General Chiropractic Council

The General Pharmaceutical Council (GPhC) has been the statutory body responsible for the regulation of pharmacy since 2010. It’s status is similar to that of the GMC and. heaven help us, the GCC. Before that the regulator was the same as the professional body, the Royal Pharmaceutical Society of Great Britain (RPS). The RPS proved to be as useless as most other regulators, as documented in detail in my 2008 post, At around the time it stopped being a regulator, the RPS started to condemn quackery more effectively, but by then it had lost the power to do much about it (I hope the latter wasn’t the cause of the former). The body that could do something, the GPhC has done essentially nothing. as described in this post.
I did a 2 year apprenticeship in Timothy White’s and Taylor’s Homeopathic (yes, really) Chemists in the 1950s.
My first degree was in pharmacy. I got my interest in pharmacology from reading Martindale’s Extra Pharmacopoeia in the shop. I soon decided that I didn’t really want to spend the rest of my life selling lipstick and Durex. The latter was quite a big seller because the Boots across the road didn’t sell contraceptives (they changed their minds in the 1960s).
In those days, we spent quite a lot of time making up (almost entirely ineffective) ‘tonics’ and ‘cough mixtures’. Now the job consists largely of counting pills. This has exacerbated the ‘chip on the shoulder’ attitude that was present even in the 1950s. For a long time now, pharmacists have wanted to become the a ‘third tier’ in the NHS, alongside GP practices and hospitals., after hospitals and doctors". . Here are a few comments on this proposition.
First let me say that I’ve met some very good and ethical pharmacists. I did a vacation job in a hospital pharmacy where the boss had an encyclopaedic knowledge of the effects and side effects of drugs, and of their dosage. His advice was often sought by doctors, and rightly so. He had no way of knowing at the time that his advice to replace barbiturates with thalidomide would lead to such a tragedy, because the evidence had been concealed by the manufacturer. Some of the problems alluded to here have already been highlighted by two excellent pharmacists, Anthony Cox and @SparkleWildfire, neither of whom work in pharmacists shops. They are absolutely spot on but they seem to be in a minority among pharmacists.
The problems seem to lie mostly in retail shops. Their shelves are laden with ineffective pills and potions. And the pharmacist has every incentive to sell them. His/her income depends on it directly if it’s a privately owned pharmacy. And his/her standing with head office depends on it in chain store pharmacies. This conflict of financial interest is the prime reason why pharmacists are not qualified to form a third tier of healthcare. The avoidance of conflicts of interest among doctors was one of the great accomplishments of the NHS. In the USA there are huge scandals when, as happens repeatedly, doctors order expensive and unnecessary treatments from which they profit. It’s no consolation that such problems are creeping back in the UK as a result of the government’s vigorous efforts to sell it off.
Here are few examples of things that have gone wrong, and who is to blame. Then I’ll consider what can be done.
Ineffective medicines
In any pharmacy you can see ineffective ‘tonics’ and ‘cough medicines’, unnecessary supplements with dishonest claims and even, heaven help us, the ultimate scam, homeopathic pills.
What’s worse, if you ask a pharmacist for advice, it’s quite likely that they’ll recommend you to buy them.
|
I was amazed to discover that a number of old-fashioned ‘tonics’ and ‘cough medicines’ still have full marketing authorisation. That’s the fault of the Medicines and Healthcare Regulatory Auhority (MHRA) who are supposed to assess efficacy and totally failed to do so, Read about that in “Some medicines that don’t work. Why doesn’t the MHRA tell us honestly?” . It’s hard to blame a pharmacist for the bad advice given by the MHRA, but a good one would tell patients to save their money. |
|
Big corporate pharmacies
Companies like Boots seem to have no interest whatsoever in ethical behaviour. All that matters is sales. They provide “(mis)educational” materials that promote nonsense They advertise ridiculous made-up claims in the newspapers, which get shot down regularly by the Advertising Standards Authority, but by that time the promotion is over so they don’t give a damn. See for example, CoQ10 scam and the ASA verdict on it. And "Lactium: more rubbish from Boots the Chemists. And a more serious problem". And "The Vitamin B scam. Don’t trust Boots"
Recently the consumer magazine Which? checked 122 High Street pharmacies. They got unsatisfactory advice from 43% of them, a disastrously bad performance for people who want to be the third tier of healthcare.
|
Even that’s probably better than my own experience. Recently, when I asked a Sainsbury’s pharmacist about a herbal treatment for prostate problems, he pointed to the MHRA’s kite mark and said it must work because the MHRA approved it -he was quite unaware that you get the THR kite mark without having to present any evidence at all about efficacy. |

|
Of course that is partly the fault of the MHRA for allowing misleading labels, but nevertheless, he should have known. See “Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me” for more on how the MHRA has betrayed its own standards.
When I’ve asked Boots’ pharmacists advice about persistent diarrhoea in an infant, saying I wanted a natural remedy, I’ve usually been guided to the homeopathic display. Only once was I told firmly that I should use rehydration not homeopathy (something every good parent knows) and when I asked that good pharmacist where she’d been educated, she said in Germany (mildly surprising given the amount of junk available in German pharmacies)
Regulators
Anthony Cox, a pharmacist who has been consistently on the side of right, says
"This is something that needs to be dealt with at a regulatory and professional body by the whole profession, and I am certain we have the majority of the UK pharmacy profession on side."
But the regulator has done nothing, and it isn’t even clear that there is a majority on his side.
At a 2009 meeting of Branch Representatives of the RPS a motion was proposed:
“…registration as a pharmacist and practice as a homeopath are not compatible, and that premises registered with the Society should not be used for the promotion of homeopathy”
Although that is obviously sensible to most people, the proposal was followed by a speaker from Leicester who thought it right to keep an open mind about Avogadro’s number and the motion was defeated. So much for the "scientists on the High Street" aspiration.
There have been two major scandals surrounding homeopathy recently. Both were revealed first by bloggers, and both came to wide notice through television programs. None were noticed by the regulators, and when they were brought to the attention of the regulator, nothing effective was done.
The malaria scandal
A lot has been wriitten about this here and on other blogs e.g. here and here. The idea that sugar pills can prevent or cure malaria is so mind-bogglingly dangerous that it was condemned by the Queen’s Homeopathic Physician, Peter Fisher. It was exposed on a BBC Newsnight programme in 2006. Watch the video.
The Gentle Art of Homeopathic Killing was an article that originally appeared on the excellent Quackometer blog produced by Andy Lewis. "The Society of Homeopaths were so outraged about one of their members flouting the code of ethics so blatantly that they took immediate action. That action was, as expected, not to do anything about the ethics breach but to threaten Andy and his hosting ISP with legal action for defamation. The article is reproduced here as a public service".
Some of the people involved in this bad advice were pharmacists, Very properly they were referred to the RPS in 2006 qnd 2009, the regulator at that time. They sat on the complaint so long that eventually the RPS was replaced by the GPhC as regulator. Nothing much has happened.
The GPhC did precisely nothing. Read their pathetic response.
Homeopathy for meningitis
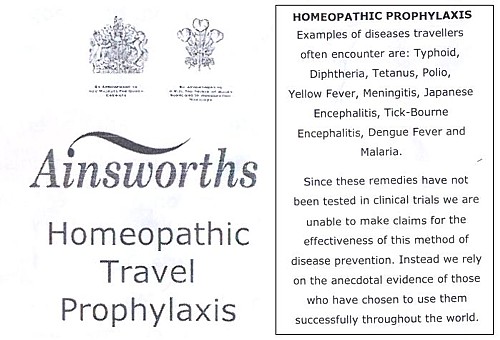
An equally murderous fraud, "homeopathic vaccines" by Ainsworth’s has long been targeted by bloggers. In January 2013, Samantha Smith made an excellent BBC South West programme about it. Watch it and get angry.
Anthony Pinkus, pharmacist at Ainsworths, has been referred to the then regulator, the RPS, in 2006 and 2009. It’s said that he took "remedial action", though there is little obvious change judged by the video above. No doubt some of the most incriminating stuff has been removed from his web site to hide it from the ASA. It’s safer to mislead people by word of mouth. Since the last video more complaints have been made to the GPhC. So far, nothing but silence.
Why doesn’t the regulator regulate?
This pamphlet is reproduced from the July 2011 Quackometer post, “Ainsworths Pharmacy: Casual Disregard for the Law“
|
It’s almost as though those royal warrants, enlarged on right, acted as a talisman that puts this dangerous company outside the grasp of regulators. I hope that the GPhC Council , and Duncan Rudkin (its chief executive and registrar), are not so worried about their knighthoods that they won’t risk upsetting the royal family, just to save patients from malaria and meningitis. Their CEO, Robert Nicholls is only a CBE so far. |
|
Another reason for their inaction might be that the GPhC Council members, and Duncan Rudkin (its chief executive and registrar), lack critical faculties. Perhaps they have not been very well educated? Many of them aren’t even pharmacists, but that curious breed of professional administrators who inhabit the vast number of quangos, tick their boxes and do harm. Or perhaps they are just more interested in protecting the income of pharmacists than in protecting their customers?
Education
The solution to most problems is education. But there is no real knowledge of how many pharmacists in the UK are educated in the critical assessment of evidence. A recent paper from the USA did not give cause for optimism. It’s discussed by the excellent US pharmacist, Scott Gavura, at Science-based medicine. The results are truly horrifying.
“Few students disagreed with any CAM therapy. There was the greatest support for vitamins and minerals (94%, mean 4.29) which could include the science-based use these products. But there was strong support for demonstrably ineffective treatments like acupuncture, with 64% agreeing it was acceptable. Even homeopathy, which any pharmacy student with basic medicinal chemistry skills ought to know is absurd, was supported by over 40% of students.”
If the numbers are similar in the UK, the results of the Which? magazine survey are not so surprising. And if they are held by the GPhC Council. their inaction is to be expected. We just don’t know, and perhaps someone should find out.
I suspect that sympathy for quackery may sometimes creep in through that old-fashioned discipline known as pharmacognosy. It is about the botany of medicinal plants, and it’s still taught, despite the fact that very few drugs are now extracted from plants. At times, it gets dangerously close to herbalism. For example, at the School of Pharmacy (now part of UCL) a book is used Fundamentals of Pharmacognosy and Phytotherapy by Michael Heinrich, Joanne Barnes, Simon Gibbons and Elizabeth M. Williamson, ot the Centre for Pharmacognosy and Phytotherapy at the School of Pharmacy. The introductory chapter says.
“TRADITIONAL CHINESE MEDICINE (TCM) The study of TCM is a mixture of myth and fact, stretching back well over 5000 years. At the time, none of the knowledge was written down, apart from primitive inscriptions of prayers for the sick on pieces of tortoise carapace and animal bones, so a mixture of superstition, symbolism and fact was passed down by word of mouth for centuries. TCM still contains very many remedies, which were selected by their symbolic significance rather than proven effects; however, this does not necessarily mean that they are all ‘quack’ remedies!”
Well, not necessarily. But as in most such books, there are good descriptions of the botany, more or less good accounts of the chemical constituents followed by uncritical lists of things that the herb might (or might not) do. The fact that even the US National Institutes of Health quackery branch, NCCAM, doesn’t claim that a single herbal treatment is useful tells you all you need to know.
Joanna Barnes is Associate Professor in Herbal Medicines, School of Pharmacy, University of Auckland, New Zealand. She has written a book, Herbal Medicines (“A useful book for learning holistic medicine”) that is desperately uncritical about the alleged theraputic effectiveness of plants. ("Simon Gibbons is on the editorial board of The Chinese Journal of Natural Medicine. Elizabeth Williamson is editor of the Journal of Phytotherapy Research, a journal that has a strong flavour of herbalism (take the infamous snoring remedy). These people aren’t quacks but they are dangerously tolerant of quacks.
The warning is in the title. "Phytotherapy" is the current euphemism for herbalism. It’s one of those red light words that tells you that what follows is unlikely to be critical. Exeter’s fantasy herbalist, Simon Mills, now describes himself as a phytotherapist. What more warning could you need?
Perhaps this explains why so many pharmacists are unworried by selling things that don’t work. Pharmacy education seems not to include much about the critical assessment of evidence. It should do.
Chemist and Druggist magazine certainly doesn’t help. It continually reinforces the idea that there is a debate about homepathy. There isn’t. And in one of its CPD modules Katherine Gascoigne says
"Homeopathic remedies are available, but are best prescribed by a homeopath"
Ms Gascoigne must be living on another planet.
Conclusions
The main conclusion from all of this is that the General Pharmaceutical Council is almost criminally negligent. It continues to allow pharmacists, Anthony Pinkus among them, to endanger lives. It fails to apply its own declared principles. The members of its Council, and Duncan Rudkin (its chief executive and registrar), are not doing their job.
Individual pharmacists vary a lot, from the superb to those who believe in quackery. Some, perhaps many, are embarrassed by the fact that their employer compels them to sell rubbish. It’s too much to expect that they’ll endanger their mortgage payments by speaking out about it, but the best ones will take you aside and explain that they can’t recommend it.
The GPhC itself is regulated by the Professional Standards Authority, the subject of my last post. We can’t expect anything sensible from them.
In the USA there is a shocking number of pharmacists who seem to believe in quackery. In the UK. nobody knows, though judging by their failure to vote against the daftest of all scams, homeopathy, there is no cause for complacency here.
It seems that there will have to be big improvements in pharmacy education before you can have much confidence in the quality of the advice that you get in a pharmacy.
Follow-up
Yesterday a talk was given at the School of Pharmacy, organised by the “The Centre for Homeopathic Education” (an oxymoron if there ever was one). The flyer had all the usual nonsense. Its mention of “Remedies & Tonics for Cancer Recovery” might well have breached the Cancer Act (1939). When I asked whether the amount received in room rental was sufficient to offest the damage to the reputation of the School of Pharmacy resulting from hosting a nutty (and possible illegal) event, I had the greatest difficulty in extracting any sort of response from the school’s director, Duncan Craig. I’m told that he considers “the policy on space rental to be a UCL management issue, rather than a matter of discussion on scientific ethics with a colleague”. Oh dear.
This article has appeared, in nearly identical form, on the UK Conversation . You can leave comments there or here.
A constitutional monarch is purely ceremonial and plays no part in politics. Well actually in the UK it isn’t quite as simple as that. The first problem is that we have no constitution. Things haven’t changed much since the 19th century when Walter Bagehot said "the Sovereign has, under a constitutional monarchy… three rights—the right to be consulted, the right to encourage, the right to warn."
These are not inconsiderable powers in a country which is meant to be run by elected representatives. But nobody knows how these powers are used: it is all done in secret. Well, almost all. Charles, Prince of Wales, has been unusually public in expressing his views. He told a conference at St James’s Palace “I was accused once of being the enemy of the Enlightenment” “I felt proud of that.” That’s a remarkable point of view for someone who, if he succeeds, will become the patron of that product of the age of enlightenment, the Royal Society.
I have no doubt that Prince Charles means well. He can’t be blamed for his lack of education. But his views on medicine date from a few centuries ago, and he has lost no opportunity to exploit his privileged position to proclaim them.
Euphemisms for quackery
He set up the Prince’s Foundation for Integrated Health (PFIH) to promote his views. ( “Integrated”, in this context, is, of course, just the latest euphemism for “alternative” or “quack”.) When the Foundation collapsed because of a financial scandal in 2010, it was replaced by the “College of Medicine”. The name changed, but not the people behind it. Initially this phoenix was to be named the “College of Integrated Health”, but by this time the prince’s views on medicine had become sufficiently discredited that the word “integrated” was quickly dropped. This might be thought less than frank, but it is just employment of the classic bait and switch technique, beloved by used car salesmen.
