence in Katie Bell, Chief Marketing Officer, who joined Middlesex University in 2009 following a career in brand marketing for Nestlé UK and GlaxoSmithKline Consumer Healthcare. Marketing people seldom have much regard for truth.
Have any of the University’s Governors ever asked what is going on in their name? It’s true that none of the long list of distinguished-sounding governors is a scientist. Surely you don’t need to be to question whether or not what follows can be described as ‘science’.
My guess is that none of these distinguished people has ever bothered to look at the dangerous nonsense that is being taught in their University. It is not in the nature of ‘managers’ to look far beyond ticked-boxes and profit, They should have done of course, but to make it easier for them, here is a small selection of the slides that I was sent (the copyright for them lies with the university: these few slides come under the heading ‘ ‘fair quotation’ and it is undoubtedly in the public interest to show them).
Course CMH 1211
e 
Uhuh, my spleen qi is well and truly knotted already though when I learned physiology it was not thought that the spleen had much to do with emotions.
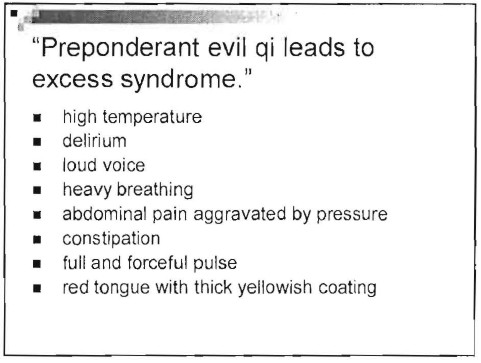
Ah so at least the problem of heavy breathers is solved. But high temperature, abdominal pain and abnormal pulse can be signs of serious illness. If your only explanation for them is “preponderant evil Qi”, you are a menace to public health.
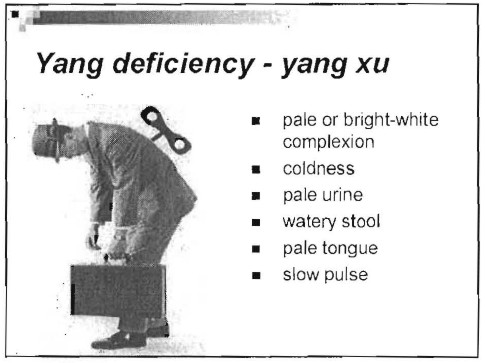
All these symptoms could be the result of a serious disease. It is not only antiquated nonsense to talk about them in terms of Yin, Yang and Qi. It endangers people,
Course CMH 2212
Chinese materia medica. Some of the herbs are likely to contain active ingredients (indeed some are very dangerous). It would be quite possible to study the ingredients of these herbs and to investigate how they work in the light of what has been learned about physiology and pharmacology in the last 200 years. Pharmacology has a long history of doing that, But is seems to play no part in this course. Herbs are “cold” or “hot” and may “check the exuberance of yang”.
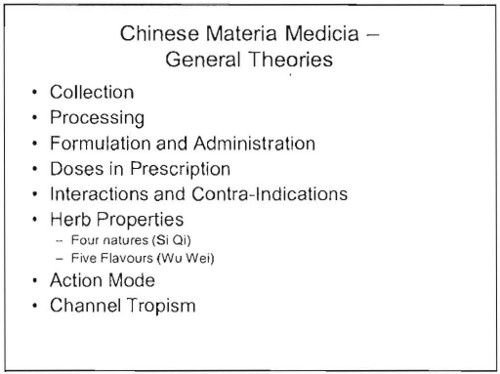
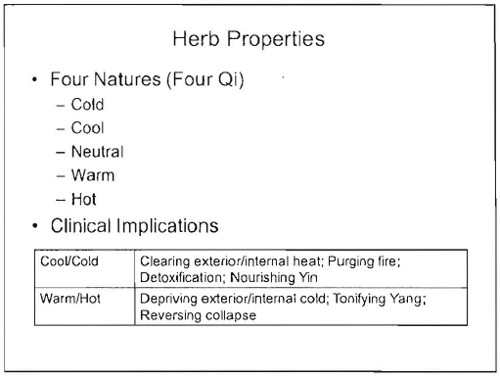
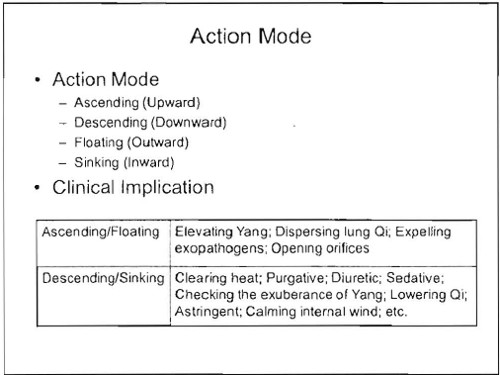
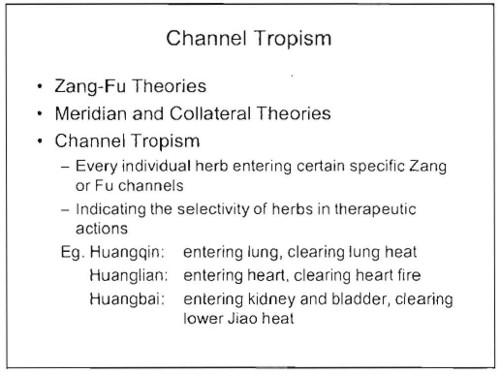
and so on, just preposterous, made-up nonsense from another era.
If it were taught as cultural history, it might be interesting. But it is being taught as though it were true, and an appropriate way to treat sick people.
Course CMH 3214
Would you trust your child to someone who’d been taught that “causes of paediatric diseases are relatively simple”, and “children are pure yang”?
Now some Chinese recipes
Course CMH 3100
![]()
This may or may not taste good, but to recommend it for diabetes is seriously irresponsible.
The programme specification for the “BSc (Hons) Traditonal Chinese medicine” can be found here. [local copy download]
It is written with all the official trappings, just as though the degree was about science. It isn’t. It is a danger to public health.
I have asked the vice-chancellor, Michael Driscoll, to express his view of these comments
Follow-up
A rather unexpected comment from a London acupuncturist.
“At least,I knew that Professor David Colquhoun is very skeptical about Chinese medicine. he comment Chinese medicine study”not only are the ideas absurd, pre-scientific, indeed antiscientific. They are also dangerous. People who have been taught this nonsense are going out and being let loose on sick people.” “
“But,I still like to read his blog as His article very is respectable. I think. Look this…”
The skeptic blog featured this post in its weekly roundup.
27 May 2010. Times Higher Education reported the decision of Middlesex University to close its philosophy department. This department seems to have a remarkable reputation, not least for a post-1992 university. Three academics and four students have been suspended and gagged in classical bullying style.
This has happened while they continue to teach dangerous rubbish like that described above.
I left a comment at Times Higher, as follows.
It is a reflection on the quality of university management that Middlesex has chosen to shut its philosophy department while continuing to run degrees in quackery. These courses not only offer an Hons BSc for memorising chunks of anti-scientific nonsense. They also pose a real danger to patients. See https://www.dcscience.net/?p=2923
I can think of no better illustration than this of the crass nature of the judgements made by Middlesex’s management. They are either ignorant of what constitutes science, or they are corrupt. I see no other possibilities. In either case they should not be running a university.
I think Prof Michael Driscoll owes the world an explanation.
Every single request for information about course materials in quack medicine that I have ever sent has been turned down by universities,
It is hardly as important as as refusal of FoI requests to see climate change documents, but it does indicate that some vice-chancellors are not very interested in openness. This secretiveness is exactly the sort of thing that leads to lack of trust in universities and in science as a whole.
The one case that I have won took over three years and an Information Tribunal decision against the University of Central Lancashire (UCLAN) before I got anything.
UCLAN spent £80,307.95.(inc VAT at 17.5%) in legal expenses alone (plus heaven knows how much in staff time) to prevent us from seeing what was taught on their now defunct “BSc (Hons) homeopathy”. This does not seem to me to be good use of taxpayers’ money. A small sample of what was taught has already been posted (more to come). It is very obvious why the university wanted to keep it secret, and equally obvious that it is in the public interest that it should be seen.
UCLAN had dropped not only its homeopathy "degree" before the information was revealed, They also set up an internal inquiry into all the rest of their courses in magic medicine which ended with the dumping of all of them.
Well, not quite all, There was one left. An “MSc” in homeopathy by e-learning. Why this was allowed to continue after the findings of UCLAN’s internal review, heaven only knows. It is run by the same Kate Chatfield who ran the now defunct BSc. Having started to defend the reputation against the harm done to it by offering this sort of rubbish, I thought I should finish. So I asked for the contents of this course too. It is, after all, much the same title as the course that UCLAN had just been ordered to release. But no, this request too was met with a refusal
Worse still, the refusal was claimed under section 43(2) if the Freedom of Information Act 2000. That is the public interest defence, The very defence that was dismissed in scathing terms by the Information Tribunal less than two months ago,
To add insult to injury, UCLAN said that it would make available the contents of the 86 modules in the course under its publication scheme, at a cost of £20 per module, That comes to £1,720 for the course, Some freedom of information.
