David Colquhoun
It is a good thing that clinical trials have to be registered, but is not good that there is no obligation to reveal the outcome. Many are never published. Nobody knows quite why they are not published but clearly it is a source of ‘publication bias’ if results that somebody doesn’t like, whether for financial or ideological reasons, simply vanish.
That has been a problem with the pharmaceutical industry, as discussed by Ben Goldacre in This is a very broken system. For example, It has turned out that the SSRI antidepressants are essentially ineffective in mild/moderate depression, but that fact was concealed because negative trials were hidden by the drug companies. Likewise, it must be very tempting for homeopaths and other advocates of magic medicine, to quietly forget about trials that don’t come out as they wish. Nobody knows how often that happens, and Homeopaths certainly don’t always bury negative results. Peter Fisher has published trials with negative results. So has George Lewith. Both, needless to say, continue to prescribe it.
It seemed until this month that burial had been the fate of a trial of homeopathy at the Bristol Homeopathic Hospital, run by Dr Elizabeth Thompson.
Dr Thompson was also an author of the infamous paper, Spence et al (2005) paper [download pdf]. This paper was no more than a customer satisfaction survey. Half the patients felt better or much better after a visiting the Homeopathic Hospital, but there was no control group and so not the slightest reason to think that they felt better because of the homeopathic treatment. This pathetic apology for a trial is, needless to say, widely cited by homeopaths. Children with asthma were the group who most often said they felt better, and that might have been taken as a hint ro do a proper trial.
That isn’t what happened though. A small unblinded trial was proposed and it was run between January 1st 2005 and September
30th 2007. In March 2006 the University Hospitals Bristol NHS Trust announced a trial that was being run by Dr Elizabeth Thompson at the Bristol Homeopathic Hospital. The press release has now vanished, but it was reported by the BBC in May 2008.
But no results appeared. Soon people stared asking where the results were. It was discussed on the UKSKeptics forum in October 2006, and on the James Randi Educational Forum. I wrote to Dr Thompson in December 2007 to ask if their results of the asthma study were available yet, and got a rather rude reply (some details below). I was also told by Dr Thompson that
"I have just submitted the funders report today and we have set ourselves the deadline to publish two inter-related papers by March 1st 2007.".
But it still didn’t appear. I and others wrote to the Hospital Trust but got nowhere. Two years later, In 2009, a Freedom of Information Act request was sent to the Hospital Trust (not by me) to try to discover what the still unpublished results were. In February 2010, the Hospital’s lawyers declined to provide the information on the grounds that publication was "imminent".
Then, at last, in July 2011,four years after it was promised, the paper appeared, in the journal Homeopathy. UCL does not, thank heavens, subscribe to that journal, but a request on Twitter produced three copies in no time: twitter is great for crowd-sourcing. The paper is The feasibility of a pragmatic randomised controlled trial to compare usual care with usual care plus individualised homeopathy, in children requiring secondary care for asthma.
It’s not surprising that publication was delayed. The results are completely negative. In fact it shows that the homeopathic treatment didn’t even produce a placebo effect, never mind an effect of its own.
Some details of the paper
The paper compared ‘usual treatment’ with ‘usual treatment plus homeopathic treatment’ for children with asthma. Children were allocated randomly to one treatment or the other (good) but of course they were aware of what treatment they were getting (not good). Ernst has pointed out that this sort of trial can never give a negative result unless the homeopathic treatment is actually harmful. The usual care plus homeopathy group can only benefit from any placebo effect produced by the homeopathic consultation.
The pills used were all 12C dilutions or even weaker, so none of them contained anything whatsoever.
The remarkable thing about this trial was that there was no detectable difference between the ‘usual treatment’ and ‘usual treatment + homeopathy’ groups.
The homeopathic treatment was not just ineffective in itself, but it didn’t even have any detectable placebo effect.
In that respect, the result resembles those in a recent paper in the British Journal of General Practice that showed acupuncture didn’t even produce any useful placebo effect.
The trial was quite small, 39 children aged 7 – 14 years, with moderate or severe asthma were divided into the two groups, and 35 finished the trial. The follow-up periods was 16 weeks which should be enough to show any substantial effect on asthma. Twelve different outcomes were measured and none showed any difference between the two groups (despite the fact that no allowance was made for multiple comparisons, and no primary outcome was specified in advance).
A cost-benefit analysis was done. There was no benefit but there was certainly a cost. On average, each of the children in the usual care group cost the NHS £323, but when homeopathy was added, the cost was £937. That’s an extra cost of £615 for no benefit.
The authors’ conclusions are simple
Conclusions: A future study using this design is not feasible,
That’s pretty feeble. They don’t state the conclusion as "homeopathy doesn’t work", far less that "homeopathy doesn’t even have a placebo effect". Just the eternal cry after every failed trial of magic medicine: the trial design was wrong and more research is needed. An excuse was offered in the form
"A further limitation was the length of the study period which may have needed to be longer in order for homeopathic treatment to make an impact in a complex disease with high variabilitythrough the year."
This is a paraphrase of the typical homeopathic modus operandi. Keep trying a different pill until the patient gets better anyway, then claim the credit.
Some details of the attempts to discover the results
Some of this was recounted in 2007, but it’s so bizarre I’ll repeat it here.
On 11 December 2007 I wrote to Dr Thompson, thus
|
In March 2006, a press release http://www.ubht.nhs.uk/press/view.asp?257 announced a randomised trial for homeopathic treatment of asthma in children. This was reported also on the BBC http://news.bbc.co.uk/1/hi/england/bristol/4971050.stm . I’d be very grateful if you could let me know when results from this trial will become available. Yours sincerely David Colquhoun |
The reply, dated 11 December 2007, was unsympathetic
|
I have just submitted the funders report today and we have set ourselves the deadline to publish two inter-related papers by March 1st 2007. Can I ask why you are asking and what authority you have to gain this information. I shall expect a reply to my questions, |
I answered this question politely on the same day, 11th December.
|
I know we disagree about the strength of the existing evidence, but nevertheless I was surprised by the strength of your reaction, and the rather abusive stance about my scientific credentials. I’m rather interested in evidence (my first academic work was a text book on statistics), and I’m always eager to see new data. From little I could learn it seemed that your data might be rather better quality than usual. If the evidence is good enough, I’m quite happy to change my mind. That’s how science works isn’t it?
With best regards David Colquhoun |
Nevertheless my innocent enquiry drew forth a rather vitriolic complaint from Dr Thompson to the Provost of UCL (dated 14 December 2007). Despite the fact that I’d replied on December 11th, she said to the provost (with a lot more invective)
"As yet I have not received a reply from Professor Colquhoun as to the authority he is using to make direct enquiries to me about my research. I would be grateful if you could reassure me th~t UCL have really thought through the implications of having someone, with such strong opinions that seem to extend beyond reason, promoting their opinions at such a high profile".
Dr. E. A. Thompson, BA Oxon, MBBS, MRCP, FFHom,
Lead Clinician/Consultant Homeopathic Physician &
Honorary Senior Lecturer in Palliative Medicine
In this case, the Provost came up trumps. On 14 January 2008 he replied to Thompson:
“I have looked at the email that you copied to me, and I must say that it seems an entirely proper and reasonable request. It is not clear to me why Professor Colquhoun should require some special authority to make such direct enquiries”.
Dr Thompson seems to be very sensitive. Now we have seen the results of her trial, perhaps it’s not surprising
Follow-up
Almost all the revelations about what’s taught on university courses in alternative medicine have come from post-1992 universities. (For readers not in the UK, post-1992 universities are the many new univerities created in 1992, from former polytechnics etc, and Russell group universities are the "top 20" research-intensive universities)
It is true that all the undergraduate courses are in post-1992 universities, but the advance of quackademia is by no means limited to them. The teaching at St Bartholomew’s Hospital Medical School, one of the oldest, was pretty disgraceful for example, though after protests from their own students, and from me, it is now better, I believe.

Quackery creeps into all universities to varying extents. The good ones (like Southampton) don’t run "BSc" degrees, but it still infiltrates through two main sources,
The first is via their HR departments, which are run by people who tend to be (I quote) "credulous and moronic" when it comes to science.
The other main source is in teaching to medical students. The General Medical Council says that medical students must know something about alterantive medicine and that’s quite right, A lot of their patients will use it. The problem is that the guidance is shockingly vague .
“They must be aware that many patients are interested in and choose to use a range of alternative and complementary therapies. Graduates must be aware of the existence and range of such therapies, why some patients use them, and how these might affect other types of treatment that patients are receiving.” (from Tomorrow’s Doctors, GMC)
In many medical schools, the information that medical students get is quite accurate. At UCL and at King’s (London) I have done some of the familiarisation myself. In other good medical schools, the students get some shocking stuff. St Bartholomew’s Hospital medical School was one example. Edinburgh University was another.
But there is one Russell group university where alternative myths are propagated more than any other that I know about. That is the University of Southampton.
In general, Southampton is a good place, I worked there for three years myself (1972 – 1975). The very first noise spectra I measured were calculated on a PDP computer in their excellent Institute of Sound and Vibration Research, before I wrote my own programs to do it.
But Southanpton also has a The Complementary and Integrated Medicine Research Unit . Oddly the unit’s web site, http://www.cam-research-group.co.uk, is not a university address, and a search of the university’s web site for “Complementary and Integrated Medicine Research Unit” produces no result. Nevertheless the unit is “within the School of Medicine at the University of Southampton”
Notice the usual euphemisms ‘complementary’ and ‘integrated’ in the title: the word ‘alternative’ is never used. This sort of word play is part of the bait and switch approach of alternative medicine.
The unit is quite big: ten research staff, four PhD students and two support staff It is headed by George Lewith.
Teaching about alternative medicine to Southampton medical students.
The whole medical class seems to get quite a lot compared with other places I know about. That’s 250 students (210 on the 5-year course plus another 40 from the 4-year graduate-entry route).
Year 1: Lecture by David Owen on ‘holism’ within the Foundation Course given to all 210 medical students doing the standard (5-year) course.
Year 2: Lecture by Lewith (on complementary medicine, focusing on acupuncture for pain) given within the nervous systems course to the whole medical student year-group (210 students).
Year 3 SBOM (scientific basis of medicine) symposium: The 3-hour session (“Complementary or Alternative Medicine: You Decide”). I’m told that attendance at this symposium is often pretty low, but many do turn up and all of them are officially ‘expected’ to attend.
There is also an optional CAM special study module chosen by 20 students in year 3, but also a small number of medical students (perhaps 2 – 3 each year?) choose to do a BMedSci research project supervised by the CAM research group and involving 16-18 weeks of study from October to May in Year 4. The CAM research group also supervise postgraduate students doing PhD research.
As always, a list of lectures doesn’t tell you much. What we need to know is what’s taught to the students and something about the people who teach it. The other interesting question is how it comes about that alternative medicine has been allowed to become so prominent in a Russell group university. It must have support from on high. In this case it isn’t hard to find out where it comes from. Here are some details.
Year 1 Dr David Owen
David Owen is not part of Lewith’s group, but a member of the Division of Medical Education headed by Dr Faith Hill (of whom, more below). He’s one of the many part-time academics in this area, being also a founder of The Natural Practice .
Owen is an advocate of homeopathy (a past president of the Faculty of Homeopathy). Homeopathy is, of course, the most barmy and discredited of all the popular sorts of alternative medicine. Among those who have discredited it is the head of the alt med unit, George Lewith himself (though oddly he still prescribes it).
And he’s also a member of the British Society of Environmental Medicine (BSEM). That sounds like a very respectable title, but don’t be deceived. It is an organisation that promotes all sorts of seriously fringe ideas. All you have to do is notice that the star speaker at their 2011 conference was none other than used-to-be a doctor, Andrew Wakefield, a man who has been responsible for the death of children from measles by causing an unfounded scare about vaccination on the basis of data that turned out to have been falsified. There is still a letter of support for Wakefield on the BSEM web site.
The BSEM specialises in exaggerated claims about ‘environmental toxins’ and uses phony allergy tests like kinesiology and the Vega test that misdiagnose allergies, but provide en excuse to prescribe expensive but unproven nutritional supplements, or expensive psychobabble like "neuro-linguistic programming".
Other registered "ecological physicians" include the infamous Dr Sarah Myhill, who, in 2010, was the subject of a damning verdict by the GMC, and Southampton’s George Lewith.
If it is wrong to expose medical students to someone who believes that dose-response curves have a negative slope (the smaller the dose the bigger the effect -I know, it’s crazy), then it is downright wicked to expose students to a supporter of Andrew Wakefield.
David Owen’s appearance on Radio Oxford, with the indomitable Andy Lewis appears on his Quackometer blog.
Year 2 Dr George Lewith
Lewith is a mystery wrapped in an enigma. He’s participated in some research that is quite good by the (generally pathetic) standards of the world of alternative medicine.
In 2001 he showed that the Vega test did not work as a method of allergy diagnosis. "Conclusion Electrodermal testing cannot be used to diagnose environmental allergies", published in the BMJ .[download reprint].
In 2003 he published "A randomized, double-blind, placebo-controlled proving trial of Belladonna 30C” [download reprint] that showed homeopathic pills with no active ingredients had no effects: The conclusion was "”Ultramolecular homeopathy has no observable clinical effects" (the word ultramolecular, in this context, means that the belladonna pills contained no belladonna).
In 2010 he again concluded that homeopathic pills were no more than placebos, as described in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again). [download reprint]
What i cannot understand is that, despite his own findings, his private practice continues to prescribe the Vega machine and continues to prescribe homeopathic pills. And he continues to preach this subject to unfortunate medical students.
Lewith is also one of the practitioners recommended by BSEM. He’s a director of the "College of Medicine". And he’s also an advisor to a charity called Yes To Life. (see A thoroughly dangerous charity: YesToLife promotes nonsense cancer treatments).
3rd year Student Selected Unit
The teaching team includes:
- David Owen – Principal Clinical Teaching Fellow SoM, Holistic Physician
- George Lewith – Professor of Health Research and Consultant Physician
- Caroline Eyles – Homeopathic Physician
- Susan Woodhead – Acupuncturist
- Elaine Cooke – Chiropractic Practitioner
- Phine Dahle – Psychotherapist
- Keith Carr – Reiki Master
- Christine Rose – Homeopath and GP
- David Nicolson – Nutritionalist
- Shelley Baker – Aromatherapist
- Cheryl Dunford – Hypnotherapist
- Dedj Leibbrandt – Herbalist
More details of the teaching team here. There is not a single sceptic among them, so the students don’t get a debate, just propaganda.
In this case. there’s no need for the Freedom of Information Act. The handouts. and the powerpoints are on their web site. They seem to be proud of them
Let’s look at some examples
Chiropractic makes an interesting case, because, in the wake of the Singh-BCA libel case, the claims of chiropractors have been scrutinised as never before and most of their claims have turned out to be bogus. There is a close relationship between Lewith’s unit and the Anglo-European Chiropractic College (the 3rd year module includes a visit there). In fact the handout provided for students, Evidence for Chiropractic Care , was written by the College. It’s interesting because it provides no real evidence whatsoever for the effectiveness of chiropractic care. It’s fairly honest in stating that the view at present is that, for low back pain, it isn’t possible to detect any difference between the usefulness of manipulation by a physiotherapist, by an osteopath or by a chiropractor. Of course it does not draw the obvious conclusion that this makes chiropractic and osteopathy entirely redundant -you can get the same result without all the absurd mumbo jumbo that chiropractors and osteopaths love, or their high-pressure salesmanship and superfluous X-rays. Neither does it mention the sad, but entirely possible, outcome that none of the manipulations are effective for low back pain. There is, for example, no mention of the fascinating paper by Artus et al [download reprint]. This paper concludes
"symptoms seem to improve in a similar pattern in clinical trials following a wide
variety of active as well as inactive treatments."
This paper was brought to my attention through the blog run by the exellent physiotherapist, Neil O’Connell. He comments
“If this finding is supported by future studies it might suggest that we can’t even claim victory through the non-specific effects of our interventions such as care, attention and placebo. People enrolled in trials for back pain may improve whatever you do. This is probably explained by the fact that patients enrol in a trial when their pain is at its worst which raises the murky spectre of regression to the mean and the beautiful phenomenon of natural recovery.”
This sort of critical thinking is conspicuously absent from this (and all the other) Southampton handouts. The handout is a superb example of bait and switch: No nonsense about infant colic, innate energy or imaginary subluxations appears in it.
Acupuncture is another interesting case because there is quite a lot of research evidence, in stark contrast to the rest of traditional Chinese medicine, for which there is very little research.
|
There is a powerpoint show by Susan Woodhead (though it is labelled British Acupuncture Council). The message is simple and totally uncritical. It works. |

|
In fact there is now a broad consensus about acupuncture.
(1) Real acupuncture and sham acupuncture have been found to be indistinguishable in many trials. This is the case regardless of whether the sham is a retractable needle (or even a toothpick) in the "right" places, or whether it is real needles inserted in the "wrong" places. The latter finding shows clearly that all that stuff about meridians and flow of Qi is sheer hocus pocus. It dates from a pre-scientific age and it was wrong.
(2) A non-blind comparison of acupuncture versus no acupuncture shows an advantage for acupuncture. But the advantage is usually too small to be of any clinical significance. In all probability it is a placebo effect -it’s hard to imagine a more theatrical event than having someone in a white coat stick long needles into you, like a voodoo doll. Sadly, the placebo effect isn’t big enough to be of much use.
Needless to say, none of this is conveyed to the medical students of Southampton. Instead they are shown crude ancient ideas that date from long before anything was known about physiology as though they were actually true. These folks truly live in some alternative universe. Here are some samples from the acupuncture powerpoint show by Susan Woodhead.
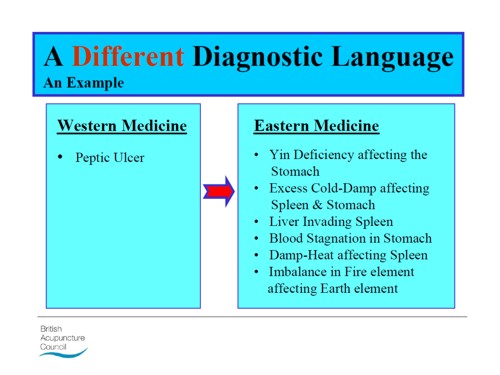
Well this is certainly a "different diagnostic language", but no attempt is made to say which one is right. In the mind of the acupuncurist it seems both are true. It is a characteristic of alternative medicine advocates that they have no difficulty in believing simultaneously several mutually contradictory propositions.
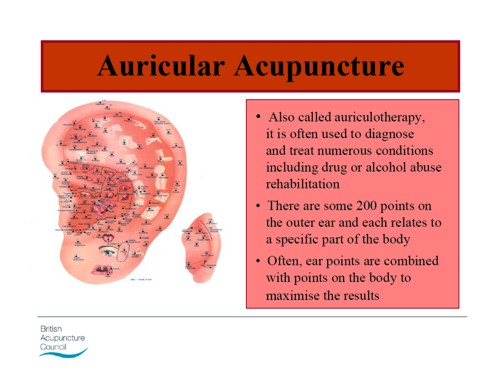
As a final exmple of barminess, just look at the acupuncture points (allegedly) on the ear The fact that it is a favoured by some people in the Pentagon as battlefield acupuncture, is more reminiscent of the mad general, Jack D. Ripper, in Dr Strangelove than it is of science.
There is an equally uncritical handout on acupuncture by Val Hopwood. It’s dated March 2003, a time before some of the most valuable experiments were done.
The handout says "sham acupuncture
is generally less effective than true acupuncture", precisely the opposite of what’s known now. And there are some bits that give you a good laugh, always helpful in teaching. I like
“There is little doubt that an intact functioning nervous system is required for acupuncture to produce
analgesia or, for that matter, any physiological changes”
and
Modern techniques: These include hybrid techniques such as electro-acupuncture . . . and Ryadoraku [sic] therapy and Vega testing.