His views were well publicised in a PFIH publication, “Complementary Healthcare: a Guide for Patients”. That volume either omitted or misrepresented the evidence about the one question that matters most to patients – does the treatment work or not? It caused me to write a much shorter, but more accurate, version, the Patients’ Guide to Magic Medicine. The PFIH guide was arguably a danger to public health. When, very properly, it was criticised by Edzard Ernst, a letter was sent from from the prince’s private secretary to Ernst’s vice-chancellor, Steve Smith. Instead of defending Ernst’s public spirited action, Smith instituted disciplinary proceedings against Ernst that lasted for a year. The prince had intervened directly in the affairs of the university. Steve Smith was rewarded with a knighthood in 2011.
None of this criticism has dimmed the prince’s enthusiasm for barmy medical ideas. He is well known to write many letters to government ministers to try to persuade them to adopt his ideas in a whole range of areas. In July 2013, the Minister of Health, Jeremy Hunt, visited the prince at Clarence House. The visit was reported to be to persuade the minister to defend homeopathy, though it was more likely to have been to press the case to confer a government stamp of approval on herbalists and traditional Chinese Medicine practitioners by giving them statutory regulation. This is a matter that was recently raised again in parliament by Charles’ greatest ally, David Tredinnick MP (Con, Bosworth) who got into trouble for charging astrology software to expenses. We shall never know what pressure was applied. A ruling of the Information Commissioner judged, reasonably enough, that there was public interest in knowing what influences were being brought to bear on public policy. But the Attorney General overruled the judgement on the grounds that “Disclosure of the correspondence could damage The Prince of Wales’ ability to perform his duties when he becomes King.” That, of course, is exactly what we are worried about.
Influence on politics
The prince’s influence seems to be big in the Department of Health (DH). He was given £37,000 of taxpayers’ money to produce his guide, and an astonishing £900,000 to prepare the ground for the setting up of the hapless self-regulator, the Complementary and Natural Healthcare Council (CNHC, also known as Ofquack). When NHS Choices (itself set up by DH to assess evidence) tried to rewrite its web page about that most discredited of all forms of quackery, homeopathy, officials in DH referred the new advice to Michael Dixon, the medical director of the Prince’s Foundation and, were it not for the Freedom of Information act, the DH would have caused inaccurate information to be provided. The DH has a chief medical officer and two scientific advisors, but prefers to take the advice of the Prince of Wales.
The Prince of Wales’ business, Duchy Originals, has been condemned by the Daily Mail, (of all places) for selling unhealthy foods. And when his business branched into selling quack “detox” and herbal nonsense he found himself censured by both the MHRA and the Advertising Standards Authority (ASA) for making unjustifiable medical claims for these products.
Ainsworth’s homeopathic pharmacy is endorsed by both Prince Charles and the Queen: it has two Royal Warrants. They sell “homeopathic vaccines” for meningitis, measles, rubella and whooping cough. These “vaccines” contain nothing whatsoever so they are obviously a real danger to public health. Despite the fact that Ainsworth’s had already been censured by the ASA in 2011 for selling similar products, Ainsworth’s continued to recommend them with a “casual disregard for the law”. The regulator (the MHRA) failed to step in to stop them until it was eventually stirred into action by a young BBC reporter, Sam Smith, made a programme for BBC South West. Then, at last, the somnolent regulator was stirred into action. The MHRA “told Ainsworths to stop advertising a number of products” (but apparently not to stop making them or selling them). They still sell Polonium metal 30C and Swine Meningitis 36C, and a booklet that recommends homeopathic “vaccination”. Ainsworth’s sales are no doubt helped by the Royal Warrants. The consequence is that people may die of meningitis. In 2011, the MHRA Chief Executive Professor Kent Woods, was knighted.
It runs in the family
The Prince of Wales is not the only member of the royal family to be obsessed with bizarre forms of medicine. The first homeopath to the British royal family, Frederick Quin, was a son of the Duchess of Devonshire (1765-1824). Queen Mary (1865-1953), wife of King George V, headed the fundraising efforts to move and expand the London Homeopathic Hospital.
King George VI was so enthusiastic that in 1948 conferred the royal title on the London Homeopathic Hospital. The Queen Mother loved homeopathy too (there is no way to tell whether this contributed to her need for a colostomy in the 1960s).
The present Queen’s homeopathic physician is Peter Fisher, who is medical director of what, until recently was called the Royal London Homeopathic Hospital (RLHH). In 2010 that hospital was rebranded as the Royal London Hospital for Integrated Medicine (RLHIM) in another unsubtle bait and switch move.
|
The RLHIM is a great embarrassment to the otherwise excellent UCLH Trust. It has been repeatedly condemned by the Advertising Standards Authority for making false claims. As a consequence, it has been forced to withdraw all of its patient information. The patron of the RLHIM is the Queen, not the Prince of Wales. It is hard to imagine that this anachronistic institution would still exist if it were not for the influence, spoken or unspoken, of the Queen. Needless to say we will never be told. |
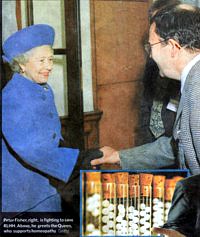 The Queen and Peter Fisher Observer 8 April 2007 |
The attorney general, while trying to justify the secrecy of Charles’ letters, said
“It is a matter of the highest importance within our constitutional framework that the Monarch is a politically neutral figure”.
Questions about health policy are undoubtedly political, and the highly partisan interventions of the prince in the political process make his behaviour unconstitutional. They endanger the monarchy itself. Whether that matters depends on how much you value tradition and how much you value the tourist business generated by the Gilbert & Sullivan flummery at which royals excel.
The least that one can ask of the royal family is that they should not endanger the health of the nation. If I wanted to know the winner of the 2.30 at Ascot, I’d ask a royal. For any question concerning science or medicine I’d ask someone with more education.
Here is some more interesting reading
Michael Baum’s “An open letter to the Prince of Wales: with respect, your highness, you’ve got it wrong”
Gerald Weissman’s essay Homeopathy: Holmes, Hogwarts, and the Prince of Wales.
Channel 4 TV documentary HRH “meddling in politics”
Observer April 2007 "Royals’ favoured hospital at risk as homeopathy backlash gathers pace. The Queen loves it. But alternative medicine centre’s future looks uncertain as more NHS trusts axe funding"
Follow-up
The Scottish Universities Medical Journal asked me to write about the regulation of alternative medicine. It’s an interesting topic and not easy to follow because of the veritable maze of more than twenty overlapping regulators and quangos which fail utterly to protect the public against health fraud. In fact they mostly promote health fraud. The paper is now published, and here is a version with embedded links (and some small updates).
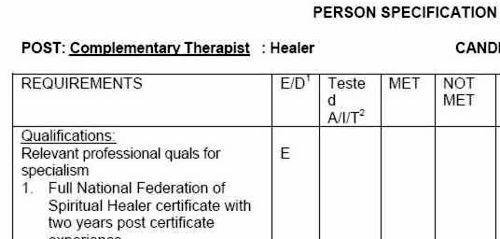
We are witnessing an increasing commercialisation of medicine. It’s really taken off since the passage of the Health and Social Security Bill into law. Not only does that mean having NHS hospitals run by private companies, but it means that “any qualified provider” can bid for just about any service. The problem lies, of course, in what you consider “qualified” to mean. Any qualified homeopath or herbalist will, no doubt, be eligible. University College London Hospital advertised for a spiritual healer. The "person specification" specified a "quallfication", but only HR people think that a paper qualification means that spiritual healing is anything but a delusion.
The vocabulary of bait and switch
First, a bit of vocabulary. Alternative medicine is a term that is used for medical treatments that don’t work (or at least haven’t been shown to work). If they worked, they’d be called “medicine”. The anti-malarial, artemesinin, came originally from a Chinese herb, but once it had been purified and properly tested, it was no longer alternative. But the word alternative is not favoured by quacks. They prefer their nostrums to be described as “complementary” –it sounds more respectable. So CAM (complementary and alternative medicine became the politically-correct euphemism. Now it has gone a stage further, and the euphemism in vogue with quacks at the moment is “integrated” or “integrative” medicine. That means, very often, integrating things that don’t work with things that do. But it sounds fashionable. In reality it is designed to confuse politicians who ask for, say, integrated services for old people.
Put another way, the salespeople of quackery have become rather good at bait and switch. The wikepedia definition is as good as any.
Bait-and-switch is a form of fraud, most commonly used in retail sales but also applicable to other contexts. First, customers are “baited” by advertising for a product or service at a low price; second, the customers discover that the advertised good is not available and are “switched” to a costlier product.
As applied to the alternative medicine industry, the bait is usually in the form of some nice touchy-feely stuff which barely mentions the mystical nonsense. But when you’ve bought into it you get the whole panoply of nonsense. Steven Novella has written eloquently about the use of bait and switch in the USA to sell chiropractic, acupuncture, homeopathy and herbal medicine: "The bait is that CAM offers legitimate alternatives, the switch is that it primarily promotes treatments that don’t work or are at best untested and highly implausible.".
The "College of Medicine" provides a near-perfect example of bait and switch. It is the direct successor of the Prince of Wales’ Foundation for Integrated Health. The Prince’s Foundation was a consistent purveyor of dangerous medical myths. When it collapsed in 2010 because of a financial scandal, a company was formed called "The College for Integrated Health". A slide show, not meant for public consumption, said "The College represents a new strategy to take forward the vision of HRH Prince Charles". But it seems that too many people have now tumbled to the idea that "integrated", in this context, means barmpottery. Within less than a month, the new institution was renamed "The College of Medicine". That might be a deceptive name, but it’s a much better bait. That’s why I described the College as a fraud and delusion.
Not only did the directors, all of them quacks, devise a respectable sounding name, but they also succeeded in recruiting some respectable-sounding people to act as figureheads for the new organisation. The president of the College is Professor Sir Graham Catto, emeritus professor of medicine at the University of Aberdeen. Names like his make the bait sound even more plausible. He claims not to believe that homeopathy works, but seems quite happy to have a homeopathic pharmacist, Christine Glover, on the governing council of his college. At least half of the governing Council can safely be classified as quacks.
So the bait is clear. What about the switch? The first thing to notice is that the whole outfit is skewed towards private medicine: see The College of Medicine is in the pocket of Crapita Capita. The founder, and presumably the main provider of funds (they won’t say how much) is the huge outsourcing company, Capita. This is company known in Private Eye as Crapita. Their inefficiency is legendary. They are the folks who messed up the NHS computer system and the courts computer system. After swallowing large amounts of taxpayers’ money, they failed to deliver anything that worked. Their latest failure is the court translation service.. The president (Catto), the vice president (Harry Brunjes) and the CEO (Mark Ratnarajah) are all employees of Capita.
The second thing to notice is that their conferences and courses are a bizarre mixture of real medicine and pure quackery. Their 2012 conference had some very good speakers, but then it had a "herbal workshop" with Simon Mills (see a video) and David Peters (the man who tolerates dowsing as a way to diagnose which herb to give you). The other speaker was Dick Middleton, who represents the huge herbal company, Schwabe (I debated with him on BBC Breakfast), In fact the College’s Faculty of Self-care appears to resemble a marketing device for Schwabe.
Why regulation isn’t working, and can’t work
There are various levels of regulation. The "highest" level is the statutory regulation of osteopathy and chiropractic. The General Chiropractic Council (GCC) has exactly the same legal status as the General Medical Council (GMC). This ludicrous state of affairs arose because nobody in John Major’s government had enough scientific knowledge to realise that chiropractic, and some parts of osteopathy, are pure quackery,
The problem is that organisations like the GCC function more to promote chiropractic than to regulate them. This became very obvious when the British Chiropractic Association (BCA) decided to sue Simon Singh for defamation, after he described some of their treatments as “bogus”, “without a jot of evidence”.
In order to support Singh, several bloggers assessed the "plethora of evidence" which the BCA said could be used to justify their claims. When, 15 months later, the BCA produced its "plethora" it was shown within 24 hours that the evidence was pathetic. The demolition was summarised by lawyer, David Allen Green, in The BCA’s Worst Day.
In the wake of this, over 600 complaints were made to the GCC about unjustified claims made by chiropractors, thanks in large part to heroic work by two people, Simon Perry and Allan Henness. Simon Perry’s Fishbarrel (browser plugin) allows complaints to be made quickly and easily -try it). The majority of these complaints were rejected by the GCC, apparently on the grounds that chiropractors could not be blamed because the false claims had been endorsed by the GCC itself.
My own complaint was based on phone calls to two chiropractors, I was told such nonsense as "colic is down to, er um, faulty movement patterns in the spine". But my complaint never reached the Conduct and Competence committee because it had been judged by a preliminary investigating committee that there was no case to answer. The impression one got from this (very costly) exercise was that the GCC was there to protect chiropractors, not to protect the public.
The outcome was a disaster for chiropractors, wno emerged totally discredited. It was also a disaster for the GCC which was forced to admit that it hadn’t properly advised chiropractors about what they could and couldn’t claim. The recantation culminated in the GCC declaring, in August 2010, that the mythical "subluxation" is a "historical concept " "It is not supported by any clinical research evidence that would allow claims to be made that it is the cause of disease.". Subluxation was a product of the fevered imagination of the founder of the chiropractic cult, D.D. Palmer. It referred to an imaginary spinal lesion that he claimed to be the cause of most diseases. .Since ‘subluxation’ is the only thing that’s distinguished chiropractic from any other sort of manipulation, the admission by the GCC that it does not exist, after a century of pretending that it does, is quite an admission.
The President of the BCA himself admitted in November 2011
“The BCA sued Simon Singh personally for libel. In doing so, the BCA began one of the darkest periods in its history; one that was ultimately to cost it financially,”
As a result of all this, the deficiencies of chiropractic, and the deficiencies of its regulator were revealed, and advertisements for chiropractic are somewhat less misleading. But this change for the better was brought about entirely by the unpaid efforts of bloggers and a few journalists, and not at all by the official regulator, the GCC. which was part of the problem. not the solution. And it was certainly not helped by the organisation that is meant to regulate the GCC, the Council for Health Regulatory Excellence (CHRE) which did nothing whatsoever to stop the farce.
At the other end of the regulatory spectrum, voluntary self-regulation, is an even worse farce than the GCC. They all have grand sounding "Codes of Practice" which, in practice, the ignore totally.
The Society of Homeopaths is just a joke. When homeopaths were caught out recommending sugar pills for prevention of malaria, they did nothing (arguably such homicidal advice deserves a jail sentence).
The Complementary and Natural Healthcare Council (CNHC) is widely know in the blogosphere as Ofquack. I know about them from the inside, having been a member of their Conduct and Competence Committee, It was set up with the help of a £900,000 grant from the Department of Health to the Prince of Wales, to oversee voluntary self-regulation. It fails utterly to do anything useful.. The CNHC code of practice, paragraph 15 , states
“Any advertising you undertake in relation to your professional activities must be accurate. Advertisements must not be misleading, false, unfair or exaggerated”.
When Simon Perry made a complaint to the CNHC about claims being made by a CNHC-registered reflexologist, the Investigating Committee upheld all 15 complaints. But it then went on to say that there was no case to answer because the unjustified claims were what the person had been taught, and were made in good faith.