Because this was a new request, it now has to go through the process of an internal reviw of the decision before it can ne referred to the Information Commissioner. That will be requested, and since internal reviews have, so far, never changed the initial judgment. the appeal to the Information Commissioner should be submitted within the month. I have been promised that the Information Commissioner will deal with it much faster this time than the two years it took last time.
And a bit more unfreedom
Middlesex University
I first asked Middlesex for materials from their homeopathy course on 1 Oct 2008. These courses are validated by Middlesex university (MU) but actually run by the Centre for Homeopathic Education. Thw MU site barely mentions homeopathy and all I got was the usual excuse that the uninsersity did not possess the teaching materials. As usual, the validation had been done without without looking at what was actually being taught. The did send me the validation document though [download it] As usual, the validation document shows no sign at all of the fact that the usbject of the "BSc" is utter nonsense. One wonderful passage says
“. . . the Panel were assured that the Team are clearly producing practitioners but wanted to explore what makes these students graduates? The Team stated that the training reflects the professional standards that govern the programme and the graduateness is achieved through developing knowledge by being able to access sources and critically analyse these sources . . . “
Given that the most prominent characteristic of homeopaths (and other advocates of magic medicine) is total lack of critical ability, this is hilarious. If they had critical ability they wouldn’t be homeopaths. Hilarious is not quite the right word, It is tragic that nonsense like this can be found in an official university document.
Middlesex, though it doesn’t advertise homeopathy, does advertise degrees in Traditional Chinese Medicine, Herbal Medicine and Ayurveda. On 2nd February 2010 I asked for teaching materials from these courses. Guess what? The request was refused. In this case the exemptions under FOIA were not even invoked but I was told that "All these materials are presently available only in one format at the University – via a student-only accessed virtual learning environment. ". Seems that they can’t print out the bits that I asked for, The internal review has been requested, then we shall see what the Information Commissioner has to say.
Two other cases are at present being considered by the Information Commissioner (Scotland), after requests under the Scottish FoIA were refused. They are interesting cases because they bear on the decision, currently being considered by the government, about whether they should implement the recommendations of the execrable Pittilo report.
Napier University Edinburgh. The first was for teaching material form the herbal medicine course at Napier University Edinburgh. I notice that this course no longer appears in UCAS or on Napier’s own web site, so maybe the idea that its contents might be disclosed has been sufficient to make the university do the sensible thing.
Robert Gordon University Aberdeen The second request was for teaching material from the “Introduction to Homeopathy” course at the Robert Gordon University Aberdeen. The particular interest that attaches to this is that the vice-chancellor of Robert Gordon university is Michael Pittilo. The fact that he is willing to tolerate such a course in his own university seems to me to disqualify him from expressing any view on medical subjects.
Michael Pittilo, Crohn’s disease and Andrew Wakefield
Michael Pittilo has not been active in science for some time now, but Medline does show scientiifc publications for Pittilo RM, between 1979 anf 1998. Between 1989 and 1995 there are five papers published jointly with one Andrew Wakefield. These papers alleged a relationship between measles virus and Crohn’s disease. The papers were published before tha infamous 1998 paper by Wakefield in the Lancet (now retracted) that brought disgrace on Wakefield and probably caused unnecessary deaths.. The link between measles and Crohn’s disease is now equally disproved.
The subject has been reviewed by Korzenik (2005) in Past and Current Theories of Etiology of IBD. Toothpaste, Worms, and Refrigerators
“Wakefield et al proposed that Crohn’s results from a chronic infection of submucosal endothelium of the intestines with the measles virus [Crohn’s disease: pathogenesis and persistent measles virus infection. Wakefield AJ, Ekbom A, Dhillon AP, Pittilo RM, Pounder RE., Gastroenterology, 1995, 108(3):911-6]”
"This led to considerable media interest and< public concern over use of live measles vaccine as well as other vaccines. A number of researchers countered these claims, with other studies finding that titers to measles were not increased in Crohn’s patients, granulomas were not associated with endothelium 49 , measles were not in granulomas50 and the measles vaccine is not associated with an increased risk of Crohn’s disease51–55 "
This bit of history is not strictly relevant to the Pittilo report, but I do find quite puzzling how the government chooses people from whom it wishes to get advice about medical problems.
Follow-up
I notice that the Robert Gordon university bulletin has announced that
“Professor Mike Pittilo, Principal of the University, has been made an MBE in the New Year Honours list for services to healthcare”.
That is a reward for writing a very bad report that has not yet been implemented, and one hopes, for the sake of patients, will never be implemented. I do sometimes wonder about the bizarre honours system in the UK.
Postcript.
On 16th February, the death of Michael Pittilo was announced. He had been suffeing from cancer and was only 55 years old. I wouldn’t wish that fate on my worst enemy.
The purpose of this post is to reveal a few samples of things that are taught on a homeopathy ‘degree’ course. The course in question was the "BSc Hons homeopathy course at the University of Central Lancashire (UCLAN). Entry to this course was closed in 2008 and, after an internal review, UCLAN closed almost all of the rest of its courses in alternative medicine too. The university is to be commended for this .
The purpose of making public some of what used to be taught is not to embarrass UCLAN, which has already done the sensible thing, but to make it clear that the sort of thing taught on such courses is both absurd and dangerous, in the hope of discouraging other courses
|
.Three years after I first asked for teaching materials, the Information Commisioner ruled that all the reasons given for refusal were invalid, and they must be handed over. However UCLAN then appealed against the decision, so the appeal went to an Information Tribunal. That appeal was lost decisively and UCLAN was.obliged to provide the whole of the course material. On Christmas Eve I got five large box files, 13.7 kg of documents, or 30 pounds, in old money. |

|
Because these documents are copyright, I rely on the twin defences of fair quotation (only a tiny proportion is being quoted) and public interest. The Information Tribunal decided very firmly that it was in the public interest that it should be known what is taught on such courses, and that can be achieved if some of it is made public. Here are a few extracts.
Code of ethics
The students are given a copy of the code of ethics of the Society of Homeopaths. This is 25 pages long, but paragraph 48 is especially interesting.
48 Advertisements, stationery and name plates maintain a high standard of propriety and
integrity to enhance the reputation of homeopathy.
- Advertising shall not contain claims of superiority.
- No advertising may be used which expressly or implicitly claims to cure named diseases.
- Advertising shall not be false, fraudulent, misleading, deceptive, extravagant or sensational.
No mention though, of the fact that this code of ethics has been repeatedly breached by the Society of Homeopaths itself, on its own website. See, for example, here in 2007 and again in 2009. as well as Ernst’s article on this topic.
Anyone who has followed dialogues among homeopaths knows that "claims to cure named diseases" is the norm not the exception. The code of ethics is just a bad joke. And the (late) course at UCLAN was no exception. Take, for example, course HP3002, Therapeutic Homeopathy, module leader Jean Duckworth.
Homeopathic treatment of cancer
There was a lecture on HP3002 called "A Homeopathic Approach to Cancer (Ramakrishnan methodology [sic])".. Here are 10 slides from that lecture. It is illegal to claim to be able to cure cancer under the Cancer Act 1939. If a homeopath were to make claims like these in public they’d be open to prosecution, not to mention in breach of the SoH’s code of ethics. If cancer is not a "named disease", what is?
Specific treatments for a named disease are recommended.
What happened to treating the whole person? Now specific organs are being treated. The term "affinity", as used here, is of course sheer hocus pocus.
It is easy to forget when reading this that none of the “medicines” contain any medicine whatsoeever.
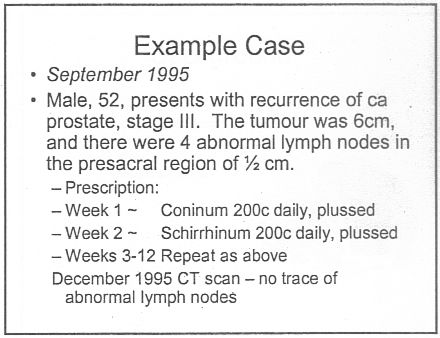
Notice that the term "remedy" is used throughout. Any reasonable person would interpret "remedy" to imply "cure", though no doubt a homeopath, if challenged, would claim that "remedy" carried no such implication. The last slide is typical of junk medicine: the personal testimonial, supplied with no detail whatsoever. Just an anecdote which is useless as evidence.
This lecture alone strikes me as a cruel (and possibly illegal) hoax perpetrated on desperate patients. Of course a true believer might get some solace from taking the sugar pills, but that is not sufficient justification.
The same course dealt with quite a lot of other "named diseases", autism, ADHD and coping with a heart attack. And, you are asked, did you think arnica is just a first aid remedy?
