acupuncture
It was a great delight to visit Amsterdam on 25 October to speak at a meeting off the Vereniging tegen de Kwakzalverij (Society against quackery). Unfortunately their excellent web site is in Dutch, so the best you can do at the moment is to use the Google translation, with its frequently hilarious renderings. Better translations coming soon, I hope.
| Symposium
Niet-reguliere geneeswijzen in de 21ste eeuw in internationaal perspectief Non-mainstream medicine in the 21st century in an international perspective |
 |
The Dutch society has 1800 members and is the oldest and biggest such society in the world. I very much hope that their web site will soon have an English version. That is only appropriate since the origin of the word quack is from the Dutch Kwakzalver. (Kwak=Chatterer, salesman, zalf = salve, ointment). (In contrast the noise made by a duck is simply described by the OED as being “imitative”, though the great Michael Quinion thinks the two usages may be connected.

De Kwakzalver, Jan Steen (1626-1679) Rijksmuseum Amsterdam. Click to enlarge

The Quack doctor, Jan Steen (1626-1679). Click to enlarge
Translations of some key parts will be posted here soon. My talk was about Support for alternative medicine in government and universities in the U.K
The meeting started with the announcement of the winner of the Meester Kackadorisprijs.
The Master Kackodoris prize
The Meester Kackadorisprijs is awarded to individuals or institutions who promote quackery and who should know better (the quacks themselves are never nominated). The short list for the 2008 prize included the vice chancellor of the Free University of Amsterdam
| Prof. dr. Lex Bouter, rector magnificus Vrije Universiteit
The vice-chancellor was on the short-list for the prize because of his part in a recent paper, “Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: systematic review and meta-analysis.” (Manheimer E, Zhang G, Udoff L, Haramati A, Langenberg P, Berman BM, Bouter LM, Brit Med J 336, 545-9) [Available free] |
 |
This paper has been cited all over the world, but it seems not to have been very good. See for example the magnificent analysis of it in “Yawn, still one more overhyped acupuncture study: Does acupuncture help infertile women conceive?” . See also the Cochrane review (it could all be placebo). The fact that the vice-chancellor appears to have been only a ‘guest author’ anyway does not count as an excuse. The large number of citations received by this paper should, incidentally, be seen as another nail in the coffin of attempts to measure quality by citation rates.
In the event, vice-chancellor Bouter did not win the Kackodoris prize this year. In a speech at the start of the symposium, it emerged that he had been narrowly beaten by the Dutch Christian Radio Association for its assiduous promotion of quackery.
The chair of the Dutch society, Cees Rencken, is doing a great job. I hope that it will soon be better known outside the Netherlands.
And it’s time we had a UK equivalent of the Kackadoris prize. There will be no shortage of worthy candidates.
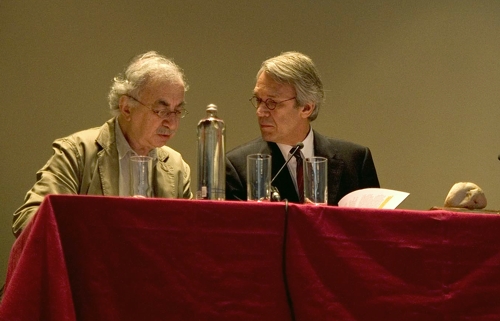
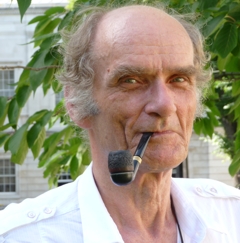
Frits Van Dam (Secretary) and Cees Renckens (Chair) of VtdK
(photo: Sofie van de Calseijde)

Some pictures of Amsterdam
(meetings photos: Sofie van de Calseijde)
Follow-up
It seems that validation committees often don’t look beyond the official documents. As a result, the validations may not be worth the paper they are written on. Try this one.


One of the best bits of news recently was the downfall of Matthias Rath. He’s the man who peddled vitamin pills for AIDS in Africa, and encouraged the AIDS denialists in the South African government. Thabo Mbeki and his Health Minister, Mrs Beetroot, have gone now, thank heavens.
Rath was one of the best illustrations of the murderous effect of selling ineffective treatments. The fact that nobody in the “nutritional therapy” industry has uttered a word of condemnation for this man illustrates better than anything one can imagine the corrupt state of “nutritional therapy”. The people who kept silent include the British Association of Nutritional Therapists (BANT).
It might be surprising, then, to find the Northern College of Acupuncture proudly adding a course in alternative nutrition to its courses in acupuncture (now known to be a theatrical placebo) and Chinese herbal medicine (largely untested and sometimes toxic). It might be even more surprising to find the boast that the course is validated by the University of Wales. It seemed a good idea to find out a bit more about how this came about. Thanks to the Freedom of Information Act, some interesting things can be discovered.
Polly Toynbee’s superb article, Quackery and superstition – available soon on the NHS, written in January 2008, mentioned diplomas and degrees in complementary therapies offered by, among others, the University of Wales. This elicited a letter of protest to Toynbee from the Vice-Chancellor of the University of Wales, Professor Marc Clement BSc, PhD, MInstP, CEng,CPhys,FIET. He invited her to visit the university to see their “validation and monitoring procedures (including the University’s very specific guidelines on health studies disciplines”.
So let’s take a look at these validation procedures and guidelines.
The validation process
The Northern College of Acupuncture submitted a 148 page proposal for the course in October 2007. The document has all the usual edu-bollocks jargon, but of course doesn’t say much about clinical trials, though it does boast about an unblinded trial of acupuncture published in 2006 which, because of lack of appropriate controls, served only to muddy the waters. : This submission was considered by the University’s validation committee last December.
|
The whole validation document is only four pages long [download it]. The most interesting thing about it is that the words ‘evidence’ or ‘critical’ do not occur in it a single time. It has all the usual bureaucratic jargon of such documents but misses entirely the central point.
Does that mean that the University of Wales doesn’t care about evidence or critical thinking? Well, not on paper. Two years previously a short document called Health Studies Guidelines had been written by Dr Brian Spriggs (Health Studies Validation Consultant, since retired) for the Health Studies Committee, and it was approved on 21 April 2005. It starts well.
“Degrees in the Health Studies field are expected to promote an understanding of the importance of the scientific method and an evidence-base to underpin therapeutic interventions and of research to expand that base.”
It even goes on to say that a BSc degree in homeopathy is “unacceptable”. Don’t get too excited though, because it also says that acupuncture and Chinese herbal stuff is quite OK. How anyone can imagine they live up to the opening sentence beats me. And it gets worse. It says that all sorts of rather advanced forms of battiness are OK if they form only part of another degree. They include Homeopathy, Crystal therapy. Dowsing, Iridology; Kinesiology, Radionics, Reflexology, Shiatsu, Healing, and Maharishi Ayurvedic Medicine.
Dowsing? Crystal therapy? Just let me remind you. We are living in 2008. It is easy to forget that when ploughing through all this new age junk.
The Validation Handbook of Quality Assurance: Health Studies (2007) runs to an astonishing 256 pages [download the whole thing]. On page 12 we find the extent of the problem.
“The University of Wales validates a number of schemes in the Health Studies field. At the current time we have undergraduate and/or postgraduate degree schemes in Acupuncture, Animal Manipulation, Chiropractic, Herbal Medicine, Integrative Psychotherapy, Osteopathy, Osteopathic Studies, Traditional Chinese Medicine and Regulatory Affairs, both in the UK and overseas.”
That sounds pretty shocking. Further down on page 12, though, we find this.
“Degrees in the Health Studies field are expected to promote an understanding of the importance of the scientific method and an evidence-base to underpin therapeutic interventions and of research to expand that base. The mission is to promote and require the critical evaluation of the practices, doctrines, beliefs, theories and hypotheses that underlie the taught therapeutic measures of the discipline.”
They are indeed fine words. The problem is that I can detect no sign in the submission, nor in its consideration by the validation committee, that any attempt whatsoever was made to ensure that the course complied with these requirements.
The only sign of concern I could detect of any concern about the quality of what was being taught came in a minute to a meeting of the Health Studies Committee meeting on 24th April 2008.
“Members received a copy of an article entitled Quackery and superstition available soon on the NHS which appeared in The Guardian newspaper in January 2008, and a copy of the Vice- Chancellors response. Members agreed that this article was now historical but felt that if/when the issue were to arise again; the key matter of scientific rigour should be stressed. The Committee agreed that this was the most critical element of all degree schemes in the University of Wales portfolio of health studies schemes. It was felt it would be timely to re-examine the schemes within the portfolio as well as the guidelines for consideration of Health Studies schemes at the next meeting. The Committee might also decide that Institutions would be required to include literature reviews (as part of their validation submission) to provide evidence for their particular profession/philosophy. It was agreed that the guidelines would be a vital document in the consideration of new schemes and during preliminary visits to prospective Institutions. “
The Press Office had passed Polly Toynbee’s article to them. Curiously the Health Studies Committee dismissed it as “historical”, simply because it was written three months earlier. That is presumably “historical” in the sense that the public will have forgotten about it, rather than in the sense that the facts of the matter have changed since January. So, at least for the nutrition degree, Toynbee’s comments were simply brushed under the carpet.
After a few cosmetic changes of wording the validation was completed on 16th January 2008. For example the word “diagnosis” was removed in 43 places and “rewritten in terms of evaluation and assessment”. There was, needless to say, no indication that the change in wording would change anything in what was taught to students.
You may think that I am being a bit too harsh. Perhaps the course is just fine after all? The problem is that the submission and the reaction of the validation committee tell you next to nothing about what actually matters, and that is what is taught. There is only a vague outline of that in the submission (and part of it was redacted on the grounds that if it were made public somebody might copy ;it. Heaven forbid).
That is why I have to say, yet again, that this sort of validation exercise is not worth the paper it’s written on.
How can we find out a bit more? Very easily as it happens. Just Google. What matters is not so much formal course outlines but who teaches them.
The nutrition course
The title of the course is just “Nutrition”, not ‘Nutritional Therapy’ or ‘Alternative Nutrition’. That sounds quite respectable but a glance at the prospectus shows immediately that it is full-blown alternative medicine.
Already in July 2007, the glowing press releases for the course had attracted attention from the wonderfully investigative web site HolfordWatch. I see no sign that the validation committee was aware of this. But if not, why not? I would describe is as dereliction of academic duty.
“This pioneering course is unique in that it is firmly rooted in both Western nutritional science and naturopathic medicine and also covers concepts of nutrition within traditional Chinese, Japanese, Tibetan and Ayurvedic medicine.
This means that graduates will gain comprehensive understanding of both modern scientific knowledge and ancient wisdom concerning nutrition and dietetics.”
Ancient wisdom, of course, means something that your are supposed to believe though there is no good reason to think it’s true. In the end, though, almost the only thing that really matters about any course is who is running it. The brochure shows that all of the people are heavily into every form of alternative nuttiness.
Course Director and Tutor: Jacqueline Young nutritionist, naturopath, clinical psychologist and Oriental medical practitioner
Nutrition Tutors:
Elaine Aldred (qualified as a chiropractor with the Anglo European Chiropractic College, as an acupuncturist with the British College of Acupuncture and as a Western Medical Herbalist with the College of Phytotherapy. She recently also qualified in Chinese herbal medicine with the Northern College of Acupuncture.)
Sue Russell (3 year diploma in nutritional therapy at the Institute of Optimum Nutrition. She currently practises as a nutritional therapist and also works part-time as a manager at the Northern College of Homeopathic Medicine.)
Anuradha Sharma (graduated as a dietician from Leeds Metropolitan University in 2002 and subsequently completed a Naturopathy certificate and a post-graduate diploma in acupuncture).
Guest Lecturers include : Dr John Briffa, Professor Jane Plant, M.B.E. (a geochemist turned quack), and, most revealingly, none other than the UK’s most notorious media celebrity and pill peddler, Patrick Holford.
So much has been written about Holford’s appalling abuse of science, one would have thought that not even a validation committee could have missed it.
“The course has been created by Jacqueline Young“, so let’s look a bit further at her track record.
Jacqueline Young has written a book, ‘Complementary Medicine for Dummies’ [Ed: ahem shouldn’t that be Dummies for Complementary Medicine?]. You can see parts of it on Google Books. Did the validation committee bother to look at it? As far as I can tell, the words ‘randomised’ or ‘clinical trial’ occur nowhere in the book.
The chapter on Tibetan medicine is not very helpful when it comes to evidence but for research we are referred to the Tibetan Medical and Astrology Institute. Guess what? That site gives no evidence either. So far not a single university has endorsed Astrology (there is a profitable niche there for some vice-chancellor).
Here are few samples from the book. The advice seems to vary from the undocumented optimism of this
Well researched? No. Safe? Nobody knows. Or this
Mandarin peel prevents colds and flu? Old wive’s tale. Then there are things that verge on the weird, like this one
or the deeply bizarre like this
The problem of Jacqueline Young’s fantasy approach to facts was pointed out at least as far back as 2004, by Ray Girvan., who wrote about it again in May 2005. The problems were brought to wider attention when Ben Goldacre wrote two articles in his Badscience column, Imploding Researchers (September 2005), and the following week, Tangled Webs.
“we were pondering the ethics and wisdom of Jacqueline Young dishing out preposterous, made-up, pseudoscientific nonsense as if it was authoritative BBC fact, with phrases such as: “Implosion researchers have found that if water is put through a spiral its electrical field changes and it then appears to have a potent, restorative effect on cells.” “
and later
“Take this from her article on cranial osteopathy, riddled with half truths: “Sutherland found that the cranial bones (the skull bones encasing the brain) weren’t fused in adulthood, as was widely believed, but actually had a cycle of slight involuntary movement.” In fact the cranial bones do fuse in adulthood.
She goes on: “This movement was influenced by the rhythmic flow of cerebrospinal fluid (the nourishing and protective fluid that circulates through the spinal canal and brain) and could become blocked.” There have now been five studies on whether “cranial osteopaths” can indeed feel these movements, as they claim, and it’s an easy experiment to do: ask a couple of cranial osteopaths to write down the frequency of the rhythmic pulses on the same person’s skull, and see if they give the same answer. They don’t. A rather crucial well-replicated finding to leave out of your story.
That was in 2005 and since then all of Young’s “preposterous, made-up, pseudoscientific nonsense” (along with most of the other stuff about junk medicine) has vanished from the BBC’s web site, after some people with a bit of common sense pointed out what nonsense it was. But now we see them resurfacing in a course validated by a serious university. The BBC had some excuse (after all, it is run largely by arts graduates). I can see no excuses for the University of Wales.
Incidentally, thanks to web archive you can still read Young’s nonsense, long after the BBC removed it. Here is a quotation.
“Implosion researchers have found that if water is put through a spiral its ,field changes and it then appears to have a potent, restorative effect on cells. In one study, seedlings watered with spiralised water grew significantly faster, higher and stronger than those given ordinary water.”
The vice-chancellor of the University of Wales, Marc Clement, is a physicist (Department of Electrical and Electronic Engineering), so can he perhaps explain the meaning of this?
Selection committees for jobs (especially senior jobs) and validation committees for courses, might make fewer mistakes if they didn’t rely so much on formal documents and did a little more investigation themselves. That sort of thing is why the managerial culture not only takes a lot more time, but also gives a worse result.
It would have taken 10 minutes with Google to find out about Young’s track record, but they didn’t bother. As a result they have spent a long time producing a validation that isn’t worth the paper it’s written on. That makes the University of Wales a bit of a laughing stock. Worse still, it brings science itself into disrepute.
Follow-up
What does the University of Wales say? So far, nothing. Last week I sent brief and polite emails to Professor Palastanga and to Professor Clement to try to discover whether it is true that the validation process had indeed missed the fact that the course organiser’s writings had been described as “preposterous, made-up, pseudoscientific nonsense” in the Guardian.