Vega testing!! That’s been disproved dozens of times (not least by George Lewith). And actually the other made-up nonsense is spelled Ryodoraku.
It’s true that there is a short paragraph at the end of the handout headed "Scientific evaluation of acupuncture" but it doesn’t cite a single reference and reads more like excuses for why acupuncture so often fails when it’s tested properly.
Homeopathy. Finally a bit about that most boring of topics, the laughable medicine that contains no medicine, homeopathy. Caroline Eyles is a member for the Society of Homeopaths, the organisation that did nothing when its members were caught out in the murderous practice of recommending homeopathy for prevention of malaria. The Society of Homeopaths also endorses Jeremy Sherr, a man so crazy that he believes he can cure AIDS and malaria with sugar pills.
The homeopathy handout given to the students has 367 references, but somehow manages to omit the references to their own boss’s work showing that the pills are placebos. The handout has all the sciencey-sounding words, abused by people who don’t understand them.
"The remedy will be particularly effective if matched to the specific/particular characteristics of the individual (the ‘totality’ of the patient) on all levels, including the emotional and mental levels, as well as just the physical symptoms. ‘Resonance’ with the remedy’s curative power will then be at it’s [sic] best."
The handout is totally misleading about the current state of research. It says
"increasing clinical research confirms it’s [sic] clinical effectiveness in treating patients, including babies and animals (where a placebo effect would be hard to justify)."
|
The powerpont show by Caroline Eyles shows all the insight of a mediaeval vitalist |
|
Anyone who has to rely on the utterly discredited Jacques Benveniste as evidence is clearly clutching at straws. What’s more interesting about this slide the admission that "reproducibility is a problem -oops, an issue" and that RCTs (done largely by homeopaths of course) have "various methodological flaws and poor external validity". You’d think that if that was the best that could be produced after 200 yours, they’d shut up shop and get another job. But, like aging vicars who long since stopped believing in god, but are damned if they’ll give up the nice country rectory, they struggle on, sounding increasingly desperate.
How have topics like this become so embedded in a medical course at a Russell group university?
The details above are a bit tedious and repetitive. It’s already established that hardly any alternative medicine works. Don’t take my word for it. Check the web site of the US National Center for Complementary and Alternative Medicine (NCCAM) who, at a cost of over $2 billion have produced nothing useful.
A rather more interesting question is how a good university like Southampton comes to be exposing its medical students to teaching like this. There must be some powerful allies higher up in the university. In this case it’s pretty obvious who thay are.
Professor Stephen Holgate MD DSc CSc FRCP FRCPath FIBiol FBMS FMed Sci CBE has to be the primary suspect, He’s listed as one of Southampton’s Outstanding Academics. His work is nothing to do with alternative medicine but he’s been a long term supporter of the late unlamented Prince of Wales’ Foundation, and he’s now on the advisory board of it’s successor, the so called "College of Medicine" (for more information about that place see the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health, and also Don’t be deceived. The new “College of Medicine” is a fraud and delusion ). His description on that site reads thus.
"Stephen Holgate is MRC Clinical Professor of Immunopharmacology at the University of Southampton School of Medicine and Honorary Consultant Physician at Southampton University Hospital Trust. He is also chair of the MRC’s Populations and Systems Medicine Board. Specialising in respiratory medicine, he is the author of over 800 peer-reviewed papers and contributions to scientific journals and editor of major textbooks on asthma and rhinitis. He is Co-Editor of Clinical and Experimental Allergy, Associate Editor of Clinical Science and on the editorial board of 25 other scientific journals."
Clearly a busy man. Personally I’m deeply suspicious of anyone who claims to be the author of over 800 papers. He graduated in medicine in 1971, so that is an average of over 20 papers a year since then, one every two or three weeks. I’d have trouble reading that many, never mind writing them.
Holgate’s long-standing interest in alternative medicine is baffling. He’s published on the topic with George Lewith, who, incidentally, is one of the directors of the "College of Medicine"..
It may be unkind to mention that, for many years now, I’ve been hearing rumours that Holgate is suffering from an unusually bad case of Knight starvation.
The Division of Medical Education appears to be the other big source of support for. anti-scientific medicine. That is very odd, I know, but it was also the medical education people who were responsible for mis-educating medical students at. St. Bartholomew’s and at Edinburgh university. Southampton’s Division of Medical Education has a mind-boggling 60 academic and support staff. Two of them are of particular interest here.
Faith Hill is director of the division. Her profile doesn’t say anything about alternative medicine, but her interest is clear from a 2003 paper, Complementary and alternative medicine: the next generation of health promotion?. The research consisted of reporting anecdotes from interviews of 52 unnamed people (this sort of thing seems to pass for research in the social sciences). It starts badly by misrepresenting the conclusions of the House of Lords report (2000) on CAM. Although it comes to no useful conclusions, it certainly shows a high tolerance of nonsensical treatments.
Chris Stephens is Associate Dean of Medical Education & Student Experience. His sympathy is shown by a paper he wrote In 2001, with David Owen (the homeopath, above) and George Lewith: Can doctors respond to patients’ increasing interest in complementary and alternative medicine?. Two of the conclusions of this paper were as follows.
"Doctors are training in complementary and alternative medicine and report benefits both for their patients and themselves"
Well, no actually. It wasn’t true then, and it’s probably even less true now. There’s now a lot more evidence and most of it shows alternative medicine doesn’t work.
"Doctors need to address training in and practice of complementary and alternative medicine within their own organisations"
Yes they certainly need to do that.
And the first thing that Drs Hill and Stephens should do is look a bit more closely about what’s taught in their own university, I hope that this post helps them,
Follow-up
4 July 2011. A correspondent has just pointed out that Chris Stephens is a member of the General Chiropractic Council. The GCC is a truly pathetic pseudo-regulator. In the wake of the Simon Singh affair it has been kept busy fending off well-justified complaints against untrue claims made by chiropractors. The GCC is a sad joke, but it’s even sadder to see a Dean of Medical Education at the University of Southampton being involved with an organisation that has treated little matters of truth with such disdain.
A rather unkind tweet from (ex)-chiropractor @RichardLanigan.
“Chris is just another light weight academic who likes being on committees. Regulatory bodies are full of them”
The Atlantic is an American magazine founded (as The Atlantic Monthly) in Boston, Massachusetts, in 1857. It is a literary and cultural magazine with a very distinguished history. Its contributors include Mark Twain and Martin Luther King. So it was pretty exciting to be asked to write something for it, even with a 12 hour deadline.

Sadly though, in recent years, the coverage of science in The Atlantic has been less than good The inimitable David Gorski has explained the problem in Blatant pro-alternative medicine propaganda in The Atlantic. The immediate cause of the kerfuffle was the publication of an article, The Triumph of New-Age Medicine. It was written by a journalist, David Freedman. It is very long and really not very good. It has been deconstructed also by Steven Novella.
Freedman’s article is very long, but it boils down to saying I know it doesn’t work but isn’t it nice. The article was followed up with Fix or Fraud: a ‘debate’., The debate is rather disappointing. It suffers from the problem, not unknown at the BBC, of thinking that ‘balance’ means giving equal time to people who think the earth is flat as it gives to people who think it is a oblate spheroid. The debate consists of 800 word contributions from seven people, six of whom are flat earthers, and one of which is very good. Try Steven Salzberg, A ‘triumph’ of hype over reality for some real sense. One of the flat earthers is director of a National Institutes of Health institute, NCCAM.
And this is a magazine that published not only Mark Twain, but Abraham Flexner, the man who, in 1910, put US medical education on a firm scientific footing, You can read Flexner in their archive. Mark Twain said
[A reply to letters recommending remedies]:
Dear Sir (or Madam):–I try every remedy sent to me. I am now on No. 67. Yours is 2,653. I am looking forward to its beneficial results. – quoted in My Father Mark Twain, by Clara Clemens
"allopathy is good for the sane and homeopathy for the insane"
So here is the piece, produced rather rapidly, for the debate. This is the original unedited version, slightly longer than appears in The Atlantic.
The title for The Atlantic piece, America, Land of the Health Hucksters, was theirs not mine. There is no shortage of health hucksters in the UK. but at least they mostly haven’t become as embedded within univerities and hospitals as much as in the USA.
|
David Freeman’s article, “The Triumph of New Age Medicine” starts by admitting that most alternative treatments don’t work, and ends by recommending them. He takes a lot more words to say it, but that seems a fair synopsis. It is the sort of thing you might expect in a cheap supermarket magazine, not in Atlantic. The article is a prime example of rather effective sales technique, much beloved of used car salesmen and health hucksters. It’s called bait and switch. It’s true that medicine can’t cure everything. That’s hardly surprising given that serious research has been going on for barely 100 years, and it turns out that the humans are quite complicated. But the answer to the limitations of medicine is not to invent fairy stories, which is what the alternative medicine industry does. There is no sensible option but to keep the research going and to test its results honestly. It’s sad but true that Big Pharma has at times corrupted medicine, by concealing negative results. But that corruption has been revealed by real scientists, not by health hucksters. In the end, science is self-correcting and the truth emerges. Health hucksters, on the other hand, seem incapable of giving up their beliefs whatever the evidence says. The idea of patient-centered care is fashionable and care is great, if you can’t cure. But there’s a whole spectrum in the wellbeing industry, from serious attempts to make people happier, to the downright nuts. The problem is that caring for patients make a very good bait, and the switch to woo tends to follow not far behind. I write from the perspective of someone who lives in a country that achieves health care for all its citizens at half the cost of the US system, and gets better outcomes in life expectancy and infant mortality. The view from outside is that US medicine rather resembles US religion. It has been taken over by fundamentalists who become very rich by persuading a gullible public to believe things that aren’t true. One of Freedman’s problems is, I think, that he vastly overestimates the power of the placebo effect. It exists, for sure, but in most cases, it seems to be small, erratic and transient. Acupuncture is a good example. It’s quite clear now that real acupuncture and sham acupuncture are indistinguishable, so it’s also quite clear that the ‘principles’ on which it’s based are simply hokum. If you do a non-blind comparison of acupuncture with no acupuncture, there is in some trials (not all) a small advantage for the acupuncture group. But it is too small to be of much benefit to the patient. By far the more important reason why ineffective voodoo like acupuncture appears to work is the “get better anyway” effect (known technically as regression to the mean). You take the needles or pills when you are at your worst, the next day you feel better. It’s natural to attribute the fact that you feel better to the needles or pills, when all you are seeing is natural fluctuations in the condition. It’s like Echinacea will cure your cold in only seven days when otherwise it would have taken a week. If the article itself was naïve and uncritical, the follow up was worse. It is rather surprising to me that a magazine like Atlantic should think it worth printing an advertorial for Andrew Weil’s business. Surely, though, Josephine Briggs, as director of an NIH institute is more serious? Sadly, no. Her piece is a masterpiece of clutching at straws. The fact is that her institute has spent over $ 2 billion of US taxpayers’ money and, for all that money it has produced not a single useful treatment. All that NCCAM has done is to show that several things do not work, something we pretty much knew already. If I were a US taxpayer, I’d be somewhat displeased by that. It should be shut down now. At first sight Dean Ornish sounds more respectable. He bases his arguments on diet and life style changes, which aren’t alternative at all. He’s done some research too. The problem is that it’s mostly preliminary and inconclusive research, on the basis of which he vastly exaggerates the strength of the evidence for what can be achieved by diet alone. It’s classical bait and switch again. The respectable, if ill-founded, arguments get you the foot in the door, and the woo follows later. This is all very sad for a country that realized quite early that the interests of patients were best served by using treatments that had been shown to work. The Flexner report of 1910 led the world in the rational education of physicians. But now even places like Yale and Harvard peddle snake oil to their students through their "integrative medicine" departments. It’s hard to see why the USA is in the vanguard of substituting wishful thinking for common sense and reason. The main reason, I’d guess, is money. Through NCCAM and the Bravewell Collaborative, large amounts of money have been thrown to the winds and businesses like Yale and Harvard have been quick to abandon their principles and grab the money. Another reason for the popularity of alternative medicine in parts of academia is that it’s a great deal easier to do ‘science’ when you are allowed to make up the answers. The "integrative medicine" symposium held at Yale in 2008 boggled the mind. Dr David Katz listed a lot of things he’d tried and which failed to work, His conclusion was not that they should be abandoned, but that we needed a "more fluid concept of evidence". You can see it on YouTube, Senator Tom Harkin’s promotion of NCCAM has done for the U.S. reputation in medicine what Dick Cheney did for the U.S. reputation in torture. It is hard to look at the USA from outside without thinking of the decline and fall of the Roman Empire. One had hoped that era was over with the election of Obama, but the hucksters won’t give up without a fight. They are making too much money to do that. |
Follow-up
The comments that appeared in The Atlantic on this piece were mostly less than enlightening -not quite what one expected of an intellectual magazine. Nevertheless I tried to answer all but the plain abusive comments.
More interesting, though, was an editorial by Jennie Rothenberg Gritz, the Atlantic Senior Editor who asked me to contribute. The Man Who Invented Medical School. It picked up on my mention of Abraham Flexner, and his famous 1910 report [download from Carnegie Foundation] which first put US medial education on a form rational footing. based on science. Now, 100 years later that’s being unpicked both in the USA and here. ms Gritz seemed to think that Flexner would have approved of Dean Ornish. In a response I begged to differ. I’m pretty sure that Felxner would have been furious of he could have seen the reecent march of quackademia, particularly, but not exclusively, in the USA. It is exactly the sort of thing his report set out, successfully, to abolish. He wrote, for example,
“the practitioner is subjected, year in, year out, to the steady bombardment of the unscrupulous manufacturer, persuasive to the uncritical, on the principle that “what I tell you three times is true.” Against bad example and persistent asseveration, only precise scientific concepts and a critical
appreciation of the nature and limits of actual demonstration can protect the young physician.” (Flexner report, 1910, pp 64-65)
It is this very “appreciation of the nature and limits of actual demonstration” that is now being abandoned by the alternative medicine industry. despite the fact that real medicine was in its infancy at the time he w as writing, he was very perceptive about the problems. Perhaps Freedman should read the report.
David Katz seems to have spotted my piece in The Atlantic, and has responded at great length in the Huffington Post (quite appropriate, given the consistent support of HuffPo for nonsense medicine). HuffPo allows only short comments with no links so I’ll reply to him here.
I fear that Dr Katz doth protest a great deal too much. He seems to object to a comment that I made about him in The Atlantic.
“… [He] listed a lot of things he’d tried and which failed to work. His conclusion was not that they should be abandoned, but that we needed a ‘a more fluid concept of evidence.'”
You don’t have to take my word for it. You can take it from the words of Dr Katz.
"What do we do when the evidence we have learned, or if we care to be more provocative, with which we have been indoctrinated, does now fully meet the needs of our patients"
It seems odd to me to regard teaching about how you distinguish what;s true and what isn’t as "indoctrination", though I can understand that knowledge of that subject could well diminish the income of alternative practitioners. You went on to say
"Some years ago the CDC funded us with a million dollars to do what they referred to initially as a systematic review of the evidence base for complementary and alternative medicine, Anybody who’s ever been involved in systematic reviews knows that’s a very silly thing. . . . Well we knew it was silly but a million dollars sounded real [mumbled] took the money and then we figurered we’d figure out what to do with it [smiles broadly]. That’s what we did ". . .
I do hope you told the CDC that you did not spend the million dollars for the sensible purpose for which it was awarded.
This infusion of calcium, magnesium and D vitamins and vitamin C ameliorates the symptoms of fibromyalgia. . . . We did typical placebo controlled randomized double-blind trial for several months . . . we saw an improvement in both our treatment and placebo groups . . .
You then describe how you tested yoga for asthma and homeopathy for attention deficit hyperactivity disorder, Neither of them worked either. Your reaction to this string of failures was just to say “we need a more fluid concept of evidence”
After telling an anecdote about one patient who got better after taking homeopathic treatment you said £I don’t care to get into a discussion of how, or even whether, homeopathy works”. Why not? It seems it doesn’t matter much to you whether the things you sell to patients work or not.
You then went on to describe quite accurately that anti-oxidants don’t work and neither do multivitamin supplements for prevention of cardiovascular problems, And once again you fail to accept the evidence, even evidence you have found yourself. Your response was
“So here too is an invitation to think more fluidly about of evidence. Absence of evidence is not evidence of absence.”
That last statement is the eternal cry of every quack. It’s true, of course, but that does not mean that absence of evidence gives you a licence to invent the answer. But inventing the answer is what you do, time after time, You seem quite incapable of saying the most important thing that anyone in your position should. I don’t know the answer.
Universities, like most businesses, cite glowing testimonials from grateful students, I doubt whether universities are any more honest than anyone else in their choice of what to publish. When I asked to see any letters that had been sent to the university, I was sent only one and extracts from it appear in the last post on Westminster. More dangerous nonsense from the University of Westminster: when will Professor Geoffrey Petts do something about it? But I knew (don’t ask how) that there had been more than that, and a slightly widened FOIA request produced some interesting results (though I’m aware of other letters that were not supplied -not good).
As always, the information came with the caveat
"Copyright in our response to your request belongs to the University of Westminster. All rights are reserved. This document is for personal use only and may not be copied, or stored in any electronic form, or reproduced in any other way or used for any other purpose, either in whole or in part, without the prior written consent of the University of Westminster.".
Why else would anyone ask for information but to make it public? And since the letter was sent in electronic form, it would be hard to comply with the second part. As always, I rely on the fair quotation and public interest defences to quote parts of the letters.
The main players here are Peter Davies (Head of herbal medicine and nutritional therapy), Julie Whitehouse (Course Leader for MSci Herbal Medicine and the BSc Honours Health Sciences), David Peters (Clinical director of Westminster’s School of Integrated Health), and the dean of the School of Life Sciences. Jane Lewis. There’s no woo about Jane Lewis. I suspect she’d have got rid of all the nonsense, given a chance. Who, I wonder, is stopping her?
Julie Whitehouse is, I see, a co-author of Brock et al. (2010) American skullcap (Scutellaria lateriflora): an ancient remedy for today’s anxiety, British Journal of Wellbeing1 (4), 25-30. I had no idea there was such a journal. UCL does not subscribe so if anyone has a reprint I’d love to see it. Judging by the abstract it’s yet more ‘preliminary work’. That’s very typical. Next to no CAM research gets past the preliminary report.