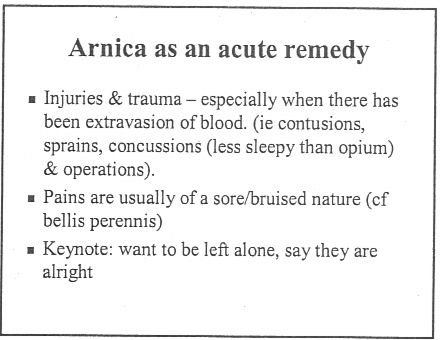
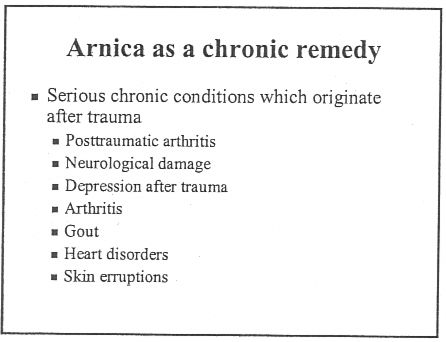
If that isn’t a list of "named diseases", what is? The code of ethics appears to be a total sham.
And of course never forget that the “arnica” doesn’t contain any arnica anyway. And if you don’t believe that you can read the words of Kate Chatfield, module leader on thie very course, as recorded in the minutes of evidence to the Select Committee on Science and Technology .
Q538 Lord Broers: I have a simple, technical question about homeopathy and drugs. Is it possible to distinguish between homeopathic drugs after they have been diluted? Is there any means of distinguishing one from the other?
Ms Chatfield: Only by the label.
You can read a lovely analysis of the views of Kate Chatfield by physicist A.P. Gaylard here.
Follow-up
The Daily Telegraph. January 8th 2009 Ian Douglas reported on this post: The workings of a BSc in homeopathy
The Lancashire Evening Post carried a big spread on January 15th, Professor seeks out the truth about ‘quackery’.
River’s Edge. News and thoughts from Preston, Lancashire reviewed the Lancashire Evening Post article on Saturday January 16th: Homeopathy at UCLAN, a degree in quackery.
The cost of trying to stop this material being revealed. UCLAN told me on 5 February 2010 that the legal costs alone were £80,307.94 (inc. VAT). That doesn’t include staff time and photocopying. I’m not convinced that this was a good way to spend taxpayers’ money.
The Yuletide edition of the BMJ carries a lovely article by Jeffrey Aronson, Patent medicines and secret remedies. (BMJ 2009;339:b5415).
I was delighted to be asked to write an editorial about it, In fact it proved quite hard work, because the BMJ thought it improper to be too rude about the royal family, or about the possibility of Knight Starvation among senior medics. The compromise version that appeared in the BMJ is on line (full text link).
The changes were sufficient that it seems worth posting the original version (with links embedded for convenience).
The cuts are a bit ironic, since the whole point of the article is to point out the stifling political correctness that has gripped the BMA, the royal colleges, and the Department of Health when it comes to dealing with evidence-free medicine. It has become commonplace for people to worry about the future of the print media, The fact of the matter is you can often find a quicker. smarter amd blunter response to the news on blogs than you can find in the dead tree media. I doubt that the BMJ is in any danger of course. It has a good reputation for its attitude to improper drug company influence (a perpetual problem for clinical journals) as well as for clinical and science articles. It’s great to see its editor, Fiona Godlee, supporting the national campaign for reform of the libel laws (please sign it yourself).
The fact remains that when it comes to the particular problem of magic medicine, the action has not come from the BMA, the royal colleges, and certainly not from the Department of Health, It has come from what Goldacre called the “intrepid, ragged band of bloggers”. They are the ones who’ve done the investigative journalism, sent complaints and called baloney wherever they saw it. This article was meant to celebrate their collective efforts and to celebrate the fact that those efforts are beginning to percolate upwards to influence the powers that be.
It seems invidious to pick on one example, but if you want an example of beautiful and trenchant writing on one of the topics dealt with here, you’d be better off reading Andrew Lewis’s piece "Meddling Princes, Medical Regulation and Licenses to Kill” than anything in a print journal.
I was a bit disappointed by removal of the comment about the Prince of Wales. In fact I’m not particularly republican compared with many of my friends. The royal family is clearly good for the tourist industry and that’s important. Since Mrs Thatcher (and her successors) destroyed large swathes of manufacturing and put trust in the vapourware produced by dishonest and/or incompetent bankers, it isn’t obvious how the UK can stay afloat. If tourists will pay to see people driving in golden coaches, that’s fine. We need the money. What is absolutely NOT acceptable is for royals to interfere in the democratic political process. That is what the Prince of Wales does incessantly. No doubt he is well-meaning, but that is not sufficient. If I wanted to know the winner of the 2.30 at Newmarket, it might make sense to ask a royal. In medicine it makes no sense at all. But the quality of the advice is irrelevant anyway. The royal web site itself says “As a constitutional monarch, the Sovereign must remain politically neutral.”. Why does she not apply that rule to her son? Time to put him over your knee Ma’am?
Two of the major bits that were cut out are shown in bold, The many other changes are small.
BMJ editorial December 2009
Secret remedies: 100 years onTime to look again at the efficacy of remedies Jeffrey Aronson in his article [1] gives a fascinating insight into how the BMA, BMJ and politicians tried, a century ago, to put an end to the marketing of secret remedies. They didn’t have much success. The problems had not improved 40 years later when A.J. Clark published his book on patent medicines [2]. It is astounding to see how little has changed since then. He wrote, for example, “On the other hand the quack medicine vendor can pursue his advertising campaigns in the happy assurance that, whatever lies he tells, he need fear nothing from the interference of British law. The law does much to protect the quack medicine vendor because the laws of slander and libel are so severe.”> Clark himself was sued for libel after he’d written in a pamphlet “ ‘Cures’ for consumption, cancer and diabetes may fairly be classed as murderous”. Although he initially tried to fight the case, impending destitution eventually forced him to apologise [3]. If that happened today, the accusation would have been repeated on hundreds of web sites round the world within 24 hours, and the quack would, with luck, lose [4]. As early as 1927, Clark had written “Today some travesty of physical science appears to be the most popular form of incantation” [5]. That is even more true today. Homeopaths regularly talk utter nonsense about quantum theory [6] and ‘nutritional therapists’ claim to cure AIDS with vitamin pills or even with downloaded music files. Some of their writing is plain delusional, but much of it is a parody of scientific writing. The style, which Goldacre [7] calls ‘sciencey’, often looks quite plausible until you start to check the references. A 100 years on from the BMA’s efforts, we need once again to look at the efficacy of remedies. Indeed the effort is already well under way, but this time it takes a rather different form. The initiative has come largely from an “intrepid, ragged band of bloggers” and some good journalists, helped by many scientific societies, but substantially hindered by the BMA, the Royal Colleges, the Department of Health and a few vice-chancellors. Even NICE and the MHRA have not helped much. The response of the royal colleges to the resurgence in magic medicine that started in the 1970s seems to have been a sort of embarrassment. They pushed the questions under the carpet by setting up committees (often populated with known sympathizers) so as to avoid having to say ‘baloney’. The Department of Health, equally embarrassed, tends to refer the questions to that well-known medical authority, the Prince of Wales (it is his Foundation for Integrated Health that was charged with drafting National Occupational Standards in make-believe subjects like naturopathy [8]. Two recent examples suffice to illustrate the problems. The first example is the argument about the desirability of statutory regulation of acupuncture, herbal and traditional Chinese medicine (the Pittilo recommendations) [9]. Let’s start with a definition, taken from ‘A patients’ guide to magic medicine’ [10]. “Herbal medicine: giving patients an unknown dose of an ill-defined drug, of unknown effectiveness and unknown safety”. It seems to me to be self-evident that you cannot start to think about a sensible form of regulation unless you first decide whether what you are trying to regulate is nonsense, though this idea does not seem to have penetrated the thinking of the Department of Health or the authors of the Pittilo report. The consultation on statutory regulation has had many submissions [11] that point out the danger to patients of appearing to give official endorsement of treatments that don’t work. The good news is that there seems to have been a major change of heart at the Royal College of Physicians. Their submission points out with admirable clarity that the statutory regulation of things that don’t work is a danger to patients (though they still have a blank spot about the evidence for acupuncture, partly as a result of the recent uncharacteristically bad assessment of the evidence by NICE [12]). Things are looking up. Nevertheless, after the public consultation on the report ended on November 16th, the Prince of Wales abused his position to make a well-publicised intervention on behalf of herbalists [13]. Sometimes I think his mother should give him a firm lesson in the meaning of the term ‘constitutional monarchy’, before he destroys it. The other example concerns the recent ‘evidence check: homeopathy’ conducted by the House of Commons Science and Technology Select Committee (SCITECH). First the definition [10]: “Homeopathy: giving patients medicines that contain no medicine whatsoever”. When homeopathy was dreamt up, at the end of the 18th century, regular physicians were lethal blood-letters, and it’s quite likely that giving nothing saved people from them. By the mid-19th century, discoveries about the real causes of disease had started, but homeopaths remain to this day stuck in their 18th century time warp. In 1842 Oliver Wendell Holmes said all that needed to be said about medicine-free medicine [14]. It is nothing short of surreal that the UK parliament is still discussing it in 2009. Nevertheless it is worth watching the SCITECH proceedings [15]. The first two sessions are fun, if only for the statement by the Professional Standards Director of Boots that they sell homeopathic pills while being quite aware that they don’t work. I thought that was rather admirable honesty. Peter Fisher, clinical director of the Royal Homeopathic Hospital, went through his familiar cherry-picking of evidence, but at least repeated his condemnation of the sale of sugar pills for the prevention of malaria. But for pure comedy gold, there is nothing to beat the final session. The health minister, Michael O’Brien, was eventually cajoled into admitting that there was no good evidence that homeopathy worked but defended the idea that the taxpayer should pay for it anyway. It was much harder to understand the position of the chief scientific advisor in the Department of Health, David Harper. He was evasive and ill-informed. Eventually the chairman, Phil Willis, said “No, that is not what I am asking you. You are the Department’s Chief Scientist. Can you give me one specific reference which supports the use of homeopathy in terms of Government policy on health?”