So far I have had no reply from the vice-chancellor, but on .26 October I did get an answer from Prof Palastaga.
| As regards the two people you asked questions about – J.Young – I personally am not familiar with her book and nobody on the validation panel raised any concerns about it. As for P.Holford similarly there were no concerns expressed about him or his work. In both cases we would have considered their CV’s as presented in the documentation as part of the teaching team. In my experience of conducting degree validations at over 16 UK Universities this is the normal practice of a validation panel. |
I have to say this reply confirms my worst fears. Validation committees such as this one simply don’t do their duty. They don’t show the curiosity that is needed to discover the facts about the things that they are meant to be judging. How could they not have looked at the book by the very person that they are validating? After all that has been written about Patrick Holford, it is simply mind-boggling that the committee seems to have been quite unaware of any of it.
It is yet another example of the harm done to science by an unthinking, box-ticking approach.
Pharmacology. A Handbook for Complementary Healthcare Professionals
Elsevier were kind enough to send me an inspection copy of this book, which is written by one of the nutrition course tutors, Elaine Aldred. She admits that pharmacology is “considered by most students to be nothing more that a ‘hoop-jumping’ exercise in the process of becoming qualified”. She also says. disarmingly. that “I was certainly not the most adept scientist at school and found my university course a trial”.
The book has all the feel of a cut and paste job. It is mostly very simple (if not simplistic). though for no obvious reason it starts with a long (and very amateur) discussion of chemical bonding Then molecules are admitted to be indivisible (but, guess what, the subject of homeopathy is avoided). There is a very short section on ion channels, though, bizarrely, it appears under the heading “How do drugs get into cells?”. Since the author is clearly not able to make the distinction between volts and coulombs, the discussion is more likely to confuse the reader than to help.
Then a long section on plants. It starts of by asserting that “approximately a quarter of prescription drugs contain at least one chemical that was originally isolated and extracted from a plant”.. This cannot be even remotely correct. There are vast tables showing complicated chemical structures, but the usual inadequate
list of their alleged actions This is followed by a quick gallop through some classes of conventional drugs, illustrated again mainly by chemical structures not data. Hormone replacement therapy is mentioned, but the chance to point out that it is one of the best illustrations of the need for RCTs is missed.
The one thing that one would really like to see in such a book is a good account of how you tell whether or not a drug works in man. This is relegated to five pages at the end of the book, and it is, frankly, pathetic. It
is utterly uncritical in the one area that matters more than any other for people who purport to treat patients. All you get is a list of unexplained bullet points.
If this book is the source of the “scientific content” of the nutrition course, things are as bad as we feared.
We know all about the sixteen or so universities that run “BSc” degrees in hokum. They are all “post-1992” universities, which used to be polytechnics. That is one reason why it saddens me to see them destroying their own attempts to achieve parity with older universities by running courses that I would regard as plain dishonest.
Older universities do not run degree courses in such nonsense. Academics (insofar as they still have any influence) certainly would not put up with it if they tried. But nevertheless you can find quackery in some of the most respected universities, and it gets there not via academics but (guess what) via Human Resources. It creeps in through two routes. One is the “training courses” that research staff now have to do (the “Roberts agenda”). The other route is through occupational health services.
Quackery in training courses
It isn’t easy to find out what happens elsewhere, but I was certainly surprised to find out that UCL’s own HR department was offering a course that promised to teach you the “core principles” of Brain Gym and Neurolinguistic Programming, both totally discredited bits of psycho-babble, more appropriate to the lifestyle section of a downmarket.women’s magazine than a university. I gather that HR’s reaction after I brought this to light was not to ask what was wrong with it, but just to get angry.
In a spirit of collegiality I offered to run a transferable skills course myself. I even offered to do it for nothing (rather than the rumoured £700 per day charged by the life style consultants). I proposed a course in ‘How to read critically’ (subtitle ‘How to detect bullshit’). This seems to me to be the ultimate transferable skill. Bullshit occurs in every walk of life. My proposal was moderately worded and perfectly serious.
Guess what? Despite several reminders, I have never had any response to my suggestion. Well, I suppose that HR people now regard themselves as senior to mere professors and there is really no need to reply to their
letters.
Quackery in occupational health. Leicester sets a good example
If you work at a university, why not search the university’s web site for “complementary medicice” or complementary therapies”. If it is a real university, you won’t find any degrees in homeopathy, or in amethysts
that emit high yin energy. But some quite surprising places are found to be recommending magic medicine through their Occupational Health service, which usually seems to be part of HR. In fact at one time even UCL was doing it, but no soon had somebody sent me the link than it disappeared. As a matter of historical record, you can see it here (it had all the usual junk, as well as harmless stuff like yoga and pilates).
While looking for something else I stumbled recently some other cases. One was at the University of Leicester, a very good university (and alma mater to the great David Attenborough who must have done more to point out the beauty of science than just about anyone). But we find on their staff wellbeing site, alongside some perfectly sensible stuff, a link to complementary therapies.
The list of ‘therapies’ includes not only the usual placebos, acupuncture, reiki, reflexology, but, even more exotically, a fraudulent Russian device called SCENAR therapy. They have a nice leaflet that explains all these things in words that run the whole gamut from meaningless gobbledygook to plain wrong. Here are some examples from the leaflet.
Reflexology
“In the feet, there are reflex areas corresponding to all the parts of the body and these areas are arranged in such a way as to form a map of the body in the feet”
Reflexology has been shown to be effective for:
- Back Pain
- Migraine
- Infertility
- Arthritis
Well no, there are no such areas in your feet. That is sheer imagination. And reflexology has not “been shown to be effective” for any of those conditions. These claims for therapeutic efficacy are not only lies. They are also illegal.
“Reiki
Each hand position is held for a few minutes, and during this time healing energy will flow into you, balancing your energy system, releasing stress, soothing pain, and promoting your body’s natural ability to heal itself.”
This is sheer idiotic mumbo-jumbo. The “flow of healing energy” is totally imaginary. Such talk is offensive to anyone with half a brain. Insofar as they claim to heal anything, it is also illegal. The comes SCENAR.
“What is SCENAR?
SCENAR is an acronym for Self Controlled Energo- Neuro Adaptive Regulator. It is a reflex biofeedback device which when used by a qualified practitioner, can help to alleviate acute and chronic pain. It is licensed in the UK for pain relief but experience has shown that it is helpful in a wide variety of conditions.”
This is even more seriously nuts than the others. The term “licensed” means merely that it is electrically safe. It certainly does not mean that it works. Pubmed shows only three publications about the SCENAR device, all in Russian,
One sales site (apparently Russian) makes the following modest claim.
“A prime goal of the Russian Space Program was to provide space travelers with a portable medical device that would become their “universal medical assistant” in space. So from the beginning, the SCENAR was designed to replace an entire medical hospital, with all its staff, diagnostic and treatment facilities, even the pharmacy. A universal, non-invasive, portable regulator of body functions (among other things) was envisaged.”
The SCENAR device (right) looks like a TV remote control (perhaps it IS a TV remote control -we aren’t anywhere told in comprehensible terms what’s in the box. The Russian site sells also the rather baffling accessory on the right. The mind boggles.

SCENAR device |

Remote rectal-vaginal electrode for SCENAR |
How does this rubbish get onto the web site of a good university?
I presume that it is just another sign of what happens when universities come to be run by non-academics. No doubt the occupational health people are well meaning and kind, but just scientifically illiterate. What about the HR person in charge of them? They are not known for scientific literacy either (which would not matter if they stuck to their job). But perhaps they just didn’t notice. There is only one way to find out. Ask. So I sent this letter.on 10th September.
| Hello
I am a pharmacologist and I have a side interest in public understanding of science, alternative medicine.and medical fraud I was quite surprised when Google led me unexpectedly to your complementary therapies page at http://www.le.ac.uk/staffwellbeing/complementary_therapy.html There is, sad to say, a great deal of information on these pages that is simply not true. For example it has NOT been shown that reflexology has been shown to be effective in any of the conditions which you list, as far as I know To take only one more example from this page, the SCENAR device is an even more extreme example. It is well known to be fraudulent. and has been investigated by the Washington State Attorney General. This sort of thing is not what one would expect from a very respectable university, and it must be a great embarrassment to your excellent medical scientists. Apart from the many scientific inaccuracies (which greatly impede the efforts of those of us who try to improve public understanding of science), you are, I hope, aware that there is a legal aspect. Since May this year, new regulations have made it illegal to make claims for health benefits if evidence cannot be produced to show that the claims are justified. I would like to put it to you that many of the claims made on this page are not only immoral, but also illegal. I wondered whether you , or your HR department, would like to make any comments Best regards David Colquhoun |
I got an immediate and very sympathetic response from the Director of HR and a week later, on17th September, he wrote
“Hi David,
I have discussed the matter with my manager of Staff Counselling and Welfare and have agreed that it is probably safest that we remove the references to ‘complimentary’[sic] therapies from the site entirely.
Thank you for your helpful input and the recommendations for reading matter.”
So there is a lesson here. If you find this sort or stuff on your own institution’s web site, all that may be needed is a simple letter that points out what nonsense it is. Admittedly the HR man seemed rather more worried about whether the claims were illegal than whether they were true, but either way, it worked.
Only one little snag. As of 6 October the pages still have not been removed.
On the assumption that they eventually will be removed, I have kept copies of the Wellbeing page, of the Complementary Therapies page, and of the ‘explanatory leaflet’. They stand as part of a historical record that
shows, once again, what can happen when scientific matters get into the hands of HR. Fortunately Leicester University has an HR director who is willing to listen to advice.
Follow-up
Something seems to have gone seriously wrong. Despite the rapid response, virtually all the nonsense is still there on 13th October. It seems not to be so simple after all.
And despite several reminders, the advertisement for SCENAR ‘therapy’ is still on the University web site on December 14th. I know that no decision by HR can be made with fewer than 25 meetings and an awayday in Majorca, but this is getting ridiculous.
After the announcement that the University of Central Lancashire (Uclan) was suspending its homeopathy “BSc” course, it seems that their vice chancellor has listened to the pressure, both internal and external, to stop bringing his university into disrepute.
An internal review of all their courses in alternative medicine was announced shortly after the course closure. Congratulations to Malcolm McVicar for grasping the nettle at last. Let’s hope other universities follow his example soon.
I have acquired, indirectly, a copy of the announcement of the welcome news.
| Homeopathy, Herbalism and cupuncture Concern has been expressed by some colleagues as to whether the University should offer courses in homeopathy, Herbalism and Acupuncture. Therefore, to facilitate proper discussion on this matter I have set up a working party to review the issues. I have asked Eileen Martin, Pro Vice-Chancellor and Dean of the Faculty of Health, to lead this working party and report to me as soon as possible. Whilst the review is taking place, we need to recognise that there are students and staff studying and teaching on these courses which have satisfied the University’s quality assurance procedures and been duly validated. I would therefore ask that colleagues would refrain from comment or speculation which would cause concern to these students and staff. Staff who wish to express their views on this issue should direct these to Eileen Martin, by the end of September. Regards Malcolm McVicar Vice-Chancellor |
Times Higher Education today reports
“The University of Central Lancashire is to review all its courses in homoeopathy, herbalism and acupuncture after some staff said it should not be offering degrees in “quackery”, Times Higher Education has learnt.
A university spokesman said: “As a university we value and practise transparency and tolerance and welcome all academic viewpoints.”
(Later, an almost identical version of the story ran on the Times Online.)
So far, so good. But of course the outcome of a committee depends entirely on who is appointed to it. Quite often such committees do no more than provide an internal whitewash.
It does seem a bit odd to appoint as chair the dean of the faculty where all these course are run, and presumably generate income. Eileen Martin has often appeared to be proud of them in the past. Furthermore, the whole investigation will (or should) turn on the assessment of evidence. It needs some knowledge of the design of clinical trials and their statistical analysis, As far as I can see, Ms Martin has essentially no research publications whatsoever.
I also worry about a bit about “satisfied the University’s quality assurance procedures and been duly validated”. One point of the investigation should be recognise frankly that the validation process is entirely circular, and consequently worth next to nothing. It must be hard for a vice-chancellor to admit that, but it will be an essential step in restoring confidence in Uclan.
Let’s not prejudge though. If there are enough good scientists on the committee, the result will be good.
I hope that transparency extends to letting us know who will be doing the judging. Everything depends on that.
Follow-up
Well well, there’s a coincidence, Once again, the week after a there is an announcement about degrees in witchcraft, what should pop up again in the column of the inimitable Laurie Taylor in THE. The University of Poppleton’s own Department of Palmistry.
| Letter to the editor
Dear Sir I was shocked to see yet another scurrilous attack upon the work of my department in The Poppletonian. Although Palmistry is in its early days as an academic discipline it cannot hope to progress while there are people like your correspondent who insist on referring to it as “a load of superstitious nonsense which doesn’t deserve a place on the end of the pier let alone in a university”. A large number of people claim to have derived considerable benefit from learning about life lines, head lines and heart lines and the role of the six major mounts in predicting their future. All of us in the Palmistry Department believe it vitally important that these claims are rigorously examined. How else can science advance? Yours sincerely, |
The Times today has given s good showing for my comment piece. It gives the case against following the advice of the Pittilo report. It simply makes no sense to have government regulation of acupuncture, herbal medicine, traditional Chinese medicine until such time as there is evidence that they work. It makes even less sense to have BSc degrees in them. The Department of Health should have more sense that to use the Prince of Wales as its scientific advisor.
Let’s hope that the recent example set by the University of Central Lancashire is the start of trend for vice-chancellors to appreciate that running such degrees brings their universities into disrepute.
I can only apologise for the dreadful title that The Times’ sub-editors put on the piece, My original title was
A bad report for the vice chancellor
The Pittilo report to the Department of Health will endanger the public and corrupt universities. There is a better way.
I like that much better than “Regulate quack nedicine? I feel sick”.
But, oh dear, the picture that I sent them is on the left, but what appeared is on the right. Spot the difference.
 |
 |
Well now, at least, I can feel I have something in common with Isambard Kingdom Brunel.
Follow-up
It so happens that Professor Pittilo wrote a letter to Times Higher Education this week. I fear that it provided a yet more evidence that he hasn’t really quite got the hang of evidence.
The Lancashire Evening Post catches up with the UCLan story, two days after you read it here.
A reply from Professor Pittilo
This response to the op-ed of 29th August appeared as a letter
in the Times on Sept 2.
| Public health needs protection
Regulation of acupuncture and herbal medicine has been subject to much scrutiny Sir, Professor Colquhoun’s campaign to discredit our report (“Regulate quack medicine? I feel sick,” Aug 29) is in danger of placing public health at risk. He is entitled to challenge existing evidence for the effectiveness of complementary and alternative medicine (CAM) but fails to acknowledge the key recommendation from the steering group on the essential need to demonstrate efficacy, safety and quality assurance as a prerequisite for NHS funding. Professor Colquhoun dismisses CAM because of the absence of a rigorous scientific foundation and he asserts that to teach and practise it is unethical. Survey data consistently demonstrates very high demand for CAM with one report estimating that 22 million visits involving 10.6 per cent of the population in England alone occurred in 2008. This demand is one reason why his alternative model of trade law enforcement will not work. He may argue that these people are uncritical recipients of nonsense, but data from the Medicines and Healthcare products Regulatory Agency confirm that they are at significant risk from poor practice. It is essential that we protect the public by implementing statutory regulation alongside demanding evidence of efficacy. Professor Colquhoun’s resistance to the teaching of science to CAM practitioners will do little to help them to critically evaluate effectiveness. Professor Michael Pittilo Chair of the Department of Health Steering Group |
And Pittilo wrote in similar vein to Times Higher Education.
