David Colquhoun
More boring politics, but it matters. The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register should normally be through a Bachelor degree with Honours
For the background on this appalling report, see earlier posts.
A very bad report: gamma minus for the vice-chancellor
The Times (blame subeditor for the horrid title), and some follow up on the Times piece
The Health Professions Council breaks its own rules: the result is nonsense
Chinese medicine -acupuncture gobbledygook revealed
Consultation opens on the Pittilo report: help stop the Department of Health making a fool of itself
Why degrees in Chinese medicine are a danger to patients
The Department of Health consultation shuts on November 2nd. If you haven’t responded yet, please do. It would be an enormous setback for reason and common sense if the government were to give a stamp of official approval to people who are often no more than snake-oil salesman.
Today I emailed my submission to the Pittilo consultation to the Department of Health, at HRDListening@dh.gsi.gov.uk
The submission
I sent the following documents, updated versions of those already posted earlier.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
- An example of dangerous (and probably illegal) claims that are routinely made by TCM practitioners [download pdf]f
I also completed their questionnaire, despite its deficiencies. In case it is any help to anyone, this is what I said:
The questionnaire
Q1: What evidence is there of harm to the public currently as a result of the activities of acupuncturists, herbalists and traditional Chinese medicine practitioners? What is its likelihood and severity?
Harm
No Harm
Unsure
Comment
The major source of harm is the cruel deception involved in making false claims of benefit to desperate patients. This applies to all three.
In the case of herbal and TCM there is danger from toxicity because herbal preparations are unstandardised so those that do contain an active ingredient are given in an unknown dose. This is irresponsible and dangerous (but would not be changed by the proposals for regulation).
In addition TCM suffers from recurrent problems of contamination with heavy metals, prescription drugs and so on. Again this would not be the business of the proposed form of regulation.
Q2: Would this harm be lessened by statutory regulation? If so, how?
Yes
No
Unsure
The proposed form of regulation would be no help at all. The HPC has already said that it is not concerned with whether or not the drug works, and, by implication, does not see itself as preventing false health claims (just as the GCC doesn’t do this). False claims are the responsibility of Trading Standards who are meant to enforce the Consumer Protection Unfair Trading Regulations (May 2008), though they do not at present enforce them very effectively. Also Advertisng Standards. The proposed regulation would not help, and could easily hinder public safety as shown by the fact that the GCC has itself been referred to the Advertisng Standards Authority.
The questions of toxicity and contamination are already the responsibility of Trading Standards and the MHRA. Regulation by the HPC would not help at all. The HPC is not competent to deal with such questions.
Q3: What do you envisage would be the benefit to the public, to practitioners and to businesses, associated with introducing statutory regulation?
Significant benefit
Some benefit
No benefit
Unsure
This question is badly formulated because the answer is different according to whether you are referring to the public, to practitioners or to businesses.
The public would be endangered by the form of regulation that is proposed, as is shown very clearly by the documents that I have submitted separately.
In the case of practitioners and businesses, there might be a small benefit, if the statutory regulation gave the impression that HM and TCM had government endorsement and must therefore be safe and effective.
There is also one way that the regulation could harm practitioners and businesses. If the HPC received a very large number of complaints about false health claims, just as the GCC has done recently, not only would it cost a large amount of money to process the claims, but the attendant bad publicity could harm practitioners. It is quite likely that this would occur since false claims to benefit sick people are rife in the areas of acupuncture, HM and TCM.
Q4: What do you envisage would be the regulatory burden and financial costs to the public, to practitioners, and to businesses, associated with introducing statutory regulation? Are these costs justified by the benefits and are they proportionate to the risks? If so, in what way?
Justified
Not Justified
Unsure
Certainly not justified. Given that I believe that the proposed form of regulation would endanger patients, no cost at all would be justified. But even if there were a marginal benefit, the cost would be quite unjustified. The number of practitioners involved is very large. It would involve a huge expansion of an existing quango, at a time when the government is trying to reduce the number of quangos. Furthermore, if the HPC were flooded with complaints about false health claims, as the GCC has been, the costs in legal fees could be enormous.
Q5: If herbal and TCM practitioners are subject to statutory regulation, should the right to prepare and commission unlicensed herbal medicines be restricted to statutorily regulated practitioners?
Yes
No
Unsure
I don’t think it would make much difference. The same (often false) ideas are shared by all HM people and that would continue to be the same with or without SR.
Q6: If herbal and TCM practitioners are not statutorily regulated, how (if at all) should unlicensed herbal medicines prepared or commissioned by these practitioners be regulated?
They could carry on as now, but the money that would have been spent on SR should instead be used to give the Office of Trading Standards and the MHRA the ability to exert closer scrutiny and to enforce more effectively laws that already exist. Present laws, if enforced, are quite enough to protect the public.
Q7: What would be the effect on public, practitioners and businesses if, in order to comply with the requirements of European medicines legislation, practitioners were unable to supply manufactured unlicensed herbal medicines commissioned from a third party?
Significant effect
Some effect
No effect
Unsure
European laws,especialliy in food area, are getting quite strict about the matters of efficacy. The proposed regulation, which ignores efficacy, could well be incompatible with European law, if not now, then soon. This would do no harm to legitimate business though it might affect adversely businesses which make false claims (and there are rather a lot of the latter).
Q8: How might the risk of harm to the public be reduced other than by orthodox statutory regulation? For example by voluntary self-regulation underpinned by consumer protection legislation and by greater public awareness, by accreditation of voluntary registration bodies, or by a statutory or voluntary licensing regime?
Voluntary self-regulation
Accreditation of voluntary bodies
Statutory or voluntary licensing
Unsure
I disagree with the premise, for reasons given in detail in separate documents. I believe that ‘orthodox statutory regulation’, if that means the Pittilo proposals, would increase, not decrease, the risk to the public. Strengthening the powers of Trading Standards, the MHRA and such consumer protection legislation would be far more effective in reducing risk to the public than the HPC could ever be. Greater public awareness of the weakness of the evidence for the efficacy of these treatments would obviously help too, but can’t do the job on its own.
Q10: What would you envisage would be the benefits to the public, to practitioners, and to businesses, for the alternatives to statutory regulation outlined at Question 8?
It depends on which alternative you are referring to. The major benefit of enforcement of existing laws by Trading Standards and/or the MHRA would be (a) to protect the public from risk, (b) to protect the public from health fraud and (c) almost certainly lower cost to the tax payer.
Q11: If you feel that not all three practitioner groups justify statutory regulation, which group(s) does/do not and please give your reasons why/why not?
Acupuncture
Herbal Medicine
TCM
Unsure
None of them. The differences are marginal. In the case of acupuncture there has been far more good research than for HM or TCM. But the result of that research is to show that in most cases the effects are likely to be no more than those expected of a rather theatrical placebo. Furthermore the extent to which acupuncture has a bigger effect than no-acupuncture in a NON-BLIND comparison, is usually too small and transient to offer any clinical advantage (so it doesn’t really matter whether the effect is placebo or not, it is too small to be useful).
In the case of HM, and even more of TCM, there is simply not enough research to give much idea of their usefulness, with a small handful of exceptions.
This leads to a conclusion that DH seems to have ignored in the past. It makes absolutely no sense to talk about “properly trained practitioners” without first deciding whether the treatments work or not. There can be no such thing as “proper training” in a discipline that offers no benefit over placebo. It is a major fault of the Pittilo recommendations that they (a) ignore this basic principle and (b) are very over-optimistic about the state of the evidence.
Q12: Would it be helpful to the public for these practitioners to be regulated in a way which differentiates them from the regulatory regime for mainstream professions publicly perceived as having an evidence base of clinical effectiveness? If so, why? If not, why not?
Yes
No
Unsure
It might indeed be useful if regulation pointed out the very thin evidence base for HM and TCM but it would look rather silly. The public would say how can it be that the DH is granting statutory regulation to things that don’t work?
Q13: Given the Government’s commitment to reducing the overall burden of unnecessary statutory regulation, can you suggest which areas of healthcare practice present sufficiently low risk so that they could be regulated in a different, less burdensome way or de-regulated, if a decision is made to statutorily regulate acupuncturists, herbalists and traditional Chinese medicine practitioners?
Yes
No
Unsure
As stated above, the.only form of regulation that is needed, and the only form that would protect the public, is through consumer protection regulations, most of which already exist (though they are enforced in a very inconsistent way). Most statutory regulation is objectionable, not on libertarian grounds, but because it doesn’t achieve the desired ends (and is expensive). In this case of folk medicine, like HM and TCM, the effect would be exactly the opposite of that desired as shown in separate documents that I have submitted to the consultation.
Q14: If there were to be statutory regulation, should the Health Professions Council (HPC) regulate all three professions? If not, which one(s) should the HPC not regulate?
Yes
No
Unsure
The HPC should regulate none of them. It has never before regulated any form of alternative medicine and it is ill-equipped to do so. Its statement that it doesn’t matter that there is very little evidence that the treatments work poses a danger to patients (as well as being contrary to its own rules).
Q15: If there were to be statutory regulation, should the Health Professions Council or the General Pharmaceutical Council/Pharmaceutical Society of Northern Ireland regulate herbal medicine and traditional Chinese medicine practitioners?
HPC
GPC/PSNI
Unsure
Neither. The GPC is unlikely to care about whether the treatments work any more than the RPSGB did, or the GCC does now. The problems would be exactly the same whichever body did it.
Q16: If neither, who should and why?
As I have said repeatedly, it should be left to Trading Standards, the MHRA and other consumer protection regulation.
Q17:
a) Should acupuncture be subject to a different form of regulation from that for herbalism and traditional Chinese medicine? If so, what?
Yes
No
Unsure
b) Can acupuncture be adequately regulated through local means, for example through Health and Safety legislation, Trading Standards legislation and Local Authority licensing?
Yes
No
Unsure
(a) No -all should be treated the same. Acupuncture is part of TCM
(b) Yes
Q18.
a) Should the titles acupuncturist, herbalist and [traditional] Chinese medicine practitioner be protected?
b) If your answer is no which ones do you consider should not be legally protected?
Yes
No
Unsure
No. It makes no sense to protect titles until such time as it has been shown that the practitioners can make a useful contribution to medicine (above placebo effect). That does not deny that placebos may be useful at times. but if that is all they are doing, the title should be ‘placebo practitioners’.
Q19: Should a new model of regulation be tested where it is the functions of acupuncture, herbal medicine and TCM that are protected, rather than the titles of acupuncturist, herbalist or Chinese medicine practitioner?
Yes
No
Unsure
No. This makes absolutely no sense when there is so little knowledge about what is meant by the ” functions of acupuncture, herbal medicine and TCM”.Insofar as they don’t work (better than placebo), there IS no function. Any attempt to define function when there is so little solid evidence (at least for HM and TCM) is doomed to failure.
Q20: If statutory professional self-regulation is progressed, with a model of protection of title, do you agree with the proposals for “grandparenting” set out in the Pittilo report?
Yes
No
Unsure
No. I believe the Pittilo report should be ignored entirely. The whole process needs to be thought out again in a more rational way.
Q22: Could practitioners demonstrate compliance with regulatory requirements and communicate effectively with regulators, the public and other healthcare professionals if they do not achieve the standard of English language competence normally required for UK registration? What additional costs would occur for both practitioners and regulatory authorities in this case?
Yes
No
Unsure
No. It is a serious problem, in TCM especially, that many High Street practitioners speak hardly any English at all. That adds severely to the already considerable risks. There would be no reliable way to convey what was expected of them. it would be absurd for the taxpayer to pay for them to learn English for the purposes of practising TCM (of course there might be the same case as for any other immigrant for teaching English on social grounds).
Q23: What would the impact be on the public, practitioners and businesses (financial and regulatory burden) if practitioners unable to achieve an English language IELTS score of 6.5 or above are unable to register in the UK?
Significant impact
Some impact
No impact
Unsure
The question is not relevant. The aim of regulation is to protect the public from risk (and it should be, but isn’t, an aim to protect them from health fraud). It is not the job of regulation to promote businesses
Q24: Are there any other matters you wish to draw to our attention?
I have submitted three documents via HRDListening@dh.gsi.gov.uk. The first of these puts the case against the form of regulation proposed by Pittilo, far more fluently than is possible in a questionnaire.
Another shows examples of what is actually taught in degrees in acupuncture, HM and TCM. They show very graphically the extent to which the Pittilo proposals would endanger the public, if they were to be implemented..
Chiropractors are getting very touchy indeed, all over the world. And no wonder, because their claims are being exposed as baseless as never before, in the wake of their attempts to stifle criticism by legal action..
In March, Shaun Holt appeared on Breakfast TV in New Zealand. Holt has done a lot of good work on TV in debunking some of the preposterous claims made by quacks. See him on YouTube.
This time he talked about chiropractic. Here is the video.
One could argue that he was over generous to chiropractic, especially when talking about their effectiveness in treating low back pain. He said, quite rightly, that chiropractors are no better than physiotherapists at treating low back pain.
But a recent trial suggests that neither are much good. “A randomised controlled trial of spinal manipulative therapy in acute low back pain” (Juni et al., 2009 in the BMJ; see also coverage in Pulse). This trial compared standard care with standard care plus spinal manipulative therapy (SMT). The results were negative, despite the fact that this sort of A + B vs B design is inherently biassed in favour of the treatment (see A trial design that generates only ”positive” results, Ernst & Lee 2008, Postgrad Med J.).
"SMT was performed by a specialist in manual medicine, chiropractice and rheumatology (GH), a specialist in physical medicine (DV) or an osteopath (RvB), all proficient in SMT."
"Conclusions: SMT is unlikely to result in relevant early pain reduction in patients with acute low back pain."
Admittedly, the trial was quite small (104 patients, 52 in each group) so it will need to be confirmed. but the result is entirely in line with what we knew already.
It also adds to the evidence that the recommendation by NICE of SMT by chiropractors constitutes their biggest failure ever to assess evidence properly. If NICE don’t amend this advice soon, they are in danger of damaging their hitherto excellent record.
Despite the moderate tone and accuracy of what Holt said on TV, the New Zealand Chiropractors’ Association made a formal complaint. That is what they like to do, as I learned recently, to my cost. It is so much easier than producing evidence.
Quite absurdly the New Zealand Broadcasting Standards Authority (BSA) has upheld some of the complaints. Their judgement can be read here.
The BSA consists of four people, two lawyers and two journalists. So not a trace of scientific expertise among them. Having people like that judging the claims of chiropractors makes as much sense as having them judged by Mr Justice Eady. They seem to be the sort of people who think that if there is a disagreement, the truth must lie half-way between the opposing views.
One of the BSA members, Tapu Misa, has used her newspaper column to quote approvingly the views of the notorious Dr Mercola web site on flu prevention “Your best defence, it says, is to eat right, get lots of sleep, avoid sugar and stress, load up on garlic, Vitamin D and krill oil”. (Snake oil is said to be good too.) There are some odd attitudes to science in some of her other columns too (e.g. here and here). Not quite the person to be judging the evidence for and against chiropractic, I think.
In fact the TV show in question was more than fair to chiropractors. It adopted the media’s usual interpretation of fair and balanced: equal time for the flat earthers. A Chiropractor was invited to reply to Holt’s piece. Here he is.
The chiropractor, Doug Blackbourn, started very plausibly, though a tendency to omit every third syllable made transcription hard work. He established that if you cut yourself you get better (without any help). He established that nerves run down the spinal cord. So far, so good. But then he quickly moved on to the usual flights of fancy.
"We have two premises. The body heals itself and the nervous system runs the body. Now the nervous system runs the body, travels down through the spinal cord so chiropractic is not based on the belief that, you know, energy flows, it’s based on the fact that your nervous system runs the body and [inaudible] affects the overall health of the body"
This statement is totally vague. It has nothing whatsoever to do with the main question, can chiropractors do anything useful. It is sheer flannel.
We’re seeing people, heck, diabetes. I had a quadriplegic come in one time for adjustment, we’ve got stroke people, we’ve got all sorts of conditions. We’re not treating the condition, We’re allowing, checking the spine to see if there’s any interference there that will slow the body down"
“Interference”? “slowing the body down”? These are utterly meaningless phrases that simply serve to distract from the only question that matters.
"Chiropractice is the most safest [sic] profession to go to to get your spine adjusted"
Hmm I thought it was the only job that uses the word ‘adjustment’.
Worst of all was his response to a question about asthma.
Presenter: "So chiropractors are not out there claiming they will cure asthma for example?". Chiropractor: "No"
This is simply untrue, both in New Zealand and in the UK. For a start, just look at what Blackbourn’s own web site says about asthma.