. But answer came there none (well, there were words, but they made no sense). Then at the end of the session Harper said “homeopathic practitioners would argue that the way randomised clinical trials are set up they do not lend themselves necessarily to the evaluation and demonstration of efficacy of homeopathic remedies, so to go down the track of having more randomised clinical trials, for the time being at least, does not seem to be a sensible way forward.” Earlier, Kent Woods (CEO of the MHRA) had said “the underlying theory does not really give rise to many testable hypotheses”. These two eminent people seemed to have been fooled by the limp excuses offered by homeopaths. The hypotheses are testable and homeopathy, because it involves pills, is particularly well suited to being tested by proper RCTs (they have been, and when done properly, they fail). If you want to know how to do it, all you have to do is read Goldacre in the Guardian [16]. It really isn’t vert complicated. “Imagine going to an NHS hospital for treatment and being sent away with nothing but a bottle of water and some vague promises.” “And no, it’s not a fruitcake fantasy. This is homeopathy and the NHS currently spends around £10million on it.” That was written by health journalist Jane Symons, in The Sun [17]. A Murdoch tabloid has produced a better account of homeopathy than anything that could be managed by the chief scientific advisor to the Department of Health. And it isn’t often that one can say that. These examples serve to show that the medical establishment is slowly being dragged, from the bottom up, into realising that matters of truth and falsehood are more important than their knighthoods. It is all very heartening, both for medicine and for democracy itself. David Colquhoun. Declaration of interests. I was A.J. Clark chair of pharmacology at UCL, 1985 – 2004. 1. Aronson, JK BMJ 2009;339:b5415 2. Clark, A,J, (1938) Patent Medicines FACT series 14, London. See also Patent medicines in 1938 and now https://www.dcscience.net/?p=257 3. David Clark “Alfred Joseph Clark, A Memoir” (C. & J. Clark Ltd 1985 ISBN 0-9510401-0-3) 4. Lewis, A. (2007) The Gentle Art of Homeopathic Killing 5. A.J. Clark (1927) The historical aspect of quackery, BMJ October 1st 1927 6. Chrastina, D (2007) Quantum theory isn’t that weak, (response to Lionel Milgrom). 7 Goldacre, B. (2008) Bad Science. HarperCollins 8. Skills for Health web site 9. A very bad report: gamma minus for the vice-chancellor 10. A Patients’ Guide to Magic Medicine, and also in the Financial Times. 12. NICE fiasco, part 2. Rawlins should withdraw guidance and start again 13. BBC news 1 December 2009 Prince Charles: ‘Herbal medicine must be regulated’. 14. Oliver Wendell Holmes (1842) Homeopathy and Its Kindred Delusions. 15. House of Commons Science and technology committee. Evidence check: homeopathy. Videos and transcripts available at http://www.viewista.com/s/fywlp2/ez/1 16. Goldacre, B. A Kind of Magic Guardian 16 November 2007. 17. Homeopathy is resources drain says |
Follow-up
There is a good account of the third SCITECH session by clinical science consultant, Majikthyse, at The Three Amigos.
16 December 2009.. Recorded an interview for BBC Radio 5 Live. It was supposed to go out early on 17th.
17 December 2009. The editorial is mentioned in Editor’s Choice, by deputy editor Tony Delamothe. I love his way of putting the problem "too many at the top of British medicine seem frozen in the headlights of the complementary medicine bandwagon". He sounds remarkably kind given that I was awarded (by the editor, Fiona Godlee, no less) a sort of booby prize at the BMJ party for having generated a record number of emails during the editing of a single editorial (was it really 24?). Hey ho.
17 December 2009. More information on very direct political meddling by the Prince of Wales in today’s Guardian, and in Press Association report.
17 December 2009. Daily Telegraph reports on the editorial, under the heading “ ‘Nonsense’ alternative medicines should not be regulated“. Not a bad account for a non-health journalist.
17 December 2009. Good coverage in the excellent US blog, Neurologica, by the superb Steven Novella.’ “Intrepid, Ragged Band of Bloggers” take on CAM‘ provides a chance to compare and contrast the problems in the UK and the USA.’
18 December 2009. Article in The Times by former special advisor, Paul Richards. “The influence of Prince Charles the lobbyist is out of hand. Our deference stops us asking questions.”
“A good starting point might be publication of all correspondence over the past 30 years. Then we will know the extent, and influence, of Prince Charles the lobbyist.”
Comments in the BMJ Quite a lot of comments had appeared by January 8th, though sadly they were mostly from the usual suspects who appear every time one suggests evidence matters. A reply was called for, so I sent this (the version below has links).
After a long delay, this response eventually appeared in the BMJ on January 15 2010.
It’s good to see so many responses, though somewhat alarming to see that several of them seem to expect an editorial to provide a complete review of the literature. I ‘ll be happy to provide references for any assertion that I made.
I also find it a bit odd that some people think that an editorial is not the place to express an opinion robustly. That view seems to me to be a manifestation of the very sort of political correctness that I was deploring. It’s a bit like the case when the then health minister, Lord Hunt, referred to psychic surgery as a “profession” when he should have called it a fraudulent conjuring trick. Anything I write is very mild compared with what Thomas Wakley wrote in the Lancet, a journal which he founded around the time UCL came into existence. For example (I quote)
“[We deplore the] “state of society which allows various sets of mercenary, goose-brained monopolists and charlatans to usurp the highest privileges…. This is the canker-worm which eats into the heart of the medical body.” Wakley, T. The Lancet 1838-9, 1
I don’t think it is worth replying to people who cite Jacques Benveniste or Andrew Wakefield as authorities. Neither is it worth replying to people who raise the straw man argument about wicked pharmaceutical companies (about which I am on record as being as angry as anyone). But I would like to reply directly to some of the more coherent comments.
Sam Lewis and Robert Watson. [comment] Thank you for putting so succinctly what I was trying to say.
Peter Fisher [comment]. I have a lot of sympathy for Peter Fisher. He has attempted to do some good trials of homeopathy (they mostly had negative outcomes). He said he was "very angry" when the non-medical homeopaths were caught out recommending their sugar pills for malaria prevention (not that this as stopped such dangerous claims which are still commonplace). He agreed with me that there was not sufficient scientific basis for BSc degrees in homeopathy. I suppose that it isn’t really surprising that he continues to cherry pick the evidence. As clinical director of the Royal London Homeopathic Hospital and Homeopathic physician to the Queen, just imagine the cognitive dissonance that would result if he were to admit publicly that is all placebo after all. He has come close though. His (negative) trial for homeopathic treatment of rheumatoid arthritis included the words "It seems more important to define if homeopathists can genuinely control patients’ symptoms and less relevant to have concerns about whether this is due to a ‘genuine’ effect or to influencing the placebo response” [2]. [download
the paper]. When it comes to malaria, it matters a lot.
Adrian White [comment] seems to be cross because I cited my own blog. I did that simply because if he follows the links there he will find the evidence. In the case of acupuncture it has been shown time after time that "real" acupuncture does not differ perceptibly from sham. That is true whether the sham consists of retractable needles or real needles in the "wrong" places. A non-blind comparison between acupuncture and no acupuncture usually shows some advantage for the former but it is, on average, too small to be of much clinical significance [3]. I agree that there is no way to be sure that this advantage is purely placebo effect but since it is small and transient it really doesn’t matter much. Nobody has put it more clearly than Barker Bausell in his book, Snake Oil Science [4]
White also seems to have great faith in peer review. I agree that in real science it is probably the best system we have. But in alternative medicine journals the "peers" are usually other true believers in whatever hocus pocus is being promoted and peer reveiw breaks down altogether.