Science vital to health study28 August 2008 Your feature on some members of staff at the University of Central Lancashire attacking science degrees in complementary and alternative medicine (“Staff attack science degrees in alternative health”, 7 August) raises a number of concerns. It is up to any university, taking account of the expert views of staff and external peer review, to determine the appropriate title and award for any degree. It is encouraging to note from the feature that new courses The recent report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and other Traditional Medicine There is no doubt that courses that provide a solid scientific foundation will greatly assist CAM practitioners in establishing evidence-based practice. It would be most unfortunate if the reported resistance to degree titles led to those wishing to practise acupuncture or herbal medicine receiving less hard science than they might have. To say that acupuncture and herbal medicine degrees have no academic justification appears arrogant in the extreme. Although it is certainly true that some content may not be scientific, this does not invalidate the legitimacy of these courses at degree level, a fact borne out by their successful validation in a number of universities. R. Michael Pittilo, Principal and vice-chancellor, The Robert Gordon University. |
This one got excellent responses from Kevin Smith (University of Abertay, Dundee), and from Peter J. Brophy (Professor of veterinary anatomy and cell biology University of Edinburgh). This was my comment to THE
There are a few very obvious responses to Professor Pittilo’s letter
For many alternative therapies the “philosophy” is simply incompatible with science. One obvious example is homeopathy. On Mondays and Wednesdays (science days) the students will be required to learn that response increases with dose. On Tuesdays and Thursdays will be taught the opposite. But for the exam they must reproduce only the latter (nonsensical) idea because their aim is to get a job as a homeopath. That makes nonsense of the idea of a university.
This seems to constitute a recognition that the evidence is still very inadequate. The time to start degrees, and the time to give official government recognition, is after the evidence is in, not before. What happens if you start degrees and then find that the subject is so much nonsense? Well, that has already happened in several areas of course. But the people who accredit the course and who act as external examiners just happen to be fervent believers in that nonsense, so all appears to be well (to bean counters anyway).
There is, as it happens, a great deal of evidence now about acupuncture, but the authors of the report do not seem to be aware of it. I recommend Barker Bausell’s book on the topic. If students are educated science, like what constitutes evidence, and our current understanding of words like “energy”, they would have to disavow the subject that there are supposed to training to practise
No, it is not a matter of arrogance, just a matter of careful attention to the evidence. Attention to evidence was notably absent in Prof Pittilo’s report, perhaps because his committee consisted entirely of people who earn their living from the subjects they were supposed to be assessing.
I have had the misfortune to have waded through a mound of such validation documents. The one thing they never consider is whether the treatment works. Sad to say, these validations are not worth the paper they are written on. |
The first major victory in the battle for the integrity of universities seems to have been won. This email was sent by Kate Chatfield who is module leader for the “BSc” in homeopathic medicine at the University of Central Lancashire (UCLAN).
| from Kate Chatfield…
Dear All, It’s a sad day for us here at UCLan because we have taken the decision not to run a first year this year due to low recruitment. The course will be put ‘on hold’ for this year and next until we see what happens with the general climate. Fortunately our masters course is thriving and we have been asked to focus upon this area and homeopathy research for the time being. Of late UCLan has been the subject of many attacks by the anti-homeopathy league. Colquhoun et al have kept the university lawyers and us quite fruitlessly busy by making claims for very detailed course information under the Freedom of Information Act. The latest demand is for 32 identified lesson plans with teaching notes, power points, handouts etc. The relentless attacks have taken their toll and it appears that they have won this small victory. The university has been very clear that this decision has been taken solely on the grounds of poor educational experience and is nothing to do with the current furore. They continue to be supportive of us and our efforts. Best wishes Kate and Jean |
There is some background here. In July 2006 I made a request to UCLAN under the Freedom of Information Act 2000, in which I asked to see some of their teaching materials. I appealed to UCLAN but Professor Patrick McGhee, Deputy Vice-Chancellor (Academic), also turned down two appeals. A letter sent directly to Professor Malcolm McVicar, vice-chancellor and president of UCLAN, failed to elicit the courtesy of a reply (standard practice I’m afraid, when a vice chancellor is faced with a difficult question). (Ironically, McVicar lists one of his interests as “health policy”.) So then I appealed to the Office of the Information Commissioner, in November 2006. Recently the case got to the top of the pile, and a judgment is expected any moment now.
Kate Chatfield’s letter to her colleagues is interesting. She describes a request ro see some of her teaching materials as an “attack”. If someone asks to see my teaching materials, I am rather flattered, and I send them. Is she not proud of what she teaches? Why all the secrecy? After all, you, the taxpayer, are paying for this stuff to be taught, so why should you not be able see it? Or is the problem that she feels that the “alternative reality” in which homeopaths live is just too complicated for mortals to grasp? Perhaps this attitude should be interpreted as flattering to the general public, because somewhere deep down she knows that the public will be able to spot gobbledygook when they see it. The revelation that the University of Westminster teaches first year undergraduates the “amethysts emit high yin energy” didn’t help their academic reputation much either.
Much credit for this decision must go also to the pressure from the many good academics at UCLAN. When it was revealed recently that UCLAN intended to open yet more courses in forms of medicine that are disproved or unproven, they naturally felt that their university was being brought into disrepute. Opposition to plans to introduce new “degrees” in acupuncture and Chinese herbal medicine were exposed in Times Higher Education recently. It particular, great credit must go to Dr Michael Eslea from UCLAN’s Psychology department. His open letter to his vice-chancellor is an example of scientific integrity in action.
The abandonment of this degree in medicines that contain no medicine is a small victory for common sense, for science and for the integrity of universities. Sadly, there is still a long way to go.
It is my understanding that ‘bringing the university into disrepute’ is a serious offence. Please note, vice-chancellor.
A few more judgments like that to suspend your homeopathy degree could work wonders for your reputation.
The follow-up
Watch this space.
The Guardian was quick off the mark -this story appeared on their education web site within 3 hours of my posting it “Homeopathy degrees suspended after criticism” by Anthea Lipsett. My comment there disappeared for a while because the Guardian legal people misunderstood the meaning of the last sentence. It’s back now, with blame allocated unambiguously to the vice-chancellors of the 16 or so universities who run this sort of course.
UCLAN’s web site seems to need some updating. The “BSc” in homeopathic medicine is still advertised there. as of 28 August.
UCLAN’s best ally. Dr Michael Eslea, has had some publicity for his attempts to rescue his university’s reputation. The story appeared in the “High Principals” column of Private Eye (Issue 1217, Aug 22, 2008). It also appeared in his local paper, the Lancashire Evening Post.
The Lancashire Evening Post catches up with homeopathy suspension story, two days after you read it here. But the UCLAN web site still advertises it.
My original piece on Integrative Baloney@Yale was posted on May 16th, after I got back from a visit there. The talk I gave there included a short video. My movie, Integrative baloney@Yale, was made entirely from clips taken from Yale’s own YouTube movies which showed something approaching three hours of its “1st Annual Scientific [sic] symposium”, entitled “Complementary and Alternative Medicine: Evidence for Integration”. I had merely interspersed a few titles to show the worst scientific absurdities of that rather pathetic event. YouTube removed the movie last week.
You can download the movie here [15.8 Mb, wmv file].
It should soon reappear on YouTube (actually it took over a month and several reminders, but eventually they kept their word in the end).
Yale’s lawyers had written to YouTube, to have my movie removed. I guess if you have no evidence, all you can do is resort to law to suppress the views of those who have the temerity to point out that the emperor is naked. Last week it was New Zealand Chiropractors’ Association Inc. This week the rather more substantial Yale University. We live in interesting times.
This is what I got on 15th August.
| Dear Member
This is to notify you that we have removed or disabled access to the following material as a result of a third-party notification by Yale University, Yale School of Medicine (CME) claiming that this material is infringing: Integrative baloney@Yale: http://uk.youtube.com/watch?v=HEl2fhfGBdI Please Note: Repeated incidents of copyright infringement will result in the deletion of your account and all videos uploaded to that account. In order to prevent this from happening |
If you clicked on the link you saw
“This video is no longer available due to a copyright claim by Yale University, Yale School of Medicine (CME)”
It seems that Yale’s Continuing Medical Education (CME) department was responsible.
Of course Yale is correct. I expect they own the copyright of their original movies, but they are not what I posted. I would argue that selecting 6 minutes from a 3 hour original amounts to “fair quotation”, no different from when one cites a short passage from somebody else’s book or paper. Perhaps Yale was just a bit jealous that my movie was getting viewed a lot more times than theirs. Or perhaps they were a bit peeved that a Google search for “Yale Integrative Medicine” produced my movie as #2 (add the word movie and I was #1).
My movie seems to me to be fair comment from someone who is a pharmacologist by trade. Apparently it didn’t seem that way to the apparatchiks of Yale Medical School, who seem to think that academic arguments should be settled by paying lawyers to suppress views they don’t like, rather than by rational discussion.
It’s interesting that the three hours of Yale’s own movie have also vanished from YouTube. Could that be because they realise that the remarks made at the meeting are so embarrassing intellectually that it would be better not to make them public? Actually, no.
What does Yale CME say?
Rather than publishing this straight away, I thought it better to delve a bit further into what had happened. I lodged an appeal with YouTube and I wrote to Ronald J. Vender, MD (Associate Dean, YSM Clinical Affairs, CMO, Yale Medical Group, Medical Director, Yale CME ). The outcome was rather interesting.
First, it turned out that the original posting of the three hours of the symposium proceedings on YouTube was itself unauthorised, which is why it suffered the same fate as my movie.
Dr Vender told me that he is new to the job, and didn’t know about the incident. What’s more surprising, he said he “did not know an Integrative Program even existed at Yale”. That does seem a bit odd indeed for an Associate Dean of Clinical Affairs.
However, Dr Vender turned out to be a very reasonable man,.After some amiable correspondence over the weekend, it took him only a day and a half to sort the matter out. After talking to Yale’s attorney, he wrote on 19th August, thus
“The University attorney believes that there is in fact a difference between the initial unauthorized filming of an entire conference as opposed to quoting from that conference. Therefore, she has agreed to withdraw the injunction that has been imposed on your use of the material. YouTube will be contacted.”
That’s good for me, but it isn’t the main thing. The movie would doubtless have been seen by more people if Yale had tried to maintain the ban. Much more impressively, Dr Vender also said
“As for this particular program, I will be speaking with Dr Belitsky and the program directors to encourage them to adopt a more critical view of the scientific basis for claims made by proponents of CAM. They will also be encouraged to develop a future program that includes faculty who have opposing points of view.”
It remains to be seen what actually happens, but so far, so good.
What next?
The removal of the original videos of the meeting is understandable because they were pretty embarrassing to Yale. But can that be the real reason? I was told that it is simply because their posting was “unauthorised”. But Yale Continuing Medical Education still boasts about the meeting on their own web site. They describe the meeting as “successful”, but if they are so proud of it, why remove the video from YouTube whether it was authorised or not? We are told
“The symposium, accredited for 7.5 AMA PRA Category 1 Credits, began what is hoped to be a long tradition at the Yale School of Medicine.”
They give credits for such miseducation?
Dr Katz’s phrase “we need a more fluid concept of evidence” now gets about 148 hits in Google, since I first helped him to publicise it.
Two of the six “learning objectives” that Yale CME lists for this symposium are particularly revealing.
- Describe therapeutic benefits and recent scientific evidence supporting a wide range of safe and practical complementary treatments, including acupuncture, massage, yoga, meditation, nutrition and exercise
- Identify and discuss barriers to CAM use, practice and research, as well as propose ways of overcoming these barriers
‘Describe the evidence supporting complementary treatments’? But don’t on any account describe the much more substantial evidence that does not support them? A question (or “learning objective”) put in this loaded way is the very antithesis of education.
Equally the second ‘learning objective’ carries with it the assumption that CAM works, otherwise why would anyone want to overcome the barriers to it?
This is indoctrination, not education. It betrays everything that a university should stand for.
Let’s hope the new head of CME, the admirable Dr Vender, succeeds in doing something about it
Follow-up
Success!. Well I think it is success. On 26 November 2008, the admirable Dr Vender wrote to me as follows.
“I do not know if another CAM/Integrative Medicine program is planned at Yale. However, based on the new ACCME standards, this program does not fulfil the standards for receiving CME accreditation (by my interpretation of the standards). At least one of last year’s program directors has been notified already.”
The article below is an editorial that I was asked to write for the New Zealand Medical Journal, as a comment on article in today’s edition about the misuse of the title ‘doctor’ by chiropractors [download pdf]. Titles are not the only form of deception used by chiropractors, so the article looks at some of the others too. For a good collection of articles that reveal chiropractic for what it is, look at Chirobase
THE NEW ZEALAND
MEDICAL JOURNAL
Journal of the New Zealand Medical Association
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716

URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Doctor Who?
Inappropriate use of titles by some alternative “medicine” practitioners
David Colquhoun
Who should use the title ‘doctor’? The title is widely abused as shown by Gilbey1 in this issue of the NZMJ in an article entitled Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. Meanwhile, Evans and colleagues 2, also in this issue, discuss usage and attitudes to alternative treatments.
Gilbey finds that the abuse of the title doctor is widespread and that chiropractors are the main culprits. An amazing 82% of 146 chiropractics used the title Doctor, andL most of them used the title to imply falsely that they were registered medical practitioners.
Although it is illegal in New Zealand to do that, it seems clear that the law is not being enforced and it is widely flouted. This is perhaps not surprising given the history of chiropractic. It has had a strong element of ruthless salesmanship since it was started in Davenport, Iowa by D.D. Palmer (1845–1913). His son, B.J. Palmer, said that their chiropractic school was founded on “a business, not a professional basis. We manufacture chiropractors. We teach them the idea and then we show them how to sell” (Shapiro 2008)3 It is the same now. You can buy advice on how to build “build high-volume, subluxation-based, cash-driven, lifetime family wellness practices”
In her recent book3 , Rose Shapiro comments on the founder of chiropractic as follows.
“By the 1890s Palmer had established a magnetic healing practice in Davenport, Iowa, and was styling himself “doctor”. Not everyone was convinced, as a piece about him in an 1894 edition of the local paper, the Davenport Leader, shows.
A crank on magnetism has a crazy notion hat he can cure the sick and crippled with his magnetic hands. His victims are the weak-minded, ignorant and superstitious,those foolish people who have been sick for years and have become tired of the regular physician and want health by the short-cut method he has certainly profited by the ignorance of his victim. His increase in business shows what can be done in Davenport, even by a quack.”
D.D. Palmer was a curious mixture: grocer, spiritual healer, magnetic therapist, fairground huckster, religious cult leader—and above all, a salesman. He finally found a way to get rich by removing entirely imaginary “subluxations”.
Over 100 years later, it seems that the “weak-minded, ignorant, and superstitious” include the UK’s Department of Health, who have given chiropractics a similar status to the General Medical Council.
The intellectual standards of a 19th Century Mid-Western provincial newspaper journalist are rather better than the intellectual standards of the UK’s Department of Health, and of several university vice-chancellors in 2007.
Do the treatments work?
Neither Gilbey nor Evans et al. really grasp the nettle of judging efficacy. The first thing one wants to know about any treatment —alternative or otherwise — is whether it works. Until that is decided, all talk of qualifications, regulation, and so on is just vacuous bureaucratese. No policy can be framed sensibly until the question of efficacy has been addressed honestly.
It is one good effect of the upsurge of interest in alternative treatments that there are now quite a lot of good trials of the most popular forms of treatments (as well as many more bad trials). Some good summaries of the results are now available too. Cochrane reviews set the standard for good assessment of evidence. New Zealand’s Ministry of Health commissioned the Complementary and Alternative Medicine
website to assess the evidence, and that seems to have done a good job too. Their assessment of chiropractic treatment of low back pain is as follows:
There appears to be some evidence from one systematic review and four other studies, although not conclusive, that chiropractic treatment is as effective as other therapies but this may be due to chance. There is very little evidence that chiropractic is more effective than other therapies.