Some testimonials
Here are some quotations from “a part-time student on the herbal medicine (HM) BSc course, currently in my 3rd year of study. I have first class honours degree in ecology, am a qualified staff nurse, and am an experienced performance and business manager."
|
cc Professor Jane Lewis, Dean of School: Biosciences "Dear Professor Petts, I hope you do not mind me writing to you personally. I am a part-time student on the herbal medicine (HM) BSc course, currently in my 3rd year of study. I have first class honours degree in ecology, am a qualified staff nurse, and am an experienced performance and business manager. I regard myself as scientist." "I would like to express to you my disappointment and frustration with my own studies at Westminster. I thought (erroneously, I have since discovered) that I was paying for a Bachelor of Science degree, and that science and scientific thinking would underpin my studies. How wrong I have been. Based on my experience at Westminster, two things really need to be done to restore credibility in the herbal medicine degree, viz. removing the antiscience and pseudoscience, and strengthening the scientific basis of both our core and herbal medicine modules. The current degree is confusing and infuriating in that it really does not know what it is." "Here is a quote from a handout (on ‘The Galenic Constitutional System in Practice’) given to 3rd year herbalists last semester: ‘Treating particular disease/conditions is more successful if the disease can be analysed in terms on hot, cold, wet and dry’. If I showed this to any modern (not 17th century) doctor they would be rolling around on the floor in hysterics and condemning this type of nonsense in the strongest possible language. I am ashamed to tell anybody what we are being taught. Is this clandestine teaching or is the University actually sanctioning this pre-scientific view of medicine?" Anti-science ideas need to be, not only banished from teaching material, but also robustly challenged every time they are raised by students (or lecturers) in the polyclinic or the classroom. But, constantly challenging anti-scientific and erroneous ideas is very wearing and wearying for me as a student, as I am sure it is for scientists on your staff. (I should say here that there are some excellent scientists who have supported and encouraged me in my studies at Westminster; Dr Gillian Shine in the core modules and Christopher Robbins in HM, leap to mind). academic institution. I should not feel threatened by challenging what I am taught when it is plainly pseudoscience or antiscience and my University should be supporting me in my challenge, which I am sure you will. |
And from the same student, this time addressed to Julie Whitehouse and copied to the dean, Jane Lewis (in 2009) [some details removed to preserve patient confidentiality].
|
… a patient attended who had been treated with a Reiki [typo for Reishi] mushroom tincture and another herbal tincture (about 6 herbs) by an HM clinic supervisor. The patient had also been advised to do ‘body brushing’ which I understand was for ‘detoxification’. This lady is being treated by an oncologist for [***] cancer and is currently undergoing chemotherapy. I do not believe her oncology team were informed before we initiated treatment and the bottles of tincture were not labelled with what they contained. I have serious ethical problems with treating anyone with cancer with herbs, but someone in the middle of chemotherapy? Not only are patients’ lives being put at risk, but students are not getting clear messages about the limitations of HM or the professional ethics involved in treating someone with cancer. I have seen patient files with ‘anti-mitotic’ or ‘anti-cancer’ herbs written in the notes. I question whether this is also bordering on the illegal. At the very least it betrays a naive belief that herbs can treat cancer. I was ignored earlier this year when I queried students being encouraged to go to a herbalist’s cancer seminars in Bristol (and she claimed to cure cancer) and this case highlights to me the dangers of Wmin condoning and teaching the ‘we treat people not diseases’ mantra. |
This second letter elicited a response from the university, and the response is worth looking at.
The response
|
2 What was done following the complaint 021209 Clinical Director met with the tutor. Reviewed notes. No indication that the patient was seeking ‘alternatives’ to chemo, nor that she was led to believe the prescription was designed to do other than support her coping with chemo which in her experience had previously been physically demanding and distressing. Procedures regarding communication with oncologists, informed consent, labeling of medicines need reviewing and reinforcing. Action by Course leader/herbal team. Report back to PC Exec 210110 151209 The student who (though she had not been present during this session, had objected to way this case was handled met with the course leader in the presence of the Senior Clinical supervisor and another tutor. The meeting was supportive rather than confrontational. The student was asked to reflect on the consequences of her (frequent) impulsive emailing and the time and effort she demands of others – and to consider the Code of Conduct she has signed. |
So the whistle-blowing student seems to have been patted on the head and told to shut up. Nevertheless the complaint had some effect, though not much.
|
050110 Course leader proposed to review current Polyclinic policies and procedures, and discuss current practice in cases of serious disease and how doctors are informed and patients consented
|
The response included "Extracts from Smith J, Rowan N & Sullivan (2000) Medicinal Mushrooms: Their therapeutic properties and current medical usage with special emphasis on cancer treatment” from Cancer Research UK."
|
In almost all the examples that will be discussed in this chapter the polysaccharides act mainly as immune- stimulants with little or no adverse drug reactions. Furthermore, several of these extracts have been shown to stimulate apoptosis in cancer cells (e.g. Fullerton et al., 2000). While there are examples where the mushroom polysaccharides have shown efficacy against specific types of cancer as monotherapy, the overwhelming successes have been demonstrated when they function together with proven and accepted chemotherapeutic agents.
|
I could not find that document at Cancer Research UK though there is a similar report, dated May 2002, "Medicinal Mushrooms: Their therapeutic properties and current medical usage with special emphasis on cancer treatments" by Smith, Rowan and Sullivan. It can be downloaded at the Cancer Research UK page, Medicinal Mushrooms and Cancer. That page, last updated 7 August 2006, lists John Smith BSc MSc PhD DSc FIBiol FRSE as Emeritus Professor of Applied Microbiology, University of Strathclyde. amd Chief Scientific Officer, MycoBiotech Ltd, Singapore, and Richard Sullivan BSc MD PhD as Head of Clinical Programmes, Cancer Research UK (a job he left in 2008). Professor John Smith is still Chief Scientific Advisor to Mycobiotech Inc, based in Singapore. This company sells various mushroom products. They are all marketed as “nutriceuticals” or “functional foods”, not as pharmaceuticals. These descriptions are a very common way of making medicinal claims for products, while describing them as foods to avoid the strict regulations about claims made for medicines.
It does not seem to me to be a good idea for Cancer Research UK to have advice on its web site from someone with a very obvious financial interest.
The quotations from the Smith report are obviously intended to defend the practice of prescribing mushrooms to people on chemotherapy. But the fact that in 2011, five years after the CRUK page, Mycobiotech still has no approved medicine approved for cancer speaks for itself. They sell Shiitake Herbal Soups. They also sell Essence of Shiitake which, they say, contains Lentinan, “which has been confirmed through research, to be an immuno-enhancer. Lentinan has been found to reduce tumour growth and to prolong the life of cancer patients”. That sounds to me like a rather strong medicinal claim for a “food”. Even Nutra-ingredients, the industry site for nutriceuticals, doesn’t claim much for it.
Now back to Westminster’s response to the student’s complaint.
|
I have found no evidence that herbal practitioners in the Polyclinic are making explicit claims to treat cancer. |
And, from David Peters.
|
DP**There is one item in the notes however which I think we need to comment on. While the paper-trail in all other respects shows that the herbal prescription was supportive, one herb in the prescription is categorised as ‘anti-tumour’. Although I am convinced after reviewing the notes and talking with the tutor involved, that the aim was to support the patient through her chemotherapy, this part of the prescription nonetheless signifies some ambivalence at least, about whether the aim was or was not to treat cancer
|
But then, from Julie Whitehouse
|
JW Yes there is antitumour as an action for many herbs and nutritional components – and several relevant actions including anything as general as anti- oxidant even – it doesn’t mean we are suggesting they are being used as treatment
|
It doesn’t take much reading between the lines to see the tension between Whitehouse and Peters. The former is very reluctant to give up the myths, the latter is slightly more cautious about claims to treat cancer.
Let’s be clear about one thing. The student was dead right. There is so little reliable information about mushrooms that neither Cochrane Reviews nor NCCAM has anything relevant to say about them. Antioxidants are a myth, much beloved by marketing people and "boosting the immune system" is the universal mantra of every advocate of magic medicine when they can’t think of anything else to make up. Why can’t Peters and Whitehouse admit it?
More complaints
This one is from a member of staff who teaches on the herbal medicine course. It was addressed to Julie Whitehouse and copied to the dean and vice-chancellor.(10 July 2009).
|
"During last week (5-9th May) I witnessed a member of the Herbal Team and a student dowsing with a pendulum to divine herbal drugs to prescribe for the student. When I approached and spoke, they defensively hid the pendulum and were clearly embarrassed. I discussed what they were doing. They freely said they were prescribing herbal medicine and cited other staff as their ‘authority’ and ‘instructors’. Diagnosing or prescribing by pendulum has no scientific credibility. Further, it is dangerous for prescribing as it both fails to identify any appropriate drugs (except by chance) and may select dangerous drugs for a patient. I know other staff have raised with you the teaching or use of such mediaeval and unscientific practices on the Wmin HM course." "I feel that such practice in the HM Course teaching or in the Polyclinic should be proscribed. I would like to suggest that you address and resolve this matter urgently. Dowsing is in conflict with the VC’s recent letter to SIH staff, specifically expecting more evidence of science within the teaching of CT Courses." "I expect that were the Department of Health to be aware of the unscientific teaching and promotion of practices like dowsing, (and crystals, iridology, astrology, and tasting to determine pharmacological qualities of plant extracts) on the Wmin HM Course, progress towards the Statutory Regulation of Herbal Medicine could be threatened." |
The writer seems to have overestimated the sense in the Department of Health. They were aware of these practices (I told them) but nevertheless went ahead with a silly form of statutory regulation.
The same lecturer wrote on 27 July 2009
|
"This happened with a supervisor, students and patient in the consultation room. The patient was invited to dowse her own "remedies" using a pendulum. A set of Bach Flower remedies (also proscribed in the HM Clinics) was placed in front of the patient and a pendulum was produced. On the basis of the dowsing, a prescription of ‘remedies’ was dispensed." "Although Julie says dowsing has been proscribed, she has been unable to present and document saying as such. Bach Flower Remedies have been proscribed for HM Clinics." |
Some of the replies were sent to me. Julie Whitehouse replied to the lecturer and Peter Davies on 10 August 2009
|
“I have written and circulated the text to be put into the handbook and have had approval from most members of the herbal team – but [the lecturer who complained] was not there at the time – hope he approves of the statement. It does not specifically say we do not dowse – but it does I think state clearly what we do – we surely do not want a list of what we don’t do – where would it end – there could be many things in a list of what we don’t do.”
|
So she explicitly refused to ban the use of dowsing in Westminster’s clinic. The lecturer replied, pointing out the unreasonableness of this attitude.
|
Dear Julie, I am afraid that I have not received any copy (home or University) of your ‘statement’ so cannot comment. Please resend me another copy. I don’t understand your not wanting ‘a list of what we don’t do – where would it end’. It is commonplace to have proscribed activities in both social and professional activities, and these are usually for clear reasons of safety and public good. Eg.: Herbal practice is constrained by the prohibitions in the Medicines Act 1968 and following, the maximum dosages under Schedule III of that Act, the prohibited herbal drugs under the MCA, Trading Standards regulations, etc. |
It seems that, despite the vice-chancellor’s assurance that the courses would become more scientific, there are still apologists for diagnosis with a pendulum, and for treating cancer with mushrooms at Westminster University.
This saga sounds only top characteristic. Complaints through official channels usually get you nowhere with big organisations. Sadly, the only way to get change is public embarrassment.
Some action from Vice-chancellor Geoftrey Petts is long overdue.
Follow-up
A kind reader sent me a copy of Brock, Whitehouse, Tewfik & Towell,. (2010) American skullcap (Scutellaria lateriflora): an ancient remedy for today’s anxiety, British Journal of Wellbeing1 (4), 25-30.. This is the paper that I described above, on the basis of the abstract, as "preliminary study".. Now that I’ve seen it I realise it isn’t study at all. They simply emailed 377 members of the National Institute of Medical Herbalists to ask what they thought of S. laterifloria. Only 62 replied (16%) and their anecdotes are listed in the paper. It is this sort of worthless information that gets herbal medicine a bad name.
10 August 2011. I notice that Professor Petts has replied to a letters sent to him by the Nightingale Collaboration. He said “Whilst I understand your concerns, colleagues of the School of Life Sciences where these courses are offered do not share them. They are not teaching pseudo-science, as you claim,…”. Well I know at least two member of the Life Sciences department who are very worried. One has now left and one has retired. The rest are presumably too scared to speak out. How he has the nerve to claim that they don’t teach pseudo-science all the teaching materials that have been revealed on this blog is hard to imagine. It is simply not true and he must know it. I find it deeply worrying when vice-chancellors say things which they know to be untrue.
The latest example to come to light is cited by Andy Lewis on his Quackometer blog
“There are some even odder characters too, such as Roy Riggs B.Sc who descibes himself as a “Holistic Geobiologist” and is “an “professional Earth Energy dowser”. He guest lectures at the London Westminster University’s School of Integrative Medicine and The Baltic Dowser’s Association of Lithuania.”
I do wonder who Professor Petts thinks he’s fooling.
One wonders about the standards of peer review at the British Journal of General Practice. The June issue has a paper, "Acupuncture for ‘frequent attenders’ with medically unexplained symptoms: a randomised controlled trial (CACTUS study)". It has lots of numbers, but the result is very easy to see. Just look at their Figure.
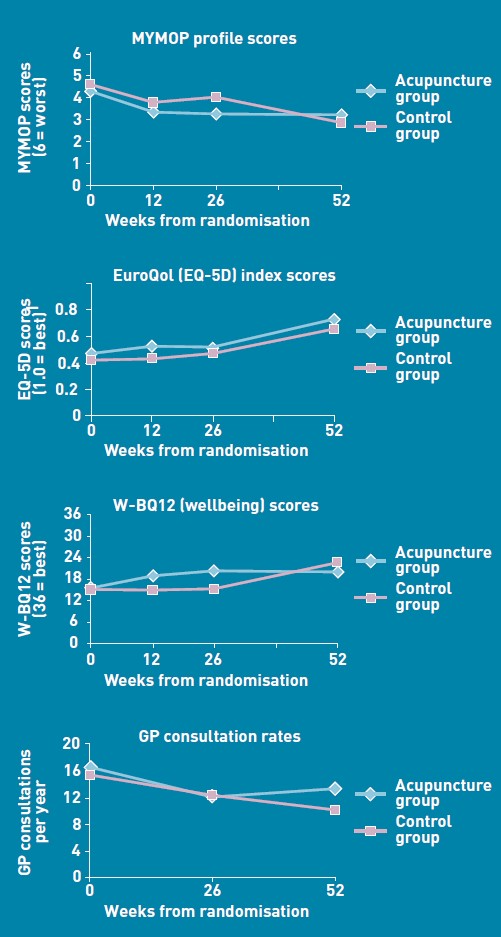
There is no need to wade through all the statistics; it’s perfectly obvious at a glance that acupuncture has at best a tiny and erratic effect on any of the outcomes that were measured.
But this is not what the paper said. On the contrary, the conclusions of the paper said
|
Conclusion The addition of 12 sessions of five-element acupuncture to usual care resulted in improved health status and wellbeing that was sustained for 12 months. |
How on earth did the authors manage to reach a conclusion like that?
The first thing to note is that many of the authors are people who make their living largely from sticking needles in people, or advocating alternative medicine. The authors are Charlotte Paterson, Rod S Taylor, Peter Griffiths, Nicky Britten, Sue Rugg, Jackie Bridges, Bruce McCallum and Gerad Kite, on behalf of the CACTUS study team. The senior author, Gerad Kite MAc , is principal of the London Institute of Five-Element Acupuncture London. The first author, Charlotte Paterson, is a well known advocate of acupuncture. as is Nicky Britten.
The conflicts of interest are obvious, but nonetheless one should welcome a “randomised controlled trial” done by advocates of alternative medicine. In fact the results shown in the Figure are both interesting and useful. They show that acupuncture does not even produce any substantial placebo effect. It’s the authors’ conclusions that are bizarre and partisan. Peer review is indeed a broken process.
That’s really all that needs to be said, but for nerds, here are some more details.
How was the trial done?
The description "randomised" is fair enough, but there were no proper controls and the trial was not blinded. It was what has come to be called a "pragmatic" trial, which means a trial done without proper controls. They are, of course, much loved by alternative therapists because their therapies usually fail in proper trials. It’s much easier to get an (apparently) positive result if you omit the controls. But the fascinating thing about this study is that, despite the deficiencies in design, the result is essentially negative.
The authors themselves spell out the problems.
“Group allocation was known by trial researchers, practitioners, and patients”
So everybody (apart from the statistician) knew what treatment a patient was getting. This is an arrangement that is guaranteed to maximise bias and placebo effects.
"Patients were randomised on a 1:1 basis to receive 12 sessions of acupuncture starting immediately (acupuncture group) or starting in 6 months’ time (control group), with both groups continuing to receive usual care."
So it is impossible to compare acupuncture and control groups at 12 months, contrary to what’s stated in Conclusions.
"Twelve sessions, on average 60 minutes in length, were provided over a 6-month period at approximately weekly, then fortnightly and monthly intervals"
That sounds like a pretty expensive way of getting next to no effect.
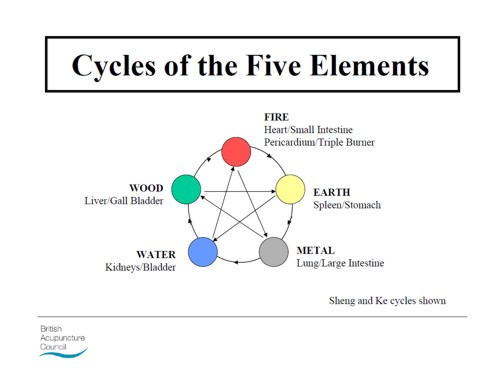
"All aspects of treatment, including discussion and advice, were individualised as per normal five-element acupuncture practice. In this approach, the acupuncturist takes an in-depth account of the patient’s current symptoms and medical history, as well as general health and lifestyle issues. The patient’s condition is explained in terms of an imbalance in one of the five elements, which then causes an imbalance in the whole person. Based on this elemental diagnosis, appropriate points are used to rebalance this element and address not only the presenting conditions, but the person as a whole".
Does this mean that the patients were told a lot of mumbo jumbo about “five elements” (fire earth, metal, water, wood)? If so, anyone with any sense would probably have run a mile from the trial.
"Hypotheses directed at the effect of the needling component of acupuncture consultations require sham-acupuncture controls which while appropriate for formulaic needling for single well-defined conditions, have been shown to be problematic when dealing with multiple or complex conditions, because they interfere with the participative patient–therapist interaction on which the individualised treatment plan is developed. 37–39 Pragmatic trials, on the other hand, are appropriate for testing hypotheses that are directed at the effect of the complex intervention as a whole, while providing no information about the relative effect of different components."
Put simply that means: we don’t use sham acupuncture controls so we can’t distinguish an effect of the needles from placebo effects, or get-better-anyway effects.
"Strengths and limitations: The ‘black box’ study design precludes assigning the benefits of this complex intervention to any one component of the acupuncture consultations, such as the needling or the amount of time spent with a healthcare professional."
"This design was chosen because, without a promise of accessing the acupuncture treatment, major practical and ethical problems with recruitment and retention of participants were anticipated. This is because these patients have very poor self-reported health (Table 3), have not been helped by conventional treatment, and are particularly desperate for alternative treatment options.".
It’s interesting that the patients were “desperate for alternative treatment”. Again it seems that every opportunity has been given to maximise non-specific placebo, and get-well-anyway effects.
There is a lot of statistical analysis and, unsurprisingly, many of the differences don’t reach statistical significance. Some do (just) but that is really quite irrelevant. Even if some of the differences are real (not a result of random variability), a glance at the figures shows that their size is trivial.
My conclusions
(1) This paper, though designed to be susceptible to almost every form of bias, shows staggeringly small effects. It is the best evidence I’ve ever seen that not only are needles ineffective, but that placebo effects, if they are there at all, are trivial in size and have no useful benefit to the patient in this case..
(2) The fact that this paper was published with conclusions that appear to contradict directly what the data show, is as good an illustration as any I’ve seen that peer review is utterly ineffective as a method of guaranteeing quality. Of course the editor should have spotted this. It appears that quality control failed on all fronts.
Follow-up
In the first four days of this post, it got over 10,000 hits (almost 6,000 unique visitors).
Margaret McCartney has written about this too, in The British Journal of General Practice does acupuncture badly.
The Daily Mail exceeds itself in an article by Jenny Hope whch says “Millions of patients with ‘unexplained symptoms’ could benefit from acupuncture on the NHS, it is claimed”. I presume she didn’t read the paper.
The Daily Telegraph scarcely did better in Acupuncture has significant impact on mystery illnesses. The author if this, very sensibly, remains anonymous.
Many “medical information” sites churn out the press release without engaging the brain, but most of the other newspapers appear, very sensibly, to have ignored ther hyped up press release. Among the worst was Pulse, an online magazine for GPs. At least they’ve publish the comments that show their report was nonsense.