R. M. Pittilo [comment] I’m glad that Professor Pittilo has replied in person because I did single out his report for particular criticism. I agree that his report said that NHS funding should be available to CAM only where there is evidence of efficacy. That was not my criticism. My point was that in his report, the evidence for efficacy was assessed by representatives of Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Every one of them would have been out of work if they had found their subjects were nonsense and that, no doubt, explains why the assessment was so bad. To be fair, they did admit that the evidence was not all that it might be and recommended (as always) more research I’d like to ask Professor Pittilo how much money should be spent on more research in the light of the fact that over a billion dollars has been spent in the USA on CAM research without producing a single useful treatment. Pittilo says "My own view is that both statutory regulation and the quest for evidence should proceed together" but he seems to neglect the possibility that the quest for evidence might fail. Experience in the USA suggests that is exactly what has, to a large extent, already happened.
I also find it quite absurd that the Pittilo report should recommend, despite a half-hearted admission that the evidence is poor, that entry to these subjects should be via BSc Honours degrees. In any case he is already thwarted in that ambition because universities are closing down degrees in these subjects having realised that the time to run a degree is after, not before, you have some evidence that the subject is not nonsense. I hope that in due course Professor Pittilo may take the same action about the courses in things like homeopathy that are run by the university of which he is vice-chancellor. That could only enhance the academic reputation of Robert Gordon’s University.
George Lewith [comment] You must be aware that the proposed regulatory body, the Health Professions Council, has already broken its own rules about "evidence-based practice" by agreeing to take on, if asked, practitioners of Herbal Medicine, Chinese Medicine and Acupuncture. They have (shamefully) excluded the idea that claims of efficacy would be regulated. In other word they propose to provide exactly the sort of pseudo-regulation which would endanger patients They are accustomed to the idea that regulation is to do only with censoring practitioners who are caught in bed with patients. However meritorious that may be, it is not the main problem with pseudo-medicine, an area in which they have no experience. I’m equally surprised that Lewith should recommend that Chinese evaluation of Traditional Chinese medicine should be included in meta-analyses, in view of the well-known fact that 99% of evaluations from China are positive: “No trial published in China or Russia/USSR found a test treatment to be ineffective” [5]. He must surely realise that medicine in China is a branch of politics. In fact the whole resurgence in Chinese medicine and acupuncture in post-war times has less to do with ancient traditions than with Chinese nationalism, in particular the wish of Mao Tse-Tung to provide the appearance of health care for the masses (though it is reported that he himself preferred Western Medicine).
1. Lord Hunt thinks “psychic surgery” is a “profession”. https://www.dcscience.net/?p=258
2. Fisher, P. Scott, DL. 2001 Rheumatology 40, 1052 – 1055. [pdf file]
3. Madsen et al, BMJ 2009;338:a3115 [pdf file]
4. R, Barker Bausell, Snake Oil Science, Oxford University Press, 2007
5. Vickers, Niraj, Goyal, Harland and Rees (1998, Controlled Clinical Trials, 19, 159-166) “Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials”. [pdf file]
15 January 2010. During the SciTech hearings, Kent Woods (CEO of the MHRA) made a very feeble attempt to defend the MHRA’s decision to allow misleading labelling of homeopathic products. Now they have published their justification for this claim. It is truly pathetic, as explained by Martin at LayScience: New Evidence Reveals the MHRA’s Farcical Approach to Homeopathy. This mis-labelling cause a great outcry in 2006, as documented in The MHRA breaks its founding principle: it is an intellectual disgrace, and Learned Societies speak out against CAM, and the MHRA.
22 January 2010 Very glad to see that the minister himself has chosen to respond in the BMJ to the editorial
|
Rt Hon. Mike O’Brien QC MP, Minister of State for Health Services I am glad that David Colquhoun was entertained by my appearance before the Health Select Committee on Homeopathy. But he is mistaken when he says, “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense.” Regulation is about patient safety. Acupuncture, herbal and traditional Chinese medicine involve piercing the skin and/or the ingestion of potentially harmful substances and present a possible risk to patients. The Pittilo Report recommends statutory regulation and we have recently held a public consultation on whether this is a sensible way forward. Further research into the efficacy of therapies such as Homeopathy is unlikely to settle the debate, such is the controversy surrounding the subject. That is why the Department of Health’s policy towards complementary and alternative medicines is neutral. Whether I personally think Homeopathy is nonsense or not is besides the point. As a Minister, I do not decide the correct treatment for patients. Doctors do that. I do not propose on this occasion to interfere in the doctor-patient relationship. |
Here is my response to the minister
|
I am very glad that the minister himself has replied. I think he is wrong in two ways, one relatively trivial but one very important. First, he is wrong to refer to homeopathy as controversial. It is not. It is quite the daftest for the common forms of magic medicine and essentially no informed person believes a word of it. Of course, as minister, he is free to ignore scientific advice, just as the Home Secretary did recently. But he should admit that that is what he is doing, and not hide behind the (imagined) controversy. Second, and far more importantly, he is wrong, dangerously wrong, to say it I was mistaken to claim that “you cannot start to think about a sensible form of regulation unless you first decide whether or not the thing you are trying to regulate is nonsense". According to that view it would make sense to grant statutory regulation to voodoo and astrology. The Pittilo proposals would involve giving honours degrees in nonsense if one took the minister’s view that it doesn’t matter whether the subjects are nonsense or not. Surely he isn’t advocating that? The minister is also wrong to suppose that regulation, in the form proposed by Pittilo, would do anything to help patient safety. Indeed there is a good case to be made that it would endanger patients (not to mention endangering tigers and bears). The reason for that is that the main danger to patients arises from patients being given “remedies” that don’t work. The proposed regulatory body, the Health Professions Council, has already declared that it is not interested in whether the treatments work or not. That in itself endangers patients. In the case of Traditional Chinese Medicine, there is also a danger to patients from contaminated medicines. The HPC is not competent to deal with that either. It is the job of the MHRA and/or Trading Standards. There are much better methods of ensuring patient safety that those proposed by Pittilo. In order to see the harm that can result from statutory regulation, it is necessary only to look at the General Chiropractic Council. Attention was focussed on chiropractic when the British Chiropractic Association decided, foolishly, to sue Simon Singh for defamation. That led to close inspection of the strength of the evidence for their claims to benefit conditions like infant colic and asthma. The evidence turned out to be pathetic, and the result was that something like 600 complaints were made to the GCC about the making of false health claims (including two against practices run by the chair of the GCC himself). The processing of these complaints is still in progress, but what is absolutely clear is that the statutory regulatory body, the GCC, had done nothing to discourage these false claims. On the contrary it had perpetrated them itself. No doubt the HPC would be similarly engulfed in complaints if the Pittilo proposals went ahead. It is one thing to say that the government chooses to pay for things like homeopathy, despite it being known that they are only placebos, because some patients like them. It is quite another thing to endanger patient safety by advocating government endorsement in the form of statutory regulation, of treatments that don’t work. I would be very happy to meet the minister to discuss the problems involved in ensuring patient safety. He has seen herbalists and other with vested interests. He has been lobbied by the Prince of Wales. Perhaps it is time he listened to the views of scientists too. |
Both the minister’s response, and my reply, were reformatted to appear as letters in the print edition of the BMJ, as well as comments on the web..
Two weeks left to stop the Department of Health making a fool of itself. Email your response to tne Pittilo consultation to this email address HRDListening@dh.gsi.gov.uk
I’ve had permission to post a submission that has been sent to the Pittilo consultation. The whole document can be downloaded here. I have removed the name of the author. It is written by the person who has made some excellent contributions to this blog under the pseudonym "Allo V Psycho".
The document is a model of clarity, and it ends with constructive suggestions for forms of regulation that will, unlike the Pittilo proposals, really protect patients
Here is the summary. The full document explains each point in detail.
|
Executive Summary
Instead, safe regulation of alternative practitioners should be through:
|
The first two recommendations for effective regulation are much the same as mine, but the the third one is interesting. The problem with the Cancer Act (1939), and with the Unfair Trading regulations, is that they are applied very erratically. They are the responsibility of local Trading Standards offices, who have, as a rule, neither the expertise nor the time to enforce them effectively. A Health Advertising Standards Authority could perhaps take over the role of enforcing existing laws. But it should be an authority with teeth. It should have the ability to prosecute. The existing Advertising Standards Authority produces, on the whole, excellent judgements but it is quite ineffective because it can do very little.