And two excellent summaries have been published as books this year. Both are by people who have had direct experience of alternative treatments, but who have no financial interest in the outcome of their assessment of evidence. The book by Singh and Ernst4 summarises the evidence on all the major alternative treatments, and the book by Bausell5 concentrates particularly on acupuncture, because the author was for 5 years involved in research in that area, Both of these books come to much the same conclusion about chiropractic. It is now really very well-established that chiropractic is (at best) no more effective than conventional treatment. But it has the disadvantage of being surrounded by gobbledygook about “subluxations” and, more importantly, it kills the occasional patient.
Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
The chiropractors of Alberta (Canada) and the Alberta Government are now facing a class-action lawsuit8. The lead plaintiff is Sandra Nette. Formerly she was a fit 41 year old. Now she is tetraplegic. Immediately
after neck manipulation by a chiropractor she had a massive stroke as a result of a torn vertebral artery.
Acupuncture comes out of the assessments equally badly. Bausell (2007) concludes that it is no more than a theatrical placebo.
Are the qualifications even real?
It is a curious aspect of the alternative medicine industry that they often are keen to reject conventional science, yet they long for academic respectability. One aspect of this is claiming academic titles on the flimsiest of grounds. You can still be held to have misled the public into thinking you are a medical
practitioner, even if you have a real doctorate. But often pays to look into where the qualifications come from.
A celebrated case in the UK concerned the ‘lifestyle nutritionist’, TV celebrity and multi-millionaire, Dr Gillian McKeith, PhD. A reader of Ben Goldacre’s excellent blog, badscience.net did a little investigation. The results appeared in Goldacre’s Bad Science column in the Guardian9.
She claimed that her PhD came from the American College of Nutrition, but it turned out to come from a correspondence course from a non-accredited US ‘college’. McKeith also boasted of having “professional membership” of the American Association of Nutritional Consultants, for which she provided proof of her degree and three professional references.
The value of this qualification can be judged by the fact that Goldacre sent an application and $60 and as a result “My dead cat Hettie is also a “certified professional member” of the AANC. I have the certificate hanging in my loo”.
Is the solution government regulation?
In New Zealand the law about misleading the public into believing you are a medical practitioner already exists. The immediate problem would be solved if that law were taken seriously, but it seems that it is not.
It is common in both the UK and in New Zealand to suggest that some sort of official government regulation is the answer. That solution is proposed in this issue of NZMJ by Evans et al2. A similar thing has been proposed recently in the UK by a committee headed by Michael Pittilo, vice-chancellor of Robert Gordon’s University, Aberdeen.
I have written about the latter under the heading A very bad report. The Pittilo report recommends both government regulation and more degrees in alternative medicine. Given that we now know that most alternative medicine doesn’t work, the idea of giving degrees in such subjects must be quite ludicrous to any thinking person.
The magazine Nature7 recently investigated the 16 UK universities who run such degrees. In the UK, first-year students at the University of Westminster are taught that “amethysts emit high yin energy” . Their vice chancellor, Professor Geoffrey Petts, describes himself a s a geomorphologist, but he cannot be tempted to express an opinion about the curative power of amethysts.
There has been a tendency to a form of grade inflation in universities—higher degrees for less work gets bums on seats. For most of us, getting a doctorate involves at least 3 years of hard experimental research in a university. But in the USA and Canada you can get a ‘doctor of chiropractic’ degree and most chiropractic (mis)education is not even in a university but in separate colleges.
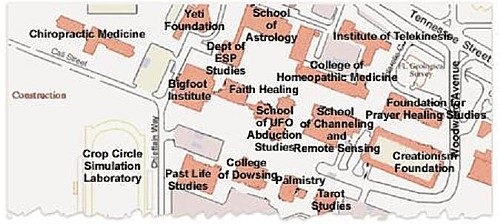
Florida State University famously turned down a large donation to start a chiropractic school because they saw, quite rightly, that to do so would damage their intellectual reputation. This map, now widely distributed on the Internet, was produced by one of their chemistry professors, and it did the trick.
Other universities have been less principled. The New Zealand College of Chiropractic [whose President styles himself “Dr Brian Kelly”,though his only qualification is B. App Sci (chiro)] is accredited by the New Zealand Qualifications Authority (NZQA). Presumably they, like their UK equivalent (the QAA), are not allowed to take into account whether what is being taught is nonsense or not. Nonsense courses are accredited by experts in nonsense. That is why much accreditation is not worth the paper it’s written on.
Of course the public needs some protection from dangerous or fraudulent practices, but that can be done better (and more cheaply) by simply enforcing existing legislation on unfair trade practices, and on false advertising. Recent changes in the law on unfair trading in the UK have made it easier to take legal action against people who make health claims that cannot be justified by evidence, and that seems the best
way to regulate medical charlatans.
Conclusion
For most forms of alternative medicine—including chiropractic and acupuncture—the evidence is now in. There is now better reason than ever before to believe that they are mostly elaborate placebos and, at best, no better than conventional treatments. It is about time that universities and governments recognised the evidence and stopped talking about regulation and accreditation.
Indeed, “falsely claiming that a product is able to cure illnesses, dysfunction, or malformations” is illegal in Europe10.
Making unjustified health claims is a particularly cruel form of unfair trading practice. It calls for prosecutions, not accreditation.
Competing interests: None.
NZMJ 25 July 2008, Vol 121 No 1278; ISSN 1175 8716
URL: http://www.nzma.org.nz/journal/121-1278/3158/ ©NZMA
Author information: David Colquhoun, Research Fellow, Dept of Pharmacology, University College London, United Kingdom (http://www.ucl.ac.uk/Pharmacology/dc.html)
Correspondence: Professor D Colquhoun, Dept of Pharmacology, University College London, Gower Street, London WC1E 6BT, United Kingdom. Fax: +44(0)20 76797298; email: d.colquhoun@ucl.ac.uk
References:
1. Gilbey A. Use of inappropriate titles by New Zealand practitioners of acupuncture, chiropractic, and osteopathy. N Z Med J. 2008;121(1278). [pdf]
2. Evans A, Duncan B, McHugh P, et al. Inpatients’ use, understanding, and attitudes towards traditional, complementary and alternative therapies at a provincial New Zealand hospital. N Z Med J. 2008;121(1278).
3 Shapiro. Rose. Suckers. How Alternative Medicine Makes Fools of Us All Random House, London 2008. (reviewed here)
4. Singh S, Ernst E. Trick or Treatment. Bantam Press; 2008 (reviewed here)
5. Bausell RB. Snake Oil Science. The Truth about Complementary and Alternative Medicine. (reviewed here)
Oxford University Press; 2007
6. Colquhoun D. Science degrees without the Science, Nature 2007;446:373–4. See also here.
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10.
8. Libin K. Chiropractors called to court. Canadian National Post; June21, 2008.
9. Goldacre B. A menace to science. London: Guardian; February 12, 2007/
10. Department for Business Enterprise & Regulatory Reform (BERR). Consumer Protection from Unfair Trading Regulations 2008. UK: Office of Fair Trading.
This, I fear, is pure plagiarism, Robert Shrimsley’s piece in today’s Financial Times was so funny that it just begged to be quoted. Here it is.
|
Surely this is a call to action. The news that Radovan Karadzic has been hiding out as some kind of homeopath has confirmed all prejudices about alternative medicine. I have had my doubts about this vicious breed ever since we were gulled into giving the kids valerian and hops to calm them down on an overnight flight and they went absolutely wild. Talk about a crime against humanity. Incidentally old Rad is not exactly an advert for homeopathy if this week’s photographs are anything to go by. Before he got into all this complementary healing, he was a sprightly, globally-feared warlord and international criminal. Now, after a decade of mixing his own marjoram, he is a strangely bearded hippy, blathering on about the need to nurture your inner self. Of course with hindsight health shops of the world were an obvious hiding place for genocidal maniacs. Remember all that talk of cleansing impurities? Well, I think we now know what that was all about. Some of you may be thinking that Karadzic was an aberration in an otherwise harmless community. But I ask you, how likely is it that the butcher of Belgrade could have kept up the pretence for so long without ever giving himself away. Were no suspicions aroused by the publication of his first book Radovan’s Remedies . Did no one notice that his patented treatment for stress prescribed ground echinacea root, essence of basil and the blood of a thousand Bosnians. Anyway, now that these collected homeopaths, herbologists and healers have finally been exposed as nothing more than a front organisation for the world’s most wanted, we will doubtless see swift action. How long can it be until the National Security Agency, operating undercover in Greenwich Village, finally pinpoints the precise location of Osama bin Laden’s reiki parlour? Crack teams of CIA operatives will surely be rounding up reflexologists in their search for Ratko Mladic. We can be confident that even now special rendition flights, crammed full of ayurvedic surgeons are en route to Guantánamo, where skilled interrogators will rearrange their chakras at no extra charge. Homeopaths will be forced to take two Disprins every four hours until they crack. US authorities have, however, pledged not to use the cruel practice of water-boarding – except perhaps on hydrotherapists. Of course we may snare a few, genuinely innocent aromatherapists on the way but as they say in the trade, you can’t make a poultice without grinding some ginger. |
During the last year, there has been a very welcome flurry of good and informative books about alternative medicine. They are all written in a style that requires little scientific background, even the one that is intended for medical students.
CAM, Cumming | Trick or Treatment | Snake Oil Science |
Testing treatments | Suckers | Healing, Hype or Harm
I’ll start with the bad one, which has not been mentioned on this blog before.
Complementary and Alternative medicine. An illustrated text.
by Allan D. Cumming, Karen R. Simpson and David Brown (and 12 others). 94 pages, Churchill Livingstone; 1 edition (8 Dec 2006).
| The authors of this book sound impressive
Allan Cumming, BSc(Hons), MBChB, MD, FRCP(E), Professor of Medical Education and Director of Undergraduate Learning and Teaching, and Honorary Consultant Physician, College of Medicine and Veterinary Medicine, University of Edinburgh, Edinburgh, UK; Karen Simpson, BA(Hons), RN, RNT, Fellow in Medical Education, College of Medicine and Veterinary Medicine David Brown, MBChB, DRCOG, General Practitioner, The Murrayfield Medical Centre, and Honorary Clinical Tutor, University of Edinburgh |
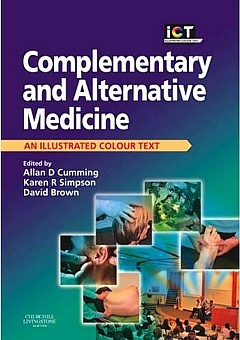 |
Sadly, this is a book so utterly stifled by political correctness that it ends up saying nothing useful at all. The slim volume is, I have to say, quite remarkably devoid of useful information. Partly that is a result of out-of-date and selective references (specially in the chapters written by alternative practitioners),
But the lack of information goes beyond the usual distortions and wishful thinking. I get the strong impression is that it results not so much for a strong commitment to alternative medicine (at least by Cumming) as from the fact that the first two authors are involved with medical education. It seems that they belong to that singularly barmy fringe of educationalists who hold that the teacher must not give information to s student for fear of imparting bias. Rather the student must be told how to find out the information themselves. There is just one little problem with this view. It would take about 200 years to graduate in medicine.
There is something that worries me about medical education specialists. Just look at the welcome given by Yale’s Dean of Medical Education, Richard Belitsky, to Yale’s own division of “fluid concepts of evidence”, as described at Integrative baloney @ Yale, and as featured on YouTube. There are a lot of cryptic allusions to alternative forms of evidence in Cumming’s book too, but nothing in enough detail to be useful to the reader.
What should a book about Alternative medicine tell you? My list would look something like this.
- Why people are so keen to deceive themselves about the efficacy of a treatment
- Why it is that are so often deceived into thinking that something works when it doesn’t
- How to tell whether a medicine works better than placebo or not,
- Summaries of the evidence concerning the efficacy and safety of the main types of alternative treatments.
The Cumming book contains chapters with titles like these. It asks most of the right questions, but fails to answer any of them. There is, time and time again, the usual pious talk about the importance of evidence, but then very little attempt to tell you what the evidence says. When an attempt is made to mention evidence, it is usually partial and out of date. Nowhere are you told clearly about the hazards that will be encountered when trying to find out whether a treatment works.
| The usual silly reflexology diagram is reproduced in Cumming’s introductory chapter, but with no comment at all, The fact that it is obviously total baloney is carefully hidden from the reader.. What is the poor medical student meant to think when they perceive that it is totally incompatible with all the physiology they have learned? No guidance is offered. | 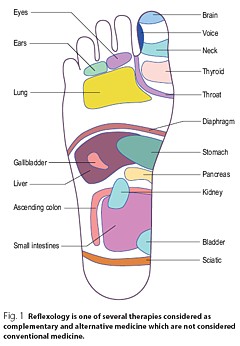 |
| You will look in vain for a decent account of how to do a good randomised controlled trial, though you do get a rather puerile cartoon, The chapter about evidence is written by a librarian. Since the question of evidence is crucial, this is a fatal omission. |  |
Despite the lack of presentation of evidence that any of it works, there seems to be an assumption throughout the book that is is desirable to integrate alternative medicine into clinical practice. In Cumming’s chapter (page 6) we see
Since it would not be in the interests of patients to integrate treatments that don’t work with treatments that do work, I see only two ways to explain this attitude. Either the authors have assumed than most alternative methods work (in which case they haven’t read the evidence), or they think integration is a good idea even if the treatment doesn’t work. Neither case strikes me as good medical education.
The early chapters are merely vague and uninformative. Some of the later chapters are simply a disgrace.
Most obviously the chapter on homeopathy is highly selective and inaccurate, That is hardly surprising because it is was written by Thomas Whitmarsh, a consultant physician at Glasgow Homeopathic Hospital (one that has still survived). It has all the usual religious zeal of the homeopath. I honestly don’t know whether people like Whitmarsh are incapable of understanding what constitutes evidence, or are simply too blinded by faith to even try. Since the only other possibility is that they are dishonest, I suppose it must be one of the former.
The chapter on “Nutritional therapy” is also written by a convert and is equally misleading piece of special pleading.
The same is true of the chapter on Prayer and Faith Healing. This chapter reproduces the header of the Cochrane Review on “Intercessory prayer for the alleviation of Ill Health”, but then proceeds to ignore entirely its conclusion “Most of the studies show no real differences”).
If you want to know about alternative medicine, don’t buy this book. Although this book was written for medical students, you will learn a great deal more from any of the following books, all of which were written for the general public.
Trick or Treatment
by Simon Singh and Edzard Ernst, Bantam Press, 2008
| Simon Singh is the author of many well-known science books, like Fermat’s Last Theorem. Edzard Ernst is the UK’s first professor of complementary and alternative medicine.
Ernst, unlike Cumming et. al is a real expert in alternative medicine. He practised it at an early stage in his career and has now devoted all his efforts to careful, fair and honest assessment of the evidence. That is what this book is about. It is a very good account of the subject and it should be read by everyone, and certainly by every medical student. |
 |
Singh and Ernst follow the sensible pattern laid out above, The first chapter goes in detail into how you distinguish truth from fiction (a little detail often forgotten in this area).
The authors argue, very convincingly, that the development of medicine during the 19th and 20th century depended very clearly on the acceptance of evidence not anecdote. There is a fascinating history of clinical trials, from James Lind (lemons and scurvy), John Snow and the Broad Street pump, Florence Nightingale’s contribution not just to hygiene, but also to the statistical analysis that was needed to demonstrate the strength of her conclusions (she became the first female member of the Royal Statistical Society, and had studied under Cayley and Sylvester, pioneers of matrix algebra).
There are detailed assessments of the evidence for acupuncture, homeopathy, chiropractic and herbalism, and shorter synopses for dozens of others. The assessments are fair, even generous in marginal cases.