The Daily Mash has given this paper a well-deserved spoofing in Made-up medicine works on made-up illnesses.
“Professor Henry Brubaker, of the Institute for Studies, said: “To truly assess the efficacy of acupuncture a widespread double-blind test needs to be conducted over a series of years but to be honest it’s the equivalent of mapping the DNA of pixies or conducting a geological study of Narnia.” ”
There is no truth whatsoever in the rumour being spread on Twitter that I’m Professor Brubaker.
Euan Lawson, also known as Northern Doctor, has done another excellent job on the Paterson paper: BJGP and acupuncture – tabloid medical journalism. Most tellingly, he reproduces the press release from the editor of the BJGP, Professor Roger Jones DM, FRCP, FRCGP, FMedSci.
"Although there are countless reports of the benefits of acupuncture for a range of medical problems, there have been very few well-conducted, randomised controlled trials. Charlotte Paterson’s work considerably strengthens the evidence base for using acupuncture to help patients who are troubled by symptoms that we find difficult both to diagnose and to treat."
Oooh dear. The journal may have a new look, but it would be better if the editor read the papers before writing press releases. Tabloid journalism seems an appropriate description.
Andy Lewis at Quackometer, has written about this paper too, and put it into historical context. In Of the Imagination, as a Cause and as a Cure of Disorders of the Body. “In 1800, John Haygarth warned doctors how we may succumb to belief in illusory cures. Some modern doctors have still not learnt that lesson”. It’s sad that, in 2011, a medical journal should fall into a trap that was pointed out so clearly in 1800. He also points out the disgracefully inaccurate Press release issued by the Peninsula medical school.
Some tweets
Twitter info 426 clicks on http://bit.ly/mgIQ6e alone at 15.30 on 1 June (and that’s only the hits via twitter). By July 8th this had risen to 1,655 hits via Twitter, from 62 different countries,
@followthelemur Selina
MASSIVE peer review fail by the British Journal of General Practice http://bit.ly/mgIQ6e (via @david_colquhoun)
@david_colquhoun David Colquhoun
Appalling paper in Brit J Gen Practice: Acupuncturists show that acupuncture doesn’t work, but conclude the opposite http://bit.ly/mgIQ6e
Retweeted by gentley1300 and 36 others
@david_colquhoun David Colquhoun.
I deny the Twitter rumour that I’m Professor Henry Brubaker as in Daily Mash http://bit.ly/mt1xhX (just because of http://bit.ly/mgIQ6e )
@brunopichler Bruno Pichler
http://tinyurl.com/3hmvan4 Made-up medicine works on made-up illnesses (me thinks Henry Brubaker is actually @david_colquhoun)
@david_colquhoun David Colquhoun,
HEHE RT @brunopichler: http://tinyurl.com/3hmvan4 Made-up medicine works on made-up illnesses
@psweetman Pauline Sweetman
Read @david_colquhoun’s take on the recent ‘acupuncture effective for unexplained symptoms’ nonsense: bit.ly/mgIQ6e
@bodyinmind Body In Mind
RT @david_colquhoun: ‘Margaret McCartney (GP) also blogged acupuncture nonsense http://bit.ly/j6yP4j My take http://bit.ly/mgIQ6e’
@abritosa ABS
Br J Gen Practice mete a pata na poça: RT @david_colquhoun […] appalling acupuncture nonsense http://bit.ly/j6yP4j http://bit.ly/mgIQ6e
@jodiemadden Jodie Madden
amusing!RT @david_colquhoun: paper in Brit J Gen Practice shows that acupuncture doesn’t work,but conclude the opposite http://bit.ly/mgIQ6e
@kashfarooq Kash Farooq
Unbelievable: acupuncturists show that acupuncture doesn’t work, but conclude the opposite. http://j.mp/ilUALC by @david_colquhoun
@NeilOConnell Neil O’Connell
Gobsmacking spin RT @david_colquhoun: Acupuncturists show that acupuncture doesn’t work, but conclude the opposite http://bit.ly/mgIQ6e
@euan_lawson Euan Lawson (aka Northern Doctor)
Aye too right RT @david_colquhoun @iansample @BenGoldacre Guardian should cover dreadful acupuncture paper http://bit.ly/mgIQ6e
@noahWG Noah Gray
Acupuncturists show that acupuncture doesn’t work, but conclude the opposite, from @david_colquhoun: http://bit.ly/l9KHLv
8 June 2011 I drew the attention of the editor of BJGP to the many comments that have been made on this paper. He assured me that the matter would be discussed at a meeting of the editorial board of the journal. Tonight he sent me the result of this meeting.
|
Subject: BJGP Dear Prof Colquhoun We discussed your emails at yesterday’s meeting of the BJGP Editorial Board, attended by 12 Board members and the Deputy Editor The Board was unanimous in its support for the integrity of the Journal’s peer review process for the Paterson et al paper – which was accepted after revisions were made in response to two separate rounds of comments from two reviewers and myself – and could find no reason either to retract the paper or to release the reviewers’ comments Some Board members thought that the results were presented in an overly positive way; because the study raises questions about research methodology and the interpretation of data in pragmatic trials attempting to measure the effects of complex interventions, we will be commissioning a Debate and Analysis article on the topic. In the meantime we would encourage you to contribute to this debate throught the usual Journal channels Roger Jones Professor Roger Jones MA DM FRCP FRCGP FMedSci FHEA FRSA |
It is one thing to make a mistake, It is quite another thing to refuse to admit it. This reply seems to me to be quite disgraceful.
20 July 2011. The proper version of the story got wider publicity when Margaret McCartney wrote about it in the BMJ. The first rapid response to this article was a lengthy denial by the authors of the obvious conclusion to be drawn from the paper. They merely dig themselves deeper into a hole. The second response was much shorter (and more accurate).
|
Thank you Dr McCartney Richard Watson, General Practitioner The fact that none of the authors of the paper or the editor of BJGP have bothered to try and defend themselves speaks volumes. Like many people I glanced at the report before throwing it away with an incredulous guffaw. You bothered to look into it and refute it – in a real journal. That last comment shows part of the problem with them publishing, and promoting, such drivel. It makes you wonder whether anything they publish is any good, and that should be a worry for all GPs. |
30 July 2011. The British Journal of General Practice has published nine letters that object to this study. Some of them concentrate on problems with the methods. others point out what I believe to be the main point, there us essentially no effect there to be explained. In the public interest, I am posting the responses here [download pdf file]
Thers is also a response from the editor and from the authors. Both are unapologetic. It seems that the editor sees nothing wrong with the peer review process.
I don’t recall ever having come across such incompetence in a journal’s editorial process.
Here’s all he has to say.
|
The BJGP Editorial Board considered this correspondence recently. The Board endorsed the Journal’s peer review process and did not consider that there was a case for retraction of the paper or for releasing the peer reviews. The Board did, however, think that the results of the study were highlighted by the Journal in an overly-positive manner. However,many of the criticisms published above are addressed by the authors themselves in the full paper.
|
If you subscribe to the views of Paterson et al, you may want to buy a T-shirt that has a revised version of the periodic table.
5 August 2011. A meeting with the editor of BJGP
Yesterday I met a member of the editorial board of BJGP. We agreed that the data are fine and should not be retracted. It’s the conclusions that should be retracted. I was also told that the referees’ reports were "bland". In the circumstances that merely confirmed my feeling that the referees failed to do a good job.
Today I met the editor, Roger Jones, himself. He was clearly upset by my comment and I have now changed it to refer to the whole editorial process rather than to him personally. I was told, much to my surprise, that the referees were not acupuncturists but “statisticians”. That I find baffling. It soon became clear that my differences with Professor Jones turned on interpretations of statistics.
It’s true that there were a few comparisons that got below P = 0.05, but the smallest was P = 0.02. The warning signs are there in the Methods section: "all statistical tests were …. deemed to be statistically significant if P < 0.05". This is simply silly -perhaps they should have read Lectures on Biostatistics. Or for a more recent exposition, the XKCD cartoon in which it’s proved that green jelly beans are linked to acne (P = 0.05). They make lots of comparisons but make no allowance for this in the statistics. Figure 2 alone contains 15 different comparisons: it’s not surprising that a few come out "significant", even if you don’t take into account the likelihood of systematic (non-random) errors when comparing final values with baseline values.
Keen though I am on statistics, this is a case where I prefer the eyeball test. It’s so obvious from the Figure that there’s nothing worth talking about happening, it’s a waste of time and money to torture the numbers to get "significant" differences. You have to be a slavish believer in P values to treat a result like that as anything but mildly suggestive. A glance at the Figure shows the effects, if there are any at all, are trivial.
I still maintain that the results don’t come within a million miles of justifying the authors’ stated conclusion “The addition of 12 sessions of five-element acupuncture to usual care resulted in improved health status and wellbeing that was sustained for 12 months.” Therefore I still believe that a proper course would have been to issue a new and more accurate press release. A brief admission that the interpretation was “overly-positive”, in a journal that the public can’t see, simply isn’t enough.
I can’t understand either, why the editorial board did not insist on this being done. If they had done so, it would have been temporarily embarrassing, certainly, but people make mistakes, and it would have blown over. By not making a proper correction to the public, the episode has become a cause célèbre and the reputation oif the journal will suffer permanent harm. This paper is going to be cited for a long time, and not for the reasons the journal would wish.
Misinformation, like that sent to the press, has serious real-life consequences. You can be sure that the paper as it still stands, will be cited by every acupuncturist who’s trying to persuade the Department of Health that he’s a "qualified provider".
There was not much unanimity in the discussion up to this point, Things got better when we talked about what a GP should do when there are no effective options. Roger Jones seemed to think it was acceptable to refer them to an alternative practitioner if that patient wanted it. I maintained that it’s unethical to explain to a patient how medicine works in terms of pre-scientific myths.
I’d have love to have heard the "informed consent" during which "The patient’s condition is explained in terms of imbalance in the five elements which then causes an imbalance in the whole person". If anyone had tried to explain my conditions in terms of my imbalance in my Wood, Water, Fire, Earth and Metal. I’d think they were nuts. The last author. Gerad Kite, runs a private clinic that sells acupuncture for all manner of conditions. You can find his view of science on his web site. It’s condescending and insulting to talk to patients in these terms. It’s the ultimate sort of paternalism. And paternalism is something that’s supposed to be vanishing in medicine. I maintained that this was ethically unacceptable, and that led to a more amicable discussion about the possibility of more honest placebos.
It was good of the editor to meet me in the circumstances. I don’t cast doubt on the honesty of his opinions. I simply disagree with them, both at the statistical level and the ethical level.
30 March 2014
I only just noticed that one of the authors of the paper, Bruce McCallum (who worked as an acupuncturist at Kite’s clinic) appeared in a 2007 Channel 4 News piece. I was a report on the pressure to save money by stopping NHS funding for “unproven and disproved treatments”. McCallum said that scientific evidence was needed to show that acupuncture really worked. Clearly he failed, but to admit that would have affected his income.
Watch the video (McCallum appears near the end).
We live under a highly ideological government. It wishes to privatise everything in sight, not least universities and the National Health Service. Of course they don’t put it that way: they call it “reform”. It’s easier to deal with open ideology than with ideology disguised as social reform, but luckily a 10-year old could see through the weasel words.
One example is the raising of tuition fees to £9,000 pa. It costs the taxpayers more than charging £3,000 did. Students obviously lose, and universities probably lose too. It takes a very blind form of ideology to devise a system in which all three parties lose money, for the sake of a principle.
No doubt Education Minister David Willetts was moved by the same ideological considerations to grant "BPP University" the status of University College in 2010 (three years after it was given degree-awarding powers). BPP became part of the international education giant for-profit Apollo Group last year. It is the first private institution to be awarded the title since the University College at Buckingham – now the University of Buckingham
It did not seem to worry Willetts that Apollo has a rather dodgy reputation. Apollo had an appeal for a conviction for securities fraud turned down in 2011. The company was found to have withheld a critical report from the US Department for Education from its shareholders. It has already paid around £8m to the government and is due to reimburse its investors around £130m. Apollo’s chief executive Charles Edelstein, is paid $6m (including bonuses and share options). That makes UCL’ provost’s salary of £400,000 look like poverty.. See also BPP’s parent company ‘deceives’ prospective students, in the Solicitor’s Journal.
In the UK the activities of BPP will be regulated by the QAA. That’s a bad sign too. The QAA has failed totally to prevent degrees in rubbish being awarded in UK universities. It is a totally ineffective box-ticking quango that costs a lot of money but id doesn’t ensure quality. On the contrary. the QAA actually harms quality by endorsing some terrible courses. For example, it endorsed the Malaysian business school as recounted in a BBC Wales television programme A young reporter has better investigative ability than Willetts, the government and the QAA. See the programme on YouTube: (Part 1, and Part 2 ).
The QAA, also endorses private courses at the McTimoney Chiropractic College, which is owned by, guess who, BPP. This college awards degrees that are accredited by the University of Wales, an institution that accredits just about anything if paid a large fee (and will probably vanish soon). This is something I revealed in 2008. See Another worthless validation: the University of Wales and nutritional therapy. Also the follow up posts,
The McTimoney Chiropractic Association would seem to believe that chiropractic is “bogus” in 2009, and, especially,
Scandal of the University of Wales and the Quality Assurance Agency (2010).
The story has now appeared in Private Eye, in the Education Round-up section. That section doesn’t appear on their web site, but since I was able to help them a bit with the story, i hope they won’t mind if I reproduce it here.
|
Pet subjects
If for-profit law and business school BPP wants to avoid questions about the legitimacy of the courses it offers, what is it doing offering courses in chiropractic treatment for… pets? The question arises as calls are growing for better regulation of the· for-profit higher education sector as a whole. This month, for example, the Higher Education Policy Institute (HEPI) think tank landed a further blow against the government’s wish to bring in more private universities, law schools, bible colleges and business schools, with a damning report which drew further attention to the "questionable legitimacy or very poor quality" of for-profit education in the United States. Two US firms, Apollo Group (which owns BPP College) and Kaplan, were lambasted following an investigation by the US Government Accountability Office; yet both are already involved in UK private education and looking to expand rapidly (see Eyes 1272 & 1275). Last month Betty Huff, president of the American Association of Collegiate Registrars and Admissions Officers, told a conference of university chiefs in Nottingham about problems caused by the rapid expansion of private providers in the US, citing one nursing college in California which had charged $60,000 for courses which left graduates unqualified for nursing work. Despite these concerns, when universities minister David Willetts recently doubled the student loans available to those attending private institutions, he said he wanted "to encourage a more open, dynamic and diverse higher education system, with new alternative providers". BPP College, Britain’s second for-profit degree-awarding university, operates law and business schools in eight English cities, as well as the McTimoney College of Chiropractic in Abingdon, Oxfordshire. Despite BPP’s degree-awarding powers, McTimoney’s degrees are currently validated by the University of Wales, which notoriously validated degrees from Malaysia’s Fazley Business School, whose former pop star boss claimed qualifications from a sham business school, and Danish and American evangelical institutions, against the advice of the UK’s Quality Assurance Agency (Eye 1282). If the scientific evidence for many of chiropractic’s claims in human medicine is feeble, good studies supporting veterinary chiropractic are non-existent. Nevertheless the college has devised two-year MSc courses in chiropractic for small animals and in animal manipulation -"currently unique in Europe, in that It is the only externally validated Masters level course that trains students in Animal Manipulation." Is that the kind of alternative provider Willetts really wants to encourage |
Follow-up
The University of Wales continues to engage in make-believe, despite all the criticism. Just after this post gone public I noticed Bursary fulfils dreams for students of McTimoney College of Chiropractic. They haven’t noticed that the University of Wales accreditation procedures are utterly discredited and that chiropractic has imploded in the wake of the Simon Singh affair.
More on Apollo. A devastating essay on BPP, by Howard Hotson, has appeared in the London Review of Books. Of the parent company, Apollo, Hotson writes
“In 2006 the company’s controller and chief accounting officer resigned amid allegations that the books had been cooked; in 2007, the Nasdaq Listing and Hearing Review Council threatened to withdraw Apollo’s listing from the stock exchange; in 2008, a US federal jury in Arizona found Apollo guilty of ‘knowingly and recklessly’ misleading investors, and instructed the group to pay shareholders some $280 million in reparations. Apollo appealed, but the appeal was rejected by the US Supreme Court on 8 March this year.”
If David Willetts did not know about this, he should have done. If he did know about it, he must be a far-right idealogue beyond comprehension.
The Economist cites Private Eye and this blog in Badmouthing BPP. It concludes that
It seems unlikely that the government would do anything as drastic as withdrawing BPP’s degree-awarding powers. But for a business school, reputation counts. It will hope the murmurs die out quickly.
That seems to me to let them off the hook much too easily.
Daily Mirror (1 June) reports Secret government talks with US private education firms sparks fears of uni privatisations.
An analogy with abuse at Winterbourne View?. Shortly after this news, the BBC’s Panorama programme revealed shocking abuse of patients with learning difficulties at a care home. The ‘care home;’ is owned by a private company, Castlebeck. The company charges the taxpayer arounf £3,500 per week. Care homes have their own box-ticking quango, the Care Quality Commission (CQC), with a very-respectable-sounding chair, Dame Jo Williams. The CQC failed to respond to a whistleblowers report. They seem to be as useless as the Quality Assurance Agency (QAA) for universities. These expensive regulators are not just ineffective, but do positive harm, by endorsing nonsense. They tick boxes, but they don’t use their brains and above all, they don’t look properly. Complaining to them will generally get you absolutely nowhere. Their somnolent members prefer the quiet life it seems. Andrew Lansely wants more private companies like Castlebeck in the NHS, just as David Willetts wants more people like "BPP University".in the education system. I don’t.
In the NHS, alarming cases like this have not always occurred in the private sector, As far as I know there are no numbers. It can’t help that both BPP’s and Castlebeck’s aim is to make money.
One of my first posts about nonsense taught in universities was about the University of Westminster (April 2008): Westminster University BSc: “amethysts emit high yin energy”. since then, there have been several more revelations.
 Professor Petts |
The vice-cnancellor of Westminster, Professor Geoffrey Petts, with whom the buck stops, did have an internal review but its report was all hot air and no action resulted (see A letter to the Times, and Progress at Westminster). That earned Professor Petts an appearence in Private Eye Crystal balls. Professor Petts in Private Eye (and it earned me an invitation to a Private Eye lunch, along with Francis Wheen, Charlie Booker, Ken Livingstone . . ). It also earned Petts an appearence in the Guardian (The opposite of science). |
By that time Salford University had closed down all its CAM, and the University of Central Lancashire was running an honest internal review which resulted in closure of (almost) all of their nonsense degrees. But Westminster proved more resistant to sense and, although they closed down homeopathy, they still remain the largest single provider of degrees in junk medicine. See, for example More make-believe from the University of Westminster. This time it’s Naturopathy, and
The last BSc (Hons) Homeopathy closes! But look at what they still teach at Westminster University.
It’s interesting that Westminster always declined to comply with Freedom of Information requests, yet I had more from them than from most places. All the information about what’s taught at Westminster came from leaks from within the university. Westminster has more moles than a suburban garden. They were people with conscience who realised that the university was harming itself. They would claim that they were trying to save the university from some remarkably bad management. I claim also that I’m working in the interests of the university.
In the wake of the victory at the Information Tribunal, I sent a Freedom of Information Act (FOIA) request for for samples of teaching materials from all of their courses. This time they couldn’t legally refuse. The first batch has just arrived, so here are a few selected gems of utter nonsense. Well, it is worse than nonsense because it endangers the health of sick people.