A letter from an acupuncturist
I had a remarkable letter recently from someone who actually practises acupuncture. Here are some extracts.
|
“I very much enjoy reading your Improbable Science blog. It’s great to see good old-fashioned logic being applied incisively to the murk and spin that passes for government “thinking” these days.” “It’s interesting that the British Acupuncture Council are in favour of statutory regulation. The reason is, as you have pointed out, that this will confer a respectability on them, and will be used as a lever to try to get NHS funding for acupuncture. Indeed, the BAcC’s mission statement includes a line “To contribute to the development of healthcare policy both now and in the future”, which is a huge joke when they clearly haven’t got the remotest idea about the issues involved.” “Before anything is decided on statutory regulation, the British Acupuncture Council is trying to get a Royal Charter. If this is achieved, it will be seen as a significant boost to their respectability and, by implication, the validity of state-funded acupuncture. The argument will be that if Physios and O.T.s are Chartered and safe to work in the NHS, then why should Chartered Acupuncturists be treated differently? A postal vote of 2,700 BAcC members is under-way now and they are being urged to vote “yes”. The fact that the Privy Council are even considering it, is surprising when the BAcC does not even meet the requirement that the institution should have a minimum of 5000 members (http://www.privy-council.org.uk/output/Page45.asp). Chartered status is seen as a significant stepping-stone in strengthening their negotiating hand in the run-up to statutory regulation.” “Whatever the efficacy of acupuncture, I would hate to see scarce NHS resources spent on well-meaning, but frequently gormless acupuncturists when there’s no money for the increasing costs of medical technology or proven life-saving pharmaceuticals.” “The fact that universities are handing out a science degree in acupuncture is a testament to how devalued tertiary education has become since my day. An acupuncture degree cannot be called “scientific” in any normal sense of the term. The truth is that most acupuncturists have a poor understanding of the form of TCM taught in P.R.China, and hang on to a confused grasp of oriental concepts mixed in with a bit of New Age philosophy and trendy nutritional/life-coach advice that you see trotted out by journalists in the women’s weeklies. This casual eclectic approach is accompanied by a complete lack of intellectual rigour. My view is that acupuncturists might help people who have not been helped by NHS interventions, but, in my experience, it has very little to do with the application of a proven set of clinical principles (alternative or otherwise). Some patients experience remission of symptoms and I’m sure that is, in part, bound up with the psychosomatic effects of good listening, and non-judgemental kindness. In that respect, the woolly-minded thinking of most traditional acupuncturists doesn’t really matter, they’re relatively harmless and well-meaning, a bit like hair-dressers. But just because you trust your hairdresser, it doesn’t mean hairdressers deserve the Privy Council’s Royal Charter or that they need to be regulated by the government because their clients are somehow supposedly “vulnerable”.” |
Earlier postings on the Pittilo recommendations
A very bad report: gamma minus for the vice-chancellor https://www.dcscience.net/?p=235
Article in The Times (blame subeditor for the horrid title)
http://www.timesonline.co.uk/tol/comment/columnists/guest_contributors/article4628938.ece
Some follow up on The Times piece
https://www.dcscience.net/?p=251
The Health Professions Council breaks its own rules: the result is nonsense
https://www.dcscience.net/?p=1284
Chinese medicine -acupuncture gobbledygook revealed
https://www.dcscience.net/?p=1950
Consultation opens on the Pittilo report: help top stop the Department of Health making a fool of itself https://www.dcscience.net/?p=2007
Why degrees in Chinese medicine are a danger to patients https://www.dcscience.net/?p=2043
One month to stop the Department of Health endorsing quackery. The Pittilo questionnaire, https://www.dcscience.net/?p=2310
Follow-up
Chiropractors are getting very touchy indeed, all over the world. And no wonder, because their claims are being exposed as baseless as never before, in the wake of their attempts to stifle criticism by legal action..
In March, Shaun Holt appeared on Breakfast TV in New Zealand. Holt has done a lot of good work on TV in debunking some of the preposterous claims made by quacks. See him on YouTube.
This time he talked about chiropractic. Here is the video.
One could argue that he was over generous to chiropractic, especially when talking about their effectiveness in treating low back pain. He said, quite rightly, that chiropractors are no better than physiotherapists at treating low back pain.
But a recent trial suggests that neither are much good. “A randomised controlled trial of spinal manipulative therapy in acute low back pain” (Juni et al., 2009 in the BMJ; see also coverage in Pulse). This trial compared standard care with standard care plus spinal manipulative therapy (SMT). The results were negative, despite the fact that this sort of A + B vs B design is inherently biassed in favour of the treatment (see A trial design that generates only ”positive” results, Ernst & Lee 2008, Postgrad Med J.).
"SMT was performed by a specialist in manual medicine, chiropractice and rheumatology (GH), a specialist in physical medicine (DV) or an osteopath (RvB), all proficient in SMT."
"Conclusions: SMT is unlikely to result in relevant early pain reduction in patients with acute low back pain."
Admittedly, the trial was quite small (104 patients, 52 in each group) so it will need to be confirmed. but the result is entirely in line with what we knew already.
It also adds to the evidence that the recommendation by NICE of SMT by chiropractors constitutes their biggest failure ever to assess evidence properly. If NICE don’t amend this advice soon, they are in danger of damaging their hitherto excellent record.
Despite the moderate tone and accuracy of what Holt said on TV, the New Zealand Chiropractors’ Association made a formal complaint. That is what they like to do, as I learned recently, to my cost. It is so much easier than producing evidence.
Quite absurdly the New Zealand Broadcasting Standards Authority (BSA) has upheld some of the complaints. Their judgement can be read here.
The BSA consists of four people, two lawyers and two journalists. So not a trace of scientific expertise among them. Having people like that judging the claims of chiropractors makes as much sense as having them judged by Mr Justice Eady. They seem to be the sort of people who think that if there is a disagreement, the truth must lie half-way between the opposing views.
One of the BSA members, Tapu Misa, has used her newspaper column to quote approvingly the views of the notorious Dr Mercola web site on flu prevention “Your best defence, it says, is to eat right, get lots of sleep, avoid sugar and stress, load up on garlic, Vitamin D and krill oil”. (Snake oil is said to be good too.) There are some odd attitudes to science in some of her other columns too (e.g. here and here). Not quite the person to be judging the evidence for and against chiropractic, I think.
In fact the TV show in question was more than fair to chiropractors. It adopted the media’s usual interpretation of fair and balanced: equal time for the flat earthers. A Chiropractor was invited to reply to Holt’s piece. Here he is.
The chiropractor, Doug Blackbourn, started very plausibly, though a tendency to omit every third syllable made transcription hard work. He established that if you cut yourself you get better (without any help). He established that nerves run down the spinal cord. So far, so good. But then he quickly moved on to the usual flights of fancy.
"We have two premises. The body heals itself and the nervous system runs the body. Now the nervous system runs the body, travels down through the spinal cord so chiropractic is not based on the belief that, you know, energy flows, it’s based on the fact that your nervous system runs the body and [inaudible] affects the overall health of the body"
This statement is totally vague. It has nothing whatsoever to do with the main question, can chiropractors do anything useful. It is sheer flannel.
We’re seeing people, heck, diabetes. I had a quadriplegic come in one time for adjustment, we’ve got stroke people, we’ve got all sorts of conditions. We’re not treating the condition, We’re allowing, checking the spine to see if there’s any interference there that will slow the body down"
“Interference”? “slowing the body down”? These are utterly meaningless phrases that simply serve to distract from the only question that matters.
"Chiropractice is the most safest [sic] profession to go to to get your spine adjusted"
Hmm I thought it was the only job that uses the word ‘adjustment’.
Worst of all was his response to a question about asthma.
Presenter: "So chiropractors are not out there claiming they will cure asthma for example?". Chiropractor: "No"
This is simply untrue, both in New Zealand and in the UK. For a start, just look at what Blackbourn’s own web site says about asthma.
"The challenge, of course, with allergy and asthma medication is there is no end-point. There is no cure. Asthma and allergies, for the most part, are lifelong conditions requiring lifelong medication. Might there be a better way, an alternative solution?
“Alternative” is the key word. Medical treatment is designed to combat symptoms, and is successful to a certain extent with allergies and asthma. Underlying causes are not addressed, however, and symptoms continue year after year. What else might be done?
Enter chiropractic care. Chiropractic health care, with its unique comprehensive approach, is able to offer positive benefit to a variety of conditions and ailments. In the case of allergies and asthma, these “hypersensitivity conditions” may respond well to therapy designed to normalize the body’s flow of nerve signals. To use a metaphor, chiropractic treatment removes roadblocks to the body’s natural healing abilities. Restoring these imbalances may help reduce such hypersensitivity reactions."
Blackbourn’s web site describes him thus
"As a Doctor of Chiropractic, Dr. Doug Blackbourn . . ."
But the qualifications of “Dr” Blackbourn are B.App.Sc (Chiro) M.N.Z.C.A , the same as those of “Dr” Brian Kelly.
After a performance like this, perhaps someone should submit a complaint to the New Zealand Broadcasting Standards Authority.
After all, I notice that they have dismissed complaints from one chiropractor, Sean Parker, after a TV programme looked at the business practices of his private chiropractic practice, The Spinal Health Foundation. Perhaps the BSA understands business better than it understands science.