Acupunture. Like the other good books (but not Cumming’s), it is pointed out that acupuncture in the West is not so much the product of ancient wisdom (which is usually wrong anyway), but rather a product of Chinese nationalist propaganda engineered by Mao Tse-tung after 1949. It spread to the West after Nixon’s visit Their fabricated demonstrations of open heart surgery under acupuncture have been known since the 70s but quite recently they managed again to deceive the BBC It was Singh who revealed the deception. The conclusion is ” . . . this chapter demonstrates that acupuncture is very likely to be acting as nothing more than a placebo . . . ”
Homeopathy. “hundreds of trials have failed to deliver significant or convincing evidence to support the use of homeopathy for the treatment of any particular ailment. On the contrary, it would be to say that there is a mountain of evidence to suggest that homeopathic remedies simply do not work”.
Chiropractic. Like the other good books (but not Cumming’s) there is a good account of the origins of chiropractic (see, especially, Suckers). D.D. Palmer, grocer, spiritual healer, magnetic therapist and fairground quack, finally found a way to get rich by removing entirely imaginary ‘subluxations’. They point out the dangers of chiropractic (the subject of court action), and they point out that physiotherapy is just as effective and safer.
Herbalism. There is a useful table that summarises the evidence. They conclude that a few work and most don’t Unlike homeopathy, there is nothing absurd about herbalism, but the evidence that most of them do any good is very thin indeed.
| “We argue that it is now the time for the tricks to stop, and for the real treatments to take priority. In the name of honesty, progress and good healthcare, we call for scientific standards, evaluation and regulation to be applied to all types of medicine, so that patients can be confident that they are receiving treatments that demonstrably generate more harm than good.” |
Snake Oil Science, The Truth about Complementary and Alternative Medicine.
R. Barker Bausell, Oxford University Press, 2007
Another wonderful book from someone who has been involved himself in acupuncture research, Bausell is a statistician and experimental designer who was Research Director of a Complementary and Alternative Medicine Specialised Research Center at the University of Maryland.
This book gives a superb account of how you find out the truth about medicines, and of how easy it is to be deceived about their efficacy.
I can’t do better than quote the review by Robert Park of the American Physical Society (his own book, Voodoo Science, is also excellent)
| “Hang up your lantern, Diogenes, an honest man has been found. Barker Bausell, a biostatistician, has stepped out of the shadows to give us an insider’s look at how clinical evidence is manipulated to package and market the placebo effect. Labeled as ‘Complementary and Alternative Medicine’, the placebo effect is being sold, not just to a gullible public, but to an increasing number of health professionals as well. Bausell knows every trick and explains each one in clear language” |  |
Bausell’s conclusion is stronger than that of Singh and Ernst.
“There is no compelling, credible scientific evidence to suggest that any CAM therapy benefits any medical condition or reduces any medical symptom (pain or otherwise) better than a placebo”.
Here are two quotations from Bausell that I love.
[Page 22] ” seriously doubt, however, that there is a traditional Chinese medicine practitioner anywhere who ever stopped performing acupuncture on an afflicted body in the presence of similarly definitive negative evidence. CAM therapists simply do not value (and most cases, in my experience, do not understand) the scientific process”
And even better,
[Page39] “But why should nonscientists care one iota about something as esoteric as causal inference? I believe that the answer to this question is because the making of causal inferences is part of our job description as Homo Sapiens.”
Testing Treatments: Better Research for Better Healthcare
by Imogen Evans, Hazel Thornton, Iain Chalmers, British Library, 15 May 2006
You don’t even need to pay for this excellent book (but buy it anyway, eg from Amazon). If you can’t afford, £15 then download it from the James Lind Library.
| This book is a unlike all the others, because it is barely mentions alternative medicine. What it does, and does very well, is to describe he harm that can be done to patients when they are treated on the basis of guesswork or ideology, rather than on the basis of proper tests. This, of course, is true whether or not the treatment is labelled ‘alternative’.
It is worth noting that one of the authors of this book is someone who has devoted much of his life to the honest assessement of evidence, Sir Iain Chalmers, one of the founders of the Cochrane Collaboration , and Editor of the James Lind Library . |
 |
A central theme is that randomised double blind trial are essentially the only way to be sure you have the right answer. One of the examples that the authors use to illustrate this is Hormone Replacement Therapy (HRT). For over 20 years, women were told that HRT would reduce their risk of heart attacks and strokes. But when, eventually, proper randomised trials were done, it was found that precisely the opposite was true. The lives of many women were cut short because the RCT had not been done,
The reason why the observational studies gave the wrong answer is pretty obvious. HRT was used predominantly by the wealthier and better-educated women. Income is just about the best predictor of longevity. The samples were biassed, and when a proper RCT was done it was revealed that the people who used HRT voluntarily lived longer despite the HRT, not because of it. It is worth remembering that there are very few RCTs that test the effects of diet. And diet differs a lot between rich and poor people. That, no doubt, is why there are so many conflicting recommendations about diet. And that is why “nutritional therapy” is little more than quackery. Sadly, the media just love crap epidemiology. One of the best discussions of this topics was in Radio 4 Programme. “The Rise of the Lifestyle Nutritionists“, by Ben Goldacre.
One of the big problems in all assessment is the influence of money, in other words corruption, The alternative industry is entirely corrupt of course, but the pharmaceutical industry has been increasingly bad. Testing Treatments reproduces this trenchant comment.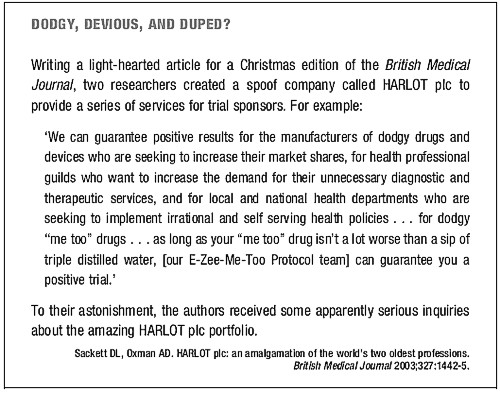
Suckers. How Alternative Medicine Makes Fools of Us All
Rose Shapiro, Random House, London 2008
| I love this book. It is well-researched, feisty and a thoroughly good read.
It was put well in the review by George Monbiot.
The chapters on osteopathy and chiropractic are particularly fascinating. |
 |
This passage describes the founder of the chiropractic religion.
“By the 1890s Palmer had established a magnetic healing practice in Davenport, Iowa, and was styling himself ‘doctor’. Not everyone was convinced as a piece about him in an 1894 edition of the local paper, the Davenport Leader, shows.”
A crank on magnetism has a crazy notion hat he can cure the sick and crippled with his magnetic hands. His victims are the eak-minded, ignorant and superstitious, those foolish people who have been sick for years and have become tired of the regular physician and want health by the short-cut method . . . he has certainly profited by the ignorance of his victims . . . His increase in business shows what can be done in Davenport, even by a quack”
Over 100 years later, it seems that the “weak-minded, ignorant and superstitious” include the UK’s Department of Health, who have given these quacks a similar status to the General Medical Council.
The intellectual standards of a 19th Century mid-western provincial newspaper leader writer are rather better than the intellectual standards of the Department of Health, and of several university vice-chancellors in 2007.
Healing Hype or Harm
Edited by Imprint Academic (1 Jun 2008)
Download the contents page
My own chapter in this compilation of essays, “Alternative medicine in UK Universities” is an extended version of what was published in Nature last year (I don’t use the term CAM because I don’t believe anything can be labelled ‘complementary’ until it has been shown to work). Download a copy if the corrected proof of this chapter (pdf).
| Perhaps the best two chapters, though, are “CAM and Politics” by Rose and Ernst, and “CAM in Court” by John Garrow.
CAM and politics gives us some horrifiying examples of the total ignorance of almost all politicians and civil servants about the scientific method (and their refusal to listen to anyone who does understand it). CAM in Court has some fascinating examples of prosecutions for defrauding the public. Recent changes in the law mean we may be seeing a lot more of these soon. Rational argument doesn’t work well very well with irrational people. But a few homeopaths in jail for killing people with malaria would probably be rather effective. |
 |
Follow-up
Healing, Hype or Harm has had some nice reviews, That isn’t so surprising from the excellent Harriet Hall at Science-Based Medicine. The introduction to my chapter was a fable about the replacemment of the Department of Physics and Astronomy by the new Department of Alternative Physics and Astrology. It was an unashamedly based on Laurie Taylor’e University of Poppleton column. Hall refers to it as “Crislip-style”, a new term to me. I guess the incomparable Laurie Taylor is not well-known in the USA, Luckily Hall gives a link to Mark Crislip’s lovely article, Alternative Flight,
“Americans want choice. Americans are increasingly using alternative aviation. A recent government study suggests that 75% of Americans have attempted some form of alternative flight, which includes everything from ultralights to falling, tripping and use of bungee cords.”
“Current airplane design is based upon a white male Western European model of what powered flight should look like. Long metal tubes with wings are a phallic design that insults the sensibilities of women, who have an alternative, more natural, emotional, way of understanding airplane design. In the one size fits all design of allopathic airlines, alternative designs are ignored and airplane design utilizing the ideas and esthetics of indigenous peoples and ancient flying traditions are derided as primitive and unscientific, despite centuries of successful use.”
Metapsychology Online Reviews doesn’t sound like a promising title for a good review of Healing, Hype or Harm, but in fact their review by Kevin Purday is very sympathetic. I like the ending.
“One may not agree with everything that is written in this book but it is wonderful that academic honesty is still alive and well.”
| A report has appeared on Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine. The report is written by people all of whom have vested interests in spreading quackery. It shows an execrable ability to assess evidence, and it advocates degrees in antiscience It would fail any examination. Sorry, Prof Pittilo, but it’s gamma minus.[Download the report] |  |
Alice Miles put it well in The Times, today.
“This week came the publication of the “Report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK”. Otherwise known as twaddle.” . . .
“Regulate the practitioners – for safety, note, not for efficacy, as that is impossible to prove – and you give them official recognition. From recognition it is but a short hop to demand and then prescription: packet of Prozac, bit of yoga and a bag of dodgy herbs for you, sir.” . . .
“The Government responded on Monday – with a three-month consultation. So join in. Write to the Health Minister Ben Bradshaw at Richmond House, 79 Whitehall, SW1A 2NS. Write, on behalf of the NHS: “What I want for my 60th birthday is… the chance to provide medical, dental, and nursing care to all. And absolutely nothing else.”
Judging by Ben Bradshaw’s speech to the Prince’s Foundation, there may be a problem in conveying to him the evidence, but one can and must try.
Why is it that a health joutnalist can do so much better than a university head? Yes, the chair of the steering group is Professor R. Michael Pittilo BSc PhD CBiol FIBiol FIBMS FRSH FLS FRSA, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. Despite all those impressive-lookin initials after his name, I believe that this is a very bad report.
Here is something about Prof Pittilo from his university’s web site (the emphasis is mine).
Professor Michael Pittilo joined The Robert Gordon University, Aberdeen, as Principal and Vice-Chancellor on 5th September, 2005.
After postdoctoral research on arterial disease at the University of London, he was appointed to Kingston University where he became Head of Life Sciences. In 1995 he became Foundation Dean of the Faculty of Health and Social Care Sciences at Kingston University and St George’s Medical School (University of London). He was appointed Pro Vice Chancellor at the University of Hertfordshire in 2001.
Professor Pittilo has held a number of additional roles, including chairing Department of Health working groups, and as a trustee for the Prince of Wales’s Foundation for Integrated Health. “
Notice that Prof Pittilo is a Trustee of the Prince’s Foundation for Integrated Health, source of some of the least reliable information about alternative medicine to be found anywhere.
This steering group is, as so often, a nest of vested interests. It does not seem to have on it any regular medical or clinical scientist whatsoever. Why not? They just might produce some embarrassing facts perhaps? Like most government committees its members seem to have been chosen to produce the desired outcome.
For a start, the university run by Prof Pittilo, Robert Gordon’s University, is itself involved in a few antiscientific courses. Since his report recommends that degrees in quackery should become mandatory, I expect he’d welcome the chance to run more. Amazingly, Robert Gordon’s University runs an Introduction to Homeopathy, just about the daftest of all the common sorts of magic medicine.
Most of the the members of the steering group represent vested interests, though strangely this is not made clear in the list of members. An earlier report, in 2006, from the steering group was more open about this. Twelve of the members of the group represent Herbal Medicine, Chinese Medicine and Acupuncture (four from each). Most of the rest are lay members or bureaucrats. With membership like that it is, I suppose, not surprising that the assessment of evidence is, to put it kindly, grossly distorted and woefully inadequate.
The report starts badly by failing to mention that the House of Lords report (2000), and the government’s response to it, set the following priorities. Both state clearly
“… we recommend that three important questions should be addressed in the following order . .
- (1) does the treatment offer therapeutic benefits greater than placebo?
- (2) is the treatment safe?
- (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?
The word ‘placebo’ does not occur a single time in the main report (and only twice in the text of the seven appendices). But they do say (page 11):
“We recommend that public funding from the NHS should be used to fund CAM therapies where there is evidence of efficacy, safety and quality assurance.”
The evidence
The problem is that the assessment of the evidence for efficacy in the report is pathetically poor. The report, sad to say, consists essentially of 161 pages of special pleading by the alternative medicine industry, served up with the usual large dose of HR gobbledygook.
There is really no excuse for this utterly incompetent assessment. There have been plenty of books this year alone that make excellent summaries of the evidence, mostly written for the lay public. They should, therefore, be understandable by any university vice-chancellor (president). The one benefit of the upsurge in public interest in magic medicine is that there are now quite a lot of good clinical trials, and when the trials are done properly, they mostly confirm what we thought before: in most cases the effects are no more than placebo.
Here is one example. Annexe1 concerns “Developing Research and Providing an Evidence Base for Acupuncture and Herbal/Traditional Medicine Treatment”. The wording of the title itself suggests, rightly, that this evidence base does not exist, in which case why on earth are we talking about them as “professions”? The discussion of the evidence in Annexe 1 is nothing if not partial. But what do you expect if you ask herbalists to assess herbal medicine? An honest assessment would put them out of business. The eternal mantra of the alternative industry appears as usual, “Absence of evidence is, of course, not evidence of absence”. True of course, but utterly irrelevant. Annexe 1 says
“Acupuncture is a complex intervention and lack of a suitable placebo control has hindered efforts to evaluate efficacy”
This is simply untrue, In recent years enormous efforts have been put into devising controls for assessment of acupuncture, but they are entirely ignored here. One thing that has been established quite clearly is that it makes no difference where you put the needles, so all the talk of Qi and meridians is obvious mumbo-jumbo.
Have the authors of Annexe 1, and Professor Pittilo, not read the relevant studies? Two books this year have dealt with the question of evidence with great care. They are both by people who have been involved personally with acupuncture research, Prof Edzard Ernst and Dr Barker Bausell. Edzard Ernst is the UK’s first Professor of Complementary Medicine. Barker Bausell was research director of an NIH-funded Complementary and Alternative Medicine Specialized Research Center at the University of Maryland.
 |
 |
Singh and Ernst discuss thoroughly the question of controls and assess all the evidence carefully. Their conclusions include the following.
- The traditional principles of acupuncture are deeply flawed, as there is no evidence at all to demonstrate the existence of Ch’i [Qi] or meridians.
- By focussing on the increasing number of high-quality research papers, reliable conclusions from systematic reviews make it clear that acupuncture does not work for a whole range of conditions, except as a placebo.
- In short, the evidence is neither consistent nor convincing. It is borderline.
Barker Bausell was himself involved in designing and analysing trialsof acupuncture. His conclusions are even less positive.
“There is no compelling, credible scientific evidence to suggest that any CAM therapy benefits any medical condition or reduces any medical symptom (pain or otherwise) better than a placebo”.