"The challenge, of course, with allergy and asthma medication is there is no end-point. There is no cure. Asthma and allergies, for the most part, are lifelong conditions requiring lifelong medication. Might there be a better way, an alternative solution?
“Alternative” is the key word. Medical treatment is designed to combat symptoms, and is successful to a certain extent with allergies and asthma. Underlying causes are not addressed, however, and symptoms continue year after year. What else might be done?
Enter chiropractic care. Chiropractic health care, with its unique comprehensive approach, is able to offer positive benefit to a variety of conditions and ailments. In the case of allergies and asthma, these “hypersensitivity conditions” may respond well to therapy designed to normalize the body’s flow of nerve signals. To use a metaphor, chiropractic treatment removes roadblocks to the body’s natural healing abilities. Restoring these imbalances may help reduce such hypersensitivity reactions."
Blackbourn’s web site describes him thus
"As a Doctor of Chiropractic, Dr. Doug Blackbourn . . ."
But the qualifications of “Dr” Blackbourn are B.App.Sc (Chiro) M.N.Z.C.A , the same as those of “Dr” Brian Kelly.
After a performance like this, perhaps someone should submit a complaint to the New Zealand Broadcasting Standards Authority.
After all, I notice that they have dismissed complaints from one chiropractor, Sean Parker, after a TV programme looked at the business practices of his private chiropractic practice, The Spinal Health Foundation. Perhaps the BSA understands business better than it understands science.
Follow-up
Is chiropractic crumbling in New Zealand? The New Zealand College of Chiropractic featured in my editorial in the New Zealand Medical Journal, and in the fallout from that article, It’s principle, “Dr” Brian Kelly (B App Sci (Chiro)) seems to be getting desperate. His college is now canvassing for recruits in Canada. They are promised all the woo.
- Subluxation centered techniques – Gonstead, Toggle Recoil, Thompson, Diversified
- Traditional philosophy featuring vitalism and innate healing – congruent curriculum
Perhaps Canada is a good place to recruit, gven the $500 million class action being brought against chiropractors in Canada, after Sandra Nette became tetraplegic immediately after a chiropractor manipulated her neck, Canadian chiropractors must be looking for somewhere to hide.
Stuff and Nonsense. jdc described this story at the time the complaint was lodged.
Shaun Holt’s own blog follows the action.
New Zealand Doctor covers the story.
Bay of Plenty Times “Bay researcher slams television complaint ruling“
In July 2008 I wrote an editorial in the New Zealand Medical Journal (NZMJ), at the request of its editor.
The title was Dr Who? deception by chiropractors. It was not very flattering and it resulted in a letter from lawyers representing the New Zealand Chiropractic Association. Luckily the editor of the NZMJ, Frank Frizelle, is a man of principle, and the legal action was averted. It also resulted in some interesting discussions with disillusioned chiropractors that confirmed one’s worst fears. Not to mention revealing the internecine warfare between one chiropractor and another.
This all occurred before the British Chiropractic Association sued Simon Singh for defamation. The strength of the reaction to that foolhardy action now has chiropractors wondering if they can survive at all. The baselessness of most of their claims has been exposed as never before. No wonder they are running scared. The whole basis of their business is imploding.
Needless to say chiropractors were very cross indeed. Then in February 2009 I had a polite email from a New Zealand chiropractor, David Owen, asking for help to find one of the references in the editorial. I’d quoted Preston Long as saying
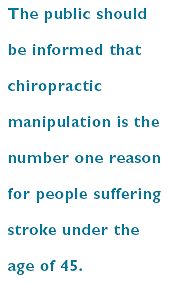
"Long (2004)7 said “the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45.”
And I’d given the reference as
7. Long PH. Stroke and spinal manipulation. J Quality Health Care. 2004;3:8–10
I’d found the quotation, and the reference, in Ernst’s 2005 article, The value of Chiropractic, but at the time I couldn’t find the Journal of Quality Healthcare. I did find the same article on the web. At least the article had the same title, the same author and the same quotation. But after finding, and reading, the article, I neglected to change the reference from J Quality Health Care to http://skepticreport.com/sr/?p=88. I should have done so and for that I apologise.
When I asked Ernst about the Journal of Quality Healthcare, he couldn’t find his copy of the Journal either, but he and his secretary embarked on a hunt for it, and eventually it was found.

![]()
|
It turns out that Journal of Quality Healthcare shut down in 2004, without leaving a trace on the web, or even in the British Library. It was replaced by a different journal, Patient Safety and Quality Healthcare (PSQH) A reprint was obtained from them. It is indeed the same as the web version that I’d read, and it highlighted the quotation in question. The reprint of the original article, which proved so hard to find, can be downloaded here. |
|
The full quotation is this
"Sixty-two clinical neurologists from across Canada, all certified members of the Royal College of Physicians and Surgeons, issued a warning to the Canadian public, which was reported by Brad Stewart, MD. The warning was entitled Canadian Neurologists Warn Against Neck Manipulation. The final conclusion was that endless non-scientific claims are being made as to the uses of neck manipulation(Stewart, 2003). They need to be stopped. The public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45."
I have often condemned the practice of citing papers without reading them (it is, of course, distressingly common), so I feel bad about this, though I had in fact read the paper in question in its web version. I’m writing about it because I feel one should be open about mistakes, even small ones.
I’m also writing about it because one small section of the magic medicine community seems to think they have nailed me because of it. David Owen, the New Zealand chiropractor, wrote to the editor of the NZMJ, thus.
|
The quote [in question] is the public should be informed that chiropractic manipulation is the number one reason for people suffering stroke under the age of 45. Long PH. Stroke and Manipulation. J Quality Health Care. 2004:3:8-10 This quote actually comes from the following blog article http://www.skepticreport.com/medicalquackery/strokespinal.htm [DC the URL is now http://skepticreport.com/sr/?p=88] I have attached all my personal communications with Colquhoun. They demonstrate this is not a citation error. Prof Colquhoun believes the origin of the quote doesn’t matter because Long was quoting from a Canadian Neurologists’ report (this is also incorrect). As you can see he fails to provide any evidence at all to support the existance [sic] of the “J Quality Health Care.” Colquhoun ‘s belief that my forwarding this complaint is me “resorting to threats” is the final nail in the coffin. If he had any leg to stand on where is the threat? This may seem pedantic but it surely reflects a serious ethical breach. Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility? Incidentally, at the end of the article, conflicts of interest are listed as none. As Colquhoun is a Professor of Pharmacology and much of his research funding no doubt comes from the pharmaceutical industry how can he have no conflict of interest with therapies that do not advocate the use of drugs and compete directly against the billions spent on pain medications each year? If I may quote Colquhoun himself in his defence of his article (Journal of the New Zealand Medical Association, 05-September-2008, Vol 121 No 1281) I’ll admit, though, that perhaps ‘intellect’ is not what’s deficient in this case, but rather honesty. David Owen |
Financial interests
Well, here is a threat: I’m exposed as a shill of Big Pharma. ". . . much of his funding no doubt comes from the pharmaceutical industry". I can’t count how many times this accusation has been thrown at me by advocates of magic medicine. Oddly enough none of them has actually taken the trouble to find out where my research funding has come from. None of them even knows enough about the business to realise the extreme improbability that the Pharmaceutical Industry would be interested in funding basic work on the stochastic properties of single molecules. They fund only clinicians who can help to improve their profits,
The matter of funding is already on record, but I’ll repeat it now. The media ‘nutritional therapist’, Patrick Holford, said, in the British Medical Journal
“I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry “
To which my reply was
” Oh dear, Patrick Holford really should check before saying things like “I notice that Professor David Colquhoun has so far not felt it relevant to mention his own competing interests and financial involvements with the pharmaceutical industry”. Unlike Holford, when I said “no competing interests”, I meant it. My research has never been funded by the drug industry, but always by the Medical Research Council or by the Wellcome Trust. Neither have I accepted hospitality or travel to conferences from them. That is because I would never want to run the risk of judgements being clouded by money. The only time I have ever taken money from industry is in the form of modest fees that I got for giving a series of lectures on the basic mathematical principles of drug-receptor interaction, a few years ago.”
I spend a lot of my spare time, and a bit of my own money, in an attempt to bring some sense into the arguments. The alternative medicine gurus make their livings (in some cases large fortunes) out of their wares.
So who has the vested interest?
Does chiropractic actually cause stroke?
As in the case of drugs and diet, it is remarkably difficult to be sure about causality. A patient suffers a vertebral artery dissection shortly after visiting a chiropractor, but did the neck manipulation cause the stroke? Or did it precipitate the stroke in somebody predisposed to one? Or is the timing just coincidence and the stroke would have happened anyway? There has been a lot of discussion about this and a forthcoming analysis will tackle the problem of causality head-on,
My assessment at the moment, for what it’s worth, is that there are some pretty good reasons to suspect that neck manipulation can be dangerous, but it seems that serious damage is rare.
In a sense, it really doesn’t matter much anyway, because it is now apparent that chiropractic is pretty well discredited without having to resort to arguments about rare (though serious) effects. There is real doubt about whether it is even any good for back pain (see Cochrane review), and good reason to think that the very common claims of chiropractors to be able to cure infant colic, asthma and so on are entirely, ahem, bogus. (See also Steven Novella, ebm-first, and innumerable other recent analyses.)
Chiropractic is entirely discredited, whether or not it may occasionally kill people.
Complaint sent to UCL
I had an enquiry about this problem also from my old friend George Lewith. I told him what had happened. Soon after this, a complaint was sent to Tim Perry and Jason Clarke, UCL’s Director and Deputy Director of Academic Services. The letter came not from Lewith or Owen, but from Lionel Milgom. Milgrom is well known in the magic medicine community for writing papers about how homeopathy can be “explained” by quantum entanglement. Unfortunately for him, his papers have been read by some real physicists and they are no more than rather pretentious metaphors. See, for example, Danny Chrastina’s analysis, and shpalman, here. Not to mention Lewis, AP Gaylard and Orac.
|
Dear Mr Perry and Mr Clark, I would like to bring to your attention an editorial (below) that appeared in the most recent issue of the New Zealand Medical Journal. In it, one of your Emeritus Professors, David Colquhoun, is accused of a serious ethical breach, and I quote – “Is it acceptable to make up a reference to try and slip any unsupported statement into a “scientific” argument and thereby give it some degree of credibility?” Professor Colquhoun is well-known for writing extensively and publicly excoriating many forms of complementary and alternative medicine, particularly with regard to the alleged unscientific nature and unethical behaviour of its practitioners. Professor Colquhoun is also a voluble champion for keeping the libel laws out of science. While such activities are doubtlessly in accord with the venerable Benthamite liberal traditions of UCL, I am quite certain hypocrisy is not. And though Professor Colquhoun has owned up to his error, as the NZMJ’s editor implies, it leaves a question mark over his credibility. As custodians of the college’s academic quality therefore, you might care to consider the possible damage to UCL’s reputation of perceived professorial cant; emeritus or otherwise. Yours Sincerely Dr Lionel R Milgrom |
So, as we have seen, the quotation was correct, the reference was correct, and I’d read the article from which it came I made a mistake in citing the original paper rather than the web version of the same paper..
I leave it to the reader to judge whether this constitutes a "serious ethical breach", whether I’d slipped in an "unsupported statement", and whether it constitutes "hypocrisy"
Follow-up
It so happens that no sooner was this posted than there appeared Part 2 of the devastating refutation of Lionel Milgrom’s attempt to defend homeopathy, written by AP Gaylard. Thanks to Mojo (comment #2) for pointing this out.
Being interested in science communication, I was pleased when the BMJ asked me to review Unscientific America , by Chris Monney and Sheril Kirshenbaum.
The BMJ provides a link that allows you access to the whole review. They have made very few changes from the submitted version, which is reproduced below (with live links in the text. [Download pdf of print version]
I very soon discovered that the book had already caused ructions in the USA, as a result of its advocacy of appeasement of religious groups. In particular there was all out war with P.Z.Myers, whose very popular blog, Pharyngula. documented the battle in detail).
It is an American book through and through, and in the USA the biggest threat to reason comes from the far-right religious fundamentalists who preach young-earth creationism. It is said that 46% of US citizens believe that the earth is less than 10,000 years old. The same far-right religious groups also preach that carrying guns is good, that Iraq was responsible for 9/11, that climate change is a socialist conspiracy and that health care for everyone is a communist plot. And they never hesitate to lie in the promotion of their ‘religious’ views. The US situation is totally different from that in Europe, where religion is all but dead, and young earth creationism is the preserve of a few cranky used-car dealers (and possibly Tony Blair?)
|
Review of the Week Trust me, I’m a scientist David Colquhoun, professor of pharmacology, University College London Unscientific America sounds like a fascinating topic, not least because the book is a follow-up from Mooney’s The Republican War on Science. It is written entirely from a US perspective (the USA sequenced the genome and invented the internet, apparently unaided). It’s reported that 46 percent of Americans believe that the earth is less than 10,000 years old. That’s certainly cause for alarm and Mooney & Kirshenbaum are certainly alarmed. They think that the public needs to be educated in science. They identify the obvious problems, evolution, climate change and quackery and ask what can be done. The problem is that they propose no good solutions, and some bad ones. Their aims are worthy but sometimes the book reads like an over-long and somewhat condescending whine about why science and scientists are not sufficiently appreciated. I simply don’t think that it’s true that the public are not interested in science, nor that they can’t understand it at a level that is sufficient to be useful. It’s true that they have been let down badly by some sections of the media. Think particularly of the “great MMR hoax”1. The disastrous fall in vaccination is more attributable to talk show presenters and air-headed celebrities than to lack of interest from the public. People are systematically deceived by anti-vaxers, climate change denialists, vitamin pill salesmen and a horde of crackpot alternative therapists. There is one problem that Mooney & Kirshenbaum don’t talk about at all, yet it seems to me to be one of the biggest problems in science communication. It isn’t lack of interest by the public, nor even lack of understanding, but lack of trust. The tendency of real science to indulge in hyperbolic self-promotion is one reason for the lack of trust. Sometimes this descends into outright dishonesty2,3. That is a tendency that is promoted by government and funding agencies by their insistence on imposing silly performance measures. The public is quite sensible enough to take with a pinch of salt the almost daily announcements of “cancer cures” that emanate from university press offices. On the face of it, one should be encouraged that ‘public engagement in science’ is the mode du jour. It isn’t quite that simple though. Only too often, universities regard public engagement as a branch of their own PR machine4. They even instruct you about what tone of voice to use when talking publicly. One reason why scientists need to talk to people outside the lab is precisely to counteract this tide of nonsense from PR people, who are paid to deceive. The problem for academics is usually time. We already do three jobs, teaching, research and coping with HR bollocks. How can we find time for a fourth job? That’s not easy, especially for the best researchers (those that do research themselves, not just lead a team). Mooney & Kirshenbaum suggest that the solution is to create a “cadre of communication and outreach experts”. I don’t think this would work. They would, by and large, be outsiders, writing uncritical paeans, dictated by big name scientists. A new cadre of PR hangers-on does not sound like a great idea. A better, and very much cheaper, solution would be to provide a course in free blogging software and we’ll do it ourselves. The two chapters that I looked forward to reading, on religion and on “The bloggers cannot save us”, proved deeply disappointing. The authors are firmly in the camp of what Richard Dawkins called the “Neville Chamberlain school of evolutionists&rdquo.; They maintain “if the goal is to create an America more friendly to science and reason, the combativeness of the New Atheists is strongly counterproductive”. They are particularly critical of P.Z. Myers5, the University of Minnesota developmental biologist who is splendidly clear in his views. Of the communion wafer, he famously said “It’s a frackin’ cracker”. But he, and Dawkins, are right. When it comes to young earth creationists we have a war on our hands, and nowhere more than in the USA. What’s more it’s a winnable war. Mooney & Kirshenbaum are all for appeasement, but appeasement won’t work. It might please the more moderate wings of the church, but they already believe in evolution and are regarded by fundamentalists as being just as big an enemy as Myers and Dawkins. And, one must ask, who has done best at getting a wide public readership? P.Z Myers’ blog, Pharyngula, has up to two million page views a month. Dawkins’ book The God Delusion has sold three million copies. In comparison the bland and often rather condescending corporate science web sites get tiny numbers of hits. In Europe in general, and the UK in particular, young earth creationists are not the major problem that they are in the USA, despite being supported by Tony Blair6. Perhaps the nearest analogy in Europe is the threat to reason from various sorts of crackpot medicine. The appeasers are widespread. The Royal Colleges and the Department of Health are at the forefront of the Neville Chamberlain approach. But appeasement hasn’t worked there either. What has worked is the revelation that university courses are teaching that “amethysts emit high yin energy”7. Or, in a lecture on herbal approaches for patients with cancer, “Legally, you cannot claim to cure cancer. This is not a problem because: ‘we treat people, not diseases’ “8. This is shocking stuff but it has not been unearthed by the corporate media, but by bloggers. I think Mooney and Kirshenbaum have it all wrong. They favour corporate communications, which are written by people outside science and which easily become mere PR machines for individuals and institutions. Such blogs are rarely popular and at their worst they threaten the honesty of science. More and more individual scientists have found that they can write their own blog. It costs next to nothing and you can say what you think. A few clicks and the world can read what you have to say. Forget corporate communications. Just do it yourself. It’s fun. And think of the money you’d save for doing science if the PR people were just fired. (1) Goldacre, B. The media’s MMR hoax. 2008 http://www.badscience.net/2008/08/the-medias-mmr-hoax/ (2) PLoS One. Ghostwriting documents now fully available on PLoS Medicine website. 21-8-2009 http://speakingofmedicine.plos.org/2009/08/21/ghostwriting-documents-now-fully-available-on-plos-medicine-website/ (3) Colquhoun, D. Universities Inc. in the UK. The Corporate Corruption of Higher Education: part 2. 6-12-2007 https://www.dcscience.net/?p=193 (4) Corbyn, Z. Nottingham raises eyebrows over definition of ‘public engagement’. 21-8-2008 http://www.timeshighereducation.co.uk/story.asp?sectioncode=26&storycode=403234 (5) Myers, P. Z. Pharyngula. 2009 http://scienceblogs.com/pharyngula/ (6) Pyke, N. Revealed: Blair’s link to schools that take the Creation literally (Independent 13 June 2004). 13-7-2004 http://www.independent.co.uk/news/uk/politics/revealed-blairs-link-to-schools-that-take-the-creation-literally-732032.html (7) Colquhoun, D. Westminster University BSc: "amethysts emit high yin energy". 23-4-2008 https://www.dcscience.net/?p=227 (8) Colquhoun, D. Herbal approaches for patients with cancer. 10-8-2009 https://www.dcscience.net/?p=2043 |
Follow-up
P.Z. Myers has posted about thie book review, on Pharyngula, as Is this book dead yet? There are a lot more comments there than here, though few of them address the question of science communications..