This is precisely the ludicrous situation which will occur again and again if reflexologists (and many other alternative therapies) are “accredited”. The CNHC said, correctly, that the reflexologist had been taught things that were not true, but then did nothing whatsoever about it apart from toning down the advertisements a bit. They still register reflexologists who make outrageously false claims.
Once again we see that no sensible regulation is possible for subjects that are pure make-believe.
The first two examples deal (or rather, fail to deal) with regulation of outright quackery. But there are dozens of other quangos that sound a lot more respectable.
European Food Standards Agency (EFSA). One of the common scams is to have have your favourite quack treatment classified as a food not as a medicine. The laws about what you can claim have been a lot laxer for foods. But the EFSA has done a pretty good job in stopping unjustified claims for health benefits from foods. Dozens of claims made by makers of probiotics have been banned. The food industry, needless to say, objects very strongly to be being forced to tell the truth. In my view, the ESFA has not gone far enough. They recently issued a directive about claims that could legally be made. Some of these betray the previously high standards of the EFSA. For example you are allowed to say that "Vitamin C contributes to the reduction of tiredness and fatigue" (as long as the product contains above a specified amount of Vitamin C. I’m not aware of any trials that show vitamin C has the slightest effect on tiredness or fatigue, Although these laws do not come into effect until December 2012, they have already been invoked by the ASA has a reason not to uphold a complaint about a multivitamin pill which claimed that it “Includes 8 nutrients that can contribute to the reduction in tiredness and fatigue”
The Advertising Standards Authority (ASA). This is almost the only organisation that has done a good job on false health claims. Their Guidance on Health Therapies & Evidence says
"Whether you use the words ‘treatment’, ‘treat’ or ‘cure’, all are likely to be seen by members of the public as claims to alleviate effectively a condition or symptom. We would advise that they are not used"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
"Before and after’ studies with little or no control, studies without human subjects, self-assessment studies and anecdotal evidence are unlikely to be considered acceptable"
They are spot on.
The ASA’s Guidance for Advertisers of Homeopathic Services is wonderful.
"In the simplest terms, you should avoid using efficacy claims, whether implied or direct,"
"To date, the ASA has have not seen persuasive evidence to support claims that homeopathy can treat, cure or relieve specific conditions or symptoms."
That seems to condemn the (mis)labelling allowed by the MHRA as breaking the rules.. Sadly, though, the ASA has no powers to enforce its decisions and only too often they are ignored. The Nightingale collaboration has produced an excellent letter that you can hand to any pharmacist who breaks the rules
The ASA has also judged against claims made by "Craniosacral therapists" (that’s the lunatic fringe of osteopathy). They will presumably uphold complaints about similar claims made (I’m ashamed to say) by UCLH Hospitals.
The private examination company Edexcel sets exams in antiscientific subjects, so miseducating children. The teaching of quackery to 16 year-olds has been approved by a maze of quangos, none of which will take responsibility, or justify their actions. So far I’ve located no fewer than eight of them. The Office of the Qualifications and Examinations Regulator (OfQual), Edexcel, the Qualifications and Curriculum Authority (QCA), Skills for Health, Skills for Care, National Occupational Standards (NOS), private exam company VTCT and the schools inspectorate, Ofsted.. Asking any of these people why they approve of examinations in imaginary subjects meets with blank incomprehension. They fail totally to protect tha public from utter nonsense.
The Department of Education has failed to do anything about the miseducation of children in quackery. In fact it has encouraged it by, for the first time, giving taxpayers’ money to a Steiner (Waldorf) school (at Frome, in Somerset). Steiner schools are run by a secretive and cult-like body of people (read about it). They teach about reincarnation, karma, gnomes, and all manner of nonsense, sometimes with unpleasant racial overtones. The teachers are trained in Steiner’s Anthroposophy, so if your child gets ill at school they’ll probably get homeopathic sugar pills. They might well get measles or mumps too, since Steiner people don’t believe in vaccination.
Incredibly, the University of Aberdeen came perilously close to appointing a chair in anthroposophical medicine. This disaster was aborted by bloggers, and a last minute intervention from journalists. Neither the university’s regulatory mechanisms. nor any others, seemed to realise that a chair in mystical barmpottery was a bad idea.
Trading Standards offices and the Office of Fair Trading.
It is the statutory duty of Trading Standards to enforce the Consumer Protection Regulations (2008) This European legislation is pretty good. it caused a lawyer to write " Has The UK Quietly Outlawed “Alternative” Medicine?". Unfortunately Trading Standards people have consistently refused to enforce these laws. The whole organisation is a mess. Its local office arrangement fails totally to deal with the age of the internet. The situation is so bad that a group of us decided to put them to the test. The results were published in the Medico-Legal Journal, Rose et al., 2012. "Spurious Claims for Health-care Products: An Experimental Approach to Evaluating Current UK Legislation and its Implementation". They concluded "EU directive 2005/29/EC is
largely ineffective in preventing misleading health claims for consumer products in
the UK"
Skills for Health is an enormous quango which produces HR style "competences" for everything under the son. They are mostly quite useless. But those concerned with alternative medicine are not just useless. They are positively harmful. Totally barmy. There are competences and National Occupational Standards for every lunatic made-up therapy under the sun. When I phoned them to discover who’d written them, I learned that the had been drafted by the Prince of Wales’ Foundation for Magic Medicine. And when I joked by asking if they had a competence for talking to trees, I was told, perfectly seriously, “You’d have to talk to LANTRA, the land-based organisation for that.”
That was in January 2008. A lot of correspondence with the head of Skills for Health got nowhere at all. She understood nothing and it hasn’t improved a jot.
This organisation costs a lot of taxpayers’ money and it should have been consigned to the "bonfire of the quangos" (but of course there was no such bonfire in reality). It is a disgrace.
The Quality Assurance Agency (QAA) is supposed to ensure the quality of university courses. In fact it endorses courses in nonsense alternative medicine and so does more harm than good. The worst recent failure of the QAA was in the case of the University of Wales: see Scandal of the University of Wales and the Quality Assurance Agency. The university was making money by validating thousands of external degrees in everything from fundamentalist theology to Chinese Medicine. These validations were revealed as utterly incompetent by bloggers, and later by BBC Wales journalist Ciaran Jenkins (now working for Channel 4).
The mainstream media eventually caught up with bloggers. In 2010, BBC1 TV (Wales) produced an excellent TV programme that exposed the enormous degree validation scam run by the University of Wales. The programme can be seen on YouTube (Part 1, and Part 2). The programme also exposed, incidentally, the uselessness of the Quality Assurance Agency (QAA) which did nothing until the scam was exposed by TV and blogs. Eventually the QAA sent nine people to Malaysia to investigate a dodgy college that had been revealed by the BBC. The trip cost £91,000. It could have been done for nothing if anyone at the QAA knew how to use Google.
The outcome was that the University of Wales stopped endorsing external courses, and it was soon shut down altogether (though bafflingly, its vice-chancellor, Marc Clement was promoted). The credit for this lies entirely with bloggers and the BBC. The QAA did nothing to help until the very last moment.
Throughout this saga Universities UK (UUK), has maintained its usual total passivity. They have done nothing whatsoever about their members who give BSc degrees in anti-scientific subjects. (UUK used to known as the Committee of Vice-Chancellors and Principals).
Council for Health Regulatory Excellence (CHRE), soon to become the PSAHSC,
Back now to the CHRE, the people who failed so signally to sort out the GCC. They are being reorganised. Their consultation document says
"The Health and Social Care Act 20122 confers a new function on the Professional Standards Authority for Health and Social Care (the renamed Council for Healthcare Regulatory Excellence). From November 2012 we will set standards for organisations that hold voluntary registers for people working in health and social care occupations and we will accredit the register if they meet those standards. It will then be known as an ‘Accredited Register’. "
They are trying to decide what the criteria should be for "accreditation" of a regulatory body. The list of those interested has some perfectly respectable organisations, like the British Psychological Society. It also contains a large number of crackpot organisations, like Crystal and Healing International, as well as joke regulators like the CNHC.
They already oversee the Health Professions Council (HPC) which is due to take over Herbal medicine and Traditional Chinese Medicine, with predictably disastrous consequences.
Two of the proposed criteria for "accreditation" appear to be directly contradictory.
Para 2.5 makes the whole accreditation pointless from the point of view of patients
2.5 It will not be an endorsement of the therapeutic validity or effectiveness of any particular discipline or treatment.
Since the only thing that matters to the patient is whether the therapy works (and is safe), accrediting of organisations that ignore this will merely give the appearance of official approval of crystal healing etc etc. This appears to contradict directly
A.7 The organisation can demonstrate that there either is a sound knowledge base underpinning the profession or it is developing one and makes that explicit to the public.
A "sound knowledge base", if it is to mean anything useful at all, means knowledge that the treatment is effective. If it doesn’t mean that, what does it mean?
It seems that the official mind has still not grasped the obvious fact that there can be no sensible regulation of subjects that are untrue nonsense. If it is nonsense, the only form of regulation that makes any sense is the law.
Please fill in the consultation. My completed return can be downloaded as an example, if you wish.
Medicines and Healthcare products Regulatory Agency (MHRA) should be a top level defender of truth. Its strapline is
"We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
The MHRA did something (they won’t tell me exactly what) about one of the most cruel scams that I’ve ever encountered, Esperanza Homeopathic Neuropeptide, peddled for multiple sclerosis, at an outrageous price ( £6,759 for 12 month’s supply). Needless to say there was not a jot of evidence that it worked (and it wasn’t actually homeopathic).
Astoundingly, Trading Standards officers refused to do anything about it.
The MHRA admit (when pushed really hard) that there is precious little evidence that any of the herbs work, and that homeopathy is nothing more than sugar pills. Their answer to that is to forget that bit about "ensuring that medicines … work"
Here’s the MHRA’s Traditional Herbal Registration Certificate for devils claw tablets.

The wording "based on traditional use only" has to be included because of European legislation. Shockingly, the MHRA have allowed them to relegate that to small print, with all the emphasis on the alleged indications. The pro-CAM agency NCCAM rates devil’s claw as "possibly effective" or "insufficient evidence" for all these indications, but that doesn’t matter because the MHRA requires no evidence whatsoever that the tablets do anything. They should, of course, added a statement to this effect to the label. They have failed in their duty to protect and inform the public by allowing this labelling.
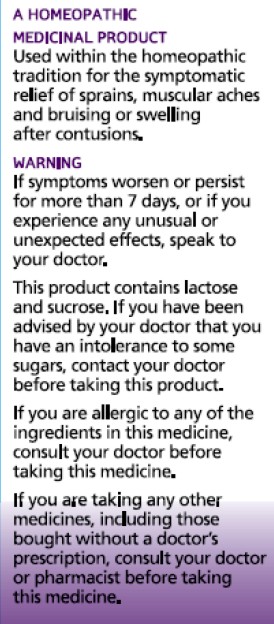
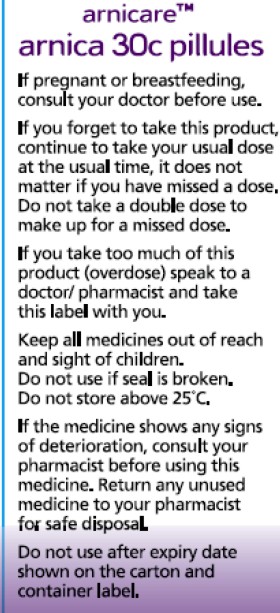
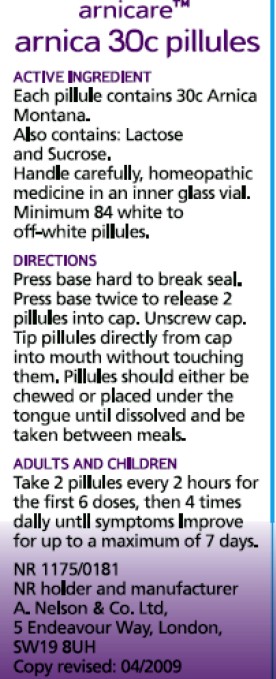
But it gets worse. Here is the MHRA’s homeopathic marketing authorisation for the homeopathic medicinal product Arnicare Arnica 30c pillules
It is nothing short of surreal.
|
|
Since the pills contain nothing at all, they don’t have the slightest effect on sprains, muscular aches or bruising. The wording on the label is exceedingly misleading.
If you "pregnant or breastfeeding" there is no need to waste you doctor’s time before swallowing a few sugar pills.
"Do not take a double dose to make up for a missed one". Since the pills contain nothing, it doesn’t matter a damn.
"If you overdose . . " it won’t have the slightest effect because there is nothing in them
And it gets worse. The MHRA-approved label specifies ACTIVE INGREDIENT. Each pillule contains 30c Arnica Montana
No, they contain no arnica whatsoever.
|
|
It truly boggles the mind that men with dark suits and lots of letters after their names have sat for hours only to produce dishonest and misleading labels like these.
When this mislabeling was first allowed, it was condemned by just about every scientific society, but the MHRA did nothing.
The Nightingale Collaboration.
This is an excellent organisation, set up by two very smart skeptics, Alan Henness and Maria MacLachlan. Visit their site regularly, sign up for their newsletter Help with their campaigns. Make a difference.
Conclusions
The regulation of alternative medicine in the UK is a farce. It is utterly ineffective in preventing deception of patients.
Such improvements as have occurred have resulted from the activity of bloggers, and sometime the mainstream media. All the official regulators have, to varying extents, made things worse.
The CHRE proposals promise to make matters still worse by offering "accreditation" to organisations that promote nonsensical quackery. None of the official regulators seem to be able to grasp the obvious fact that is impossible to have any sensible regulation of people who promote nonsensical untruths. One gets the impression that politicians are more concerned to protect the homeopathic (etc, etc) industry than they are to protect patients.
Deception by advocates of alternative medicine harms patients. There are adequate laws that make such deception illegal, but they are not being enforced. The CHRE and its successor should restrict themselves to real medicine. The money that they spend on pseudo-regulation of quacks should be transferred to the MHRA or a reformed Trading Standards organisation so they can afford to investigate and prosecute breaches of the law. That is the only form of regulation that makes sense.
Follow-up
The shocking case of the continuing sale of “homeopathic vaccines” for meningitis, rubella, pertussis etc was highlighted in an excellent TV programme by BBC South West. The failure of the MHRA and the GPC do take any effective action is a yet another illustration of the failure of regulators to do their job. I have to agree with Andy Lewis when he concludes
“Children will die. And the fault must lie with Professor Sir Kent Woods, chairman of the regulator.”
Since writing about anti-scientific degrees in Nature (March 2007), much has been revealed about the nonsense that is taught on these degrees. New Year’s day seems like a good time to assess how far we’ve got, five years on.
At the beginning of 2007 UCAS (the universities central admission service) offered 45 different BSc degrees in quackery, at 16 universities.
Now there are only 24 such degrees.
If you exclude chiropractic and osteopathy, which all run at private colleges, with some sort of "validation" from a university, there are now only 18 BSc/MSc courses being offered in eight universities.
Degrees in homeopathy, naturopathy and "nutritional therapy", reflexology and aromatherapy have vanished altogether from UCAS.
In the race to provide BScs in anti-science, Middlesex University has now overhauled the long-standing leader, Westminster, by a short head.
 Michael Driscoll, vice-chancellor of Middlesex |
|
Let’s see what’s gone.