A letter to the university from a student
Before getting on to the slides, here’s a letter that was supplied under FOIA. It was sent anonymously to the university. I was told that this was the only letter of complaint but I happen to know that’s not true so I’ve asked again. This one was forwarded to the vice-chancellor in 2008, and to the review committee. Both seem to have ignored it. Judging from the wording, one would guess that it came from one of their own undergraduates. :Here are some extracts.[download whole letter]
|
It is a flagrant contradiction of a ‘science’ in the BSc to have these practices, but it also jeopardises our profession, which is under DoH review and being constantly attacked in the media Gustifiable I suggest). We are taught that simply tasting plant tinctures can tell us which part of the body they work. on and what they do in the body. We are given printed charts with an outline of the body on to record our findings on. This is both nonsense, but is dangerous as it implies that the pharmacology of plant tinctures can be divined by taste alone. In class we are taught that we can divine the drug actions or use of an unknown plant simply by tasting an alcohol extract. Science? or dangerous fantasy. There are lecturers taking clinics who allow students to dowse and partake themselves in dowsing or pendulums to diagnose and even to test suitability of plant drugs. Dowsing is taught to us by some lecturers and frowned upon by others but we feel it brings the herbal medicine into a poor light as it is unscientific and bogus nonsense. We are concerned that we have seen the course leader brush over this practice as though she is frightened to make a stand. |
The letter seems to refer to a course in herbal medicine. That is a subject that could be studied scientifically, though to do so would leave students unemployed because so few herbal treatments have been shown to work. It obviously is not being studied scientifically: but even teaching students about dowsing and pendulums does not seem to have stirred the vice-chancellor into action.
David Peters: wishful thinking?
David Peters is a nice man. He’s the Clinical Director of Westminster’s School of Integrated Health. I debated with him on the excellent Radio 4 Programme, Material World.
His lecture on "Complementary Healthcare in the NHS" showed some fine wishful thinking.
It shows the progress of the euphemisms that quacks use to try to gain respectability, but little else. Interestingly, later slides show a bit more realism.
So he has noticed that the tide has turned and that a lot of people are no longer willing to be palmed off with new age gobbledygook. And yes, courses are shutting. Perhaps his course will be the next to shut?
According to an internal Westminster email that found its way to me,
The following courses have been closed/identified for closure due to poor recruitment :
- BSc degrees in Homeopathy and Remedial Massage & Neuromuscular Therapy, students completing by September 2011
- MA degrees in International Community development, Community development and Faith-based Community development, students completing by September 2011
- BSc degree Complementary Medicine
- Graduate diploma BMS
The following courses have been identified as ‘at risk’ (School definition) and will be discussed at the APRG and University Review Group2, due to poor recruitment and high cost of delivery:
- Integrated Health Scheme: BSc Complementary Medicine, Naturopathy; BSc Chinese Medicine; BSc Nutritional Therapy; BSc Herbal Medicine
The BSc (Hons) degree in naturopathy
Naturopathy us pretty bizarre, because it consists largely of doing nothing at all, beyond eating vegetables . Being ill is good for you.
Perhaps the best source to judge claims is the US National Center for Complementary and Alternive Medicine (NCCAM), a branch of the National Institutes of Health. This is the outfit that has spent over a billion dollars of US taxpayers’ money testing alternative medicines and for all that money has not come up with a single useful treatment. They never link to any sort of critical comment, and are nothing if not biassed towards all things alternative. If they can’t come up with evidence. nobody can. Two useful links to NCCAM are Herbs at a glance, and Health Topics A – Z.
Uses of herbal teas in naturopathic dietary care
I was sent a set of over 50 slides on "Herbal Teas/Decoctions (3CMWS03, 1/02, Uses of herbal teas in naturopathic dietary care). About half of them amount to little more than ‘how to make a cup of tea’. but then we get onto uses, but then a lot of fantasy ensues.
What NNCAM says about dandelion. There is no compelling scientific evidence for using dandelion as a treatment for any medical condition.
What Westminster says
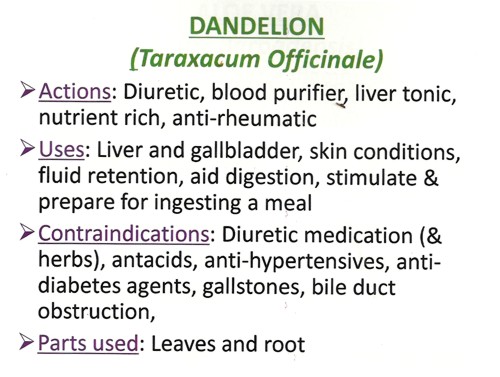
Well I know what a diuretic is, but "blood purifier" and "liver tonic" are meaningless gobbledygook. We’ve been through this before with Red Clover (see Michael Quinion’s .look at the term "blood cleanser"). Using words like them is the very opposite of education.
What NCCAM says.about chamomile: Chamomile has not been well studied in people so there is little evidence to support its use for any condition.
What Westminster says
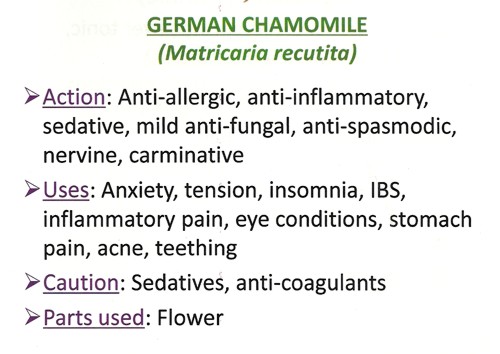
So, judging by NCCAM, these claims are unjustified. It’s teaching folk-lore as though it meant something.
More dangerous advice comes when we get to the ‘repertories’.
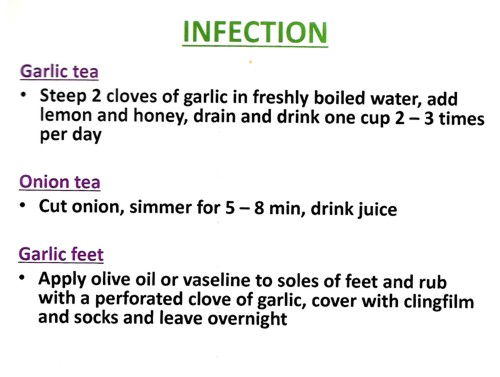
Infections can kill you, They are one of the modest number of things that pharmacology can usually cure, rather than treat symptomatically. If you go to a Westminster-trained naturopath with a serious infection and follow their advice to put garlic in your socks, you will not just be smelly, You could die.
Allergy and Intolerance 3CMwS03 18/02
|
Treating allergies, misdiagnosed by fraudulent tests, is very big business for the ‘health food industry’, This lecture, by R. Newman Turner ND, DO, BAc, started tolerably but descended to a nadir when it mentions, apparently seriously, two of the best known fraudulent methods of allergy diagnosis, the Vega test and "Applied Kinesiology". Kinesiology Sounds sort of sciencey, but Applied Kinesiology is actually a fraudulent and totally ineffective diagnostic method invented by (you guessed) a chiropractor. It has been widely used by alternative medicine to misdiagnose food allergies. It does not work (Garrow, 1988: download reprint). |
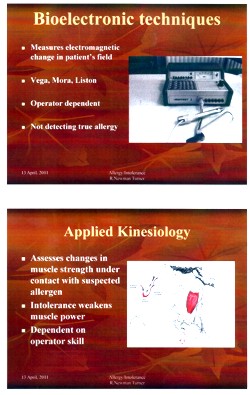
|
Could this be the same R Newman Turner who wrote a book on Naturopathic First Aid? The mind boggles.
Naturopathic Detoxification 23 CMES03 25/02 Detox Myth of Fact
|
This lecture was the responsibility of Irving S Boxer ND DO MRN LCH, a naturopath, homeopath and osteopath in private practice. Don’t be fooled by the implied question in the title. It might have been taken to suggest a critical approach. Think again. There is all the usual make-believe about unspecified and imaginary toxins that you must get rid of with enemas and vegetables. |
|
|
The skin brushing does not quite plumb the depths of Jacqueline Young’s Taking an air bath , but presumably it is something similar. "Liver activation" by castor oil packs is pure unadulterated gobblydygook. The words mean nothing. Their attempt to divide all foods into those that cleanse and those that clog sounds reminiscent of the Daily Mail’s ontological oncology project. |
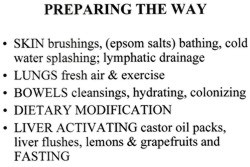 
|
The practice of healing (3CMSS01 2/12)
Next we retreat still further into fantasy land
|
|
All pure hokum, of course’ She could have added "craniosacral therapy" (at present the subject of a complaint against the UCL Hospitals Trust (that’s the NHS, not UCL) to the Advertising Standards Authority,
 |
 |
Is that definition quite clear?
In fact this sort of nonsense about rays coming from your hands was disproved experimentally, in a rather famous paper, the only paper in the Journal of the American Medical Association to have been written by a 9-year old. Emily Rosa. She (with some help from her parents) devised a simple test for her 4th (US) grade science fair project. It was later repeated under more controlled conditions and written up for JAMA [download reprint] . It showed that the claims of ‘therapeutic touch" practitioners to be able to detect "auras" were totally false. No subsequent work has shown otherwise. Why, then, does the University of Westminster teach it as part of a Bachelor of Science degree?
You can see Emily Rosa herself explain why “therapeutic touch is bullshit” with Penn and Teller, in Penn and Teller Expose Therapeutic Touch.
Environmental stress
The last bit of hokum (for the moment) is one of the best. This one has every myth under the sun (including some I hadn’t heard of).
|
The lecturer, Val Bullen, was also responsible for the infamous "Amethysts emit high Yin energy" slide. One of her own students desribes her as "sweet but deluded". I have nothing against Ms Bullen, She can believe whatever she wants. My problem is with the vice-chancellor, Prof Geoffrey Petts, who seems to think that this sort of stuff is appropriate for a BSc. |
|
Everything barmy is here. Mobile phones, power lines, underwater streams, ley lines, sick building syndrome, are all reasons why you don’t feel 100 percent, Actually my reason is having to read this junk. The "definitions" are, as always, just meaningless words.
|
But don’t despair. Help is at hand.
Just in case you happen to have run out of Alaskan Calling All Angels Essence, you can buy it from Baldwin’s for £19.95. It’s "designed to invoke the nurturing, uplifting and joyful qualities of the angelic kingdom.", and what’s more "can also use them any time to cleanse, energize, and protect your auric field." Well that’s what it says.in the ad.
Yarrow Environmental Solution looks like good stuff too. Only £7.95 for 7.5 ml. For that you get a lot. It will
" . . strengthen and protect against toxic environmental influences, geopathic stress, and other hazards of technology-dominated modern life. This includes the disruptive effects of radiation on human energy fields from X-rays, televisions, computer monitors, electromagnetic fields, airplane flights or nuclear fall-out."
OK stop giggling. This is serious stuff, taught in a UK university as part of a BSc degree, and awarded a high score by the Quality Assurance Agency (QAA).
Professor Petts, are you listening? I believe it is you, not I, who is bringing your university into disrepute.
The slides shown here are copyright of the University of Westminster or of the author of the lecture. They are small sample of what I was sent and are reproduced under the “fair quotation” provision, in the public interest.
Follow-up
5 May 2011. By sheer coincidence, Emily and Linda Rosa were passing through London. They called for lunch and here’s a picture (with Ben Goldacre) in UCL’s (endangered) Housman room. Linda kindly gave me a copy of her book Attachment Therapy on Trial: The Torture and Death of Candace Newmaker. [Download reprint of Rosa’s paper..]

.
6 May 2011. Talking of the “vibrational medicine” fantasy, I had an email that pointed out a site that plumbs new depths in fantasy physics. It’s on the PositiveHealthOnline website: A post there, Spirals and Energy in Nature, was written by Robert McCoy. He claims to have worked on microprocessor layout design, but anyone with school physics could tell that the article is sheer nonsense. In a way it is much more objectionable that the silly slides with coloured rays used in the Westminster course. McCoy’s post seeks to blind with sciencey-sounding language, that in fact makea no sense at all. Luckily my retweet of the site attracted the attention of a real physicist, A.P. Gaylard, who made a very welcome return to blogging with Fantasy physics and energy medicine. He dismantles the physics, line-by-line, in a devastating critique. This sort of junk physics is far more dangerous than the perpetual motion pundits and the cold-fusion fantasists. At PositiveHealthOnline it is being used to push pills that do you no good and may harm you. It is a danger to public health.
This is a slightly-modified version of the article that appeared in BMJ blogs yesterday, but with more links to original sources, and a picture. There are already some comments in the BMJ.
The original article, diplomatically, did not link directly to UCL’s Grand Challenge of Human Wellbeing, a well-meaning initiative which, I suspect, will not prove to be value for money when it comes to practical action.
Neither, when referring to the bad effects of disempowerment on human wellbeing (as elucidated by, among others, UCL’s Michael Marmot), did I mention the several ways in which staff have been disempowered and rendered voiceless at UCL during the last five years. Although these actions have undoubtedly had a bad effect on the wellbeing of UCL’s staff, it seemed a litlle unfair to single out UCL since similar things are happening in most universities. Indeed the fact that it has been far worse at Imperial College (at least in medicine) has probably saved UCL from being denuded. One must be thankful for small mercies.
There is, i think, a lesson to be learned from the fact that formal initiatives in wellbeing are springing up at a time when university managers are set on taking actions that have exactly the opposite effect. A ‘change manager’ is not an adequate substitute for a vote. Who do they imagine is being fooled?
The A to Z of the wellbeing industry
From angelic reiki to patient-centred care
Nobody could possibly be against wellbeing. It would be like opposing motherhood and apple pie. There is a whole spectrum of activities under the wellbeing banner, from the undoubtedly well-meaning patient-centred care at one end, to downright barmy new-age claptrap at the other end. The only question that really matters is, how much of it works?
Let’s start at the fruitcake end of the spectrum.
One thing is obvious. Wellbeing is big business. And if it is no more than a branch of the multi-billion-dollar positive-thinking industry, save your money and get on with your life.
In June 2010, Northamptonshire NHS Foundation Trust sponsored a “Festival of Wellbeing” that included a complementary therapy taster day. In a BBC interview one practitioner used the advertising opportunity, paid for by the NHS, to say “I’m an angelic reiki master teacher and also an angel therapist.” “Angels are just flying spirits, 100 percent just pure light from heaven. They are all around us. Everybody has a guardian angel.” Another said “I am a member of the British Society of Dowsers and use a crystal pendulum to dowse in treatment sessions. Sessions may include a combination of meditation, colour breathing, crystals, colour scarves, and use of a light box.” You couldn’t make it up.
The enormous positive-thinking industry is no better. Barbara Ehrenreich’s book, Smile Or Die: How Positive Thinking Fooled America and the World, explains how dangerous the industry is, because, as much as guardian angels, it is based on myth and delusion. It simply doesn’t work (except for those who make fortunes by promoting it). She argues that it fosters the sort of delusion that gave us the financial crisis (and pessimistic bankers were fired for being right). Her interest in the industry started when she was diagnosed with cancer. She says
”When I was diagnosed, what I found was constant exhortations to be positive, to be cheerful, to even embrace the disease as if it were a gift. If that’s a gift, take me off your Christmas list,”
It is quite clear that positive thinking does nothing whatsoever to prolong your life (Schofield et al 2004; Coyne et al 2007; 2,3), any more than it will cure tuberculosis or cholera. “Encouraging patients to “be positive” only may add to the burden of having cancer while providing little benefit” (Schofield et al 2004). Far from being helpful, it can be rather cruel.
Just about every government department, the NHS, BIS, HEFCE, and NICE, has produced long reports on wellbeing and stress at work. It’s well known that income is correlated strongly with health (Marmot, M., 2004). For every tube stop you go east of Westminster you lose a year of life expectancy (London Health Observatory). It’s been proposed that what matters is inequality of income (Wilkinson & Pickett, 2009). The nature of the evidence doesn’t allow such a firm conclusion (Lynch et al. 2004), but that isn’t really the point. The real problem is that nobody has come up with good solutions. Sadly the recommendations at the ends of all these reports don’t amount to a hill of beans. Nobody knows what to do, partly because pilot studies are rarely randomised so causality is always dubious, and partly because the obvious steps are either managerially inconvenient, ideologically unacceptable, or too expensive.
Take two examples:
Sir Michael Marmot’s famous Whitehall study (Marmot, M., 2004) has shown that a major correlate of illness is lack of control over one’s own fate: disempowerment. What has been done about it?
In universities it has proved useful to managers to increase centralisation and to disempower academics, precisely the opposite of what Marmot recommends.
|
As long as it’s convenient to managers they are not going to change policy. Rather, they hand the job to the HR department which appoints highly paid “change managers,” who add to the stress by sending you stupid graphs that show you emerging from the slough of despond into eternal light once you realise that you really wanted to be disempowered after all. Or they send you on some silly “resilience” course. |
|
A second example comes from debt. According to a BIS report (Mental Capital and Wellbeing), debt is an even stronger risk factor for mental disorder than low income. So what is the government’s response to that? To treble tuition fees to ensure that almost all graduates will stay in debt for most of their lifetime. And this was done despite the fact that the £9k fees will save nothing for the taxpayer: in fact they’ll cost more than the £3k fees. The rise has happened, presumably, because the ideological reasons overrode the government’s own ideas on how to make people happy.
Nothing illustrates better the futility of the wellbeing industry than the response that is reported to have been given to a reporter who posed as an applicant for a “health, safety, and wellbeing adviser” with a local council. When he asked what “wellbeing” advice would involve, a member of the council’s human resources team said: “We are not really sure yet as we have only just added that to the role. We’ll want someone to make sure that staff take breaks, go for walks — that kind of stuff.”
The latest wellbeing notion to re-emerge is the happiness survey. Jeremy Bentham advocated “the greatest happiness for the greatest number,” but neglected to say how you measure it. A YouGov poll asks, “what about your general well-being right now, on a scale from 1 to 10.” I have not the slightest idea about how to answer such a question. As always some things are good, some are bad, and anyway wellbeing relative to whom? Writing this is fun. Trying to solve an algebraic problem is fun. Constant battling with university management in order to be able to do these things is not fun. The whole exercise smacks of the sort of intellectual arrogance that led psychologists in the 1930s to claim that they could sum up a person’s intelligence in a single number. That claim was wrong and it did great social harm.
HEFCE has spent a large amount of money setting up “pilot studies” of wellbeing in nine universities. Only one is randomised, so there will be no evidence for causality. The design of the pilots is contracted to a private company, Robertson Cooper, which declines to give full details but it seems likely that the results will be about as useless as the notorious Durham fish oil “trials”(Goldacre, 2008).
Lastly we get to the sensible end of the spectrum: patient-centred care. Again this has turned into an industry with endless meetings and reports and very few conclusions. Epstein & Street (2011) say
“Helping patients to be more active in consultations changes centuries of physician-dominated dialogues to those that engage patients as active participants. Training physicians to be more mindful, informative, and empathic transforms their role from one characterized by authority to one that has the goals of partnership, solidarity, empathy, and collaboration.”
That’s fine, but the question that is constantly avoided is what happens when a patient with metastatic breast cancer expresses a strong preference for Vitamin C or Gerson therapy, as advocated by the YesToLife charity. The fact of the matter is that the relationship can’t be equal when one party, usually (but not invariably) the doctor, knows a lot more about the problem than the other.
What really matters above all to patients is getting better. Anyone in their right mind would prefer a grumpy condescending doctor who correctly diagnoses their tumour, to an empathetic doctor who misses it. It’s fine for medical students to learn social skills but there is a real danger of so much time being spent on it that they can no longer make a correct diagnosis. Put another way, there is confusion between caring and curing. It is curing that matters most to patients. It is this confusion that forms the basis of the bait and switch tactics (see also here) used by magic medicine advocates to gain the respectability that they crave but rarely deserve.