Butterflies and Wheels is generating a lot of hits
The King’s Fund recently published Assessing complementary practice Building consensus on appropriate research methods [or download pdf].

It is described as being the “Report of an independent advisory group”. I guess everyone knows by now that an “expert report” can be produced to back any view whatsoever simply by choosing the right “experts”, so the first things one does is to see who wrote it. Here they are.
- Chair: Professor Dame Carol Black
- Harry Cayton, Chief Executive, Council for Healthcare Regulatory Excellence
- Professor Adrian Eddleston, then Vice-Chairman, The King’s Fund
- Professor George Lewith, Professor of Health Research, Complementary and Integrated Medicine Research Unit, University of Southampton
- Professor Stephen Holgate, MRC Clinical Professor of Immunopharmacology, University of Southampton
- Professor Richard Lilford, Head of School of Health and Population Sciences, University of Birmingham
We see at once two of the best known apologists for alternative medicine, George Lewith (who has appeared here more than once) and Stephen Holgate.
Harry Cayton is CEO of Council for Healthcare Regulatory Excellence (CHRE) which must be one of the most useless box-ticking quangos in existence. It was the CHRE that praised the General Chiropractic Council (GCC) for the quality of its work. That is the same GCC that is at present trying to cope with 600 or so complaints about the people it is supposed to regulate (not to mention a vast number of complaints to Trading Standards Offices). The GCC must be the prime example of the folly of giving government endorsement to things that don’t work. But the CHRE were not smart enough to spot that little problem. No doubt Mr Cayton did good work for the Alzheimer’s Society. His advocacy of patient’s choice may have helped me personally. But it isn’t obvious to me that he is the least qualified to express an opinion on research methods in anything whatsoever. According to the Guardian he is “BA in English and linguistics from the University of Ulster; diploma in anthropology from the University of Durham; B Phil in philosophy of education from the University of Newcastle.”
Adrian Eddlestone is a retired Professor of Medicine. He has been in academic administration since 1983. His sympathy for alternative medicine is demonstrated by the fact that he is also Chair of the General Osteopathic Council, yet another “regulator” that has done nothing to protect the public
from false health claims (and which may, soon, find itself in the same sort of trouble as the GCC).
Richard Lilford is the only member of the group who has no bias towards alternative medicine and also the only member with expertise in clinical research methods His credentials look impressive, and his publications show how he is the ideal person for this job. I rather liked also his article Stop meddling and let us get on.. He has written about the harm done by postmodernism and relativism, the fellow-travellers of alternative medicine.
Most damning of all, Lewith, Eddlestone and Holgate (along with Cyril Chantler, chair of the King’s Fund, and homeopaths, spiritual healers and Karol Sikora) are Foundation Fellows of the Prince of Wales Foundation for Magic Medicine, an organisation that is at the forefront of spreading medical misinformation.
I shall refer here to ‘alternative medicine’ rather than ‘complementary medicine’ which is used in the report. It is not right to refer to a treatment as ‘complementary’ until such time as it has been shown to work. The term ‘complementary’ is a euphemism that, like ‘integrative’, is standard among alternative medicine advocates whose greatest wish is to gain respectability.
The Report
The recommendations
On page 10 we find a summary of the conclusions.
The report identifies five areas of consensus, which together set a framework for moving forward. These are:
- the primary importance of controlled trials to assess clinical and cost effectiveness.
- the importance of understanding how an intervention works
- the value of placebo or non-specific effects
- the need for investment and collaboration in creating a sound evidence base
- the potential for whole-system evaluation to guide decision-making and subsequent research.
The first recommendation is just great. The rest sound to me like the usual excuses for incorporating ineffective treatments into medical practice. Notice the implicit assumption in the fourth point
that spending money on research will establish “a sound evidence base". There is a precedent, but it is ignored. A huge omission from the report is that it fails to mention anywhere that a lot of research has already been done.
Much research has already been done (and failed)
The report fails to mention at all the single most important fact in this area. The US National Institutes of Health has spent over a billion dollars on research on alternative medicines, over a period
of more than 10 years. It has failed to come up with any effective treatments whatsoever. See, for example Why the National Center for Complementary and Alternative Medicine (NCCAM) Should Be Defunded; Should there be more alternative research?; Integrative baloney @ Yale, and most recently, $2.5B Spent, No Alternative Med Cures found. .
Why did the committee think this irrelevant? I can’t imagine. You guess.
The report says
“This report outlines areas of potential consensus to guide research funders, researchers, commissioners and complementary practitioners in developing and applying a robust evidence base for complementary practice.”
As happens so often, there is implicit in this sentence the assumption that if you spend enough money evidence will emerge. That is precisely contrary to the experence in the USA where spending a billion dollars produced nothing beyond showing that a lot of things we already thought didn’t work were indeed ineffective.
And inevitably, and tragically, NICE’s biggest mistake is invoked.
“It is noteworthy that the evidence is now sufficiently robust for NICE to include acupuncture as a treatment for low back pain.” [p ]
Did the advisory group not read the evidence used (and misinterpeted) by NICE? It seems not. Did the advisory group not read the outcome of NIH-funded studies on acupuncture as summarised by Barker Bausell in his book, Snake Oil Science? Apparently not. It’s hard to know because the report has no references.
George Lewith is quoted [p. 15] as saying “to starve the system of more knowledge means we will continue to make bad decisions”. No doubt he’d like more money for research, but if a billion dollars
in the USA gets no useful result, is Lewith really likely to do better?
The usual weasel words of the alternative medicine industry are there in abundance
“First, complementary practice often encompasses an intervention (physical treatment or manipulation) as well as the context for that intervention. Context in this setting means both the physical setting for the delivery of care and the therapeutic relationship between practitioner and patient.” [p. 12]
Yes, but ALL medicine involves the context of the treatment. This is no different whether the medicine is alternative or real. The context (or placebo) effect comes as an extra bonus with any sort of treatment.
“We need to acknowledge that much of complementary practice seeks to integrate the positive aspects of placebo and that it needs to be viewed as an integral part of the treatment rather than an aspect that should be isolated and discounted.” [p. 13]
This is interesting. It comes very close (here and elsewhere) to admitting that all you get is a placebo effect, and that this doesn’t matter. This contradicts directly the first recommendation of the House of Lords report (2000).. Both the House of Lords report on Complementary and Alternative Medicine, and the Government’s response to it, state clearly
“. . . we recommend that three important questions should be addressed in the following order”. (1) does the treatment offer therapeutic benefits greater than placebo? (2) is the treatment safe? (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?.
The crunch comes when the report gets to what we should pay for.
“Should we be prepared to pay for the so-called placebo effect?
The view of the advisory group is that it is appropriate to pay for true placebo (rather than regression to the mean or temporal effects).” [p 24]
Perhaps so, but there is very little discussion of the emormous ethical questions:that this opinion raises:
- How much is one allowed to lie to patients in order to elicit a placebo effect?
- Is is OK if the practitioner believes it is a placebo but gives it anyway?
- Is it OK if the pratitioner believes that it is not a placebo when actually it is?
- Is it OK for practitioners to go degrees taught by people who believe that it is not a placebo when actually it is?
The report fails to face frankly these dilemmas. The present rather absurd position in which it is considered unethical for a medical practitioner to give a patient a bottle of pink water, but
perfectly acceptable to refer them to a homeopath. There is no sign either of taking into account the cultural poison that is spread by telling people about yin, yang and meridians and such like preposterous made-up mumbo jumbo. That is part of the cost of endorsing placebos. And just when one thought that believing things because you wished they were true was going out of fashion
Once again we hear a lot about the alleged difficulties posed by research on alternative medicine. These alleged difficulties are, in my view, mostly no more than excuses. There isn’t the slightest
difficulty in testing things like herbal medicine or homeopathy, in a way that preserves all the ‘context’ and the ways of working of homeopaths and herbalists. Anyone who reads the Guardian knows
how to do that.
In the case of acupuncture, great ingenuity has gone into divising controls. The sham and the ‘real’ acupuncture always come out the same. In a non-blind comparison between acupuncture and no acupuncture the latter usually does a bit worse, but the effects are small and transient and entirely compatible with the view that it is a theatrical placebo.
Despite these shortcomings, some of the conclusions [p. 22] are reasonable.
“The public needs more robust evidence to make informed decisions about the use of complementary practice.
Commissioners of public health care need more robust evidence on which to base decisions about expenditure of public money on complementary practice.”
What the report fails to do is to follow this with the obvious conclusion that such evidence is largely missing and that until such time as it is forthcoming there should be no question of the NHS paying for alternative treatments.
Neither should there be any question of giving them official government recognition in the form of ‘statutory regulation’. The folly of doing that is illustrated graphically by the case of chiropractic which is now in deep crisis after inspection of its claims in the wake of the Simon Singh defamation case. Osteopathy will, I expect, suffer the same fate soon.
In the summary on p.12 we see a classical case of the tension
Controlled trials of effectiveness and cost-effectiveness are of primary importance
We recognise that it is the assessment of effectiveness that is of primary importance in reaching a judgement of different practices. Producing robust evidence that something works in practice – that it is effective – should not be held up by the inevitably partial findings and challenged interpretations arising from inquiries into how the intervention works.
The headline sounds impeccable, but directly below it we see a clear statement that we should use treatments before we know whether they work. “Effectiveness”, in the jargon of the alternative medicine business, simply means that uncontrolled trials are good enough. The bit about “how it works” is another very common red herring raised by alternative medicine people. Anyone who knows anything about pharmacology that knowledge about how any drug works is incomplete and often turns out to be wrong. That doesn’t matter a damn if it performs well in good double-blind randomised controlled trials.
One gets the impression that the whole thing would have been a lot worse without the dose of reality injected by Richard Lilford. He is quoted as a saying
“All the problems that you find in complementary medicine you will encounter in some other kind of treatment … when we stop and think about it… how different is it to any branch of health care – the answer to emerge from our debates is that it may only be a matter of degree.” [p. 17]
I take that to mean that alternative medicine poses problems that are no different from other sorts of treatment. They should be subjected to exactly the same criteria. If they fail (as is usually the case) they should be rejected. That is exactly right. The report was intended to produce consensus, but throughout the report, there is a scarcely hidden tension between believers on one side, and Richard Lilford’s impeccable logic on the other.
Who are the King’s Fund?
The King’s Fund is an organisation that states its aims thus.
“The King’s Fund creates and develops ideas that help shape policy, transform services and bring about behaviour change which improve health care.”
It bills this report on its home page as “New research methods needed to build evidence for the effectiveness of popular complementary therapies”. But in fact the report doesn’t really recommend ‘new research methods’ at all, just that the treatments pass the same tests as any other treatment. And note the term ‘build evidence’. It carries the suggestion that the evidence will be positive. Experience in the USA (and to a smaller extent in the UK) suggests that every time some good research is done, the effect is not to ‘build evidence’ but for the evidence to crumble further
If the advice is followed, and the results are largely negative, as has already happened in the USA, the Department of Health would look pretty silly if it had insisted on degrees and on statutory regulation.
The King’s Fund chairman is Sir Cyril Chantler and its Chief Executive is Niall Dickson. It produces reports, some of which are better than this one. I know it’s hard to take seriously an organisation that wants to “share its vision” withyou, but they are trying.
“The King’s Fund was formed in 1897 as an initiative of the then Prince of Wales to allow for the collection and distribution of funds in support of the hospitals of London. Its initial purpose was to raise money for London’s voluntary hospitals,”
It seems to me that the King’s Fund is far too much too influenced by the present Prince of Wales. He is, no doubt, well-meaning but he has become a major source of medical misinformation and his influence in the Department of Health is deeply unconstitutional. I was really surprised to see thet Cyril Chantler spoke at the 2009 conference of the Prince of Wales Foundation for Integrated Health, despite having a preview of the sort of make-believe being propagated by other speakers. His talk there struck me as evading all the essential points. Warm, woolly but in the end, a danger to patients. Not only did he uncritically fall for the spin on the word “integrated”, but he also fell for the idea that “statutory regulation” will safeguard patients.
Revelation of what is actually taught on degrees in these subjects shows very clearly that they endanger the public.
But the official mind doesn’t seem ever to look that far. It is happy ticking boxes and writing vacuous managerialese. It lacks curiosity.
Follow-up
The British Medical Journal published today an editorial which also recommends rebranding of ‘pragmatic’ trials. No surprise there, because the editorial is written by Hugh MacPherson, senior research fellow, David Peters, professor of integrated healthcare and Catherine Zollman, general practitioner. I find it a liitle odd that the BMJ says “Competing Interests: none. David Peters interest is obvious from his job description. It is less obvious that Hugh MacPherson is an acupuncture enthusiast who publishes mostly in alternative medicine journals. He has written a book with the extraordinary title “Acupuncture Research, Strategies for Establishing an Evidence Base”. The title seems to assume that the evidence base will materialise eventually despite a great deal of work that suggests it won’t. Catherine Zollman is a GP who is into homeopathy as well as acupuncture. All three authors were speakers at the Prince of Wales conference, described at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’.
The comments that follow the editorial start with an excellent contribution from James Matthew May. His distinction between ‘caring’ and ‘curing’ clarifies beautifully the muddled thinking of the editorial.
Then a comment from DC, If your treatments can’t pass the test, the test must be wrong. It concludes
“At some point a stop has to be put to this continual special pleading. The financial crisis (caused by a quite different group of people who were equally prone to wishful thinking) seems quite a good time to start.”

Conservatives in the USA have been lying about the NHS on a massive scale. As Simon Hoggart comments today “There are few tribes more loathsome than the American right”.
In the forefront has been a far-right lobby group, Conservatives for Patients’ Rights (CPR). Even I was surprised to read in the Washington Post
“The campaign is being coordinated by CRC Public Relations, the group that masterminded the “Swift boat” attacks against 2004 Democratic presidential candidate, John F. Kerry”
CRC Public Relations is a conservative PR firm previously known as Creative Response Concepts. ‘Creative’ appears to mean ‘lying’, but I guess that is what PR is all about.
The founder of CPR, Rick Scott, has an interesting background. According to Stephen Barrett
“In 1987, he founded and became chief operating officer of a hospital chain that grew into the 23 billion-dollars-a-year Columbia/HCA. In 1997, a few weeks after the FBI raided HCA hospitals in five states, Scott was ousted as CEO and three executives were indicted on charges of Medicare fraud. The FBI’s investigation found that the hospital chain had been overbilling Medicare and giving kickbacks to doctors who steered patients to its hospitals. The overbilling included upcoding lesser procedures to get higher reimbursements and billing for lab tests that were not medically necessary and were not ordered by physicians. The situation was settled with a set of guilty pleas and criminal and civil fines totalling $1.7 billion. The U.S. Department of Justice referred to the matter as the “largest health care fraud case in U.S. history.”