These are serious authors with direct experience in CAM research, which is more than can be said of anyone on the steering group. Why are their conclusions ignored entirely? That is sheer incompetence.
Degrees in anti-science
One conclusion of the report is that
“The threshold entry route to the register will normally be through a Bachelor degree with Honours”
This is utter nonsense. It is quite obvious surely that you can’t award honours degrees until after you have the evidence. You can read on page 55 of the report
“3a: Registrant acupuncturists must:
understand the following aspects and concepts for traditional East-Asian acupuncture:
– yin/yang, /5 elements/phases, eight principles, cyclical rhythms, qi ,blood and body fluids, different levels of qi, pathogenic factors, 12 zang fu and 6 extraordinary fu, jing luo/ meridians, the major acupuncture points, East-Asian medicine disease categorisation, the three burners, the 4 stages/levels and 6 divisions
– causes of disharmony/disease causation
– the four traditional diagnostic methods: questioning, palpation, listening and observing”
This is utter baloney. Anyone who advocates giving honours degrees in such nonsense deserves to be fired for bringing his university into disrepute (and, in the process, bringing all universities and science itself into disrepute).
That includes also degrees that teach that “amethysts emit high yin energy“.
So what should be done?
If making peole do degrees in mumbo-jumbo is not the answer, what is? Clearly it would be far too draconian to try to ban quackery (and it would only increase its popularity anyway).
The answer seems to me to be quite simple. All that needs to done is to enforce existing laws. It is already illegal to sell contaminated and poisonous goods to the public. It is already illegal to make fraudulent advertisemants and to sell goods that are not as described on the label.
The only problem is that the agencies that enforce these rules are toothless and that there are a lot of loopholes and exceptions that work in favour of quackery. I have tried myself to complain about mislabelling of homeopathic pills to the Office of Fair Trading on the grounds that are labelled Arnica 30C but contain no Arnica. They solemnly bought a bottle and sent it to an analyst and of course they found no arnica, But nothing happened, because an exception to the usual law applies to homeopathic pills.
The Advertising Standards Authority is good as far as it goes. They quickly told Boots Pharmacies to withdraw advertisements that claimed CoQ10 “increased vitality”. But they can exact no penalties and they can’t deal with lies that are told to you orally, or with anything at all on the web.
The Health Professions Council (HPC) says that one of the criteria for registering new professions is aspirant groups must “Practise based on evidence of efficacy”. If that were actually applied, none of this process would occur anyway. No doubt the HPC will fail to apply its own criteria. On past form, it can be expected to adopt a “fluid concept of evidence“.,
One more thing, New European legislation was described recently in the BMJ
“Consumers in the United Kingdom are to receive stronger legal safeguards against products that claim, without any identifiable scientific evidence, to provide physical and mental health benefits such as tackling obesity or depression.”
“The scope of the legislation is deliberately wide and is the biggest shake up in consumer law for decades. It targets any unfair selling to consumers by any business.”
Politicians seem to be immune to rational argument when it comes to quackery. But a few legal actions under these laws could bring the house of cards tumbling so fast that this gamma-minus report would become rapidly irrelevant. There will be no shortage of people to bring the actions. I can’t wait.
Follow up
Dominic Lawson, 24 June 2008. An excellent column appeared today in the Independent. Dominic Lawson writes about the Pittilo report: “So now we will have degrees in quackery. What, really, is the difference between acupuncture and psychic surgery?“. The reference to that well known conjuring trick, “psychic surgery” as a “profession”, revealed here, causes Lawson to say
“It makes it clear that the lunatics have taken over the asylum. For a start, how could Philip Hunt, previously director of the National Association of Health Authorities and Trusts, possibly have thought that “psychic healing” constituted a “profession” – let alone one which would “develop its own system of voluntary self-regulation?”
“One can see how this might fit in with the Government’s “never mind the quality, feel the width” approach to university education. One can also see how established practitioners of such therapies might see this as a future source of income – how pleasant it might be to become Visiting Professor of Vibrational Medicine at the University of Westminster.
Thus garlanded with the laurels of academic pseudo-science, the newly professionalised practitioners of “alternative medicine” can look down on such riff-raff as the “psychic surgeons”
Once again I have to ask, how is it that we have to rely on journalists to prevent vice-chancellors eroding academic standards; indeed eroding simple common sense? I guess it is just another sign of the delusional thinking engendered by the culture of managerialism that grips universities.
We have often had cause to criticise Boots Alliance, the biggest retail pharmacist in the UK, because of its deeply unethical approach to junk medicine. Click here to read the shameful litany. The problem of Boots was raised recently also by Edzard Ernst at the Hay Literary Festival. He said
“The population at large trusts Boots more than any other pharmacy, but when you look behind the smokescreen, when it comes to alternative medicines, that trust is not justified.”

Ernst accused Boots of breaching ethical guidelines drawn up by the Royal Pharmaceutical Society of Great Britain, by failing to tell customers that its homeopathic medicines contain no active ingredients and are ineffective in clinical trials.
Another chain, Lloyds Pharmacy, are just as bad. Many smaller pharmacies are no more honest when it comes to selling medicines that are known to be ineffective.
Pharmacists are fond of referring to themselves as “professionals” who are regulated by a professional body, the Royal Pharmaceutical Society of Great Britain (RPSGB). It’s natural to ask where their regulatory body stands on the question of junk medicine. So I asked them, and this is what I found.
| 17 April, 2008
I am writing an article about the role of pharmacists in giving advice about (a) alternative medicines and (b) nutritional supplements. I can find no clear statements about these topics on the RPSGB web site. Please can you give me a statement on the position of the Royal Pharmaceutical Society on these two topics. In particular, have you offered guidance to pharmacists about how to deal with the conflict of interest that arises when they can make money by selling something that they know to have no good evidence for efficacy? This question has had some publicity recently in connection with Boots’ promotion of CCoQ10 to give you “energy”, and only yesterday when the bad effects of some nutritional supplements were in the news. |
Here are some extracts from the first reply that I got from the RPSGB’s Legal and Ethical Advisory Service (emphasis is mine).
| 28 April 2008
Pharmacists must comply with the Code of Ethics and its supporting documents. Principle 5 of the Code of Ethics requires pharmacists to develop their professional knowledge and competence whilst Principle 6 requires pharmacists to be honest and trustworthy. The Code states: 5. DEVELOP YOUR PROFESSIONAL KNOWLEDGE AND COMPETENCE At all stages of your professional working life you must ensure that your knowledge, skills and performance are of a high quality, up to date and relevant to your field of practice. You must: 5.1 Maintain and improve the quality of your work by keeping your knowledge and skills up to date, evidence-based and relevant to your role and responsibilities. 5.2 Apply your knowledge and skills appropriately to your professional responsibilities. 5.3 Recognise the limits of your professional competence; practise only in those areas in which you are competent to do so and refer to others where necessary. 5.4 Undertake and maintain up-to-date evidence of continuing professional development relevant to your field of practice. 6. BE HONEST AND TRUSTWORTHY Patients, colleagues and the public at large place their trust in you as a pharmacy professional. You must behave in a way that justifies this trust and maintains the reputation of your profession. You must: 6.2 Ensure you do not abuse your professional position or exploit the vulnerability or lack of knowledge of others. 6.3 Avoid conflicts of interest and declare any personal or professional interests to those who may be affected. Do not ask for or accept gifts, inducements, hospitality or referrals that may affect, or be perceived to affect, your professional judgement. 6.4 Be accurate and impartial when teaching others and when providing or publishing information to ensure that you do not mislead others or make claims that cannot be justified. |
And, on over-the counter prescribing
| In addition the “Professional Standards and Guidance for the Sale and Supply of Medicines” document which supports the Code of Ethics states:
“2. SUPPLY OF OVER THE COUNTER (OTC) MEDICINES STANDARDS When purchasing medicines from pharmacies patients expect to be provided with high quality, relevant information in a manner they can easily understand. You must ensure that: 2.1 procedures for sales of OTC medicines enable intervention and professional advice to be given whenever this can assist the safe and effective use of medicines. Pharmacy medicines must not be accessible to the public by self-selection. |
Evidence-based? Accurate and impartial? High quality information? Effective use?
These words don’t seem to accord with Boots’ mendacious advertisements for CoQ10 (which were condemned by the ASA).
Neither does it accord with the appalling advice that I got from a Boots pharmacist about Vitamin B for vitality.
Or their bad advice on childhood diarrhoea.
Or the unspeakable nonsense of the Boots (mis)-education web site.
Then we get to the nub. This is what I was told by the RPSGB about alternative medicine (the emphasis is mine).
| 8. COMPLEMENTARY THERAPIES AND MEDICINES
STANDARDS You must ensure that you are competent in any area in which you offer advice on treatment or medicines. If you sell or supply homoeopathic or herbal medicines, or other complementary therapies, you must: 8.1 assist patients in making informed decisions by providing them with necessary and relevant information. 8.2 ensure any stock is obtained from a reputable source. 8.3 recommend a remedy only where you can be satisfied of its safety and quality, taking into account the Medicines and Healthcare products Regulatory Agency registration schemes for homoeopathic and herbal remedies.” Therefore pharmacists are required to keep their knowledge and skills up to date and provide accurate and impartial information to ensure that you do not mislead others or make claims that cannot be justified. |
It does seem very odd that “accurate and impartial information” about homeopathic pills does not include mentioning that they contain no trace of the ingredient on the label. and have been shown in clinical trials to be ineffective. These rather important bits of information are missing from both advertisements and from (in my experience) the advice given by pharmacists in the shop.
If you look carefully, though, the wording is a bit sneaky. Referring to over-the-counter medicines, the code refers to “safe and effective use of medicines”, but when it comes to alternative medicines, all mention of ‘effectiveness’ has mysteriously vanished.
So I wrote again to get clarification.
| 29 April, 2008
Thanks for that information. I’d appreciate clarification of two matters in what you sent. (1) Apropros of complementary and alternative medicine, the code says 8.3 recommend a remedy only where you can be satisfied of its safety and quality I notice that this paragraph mentions safety and quality but does not mention efficacy. Does this mean that it is considered ethical to recommend a medicine when there is no evidence of its efficacy? Apparently it does. This gets to the heart of my question and I’d appreciate a clear answer. |
This enquiry was followed by a long silence. Despite several reminders by email and by telephone nothing happened until eventually got a phone call over a month later (May 3) from David Pruce, Director of Practice & Quality Improvement, Royal Pharmaceutical Society of Great Britain. The question may be simple, but the RPSGB evidently it hard, or more likely embarrassing, to answer.
When I asked Pruce why para 8.3 does not mention effectiveness, his reply, after some circumlocution, was as follows.
Pruce: “You must assist patients in making informed decisions by providing necessary and relevant information . . . we would apply this to any medicine, the pharmacist needs to help the patient assess the risks and benefits.”
DC: “and would that include saying it doesn’t work better than placebo?”
Pruce “if there is good evidence to show that it may, but it depends on what the evidence is, what the level of evidence is, and the pharmacist’s assessment of the evidence”
DC “What’s your assessment of the evidence?”
Pruce, “I don’t think my personal assessment is relevant. I wouldn’t want to be drawn on my personal assessment”. “If a pharmacist is selling homeopathic medicines they have to assist the patient in making informed decisions”
“I don’t think we specifically talk about the efficacy of any other medicine” [DC: not true, see para 2.1, above]
“We would expect pharmacists to be making sure that what they are providing to a patient is safe and efficacious”
DC “So why doesn’t it mention efficacious in para 8.3”
Pruce “What we are trying to do with the Code of Ethics is not go down to the nth degree of detail ” . . . “there are large areas of medicine where there is an absence of data”
DC “Yes, actually homeopathy isn’t one of them. It used to be.”
Pruce. “uh, that’s again a debatable point”
DC I don’t think it’s debatable at all, if you’ve read the literature
Pruce. “well many people would debate that point” “This [homeopathy] is a controversial area where opinions are divided on it”
DC “Not informed opinions”
Pruce “Well . . . there are also a large number of people that do believe in it. We haven’t come out with a categorical statement either way.”
I came away from this deeply unsatisfactory conversation with a strong impression that the RPSGB’s Director of Practice & Quality Improvement was either not familiar with the evidence, or had been told not to say anything about it, in the absence of any official statement about alternative medicine.
I do hope that the RPSGB does not really believe that “there are also a large number of people that do believe in it” constitutes any sort of evidence.
It is high time that the RPSGB followed its own code of ethics and required, as it does for over-the-counter sales, that accurate advice should be given about “the safe and effective use of medicines”.
“The scientist on the High Street”
The RPS publishes a series of factsheets for their “Scientist in the High Street” campaign. One of these “factsheets” concerns homeopathy, [download pdf from the RPSGB]. Perhaps we can get an answer there?
Well not much. For the most part the “factsheet” just mouths the vacuous gobbledygook of homeopaths. It does recover a bit towards the end, when it says
“The methodologically “best” trials showed no effect greater than that of placebo”.
But there is no hint that this means pharmacists should not be selling homeopathic pills to sick people..
That is perhaps not surprising, because the Science Committee of the RPSGB copped out of their responsibility by getting the factsheet written by a Glasgow veterinary homeopath, Steven Kayne. You can judge his critical attitude by a paper (Isbell & Kayne, 1997) which asks whether the idea that shaking a solution increases its potency. The paper is a masterpiece of prevarication, it quotes only homeopaths and fails to come to the obvious conclusion. And it is the same Steven Kayne who wrote in Health and Homeopathy (2001)
“Homeopathy is not very good for treating bacterial infections directly, apart from cystitis that often responds to a number of medicines, including Berberis or Cantharis”.
So there is a bacterial infection that can be cured by pills that contain no medicine? Is this dangerous nonsense what the RPSGB really believes?
More unreliable advice
While waiting for the train to Cardiff on April 16th (to give a seminar at the Welsh School of Pharmacy), I amused myself by dropping into the Boots store on Paddington station.
| DC I’ve seen your advertisements for CoQ10. Can you tell me more? Will they really make me more energetic?
Boots: Yes they will, but you may have to take them for several weeks. DC. Several weeks? Boots: yes the effect develops only slowly Peers at the label and reads it out to me DC I see. Can you tell me whether there have been any trials that show it works? Boots. I don’t know. I’d have to ask. But there must be or they wouldn’t be allowed to sell it. DC. Actually there are no trials, you know Boots. Really? I didn’t think that was allowed. But people have told me that they feel better after taking it. DC You are a pharmacist? Boots. Yes |
Sadly, this abysmal performance is only too typical in my experience, Try it yourself.
The malaria question
After it was revealed that pharmacists were recommending, or tolerating recommendations, of homeopathic treatment of malaria, the RPSGB did, at last. speak out. It was this episode that caused Quackometer to write his now famous piece on ‘The gentle art of homeopathic killing‘ (it shot to fame when the Society of Homeopaths tried to take legal action to ban it) Recommending pills that contain no medicine for the treatment or prevention or treatment of malaria is dangerous. If it is not criminal it ought to be [watch the Neals Yard video]. .
The RPSGB says it is investigating the role of pharmacists in the Newsnight sting (see the follow-up here). That was in July 2006, but they are stlll unwilling to say if any action will be taken. Anyone want to bet that it will be swept under the carpet?
The statement issued by the RPSGB, 5 months after the malaria sting is just about the only example that I can find of them speaking out against dangerous and fraudulent homeopathic practices. Even in this case, it is pretty mild and restricted narrowly to malaria prevention.