If, as is only too often the case, the patient can’t be cured, then certainly they should be cared for. That’s a moral obligation when medicine fails in its primary aim. There is a lot of talk about individualised care. It is a buzzword of quacks and also of the libertarian wing which says NICE is too prescriptive. It sounds great, but it helps only if the individualised treatment actually works.
Nobody knows how often medicine fails to be “patient-centred.”. Even less does anyone know whether patient-centred care can improve the actual health of patients. There is a strong tendency to do small pilot trials that are as likely to mislead as inform. One properly randomised trial (Kinmonth et al., 1998) concluded
“those committed to achieving the benefits of patient centred consulting should not lose the focus on disease management.”
Non-randomised studies may produce more optimistic conclusions (e.g. Hojat et al, 2011), but there is no way to tell if this is simply because doctors find it easy to be empathetic with patients who have better outcomes.
Obviously I’m in favour of doctors being nice to patients and to listening to their wishes. But there is a real danger that it will be seen as more important than curing. There is also a real danger that it will open the doors to all sorts of quacks who claim to provide individualised empathic treatment, but end up recommending Gerson therapy for metastatic breast cancer. The new College of Medicine, which in reality is simply a reincarnation of the late unlamented Prince’s Foundation for Integrated Health, lists as its founder Capita, the private healthcare provider that will, no doubt, be happy to back the herbalists and homeopaths in the College of Medicine, and, no doubt, to make a profit from selling their wares to the NHS.
In my own experience as a patient, there is not nearly as much of a problem with patient centred care as the industry makes out. Others have been less lucky, as shown by the mid-Staffordshire disaster (Delamothe, 2010), That seems to have resulted from PR being given priority over patients. Perhaps all that’s needed is to save money on all the endless reports and meetings (“the best substitute for work”), ban use of PR agencies (paid lying) and to spend the money on more doctors and nurses so they can give time to people who need it. This is a job that will be hindered considerably by the government’s proposals to sell off NHS work to private providers who will be happy to make money from junk medicine.
Reference
Wilkinson. R & Pickett, K. 2009 , The Spirit Level, ISBN 978 1 84614 039 6
A footnote on Robertson Cooper and "resilience"
I took up the offer of Robertson Cooper to do their free "resilience" assessment, the company to which HEFCE has paid an undisclosed amount of money.
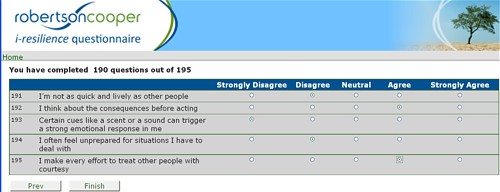
The first problem arose when it asked about your job. There was no option for scientist, mathematician, university or research, so I was forced to choose "education and training". (a funny juxtaposition since training is arguably the antithesis of education). It had 195 questions. mostly as unanswerable as in the YouGov happiness survey. I particularly liked question 124 "I see little point in many of the theoretical models I come across". The theoretical models that I come across most are Markov models for the intramolecular changes in a receptor molecule when it binds a ligand (try, for example, Joint distributions of apparent open and shut times of single-ion channels and maximum likelihood fitting of mechanisms). I doubt the person who wrote the question has ever heard of a model of that sort. The answer to that question (and most of the others) would not be worth the paper they are written on.
The whole exercise struck me as the worst sort of vacuous HR psychobabble. It is worrying that HEFCE thinks it is worth spending money on it.
Follow-up
The absurdness of allowing statutory regulation of herbal medicines, both Western and Chinese has already been pointed out here, in Government lends credibility to quacks and charlatans, and by Andrew Lewis in “How to Spot Bad Regulation of Alternative Medicine“
The harm done by the government’s endorsement of herbal products could be ameliorated if they were labelled honestly. The labelling is a matter for the Medicines and Healthcare products Regulatory Authority (MHRA), and for a while I have been writing to the head of the MRH, Kent Woods, and to Richard Woodfield (head of MHRA herbal medicine policy), in an attempt to work out their reasons for not telling the consumer the simple truth.
A similar (but even worse) problem arises in the labels that have been allowed by the MHRA for homeopathic pills. That has been discussed in Pseudo-regulation: another chance to save the MHRA from looking idiotic . The matter is not yet decided, but on past performance, I’m pessimistic about whether the MHRA will listen to scientists.
The Traditional Herbal Registration (THR) scheme allows herbal medicines that are registered on this scheme to be sold if they are safe, and have been in use for 30 years. There is need to supply any information whatsoever about whether they work or not. That itself is very odd, given that the MHRA’s strap line says
"We enhance and safeguard the health of the public by ensuring that medicines and medical devices work and are acceptably safe."
In the case of herbals, the bit about ensuring that medicines work has been brushed under the carpet.
A typical dishonest label
Take "Echina Cold Relief". The Traditional Herbal Regulation document specifies the label.
Note, first of all, the therapeutic claim in the brand name itself. This is blatant practice for most herbals and appears to be unregulated. The label says
|
It is my contention that most people would interpret this label as a claim that the tablets would have a beneficial effect on the symptoms of "common cold and influenza type infections". The impression is reinforced by the government stamp of approval on the package. The MHRA tell me that no tests have been done to discover how shoppers interpret these words. They should have been done.
|

|
Why is there nothing on the label that tells the plain, unvarnished truth? Perhaps something like this
"There is no evidence that this product works for the indications mentioned".
Or
"Clinical trials have shown this product to be ineffective for xxx "
or, at a minimum
"The MHRA kite mark does not imply that this product is effective".
Some Evidence
Echinacea is a generous choice of example because, unlike most herbs, there is a bit of evidence about its effectiveness. A Cochrane review says
Sixteen trials including a total of 22 comparisons of Echinacea preparations and a control group (19 placebo, 2 no treatment, 1 another herbal preparation) met the inclusion criteria. All trials except one were double-blinded. The majority had reasonable to good methodological quality. Three comparisons investigated prevention; 19 comparisons investigated treatment of colds. A variety of different Echinacea preparations were used. None of the prevention trials showed an effect over placebo. Comparing an Echinacea preparation with placebo as treatment, a significant effect was reported in nine comparisons, a trend in one, and no difference in six. Evidence from more than one trial was available only for preparations based on the aerial parts of Echinacea purpurea (E. purpurea).
“It seems that some preparations based on the herb of Echinacea purpurea might be effective for this purpose in adults, while there is no clear evidence that other preparations are effective or that children benefit. Side effects were infrequent but rashes were reported in one trial in children.”
The US agency NCCAM has spent over a billion dollars on testing various sorts of alternative treatment, and has failed to find a single useful treatment, They say
"Two NCCAM-funded studies did not find a benefit from echinacea, either as Echinacea purpurea fresh-pressed juice for treating colds in children, or as an unrefined mixture of Echinacea angustifolia root and Echinacea purpurea root and herb in adults."
So the evidence is a mess. There is no evidence that Echinacea can prevent colds, and, at the very best, it might shorten slightly the time for which cold symptoms last. The most likely interpretation of the mixture of contradictory results, many negative trials with a handful of small positive effects, is that for practical purposes, echinacea is useless. There is NO treatment known that affects the duration of a cold to any useful extent.
I wrote to Kent Woods in February 2011
|
Hello
Sorry to bother you again, but recent events have caused me to think about a rather fundamental question, and I have never seen it discussed in any official documents. I suspect it needs to be answered at the highest level. Question, Do you make any distinction between (a) herbs that have unknown efficacy (most of them). and (b) herbs that have been shown in good trials to have no useful effect (like echinacea)? It is one thing to say “traditionally used for …” when you don’t know whether it is true or not. It is quite another thing to say “traditionally used for. . . ” when you know it is untrue No such distinction seems to be made at the moment. Is that because the distinction has never been considered by the MHRA? Or is it because it has been considered, but dismissed as unimportant? Or is it considered important but you are prevented from doing anything about it (and, if this is the case, what prevents you?) Best wishes |
His reply was, essentially, that herbs come in so many different forms that they can’t all be tested so it is never possible to say that a herb “does not work to any useful extent”
|
. . . Based on our experience of regulating herbal medicines, we think it unlikely for the foreseeable future that there would be available for particular herbs a comprehensive body of published studies that meet medicines regulatory standards and cover systematically the numerous possible permutations as to type of extract, plant species and part of plant. Consequently, it is unlikely that evidence would be available for MHRA to know that a traditional herbal product did not have efficacy. In summary, you suggest an interesting scenario the handling of which would be worthy of further consideration in the event of major advances in the range and quality of clinical trials of herbal medicines – but for the foreseeable future we would see the dilemma as largely a theoretical one.
Regards Kent Woods
|
This strikes me as a cop-out. It amounts to saying that it’s impossible ever to say that a treatment us useless. If NICE took the same view, no medicine would ever be ruled out as having no useful effect.
Then I asked about a press release from the MHRA, dated 18 March 2011.
|
Hello It says (my emphasis)
Since the main sort of information that people want about a medicine is whether it works, and you have explicitly ruled out any information about that, the description "informed choice" seems to me to be exaggerated to the point of dishonesty. This raises another question. Many people think that the wording that you approve is deceptive. can you tell me whether you have yet done tests to discover whether or not the average consumer interprets your wording as suggesting effectiveness? This was raised (apropos oh homeopathics) with Kent Woods at the SciTech enquiry and they were assured such tests had been done. Still nobody has seen the result of such tests. Please will you let me know if they have been done, and, if they have, what the results were? if they have not been done, why not? Best regards |
The legal requirement
In response to my letter, Richard Woodfield said
"Specifically on the question of wording affecting efficacy, we have to comply with the requirements of the herbals Directive which specifies the required product information about the traditional basis of the registration. We have not user tested the required statement in the Directive.
"
The European Herbals directive 2004/24/EC [download it] does make it mandatory to include the words used by the MHRA
“In addition to the requirements of Articles 86 to 99, any advertisement for a medicinal product registered under this chapter shall contain the following statement: Traditional herbal medicinal product for use in specified indication( s) exclusively based upon long-standing use.”
Telling the truth on the label
I asked the MHRA whether there was any legal reason why they could not add the following notice to the wording required by the European Directive. I had to ask the question several times before I got a straight answer, but the answer eventually turned out to be that there is no legal reason that bars honest labels. Eventually Richard Woodfield told me there was no legal reason.
|
Dear Prof Colquhoun There is no specific bar in the European Directive that would definitely preclude requiring additional statements that were consistent with the Directive. Obviously one would have to look at the specifics of what was proposed.
The main bar is that of Government policy. Under the previous Administration when the scheme was set up there was a strong policy of avoiding gold plating of European legislation – and this would clearly be a case of gold plating. Under the new Government that policy of avoiding gold plating has been strengthened further. And added to that there is now a presumption that wherever possible Directives should be transposed by “copy out” of the text rather than elaborating upon the requirements of the Directive.
The onus would be on those seeking gold plating to demonstrate that it was necessary. In the present absence of evidence of significant detriment under the THR scheme to consumers who for example choose to take a THR to help with a condition such as mild indigestion we have no present plans to propose the introduction of a form of retrospective gold plating of this legislation. As recognised in your last email, I think that is about as far as we can usefully comment on the issue for the time being. Regards
Richard Woodfield |
So, at last we have the answer. And pretty pathetic it is. “Gold-plating” is a term that is used by the anti-European lobby to describe the process of not simply implementing European law but making it more strict that is essential. In this case, I would claim that making the label honest was the opposite of gold-plating, The European law is obviously designed to encourage the herbal industry by disguising the lack of evidence for the herbs. The MHRA should correct that deficiency but has declined to do so.
Safety
The herbal medicine business, especially the Chinese Traditional medicine, is riddled with impure, contaminated and sometimes lethally toxic rubbish. Of course it is right that the public should be protected from this. Probably it is a job that should be done by Trading Standards officers, but sadly they have shown themselves time and time again to be incompetent and unwilling to enforce the law when it comes to false health claims. The MHRA make a reasonably good job on this front, but that is no reason for them to endorse misleading labels. Statutory regulation by the HPC will do nothing to help: on the contrary it will endorse courses that teach dangerous nonsense.
The Herbal Medicines Advisory Committee
The MHRA’s Herbal Medicines Advisory Committee should have resisted this misleading labelling, but they do not seem to have not done so (it’s hard to tell because the published minutes are totally free of any useful information). The chairman of that committee is Professor Philip A Routledge OBE MB BS MD FRCP FRCPE. If I had been in his position, I would have resigned. I believe that he has let down honest science, and potentially endangered patients by not insisting on honest labels. I do hope that this was not a result of pressure from the Prince of Wales. We know he has lobbied Kent Woods and Philip Routledge. Incidentally, Routledge is president elect of the British Pharmacological Society. Quackery has crept in even there.
What can be done
There us no reason why, even now, the MHRA could not change the labels to something honest. I expect the government is pressing them to support the herbal industry, and big business usually wins over regulators (as with banks).
Freedom of choice by consumers was mentioned several times by the MHRA. That’s fine. Nobody wants to ban echinacea. The whole point of labels is to ensure that it is informed choice. Labels that mislead do not help anyone. They hurt the consumer and they are disastrous for the reputation for integrity of the MHRA.
We should keep up the pressure on the MHRA. Here are a couple of my recent efforts, on BBC Breakfast TV.
The second interview was joint with Dick Middleton. It should have been made clear that Middleton is a pharmacist who is technical director of Schwabe Pharma, a company that sells expensive herbal pills, so has a vested financial interest in disguising the lack of evidence for efficacy,
Follow-up
1 May 2011. The new herbal regulations have come into effect. Radio 5 put me up against the herbal industry representative, Michael McIntyre (chair of the European Herbal & Traditional Medicine Practitioners Association). I was pleased to get the chance to debate directly with him, because he has been misrpresenting the evidence for years. See, for example, Some truly appalling reporting of science by the BBC. and Government lends credibility to quacks and charlatans. I was able, at last, to ask him directly, which herb had the best evidence for its efficacy. He repeatedly refused to answer: “I’m not going to get into detail”. Eventually he resorted to the argument that herbalists treat people not diseases. I pointed out that the MHRA-approved labels list all sorts of diseases. No response. He then misquotes Sackett, who did NOT say that experience was as good as RCTs.
McIntyre goes on to misrepresent the BMJ Clinical Evidence paper which, he says, shows that 46% of all treatments are not proven to be effective. It is hard to be believe that McIntyre is really unaware that a large proportion of those that were not shown to be effective are CAM treatments, herbal medicine and the like. Professor John Garrow has pointed this out (see, also Healthwatch). Either he doesn’t read the literature or he deliberately misrepresents it.
Then a caller came in to swear that Chinese Medicine had cured his prostate problem and his wife’s hair. Of course he hadn’t any idea of how is prostate would have progressed if he hadn’t taken the Chinese medicine. Luckily for him, he didn’t have prostate cancer (the people who take Chinese medicine for cancer are probably dead so they can’t appear on the radio). These people are difficult to deal with without appearing rude, by saying they are gullible and deceived. I tried. Interestingly McIntyre did not leap to the defence of Chinese herbs.
An email yesterday alerted me to YesToLife. This outfit seemed to me to be so dangerous that a word of warning is in the public interest.
Their own description says “YES TO LIFE is a new charitable initiative to open up a positive future for people with cancer in the UK by supporting an integrative* approach to cancer care”. That sounds sort of cuddly but lets look below the surface.
As so often, the funding seems to have been raised as the result of the death of an unfortunate 23 year old woman. Instead of putting the money into real research, yet another small charity was formed. My correspondent pointed out that “I came across them at St Pancras Station on Friday afternoon — they had a live DJ to draw in the crowd and were raising funds through bucket collections”. No doubt many people just see the word ‘cancer’ and put money in the bucket, without realising that their money will be spent on promoting nonsensical and ineffective treatments.
The supporters list.
The list of supporters tells you all you need to know, if you are familiar with the magic medicine business, though it might look quite convincing if you don’t know about the people. Sadly the list starts with some celebrities (I didn’t know before that Maureen Lipman was an enthusiast foir quackery -how very sad). But never mind the air-head celebrities. The more interesting supporters come later.
- Dr Rosy Daniel of Health Creation is an old friend. After I complained about her promotion of some herbal concoction called Carctol to “heal cancer”, she was reprimanded by Trading Standards for breaching the Cancer Act 1939, and forced to change the claims (in my view she should have neen prosecuted but, luckily of her, Trading Standards people are notoriously ineffective). There is, of course not the slightest reason to to think that Carctol works (download Carctol: Profits before Patients?). Read also what Cancer Research UK say about carctol.
Dr Daniel is also well known because ran a course that was, for one year, accredited by the University of Buckingham. But once the university became aware of the nonsense that was being taught on the course, they first removed her as the course director, and then removed accreditation from the course altogether. She then tried to run the course under the aegis of the Prince’s Foundation for Integrated Health, but even they turned her down. Now it is running as a private venture, and is being advertised by YesToLife. - Boo Armstrong, “Chief Executive of The Prince’s Foundation for Integrated Health and Founder and Executive Director GetWellUK”. The web site is out of date since the Prince’s Foundation shut its doors a year ago. She runs a private company, GetWellUK, that was responsible for a very poor study of alternative medicine in Northern Ireland. So she has a vested interest in promoting it. See Peter Hain and GetwellUK: pseudoscience and privatisation in Northern Ireland
- Professor George Lewith. This is beginning to look like the usual list of suspects. I’ve had cause to write twice about the curious activities of Dr Lewith. See Lewith’s private clinic has curious standards, in 2006, and this year George Lewith’s private practice. Another case study. The make up your own mind about whether you’d trust him.
- Dr Michael Dixon OBE, Chairman NHS Alliance and Medical Director The Prince’s Foundation for Integrated Health. Again the job description is a year out of date. You can read about Dr Dixon at Prince of Wales Foundation for magic medicine: spin on the meaning of ‘integrated’. He seems to be a well meaning man for whom no new-age idea is too barmy.
In fact both Dixon and Lewith have moved to a reincarnation of the Prince’s Foundation known as the “College of Medicine” (actually it’s a couple of offices in Buckingham Street). See Don’t be deceived. The new “College of Medicine” is a fraud and delusion.
It seems to me incomprehensible that people such as Sir Graeme Catto, Sir Cyril Chantler and Sir Muir Grey are willing to be associated with people who behave like this. - Charlotte Grobien, Managing Director, Give it Away. This seems to be a fund-raising organisation that has supported YesToLife. The lesson seems to be, never give money to fundraisers unless you know exactly where your money is going.
The Help Centre
YesToLife has a help centre. But beware, There is no medical person there. Just Traditional Chinese medicine (rather dangerous), acupuncture, osteopath and naturopathy (which means, roughly, do nothing and hope for the best).
Patrick Holford,
There can be no better indication of the standard of advice to be expected from YesToLife than the fact they are advertising a lecture by Holford, with the enticing title "Say no to cancer"."Through learning about the effects of diet and nutrition, people with cancer or at risk of developing cancer can be empowered to say Yes to Life and No to Cancer". Would that it were so easy. It will cost you £15.00.
Just in case there is still nobody who has heard of Holford, he is the media nutritionist who has an entire chapter devoted to him in Ben Goldacre’s Bad Science book, He has a whole website that has exposed his dubious advice, the excellent HolfordWatch. And you can find quite a lot about him on this blog. Try, for example, Patrick Holford’s CV: the strange case of Dr John Marks, and Response to a threatening letter from Mr Holford, or Holford’s untruthful and unsubstantiated advertisement
The treatments directory
Now we get to the truly scary bit of YesToLife, their treatment directory. Try searching for ‘cancer type’ and then "breast (metastatic)".. We find no mention of the advances in understanding of the genetics of breast cancer, nor ot real therapies like tamoxifen. What we find are four "alternative treatments".