Follow-up
Is chiropractic crumbling in New Zealand? The New Zealand College of Chiropractic featured in my editorial in the New Zealand Medical Journal, and in the fallout from that article, It’s principle, “Dr” Brian Kelly (B App Sci (Chiro)) seems to be getting desperate. His college is now canvassing for recruits in Canada. They are promised all the woo.
- Subluxation centered techniques – Gonstead, Toggle Recoil, Thompson, Diversified
- Traditional philosophy featuring vitalism and innate healing – congruent curriculum
Perhaps Canada is a good place to recruit, gven the $500 million class action being brought against chiropractors in Canada, after Sandra Nette became tetraplegic immediately after a chiropractor manipulated her neck, Canadian chiropractors must be looking for somewhere to hide.
Stuff and Nonsense. jdc described this story at the time the complaint was lodged.
Shaun Holt’s own blog follows the action.
New Zealand Doctor covers the story.
Bay of Plenty Times “Bay researcher slams television complaint ruling“
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
This post has been translated into Belorussian..
Chinese medicine and herbal medicine are in the news at the moment. There is a real risk that the government could endorse them by accepting the Pittilo report.
In my view traditional Chinese medicine endangers people. The proposed ‘regulation’ would do nothing to protect the public. Quite on the contrary, it would add to the dangers, by giving an official stamp of approval while doing nothing for safety.
The government’s idea of improving safety is to make sure that practitioners are ‘properly trained’. But it is the qualifications that cause the danger in the first place. The courses teach ideas that are plain wrong and often really dangerous.
Why have government (and some universities) not noticed this? That’s easy to see. Governments, quangos and university validation committees simply don’t look. They tick boxes but never ask what actually goes on. Here’s some examples of what goes on for them to think about. They show clearly the sort of dangerous rubbish that is taught on some of these ‘degrees’.
These particular slides are from the University of Westminster, but similar courses exist in only too many other places. Watch this space for more details on courses at Edinburgh Napier University, Middlesex University and the University of East London
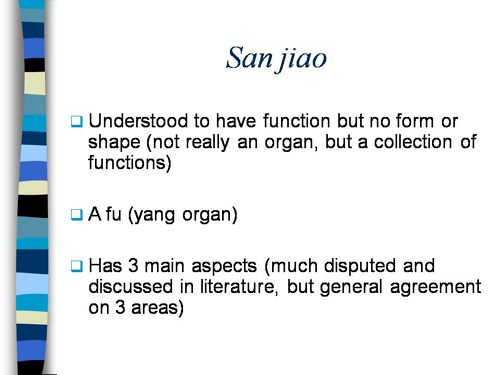
Just a lot of old myths. Sheer gobbledygook,
SO much for a couple of centuries of physiology,
It gets worse.
Plain wrong.
Curious indeed. The fantasy gobbledygook gets worse.
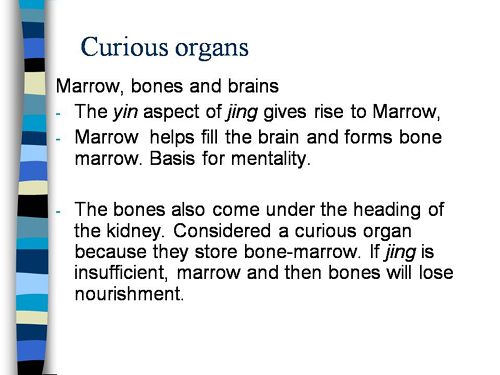
Now it is getting utterly silly. Teaching students that the brain is made of marrow is not just absurd, but desperately dangerous for anyone unlucky (or stupid) enough to go to such a person when they are ill.
Here’s another herbal lecture., and this time the topic is serious. Cancer.
Herbal approaches for patients with cancer.
I’ve removed the name of the teacher to spare her the acute embarrassment of having these dangerous fantasies revealed. The fact that she probably believes them is not a sufficient excuse for endangering the public. There is certainly no excuse for the university allowing this stuff to be taught as part of a BSc (Hons).
First get them scared with some bad statistics.
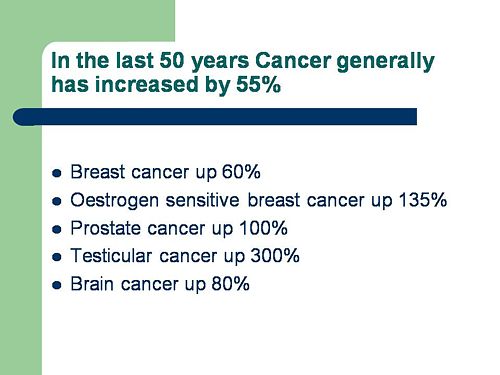
No fuss there about distinguishing incidence, age-standardisation and death rates. And no reference. Perhaps a reference to the simple explanation of statistics at Cancer Research UK might help? Perhaps this slide would have been better (from CDC). Seems there is some mistake in slide 2.
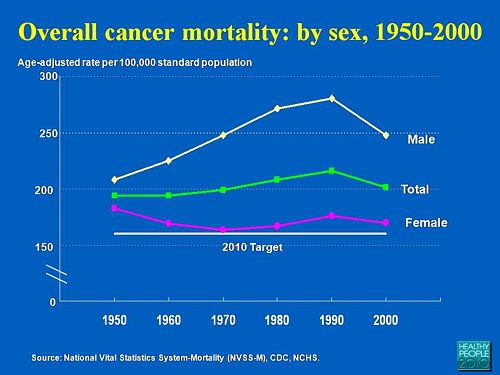
Straight on to a truly disgraceful statement in slide 3
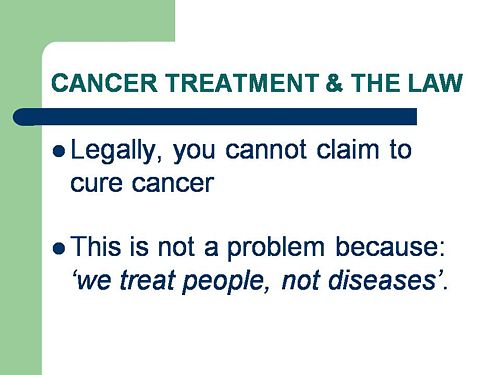
The is outrageous and very possibly illegal under the Cancer Act (1939). It certainly poses a huge danger to patients. It is a direct incentive to make illegal, and untrue claims by using weasel words in an attempt to stay just on the right side of the law. But that, of course, is standard practice in alternative medicine,
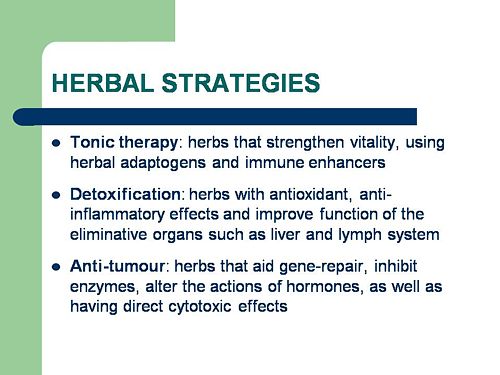
Slide 11 is mostly meaningless. “Strengthen vitality” sounds good but means nothing. And “enhancing the immune system” is what alternative medicine folks always say when they can think of nothing else. Its meaning is ill-defined and there is no reason to think that any herbs do it.
The idea of a ‘tonic’ was actually quite common in real medicine in the 1950s. The term slowly vanished as it was realised that it was a figment of the imagination. In the fantasy world of alternative medicine, it lives on.
Detoxification, a marketing term not a medical one, has been extensively debunked quite recently. The use of the word by The Prince of Wales’ company, Duchy Originals recently fell foul of the Advertising Standards Authority, and his herbal ‘remedies’ were zapped by the MHRA (Medicines and Health Regulatory Authority).
And of course the antioxidant myth is a long-disproved hypothesis that has become a mere marketing term.
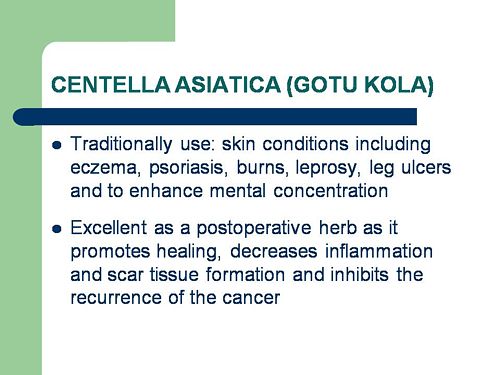
“Inhibits the recurrence of cancer”! That sounds terrific. But if it is so good why is it not even mentioned in the two main resources for information about herbs?