Disgracefully, Karol Sikora, a former oncologist at the Hammersmith Hospital, supported CPR on US television. See Karol Sikora makes a fool of himself at NHSblogdoctor. I quote
“Karol Sikora had been duped by a slick American businessman into providing a “rent-a-quote” service for a notorious right-wing American organisation”
This post was reproduced on the US site, Trusted.MD
Sikora now works for the UK’s only private university and a private cancer treatment company. He is also famous for claiming,
falsely, to be a professor at Imperial College (he has an honorary contract with the Imperial College Hospital Trust but nothing with the University). And for promoting a load of nonsense about
alternative medicine (a lot more on that coming up shortly).
This is why love the NHS
Europe as a whole gets better health care for less money than in the USA. The fact that every US doctor has a financial interest in ordering expensive treatments whether they are needed or not,
is an obscenity. The fact that over 40 million Americans have no insurance is an obscenity (see The brutal truth about America’s healthcare).
Just look at the numbers (Source: WHO/OECD Health Data 2009)
Health spending as a share of GDP.
US 16% UK 8.4%
Public spending on healthcare (% of total spending on healthcare)
US 45% UK 82%
Health spending per head
US $7,290 UK $2,992
Practising physicians (per 1,000 people)
US 2.4 UK 2.5
Nurses (per 1,000 people)
US 10.6 UK 10.0
Acute care hospital beds (per 1,000 people)
US 2.7 UK 2.6
Life expectancy:
US 78 UK 80
Infant mortality (per 1,000 live births)
US 6.7 UK 4.8
My experience
Yes I know this is anecdote, but it matters a lot to me. I already posted a version of this story, but this seems like the time to repeat it.
On December 13th 1984, my wife had a subarachnoid haemorrhage when she was seven months pregnant. After an initial misdiagnosis by an obstetrician at St Peter’s Hospital, Chertsey, she was moved to UCH and diagnosed very quickly. The next morning I was called to see the neurourgeon, the great Alan Crockard. He was sitting surrounded by medical students some of whom I’d taught the previous year. He told me my wife had had a subarachnoid haemorrhage (at 33!) and they would operate straight away. And “I have to ask you, if we can save only the mother or the baby, which shall it be”. It’s as well to write that down because even 24 years later I can’t say it without a lump rising in my throat.
That same day she had neurosurgery to pin an aneurysm at the Maida Vale Neurosurgical Hospital, part of the UCLH group (it no longer exists). The surgeon, Alan Crockard, came out of theatre after five hours, looking rather tired and said “it was adhered to the optic chiasma on one side and about a millimetre from the pituitary on the other. It was a bit tricky but I think we got it”. Obstetricians were in theatre too because all this was done with the baby still in situ
| After a week in intensive care, under heavy sedation, Margaret’s blood pressure was not low enough and they decided to deliver the baby. At about 4 pm on a snowy Christmas Eve, a team of neurosurgeons and a team of obstetricians gathered and soon after, Andrew Stuart Colquhoun emerged in a small incubator to be whisked off in an ambulance to the Special Care Baby Unit at UCH (run, at that time, by Osmund Reynolds). Christmas day was spent in the hospital, with Margaret’s mother. Andrew weighed 1.4 kg at birth, but by Christmas day he had pulled out his ventilator himself, and was doing fine. He was so tiny that it was a couple of days before I dared to hold him. The Unit had racks of doll-sized clothes, knitted by volunteers. The care was superb. | 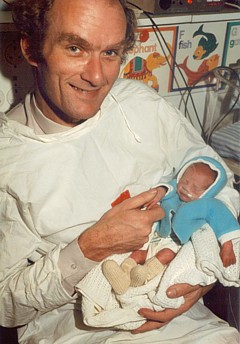
Andrew (at 9 days) and Dad. Jan 2, 1985. Click for album. |
Once Margaret was well enough, she was given a side room in a neurosurgical ward with a cot for Andrew by her bed, an arrangement that gave the neurosurgical nurses some fun. They were in UCLH continuously until 27th April before Margaret had recovered enough to go home, [Full photo album here]
Now they are both fine.and Andrew is 6′ 7″ (200.5 cm)..
It is episodes like this that make one very proud of the NHS. She and Andrew were in hospital continuously for more than four months. Not a penny changed hands. Heaven knows what it would have cost in the USA, or even of insurance would have covered such a gargantuan bill.
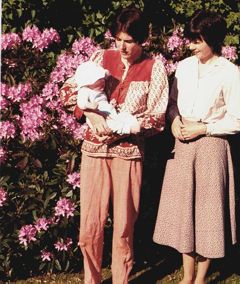
Margaret & Andrew, with carer, Anna, June 2, 1985 |
Andrew (left) playing cricket in Bangladesh, Feb 2005. |
My own experience is trivial compared with that of Margaret and Andrew, but it has been as near perfect as anyone could wish. I had a lumbar spinal fusion (L3 – L4) in 1995, after several attempts at less drastic solutions. I’ve had two artificial hips. They allowed me to walk across the Alps for my 65th birthday. Then a few trivial things like bilateral hernia and DVT (I had been scanned and was on anticoagulant therapy within 4 hours of walking into UCLH’s Accident and Emergency). And now it looks as though I’ll be getting a partial or total nephrectomy too.
And not a penny has changed hands.
The NHS is a beautiful thing. OK it has has the usual excessive number of managers and HR-bollocks, like most big companies. It isn’t perfect but it is a great deal closer to perfection
than the US system.
 Approaching Seescharte (2600 m) at 08.20, 21 August 2001. Memminger Hütte visible below. With fused vertebrae and right prosthetic hip, thanks to the NHS. (Click for bigger picture.) |
Bush may have gone, but a large fraction of Americans seem to be unrepentant Bush-ites. Almost all of my many friends in the USA think more or less like I do. Even Obama is to the right of most European conservatives, The other 48% are to the right of Attila the Hun. The extent of the polarisation that still exists is nothing short of terrifying.
|
Thanks to the great Aneurin Bevan who established the NHS in 1948 for ordinary people like me, in the face of fierce opposition from the medical establishment.
|
 Statue of Bevan in Cardiff |
Ah well, The Daily Mash. is always there when you need a (wry) laugh
Follow-up
Paul Krugman in the New York Times is magnificent as always. In The Swiss Menace he points out that Obama’s scheme is nothing like the NHS anyway, but more like that in Switzerland.
“The plans on the table would, roughly speaking, turn America into Switzerland — which may be occupied by lederhosen-wearing holey-cheese eaters, but wasn’t a socialist hellhole the last time I looked.”
“In Britain, the government itself runs the hospitals and employs the doctors. We’ve all heard scare stories about how that works in practice; these stories are false.”
“So we can do this. At this point, all that stands in the way of universal health care in America are the greed of the medical-industrial complex, the lies of the right-wing propaganda machine, and the gullibility of voters who believe those lies.”
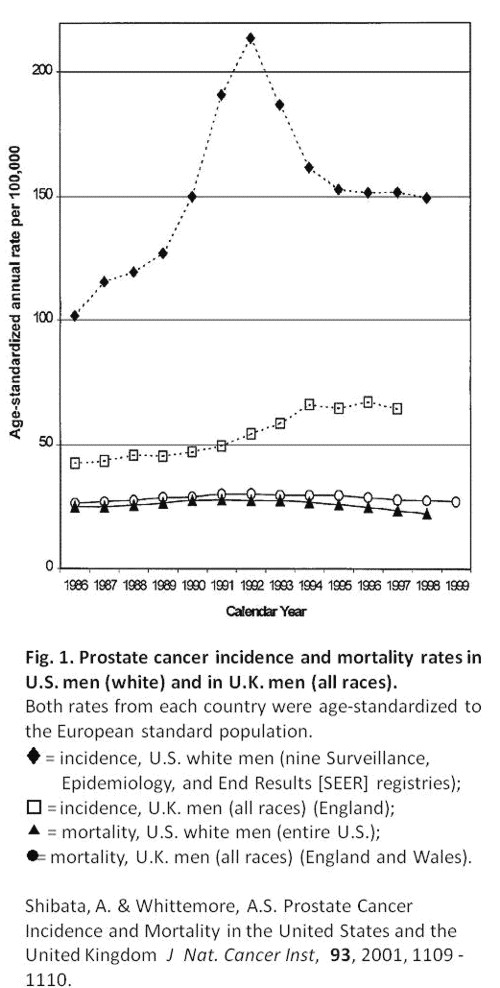
Comparing US and UK cancer statistics . As Ben Goldacre says, “I think you’ll find it’s a bit more complicated than that”. There’s an interesting analysis at Cancer Research UK
The US uses the PSA blood test far more widely than we do in the UK – despite questions over how effective it is at spotting cancers that would actually kill, as opposed to those that cause no symptoms. As a result, the USA has one of the highest recorded rates of prostate cancer in the world.
So although it’s undoubtedly ‘better’ at spotting prostate cancers, it’s also fair to say that some of these Americans will never die from their disease. This ‘overdiagnosis‘ inflates the survival statistics, at the expense of ‘overtreating‘ men – which is expensive and can cause long-term side effects (which can need further treatment).
In fact the age-standardised death rates per 100,000 people are almost the same in the UK (all races) when compared with the USA (whites only). What is different is that far more cases of prostate cancer are diagnosed in the USA. If the rate of ‘real’ (potentially fatal) prostate cancer were similar in both countries then both countries have much the same success in treating it, If, on the other hand, US men had a genuinely higher incidence of real prostate cancer, the US would be doing better, There is no way to distinguish between these two interpretations,
This post has been translated into Belorussian..
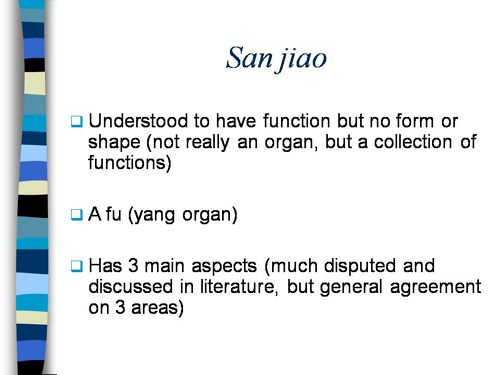
Chinese medicine and herbal medicine are in the news at the moment. There is a real risk that the government could endorse them by accepting the Pittilo report.
In my view traditional Chinese medicine endangers people. The proposed ‘regulation’ would do nothing to protect the public. Quite on the contrary, it would add to the dangers, by giving an official stamp of approval while doing nothing for safety.
The government’s idea of improving safety is to make sure that practitioners are ‘properly trained’. But it is the qualifications that cause the danger in the first place. The courses teach ideas that are plain wrong and often really dangerous.
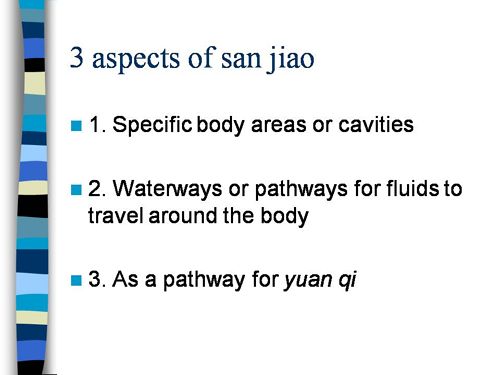
Why have government (and some universities) not noticed this? That’s easy to see. Governments, quangos and university validation committees simply don’t look. They tick boxes but never ask what actually goes on. Here’s some examples of what goes on for them to think about. They show clearly the sort of dangerous rubbish that is taught on some of these ‘degrees’.
These particular slides are from the University of Westminster, but similar courses exist in only too many other places. Watch this space for more details on courses at Edinburgh Napier University, Middlesex University and the University of East London
Just a lot of old myths. Sheer gobbledygook,
SO much for a couple of centuries of physiology,
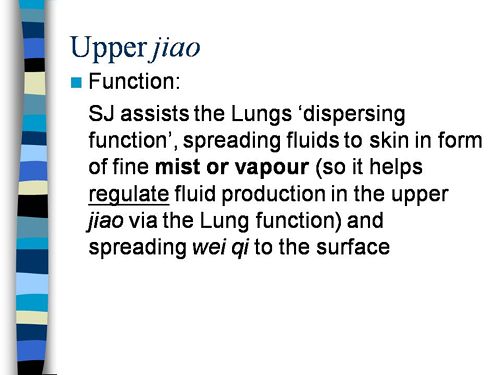
It gets worse.
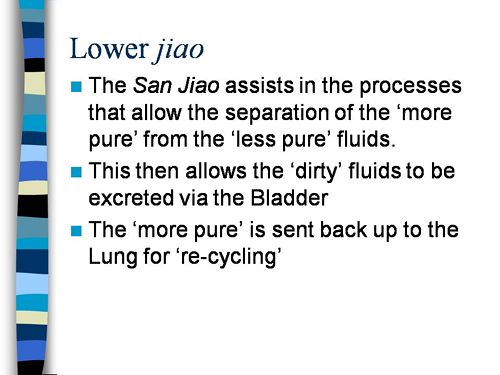
Plain wrong.
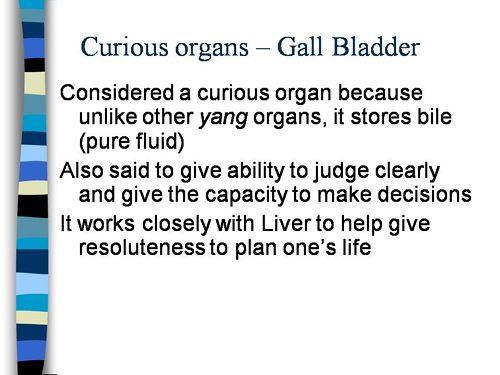
Curious indeed. The fantasy gobbledygook gets worse.
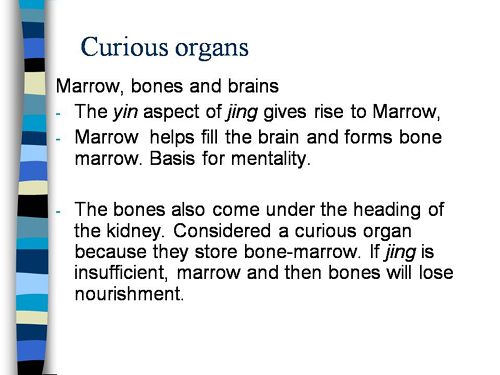
Now it is getting utterly silly. Teaching students that the brain is made of marrow is not just absurd, but desperately dangerous for anyone unlucky (or stupid) enough to go to such a person when they are ill.
Here’s another herbal lecture., and this time the topic is serious. Cancer.
Herbal approaches for patients with cancer.
I’ve removed the name of the teacher to spare her the acute embarrassment of having these dangerous fantasies revealed. The fact that she probably believes them is not a sufficient excuse for endangering the public. There is certainly no excuse for the university allowing this stuff to be taught as part of a BSc (Hons).
First get them scared with some bad statistics.
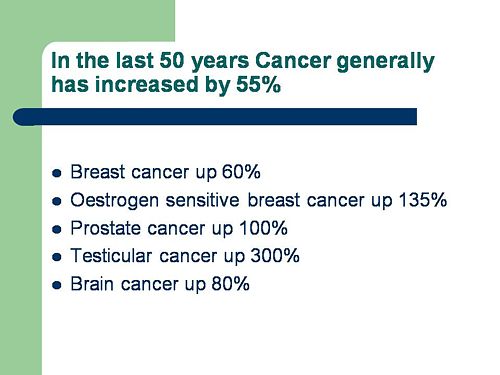
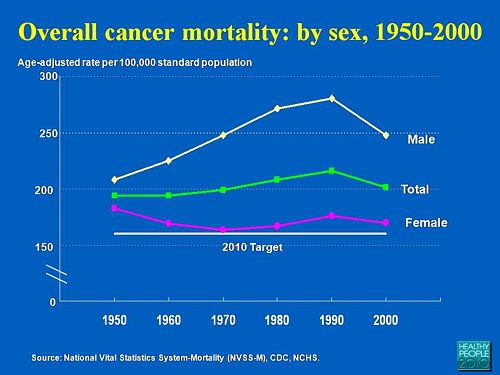
No fuss there about distinguishing incidence, age-standardisation and death rates. And no reference. Perhaps a reference to the simple explanation of statistics at Cancer Research UK might help? Perhaps this slide would have been better (from CDC). Seems there is some mistake in slide 2.