The University of Central Lancashire (UCLAN) was the first to see sense. In August 2008 they announced closure of their “BSc” degree in homeopathy. On September 2008 they announced an internal review of their courses in homeopathy. herbalism and acupuncture. The report of this review closed down all of them in July 2009. I first asked for their teaching materials in July 2006. I finally got them in December 2010, after winning an appeal to the Information Commissioner, and then winning an appeal against that decision at an Information tribunal . By the time I got them, the course had been closed for over two years. That is just as well, because it turned out that UCLAN’s students were being taught dangerous nonsense. No wonder they tried so hard to conceal it.
Salford University was the next to go. They shut down their courses in complementary medicine, homeopathy and acupuncture. In January 2009 they announced " they are no longer considered “a sound academic fit” ". Shortly afterwards. a letter appeared in The Times from three heavyweights (plus me) congratulating the vice-chancellor on his decision.
University of Westminster
For many years, Westminster was the biggest supplier of BSc degrees in quackery. At the beginning of 2007 they offered 14 different BSc degrees in homeopathy, naturopathy, nutritional therapy, "complementary therapies", (western) herbal medicine and traditional Chinese medicine with acupuncture. Some of their courses were so bizarre that some of the students and even staff sent me slides which taught things like "amethysts emit high Yin energy". Like UCLAN, Westminster also held an internal review. Unlike UCLAN it came to the absurd conclusion that all would be well if they injected more science into the courses. The incompetence of the review meant that those who wrote it hadn’t noticed that if you try to put science into homeopathy or naturopathy, the whole subject vanishes in a puff of smoke. Nevertheless Westminster closed down entry to BSc homeopathy in March 2009 (though the subject remained as part of other courses).
Three years after the Nature article, all five BSc homeopathy degrees had shut their doors.
During 2011, Westminster shut down Naturopathy, Nutritional therapy, Therapeutic bodywork and Complementary Medicine. See, for example,
More dangerous nonsense from the University of Westminster: when will Professor Geoffrey Petts do something about it?
Now Westminster has only four courses in two subjects. They still teach some dangerous and untrue things, but I suspect the writing is on the wall for these too.
I have seen a document, dated 11 April 2011, which states
“The following courses have been identified as ‘at risk’ (School definition) and will be discussed at the APRG and University Review Group2, due to poor recruitment and high cost of delivery:
Integrated Health Scheme: BSc Complementary Medicine, Naturopathy; BSc Chinese Medicine; BSc Nutritional Therapy; BSc Herbal Medicine”
All but Chinese medicine and Herbal medicine have already gone. Almost there.
University of Wales
Since my first post in 2008 about the validation scam operated by the University of Wales, and some good investigations by BBC Wales TV, the outcome was the most spectacular so far. The entire institution collapsed. They no longer "validate" external degrees at dodgy business colleges, loony religious colleges or magic medicine colleges.
Another worthless validation: the University of Wales and nutritional therapy (October 2008) This is a ‘degree’ in nutrtional therapy. It is even more hilarious than usual, but it passed the validation anyway.
Scandal of the University of Wales and the Quality Assurance Agency (November 2010). This post followed the BBC Wales TV programme. At last the QAA began to notice, yet further confirmation of its utter ineptitude.
The University of Wales disgraced (but its vice chancellor is promoted) (October, 2011) The eventual collapse of the university was well-deserved. But it is very weird that the people who were responsible for it have still got their jobs. In fact the vice-chancellor, Marc Clement, was promoted despite his mendacious claim to be unaware of what was going on.
It remains to be seen how many of the many quack courses that were validated by the University of Wales will be taken on by other universities. The McTimoney College of Chiropractic is owned by BPP University (so much for their quality control, as explained in Private Eye). but still claims to be validated by Wales until 2017.
Some of the more minor players
Edinburgh Napier University. After an FOI request (rejected), Napier closed their herbal medicine degree in 2010.
Hot and cold herbal nonsense from Napier University Edinburgh: another course shuts. (June 2010)
As expected, the Scottish Information Commissioner agreed with that for England and Wales and ordered material to be sent. Edinburgh Napier University teaches reflexology, aromatherapy and therapeutic touch. Scottish Information Commissioner says you should know. Some of the horrors so discovered appeared in Yet more dangerous nonsense inflicted on students by Edinburgh Napier University. The embarrassment seems to have worked. Their remaining degrees in aromatherapy and reflexology have now vanished from UCAS too. All that remains is a couple of part time “Certificates of Credit” for aromatherapy and reflexology
Anglia Ruskin Univerity Not only have BSc degrees gone in aromatherapy and reflexology, but their midwifery degree now states "We are unable to accept qualifications in aromatherapy, massage and reflexology."
University of Derby Reflexology and aromatherapy have gone, though doubtless Spa management therapies have much nonsense left
University of Greenwich. BSc in Complementary Therapies (Nutritional Health) and BSc in Complementary Therapies (Nutritional Health) have been shut. The BSc Acupuncture is listed on their web site but it is under review, and is not listed in UCAS for 2012. (Acupuncture is run at International College of Oriental medicine, validated by Greenwich.). Only osteopathy (MOst) is still running, and that is a validation of an external course run at The European School of Osteopathy, in Maidstone
Thames Valley University was renamed the University of West London in 2010. The nonsense that was run there (e.g. Nutritional Fairy Tales from Thames Valley University) seems to have vanished. Their previous alt med guru, Nicola Robinson, appears now to be at London South Bank University (ranked 116 out of the 116 UK universities)
What’s left?
Chiropractic Surprisingly, given the total discreditation of chiropractic in the wake of the Simon Singh affair, and the internecine warfare that followed it, none of the chiropractic courses have shut yet. Some are clearly in trouble, so watch this space.
Osteopathy has also had no course closures since 2007. Like chiropractic it also suffers from internecine warfare. The General Osteopathic Council refuses to disown the utter nonsense of "craniosacral" osteopathy. But the more sensible practitioners do so and are roughly as effective as physiotherapists (though there are real doubts about how effective that is).
Excluding chiropractic and osteopathy, this is all that’s left. It now consists almost entirely of Chinese medicine and a bit of herbal.
Glyndwr university (Known as North East Wales Institute until 2008) Ranked 104 out of 116 UK universities
BSc Acupuncture (B341) BSc
BSc Complementary Therapies for Healthcare (B343)
Cardiff Metropolitan University (UWIC) (Known as University of Wales Institute Cardiff (UWIC) until Nov 2011.) The vice-chancellor of Cardiff Metropolitan, Antony Chapman, is in the QAA’s board of directors, so perhaps it isn’t surprising that the QAA has done nothing.
BSc Complementary Therapies (3 years) (B390)
BSc Complementary Therapies (4 yrs inc Foundation) (B300)
University of Lincoln
Acupuncture (B343) 3FT Hon BSc
Herbal Medicine (B342) 3FT Hon BSc
University of East London Ranked 113 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
London South Bank University Ranked 116 out of 116 UK universities
Acupuncture (B343) 4FT Deg MCM
The Manchester Metropolitan University Ranked 93 out of 116 UK universities
Acupuncture (B343) 3FT Hon BSc
Middlesex University
Acupuncture (B348) 3FT Hon BSc
Ayurvedic Medicine (A900) 4FT Oth MCM
Herbal Medicine (B347) 3FT Hon BSc
Traditional Chinese Medicine (BT31) 4FT Hon BSc
University of Westminster
Chinese Medicine: Acupuncture (B343) 3FT Hon BSc
Chinese Medicine: Acupuncture with Foundation (B341) 4FT/5FT Hon BSc/MSci
Herbal Medicine (B342) 3FT Hon BSc
Herbal Medicine with Foundation Year (B340) 4FT/5FT Hon BSc/MSci
It seems that acupuncture hangs on in universities that are right at the bottom of the rankings.
Manchester Metropolitan gets the booby prize for actually starting a new course, just as all around are closing theirs. Dr Peter Banister, who was on the committee that approved the course (but now retired), has told me ” I am sceptical in the current economic climate whether it will prove to be successful”. Let’s hope he’s right.
But well done Westminster. Your position as the leader in antiscientific degrees has now been claimed by Middlesex University. Their "degrees" in Ayurveda mark out Middlesex University as the new King of Woo.
Over to you, Professor Driscoll. As vice-chancellor of Middlesex University, the buck stops with you.
Both still teach Chinese and herbal medicine, which are potentially dangerous. There is not a single product from either that has marketing authorisation from the MHRA, though the MHRA has betrayed its trust by allowing misleading labelling of herbal medicines without requiring any evidence whatsoever that they work, see, for example
Why degrees in Chinese medicine are a danger to patients
More quackedemia. Dangerous Chinese medicine taught at Middlesex University
Why does the MHRA refuse to label herbal products honestly? Kent Woods and Richard Woodfield tell me
Sub-degree courses
In contrast to the large reduction in the number of BSc and MSc degrees, there has actually been an increase in two year foundation degrees and HND courses in complementary medicine, at places right near the bottom of the academic heap. The subject is sinking to the bottom. With luck it will vanish entirely from universities before too long.
Research-intensive Universities
Although all of the degrees in magic medicine are from post-1992 universities, the subject has crept into more prestigious universities. Of these, the University of Southampton is perhaps the worst, because of the presence of George Lewith, and his defender, Stephen Holgate. Others have staunch defenders of quackery, including the University of Warwick, University of Edinburgh and St Batholomew’s.
Why have all these courses closed?
One reason is certainly the embarrassment caused by exposure of what’s taught on the courses. Professors Petts (Westminster) and Driscoll (Middlesex) must be aware that googling their names produces references to this and other skeptical blogs on the front page. Thanks to some plain brown emails, and, after a three year battle, the Freedom of Information Act, it has been possible to show here the nonsense that has been foisted on students by some universities. Not only is this a burden on the taxpayer, but, more importantly, some of it is a danger to patients.
When a course closes, it is often said that it is because of falling student numbers (though UCLAN and Salford did not use that excuse). Insofar as that is true, the credit must go to the whole of the skeptical movement that has grown so remarkably in the last few years. Ben Goldacre’s "ragged band of bloggers" have produced a real change in universities and in society as a whole.
The people who should have done the job have either been passive or an active hindrance. The list is long. Vice-chancellors and Universities UK (UUK), the Quality Assurance Agency (QAA), the Hiigher Education Funding Council England (HEFCE), Skills for Health, the Medicines and Health Regulatory Authority ( MHRA) , the Health Professions Council (HPC), the Department of Health, the Prince of Wales and his reincarnated propaganda organisation, the "College of Medicine", the King’s Fund, the Universities and Colleges Union (UCU), OfQual, Edexcel, National Occupational Standards and Qualifications and the Curriculum Authority (QCA).
Whatever happened to that "bonfire of the quangos"?
Follow-up
2 January 2012 The McTimoney College of Chiropractic (owned by BPP University) claims that its “validation” by the University of Wales will continue until 2017. This contradicts the statement from UoW. Watch this space.
3 January 2012. Thanks to Neil O’Connell for drawing my attention to a paper in Pain. The paper is particularly interesting because it comes from the Southampton group which has previously been sympathetic to acupuncture. Its authors include George Lewith. It shows, yet again that there is no detectable difference between real and sham acupuncture treatment. It also shows that the empathy of the practitioner has little effect: in fact the stern authoritarian practitioner may have been more effective.
Patients receiving acupuncture demonstrated clinically important improvements from baseline (i.e., a 29.5% reduction in pain), but despite this, acupuncture has no specific efficacy over placebo for this group of patients. The clinical effect of acupuncture treatment and associated controls is not related to the use of an acupuncture needle, nor mediated by empathy, but is practitioner related and may be linked to the perceived authority of the practitioner.”
Sadly. the trial didn’t include a no-treatment group, so it is impossible to say how much of the improvement is regression to the mean and how much is a placebo effect. The authors admit that it could be mostly the former.
Surely now the misplaced confidence in acupuncture shown by some medical and university people must be in tatters.
In yet another sign that even acupuncture advovates are beginning to notice that it doesn’t work, a recent article Paradoxes in Acupuncture Research: Strategies for Moving Forward, shows some fascinating squirming.
3 January 2012. The Daily Telegraph has carried a piece about closure of university courses, written by Michael Hanlon. On 31 January they carried a much longer piece.
3 January 2012. It is a great pity that some physiotherapists seem to have fallen hook, line and sinker for the myths of acupuncture. Physiotherapists are, by and large, the respectable face of manipulative therapy. Their evidence base is certainly not all one would wish, but at least they are free of the outrageous mumbo humbo of chiropractors. Well, most of them are, but not the Acupuncture Association of Chartered Physiotherapists (AACP), or, still worse, The Association of Chartered Physiotherapists in Energy Medicine, a group that is truly away with the fairies. These organisations are bringing a very respectable job into disrepute. And the Health Professions Council, which is meant to be their regulator, has, like most regulators, done nothing whatsoever to stop it.
5 January 2012. Times Higher Education gives a history of the demise of the University of Wales, Boom or Bust. It’s a useful timeline, but like so many journalists, it’s unwilling to admit that bloggers were on to the problem long before the BBC, never mind the QAA.
There was also a leader on the same topic, Perils of the export business. It again fails to take the QAA to task for its failures.
Interviews for Deutsche Welle and Middle East Broadcasting Center TV.
17 January 2012 Another question answered. I just learned that the ludicrous course in Nutritional Therapy, previously validated by the University of Wales (and a contributor to its downfall), is now being validated by, yes, you guessed, Middlesex University. Professor Driscoll seems determined to lead his univerity to the bottom of the academic heap. His new partnership with the Northern college of Acupuncture is just one of a long list of validations that almost rivals that of the late University of Wales. The course has, of course, an enthusiastic testimonial, from a student. It starts
I work full time as a team leader for a pension company but I am also a kinesiologist and work in my spare time doing kinesiology, reiki and Indian head massage.
Evidently she’s a believer in the barmiest and totally disproved forms of magic medicine. And Middlesex University will give her a Master of Science degree. I have to say I find it worrying that she’s a team leader for a pension company. Does she also believe in the value of worthless derivatives. I wonder?
18 January 2012. the story has gone international, with an interview that I did for Deutsche Welle, UK universities drop alternative medicine degree programs. I’m quoted as saying “They’re dishonest, they teach things that aren’t true, and things that are dangerous to patients in some cases”. That seems fair enough.
There is also an interesting item from July 2010 about pressure to drop payment for homeopathy by German health insurance
31 January 2012
The Daily Telegraph carried a prominent 1200 word account (the title wasn’t mine). The published version was edited slightly.
More boring politics, but it matters. The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register should normally be through a Bachelor degree with Honours
For the background on this appalling report, see earlier posts.
A very bad report: gamma minus for the vice-chancellor
The Times (blame subeditor for the horrid title), and some follow up on the Times piece
The Health Professions Council breaks its own rules: the result is nonsense
Chinese medicine -acupuncture gobbledygook revealed
Consultation opens on the Pittilo report: help stop the Department of Health making a fool of itself
Why degrees in Chinese medicine are a danger to patients
The Department of Health consultation shuts on November 2nd. If you haven’t responded yet, please do. It would be an enormous setback for reason and common sense if the government were to give a stamp of official approval to people who are often no more than snake-oil salesman.
Today I emailed my submission to the Pittilo consultation to the Department of Health, at HRDListening@dh.gsi.gov.uk
The submission
I sent the following documents, updated versions of those already posted earlier.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
- An example of dangerous (and probably illegal) claims that are routinely made by TCM practitioners [download pdf]f
I also completed their questionnaire, despite its deficiencies. In case it is any help to anyone, this is what I said:
The questionnaire
Q1: What evidence is there of harm to the public currently as a result of the activities of acupuncturists, herbalists and traditional Chinese medicine practitioners? What is its likelihood and severity?