The RPSGB and the Quacktioner Royal
The RPSGB submitted a response to the ‘consultation’ held by the Prince’s Foundation for Integrated Health, about their Complementary Healthcare; a guide for patients.
| Response by the Royal Pharmaceutical Society of Great Britain Dr John Clements, Science Secretary “We believe that more emphasis should be given to the need for members of the public who are purchasing products (as opposed to services) to ask for advice about the product. Pharmacists are trained as experts on medicines and the public, when making purchases in pharmacies, would expect to seek advice from pharmacists” |
So plenty of puffery for the role of pharmacists. But there is not a word of criticism about the many barmy treatments that are included in the “Guide for Patients”. Not just homeopathy and herbalism, but also Craniosacral therapy, Laying on of Hands, chiropractic, Reiki, Shiatsu –every form of barminess under the sun drew no comment from the RPS.
I can’t see how a response like this is consistent with the RPS’s own code of ethics.
A recent president of the RPSGB was a homeopath
| Christine Glover provides perhaps the most dramatic reason of all for thinking thst, despite all the fine words, the RPSGB cares little for evidence and truth The NHS Blogdoctor published “Letter from an angry pharmacist”. |  |
Mrs Glover was president of the RPSGB from 1999 to 2001, vice-president in 1997-98, and a member of the RPSGB Council until May 2005. She is not just a member, but a Fellow. (Oddly, her own web site says President from 1998 – 2001.)
So it is relevant to ask how the RPSGB’s own ex-president obeys their code of ethics. Here are some examples on how Ms Glover helps to assist the safe and effective use of medicines. . Much of her own web site seems to have vanished (I wonder why) so I’ll have to quote the “Letter from an angry pharmacist”., as revealed by NHS Blogdoctor,
“What has Christine got to offer?
- “We offer a wide range of Homeopathic remedies (over 3000 different remedies and potencies) as well as Bach flower remedies, Vitamins, Supplements, some herbal products and Essential Oils.”
- Jetlag Tablets highly recommended in ‘Wanderlust’ travel magazine. Suitable for all ages.
- Wind Remedy useful for wind particularly in babies. In can be supplied in powder form for very small babies. Granules or as liquid potency.
- Udder Care 100ml £80.00 One capful in sprayer filled with water. Two jets to be squirted on inner vulva twice daily for up to 4 days until clots reduced. Discard remainder. Same dose for high cell-counting cows detected.
Udder Care? Oh! I forgot to say, “Glover’s Integrated Healthcare” does cows as well as people. Dr Crippen would not suggest to a woman with sore breasts that she sprayed something on her inner vulva. But women are women and cows are cows and Dr Crippen is not an expert on bovine anatomy and physiology. But, were he a farmer, he would need some persuasion to spend £80.00 on 100 mls of a liquid to squirt on a cow’s vulva. Sorry, inner vulva.”
Nothing shows more clearly that the RPSGB will tolerate almost any quackery than the fact that they think Glover is an appropriate person to be president. Every item on the quotation above seems to me to be in flagrant breach of the RPSGB’s Code of Ethics. Just like the Society of Homeopaths, the code seems to be there merely for show, at least in the case of advice about junk medicine..
A greater role for pharmacists?
This problem has become more important now that the government proposes to give pharmacists a greater role in prescribing. Needless to say the RPSGB is gloating about their proposed new role. Other people are much less sure it is anything but a money–saving gimmick and crypto-privatisation.
I have known pharmacists who have a detailed knowledge of the actions of drugs, and I have met many more who haven’t. The main objection, though, is that pharmacists have a direct financial interest in their prescribing. Conflicts of interest are already rife in medicine, and we can’t afford them.
Conclusion
The Royal Pharmaceutical Society is desperately evasive about a matter that is central to their very existence, giving good advice to patients about which medicines work and which don’t. Pharmacists should be in the front line in education of the public, about medicines, the ‘scientist on the High Street’. Some of them are, but their professional organisation is letting them down badly.
Until such time as the RPSGB decides to take notice of evidence, and clears up some of the things described here, it is hard to see how they can earn the respect of pharmacists, or of anyone else.
Follow-up
Stavros Isaiadis’ blog, Burning Mind, has done a good piece on “More on Quack Medicine in High Street Shops“.
The Chemist and Druggist reports that the RPSGB is worried about the marketing of placebo pills (‘obecalp’ -geddit?). It does seem very odd that the RPSGB should condemn honest placebos, but be so very tolerant about dishonest placebos. You couldn’t make it up.
A complaint to the RPSGB is rejected
Just to see what happened, I made a complaint to thr RPSGB about branches of their own Code of Ethics at Boots in Hexham and in Evesham. Both of them supported Homeopathy Awareness Week These events had been publicised in those particularly unpleasent local ‘newspapers’ that carry paid advertising disguised as editorial material. In this case it was the Evesham Journal and the Hexham Courant.
Guess what? The RPSGB replied thus
“Your complaint has been reviewed bt Mrs Jill Williams and Mr David Slater who are both Regional Lead Inspectors. Having carried out a review they have concluded that support of homeopathic awareness week does not constitute a breach of the Society’s Code of Ethics or Professional Standards.”
In case you have forgotten, the Professional Standards say
2.1 procedures for sales of OTC medicines enable intervention and professional advice to be given whenever this can assist the safe and effective use of medicines.
The RPSGB has some very quaint ideas on how to interpret their own code of ethics
The extent to which irrationality has become established in US Medicine is truly alarming I wrote about Quackademics in the USA and Canada on my last trip to the USA, and on my May trip I visited Yale, where I decided to try a full frontal attack. [download the poster]

Several US blogs have written about this phenomenon. For example the incomparable Orac at the The Academic Woo Aggregator , and Dr RW (R.W. Donnell) , see particularly his articles on How did pseudoscience get admitted to medical school? and What is happening to our medical schools? Abraham Flexner is turning over in his grave. Excellent US stuff too at Science-based Medicine (try this and this). There is also a good analysis of what’s happening at Yale by Sandy Szwarc at Junkfood Science.
Remember that the terms ‘integrative’ and ‘complementary’ are euphemisms coined by quacks to make their wares sound more respectable, There is no point integrating treatments that don’t work with treatments that do work.
‘Integrative Medicine’ at Yale says, like all the others on the roll of shame, says “we aim to improve awareness and access to the best in evidence-based, comprehensive medical care available worldwide”. They all pay lip service to being “evidence based”, but there is just one snag. It is untrue. In almost all cases, the evidence is either negative or absent. But this does not put them off for a moment. The whole process is simply dishonest.
The evidence
The evidence has been summarised in several books recently, The following books are particularly interesting because they are all ‘views from the inside. Edzard Ernst is the UK’s first Professor of Complementary Medicine. Barker Bausell was research director of an NIH funded Complementary and Alternative Medicine Specialized Research Center at the University of Maryland.
The first two books go through the evidence fairly and carefully. They show no bias against alternative treatments (if anything, I’d say they are rather generous in cases of doubt).
 |
 |
For a first class US account try Barker Bausell’s Snake Oil Science
Bausell’s book gives an excellent account of how to test treatments properly, and of all the ways you can be fooled into thinking something works when it doesn’t. Bausell concludes
|
 |
| For an excellent account of how to find the truth, try Testing Treatments (Evans. Thornton and Chalmers). One of the authors, Iain Chalmers, is a founder of the Cochrane library and a world authotity on how to separate medical fact from medical myth. |  |
It can now be said with some certainty that the number of alternative treatments that have been shown to work better than placebo is very small, and quite possibly zero,
With that settled, what’s going on at Yale (and many others on the roll of shame)?
David L. Katz, MD, MPH, FACPM, FACP, is founder and director of the Integrative Medicine Center (IMC) at Griffin Hospital in Derby, Connecticut. He is also an associate professor, adjunct, of Public Health and director of the Prevention Research Center (PRC) at the Yale University School of Medicine in New Haven, Connecticut.
That sounds pretty respectable. But he is into not just good nutrition, exercise, relaxation and massage, but also utterly barmy and disproved things like homeopathy and ‘therapeutic touch’.
| Watch the movie
It so happens that Yale recently held an “Integrative Medicine Scientific Symposium”. Can we find the much vaunted evidence base there? That is easy to answer because three hours of this symposium have appeared on YouTube. So this is the public face of Yale medical school. There’s some interesting history and a great deal of bunkum and double-speak. To save you time, I’ve cut out about 6 minutes from the movies. |
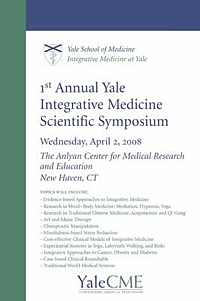 |
View or download the movie here > [18.5 Mb, flv file].
Dean of education Richard Belitsky and Dr David Katz
Pretty remarble uh? Dr Katz goes through several different trials, all of which come out negative. And what is his conclusion? You guessed.
His conclusion is not that the treatments don’t work but that we need a “more fluid concept of evidence” .
It’s equally bizarre to hear Richard Belitsky, Dean of Medical Education at Yale saying he is “very proud” of this betrayal of enlightenment values. If this is what Yale now considers to be education, it might be better to go somewhere else.
This is not science. It isn’t even common sense. It is a retreat to the dark ages of medicine when a physician felt free to guess the answer. In fact it’s worse. In the old days there was no evidence to assess. Now there is a fair amount of evidence, but Dr Katz feels free to ignore it and guess anyway. He refers to teaching about evidence as ‘indoctrination’, a pretty graphic illustration of his deeply anti-scientific approach to knowledge. And he makes a joke about having diverted a $1m grant from CDC, for much needed systematic reviews, into something that fits his aims better.
Katz asks, as one must, what should we do if there is no treatment that is known to help a patient. That is only too frequent a problem. The reasonable thing to say is “there is no treatment that is known to help”. But Dr Katz thinks it’s better to guess an answer. There is nothing wrong with placebo effects but there is everything wrong with trying to pretend that you are doing more than give placebos. Perhaps he should consider the dilemmas of alternative medicine.
You can read about more about Yale’s activities here and in interviews here. Dr Katz says “The founding approach—and I think Andrew Weil, MD, gets the lion’s share of credit for establishing the concept —is training conventional practitioners in complementary disciplines”. Let’s take a look at this hero. Try, for example, Arnold Relman’s “A trip to Stonesville“.
“According to Weil, many of his basic insights about the causes of disease and the nature of healing come from what he calls “stoned thinking,” that is, thoughts experienced while under the influence of psychedelic agents or during other states of “altered consciousness” induced by trances, ritual, magic, hypnosis, meditation, and the like.”
“To the best of my knowledge, Weil himself has published nothing in the peer-reviewed medical literature to document objectively his personal experiences with allegedly cured patients or to verify his claims for the effectiveness of any of the unorthodox remedies he uses.”
Here is the advertisment for Andrew Weil’s nutrition symposium.

Not only does this yet again propagate the great antioxidant myth, but a few moments with Google show that it is riddled with vested interests, as already pointed out on Quackademics in USA and Canada.
What has brought medical schools down to this level?
That isn’t hard to see, The main thing is simply money. Very few university administrators have the intellectual integrity to turn down money, whatever the level of dishonesty that is required by its acceptance. You can buy a lot of silence for $100m
The US Taxpayer has given almost a billion dollars, via NIH.
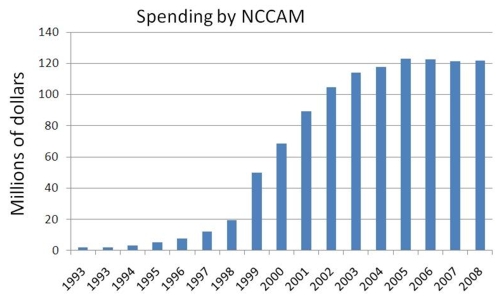
Wallace Sampson, MD says of NCCAM
“. . it has not proved effectiveness for any ‘alternative’ method. It has added evidence of ineffectiveness of some methods that we knew did not work before NCCAM was formed”
“Its major accomplishment has been to ensure the positions of medical school faculty who might become otherwise employed in more productive pursuits.”
“Special commercial interests and irrational, wishful thinking created NCCAM. It is the only entity in the NIH devoted to an ideological approach to health.”
NCCAM has given money from some very dubious trials too, Both Orac on Respectful Insolence and Dr RW (R.W. Donnell) have written recently about the NCCAM-funded trial of “chelation therapy”, as first exposed in a devastating article by Kimball C. Atwood IV, MD; Elizabeth Woeckner, AB, MA; Robert S. Baratz, MD, DDS, PhD; Wallace I. Sampson, MD on Medscape Today. This is a $30 million, 5-year, phase 3 Trial to Assess Chelation Therapy (TACT) for coronary artery disease.
“But how did such a crappy study ever come to be, much less be funded by the NIH to the tune of $30 million? The answer, not surprisingly, involves one of the foremost promoters of quackery in the federal government, Representative Dan Burton (R-IN).”
“We conclude that the TACT is unethical, dangerous, pointless, and wasteful. It should be abandoned.”
Orac comments
“TACT is not the only example of an unethical and scientifically worthless trial being funded not because the science is compelling but because powerful lobbies and legislators who are true believers in woo applied pressure to the NIH to do them”
The Bravewell Collaboration is the other major source of money. Forbes Business says “Bravewell is not some flaky New Age group”. Well dead wrong there, That is precisely what it is.
This group of ultra-rich people, according to its boss, Christy Mack, has a
So Bravewell is corrupting the search for real knowledge and real cures with big bucks. You can buy a lot of hokum for $100m. |
 |
The money comes from Morgan Stanley,
|
 |
Bravewell is run by his wife, Christy Mack (Mack-the-wife?) Vice-President, The C.J. Mack Foundation, Member, Board of Directors, The Bravewell Collaborative.
The Flexner report.
The story of Bravewell stands in chilling contrast to another case of philanthropy. Andrew Carnegie’s foundation financed the report by Abraham Flexner, “Medical Education in the United States and Canada” (1910) [download, 15 Mb] . That report was responsible for dragging medical education out of the dark ages
almost a century ago. It resulted in creation of some of the best medical schools anywhere (including Yale).
“By educational patriotism I mean this: a university has a mission greater than the formation of a large student body or the attainment of institutional completeness, namely, the duty of loyalty to the standards of common honesty, of intellectual sincerity, of scientific accuracy.”
“The tendency to build a system out of a few partially apprehended facts, deductive inference filling in the rest, has not indeed been limited to medicine, but it has nowhere else had more calamitous consequences.”
Flexner (1910).
Now another philanthropist is using big bucks to reverse the process and push medicine back into the 19th century.
Flexner would have thought it quite inconceivable that in 2007 medical schools would be offering Continuing Medical Education in homeopathy.
Why are Yale’s academics so quiet about this?
Perhaps they don’t even know it’s happening. If they say firmly that they don’t want it, it will go,
It’s been done before
Florida State University, allegedly under political pressure, proposed to set up a school of Chiropractic. That would have made it Florida State school of snake-oil salesmanship. What a sad fate. [ Science magazine comment] [comment form Paul Lee] [Comment in St Petersburg Times]
But the academics stopped it. An FSU professor, Albert Stiegman, predicted the future campus map.
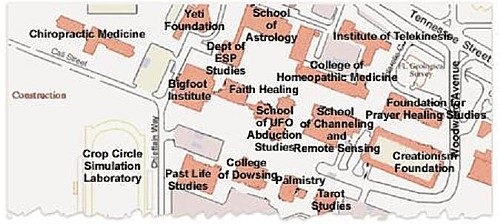
According to FSUnews
“The Florida Board of Governors voted 10-3 Thursday to deny Florida State University’s request to build a chiropractic school.”
“However, the passage of the bill for the chiropractic school by the Legislature seemingly bypassed the Board of Governors.”
In the end, reason won. Let’s hope that Yale follows their example.
Follow up
The problem of Yale has been taken up with great eloquence by some US commentators
Dr RW (R.W, Donnell): “Quackademic Medicine at Yale”
“By the way, where’s the AAMC in all this? Aren’t they supposed to be guardians of integrity and professionalism in medical education? Are they asleep at the switch or is money silencing them too?”
Orac (Respectful Insolence): “Integrative” medicine at Yale: A more “fluid” concept of evidence?”