Straight on to a truly disgraceful statement in slide 3
The is outrageous and very possibly illegal under the Cancer Act (1939). It certainly poses a huge danger to patients. It is a direct incentive to make illegal, and untrue claims by using weasel words in an attempt to stay just on the right side of the law. But that, of course, is standard practice in alternative medicine,
Slide 11 is mostly meaningless. “Strengthen vitality” sounds good but means nothing. And “enhancing the immune system” is what alternative medicine folks always say when they can think of nothing else. Its meaning is ill-defined and there is no reason to think that any herbs do it.
The idea of a ‘tonic’ was actually quite common in real medicine in the 1950s. The term slowly vanished as it was realised that it was a figment of the imagination. In the fantasy world of alternative medicine, it lives on.
Detoxification, a marketing term not a medical one, has been extensively debunked quite recently. The use of the word by The Prince of Wales’ company, Duchy Originals recently fell foul of the Advertising Standards Authority, and his herbal ‘remedies’ were zapped by the MHRA (Medicines and Health Regulatory Authority).
And of course the antioxidant myth is a long-disproved hypothesis that has become a mere marketing term.
“Inhibits the recurrence of cancer”! That sounds terrific. But if it is so good why is it not even mentioned in the two main resources for information about herbs?
In the UK we have the National Library for Health Complementary and Alternative Medicine Specialist Library (NeLCAM), now a part of NHS Evidence. It was launched in 2006. The clinical lead was none other than Peter Fisher, clinical director of the Royal London Homeopathic Hospital, and the Queen’s homeopathic physician. The library was developed with the School of Integrated Health at the University of Westminster (where this particular slide was shown to undergraduates). Nobody could accuse these people of being hostile to magic medicine,
It seems odd, then, that NeLCAM does not seem to thnk to think that Centella asiatica, is even worth mentioning.
In the USA we have the National Center for Alternative and Complementary Medicine (NCCAM), an organisation that is so friendly to alternative medicine that it has spent a billion dollars on research in the area, though it has produced not a single good treatment for that vast expenditure. But NCCAM too does not even mention Centella asiatica in its herb list. It does get a mention in Cochrane reviews but only as a cosmetic cream and as an unproven treatment for poor venous circulation in the legs.
What on earth is a “lymph remedy”. Just another marketing term?
“especially valuable in the treatment of breast, throat and uterus cancer.“
That is a very dramatic claim. It as as though the hapless students were being tutored in doublespeak. What is meant by “especially valuable in the treatment of”? Clearly a desperate patient would interpret those words as meaning that there was at least a chance of a cure. That would be a wicked deception because there isn’t the slightest reason to think it works. Once again there this wondrous cure is not even mentioned in either NELCAM or NCCAM. Phytolacca is mentioned, as Pokeweed, in Wikipedia but no claims are mentioned even there. And it isn’t mentioned in Cochrane reviews either. The dramatic claims are utterly unfounded.
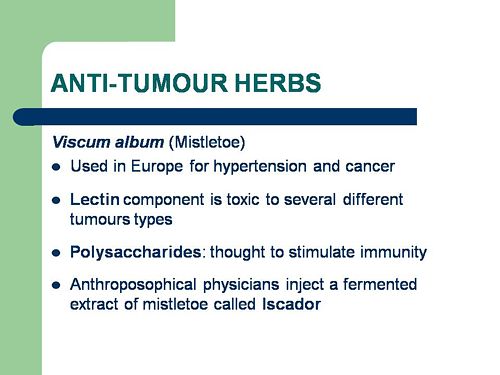
Ah the mistletoe story, again.
NHS Evidence (NeLCAM) lists three completed assessments. One concludes that more research is needed. Another concludes that “Rigorous trials of mistletoe extracts fail to demonstrate efficacy of this therapy”, and the third says “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
NCCAM says of mistletoe
- More than 30 human studies using mistletoe to treat cancer have been done since the early 1960s, but major weaknesses in many of these have raised doubts about their findings (see Question 6).
- Very few bad side effects have been reported from the use of mistletoe extract, though mistletoe plants and berries are poisonous to humans (see Question 7).
- The U.S. Food and Drug Administration (FDA) has not approved mistletoe as a treatment for cancer or any other medical condition (see Question 8).
- The FDA does not allow injectable mistletoe to be imported, sold, or used except for clinical research (see Question 8).
Cochrane reviews lists several reviews of mistletoe with similar conclusions. For example “The evidence from RCTs to support the view that the application of mistletoe extracts has impact on survival or leads to an improved ability to fight cancer or to withstand anticancer treatments is weak”.
Anthroposophy is one of the highest grades of fantasy you can find. A post on that topic is in the works.
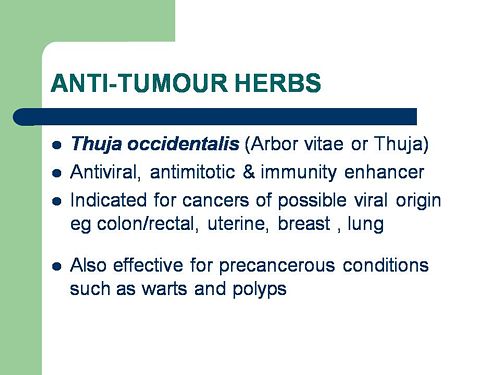
“Indicated for cancers . . . colon/rectal, uterine, breast, lung“. A cure for lung cancer? That, of course, depends on how you interpret the weasel words “indicated for”. Even Wikipedia makes no mention of any claims that Thuja benefits cancer. NHS Evidence (NeLCAM) doesn’t mention Thuja for any indication. Neither does NCCAM. Nor Cochrane reviews. That is not the impression the hapless students of this BSc lecture were given. In my view suggestions that you can cure lung cancer with this tree are just plain wicked.
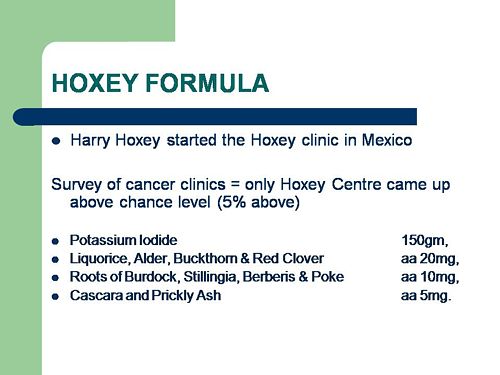
Pure snake oil, and not even spelled correctly, Harry Hoxsey’s treatment centres in the USA were closed by court order in the 1950s.
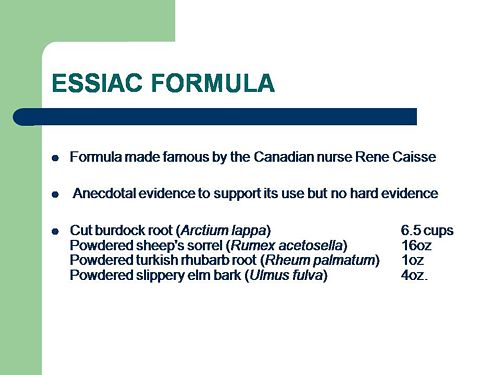
At least this time it is stated that there is no hard evidence to support this brand of snake oil.
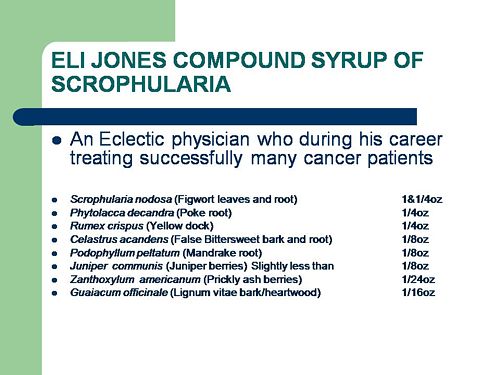
More unfounded claims when it says “treated successfully many cancer patients”. No references and no data to support the claim. It is utterly unfounded and claims to the contrary endanger the public.
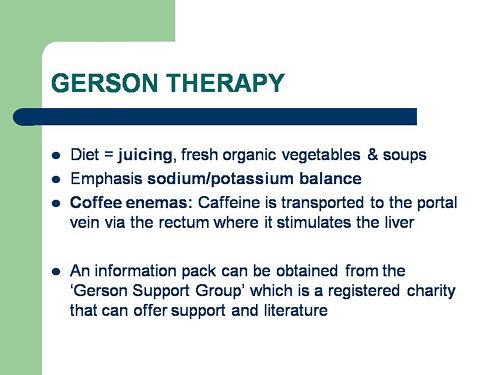
Gerson therapy is one of the most notorious and unpleasant of the quack cancer treatments. The Gerson Institute is on San Diego, but their clinics are in Mexico and Hungary. It is illegal in the USA. According to the American Cancer Society you get “a strict low-salt, low-fat, vegetarian diet and drinking juice from about twenty pounds of fresh fruits and vegetables each day. One glass of juice is consumed each hour, thirteen times a day. In addition, patients are given several coffee enemas each day. Various supplements, such as potassium, vitamin B12, pancreatic enzymes, thyroid hormone, and liver extracts, are used to stimulate organ function, particularly of the liver and thyroid.”. At one time you also got several glasses of raw calf liver every day but after infections killed several people] carrot juice was given instead.
Cancer Research UK says “there is no evidence to show that Gerson therapy works as a cure for cancer”, and “The Gerson diet can cause some very serious side effects.” Nobody (except perhaps the Price of Wales) has any belief in this unpleasant, toxic and expensive folk-lore.
Again patients are endangered by teaching this sort of stuff.
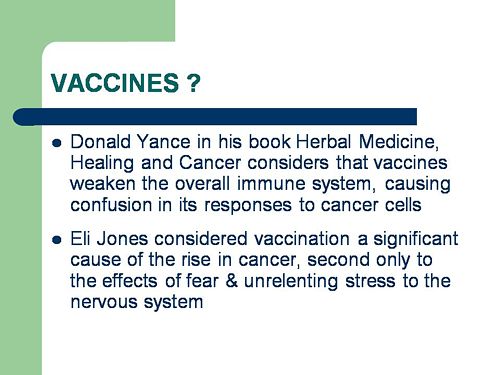
And finally, the usual swipe at vaccines. It’s nothing to do with herbalism. but just about every alternative medicine advocate seems to subscribe to the anti-vaccination lobby.. It is almost as though they have an active preference for things that are known to be wrong. They seem to believe that medicine and science are part of an enormous conspiracy to kill everyone.
Perhaps this dangerous propaganda might have been ameliorated if the students had been shown this slide (from a talk by Melinda Wharton).
Left to people like this, we would still have smallpox, diphtheria. tetanus and rabies, Take a look at Vaccine-preventable diseases.
This is the sort of ‘education’ which the Pittilo report wants to make compulsory.
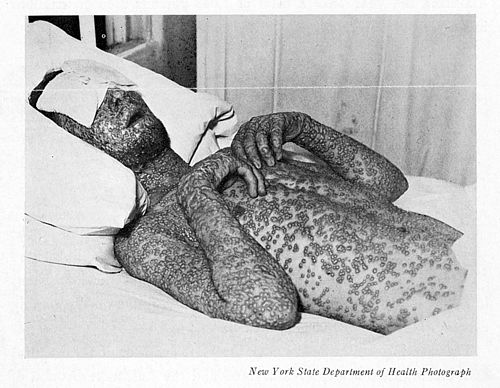
Smallpox in Baltimore, USA, 1939. This man was not vaccinated.
Conclusion
This selection of slides shows that much of the stuff taught in degrees in herbal medicine poses a real danger to public safety and to public health.
Pittilo’s idea that imposing this sort of miseducation will help safety is obviously and dangerously wrong. The Department of Health must reject the Pittilo recommendations on those grounds.
Follow-up
The much-delayed public consultation on the Pittilo report has just opened.
It is very important that as many people as possible respond to it. It’s easy to say that the consultation is sham. It will be if it is left only to acupuncturists and Chinese medicine people to respond to it. Please write to them before the closing date, November 2nd 2009. The way to send your evidence is here.
There is a questionnaire that you can complete, with the usual leading questions. Best do it anyway, but I’d suggest also sending written evidence as attachment too. I just got from DoH the email address where you can send it. They said
| if you have material you wish to send which you can’t easily “shoehorn” into the questionnaire, please send it to the following mailbox:
HRDListening@dh.gsi.gov.uk |
Here are three documents that I propose to submit in response to the consultation.I ‘d welcome criticisms that might make it more convincing. Use any parts of them you want in your own response.
- Submission to the Department of Health, for the consultation on the Pittilo report [download pdf].
- What is taught in degrees in herbal and traditional Chinese medicine? [download pdf]
- $2.5B Spent, No Alternative Med Cures [download pdf]
|
I’ve written quite a lot about the Pittilo report already, in particular A very bad report: gamma minus for the vice-chancellor, and in The Times (see also the blog version).
Intriguingly, these posts are at number 2 in a Google search for “Michael Pittilo”. |
 |
Briefly, the back story is this.
It is now over a year since the Report to Ministers from “The Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK” [download the report].
The chair of the steering group was Professor R. Michael Pittilo, Principal and Vice-Chancellor of The Robert Gordon University, Aberdeen. The reason thet the report is so disastrously bad in its assessment of evidence is that it was written entirely by people with vested interests.
The committee consisted of five acupuncturists, five herbalists and five representatives of traditional Chinese medicine (plus eleven observers). There was not a single scientist or statistician to help in the assessment of evidence. And it shows: The assessment of the evidence in the report was execrable. Every one of the committee members would have found themselves out of work if they had come to any conclusion other than that their treatment works, Disgracefully, these interests were not declared in the report, though they are not hard to find. The university of which the chair is vice-chancellor runs a course in homeopathy, the most discredited of the popular forms of alternative medicine. That tells you all you need to know about the critical faculties of Michael Pittilo.
The two main recommendations of this Pittilo report are that
- Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine should be subject to statutory regulation by the Health Professions Council
- Entry to the register normally be through a Bachelor degree with Honours
Let’s consider the virtue of these two recommendations.
Regulation by the Health Professions Council (HPC) breaks their own rules
For a start, this should be ruled out by the HPC’s own rules, which require “Practise based on evidence of efficacy” as a condition for registration. Since there is practically no “evidence of efficacy”, it follows that the HPC can’t regulate acupuncture, herbal and Chinese medicine as Pittilo recommends. Or so you’d think. But the official mind seems to have an infinite capacity for doublespeak. The HPC published a report on 11 September 2008, Regulation of Medical Herbalists, Acupuncturists and Traditional Chinese Medicine Practitioners.
The report says
1. Medical herbalists, acupuncturists and traditional Chinese medicine practitioners should be statutorily regulated in the public interest and for public safety reasons.
2. The Health Professions Council is appropriate as the regulator for these professions.
3. The accepted evidence of efficacy overall for these professions is limited, but regulation should proceed because it is in the public interest.
In other words, the HPC simply decided to ignore its own rules, Its excuse for doing so is that regulation would protect “public safety” . But it simply would not do that. It is ell known that some Chinese herbs are adulterated with dangerous substances, but laws against that already exist. Trading Standards are much more likely to take appropriate action than the HPC. The Medicines and Health Regulatory Authority (MHRA) already deals with the licensing of herbal medicines. and, despite the fact that it recently betrayed its trust by allowing them to be labelled in a misleading way, they are the people to do it, not the HPC.
The Pittilo report (page 11) says
In future, it is hoped that more Government funding can be allocated to research into traditional/herbal medicines and acupuncture and that grants will become available to encourage practitioners to undertake postgraduate research work.
So they are asking for more government money.
In March 2007, the Chinese Government pledged to spend over $130 million over the next five years on research into the effectiveness of traditional Chinese medicine. It is to be hoped that this money will be targeted effectively to evaluate TCM.
It seems to have escaped the notice of Pittilo that roughly 100 percent of trials of Chinese medicine done in China come out positive. Elsewhere, very few come out positive,(see Vickers et al., 1998, Controlled Clinical Trials, 19, 159-166: download reprint) The Department of Health would be unwise to rely on Chinese research. Remember that modern acupuncture was not so much a product of ancient wisdom, but rather it stems from nationalist propaganda by Mao Tse-Tung, who needed a cheap way to keep the peasants quiet, though he was too sensible to use it himself.
The HPC report (page 5) cites these with the words
” . . . a lack of evidence of efficacy should not prevent regulation but that the professions should be encouraged and funded to strengthen the evidence base.”