Harm
No Harm
Unsure
Comment
The major source of harm is the cruel deception involved in making false claims of benefit to desperate patients. This applies to all three.
In the case of herbal and TCM there is danger from toxicity because herbal preparations are unstandardised so those that do contain an active ingredient are given in an unknown dose. This is irresponsible and dangerous (but would not be changed by the proposals for regulation).
In addition TCM suffers from recurrent problems of contamination with heavy metals, prescription drugs and so on. Again this would not be the business of the proposed form of regulation.
Q2: Would this harm be lessened by statutory regulation? If so, how?
Yes
No
Unsure
The proposed form of regulation would be no help at all. The HPC has already said that it is not concerned with whether or not the drug works, and, by implication, does not see itself as preventing false health claims (just as the GCC doesn’t do this). False claims are the responsibility of Trading Standards who are meant to enforce the Consumer Protection Unfair Trading Regulations (May 2008), though they do not at present enforce them very effectively. Also Advertisng Standards. The proposed regulation would not help, and could easily hinder public safety as shown by the fact that the GCC has itself been referred to the Advertisng Standards Authority.
The questions of toxicity and contamination are already the responsibility of Trading Standards and the MHRA. Regulation by the HPC would not help at all. The HPC is not competent to deal with such questions.
Q3: What do you envisage would be the benefit to the public, to practitioners and to businesses, associated with introducing statutory regulation?
Significant benefit
Some benefit
No benefit
Unsure
This question is badly formulated because the answer is different according to whether you are referring to the public, to practitioners or to businesses.
The public would be endangered by the form of regulation that is proposed, as is shown very clearly by the documents that I have submitted separately.
In the case of practitioners and businesses, there might be a small benefit, if the statutory regulation gave the impression that HM and TCM had government endorsement and must therefore be safe and effective.
There is also one way that the regulation could harm practitioners and businesses. If the HPC received a very large number of complaints about false health claims, just as the GCC has done recently, not only would it cost a large amount of money to process the claims, but the attendant bad publicity could harm practitioners. It is quite likely that this would occur since false claims to benefit sick people are rife in the areas of acupuncture, HM and TCM.
Q4: What do you envisage would be the regulatory burden and financial costs to the public, to practitioners, and to businesses, associated with introducing statutory regulation? Are these costs justified by the benefits and are they proportionate to the risks? If so, in what way?
Justified
Not Justified
Unsure
Certainly not justified. Given that I believe that the proposed form of regulation would endanger patients, no cost at all would be justified. But even if there were a marginal benefit, the cost would be quite unjustified. The number of practitioners involved is very large. It would involve a huge expansion of an existing quango, at a time when the government is trying to reduce the number of quangos. Furthermore, if the HPC were flooded with complaints about false health claims, as the GCC has been, the costs in legal fees could be enormous.
Q5: If herbal and TCM practitioners are subject to statutory regulation, should the right to prepare and commission unlicensed herbal medicines be restricted to statutorily regulated practitioners?
Yes
No
Unsure
I don’t think it would make much difference. The same (often false) ideas are shared by all HM people and that would continue to be the same with or without SR.
Q6: If herbal and TCM practitioners are not statutorily regulated, how (if at all) should unlicensed herbal medicines prepared or commissioned by these practitioners be regulated?
They could carry on as now, but the money that would have been spent on SR should instead be used to give the Office of Trading Standards and the MHRA the ability to exert closer scrutiny and to enforce more effectively laws that already exist. Present laws, if enforced, are quite enough to protect the public.
Q7: What would be the effect on public, practitioners and businesses if, in order to comply with the requirements of European medicines legislation, practitioners were unable to supply manufactured unlicensed herbal medicines commissioned from a third party?
Significant effect
Some effect
No effect
Unsure
European laws,especialliy in food area, are getting quite strict about the matters of efficacy. The proposed regulation, which ignores efficacy, could well be incompatible with European law, if not now, then soon. This would do no harm to legitimate business though it might affect adversely businesses which make false claims (and there are rather a lot of the latter).
Q8: How might the risk of harm to the public be reduced other than by orthodox statutory regulation? For example by voluntary self-regulation underpinned by consumer protection legislation and by greater public awareness, by accreditation of voluntary registration bodies, or by a statutory or voluntary licensing regime?
Voluntary self-regulation
Accreditation of voluntary bodies
Statutory or voluntary licensing
Unsure
I disagree with the premise, for reasons given in detail in separate documents. I believe that ‘orthodox statutory regulation’, if that means the Pittilo proposals, would increase, not decrease, the risk to the public. Strengthening the powers of Trading Standards, the MHRA and such consumer protection legislation would be far more effective in reducing risk to the public than the HPC could ever be. Greater public awareness of the weakness of the evidence for the efficacy of these treatments would obviously help too, but can’t do the job on its own.
Q10: What would you envisage would be the benefits to the public, to practitioners, and to businesses, for the alternatives to statutory regulation outlined at Question 8?
It depends on which alternative you are referring to. The major benefit of enforcement of existing laws by Trading Standards and/or the MHRA would be (a) to protect the public from risk, (b) to protect the public from health fraud and (c) almost certainly lower cost to the tax payer.
Q11: If you feel that not all three practitioner groups justify statutory regulation, which group(s) does/do not and please give your reasons why/why not?
Acupuncture
Herbal Medicine
TCM
Unsure
None of them. The differences are marginal. In the case of acupuncture there has been far more good research than for HM or TCM. But the result of that research is to show that in most cases the effects are likely to be no more than those expected of a rather theatrical placebo. Furthermore the extent to which acupuncture has a bigger effect than no-acupuncture in a NON-BLIND comparison, is usually too small and transient to offer any clinical advantage (so it doesn’t really matter whether the effect is placebo or not, it is too small to be useful).
In the case of HM, and even more of TCM, there is simply not enough research to give much idea of their usefulness, with a small handful of exceptions.
This leads to a conclusion that DH seems to have ignored in the past. It makes absolutely no sense to talk about “properly trained practitioners” without first deciding whether the treatments work or not. There can be no such thing as “proper training” in a discipline that offers no benefit over placebo. It is a major fault of the Pittilo recommendations that they (a) ignore this basic principle and (b) are very over-optimistic about the state of the evidence.
Q12: Would it be helpful to the public for these practitioners to be regulated in a way which differentiates them from the regulatory regime for mainstream professions publicly perceived as having an evidence base of clinical effectiveness? If so, why? If not, why not?
Yes
No
Unsure
It might indeed be useful if regulation pointed out the very thin evidence base for HM and TCM but it would look rather silly. The public would say how can it be that the DH is granting statutory regulation to things that don’t work?
Q13: Given the Government’s commitment to reducing the overall burden of unnecessary statutory regulation, can you suggest which areas of healthcare practice present sufficiently low risk so that they could be regulated in a different, less burdensome way or de-regulated, if a decision is made to statutorily regulate acupuncturists, herbalists and traditional Chinese medicine practitioners?
Yes
No
Unsure
As stated above, the.only form of regulation that is needed, and the only form that would protect the public, is through consumer protection regulations, most of which already exist (though they are enforced in a very inconsistent way). Most statutory regulation is objectionable, not on libertarian grounds, but because it doesn’t achieve the desired ends (and is expensive). In this case of folk medicine, like HM and TCM, the effect would be exactly the opposite of that desired as shown in separate documents that I have submitted to the consultation.
Q14: If there were to be statutory regulation, should the Health Professions Council (HPC) regulate all three professions? If not, which one(s) should the HPC not regulate?
Yes
No
Unsure
The HPC should regulate none of them. It has never before regulated any form of alternative medicine and it is ill-equipped to do so. Its statement that it doesn’t matter that there is very little evidence that the treatments work poses a danger to patients (as well as being contrary to its own rules).
Q15: If there were to be statutory regulation, should the Health Professions Council or the General Pharmaceutical Council/Pharmaceutical Society of Northern Ireland regulate herbal medicine and traditional Chinese medicine practitioners?
HPC
GPC/PSNI
Unsure
Neither. The GPC is unlikely to care about whether the treatments work any more than the RPSGB did, or the GCC does now. The problems would be exactly the same whichever body did it.
Q16: If neither, who should and why?
As I have said repeatedly, it should be left to Trading Standards, the MHRA and other consumer protection regulation.
Q17:
a) Should acupuncture be subject to a different form of regulation from that for herbalism and traditional Chinese medicine? If so, what?
Yes
No
Unsure
b) Can acupuncture be adequately regulated through local means, for example through Health and Safety legislation, Trading Standards legislation and Local Authority licensing?
Yes
No
Unsure
(a) No -all should be treated the same. Acupuncture is part of TCM
(b) Yes
Q18.
a) Should the titles acupuncturist, herbalist and [traditional] Chinese medicine practitioner be protected?
b) If your answer is no which ones do you consider should not be legally protected?
Yes
No
Unsure
No. It makes no sense to protect titles until such time as it has been shown that the practitioners can make a useful contribution to medicine (above placebo effect). That does not deny that placebos may be useful at times. but if that is all they are doing, the title should be ‘placebo practitioners’.
Q19: Should a new model of regulation be tested where it is the functions of acupuncture, herbal medicine and TCM that are protected, rather than the titles of acupuncturist, herbalist or Chinese medicine practitioner?
Yes
No
Unsure
No. This makes absolutely no sense when there is so little knowledge about what is meant by the ” functions of acupuncture, herbal medicine and TCM”.Insofar as they don’t work (better than placebo), there IS no function. Any attempt to define function when there is so little solid evidence (at least for HM and TCM) is doomed to failure.
Q20: If statutory professional self-regulation is progressed, with a model of protection of title, do you agree with the proposals for “grandparenting” set out in the Pittilo report?
Yes
No
Unsure
No. I believe the Pittilo report should be ignored entirely. The whole process needs to be thought out again in a more rational way.
Q22: Could practitioners demonstrate compliance with regulatory requirements and communicate effectively with regulators, the public and other healthcare professionals if they do not achieve the standard of English language competence normally required for UK registration? What additional costs would occur for both practitioners and regulatory authorities in this case?
Yes
No
Unsure
No. It is a serious problem, in TCM especially, that many High Street practitioners speak hardly any English at all. That adds severely to the already considerable risks. There would be no reliable way to convey what was expected of them. it would be absurd for the taxpayer to pay for them to learn English for the purposes of practising TCM (of course there might be the same case as for any other immigrant for teaching English on social grounds).
Q23: What would the impact be on the public, practitioners and businesses (financial and regulatory burden) if practitioners unable to achieve an English language IELTS score of 6.5 or above are unable to register in the UK?
Significant impact
Some impact
No impact
Unsure
The question is not relevant. The aim of regulation is to protect the public from risk (and it should be, but isn’t, an aim to protect them from health fraud). It is not the job of regulation to promote businesses
Q24: Are there any other matters you wish to draw to our attention?
I have submitted three documents via HRDListening@dh.gsi.gov.uk. The first of these puts the case against the form of regulation proposed by Pittilo, far more fluently than is possible in a questionnaire.
Another shows examples of what is actually taught in degrees in acupuncture, HM and TCM. They show very graphically the extent to which the Pittilo proposals would endanger the public, if they were to be implemented..
Chiropractors are getting very touchy indeed, all over the world. And no wonder, because their claims are being exposed as baseless as never before, in the wake of their attempts to stifle criticism by legal action..
In March, Shaun Holt appeared on Breakfast TV in New Zealand. Holt has done a lot of good work on TV in debunking some of the preposterous claims made by quacks. See him on YouTube.
This time he talked about chiropractic. Here is the video.
One could argue that he was over generous to chiropractic, especially when talking about their effectiveness in treating low back pain. He said, quite rightly, that chiropractors are no better than physiotherapists at treating low back pain.
But a recent trial suggests that neither are much good. “A randomised controlled trial of spinal manipulative therapy in acute low back pain” (Juni et al., 2009 in the BMJ; see also coverage in Pulse). This trial compared standard care with standard care plus spinal manipulative therapy (SMT). The results were negative, despite the fact that this sort of A + B vs B design is inherently biassed in favour of the treatment (see A trial design that generates only ”positive” results, Ernst & Lee 2008, Postgrad Med J.).
"SMT was performed by a specialist in manual medicine, chiropractice and rheumatology (GH), a specialist in physical medicine (DV) or an osteopath (RvB), all proficient in SMT."
"Conclusions: SMT is unlikely to result in relevant early pain reduction in patients with acute low back pain."
Admittedly, the trial was quite small (104 patients, 52 in each group) so it will need to be confirmed. but the result is entirely in line with what we knew already.
It also adds to the evidence that the recommendation by NICE of SMT by chiropractors constitutes their biggest failure ever to assess evidence properly. If NICE don’t amend this advice soon, they are in danger of damaging their hitherto excellent record.
Despite the moderate tone and accuracy of what Holt said on TV, the New Zealand Chiropractors’ Association made a formal complaint. That is what they like to do, as I learned recently, to my cost. It is so much easier than producing evidence.
Quite absurdly the New Zealand Broadcasting Standards Authority (BSA) has upheld some of the complaints. Their judgement can be read here.
The BSA consists of four people, two lawyers and two journalists. So not a trace of scientific expertise among them. Having people like that judging the claims of chiropractors makes as much sense as having them judged by Mr Justice Eady. They seem to be the sort of people who think that if there is a disagreement, the truth must lie half-way between the opposing views.
One of the BSA members, Tapu Misa, has used her newspaper column to quote approvingly the views of the notorious Dr Mercola web site on flu prevention “Your best defence, it says, is to eat right, get lots of sleep, avoid sugar and stress, load up on garlic, Vitamin D and krill oil”. (Snake oil is said to be good too.) There are some odd attitudes to science in some of her other columns too (e.g. here and here). Not quite the person to be judging the evidence for and against chiropractic, I think.
In fact the TV show in question was more than fair to chiropractors. It adopted the media’s usual interpretation of fair and balanced: equal time for the flat earthers. A Chiropractor was invited to reply to Holt’s piece. Here he is.
The chiropractor, Doug Blackbourn, started very plausibly, though a tendency to omit every third syllable made transcription hard work. He established that if you cut yourself you get better (without any help). He established that nerves run down the spinal cord. So far, so good. But then he quickly moved on to the usual flights of fancy.
"We have two premises. The body heals itself and the nervous system runs the body. Now the nervous system runs the body, travels down through the spinal cord so chiropractic is not based on the belief that, you know, energy flows, it’s based on the fact that your nervous system runs the body and [inaudible] affects the overall health of the body"
This statement is totally vague. It has nothing whatsoever to do with the main question, can chiropractors do anything useful. It is sheer flannel.
We’re seeing people, heck, diabetes. I had a quadriplegic come in one time for adjustment, we’ve got stroke people, we’ve got all sorts of conditions. We’re not treating the condition, We’re allowing, checking the spine to see if there’s any interference there that will slow the body down"
“Interference”? “slowing the body down”? These are utterly meaningless phrases that simply serve to distract from the only question that matters.
"Chiropractice is the most safest [sic] profession to go to to get your spine adjusted"
Hmm I thought it was the only job that uses the word ‘adjustment’.
Worst of all was his response to a question about asthma.
Presenter: "So chiropractors are not out there claiming they will cure asthma for example?". Chiropractor: "No"
This is simply untrue, both in New Zealand and in the UK. For a start, just look at what Blackbourn’s own web site says about asthma.