- Neuroimmunomodulation Therapy It sounds impressive until you learn that its only proponent is a an 82 year old Venezuelan doctor with a clinic in Caracas. Even YesToLife doesn’t pretend that there is any evidence that it works
- Vitamin C Therapy The old chestnut cure-all Vitamin C Again even YesToLife don’t pretend there is any good evidence but it is still offered; treatment cost £3140.00 (what? Vitamin C is very cheap indeed)
- Dendritic Cell Therapy Said by YesToLife to be "well-researched", though that isn’t so for breast cancer (metastatic). Although possibly not as barmy as the other things that are recommended, it is nevertheless not shown to be effective for any sort of cancer,
- Gerson Therapy It is a sign of the extreme unreliability of advice given by YesToLife that they should still recommend anything as totally discredited as Gerson Therapy.Although YesToLife describes it as "well-researched" that is simply not true: there are no proper clinical trials. Cancer Research UK say
"Overall, there is no evidence to show that Gerson therapy works as a cure for cancer. "
"Available scientific evidence does not support claims that Gerson therapy can treat cancer. It is not approved for use in the United States. Gerson therapy can be very harmful to your health. Coffee enemas have been linked to serious infections, dehydration, constipation, colitis (inflammation of the colon), and electrolyte imbalances. In some people, particular aspects of the diet such as coffee enemas have been thought to be responsible for their death."Recommended reading: The (Not-So-)Beautiful (Un)Truth about the Gerson protocol and cancer quackery, by David Gorski (breast cancer surgeon, writing in Science-based Medicine.
Conclusion
The information supplied by YesToLife is more likely to kill you than to cure you.
The next time you see somebody collecting for a "cancer charity" be very careful before you give them money.
Follow-up
November 2012. It gets worse.
I had an email from someone who was distressed because a friend was trying to raise £15,000 to cover the cost of treatments recommended by YesToLife. The treatment is high-dose intravenous Vitamin C infusion. This is pure quackery. There isn’t the slightest reason to think it will affect the course of cancer, or the wellbeing of the patient. It is exploitation of the desperate. My heart sinks at the thought that a “charity” can be quite so wicked.
|
Last year the Royal London Homeopathic Hospital was rebranded as the Royal London Hospital for Integrated Medicine (RLHIM). The exercise seems to have been entirely cosmetic. Sadly, they still practise the same nonsense, as described in Royal London Homeopathic Hospital rebranded. But how different will things be at the Royal London Hospital for Integrated Medicine?. Recently I came across a totally disgraceful pamphlet issued by the RLHIM [download pamphlet]. If you haven’t come across craniosacral therapy (and who could blame you, a new form of nonsense is invented daily), try these sources.
|
In short, it is yet another weird invention of an eccentric American osteopath, dating from the 1930s. Like Osteopathy and Chiropractic, there is no ancient wisdom involved, just an individual with an eye for what makes money.
What the UCLH pamphlet claims
|
The claims made in this pamphlet are utterly baseless. In fact there isn’t the slightest evidence that craniosacral therapy is good for anything. And its ‘principles’ are pure nonsense. No doubt that is why the Advertising Standards Authority has already delivered a damning indictment of rather similar claims made in a leaflet issued by the Craniosacral Therapy Association (CSTA) |
The Advertising Standards judgement concluded
" . . the ad breached CAP Code clauses 3.1 (Substantiation), 7.1 (Truthfulness) and 50.1 (Health and beauty products and therapies)."
"We noted that the CSTA believed that the leaflet was merely inviting readers to try CST to see if it could alleviate some of their symptoms and did not discourage them from seeing a doctor. However, we considered that the list of serious medical conditions in the ad, and the references to the benefit and help provided by CST, could encourage readers to use CST to relieve their symptoms rather than seek advice from a medical professional. We therefore concluded that the ad could discourage readers from seeking essential treatment for serious medical conditions from a qualified medical practitioner.
Complaint through the official channels. It took 3 months to extract “No comment” from Dr Gill Gaskin
Given that I have every reason to be grateful to UCL Hospitals for superb care, i was hesitant to leap into print to condemn the irresponsible pamphlet issued by one of their hospitals. It seemed better to go through the proper channels and make a complaint in private to the UCL Hospitals Trust.
On 21st December 2010 I wrote to the directors of UCLH Trust
|
I have just come across the attached pamphlet. “Craniosacral” therapy is a preposterous made-up invention. More to the point, there is no worthwhile evidence for the claims made in the pamphlet. The leaflet is, I contend, illegal under the Consumer protection regulations 2008. It is also deeply embarrassing that UCLH should be lending its name to this sort of thing. If you can think of any reason why I should not refer the pamphlet to the Advertising Standards Association, and to the office of Trading Standards, please let me know quickly. Best regards David Colquhoun |
On 7th January 2011 I got an acknowledgment, which told me that my letter had been forwarded to the Medical Director for Specialist Hospitals for a response.
The Specialist Hospitals of the Trust include the Eastman Dental Hospital, The Heart Hospital, The National Hospital for Neurology & Neurosurgery (the famous Queen’s Square hospital) and, yes, The Royal London Hospital for Integrated Medicine. I’ve been a patient at three of them and have nothing but praise, Queen’s Square and the UCLH baby unit saved the life of my wife and my son in 1984 (see Why I love the National Health Service).
The Medical Director for Specialist Hospitals is Dr Gill Gaskin, and it is to her that my letter was forwarded. Of course it is not her fault that, in 2002, the Royal London Homeopathic Hospital (as it then was) was acquired by the UCLH Trust in 2002, The excuse given at the time was that the space was needed and the nonsense espoused by the RLHH would be squeezed out. That hasn’t yet happened.
After that nothing happened so I wrote directly to Dr Gaskin on 14th February 2011
|
Dear Dr Gaskin
The letter below was sent to the Trust on 20 December last year. I am told it was forwarded to you. I’m disappointed that I have still had no reply, after almost two months. It was a serious enquiry and it has legal implications for the Trust. Would it help to talk about it in person? David Colquhoun |
I got a quick reply, but sadly, as so often, the complaint had simply been forwarded to the object of the complaint. This sort of buck-passing is standard procedure for heading off complaints in any big organisation, in my experience.
|
From: <Gill.Gaskin@uclh.nhs.uk>
To: <d.colquhoun@ucl.ac.uk> Cc: <jocelyn.laws@uclh.nhs.uk>, <Rachel.Maybank@uclh.nhs.uk> Dear Professor Colquhoun
With best wishes
Dr Gill Gaskin Medical Director Specialist Hospitals Board UCLH NHS Foundation Trust |
I don’t know who wrote this self-serving nonsense because there is no sign on the web of a job called "Associate Clinical Director of the Royal London Hospital for Integrated Medicine".
It is absurd to say that the leaflet makes “makes no claims of efficacy”. It says "Craniosacral therapy can be offered to children and adults for a variety of conditions:" and then goes on to list a whole lot of conditions, some of which are potentially serious, like "Recurrent ear infections and sinus infections, glue ear " and "Asthma". Surely anyone would suppose that if a UCLH Hopsital were offering a treatment for conditions like these, there would be at least some evidence that they worked. And there is no such evidence. This reply seemed to me to verge on the dishonest.
Remember too that this response was written on 16th February 2011, long after the Advertising Standards Association had said that there is no worthwhile evidence for claims of this sort, on 8th September 2010.
I replied at once
|
Thanks for the reply, but I thought that this was your responsibility. Naturally the RLHIM will stick up for itself, so asking them gets us nowhere at all. The buck stops with the Trust (in particular with you, I understand) and it is for you to judge whether pamphlets such as that I sent bring the Trust into disrepute . . .. I’d be very pleased to hear your reaction (rather than that of the RLHIM) to these comments. It seems a reasonable thing to ask for, since responsibility for the RLHIM rests with you David Colquhoun |
On the 13th March, after a couple of reminders, Dr Gaskin said "I will respond to you tomorrow or Tuesday,". No such luck though. On 25th March, more than three months after I first wrote, I eventually got a reply (my emphasis).
|
I do not wish to comment further on the matter of the leaflets as a complaint to the advertising standards authority would be dealt with formally. I am aware of your views on complementary medicine, and of course am entirely open to you pointing out areas where you believe there is misleading information, and I ask colleagues to review such areas when highlighted. I would make several additional comments: – patients are referred into NHS services by their GPs (or occasionally by consultants in other services) and cannot self-refer – patients attending the Royal London Hospital for Integrated Medicine report positively on NHS Choices – GPs continue to make referrals to the Royal London Hospital for Integrated Medicine and many request that patients stay under follow-up, when UCLH seeks to reconfirm this – UCLH is engaging with North Central London NHS commissioners on work on their priorities, and that includes work on complementary medicine (and combinations of conventional and complementary approaches) I think you will understand that I will not wish to engage in lengthy correspondence, and have many other competing priorities at present. With best wishes Gill Gaskin |
So, after three months’ effort, all I could get was ‘no comment‘, plus some anecdotes about satisfied customers -the stock in trade of all quacks.
I guess it is well known that complaints against any NHS organisation normally meet with a stonewall. That happens with any big organisation (universities too). Nevertheless it strikes me as dereliction of duty to respond so slowly, and in the end to say nothing anyway.
The Advertising Standards Authority have already given their judgement, and it appears to be based on sounder medicine than Dr Gaskin’s ‘reply’..
There are plans afoot to refer the UCLH pamphlet to the the Office of Trading Standards.IIt is for them to decide whether to prosecute the UCLH Trust for making false health claims. It is sad to have to say that they deserve to be prosecuted.
Follow-up
28 March 2011. Two days after this post went up, a Google search for “Dr Gill Gaskin” brought up this post as #5 on the first page. Amazing.
On 25 May, the same search alluded to this post in positions 2, 3, 4 and 5 on the first page of Google.
29 June 2013
Despite several judgements by the Advertising Standards Authority (ASA) against claims made for craniosacral therapy, nothing was done.
But after UCLH Trust was comprehensively condemned by the ASA for the claims made for acupuncture by the RLHIM, at last we got action. All patient pamphlets have been withdrawn, and patient information is being revised.
. It isn’t obvious why this has taken more that two years (and one can only hope that the revised information will be more accurate)
As promised in my last post about Edinburgh Napier University, I wrote to the vice-chancellor of the university, Professor Dame Joan K. Stringer DBE, BA (Hons) CertEd PhD CCMI FRSA FRSE, to invite her to respond.
|
7 February, 2011 Dear Professor Stringer, I should be grateful if you could let me know about your opinion of the degrees that you offer in Aromatherapy and Reflexology I have posted on my blog a bit of the material that was sent to me as result of recent FoI requests. See https://www.dcscience.net/?p=4049 I submit that degrees like this detract from the intellectual respectability of what is, not doubt, in other respects a good university, but since you are mentioned in the post, it’s only fair to give you the chance to defend yourself. In fact you’d be very welcome to do so publicly by commenting on the post. Best regards David Colquhoun |
Over a month later, I have received no response at all. This seems to me to be a bit discourteous.
There is nothing new in failing to get any answer to letters to vice-chancellors. The only VC who has ever thanked me for opening his eyes is Terence Kealey, of the University of Buckingham. All the rest have stayed silent. I can interpret this silence only as guilt. They know it’s nonsense, but dare not say so. Of course it isn’t infrequent for the course to close down after public exposure of the nonsense they teach. So perhaps the letters get read, even if they don’t elicit a reply.
Meanwhile the university sent me more materials that are used to teach their students. So here is another sample, largely from what’s taught to the unfortunate “reflexology” students.
Remember, these pre-scientific myths are not being taught as history or anthropology. They are taught as though they were true, to students who are then let loose on patients, so they can make money from anyone who is gullible enough to believe what they say.
There are no "excess body energies". It’s made-up nonsense.
The diagram is pure imagination. It dates form a time before we knew anything about physiology, yet it is still being taught as though it meant something.
The admission that there is controversy is interesting. But it doesn’t seem to deter Napier’s teachers in the slightest.
How can anyone in the 21st century believe that the heart is "king of our emotional existence”?. That’s just preposterous pre-scientific myth,
You must be joking.
"Vibrational medicine" is a non-existent subject. Pure gobbledygook.
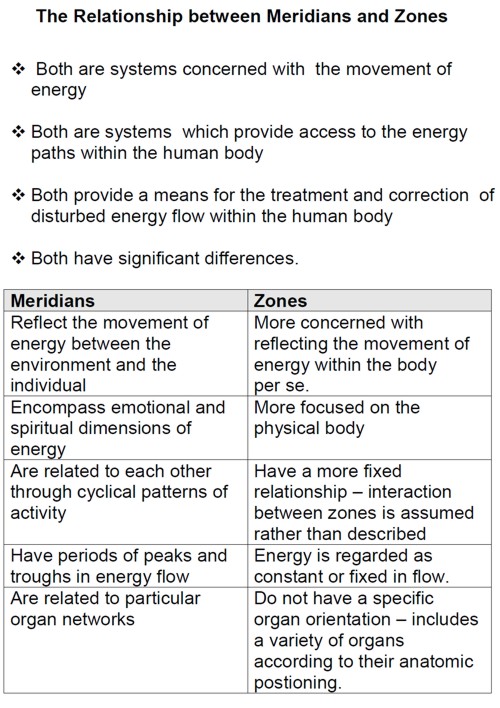
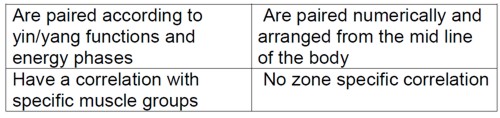
This is partly old, partly quite new. It is all preposterous made-up nonsense. There isn’t the slightest reason to think that "zones" or "meridians" exist. In fact there is good evidence from acupuncture studies to think that they don’t exist.
Now some slides from course CPT08102. The mention of the word ‘energy’ in the alternative world always rings alarm bells. Here’s why.
Well, it’s a good question. Pity about the answer.
Shouldn’t that read "as a practising reflexologist it is important than you have a MISunderstanding of the energy that surrounds us"?.
![]()
What logic? Have these people never heard of Hodgkin & Huxley (the answer, I imagine, is no)?
The mention of Kim Jobst immediately raises suspicions. He is a homeopath and endorser of the obviously fraudulent Q-link
pendant.
"when you as a reflexologist palpate the foot you not only produce the physical responses in the CNS but also enter the energetic body and move energy , , ". Well, no you don’t. This is purely made-up nonsense. The words sound "sciencey" but the meaning of the words is utterly obscure.
Yes we do live in an interconnected world. And sadly, that interconnectedness is used to spread myth and misinformation, usually with the aim of making money.
I guess Edinburgh Napier University makes money by teaching ancient myths as though they were true. In so doing they destroy their academic reputation.
Here you are tested to see how much nonsense you have memorised successfully. If only they had sent ‘model answers’.
Remember, these pre-scientific myths are not being taught as history or anthropology. They are taught as though they were true, to students who are then let loose on patients, so they can make money from anyone who is gullible enough to believe what they say.
A 2009 systematic review of randomised controlled trials concludes that “The best evidence available to date does not demonstrate convincingly that reflexology is an effective treatment for any medical condition.”. So forget it.
How about it Professor Stringer? Isn’t it time to clean up your university?
Follow-up
|
Professor George Lewith is perhaps the most prominent advocate of alternative medicine within quackademia, at least in Russell Group University. He claims to be a member of “The Complementary and Integrated Medicine Research Unit is within the School of Medicine at the University of Southampton.”. |
The URL for this unit is actually http://www.cam-research-group.co.uk/. Strangely, though, a search of Southampton University’s own web site for “Complementary and Integrated Medicine Research Unit” yields very little information about this unit.
But Lewith does not spend all of his time on his academic duties. He also spends time in London at his private practice, at the Centre for Complementary and Integrated Medicine. This practice, I discovered in 2006, was selling to patients that well known method for misdiagnosing food intolerance, the Vega test. It was doing so despite the fact that Lewith himself had written a paper that concluded that the Vega machine does not work, The paper was in the British Medical Journal, 2001;322:131-4. It concludes “Electrodermal testing cannot be used to diagnose environmental allergies”. This history is recorded in Lewith’s private clinic has curious standards.
Dr Lewith was in the news again recently when he published a paper that showed (yet again) that homeopathic pills work no better than placebo. No surprise there of course. The paper has been described here, in Despite the spin, Lewith’s paper surely signals the end of homeopathy (again).
So we can congratulate Lewith for being one of the few members of the magic-medicine community to have published papers of reasonable quality that show that neither homeopathy nor the Vega test work. In fact there was nothing novel in the conclusions about the Vega machine. It has been debunked again and again.
The BBC’s Inside Out programme in 2003 found that when the Vega test was taken in three different branches of Holland and Barrett, the results were quite different every time. The reporter was advised to by a total of 20 different supplements, but got different advice from every store.
In 2006, the test was destroyed again in, of all places, the Daily Mail which published ‘The great allergy con‘.
In 2011, BBC’s Watchdog programme looked again at food intolerance tests, with results as crazy as before. Holland & Barrett said “In light of this report, however, we have instructed The UK Health Partnership to investigate the findings and review their current training practices”. That’s odd, because in 2001 they had said “”In light of the issues raised, we are already carrying out a full review of the services that HSL provide.” So not much progress there.
What is rather more surprising is to find that Dr Lewith, having himself shown that neither the Vega test nor homeopathy work, continues to sell both to patients in his private practice.
I recently heard from a young student about her experiences when she went to Prof Lewith’s private practice. If you want to read her letter in full, download the pdf. Some quotations from it suffice to tell the tale.
“I had suffered from CFS/ME for nearly 8 years when on March 18th 2009 I had my first appointment with doctor Lewith”
“We talked for 7 to 10 minutes about my history and gave a very brief outline of my medical past. I did feel that this was a bit rushed”
“He said that he would treat me with a mixture of homeopathic medicine and conventional treatments and then hooked me up to a machine to determine any food intolerances.”
“He put me off all dairy products and said that he would send me some homeopathic remedies and food supplements”
“Having suffered with the illness for so long and having been involved with the conventional practices for treating ME with no relief I went to Dr Lewith desperate. I left this first consultation a little shocked at the rushed pace and a little wary of homeopathy but determined to carry on. ”
“I waited for my remedies in the post but only the food supplements and the blood test results arrived.”
“On April 8th 2009, I went back for my 30 minute follow up consultation. We talked briefly about how I was doing. Dr Lewith exclaimed that I looked so much better than last time and that the treatments that he had sent me had obviously worked. I assumed he meant the food supplements. It quickly transpired that he meant the homeopathic drops that I had never received. I suggested that I was probably better than last time because I was not recently recovering from tonsillitis. My confidence was immediately lost as I felt I was being coerced into thinking that the drugs he had provided were the reason for my recovery. Someone with knowledge of ME should be aware that a sufferer is not in a permanent state of ill health but generally that they follow what is known as ‘Boom and Bust’. I was going through a good patch, which after 8 years of being ill was the normal pattern. This was a maximum 5 minute conversation.”
“He hooked me up to the machine again still without any real explanation. ”
“I cancelled my next appointment with Dr Lewith having completely lost faith in his methods. I subsequently received two packages of drugs by post which I have returned. Neither at the consultation nor with the packages of drugs was there any explanation of what each drug was prescribed to achieve.”
“It was soon after that Lewith was chasing me for payment of the cancelled appointment and the homeopathic drugs that I had sent back. This was a total of £230. I had already spent nearly £300. I refused to pay as I did not feel that I had received the proper medical care that is expected of a GP.”
“He threatened to lay a claim against me at the small claims court.”
“I submitted both a Defence and Counterclaim to his action against me.”