This sentence seems to assume that the outcomes of research will be to strengthen the evidence base. Thus far, precisely the opposite has been the case. The Pittilo group has apparently not noticed that the US National Institutes of Health has already spent a billion dollars on research in alternative medicine and failed to come up with a single effective treatment. There are better ways to spend money on health. See, for example $2.5B Spent, No Alternative Med Cures found. .An enornous amount of research has already been done and the outcomes have produced no good treatments,
The proposed regulation would endanger the public, not protect it.
The excuse given by the HPC for breaking its own rules is that it should do so to protect the public.
Likewise Ann Keen, Health Minister, said:
“Patient safety is paramount, whether people are accessing orthodox health service treatments or using alternative treatments”
So first we need to identify what dangers are posed by acupuncture, herbal medicine and traditional Chinese medicine.
- Acupuncture is fairly safe. Its biggest danger lies in the unjustified claims that are routinely made for what can be achieved by being impaled by needles. This poses a danger that people may use acupuncture in place of treatments that work
- Herbal medicines are unstandardised, so even the very few that may work are dangerous to patients because the dose of active principle is unknown and varies from one batch to another. Taking a herbal medicine is a bit like swallowing a random number of tablets, False health claims pose a danger to patients too, when they cause patients to avoid treatments that work.
- Traditional Chinese Medicine is probably the most dangerous. Like the other two, the medicines are unstandardised so the dose is never known. False health claims abound. And in addition to these dangers, many cases have been found of Chinese medicines being adulterated with poisonous substances or with conventional drugs.
The form of regulation proposed by Pittilo would do little or nothing to protect the public from any of these dangers.
The proposals accept the herbal and Chinese medicine as traditionally practised. Nothing would be done about one of the major dangers, the lack of standardisation. That is a problem that was solved by pharmacologists in the 1930s, when international standards were set for the biological activity of things like tincture of digitalis, and assays were devised so that different batches could be adjusted to the same potency. Now, 80 years later, it is being proposed by Pittilo that we should return to the standards of safety that existed at the beginning of the last century. That is a threat to public safety., but the proposed regulation would do nothing whatsoever to protect the public from this dangerous practice. On the contrary, it would give official government sanction to it.
The other major danger is that patients are deceived by false health claims. This is dangerous (as well as dishonest) because it can cause patients to avoid treatments that work better, The internet abounds with claims that herbs can cure anything from diabetes to cancer. Many are doubtless illegal, but regulators like the HPC have traditionally ignored such claims: they are left to Trading Standards, Advertising Standards and the Medicines and Health Regulatory Authority (MHRA) to deal with. The MHRA already also has responsibility for monitoring side effects. The HPC would not do this.
The analogy with chiropractic and the GCC
The foolishness of allowing statutory regulation for unproven treatments has recently been illustrated quite dramatically by the case of chiropractic. Chiropractors have had statutory regulation by the General Chiropractic Council, which was established by the Chiropractors Act of 1994. The British Chiropractic Association (BCA) recently decided to sue the science writer, Simon Singh, for defamation when he cast doubt on some of the claims made by chiropractors, in particular their claims to be able to cure colic and asthma in children. That led to close examination of the claims. In fact there is no reason to think that spinal manipulation works for asthma, or that it works for colic. In fact there is quite good evidence that the claims are false. The result was that about 600 well-justified complaints have been lodged with the GCC (enough to bankrupt the GCC if the complaints are dealt with properly).
The point of this story is that the statutory regulator had nothing whatsoever to prevent these false health claims being made. Two of the complaints concern practices run by the chair of the GCC. Worse, the GCC actually endorsed such claims. The statutory regulator saw its duty to defend chiropractic (apart from a handful of cases of sexual misdemeanours), not to protect the patient from false health claims. The respectability conferred by statutory regulation made false health claims easier and endangered the public. It would be a disaster if the same mistake were made again.
On 11th December 2008 I got a letter form the HPC which said
in our opinion a lack of evidence of efficacy would not impede our ability to set standards or deal with complaints we receive. The vast majority of cases we consider are related to conduct.
But perhaps that is because they haven’t tried “regulating” quacks before. Now that the public is far more conscious about health fraud than it used to be, one can predict confidently that the HPC would be similarly overwhelmed by a deluge of complaints about the unjustified health claims made by acupuncturists, herbal medicine and traditional Chinese medicine practitioners. There is no shortage of them to complain about.
The education problem
The Pittilo report recommends that the entry level for registration should be a bachelors degree with honours. At first sight it seems reasonable to ask that practitioners should be ‘properly qualified’, but when one looks at what is actually taught on these degrees it becomes clear that they endanger, rather than protect, the public,
There are two very big problems with this recommendation.
Firstly, you can’t have a bachelors degree with honours until after you have decided whether or not there is anything useful to teach. If and when any of the subjects under consideration and shown to work to a useful extent, then it would be quite reasonable to establish degrees in them. Even the report does not pretend seriously that that stage has been reached. The proposal to set up degrees in subjects, at least some of which are quite likely to have no more than placebo value, is self-evidently nonsense,
The time for degrees, and the time for government endorsement by statutory regulation, is after the therapies have been shown to work, not before.
The absurdity of thinking that the public will be protected because a practitioner has a degree in, say, acupuncture, is shown with startling clarity by a recently revealed examination paper in acupuncture’
You can download the entire exam paper. Here are a few highlights from it.
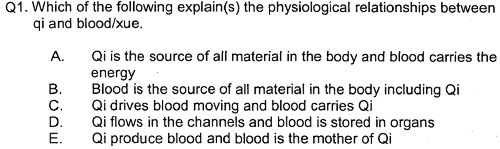
So students, in 2009, are being taught the crudest form of vitalism.
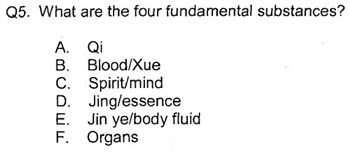
Teaching of traditional Chinese medicine is just as bad. Here are two slides from a course run by the University of Westminster.
The first ‘explains’ the mysterious and entirly mythical “Qi”.
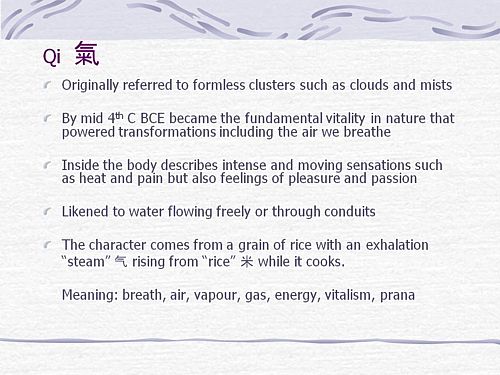
So “Qi” means breath, air, vapour, gas, energy, vitalism. This is meaningless nonsense.
The second slide shows the real dangers posed by the way Chinese medicine is taught, The symptoms listed at the top could easily be a clue to serious illness, yat students are taught to treat them with ginger. Degrees like this endanger the public.
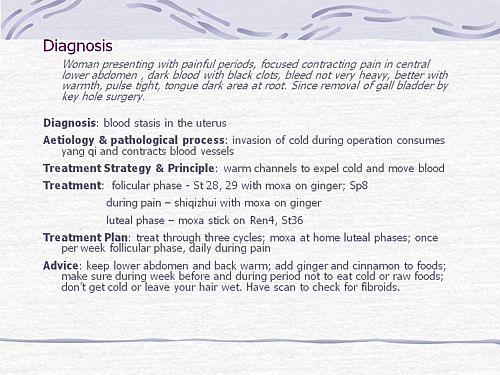
There are more mind-boggling slides from lectures on Chinese medicine and cancer: they show that what students are being taught is terrifyingly dangerous to patients.
It is entirely unacceptable that students are being taught these ancient myths as though they were true, and being encouraged to treat sick people on their basis. The effect of the Pittilo recommendations would be to force new generations of students to have this sort of thing forced on them. In fact the course for which this exam was set has already closed its doors. That is the right thing to do.
Here’s another example. The course leader for “BSc (Hons) Herbal Medicine” at the Univsrsity of Central Lancashire is Graeme Tobyn BA. But Tobyn is not only a herbalist but also an astrologer. In an interview he said
“At the end I asked her if I could cast her horoscope. She threw up her hands and said, ‘I knew this would happen if I came to an alternative practitioner.”
“I think the ruler of the ascendant was applying to Uranus in the ninth house, which was very pertinent.”
This would be preposterous even in the life style section of a downmarket women’s magazine, The Pittilo report wants to make degrees run my people like this compulsory. Luckily the Univerity of Central Lancashire is much more sensible and the course is being closed.
The matter is, in any case, being taken out of the hands of the government by the fact that universities are closing degrees in complementary medicine, including courses in some of those under discussion here, The University of Salford and the University of Central Lancashire have recently announced the closure of all the degree programmes in complementary and alternative medicine. The largest provider of such degrees, the University of Westminster has already shut down two of them, and the rest are being assessed at the moment. It is likely that the rest will be closed in the future.
The revelation that Westminster had been teaching its first year students that “amethysts emit high yin energy” and that students had been taught to diagnose disease and choose treatments by means of a dowsing pendulum, showed very clearly the sort of utter nonsense that undergraduates were being forced to learn to get a ‘bachelors degree with honours’. It stretches credulity to its limits to imagine that the public is protected by degrees like this. Precisely the opposite is true. The universities have recognised this, and shut the degrees. One exception is Professor Pittilo’s own university which continues to run a course in homeopathy, the most discredited of all the popular types alternative medicine.
A simpler, more effective and cheaper way to protect the public
I must certainly agree with the minister that protection of the public is an important matter. Having established that the Pittllo recommendations are more likely to endanger the public than protect them, it is essential to suggest alternative proposals that would work better.
Luckily, that is easy, because mechanisms already exist for dealing with the dangers that were listed above. The matter of adulteration, which is serious in traditional Chinese medicine, is a matter that is already the responsibility of the Office of Trading Standards. The major problem of false claims being made for treatment is also the responsibility of the Office of Trading Standards, which has a statutory duty to enforce the Unfair Trading Consumer Protection Regulations of May 2008. These laws state, for example, that
“One of the 31 commercial practices which are in all circumstances considered unfair is “falsely claiming that a product is able to cure illnesses, dysfunction or malformations”
The monitoring of false claims, and of side effects of treatments, is also the responsibility of the Medicines and Health Regulatory Authority (MHRA).
Rather than setting up complicated, expensive and ineffective ‘regulation’ by the HPC, all that need to be done is to ensure that the MHRA and/or Trading Standards have the funds to enforce existing laws. At the moment, they are not being implemented effectively, so I’d recommend that responsibility for enforcing the law against false health claims be transferred entirely to the MHRA, which has much more expertise in such matters than Trading Standards This would be both cheaper and more effective than the present system in which the responsibility is divided between the two organisations in an unclear way.
This proposal would protect the public against unsafe and adulterated treatments, and it would protect the public against false and fraudulent claims. That is what matters. It would do so more effectively,
more cheaply and more honestly than the Pittilo recommendations. There would be no reduction in patient choice either, There is no proposal to ban acupuncture, herbal medicine or traditional Chinese medicine. All that is necessary is to ensure that they don’t endanger the public.
Since the root of the problem lies in the fact that the evidence for the effectiveness is very weak. the question of efficacy, and cost-benefit ratio, should be referred to NICE. This was recommended by the House of Lords Report (2000). It is recommended again by the Smallwood report (sponsored by the Prince of Wales Foundation). It is baffling that this has not been done already. It does not seem wise to spend large amounts of money on new research at the moment, in the light of the fact that the US National Institutes of Health has already spent over $1 billion on such research without finding a single useful treatment.
The results of all this research has been to show that hardly any alternative treatment are effective. That cannot be ignored.
Conclusion
Recent events show that the halcyon days for alternative medicine are over. When the Pittilo report first appeared, it was greeted with derision in the media. For example, in The Times Alice Miles wrote
“This week came the publication of the Report to Ministers from the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK. Otherwise known as twaddle.”
In the Independent, Dominic Lawson wrote
So now we will have degrees in quackery.
What, really, is the difference between acupuncture and psychic surgery?
People will no doubt continue to use it and that is their right and their responsibility. But if the government were to accept the recommendations of the Pittilo report it would be seen, quite rightly, as being anti-scientific and of posing a danger to the public.
Fortunately there is a better, and cheaper, way to protect the public.
Follow-up
Margaret McCartney’s blog in the Financial Times puts rhw view of a GP with her usual sense, humour and incisiveness.
“This report would, if implemented, create lots more nonsense exam papers funded by a lot more public money – and would produce practitioners without the absolutely crucial skill of how to assess evidence and reject or use it appropriately”
The Times has covered the story (with some interesting comments) Consultation on how to regulate complementary and alternative therapies
Times Higher Education UK-wide consultation on CAM regulation is launched Excellent response from Andy Lewis.
The Sun has by far the best coverage up to now, Jane Symons writes “Regulating quacks helps them prey on gullible patients“
Today, 29 July 2009, a large number of magazines and blogs will publish simultaneously Simon Singh’s article. The Guardian was forced to withdraw it, but what he said must be heard (even if the word ‘bogus’ is now missing).
This is an edited version if the article in the Guardian that resulted in the decision of the British Chiropractic Association to sue Singh for libel. That decision was bad for Singh, though its effects could yet be good for the rest of the world, Firstly the decision to use law rather than rational argument stands a good chance of destroying chiropractic entirely because its claims have now come under scrutiny as never before, and they have been found wanting. Secondly, the support for Singh has been so enormous that there must now be a good chance of getting the UK’s iniquitous laws about defamation changed.
I’d rather have reproduced the original article in its entirety, but this bowdlerised version still presents the case very strongly (and the unedited version appears here and here).
Beware the spinal trapSome practitioners claim it is a cure-all, but the research suggests chiropractic therapy has mixed results – and can even be lethal, says Simon Singh. You might be surprised to know that the founder of chiropractic therapy, Daniel David Palmer, wrote that “99% of all diseases are caused by displaced vertebrae”. In the 1860s, Palmer began to develop his theory that the spine was involved in almost every illness because the spinal cord connects the brain to the rest of the body. Therefore any misalignment could cause a problem in distant parts of the body. In fact, Palmer’s first chiropractic intervention supposedly cured a man who had been profoundly deaf for 17 years. His second treatment was equally strange, because he claimed that he treated a patient with heart trouble by correcting a displaced vertebra. You might think that modern chiropractors restrict themselves to treating back problems, but in fact some still possess quite wacky ideas. The fundamentalists argue that they can cure anything, including helping treat children with colic, sleeping and feeding problems, frequent ear infections, asthma and prolonged crying – even though there is not a jot of evidence. I can confidently label these assertions as utter nonsense because I have co-authored a book about alternative medicine with the world’s first professor of complementary medicine, Edzard Ernst. He learned chiropractic techniques himself and used them as a doctor. This is when he began to see the need for some critical evaluation. Among other projects, he examined the evidence from 70 trials exploring the benefits of chiropractic therapy in conditions unrelated to the back. He found no evidence to suggest that chiropractors could treat any such conditions. But what about chiropractic in the context of treating back problems? Manipulating the spine can cure some problems, but results are mixed. To be fair, conventional approaches, such as physiotherapy, also struggle to treat back problems with any consistency. Nevertheless, conventional therapy is still preferable because of the serious dangers associated with chiropractic. In 2001, a systematic review of five studies revealed that roughly half of all chiropractic patients experience temporary adverse effects, such as pain, numbness, stiffness, dizziness and headaches. These are relatively minor effects, but the frequency is very high, and this has to be weighed against the limited benefit offered by chiropractors. More worryingly, the hallmark technique of the chiropractor, known as high-velocity, low-amplitude thrust, carries much more significant risks. This involves pushing joints beyond their natural range of motion by applying a short, sharp force. Although this is a safe procedure for most patients, others can suffer dislocations and fractures. Worse still, manipulation of the neck can damage the vertebral arteries, which supply blood to the brain. So-called vertebral dissection can ultimately cut off the blood supply, which in turn can lead to a stroke and even death. Because there is usually a delay between the vertebral dissection and the blockage of blood to the brain, the link between chiropractic and strokes went unnoticed for many years. Recently, however, it has been possible to identify cases where spinal manipulation has certainly been the cause of vertebral dissection. Laurie Mathiason was a 20-year-old Canadian waitress who visited a chiropractor 21 times between 1997 and 1998 to relieve her low-back pain. On her penultimate visit she complained of stiffness in her neck. That evening she began dropping plates at the restaurant, so she returned to the chiropractor. As the chiropractor manipulated her neck, Mathiason began to cry, her eyes started to roll, she foamed at the mouth and her body began to convulse. She was rushed to hospital, slipped into a coma and died three days later. At the inquest, the coroner declared: “Laurie died of a ruptured vertebral artery, which occurred in association with a chiropractic manipulation of the neck.” This case is not unique. In Canada alone there have been several other women who have died after receiving chiropractic therapy, and Edzard Ernst has identified about 700 cases of serious complications among the medical literature. This should be a major concern for health officials, particularly as under-reporting will mean that the actual number of cases is much higher. If spinal manipulation were a drug with such serious adverse effects and so little demonstrable benefit, then it would almost certainly have been taken off the market. Simon Singh is a science writer in London and the co-author, with Edzard Ernst, of Trick or Treatment? Alternative Medicine on Trial. This is an edited version of an article published in The Guardian for which Singh is being personally sued for libel by the British Chiropractic Association. |
That’s a great account of the evidence. Notice the conclusion,
“If spinal manipulation were a drug with such serious adverse effects and so little demonstrable benefit, then it would almost certainly have been taken off the market“.