"The challenge, of course, with allergy and asthma medication is there is no end-point. There is no cure. Asthma and allergies, for the most part, are lifelong conditions requiring lifelong medication. Might there be a better way, an alternative solution?
“Alternative” is the key word. Medical treatment is designed to combat symptoms, and is successful to a certain extent with allergies and asthma. Underlying causes are not addressed, however, and symptoms continue year after year. What else might be done?
Enter chiropractic care. Chiropractic health care, with its unique comprehensive approach, is able to offer positive benefit to a variety of conditions and ailments. In the case of allergies and asthma, these “hypersensitivity conditions” may respond well to therapy designed to normalize the body’s flow of nerve signals. To use a metaphor, chiropractic treatment removes roadblocks to the body’s natural healing abilities. Restoring these imbalances may help reduce such hypersensitivity reactions."
Blackbourn’s web site describes him thus
"As a Doctor of Chiropractic, Dr. Doug Blackbourn . . ."
But the qualifications of “Dr” Blackbourn are B.App.Sc (Chiro) M.N.Z.C.A , the same as those of “Dr” Brian Kelly.
After a performance like this, perhaps someone should submit a complaint to the New Zealand Broadcasting Standards Authority.
After all, I notice that they have dismissed complaints from one chiropractor, Sean Parker, after a TV programme looked at the business practices of his private chiropractic practice, The Spinal Health Foundation. Perhaps the BSA understands business better than it understands science.
Follow-up
Is chiropractic crumbling in New Zealand? The New Zealand College of Chiropractic featured in my editorial in the New Zealand Medical Journal, and in the fallout from that article, It’s principle, “Dr” Brian Kelly (B App Sci (Chiro)) seems to be getting desperate. His college is now canvassing for recruits in Canada. They are promised all the woo.
- Subluxation centered techniques – Gonstead, Toggle Recoil, Thompson, Diversified
- Traditional philosophy featuring vitalism and innate healing – congruent curriculum
Perhaps Canada is a good place to recruit, gven the $500 million class action being brought against chiropractors in Canada, after Sandra Nette became tetraplegic immediately after a chiropractor manipulated her neck, Canadian chiropractors must be looking for somewhere to hide.
Stuff and Nonsense. jdc described this story at the time the complaint was lodged.
Shaun Holt’s own blog follows the action.
New Zealand Doctor covers the story.
Bay of Plenty Times “Bay researcher slams television complaint ruling“
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”
Today, 29 July 2009, a large number of magazines and blogs will publish simultaneously Simon Singh’s article. The Guardian was forced to withdraw it, but what he said must be heard (even if the word ‘bogus’ is now missing).
This is an edited version if the article in the Guardian that resulted in the decision of the British Chiropractic Association to sue Singh for libel. That decision was bad for Singh, though its effects could yet be good for the rest of the world, Firstly the decision to use law rather than rational argument stands a good chance of destroying chiropractic entirely because its claims have now come under scrutiny as never before, and they have been found wanting. Secondly, the support for Singh has been so enormous that there must now be a good chance of getting the UK’s iniquitous laws about defamation changed.
I’d rather have reproduced the original article in its entirety, but this bowdlerised version still presents the case very strongly (and the unedited version appears here and here).
Beware the spinal trapSome practitioners claim it is a cure-all, but the research suggests chiropractic therapy has mixed results – and can even be lethal, says Simon Singh. You might be surprised to know that the founder of chiropractic therapy, Daniel David Palmer, wrote that “99% of all diseases are caused by displaced vertebrae”. In the 1860s, Palmer began to develop his theory that the spine was involved in almost every illness because the spinal cord connects the brain to the rest of the body. Therefore any misalignment could cause a problem in distant parts of the body. In fact, Palmer’s first chiropractic intervention supposedly cured a man who had been profoundly deaf for 17 years. His second treatment was equally strange, because he claimed that he treated a patient with heart trouble by correcting a displaced vertebra. You might think that modern chiropractors restrict themselves to treating back problems, but in fact some still possess quite wacky ideas. The fundamentalists argue that they can cure anything, including helping treat children with colic, sleeping and feeding problems, frequent ear infections, asthma and prolonged crying – even though there is not a jot of evidence. I can confidently label these assertions as utter nonsense because I have co-authored a book about alternative medicine with the world’s first professor of complementary medicine, Edzard Ernst. He learned chiropractic techniques himself and used them as a doctor. This is when he began to see the need for some critical evaluation. Among other projects, he examined the evidence from 70 trials exploring the benefits of chiropractic therapy in conditions unrelated to the back. He found no evidence to suggest that chiropractors could treat any such conditions. But what about chiropractic in the context of treating back problems? Manipulating the spine can cure some problems, but results are mixed. To be fair, conventional approaches, such as physiotherapy, also struggle to treat back problems with any consistency. Nevertheless, conventional therapy is still preferable because of the serious dangers associated with chiropractic. In 2001, a systematic review of five studies revealed that roughly half of all chiropractic patients experience temporary adverse effects, such as pain, numbness, stiffness, dizziness and headaches. These are relatively minor effects, but the frequency is very high, and this has to be weighed against the limited benefit offered by chiropractors. More worryingly, the hallmark technique of the chiropractor, known as high-velocity, low-amplitude thrust, carries much more significant risks. This involves pushing joints beyond their natural range of motion by applying a short, sharp force. Although this is a safe procedure for most patients, others can suffer dislocations and fractures. Worse still, manipulation of the neck can damage the vertebral arteries, which supply blood to the brain. So-called vertebral dissection can ultimately cut off the blood supply, which in turn can lead to a stroke and even death. Because there is usually a delay between the vertebral dissection and the blockage of blood to the brain, the link between chiropractic and strokes went unnoticed for many years. Recently, however, it has been possible to identify cases where spinal manipulation has certainly been the cause of vertebral dissection. Laurie Mathiason was a 20-year-old Canadian waitress who visited a chiropractor 21 times between 1997 and 1998 to relieve her low-back pain. On her penultimate visit she complained of stiffness in her neck. That evening she began dropping plates at the restaurant, so she returned to the chiropractor. As the chiropractor manipulated her neck, Mathiason began to cry, her eyes started to roll, she foamed at the mouth and her body began to convulse. She was rushed to hospital, slipped into a coma and died three days later. At the inquest, the coroner declared: “Laurie died of a ruptured vertebral artery, which occurred in association with a chiropractic manipulation of the neck.” This case is not unique. In Canada alone there have been several other women who have died after receiving chiropractic therapy, and Edzard Ernst has identified about 700 cases of serious complications among the medical literature. This should be a major concern for health officials, particularly as under-reporting will mean that the actual number of cases is much higher. If spinal manipulation were a drug with such serious adverse effects and so little demonstrable benefit, then it would almost certainly have been taken off the market. Simon Singh is a science writer in London and the co-author, with Edzard Ernst, of Trick or Treatment? Alternative Medicine on Trial. This is an edited version of an article published in The Guardian for which Singh is being personally sued for libel by the British Chiropractic Association. |
That’s a great account of the evidence. Notice the conclusion,
“If spinal manipulation were a drug with such serious adverse effects and so little demonstrable benefit, then it would almost certainly have been taken off the market“.
It is the job of NICE to evaluate critically that sort of thing, which makes it all the odder that the NICE guidance group, very unusually, failed to assess properly the evidence for chiropractic.
If you aren’t one of the 15,000 people who have already signed Singh’s statement, please do it now
Follow-up
Resignation of Pain Society president. While we are on the topic of chiropractic, my comment, The hidden cost of endorsing voodoo, appeared at last on the BMJ article about NICE’s low back pain guidance. The thread came back to life after the British Pain Society voted out its president, Paul Watson, a physiotherapist who was a member of the group that wrote the guidance.
Some of the links Links to some of the many repostings of Singh’s article today are aggregated at Sense about Science. There where over 200 in a single day. The British Chiropractic Association tried to suppress criticism, but they clearly don’t understand the web.
“An intrepid, ragged band of bloggers. Chiropractors may regret choosing to sue Simon Singh, springing online scientists into action”. Ben Goldacre has summed up the reaction of the blogosphere with characteristically fine style in the Guardian. Ragged? Moi? The blog version (with links) is here.
It’s good to see the BMJ joining the campaign for free speech (only a month or two behind the blogs). The suing of Simon Singh for defamation by the British Chiropractic Association has stirred up a hornet’s nest that could (one hopes) change the law of the land, and destroy chiropractic altogether. The BMJ’s editor, Fiona Godlee, has a fine editorial, Keep the libel laws out of science. She starts “I hope all readers of the BMJ are signed up to organised scepticism” and says
“Weak science sheltered from criticism by officious laws means bad medicine. Singh is determined to fight the lawsuit rather than apologise for an article he believes to be sound. He and his supporters have in their sights not only the defence of this case but the reform of England’s libel laws.”
Godlee refers to equally fine articles by the BMJ’s Deputy Editor, Tony Delamothe, Thinking about Charles II“, and by Editor in Chief, Harvey Marcovitch, “Libel law in the UK“.
The comments on Godlee’s editorial, show strong support, (apart from one from the infamous quantum fantasist, Lionel Milgrom). But there was one that slighlty surprised me, from Tricia Greenhalgh, author of the superb book, “How to read a paper”. She comments
“the use of the term ‘bogus’ seems both unprofessional and unscholarly. The argument would be stronger if expressed in more reserved terms”
That set me thinking, not for the first time, about the difference between journalism and scholarship. I can’t imagine ever using a word like ‘bogus’ in a paper about single ion channels. But Singh was writing in a newspaper, not in a scientific paper. Even more to the point, his comments were aimed at people who are not scholars and who, quite explicitly reject the normal standards of science and evidence. The scholarly approach has been tried for centuries, and it just doesn’t work with such people. I’d defend Singh’s language. It is the only way to have any effect. That is why I sent the following comment.
The ultimate irony is that the comment was held up by the BMJ’s lawyers, and has still to appear.
|
Thanks for an excellent editorial. I doubt that it’s worth replying to Lionel Milgrom whose fantasy physics has been totally demolished by real physicists. Trisha Greenhalgh is, though, someone whose views I’d take very seriously. She raises an interesting question when she says “bogus” is an unprofessional word to use. Two things seem relevant. First, there is little point in writing rational scholarly articles for a group of people who do not accept the ordinary rules of evidence or scholarship. We are dealing with fantasists. Worse still, we are dealing with fantasists whose income depends on defending their fantasies. You can point out to your heart’s content that “subluxations” are figment of the chiropractors’ imagination, but they don’t give a damn. They aren’t interested in what’s true and what isn’t. Throughout my lifetime, pharmacologists and others have been writing scholarly articles about how homeopathy and other sorts of alternative medicine are bogus. All this effort had little effect. What made the difference was blogs and investigative journalism. When it became possible to reveal leaked teaching materials that taught students that “amethysts emit high yin energy“, and name and shame the vice-chancellors who allow that sort of thing to happen (in this case Prof Geoffrey Petts of Westminster University), things started to happen. In the last few years all five “BSc” degrees in homeopathy have closed and that is undoubtedly a consequence of the activities of bloggers and can assess evidence but who work more like investigative journalists. When the BCA released, 15 months after the event, its “plethora of evidence” a semi-organised effort by a group of bloggers produced, in less than 24 hours, thoroughly scholarly analyses of all of them (there is a summary here). As the editorial says, they didn’t amount to a hill of beans, They also pointed out the evidence that was omitted by the BCA. The conventional press just followed the bloggers. I find it really rather beautiful that a group of people who have other jobs to do, spent a lot of time doing these analyses, unpaid, in their own time, simply to support Singh, because they believed it is the right thing to do. Simon Singh has analysed the data coolly in his book. But In the case that gave rise to the lawsuit he was writing in a newspaper. It was perfectly clear from the context what ‘bogus’ meant. but Mr Justice Eady (aided by a disastrous law) chose to ignore entirely the context and the question of truth. The description ‘bogus’. as used by Singh, seems to be entirely appropriate for a newspaper article. To criticise him for using “unprofessional” language is inappropriate because we are not dealing with professionals. At the heart of the problem is the sort of stifling political correctness that has resulted in quacks being referred to as “professions” rather than fantasists and fraudsters [of course I use the word fraudster with no implication that it necessarily implies conscious lying]. At least there are some laughs to be had from the whole sorry affair. Prompted by that prince among lawyers known as Jack of Kent there was a new addition to my ‘Patients’ Guide to Magic Medicine‘, as featured in the Financial Times.
|
It is, perhaps, misplaced political correctness that lies at the heart of the problem. Who can forget the letter from Lord Hunt, while he was at the Department of Health, in which he described “psychic surgery” (one of the best known fraudulent conjuring tricks) as a “profession”.
Follow-up
Two days later, the comment has appeared in the BMJ at last. But it has been altered a bit.
|
Unprofessional language is appropriate when dealing with unprofessional people Thanks for an excellent editorial. I doubt that it’s worth replying to Lionel Milgrom whose fantasy physics has been totally demolished by real physicists. Trisha Greenhalgh is, though, someone whose views I’d take very seriously. She raises an interesting question when she says “bogus” is an unprofessional word to use. Two things seem relevant. First, there is little point in writing rational scholarly articles for a group of people who do not seem to accept the ordinary rules of evidence or scholarship. You can point out to your heart’s content that “subluxations” are figment of the chiropractors’ imagination, but they don’t give a damn. Throughout my lifetime, pharmacologists and others have been writing scholarly articles about how homeopathy and other sorts of alternative medicine are bogus. All this effort had little effect. What made the difference was blogs and investigative journalism. When it became possible to reveal leaked teaching materials that taught students that “amethysts emit high yin energy”, and name and shame the vice-chancellors who allow that sort of thing to happen (in this case Prof Geoffrey Petts of Westminster University), things started to happen. In the last few years all five “BSc” degrees in homeopathy have closed and that is undoubtedly a consequence of the activities of bloggers and can assess evidence but who work more like investigative journalists. When the BCA released, 15 months after the event, its “plethora of evidence” a semi-organised effort by a group of bloggers produced, in less than 24 hours, thoroughly scholarly analyses of all of them (there is a summary here). As the editorial says, they didn’t amount to a hill of beans, They also pointed out the evidence that was omitted by the BCA. The conventional press just followed the bloggers. I find it really rather beautiful that a group of people who have other jobs to do, spent a lot of time doing these analyses, unpaid, in their own time, simply to support Singh, because they believed it is the right thing to do. Simon Singh has analysed the data coolly in his book. But In the case that gave rise to the lawsuit he was writing in a newspaper. It was perfectly clear from the context what ‘bogus’ meant. but Mr Justice Eady (aided by a disastrous law) chose to ignore entirely the context. The description ‘bogus’. as used by Singh, seems to be entirely appropriate for a newspaper article. To criticise him for using “unprofessional” language is inappropriate because we are not dealing with professionals. At least there are some laughs to be had from the whole sorry affair. Prompted by that prince among lawyers known as Jack of Kent there was a new addition to my ‘Patients’ Guide to Magic Medicine’, as featured in the Financial Times.
|
Here are the changes that were made. Hmm.very interesting.
Here is a short break from the astonishing festival of chiropractic that has followed the British Chiropractic Association (BCA) v Simon Singh defamation case, and the absurd NICE guidance on low back pain.
|
Singh’s statement already has over 10000 signatories, many very distinguished, Sign it now if you haven’t already. And getting on for 600 separate complaints about exaggerated and false claims by chiropractors have been lodged with the General Chiropractic Council and with Trading Standards offices. |
The BCA has exposed the baselessness of most of chiropractic’s claims more effectively than any sceptic could have done.