In the UK we have the National Library for Health Complementary and Alternative Medicine Specialist Library (NeLCAM), now a part of NHS Evidence. It was launched in 2006. The clinical lead was none other than Peter Fisher, clinical director of the Royal London Homeopathic Hospital, and the Queen’s homeopathic physician. The library was developed with the School of Integrated Health at the University of Westminster (where this particular slide was shown to undergraduates). Nobody could accuse these people of being hostile to magic medicine,
It seems odd, then, that NeLCAM does not seem to thnk to think that Centella asiatica, is even worth mentioning.
In the USA we have the National Center for Alternative and Complementary Medicine (NCCAM), an organisation that is so friendly to alternative medicine that it has spent a billion dollars on research in the area, though it has produced not a single good treatment for that vast expenditure. But NCCAM too does not even mention Centella asiatica in its herb list. It does get a mention in Cochrane reviews but only as a cosmetic cream and as an unproven treatment for poor venous circulation in the legs.
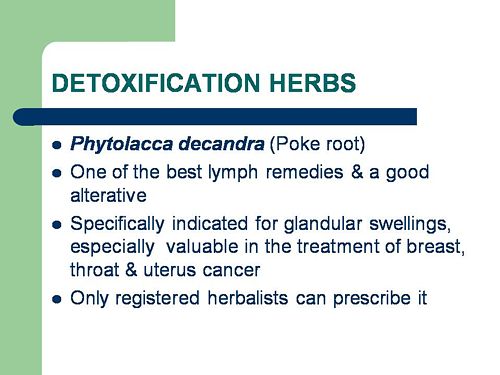
What on earth is a “lymph remedy”. Just another marketing term?
“especially valuable in the treatment of breast, throat and uterus cancer.“
That is a very dramatic claim. It as as though the hapless students were being tutored in doublespeak. What is meant by “especially valuable in the treatment of”? Clearly a desperate patient would interpret those words as meaning that there was at least a chance of a cure. That would be a wicked deception because there isn’t the slightest reason to think it works. Once again there this wondrous cure is not even mentioned in either NELCAM or NCCAM. Phytolacca is mentioned, as Pokeweed, in Wikipedia but no claims are mentioned even there. And it isn’t mentioned in Cochrane reviews either. The dramatic claims are utterly unfounded.
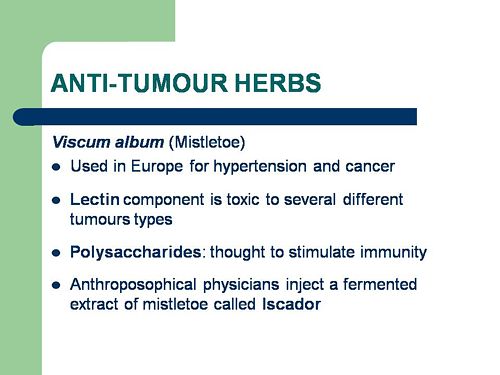
Ah the mistletoe story, again.
NHS Evidence (NeLCAM) lists three completed assessments. One concludes that more research is needed. Another concludes that “Rigorous trials of mistletoe extracts fail to demonstrate efficacy of this therapy”, and the third says “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
NCCAM says of mistletoe
- More than 30 human studies using mistletoe to treat cancer have been done since the early 1960s, but major weaknesses in many of these have raised doubts about their findings (see Question 6).
- Very few bad side effects have been reported from the use of mistletoe extract, though mistletoe plants and berries are poisonous to humans (see Question 7).
- The U.S. Food and Drug Administration (FDA) has not approved mistletoe as a treatment for cancer or any other medical condition (see Question 8).
- The FDA does not allow injectable mistletoe to be imported, sold, or used except for clinical research (see Question 8).
Cochrane reviews lists several reviews of mistletoe with similar conclusions. For example “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
Anthroposophy is one of the highest grades of fantasy you can find. A post on that topic is in the works.
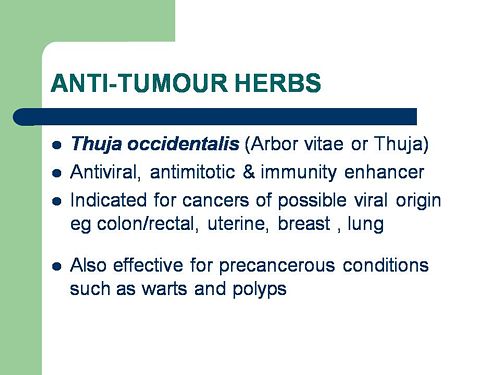
“Indicated for cancers . . . colon/rectal, uterine, breast, lung“. A cure for lung cancer? That, of course, depends on how you interpret the weasel words “indicated for”. Even Wikipedia makes no mention of any claims that Thuja benefits cancer. NHS Evidence (NeLCAM) doesn’t mention Thuja for any indication. Neither does NCCAM. Nor Cochrane reviews. That is not the impression the hapless students of this BSc lecture were given. In my view suggestions that you can cure lung cancer with this tree are just plain wicked.
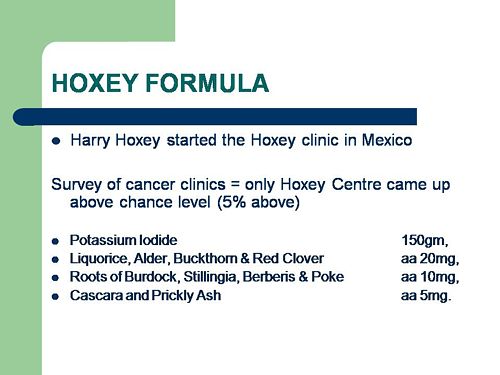
Pure snake oil, and not even spelled correctly, Harry Hoxsey’s treatment centres in the USA were closed by court order in the 1950s.
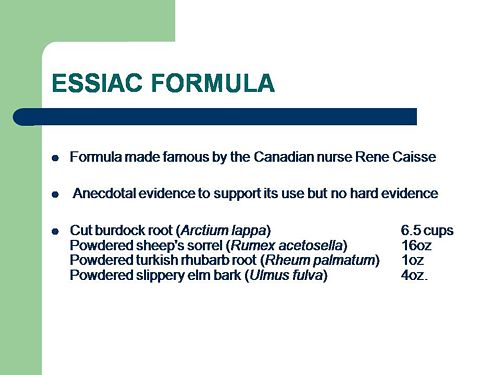
At least this time it is stated that there is no hard evidence to support this brand of snake oil.
More unfounded claims when it says “treated successfully many cancer patients”. No references and no data to support the claim. It is utterly unfounded and claims to the contrary endanger the public.
Gerson therapy is one of the most notorious and unpleasant of the quack cancer treatments. The Gerson Institute is on San Diego, but their clinics are in Mexico and Hungary. It is illegal in the USA. According to the American Cancer Society you get “a strict low-salt, low-fat, vegetarian diet and drinking juice from about twenty pounds of fresh fruits and vegetables each day. One glass of juice is consumed each hour, thirteen times a day. In addition, patients are given several coffee enemas each day. Various supplements, such as potassium, vitamin B12, pancreatic enzymes, thyroid hormone, and liver extracts, are used to stimulate organ function, particularly of the liver and thyroid.”. At one time you also got several glasses of raw calf liver every day but after infections killed several people] carrot juice was given instead.
Cancer Research UK says “there is no evidence to show that Gerson therapy works as a cure for cancer”, and “The Gerson diet can cause some very serious side effects.” Nobody (except perhaps the Price of Wales) has any belief in this unpleasant, toxic and expensive folk-lore.
Again patients are endangered by teaching this sort of stuff.
And finally, the usual swipe at vaccines. It’s nothing to do with herbalism. but just about every alternative medicine advocate seems to subscribe to the anti-vaccination lobby.. It is almost as though they have an active preference for things that are known to be wrong. They seem to believe that medicine and science are part of an enormous conspiracy to kill everyone.
Perhaps this dangerous propaganda might have been ameliorated if the students had been shown this slide (from a talk by Melinda Wharton).
Left to people like this, we would still have smallpox, diphtheria. tetanus and rabies, Take a look at Vaccine-preventable diseases.
This is the sort of ‘education’ which the Pittilo report wants to make compulsory.
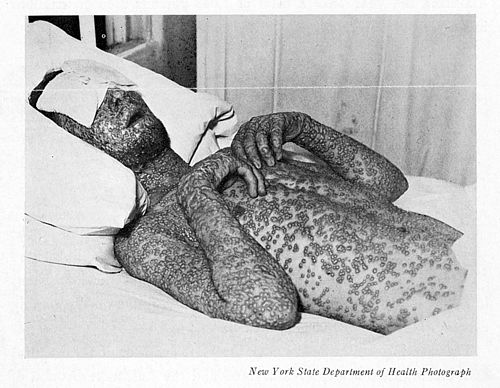
Smallpox in Baltimore, USA, 1939. This man was not vaccinated.
Conclusion
This selection of slides shows that much of the stuff taught in degrees in herbal medicine poses a real danger to public safety and to public health.
Pittilo’s idea that imposing this sort of miseducation will help safety is obviously and dangerously wrong. The Department of Health must reject the Pittilo recommendations on those grounds.