It is the job of NICE to evaluate critically that sort of thing, which makes it all the odder that the NICE guidance group, very unusually, failed to assess properly the evidence for chiropractic.
If you aren’t one of the 15,000 people who have already signed Singh’s statement, please do it now
Follow-up
Resignation of Pain Society president. While we are on the topic of chiropractic, my comment, The hidden cost of endorsing voodoo, appeared at last on the BMJ article about NICE’s low back pain guidance. The thread came back to life after the British Pain Society voted out its president, Paul Watson, a physiotherapist who was a member of the group that wrote the guidance.
Some of the links Links to some of the many repostings of Singh’s article today are aggregated at Sense about Science. There where over 200 in a single day. The British Chiropractic Association tried to suppress criticism, but they clearly don’t understand the web.
“An intrepid, ragged band of bloggers. Chiropractors may regret choosing to sue Simon Singh, springing online scientists into action”. Ben Goldacre has summed up the reaction of the blogosphere with characteristically fine style in the Guardian. Ragged? Moi? The blog version (with links) is here.
Acupuncture has been in the news since, in a moment of madness, NICE gave it some credence,
Some people still seem to think that acupuncture is somehow more respectable than, say, homeopathy and crystal healing. If you think that, read Barker Bausell’s book ot Trick or Treatment. It is now absolutely clear that ‘real’ acupuncture is indistinguishable from sham, whether the sham control uses retractable needles, or real needles in the ‘wrong’ places. There has been no clear demonstration of long-lived benefits in any condition, and it is likely that it is no more than a theatrical placebo.
In particular, the indistinguishability of ‘real’ and sham acupuncture shows, beyond reasonable doubt that all the stuff about “energy flow in meridians” is so much hokum.
There is a small group of ‘medical acupuncturists‘ that believes that it is hokum. but who nonetheless maintain that acupuncture works, despite the evidence to the contrary. But most acupuncturists go for the wholesale gobbledygook.
If you don’t believe that, take a look at the exam paper that has come into my possession. It is this year’s exam from the University of Salford. Salford has, very sensibly, now decided to stop all its degrees in alternative medicine, so don’t hold this against the university too much.
You can download the entire exam paper. Here are a few highlights.
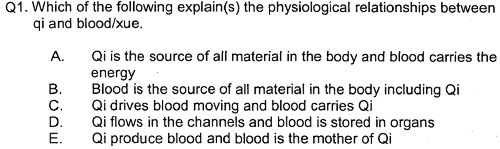
So students, in 2009, are being taught the crudest form of vitalism.
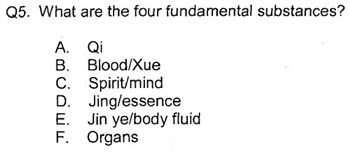
Oh really. Perhaps protons neutrons and electrons?
OK I’d fail that one because the words have no obvious meaning at all.
Perhaps an elementary textbook of embryology would help?
How one would love to see a set of model answers for these questions.
All this is ancient hokum being taugh to hapless students in the 21st century as though it were fact. The University of Salford has understood that and closed the course. All we need now is for NICE and the Department of Health to understand what it is that they are promoting.
NICE neglected the cultural cost of their guidance
When National Institute for Health and Clinical Excellence (NICE) included an acupuncture option on their low back pain guidance, they quite forget that one effect of their decision would be to ensure that new generations of students would have their minds poisoned with intellectual junk like this. That is why NICE really must think again. . See also
NICE falls for bait and switch by acupuncturists and chiropractors
NICE fiasco part 2 Rawlins should withdraw guidance and start again
NICE fiasco Part 3. Too many vested interests, not enough honesty
Pittilo and statutory regulation
Public consultation is due to open shortly on the appalling report of the Department of Health Steering Group on the Statutory Regulation of Practitioners of Acupuncture, Herbal Medicine, Traditional Chinese Medicine and Other Traditional Medicine Systems Practised in the UK (see also, The Times)
One of the recommendations is that acupuncture and Chinese herbal medicine should have statutory regulation by the Health Professions Council (HPC), despite the fact that that would involve the HPC breaking its own rules. Another recommendation of Pittilo is that entry to the “profession” (his word, not mine) should be by means of honours degree only. So he wants to impose on students exams like this one in order to “protect the public”? The absurdity of that proposal should be obvious now. This exam paper will form part of my evidence to the consultation.
And there is one other small problem. Universities are busy shutting down their degrees in alternative medicine, now that the ridiculousness of what is taught has been exposed. They have shut down entirely at the University of Salford and at the University of Central Lancashire, And even the University of Westminster is working on closing them.
All we need now is for the common sense and integrity that has been shown by these universities to spread to the Department of Health (and NICE).
Follow-up
|
.The University of Central Lancashire (UCLAN) is the first place I asked to see teaching materials that were used on its homeopathy “BSc” course. The request was refused, and subsequent internal appeals were refused too, Clearly UCLAN had something to hide. |

|
An appeal to the information commissioner took almost two years to be judged, but the case was won. The eventual decision by the Information
Commissioner rejected all the grounds that UClan had used to evade the Freedom of Information Act.
UClan appealed against the judgement and I still haven’t got the stuff but that hardly matters now, because the course in question shut its doors. In any case, plenty of stuff from similar courses has leaked out already.
Meanwhile, in September 2008, UCLAN announced an internal review of all its courses in magic medicine, The review seemed to be genuine. For a start they asked me to give evidence to the review (something that no other university has done). They also asked Michael Eslea to give evidence. He is the UCLAN psychologist, whose magnificent open letter probably tipped the authorities into holding the review.
Just in case it is useful to anyone, here is a copy of the written evidence that I sent [download pdf],
|
Report of the Working Party on the Review of issues associated with Homeopathy, Acupuncture and Chinese Herbal Medicine
1. Introduction As a consequence of concerns expressed by some colleagues within the University of Central Lancashire (UCLan) Dr Malcolm McVicar, Vice Chancellor appointed a working party to review the issues associated with the University offering courses in Homeopathy, Acupuncture and Chinese Herbal Medicine. MEMBERSHIP: Eileen Martin (Chair) Pro-Vice Chancellor and Dean of Faculty of Health and Social Care |
The report was the subject of a special meeting of UCLAN’s Academic Board on 9th July 2009. The following resolutions were passed.
|
Resolutions R1 That further minor revisions be made to the report prior to publication on the University’s website; R2 That the University refrain from offering any practitioner-qualifying courses in Homeopathy, Acupuncture and Chinese Herbal Medicine until such disciplines have achieved statutory regulation status; R3 That the University consider offering a limited number of postgraduate research studentships (leading to Masters by Research of PhD) to suitably qualified UCLan students and staff in these disciplines. They should have interdisciplinary supervisory teams to facilitate development of a broad range of research skills and to contribute to the generation of knowledge in CAM; R4 That the University consider how more interdisciplinary teaching can be achieved, where appropriate, within both undergraduate and postgraduate teaching to facilitate greater exposure to subject expertise and different paradigms. |
Resolutions 1, 3 and 4 say very little. Resolution 4 sounds thoroughly relativist. We are talking about medicine, about treating sick patients. There is only one “paradigm”. That is to find treatments that are as effective and safe as possible. There aren’t two sorts of medicine, regular and alternative. There is just medicine that works and medicine that doesn’t work. It’s a good illustration of DC’s rule number 2, “never trust anyone who uses the word paradigm”.
Resolution 2 is the really interesting one, because none if the topics, Homeopathy, Acupuncture and Chinese Herbal Medicine, is subject to statutory regulation.
If taken literally, resolution 2 means that all the UCLan courses in alternative medicine will close their doors. Bafflingly, this inevitable conclusion is not stated explicitly.
At least resolution 2 means that homeopathy, already closed, will stay closed. It is never likely to get statutory regulation.
For practical purposes, we can ignore for the moment the obvious fact that statutory regulation of nonsense subjects results only in nonsense. The only forms of alternative medicine that have got “statutory regulation” at the moment are chiropractic and osteopathy. The public has not been safeguarded by the General Chiropractic Council (GCC). The GCC, on the contrary, has endangered the public by allowing false health claims to be made with impunity. Perhaps the members of the review committee had not noticed that the Simon SIngh affair has resulted in almost 600 complaints being made to the GCC? The faith of the review in statutory regulation is clearly misplaced.
The Pittilo report is critical for what happens next
Acupuncture and Chinese Herbal Medicine are not subject to statutory regulation at present, so one would suppose that these degrees will close their doors too. However the infamous Pittilo report has proposed that they should become regulated by the Health Professions Council (HPC). The many problems of the Pittilo report have been documented here, in “A very bad report: gamma minus for the vice-chancellor“. There was also a high-profile critique of the report in The Times (and on this blog).
The HPC has, as one of its criteria for regulation, “evidence-based practice”. Disgracefully, the HPC has already shown its willingness to ignore its own rules and to act as statutory regulator for Acupuncture and Chinese Herbal medicine. This rather disgraceful behaviour is documented in “Health Professions Council ignores its own rules: the result is nonsense“.
The UCLAN report seems to assume that the recommendations of the Pittilo report will be accepted. But the long-awaited consultation has still not opened. We can be sure that when it does, the opposition to it will be very strong indeed.
The report in full
Here are a few comments on the report itself. Download the full report (as of July 15th).
i have to say that when I visited Preston to give evidence, my views seem to be treated seriously, even sympathetically, so it was a great disappointment to see the outcome. So what’s wrong? The major disaster is declared early in the report.
Section 2, Context
The debate is centred on a number of key themes which relate to:-
1. The quality of and/or absence of an evidence base to support claims of the efficacy and benefits of such treatments, linked to issues of public safety/protection and professional regulation.
Sounds good. What matters about any sort of medicine is whether or not it works and whether it is safe. It therefore verges on the incredible that we read in section 4.1
“conclusions from research into the efficacy of the various CAM’s are outside the remit of this report.”
The whole point about CAM is that there is very little evidence that any of it works. So the review committee decided to ignore the most important problem of the lot. I can’t see how any rational decision can be made without first deciding whether the treatment is better than placebo. That, surely, is the main question, and it was dodged.
UCLAN has failed to grasp the nettle, just as the Department of Health has also consistently failed to do so.
Section 4,1 Efficacy This section repeats the assertion, absurd to my mind, that it is possible to judge CAM courses while declining to assess whether they work or not.
Section 4.2 Role of Universities in Society.
There is universal agreement that critical thinking is crucial to the idea of a university, but the judgement of whether CAM teaches critical thinking is simply fudged. Again the report fails to grasp the nettle.
“Disagreements about critical thinking within CAMs arises because some will argue that such substantiation and assessment can occur within the discipline, whilst others will argue that the methodology for substantiation, that is evidence provision, is universal. As a result, the latter will demand that evidence is provided using methods from one field (e.g. randomised controlled trials) for use in another.”
Sadly, the report dodged the crucial judgement once again. The most obvious characteristic of every form of alternative medicine is their total lack of critical self-appraisal. It is very sad that the review committee could not bring itself to say so.
Section 4.4 Nomenclature of degrees
Recommendation
The nomenclature of courses, leading to a professional as well as an academic award, should reflect the professional route; for example Bachelor with Honours in Complementary Medicine, B Comp. Med.(Hons) or B Acupuncture (Hons).
This sounds to me like another truly pathetic fudge. What on earth is solved by changing the name of the degree? You’d still be teaching students the same load of gobbledygook and then letting them loose on sick people, whether you call it a Bachelor of Science, a Bachelor of Arts, or, as is recommended here, a Bachelor of nothing whatsoever.
Well, I suppose there is a (doubtless unintended) irony in calling CAM degrees “Bachelor of nothing whatsoever”.
Section 4.4 Ethical, non-harm and economic considerations
This section list a lot of reasons why teaching alternative medicine should be unethical. but nevertheless manages to conclude that
” . . . it is not unethical to offer courses in Homeopathy, Acupuncture and Chinese Herbal Medicine at a university.”
I find the logic by which this bizarre conclusion was reached quite impossible to follow. Like much of the rest of the report this conclusion seems to stem from a reluctance to grapple with the really important questions, like ‘does it work or not?’.
Despite this the recommendation is perhaps the most interesting of all.
“Recommendation
• The University refrains from offering any CAM courses until such disciplines have achieved statutory regulation status.”
This recommendation was accepted, and passed as a resolution at Academic Board. If it is implemented now, than there will be no more alternative medicine degrees next year at the University of Central Lancashire. If and when this happens, the University must be congratulated on its return to rational medicine.
Follow-up
Michael Eslea, UCLAN’s hero in resisting nonsense from the inside, has posted on this topic.
17 July 2009. It seemed odd that that no announcement was made about the future if the remaining CAM courses at UCLAN. So I asked deputy Vice-Chancellor Patrick McGhee for clarification. After a couple of days, I got this response.
|
From: CTheobald@uclan.ac.uk To: d.colquhoun@ucl.ac.uk Hi David, I have been asked to respond to your question below on the running of acupuncture and Chinese herbal medicine at UCLan. It is correct to assume that UCLan will not be taking any new entrants onto these programmes until further notice. Best Wishes Chris Chris Theobald |
So the report may have been disappointing, but it has done the job. As several people have pointed out in comments, it would be asking too much to expect a university to say “sorry we just noticed that we have been running junk-science courses for years”. But they have done the right thing anyway.
It’s good to see the BMJ joining the campaign for free speech (only a month or two behind the blogs). The suing of Simon Singh for defamation by the British Chiropractic Association has stirred up a hornet’s nest that could (one hopes) change the law of the land, and destroy chiropractic altogether. The BMJ’s editor, Fiona Godlee, has a fine editorial, Keep the libel laws out of science. She starts “I hope all readers of the BMJ are signed up to organised scepticism” and says
“Weak science sheltered from criticism by officious laws means bad medicine. Singh is determined to fight the lawsuit rather than apologise for an article he believes to be sound. He and his supporters have in their sights not only the defence of this case but the reform of England’s libel laws.”
Godlee refers to equally fine articles by the BMJ’s Deputy Editor, Tony Delamothe, Thinking about Charles II“, and by Editor in Chief, Harvey Marcovitch, “Libel law in the UK“.
The comments on Godlee’s editorial, show strong support, (apart from one from the infamous quantum fantasist, Lionel Milgrom). But there was one that slighlty surprised me, from Tricia Greenhalgh, author of the superb book, “How to read a paper”. She comments
“the use of the term ‘bogus’ seems both unprofessional and unscholarly. The argument would be stronger if expressed in more reserved terms”
That set me thinking, not for the first time, about the difference between journalism and scholarship. I can’t imagine ever using a word like ‘bogus’ in a paper about single ion channels. But Singh was writing in a newspaper, not in a scientific paper. Even more to the point, his comments were aimed at people who are not scholars and who, quite explicitly reject the normal standards of science and evidence. The scholarly approach has been tried for centuries, and it just doesn’t work with such people. I’d defend Singh’s language. It is the only way to have any effect. That is why I sent the following comment.