“after the Dean of the Yale School Medicine embarrassed himself in the introduction by saying he’s proud of how far this nonsense has come, Dr. Katz takes the stage and demonstrates the sort of hostile attitude towards science that, if allowed to take root will be the death of scientific medicine in any meaningful form at U.S. medical schools”
Junkfood Science. Sandy Szwarc on “Quote of the day: ;We need a more fluid concept of evidence’”
“Will healthcare professionals and consumers . . . . speak out against these wellness programs being enacted by government agencies, insurers and employers? Or is the money too good?”
Science-based Medicine. Steven Novella writes on “Changing the rules of evidence“. When alternative medicine people do not like the evidence, they change the rules to get the outcome that they want, as seen so graphically in this post. They have always done this, but it is only recently that this sort of behaviour has been endorsed by places like Yale.
The Macho Response, another US blog, comments bluntly, in “Yale wants a more fluid concept of evidence”
This is beyond embarrassing – it’s a fucking crime – and it’s happening at Yale University and many others.
If you’re in the medical profession (and I know many of my readers are) you need to go here – now.
Kiosque Médias writes as follows
Pour ceux qui s’intéressent à la médecine et à la santé, le blog de David Colquhoun vaut probablement le détour. Ce professeur-chercheur au département de neurosciences, de physiologie et de pharmacologie de l’University College London y décrypte les résultats d’études médicales, en mettant l’accent sur les médecines alternatives. Et il est rarement tendre!
James Randi Newsletter. The hit rate soars after a recommendation this piece by the amazing Randi.
Hokum-Balderdash Assay. Edwardson writes
“Yale University is going to the ducks. It now has an Integrative Medicine program and in April held its first annual Integrative Medicine Scientific Symposium. I think there must’ve been a typo there. They must’ve meant “Ist Annual I.M. Pseudoscientific Symposium.” There! Now we’ve done away with the oxymoron.”
Why is Yale so secretive about its quackery department?,
Most universities are only to keen to boast about their grant income. Not in this case though. When I asked how they funded their quackery, all I got was a letter that had very obviously been drafted by a lawyer.
“As a private institution, Yale University is not generally subject to the U.S. Freedom of Information Act. We therefore respectfully decline to compile and provide the information you have requested.”
So pretty clear signs of guiltiness there.
Dr David Katz, yes, he of the “fluid concept of evidence”, has posted an article, Health Hazards of rhe Blogoshere. If it quacks like a duck . . .
It seems that he has been a bit alarmed by the reaction of the bloggers. It starts, rather pompously, thus.
“Being well educated does not guarantee you’ll always be right, and it certainly doesn’t guarantee everyone will agree with you. But it still matters. Or at least it used to “
But the rest if it reads less like a defence than as an admission of guilt, thus prompting the next item.
Paul Hutchinson’s blog
| A quack who admits it picks out a quotation from Dr Katz’s response and turned into a cartoon, released to the public domain, So here it is. | 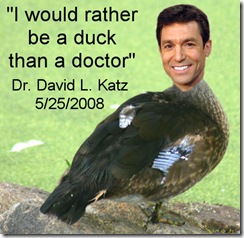 |
Respectful Insolence.
Orac comments too, in “Fluid evidence” strikes back: Dr. Katz versus the skeptical blogsophere”. He does a terrific job in taking apart the response from the hapless Dr Katz.
“No, Dr. Katz does not like his first encounter with the medical blogosphere at all. Indeed, he is so unhappy that apparently a few weeks ago he tried t answer the bloggers who had raked him over the coals for blatantly advocating “integrating” unscientific woo like homeopathy with scientific medicine. Unfortunately for him, he did not do a particularly good job of it. Indeed, what most stood out as I read his rejoinder was that he does not answer a single substantive criticism leveled at his comments. Not one. Instead, he does what pretty much all woo-meisters do when criticized for shifting goalposts and appealing to other ways of knowing besides science as a means of “proving” that their preferred fairy dust works; he wraps himself in the mantle of the brave iconoclast willing to challenge accepted dogma and whines about the peons who criticized him, heaping contempt on the bloggers who had the temerity to criticize his advocacy for pseudoscience because to him they have not earned the right to criticize his (at least in his opinion, apparently) greatness in comparison to him.”
| Last year, Nature published a pretty forthright condemnation of the award of Bachelor of Science degrees in subjects that are not science: in fact positively anti-science. This topic has come up again in Times Higher Education (24 April 2008). A league table shows that the largest number of anti-science courses is run by the University of Westminster [download paper version]. |
 |
Vice chancellors have consistently refused to answer letters, from me, from the Times Higher Education or from the BBC, asking them to defend their practices.
The vice chancellors union, Universities UK, has simply refused to consider this very basic threat to academic standards.
It is particularly amazing that vice-chancellors continue to support courses in homeopathy when they have been condemned by no less a person than the head honcho of homeopathy in the UK, Dr Peter Fisher. He is clinical director of the Royal London Homeopathic Hospital and Homeopathic Physician to the Queen. Peter Fisher and I were interviewed on BBC London News after publication of the Nature article. At the end, Fisher was asked by the presenter, Riz Lateef, about whether homeopathy was a suitable subject for a science degree.[Watch the movie]
| Riz Lateef (presenter): “Dr Fisher, could you ever see it [homeopathy] as a science degree in the future? Dr Peter Fisher: “I would hope so. I wouldn’t deny that a lot of scientific research needs to be done, and I would hope that in the future it would have a scientific basis. I have to say that at the moment that basis isn’t comprehensive. To that extent I would agree with Professor Colquhoun.” |
The one exception was a response, of sorts, that I got from Westminster University.
I can interpret this lack of response only as a sign of guilt on the part of the vice chancellors of the 16 or so universities who teach this stuff. That interpretation is reinforced by the refusal of two of them to release their teaching materials, despite requests under the Freedom of Information Act 2000. Both the University of Central Lancashire and the University of Westminster have turned down appeals, and refused to hand over anything. The former case has been with the Information Commissioner for some time now, and if the ruling goes as a hope, the taxpayer may soon be able to see how their money is being spent.
But the wonderful thing about the electronic age is that it has become really quite difficult to keep secrets. Last year I managed to find an exam paper set by the University of Westminster in Homeopathic Materia Medica, and a question from that paper has already appeared in Nature.
I recently acquired copies of a course handbook. and of the powerpoint slides used for the lecture on ‘Vibrational Medicine’ by the University of Westminster. This appears to be from a course in Complementary Therapies, part of “Health Sciences: Complementary Therapies BSc Honours”, according to Westminster’s web site. A lot of people have access to this first year course material, so Westminster needn’t bother trying to guess how I got hold of this interesting material
In the public interest, here are a few quotations. Taxpayers should know how their money is being spent.
According to the handbook
“Complementary Therapies is a core module for the Therapeutic Bodywork, Herbal Medicine, Homœopathy, Nutritional Therapy and Complementary Therapies courses. Therefore all students of these degree courses are required to take this module.”
The University of Central Lancashire also has “Vitalistic Medicine” as part of its BSc Homeopathy (but, like Westminster, has some excellent people too).
There is a rather good Wikipedia entry on Vitalism, a topic that is now largely the preserve of cranks.

The handbook is wonderful. The word ‘evidence’. in the context of ‘does it work?’, does not occur a single time. There is plenty of the usual edu-bollocks jargon that is so beloved by bureaucrats, but not the slightest hint of critical thinking about assessment of the ‘therapies’.
The course seems to be a romp through almost every form of battiness known to humankind. Not just homeopathy, traditional Chinese medicine and nutritional therapy, but also dowsing, crystal healing and other forms of advanced delusional thinking. Before somebody grumbles, let me emphasise that ‘nutrition’ is to be distinguished from ‘nutritional therapy’: the latter involves imaginative claims that buying expensive supplements can prevent or cure almost anything. There’s a lot more about that here, and here.
Here are just 5 days from the timetable.
| 9am-1.00pm : Homœopathy (group work and video) |
| 9am-1.00pm : Traditional Chinese Medicine |
| 9am-10.45pm : BODYWORK THERAPIES |
| 11.15-1.00pm : Nutritional Therapy |
| 9am-1.00pm : Vibrational Medicine/Energy Concepts (L&P) |
All this can be yours -at a cost.
Full-time UK/EU fee – £3,145
Full-time Overseas fee – £9,450
The slides for the last of these lectures show some of the most glorious examples of the abuse of sciencey-sounding words that I’ve seen in a while.
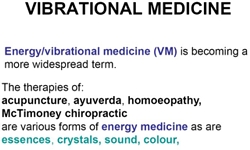 |
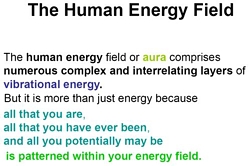 |
Sigh. All this is sheer imagination. It is ancient vitalism dressed up pretentiously in sciencey words.Then a bit later we come to the general theory -“energy concepts”.
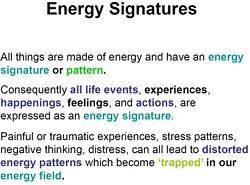 |
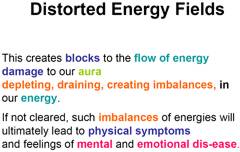 |
More plausible-sounding, but utterly meaningless words about vibrations. And then on to old superstitions about dowsing with rods and pendulums.
 |
 |
.
Not a single word of scepticism appears about any of this mumbo jumbo. Can it get worse? Yes it can. CRYSTAL HEALING comes next.
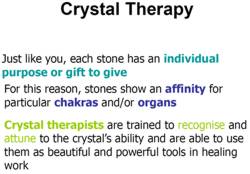 |
 |
Are you having difficulty in understanding what all these words mean? I certainly hope so, because they have no meaning to understand. Don’t worry too much though, There are some helpful diagrams.
 |
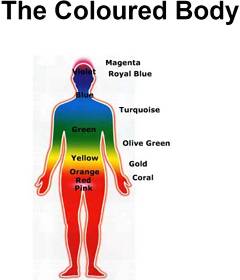 |
Aura photographs? They are just fairground conjuring tricks. Well, that is what you thought. But here we see them presented, apparently in all seriousness, as part of a vocational bachelor of science degree in a UK
university.Never mind, it is all assessed properly, with all the right box-ticking jargon. The course handbook says
| Learning Outcomes On successful completion of this module you will be able to: • describe the theoretical basis and classification of a range of complementary therapies |
What theoretical basis? There isn’t any theoretical basis, just a meaningless jumble of words.
You just couldn’t make it up.
Westminster University is not all like this
This post is not intended as an attack on the University of Westminster as a whole. Last year I had an invitation from their biomedical people to give a talk there. They asked for a talk on “What is is the evidence for Alternative Medicine?”. But then I got an email from them saying
“I was surprised to be sat on heavily on return from said trip by the VC, Provosts and Deans (including Peter Davies the leader of the Alt Med School !) once news of your talk leaked out. Could you give a talk on your research instead- yep I know its pusillanimous of me and yep I know unis stand for freedom of speech and yep I know that fellow members of staff suggested you come and others were keen to listen to your views on quackery.”
So on November 2nd 2007 I gave a seminar about single ion channel work (our new ideas about partial agonists). Of course all the excellent staff whom I met agreed with me about the embarrassment that having degrees in homeopathy etc. The fault lies not with their academic staff, but with their administration. Freedom of speech does not seem to be high on their agenda.
Postscript I recently learned that when Times Higher Education asked Westminster about my seminar, they were given the following statement.
“Prof David Colquhoun was invited to take part in a research seminar series organised by the University’s School of Biosciences last year. As part of this series, on Friday 2 November 2007, he gave a talk on the agreed topic of “Single ion Channel studies suggest a new mechanism for partial agonism” – his area of research.”
Perhaps I am naive, but it truly shocks me that a university can issue such a dishonest account of what happened.
 |
 |
The Times published a letter from Edzard Ernst and Simon Singh on April 16th. In their forthcoming book, Trick or Treatment? Alternative Medicine on Trial, they go carefully through all the evidence for all sorts of ‘alternative’ treatments. They find some evidence that a handful of them work. For most the answer is ‘not enough evidence’, and for a number there is good evidence that many of them don’t work to any useful extent.
“Sir, For over two decades the Prince of Wales has been actively promoting alternative medicine and his Foundation for Integrated Health continues to encourage the use of treatments such as homoeopathy or reflexology.””In light of this “rigorous scientific evidence”, we strongly advise that the Prince of Wales and the Foundation for Integrated Health withdraw the publications Complementary Health Care: A Guide for Patients and the Smallwood report. They both contain numerous misleading and inaccurate claims concerning the supposed benefits of alternative medicine. The nation cannot be served by promoting ineffective and sometimes dangerous alternative treatments.”
Thank heavens that someone has the courage to say it as it is.
If only the ineffectual and ill-educated people in the Department of Health wouold do the same. But no, instead they gave £37 000 to the Prince of Wales Foundation to write their make-believe guides. And £900 000 to write nonsense for the Complementary and Natural Healthcare Council (also known as Ofquack), and Skills for Health,
The next day The Times ran an article by their science editor, Mark Henderson, Prince of Wales’s guide to alternative medicine ‘inaccurate’. Natasha Finlayson, of the Prince’s Foundation for Integrated Health, is quoted as saying “The foundation does not promote complementary therapies.”. That takes some beating for sheer bare-faced dishonesty.
Edzard Ernst appeared on the Today Program on 18th April. He was interveiwed by the formidable John Humphrys, along with Kim Lavely, Chief Executive, The Prince’s Foundation for Integrated Health (FIH). Ernst points out that the FIH guide suggests that chiropractic is effective in asthma, and that acupuncture is good for addiction, whereas the evidence says the opposite. Lavely retorts, rather lamely (OK I’m biassed).
Lavely: ” . . . we didn’t attempt to give detailed evidence on every therapy”. “We think they [the public] have the right to know and what doesn’t”
Humphrys: “Well isn’t that the whole point? the professor is saying here is that these things do not work, at least in terms of the claims that are made for them, such as homeopathy and chiropractic . . . ”
Lavely: “There are no claims made in this guide for what works and what doesn’t. What we have said is that some therapies are used for some things but we aren’t saying they are effective for those things . . . “
So, one might ask, what on earth is the use of a guide is it that offers no indication of effectiveness? Lavely’s second quotation contradicts directly her first. A pretty pathetic performance.
Listen to the interview [mp3 file]
The Sunday Times, on April 20th, pblished a pretty good review of Trick of Treatment?. “Their case against the folly, vanity and damage of HRH et al. is hard to argue with.”
Of course, the letters column drew the expected response from the quacks, most verging on the hilarious.
Another blow for the alternative industry came in the same week, The authoratitve Cochrane review confirmed earlier reports that vitamin supplements not only do not help you but some actually increase mortality. The antioxidant myth nevertheless rumbles on, and on, and on. There is too much money in it for it to die easily.
Predictably enough, the conclusions were denied by the Health Food Manufacturers’ Association (HFMA). They wheeled out several pop singers to say how wonderful their products are. Read about that pathetic defence on Holfordwatch.
Who is behind HFMA? Incidentally, HFMA are strangely reticent about the identity of their 120 members. They will not reveal who they are. Does anybody out there know the answer? I’ll buy a good dinner for anyone who can root this out. If it is anything like the ‘Health Supplements Information Service‘ it is likely to be backedby the very big pharmaceutical companies that the alternative industry loves to hate.
Take the test
Prince of Wales Guide
“Reflexologists work with a wide range of conditions including certain types of pain, particularly back and neck pain, migraine and headaches, chronic fatigue, sinusitis, arthritis, insomnia, digestive problems such as irritable bowel syndrome, and constipation, stress-related disorders and menopausal symptoms.”
Singh & Ernst
“The notion that reflexology can be used to diagnose health problems has been disproved and there is no convincing evidence that it is effective for any condition.”