“We went to court yesterday [January 17 2011] where Dr Lewith did not attend. ”
“He failed to submit witness statements and a Defence to my Counterclaim. The judge struck the case off and my costs awarded against Dr Lewith.”
“Conventional medicine had not been successful in helping me with ME and at 20 years old and at university I was desperate for a cure. I feel that complementary medicine takes advantage of people in my situation – I witnessed extortionate fees, blatant coercion to believe that it was working and blasé professionalism”
In response to a subsequent enquiry, the student told me
“He never told me what the homeopathic drugs were or what they were meant to do. When I received them I sent them straight back.”
“I am pretty sure that I was given general vitamins and minerals and some magnesium (if that makes sense?)”
|
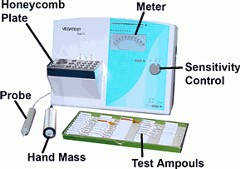 A Vega machine |
The student also paid £85 for an ATP metabolism test, done by Acumen, a private company run by Dr John McLaren-Howard. This test allegedly found defects in ATP metabolism on the basis of which the student was charged £91.91 for CoQ10 tablets. Neither the test, nor CoQ10, have any verified usefulness for her condition.
Here’s the bill for the homeopathic pills prescribed by Lewith.
These are the facts. Make of them what you will. At a cost of over £500, no good was done.
It isn’t surprising that Lewith’s claim was dismissed by the court.
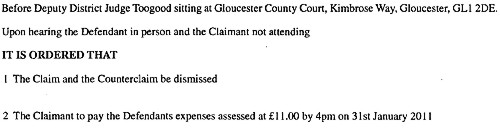
The College of Medicine
We notice that Professor Lewith plays is vice-chair of the “College of Medicine” that has arisen from the ashes of the Prince’s Foundation for Integrated Health (for more details see Don’t be deceived. The new “College of Medicine” is a fraud and delusion). That organisation is supposed to be devoted to “patient-centered medicine”. The reader can judge whether the case related here is a good example.
It is often said that one reason that people go to alternative practitioners is because real medicine can do nothing for them. That, only too often, is the case. People get desperate and clutch at straws. That is bad enough even in cases where the alternative practitioner believes sincerely, if wrongly, that their treatments work.
For the alternative practitioner to prescribe things which he knows full well don’t work, is, perhaps, rather worse.
Follow-up
Just as this post was about to go up, George Lewith popped up again in a BCC piece about how expectations affect the perception of pain (something that has been known for years). Lewith is quoted as saying “It completely blows cold randomised clinical trials, which don’t take into account expectation.” This comment shows a total misunderstand of how a randomised trial works. It is all explained properly by Majikthyse, in The wrong end of the stick
Just for fun, here is a discussion that I had with Lewith on Channel 4 News, as edited (not by me) for YouTube.
The long-awaited government decision concerning statutory regulation of herbalists, traditional Chinese medicine (TCM) and acupuncture came out today.
Get the Department of Health (DH) report [pdf]
It is not good news. They have opted for statutory regulation by the Health Professions Council (HPC). This is much what was recommended by the disgraceful Pittilo report, about which I wrote a commentary in the Times (or free version here), and A very bad report: gamma minus for the vice-chancellor.
The DH report is merely an analysis of responses to the consultation, but the MHRA says
"The Health Professions Council (HPC) has now been asked to establish a statutory register for practitioners supplying unlicensed herbal medicines. The proposal is, following creation of this register, to make use of a derogation in European medicines legislation (Article 5 (1) of Directive 2001/83/EC) that allows national arrangements to permit those designated as “authorised healthcare professionals” to commission unlicensed medicines to meet the special needs of their patients."
The MHRA points out that this started 11 years ago with the publication of the House of Lords report (2000). Both that report, and the government’s response to it, set the following priorities. Both state clearly
“… we recommend that three important questions should be addressed in the following order . .
- (1) does the treatment offer therapeutic benefits greater than placebo?
- (2) is the treatment safe?
- (3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?
The report of DH and the MHRA’s response have ignored totally two of these three requirements. There is no consideration whatsoever of whether treatments work better than placebo (point one) and there is no consideration whatsoever of cost-effectiveness (point 3). These two important recommendations in the Houss of Lords report have simply been brushed under the carpet.
Needless to say, herbalists are head over heels with joy at this sign of official endorsement (here is one reaction)
Here are my first reactions. The post will be updated soon.
The DH report is, in a sense, democratic. They have simply counted the responses, for and against each proposal. They seem to be quite unaware that most of the responses come from High Street herbailsts whose main aim is to gain respectability. The response of the Academy of Royal Medical Colleges counts as one vote, just the same as the owner of a Chinese medicine shop. This is not how health policy should be determined. Some intervention of the brain is needed, but that isn’t apparent in the report.
At present the HPC regulates Arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dietitians, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, prosthetists/orthotists, radiographers and speech & language therapists. I shudder to think what all these good people will think about being lumped together with people who practice evidence-free medicine (or, worse, forms of medicine where there is good evidence that they don’t work).
The vast majority of herbalists, traditional Chinese medicine (TCM) and acupuncture has no good evidence that it works, In the case of soem herbal medicines and acupuncture, there is good evidence that they don’t work. Yet the HPC has, as one of its criteria, that aspiring to be regulated by them requires
"practise based on evidence of efficacy"
The Department of Health seems to have quietly forgotten about this criterion. It cannot possibly be met. The HPC has already expressed its willingness to go along with this two-faced approach (see Health Professions Council ignores its own rules: the result is nonsense )
Another mistake made by the Department of Health regards the value of "training". The report (page 11) says
Would statutory regulation lessen the risk of harm? (Q2)
Again, the vast majority of respondents thought it would. Reasons given were that statutory regulation would ensure that herbal practitioners and acupuncturists are carefully and thoroughly trained. That training is subject to accreditation, evaluation and periodic review by independent educational and training professionals, and disciplinary oversight by a regulating body. Incompetent or unscrupulous practitioners could be struck off the register and prevented from practising.
Although it is pointed out to them in several responses, the Department of Health seems quite incapable of understanding a simple and obvious truth. Spending three years training people to learn things that are not true, safeguards nobody. On the contrary, it endangers the public. Training in nonsense is obviously a nonsense.
At the end of the report is a list of organisations who responded, As expected, they are predominantly trade bodies that have a vested interest in allowing thinks to be sold freely regardless of whether they work or not. The first four are Alliance of Herbal Medicine Practitioners. European herbal and Traditional Medicine Practitioners Association (ETMPA), Association Chinese Medicine Practitioners (UK) (ACMP) and Acupuncture Society. And so on.
More coming soon.
Follow-up
16 February 2011. Later the same day, we see one reason why Michael Mcintyre, chair of the European Herbal Practitioners Association, got what he wanted to promote his trade. They had evidently hired a PR Agency, Cogitamus, to push their case. Now they are crowing about their victory. And of course his profits were not harmed by the free publicity that was given to his cause by the BBC,
The pinheads in the Department of Health are more easily persuaded by a PR agency than by any number of people who know a lot more about it, and who have no profit motive.
17 February 2011.
The herbal problem was front page news in the London free paper, the Metro: Chinese medicine and herbal ban to see Britain defy EU laws
The Daily Telegraph covered the story: Herbal medicine to be regulated, says Andrew Lansley. The comments featured some pretty mad rants from herbalists, to which I tried to reply.
The Metro article elicited a fine bit of abuse from a Lynda Kane. I’m constantly amazed at the downright viciousness of cuddly holistic therapists when they get found out. I guess it is just another bad case of cognitive dissonance. I can’t resist a few quotations.
Sir,
“I have just come across your asinine comments quoted in the London Metro newspaper re the EU herbal medicine directive. For a supposed scientist your mis-informed, closed-minded, unsubstantiated bigotry leaves me speechless”
“As a scientist myself, I abide by the virtues of open-minded neutrality and accepting the hypothesis until proven otherwise by null-hypothesis based research.”
“How many of the innumerable studies on the efficacy of herbal medicine have you read? “
“Perhaps in your ‘day’ professors could say whatever they liked and be listened to. That day is long gone, as you must know from the various law-suits you have been party to.”
I love the idea that statistics allow you to accept any hypothesis whatsoever until someone shows it to be wrong.
This would be funny if it were not so sad (and rather painful). As always I replied politely and referred her to NCCAM’s Guide to Herbs, so she can check up on that plethora of evidence that she seems to think exists.
This is Lynda Kane of energyawareness.org. I can recommend her web site, if you want some truly jaw-dropping woo. She’ll sell you a “White Jade Energy Egg – may provide up to 5 times as much protection from wifi and from other peoples’ energies – costs £47.00”. Hmm, sounds good. How does it work? Easy.
“The human energy or “qi” field is shaped like an egg. It is being attacked by many forms of natural and man-made environmental stress 24 hours a day.”
I guess that’s OK according to Ms Kane’s interpretation of statistics which allows you to accept any hypothesis whatsoever until someone shows it to be wrong.
Anyone for Trading Standards or the ASA?
17 February 2011. The excellent Andy Lewis has posted on similar problems “How to Spot Bad Regulation of Alternative Medicine“
.20 July 2013
Nothing visible happened after this announcement. Until the government’s resident medical loon, David Tredinnick MP forced a debate on the matter. His introduction to the debate was his usual make-believe. Sadly it made much of an exhibit at the Royal Society Summer Science exhibition -a bit of bait and swich by aromatherapists.
After ploughing your way through pages of nonsense, you get to the interesting bit. At 10.38 am, The Parliamentary Under-Secretary of State for Health, Dr Daniel Poulter, announced what was happening. It seems that there may, after all, have been some effect of all the sensible submissions which pointed out the impossibility of regulating nonsense. The question of regulation has, yet again, been postponed.
"To ensure that we take forward the matter effectively, we want to bring together experts and interested parties from all sides of the debate to form a working group that will gather evidence and consider all the viable options in more detail,"
One wonders who will be on this working group? If they don’t choose the right people, it could be as bad as the Pittilo report. It wasn’t reassuring to read
" we want to set up a working group and to work with my hon. Friend [Tredinnick], and herbalists and others, to ensure that the legislation is fit for purpose."
|
The Science Museum is a wonderful place. As a child it seemed magical. So all the more disappointing to find that it houses an exhibition that promotes quackery. The exhibition is uncritical and sometimes downright dangerous. It does not teach you anything about science, it teaches anti-science and uncritical thinking. It was not originally like this. Most of the objects in the exhibition were originally part of Henry Wellcome’s Wellcome Museum of Medical History, based at 183 Euston Road. It was moved on permanent loan to the Science Museum in 1977 where it was known as The Wellcome Museum of the History of Medicine. |
|
Recently the Wellcome-Trust sponsored exhibition was the subject of a blog post at Purely a figment of your imagination, written by Alex Davenport. That reminded me that last June I was sent a lot of pictures of the exhibition but never got round to finishing writing them up. Here, somewhat tardily, is some of what I got.
It seems that the Wellcome Trust is not to blame, The free advertising for quacks was something added to the Wellcome collection by the Science Museum itself.
At the time, I wrote to the Science Museum to find out what was going on. The response was very disappointing, merely bland PR stuff. I was told that the person responsible for the display was Lisa O’Sullivan, Senior Curator of Medicine, but she was on sabbatical, so no response from her.
The clue to what went wrong came in a letter from Dr. Tim Boon, the Science Museum’s Chief Curator. The letter was relayed via the Museum’s Press Officer. A subsequent letter to Boon himself was not answered.
"Therefore, in addition to the overwhelming majority of the Upper Wellcome gallery that tells the story of the history of Western medicine since the rise of Civilisation up to the modern era, we devote a small section to these more anthropological concerns in our display called ‘Living Medical Traditions’.
Our message in this display is that these traditions are not ‘alternative’ systems in some parts of the world. Instead they are often the only choice of medical care to those communities. We do not make any claims for the validity of these traditions. For example, we include the use of acupuncture but do not say that acupuncture ‘works’. "
Unfortunately this is really not true: the tone is very much that it does work. The reason is clear in the next paragraph.
"As with all Science Museum galleries independent experts were consulted when developing this gallery. In this instance advice was sought from leading academics in the history of non-western medical traditions as well as practitioners and users of these traditions. We maintained editorial control throughout.”
Aha they asked "experts", but of course it is always possible to find some ‘expert’ to advocate any view, however barmy. The only experts that were consulted, we are told, is historians and practitioners of anti-scientific medicine. No scientists. Clearly the Museum allowed the quacks to write their own script, with no supervision from anyone who understands the science, It is meant to be a Science Museum, not a museum of anthropology.
The nonsense of quack medicine provides an excellent opportunity to explain simply how science tries to separate truth from falsehood. The Museum has not only missed that opportunity but it has actively promoted anti-science.
The Museum declined to name these mystery experts, but one of them is revealed in the 2006 newsletter of the British Medical Acupuncture Society [download the newsletter]. An article by Jonathan Freedman shows the delight of acupuncturists.
"The BMAS were approached by the Museum last Summer and asked if any members would be able to contribute a case study about acupuncture to feature in the ‘personal stories’ section of the exhibition."
"I think the final product has worked extremely well and shows Western Medical Acupuncture in a positive light. A selection of needles is displayed along with the BMAS leaflet and my own practice acupuncture leaflet."
In fact the Science Museum’s good name is used by Freedman to advertise his private practice.
Here is the free advertising in the Science Museum.
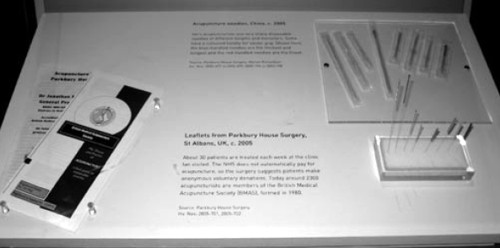
Traditional Chinese Medicine
There is plenty of this and it is totally uncritical. All it does is repeat the gobbledygook used by practitioners. In fact it was largely written by them.
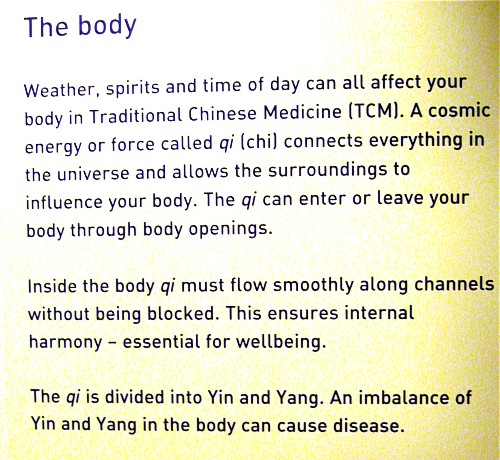
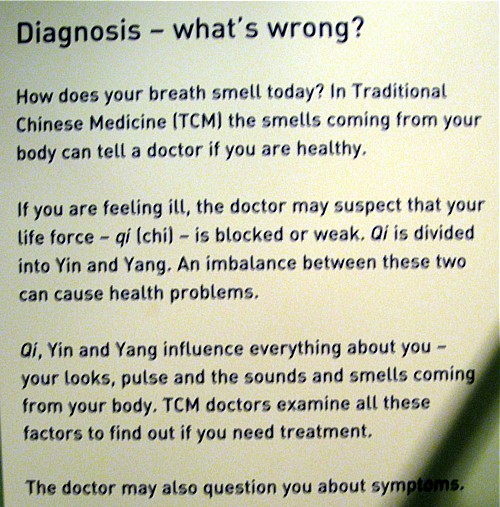
There are recorded commercials too. Listen to this one.
Advertising for cupping at the Asanté Clinic.
In the recording, Dr Ke diagnoses an asthma patient as having mucus in the lungs -by looking at his tongue (no kidding) -and recommends cupping. He says
“We need to clear this mucus, or the phlegm, in the chest by using cupping, It’s improving, sort of, the flow of the water, and flow out, in other words, suck out the badness from the body”
This, needless to say, is total rubbish.
The recording took place at the Asanté Clinic, on the Archway campus of the University of Middlesex. Ah yes, Middlesex. Take a look at ‘More quackedemia. Dangerous Chinese medicine taught at Middlesex University‘.
Unani medicine, Another advertisement for a private clinic.
|
|
|
Listen to a diagnosis being made by looking at the iris.
Iridology is, of course, total bunk Just one of the many phoney methods of diagnosis used by alternative practitioners, as an aid to selling you an expensive treatment.
Ayervedic medicine
Listen to another advertisement, for private Ayurveda clinic
The display that accompanies the recording is totally uninformative. The practitioners have been allowed to advertise their wares with no trace of critical thought. No trace of science.
|
|
|
|
|
|
|
|
|
The power of blogs
I guess this incident is yet another example of the power of blogs. My own letters to the science museum produced precisely nothing, as is usually the case if you go through the “proper channels”. Alex Davenport’s blog,on the other hand, stung the Science Museum into a public response. It’s true that the response is much the same as the patronising PR junk that was sent to me last year, though it was labelled as being by Susannah Shute, Web Content Coordinator. The response even linked to a picture of the homeopathy exhibit.
It seems a bit more pressure is needed to persuade the museum to change this particular exhibition into science, rather than its present anti-science.
Follow-up
13 April 2011. Simon Singh arranged a meeting with the new director of the Science Museum, Ian Blatchford, and deputy director Heather Mayfield Our deputation consisted of Simon Singh, Alex Davenport, Marianne Baker and me. It was Alex’s blog on the science museum exhibit, and my post on the museum which followed it shortly, that caused the meeting. Alex had a follow-up blog too. I hadn’t realised that Simon had resigned as a trustee of the museum five years ago, in protest about the (dreadful) alternative medicine exhibit. I had various stonewalling responses to my attempts to pursue the matter out of the limelight, so eventually went public. After the blogs appeared, the Science Museum published a response which was, sadly, entirely vacuous. We had an excellent discussion, during which Ian Blatchford said he regretted the official response and changes to the exhibit are promised. there is an account of the meeting here.
We were sent a revised version, which was improved, but not, we said improved enough.
10 May 2011. Got an email from the person who originally brought the problem to my attention.
“Visited Science museum yesterday , wonderful news – all offensive material gone, and different ok stuff there”.
Well done, Science Museum.

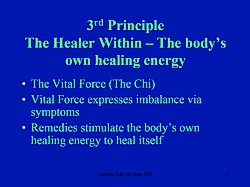
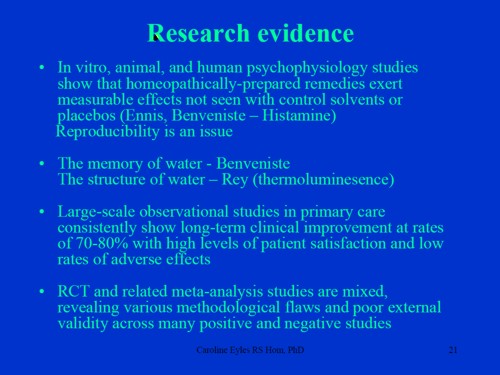
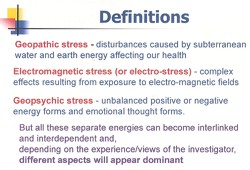
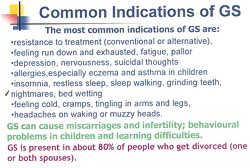
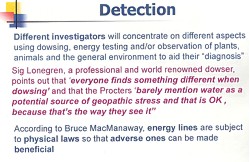
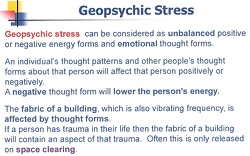
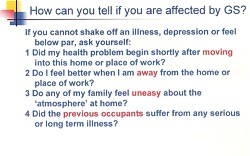

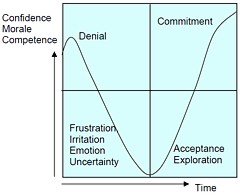



 >
>