The ultimate irony is that the comment was held up by the BMJ’s lawyers, and has still to appear.
|
Thanks for an excellent editorial. I doubt that it’s worth replying to Lionel Milgrom whose fantasy physics has been totally demolished by real physicists. Trisha Greenhalgh is, though, someone whose views I’d take very seriously. She raises an interesting question when she says “bogus” is an unprofessional word to use. Two things seem relevant. First, there is little point in writing rational scholarly articles for a group of people who do not accept the ordinary rules of evidence or scholarship. We are dealing with fantasists. Worse still, we are dealing with fantasists whose income depends on defending their fantasies. You can point out to your heart’s content that “subluxations” are figment of the chiropractors’ imagination, but they don’t give a damn. They aren’t interested in what’s true and what isn’t. Throughout my lifetime, pharmacologists and others have been writing scholarly articles about how homeopathy and other sorts of alternative medicine are bogus. All this effort had little effect. What made the difference was blogs and investigative journalism. When it became possible to reveal leaked teaching materials that taught students that “amethysts emit high yin energy“, and name and shame the vice-chancellors who allow that sort of thing to happen (in this case Prof Geoffrey Petts of Westminster University), things started to happen. In the last few years all five “BSc” degrees in homeopathy have closed and that is undoubtedly a consequence of the activities of bloggers and can assess evidence but who work more like investigative journalists. When the BCA released, 15 months after the event, its “plethora of evidence” a semi-organised effort by a group of bloggers produced, in less than 24 hours, thoroughly scholarly analyses of all of them (there is a summary here). As the editorial says, they didn’t amount to a hill of beans, They also pointed out the evidence that was omitted by the BCA. The conventional press just followed the bloggers. I find it really rather beautiful that a group of people who have other jobs to do, spent a lot of time doing these analyses, unpaid, in their own time, simply to support Singh, because they believed it is the right thing to do. Simon Singh has analysed the data coolly in his book. But In the case that gave rise to the lawsuit he was writing in a newspaper. It was perfectly clear from the context what ‘bogus’ meant. but Mr Justice Eady (aided by a disastrous law) chose to ignore entirely the context and the question of truth. The description ‘bogus’. as used by Singh, seems to be entirely appropriate for a newspaper article. To criticise him for using “unprofessional” language is inappropriate because we are not dealing with professionals. At the heart of the problem is the sort of stifling political correctness that has resulted in quacks being referred to as “professions” rather than fantasists and fraudsters [of course I use the word fraudster with no implication that it necessarily implies conscious lying]. At least there are some laughs to be had from the whole sorry affair. Prompted by that prince among lawyers known as Jack of Kent there was a new addition to my ‘Patients’ Guide to Magic Medicine‘, as featured in the Financial Times.
|
It is, perhaps, misplaced political correctness that lies at the heart of the problem. Who can forget the letter from Lord Hunt, while he was at the Department of Health, in which he described “psychic surgery” (one of the best known fraudulent conjuring tricks) as a “profession”.
Follow-up
Two days later, the comment has appeared in the BMJ at last. But it has been altered a bit.
|
Unprofessional language is appropriate when dealing with unprofessional people Thanks for an excellent editorial. I doubt that it’s worth replying to Lionel Milgrom whose fantasy physics has been totally demolished by real physicists. Trisha Greenhalgh is, though, someone whose views I’d take very seriously. She raises an interesting question when she says “bogus” is an unprofessional word to use. Two things seem relevant. First, there is little point in writing rational scholarly articles for a group of people who do not seem to accept the ordinary rules of evidence or scholarship. You can point out to your heart’s content that “subluxations” are figment of the chiropractors’ imagination, but they don’t give a damn. Throughout my lifetime, pharmacologists and others have been writing scholarly articles about how homeopathy and other sorts of alternative medicine are bogus. All this effort had little effect. What made the difference was blogs and investigative journalism. When it became possible to reveal leaked teaching materials that taught students that “amethysts emit high yin energy”, and name and shame the vice-chancellors who allow that sort of thing to happen (in this case Prof Geoffrey Petts of Westminster University), things started to happen. In the last few years all five “BSc” degrees in homeopathy have closed and that is undoubtedly a consequence of the activities of bloggers and can assess evidence but who work more like investigative journalists. When the BCA released, 15 months after the event, its “plethora of evidence” a semi-organised effort by a group of bloggers produced, in less than 24 hours, thoroughly scholarly analyses of all of them (there is a summary here). As the editorial says, they didn’t amount to a hill of beans, They also pointed out the evidence that was omitted by the BCA. The conventional press just followed the bloggers. I find it really rather beautiful that a group of people who have other jobs to do, spent a lot of time doing these analyses, unpaid, in their own time, simply to support Singh, because they believed it is the right thing to do. Simon Singh has analysed the data coolly in his book. But In the case that gave rise to the lawsuit he was writing in a newspaper. It was perfectly clear from the context what ‘bogus’ meant. but Mr Justice Eady (aided by a disastrous law) chose to ignore entirely the context. The description ‘bogus’. as used by Singh, seems to be entirely appropriate for a newspaper article. To criticise him for using “unprofessional” language is inappropriate because we are not dealing with professionals. At least there are some laughs to be had from the whole sorry affair. Prompted by that prince among lawyers known as Jack of Kent there was a new addition to my ‘Patients’ Guide to Magic Medicine’, as featured in the Financial Times.
|
Here are the changes that were made. Hmm.very interesting.
Now back to the Ed Biz, for a moment. An article in Times Higher Education last week caused something of a stir.
V-cs’ candid views slip out online. 2 July 2009 By Zöe Corbyn
Prematurely released paper reveals fears of staff revolution and desire to cash in, writes Zöe Corbyn
The article refers to a paper that appeared on the web site of the journal Higher Education Quarterly. It is Perspectives of UK Vice-Chancellors on Leading Universities in a Knowledge-Based Economy by Lynn Bosetti, University of Calgary, and Keith Walker, University of Saskatchewan. The paper quotes ten different university vice-chancellors (presidents) of UK universities. Some of the comments caused quite a stir when they were quoted anonymously in an article in Times Higher Education. But the paper soon vanished and still has not reappeared. A version that lacks some of the names is expected to appear soon. The original uncensored version has now appeared on Wikileaks. Its source is no great mystery since it was available to the public for a short time. It seems a pity if vice-chancellors want to hide their views, so here are a few quotations from the original version.
The Vice-Chancellor of Oxford, Colin Lucas, cautions:
“One of the greatest distortions is this sense that the only thing that universities are for, is to drive the economy. The core mission of universities is threatened by a narrow value system.”
Steven Schwartz was vice-chancellor of Brunel University until February 2006 when he became Vice Chancellor of Macquarie University in Sydney, Australia. He’s quoted as saying
We all know that education is a commodity that can be bought and sold, often at a very high price. So universities are busy doing that – charging students a large amount of money to study in England because it is a popular destination. Branding and marketing take the font seat and education is in the back. (S. Schwartz, Brunel University)
Reflecting on the traditional role of the university, the Vice-Chancellor of University of Oxford, Colin Lucas, is concerned that
“commodification threatens to destroy not only scholarly democracy but civilisation itself.”
“The vice-chancellor needs to have a network of people involved in ‘intelligence gathering’ to be able to swiftly deal with ‘even the faintest hint of a revolution’ (S. Schwartz, Brunel University)”
That sounds a bit like the secret police and their network of informers. Hardly a good way to get the loyalty of your staff.
“you have to lead with flow and authority.You can never be out of touch with what faculty are thinking . . . if in the end faculty don’t follow you, it isn’t because they are stupid, it’s because you are out of touch’ (S. Schwartz)”
And that seems to say that you need to know how faculty think, not in order to listen to their views, but only to know how to beat them. Perhaps it has never occurred to Steven Schwartz that he might, just occasionally, be wrong?
Drummond Bone succeeded Howard Newby (of whom more here) as vice-chancellor of the University of Liverpool. he also seems to regard the drive to corporatisation of univeristies as a war against his own staff.
“You need to start by setting the agenda for change, then you have to look at who is going to be a driver or champion of that change, who is going to be a passenger and who, quite frankly, is going to stand against it’ (J. Drummond Bone)”.
Steven Schwartz again.
“we filled our senior management positions with people who had never worked in universities before. The HR [human relations] person came from mining, another from banking. It’s probably made a big difference to Brunel and its ability to move, in that people aren’t weighted down with a lot of public service type history.”
This attitude seems to me to be at the heart of the problem. it is based on a mistaken idea of what it is that gives a university a good reputation. The reputation, at least in academia, is the sum of the reputations of eminent people who work there, Physiologists will think of Bernard Katz and Andrew Huxley. Pharmacologists will think of Heinz Schild and James Black, People in English literature may never have heard of them, but they will think of John Sutherland and Rosemary Ashton, Each of them gives UCL a bit of reflected glory..But nobody will think about our Public Relations attempts at corporate image building. The only way to have a great university is to have great people doing the research and teaching. Anything that makes a university unattractive to them will, in the long run, harm the place. And one thing that makes a university unattractive is the perception that it is run by people who view it as a business, and who know nothing about what makes the place great. The sort of people whom Steven Schwartz seems to have gone out of his way to employ.
I was asked recently by the head of media relations to answer some questions about UCL’s attempts to build its “corporate identity” (nice to be asked, for a change). My answer was that I though they probably did more harm than good. The reason for saying that is that they are, only too often, downright embarrassing. I’ve mentioned the examples of ‘sustainable degrees‘, the concordat fiasco and ‘research days‘. And the new-age junk forced on our research staff by Human Resources is acutely embarrassing. Luckily for UCL, all universities have pursued this corporate path, so there is nowhere to run to,
The general public, having lived through the Blair era, is able to detect vacuous spin when it hears it. And there is no shortage of that in universities now. The aim of science is to discover truth. The aim of PR is to disguise truth, They are utterly incompatible. In the words of the “unrepentant capitalist” Luke Johnson, in the Financial Times,
“I have radically downsized HR in several companies I have run, and business has gone all the better for it.”
Another way to dismepower academics Steven Schwartz, with his spy network, is quite excessively conspiritorial. There is a much easier way to do it, You have a consultation. You hold open “town meetings”. The opposition then reveal themselves. Having taken the precaution of neutering the academic board, you are under no obligation to take the slightest notice of what anyone else says, and public humiliation of opponents will ensure there aren’t too many of them. I have seen this plan in action. It works rather well, in the short run. In the long run, though, academics lose morale, loyalty and altruism when treated in that way. Vice-chancellors who behave like that are bringing their institution into disrepute.
This was poeted from the train to Edinburgh,where I’ll be giving the Paton lecture, on a related topics.
Follow-up
The modified paper has now been published in Higher Education Quarterly. And, guess what, Steven Schwartz’s name is not mentioned in it.
On July 1st. the journal Nature, published three reports that described genetic differences between people with schizophrenia and the rest of us. Nature held a big press conference, at the World Conference of Science Journalists, Many of the individual institutions involved in the studies also issued press releases. As so often in press releases, descriptions like “landmark”, “major step forward” and “real scientific breakthrough” were used liberally.
In short, there is no simple genetic basis for schizophrenia. The pooled results of the three studies gave 8,014 cases and 19,090 controls. A huge amount of genetic analysis was involved. Many thousands of small genetic differences were found between the schizophrenics and the controls, but no single mutation alone had much effect. There could be even more, because it is still not possible to sequence the entire genome of so many people. . In total, the effects of the many small differences might account for 30 percent of the disease risk. That’s more than the few percent that could be predicted before, though it’s still well short of the 70 or 80 percent figure that is often quoted for the genetic component of schizophrenia.
What is observed is a correlation between differences in the genome and having schizophrenia. The results don’t tell us directly about the cause of schizophrenia, and they don’t even (so far anyway) tell us much about the mechanisms that give rise to schizophrenia.
The reporting of this event makes a fascinating contrast in styles of scientific journalism. I’ll compare only two of the reports. One is by Steve Connor in the Independent (he of the recent contretemps). The other is by Nicholas Wade in the New York Times.

The headline sounds pretty hyped up to me, but headlines are often written by sub-editors, not by the author of the article. The article itself seems to be a pretty straight account that uses mostly quotations from the press releases. And it is accompanied by an irrelevant picture of a brain image, that’s alleged to show areas of the brain that contain dopamine receptors, though the work being discussed shows exactly that It’s not just a matter of a disorder in a transmitter system.. So the article is OK but it doesn’t contribute anything itself.
The fact of the matter is that the results of the gargantuan effort put into this study is to show how enormously complicated the problem is and just how little we understand, The prospect of inventing ‘cures’ looks almost hopeless in the face of such complexity. Nobody said it would be easy, but it has turned
out to be even harder than pessimists guessed. I would prefer a report that conveyed this reality better than the press releases do, and better than most of the hundreds of newspaper reports based on the press releases. There is one such report, that in the New York Times.

|
The journal Nature held a big press conference in London Wednesday, at the World Conference of Science Journalists, to unveil three large studies of the genetics of schizophrenia. Press releases from five American and European institutions celebrated the findings, one using epithets like “landmark,” “major step forward,” and “real scientific breakthrough.” It was the kind of hoopla you’d expect for an actual scientific advance. It seems to me the reports represent more of a historic defeat, a Pearl Harbor of schizophrenia research. The defeat points solely to the daunting nature of the adversary, not to any failing on the part of the researchers, who were using the most advanced tools available. Still, who is helped by dressing The principal news from the three studies is that schizophrenia is caused by a very large number of errant genes, not a manageable and meaningful handful. The rationale behind the long search for schizophrenia genes was entirely justifiable. Since schizophrenia is highly heritable, it must have a strong genetic component. And it has long seemed possible that the responsible genetic variants underlying most common diseases would also be common. Natural selection gives us strong protection against diseases that strike before the age of reproduction. But its power to eliminate harmful genes is thought to wane sharply thereafter. So bad versions of genes that are bad only late in life could build up in the population, explaining why the common diseases that strike later in life are so common. And if researchers could identify the few major variants assumed to underlie each of these common diseases, from schizophrenia to heart disease to cancer, they could devise drugs to offset the genes’ effects. But nature is often a lot more complex than assumed. It now seems that the arm of natural selection is far longer than thought. It has reached way beyond our reproductive years and zapped most harmful genetic variants before they could get to be common in the population. That leaves relatively uncommon variants, lots and lots of them in each case, as the genetic cause of each common disease. In the last few years gene hunters in one common disease after another have turned up a few causative variant genes, after vast effort, but the variants generally account for a small percentage of the overall burden of illness. With most common diseases, it turns out, the disease is caused not by ten very common variant genes but by 10,000 relatively rare ones. Today it’s the turn of schizophrenia researchers to make the same discovery, though one perhaps more to be expected since schizophrenia is not good for reproduction. Schizophrenia too seems to be not a single disease, but the end point of 10,000 different disruptions to the delicate architecture of the human brain. Yes, that discovery is a landmark. The kind that says you have 10,000 miles yet to go. The march of science is not direct but two steps forward, one step back. This was the step back. But it was a completely necessary one. So the press release writers could have cast it as a noble defeat, were words like defeat a part of their vocabulary, or frankness their masters’ priority. |
This account may sound a bit pessimistic, but it also seems to me to be the most realistic of the lot.
Schizophrenia is not alone in proving to be a lot more complicated than one would have hoped. One of the most interesting outcomes of the genomic age has been to show that far simpler conditions than schizophrenia turn out to be not so simple after all. The simplest genetically transmitted diseases are those caused by mutation of a single amino acid in a single protein of known function. For example, one of the best understood receptors is the type of acetylcholine receptor that is responsible for transmitting an impulse from a motor nerve to a muscle cell, Curare blocks them and so paralyses voluntary movement, A rare form of muscle weakness, slow channel congenital myasthenic syndrome (SCCMS), is caused when one of the amino acids in the protein mutates. But it has turned out that there is not just one mutation. It would be nearer to the truth to say that each family that suffers from the disease has its own mutation. Each of the mutations has a rather similar effect on the function of the protein, but there is not just one SCCMS but dozens.
The same is true of mutations in the glycine receptor that cause the rare congenital condition, ‘startle disease’ (posh name, hyperekplexia), The glycine receptor mediates inhibitory actions in the spinal cord. It is blocked by strychine, Strychnine causes exaggerated reflexes and eventually tonic convulsions: your muscles tighten so you die with the risus sardonicus. Mutations in the glycine receptor that stop it working so well have an effect rather like strychnine. But rare though the disease is, at least 15 different mutations, each in a different family, have been found to produce similar effects. There is just one startle disease, but many.
Cystic fibrosis is even more complicated. Mutations in a single protein, with a function that is now quite well understood, can cause the disease. But every patient does not have the same mutation. Around 1500 mutations have been found in the 20 years since the gene was sequenced. And to make it still more complicated, the symptoms shown by two patients with the same mutation may not be identical. The effects depend, it seems, on the rest of the genetic make-up of the individual. There is a nice account in ‘The promise of a cure: 20 years and counting’..
The same pattern is repeated again and again. Schizophrenia is just a very extreme example of a common phenomenon Not so long ago it was the dogma was that the future of drug discovery lay in genomics and high-throughput screening, Richard Sykes, when head of GSK, put the vast resources of GSK into this approach. It did not really work (which might explain why he left GSK to become rector of Imperial College). Now we know why.
It turns out to be a bit more complicated than anyone had foreseen, and one suspects it will take a long time to sort it out.
Follow-up
There is some comment on the reports on the Nature web site.
As so often, there is a first class level-headed account of the facts and what they mean on the NHS Choices site.