The University of Westminster is seeing the light?
It is only recently that the University of Westminster suspended entry to degrees in homeopathy and remedial massage and neuromuscular therapy. Luckily for science, they have a new Dean who knows bullshit when she sees it. I suspect than she has been instrumental in starting to restore Westminster’s reputation. The job isn’t finished yet though. According to the UCAS site Westminster still offers
- Chinese Medicine: Acupuncture with Foundation (B341) 4FT Hon BSc
- Health Sciences: Complementary Ther with Foundn (B300) 4FT Hon BSc
- Health Sciences: Complementary Therapies (B255) 3FT Hon BSc
- Health Sciences: Herbal Medicine (B342) 3FT Hon BSc
- Health Sciences: Herbal Medicine with Foundation (B340) 4FT Hon BSc
- Health Sciences: Naturopathy (B391) 3FT Hon BSc
- Health Sciences: Naturopathy with Foundation (B392) 4FT Hon BSc
- Health Sciences: Nutritional Therapy (B400) 3FT Hon BSc
- Health Sciences: Nutritional Therapy with Foundn (B402) 4FT Hon BSc
With the possible exception of herbal medicine, which could be taught scientifically. all the rest is as delusional as homeopathy.
Rumour has it that Naturopathy may be next for the chop, so it seems appropriate to help the dean by showing a bit more of what the hapless students get taught. Remember that, according to Westminster, this is a bachelor of science degree!
Psychotherapeutic Approaches in Naturopathy 3CMW606
“This module is a core subject for BSc (Hons) Health Sciences: Naturopathy and option for BSc (Hons) Health Sciences: Complementary Therapies; BSc (Hons) Health Sciences: Therapeutic Bodywork; Graduate Diploma in Therapeutic Bodywork.”
Lectures 3 – 5 of this course are about the Theory and Application of EmoTrance.
EMOTRANCE? No I had never heard of it either. But it takes only two minutes with Google to discover that it yet another product of the enormous navel-gazing self-help industry. A new variant is born almost every day, and no doubt they make buckets of money for their inventors. You can download a primer from http://emotrance.com/. The web site announces.
“EmoTrance REAL energy healing for the 21st Century”
Here are three quotations from the primer.
|
And then I thought of the lady in the supermarket whose husband had died, and I spend the following time sending her my best wishes, and my best space time quantum healing efforts for her void. It doesn’t matter how “bad”; something is or how old, it is ONLY AN ENERGY and energy can be moved with consciousness in quantum time, easily, and just for the asking. Is EmoTrance a Science? |
Now back to Westminster
Here are a few slides about EmoTrance
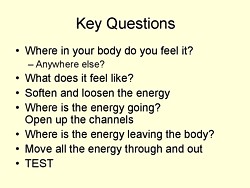
|
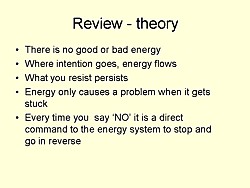
|
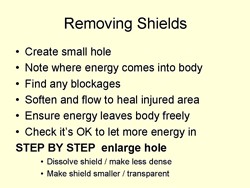
|
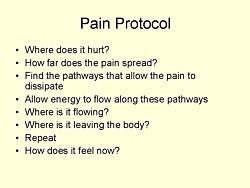
|
So it is pure vitalistic psycho-babble. The usual undefined use of impressive sounding words like “energy” and “quantum” with no defined meaning. Just preposterous made-up gobbledygook.
Before getting to EmoTrance, the course Psychotherapeutic Approaches in Naturopathy (3CMW606) had a lecture on Flower Essences. The evidence says, not surprisingly, that the effects of flower essences is not distinguishable from placebo “The hypothesis that flower remedies are associated with effects beyond a placebo response is not supported by data from rigorous clinical trials.” (See Ernst Wien. Klin. Wochenschr. 2002 114(23-24):963-6). Here are two of the slides.
This last slide departs from the simply silly to the totally mad. Dowsing? Kinesiology?
Pendulums I’m told from more than one source that the use of pendulums is not uncommon. both in teaching and by students in the Westminster University polyclinic Apparently they provide an excellent way to choose a ‘remedy’ or make a diagnosis (well, I expect they are as good as the alternatives). If in doubt, guess.
Of course pendulums were popular with Cherie Blair who is reported to have taken her son Leo to a pendulum waver, Jack Temple, rather than have him vaccinated with MMR. At least her delusions affected fewer people than those of her husband (the latest Iraq body count is about 100,000).
Kinesiology was originally a word that applied to the perfectly sensible science of human movement. But Applied Kinesiology more often refers now to a fraudulent and totally ineffective diagnostic method invented by (you guessed) a chiropractor. It has been widely used by alternative medicine to misdiagnose food allergies. It does not work (Garrow, 1988: download reprint).
General Chiropractic Council It is a mind-boggling sign of the incompetence of the General Chiropractic Council that they manage to include kinesiology within their definition of “evidence based care”. Their definition is clearly sufficiently flexible to include anything whatsoever. The incompetence of the GCC is documented in superb detail on jdc325’s blog (James Cole).
Council for Healthcare Regulatory Excellence (CHRE) is yet another example of the network of ineffective and incompetent quangos that plague us.. It is meant to ensure that regulation is effective but utterly fails to do so. The CHRE is quoted as saying “[The GCC] takes its role seriously and aspires to, and often maintains, excellence.”. Like endorsing kinesiology and ‘craniosacral therapy’ perhaps? Quangos like the CHRE not only fail to ensure regulatory excellence, they actually endorse rubbish. They do more harm than good.
The reading list for the course includes the following books. I guess the vibrational medicine (whatever that means) was covered already in the now infamous ‘amethysts emit high yin energy‘ lectures.
Reading List
Essential:
Hartman S (2003) Oceans of Energy: The Patterns and Techniques of EmoTrance: Vol 1.DragonRising. ISBN: 1873483732.
Lynch V and Lynch P (2001) Emotional Healing in Minutes. Thorsons: London. ISBN: 0007112580Recommended:
Gerber R (2001) Vibrational Medicine for the 21st Century. Piatkus Publishers: London.
Gurudas (1989) Flower Essences and Vibrational Medicine. Cassandra Press: California, USA
Hartman S (2000) Adventures in EFT: The Essential Field Guide to Emotional Freedom Techniques. DragonRising. ISBN: 1873483635.
Hartman S (2004) Living Energy: The Patterns and Techniques of EmoTrance: Vol 2. DragonRising.ISBN: 1873483740.
Hartman S (2006) Energy Magic: The Patterns and Techniques of EmoTrance: Vol 3. Dragon Rising.ISBN: 1873483767.
Real magic.
Sylvia Hartman’s books seem to feature heavily in the reading list. I just got news of her latest effort
Welcome to a special update to the June 2009 newsletter to announce Silvia Hartmann’s latest book “Magic, Spells & Potions” is now available to pre-order from our site. The eBook edition will be released this Sunday, the most magical day of the year.
http://DragonRising.com/store/magic_spells_and_potions/?r=DR0609MSAP
If you do pre-order this exciting new book, not only will you be amongst the first to receive your copy, but you will also be entered into an exciting competition for Silvia Hartmann’s handmade copal amber magic pendant. Each paperback book pre-ordered will also be signed by the author and contain a unique blessing for the reader.
Because this is a serious book on real magic, potions and fortune telling if you are a beginner Silvia has provided ample sample spells and potions for you to practice working with before you start covering the advanced material.
What? No honestly, I didn’t invent that.
The idea that stuff of this sort is appropriate for a bachelor of science degree is simply ludicrous. I have no doubt that Westminster’s new dean can see that as well as anyone else. She has the delicate diplomatic job of extirpating the nonsense, I wish her well.
Follow-up
A flood of complaints against chiropractors has arrived at the General Chiropractic Council (GCC) in the wake of the British Chiropractic Association (BCA) v Singh affair. It is really rather beautiful that people have put some such enormous effort into writing complaints for no gain to themselves.
My own paltry two complaints to the GCC produced an interesting reaction. Yesterday I was told by the GCC
“Under the provisions of the General Chiropractic Council (Investigating Committee) Rules
2000 (“the Rules”), the Committee is required to invite you to make a statement of evidence in relation to your complaint by way of statutory declaration or affidavit. If you wish to, you can discuss your complaint with a solicitor who acts on behalf of the Committee who could help you draft a statement of evidence that meets the requirements of the Rules. The General Chiropractic Council will pay for the Investigating Committee solicitor’s costs and will reimburse you for any fee you subsequently pay for having your witness statement sworn at a location convenient to you.”
Naturally I shall take up this offer. If the same offer is made to everyone who complained (must be approaching 600), the legal fees incurred by the GCC would presumably be enough to bankrupt them. No wonder they are wriggling.
Here is a letter sent by the GCC’s Chief Executive and Registrar, Margaret Coats, a couple of days ago. It reached me by more than one route, but it is already on the web anyway, on Richard Lanigan’s site, Told you the General Chiropractic Council would find a way to dismiss the complaints. “Protecting the public” my arse! Protecting themselves more like it.. (The GCC has been under attack from within for some time, though mainly because some chiropractors think it regulates too much, not too little)
The bit that is especially interesting is para 2
In quangos like the GCC, complaints don’t necessarily get considered at all. First they go to an investigating committee (IC) which has to decide if there is a ‘case to answer’. Now the GCC wants that criterion to be changed to ‘realistic prospect of success’. Given the GCC’s attitude to evidence it is hard to imagine that any complaint will have a ‘realistic prospect of success’.
The second idea is even more grotesque. The GCC want to be able to dismiss without consideration rafts of complaints where in their opinion, referral to the Professional Conduct Committee (PCC) ‘is not required in the public interest. Or, more likely, not required in the interests of the GCC.
Will the Privy Council acquiesce in this disgraceful attempt to evade complaints? Wel, until January 2008, Graham Donald was a senior civil Servant at the Privy Council bit he now works for the GCC. That must help.
The GCC has been contacted by several Trading Standards Offices too, after complaints made to them about chiropractors. . A response was sent by the GCC on 5 June [download the whole response]. It includes
“It is important to emphasise that the GCC doesn’t claim that chiropractors ‘treat’ asthma, headaches (including migraine) and infant colic. It is possible that chiropractic care may help to alleviate the symptoms of some of these conditions.”
What on earth is that meant to mean?
One hopes that Trading Standards officers are too smart to be taken in by weasel words like that.
The attitude of the GCC to evidence is amply illustrated by the fact that they have said that the rather crude myths known as craniosacral therapy and applied kinesiology fall within their definition of evidence-based care.
Any organisation that can say that is clearly incompetent.
Follow-up
Peter Dixon is a chiropractor. He is chair of the General Chiropractic Council (GCC). He was also a member of the hotly-disputed NICE low back pain guidance group that endorsed (you guessed it) the use of chiropractic, a decision that has led to enormous criticism of the standards of the National Institute of health and Clinical Excellence (NICE).
As a consequence largely of the decision of the British Chiropractic Association (BCA) to sue Simon Singh for defamation, there has been an unprecedented interest taken in the claims made by chiropractors in general.
Peter Dixon has a problem because something like 600 individual complaints about unjustified health claims have been sent to the GCC. Even when a web site does not claim to be able to benefit things like asthma and colic, a phone call may reveal that claims are made in private (one of the many complaints to the GCC concerns such behaviour by two practices belonging to, ahem, Peter Dixon Associates).
The crucial question is, as always, one of evidence. The BCA claim to have a plethora of evidence for their claims, but they have been strangely reluctant to produce it. In fact evidence is cited on the “Your first visit” page on Dixon’s site.
At the bottom we see “How effective is Chiropractic?”.
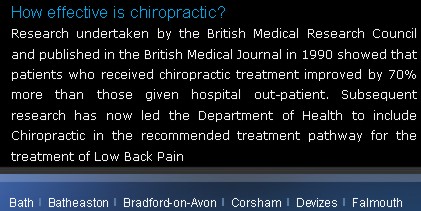
That sounds very impressive indeed: . ” . . . patients who received chiropractic treatment improved by 70% more than those given hospital out-patient.”
But hang on. If we look at the paper, Meade et al., 1990 [download reprint], we see that Figure 2 looks like this.
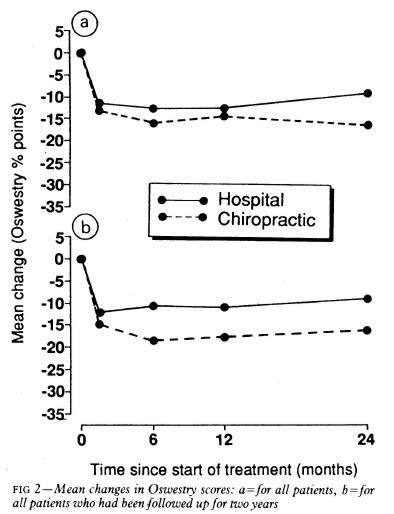
Several things jump out. First, the Oswestry disability index scale runs for 0 to 100, but scores are plotted only from 0 to 35, so the size of the effects are exaggerated. Second, there are no error bars on the points. Third there is essentially no advantage for chiropractic at all when all patients are taken together (top graph). Fourth, and most important, the patients who were followed up for two years (bottom graph) seem to show a slight advantage for chiropractic but on average, the effect is 7 percent (on the 100 point scale, NOT 70 percent as claimed on the web site of Peter Dixon Associates.
What sort of mistake was made?
The abstract of the paper itself says “A benefit of about 7% points on the Oswestry scale was seen at two years.” How did this become “improved by 70% more”?
It could have been simple a typographical error, but that seems unlikely, Who’d boast about a 7% improvement?
Perhaps it is a question of relative versus absolute change. The Figure does not show the actual scores on the 100 point scale, but rather the change in score, relative to a questionnaire given just before starting treatment. If we look at the lower part of the Figure, restricted to those patients who stayed with the trail for 2 years (by this time 28% of the patients had dropped out), we see that there is a reduction in score (improvement) of about 10 points on the 100 point scale with hospital treatment (not a very impressive response). The improvement with those sent to private chiropractic clinics was about seven points bigger. So a change from 10 to 17 is a 70 percent change. What’s wrong with that?
What’s wrong is that it is highly misleading, as relative changes often are. Imagine that the hospital number had been 7 points and the chiropractic number had been 14 (both out of 100). That would mean that both treatments had provided very modest benefits to the patients. Would it then be fair to describe the chiropractic patients as have improved by 100 percent more than the hospital patients, when in fact neither got much benefit? Of course it would not. To present the results in this way would be highly deceptive.
Put another way, a 70% increase in a trivial effect is still pretty trivial.
That isn’t all either. The paper has been analysed in some detail on the ebm-first site. The seven point difference on a 100 point scale, though it may be real, is too small to be ‘clinically significant’ In other words the patient would scarcely notice such a small change. Another problem lies in the nature of the comparison. Patients were, quite properly, allocated at random to chiropractic or to to hospital treatment. BUT the comparion was very from blind. one group was treated in hospital. The other group was sent to private chiropractic clinics. The trivial 7 point difference could easily be as much to do with the thickness of the carpets rather than any effect of spinal manipulation.
What this paper really tells you is that neither treatment is very effective and that there is little to choose between them.
It is really most unfortunate that the chairman of the GCC should show himself to be so careless about evidence at a time when the evidence for the claims of chiropractors is under inspection as never before. It does not add to their case for criticising Simon Singh and it does not add to one’s confidence in the judgement of the NICE guidance group.
Follow-up
The Pain Society revolt. A letter has been sent from several distinguished members of the British Pain Society to its President and Council.
“We, the undersigned, call upon the President of the British Pain Society to issue a statement to NICE and to the press condemning outright the conclusions of the recent UK National Institute for Health and Clinical Excellence (NICE) guidelines . . .”
The sigificance of this letter is that the present president of the British Pain Society is Professor Paul Watson who was a member of the NICE guidance group that produced the recommendations which have engendered such criticism. He was clinical advisor to the guidance group. There is a video of Paul Watson talking about back pain, that seems to me to illustrate very well the problem with the guidance. He says it is a huge problem (everyone knows that) and that something must be done, but he doesn’t say what. There is no admission that, in very many cases, nobody knows what to do. It is exactly this sort of hubris that that makes the NICE report so bad,
One caustic comment on the letter says
“We are led by a physiotherapist! A Professor who cannot even interpret straight forward evidence when it is presented to him on a plate.
Who’s going to be the next BPS President? A Hospital Porter?”
This is another short interruption in the epic self-destruction of chiropractors. In a sense it is more serious. One expects quacks to advocate quackery. What you don’t expect is that the National Institute of Clinical Excellence (NICE) will endorse it. Neither do you expect the Medicines and Healthcare products Regulatory Agency (MHRA) to betray its mandate to make sure that medicines work.
The saga of the NICE low back pain guidance has been the subject of a deluge of criticism, It seems doubtful that the guidance can survive, not least because of its absurd endorsement of chiropractic, at a time when chiropractic is undergoing self-immolation as a consequence of the persecution of Simon Singh by the British Chiropractic Association (see here, and here, and here, and here and thousands of other sites).
The other betrayal has come to the for after the MHRA approved highly misleading labelling of a homeopathic preparation. At the time,
in 2006, when the principle was approved by the MHRA, just about every scientific organisation, even the Royal Society, condemned the action. What was discouraging that the clinical organisations all stayed silent. It is still a mystery why the MHRA made this enormous mistake, Some said that European regulations required it, but that is quite untrue, as Les Rose has shown. It appears to have been the result of a pusillanimous MHRA bowing to pressure from a deeply unscientific Department of Health (a letter from Caroline Flint at the time borders on the surreal).
On 20 May 2009, the British Medical Journal printed an article Drugs agency grants its first licence to homoeopathic product by Deborah Cohen (available free). The comments were mostly highly critical of the MHRA. The BMJ asked, as it does from time to time, for my comment to be converted to a letter
for the print edition. That isn’t freely available, so here it is.
|
Published 9 June 2009, doi:10.1136/bmj.b2333 LettersHomoeopathic product licenceMHRA label seems to be illegalThe strap line for the Medicines and Healthcare products Regulatory Agency (MHRA) is “We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe.” Yet the MHRA has made mockery of its own aims by ignoring the bit about “ensuring that medicines work” and allowing Arnica 30C pills to be labelled: “a homoeopathic medicinal product used within the homoeopathic tradition for the symptomatic relief of sprains, muscular aches, and bruising or swelling after contusions.”1 This label should be illegal anyway because the pills contain no trace of the ingredient on the label, but this deceit has been allowed through a legal loophole for a long time now. If you sold strawberry jam that contained not a trace of strawberry you’d be in trouble. But I can see no legal loophole that allows the manufacturers of Arnica 30C to evade the provisions of the Consumer Protection from Unfair Trading Regulations 2008. One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction, or malformations.” The consumer protection laws apply to the way that “the average consumer” will interpret the label. The average consumer is unlikely to know that “used within the homoeopathic tradition” is a form of weasel words that actually means “there isn’t a jot of evidence that the medicine works.” Since there is not the slightest evidence that Arnica 30C pills provide symptomatic relief of sprains, etc, the labelling that the MHRA has approved seems to be illegal. The MHRA is not selling anything itself, so I presume that it won’t find itself in court, but anyone who follows its advice could well do so. Cite this as: BMJ 2009;338:b2333 David Colquhoun, research professor1 University College London, London WC1E 6BT Competing interests: None declared. References |
It is, I suppose, just a sign of the chaos that reigns in the multiple agencies and quangos responsible for ‘regulation’ that one arm of government proposes action that a different branch would consider illegal. That is an inevitable consequence of trying to regulate something without first deciding whether it is nonsense or not. The Department of Health appears to be quite incapable of grasping this simple and obvious fact.
Follow-up
Health: best treatments. The Guardian seems to the be picking up BMJ stories and ran this one.
The first post was NICE falls for Bait and Switch by acupuncturists and chiropractors: it has let down the public and itself.
That was followed by NICE fiasco, part 2. Rawlins should withdraw guidance and start again.
Since then, something of a maelstrom has engulfed NICE, so it’s time for an update.
It isn’t only those who are appalled that NHS should endorse voodoo medicine on the basis of very slim evidence who are asking NICE to rethink their guidance on low back pain. Pain specialists are up in arms too, and have even started a blog, ‘Not Nearly as NICE as you think …‘, to express their views. Equally adverse opinions are being expressed in the Britsh Medical Journal. A letter there is signed by over 50 specialists in pain medicine. It ends thus
“Because of these new guidelines patients will continue to experience unnecessary pain and suffering and their rights to appropriately individually tailored treatment have been removed on the basis of a flawed analysis of available evidence. We believe the guidelines do not reflect best practice, remove patient choice and are not in our patients’ best interests.”
In a contribution headed “NICE misguidance”. Dr Michel Vagg ends
It seems to me that this guideline has been used as a propaganda vehicle to allow cherry-picked evidence to be enshrined as doctrine. This is an abuse of the guideline development process . . . ”
I have to say, though, that it seems to me that some of these people are promoting their own interests as much as chiropractors and acupuncturists. The evidence that spinal injections produce worthwhile benefits seems to be as thin as the evidence that chiropractic and acupuncture produce worthwhile benefits. But no doubt the injections are good for the budgets of PCTs or private practice doctors.. Could it perhaps be the case that some of the clinicians’ anger is being generated by doctors who are rushing to defend their own favourite ineffective treatment?
Why, oh why, can’t either NICE or the pain consultants bring themselves to state the obvious, that nothing works very well. The only thing that can be said for most of the regular treatments is that although they may not be much more effective than acupuncture or chiropractic, at least they don’t come with the intellectually-offensive hokum that accompanies the latter. Very sensible attempts have been made to identify the cause of low back pain [reviewed here], Occasionally they succeed. Mostly they don’t.
One clinician’s letter deserves special attention because it goes into the evidence, and the costs, in some detail. Its conclusions are very different from those in the NICE guidance.
The letter, a Review of NICE guidance, is from Dr C.J.D. Wells [download the whole letter]. He is a pain relief consultant from Liverpool.
Let’s look at some highlights.
Wells points out the absurdity of the cost estimates
“In the pricing section, they estimate that this will require an increase of facilities so that 3,500 patients can be treated instead of 1,000 at present (again see comments on pricing). This is not many treatments for the 20 million sufferers, of whom we can estimate that at least 2 million will have significant long-term disability and psychological distress”
And that is without even costing all the secondary costs of miseducating a new generation of students in fables about “Qi”, meridians, energy flow, subluxations and innate intelligence.
“The abysmal ignorance of the committee is reflected in the poor overall advice. So if you have a committee with special interests in Exercise, Manipulation, PMP’s, and Surgery, and you call an expert on Acupuncture, you get advice to use Exercise, Manipulation, Acupuncture, PMP’s and Surgery. Amazing.”
Another pain consutant, Charles Guaci, says in a comment in the Daily Mail.
I am a Pain Consultant of 30 years experience, have published two books (one translated into different languages).
NICE never asked me for my opinion.
This is the most ridicuculous pseudo-scientific document I have ever seen.
The panel consisted of a surgeon, psychologist, osteopath, acupuncturist a physiotherapist and an academic; not one pain consultant! The conclusions are simply a means of increasing the employment of their friends!
All evidence submitted to NICE was ignored.
It is almost certain than unless NICE rethink their ideas that Pain Consultants will be seeking a judicial review as well as full disclosure of how the panel arrived at their bizarre findings under the Freedom of information act.
Patients should realise that they are being taken for a ride.
Despite the outcry from opponents of magic medicine and from pain specialists, the assessment by the normally excellent NHS Choices site was disappointing. It made no mention at all of the secondary consequences of recommending CAM and described the assertions of the guidance group quite uncritically.
The reputation of NICE
NICE has been criticised before, though usually unjustly. In the past I have often supported them. For example. when NICE said that treatment of dementia with anticholinesterase drugs like galantamine was ineffective, there was a great outcry, but NICE were quite right. There is little or no rationale for such treatments, and more importantly, very little evidence that they work. But patients, especially when they are desperate, have greater faith in drug treatments than most pharmacologists, They want to clutch at straws. A bit like the NICE guidance committee, faced with a bunch of treatments most of which are almost ineffective, clutched at the straws of acupuncture and chiropractic. But this time it isn’t only the patients who are cross. It is most of the medical and scientific world too.
One interpretation of these bizarre events is that they represent a case of medical/scientific arrogance. Ben Goldacre wrote of another aspect of the same problem thus week, in Dodgy academic PR [download the paper on which this is based].
The first job of a scientist is to say openly when the answer to a question is not known. But scientists are under constant pressure to exaggerate the importance of their results. Last year we published an article which I feel may, if verified, turn out to be the second most important that I have ever been an author on. Because it happened to be published in Nature (not because of its quality), a press release was written (by an arts graduate!). It took some argument to prevent the distorted and exaggerated account being imposed on the public. This is typical of the sort of thing reported in Goldacre’s column. I reported a similar case a while ago, Why honey isn’t a wonder cough cure: more academic spin.
If NICE does not reconsider this guidance, it is hard to see how it can be taken seriously in the future. I hope that when NICE’s director, Professor Sir Michael Rawlins, returns from his trips abroad, he will find time to look at the case himself.
Indirectly, then, it can be argued that NICE’s bizarre guidance is just another manifestation of the management of science being passed from the hands of scientists into the hands of administrators and spin experts. It is yet another example of DC’s rule
Never trust anyone who uses the word ‘stakeholder’
Some bone-headed bureaucrat decides that any charlatan or quack is a ‘stakeholder’ in the provision of NHS care and gives them a quite disproportionate say in how taxpayers’ money is spent. The bureaucrats are so busy following processes and procedures, ticking boxes, and so deficient in scientific education, that they failed to notice that they’ve been caught out by the old trick of used car salesmen, bait and switch.
The consequences
The expected consequences have already started to materialise. The Prince of Wales’ Foundation for Magic Medicine is jubilant about having been endorsed by NICE. And I’m told that “The chiropractors have now just written letters to all health boards in Scotland asking for contracts for their services to deal with back pain”.
There could hardly have been a worse time for NICE to endorse chiropractic. We are in the middle of a storm about free speech because of the disgraceful action of the British Chiropractic Associaton in suing one of our best science writers, Simon Singh, for defamation because he had the temerity to express an opinion, Of course, even if the BCA wins in court, it will be the overall loser, because chiropractic claims are now being scrutinised as never before (just look at what they told me).
Follow-up
A much-cited paper. The paper that is most often cited by chiropractors who claim to be able to cure colic by spinal manipulation is Klougart N, Nilsson N and Jacobsen J (1989) Infantile Colic Treated by Chiropractors: A Prospective Study of 316 Cases, J Manip Physiol Ther,12:281-288. This is not easy to get hold of but Steve Vogel has sent me s scanned copy which you can download here. As evidence it is about as useless as the infamous Spence study so beloved of homeopaths. There was no control group at all. It simply follows 316 babies and found that most of them eventually got better. Well, they do, don’t they? It is a sign of the pathetic standard of reaearch in chiropractic that anyone should think this paper worth mentioning at all.
June 6 2009. More flak for NICE from the Royal College of Anaesthetists, and more adverse comment in the BMJ. And of course the blogs. for example, “If this is “evidence based medicine” I want my old job back“.
“Acupuncture on the NHS: a dangerous precedent”: a good analysis at counterknowledge.com.
June 6 2009, Comment sent to the BMJ. The comment was submitted, as below, early on Friday 5th June. The BMJ said it was a “sensitive issue” and for the next five days lawyers pondered over it.
Underwood and Littlejohns describe their guidance as being a “landmark”. I can only agree with that description. It is the first time that NICE has ever endorsed alternative medicine in the face of all the evidence. The guidance group could hardly have picked a worse moment to endorse chiropractic. Chiropractors find it so hard to find evidence for their practices that, when one of our finest science writers, Simon Singh, asked to see the evidence they sued him for defamation. I suggest that the guidance group should look at the formidable list of people who are supporting Singh, after his brave decision to appeal against this iniquitous persecution.
Of course I’m sure this bizarre decision has nothing to do with the presence on the guidance group of Peter Dixon, chair of the General Chiropractic Council. Nevertheless, I am curious to know why it is that when I telephoned two of the practices belonging to Peter Dixon Associates, I was told that they could probably treat infantile colic and asthma. Such claims have just been condemned by the Advertising Standards Authority.
The low back pain guidance stands a good chance of destroying NICE’s previously excellent reputation for dispassionate assessment of benefits and costs. Yes, that is indeed a landmark of sorts.
If NICE is ever to recover its reputation, I think that it will have to start again. Next time it will have to admit openly that none of the treatments work very well in most cases. And it will have to recognise properly the disastrous cultural consequences of giving endorsement to people who, when asked to produce evidence, resort to legal intimidation.
Eventually, on Wednesday 10 June the comment appeared in the BMJ, and it wasn’t greatly changed. Nevertheless if is yet another example of legal chill. This is the final version.
Underwood and Littlejohns describe their guidance as being a “landmark”. I can only agree with that description. It is the first time that NICE has ever endorsed alternative medicine in the face of all the evidence. The guidance group could hardly have picked a worse moment to endorse chiropractic. Chiropractors are so sensitive about criticisms of their practices that, when one of our finest science writers, Simon Singh, queried the evidence-base for their therapeutic claims they sued him for defamation. I suggest that the guidance group should look at the formidable list of people who are supporting Singh, after his brave decision to appeal against an illiberal court ruling in this iniquitous persecution.
One wonders whether this bizarre decision by NICE has anything to do with the presence on the guidance group of Peter Dixon, chair of the General Chiropractic Council. I am also curious to know why it is that when I telephoned two of the practices belonging to Peter Dixon Associates, I was told that chiropractic could be effective in the treatment of infantile colic and asthma. Similar claims about treating colic have just been condemned by the Advertising Standards Authority.
The low back pain guidance stands a good chance of destroying NICE’s previously excellent reputation for dispassionate assessment of benefits and costs. Yes, that is indeed a landmark of sorts.
If NICE is ever to recover its reputation, I think that it will have to start again. Next time it will have to admit openly that none of the treatments works very well in most cases. And it will have to recognise properly the disastrous cultural consequences of giving endorsement to people who, instead of engaging in scientific debate, resort to legal intimidation.
Bait and switch. Oh dear, oh dear. Just look at this. British Chiropractic Association tell their members to hide their sins from prying eyes.
Excellent round-up of the recent outburst of writing about “chiroquacktic” (Tut, tut, is there no respect?).
Dr Crippen writes “NICE recommends a cure for all known disease” [Ed some exaggeration, surely]